Abstract
Background
Because treatment options for coronavirus disease 2019 (COVID-19) are very limited, the use of convalescent plasma has bee explored.
Case presentation and treatment
A male centenarian with cough and dyspnea for 2 months was diagnosed with COVID-19. Without effective treatments and with the increased risks of antiviral therapy for the elderly, this patient was given convalescent plasma. The viral load, complete blood count, inflammatory indicators, vital signs, and clinical symptoms were observed before and after COVID-19 convalescent plasma transfusion.
Results
After convalescent plasma transfusion, significant improvement was observed on laboratory indicators and clinical symptoms of the patient. Concurrently, SARS-CoV-2 viral load decreased sharply after the first transfusion (from 2.55 × 104 to 1.39 × 103 copies/mL) and became undetectable after the second transfusion.
Conclusions
With the substantial increase of COVID-19 in recent months,treatment for elderly patients has become restricted in some countries. The successful treatment of this 100-year-old patient using convalescent plasma suggests that we should consider adding convalescent plasma in th management of the elderly.
Keywords: Coronavirus Disease 2019, convalescent plasma, transfusion
1. Introduction
Since the end of December 2019, an acute pneumonia identified as COVID-19 has becoming a global epidemic. Senior patients are at high risk of COVID-19 and have a high mortality rate due to their decreased immunity [1], some countries even began to adopt strategies that abandon treatment for elder patients since the limited medical resources. However, antiviral effects of convalescent plasma may provide potential treatment for elder patients. Here we reported a case of successful treatment of a 100-year-old male COVID-19 patient with convalescent plasma.
2. Case Presentation
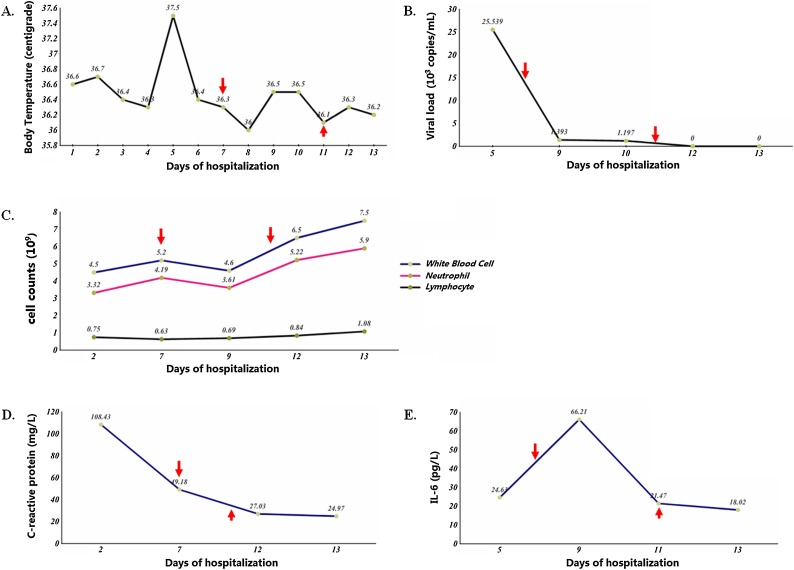
A 100-year-old male with a persistent cough, difficulty expectorating, and dyspnea for 2 months was admitted to a tertiary hospital due to COVID-19 in Wuhan, Hubei province in Feb 2020. The patient was a local resident and had no obvious exposure to COVID-19. Initially, he received supportive care at a local geriatric hospital in December 2019. After receiving symptomatic treatment for one week to reduce his cough, the patient continued to suffer from shortness of breath. Two months later, in Feb 2020, the real-time PCR (RT-PCR) test for COVID-19 was performed for the patient at a community health center, and this test yielded a positive result. He was then admitted to a tertiary hospital in Wuhan. The patient had a significant past medical history, including a 30-year record of hypertension, abdominal aortic aneurysm, cerebral infarction, prostate hyperplasia, and complete loss of cognitive function for the preceding 3 years. Upon his hospital admission due to the COVID-19 diagnosis, the patient had stable vital signs, with a body temperature of 36.6 ℃ (Fig. 1 A), pulse of 87 beats/min, respiratory rate of 18 beats/min, blood pressure of 125/63 mmHg, and oxygen saturation of 98% on room air. He had the following laboratory findings: red blood cell and lymphocyte counts were relatively low at 3.47 × 1012/L and 0.75 × 109/L, respectively, whereas white blood cell, neutrophil, and monocyte counts were within the normal range, at 4.5 × 109/L, 3.32 × 109/L, and 0.37 × 109/L, respectively. C-reactive protein was elevated at 108.43 mg/L. His fibrinogen level was 5.88 g/L, D-dimer was 2.63 mg/L, and other coagulation test results were normal. Liver functions were normal with alanine aminotransferase (ALT) and aspartate aminotransferase (AST) at 34.2U/L and 23.8U/L, respectively. A chest radiograph obtained upon admission showed slight patchy and cord-like dense enhancements in both lungs and bronchovascular bundle thickening.
Fig. 1.
Clinical indicators of the patient during admission.
(A) The body temperature of the patient during admission. (B) The viral load of the patient during admission. (C) The absolute value of white blood cell, neutrophil and lymphocyte of the patient during admission. (D) The concentration of C-reactive protein of the patient during admission. (E) The concentration of IL-6 of the patient during admission.
Arrows show the times when convalescent plasma was transfused.
Following admission, the patient was given high-flow oxygen, nutritional support, and symptomatic treatment. Due to the patient’s advanced age and increased risk for drug-induced toxicity, antiviral medications were not administered at that time. On day 5 of hospitalization, he had a relatively high SARS-CoV-2 viral load (2.55 × 104 copies/mL) by quantitative RT-PCR from a nasopharyngeal swab (Fig. 1B). Because the patient was not suitable for antiviral treatment and there was no other effective therapy, the clinical team recommended that the patient receive convalescent plasma. Convalescent plasma was collected via plasmapheresis from a donor who had recovered from COVID-19 for more than two weeks and had a SARS-CoV-2 S-RBD-specific IgG titer of >1:640. The patient received convalescent plasma twice from the same donor: 200 ml at 9:45 p.m. on the seventh day of hospitalization and 100 ml at 6:50 p.m. on the eleventh day of hospitalization. After convalescent plasma transfusions, the levels of white blood cells and neutrophils fluctuated but eventually stabilized within the normal range. The absolute lymphocyte counts had a downward trend from the time of admission (from 0.75 × 109/L to 0.63 × 109/L) but increased after the transfusions of convalescent plasma, reaching 1.08 × 109/L at the time of discharge (Fig. 1C). C-reactive protein showed a downward trend after convalescent plasma infusion (Fig. 1D). IL-6 increased to 66.21 pg/ml after the first infusion of convalescent plasma but subsequently declined (Fig. 1E). Patient’s viral load decreased significantly, by a factor of approximately 18 (from 2.55 × 104 to 1.39 × 103 copies/mL), 24 hours after the first transfusion of convalescent plasma. Following the initial convalescent plasma transfusion, the patient also received antiviral treatment with the traditional Chinese medicine, but no significant decline in viral load was observed 24 hours after the treatment (from 1.39 × 103 to 1.20 × 103 copies/mL). As a result, a second transfusion of convalescent plasma was given to the patient, and then the viral load became undetectable (Fig. 1B). The patient had additional viral load testing on days 12 and 13 of hospitalization, with both days producing negative results, and he was discharged on day 13 of hospitalization. At the time of discharge, the patient had stable vital signs, with significant improvement in his cough and dyspnea. Given the age of the patient and his relatively minor lung changes at presentation, a chest radiograph was not repeated at discharge.
3. Discussion
COVID-19 presentations are mainly characterized by fever, fatigue, dry cough, and dyspnea [2]. Sustained reduction of peripheral blood lymphocytes and continuous increases of inflammatory factors can lead to adverse treatment outcomes for patients due to cytokine storm syndrome. Most elderly patients with COVID-19 develop advanced pneumonia and require ICU monitoring as a result of organ failure and declined immunity [3]. Moreover, senior patients have a high mortality rate. The patient in our report is an elderly man with multiple co-morbidities. Interestingly, he had a mild presentation with a persistent and prolonged course of COVID-19. He had respiratory symptoms but no obvious fever, although there was some temperature fluctuation (Fig. 1A), which may be attributable to his advanced age and decreased immunity. Fortunately, this 100-year-old man tolerated the transfusion of convalescent plasma in addition to the standard treatments and achieved good therapeutic outcomes.
The therapeutic effect of convalescent plasma is most likely realized through the antiviral activity of neutralizing antibodies, but patients may also experience an immune response, which can lead to fluctuations in the level of inflammatory cells and factors [[4], [5]]. We did observe significant decreases in viral load after convalescent plasma transfusions, suggesting that convalescent plasma therapy may be a viable option for treating COVID-19. This result is consistent with the findings of other reports [[6], [7], [8]]. We also observed other changes, such as improved cell counts and decreased level of C-reactive protein, as previously reported [9]. The patient tolerated the transfusions well, although there was a transient increase of IL6 level.
Due to a drastic increase in the number of COVID-19 and limited medical resources, several countries have begun to limit or even deny treatments for elderly patients due to their shortened life expectancy and higher mortality rates from COVID-19 [10]. If, however, COVID-19 convalescent plasma is readily available and can be used to treat COVID-19 effectively and safely, its use should be considered in the management of older patients. In addition, untreated elderly patients with COVID-19 and with mild symptoms, such as the patient in our report, may represent a persistent infectious source; therefore, perhaps we should be more vigilant with our treatment decisions for elderly patients if a relatively inexpensive approach such as convalescent plasma is available.
Ethics and patient consent
Ethical approval was received from the Institute of blood transfusion, Chinese Academy of Medical Sciences and Peking Union Medical College (approval number: 202002). Informed consent was signed by a legal representative of the patient.
Declaration of Competing Interest
We declare no relevant conflicts of interest.
Funding sources
This work was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS) (Grant Nos. 2020-I2M-CoV19-006 and 2016-I2M-3-024) and Non-profit Central Research Institute Fund of Chinese Academy of Medical Sciences (Grant Nos. 2018PT32016).
CRediT authorship contribution statement
Yujie Kong: Data curation, Formal analysis, Writing - original draft. Chen Cai: Data curation, Formal analysis, Writing - original draft. Li Ling: Methodology, Data curation. Li Zeng: Data curation. Meihong Wu: Data curation. Yanyun Wu: Writing - review & editing. Wei Zhang: Conceptualization. Zhong Liu: Conceptualization.
References
- 1.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) — United States, February 12–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(12):343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan W.J., Ni Z.Y., Hu Y. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020 doi: 10.1056/NEJMoa2002032. [DOI] [Google Scholar]
- 3.Huang C., Wang Y., Li X. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garraud Olivier. Use of convalescent plasma in Ebola virus infection. Transfusion and apheresis science. 2017;56(1):31–34. doi: 10.1016/j.transci.2016.12.014. [DOI] [PubMed] [Google Scholar]
- 5.Choi S., Kim Mc, Kwon Js. Case Report: Use of Plasma Exchange Followed by Convalescent Plasma Therapy in a Critically Ill Patient with Severe Fever and Thrombocytopenia Syndrome–Associated Encephalopathy: Cytokine/Chemokine Concentrations, Viral Loads, and Antibody Responses. Am J Trop Med Hyg. 2018;99(6):1466–1468. doi: 10.4269/ajtmh.17-0766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mair-Jenkins J., Saavedra-Campos M., Baillie J.K. The effectiveness of convalescent plasma and hyperimmune immunoglobulin for the treatment of severe acute respiratory infections of viral etiology: a systematic review and exploratory meta-analysis. J Infect Dis. 2015;211(1):80–90. doi: 10.1093/infdis/jiu396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Van Griensven J., Edwards T., Gallian P. Convalescent Plasma for Ebola Virus Disease. N Engl J Med. 2016;374(25):2500. doi: 10.1056/NEJMc1602284. [DOI] [PubMed] [Google Scholar]
- 8.Chen L., Xiong J., Bao L. Convalescent plasma as a potential therapy for COVID-19. Lancet Infect Dis. 2020;20(4):398–400. doi: 10.1016/S1473-3099(20)30141-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hui D.S., Lee N., Chan P.K. Adjunctive therapies and immunomodulatory agents in the management of severe influenza. Antiviral Research. 2013;98(3):410–416. doi: 10.1016/j.antiviral.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lisa Rosenbaum M.D. Facing Covid-19 in Italy — Ethics, Logistics, and Therapeutics on the Epidemic’s Front Line. N Engl J Med. 2020 doi: 10.1056/NEJMp2005492. [DOI] [PubMed] [Google Scholar]