Abstract
Anxiety and depression are commonly found in patients with diabetes, but little is known about how the anxiety and depression symptoms of diabetes patients and the health-related quality of life (HRQoL) over time influence each other. Therefore, we conducted a survey among patients with diabetes (T1) and repeated the survey after 3 months (T2). Linear regression models and cross-lagged structural equation models were used to analyze the associations between anxiety and depression symptoms and HRQoL within and across time intervals. Correcting for baseline index and potential confounders, the HRQoL index at T2 reflected the change in anxiety/depression between T1 and T2 more than anxiety/depression at T1 (P < 0.05). Similarly, anxiety and depression at T2 reflected the change in the EQ-5D index over time more than the index at baseline (P < 0.05). Our longitudinal data fitted well in a cross-lagged model with bi-directional pathways of associations between anxiety and HRQoL, as well as depression and HRQoL, among adult patients with diabetes (x2/df = 1.102, P = 0.256; CFI = 1.000, RMSEA = 0.030). Our findings support early detection of anxiety and depression, as well as comprehensive efforts improving HRQoL for patients with diabetes.
Subject terms: Depression, Preventive medicine, Epidemiology, Outcomes research, Preclinical research
Introduction
Diabetes is an increasing health problem, especially in Western countries1,2. In 2000, the global prevalence of diabetes for all age groups was estimated at 2.8% whereas the expected prevalence in 2030 is 4.4%1. In recent years, health-related quality of life (HRQoL) has become one of the major indicators for the health assessment of diabetes care. Improving diabetics’ HRQoL has been considered an important goal of prevention and treatment. HRQoL incorporates physical, psychological and social functioning dimensions3. Despite a growing understanding of clinical and laboratory measures to improve HRQoL for diabetes patients4,5, few attempts have been made to rigorously study the relationship between HRQoL and psychological factors, like symptoms of anxiety and depression, in diabetes care.
Anxiety and depression commonly exist and affect patients with diabetes2,6–10. A previous meta-analyses on the prevalence of depression in adults with diabetes concluded that the likelihood of depression among people with diabetes doubles those among a general population without diabetes7. Furthermore, evidence shows that symptoms of anxiety and depression often remain unrecognized in diabetes care11. Anxiety and depression may influence how people assess their objective health status, and impact the course of diabetes such as poor glycemic control and medication non-compliance12. Also, given anxiety and/or depression is an important domain of the broad concept of HRQoL13, it’s easily understandable that the co-occurrence of anxiety and/or depression in patients with diabetics may be associated with a lower HRQoL compared to patients without the co-occurrence of anxiety and depression.
In spite of demonstrating the negative association between anxiety/depression and HRQoL in diabetes care, most previous studies that have been performed on the association had used a cross-sectional design and it’s impossible to determine the casual relationship due to the cross-sectional nature of the studies12. As a result, there is little evidence that supports the relationships between anxiety/depression symptoms and HRQoL over time, not to mention relationships taking into account variation among different clinic and demographic subgroups of diabetes patients. In addition, recent studies suggest that depression is bi-directionally associated with several determinants of HRQoL in diabetes care, such as obesity14, metabolic syndrome15, sexual dysfunction16, and severe hypoglycemic and hyperglycemic events17, however, to date it’s unknown whether or not anxiety/depression is bi-directionally associated with the overall HRQoL of diabetes.
Longitudinal data are necessary in order to assess the effect of anxiety/depression on HRQoL over time, or vice versa. The hypothesis in this study is that anxiety and depression are associated bi-directionally with HRQoL of diabetes in time. This would suggest a synchronous association between changes in anxiety/depression and HRQoL in diabetes care, which is perhaps similar to the relationship between fatigue and pain in primary care18. For example, current HRQoL of diabetes may directly predict anxiety and depressive symptoms in the future. Alternatively, anxiety and depression symptoms may be a consequence of experiencing different HRQoL in diabetes care over time.
This study aims to explore the prevalence of anxiety and depression symptoms and HRQoL in adult patients with diabetes in the Netherlands, and to assess associations between anxiety/depression and HRQoL in time, taking into account adult patients with different demographic and diabetes characteristics. Past evidence has shown that anxiety and depression are remarkably different having distinctive risks, patterns, and familial associations19. We therefore investigate the co-occurrence of anxiety and depression symptoms in diabetes patients separately in this study.
Methods
This is a prospective observational study, and it is part of an implementation study of screening and treatment of depression in diabetes patients following the guidelines at the Erasmus MC, University Medical Center Rotterdam in the Netherlands. The measurements involve digital questionnaires that were administered at baseline (T1) and 3 months’ follow-up (T2). During the preparation phase, the participating healthcare workers received training from the research team, including instructions on study logistics, use of the online screening program, interpretation of scores, discussion of outcomes and advising on referral to a psychologist if indicated. Study data were transferred and saved at the central database of the medical center throughout the project. The study protocol was approved by the ethics committee at the Erasmus University Medical Center Rotterdam and informed consent was obtained from all participants. All methods were performed in accordance with the relevant guidelines and regulations.
Patients
Adults (aged >18 years) who were diagnosed with type 1 or type 2 diabetes and visited the diabetes outpatient clinic of the hospital from November 2016 to March 2017 were invited for participation in an online survey, after completing a screening program for detecting their risk of depression. The implementation of the screening program followed Dutch National Guidelines20 and consisted of two components: a self-administrative anxiety and depression risk assessment, followed by a personal interview of patients who were assessed with risks for anxiety and/or depression. Those who indicated having difficulties to complete the online survey, due to reasons including no computer access, insufficient computer skills, language barriers and cognitive problems, were assisted by trained nurses with tablets onsite. Patients who completed the online survey received an email with a link after 3 months, asking them to repeat the survey.
Measures
The self-administered digital questionnaire at T1 and T2 included the following aspects.
Demographic and diabetes characteristic
Patients were asked about their gender, age, type of diabetes, years living with diabetes, employment status, education background, and the country of birth of themselves and their parents. Individuals were defined as ethnicity of majority if both of their parents were born in the Netherlands; ethnicity of minority if he/she was born abroad and at least one of the parents was born abroad (1st generation), or if he/she was born in the Netherlands with at least one of the parents born abroad (2nd generation)21.
Anxiety and depression
The validated Dutch version of the Hospital Anxiety and Depression Scale (HADS) was used to detect anxiety and depression symptoms in diabetes patients22. This scale has been validated in many countries and its capacity to detect anxiety and depressive disorders is widely recognized23. It consists of 14 items, seven of which relate to anxiety symptoms and seven to depressive symptoms. Each item was scored from 0 to 3, therefore participants can score between 0 to 21 for either anxiety or depression. Scores at the anxiety subscale (HADS-A) and depression subscale (HADS-D) were measured as continuous variables in this study, except for the prevalence of anxiety and depression symptoms. We defined a score of 8 or more on either HADS-A or HADS-D to identify DSM-III anxiety and depression symptoms as suggested by Bjelland and colleagues24.
Health-related quality of life
The validated Dutch version of the five-level EuroQol five-dimensional questionnaire (EQ-5D-5L), developed by EuroQol Research Foundation, was applied to measure health-related quality of life (HRQoL) on five dimensions, i.e. mobility, self-care, usual activities, pain/discomfort and anxiety/depression25. Additionally, cognitive functioning was added as a sixth dimension to the five existing dimensions (EQ-5D + C)26,27. Each dimension included five severity levels, i.e. no problems, some problems, moderate problems, severe problems, and extreme problems. Furthermore, the EQ visual analogue scale (VAS) was used to measure respondent’s self-rated health. The score ranges from 0 to 100, indicating the “the worst health you can imagine” to “the best health you can imagine”28. An EQ-5D summary index was calculated using scores at EQ-5D and the Dutch tariff established from the Dutch population13. All dimensions of EQ-5D + C were measured as categorical variables, while EQ VAS, EQ-5D summary index measured as continuous variables in this study.
Statistical analyses
Data were analyzed using IBM SPSS Statistics and AMOS version 24.0. Descriptive analyses were conducted for demographical and diabetes characteristics, anxiety and depression subscales (HADS), and all dimensions of the EQ-5D + C. Paired chi-square tests and one-way analysis of variance tests were performed to assess differences between T1 and T2 for those variables. Also, differences in diabetes EQ-5D were compared by identifying if a patient filled in a different level of problems on one or more dimensions at T2 compared to the T1. We investigated the longitudinal associations in three steps. First, we assessed the association between HADS and HRQoL at T1 and T2, respectively. The mean and its 95% confidence interval (CI) of HADS-A and HADS-D were calculated and mapped at each of the five severity levels for the dimensions with anxiety/depression dimension excluded. Univariate linear regression analyses were conducted and mapped using HADS-A and HADS-D scores separately to explain the variation at EQ-5D summary index and EQ VAS score within time intervals. Second, we assessed the association across time intervals in four linear regression models, predicting three outcomes at T2, i.e. EQ-5D summary index (Models 1 and 2), HADS-A (Model 3) and HADS-D (Model 4). In the Model 1 and 2, HADS-A/HADS-D at T1 and change in HADS-A/HADS-D between T1 and T2 were firstly added as main predicators separately, then EQ-5D summary index at T1 was adjusted; In the Model 3 and 4, EQ-5D summary index at T1 and change in the index were added as main predicators separately, then HADS-A/HADS-D at T1 was adjusted. We tested the full models by including both main predictors, outcome at T1, and demographical and diabetes characteristics as predicators. Finally, a cross-lagged panel structural equation modelling (SEM) was used to assess the longitudinal association among anxiety, depression and HRQoL (EQ-5D summary index) at T1 and T2. All variables were modeled as observed variables with error terms included to correct for external factors that may contribute to observed effects. We used a number of fit indices to evaluate the model: chi-square (Χ2)/degrees of freedom (df) of 2.00 or below, Comparative Fit Index (CFI) values of 0.90 or above, and root mean square error of approximation (RMSEA) values of 0.06 or below were used as standards of acceptable fit29.
Results
Demographic and diabetes characteristics
At T1, among 305 patients who completed the screening questions, 131 (42.9%) completed the survey for this study (Table 1). The respondents were aged from 23 to 81 years (mean: 54 years). The majority were male (50.4%), Dutch inhabitants (73.6%), living with type 2 diabetes (58.6%) for over 19 years, with a paid employment (43.2%) or social welfare (including retirement) (40%), had received education lower than the college level (71.5%). At T2, among 131 eligible respondents, 113 (86.3%) patients completed the second survey and 18 (13.7%) were lost to follow-up. No statistically significant differences were found regarding the demographic and diabetes characteristics between T1 and T2 (P > 0.05).
Table 1.
Demographic and diabetes characteristics of patients with diabetes at T1 and T2.
| T1 (n = 131) | T2 (n = 113) | P-value | |||||
|---|---|---|---|---|---|---|---|
| n | % | Mean (SD) | n | % | Mean (SD) | ||
| Gender | |||||||
| Male | 66 | 50.4 | 57 | 50.4 | 1.000 | ||
| Female | 65 | 49.6 | 56 | 49.6 | |||
| Diabetes type | |||||||
| Type 1 | 46 | 41.4 | 41 | 42.7 | 0.982 | ||
| Type 2 | 65 | 58.6 | 55 | 57.3 | |||
| Age (year) | 54.0 (13.1) | 54.4 (12.7) | 0.776 | ||||
| Duration of living with diabetes (year) | 19.4 (14.3) | 19.9 (14.7) | 0.807 | ||||
| Employment | |||||||
| Paid employment | 54 | 43.2 | 46 | 43.4 | 0.934 | ||
| Social welfare or retirement | 50 | 40.0 | 44 | 41.5 | |||
| Unemployment | 21 | 16.8 | 16 | 15.1 | |||
| Education level | |||||||
| Low (LTS, VMBO, MAVO, VMBO-t) | 54 | 41.5 | 47 | 42.0 | 0.910 | ||
| Intermediate (MTS, HBS, HAVO, VWO) | 39 | 30.0 | 31 | 27.7 | |||
| High (HBO, WO) | 37 | 28.5 | 34 | 30.4 | |||
| Ethnicity | |||||||
| Majority/no migrant | 95 | 73.6 | 87 | 78.4 | 0.566 | ||
| 1st generation migrant | 24 | 18.6 | 15 | 13.5 | |||
| 2nd generation migrant | 10 | 7.8 | 9 | 8.1 | |||
Note: LTS, lage technische school; VMBO, voorbereidend middelbaar beroepsonderwijs; MAVO, middelbaar algemeen voortgezet onderwijs; VMBO-t, voorbereidend middelbaar beroepsonderwijs-theoretical; MTS, middelbaar technische school; HBS, hoge burger school; HAVO, hoger algemeen voortgezet onderwijs; VWO, voorbereidend wetenschappelijk onderwijs; HBO, hoger beroeps opleiding; WO, wetenschappelijk onderwijs.
Prevalence of anxiety, depression and HRQoL
Of all respondents at T1 (Table 2), 36 (27.5%) had anxiety symptoms and 26 (19.8%) had depression symptoms. Twenty (15.3%) patients had both depression and anxiety symptoms. Regarding HRQoL, over half of the diabetes patients reported that they had experienced problems in usual activities (53.4%), pain (74.8%) and cognition (51.9%). The mean EQ VAS score was 70.1 (SD: 20.1) out of 100 (best health), the averaged EQ-5D summary index was 0.73 (SD: 0.27) out of 1 (best HRQoL). Among 113 respondents who filled out the survey both at T1 and T2, 61 (46.6%) reported less problems on the EQ-5D dimensions at T2 while 49 (37.4%) reported more problems on the EQ-5D dimensions at T2. No statistically significant differences were found between T1 and T2 regarding anxiety symptoms, depression symptoms, and all dimensions of HRQoL (P > 0.05).
Table 2.
Hospital Anxiety and Depression Scale (HADS) scores, percentage of reported problems on the European Quality of Life at 5 dimensions (EQ-5D) and extended cognitive dimension, the mean score of patients with diabetes for EQ-5D summary score and index and EQ visual analogue scale (VAS) at T1 and T2.
| T1 (n = 131) | T2 (n = 113) | P-value | |||||
|---|---|---|---|---|---|---|---|
| n | % | Mean (SD) | n | % | Mean (SD) | ||
| Anxiety and depression | |||||||
| HADS – Anxiety (0–21) | 5.81 (4.12) | 5.66 (4.20) | 0.778 | ||||
| Cut-off score:8 | 36 | 27.5 | 31 | 27.9 | 0.938 | ||
| HADS – Depression (0–21) | 4.64 (3.94) | 4.80 (4.33) | 0.763 | ||||
| Cut-off score:8 | 26 | 19.8 | 26 | 23.4 | 0.500 | ||
| EQ-5D-5L | |||||||
| Mobility | 1.76 (1.01) | 1.70 (0.97) | 0.678 | ||||
| No problem (1) | 73 | 55.7 | 63 | 56.8 | 0.897 | ||
| Problems (2–5) | 58 | 44.3 | 48 | 43.2 | |||
| Self-Care | 1.18 (0.58) | 1.15 (0.47) | 0.760 | ||||
| No problem (1) | 116 | 88.5 | 97 | 88.2 | 1.000 | ||
| Problems (2–5) | 15 | 11.5 | 13 | 11.8 | |||
| Usual activities | 1.92 (1.07) | 1.95 (1.01) | 0.773 | ||||
| No problem (1) | 61 | 46.6 | 46 | 41.4 | 0.439 | ||
| Problems (2–5) | 70 | 53.4 | 65 | 58.6 | |||
| Pain/discomfort | 2.24 (0.99) | 2.09 (0.92) | 0.219 | ||||
| No problem (1) | 33 | 25.2 | 32 | 29.1 | 0.561 | ||
| Problems (2–5) | 98 | 74.8 | 78 | 70.9 | |||
| Anxiety/depression | 1.69 (1.00) | 1.58 (0.79) | 0.339 | ||||
| No problem (1) | 76 | 58.0 | 64 | 58.2 | 1.000 | ||
| Problems (2–5) | 55 | 42.0 | 46 | 41.8 | |||
| Additional: Cognition | 1.72 (0.84) | 1.69 (0.75) | 0.798 | ||||
| No problem (1) | 63 | 48.1 | 50 | 45.5 | 0.699 | ||
| Problems (2–5) | 68 | 51.9 | 60 | 54.5 | |||
| EQ-5D Index (0–1) | 0.73 (0.27) | 0.77 (0.22) | 0.220 | ||||
| EQ VAS (0–100) | 70.1 (20.1) | 68.8 (21.5) | 0.631 | ||||
Negative association between anxiety/depression and HRQoL within time intervals
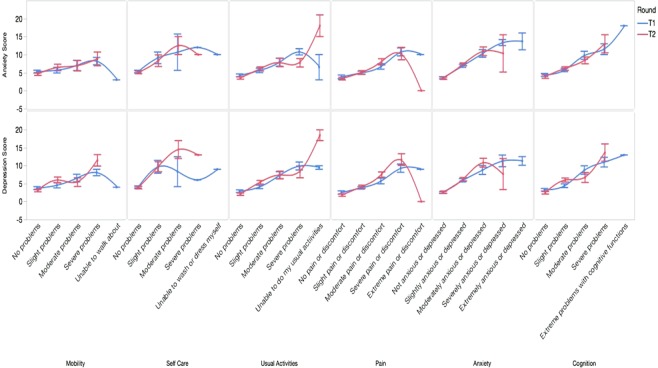
Fig. 1 shows that, within both time intervals, diabetes patients with a higher score in the anxiety subscale had experienced significantly more problems on all EQ-5D + C dimensions in general, i.e. mobility, self-care, usual activities, pain/discomfort and cognition (P < 0.05). However, respondents who had experienced extreme problems in mobility, self-care, usual activities and pain/discomfort reported fewer anxiety symptoms than those experienced moderate or severe problems (P < 0.05). The association between anxiety and all EQ-5D + C dimensions is similar to the association between depression and the EQ-5D + C dimensions within both time intervals, except for the non-linear association between depression and self-care at T1.
Figure 1.
The mean anxiety and depression subscale scores and its 95% confidence interval (CI) and the level of severity of problems (from left to right: weakest to strongest problems) for each of the EQ-5D dimensions and extended cognitive dimension at T1 and T2. Note: EQ-5D, the European Quality of Life at 5 dimensions.
Regarding overall HRQoL in diabetes patients, those with more anxiety symptoms had a significantly lower overall rate at EQ VAS at both T1 (P < 0.01; R2 = 0.27) and T2 (P < 0.01; R2 = 0.35). The linear regression models using depression score to predict EQ VAS rate are similar to using anxiety as predictor (R2 = 0.29 at T1; R2 = 0.50 at T2).
Effects of anxiety and depression on HRQoL over time, and vice versa
Table 3 shows that the EQ-5D summary index at T2 reflected the change in anxiety and depression symptoms between time intervals (B = −0.03) more than baseline anxiety (B = −0.01) and depression symptoms (B = −0.02). Both of the changes in anxiety and depression symptoms between T1 and T2, as well as depression at T1, significantly explained the EQ-5D summary index at T2 (P < 0.05), correcting for baseline EQ-5D summary index, patient’s demographic and diabetes characteristics in the Model 1 (R2 = 0.467) and Model 2 (R2 = 0.561). At univariate models: Patients who were living with diabetes type 1, employed, higher education background, and a majority ethnicity had significantly higher EQ-5D Index, thus better HRQoL (B > 0; P < 0.05). However, none of those characteristics were significantly associated with EQ-5D index in the multivariable models (P > 0.05).
Table 3.
Linear models of anxiety/depression at T1 and change in anxiety/depression over time predicting the EQ-5D summary index at T2 (Model 1 and 2); and of the EQ-5D summary index at T1 and change in the summary index over time predicting anxiety/depression at T2 (Model 3 and 4).
| Crude model | Adjusted model for baseline outcome * | Adjusted model for baseline outcome and confounders # | Adjusted R2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Β (SE) | P | Β (SE) | P | Β (SE) | P | ||||
| Outcome: EQ-5D Index at T2 | |||||||||
| Model 1 | Predictor | Anxiety at T1 | −0.03 (0.01) | <0.001 | 0.00 (0.01) | 0.949 | −0.01 (0.01) | 0.121 | 0.467 |
| Change in Anxiety | −0.01 (0.01) | 0.132 | −0.02 (0.01) | <0.001 | −0.03 (0.01) | <0.001 | |||
| Model 2 | Predictor | Depression at T1 | −0.03 (0.01) | <0.001 | 0.00 (0.01) | 0.477 | −0.02 (0.01) | 0.025 | 0.561 |
| Change in Depression | −0.02 (0.01) | 0.014 | −0.02 (0.00) | <0.001 | −0.03 (0.01) | <0.001 | |||
| Outcome: Anxiety at T2 | |||||||||
| Model 3 | Predictor | EQ-5D Index at T1 | −9.49 (1.35) | <0.001 | −1.55 (1.39) | 0.263 | −3.14 (1.74) | 0.072 | 0.707 |
| Change in EQ-5D Index | −0.04 (2.04) | 0.986 | −4.78 (1.36) | <0.001 | −6.50 (1.46) | <0.001 | |||
| Outcome: Depression at T2 | |||||||||
| Model 4 | Predictor | EQ-5D Index at T1 | −12.4 (1.19) | <0.001 | −6.65 (1.64) | <0.001 | −7.43 (1.87) | <0.001 | 0.720 |
| Change in EQ-5D Index | 0.52 (2.12) | 0.807 | −4.07 (1.51) | 0.007 | −7.24 (1.43) | <0.001 | |||
Note: B, standardized coefficient; SE, standard error; EQ-5D, the European Quality of Life at five dimensions; Higher score on EQ-5D index indicate better quality of life in mobility, self-care, usual activities, pain/discomfort and anxiety/depression, while higher scores on anxiety and depression subscales indicates more anxiety/depression symptoms. *Interactions between baseline outcome and predictor were excluded in the model, as no statistically significant interactions were found (P > 0.05). #Model adjusted for demographic and diabetes characteristics, including gender, age, diabetes type, diabetes duration, employment status, education level, ethnicity; both of the baseline predictor and change in predictor were included in the model.
Similarly, the change in EQ-5D summary index between T1 and T2 significantly explained the anxiety and depression scores at T2 (P < 0.05), correcting for baseline anxiety and depression scores, patient’s demographic and diabetes characteristics in the Model 3 (R2 = 0.707) and Model 4 (R2 = 0.720). The anxiety score at T2 significantly reflected the change in EQ-5D index between time intervals (B = −6.50) more than baseline EQ-5D index (B = −3.14), while depression at T2 reflects the change in HRQoL (B = −7.24) as much as HRQoL at T1 (B = −7.43). Patients who were employed and living with a majority ethnicity were less likely to have anxiety symptoms, while those who were employed, with lower education background, and a majority ethnicity were less likely to have depression symptoms (B < 0; P < 0.05); However, none of those characteristics were significantly associated with anxiety and depression scores in the multivariable models (P > 0.05).
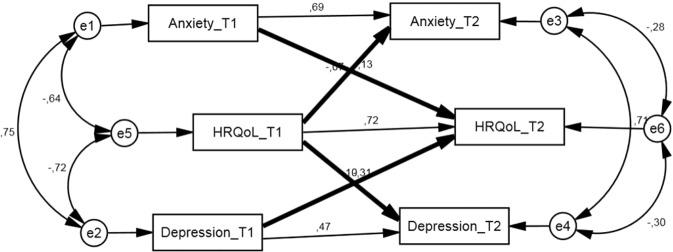
Longitudinal association between anxiety/depression and HRQoL with directions
We fitted our longitudinal data in a cross-lagged model with the hypothesis that there are bi-directional pathways of negative associations between anxiety symptoms and HRQoL, as well as depression symptoms and HRQoL, among adult patients with diabetes (Fig. 2). This model reached the standard of acceptable fitness (x2/df = 1.102, P = 0.256; CFI = 1.000, RMSEA = 0.030). Statistical significance was found in all the path coefficients (P < 0.05). Overall at T2, 46.9% of the variance in anxiety, 65.8% of the variance in depression and 86.0% of the variance in HRQoL were explained by the model.
Figure 2.
The cross-lagged model hypothesized to analyze the longitudinal association among anxiety, depression and health-related quality of life (HRQoL) summary index. Note: HRQoL is measured by EQ-5D summary index with higher score on EQ-5D index indicating better quality of life in mobility, self-care, usual activities, pain/discomfort and anxiety/depression; Numbers above arrows indicate standardized correlation coefficients; Thick arrows indicate the paths of interest, which are the bidirectional, longitudinal paths between anxiety/depression and HRQoL. The overall model fit was x2/df = 1.102; CFI = 1.000, RMSEA = 0.030.
Discussion
This longitudinal study points at bi-directional negative associations between anxiety as well as depression symptoms and health-related quality of life (HRQoL) among adult patients with diabetes. Despite receiving diabetes care, our results during follow-up of the patients suggest direct effects of changes in anxiety and depression symptoms on HRQoL over time, as well as a direct effect of changes in HRQoL on anxiety and depression symptoms. In addition, this study shows that symptoms of anxiety and depression are common in diabetes patients, and HRQoL is suboptimal in general for patients with diabetes.
Anxiety and depression symptoms prevalence rates found in this study (27.5% and 19.8%) are almost twice as low compared to those found in another recent longitudinal study by Tonje and colleagues (47% and 38%)30. Both used the same instrument and thresholds to measure anxiety and depression; however, Tonje’s study included patients living with both diabetes and gastroparesis symptoms in Norway, which may explain the discrepancy. Our identified prevalence rate of depression symptoms (19.8%) is very similar to the finding of a previous review on epidemiology of depression in people with type 2 diabetes (19.1%)31. Also, we found that over half of the diabetes patients who had anxiety symptoms lived also with depression symptoms. This result is expected as symptoms of depression and anxiety often overlap and anxiety-depression comorbidity has been found among various populations32,33.
Unemployed patients with diabetes of a minority ethnic background and lower HRQoL were susceptible to develop anxiety symptoms; while those who were unemployed with higher education of a minority ethnic background and lower HRQoL were subject to depression symptoms. Nevertheless, we found that the change in HRQoL between time intervals was the most significantly associated with anxiety and depression symptoms developed over time, independent of all measured social demographics and baseline anxiety/depression level. Mood may be influenced by HRQoL through anxiety and depression systems with factors like social support and support utilization, which have a proven relationship with changing HRQoL34 and a proven association with psychological adjustment that influences risks of anxiety and depression35. This emphasizes the importance of efforts to maximize HRQoL in order to prevent anxiety and/or depression in diabetes. Future efforts to prevent anxiety and depression in diabetes care should take into consideration factors influencing HRQoL. For instance, pay attention to patients with diabetes who are struggling with insulin therapy, obesity and suffer from diabetic complications, low self-efficacy and social support, which all associate with suboptimal HRQoL36–38.
With regard to HRQoL status itself, we identified the average index score 0.73 at baseline, which is identical to a previous study using the same instrument among Dutch patients with type 2 diabetes36. Similarly, the majority of the patients with diabetes in this study reported problems in daily activities, pain and cognition, which is consistent with previous empirical findings in the US39. The reported mean EQ VAS rating was lower than that among a general population of the Netherlands (70.1 VS 77.7)40. The identified suboptimal HRQoL highlights an urgent need of interventions to improve the HRQoL in our patients with diabetes. Previous studies indicated social demographics, like ethnicity41, age, sex and occupation42, as possible determinants of HRQoL. However, we found that changes in anxiety and depression, as well as baseline depression symptoms, were the most significantly associated with HRQoL over time and independent of all measured social demographics. This indicates that interventions to prevent anxiety and depression could be beneficial to improve HRQoL in diabetes care. An important way to reduce unrecognized depression and anxiety is by advocating depression screening programs in diabetes care, particularly for patients with lower socioeconomic status and patients without a previous diagnosis of major depressive disorder43,44. Future efforts to improve HRQoL of diabetes patients should take into account other determinants of anxiety and depression. For instance, patients who suffer from central obesity, neuropathy, peripheral vascular disease, diabetic foot disease and pill burden are at risk for depression45. Poor glycemic control46, systolic blood pressure and fasting blood triglycerides47 may be indicators of a combination of depressive and anxiety symptoms in diabetes patients.
An unexpected yet interesting result is that the respondents who reported extreme problems in mobility, self-care, daily activities and pain reported fewer anxiety symptoms than those experienced moderate or severe problems. A possible explanation is resilience – patients who have been suffering from diabetes with complications for a long period may know better what they are dealing with, and have developed a better capacity to navigate their way to the psychological resources that sustain their mental well-being or accepting their situation48,49. Another explanation may be attrition - patients with severe health problems and anxiety and/or depression have already died, thus were not recruited by this study50.
This study investigated the prevalence of anxiety, depression and HRQoL among a population of adults with diabetes. To the best of our knowledge, this is the first longitudinal study evaluating the bi-directional association between anxiety symptoms and HRQoL, as well as depression symptoms and HRQoL, for diabetes patients. The questionnaires we used to measure symptoms of anxiety, depression and HRQoL had been validated widely and the results are comparable globally. In addition, considering anxiety/depression is one of the dimensions of EQ-5D, we investigated the associations of HRQoL using not only the EQ-5D summary index, but also five levels of problems for all dimensions besides anxiety/depression. Although 13.7% of the respondents were lost to follow-up, no significant differences in social demographics of respondents were found between two time points. Our study has several limitations. First, due to the nature of self-reported data, our information is likely influenced by recall bias and social desirability bias51. Second, we did not take into account the impact of the screening program conducted between T1 and T2, given the fact that we did not find any statistically significant difference with regards to the prevalence rates of anxiety, depression and HRQoL between the measured time points. Of course, three months of follow-up is not likely to have adequate power to detect such differences52. Third, we tested the direct paths between anxiety, depression and HRQoL in time, without considering possible mediators like socio-demographical characteristics, diabetes type and perceived social support, for instance, that might tangle those paths53. Finally, we are lacking information regarding differences between our respondents and those who did not completed the survey during the recruitment of participates, thus our sample may not be representative of all adult patients with diabetes, and we cannot exclude effects regarding order or repetition of questions in repeated surveys.
Our research results provide direct evidence to support guidelines recommending mental health screening in diabetes care, and promote efforts improving HRQoL for patients with diabetes in general. An important clinical implication is that efforts to decrease anxiety and/or depression could significantly improve HRQoL of patients with diabetes and should be tested and eventually added to diabetes care. Likewise, interventions to improve HRQoL in diabetes care are able to assist in preventing patients from developing anxiety and depression during diabetes management. Adopting an evidence-based and population-tailored collaborative care model might have potential to improve both54. We recommend future studies to investigate the associations between anxiety/depression and HRQoL in a prospective design with a follow-up period longer than three months, and to include more potential determinants besides social demographics, such as timing of anxiety/depression onset, obesity, insulin therapy and lifestyle factors36, and explore their effects in marginal models (e.g. Generalized Estimating Equations) or conditional models (e.g. Generalized Linear Mixed Models)55 to optimize and test future preventive measures.
Acknowledgements
We thank all of the patients and the staff members of the Erasmus MC who participated in this research for their valuable contributions. We also gratefully acknowledge Frank Santegoets for valuable assistance in data collection.
Author contributions
X.L. and J.H. researched data and drafted the manuscript. L.B., H.B and V.E. carried out the acquisition of the data and edited the manuscript. S.P. designed the study and edited the manuscript. E.S. and J.M. contributed to the discussion and reviewed the manuscript.
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to the terms of consent to which the participants agreed, but are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Schram MT, Baan CA, Pouwer F. Depression and quality of life in patients with diabetes: a systematic review from the European depression in diabetes (EDID) research consortium. Curr. Diabetes Rev. 2009;5:112–119. doi: 10.2174/157339909788166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smith-Palmer J, et al. Evaluating health-related quality of life in type 1 diabetes: a systematic literature review of utilities for adults with type 1 diabetes. Clinicoecon Outcomes Res. 2016;8:559–571. doi: 10.2147/CEOR.S114699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barendse S, Singh H, Frier BM, Speight J. The impact of hypoglycaemia on quality of life and related patient-reported outcomes in Type 2 diabetes: a narrative review. Diabet. Med. 2012;29:293–302. doi: 10.1111/j.1464-5491.2011.03416.x. [DOI] [PubMed] [Google Scholar]
- 5.Hogg FR, Peach G, Price P, Thompson MM, Hinchliffe RJ. Measures of health-related quality of life in diabetes-related foot disease: a systematic review. Diabetologia. 2012;55:552–565. doi: 10.1007/s00125-011-2372-5. [DOI] [PubMed] [Google Scholar]
- 6.Grigsby AB, Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. Prevalence of anxiety in adults with diabetes: a systematic review. J. Psychosom. Res. 2002;53:1053–1060. doi: 10.1016/S0022-3999(02)00417-8. [DOI] [PubMed] [Google Scholar]
- 7.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 8.Maia AC, Braga Ade A, Brouwers A, Nardi AE, Oliveira e Silva AC. Prevalence of psychiatric disorders in patients with diabetes types 1 and 2. Compr. Psychiatry. 2012;53:1169–1173. doi: 10.1016/j.comppsych.2012.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Goldney RD, Phillips PJ, Fisher LJ, Wilson DH. Diabetes, depression, and quality of life: a population study. Diabetes Care. 2004;27:1066–1070. doi: 10.2337/diacare.27.5.1066. [DOI] [PubMed] [Google Scholar]
- 10.Golden SH, et al. The Prevalence and Specificity of Depression Diagnosis in a Clinic-Based Population of Adults With Type 2 Diabetes Mellitus. Psychosomatics. 2017;58:28–37. doi: 10.1016/j.psym.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meader N, et al. Case identification of depression in patients with chronic physical health problems: a diagnostic accuracy meta-analysis of 113 studies. Br. J. Gen. Pract. 2011;61:e808–820. doi: 10.3399/bjgp11X613151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ali S, et al. The association between depression and health-related quality of life in people with type 2 diabetes: a systematic literature review. Diabetes Metab. Res. Rev. 2010;26:75–89. doi: 10.1002/dmrr.1065. [DOI] [PubMed] [Google Scholar]
- 13.M MV, et al. Dutch Tariff for the Five-Level Version of EQ-5D. Value Health. 2016;19:343–352. doi: 10.1016/j.jval.2016.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Pan A, et al. Bidirectional association between depression and obesity in middle-aged and older women. Int. J. Obes. 2012;36:595–602. doi: 10.1038/ijo.2011.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan A, et al. Bidirectional Association Between Depression and Metabolic Syndrome A systematic review and meta-analysis of epidemiological studies. Diabetes Care. 2012;35:1171–1180. doi: 10.2337/dc11-2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Atlantis E, Sullivan T. Bidirectional Association Between Depression and Sexual Dysfunction: A Systematic Review and Meta-Analysis. J. Sex. Med. 2012;9:1497–1507. doi: 10.1111/j.1743-6109.2012.02709.x. [DOI] [PubMed] [Google Scholar]
- 17.Gilsanz P, Karter AF, Beeri MS, Quesenberry CPJ, Whitmer RA. The Bidirectional Association Between Depression and Severe Hypoglycemic and Hyperglycemic Events in Type 1 Diabetes. Diabetes Care. 2018;41:446–452. doi: 10.2337/dc17-1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nijrolder I, van der Windt DA, Twisk JW, van der Horst HE. Fatigue in primary care: longitudinal associations with pain. Pain. 2010;150:351–357. doi: 10.1016/j.pain.2010.05.030. [DOI] [PubMed] [Google Scholar]
- 19.Beesdo K, Pine DS, Lieb R, Wittchen HU. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Arch. Gen. Psychiatry. 2010;67:47–57. doi: 10.1001/archgenpsychiatry.2009.177. [DOI] [PubMed] [Google Scholar]
- 20.Federation. N. D. (Netherlands Diabetes Federation Amersfoort, the Netherlands, 2013).
- 21.Stronks K, Kulu-Glasgow I, Agyemang C. The utility of ‘country of birth’ for the classification of ethnic groups in health research: the Dutch experience. Ethn. Health. 2009;14:255–269. doi: 10.1080/13557850802509206. [DOI] [PubMed] [Google Scholar]
- 22.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 23.Thombs BD, et al. Diagnostic accuracy of the Depression subscale of the Hospital Anxiety and Depression Scale (HADS-D) for detecting major depression: protocol for a systematic review and individual patient data meta-analyses. BMJ Open. 2016;6:e011913. doi: 10.1136/bmjopen-2016-011913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale. An updated literature review. J. Psychosom. Res. 2002;52:69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 25.Herdman M, et al. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L) Qual. Life Res. 2011;20:1727–1736. doi: 10.1007/s11136-011-9903-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoeymans N, van Lindert H, Westert GP. The health status of the Dutch population as assessed by the EQ-6D. Qual. Life Res. 2005;14:655–663. doi: 10.1007/s11136-004-1214-z. [DOI] [PubMed] [Google Scholar]
- 27.Geraerds A, et al. The added value of the EQ-5D with a cognition dimension in injury patients with and without traumatic brain injury. Qual. Life Res. 2019;28:1931–1939. doi: 10.1007/s11136-019-02144-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual. Life Res. 2014;23:977–989. doi: 10.1007/s11136-013-0537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Markus KA. Principles and Practice of Structural Equation Modeling, 3rd edition. Struct. Equ. Modeling. 2012;19:509–512. doi: 10.1080/10705511.2012.687667. [DOI] [Google Scholar]
- 30.Teigland T, Iversen MM, Sangnes DA, Dimcevski G, Softeland E. A longitudinal study on patients with diabetes and symptoms of gastroparesis - associations with impaired quality of life and increased depressive and anxiety symptoms. J. Diabetes Complications. 2018;32:89–94. doi: 10.1016/j.jdiacomp.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 31.Roy T, Lloyd CE. Epidemiology of depression and diabetes: a systematic review. J. Affect. Disord. 2012;142(Suppl):S8–21. doi: 10.1016/S0165-0327(12)70004-6. [DOI] [PubMed] [Google Scholar]
- 32.Rajput R, Gehlawat P, Gehlan D, Gupta R, Rajput M. Prevalence and predictors of depression and anxiety in patients of diabetes mellitus in a tertiary care center. Indian. J. Endocrinol. Metab. 2016;20:746–751. doi: 10.4103/2230-8210.192924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wei CB, et al. Overlap between Headache, Depression, and Anxiety in General Neurological. Clinics: A Cross-sectional Study. Chin. Med. J-Peking. 2016;129:1394–1399. doi: 10.4103/0366-6999.183410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jalali-Farahani S, et al. Perceived social support and health-related quality of life (HRQoL) in Tehranian adults: Tehran lipid and glucose study. Health Qual. Life Outcomes. 2018;16:90. doi: 10.1186/s12955-018-0914-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ghorbani Saeedian R, et al. The role of social support in anxiety and depression among Parkinson’s disease patients. Disabil. Rehabil. 2014;36:2044–2049. doi: 10.3109/09638288.2014.886727. [DOI] [PubMed] [Google Scholar]
- 36.Redekop WK, et al. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care. 2002;25:458–463. doi: 10.2337/diacare.25.3.458. [DOI] [PubMed] [Google Scholar]
- 37.Papadopoulos, A. A., Kontodimopoulos, N., Frydas, A., Ikonomakis, E. & Niakas, D. Predictors of health-related quality of life in type II diabetic patients in Greece. Bmc Public Health7 (2007). [DOI] [PMC free article] [PubMed]
- 38.Aalto AM, Uutela A, Aro AR. Health related quality of life among insulin-dependent diabetics: Disease-related and psychosocial correlates. Patient Educ. Couns. 1997;30:215–225. doi: 10.1016/S0738-3991(96)00963-9. [DOI] [PubMed] [Google Scholar]
- 39.Stevens GD, Shi LY, Vane C, Nie XY, Peters AL. Primary Care Medical Home Experience and Health-Related Quality of Life Among Adult Medicaid Patients with Type 2 Diabetes. J. Gen. Intern. Med. 2015;30:161–168. doi: 10.1007/s11606-014-3033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stolk, E., Krabbe, P. & Busschbach, J. Using the Internet to collect EQ-5D norm scores: a valid alternative? 153–165 (2009).
- 41.Friedenberg FK, Kowalczyk M, Parkman HP. The influence of race on symptom severity and quality of life in gastroparesis. J. Clin. Gastroenterol. 2013;47:757–761. doi: 10.1097/MCG.0b013e3182819aae. [DOI] [PubMed] [Google Scholar]
- 42.ElShazly HM, Hegazy NN. Socioeconomic determinants affecting the quality of life among diabetic and hypertensive patients in a rural area, Egypt. J. Family Med. Prim. Care. 2017;6:141–145. doi: 10.4103/jfmpc.jfmpc_31_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Arteaga-Zarate, G., Demarini-Olivares, G. & Torres-Slimming, P. A. Symptoms of anxiety and depression in type 2 diabetes: Associations with clinical diabetes measures and self-management outcomes in the norwegian HUNT study. Psychoneuroendocrinology (2017). [DOI] [PubMed]
- 44.Barnacle M, Strand MA, Werremeyer A, Maack B, Petry N. Depression Screening in Diabetes Care to Improve Outcomes: Are We Meeting the Challenge? Diabetes Educ. 2016;42:646–651. doi: 10.1177/0145721716662917. [DOI] [PubMed] [Google Scholar]
- 45.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian. J. Med. Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 46.Sun N, et al. Prevalence and determinants of depressive and anxiety symptoms in adults with type 2 diabetes in China: a cross-sectional study. BMJ Open. 2016;6:e012540. doi: 10.1136/bmjopen-2016-012540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Khuwaja, A. K. et al. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetology & Metabolic Syndrome2 (2010). [DOI] [PMC free article] [PubMed]
- 48.Popa-Velea O, Diaconescu L, Jidveian Popescu M, Trutescu C. Resilience and active coping style: Effects on the self-reported quality of life in cancer patients. Int. J. Psychiatry Med. 2017;52:124–136. doi: 10.1177/0091217417720895. [DOI] [PubMed] [Google Scholar]
- 49.Yi-Frazier JP, et al. A Person-Focused Analysis of Resilience Resources and Coping in Diabetes Patients. Stress. Health. 2010;26:51–60. doi: 10.1002/smi.1258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Archer VE. Spurious bias in the attribution of lung cancer as a cause of death. Epidemiology. 1993;4:562–563. doi: 10.1097/00001648-199311000-00025. [DOI] [PubMed] [Google Scholar]
- 51.Nolte S, Elsworth GR, Osborne RH. Absence of social desirability bias in the evaluation of chronic disease self-management interventions. Health Qual. Life Outcomes. 2013;11:114. doi: 10.1186/1477-7525-11-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Clark TG, Bradburn MJ, Love SB, Altman DG. Survival analysis part I: basic concepts and first analyses. Br. J. Cancer. 2003;89:232–238. doi: 10.1038/sj.bjc.6601118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xiaowen W, et al. Depression and anxiety mediate perceived social support to predict health-related quality of life in pregnant women living with HIV. AIDS Care. 2018;30:1147–1155. doi: 10.1080/09540121.2018.1456640. [DOI] [PubMed] [Google Scholar]
- 54.Johnson JA, et al. Collaborative care versus screening and follow-up for patients with diabetes and depressive symptoms: results of a primary care-based comparative effectiveness trial. Diabetes Care. 2014;37:3220–3226. doi: 10.2337/dc14-1308. [DOI] [PubMed] [Google Scholar]
- 55.Mehrotra, D. V. A comparison of generalized linear mixed model procedures with estimating equations for variance and covariance parameter estimation in longitudinal studies and group randomized trials. Stat Med21, 3745–3747; author reply 3747–3748 (2002). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are not publicly available due to the terms of consent to which the participants agreed, but are available from the corresponding author on reasonable request.