Abstract
Pituitary macroadenoma is the most common suprasellar lesion in adults. If symptomatic, it is managed surgically via transsphenoidal resection. Patients commonly present with headache and visual disturbances. If the tumour is large enough, it may have mass effect and patient may present with symptoms of elevated intracranial pressure like severe headache, nausea and vomiting. Functional adenomas may cause endocrine dysfunction. Here, we present a case of pituitary macroadenoma in a young adult female who presented with headache. Initial CT and MRI revealed a pituitary macroadenoma. However, repeat imaging done preoperatively showed complete regression of the lesion and a normal appearing pituitary gland.
Keywords: Pituitary apoplexy, Macroadenoma, Spontaneous regression
Introduction
Spontaneous regression of pituitary adenoma is a relatively rare phenomenon [1,2]. It is usually described as a result of apoplexy. Pituitary apoplexy is hemorrhage, infection or infarction of the pituitary gland. Pituitary macroadenoma is the most common suprasellar lesion in adults [3]. If symptomatic, it is managed surgically via transsphenoidal resection. Patients commonly present with headache and visual disturbances. If the tumor is large enough, it may have mass effect and patient may present with symptoms of elevated intracranial pressure like severe headache, nausea, and vomiting. Functional adenomas may cause endocrine dysfunction [3]. Here, we describe a case of pituitary adenoma in a young adult female who presented with headache. Further evaluation revealed a significantly enlarged pituitary gland with an adenoma. Surgical planning was done for a transsphenoidal resection. However, repeat preoperative imaging revealed spontaneous resolution of the tumor.
Case history
A 22-year-old female presented to the Neurosurgery Department with complaints of headache for 1 month. She also gave history of weight gain in the last 6 months.
On examination, her vitals were within normal limits. She was conscious, oriented, and obeying verbal commands. There was no sensory loss or motor deficits. Cranial nerves were normal and pupils were reactive. Visual field examination by confrontation method was normal.
Contrast-enhanced computed tomography (CT) brain done at the time of admission revealed small well-defined extra-axial homogeneously enhancing midline suprasellar lesion. Following this, a contrast-enhanced magnetic resonance imaging (MRI) was done which showed diffusely bulky pituitary gland showing heterogeneous post contrast enhancement. Superiorly, it was crossing the diaphragma sellae, and abutting the optic chiasm. Laterally, on either side, it was abutting bilateral cavernous internal carotid artery (ICAs) with angle of contact <180°. A diagnosis of pituitary macroadenoma was made.
Hormonal profile was done, which showed mild elevation of prolactin and decrease in serum thyroid stimulating hormone (TSH). Rest of the hormones (serum cortisol, T3, T4, FSH and LH) were within normal limits.
Patient was started on thyroxin and planned for transnasal, transsphenoidal endoscopic tumor excision. Repeat preoperative MRI was done 17 days later which showed normal size of the pituitary gland with homogeneous post contrast enhancement and no evidence of previously visualized macroadenoma.
Surgery was withheld and patient was planned to be managed conservatively. She was discharged in hemodynamically stable condition.
Discussion
We present a case of pituitary lesion which showed resolution or regression in a matter of just 17 days without any steroid treatment. The differential diagnoses for sellar and suprasellar lesions comprise of a variety of neoplastic, vascular, and non-neoplastic inflammatory pathologies. Neoplastic causes include pituitary adenomas, metastases, Rathke's cleft cyst, craniopharyngioma and meningioma. Inflammatory lesions include sarcoid and autoimmune hypophysitis [3]. Spontaneous regression of pituitary adenoma is frequently reported. However, the underlying mechanism resulting in regression is not clearly understood [1,2,4]. One of the mechanisms to explain this is pituitary apoplexy [1,2].
Pituitary apoplexy is a rare but life-threatening complication [1]. It is usually seen in highly vascular adenomas namely prolactinomas and corticotropinomas [5]. Spontaneous regression of nonfunctioning pituitary adenoma is rare [2]. Pituitary adenoma can be asymptomatic or pituitary apoplexy may be the first indication that a tumor is present, especially when it is nonfunctional [5,6]. Patients may present with headache, nausea, vomiting, visual field defect, ophthalmoplegia, altered sensorium and in severe cases subarachnoid hemorrhage [2,3,6]. The most common symptom is headache [2,6], as in our case followed by visual deficits, nausea, vomiting and ocular palsy [2].
The start of spontaneous regression of pituitary adenoma following apoplexy has not been clearly defined. It can occur as early as 1 week following an apoplectic event [2]. Apoplexy occurs when there a rapidly growing tumor which exceeds its vascular supply [6]. Another theory to explain apoplexy is that the growing mass results in compression of the portal vessels which results in ischemic necrosis with or without hemorrhage [1,6]. Risk of apoplexy is increased if there is concomitant anticoagulant medication, use of oral contraceptive pills, clomiphene, following provocative tests for pituitary reserve assessment, head trauma, neurosurgery, pregnancy, thrombocytopenia and increased intracranial pressure [4,5].
CT and MRI are excellent imaging tools for the diagnosis of pituitary adenoma. On CT, patchy or confluent areas of hyperdensity that correspond to areas of hemorrhage which are seen in apoplexy [2]. However, MRI is superior to CT in detecting pituitary adenoma and the various stages of bleed within the adenoma. In the acute phase, the hemorrhagic area appears hyperintense of T1-weighted image and mixed hypo- and hyperintense on T2-weighted image [2].
Pituitary apoplexy requires urgent neurosurgical intervention in the form of early transsphenoidal decompression [6]. However, in case of absolute contraindication, medical management can also be done. Initial management like correction of electrolyte imbalance, hemodynamic stabilization and corticosteroid replenishment may be required [3,6]. Our case did not require it as she was completely stable.
In our case, since the pathology was not obtained, we cannot rule out any physiological cause of pituitary hyperplasia. MRI showed complete resolution of the adenoma. However microscopic remnants of tumor cells cannot be ruled out. The patient may be at a risk of recurrence [4]. Therefore, such patients need careful long-term follow up [1].
Conclusion
Pituitary apoplexy is one of the rare but documented cause of sudden disappearance of pituitary macroadenomas. There is no definite evidence to diagnose a case of apoplexy but a very strong clinical suspicion for it. This entity must be considered as a differential in a case of nonvisualization or a decrease in size of a previously documented pituitary lesion who has not been treated in any other way (Fig. 1, Fig. 2, Fig. 3).
Fig. 1.
Sagittal and coronal contrast-enhanced CT images showing heterogeneously enhancing pituitary gland in the sellar region.
Fig. 2.
Sagittal and coronal contrast-enhanced T1-weighted MR images showing heterogeneously enhancing enlarged pituitary gland crossing the diaphragma sellae, and abutting the optic chiasm. Laterally, on either side, it was abutting bilateral cavernous ICAs.
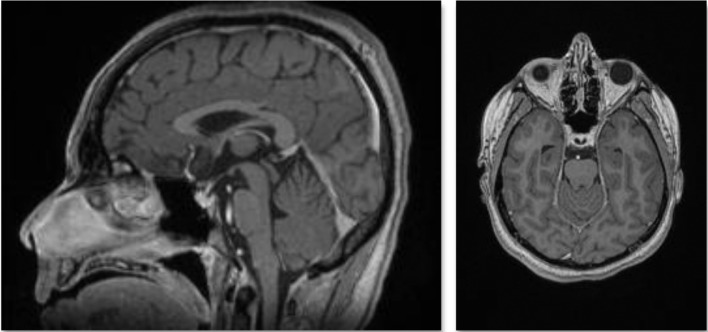
Fig. 3.
Sagittal and axial T1-weighted contrast-enhanced MR images, taken 17 days later, showing a normal sized pituitary gland.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Footnotes
Financial support: Nil.
Competing Interests: There are no conflicts of interest.
References
- 1.Liu S, Wang X, Liu Y, Mao Q. Spontaneous disappearance of the pituitary macroadenoma after apoplexy: a case report and review of the literature. Neurol India. 2012;60(5):530. doi: 10.4103/0028-3886.103211. [DOI] [PubMed] [Google Scholar]
- 2.Kameno K, Yano S, Shinojima N, Kuratsu J. Spontaneous regression of nonfunctioning pituitary macroadenoma: a case report. Interdiscip Neurosurg. 2016;5:45–47. [Google Scholar]
- 3.Sieg EP, Stepanyan H, Payne R, Ouyang T, Zacharia BE. Vanishing pituitary macroadenoma: a case report. Cureus [Internet] 2016 doi: 10.7759/cureus.838. http://www.cureus.com/articles/5166-vanishing-pituitary-macroadenoma-a-case-report cited 2019 Nov 24]Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoshino A, Katayama Y, Watanabe T, Hirota H. Vanishing pituitary mass revealed by timely magnetic resonance imaging: two cases of spontaneous resolution of nonfunctioning pituitary adenoma. Acta Neurochir (Wien) 2005;147(3):253–257. doi: 10.1007/s00701-004-0443-9. [DOI] [PubMed] [Google Scholar]
- 5.Saberifard J, Yektanezhad T, Assadi M. An interesting case of a spontaneous resolution of pituitary adenoma after apoplexy. J Belg Soc Radiol. 2015;99(1):101–102. doi: 10.5334/jbr-btr.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jackson DL, Van Gompel JJ. Rapid pituitary apoplexy regression: what is the time course of clot resolution? Case Rep Radiol. 2015;2015:1–5. doi: 10.1155/2015/268974. [DOI] [PMC free article] [PubMed] [Google Scholar]