Abstract
The National Clinical Database (NCD) of Japan grew rapidly, harvesting over 11 million cases of data between 2011 and 2018 from more than 5000 facilities. This is the Report of the NCD based upon gastrointestinal surgery information in 4 420 175 cases from 2011 to 2018. More than 70% of all gastrointestinal surgeries were performed at certified institutions, and the percentage of surgeries performed at certified institutions was particularly high for the esophagus (93.8% in 2018), liver (89.4%), pancreas (91.3%), and spleen (86.9%). Also, more than 70% of the surgeries were performed with the participation of the board‐certified surgeon. As the patients have been getting older, the morbidities have been increasing. However, the mortalities have been kept at a low level. The rates of endoscopic surgery have been increasing year by year, especially high in low anterior resection (67.0%) and esophagectomy (61.0%). Nationwide, this database is surely expecting to ensure the quality of board certification system and surgical outcomes in gastroenterological surgery.
Keywords: gastroenterological surgery, NCD, surgical outcome
This is the Report of the National Clinical Database (NCD) based upon gastrointestinal surgery information in 4 420 175 cases from 2011 to 2018. Nationwide this database is surely expecting to ensure the quality of the board certification system and surgical outcomes in gastroenterological surgery.

1. INTRODUCTION
The Japanese National Clinical Database (NCD), which started its data registration in 2011, has grown into a large nationwide database covering more than 95% of the surgeries performed by regular surgeons in Japan. 1 As of the end of December 2019, 5276 facilities have enrolled in the NCD, and about 1 500 000 cases have been registered every year. 2
In the gastroenterological section of the NCD, the Japanese Society of Gastroenterological Surgery (JSGS) selected 115 gastrointestinal operative procedures as important for the board certification system, and eight main procedures as especially important in terms of medical standards for improvement of surgical quality. All surgical cases are registered in the NCD with input of postoperative complications for the 115 procedures, and with detailed input such as comorbidities and morbidities for the eight main procedures; namely, esophagectomy, partial/total gastrectomy, right hemicolectomy, low anterior resection, hepatectomy, pancreaticoduodenectomy, and surgery for acute diffuse peritonitis. 3 , 4 Risk models of mortality 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 and morbidity 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 for these eight main procedures have been reported, which were all the first‐risk stratification studies based on a Japanese nationwide web‐based database. The risk calculator has been implemented using the risk models, which enables predictions of morbidity and mortality of patients after inputting the preoperative data. 21 To secure the reliability of data collected from the gastroenterological section of the NCD, the JSGS started data verification activity in 2016 and found a high accuracy of data entry. 22
Following the previous annual reports, 3 , 4 the Report of the NCD 2011‐2018 is based upon gastrointestinal surgery information in 4 420 175 cases of surgery performed and recorded from 2011 to 2018. It is our pleasure that this report would reflect the real world of Japanese surgical outcomes of gastroenterological surgery.
2. SUBJECTS AND METHOD
As previously reported, 3 , 4 the subjects were patients whose surgical data were recorded in the NCD, and who underwent one or more of the 115 surgical procedures stipulated by the “Training Curriculum for Board Certified Surgeons in Gastroenterology,“ using the “New Classification of Surgical Difficulty.” The board certification system of the JSGS consists of board‐certified training institutions and board‐certified surgeons in gastroenterological surgery. 23 Requirements for board‐certified training institutions are 600 or more gastroenterological operations determined by the certified committee (more than 120 of which are essential major surgery) in the last 3 years. And board‐certified surgeons are required the experience performing 450 or more gastroenterological operations, and gastroenterological surgical training for more than 5 years according to the training curriculum in a board‐certified training institution authorized by the JSGS. We targeted data from 2011 to 2018, adding data of complications to data already reported in the Annual Report 2011‐2017. Complications included surgical site infection (SSI), wound dehiscence, anastomotic leakage, pancreatic fistula, bile leakage, pneumonia, unplanned intubation, pulmonary embolism, ventilator‐assisted respiration longer than 48 hours, progressive renal insufficiency, acute renal failure, urinary tract infection, cerebrovascular accident with neurological deficit, coma longer than 24 hours, peripheral nerve injury, cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, bleeding complications defined by transfusions in excess of one unit of blood, deep venous thrombosis, and sepsis. Postoperative complications were categorized into six grades according to the Clavien–Dindo (C–D) classification. 24 In this study, grade III (complications requiring intervention) or higher complications were defined as severe complications. Furthermore, we separated and studied the eight main operative methods that we deemed important in terms of medical standards among these 115 procedures.
We clarified the number of surgical cases and the mortality rates related to the selected 115 gastrointestinal operative procedures, and also the eight main operative procedures from 2011 to 2018. We also comparatively studied patient sex, age groups, institution groups, and the percentage contribution of certified surgeons related to the eight main operative procedures.
The following points need to be considered in the interpretation of the data reported here: (a) since a maximum of eight operative procedures can be recorded per each case in the NCD, the total number of surgeries in “Results of the 115 gastrointestinal surgical procedures for board certification system” is not the actual total number of surgical cases; (b) cases with errors in patient age, sex, and postoperative 30‐day status were excluded; (c) cases in which several operative methods were performed simultaneously were tallied per all operative methods; (d) postoperative 30‐day mortality included all cases of mortality within 30 days of surgery regardless of pre‐ or post‐discharge status. The calculation of operative mortality included all patients who died during the index hospitalization, including hospital stays up to 90 days, and any patient who died after hospital discharge within 30 days of the operation date.
3. RESULTS
3.1. The 115 selected gastrointestinal operative procedures in the “Training Curriculum for Board Certified Surgeons in Gastroenterology“
The total number of cases represented by the 115 selected gastrointestinal surgical procedures, recorded in the NCD between 1 January and 31 December 2018 was 601 754. Based on organ involvement, 9286 cases involved the esophagus (1.5%); 65 152 cases, the stomach and duodenum (10.8%); 236 496 cases, the small intestine and colon (39.3%); 56 162 cases, the rectum and anus (9.3%); 26 531 cases, the liver (4.4%); 139 844 cases, the gall bladder (23.2%); 19 152 cases, the pancreas (3.2%); 2544 cases, the spleen (0.4%); and 46 587 cases, other organs (7.7%) (Table 1). The increase of cases, especially with malignant colorectal diseases, was remarkable, while cases of the stomach and duodenum decreased. Year by year, older patients have been increasing for procedures across all organs (Table 1).
TABLE 1.
Annual changes of surgeries by sex, age group, and organ for the selected 115 gastrointestinal operative procedures in the training curriculum for board certified surgeons in gastroenterology
| Organ | Year | No. surgeries | Percentage by sex | Percentage according to age group (y) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | <60 | 60 to <65 | 65 to <70 | 70 to <75 | 75 to <80 | ≥80 | |||
| Esophagus | 2011 | 7246 | 81.8 | 18.2 | 22.5 | 19.6 | 21.1 | 18.7 | 12.0 | 6.0 |
| 2012 | 8819 | 82.2 | 17.8 | 22.1 | 19.7 | 20.0 | 19.5 | 12.9 | 6.0 | |
| 2013 | 8642 | 81.5 | 18.5 | 20.8 | 17.5 | 21.0 | 20.6 | 13.2 | 6.9 | |
| 2014 | 9021 | 81.5 | 18.4 | 20.8 | 16.5 | 21.4 | 20.9 | 13.8 | 6.6 | |
| 2015 | 8943 | 80.8 | 19.2 | 19.6 | 15.3 | 22.4 | 22.5 | 13.1 | 7.1 | |
| 2016 | 9212 | 79.6 | 20.4 | 20.1 | 14.4 | 22.9 | 20.5 | 14.5 | 7.5 | |
| 2017 | 9359 | 80.0 | 20.0 | 19.3 | 13.4 | 24.4 | 19.4 | 15.5 | 8.0 | |
| 2018 | 9286 | 78.4 | 21.6 | 19.0 | 12.8 | 21.3 | 21.6 | 16.7 | 8.7 | |
| Stomach and duodenum | 2011 | 66 740 | 68.0 | 32.0 | 20.1 | 14.4 | 14.0 | 17.1 | 16.4 | 18.0 |
| 2012 | 76 186 | 68.3 | 31.7 | 18.9 | 14.4 | 14.5 | 17.1 | 16.4 | 18.6 | |
| 2013 | 75 583 | 67.9 | 32.1 | 18.6 | 13.1 | 15.5 | 17.2 | 16.9 | 18.7 | |
| 2014 | 74 920 | 67.6 | 32.4 | 17.9 | 12.1 | 16.0 | 17.8 | 16.7 | 19.5 | |
| 2015 | 73 877 | 67.8 | 32.2 | 17.4 | 11.1 | 17.1 | 17.8 | 16.6 | 19.9 | |
| 2016 | 72 234 | 67.8 | 32.2 | 17.0 | 10.2 | 18.1 | 17.1 | 16.6 | 21.0 | |
| 2017 | 68 287 | 67.2 | 32.8 | 16.3 | 9.9 | 17.5 | 17.3 | 17.2 | 21.8 | |
| 2018 | 65 152 | 66.9 | 33.1 | 16.0 | 9.0 | 16.4 | 18.0 | 17.5 | 23.2 | |
| Small intestine and colon | 2011 | 151 143 | 56.7 | 43.3 | 37.4 | 10.9 | 10.5 | 12.1 | 12.2 | 16.9 |
| 2012 | 184 810 | 56.7 | 43.3 | 36.4 | 10.7 | 10.7 | 12.2 | 12.5 | 17.4 | |
| 2013 | 198 677 | 56.9 | 43.1 | 35.6 | 10.1 | 11.3 | 12.7 | 12.4 | 17.8 | |
| 2014 | 206 857 | 56.9 | 43.1 | 34.7 | 9.4 | 12.0 | 13.1 | 12.4 | 18.4 | |
| 2015 | 214 453 | 57.1 | 42.9 | 34.0 | 8.9 | 12.9 | 13.1 | 12.3 | 18.7 | |
| 2016 | 218 228 | 57.3 | 42.7 | 33.7 | 8.4 | 13.6 | 12.5 | 12.4 | 19.3 | |
| 2017 | 235 359 | 56.7 | 43.3 | 32.7 | 8.0 | 13.2 | 12.7 | 12.9 | 20.5 | |
| 2018 | 236 496 | 56.9 | 43.1 | 32.2 | 7.7 | 12.6 | 13.4 | 13.2 | 21.1 | |
| Rectum and anus | 2011 | 41 061 | 59.1 | 40.9 | 22.0 | 16.1 | 14.6 | 15.4 | 14.2 | 17.7 |
| 2012 | 49 704 | 58.3 | 41.7 | 22.3 | 14.8 | 14.6 | 15.5 | 14.3 | 18.5 | |
| 2013 | 49 980 | 58.0 | 42.0 | 20.9 | 13.9 | 15.2 | 16.1 | 14.6 | 19.3 | |
| 2014 | 51 454 | 58.3 | 41.7 | 20.4 | 13.1 | 16.0 | 16.4 | 14.2 | 19.9 | |
| 2015 | 56 092 | 57.8 | 42.2 | 22.3 | 11.8 | 16.7 | 15.7 | 14.0 | 19.4 | |
| 2016 | 55 666 | 57.3 | 42.7 | 22.0 | 11.1 | 17.9 | 15.0 | 13.6 | 20.4 | |
| 2017 | 56 144 | 56.7 | 43.3 | 22.2 | 10.2 | 17.3 | 15.1 | 14.2 | 21.0 | |
| 2018 | 56 162 | 56.9 | 43.1 | 22.2 | 9.8 | 15.9 | 15.8 | 14.6 | 21.6 | |
| Liver | 2011 | 22 855 | 67.3 | 32.7 | 22.2 | 16.5 | 16.3 | 18.7 | 17.2 | 9.2 |
| 2012 | 26 288 | 66.3 | 33.7 | 22.1 | 15.7 | 16.7 | 18.0 | 17.4 | 10.2 | |
| 2013 | 25 814 | 66.1 | 33.9 | 21.3 | 14.6 | 17.6 | 18.7 | 17.3 | 10.5 | |
| 2014 | 26 518 | 66.3 | 33.7 | 21.5 | 13.7 | 18.1 | 19.8 | 16.6 | 10.3 | |
| 2015 | 26 378 | 65.7 | 34.3 | 20.8 | 12.8 | 18.9 | 19.4 | 16.5 | 11.5 | |
| 2016 | 27 212 | 66.4 | 33.6 | 20.3 | 11.5 | 20.5 | 18.6 | 17.0 | 12.1 | |
| 2017 | 27 397 | 65.8 | 34.2 | 20.1 | 11.0 | 20.2 | 18.8 | 17.2 | 12.7 | |
| 2018 | 26 531 | 66.5 | 33.5 | 19.6 | 10.3 | 18.8 | 19.6 | 17.8 | 13.8 | |
| Gall bladder | 2011 | 103 183 | 54.5 | 45.4 | 34.3 | 14.0 | 12.2 | 13.8 | 12.8 | 13.0 |
| 2012 | 122 513 | 55.2 | 44.8 | 32.9 | 13.8 | 12.4 | 13.9 | 13.2 | 13.8 | |
| 2013 | 129 162 | 55.3 | 44.7 | 32.6 | 12.9 | 13.0 | 14.2 | 13.2 | 14.0 | |
| 2014 | 131 182 | 55.6 | 44.4 | 32.1 | 11.8 | 13.9 | 14.5 | 13.2 | 14.5 | |
| 2015 | 133 126 | 55.6 | 44.4 | 32.0 | 11.2 | 15.0 | 14.1 | 13.0 | 14.8 | |
| 2016 | 137 360 | 55.4 | 44.6 | 32.6 | 10.6 | 15.5 | 13.1 | 12.9 | 15.3 | |
| 2017 | 138 267 | 55.6 | 44.4 | 32.2 | 10.2 | 15.1 | 13.5 | 13.2 | 15.8 | |
| 2018 | 139 844 | 55.3 | 44.7 | 31.8 | 9.7 | 14.2 | 14.2 | 13.4 | 16.7 | |
| Pancreas | 2011 | 13 477 | 59.9 | 40.1 | 20.0 | 15.6 | 16.9 | 19.7 | 17.7 | 10.2 |
| 2012 | 15 550 | 60.0 | 40.0 | 19.8 | 15.2 | 17.0 | 19.5 | 18.2 | 10.3 | |
| 2013 | 16 380 | 59.7 | 40.3 | 19.1 | 13.6 | 18.0 | 20.7 | 17.7 | 10.9 | |
| 2014 | 17 313 | 59.5 | 40.5 | 18.4 | 12.4 | 19.0 | 21.0 | 18.2 | 11.1 | |
| 2015 | 17 407 | 59.1 | 40.9 | 18.2 | 11.3 | 19.4 | 21.6 | 18.1 | 11.4 | |
| 2016 | 18 238 | 58.9 | 41.1 | 18.2 | 10.4 | 19.9 | 20.4 | 19.0 | 12.2 | |
| 2017 | 19 138 | 59.2 | 40.8 | 17.7 | 9.9 | 19.5 | 19.9 | 20.1 | 12.9 | |
| 2018 | 19 152 | 58.6 | 41.4 | 16.9 | 9.2 | 18.2 | 21.5 | 20.4 | 13.7 | |
| Spleen | 2011 | 3609 | 61.3 | 38.7 | 35.3 | 15.6 | 14.7 | 14.8 | 11.9 | 7.8 |
| 2012 | 4142 | 61.4 | 38.6 | 32.9 | 16.3 | 15.0 | 15.1 | 12.9 | 7.8 | |
| 2013 | 4509 | 61.8 | 38.2 | 30.8 | 14.9 | 15.9 | 16.5 | 13.1 | 8.7 | |
| 2014 | 4272 | 61.8 | 38.2 | 29.9 | 13.0 | 17.3 | 17.0 | 13.8 | 9.1 | |
| 2015 | 3568 | 60.4 | 39.6 | 29.7 | 11.4 | 17.3 | 16.6 | 14.1 | 10.8 | |
| 2016 | 3171 | 57.3 | 42.7 | 31.9 | 11.7 | 17.7 | 15.7 | 12.5 | 10.5 | |
| 2017 | 2864 | 58.7 | 41.3 | 31.6 | 11.0 | 18.1 | 16.0 | 13.3 | 10.0 | |
| 2018 | 2544 | 56.6 | 43.4 | 32.6 | 9.9 | 15.6 | 16.9 | 13.9 | 11.1 | |
| Others | 2011 | 23 218 | 55.0 | 45.0 | 32.0 | 11.9 | 11.3 | 13.3 | 13.8 | 17.6 |
| 2012 | 28 779 | 55.4 | 44.6 | 31.1 | 11.7 | 11.7 | 13.8 | 13.7 | 18.0 | |
| 2013 | 36 363 | 53.1 | 46.9 | 28.3 | 10.9 | 12.7 | 14.1 | 14.8 | 19.1 | |
| 2014 | 39 854 | 53.7 | 46.3 | 28.1 | 10.1 | 13.1 | 14.5 | 14.4 | 19.8 | |
| 2015 | 41 465 | 53.2 | 46.8 | 27.4 | 9.4 | 14.0 | 14.5 | 14.2 | 20.6 | |
| 2016 | 43 523 | 54.0 | 46.0 | 27.5 | 9.2 | 14.6 | 13.5 | 14.0 | 21.2 | |
| 2017 | 45 622 | 54.1 | 45.9 | 27.0 | 8.2 | 14.7 | 13.5 | 14.6 | 21.9 | |
| 2018 | 46 587 | 54.1 | 45.9 | 26.8 | 8.2 | 14.0 | 14.4 | 14.7 | 21.9 | |
In terms of the institutional groups in which the surgeries were performed, more than 70% of all surgeries were performed at certified institutions, and the percentage of surgeries performed at certified institutions has been increasing for all organs (Table 2). Also, more than 70% of the surgeries were performed with the participation of the board‐certified surgeon. The percentage of certified surgeons that were operators was high for the esophagus (75.2% in 2018), liver (64.1%), and pancreas (66.5%). The complication rates were comparatively higher and increasing for the esophagus and the pancreas, however, the mortality rates for procedures on these organs were not so high (Table 3 and Figure 1). Tables 4, 5, 6, 7, 8, 9, 10, 11, 12 show the number of surgeries, endoscopic surgeries, and morbidity/mortality rates according to the selected 115 gastrointestinal operative procedures in 2018.
TABLE 2.
Institution and anesthesiologist and specialist participation rates by organ for the selected 115 gastrointestinal operative procedures
| Organ | Year | No. surgeries | Percentage by institution group | Anesthesiologist Participation (%) | Board‐certified surgeon participation (%) | Medical practitioners (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| Certified institution | Related institution | Other | Board‐certified Surgeons | Non‐board‐certified surgeons | |||||
| Esophagus | 2011 | 7246 | 93.5 | 5.9 | 0.6 | 97.0 | 87.0 | 62.8 | 37.2 |
| 2012 | 8819 | 78.1 | 5.9 | 16.0 | 97.4 | 87.0 | 62.7 | 37.3 | |
| 2013 | 8642 | 90.6 | 7.1 | 2.4 | 97.3 | 88.4 | 64.4 | 35.6 | |
| 2014 | 9021 | 91.1 | 6.1 | 2.8 | 97.9 | 90.1 | 67.6 | 32.4 | |
| 2015 | 8943 | 91.5 | 6.0 | 2.5 | 97.9 | 91.1 | 69.4 | 30.6 | |
| 2016 | 9212 | 92.4 | 5.0 | 2.6 | 98.2 | 91.2 | 70.0 | 30.0 | |
| 2017 | 9359 | 92.7 | 4.0 | 3.3 | 97.9 | 92.5 | 71.8 | 28.2 | |
| 2018 | 9286 | 93.8 | 4.0 | 2.2 | 98.5 | 94.7 | 75.2 | 24.8 | |
| Stomach and duodenum | 2011 | 66 740 | 80.2 | 17.3 | 2.6 | 92.8 | 69.3 | 35.1 | 64.9 |
| 2012 | 76 186 | 63.5 | 15.6 | 20.9 | 93.5 | 70.3 | 35.6 | 64.4 | |
| 2013 | 75 583 | 76.3 | 19.3 | 4.4 | 93.3 | 73.5 | 37.7 | 62.3 | |
| 2014 | 74 920 | 77.0 | 18.2 | 4.8 | 93.6 | 75.9 | 39.2 | 60.8 | |
| 2015 | 73 877 | 77.1 | 18.3 | 4.6 | 93.9 | 76.1 | 39.2 | 60.8 | |
| 2016 | 72 234 | 79.6 | 16.1 | 4.3 | 94.6 | 78.7 | 41.0 | 59.0 | |
| 2017 | 68 287 | 79.6 | 15.3 | 5.1 | 94.8 | 79.7 | 41.8 | 58.2 | |
| 2018 | 65 152 | 80.0 | 14.8 | 5.1 | 95.1 | 81.4 | 43.2 | 56.8 | |
| Small intestine and colon | 2011 | 151 143 | 76.8 | 20.2 | 2.9 | 88.1 | 59.2 | 25.1 | 74.9 |
| 2012 | 184 810 | 60.6 | 18.2 | 21.2 | 88.9 | 59.9 | 25.4 | 74.6 | |
| 2013 | 198 677 | 72.6 | 22.2 | 5.2 | 89.6 | 62.7 | 26.6 | 73.4 | |
| 2014 | 206 857 | 73.0 | 21.4 | 5.6 | 90.8 | 65.4 | 28.1 | 71.9 | |
| 2015 | 214 453 | 73.8 | 20.7 | 5.5 | 91.6 | 66.3 | 28.5 | 71.5 | |
| 2016 | 218 228 | 75.6 | 19.0 | 5.5 | 92.4 | 68.1 | 29.5 | 70.5 | |
| 2017 | 235 359 | 76.0 | 18.0 | 6.0 | 92.9 | 70.1 | 31.1 | 68.9 | |
| 2018 | 236 496 | 76.3 | 17.5 | 6.1 | 93.3 | 71.8 | 32.6 | 67.4 | |
| Rectum and anus | 2011 | 41 061 | 76.9 | 19.0 | 4.1 | 86.3 | 68.3 | 36.9 | 63.1 |
| 2012 | 49 704 | 60.4 | 18.2 | 21.4 | 85.7 | 68.6 | 37.6 | 62.4 | |
| 2013 | 49 980 | 72.9 | 21.7 | 5.4 | 87.3 | 71.2 | 39.4 | 60.6 | |
| 2014 | 51 454 | 73.5 | 20.9 | 5.6 | 87.9 | 73.7 | 41.6 | 58.4 | |
| 2015 | 56 092 | 72.5 | 20.8 | 6.7 | 84.9 | 73.5 | 41.5 | 58.5 | |
| 2016 | 55 666 | 74.1 | 19.4 | 6.6 | 85.7 | 74.7 | 42.1 | 57.9 | |
| 2017 | 56 144 | 73.8 | 18.2 | 8.0 | 84.8 | 76.1 | 43.9 | 56.1 | |
| 2018 | 56 162 | 74.1 | 17.9 | 8.0 | 85.2 | 77.2 | 46.7 | 53.3 | |
| Liver | 2011 | 22 855 | 89.3 | 9.7 | 1.1 | 95.6 | 85.2 | 55.2 | 44.8 |
| 2012 | 26 288 | 74.2 | 9.2 | 16.7 | 95.4 | 85.7 | 57.4 | 42.6 | |
| 2013 | 25 814 | 86.3 | 10.7 | 2.9 | 96.3 | 87.5 | 57.1 | 42.9 | |
| 2014 | 26 518 | 86.3 | 10.0 | 3.7 | 96.4 | 89.0 | 59.6 | 40.4 | |
| 2015 | 26 378 | 87.3 | 9.5 | 3.2 | 96.6 | 89.1 | 59.1 | 40.9 | |
| 2016 | 27 212 | 88.4 | 8.8 | 2.9 | 96.8 | 90.0 | 59.6 | 40.4 | |
| 2017 | 27 397 | 89.0 | 7.8 | 3.1 | 97.1 | 91.8 | 62.5 | 37.5 | |
| 2018 | 26 531 | 89.4 | 7.1 | 3.5 | 97.3 | 92.8 | 64.1 | 35.9 | |
| Gall bladder | 2011 | 103 183 | 73.9 | 22.5 | 3.6 | 91.8 | 61.9 | 26.4 | 73.6 |
| 2012 | 122 513 | 57.5 | 19.6 | 22.9 | 92.1 | 62.8 | 26.3 | 73.7 | |
| 2013 | 129 162 | 69.9 | 24.1 | 5.9 | 92.2 | 65.4 | 27.3 | 72.7 | |
| 2014 | 131 182 | 70.3 | 23.3 | 6.4 | 92.3 | 67.4 | 28.1 | 71.9 | |
| 2015 | 133 126 | 70.8 | 22.8 | 6.4 | 92.9 | 68.4 | 28.1 | 71.9 | |
| 2016 | 137 360 | 72.4 | 21.3 | 6.3 | 93.5 | 69.4 | 28.9 | 71.1 | |
| 2017 | 138 267 | 72.6 | 20.1 | 7.3 | 93.7 | 71.4 | 29.9 | 70.1 | |
| 2018 | 139 844 | 72.5 | 20.1 | 7.4 | 94.1 | 73.1 | 31.1 | 68.9 | |
| Pancreas | 2011 | 13 477 | 88.1 | 10.8 | 1.2 | 95.8 | 85.2 | 57.7 | 42.3 |
| 2012 | 15 550 | 72.8 | 8.7 | 18.5 | 96.3 | 86.5 | 59.9 | 40.1 | |
| 2013 | 16 380 | 86.5 | 11.0 | 2.4 | 95.9 | 87.6 | 60.2 | 39.8 | |
| 2014 | 17 313 | 86.9 | 9.9 | 3.3 | 96.2 | 89.1 | 61.3 | 38.7 | |
| 2015 | 17 407 | 88.4 | 9.1 | 2.4 | 96.4 | 90.3 | 61.6 | 38.4 | |
| 2016 | 18 238 | 89.8 | 8.0 | 2.3 | 96.8 | 91.1 | 62.4 | 37.6 | |
| 2017 | 19 138 | 90.4 | 7.1 | 2.5 | 97.2 | 92.3 | 63.9 | 36.1 | |
| 2018 | 19 152 | 91.3 | 6.4 | 2.3 | 97.3 | 93.4 | 66.5 | 33.5 | |
| Spleen | 2011 | 3609 | 87.0 | 11.6 | 1.4 | 94.6 | 75.2 | 44.9 | 55.1 |
| 2012 | 4142 | 70.5 | 9.5 | 20.0 | 81.7 | 75.8 | 44.4 | 55.6 | |
| 2013 | 4509 | 83.2 | 13.8 | 3.0 | 95.2 | 75.4 | 43.3 | 56.7 | |
| 2014 | 4272 | 85.4 | 11.5 | 3.1 | 94.6 | 77.5 | 45.2 | 54.8 | |
| 2015 | 3568 | 85.6 | 12.3 | 2.1 | 94.8 | 78.9 | 45.5 | 54.5 | |
| 2016 | 3171 | 86.8 | 10.1 | 3.1 | 95.7 | 80.5 | 48.0 | 52.0 | |
| 2017 | 2864 | 87.4 | 9.3 | 3.3 | 95.3 | 82.3 | 49.1 | 50.9 | |
| 2018 | 2544 | 86.9 | 9.7 | 3.4 | 95.3 | 84.7 | 49.3 | 50.7 | |
| Others | 2011 | 23 218 | 80.2 | 17.0 | 2.8 | 90.3 | 60.4 | 27.2 | 72.8 |
| 2012 | 28 779 | 65.7 | 15.2 | 19.1 | 91.0 | 61.1 | 27.6 | 72.4 | |
| 2013 | 36 363 | 76.1 | 19.3 | 4.6 | 91.5 | 63.4 | 28.5 | 71.5 | |
| 2014 | 39 854 | 76.6 | 18.2 | 5.1 | 91.9 | 64.9 | 29.7 | 70.3 | |
| 2015 | 41 465 | 78.0 | 17.2 | 4.8 | 92.4 | 65.6 | 29.4 | 70.6 | |
| 2016 | 43 523 | 79.4 | 15.8 | 4.8 | 92.7 | 67.3 | 30.3 | 69.7 | |
| 2017 | 45 622 | 80.1 | 14.8 | 5.1 | 93.1 | 69.7 | 32.3 | 67.7 | |
| 2018 | 46 587 | 80.2 | 14.2 | 5.7 | 93.8 | 71.2 | 33.1 | 66.9 | |
TABLE 3.
Number of surgeries and mortality rates according to organ treated using the selected 115 gastrointestinal operative procedures
| Organ | Year | No. surgeries | Number of postoperative complicationsa/rate (%) | Number of postoperative 30‐d mortalities/rate (%) | Number of postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|
| Esophagus | 2011 | 7246 | 1294/17.9 | 87/1.2 | 279/3.9 |
| 2012 | 8819 | 1653/18.7 | 117/1.3 | 315/3.6 | |
| 2013 | 8642 | 1593/18.4 | 121/1.4 | 327/3.8 | |
| 2014 | 9021 | 1679/18.6 | 115/1.3 | 289/3.2 | |
| 2015 | 8943 | 1709/19.1 | 103/1.2 | 304/3.4 | |
| 2016 | 9212 | 1805/19.6 | 100/1.1 | 238/2.6 | |
| 2017 | 9359 | 1938/20.7 | 108/1.2 | 208/2.2 | |
| 2018 | 9286 | 2065/22.2 | 108/1.2 | 246/2.6 | |
| Stomach and duodenum | 2011 | 66 740 | 5354/8.0 | 992/1.5 | 2183/3.3 |
| 2012 | 76 186 | 6447/8.5 | 1085/1.4 | 2381/3.1 | |
| 2013 | 75 583 | 6380/8.4 | 1059/1.4 | 2269/3.0 | |
| 2014 | 74 920 | 6328/8.4 | 1064/1.4 | 2174/2.9 | |
| 2015 | 73 877 | 6418/8.7 | 1007/1.4 | 2110/2.9 | |
| 2016 | 72 234 | 6413/8.9 | 1066/1.5 | 2016/2.8 | |
| 2017 | 68 287 | 6455/9.5 | 1046/1.5 | 1863/2.7 | |
| 2018 | 65 152 | 6228/9.6 | 1048/1.6 | 1833/2.8 | |
| 2011 | 151 143 | 12 184/8.1 | 2943/1.9 | 5390/3.6 | |
| 2012 | 184 810 | 15 395/8.3 | 3564/1.9 | 6583/3.6 | |
| 2013 | 198 677 | 16 709/8.4 | 3723/1.9 | 6803/3.4 | |
| 2014 | 206 857 | 17 776/8.6 | 3822/1.9 | 6961/3.4 | |
| 2015 | 214 453 | 18 372/8.6 | 4019/1.9 | 7092/3.3 | |
| 2016 | 218 228 | 19 020/8.7 | 3933/1.8 | 6621/3.0 | |
| 2017 | 235 359 | 21 854/9.3 | 4588/1.9 | 7118/3.0 | |
| 2018 | 236 496 | 21 881/9.3 | 4452/1.9 | 7116/3.0 | |
| Rectum and anus | 2011 | 41 061 | 3584/8.7 | 395/1.0 | 676/1.6 |
| 2012 | 49 704 | 4488/9.0 | 462/0.9 | 802/1.6 | |
| 2013 | 49 980 | 4684/9.4 | 517/1.0 | 858/1.7 | |
| 2014 | 51 454 | 4711/9.2 | 449/0.9 | 792/1.5 | |
| 2015 | 56 092 | 4986/8.9 | 519/0.9 | 824/1.5 | |
| 2016 | 55 666 | 5194/9.3 | 503/0.9 | 766/1.4 | |
| 2017 | 56 144 | 5600/10.0 | 556/1.0 | 829/1.5 | |
| 2018 | 56 162 | 5622/10.0 | 522/0.9 | 803/1.4 | |
| Liver | 2011 | 22 855 | 1933/8.5 | 309/1.4 | 590/2.6 |
| 2012 | 26 288 | 2454/9.3 | 310/1.2 | 605/2.3 | |
| 2013 | 25 814 | 2549/9.9 | 275/1.1 | 575/2.2 | |
| 2014 | 26 518 | 2466/9.3 | 246/0.9 | 481/1.8 | |
| 2015 | 26 378 | 2537/9.6 | 234/0.9 | 451/1.7 | |
| 2016 | 27 212 | 2543/9.3 | 222/0.8 | 382/1.4 | |
| 2017 | 27 397 | 2724/9.9 | 214/0.8 | 364/1.3 | |
| 2018 | 26 531 | 2737/10.3 | 189/0.7 | 372/1.4 | |
| Gall bladder | 2011 | 103 183 | 3473/3.4 | 483/0.5 | 946/0.9 |
| 2012 | 122 513 | 4587/3.7 | 531/0.4 | 1082/0.9 | |
| 2013 | 129 162 | 4982/3.9 | 546/0.4 | 1130/0.9 | |
| 2014 | 131 182 | 5020/3.8 | 569/0.4 | 1097/0.8 | |
| 2015 | 133 126 | 5231/3.9 | 541/0.4 | 1036/0.8 | |
| 2016 | 137 360 | 5320/3.9 | 559/0.4 | 980/0.7 | |
| 2017 | 138 267 | 5761/4.2 | 576/0.4 | 968/0.7 | |
| 2018 | 139 844 | 5964/4.3 | 584/0.4 | 954/0.7 | |
| Pancreas | 2011 | 13 477 | 1994/14.8 | 175/1.3 | 386/2.9 |
| 2012 | 15 550 | 2595/16.7 | 213/1.4 | 437/2.8 | |
| 2013 | 16 380 | 2917/17.8 | 211/1.3 | 482/2.9 | |
| 2014 | 17 313 | 2966/17.1 | 195/1.1 | 423/2.4 | |
| 2015 | 17 407 | 3229/18.6 | 185/1.1 | 379/2.2 | |
| 2016 | 18 238 | 3543/19.4 | 185/1.0 | 390/2.1 | |
| 2017 | 19 138 | 4076/21.3 | 219/1.1 | 365/1.9 | |
| 2018 | 19 152 | 4309/22.5 | 178/0.9 | 325/1.7 | |
| Spleen | 2011 | 3609 | 400/11.1 | 83/2.3 | 137/3.8 |
| 2012 | 4142 | 528/12.7 | 84/2.0 | 138/3.3 | |
| 2013 | 4509 | 575/12.8 | 79/1.8 | 139/3.1 | |
| 2014 | 4272 | 549/12.9 | 88/2.1 | 137/3.2 | |
| 2015 | 3568 | 543/15.2 | 88/2.5 | 144/4.0 | |
| 2016 | 3171 | 449/14.2 | 76/2.4 | 117/3.7 | |
| 2017 | 2864 | 434/15.2 | 65/2.3 | 89/3.1 | |
| 2018 | 2544 | 418/16.4 | 69/2.7 | 104/4.1 | |
| Others | 2011 | 23 218 | 3494/15.0 | 1163/5.0 | 1887/8.1 |
| 2012 | 28 779 | 4388/15.2 | 1399/4.9 | 2293/8.0 | |
| 2013 | 36 363 | 4712/13.0 | 1401/3.9 | 2346/6.5 | |
| 2014 | 39 854 | 5176/13.0 | 1521/3.8 | 2489/6.2 | |
| 2015 | 41 465 | 5380/13.0 | 1541/3.7 | 2545/6.1 | |
| 2016 | 43 523 | 5975/13.7 | 1760/4.0 | 2684/6.2 | |
| 2017 | 45 622 | 6539/14.3 | 1909/4.2 | 2699/5.9 | |
| 2018 | 46 587 | 6645/14.3 | 1865/4.0 | 2710/5.8 |
Complications were defined by Clavien‐Dindo gradeⅢa‐Ⅴ.
FIGURE 1.
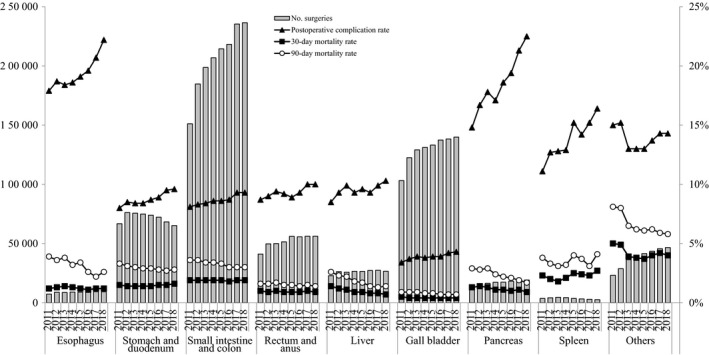
Annual changes of number of surgeries, 30‐Day mortality, operative mortality, and complications: Analysis of 115 surgical procedures. Postoperative complication rate: the rate of Clavien–Dindo (C–D) classification grade III (complications requiring intervention) or higher complications
TABLE 4.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (esophagus)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities /rate (%) | No. postoperative 30‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Esophagus | Low | Cervical periesophageal abscess drainage | 40 | 5/12.5 | 13/32.5 | 2/5.0 | 2/5.0 |
| Med | Esophageal suture (perforation, injury) | 211 | 22/10.4 | 81/38.4 | 9/4.3 | 12/5.7 | |
| Med | Thoracic periesophageal abscess drainage | 27 | 1/3.7 | 15/55.6 | 1/3.7 | 3/11.1 | |
| Med | Esophageal foreign body extraction | 36 | 2/5.6 | 9/25.0 | 1/2.8 | 2/5.6 | |
| Med | Esophageal diverticulum resection | 53 | 26/49.1 | 2/3.8 | 0/0.0 | 0/0 | |
| Med | Benign esophageal tumor removal | 76 | 48/63.2 | 5/6.6 | 0/0 | 1/1.3 | |
| Med | Esophageal resection (removal only) | 687 | 403/58.7 | 102/14.8 | 12/1.7 | 31/4.5 | |
| Med | Esophageal reconstruction: reconstruction only (gastric tube reconstruction) | 647 | 372/57.5 | 157/24.3 | 7/1.1 | 15/2.3 | |
| Med | Esophageal fistula construction | 192 | 69/35.9 | 56/29.2 | 11/5.7 | 22/11.5 | |
| Med | Esophagocardioplasty | 306 | 210/68.6 | 19/6.2 | 2/0.7 | 2/0.7 | |
| Med | Achalasia surgery | 232 | 162/69.8 | 2/0.9 | 0/0 | 0/0 | |
| High | Esophagectomy | 6207 | 3788/61.0 | 1420/22.9 | 53/0.9 | 115/1.9 | |
| High | Esophageal reconstruction: reconstruction only (colon reconstruction) | 31 | 15/48.4 | 10/32.3 | 0/0 | 2/6.5 | |
| High | Esophageal bypass | 152 | 18/11.8 | 55/36.2 | 6/3.9 | 18/11.8 | |
| High | Bronchoesophageal fistula surgery | 3 | 1/33.3 | 2/66.7 | 0/0 | 0/0 | |
| High | Secondary esophageal reconstruction | 386 | 39/10.1 | 117/30.3 | 4/1.0 | 21/5.4 |
TABLE 5.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (stomach and duodenum)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Stomach and duodenum | Low | Gastrostomy and suture gastrorrhaphy | 61 | 9/14.8 | 3/4.9 | 3/4.9 | 3/4.9 |
| Low | Diverticulum, polypectomy (excluding endoscopic resection) | 169 | 19/11.2 | 19/11.2 | 2/1.2 | 3/1.8 | |
| Low | Truncal vagotomy | 4 | 2/50.0 | 1/25.0 | 1/25.0 | 1/25.0 | |
| Low | Gastroenterostomy (Including duodenal jejunostomy) | 5882 | 1406/23.9 | 974/16.6 | 300/5.1 | 615/10.5 | |
| Low | Gastric fistula construction (Excluding PEG) | 1560 | 244/15.6 | 303/19.4 | 98/6.3 | 162/10.4 | |
| Low | Gastric pyloroplasty | 66 | 12/18.2 | 8/12.1 | 1/1.5 | 2/3.0 | |
| Low | Gastric volvulus (volvulus) surgery and rectopexy | 53 | 29/54.7 | 4/7.5 | 0/0 | 0/0 | |
| Low | Gastric suture (including gastric suture for gastric rupture, Suture closure for gastroduodenal perforation, omental implantation and omental transposition) | 5801 | 1975/34.0 | 925/15.9 | 250/4.3 | 361/6.2 | |
| Low | Local gastrectomy (including wedge resection)) | 4338 | 2925/67.4 | 135/3.1 | 18/0.4 | 28/0.6 | |
| Med | Gastrectomy (including distal gastrectomy, pylorus preserving gastrectomy and segmental [transverse] gastrectomy) | 33 988 | 16 355/48.1 | 2327/6.8 | 227/0.7 | 393/1.2 | |
| Med | Selective vagotomy | 7 | 2/28.6 | 0/0 | 0/0 | 0/0 | |
| High | Total gastrectomy (including fundusectomy)) | 13 223 | 3344/25.3 | 1529/11.6 | 148/1.1 | 265/2.0 | |
| High | Left upper abdominal exenteration | 0 | 0/0 | 0/0 | 0/0 | 0/0 |
TABLE 6.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (small intestine and colon)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Small intestine and colon | Low | Enterotomy and enterorrhaphy | 4501 | 684/15.2 | 791/17.6 | 183/4.1 | 392/8.7 |
| Low | Disinvagination (invasive) | 225 | 62/27.6 | 20/8.9 | 12/5.3 | 13/5.8 | |
| Low | Partial enterectomy (benign) | 9381 | 1601/17.1 | 1845/19.7 | 572/6.1 | 830/8.8 | |
| Low | Ileocecal resection (benign) | 4784 | 1765/36.9 | 452/9.4 | 83/1.7 | 118/2.5 | |
| Low | Partial colectomy and sigmoid colectomy (benign) | 8073 | 2319/28.7 | 1243/15.4 | 301/3.7 | 430/5.3 | |
| Low | Appendectomy | 54 877 | 35 558/64.8 | 1001/1.8 | 58/0.1 | 89/0.2 | |
| Low | Enterostomy and closure (without enterectomy) | 26 086 | 8163/31.3 | 4482/17.2 | 1013/3.9 | 1796/6.9 | |
| Med | Enterectomy (malignant) | 3717 | 927/24.9 | 446/12.0 | 85/2.3 | 157/4.2 | |
| Med | Ileocecal resection (malignant) | 13 858 | 7995/57.7 | 756/5.5 | 87/0.6 | 162/1.2 | |
| Med | Partial colectomy and sigmoid colectomy (malignant) | 32 212 | 18 626/57.8 | 2176/6.8 | 199/0.6 | 336/1.0 | |
| Med | Right hemicolectomy | 22 610 | 11 165/49.4 | 1679/7.4 | 276/1.2 | 424/1.9 | |
| Med | Left hemicolectomy | 6072 | 2964/48.8 | 667/11.0 | 124/2.0 | 177/2.9 | |
| Med | Total colectomy | 1760 | 489/27.8 | 404/23.0 | 144/8.2 | 179/10.2 | |
| Med | Intestinal obstruction surgery (with bowel resection) | 24 572 | 5248/21.4 | 2532/10.3 | 577/2.3 | 835/3.4 | |
| Med | Enterostomy and closure (with enterectomy) | 23 313 | 3722/16.0 | 3325/14.3 | 734/3.1 | 1173/5.0 | |
| High | Proctocolectomy and ileoanal (canal) anastomosis | 455 | 195/42.9 | 62/13.6 | 4/0.9 | 5/1.1 |
TABLE 7.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (rectum and anus)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Rectum | Low | Transanal rectal tumor removal | 3751 | 103/2.7 | 22/0.6 | 2/0.1 | 3/0.1 |
| Low | Proctocele surgery (transanal) | 2870 | 29/1.0 | 49/1.7 | 9/0.3 | 14/0.5 | |
| Med | Rectectomy (benign) | 1371 | 118/8.6 | 265/19.3 | 23/1.7 | 43/3.1 | |
| Med | High anterior resection | 10 741 | 7081/65.9 | 744/6.9 | 50/0.5 | 78/0.7 | |
| Med | Hartmann's procedure | 6075 | 1040/17.1 | 1238/20.4 | 309/5.1 | 448/7.4 | |
| Med | Proctocele surgery (abdominoperineal) | 1993 | 1058/53.1 | 31/1.6 | 9/0.5 | 10/0.5 | |
| Med | Malignant anorectal tumor excision (transanal) | 663 | 80/12.1 | 15/2.3 | 1/0.2 | 1/0.2 | |
| Med | Anal sphincteroplasty (by tissue replacement) | 2641 | 15/0.6 | 16/0.6 | 4/0.2 | 6/0.2 | |
| High | Rectectomy (malignant) | 4935 | 3144/63.7 | 660/13.4 | 23/0.5 | 49/1.0 | |
| High | Low anterior resection | 20 636 | 13 825/67.0 | 2454/11.9 | 90/0.4 | 142/0.7 | |
| High | Pelvic evisceration | 441 | 85/19.3 | 121/27.4 | 2/0.5 | 9/2.0 | |
| High | Anorectal malignant tumor excision (posterior approach) | 45 | 5/11.1 | 7/15.6 | 0/0 | 0/0 |
TABLE 8.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (liver)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐day mortalities/rate (%) | No. postoperative 90‐day mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Liver | Low | Hepatorrhaphy | 54 | 3/5.6 | 21/38.9 | 8/14.8 | 9/16.7 |
| Low | Liver abscess drainage (excluding percutaneous procedures) | 47 | 4/8.5 | 9/19.1 | 0/0.0 | 1/2.1 | |
| Low | Hepatic cyst resection. Suture. Drainage | 794 | 618/77.8 | 42/5.3 | 3/0.4 | 5/0.6 | |
| Low | Partial hepatectomy | 12 543 | 4072/32.5 | 940/7.5 | 52/0.4 | 96/0.8 | |
| Low | Liver biopsy (excluding percutaneous procedures) | 235 | 41/17.4 | 10/4.3 | 4/1.7 | 7/3.0 | |
| Low | Liver coagulonecrotic therapy (excluding percutaneous procedures) | 705 | 143/20.3 | 57/8.1 | 6/0.9 | 15/2.1 | |
| Med | Lateral segmentectomy of the liver | 1626 | 564/34.7 | 90/5.5 | 5/0.3 | 14/0.9 | |
| Med | Esophageal and gastric varix surgery | 42 | 29/69.0 | 5/11.9 | 1/2.4 | 2/4.8 | |
| High | Hepatectomy (segmented or more; excluding lateral segments) | 7192 | 791/11.0 | 1137/15.8 | 83/1.2 | 163/2.3 | |
| High | Systematic subsegmentectomy | 2474 | 455/18.4 | 210/8.5 | 7/0.3 | 23/0.9 | |
| High | Liver transplant | 705 | 1/0.1 | 165/23.4 | 17/2.4 | 33/4.7 | |
| High | Hepatopancreatoduodenectomy | 114 | 2/1.8 | 51/44.7 | 3/2.6 | 4/3.5 |
TABLE 9.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (gall bladder)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Gall bladder | Low | Cholangiotomy | 100 | 10/10.0 | 16/16.0 | 1/1.0 | 1/1.0 |
| Low | Cysticolithectomy | 60 | 8/13.3 | 12/20.0 | 1/1.7 | 1/1.7 | |
| Low | Cholecystectomy | 132 548 | 90 831/68.5 | 4782/3.6 | 469/0.4 | 735/0.6 | |
| Low | External cholecystostomy | 121 | 16/13.2 | 27/22.3 | 10/8.3 | 15/12.4 | |
| Low | Cystoenteric anastomosis | 53 | 8/15.1 | 12/22.6 | 2/3.8 | 5/9.4 | |
| Med | Cysticolithectomy | 2664 | 693/26.0 | 248/9.3 | 25/0.9 | 55/2.1 | |
| Med | Biliary tract reconstruction | 336 | 13/3.9 | 75/22.3 | 2/0.6 | 3/0.9 | |
| Med | Biliary bypass | 1210 | 67/5.5 | 187/15.5 | 31/2.6 | 62/5.1 | |
| Med | Cholangioplasty | 113 | 16/14.2 | 22/19.5 | 3/2.7 | 6/5.3 | |
| Med | Duodenal papilloplasty | 32 | 1/3.1 | 6/18.8 | 0/0 | 0/0 | |
| Med | Choledocal dilatation | 289 | 45/15.6 | 29/10.0 | 0/0.0 | 1/0.3 | |
| Med | Biliary fistula closure | 38 | 7/18.4 | 8/21.1 | 1/2.6 | 1/2.6 | |
| High | Malignant gallbladder tumor surgery (excluding simple cholecystectomy)) | 1007 | 39/3.9 | 117/11.6 | 6/0.6 | 8/0.8 | |
| High | Malignant bile duct tumor surgery | 1263 | 12/1.0 | 423/33.5 | 33/2.6 | 61/4.8 | |
| High | Biliary atresia surgery | 10 | 0/0 | 0/0 | 0/0 | 0/0 |
TABLE 10.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (pancreas)
| Organ | Degree of difficulty | Procedure | No. of surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Pancreas | Low | External pancreatic cyst drainage | 21 | 4/19.0 | 11/52.4 | 1/4.8 | 2/9.5 |
| Low | External pancreatic duct drainage | 6 | 0/0.0 | 2/33.3 | 0/0.0 | 1/16.7 | |
| Med | Pancreatorrhaphy | 13 | 0/0.0 | 8/61.5 | 3/23.1 | 4/30.8 | |
| Med | Partial pancreatic resection | 162 | 36/22.2 | 36/22.2 | 0/0.0 | 1/0.6 | |
| Med | Distal pancreatectomy (benign) | 1493 | 599/40.1 | 293/19.6 | 5/0.3 | 9/0.6 | |
| Med | Pancreatoenteric anastomosis | 28 | 1/3.6 | 3/10.7 | 1/3.6 | 2/7.1 | |
| Med | Pancreatic (duct) anastomosis | 286 | 4/1.4 | 48/16.8 | 7/2.4 | 9/3.1 | |
| Med | Acute pancreatitis surgery | 88 | 8/9.1 | 41/46.6 | 5/5.7 | 12/13.6 | |
| Med | Pancreatolithiasis surgery | 8 | 0/0 | 1/12.5 | 0/0 | 0/0 | |
| Med | Plexus pancreaticus capitalis resection | 0 | 0/ | 0/ | 0/ | 0/ | |
| High | Pancreaticoduodenectomy | 11 626 | 194/1.7 | 2716/23.4 | 111/1.0 | 204/1.8 | |
| High | Distal pancreatectomy (malignant)) | 4611 | 795/17.2 | 971/21.1 | 19/0.4 | 42/0.9 | |
| High | Total pancreatectomy | 599 | 9/1.5 | 105/17.5 | 25/4.2 | 38/6.3 | |
| High | Duodenum preserving pancreas head resection | 49 | 0/0.0 | 14/28.6 | 0/0.0 | 0/0 | |
| High | Segmental pancreatic resection | 136 | 5/3.7 | 52/38.2 | 1/0.7 | 1/0.7 | |
| High | Distal pancreatectomy | 26 | 0/0 | 8/30.8 | 0/0 | 0/0 |
TABLE 11.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (spleen)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Spleen | Low | Splenorrhaphy | 23 | 4/17.4 | 6/26.1 | 1/4.3 | 1/4.3 |
| Med | Splenectomy | 2490 | 694/27.9 | 409/16.4 | 68/2.7 | 103/4.1 | |
| Med | Partial splenic resection | 31 | 16/51.6 | 3/9.7 | 0/0 | 0/0 |
TABLE 12.
Number of surgeries, endoscopic surgery, and mortality rates according to the selected 115 gastrointestinal operative procedures in 2018 (other)
| Organ | Degree of difficulty | Procedure | No. surgeries | No. Endoscopic surgeries/ rate (%) | No. postoperative complications*/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|---|
| Other | Low | Localized intra‐abdominal abscess surgery | 2617 | 645/24.6 | 400/15.3 | 56/2.1 | 114/4.4 |
| Low | Exploratory laparotomy | 10 825 | 5335/49.3 | 1329/12.3 | 515/4.8 | 718/6.6 | |
| Med | Acute diffuse peritonitis surgery | 14 835 | 2820/19.0 | 3943/26.6 | 1117/7.5 | 1617/10.9 | |
| Med | Ventral hernia surgery | 13 768 | 3931/28.6 | 497/3.6 | 84/0.6 | 117/0.8 | |
| Med | Diaphragm suture | 243 | 76/31.3 | 30/12.3 | 4/1.6 | 6/2.5 | |
| Med | Esophageal hiatus hernia surgery | 1033 | 668/64.7 | 81/7.8 | 19/1.8 | 25/2.4 | |
| Med | Retroperitoneal tumor surgery | 866 | 129/14.9 | 60/6.9 | 5/0.6 | 10/1.2 | |
| Med | Abdominal wall/mesenteric/omental tumor resection | 1832 | 422/23.0 | 151/8.2 | 25/1.4 | 41/2.2 | |
| Med | Gastrointestinal perforation closure | 511 | 60/11.7 | 149/29.2 | 39/7.6 | 59/11.5 | |
| High | Diaphragmatic hiatus hernia surgery | 57 | 17/29.8 | 5/8.8 | 1/1.8 | 3/5.3 |
3.2. Eight main operative procedures
The number of surgeries carried out annually for the eight main operative procedures, the percentage by gender, and the percentage according to age group between 2011 and 2018 are shown in Table 13. The percentages of elderly patients have been increasing, especially for gastrectomy (distal and total), right hemicolectomy, and acute diffuse peritonitis surgery. Regarding the Institutional groups in which surgeries were performed, more than 70% of the surgeries were performed at certified institutions, and more than 90% were for esophagectomy, hepatectomy (non‐lateral segments), and pancreaticoduodenectomy in 2018 (Table 14). Board‐certified surgeon participation rates have been increasing year by year for all procedures. Table 15 shows the morbidity and mortality rates of the eight main operative procedures. Other than acute diffuse peritonitis surgery, the postoperative 30‐day mortality rate was 0.4%‐1.2% and the operative mortality rate was 0.7%‐2.3%; a very low level relatively. The postoperative 30‐day mortality rate and operative mortality rate for acute diffuse peritonitis surgery was 7.5% and 10.9% in 2018, respectively. Figure 2 shows the annual changes in the number of surgeries, postoperative complication rate, and mortalities. Although the complication rates were increasing for esophagectomy (22.9% in 2018) and pancreaticoduodenectomy (23.4%), the mortality rates for these procedures (0.9% and 1.9%, 1.0% and 1.8%, in 2018, respectively) were decreasing. The case numbers for acute diffuse peritonitis surgery were increasing; however, the morbidity and mortality rates were decreasing.
TABLE 13.
Annual changes of surgeries by sex, age group, and organ for eight main operative procedures
| Procedure | Year | No. surgeries | Percentage by sex | Percentage according to age group (y) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Male | Female | <60 | 60 to < 65 | 65 to < 70 | 70 to < 75 | 75 to < 80 | ≥80 | |||
| Esophagectomy | 2011 | 4916 | 84.1 | 15.9 | 20.4 | 20.8 | 22.5 | 19.4 | 12.2 | 4.7 |
| 2012 | 5946 | 84.4 | 15.6 | 19.7 | 21.3 | 20.7 | 20.3 | 13.1 | 4.9 | |
| 2013 | 5694 | 83.6 | 16.4 | 18.3 | 18.3 | 22.6 | 21.3 | 13.8 | 5.8 | |
| 2014 | 6091 | 84.0 | 16.0 | 18.7 | 17.8 | 22.8 | 22.0 | 13.4 | 5.2 | |
| 2015 | 6060 | 82.9 | 17.1 | 17.9 | 16.3 | 23.6 | 23.5 | 13.1 | 5.7 | |
| 2016 | 6041 | 81.7 | 18.3 | 17.8 | 15.8 | 25.3 | 21.6 | 14.3 | 5.2 | |
| 2017 | 6100 | 82.3 | 17.7 | 17.0 | 14.6 | 25.6 | 20.6 | 15.8 | 6.3 | |
| 2018 | 6207 | 80.5 | 19.5 | 17.2 | 14.2 | 22.6 | 22.8 | 16.8 | 6.5 | |
| Gastrectomy (distal) | 2011 | 34 160 | 66.6 | 33.4 | 18.1 | 15.0 | 14.2 | 17.4 | 16.8 | 18.5 |
| 2012 | 38 750 | 66.9 | 33.1 | 16.9 | 14.8 | 15.0 | 17.8 | 16.5 | 18.8 | |
| 2013 | 39 957 | 66.7 | 33.3 | 16.3 | 13.5 | 15.8 | 17.8 | 17.6 | 19.0 | |
| 2014 | 38 584 | 66.4 | 33.6 | 15.7 | 12.4 | 16.6 | 18.4 | 17.3 | 19.5 | |
| 2015 | 37 819 | 66.6 | 33.4 | 14.8 | 11.3 | 17.5 | 18.2 | 17.5 | 20.6 | |
| 2016 | 36 852 | 66.6 | 33.4 | 14.5 | 10.4 | 18.5 | 17.6 | 17.4 | 21.6 | |
| 2017 | 35 517 | 66.8 | 33.2 | 13.4 | 9.9 | 18.0 | 18.1 | 18.0 | 22.6 | |
| 2018 | 33 988 | 66.6 | 33.4 | 12.9 | 9.1 | 16.9 | 19.0 | 18.1 | 24.0 | |
| Total gastrectomy | 2011 | 18 652 | 73.7 | 26.3 | 16.6 | 14.7 | 16.0 | 19.7 | 18.0 | 15.0 |
| 2012 | 21 122 | 74.2 | 25.8 | 15.5 | 14.8 | 15.7 | 19.2 | 18.5 | 16.3 | |
| 2013 | 19 035 | 74.0 | 26.0 | 14.7 | 13.5 | 16.9 | 19.4 | 19.2 | 16.3 | |
| 2014 | 19 071 | 73.7 | 26.3 | 14.0 | 12.3 | 17.2 | 20.1 | 18.9 | 17.5 | |
| 2015 | 18 695 | 74.5 | 25.5 | 13.7 | 11.1 | 18.9 | 20.8 | 18.2 | 17.4 | |
| 2016 | 17 670 | 74.4 | 25.6 | 12.6 | 10.3 | 19.6 | 19.5 | 19.0 | 19.0 | |
| 2017 | 14 840 | 74.2 | 25.8 | 12.2 | 9.9 | 19.0 | 19.6 | 19.8 | 19.5 | |
| 2018 | 13 223 | 74.4 | 25.6 | 10.8 | 9.1 | 18.0 | 20.6 | 20.6 | 20.9 | |
| Right hemicolectomy | 2011 | 17 890 | 50.5 | 49.5 | 12.8 | 11.6 | 13.1 | 17.3 | 18.8 | 26.5 |
| 2012 | 21 034 | 50.3 | 49.7 | 13.1 | 10.9 | 13.1 | 17.0 | 19.0 | 26.9 | |
| 2013 | 21 814 | 50.6 | 49.4 | 13.0 | 10.0 | 13.4 | 17.6 | 18.9 | 27.1 | |
| 2014 | 22 446 | 50.6 | 49.4 | 12.0 | 9.2 | 13.8 | 18.2 | 18.6 | 28.2 | |
| 2015 | 22 850 | 50.5 | 49.5 | 11.5 | 8.6 | 14.6 | 18.1 | 18.1 | 29.1 | |
| 2016 | 22 829 | 51.3 | 48.7 | 11.4 | 7.7 | 15.9 | 16.7 | 18.5 | 29.8 | |
| 2017 | 22 543 | 50.9 | 49.1 | 11.3 | 7.4 | 14.9 | 16.3 | 19.3 | 30.8 | |
| 2018 | 22 610 | 51.4 | 48.6 | 10.7 | 6.9 | 13.9 | 17.7 | 19.6 | 31.2 | |
| Low anterior resection | 2011 | 16 984 | 64.8 | 35.2 | 24.1 | 18.5 | 16.5 | 16.2 | 12.9 | 11.7 |
| 2012 | 20 321 | 64.8 | 35.2 | 24.2 | 17.6 | 16.5 | 16.6 | 13.1 | 12.0 | |
| 2013 | 21 096 | 64.2 | 35.8 | 23.8 | 16.5 | 17.4 | 16.9 | 13.5 | 11.8 | |
| 2014 | 21 861 | 64.8 | 35.2 | 23.1 | 15.7 | 18.3 | 17.9 | 13.1 | 11.9 | |
| 2015 | 22 493 | 64.4 | 35.6 | 23.5 | 14.2 | 19.6 | 17.1 | 13.6 | 12.0 | |
| 2016 | 21 387 | 64.4 | 35.6 | 23.4 | 13.6 | 20.7 | 16.8 | 13.2 | 12.2 | |
| 2017 | 20 879 | 64.2 | 35.8 | 23.2 | 12.6 | 20.9 | 16.7 | 13.5 | 13.2 | |
| 2018 | 20 636 | 64.9 | 35.1 | 22.9 | 12.5 | 19.3 | 18.0 | 14.4 | 12.9 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7434 | 70.4 | 29.6 | 20.1 | 16.4 | 16.5 | 20.4 | 18.0 | 8.7 |
| 2012 | 8239 | 69.5 | 30.5 | 19.8 | 16.1 | 17.4 | 19.5 | 18.5 | 8.8 | |
| 2013 | 7937 | 69.4 | 30.6 | 19.4 | 14.2 | 18.0 | 20.3 | 18.2 | 9.9 | |
| 2014 | 7666 | 69.2 | 30.8 | 18.5 | 13.8 | 18.5 | 21.5 | 17.6 | 10.0 | |
| 2015 | 7439 | 68.9 | 31.1 | 18.7 | 12.5 | 19.3 | 20.9 | 17.6 | 11.1 | |
| 2016 | 7610 | 68.7 | 31.3 | 18.0 | 11.9 | 21.1 | 20.4 | 17.5 | 11.1 | |
| 2017 | 7698 | 69.5 | 30.5 | 17.2 | 11.3 | 20.5 | 20.4 | 18.7 | 11.9 | |
| 2018 | 7192 | 69.5 | 30.5 | 17.2 | 9.6 | 19.1 | 21.4 | 19.4 | 13.3 | |
| Pancreaticoduodenectomy | 2011 | 8305 | 61.9 | 38.1 | 16.1 | 16.0 | 17.3 | 20.9 | 18.8 | 10.9 |
| 2012 | 9329 | 62.0 | 38.0 | 14.7 | 15.8 | 18.0 | 20.6 | 20.2 | 10.6 | |
| 2013 | 10 068 | 60.9 | 39.1 | 14.0 | 12.6 | 19.6 | 22.5 | 19.4 | 11.8 | |
| 2014 | 10 400 | 59.5 | 40.5 | 18.4 | 12.4 | 19.0 | 21.0 | 18.2 | 11.1 | |
| 2015 | 10 576 | 60.7 | 39.3 | 14.2 | 11.7 | 20.0 | 22.9 | 19.3 | 12.0 | |
| 2016 | 11 028 | 61.1 | 38.9 | 14.2 | 10.3 | 20.6 | 21.8 | 20.3 | 12.7 | |
| 2017 | 11 580 | 61.1 | 38.9 | 13.8 | 9.8 | 20.4 | 20.8 | 21.6 | 13.6 | |
| 2018 | 11 626 | 60.3 | 39.7 | 13.3 | 9.1 | 18.9 | 22.2 | 22.0 | 14.6 | |
| Acute diffuse peritonitis surgery | 2011 | 7753 | 60.0 | 40.0 | 31.4 | 11.2 | 9.7 | 11.7 | 13.2 | 22.9 |
| 2012 | 9177 | 61.0 | 39.0 | 30.3 | 11.2 | 10.1 | 11.6 | 13.4 | 23.4 | |
| 2013 | 10 447 | 60.1 | 39.9 | 29.1 | 10.3 | 11.5 | 11.8 | 13.1 | 24.1 | |
| 2014 | 12 085 | 61.2 | 38.8 | 28.4 | 9.5 | 12.2 | 12.3 | 12.9 | 24.7 | |
| 2015 | 13 030 | 59.4 | 40.6 | 28.2 | 8.9 | 12.5 | 13.1 | 12.3 | 25.0 | |
| 2016 | 13 981 | 60.2 | 39.8 | 27.4 | 8.6 | 13.4 | 12.4 | 12.3 | 26.0 | |
| 2017 | 14 423 | 59.4 | 40.6 | 26.5 | 7.8 | 13.0 | 12.0 | 13.6 | 27.1 | |
| 2018 | 14 835 | 59.2 | 40.8 | 26.1 | 7.7 | 12.7 | 13.1 | 13.5 | 26.9 | |
TABLE 14.
Institution and anesthesiologist and specialist participation rates by organ for eight main operative procedures
| Procedure | Year | No. surgeries | Percentage by institution group | Anesthesiologist Participation (%) | Board‐certified Surgeon participation (%) | Medical practitioners (%) | |||
|---|---|---|---|---|---|---|---|---|---|
| Certified institution | Related institution | Other | Board‐certified Surgeons | Non‐board‐certified surgeons | |||||
| Esophagectomy | 2011 | 4916 | 94.2 | 5.3 | 0.5 | 97.6 | 88.4 | 63.5 | 36.5 |
| 2012 | 5946 | 78.3 | 4.9 | 16.8 | 98.1 | 89.0 | 64.8 | 35.2 | |
| 2013 | 5694 | 92.9 | 5.9 | 1.2 | 98.0 | 90.8 | 66.6 | 33.4 | |
| 2014 | 6091 | 93.6 | 4.7 | 1.7 | 98.6 | 92.6 | 70.2 | 29.8 | |
| 2015 | 6060 | 93.6 | 4.6 | 1.8 | 98.5 | 93.5 | 72.1 | 27.9 | |
| 2016 | 6041 | 94.5 | 3.8 | 1.7 | 98.8 | 93.7 | 73.2 | 26.8 | |
| 2017 | 6100 | 95.3 | 3.1 | 1.7 | 98.8 | 94.8 | 74.7 | 25.3 | |
| 2018 | 6207 | 95.9 | 2.7 | 1.4 | 99.1 | 96.6 | 78.8 | 21.2 | |
| Gastrectomy (distal) | 2011 | 34 160 | 81.1 | 16.6 | 2.3 | 93.2 | 71.3 | 37.0 | 63.0 |
| 2012 | 38 750 | 64.5 | 15.2 | 20.3 | 93.9 | 72.5 | 37.9 | 62.1 | |
| 2013 | 39 957 | 76.6 | 19.2 | 4.1 | 93.6 | 76.1 | 40.6 | 59.4 | |
| 2014 | 38 584 | 77.7 | 17.8 | 4.5 | 94.0 | 78.4 | 42.1 | 57.9 | |
| 2015 | 37 819 | 77.3 | 18.3 | 4.4 | 94.1 | 78.1 | 41.3 | 58.7 | |
| 2016 | 36 852 | 80.2 | 15.9 | 4.0 | 95.0 | 81.8 | 43.8 | 56.2 | |
| 2017 | 35 517 | 80.2 | 14.9 | 4.8 | 95.4 | 82.4 | 45.2 | 54.8 | |
| 2018 | 33 988 | 80.7 | 14.4 | 4.8 | 95.6 | 84.2 | 46.6 | 53.4 | |
| Total gastrectomy | 2011 | 18 652 | 80.9 | 16.8 | 2.3 | 93.9 | 71.6 | 37.4 | 62.6 |
| 2012 | 21 122 | 63.0 | 15.3 | 21.7 | 94.3 | 72.1 | 38.0 | 62.0 | |
| 2013 | 19 035 | 77.2 | 18.9 | 3.9 | 94.2 | 75.0 | 39.5 | 60.5 | |
| 2014 | 19 071 | 77.8 | 17.9 | 4.3 | 94.4 | 77.7 | 41.7 | 58.3 | |
| 2015 | 18 695 | 77.9 | 17.9 | 4.1 | 94.5 | 78.2 | 42.6 | 57.4 | |
| 2016 | 17 670 | 80.0 | 15.9 | 4.0 | 95.0 | 81.4 | 45.0 | 55.0 | |
| 2017 | 14 840 | 79.3 | 15.8 | 4.9 | 95.0 | 80.7 | 44.3 | 55.7 | |
| 2018 | 13 223 | 79.6 | 15.5 | 4.9 | 95.4 | 82.6 | 46.2 | 53.8 | |
| Right hemicolectomy | 2011 | 17 890 | 75.7 | 21.2 | 3.1 | 92.7 | 66.0 | 30.5 | 69.5 |
| 2012 | 21 034 | 60.0 | 18.3 | 21.7 | 93.0 | 67.1 | 30.8 | 69.2 | |
| 2013 | 21 814 | 72.1 | 22.3 | 5.6 | 92.9 | 69.7 | 32.6 | 67.4 | |
| 2014 | 22 446 | 71.2 | 23.1 | 5.7 | 93.4 | 71.9 | 33.6 | 66.4 | |
| 2015 | 22 850 | 72.1 | 22.0 | 5.9 | 94.1 | 72.4 | 33.5 | 66.5 | |
| 2016 | 22 829 | 73.8 | 20.1 | 6.1 | 94.5 | 74.2 | 34.3 | 65.7 | |
| 2017 | 22 543 | 75.0 | 18.4 | 6.6 | 94.7 | 76.4 | 37.1 | 62.9 | |
| 2018 | 22 610 | 74.8 | 19.0 | 6.2 | 94.7 | 77.8 | 38.2 | 61.8 | |
| Low anterior resection | 2011 | 16 984 | 79.4 | 17.7 | 2.9 | 93.4 | 72.7 | 41.6 | 58.4 |
| 2012 | 20 321 | 64.0 | 16.2 | 19.7 | 93.8 | 73.0 | 42.3 | 57.7 | |
| 2013 | 21 096 | 76.3 | 19.5 | 4.2 | 93.7 | 75.5 | 44.3 | 55.7 | |
| 2014 | 21 861 | 76.2 | 19.0 | 4.9 | 94.4 | 78.2 | 47.2 | 52.8 | |
| 2015 | 22 493 | 76.9 | 18.3 | 4.8 | 94.6 | 79.2 | 47.7 | 52.3 | |
| 2016 | 21 387 | 79.0 | 16.4 | 4.7 | 95.0 | 81.0 | 48.8 | 51.2 | |
| 2017 | 20 879 | 79.3 | 15.6 | 5.1 | 95.2 | 83.1 | 51.2 | 48.8 | |
| 2018 | 20 636 | 80.9 | 14.3 | 4.8 | 95.2 | 84.5 | 54.4 | 45.6 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7434 | 91.1 | 8.0 | 0.8 | 96.4 | 88.9 | 61.5 | 38.5 |
| 2012 | 8239 | 75.9 | 7.9 | 16.3 | 96.8 | 89.3 | 64.0 | 36.0 | |
| 2013 | 7937 | 88.1 | 9.7 | 2.2 | 96.9 | 91.0 | 65.2 | 34.8 | |
| 2014 | 7666 | 88.2 | 8.7 | 3.1 | 96.7 | 92.3 | 66.6 | 33.4 | |
| 2015 | 7439 | 89.2 | 8.6 | 2.2 | 97.2 | 92.3 | 66.6 | 33.4 | |
| 2016 | 7610 | 90.7 | 7.1 | 2.1 | 97.1 | 93.3 | 67.7 | 32.3 | |
| 2017 | 7698 | 91.2 | 6.6 | 2.2 | 97.7 | 95.1 | 72.3 | 27.7 | |
| 2018 | 7192 | 92.8 | 5.2 | 2.0 | 97.7 | 95.8 | 72.8 | 27.2 | |
| Pancreaticoduodenectomy | 2011 | 8305 | 87.8 | 11.0 | 1.2 | 95.9 | 85.7 | 58.7 | 41.3 |
| 2012 | 9329 | 72.4 | 8.8 | 18.8 | 96.6 | 87.2 | 60.9 | 39.1 | |
| 2013 | 10 068 | 85.9 | 11.7 | 2.4 | 96.0 | 87.9 | 60.5 | 39.5 | |
| 2014 | 10 400 | 86.4 | 10.4 | 3.3 | 96.4 | 90.3 | 62.2 | 37.8 | |
| 2015 | 10 576 | 88.5 | 9.2 | 2.4 | 96.9 | 90.9 | 62.1 | 37.9 | |
| 2016 | 11 028 | 89.4 | 8.3 | 2.3 | 97.1 | 91.7 | 63.3 | 36.7 | |
| 2017 | 11 580 | 90.5 | 7.2 | 2.3 | 97.3 | 93.0 | 65.0 | 35.0 | |
| 2018 | 11 626 | 91.4 | 6.4 | 2.2 | 97.4 | 94.0 | 67.6 | 32.4 | |
| Acute diffuse peritonitis surgery | 2011 | 7753 | 80.6 | 16.9 | 2.4 | 90.0 | 58.5 | 23.5 | 76.5 |
| 2012 | 9177 | 65.2 | 16.4 | 18.4 | 90.4 | 59.4 | 22.7 | 77.3 | |
| 2013 | 10 447 | 77.7 | 18.1 | 4.2 | 91.2 | 62.4 | 23.9 | 76.1 | |
| 2014 | 12 085 | 77.7 | 17.2 | 5.1 | 91.9 | 63.3 | 25.1 | 74.9 | |
| 2015 | 13 030 | 79.8 | 15.9 | 4.3 | 92.2 | 64.5 | 24.9 | 75.1 | |
| 2016 | 13 981 | 82.2 | 13.8 | 4.0 | 93.0 | 66.8 | 26.1 | 73.9 | |
| 2017 | 14 423 | 83.1 | 13.0 | 3.8 | 93.3 | 69.0 | 27.2 | 72.8 | |
| 2018 | 14 835 | 83.4 | 12.4 | 4.2 | 93.6 | 70.4 | 28.7 | 71.3 | |
TABLE 15.
Number of surgeries and mortality rates according to organ treated using the eight main operative procedures
| Procedure | Year | No. surgeries | No. postoperative complications*/rate (%) | No. re‐operation/rate (%) | No. postoperative 30‐d mortalities/rate (%) | No. postoperative 90‐d mortalities/rate (%) |
|---|---|---|---|---|---|---|
| Esophagectomy | 2011 | 4916 | 879/17.9 | 310/6.3 | 55/1.1 | 158/3.2 |
| 2012 | 5946 | 1135/19.1 | 345/5.8 | 63/1.1 | 183/3.1 | |
| 2013 | 5694 | 1067/18.7 | 375/6.6 | 67/1.2 | 161/2.8 | |
| 2014 | 6091 | 1178/19.3 | 367/6.0 | 49/0.8 | 140/2.3 | |
| 2015 | 6060 | 1171/19.3 | 392/6.5 | 57/0.9 | 166/2.7 | |
| 2016 | 6041 | 1240/20.5 | 357/5.9 | 49/0.8 | 109/1.8 | |
| 2017 | 6100 | 1374/22.5 | 355/5.8 | 61/1.0 | 108/1.8 | |
| 2018 | 6207 | 1420/22.9 | 367/5.9 | 53/0.9 | 115/1.9 | |
| Gastrectomy (distal) | 2011 | 34 160 | 1774/5.2 | 709/2.1 | 208/0.6 | 451/1.3 |
| 2012 | 38 750 | 2205/5.7 | 849/2.2 | 232/0.6 | 516/1.3 | |
| 2013 | 39 957 | 2450/6.1 | 892/2.2 | 239/0.6 | 542/1.4 | |
| 2014 | 38 584 | 2356/6.1 | 941/2.4 | 264/0.7 | 523/1.4 | |
| 2015 | 37 819 | 2325/6.1 | 851/2.3 | 222/0.6 | 452/1.2 | |
| 2016 | 36 852 | 2314/6.3 | 825/2.2 | 249/0.7 | 473/1.3 | |
| 2017 | 35 517 | 2445/6.9 | 859/2.4 | 253/0.7 | 437/1.2 | |
| 2018 | 33 988 | 2327/6.8 | 737/2.2 | 227/0.7 | 393/1.2 | |
| Total gastrectomy | 2011 | 18 652 | 1716/9.2 | 634/3.4 | 177/0.9 | 427/2.3 |
| 2012 | 21 122 | 2135/10.1 | 758/3.6 | 224/1.1 | 503/2.4 | |
| 2013 | 19 035 | 1831/9.6 | 642/3.4 | 169/0.9 | 428/2.2 | |
| 2014 | 19 071 | 1840/9.6 | 698/3.7 | 185/1.0 | 379/2.0 | |
| 2015 | 18 695 | 1907/10.2 | 654/3.5 | 178/1.0 | 387/2.1 | |
| 2016 | 17 670 | 1835/10.4 | 638/3.6 | 174/1.0 | 336/1.9 | |
| 2017 | 14 840 | 1702/11.5 | 514/3.5 | 161/1.1 | 293/2.0 | |
| 2018 | 13 223 | 1529/11.6 | 487/3.7 | 148/1.1 | 265/2.0 | |
| Right hemicolectomy | 2011 | 17 890 | 1150/6.4 | 588/3.3 | 213/1.2 | 410/2.3 |
| 2012 | 21 034 | 1470/7.0 | 677/3.2 | 263/1.3 | 471/2.2 | |
| 2013 | 21 814 | 1527/7.0 | 721/3.3 | 280/1.3 | 538/2.5 | |
| 2014 | 22 446 | 1544/6.9 | 771/3.4 | 287/1.3 | 530/2.4 | |
| 2015 | 22 850 | 1607/7.0 | 769/3.4 | 301/1.3 | 534/2.3 | |
| 2016 | 22 829 | 1510/6.6 | 791/3.5 | 253/1.1 | 449/2.0 | |
| 2017 | 22 543 | 1648/7.3 | 785/3.5 | 296/1.3 | 450/2.0 | |
| 2018 | 22 610 | 1679/7.4 | 740/3.3 | 276/1.2 | 424/1.9 | |
| Low anterior resection | 2011 | 16 984 | 1616/9.5 | 1213/7.1 | 75/0.4 | 136/0.8 |
| 2012 | 20 321 | 2092/10.3 | 1413/6.9 | 88/0.4 | 149/0.7 | |
| 2013 | 21 096 | 2059/9.8 | 1473/7.0 | 80/0.4 | 175/0.8 | |
| 2014 | 21 861 | 2098/9.6 | 1546/7.1 | 70/0.3 | 152/0.7 | |
| 2015 | 22 493 | 2210/9.8 | 1550/6.9 | 95/0.4 | 156/0.7 | |
| 2016 | 21 387 | 2306/10.8 | 1492/7.0 | 68/0.3 | 126/0.6 | |
| 2017 | 20 879 | 2376/11.4 | 1330/6.4 | 96/0.5 | 148/0.7 | |
| 2018 | 20 636 | 2454/11.9 | 1424/6.9 | 90/0.4 | 142/0.7 | |
| Hepatectomy (non‐lateral segments) | 2011 | 7434 | 886/11.9 | 203/2.7 | 155/2.1 | 303/4.1 |
| 2012 | 8239 | 1146/13.9 | 248/3.0 | 142/1.7 | 293/3.6 | |
| 2013 | 7937 | 1135/14.3 | 226/2.8 | 130/1.6 | 290/3.7 | |
| 2014 | 7666 | 1052/13.7 | 242/3.2 | 94/1.2 | 208/2.7 | |
| 2015 | 7439 | 1049/14.1 | 213/2.9 | 87/1.2 | 182/2.4 | |
| 2016 | 7610 | 1046/13.7 | 220/2.9 | 96/1.3 | 178/2.3 | |
| 2017 | 7698 | 1160/15.1 | 221/2.9 | 97/1.3 | 169/2.2 | |
| 2018 | 7192 | 1137/15.8 | 211/2.9 | 83/1.2 | 163/2.3 | |
| Pancreaticoduodenectomy | 2011 | 8305 | 1285/15.5 | 299/3.6 | 97/1.2 | 238/2.9 |
| 2012 | 9329 | 1654/17.7 | 365/3.9 | 137/1.5 | 281/3.0 | |
| 2013 | 10 068 | 1853/18.4 | 407/4.0 | 142/1.4 | 307/3.0 | |
| 2014 | 10 400 | 1847/17.8 | 374/3.6 | 111/1.1 | 267/2.6 | |
| 2015 | 10 576 | 2025/19.1 | 378/3.6 | 120/1.1 | 247/2.3 | |
| 2016 | 11 028 | 2242/20.3 | 393/3.6 | 98/0.9 | 232/2.1 | |
| 2017 | 11 580 | 2539/21.9 | 413/3.6 | 145/1.3 | 232/2.0 | |
| 2018 | 11 626 | 2716/23.4 | 402/3.5 | 111/1.0 | 204/1.8 | |
| Acute diffuse peritonitis surgery | 2011 | 7753 | 2022/26.1 | 634/8.2 | 697/9.0 | 1096/14.1 |
| 2012 | 9177 | 2456/26.8 | 685/7.5 | 785/8.6 | 1289/14.0 | |
| 2013 | 10 447 | 2652/25.4 | 786/7.5 | 861/8.2 | 1408/13.5 | |
| 2014 | 12 085 | 2966/24.5 | 937/7.8 | 927/7.7 | 1472/12.2 | |
| 2015 | 13 030 | 3126/24.0 | 1051/8.1 | 943/7.2 | 1551/11.9 | |
| 2016 | 13 981 | 3445/24.6 | 1068/7.6 | 1052/7.5 | 1572/11.2 | |
| 2017 | 14 423 | 3756/26.0 | 1125/7.8 | 1152/8.0 | 1575/10.9 | |
| 2018 | 14 835 | 3943/26.6 | 1183/8.0 | 1117/7.5 | 1617/10.9 |
Complications were defined by Clavien‐Dindo gradeⅢa‐Ⅴ.
FIGURE 2.
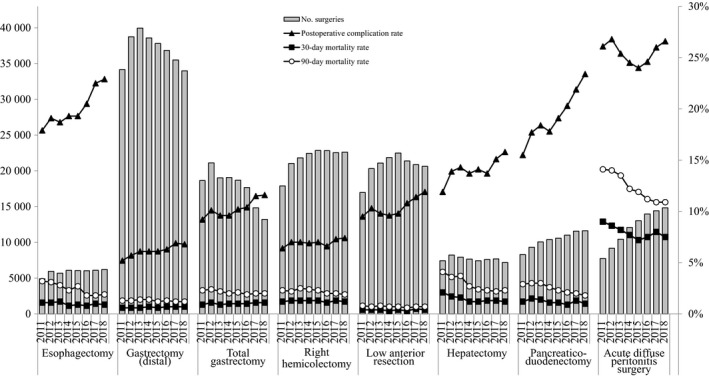
Annual changes of number of surgeries, 30‐Day mortality, operative mortality, and complications: Analysis of 8 major surgical procedures. Postoperative complication rate: the rate of C–D classification grade III or higher complications
An increase in the incidence of endoscopic surgery over time is shown in Figure 3. Endoscopic surgeries have been prevalent, especially in gastrointestinal procedures, with 67.0% for low anterior resection and 61.0% for esophagectomy in 2018. Even for acute diffuse peritonitis, laparoscopic surgery had been done in 19.0% of cases in 2018.
FIGURE 3.
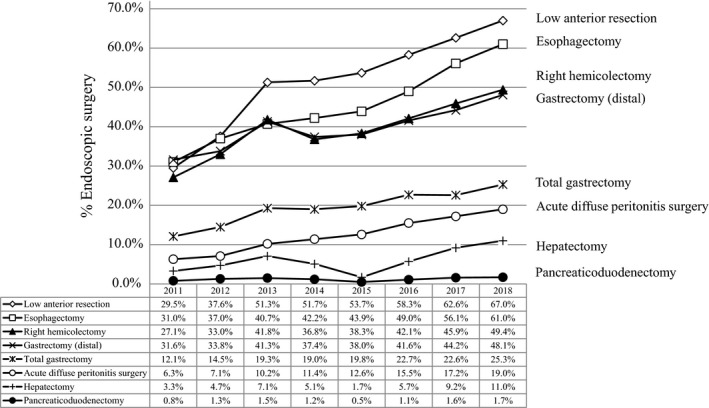
Annual changes in the percentage of surgeries carried out by endoscopic surgery: analysis of the eight major surgical procedures
4. DISCUSSION
The National Clinical Database, a robust nationwide registry on surgical outcomes, shows the real status of Japanese surgical treatment. The purpose of NCD was to systematically gather clinical information, analyze these data for quality improvement, follow the best medical practices, and maintain a high standard of care for all people in Japan.
More than half of all patients who underwent surgical treatment in the gastroenterological field were senior patients aged 65 years or over. With the increase in the aging population, the rates of preoperative comorbidities such as diabetes mellitus or hypertension also increased. Age category was reported as a risk factor both for operative morbidity and mortality in all eight main procedures. 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 Although the annual rate of postoperative complications with C‐D classification of grade III or higher gradually increased over time, the postoperative mortality was kept at a low level. These results may be explained by the high participation rate of board‐certified surgeons in gastroenterological surgeries. 23 The annual percentage of surgeries with participation of board‐certified surgeons in gastroenterological surgeries in the eight procedures gradually increased and the operative mortality was kept at a low level. Also, centralization of the surgical center may be important for improving surgical outcomes. The operative mortality rate after distal gastrectomy definitively decreased as both surgeon volume and hospital volume increased. 25 After risk adjustment for surgeon and hospital volume and patient characteristics, hospital volume was significantly associated with low operative mortality. As for esophagectomy, high‐volume hospitals had a lower risk‐adjusted mortality rate compared with low‐volume hospitals. 26 The factors causing these phenomena should be investigated for each procedure.
The rates of endoscopic surgery have been increasing year by year. This is the first report of the annual number of endoscopic surgeries in the selected 115 gastrointestinal operative procedures in the training curriculum for board‐certified surgeons in gastroenterology. Studies using the NCD data showed that the length of hospital stay was significantly shorter in patients who underwent endoscopic surgery for gastrectomy 27 , 28 , 29 , 30 and hepatectomy. 31 , 32 Laparoscopic liver resection has been safely developed with a low mortality and complication rates relative to open liver resection. 32 Laparoscopic gastrectomy is also safe and feasible even for elderly patients 33 or those with poor physical status, such as the American Society of Anesthesiologists physical status (ASA‐PS) class ≥3. 34
A risk‐adjusted analysis based on nationwide data allows personnel to establish and provide feedback on the risks that patients face before undergoing a procedure. 21 The risk calculator for all eight procedures is available on the websites of the hospitals that are part of the NCD. Standardized information on patient risk and predicted mortality can be reformulated as case reports and shared at conferences. In liver transplant recipients, real‐time risk models of postoperative morbidities and mortality at various perioperative time points were established. 35 These real‐time risk models provide the expected risk of morbidities and mortality at any time point from pre‐, intra‐, and postoperative periods within 30 days after the surgery. With the availability of real‐time risk models of postoperative morbidity and mortality at each time point post‐surgery, the treatment team and caregivers might be encouraged to pay attention and possibly prevent or enhance recovery from specific morbidities and avoid mortality. These real‐time risk models may be applicable to other surgical procedures. The NCD also provides data on each facility's severity‐adjusted clinical performance (benchmark), which can be compared with national data. 21 , 36 , 37 We can trace, periodically, where we are in the national standard, which will improve surgical care on an international basis.
Many valuable studies that use “big data” from the NCD have been published in succession. The NCD has contributed to evidence‐based medicine, to the accountability of medical professionals, and to quality assessment/improvement of surgery in Japan.
DISCLOSURE
Conflict of interests: Arata Takahashi, Hiroyuki Yamamoto, and Hiroaki Miyata are affiliated with the Department of Healthcare Quality Assessment at the University of Tokyo. The department is a social collaboration department supported by grants from the National Clinical Database, Johnson & Johnson KK, and Nipro Co.
ACKNOWLEDGEMENTS
We thank all the data managers and hospitals participating in this NCD project for their continued efforts in entering the data.
Kakeji Y, Takahashi A, Hasegawa H, et al. Surgical outcomes in gastroenterological surgery in Japan: Report of the National Clinical Database 2011‐2018. Ann Gastroenterol Surg. 2020;4:250–274. 10.1002/ags3.12324
REFERENCES
- 1. Seto Y, Kakeji Y, Miyata H, Iwanaka T. National Clinical Database (NCD) in Japan for gastroenterological surgery: Brief introduction. Ann Gastroenterol Surg. 2017;1:80–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Clinical Database . Home page. [cited 2019 Dec 31]. Available from http://www.ncd.or.jp/
- 3. Kakeji Y, Takahashi A, Udagawa H, Unno M, Endo I, Kunisaki C, et al. Surgical outcomes in gastroenterological surgery in Japan: Report of National Clinical database 2011–2016. Ann Gastroenterol Surg. 2018;2:37–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hasegawa H, Takahashi A, Kakeji Y, Ueno H, Eguchi S, Endo I, et al. Surgical outcomes in gastroenterological surgery in Japan: Report of National Clinical database 2011–2017. Ann Gastroenterol Surg. 2019;3(4):426–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Takeuchi H, Miyata H, Gotoh M, Kitagawa Y, Baba H, Kimura W, et al. A risk model for esophagectomy using data of 5354 patients included in a Japanese nationwide web‐based database. Ann Surg. 2014;260:259–66. [DOI] [PubMed] [Google Scholar]
- 6. Kurita N, Miyata H, Gotoh M, Shimada M, Imura S, Kimura W, et al. Risk model for distal gastrectomy when treating gastric cancer on the basis of data from 33,917 Japanese patients collected using a nationwide web‐based data entry system. Ann Surg. 2015;262:295–303. [DOI] [PubMed] [Google Scholar]
- 7. Watanabe M, Miyata H, Gotoh M, Baba H, Kimura W, Tomita N, et al. Total gastrectomy risk model: data from 20,011 Japanese patients in a nationwide internet‐based database. Ann Surg. 2014;260:1034–9. [DOI] [PubMed] [Google Scholar]
- 8. Kobayashi H, Miyata H, Gotoh M, Baba H, Kimura W, Kitagawa Y, et al. Risk model for right hemicolectomy based on 19,070 Japanese patients in the National Clinical Database. J Gastroenterol. 2014;49:1047–55. [DOI] [PubMed] [Google Scholar]
- 9. Matsubara N, Miyata H, Gotoh M, Tomita N, Baba H, Kimura W, et al. Mortality after common rectal surgery in Japan: a study on low anterior resection from a newly established nationwide large‐scale clinical database. Dis Colon Rectum. 2014;57:1075–81. [DOI] [PubMed] [Google Scholar]
- 10. Kenjo A, Miyata H, Gotoh M, Kitagawa Y, Shimada M, Baba H, et al. Risk stratification of 7,732 hepatectomy cases in 2011 from the National Clinical Database for Japan. J Am Coll Surg. 2014;218:412–22. [DOI] [PubMed] [Google Scholar]
- 11. Kimura W, Miyata H, Gotoh M, Hirai I, Kenjo A, Kitagawa Y, et al. A pancreaticoduodenectomy risk model derived from 8575 cases from a national single‐race population (Japanese) using a web‐based data entry system: the 30‐day and in‐hospital mortality rates for pancreaticoduodenectomy. Ann Surg. 2014;259:773–80. [DOI] [PubMed] [Google Scholar]
- 12. Nakagoe T, Miyata H, Gotoh M, Anazawa T, Baba H, Kimura W, et al. Surgical risk model for acute diffuse peritonitis based on a Japanese nationwide database: an initial report on the surgical and 30‐day mortality. Surg Today. 2015;45:1233–43. [DOI] [PubMed] [Google Scholar]
- 13. Ohkura Y, Miyata H, Konno H, Udagawa H, Ueno M, Shindoh J, et al. Development of a model predicting the risk of eight major postoperative complications after esophagectomy based on 10,826 cases in the Japan National Clinical Database. J Surg Oncol. 2019. [Online ahead of print]. 10.1002/jso.25800 [DOI] [PubMed] [Google Scholar]
- 14. Kunisaki C, Miyata H, Konno H, Saze Z, Hirahara N, Kikuchi H, et al. Modeling preoperative risk factors for potentially lethal morbidities using a nationwide Japanese web‐based database of patients undergoing distal gastrectomy for gastric cancer. Gastric Cancer. 2017;20:496–507. [DOI] [PubMed] [Google Scholar]
- 15. Kikuchi H, Miyata H, Konno H, Kamiya K, Tomotaki A, Gotoh M, et al. Development and external validation of preoperative risk models for operative morbidities after total gastrectomy using a Japanese web‐based nationwide registry. Gastric Cancer. 2017;20:987–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Yoshida T, Miyata H, Konnno H, Kumamaru H, Tangoku A, Furukita Y, et al. Risk assessment of morbidities after right hemicolectomy based on the National Clinical Database in Japan. Ann Gastroenterol Surg. 2018;2:220–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Watanabe T, Miyata H, Konno H, Kawai K, Ishihara S, Sunami E, et al. Prediction model for complications after low anterior resection based on data from 33,411 Japanese patients included in the National Clinical Database. Surgery. 2017;161:1597–608. [DOI] [PubMed] [Google Scholar]
- 18. Yokoo H, Miyata H, Konno H, Taketomi A, Kakisaka T, Hirahara N, et al. Models predicting the risks of six life‐threatening morbidities and bile leakage in 14,970 hepatectomy patients registered in the National Clinical Database of Japan. Medicine (Baltimore). 2016;95:e5466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Aoki S, Miyata H, Gotoh M, Motoi F, Kumamaru H, Konno H, et al. Risk factors of serious postoperative complications after pancreaticoduodenectomy and risk calculators for predicting postoperative complications: a nationwide study of 17,564 patients in Japan. J Hepatobiliary Pancreat Sci. 2017;24:243–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Saze Z, Miyata H, Konno H, Gotoh M, Anazawa T, Tomotaki A, et al. Risk models of operative morbidities in 16,930 critically ill surgical patients based on a Japanese nationwide database. Medicine (Baltimore). 2015;94:e1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gotoh M, Miyata H, Hashimoto H, Wakabayashi G, Konno H, Miyakawa S, et al. National Clinical Database feedback implementation for quality improvement of cancer treatment in Japan: from good to great through transparency. Surg Today. 2016;46:38–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kanaji S, Takahashi A, Miyata H, Marubashi S, Kakeji Y, Konno H, et al. Initial verification of data from a clinical database of gastroenterological surgery in Japan. Surg Today. 2019;49:328–33. [DOI] [PubMed] [Google Scholar]
- 23. Konno H, Kamiya K, Kikuchi H, Miyata H, Hirahara N, Gotoh M, et al. Association between the participation of board‐certified surgeons in gastroenterological surgery and operative mortality after eight gastroenterological procedures. Surg Today. 2017;47:611–8. [DOI] [PubMed] [Google Scholar]
- 24. Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien‐Dindo classification of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. IwatsukiM YH, Miyata H, Kakeji Y, YoshidaK KH,Yoshida K, Konno H, et al. Effect of hospital and surgeon volume on postoperative outcomes after distal gastrectomy for gastric cancer based on data from 145,523 Japanese patients collected from a nationwide web‐based data entry system. Gastric Cancer. 2019;22:190–201. [DOI] [PubMed] [Google Scholar]
- 26. Nishigori T, Miyata H, Okabe H, Toh Y, Matsubara H, Konno H, et al. Impact of hospital volume on risk‐adjusted mortality following oesophagectomy in Japan. Br J Surg. 2016;103:1880–6. [DOI] [PubMed] [Google Scholar]
- 27. Yoshida K, Honda M, Kumamaru H, Kodera Y, Kakeji Y, Hiki N, et al. Surgical outcomes of laparoscopic distal gastrectomy compared to open distal gastrectomy: a retrospective cohort study based on a nationwide registry database in Japan. Ann Gastroenterol Surg. 2017;2:55–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hiki N, Honda M, Etoh T, Yoshida K, Kodera Y, Kakeji Y, et al. Higher incidence of pancreatic fistula in laparoscopic gastrectomy. Real‐world evidence from a nationwide prospective cohort study. Gastric Cancer. 2018;21:162–70. [DOI] [PubMed] [Google Scholar]
- 29. Kodera Y, Yoshida K, Kumamaru H, Kakeji Y, Hiki N, Etoh T, et al. Introducing laparoscopic total gastrectomy for gastric cancer in general practice: a retrospective cohort study based on a nationwide registry database in Japan. Gastric Cancer. 2019;22:202–13. [DOI] [PubMed] [Google Scholar]
- 30. Etoh T, Honda M, Kumamaru H, Miyata H, Yoshida K, Kodera Y, et al. Morbidity and mortality from a propensity score‐matched, prospective cohort study of laparoscopic versus open total gastrectomy for gastric cancer: data from a nationwide web‐based database. Surg Endosc. 2018;32:2766–73. [DOI] [PubMed] [Google Scholar]
- 31. Takahara T, Wakabayashi G, Konno H, Gotoh M, Yamaue H, et al. Comparison of laparoscopic major hepatectomy with propensity score matched open cases from the National Clinical Database in Japan. J Hepatobiliary Pancreat Sci. 2016;23:721–34. [DOI] [PubMed] [Google Scholar]
- 32. Ban D, Tanabe M, Kumamaru H, Nitta H, Otsuka Y, Miyata H, et al., Safe dissemination of laparoscopic surgery in 148,507 liver resections between 2011 and 2017 from the National Clinical Database of Japan. Ann Surg in press. [DOI] [PubMed] [Google Scholar]
- 33. Honda M, Kumamaru H, Etoh T, Miyata H, Yamashita Y, Yoshida K, et al. Surgical risk and benefits of laparoscopic surgery for elderly patients with gastric cancer: a multicenter prospective cohort study. Gastric Cancer. 2019;22:845–52. [DOI] [PubMed] [Google Scholar]
- 34. Inokuchi M, Kumamaru H, Nakagawa M, Miyata H, Kakeji Y, Seto Y, et al. Feasibility of laparoscopic gastrectomy for patients with poor physical status: a retrospective cohort study based on a nationwide registry database in Japan. Gastric Cancer. 2020;23:310–318. [DOI] [PubMed] [Google Scholar]
- 35. Marubashi S, Ichihara N, Kakeji Y, Miyata H, Taketomi A, Egawa H, et al. “Real‐time” risk models of postoperative morbidity and mortality for liver transplants. Ann Gastroenterol Surg. 2019;3:75–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Anazawa T, Paruch JL, Miyata H, Gotoh M, Ko CY, Cohen ME, et al. Comparison of national operative mortality in gastroenterological surgery using web‐based prospective data entry systems. Medicine (Baltimore). 2015;94:e2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Marubashi S, Liu JY, Miyata H, Cohen ME, Ko CY, Seto Y, et al. Surgical quality improvement programs in Japan and USA: Report from the collaborative projects between Japanese Society of Gastroenterological Surgery and American College of Surgeons National Surgical Quality Improvement Program. Ann Gastroenterol Surg. 2019;3:343–51. [DOI] [PMC free article] [PubMed] [Google Scholar]


