Abstract
Pelvic-ring-injuries are bony and/or ligamentous disruptions that might lead to pelvic instabilities and asymmetries. For surgical treatment, knowledge of the different possible approaches and stabilization-techniques is essential.
From 2003 to 2017, we analyzed all complications in operative and non-operative treatment of pelvic-ring-injuries in our institution. Besides complication rates, we describe the reachable anatomical structures for different surgical approaches to the pelvic-ring focusing on strategies to reduce surgical complications.
Of 1848 patients with a pelvic fracture, 1463 patients had a pelvic-ring-fracture. We found an overall complication-rate of 14.4%.
For reducing approach-related morbidity, preoperative planning and knowledge of approach-related complications is important.
Keywords: Osteoporosis, Pelvis, Pelvic ring fracture, Approach-related complications
1. Introduction
Fractures of the pelvic ring are rare injuries which make up about 3–8% of all fractures. Pelvic ring injuries mainly occur in two patient groups: (1) younger patients around the 2nd to 3rd decade and (2) older patients around the 7th to 8th decade.1 While the main reason for pelvic fractures in the younger patient usually is a high energy trauma (like motor vehicle accidents or fall from great heights), elderly patients acquire the pelvic injury by a low energy trauma (e.g. fall from the stand or out of the bed). Due to the demographic development, the frequency of these age-associated pelvic injuries has been increasing over recent years.2
For the surgeon's decision whether to stabilize a pelvic instability, it is necessary to assess the potential benefits and the risks of the surgical procedure. Besides the primary stability of the injury, the general condition and concomitant diseases of the patient as well as the activity level of the patient plays a crucial role in the surgeon's decision to operate or to initiate conservative treatment. However, regarding the risks of the surgical procedure, especially the available surgical approaches and the approach-related morbidity are of major interest.3,4 This means for the pelvic trauma surgeon that knowledge of the different approaches to the pelvic ring or acetabulum and their pitfalls is essential for decision-making.
We analyzed our complications in pelvic ring surgery. Based on our data and experience over the years, we present an overview of the most common surgical approaches to the pelvic ring with a brief description of the surgical technique together with approach-specific risks and suggestions how to avoid these risks.
2. Patients and methods
From January 2003 to December 2017, we documented and analyzed all complications in operative and non-operative treatment of pelvic ring injuries in our institution, a Level 1 Trauma Center. We correlated each approach related complication with the respective surgical approach and we compared different surgical approaches to the pelvic ring regarding their related complications.
2.1. Study population
1.848 consecutive patients with a pelvic fracture were registered at our institution, a tertiary trauma center. The data from patients with a pelvic ring fracture were analyzed retrospectively for this study. The local ethics committee of our university approved the study (No. 351/2019BO2).
The patients were divided into two groups: (1) Patients with a surgically treated pelvic ring fracture and (2) patients with a conservatively treated pelvic ring fracture.
2.2. Analyzed parameters
The following demographic parameters were analyzed:
-
•
Age
-
•
Gender
-
•
Fracture type according to Tile-Classification
-
•
Number of osteosynthetic operations
-
•
Surgical approach
-
•
Length of hospital stay (in days)
-
•
Overall complication rate
-
•
Mortality
The following complications were recorded
-
•
Bleeding
-
•
Thromboembolic events
-
•
Surgical site infection
-
•
Neurologic complications (excluding fracture-related neurologic complications)
-
•
Pulmonary complications
-
•
Abdominal complications
-
•
Implant loosening/failure
-
•
Secondary dislocation
-
•
Incisional abdominal wall hernias
-
•
Others
2.3. Correlation between surgical approach and approach-related complications
Surgical site infections, bleeding, neurologic complications, bladder injuries, abdominal injuries or incisional hernias were defined as approach-related complications.
Patients were grouped according to the surgical approach: (1) open approaches to the anterior pelvic ring (Pfannenstiel-approach or modified Stoppa-appoach), (2) minimally invasive approaches to the anterior pelvic ring (external fixator, percutaneous screws or EASY-approach), (3) open anterior approaches to the posterior pelvic ring or sacrum, (4) open posterior approaches to the posterior pelvic ring or sacrum (5) minimally invasive approaches to the posterior pelvic ring or sacrum.
We then correlated each approach-related complication with the respective surgical approach and finally compared different surgical approaches regarding their approached-related complication rates.
3. Results
Of the 1848 patients with a pelvic fracture, 1463 patients had a pelvic ring fracture. Of these, 1322 patients had an isolated pelvic ring fracture, and 141 patients had combined fractures of the pelvic ring and the acetabulum.
3.1. Demographics and fracture distribution
The mean age of the patients was 63.7 ± 23.7 years (range 4–103 years). The gender distribution was 40.6% male (594 patients) to 59.6% female (869 patients). The mean length of hospital stay was 19.1 ± 23.1 days (range 0–255 days).
The fracture types according to the Tile-classification were distributed as follows:
-
•
381 Tile-A-fractures
-
•
592 Tile-B-fractures
-
•
411 Tile-C-fractures
-
•
79 isolated sacral fractures
3.2. Surgical treatment and surgical approaches
Of the 1463 patients with a pelvic ring fracture, 470 patients were operated and the pelvic ring was stabilized. Of the 470 operated patients, 18 patients had a Tile-A-fracture, 121 patients had a Tile-B-fracture, 306 patients had a Tile-C-fracture and 25 patients had an isolated sacral fracture.
The following approaches were performed on the 470 patients (multiple approaches per patient possible):
-
(1)
177 open approaches to the anterior pelvic ring
-
(2)
146 minimally invasive approaches to the anterior pelvic ring
-
(3)
59 open anterior approaches to the posterior pelvic ring
-
(4)
76 open posterior approaches to the posterior pelvic ring
-
(5)
240 minimally invasive approaches to the posterior pelvic ring
3.3. Complications
Of the 1463 patients with a pelvic ring fracture, 211 patients had a complication, resulting in an overall complication rate of 14.4%. Surgically treated patients had a higher overall complication rate of 27.0% (127/470) compared to the group of conservatively treated patients with an overall complication rate of 8.3% (82/993).
In the group of the conservatively treated patients, a total of 95 complications occurred in 82 patients (multiple complications possible):
-
•
5 neurological complications
-
•
7 bleeding complications
-
•
8 thromboembolic events
-
•
6 intraabdominal complications
-
•
15 pulmonary complications
-
•
44 other complications
In the group of the surgically treated patients, a total of 260 complications occurred in 127 patients (multiple complications possible):
-
•
23 neurological complications
-
•
34 bleeding complications
-
•
36 thromboembolic events
-
•
52 surgical site infections
-
•
3 intraabdominal complications
-
•
17 pulmonary complications
-
•
3 incisional abdominal wall hernias
-
•
34 implant loosening/implant failure
-
•
14 secondary dislocations
-
•
44 other complications
No iatrogenic bladder injuries were registered. The correlation of the surgical approaches with the respective approach-related complications is presented in Table 1.
Table 1.
Surgical approaches and the related complication rates: surgical site infections, neurovascular complications, bladder injuries, incisional hernias, abdominal injuries.
| Surgical approach | n | Overall complication rate (%) | Approach-related complication rate (%) |
|---|---|---|---|
| None (conservative treatment) | 993 | 82 (8.3%) | – |
| Open approaches to the anterior pelvic ring | 177 | 52 (29.4%) | 30 (16.9%) |
| Minimally invasive approaches to the anterior pelvic ring | 146 | 37 (25.3%) | 22 (15.1%) |
| Open anterior approaches to the posterior pelvic ring | 59 | 26 (44.1%) | 15 (25.4%) |
| Open posterior approaches to the posterior pelvic ring | 76 | 26 (34.2%) | 18 (23.7%) |
| Minimally invasive approaches to the posterior pelvic ring | 240 | 43 (17.5%) | 30 (12.2%) |
4. Discussion
We think surgical complications might be subjectively underestimated. Especially injuries of the pelvis are known to be associated with different neurovascular and or organ lesions. We found a significantly higher complication rate for surgical treatment than for non-surgical treatment of pelvic ring injuries. Higher-grade injuries are more likely to be treated operatively than low-grade injuries. However, in literature as in our study, especially open approaches for treatment of unstable pelvic ring injuries are correlated with a rather high complication rate.5 We found a tendency for a higher complication risk for open approaches to the posterior pelvic ring than to the anterior pelvic ring. Minimally invasive approaches showed a significantly lower complication rate than open approaches. Probably, modern intraoperative imaging like intraoperative 3-D scans, CT, and navigation are helpful tools in using minimally invasive techniques.
The pelvic ring can be both anatomically and biomechanically divided into an anterior and a posterior part. The anterior pelvic ring includes the pubic symphysis, the superior and inferior pubic rami up to the anterior column of the acetabulum and the inferior ramus of the ischium. The posterior pelvic ring consists of the sacral bone and the sacroiliac (SI) joints with the adjacent parts of the iliac bones. The major part of the stability of the pelvic ring is provided by the ligamentous structures of the SI joints and there especially by the dorsal parts. Injuries of the anterior pelvic ring include ruptures of the pubic symphysis, fractures of the superior and inferior pubic rami and less common of the ischium rami, while injuries of the posterior pelvic ring affect the SI joints and the sacral bone.6
The classification of pelvic ring fractures usually follows the Tile-classification or the Young/Burgess-classification. An indication for a stabilization of anterior pelvic ring injuries usually exists if there is also an unstable posterior pelvic ring.6 These combined injuries of the anterior and posterior pelvic ring may be a ruptured symphysis along with an injury of the SI joints (open-book-injury) or injuries with a complete disrupted posterior pelvic ring (Type C injuries according to the Tile-classification).
An overview over the most common approaches to the anterior pelvic ring together with the accessible anatomical structures is given in Table 2.
Table 2.
Surgical approaches to the anterior pelvic ring.
| Approach | Approachable structures | Possible complications | Avoid complications |
|---|---|---|---|
| Pfannenstiel approach7,8 | Symphysis, Medial upper pubic bones |
Injury of peritoneum | Mid-line dissection |
| Injury of inferior epigastric artery | Mid-line dissection | ||
| Injury of bladder | Place urinary catheter preoperatively, Blunt dissection of retrosymphyseal space |
||
| Injury of Corona mortis | Avoid dissection too far lateral | ||
| Injury of spermatic cord | Mid-line dissection | ||
| Incisional hernia |
Limited dissection of muscles from upper pubic bone, transosseous refixation if necessary |
||
| Modified Stoppa (intrapelvine) approach (+1st window of ilioinguinal approach)10 | Symphysis, Whole upper pubic bones, Anterior acetabulum column, Quadrilateral plate, (sacroiliac joint) |
Injury of peritoneum | Mid-line dissection |
| Injury of inferior epigastric artery | Mid-line dissection | ||
| Injury of bladder | Place urinary catheter preoperatively, Blunt dissection of retrosymphyseal space |
||
| Injury of Corona mortis | Identify the vessel in the middle of the upper pubic bone and ligate it | ||
| Injury of spermatic cord | Mid-line dissection | ||
| Injury of vasa obturatoria | Subperiosteal dissection underneath obturator internus muscle | ||
| Injury of obturator nerve | Subperiosteal dissection underneath obturator internus muscle | ||
| Injury of sciatic nerve | Avoid deep dissection along quadrilateral plate | ||
| Incisional hernia |
Limited dissection of muscles from upper pubic bone, transosseous refixation if necessary |
||
| EASY approach (endoscopic approach to the symphysis)13 | Symphysis, Whole upper pubic bones, Anterior acetabulum column, Quadrilateral plate, Sacroiliac joint |
Injury of the peritoneum | Stop dissection, if sight is not optimal |
4.1. Pfannenstiel approach
The Pfannenstiel approach is named after the gynecologist H.J. Pfannenstiel. He performed different gynecological and obstetrical operations via this approach at the beginning of the 20th century.7 In the orthopedic context it is used for the osteosynthesis of medial pubic rami fractures or a pubic symphysis rupture.8
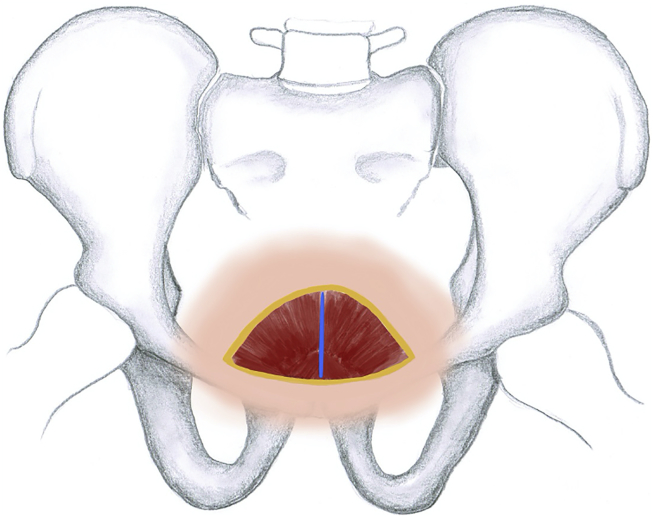
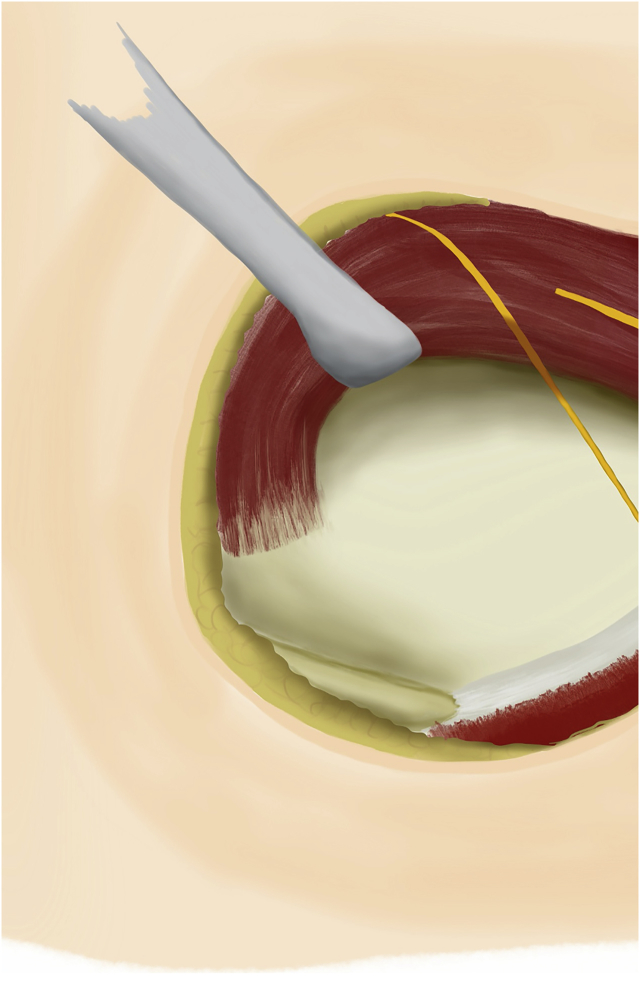
The skin is incised transversely about 2 cm proximal to the symphysis over a distance of about 10 cm. After preparation down to the rectus sheath the midline of the fascia is incised longitudinally. On one hand, both rectus sheaths should be preserved, on the other hand too deep dissection would open the peritoneal sac and should be avoided. For a better overview of the situs, one of the two pyramid muscles can be sharply transected from the superior pubic ramus to the lateral side. Now the retropubic space can be dissected bluntly and the urinary bladder can be shoved off dorsally. By dissection of the periosteum from the superior pubic rami to the lateral side, the medial parts of the superior pubic rami as well as the pubic symphysis can be explored and visualized (Fig. 1). Complications due to the Pfannenstiel incision occur in up to 19%.9 Typical risks as well as strategies to avoid them are presented in Table 2.
Fig. 1.
Pfannenstiel approach.
4.2. Modified Stoppa (intrapelvine) approach
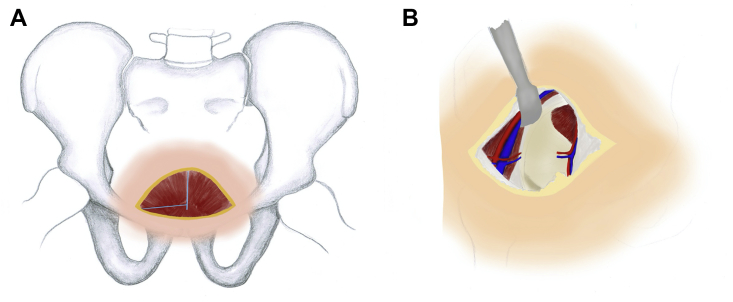
The original Stoppa approach was presented in 1973 by R. Stoppa for the preperitoneal mesh-repair of bilateral groin hernias.10 In principle, it is an extended Pfannenstiel approach. Via the Stoppa approach the entire anterior pelvic ring can be exposed except for the ischial rami.8 Together with the first window of the ilioinguinal approach, the Stoppa approach can be used for the osteosynthesis of acetabular fractures with dislocation of the anterior column or the quadrilateral plate.11 The initial preparation is according to the Pfannenstiel approach. However, contrary to the Pfannenstiel approach, the transection of one pyramid muscle from the superior pubic ramus is absolutely necessary to get an adequate vision of the lateral structures (Fig. 2). Along the pubic rami the periosteum is dissected to the lateral side. In case of an existing corona mortis vessel, this anastomosis between the inferior epigastric artery and the obturator artery should be divided and ligated. Now the quadrilateral plate of the acetabulum can be prepared along the internal obturator muscle down to the ischial spine. In this phase, the obturator vessels and the obturator nerve must be taken care of. By further preparation of the periosteum posteriorly the anterior part of the SI joint can be reached. In a systematic review, the overall complication rate of the modified Stoppa approach was as high as 17.5%.12 Additional to the risks of the Pfannenstiel approach the modified Stoppa approach has some more specific risks which are presented in Table 2 together with complication avoiding strategies.
Fig. 2.
Intrapelvine (Modified Stoppa) approach.
A: Muscle preparation after Pfannenstiel incision.
B: Exposure of the quadrilateral plate after ligating and cutting the corona mortis vessel.
4.3. EASY-approach (endoscopic approach to the symphysis)
Groin hernias are treated endoscopically since the early 1990s. By further development of the surgical techniques and endoscopic instruments during the last three decades, the endoscopic hernia repair nowadays is a standard treatment. Based on the total extraperitoneal approach for groin hernia repair the EASY-approach was developed for the treatment of anterior pelvic ring injuries.13
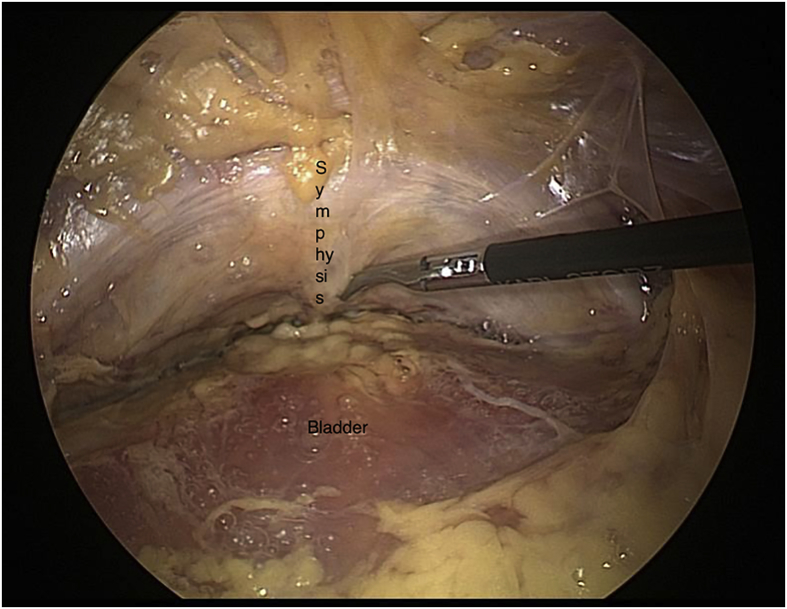
A 3–4 cm transverse skin incision is placed 2 cm infraumbilically and the anterior rectus sheath is prepared. After incision of the anterior rectus sheath (without crossing the midline!) a balloon trocar is pushed distally inside the rectus sheath up to the symphysis. By inflating the balloon, the extraperitoneal and retropubic space is dissected bluntly. This can be controlled by endoscopic view through the trocar. Then, an additional working trocar (5 mm) is placed under direct vision about 1–2 cm proximal of the symphysis in the midline. By blunt dissection in the avascular plane along the superior pubic rami to the lateral as well as the retropubic space, the anterior pelvic ring can be prepared analogous to the Stoppa approach (Fig. 3).
Fig. 3.
EASY approach (Endoscopic approach to the symphysis).
In principle, the EASY-approach has the same risks like the modified Stoppa approach. However, by better visualization and magnification of the structures, injuries to the vessels or nerves as well as the urinary bladder are extremely rare. The risk of incisional hernias is reduced significantly as the muscles must not be transected from the pubic rami. The risk of opening the peritoneal sac can be reduced by strict preparation inside the rectus sheath. Therefore, the rectus sheath must not be opened in the midline.
However, as after intraabdominal or urogenital surgery or previous groin hernia repair there are severe adhesions inside the preperitoneal space, the EASY-approach is associated with an increased risk for injuries of the bladder or the peritoneal sac. In these patients, the EASY-approach should only be performed by experienced laparoscopic surgeons.
A further prospective investigation of the EASY-approach regarding complications and reduction quality is going on.
4.4. Caudal approach to the ischial tuberosity
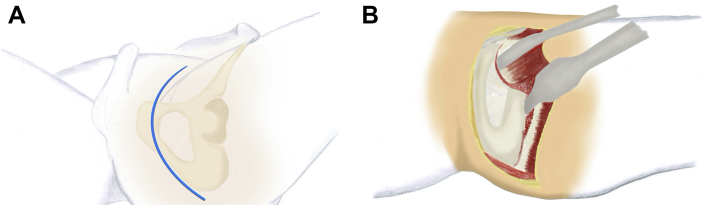
Injuries of the inferior pubic rami and the rami ischium can be treated via the caudal approach. The patient can be positioned on the side or in lithotomy position. The skin incision is along the border of the gluteus muscle from the pubic tubercle to the ischial tuberosity (Fig. 4a). Starting from the adductor muscles and the great gluteus muscle the inferior pubic ramus is prepared by dissecting the adductor muscles and shoving the periost to the lateral. Now the entire inferior pubic ramus as well as the ischial ramus can be visualized (Fig. 4b). Risks of the caudal approach and strategies to avoid them are shown in Table 3.
Fig. 4.
Caudal approach.
A: Skin incision.
B: Bony exposure.
Table 3.
Caudal surgical approach to the pelvis.
| Approachable structures | Possible complications | Avoid complications |
|---|---|---|
| Ischial tuberosities, Ramus ossis ischii, Lower pubic bones |
Injury of spermatic cord | Stop anterior dissection at the inguinal ligament |
| Injury of vasa obturatoria | Dissect adductor muscles in cranial and lateral direction not further than the middle of ischial or pubic bone | |
| Injury of sciatic nerve | Subperiosteal dissection at ischial tuberosity | |
| Injury of vasa pudenda | Subperiosteal dissection at lower pubic bone |
Injuries of the posterior pelvic ring can be treated by the surgical approaches listed in Table 4.
Table 4.
Surgical approaches to the posterior pelvic ring.
| Approach | Indications | Possible complications | Avoid complications |
|---|---|---|---|
| Dorsal approach | Fractures of the sacrum with stenosis of neuroforamina, Spino-pelvic dissociation |
Nerve root injuries | Careful dissection and decompression before reduction |
| Injury of Truncus lumbosacralis | 1st window preparation: stop dissection at the anterior sacrum 15 mm medial of the sacroiliac joint | ||
| Injury of bladder | Place urinary catheter preoperatively, Blunt dissection of retrosymphyseal space |
||
| Injury of Corona mortis | 2nd window preparation: identification in the middle of the upper pubic bone and ligation | ||
| Injury of spermatic cord | 2nd window preparation: dissect abdominal muscles from inguinal ligament | ||
| Injury of vasa obturatoria | Subperiosteal dissection underneath the obturator internus muscle | ||
| Injury of obturator nerve | Subperiosteal dissection underneath the obturator internus muscle | ||
| Injury of sciatic nerve | Avoid deep dissection along quadrilateral plate | ||
| Incisional hernia |
Refixation of oblique abdominal muscles to iliac crest and inguinal ligament |
||
| 1st window of ilioinguinal approach | Fracture of pelvic wing, Sacroiliac dislocation |
Injury of the lateral cutaneous femoral nerve | Skin incision and dissection to iliac crest lateral of anterior superior iliac spine |
| Injury of Truncus lumbosacralis | Stop dissection at the anterior sacrum 15 mm medial of the sacroiliac joint | ||
| Incisional hernia |
Refixation of oblique abdominal muscles to iliac crest |
||
| Percutaneous lateral approach | Fractures of the sacrum, Sacroiliac dissociations |
Injury of S1 or S2 nerve roots or vessels because of malpositioning of sacroiliac screw | Application of laxatives starting two days before surgery to reduce enteral air and to improve intraoperative x-ray imaging of all important bony landmarks |
4.5. Lateral window of the ilioinguinal approach
Emile Letournel presented his ilioinguinal approach in the 1960s as an anterior approach for the treatment of pelvic ring or acetabular fractures.14 The original ilioinguinal approach consists of three windows which are developed from the lateral to the medial side. Via the first window the dorsal parts of the pelvic ring can be visualized.
For the first window the skin is incised along the iliac crest with the starting point around 2 cm laterally from the anterior superior iliac spine (ASIS) over a length of 10–12 cm. After transection of the oblique abdominal muscles from the iliac crest the iliac muscle is lifted from the iliac wing subperiosteally. Preparation is continued down to the SI joint and the lateral parts of the sacral bones (Fig. 5). Specific risks for this approach are iatrogenic nerve lesions (namely the cutaneous lateral femoral nerve and the lumbosacral plexus) or incisional hernias. There is no evidence how high the rate for iatrogenic nerve lesions is in this approach, while for the complete ilioinguinal approach it is about 8%. However, this rate includes lesions to the femoral and obturator nerves as well.15 The rate of incisional hernias is up to 9%.16 Strategies to avoid these lesions are listed in Table 4.
Fig. 5.
Lateral (1st) window of the ilioinguinal approach.
4.6. Percutaneous lateral approach
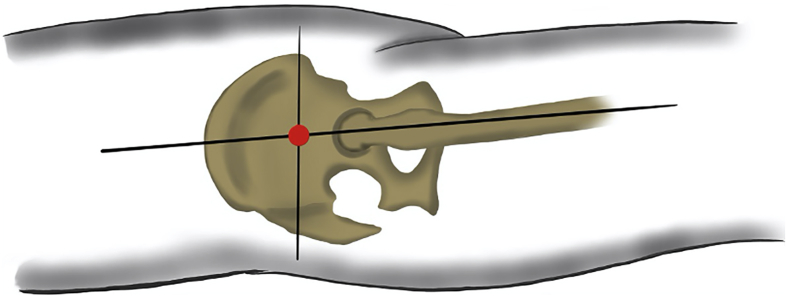
The minimally invasive percutaneous screw osteosynthesis of the SI joint for stabilization of non or little dislocated sacral fractures or SI joint injuries gained acceptance over the last years.17,18 This procedure can be performed in supine or prone position, either guided by fluoroscopy or CT-scan.
To achieve a good imaging quality by fluoroscopy, preoperative bowel preparation is essential to reduce artefacts by intraluminal air. The ca. 2 cm long skin incision is made at the crossing point of the line between both ASIS and the continuation of the femoral axis through the major trochanter (Fig. 6) followed by preparation onto the external face of the iliac wing. Guided by fluoroscopy or CT-scan the SI-screw is placed in the middle of the first sacral vertebral body. The most common problem is malpositioning of the screw with consecutive nerval irritation which is reported with a frequency up to 17%.19 Tips to avoid this are listed in Table 4.
Fig. 6.
Percutaneous lateral approach.
4.7. Dorsal approach to the sacrum
The dorsal approach to the sacral bone is suitable for treatment of sacral fractures with narrowing of the neural foramina, for severely dislocated injuries of the iliosacral joints, or for spinopelvic dissociations. The operation is performed in prone position. The skin incision is done in the midline over the sacral bone from the spinous process of L5 down to the beginning of the anal cleft. After preparing and incising the sacral fascia the down lying muscles are prepared to the lateral side and the boney structures can be exposed (Fig. 7). The main risk of the dorsal approach are surgical site infections with consecutive chronic osteomyelitis with an incidence of up to 16%.20 This can be provided by carefully dressing the surgical site with special care of the anal cleft.
Fig. 7.
Dorsal approach (to the sacrum).
5. Conclusions
Injuries of the pelvic ring should be divided into anterior and posterior pelvic ring injuries. Whether an operative stabilization is necessary depends on the grade of dislocation and instability. In order to reduce approach-related morbidity, the surgical approach should be planned carefully dependent on the surgical anatomy and goal being aware of the most common approach-related complications.
Declaration of competing interest
The authors declare that they have no conflict of interest.
References
- 1.Hoge S., Chauvin B.J. Acetabular fractures. Stat Pearls. 2019 [PubMed] [Google Scholar]
- 2.Oberkircher L., Ruchholtz S., Rommens P.M., Hofmann A., Bücking B., Krüger A. Osteoporotic pelvic fractures. Dtsch Arztebl Int. 2018;115:70–80. doi: 10.3238/arztebl.2018.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rommens P.M., Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44:1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 4.Wagner D., Ossendorf C., Gruszka D., Hofmann A., Rommens P.M. Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg. 2015;41:349–362. doi: 10.1007/s00068-015-0530-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Culemann U., Oestern H.J., Pohlemann T. Current treatment of pelvic ring fractures. Chirurg. 2013;84:809–826. doi: 10.1007/s00104-012-2391-x. [DOI] [PubMed] [Google Scholar]
- 6.Tile M., Helfet D.L., Kellam J.F., Vrahas M. fourth ed. 2015. Fractures of the Pelvis and Acetabulum: Principles and Methods of Management. Thieme. [Google Scholar]
- 7.Pfannenstiel H. Über die Vortheile des suprasymphysären Fascienquerschnitts Fur die gynäkologischen Koliotomien, zugleich ein Beitrag zu der Indikationsstellung der Operationswege. Sammlung klin Vortr. 1900;97:1735–1756. [PubMed] [Google Scholar]
- 8.Becker S.C., Holstein J.H., Pizanis A., Pohlemann T. Anterior approaches to the pelvic ring. Unfallchirurg. 2013;116:198–204. doi: 10.1007/s00113-012-2329-2. [DOI] [PubMed] [Google Scholar]
- 9.Marrs C., Blackwell S., Hester A. Pfannenstiel versus vertical skin incision for cesarean delivery in women with class III obesity: a randomized trial. Am J Perinatol. 2019;36:97–104. doi: 10.1055/s-0038-1667287. [DOI] [PubMed] [Google Scholar]
- 10.Stoppa R., Petit J., Abourachid H. Original procedure of groin hernia repair: interposition without fixation of Dacron tulle prosthesis by subperitoneal median approach. Chirurgie. 1973;99:119–123. [PubMed] [Google Scholar]
- 11.Ismail H.D., Djaja Y.P., Fiolin J. Minimally invasive plate osteosynthesis on anterior pelvic ring injury and anterior column acetabular fracture. J Clin Orthop Trauma. 2017;8:232–240. doi: 10.1016/j.jcot.2017.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Meena S., Sharma P.K., Mittal S., Sharma J., Chowdhury B. Modified Stoppa approach versus ilioinguinal approach for anterior acetabular fractures; A systematic review and meta-analysis. Bull Emerg Trauma. 2017;5:6–12. [PMC free article] [PubMed] [Google Scholar]
- 13.Küper M.A., Trulson A., Trulson I.M. EASY (endoscopic approach to the symphysis): a new minimally invasive approach for the plate-osteosynthesis of the symphysis and the anterior pelvic ring – a cadaver study and first clinical results. Eur J Trauma Emerg Surg. 2018;45:745–755. doi: 10.1007/s00068-018-0928-5. [DOI] [PubMed] [Google Scholar]
- 14.Letournel E. Les fractures du cotyle. Etude d’une serie de 75 cas. J Chronic Dis. 1961;82:47–87. [PubMed] [Google Scholar]
- 15.Giannoudis P.V., Grotz M.R., Papakostidis C., Dinopoulos H. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 16.Do M.V., Richardson W.S. Lumbar incisional hernia repair after iliac crest bone graft. Ochsner J. 2012;12:80–81. [PMC free article] [PubMed] [Google Scholar]
- 17.Mosheiff R., Khoury A., Weil Y., Liebergall M. First generation computerized fluoroscopic navigation in percutaneous pelvic surgery. J Orthop Trauma. 2004;18:106–111. doi: 10.1097/00005131-200402000-00009. [DOI] [PubMed] [Google Scholar]
- 18.Acklin Y.P., Zderic I., Grechenig S., Richards R.G., Schmitz P., Gueorguiev B. Are two retrograde 3.5 mm screws superior to one 7.3 mm screw for anterior pelvic ring fixation in bones with low bone mineral density? Bone Joint Res. 2017;6:8–13. doi: 10.1302/2046-3758.61.BJR-2016-0261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Osterhoff G., Ossendorf C., Wanner G.A., Simmen H.P., Werner C.M. Percutaneous iliosacral screw fixation in S1 and S2 for posterior pelvic ring injuries: technique and perioperative complications. Arch Orthop Trauma Surg. 2011;131:809–813. doi: 10.1007/s00402-010-1230-0. [DOI] [PubMed] [Google Scholar]
- 20.Schildhauer T.A., Bellabarba C., Nork S.E., Barei D.P., Routt M.L., Jr., Chapman J.R. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20:447–457. doi: 10.1097/00005131-200608000-00001. [DOI] [PubMed] [Google Scholar]