Abstract
Background
Low vaccine uptake results in regular outbreaks of severe diseases, such as measles. Selective mandates, e.g. making measles vaccination mandatory (as currently implemented in Germany), could offer a viable solution to the problem. However, prior research has shown that making only some vaccinations mandatory, while leaving the rest to voluntary decisions, can result in psychological reactance (anger) and decreased uptake of voluntary vaccines. Since communicating the concept of herd immunity has been shown to increase willingness to vaccinate, this study assessed whether it can buffer such reactance effects.
Methods
A total of N = 576 participants completed a preregistered 2 (policy: selective mandate vs. voluntary decision) × 2 (communication: herd immunity explained yes vs. no) factorial online experiment (AsPredicted #26007). In a first scenario, the concept of herd immunity was either introduced or not and vaccination either mandatory or voluntary, depending on condition. The dependent variable was the intention to vaccinate in the second scenario, where vaccination was always voluntary. Additionally, we explored the mediating role of anger between policies and intentions.
Findings
Herd immunity communication generally increased vaccination intentions; selective mandates had no overall effect on intentions, and there was no interaction of the factors. However, selective mandates led to increased anger when herd immunity was not explained, leading in turn to lower subsequent vaccination intentions.
Interpretation
Explaining herd immunity can counter potential detrimental effects of selective mandates by preventing anger (reactance).
Funding
This study was funded by the University of Erfurt and the German Research Foundation (BE-3979/11–1).
Keywords: Vaccination, Selective mandates, Reactance
Research in context.
Evidence before the study
Prior research on the psychological and behavioral consequences of selective mandates indicates that (a) making some vaccinations mandatory while leaving the rest up to voluntary decisions can result in psychological reactance and low uptake for voluntary vaccines, (b) psychological reactance is related to the subjective importance of individual freedom, and (c) explaining the prosocial effect of herd immunity can have a positive effect on individual vaccination intentions, even if individuals value freedom of choice and liberty.
Added value of the study
We integrated the given research into a preregistered experimental study about selective vaccination mandates. The results indicate that the introduction of a selective mandate can elicit anger (an indicator of reactance), leading to low uptake of voluntary vaccinations, but only if no information about herd immunity is given. While there is evidence of the positive effects of herd immunity communication on vaccination intentions, we could show that such communication can also buffer reactance effects of selective mandates.
Implications of all the available evidence
Given the recent change to a selective mandate (measles only) in Germany, there is an urgent need to improve and shape immunity communication strategies. In communication regarding selective mandates, the prosocial benefits of vaccination should be highlighted, for example, on information sheets provided before the mandatory vaccination, in communications with healthcare personnel, and in information campaigns.
Alt-text: Unlabelled box
1. Introduction
Vaccination coverage against highly contagious diseases, such as measles, is often too low to prevent outbreaks [1,2]. In 2018, in the WHO European Region alone, more than 80,000 people caught this disease [3], and in 2019/2020 the Samoa outbreak caused over 80 deaths, mainly of children [4,5]. Given the high burden of disease, mandates are often discussed as a means to counter low vaccine uptake. Policymakers sometimes propose selective mandates, laws requiring only one specific vaccine or a subset of recommended vaccinations, while the rest remain voluntary. A couple of European countries recently changed their vaccination policies accordingly, making several vaccinations mandatory [6,7]. For instance, Germany passed the Measles Protection Act, which came into force in March 2020 [8]. Currently, the German National Standing Committee on Vaccination recommends a vaccination administered in two doses, the first at 11–14 months, the second at 15–23 months of age [9]. While data from country-wide health insurance claims indicate that vaccination coverage has been improving over the past years, children are often vaccinated too late, especially with regard to the second dose [10]. To mitigate the risk of outbreaks, the new law requires children, asylum seekers, and staff in healthcare and childcare facilities to be vaccinated against measles twice. Parents who refuse to get their children vaccinated face fines of up to 2500 EUR and a ban from daycare [8]. Under the new German act, all vaccines except measles remain voluntary.
Health professionals speak both for and against such legislations [11]. The recent analysis by Vaz and colleagues shows that, across several European countries, mandatory vaccination against measles and pertussis was indeed associated with higher vaccination coverage for exactly these two diseases [12]. However, leaving ethical considerations to one side, there may be negative effects of selective mandates on the uptake of still-voluntary vaccines [13]. When considering ethics, freedom of choice is usually weighed against social welfare concerns. In Germany, for example, the national ethics committee made a strong case against mandates [14]. Regarding the potential effect on voluntary vaccines, previous work in other areas has shown that decreasing people's freedom of choice can result in reactance, a feeling of anger that elicits the motivation to reassert the constricted freedom [15,16]. Translating this principle to the area of vaccination, a behavioral experiment showed that selective mandates increased the level of anger among individuals with a rather negative vaccination attitude [17]. In a subsequent voluntary vaccination decision, those individuals’ vaccination uptake decreased by 39% compared to control group participants who had not previously been forced to vaccinate. In summary, introducing selective mandates could have a negative impact on the overall vaccine uptake, given that people feel reactance and, as a consequence, opt out of further voluntary vaccinations. Negative attitudes toward vaccination would foster the effect [17]. In consequence, Omer, Betsch, and Leask explicitly warned Germany against introducing a mandate for (just) measles [18]. German policymakers highlight the public's support for mandatory measles vaccination. While the 86% agreement found in a 2019 representative survey might seem fairly high, about 14% of the population are against such legislation [19]. Thus, this considerable part of the target group could be annoyed when the act comes into force, consequently showing reactance and opting out of other vaccines that are still voluntary. As for vaccine coverage, a decrease of only a few percentage points could make a dramatic difference, and, in the absence of suitable mitigation strategies, the well-meant mandates could put vaccine coverages for other diseases at risk.
The goal of this contribution was therefore to investigate a communication strategy that could counter the expected reactance effect: emphasizing the concept of herd immunity. With herd immunity, a sufficient proportion of a population is immune to an infectious disease, making it unlikely to spread from person to person; this immunity is usually achieved through vaccination. As a consequence, non-vaccinated individuals, including those who cannot be vaccinated because they are too young or suffer from immunodeficiencies, are protected as well [20]. An online experiment, with more than 2,000 participants from multiple countries, demonstrated the positive effect of explaining herd immunity on individual vaccination intentions [21]. This positive effect even holds for individuals who value freedom of choice and liberty [22]. Since reactance is related to the subjective importance of individual freedom, we hypothesized that emphasizing the concept of herd immunity would curb reactance effects driven by selective mandates [23]. This assumption is based on research showing that perspective-taking can reduce reactance [24]. Since valuing the collective benefit of vaccination is related to higher individual empathy [25], emphasizing the collective benefit of vaccination may elicit enough perspective-taking empathy to counter the detrimental effects of selective mandates. Moreover, individual characteristics, personality traits, and confidence in vaccines may have an additional impact on the effect of herd immunity communication. For instance, having a child who cannot be vaccinated and has to rely on herd immunity could foster support for selective mandates – given that the parent knows about herd immunity. Furthermore, previous research has shown that people high in communal orientation tend to support vaccinations for the protection of the community [25]. Accordingly, individuals who care for the wellbeing of others could be especially sensitive to the prosocial rationale of herd immunity communication. Confidence in vaccination may play an important role as well. Betsch and Böhm showed vaccination attitudes to be negatively related to anger when faced with selective mandates (more negative attitudes elicit more anger) [17]. Therefore, it is worthwhile exploring whether an explanation of herd immunity has the same anger-buffering effect in individuals low in vaccine confidence.
Working from the above considerations, we set up an online experiment and collected participants’ responses to a fictitious scenario. Two hypotheses were preregistered. First, we expected that the intention to get vaccinated would be higher when herd immunity had been communicated than when it had not (H1) [21,22]. Second, we expected that selective mandates would decrease the intention to get a second, voluntary vaccine against a different disease when the social benefits of herd immunity had not been explained (H2). We further explored the role of reactance, assessing its role in mediating the relationship between the different policies and the vaccination intention for the voluntary vaccine. Finally, we explored the results for potential effects of communal orientation and the confidence in vaccines, as well as to discover whether participants’ children were old enough to be vaccinated themselves or whether they had to rely on herd immunity.
2. Methods
2.1. Design and participants
We decided to conduct the experiment with an American sample. Since people from the US are already used to selective vaccination mandates, we expected rather conservative estimates of the effects of herd immunity communication. Due to cultural similarity regarding previous studies on vaccine communication, the findings should be generalizable for European countries as well [21]. The study was preregistered (see AsPredicted #26007, https://aspredicted.org/di34y.pdf).
2.1.1. Design
The study implemented a 2 (communication: herd immunity communication vs. no herd immunity communication) × 2 (policy: selective mandate vs. voluntary vaccination) factorial between-subjects design.
2.1.2. Participants
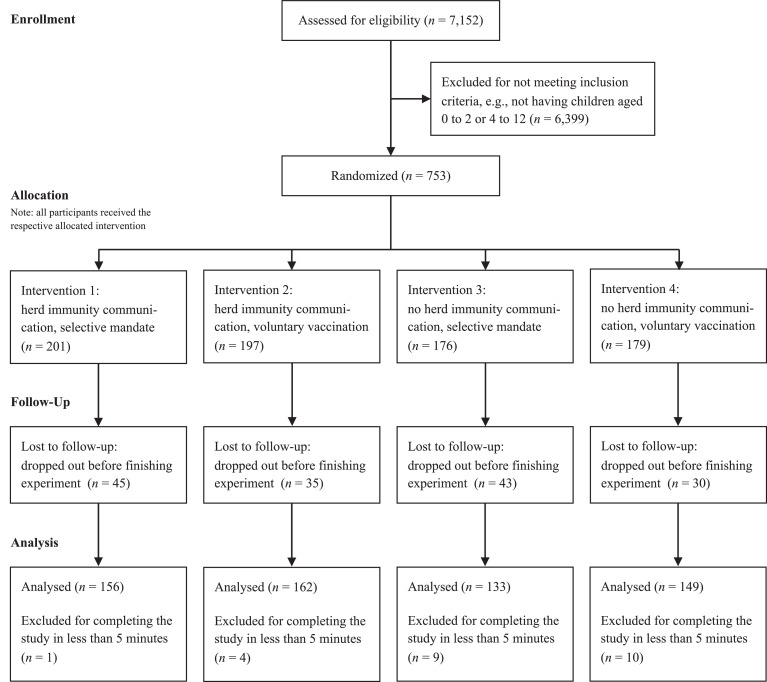
To determine the sample size for this between-subjects design, we assumed a small- to medium-sized interaction effect (policy × communication; Cohen's f = 0.25) and a high statistical test power of 1-β > 0.99, resulting in a required N of 300 participants. We also planned an explorative analysis to contrast the effects for parents of children that could and could not be vaccinated; we therefore doubled the sample size to N = 600, with exactly half having children up to 2 years (who could not be vaccinated, according to the scenario) and the other half having children between 4 and 12 years (who could be vaccinated; see below). Data collection took place in July 2019. Participants were recruited online using Amazon Mechanical Turk, a crowdsourcing platform known for inexpensive, rapid collection of high-quality data [26]. Of 7152 participants who started the study, 753 were eligible and 600 completed the study (Fig. 1). They received a fixed compensation of 1.00 USD after completion. Twenty-four individuals had to be excluded from further analysis because they completed the study in less than five minutes (preregistered exclusion criterion). The final sample included in the analysis was n = 576 Americans (52.4% female, 46.0% male), aged 18–49 years (mean M = 31.91, standard deviation SD = 5.96).
Fig. 1.
CONSORT flow diagram. Note: Non-applicable elements of the CONSORT template were removed. There was no time interval between intervention allocation and follow-up.
2.1.3. Randomization
The study was conducted with the online software Unipark by Questback, which automatically performed randomization. The experimenters had no influence on the process.
2.1.4. Ethics and consent
The study was conducted in accordance with German Psychological Association guidelines. All participants provided written informed consent to use and share their data for scientific purposes without disclosure of their identities. The experiment was conducted at a German university, where institutional review boards or committees are not mandatory. The research is negligible-risk research, with no foreseeable risk of harm or discomfort other than potential inconvenience expected from participation. All participants knew that they were free to quit the study at any time.
2.2. Materials and measures
After providing demographic information (age, gender, education, religion, and children's age), all participants were presented with two identically constructed scenarios: in each, a fictitious disease (Table 1: Cornosis and Holtosis, randomly drawn as first or second disease) was described as leading to symptoms of low to medium severity in adults and children above three years of age. Younger children were described as being at risk for more severe complications and long-term consequences. Vaccination against the disease was available, but only for those three years old or more. The fictitious vaccine also had some side effects, so that the participants had to weigh the pros and cons of vaccination, one of the pros being the protection of others. Participants had to pass a short cloze test to ensure proper encoding. Those who failed the test returned to the materials, read about the disease again, and repeated the test until they passed it. While the two diseases differed in symptoms and adverse events, the respective severities and probabilities were designed to be equal.
Table 1.
Fictitious diseases presented in the first and second scenarios.
| Cornosis | Holtosis |
|---|---|
| Cornosis spreads through the air from one person to another. When infected, people like you normally suffer from fever and rash. Restlessness and dizziness are also common. For most adults and children being 3 years or older, symptoms disappear within two weeks. | Holtosis spreads through the air from one person to another. When infected, people like you normally suffer from seizures and stomach ache. Qualm and lack of concentration are also common. For most adults and children being 3 years or older, symptoms disappear within two weeks. |
| But for children below 3 years, symptoms are much worse. They often face severe vomiting and diarrhea with extreme dehydration, potentially leading to kidney failure. | But for children below 3 years, symptoms are much worse. They often face severe tinnitus and ague, potentially leading to palsy of separate parts of the body. |
| There is a vaccination against Cornosis. This vaccination effectively protects against infection but is not available for those at high risk – children below 3 years cannot get vaccinated. | There is a vaccination against Holtosis. This vaccination effectively protects against infection but is not available for those at high risk – children below 3 years cannot get vaccinated. |
| For those who can get vaccinated, adverse events such as fever, rash, restlessness, dizziness, vomiting and dehydration have been reported. | For those who can get vaccinated, adverse events such as seizures, stomach ache, qualm, lack of concentration, tinnitus and ague have been reported. |
Note: For each participant, the choice of disease for the first scenario was made at random, the disease not drawn becoming the one used in the second scenario. Vaccination was mandatory or voluntary in the first scenario, depending on policy condition, and always voluntary in the second scenario. Full materials are available at https://osf.io/pnjs9/.
2.2.1. Manipulation of herd immunity communication
The herd immunity manipulation took place directly after the first scenario. Participants in the herd immunity communication condition were presented with an interactive simulation already used by Betsch et al. [21]. The simulation allowed the observation of the spread or decline of an infection, given low versus high coverage over time. Participants could move back and forth in time to see the advantage of herd immunity induced by high vaccination rates. A short text emphasized the social benefits of getting vaccinated (that is, the protection of young children who could not be vaccinated against the fictitious diseases). The other participants did not receive any information about the concept of herd immunity.
2.2.2. Policy manipulation
After reading the first scenario, participants in the selective mandates policy condition were informed that the government had recently introduced mandatory vaccination for the disease and that they were going to be vaccinated by their doctor during the next regular check-up. Individuals in the voluntary vaccination policy condition were informed that the vaccination was voluntary but recommended by the government.
2.2.3. Dependent measure
After reading the second disease scenario, participants were asked how likely they were to get vaccinated against the disease if they had the chance to do it right now (on a 20-point sliding scale ranging from 1 = not at all to 20 = very much; no numerical anchors were provided in any of the measures; this resembles a probability estimate in 5-point steps).
2.2.4. Additional measures
We measured the level of anger [27] as a proxy for reactance, represented by the mean of ratings of how angry, irritated, and annoyed participants felt after the first scenario, having learnt about the selective mandate or voluntary vaccination policy. Three corresponding items and two fillers were presented after asking participants about how they felt about the vaccination decision (sample item: I feel angry; ratings ranged from 1 = not at all to 7 = very much; Cronbach's alpha = 0.95). At the start of the study, right after asking participants for demographic information, we also assessed their communal orientation using a subset of the scale established by Clark, Ouellette, Powell, and Milberg, with six items rated on scales ranging from 1 = not at all to 7 = very much (sample item: I believe people should go out of their way to be helpful; Cronbach's alpha = 0.78) [28]. At the end of the study, we measured the 5C psychological antecedents of vaccination (short form), including vaccine confidence (each of the five items was measured on a scale ranging from 1 = not at all to 7 = very much) [25].
2.3. Analysis software
Statistical analyses were performed in R (version 3.5.2). For the moderated mediation analysis, the lavaan package (version 0.6–5) was used [29].
2.4. Role of funding
This study was funded by the University of Erfurt and the German Research Foundation (BE-3979/11–1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
3. Results
We conducted the preregistered regression analysis to examine the effects of policy (selective mandates vs. voluntary vaccination) and communication (herd immunity vs. no herd immunity) as well as their interaction on vaccination intentions for the voluntary second vaccination (adjusted R2 = 0.038, F(3, 572) = 8-605, p < .001). Results revealed a statistically significant main effect of herd immunity communication, β = 2.802, t(572) = 4.418, p < .001, η2 = 0.040. Participants in the herd immunity communication condition reported a mean likeliness to get vaccinated of 16.14 or 79.9% (SD = 4.67 or 24.6 percentage points), compared to 13.92 or 68.0% (SD = 6.25 or 32.9 percentage points) for those who received no information about herd immunity. This confirms H1. There was no evidence for a main effect of policy, |t| < 1. Furthermore, no significant interaction between the communication and policy conditions could be found, t(572) = −1.299, p = .195, contradicting H2.
3.1. Exploratory analysis
We explored the effects of age, gender, education, and religion, none of which revealed any additional main or interaction effects in the above analysis. Moreover, we extended the above regression model by adding the predictors communal orientation (M = 5.21, SD = 1.03), whether children were old enough to get vaccinated, and all possible interaction terms. In comparison to the original model (adjusted R2 = 0.038), the amount of explained variance decreased (adjusted R2 = 0.035). No additional significant main or interaction effects could be found. In sum, demographic variables, communal orientation, and children's ages played no significant roles in predicting vaccination intentions.
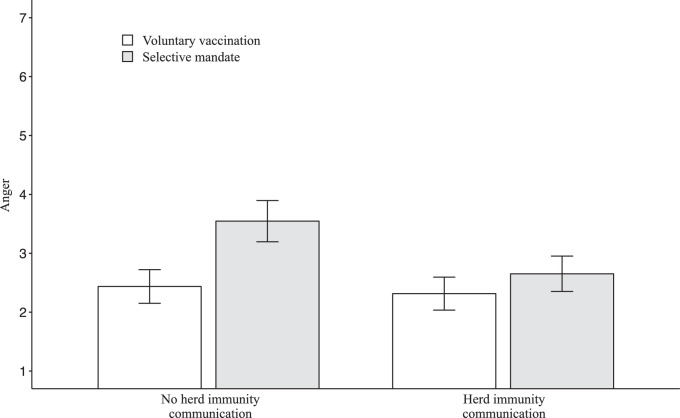
As anger was a relevant variable in previous work [17], we explored its role here, too. The mean anger was M = 2.70, SD = 1.89. Selective mandates in the first scenario significantly elicited anger (Table 2, top panel). However, herd immunity communication reduced anger in the selective mandates policy condition, revealing a significant interaction effect (Fig. 2 and Table 2, top panel). When forced to vaccinate in the first scenario, those who were not briefed about herd immunity felt more anger than those who were briefed (simple slope: β = 1.109, SE = 0.226, 95%CI [0.667, 1.552]). This effect was much weaker and not significant for those participants who were provided with information about herd immunity (simple slope: β = 0.337, SE = 0.207, 95%CI [−0.068, 0.742]).
Table 2.
Moderated mediation regression analysis.
| Mediator variable model (outcome: level of anger) | ||||
|---|---|---|---|---|
| Predictor | B | SE | CI lower | CI upper |
| Constant | 2.436 | 0.155 | 2.133 | 2.740 |
| Policy (a1) | 1.109 | 0.226 | 0.667 | 1.552 |
| Communication condition (a2) | −0.122 | 0.213 | −0.539 | 0.294 |
| Policy × Communication condition (a3) | −0.772 | 0.306 | −1.372 | −0.172 |
| Dependent variable model (outcome: vaccination intention in second scenario) | ||||
| Predictor | B | SE | CI lower | CI upper |
| Constant | 17.628 | 0.412 | 16.820 | 18.436 |
| Policy (c) | 0.454 | 0.443 | −0.415 | 1.323 |
| Anger (b) | −1.007 | 0.118 | −1.238 | −0.777 |
| Conditional indirect effect of selective mandate via level of anger on vaccination intention in second scenario | ||||
| Moderator condition | B | SE | CI lower | CI upper |
| Herd immunity communication ((a1 + a3) * b) | −0.340 | 0.212 | −0.755 | 0.076 |
| No herd immunity communication (a1 * b) | −1.117 | 0.262 | −1.631 | −0.603 |
Note: Policy condition: 0 = voluntary vaccination, 1 = selective mandate. Communication condition: 0 = no herd immunity communication, 1 = herd immunity communication. Both mediator and dependent variable models are based on OLS regressions. Letters in parentheses refer to the coefficients displayed in Fig. 3. Bold values are statistically significant with p < .05. CI lower and CI upper are the lower and upper endpoints of the 95% confidence interval.
Fig. 2.
Effects of policy and communication on anger. Note: Selective vaccination mandates caused higher ratings of anger than voluntary vaccinations did. When information about herd immunity was given, this effect did not appear. Anger was assessed as a mean of angriness, annoyance, and irritation after the first vaccination. Error bars indicate 95% confidence intervals. Further analysis revealed that higher levels of anger had a significant negative effect on the intention to receive a voluntary vaccination (middle panel of Table 1).
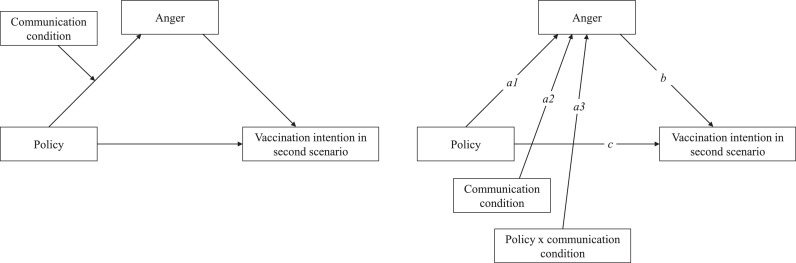
Given these differences, we explored whether anger mediated the relationship between policy and vaccination intentions in the second scenario and whether this was only the case when herd immunity had been communicated. Fig. 3 displays the tested moderated mediation model.
Fig. 3.
Moderated mediation model. Note: This model explores whether anger elicited by the selective mandate (vs. voluntary vaccination) policy mediates the relation between policy and the intention to get the second voluntary vaccine—and whether this is only the case when herd immunity has been communicated. The indices in the conceptual diagram (left) and statistical model (right) refer to the effects indicated in Table 2. The results show a significant conditional indirect effect (policy on intention via anger, but only when herd immunity was not communicated).
Table 2 provides the results (bottom panel). Indeed, the moderated mediation analysis showed that the indirect effect of selective mandates via anger on vaccination intentions (a1 × b) was only significant when no information about herd immunity was given. Results remained stable and did not qualitatively change when controlling for participants’ age, gender, education, religion, communal orientation, or whether their children were old enough to get vaccinated.
We finally explored whether vaccine confidence (M = 5.28, SD = 1.68) played a role in the level of anger elicited and whether herd immunity communication altered the level. Please note, however, that confidence was assessed after the dependent variables. We conducted an OLS regression with policy condition, herd immunity communication, and confidence as predictors (see https://osf.io/pnjs9/). While the pattern reported above remained stable, low confidence increased anger after mandatory vaccination (interaction policy x confidence, β = −0.438, SE = 0.128, 95%CI [−0.690, −0.186]); it did not, however, affect the effectiveness of the herd immunity communication (no three-way interaction, β = 0.060, SE = 0.175, 95%CI [−0.283, 0.402]).
4. Discussion
In order to ensure herd immunity against vaccine-preventable contagious diseases, it is essential that the vaccination coverage of the population remains above a disease specific threshold, e.g. 95% for measles [2,20]. In many countries, vaccine hesitancy hinders immunization efforts, resulting in regular outbreaks [1]. Selective vaccination mandates may represent a viable solution to the problem. In Italy, for instance, mandatory vaccinations against ten infectious diseases were introduced in 2017 after the country was struck by repeated measles outbreaks. Within 24 months after the change in legislation, coverage rates for the mandated vaccines had increased by between 3% and 7% depending on the disease [30]. For measles, the required immunization threshold of 95% was nearly attained [30]. Despite the measurable improvement in coverage rates, debates about ethical concerns and reactance effects of selective mandates on voluntary vaccinations are unbroken. The present study focused on diminishing potential negative psychological and behavioral effects of selective mandates by providing individuals with information about the concept of herd immunity. The analyses showed that communicating (vs. not communicating) about herd immunity had a significant positive effect on the intention to get vaccinated, replicating previous work [15]. Interestingly, this effect occurred independently of participants’ communal orientation and whether herd immunity was expected to be relevant to them because their children could not get vaccinated. Previous research showed that the benefit of communicating herd immunity is also independent of underlying moral values [16]. Cumulative evidence, demonstrating several replications and independence from individual dispositions and conditions, suggests that emphasizing the social benefits of vaccination has great value in vaccine communication. This finding is in line with our first hypothesis.
Selective mandates, however, did not have the expected overall negative effect on the intention to receive another voluntary vaccine, and there was no mitigating interaction effect(policy × communication); this finding contradicts our second hypothesis. However, the explorative moderated mediation showed that the selective mandate in the first scenario significantly elicited anger, but only when no information about herd immunity was given. Also, higher levels of anger had a negative effect on the intention to get vaccinated in the second scenario, voluntary vaccination. Thus, information about the social benefits of herd immunity buffered the negative effect of the selective mandate.
Analysis of the potentially moderating effects of vaccine confidence revealed that, for people low in confidence, the introduction of selective mandates resulted in especially high reactance. This is understandable because forcing someone into an untrusted behavior probably leads to even lower trust and confidence. However, importantly, the herd immunity communication worked equally well in these participants (as there was no three-way interaction). It is noteworthy, however, that most people in this study, as in real life [31], had high vaccine confidence. We suggest that further studies explicitly focus on individuals who hold negative attitudes toward vaccination (or have low vaccine confidence), assessing the impact of herd immunity communication in these especially vulnerable populations. Assessing its effectiveness also given different antecedents and barriers of getting vaccinated seems valuable, too, thus including not only confidence but also complacency, calculation, and constraints [25]. Finally, confidence should be measured before the assessment of vaccination intentions to be tested as a real experimental moderator.
The results should be generalized with caution. They were drawn from an American sample, but we expect a similar or even stronger effect of herd immunity communication for European countries like Germany. As stated above, people from the US are used to selective mandates. For Germany, where there have been no mandates for decades, herd immunity communication may even have a stronger impact on mitigating reactance induced by mandatory vaccination. Moreover, the fictitious scenario and the assessment of vaccination intentions without prior medical consultation may not be a perfect representation of real vaccine decision-making. Although intention usually predicts behavior, there may be a gap between the two caused by barriers such as limited access to vaccination services [25,32,33]. However, such lab research is important to inform future, potentially expensive, field studies. To overcome this limitation, we highly recommend conducting a field study about the effects of introducing selective vaccination mandates. For instance, as soon as the measles vaccination mandate is enacted in Germany in 2020, (a) detrimental effects on the acceptance of still-voluntary vaccinations against, for example, meningococcus, pneumococcus, or HPV, should be monitored; and (b) the buffering effect of herd immunity communication revealed in this study should be investigated under real-life conditions.
In sum, communicating the social benefits of herd immunity has several benefits. First, it can generally increase vaccination intentions by triggering prosocial motives. Second, it provides full information about the rationale of the mandate, increasing transparency in public policy and reducing objections toward vaccination mandates. Third, it could reduce reactance effects elicited in those feeling forced by policies. If selective mandates are introduced, the prosocial benefits of vaccination should therefore be highlighted on information sheets provided before the mandatory vaccinations take place. Of course, descriptions of the principle should be easy to understand and ideally supported by an interactive simulation [21]. Further, it should be emphasized that the vaccination especially protects those who have low responsibility for not being vaccinated, such as young children or individuals suffering from immunodeficiencies [34]. The dialog between healthcare personnel and patients plays a crucial role as well. For patients and parents, healthcare professionals are the most trusted source of information regarding vaccination [35]. Thus, when talking about vaccination, doctors and nurses should stress the importance of protecting others—loved ones, friends, the community, and society as a whole. On a larger scale, the introduction of selective vaccination mandates should be accompanied by public information campaigns highlighting the social benefits of vaccination. Overall, we conclude that communicating the social benefits of herd immunity is a crucial communication measure, especially when introducing selective vaccination mandates. Without it, vaccination uptake for other diseases may decline, putting public health at risk.
Declaration of Competing Interest
The authors have no conflicts of interest.
Acknowledgments
Authors’ contributions
Philipp Sprengholz: Conceptualization, Methodology, Investigation, Formal analysis, Writing—Original draft preparation, Visualization. Cornelia Betsch: Conceptualization, Methodology, Resources, Supervision, Writing—Review & Editing.
Footnotes
The preregistration form, experimental materials, data and the data analysis script are available at https://osf.io/pnjs9/.
Appendix. Supplementary materials
References
- 1.Dubé E., Gagnon D., Nickels E., Jeram S., Schuster M. Mapping vaccine hesitancy—Country-specific characteristics of a global phenomenon. Vaccine. 2014;32:6649–6654. doi: 10.1016/j.vaccine.2014.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wallinga J., Heijne J.C.M., Kretzschmar M. A measles epidemic threshold in a highly vaccinated population. PLoS Med. 2005;2:e316. doi: 10.1371/journal.pmed.0020316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thornton J... Measles cases in Europe tripled from 2017 to 2018. BMJ. 2019:l634. doi: 10.1136/bmj.l634. [DOI] [PubMed] [Google Scholar]
- 4.Government of Samoa. National emergency operation centre: update on the measles outbreak (Press release 23). 2019. https://reliefweb.int/report/samoa/national-emergency-operation-centre-update-measles-outbreak-press-release-23-december-9. (accessed Feb 25, 2020).
- 5.WHO. Measles outbreak in the pacific - Situation Report No. 9. 2019, https://www.who.int/docs/default-source/wpro---documents/dps/outbreaks-and-16emergencies/measles-2019/measles-pacific-who-unicef-sitrep-20200103.pdf?sfvrsn=82f90381_2. (accessed Feb 25, 2020).
- 6.Signorelli C., Odone A., Cella P., Iannazzo S. Childhood vaccine coverage in Italy after the new law on mandatory immunization. Ann Ig. 2018;30:1–10. doi: 10.7416/ai.2018.2227. [DOI] [PubMed] [Google Scholar]
- 7.Lévy-Bruhl D., Desenclos J.-.C., Quelet S., Bourdillon F. Extension of French vaccination mandates: from the recommendation of the steering committee of the citizen consultation on vaccination to the law. Eurosurveillance. 2018;23 doi: 10.2807/1560-7917.ES.2018.23.17.18-00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deutscher Bundestag. Entwurf eines Gesetzes für den Schutz vor Masern und zur Stärkung der Impfprävention. 2019. http://dipbt.bundestag.de/dip21/btd/18/112/1811277.pdf. (accessed Feb 1, 2020).
- 9.Robert Koch Institut. Epidemiologisches bulletin 34/2019. 2019. https://www.rki.de/DE/Content/Infekt/EpidBull/Archiv/2019/Ausgaben/34_19.pdf?__blob=publicationFile. (accessed March 20, 2020).
- 10.Robert Koch Institut. Annual status update on measles and rubella elimination: Germany. 2019.https://www.rki.de/DE/Content/Kommissionen/NAVKO/Berichte/Bericht_2018_en.pdf?__blob=publicationFile. (accessed Feb 1, 2020).
- 11.Gualano M., Olivero E., Voglino G. Knowledge, attitudes and beliefs towards compulsory vaccination: a systematic review. Hum Vaccin Immunother. 2019;15:918–931. doi: 10.1080/21645515.2018.1564437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vaz O.M., Ellingson M.K., Weiss P. Mandatory vaccination in Europe. Pediatrics. 2020 doi: 10.1542/peds.2019-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Williamson L., Glaab H... Addressing vaccine hesitancy requires an ethically consistent health strategy. BMC Med Ethics. 2018;19:84. doi: 10.1186/s12910-018-0322-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deutscher Ethikrat. Maßnahmenbündel zur Erhöhung der masernimpfquote statt allgemeiner impfpflicht. 2019. https://www.ethikrat.org/mitteilungen/2019/deutscher-ethikrat-massnahmenbuendel-zur-erhoehung-der-masernimpfquote-statt-allgemeiner-impfpflicht/. (accessed Feb 1, 2020).
- 15.Bensley L.S., Wu R... The role of psychological reactance in drinking following alcohol prevention messages1. J Appl Soc Psychol. 1991;21:1111–1124. [Google Scholar]
- 16.Brehm J.W... Academic Press; Oxford, England: 1966. A theory of psychological reactance. [Google Scholar]
- 17.Betsch C., Böhm R... Detrimental effects of introducing partial compulsory vaccination: experimental evidence. Eur J Public Health. 2016;26:378–381. doi: 10.1093/eurpub/ckv154. [DOI] [PubMed] [Google Scholar]
- 18.Omer S.B., Betsch C., Leask J. Mandate vaccination with care. Nature. 2019;571:469–472. doi: 10.1038/d41586-019-02232-0. [DOI] [PubMed] [Google Scholar]
- 19.YouGov. Eine impfpflicht bei masern? Die deutschen sagen ‘Ja’. 2019. https://yougov.de/news/2019/07/29/eine-impfpflicht-bei-masern-die-deutschen-sagen-ja/(accessed Feb 1, 2020).
- 20.Fine P., Eames K., Heymann D.L. Herd immunity: a rough guide. Clin Infect Dis. 2011;52:911–916. doi: 10.1093/cid/cir007. [DOI] [PubMed] [Google Scholar]
- 21.Betsch C., Böhm R., Korn L., Holtmann C. On the benefits of explaining herd immunity in vaccine advocacy. Nat Hum Behav. 2017;1:0056. [Google Scholar]
- 22.Betsch C., Böhm R. Moral values do not affect prosocial vaccination. Nat Hum Behav. 2018;2:881–882. doi: 10.1038/s41562-018-0478-1. [DOI] [PubMed] [Google Scholar]
- 23.Iyer R., Koleva S., Graham J., Ditto P., Haidt J. Understanding libertarian morality: the psychological dispositions of self-identified libertarians. PLoS ONE. 2012;7:e42366. doi: 10.1371/journal.pone.0042366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Steindl C., Jonas E... What reasons might the other one have?—Perspective taking to reduce psychological reactance in individualists and collectivists. Psychology. 2012;03:1153–1160. doi: 10.4236/psych.2012.312A170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Betsch C., Schmid P., Heinemeier D., Korn L., Holtmann C., Böhm R. Beyond confidence: development of a measure assessing the 5C psychological antecedents of vaccination. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0208601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buhrmester M., Kwang T., Gosling S.D. Amazon's mechanical turk. Perspect Psychol Sci. 2011;6:3–5. doi: 10.1177/1745691610393980. [DOI] [PubMed] [Google Scholar]
- 27.Dillard J.P., Shen L... On the nature of reactance and its role in persuasive health communication. Commun Monogr. 2005;72:144–168. [Google Scholar]
- 28.Clark M.S., Oullette R., Powell M.C., Milberg S. Recipient's mood, relationship type, and helping. J Pers Soc Psychol. 1987;53:94–103. doi: 10.1037//0022-3514.53.1.94. [DOI] [PubMed] [Google Scholar]
- 29.Rosseel Y... lavaan : an r package for structural equation modeling. J Stat Softw. 2012;48 [Google Scholar]
- 30.D'Ancona F., D'Amario C., Maraglino F., Rezza G., Iannazzo S. The law on compulsory vaccination in Italy: an update 2 years after the introduction. Eurosurveillance. 2019;24 doi: 10.2807/1560-7917.ES.2019.24.26.1900371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Larson H.J... The state of vaccine confidence. Lancet. 2018;392:2244–2246. doi: 10.1016/S0140-6736(18)32608-4. [DOI] [PubMed] [Google Scholar]
- 32.Sheeran P. Intention—Behavior relations: a conceptual and empirical review. Eur Rev Soc Psychol. 2002;12:1–36. [Google Scholar]
- 33.Lehmann B.A., Ruiter R.A.C., Chapman G., Kok G. The intention to get vaccinated against influenza and actual vaccination uptake of Dutch healthcare personnel. Vaccine. 2014;32:6986–6991. doi: 10.1016/j.vaccine.2014.10.034. [DOI] [PubMed] [Google Scholar]
- 34.Böhm R., Meier N.W., Groß M., Korn L., Betsch C. The willingness to vaccinate increases when vaccination protects others who have low responsibility for not being vaccinated. J Behav Med. 2019;42:381–391. doi: 10.1007/s10865-018-9985-9. [DOI] [PubMed] [Google Scholar]
- 35.Gust D.A., Kennedy A., Shui I., Smith P.J., Nowak G., Pickering L.K. Parent attitudes toward immunizations and healthcare providers. Am J Prev Med. 2005;29:105–112. doi: 10.1016/j.amepre.2005.04.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.