This meta-analysis of 10 randomized clinical trials assesses whether complete revascularization is associated with reduced cardiovascular mortality and whether heterogeneity is found in treatment outcomes when fractional flow reserve– and angiography-guided nonculprit lesion percutaneous coronary intervention strategies are performed.
Key Points
Question
Compared with a culprit-lesion-only percutaneous coronary intervention strategy, is a strategy of complete revascularization with multivessel percutaneous coronary intervention associated with decreased cardiovascular mortality in ST-segment elevation myocardial infarction, and what is the association when fractional flow reserve– and angiography-guided complete revascularization approaches are used?
Findings
In this systematic review and meta-analysis of 10 randomized clinical trials of 7030 unique patients, a 31% relative risk reduction in cardiovascular death (no significant reduction in all-cause mortality) was associated with a complete revascularization strategy. Consistent associations were found when a fractional flow reserve– or angiography-guided complete revascularization approach was used.
Meaning
These results potentially extend the benefit of a complete revascularization strategy to include a reduction in cardiovascular mortality with a consistent benefit of a fractional flow reserve– or angiography-guided percutaneous coronary intervention approach on hard clinical events.
Abstract
Importance
Recently, the Complete vs Culprit-Only Revascularization to Treat Multivessel Disease After Early PCI (percutaneous coronary intervention) for STEMI (ST-segment elevation myocardial infarction [MI]) (COMPLETE) trial showed that angiography-guided PCI of the nonculprit lesion with the goal of complete revascularization reduced cardiovascular (CV) death or new MI compared with PCI of the culprit lesion only in STEMI. Whether complete revascularization also reduces CV mortality is uncertain. Moreover, whether the association of complete revascularization with hard clinical outcomes is consistent when fractional flow reserve (FFR)– and angiography-guided strategies are used is unknown.
Objective
To determine through a systematic review and meta-analysis (1) whether complete revascularization is associated with decreased CV mortality and (2) whether heterogeneity in the association occurs when FFR- and angiography-guided PCI strategies for nonculprit lesions are performed.
Data Sources
A systematic search of MEDLINE, Embase, ISI Web of Science, and CENTRAL (Cochrane Central Register of Controlled Trials) from database inception to September 30, 2019, was performed. Conference proceedings were also reviewed from January 1, 2002, to September 30, 2019.
Study Selection
English-language randomized clinical trials comparing complete revascularization vs culprit-lesion-only PCI in patients with STEMI and multivessel disease were included.
Data Extraction and Synthesis
The combined odds ratio (OR) was calculated with the random-effects model using the Mantel-Haenszel method (sensitivity with fixed-effects model). Heterogeneity was measured using the I2 statistic. Publication bias was evaluated using the inverted funnel plot approach. Data were analyzed from October 2019 to January 2020.
Main Outcomes and Measures
Cardiovascular death and the composite of CV death or new MI.
Results
Ten randomized clinical trials involving 7030 unique patients were included. The weighted mean follow-up time was 29.5 months. Complete revascularization was associated with reduced CV death compared with culprit-lesion-only PCI (80 of 3191 [2.5%] vs 106 of 3406 [3.1%]; OR, 0.69 [95% CI, 0.48-0.99]; P = .05; fixed-effects model OR, 0.74 [95% CI, 0.55-0.99]; P = .04). All-cause mortality occurred in 153 of 3426 patients (4.5%) in the complete revascularization group vs 177 of 3604 (4.9%) in the culprit-lesion-only group (OR, 0.84 [95% CI, 0.67-1.05]; P = .13; I2 = 0%). Complete revascularization was associated with a reduced composite of CV death or new MI (192 of 2616 [7.3%] vs 266 of 2586 [10.3%]; OR, 0.69 [95% CI, 0.55-0.87]; P = .001; fixed-effects model OR, 0.69 [95% CI, 0.57-0.84]; P < .001), with no heterogeneity in this outcome when complete revascularization was performed using an FFR-guided strategy (OR, 0.78 [95% CI, 0.43-1.44]) or an angiography-guided strategy (OR, 0.61 [95% CI, 0.38-0.97]; P = .52 for interaction).
Conclusions and Relevance
In patients with STEMI and multivessel disease, complete revascularization was associated with a reduction in CV mortality compared with culprit-lesion-only PCI. There was no differential association with treatment between FFR- and angiography-guided strategies on major CV outcomes.
Introduction
The 2017 European Society of Cardiology guidelines for management of ST-segment elevation myocardial infarction (STEMI) state that routine revascularization of non–infarct-related artery lesions should be considered in patients with multivessel disease before hospital discharge with a class IIA (level of evidence A) recommendation.1 The 2015 American College of Cardiology/American Heart Association/Society for Cardiovascular Angiography and Interventions focused update on STEMI supports nonculprit-vessel intervention as a class IIB (level of evidence B) recommendation.2 These recommendations were based on the results of recent randomized clinical trials (RCTs) and meta-analyses documenting improved outcomes with complete revascularization with percutaneous coronary intervention (PCI) in STEMI. However, these results have been driven mainly by composite end points that include subsequent ischemia-driven revascularization.3 Recently, the Complete vs Culprit-Only Revascularization to Treat Multivessel Disease After Early PCI for STEMI (COMPLETE) study demonstrated that a strategy of complete revascularization with staged PCI of the nonculprit lesion reduced the composite of cardiovascular (CV) death and new myocardial infarction (MI).4 The COMPLETE trial was not powered to detect reductions in CV death alone, hence it remains uncertain whether complete revascularization reduces this outcome. In addition, it is unclear whether a difference in CV events occurs when a fractional flow reserve (FFR)– or an angiography-guided strategy is used for complete revascularization. Accordingly, we performed a collaborative meta-analysis of RCTs to determine (1) whether complete revascularization is associated with decreased CV mortality and (2) the consistency of the association when FFR- and angiography-guided nonculprit-lesion PCI strategies are performed.
Methods
The present systematic review and meta-analysis was performed in accordance with the Cochrane Handbook for Systematic Reviews and Interventions.5 Analysis is reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement in health care interventions.
Search Strategy
We searched PubMed/MEDLINE, Ovid/Embase, ISI Web of Science, and CENTRAL (Cochrane Central Register of Controlled Trials) from database inception through the final search date of September 30, 2019, for studies published in English. Conference presentations and abstracts from the American Heart Association, American College of Cardiology, Transcatheter Therapeutics, European Society of Cardiology, and EuroPCR were hand-searched from January 1, 2002, to September 30, 2019. Reference lists of included studies, relevant articles, and related systematic reviews were assessed. The search strategy used the following keywords: “ST elevation myocardial infarction,” “myocardial infarction,” “complete revascularization,” “multivessel revascularization,” and “nonculprit coronary artery” (eTable in the Supplement).
Study Selection
Two reviewers (K.R.B., S.R.M.) independently screened for RCTs comparing complete vs culprit-lesion-only PCI in patients with STEMI and multivessel disease. Only RCTs comparing multivessel vs culprit-lesion-only PCI in patients with STEMI and multivessel disease undergoing primary PCI were included. Studies enrolling patients with a diagnosis other than STEMI or comparing revascularization strategies other than PCI were excluded. Full-text citations and abstracts (ie, unpublished) were selected and independently screened for eligibility. Unpublished citations were intentionally included to mitigate publication bias. A PRISMA flow diagram can be found in eFigure 1 in the Supplement.
Data Abstraction
Information regarding the study design, intervention performed, number of patients enrolled, inclusion and exclusion criteria, clinical outcomes, and follow-up duration was obtained. The quality of abstracted studies was assessed using the Cochrane Collaboration’s tool for assessing risk of bias for randomized studies. Only results calculated using the intention-to-treat principle were included.
Outcomes
Information regarding CV death and a composite of CV death or new MI were collected. The composite outcome was stratified according to FFR- or angiography-guided PCI.
Statistical Analysis
Data were analyzed from October 2019 to January 2020. All statistical analysis was performed using Review Manager, version 5 (Cochrane Center). Odds ratios (ORs) with 95% CIs were used as summary estimates. The pooled OR was calculated with the random-effects model using the Mantel-Haenszel method. Heterogeneity was measured using the I2 statistic ([I2 − Q − df]/Q], where Q is the χ2 statistic and df is degrees of freedom). A value for I2 of 0 to 30% represents low heterogeneity; greater than 30% to 60%, moderate heterogeneity; and greater than 60% to 90%, severe heterogeneity (ie, should be explored). Values greater than 90% to 100% must be evaluated with extreme caution. The potential for publication bias was evaluated using the inverted funnel plot approach. Two-sided P < .05 indicated significance and was calculated using a z test of the null hypothesis that there is no average effect in the random-effects model of complete revascularization versus culprit-lesion-only PCI.
Sensitivity Analysis
A pooled OR with 95% CI was calculated for the outcomes using a fixed-effects model with the Mantel-Haenszel method. A pooled OR with 95% CI was calculated for CV mortality with the addition of the CULPRIT-SHOCK (Culprit Lesion Only PCI Vs Multivessel PCI in Cardiogenic Shock) trial.6
Results
Search and Selection of Studies
In total, 125 abstracts were identified, and 31 were selected for full-text or abstract (unpublished) review. Of these 31 eligible studies, 21 were excluded for the following reasons: therapies were not randomly allocated (n = 14), a control group was not identified (n = 3), patients without STEMI were included (n = 3), or coronary artery bypass grafting surgery was performed (n = 1). Ten RCTs fulfilled the eligibility criteria and were included in the present systematic review.4,7,8,9,10,11,12,13,14,15 The inverted funnel plots for the primary outcome of CV mortality alone and CV mortality or new MI did not suggest publication bias (eFigures 2 and 3 in the Supplement).
Included Studies
Ten RCTs of complete vs culprit-lesion-only PCI involving 7030 patients (3426 undergoing complete revascularization and 3604 undergoing culprit-lesion-only PCI) were included.4,7,8,9,10,11,12,13,14,15 The weighted mean follow-up time was 29.5 months. The Table presents the characteristics of the included studies. Three studies performed complete revascularization with FFR-guided nonculprit-lesion PCI,9,12,15 whereas the 7 remaining studies used an angiography-guided approach for nonculprit-lesion PCI.4,7,8,10,11,13,14 Complete revascularization with multivessel PCI was performed exclusively during the same sitting in 2 studies7,10 and largely during the same sitting in a further 2 studies.13,15 In 1 study,8 nonculprit-lesion PCI was performed during the same sitting or as a staged procedure. In the 4 remaining studies,4,9,11,12 complete revascularization was performed only as a staged procedure.
Table. Summary of 10 RCTs Comparing Complete Revascularization With Culprit-Lesion-Only PCI.
| Source | Intervention | No. of patients | Inclusion criteria | Exclusion criteria | Primary outcome |
|---|---|---|---|---|---|
| Di Mario et al,7 2004 | Culprit-vessel PCI with additional revascularization at the investigators’ discretion vs culprit-vessel PCI with immediate multivessel treatment during index catheterization | 69 | STEMI with MVD and 1-3 lesions in nonculprit artery technically amenable to revascularization by stent | Lesion in vein and arterial grafts, prior angioplasty, thrombolysis, cardiogenic shock, LM disease | 12-mo Incidence of repeated revascularization (any revascularization, IRA as well as non-IRA) |
| Politi et al,8 2010 | Culprit-vessel PCI vs culprit-vessel PCI plus multivessel PCI during index catheterization or staged procedure | 214 | STEMI with >70% stenosis of ≥2 coronary arteries or major branches | Cardiogenic shock, LM disease, previous CABG, severe valvular heart disease, unsuccessful procedure | Mean: 30-mo MACE defined as cardiac or noncardiac death, in-hospital death, reinfarction, rehospitalization for acute coronary syndrome, repeated coronary revascularization |
| Ghani et al,9 2012 | Culprit-vessel PCI with ischemia-guided additional revascularization only if symptoms recurred vs culprit-vessel PCI plus PCI of severe lesion (>90%) or FFR-guided PCI in vessels with significant stenosis (<90%) as a staged procedure | 119 | STEMI with >50% stenosis of ≥2 epicardial arteries | Urgent revascularization, aged >80 y, CTO of non-IRA, prior CABG, LM≥50%, ISR in non-IRA, chronic atrial fibrillation, limited life expectancy, other factors that make follow-up unlikely | 36-mo MACE defined as death, nonfatal reinfarction, additional revascularization procedures |
| Wald et al,10 2013 | Culprit-vessel-only PCI vs preventive PCI with culprit- and nonculprit-vessel PCI performed during the index catheterization | 465 | STEMI with MVD of >50% stenosis of ≥2 epicardial arteries | Cardiogenic shock, LM disease, previous CABG, CTO | Mean: 23-mo death due to cardiac causes, nonfatal MI, refractory angina |
| Gershlick et al,13 2015 | Culprit-only PCI vs complete revascularization mainly index admission (mainly same sitting) | 296 | STEMI of <12 h onset with MVD and noninfarct artery stenosis >70% | Cardiogenic shock, prior CABG, CKD, VSD, severe MR, previous q wave infarction | 12-mo All-cause death, recurrent MI, heart failure, ischemia-driven revascularization |
| Engstrøm et al,12 2015 | Culprit-only PCI vs complete FFR-guided revascularization as a staged PCI (2 d later) | 627 | STEMI of <12 h onset with MVD and noninfarct artery stenosis >70% | Cardiogenic shock, stent thrombosis, CABG, intolerance of contrast media, increased bleeding risk | Median (range): 27 (12-44)-mo all-cause mortality, nonfatal MI, ischemia-driven revascularization of lesions in non-IRAs |
| Hlinomaz et al,11 2015 | Culprit-only PCI vs complete revascularization as a staged PCI (3-40 d later) | 214 | STEMI with MVD and noninfarct artery stenosis ≥70% | Cardiogenic shock, LM disease, significant valve disease, angina (CCS II) lasting 1 mo before STEMI | Median: 38-mo all-cause mortality, nonfatal MI, stroke |
| Hamza et al,14 2016 | Culprit-vessel-only vs complete revascularization during index procedure or staged within 72 h in patients with diabetes | 100 | STEMI with MVD in patients with diabetes within 12 h of symptoms | MVD with 50%-70% stenosis, CTO, prior CABG, LM disease | 6-mo All-cause mortality, recurrent MI, ischemia-driven revascularization |
| Smits et al,15 2017 | Culprit-vessel-only vs FFR-guided multivessel PCI during the index procedure | 885 | STEMI with MVD that was appropriate for FFR and PCI | Hemodynamically unstable | 12-mo Death due to any cause, nonfatal MI, revascularization, cerebrovascular event |
| Mehta et al,4 2019 | Culprit-vessel-only vs staged complete revascularization either in hospital or electively (within 45 d) | 4041 | STEMI randomized within 72 h after culprit-lesion PCI | Prerandomization revascularization of a nonculprit lesion, planned surgical intervention, prior CABG | 3-y Coprimary outcome of a composite of cardiovascular death or new MI and composite of cardiovascular death, new MI, or ischemia-driven revascularization |
Abbreviations: CABG, coronary artery bypass grafting; CCS, Canadian Cardiovascular Society; CKD, chronic kidney disease; CTO, chronic total occlusion; FFR, fractional flow reserve; IRA, infarct-related artery; ISR, in-stent restenosis; LM, left main; MACE, major adverse cardiovascular events; MI, myocardial infarction; MR, mitral regurgitation; MVD, multivessel disease; PCI, percutaneous coronary intervention; RCT, randomized clinical trial; STEMI, ST-segment elevation myocardial infarction; VSD, ventricular septal defect.
Clinical Outcomes
Cardiovascular Death
A total of 80 CV deaths (2.5%) occurred in 3191 patients undergoing complete revascularization compared with 106 (3.1%) in 3406 patients undergoing culprit-lesion-only PCI, a 31% relative risk reduction, among the 7 trials reporting this outcome4,7,8,10,12,13,15 (OR, 0.69 [95% CI, 0.48-0.99]; P = .05; I2 = 9%) (Figure 1). Similar results were observed using a fixed-effects model (OR, 0.74 [95% CI, 0.55-0.99]; P = .04; I2 = 9%).
Figure 1. Forest Plot of Long-term Cardiovascular Death in Patients With Complete Revascularization or Culprit-Lesion-Only Percutaneous Coronary Intervention (PCI).
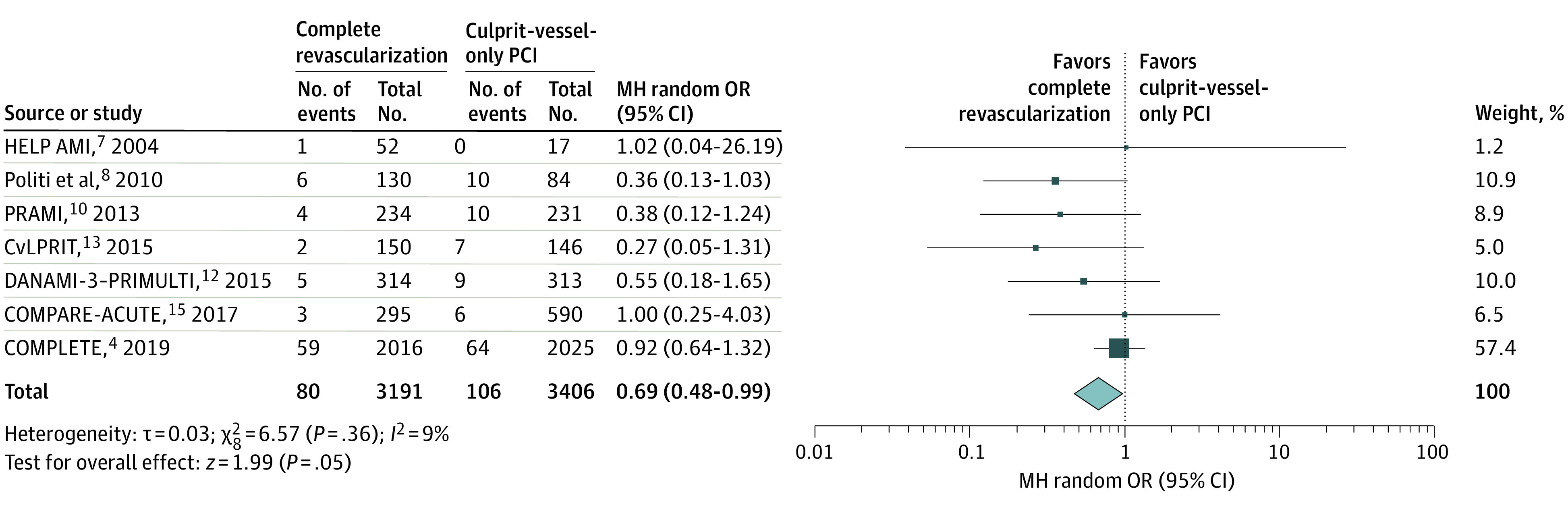
Size of markers represents weight. Squares and diamonds indicate odds ratios (ORs); error bars, 95% CIs. COMPARE-ACUTE indicates Fractional Flow Reserve Guided Primary Multivessel Percutaneous Coronary Intervention to Improve Guideline Indexed Actual Standard of Care for Treatment of ST-Elevation Myocardial Infarction in Patients With Multivessel Coronary Disease; COMPLETE, Complete vs Culprit-Only Revascularization to Treat Multivessel Disease After Early PCI for STEMI; CvLPRIT, Complete vs Lesion-Only Primary PCI Trial; DANAMI-3–PRIMULTI, Primary PCI in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease: Treatment of Culprit Lesion Only or Complete Revascularization; HELP AMI, Hepacoat for Culprit or Multivessel Stenting for Acute Myocardial Infarction; MH random, random-effects model using the Mantel-Haenszel method; and PRAMI, Preventive Angioplasty in Myocardial Infarction.
Among the 10 studies reporting all-cause death,4,7,8,9,10,11,12,13,14,15 153 deaths (4.5%) among 3426 patients occurred with complete revascularization vs 177 deaths (4.9%) among 3604 patients with culprit-lesion-only PCI (OR, 0.84 [95% CI, 0.67-1.05]; P = .13; I2 = 0%) (eFigure 4 in the Supplement). Similar results were observed using a fixed-effects model (OR, 0.84 [95% CI, 0.67-1.05]; P = .13; I2 = 0%).
CV Death or New MI
Four studies4,7,10,12 reported CV death or new MI (Figure 2). Among these studies, 192 events (7.3%) occurred in the 2616 patients undergoing complete revascularization compared with 266 events (10.3%) in 2586 patients undergoing the culprit-lesion-only strategy (OR, 0.69 [95% CI, 0.55-0.87]; P = .001; I2 = 6%). Similar results were noted using a fixed-effects model (OR, 0.69 [95% CI, 0.57-0.84]; P < .001; I2 = 6%).
Figure 2. Forest Plot of Long-term Cardiovascular Death or New Myocardial Infarction in Patients With Complete Revascularization or Culprit-Lesion-Only Percutaneous Coronary Intervention (PCI).
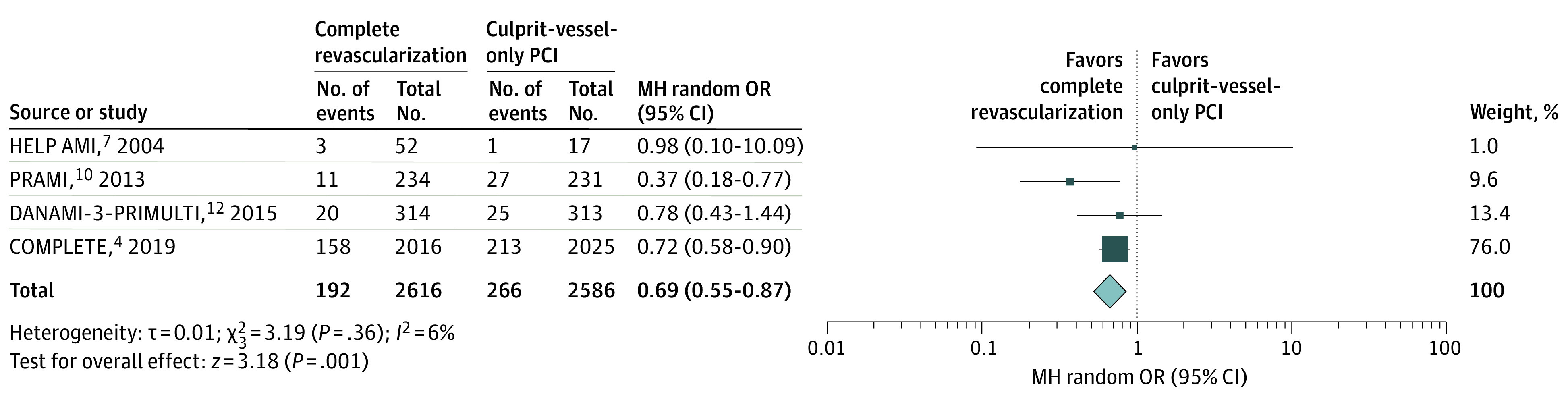
Size of markers represents weight. Squares and diamonds indicate odds ratios (ORs); error bars, 95% CIs. COMPLETE indicates Complete vs Culprit-Only Revascularization to Treat Multivessel Disease After Early PCI for STEMI; DANAMI-3–PRIMULTI, Primary PCI in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease: Treatment of Culprit Lesion Only or Complete Revascularization; HELP AMI, Hepacoat for Culprit or Multivessel Stenting for Acute Myocardial Infarction; MH random, random-effects model using the Mantel-Haenszel method; and PRAMI, Preventive Angioplasty in Myocardial Infarction.
New MI
Ten studies4,7,8,9,10,11,12,13,14,15 reported new MI (eFigure 5 in the Supplement). A total of 175 new MIs (5.1%) occurred in the 3426 patients undergoing complete revascularization compared with 247 (6.9%) in 3604 patients undergoing culprit-lesion-only PCI (OR, 0.68 [95% CI, 0.49-0.96]; P = .03; I2 = 26%). This result was consistent when a fixed-effects model was used (OR, 0.70 [95% CI, 0.57-0.85]; P < .001; I2 = 26%).
FFR- vs Angiography-Guided Nonculprit-Lesion PCI
For CV death or new MI, a consistent benefit with complete revascularization was found compared with culprit-lesion-only PCI when an FFR-guided nonculprit-lesion PCI strategy was used (OR, 0.78 [95% CI, 0.43-1.44]; P = .43) and when an angiography-guided nonculprit-lesion PCI strategy was used (OR, 0.61 [95% CI, 0.38-0.97]; P = .04; I2 = 34%), with no evidence of heterogeneity between these subgroups (P = .52 for interaction) (Figure 3). Similarly, no differential association of treatment was found between an FFR-guided (OR, 0.69 [95% CI, 0.29-1.64]; P = .40; I2 = 0%) or an angiography-guided (OR, 0.57 [95% CI, 0.32-1.03]; P = .06; I2 = 34%) complete revascularization strategy compared with a culprit-lesion-only strategy on CV death alone (P = .73 for interaction) (Figure 4). In addition, there was no differential association with treatment between FFR-guided multivessel PCI (OR, 1.03 [95% CI, 0.32-3.29]; P = .95; I2 = 70%) or angiography-guided multivessel PCI (OR, 0.65 [95% CI, 0.52-0.82]; P < .001; I2 = 0%) on MI alone (P = .44 for interaction) (eFigure 6 in the Supplement).
Figure 3. Forest Plot of Long-term Cardiovascular Death or New Myocardial Infarction Stratified by Approach in Patients With Complete Revascularization or Culprit-Lesion-Only Percutaneous Coronary Intervention (PCI).
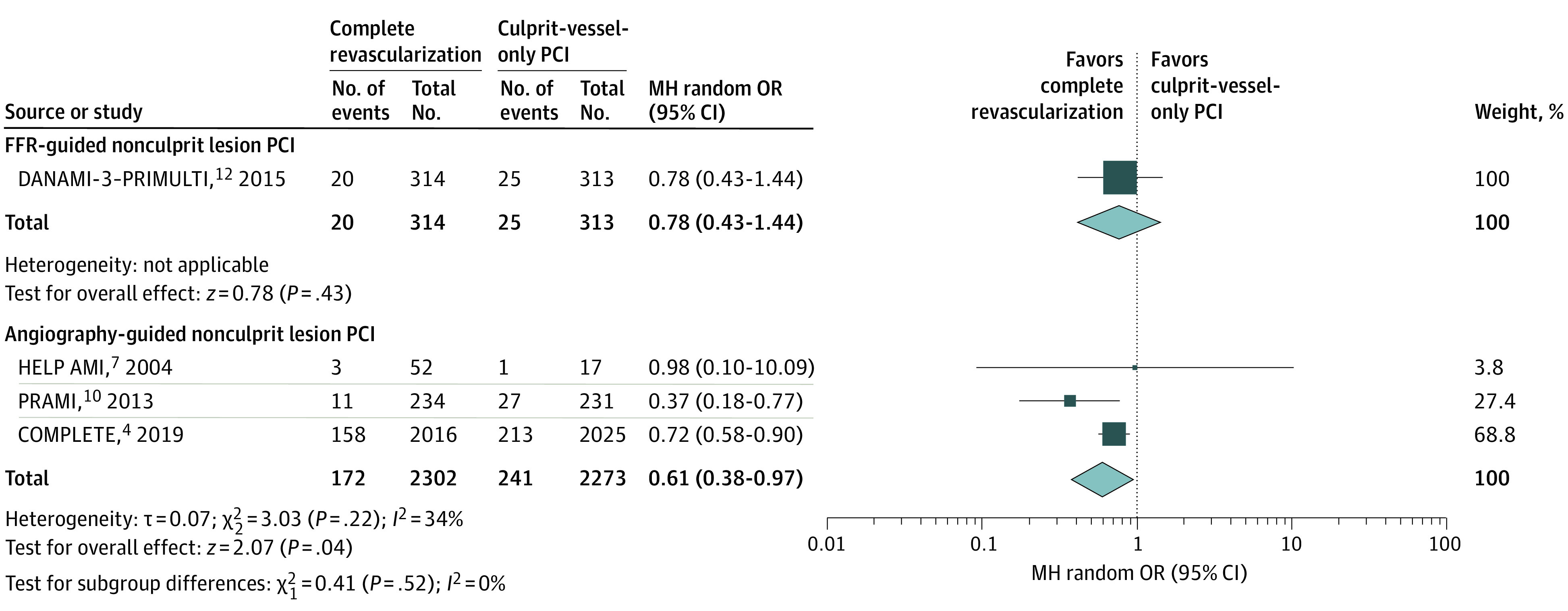
Patients were stratified by a fractional flow reserve (FRR)– vs angiography-guided nonculprit-lesion approach. Size of markers represents weight. Squares and diamonds indicate odds ratios (ORs); error bars, 95% CIs. COMPLETE, Complete vs Culprit-Only Revascularization to Treat Multivessel Disease After Early PCI for STEMI; DANAMI-3–PRIMULTI, Primary PCI in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease: Treatment of Culprit Lesion Only or Complete Revascularization; HELP AMI, Hepacoat for Culprit or Multivessel Stenting for Acute Myocardial Infarction; MH random, random-effects model using the Mantel-Haenszel method; and PRAMI, Preventive Angioplasty in Myocardial Infarction.
Figure 4. Forest Plot of Long-term Cardiovascular Death Stratified by Approach in Patients With Complete Revascularization or Culprit-Lesion-Only Percutaneous Coronary Intervention (PCI).
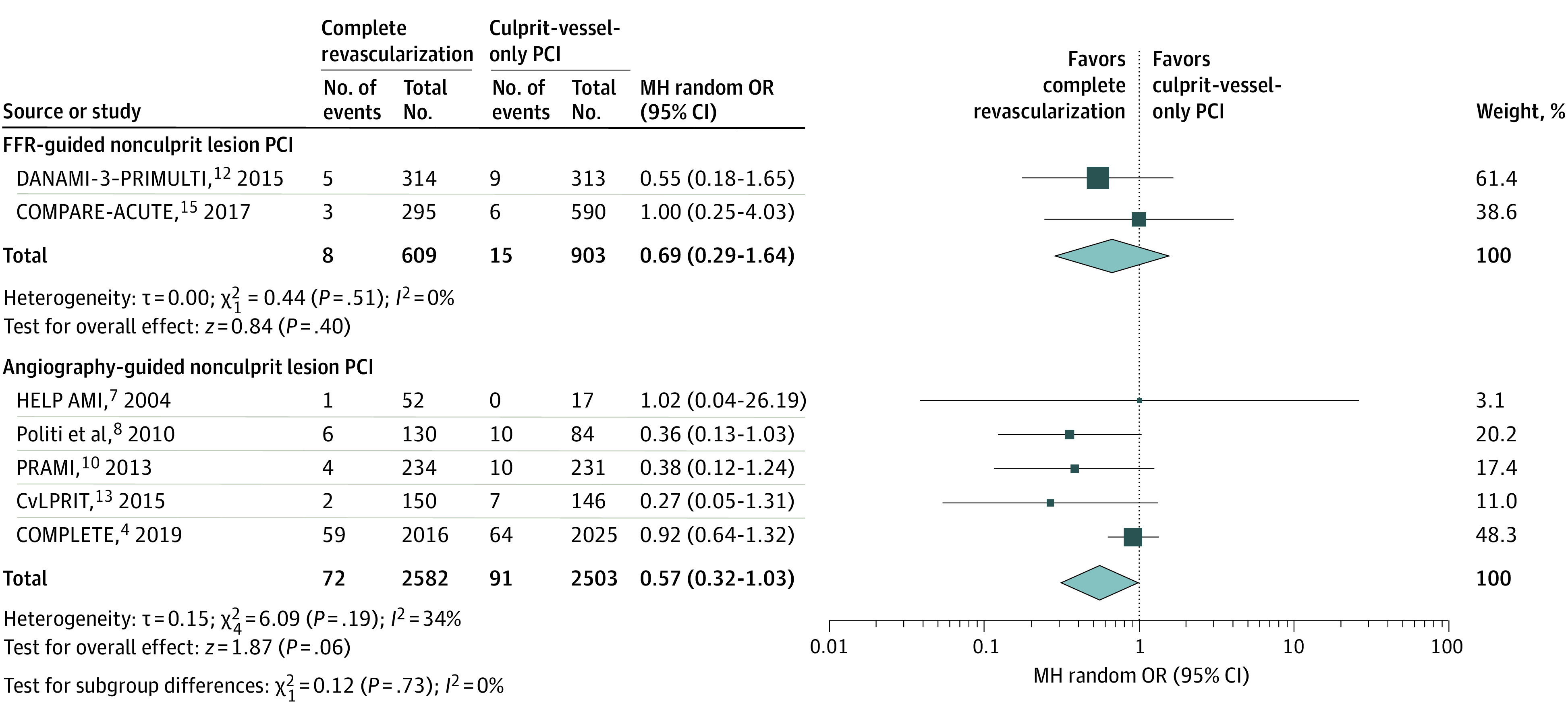
Patients were stratified by a fractional flow reserve (FRR)– vs angiography-guided nonculprit-lesion approach. Size of markers represents weight. Squares and diamonds indicate odds ratios (ORs); error bars, 95% CIs. COMPLETE indicates Complete vs Culprit-Only Revascularization to Treat Multivessel Disease After Early PCI for STEMI; CvLPRIT, Complete vs Lesion-Only Primary PCI Trial; DANAMI-3–PRIMULTI, Primary PCI in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease: Treatment of Culprit Lesion Only or Complete Revascularization; HELP AMI, Hepacoat for Culprit or Multivessel Stenting for Acute Myocardial Infarction; MH random, random-effects model using the Mantel-Haenszel method; and PRAMI, Preventive Angioplasty in Myocardial Infarction.
Single-Sitting vs Staged Approach to Complete Revascularization
In an analysis stratified by timing of nonculprit-lesion PCI, complete revascularization compared with culprit-lesion-only PCI was associated with reduced CV death or new MI in patients undergoing same-sitting multivessel PCI (OR, 0.41 [95% CI, 0.20-0.81]; P = .01; I2 = 0%) as well those treated with a staged approach (OR, 0.73 [95% CI, 0.60-0.89]; P = .002; I2 = 0%), with no difference in the association of treatment (P = .11 for interaction) (eFigure 7 in the Supplement). Similar findings were observed with the individual end points of CV death alone for same-sitting PCI (OR, 0.49 [95% CI, 0.26-0.94]; P = .03; I2 = 0%) and staged-approach PCI (OR, 0.88 [95% CI, 0.62-1.24]; P = .46; I2 = 0%; P = .12 for interaction) (eFigure 8 in the Supplement) and MI alone for same-sitting PCI (OR, 0.46 [95% CI, 0.27-0.77]; P = .003; I2 = 0%) and staged PCI (OR, 0.93 [95% CI, 0.55-1.58]; P = .80; I2 = 50%; P = .06 for interaction) (eFigure 9 in the Supplement).
As a sensitivity analysis, we added the results of CV mortality (sudden cardiac death, death due to cardiogenic shock, or death due to recurrent MI) from the CULPRIT-SHOCK trial.6 We found a directionally consistent result for CV mortality (OR, 0.80 [95% CI, 0.58-1.09]; P = .15; I2 = 25%) (eFigure 10 in the Supplement).
Discussion
In the largest meta-analysis performed to date, a strategy of complete revascularization with nonculprit-lesion PCI was associated with a reduction in CV mortality compared with a strategy of culprit-lesion-only PCI in patients with STEMI and multivessel disease without cardiogenic shock at presentation. Furthermore, we have shown a reduction in the composite outcome of CV death or new MI with complete revascularization irrespective of whether it is performed with an FFR- or an angiography-guided nonculprit-lesion PCI strategy.
None of the individual RCTs comparing complete revascularization with a culprit-lesion-only strategy were adequately powered to detect reductions in CV mortality. In the largest meta-analysis, to our knowledge, involving more than 7000 patients from these trials, we observed a 31% relative risk reduction in CV mortality with complete revascularization. Although this outcome was nominally significant, a fixed-effects analysis demonstrated a similar outcome. Moreover, our findings have been confirmed in a recent meta-analysis of 6 randomized studies16 (6528 patients) showing a 38% reduction in CV death. This reduction in CV mortality is consistent with a robust reduction in new MI observed with complete revascularization. Results from the Optical Coherence Tomography (OCT) COMPLETE substudy have demonstrated that approximately one-half of obstructive nonculprit lesions contain unstable plaque morphology.17 Hence, routine nonculprit-lesion PCI as a preventive strategy could reduce subsequent MI and potentially improve CV long-term survival.
A novel finding of our meta-analysis is the consistent benefit of an FFR- and angiography-guided, nonculprit-lesion complete revascularization approach. Although FFR might underestimate in some cases the severity of nonculprit lesions in the acute and subacute phases,18,19 the outcomes of the FFR-guided trials were consistent with those of the angiography-guided studies, even after deferring PCI of nonculprit lesions in 31% to 44% of the patients.12,15 Still, a recent study has speculated regarding the accuracy of hyperemic and resting indices of nonculprit STEMI lesions,20 and the optimal timing of performing these measurements is unclear.21 Moreover, unlike an angiography-guided approach, the individual FFR-guided PCI trials have not shown a reduction in CV death or MI. However, a recent patient-level pooled analysis of FAME II (Fractional Flow Reserve-Guided Percutaneous Coronary Intervention Plus Optimal Medical Treatment Vs Optimal Medical Treatment Alone in Patients With Stable Coronary Artery Disease), DANAMI-PRIMULTI (Primary PCI in Patients With ST-Elevation Myocardial Infarction and Multivessel Disease: Treatment of Culprit Lesion Only or Complete Revascularization), and COMPARE-ACUTE (Fractional Flow Reserve Guided Primary Multivessel Percutaneous Coronary Intervention to Improve Guideline Indexed Actual Standard of Care for Treatment of ST-Elevation Myocardial Infarction in Patients With Multivessel Coronary Disease) did show a reduction in CV death or MI (mainly driven by a decreased risk of MI) with FFR-guided PCI.22 Hence, we believe there is equipoise as to the optimal strategy for complete revascularization in STEMI with multivessel disease that needs to be addressed in a large RCT.
We demonstrated consistent benefits of complete revascularization regardless of whether the nonculprit-lesion PCI procedure was performed during the same sitting or as a staged procedure. In the COMPLETE trial, recurrent events were reduced mainly during the long term with complete revascularization, with little difference in the first 45 days after the index STEMI.4 No heterogeneity in the association with treatment was detected in those patients with staged complete revascularization early during the index hospitalization or electively as an outpatient (≤45 days).23 This finding suggests that early events after STEMI are mainly owing to the size and severity of the index STEMI itself rather than nonculprit lesions. Analogous to revascularization outcomes with coronary artery bypass grafting surgery, the benefits of complete revascularization with PCI appear to accrue long term. Hence, our data provide reassurance to clinicians who are contemplating the timing of complete revascularization with PCI.
In the context of our meta-analysis, the findings of the CULPRIT-SHOCK trial deserve attention. In patients with acute MI (STEMI or non-STEMI) and cardiogenic shock, a significant reduction in the primary composite of all-cause death or severe renal failure requiring renal replacement therapy was observed with a culprit-lesion-only strategy compared with compete revascularization during the index event, with an 8.2% absolute reduction in mortality at 30 days (recognizing staged revascularization was encouraged in the culprit-lesion-only strategy because 21.5% underwent staged or urgent repeated revascularization).6 At 1 year, no significant difference in all-cause mortality was observed.24 Although provocative, the issue with cardiogenic shock is that early mortality is high and the ability to perform complete revascularization is low (<50% in CULPRIT-SHOCK), which does not allow for proper evaluation of complete revascularization. As well, not all patients in the trial presented with STEMI (approximately 40% had non-STEMI). The studies included in our meta-analysis largely excluded cardiogenic shock.
Before the COMPLETE trial, guideline recommendations were limited to small-sample-size RCTs with lower power to detect differences in CV death or new MI. In addition, most trials included revascularization in the primary composite outcome, which is subject to criticism in an open-label trial. We now believe reasonable conclusions can be made with the results of our meta-analysis on hard clinical end points, including the potential for reduction in CV death alone. Moreover, these results appear consistent with FFR- and angiography-guided complete revascularization.
Limitations
Publication bias supporting multivessel PCI in STEMI is a potential limitation, although we included unpublished abstracts to minimize such bias. Furthermore, we performed an inverted funnel plot for CV death alone and CV death or new MI and found no publication bias (eFigures 2 and 3 in the Supplement). Individual patient data were not available for all included studies, precluding subgroup and other exploratory analyses. Admission and follow-up medications were not summarized. Follow-up left ventricular systolic function was not captured. We were not able to evaluate chronic total occlusions because most of the selected studies did not report this finding in STEMI. Limited randomized studies were available for FFR-guided multivessel PCI compared with angiographic-guided multivessel PCI, making it difficult to draw any firm conclusions on which of these approaches to complete revascularization is optimal. Finally, although we did find a significant reduction in CV mortality, the largest trial, COMPLETE, did not show a significant reduction in CV mortality alone but was not powered for this outcome (hence the reason for performing this meta-analysis). Still, we acknowledge the contribution of smaller RCTs with large CV mortality differences, which could conceivably influence our results.
Conclusions
Among patients with STEMI and multivessel disease, our meta-analysis involving 7030 patients found complete revascularization was associated with reduction in CV death compared with a culprit-lesion-only PCI in patients without cardiogenic shock at presentation. Moreover, consistency in the results was found for hard clinical outcomes when an FFR- or angiography-guided nonculprit-lesion PCI approach was used.
eTable. Search Strategy Used for MEDLINE
eFigure 1. PRISMA 2009 Flow Diagram
eFigure 2. Funnel Plot for CV Death
eFigure 3. Funnel Plot for CV Death or New Myocardial Infarction
eFigure 4. Forest Plot of Long-term All-Cause Mortality With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention
eFigure 5. Forest Plot of Long-term Recurrent Myocardial Infarction With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention
eFigure 6. Forest Plot of Long-term Recurrent Myocardial Infarction With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention Stratified by Multivessel Strategy
eFigure 7. Forest Plot of Long-term Cardiovascular Death or New Myocardial Infarction Stratified by Timing of Nonculprit Percutaneous Coronary Intervention
eFigure 8. Forest Plot of Long-term Cardiovascular Death Stratified by Timing of Nonculprit Percutaneous Coronary Intervention
eFigure 9. Forest Plot of Long-term Myocardial Infarction Stratified by Timing of Nonculprit Percutaneous Coronary Intervention
eFigure 10. Forest Plot of Cardiovascular Death in Patients With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention Including the CULPRIT SHOCK Trial
References
- 1.Ibanez B, James S, Agewall S, et al. ; ESC Scientific Document Group . 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 2.Levine GN, Bates ER, Blankenship JC, et al. 2015 ACC/AHA/SCAI focused update on primary percutaneous coronary intervention for patients with ST-elevation myocardial infarction: an update of the 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention and the 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation. 2016;133(11):1135-1147. doi: 10.1161/CIR.0000000000000336 [DOI] [PubMed] [Google Scholar]
- 3.Bainey KR, Welsh RC, Toklu B, Bangalore S. Complete vs culprit-only percutaneous coronary intervention in STEMI with multivessel disease: a meta-analysis and trial sequential analysis of randomized trials. Can J Cardiol. 2016;32(12):1542-1551. doi: 10.1016/j.cjca.2016.02.077 [DOI] [PubMed] [Google Scholar]
- 4.Mehta SR, Wood DA, Storey RF, et al. ; COMPLETE Trial Steering Committee and Investigators . Complete revascularization with multivessel PCI for myocardial infarction. N Engl J Med. 2019;381(15):1411-1421. doi: 10.1056/NEJMoa1907775 [DOI] [PubMed] [Google Scholar]
- 5.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2011. https://training.cochrane.org/handbook
- 6.Thiele H, Akin I, Sandri M, et al. ; CULPRIT-SHOCK Investigators . PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017;377(25):2419-2432. doi: 10.1056/NEJMoa1710261 [DOI] [PubMed] [Google Scholar]
- 7.Di Mario C, Mara S, Flavio A, et al. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised Hepacoat for Culprit or Multivessel Stenting for Acute Myocardial Infarction (HELP AMI) study. Int J Cardiovasc Intervent. 2004;6(3-4):128-133. doi: 10.1080/14628840310030441 [DOI] [PubMed] [Google Scholar]
- 8.Politi L, Sgura F, Rossi R, et al. A randomised trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010;96(9):662-667. doi: 10.1136/hrt.2009.177162 [DOI] [PubMed] [Google Scholar]
- 9.Ghani A, Dambrink JHE, van ’t Hof AWJ, Ottervanger JP, Gosselink ATM, Hoorntje JCA. Treatment of non-culprit lesions detected during primary PCI: long-term follow-up of a randomised clinical trial. Neth Heart J. 2012;20(9):347-353. doi: 10.1007/s12471-012-0281-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wald DS, Morris JK, Wald NJ, et al. ; PRAMI Investigators . Randomized trial of Preventive Angioplasty in Myocardial Infarction. N Engl J Med. 2013;369(12):1115-1123. doi: 10.1056/NEJMoa1305520 [DOI] [PubMed] [Google Scholar]
- 11.Hlinomaz O, Groch L, Polokova K, et al. ; PRAGUE 13 Investigators. Multivessel coronary disease diagnosed at the time of primary PCI for STEMI: complete revascularization versus conservative strategy. PRAGUE 13 trial. In: EuroPCR 2015. Accessed April 17, 2020. https://media.pcronline.com/diapos/EuroPCR2015/2173-20150519_1445_Main_Arena_Hlinomaz_Ota_1111_(6859)/Hlinomaz_Ota_20150519_1445_Main_Arena.pdf
- 12.Engstrøm T, Kelbæk H, Helqvist S, et al. ; DANAMI-3—PRIMULTI Investigators . Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015;386(9994):665-671. doi: 10.1016/S0140-6736(15)60648-1 [DOI] [PubMed] [Google Scholar]
- 13.Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. 2015;65(10):963-972. doi: 10.1016/j.jacc.2014.12.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamza M, Mahmoud N, Elgendy IY. A randomized trial of complete versus culprit-only revascularization during primary percutaneous coronary intervention in diabetic patients with acute ST elevation myocardial infarction and multi vessel disease. J Interv Cardiol. 2016;29(3):241-247. doi: 10.1111/joic.12293 [DOI] [PubMed] [Google Scholar]
- 15.Smits PC, Abdel-Wahab M, Neumann F-J, et al. ; COMPARE-ACUTE Investigators . Fractional flow reserve–guided multivessel angioplasty in myocardial infarction. N Engl J Med. 2017;376(13):1234-1244. doi: 10.1056/NEJMoa1701067 [DOI] [PubMed] [Google Scholar]
- 16.Pavasini R, Biscaglia S, Barbato E, et al. Complete revascularization reduces cardiovascular death in patients with ST-segment elevation myocardial infarction and multivessel disease: systematic review and meta-analysis of randomized clinical trials. Eur Heart J. 2019;(December):ehz896. doi: 10.1093/eurheartj/ehz896 [DOI] [PubMed] [Google Scholar]
- 17.Pinilla-Echeverri N, Mehta SR, Wang J, et al. Non-culprit lesion plaque morphology in patients with ST-segment elevation myocardial infarction: results from the COMPLETE Trial Optical Coherence Tomography (OCT) Substudy. Scientific Sessions. Posted November 19, 2019. Accessed April 17, 2020. https://www.crtonline.org/presentation-detail/non-culprit-lesion-plaque-morphology-in-patients-w [DOI] [PubMed] [Google Scholar]
- 18.De Bruyne B, Pijls NH, Bartunek J, et al. Fractional flow reserve in patients with prior myocardial infarction. Circulation. 2001;104(2):157-162. doi: 10.1161/01.CIR.104.2.157 [DOI] [PubMed] [Google Scholar]
- 19.Samady H, Lepper W, Powers ER, et al. Fractional flow reserve of infarct-related arteries identifies reversible defects on noninvasive myocardial perfusion imaging early after myocardial infarction. J Am Coll Cardiol. 2006;47(11):2187-2193. doi: 10.1016/j.jacc.2006.01.065 [DOI] [PubMed] [Google Scholar]
- 20.van der Hoeven NW, Janssens GN, de Waard GA, et al. Temporal changes in coronary hyperemic and resting hemodynamic indices in nonculprit vessels of patients with ST-segment elevation myocardial infarction. JAMA Cardiol. 2019;4(8):736-744. doi: 10.1001/jamacardio.2019.2138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Thim T, Götberg M, Fröbert O, et al. Nonculprit stenosis evaluation using instantaneous wave-free ratio in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2017;10(24):2528-2535. doi: 10.1016/j.jcin.2017.07.021 [DOI] [PubMed] [Google Scholar]
- 22.Zimmermann FM, Omerovic E, Fournier S, et al. Fractional flow reserve-guided percutaneous coronary intervention vs medical therapy for patients with stable coronary lesions: meta-analysis of individual patient data. Eur Heart J. 2019;40(2):180-186. doi: 10.1093/eurheartj/ehy812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wood DA, Cairns JA, Wang J, et al. Timing of staged non-culprit revascularization in ST-segment elevation myocardial infarction: insights from the COMPLETE trial. J Am Coll Cardiol. 2019;74(22):2713-2723. [DOI] [PubMed] [Google Scholar]
- 24.Thiele H, Akin I, Sandri M, et al. ; CULPRIT-SHOCK Investigators . One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018;379(18):1699-1710. doi: 10.1056/NEJMoa1808788 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. Search Strategy Used for MEDLINE
eFigure 1. PRISMA 2009 Flow Diagram
eFigure 2. Funnel Plot for CV Death
eFigure 3. Funnel Plot for CV Death or New Myocardial Infarction
eFigure 4. Forest Plot of Long-term All-Cause Mortality With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention
eFigure 5. Forest Plot of Long-term Recurrent Myocardial Infarction With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention
eFigure 6. Forest Plot of Long-term Recurrent Myocardial Infarction With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention Stratified by Multivessel Strategy
eFigure 7. Forest Plot of Long-term Cardiovascular Death or New Myocardial Infarction Stratified by Timing of Nonculprit Percutaneous Coronary Intervention
eFigure 8. Forest Plot of Long-term Cardiovascular Death Stratified by Timing of Nonculprit Percutaneous Coronary Intervention
eFigure 9. Forest Plot of Long-term Myocardial Infarction Stratified by Timing of Nonculprit Percutaneous Coronary Intervention
eFigure 10. Forest Plot of Cardiovascular Death in Patients With Multivessel or Culprit-Lesion-Only Percutaneous Coronary Intervention Including the CULPRIT SHOCK Trial


