Abstract
Purpose
To describe our experience of Gonioscopy-Assisted Transluminal Trabeculotomy (GATT) in four eyes with infantile primary congenital glaucoma (PCG).
Observations
We report the first two GATT procedures performed in six-month-old infants with PCG. We also report the same procedure in two eyes of a two-year-old boy with PCG who had previous goniotomies with subsequent peripheral anterior synechiae formation. In all four eyes, the IOP remained under 20 mmHg at years three and four postoperatively, without glaucoma medication or conjunctival surgery.
Conclusions and importance
Our cases confirm that GATT is an alternative to traditional ab externo glaucoma surgery in PCG and can be successfully performed within the first months of life, or in infants with failed or partially functioning goniotomies, avoiding the need for invasive conjunctival or scleral surgery.
Keywords: Congenital glaucoma, ab interno, Trabeculotomy, 360-Degree, GATT
1. Introduction
Treatment of infantile primary congenital glaucoma (PCG) is principally via a surgical approach.1 Both ab interno and ab externo trabecular incisional surgeries have been recommended as first-line treatments.1 The choice of ab interno versus ab externo depends on the surgeon's ability to visualize anatomical structures as well as their training and preference.1
Goniotomy was first described by Barkan2 in 1942 and remains a popular approach in treating PCG due to the ab interno advantages of avoiding conjunctival and scleral dissection,1 particularly as further glaucoma surgery may be required. Goniotomy incisions are thought to induce maturation of the underdeveloped trabecular meshwork (TM).3 However, subsequent goniotomies (nasal and temporal) are often required.4
Ab externo trabeculotomy was described in 1962 by R Smith5 using a nylon suture to treat 140° of the TM. Beck and Lynch modified this technique in 1995,6 using a prolene suture to treat 360 degrees of the TM. In parallel, surgeons also performed trabeculotomy using a rigid metal trabeculotome to treat the superior portion of the TM.1 The introduction of an illuminated microcatheter was described by Sarkisan7 and Girkin,8 and facilitates intraoperative tracking of the catheter tip, thereby avoiding inadvertent passage of the catheter into the suprachoroidal or subretinal spaces.9,10 All these ab externo approaches are particularly useful when corneal clarity is compromised.
Grover and colleagues recently described an ab interno approach to circumferential trabeculotomy in children, termed gonioscopy-assisted transluminal trabeculotomy (GATT).11 In their report, they included four eyes of three PCG children, who underwent surgery between 17 months and 16 years of age.
The authors set out to describe their experience using this ab interno approach in four PCG eyes of three children. Two infants underwent surgery at 6-months for unilateral PCG. To our knowledge, there are no previous published reports in this age group. We describe two additional eyes in a 2-year-old with prior multiple bilateral goniotomies and established peripheral anterior synechiae (PAS). All cases underwent GATT by a single surgeon (ES). Success was defined as IOP between 6 and 21 mmHg without glaucoma medications (complete success) or with medications (qualified success). Failure was defined as IOP above 21 mmHg on two consecutive visits after a post-operative period of 3 months or further glaucoma surgery.
2. Findings
2.1. Case 1
A 6-month-old boy was referred via his ophthalmologist, after his mother noticed an enlarged left eye (OS) and intermittent photophobia. Examination under anesthesia (EUA) using a Schiøtz tonometer, revealed an IOP of 29 mmHg (OS) on latanoprost, and 12 mmHg in the right eye (OD) without treatment. Corneal white-to-white diameters (WTWD) were 12.0 mm (OD), 13.5 mm (OS). Fundus examination revealed cup to disc ratio (CDR) of 0.1 (OD), 0.5 (OS). The axial length (AL) was 20.45 mm (OD), 22.42 mm (OS). For the surgical procedure, topical 2% pilocarpine was applied preoperatively. After 5% iodine disinfection, a temporal paracentesis was made and viscoelastic injected into the anterior chamber (AC). The iridocorneal angle was visualized nasally using a Swan Jacob gonioscope. The TM was barely visible and unlike older children, there was only a faint discoloration of the TM,3 seen on maximal magnification, approximately 1–2 mm above the iris insertion. There was an absence of blood reflux into the TM despite lowering the IOP intraoperatively (Fig. 1A). Using a crescent shaped goniotomy blade, a 1–2 mm horizontal incision was made where the TM was considered to be. The soft inner surface of the TM was then removed using a downward scraping motion, until the blade came to rest on a rigid structure, presumed to be the scleral spur, approximately 1 mm anterior to the iris base (Fig. 2). Using microsurgical forceps (25 Ga diamondized, end-gripping forceps, FCI Ophtalmics, Paris, France), the illuminated catheter (iTrack 250A; iScience Interventional, Menlo Park, CA) was introduced via a separate paracentesis and introduced into this goniotomy incision and advanced parallel to the iris plane to circumnavigate the canal. The transscleral illumination of the catheter tip enabled visualization of its position at all times. After approximately 100 degrees of circumferential travel, the illuminated iTrack catheter was seen to exit the canal in a posterior direction, presumably into the suprachoroidal space. The catheter was immediately retracted and reintroduced into the same goniotomy incision via another paracentesis, but in the reverse direction and advanced for 360 degrees. The catheter was externalized into the AC, thereby creating a 360-degree ab interno trabeculotomy. The iris base was seen to immediately fall posteriorly following the trabeculotomy, giving the surgeon an impression that a membranous connection between the TM and iris base had been incised (Fig. 1B). The viscoelastic in the AC was removed, using an irrigation-aspiration system and the corneal incisions were sutured. Postoperative medication included topical ofloxacin, diclofenac 0.1%, pilocarpine 2% and rimexolone 1% drops for 1 month.
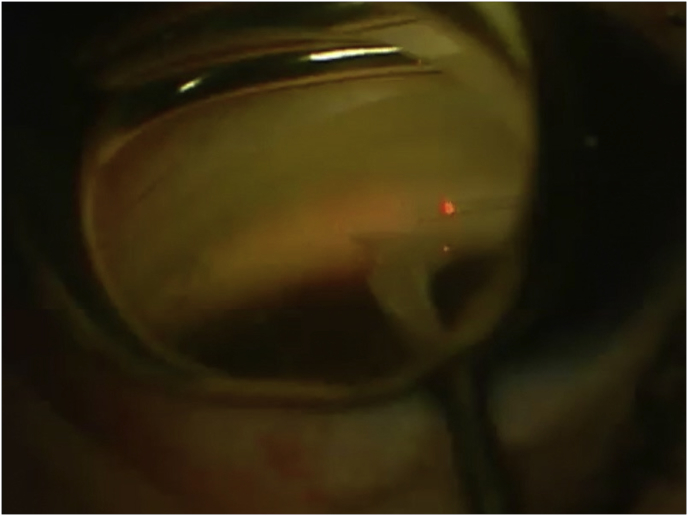
Fig. 1.
Intraoperative gonioscopy.
In case 2 (6 months-old), trabecular meshwork (TM) was barely visible (A) and the iris base was seen to immediately fall back posteriorly (B) opening the shelf (yellow arrow). In case 3 (2 years-old), the TM was moderately pigmented (C; black solid arrow), easily identifiable and demarcated from the scleral spur. There was a large nasal peripheral anterior synechia (black empty arrows). Two weeks post-operatively (D), we can observe the iris and the fibrous membrane (white arrows) pulling the posterior portion of the trabecular shelf in a centripetal fashion, opening the shelf to a great extent than seen in adults (yellow arrow). (For interpretation of the references to color in this figure legend, the reader is referred to the Web version of this article.)
Fig. 2.
Intraoperative gonioscopic view during surgery (case 2): A 1–2 mm horizontal incision was made where the trabecular meshwork was considered to be, using a downward scraping motion removing the soft inner surface of the TM, until the blade used came to rest on the scleral spur, approximately 1 mm anterior to the iris base. The illuminated catheter was introduced into this goniotomy incision and advanced parallel to the iris plane, within the canal, using microsurgical forceps.
Postoperatively, day 1: IOP was 24 mmHg OS with a 3mm hyphema, at week 1 and month 1: IOP was 9 mmHg on latanoprost, which was stopped after 1 month. IOP at 3, 12, 24 and 48 months remained between 11 and 13 mmHg without treatment. The disc examination revealed a CDR of 0.1 (OD) and 0.2 (OG) at 12, 24 and 48 months. All postoperative IOP measurements were performed in office with the Icare® tonometer (Icare TA01i, Finland Oy, Finland).
2.2. Case 2
A 5-month-old boy was referred by his pediatrician due to asymmetrical ocular size. EUA revealed IOP of 8 mmHg (OD) and 25 mmHg (OS). Corneal WTWD were 11.75 mm (OD), 13.5 mm (OS), without Haab striae. The AL was 19.75 mm (OD), 21.8 mm (OS). CDR was 0.2 (OD), 0.7 (OS). Treatment (OS) included pilocarpine 2%, timolol 0.5% and travoprost 0.004%. The patient underwent the same procedure and postoperative medication as described above with similar gonioscopy findings such as the lack of TM pigmentation and poorly demarcated angle structures. In this case, the iTrack catheter was also seen to exit the canal in a posterior direction after approximately 130 degrees. The catheter was retracted and reintroduced into the same goniotomy incision via another paracentesis in the reverse direction and advanced for 360 degrees.
Postoperatively, at week 1 and month 1, IOP was 15 mmHg OS on timolol 0.1%. At 3, 12, 24 and 48 months, IOP was 10–11 mmHg (OD) and 11–14 mmHg (OS) without medication (performed in the office with the Icare® tonometer). At 12, 24, and 48 months postoperatively, CDR was 0.1 (OD) and 0.3 (OG).
2.3. Case 3
A 2-year-old boy diagnosed with PCG at 3 months of age, initially presented with cloudy corneas, buphthalmia and elevated IOP. He had a history of multiple bilateral goniotomies, two nasal and one temporal, which were performed in each eye at 6 months of age, resulting in IOP below 21 mmHg using 3 glaucoma medications, for approximately 18 months. Subsequently, IOP in OS increased to 26 mmHg (measured in the office with the Icare® tonometer), and EUA revealed an increasing WTWD in OS vs OD: 13.75 (OS), 13.25 (OD), and AL 22.5mm (OS), 21.75mm (OD), despite using travoprost 0.004%, timolol 0.5% and brinzolamide 1% in both eyes. A decision was made to undergo circumferential ab interno trabeculotomy in OS. The surgical procedure was similar to the previous case. However, in this older child, the TM was moderately pigmented, easily identifiable and well demarcated from the scleral spur (Fig. 1C). There were large nasal and temporal PAS (due to the previous goniotomies). Interestingly, these did not obstruct the intraluminal passage of the catheter within the canal. Following the exteriorization of the catheter the iris was seen to drop posteriorly suggesting the presence of connective tissue between the iris base and posterior trabecular shelf. Two weeks later, during removal of the paracentesis sutures, gonioscopy revealed a white circular fibrous membrane at the iris base tethering the posterior trabecular shelf open (Fig. 1D). Postoperatively, there was a hyphema during the first week and IOP reduced gradually over 2–3 months allowing cessation of all glaucoma medication by 3 months. At 30 months, the IOP in OS remained between 15 and 17 mmHg without medication (performed in the office with the Icare® tonometer). In OD the IOP was 17 mmHg, on 3 medications. Therefore, the patient underwent the same procedure in OD achieving an IOP of 18 mmHg without medication.
3. Discussion
GATT performed within the first months of life presents the glaucoma surgeon with particular challenges. When faced with cloudy corneas due to elevated IOP, surgical removal of the corneal epithelium can improve visualization of the angle structures. However, despite a clearer view, TM identification remains challenging due to lack of pigmentation of the immature TM, a translucent uveal meshwork3 and in our experience, there is often an absence of blood reflux into the TM, after lowering the IOP intraoperatively, unlike in older children.12
In the two 6-month-old infants, a goniotomy blade and illuminated catheter were required to locate the TM, which was found 1–2 mm above the iris base. Difficulty finding Schlemm's canal, due to the altered infantile anatomy in buphthalmic eyes, is well recognized even using an ab externo approach. We therefore prefer to attempt ab interno insertion of the illuminated catheter before attempting an ab externo approach.
Alternatively, if surgeons prefer to avoid an ab externo approach, but the TM is too difficult to locate in a young infant, they may choose to initially perform a nasal goniotomy to lower IOP, and wait until the TM is more easily identifiable to perform a full 360-degree GATT as a second procedure (case 3).
Previous studies have shown greater success rates following ab externo 360-degree circumferential trabeculotomy compared to goniotomy,4,13 or metal trabeculotomy.14 Several authors have outlined the advantages of treating the entire 360 degrees of TM in one procedure thereby maximizing IOP reduction and minimizing the risks of multiple anesthesia.4,13, 14, 15 Mendicino et al.4 compared 360-degree trabeculotomy to goniotomy in a six-year study. They found better visual outcomes and IOP reduction in the 360-degree treatment group. Furthermore, unlike goniotomy, there was no increase in failure rates after the early postoperative period following circumferential trabeculotomy.4
The authors believe GATT is a valuable alternative to traditional pediatric ab externo glaucoma surgeries. Trabeculectomy and tube-shunts are associated with marked hypotony-related complications as well as long-term sight-threatening complications, including corneal decompensation and bleb-related endophthalmitis, which are particularly worrisome in this age group with long life expectancy.16
Given that GATT is a relatively new procedure, and all four eyes achieved complete success, we believe the 30–48 months follow up data is promising and therefore expect similar long-term results to ab externo 360-degree surgery.
4. Conclusions
Our cases confirm that gonioscopy-assisted transluminal trabeculotomy is a viable alternative to ab externo glaucoma surgery in PCG and can be successfully performed within the first few months of life. Furthermore, it may be performed in infants with failed or partially functioning goniotomies, avoiding the need for more invasive conjunctival and scleral surgery.
Patient consent
This report does not contain any personal information that could lead to the identification of the patient.
Declaration of competing interest
The following authors have no financial disclosures: LL, YS, AG, ES.
Acknowledgements
None.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ajoc.2020.100733.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Institutional review board
Approval obtained.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Tan Y.L., Chua J., Ho C.L. Updates on the surgical management of pediatric glaucoma. Asia Pac J Ophthalmol (Phila). 2016 Jan-Feb;5(1):85–92. doi: 10.1097/APO.0000000000000182. [DOI] [PubMed] [Google Scholar]
- 2.Barkan O. Surgery of congenital glaucoma; review of 196 eyes operated by goniotomy. Am J Ophthalmol. 1953 Nov;36(11):1523–1534. doi: 10.1016/0002-9394(53)91780-2. [DOI] [PubMed] [Google Scholar]
- 3.Yu Chan J.Y., Choy B.N., Ng A.L., Shum J.W. Review on the management of primary congenital glaucoma. J Curr Glaucoma Pract. 2015 Sep-Dec;9(3):92–99. doi: 10.5005/jp-journals-10008-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mendicino M.E., Lynch M.G., Drack A. Long-term surgical and visual outcomes in primary congenital glaucoma: 360 degrees trabeculotomy versus goniotomy. J Am Assoc Pediatr Ophthalmol Strabismus. 2000 Aug;4(4):205–210. doi: 10.1067/mpa.2000.106201. [DOI] [PubMed] [Google Scholar]
- 5.Smith R. Nylon filament trabeculotomy in glaucoma. Trans Ophthalmol Soc U K. 1962;82:439–454. [PubMed] [Google Scholar]
- 6.Beck A.D., Lynch M.G. 360 degrees trabeculotomy for primary congenital glaucoma. Arch Ophthalmol. 1995 Sep;113(9):1200–1202. doi: 10.1001/archopht.1995.01100090126034. [DOI] [PubMed] [Google Scholar]
- 7.Sarkisian S.R., Jr. An illuminated microcatheter for 360-degree trabeculotomy [corrected] in congenital glaucoma: a retrospective case series. J Am Assoc Pediatr Ophthalmol Strabismus. 2010 Oct;14(5):412–416. doi: 10.1016/j.jaapos.2010.07.010. Erratum in: J AAPOS. 2011 Feb;15(1):115. [DOI] [PubMed] [Google Scholar]
- 8.Girkin C.A., Marchase N., Cogen M.S. Circumferential trabeculotomy with an illuminated microcatheter in congenital glaucomas. J Glaucoma. 2012 Mar;21(3):160–163. doi: 10.1097/IJG.0b013e31822af350. [DOI] [PubMed] [Google Scholar]
- 9.Verner-Cole E.A., Ortiz S., Bell N.P., Feldman R.M. Subretinal suture misdirection during 360 degrees suture trabeculotomy. Am J Ophthalmol. 2006 Feb;141(2):391–392. doi: 10.1016/j.ajo.2005.08.038. [DOI] [PubMed] [Google Scholar]
- 10.Neely D.E. False passage: a complication of 360 degrees suture trabeculotomy. J Am Assoc Pediatr Ophthalmol Strabismus. 2005 Aug;9(4):396–397. doi: 10.1016/j.jaapos.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 11.Grover D.S., Smith O., Fellman R.L. Gonioscopy assisted transluminal trabeculotomy: an ab interno circumferential trabeculotomy for the treatment of primary congenital glaucoma and juvenile open angle glaucoma. Br J Ophthalmol. 2015 Aug;99(8):1092–1096. doi: 10.1136/bjophthalmol-2014-306269. [DOI] [PubMed] [Google Scholar]
- 12.Carreon T., van der Merwe E., Fellman R.L., Johnstone M., Bhattacharya S.K. Aqueous outflow - a continuum from trabecular meshwork to episcleral veins. Prog Retin Eye Res. 2017 Mar;57:108–133. doi: 10.1016/j.preteyeres.2016.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Girkin C.A., Rhodes L., McGwin G., Marchase N., Cogen M.S. Goniotomy versus circumferential trabeculotomy with an illuminated microcatheter in congenital glaucoma. J Am Assoc Pediatr Ophthalmol Strabismus. 2012 Oct;16(5):424–427. doi: 10.1016/j.jaapos.2012.05.013. [DOI] [PubMed] [Google Scholar]
- 14.Lim M.E., Neely D.E., Wang J., Haider K.M., Smith H.A., Plager D.A. Comparison of 360-degree versus traditional trabeculotomy in pediatric glaucoma. J Am Assoc Pediatr Ophthalmol Strabismus. 2015 Apr;19(2):145–149. doi: 10.1016/j.jaapos.2015.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Chin S., Nitta T., Shinmei Y. Reduction of intraocular pressure using a modified 360-degree suture trabeculotomy technique in primary and secondary open-angle glaucoma: a pilot study. J Glaucoma. 2012 Aug;21(6):401–407. doi: 10.1097/IJG.0b013e318218240c. [DOI] [PubMed] [Google Scholar]
- 16.Beck A.D., Freedman S., Kammer J., Jin J. Aqueous shunt devices compared with trabeculectomy with Mitomycin-C for children in the first two years of life. Am J Ophthalmol. 2003 Dec;136(6):994–1000. doi: 10.1016/s0002-9394(03)00714-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.