Abstract
Objectives
To estimate the effect of Medicaid expansion under the Affordable Care Act (ACA) on the frequency and payment source for Emergency Department (ED) visits for dental care.
Study Design
Retrospective, quasi‐experimental study.
Data Sources/Study Setting
We used the State Emergency Department Database to compare changes in ED visit rates and payment source for dental conditions among patients from 33 states. These states represent four distinct policy environments, based on whether they expanded Medicaid and whether their Medicaid programs provide dental benefits. We first assessed the number of ED dental visits before (2012) and after (2014) the ACA. Then, we used differences‐in‐differences regression to estimate changes in insurance for dental visits by nonelderly adults.
Principal Findings
Our sample contained 375 944 dental ED visits. In states that expanded Medicaid and offered dental coverage, dental ED visits decreased by 14.1 percent (from 19 443 to 16 709, for a net difference of 2734). By contrast, in the remaining three state groups, dental ED visits rose. Meanwhile, the expansion significantly increased Medicaid coverage and decreased the rate of self‐pay for ED dental visits.
Conclusions
Medicaid expansion, combined with adult dental coverage in Medicaid, was associated with a reduction in ED utilization for dental visits.
Keywords: dentistry/dental care, emergency service, health policy/politics/law/regulation, hospital, medicaid, observational data/quasi‐experiments
What this study adds.
What is already known on this topic
A significant number of ED dental visits are preventable and can be treated in outpatient dental clinics. However, reliance on the ED for receiving dental care continues to rise due to barriers including lack of health insurance and cost of treatment.
Medicaid expansion increased access to health care to low‐income adults but the effect of the ACA expansion on the frequency and payment source for ED dental visits remains unclear.
What this study adds
This study suggests that Medicaid expansion, combined with adult dental coverage in Medicaid, is associated with a reduction in ED utilization for dental visits.
1. INTRODUCTION
Emergency Department (ED) services are a significant contributor to health care costs in the United States.1, 2 ED visits for dental care alone cost the health system nearly $2 billion in 2015.3 Although a significant number of such dental visits are preventable and can be treated in outpatient dental clinics, reliance on the ED for receiving dental care continues to rise.4, 5 This trend is largely driven by barriers to obtaining routine dental care, including lack of health insurance and cost of treatment.6, 7 Therefore, the ED has become the safety net for dental care for a significant proportion of the population.
Nearly 50 million Americans lacked health insurance prior to the implementation of the Affordable Care Act (ACA).8 The ACA sought to expand coverage to low‐income adults, and since its implementation, evidence suggests that the legislation reduced the uninsured rate, improved several health outcomes, and achieved significant progress in reducing health inequalities.9, 10 Adult dental care, however, is not included as an essential health benefit under the ACA, and coverage varies widely by state. Dental benefits under Medicaid coverage range from emergency treatment only to full comprehensive care. As of 2016, four states did not cover any Medicaid dental services for adults, and 13 states offered only emergency dental services to Medicaid nonelderly adults. 11, 12
Previous studies examined the early impact of the Medicaid expansion and demonstrated increased access to and utilization of dental care, particularly in states that provide Medicaid adult dental benefits.13, 14 However, few studies have assessed the impact of health insurance on ED utilization for dental conditions.15, 16, 17, 18 In this study, we sought to estimate the effect of Medicaid expansion—with and without dental coverage—on the frequency and payment source for ED visits related to dental care. We hypothesized that Medicaid expansion combined with adult dental coverage would increase access to dental care for low‐income adults and therefore would reduce ED visits for dental problems in states that provide Medicaid adult dental benefits.
2. METHODS
2.1. Data source
We used data from the State Emergency Department Databases (SEDD) gathered by the Healthcare Cost and Utilization Project (HCUP) and sponsored by the Agency for Healthcare Research and Quality (AHRQ). SEDD includes information from 39 states on emergency room visits that did not result in hospital admission, with state‐year data available for purchase from AHRQ. The data provide information on patients’ demographics, diagnoses, procedures, total charges, and expected payment source for ED visit. SEDD data have been available since 1999 but the extent of available information varies by state and year.19
Our analyses utilize US state‐level variation in electing to expand Medicaid under the ACA, as well as variation in coverage of adult dental benefits under Medicaid. We defined a state as providing dental benefit if it offers either comprehensive or limited adult dental coverage under Medicaid, while states that provide no adult dental coverage or only emergency services were considered to lack dental benefits. 11, 12
We obtained hospital data from eight states (AZ, FL, IA, MD, NC, NJ, UT, and WI) and compared data both prior to (2012) and following (2014) the Medicaid expansion under ACA. These states were chosen because they represented distinct policy environments related to Medicaid expansion as well as adult dental coverage in Medicaid; the number of state‐years analyzed was limited by our study’s budget constraint. While our sample draws on hospitals in only eight states, this sample includes a substantial number of patient visits from patients residing in other states (typically nearby border areas). Since Medicaid eligibility and coverage (including dental benefits) are dictated by the state of residence, not where a person obtains emergency care, this allowed us to assess a patient population drawn from 33 states, representing four distinct policy environments: 1) states that expanded Medicaid and offer dental coverage for adults through Medicaid (AR, CT, DC, IA, KY, MA, MI, MN, NJ, NM, NY, OH, OR); 2) states that expanded Medicaid but do not offer dental coverage for adults (AZ, MD, NV, WV); 3) states that did not expand but offer dental coverage (IN, NE, NC, PA, WI); and 4) states that did not expand and do not provide dental coverage (AL, FL, GA, LA, MS, MO, OK, TN, TX, UT, VA). States with fewer than 1000 observations were excluded from the sample.
The SEDD does not record individuals’ income, but provides median household income (in quartiles) based on their zip code of residence. We restricted our primary analytic sample to nonelderly adults between the ages of 19 and 64 years whose zip codes are in the bottom income quartile in an attempt to narrow our sample to a population more likely to be affected by the ACA’s Medicaid eligibility expansion for families with incomes up to 138 percent of the federal poverty level (FPL).20
2.2. Variables
Our study outcomes were Emergency Department (ED) visits as well as payment source for the treatment of dental conditions. We used the following International Classification of Diseases (ICD‐9‐CM) diagnostic codes to define ED visits for dental‐related conditions21:520.0‐529.9, 792.4, 784.92, 802.2‐802.5, 873.6‐873.79, V52.3, V53.4, V58.5, V72.2, V45.84. In secondary analyses, we further distinguished between ED dental visits due to nontraumatic dental conditions (520.0‐525.10, 525.12‐529.9, V52.3, V53.4, V58.5, V72.2, V45.84, 792.4, 784.92) versus those due to traumatic dental conditions (525.11, 802.2‐802.5, 873.6‐873.79).
The categories of payment sources for ED visits were Medicare, Medicaid, private insurance, self‐pay, and other. Our analyses primarily focused on Medicaid and the self‐pay (ie, uninsured) population.
2.3. Data analysis
We conducted two broad analyses. First, we measured the overall frequency of dental ED visits before and after the Medicaid expansion, using the population of ED visits in these states. This analysis has only 66 observations—one for each state and year—but represents the full universe of visits at these hospitals and is not subject to sampling error. We therefore calculated the net change after expansion, for expansion vs control states, but do not present sample‐based statistical estimates. Then, to investigate changes in payment source before and after the expansion, we used differences‐in‐differences linear regression based on individual‐level data.
The causal estimate of interest is the interaction term β 3 between expansion (yes/no) and time period (before/after ACA).22 Two models were used to examine changes in payment source, one representing Medicaid coverage and the other self‐pay/uninsured. We first conducted the analysis for the full sample comparing expansion states to control states. We then repeated this model separately for those states with adult dental benefits vs states without adult dental benefits in Medicaid. We used robust standard errors clustered at state level and adjusted regression models for age, sex, race, rural/urban residence, state‐year unemployment rate, number of dentists per capita in each state, year, and state.
Our study design relies on the assumption that changes in ED visits and coverage would have been similar for expansion and nonexpansion states, if not for the ACA Medicaid expansion. We used monthly observations in year 2012 to test for pre‐existing trends between expansion and nonexpansion states before Medicaid expansion.
We additionally conducted a falsification test in which we examined data for patients aged 65 years and above who generally would qualify for Medicare to see whether there were any differential changes in dental ED utilization by state during this time period that should not have been impacted by the Medicaid expansion.
3. RESULTS
3.1. Sample characteristics
The sample included 9 603 203 ED visits in the 33 states during the two study years, of which 375 944 ED visits were due to dental‐related conditions. The demographic characteristics between Medicaid expansion and nonexpansion states were roughly similar in terms of gender and age, but Medicaid expansion states had higher proportion of Hispanic population (22 vs 12 percent), fewer black (37 vs 39 percent), and rural residents (5 vs 10 percent) compared to nonexpansion states (Table 1).
Table 1.
Characteristics of study sample at baselinea
| Variable | Medicaid expansion statesb | Nonexpansion statesc |
|---|---|---|
| Total ED visits, No. | 1 215 120 | 3 199 891 |
| ED visits for dental conditions (%) | 3.92 | 4.00 |
| Gender (%) | ||
| Male | 42.69 | 39.94 |
| Female | 57.31 | 60.06 |
| Age (%) | ||
| 19‐34 | 46.03 | 46.78 |
| 35‐44 | 20.24 | 20.40 |
| 45‐54 | 20.63 | 19.72 |
| 55‐64 | 13.10 | 13.09 |
| Race (%) | ||
| White | 35.77 | 46.14 |
| Black | 36.93 | 39.23 |
| Hispanic | 22.34 | 11.58 |
| Asiand | 0.68 | 0.40 |
| Othere | 4.28 | 2.66 |
| Rural (%) | ||
| Urban | 95.45 | 90.10 |
| Rural | 4.55 | 9.90 |
| Primary payer (%) | ||
| Medicare | 9.69 | 10.19 |
| Medicaid | 34.32 | 29.00 |
| Private insurance | 22.50 | 21.44 |
| Self‐pay/uninsured | 29.58 | 33.49 |
| Otherf | 3.91 | 5.89 |
Sample limited to adults aged 19‐64 yrs with income within the first income quartile calculated for median household income for patient’s ZIP code.
Abbreviation: ED, Emergency Department.
Baseline refers to the sample prior to Medicaid expansion, year 2012.
Medicaid expansion states: AR, AZ, CT, DC, IA, KY, MD, MA, MI, MN, NV, NJ, NM, NY, OH, OR, WV.
Nonexpansion states: AL, FL, GA, IN, LA, MS, MO, NE, NC, OK, PA, TN, TX, UT, VA, WI.
Includes Asian/Pacific Islander.
Includes Native American and other.
Includes Worker’s Compensation, CHAMPUS, CHAMPVA, Title V, other government programs, and no charge.
3.2. Frequency of ED dental visits
There was an overall increase in ED dental visits from 175 746 to 200 198 and a net difference of 24 452 (+13.9 percent) between 2012 and 2014 across the sample as a whole (Table 2 and Figure S1). Nonexpansion states (with and without adult dental benefits in Medicaid) and expansion states without adult dental benefits all experienced increases in ED dental visits, with changes ranging from + 8.6 percent (from 60 798 to 66 036, for a net difference of 5238) to + 27.8 percent (from 67 296 to 86 026 for a net difference of 18 730). In contrast, states that expanded Medicaid and offer adult dental benefits experienced a decrease in ED dental visits from 19 443 to 16 709 and a net difference of 2734 (−14.1 percent). We observed a similar trend when restricting the sample to Medicaid and self‐pay/uninsured population. Table 2 and Figure 1 present unadjusted changes in ED visit counts for those with Medicaid or self‐pay/uninsured. We found a reduction from 14 211 to 11 655 and a net difference of 2556 (−18.0 percent) in dental ED visits in states that expanded Medicaid and provide adult dental benefits, compared to increases ranging from + 7.3 percent (from 47 886 to 51 398, for a net difference of 3512) to + 25.4 percent (from 52 037 to 65 251, for a net difference of 13 214) in the remaining three state groups.
Table 2.
Changes in emergency department visits for dental conditions in 2012‐2014
| Before ACA | After ACA | Net change after ACA expansion (%) | ||
|---|---|---|---|---|
| All Payers | ||||
| Full sample | 175 746 | 200 198 | 24 452 | (+13.9%) |
| States with dental benefits | ||||
| Expansion states | 19 443 | 16 709 | −2734 | (−14.1%) |
| Nonexpansion states | 60 798 | 66 036 | 5238 | (+8.6%) |
| States without dental benefits | ||||
| Expansion states | 28 209 | 31 427 | 3218 | (+11.4%) |
| Nonexpansion states | 67 296 | 86 026 | 18 730 | (+27.8%) |
| Self‐pay/uninsured and Medicaid | ||||
| Full sample | 136 842 | 153 859 | 17 017 | (+12.4%) |
| States with dental benefits | ||||
| Expansion states | 14 211 | 11 655 | −2556 | (−18.0%) |
| Nonexpansion states | 47 886 | 51 398 | 3512 | (+7.3%) |
| States without dental benefits | ||||
| Expansion states | 22 708 | 25 555 | 2847 | (+12.5%) |
| Nonexpansion states | 52 037 | 65 251 | 13 214 | (+25.4%) |
Sample limited to adults aged 19‐64 yrs with income within the first income quartile calculated for median household income for patient’s ZIP code. Before ACA = year 2012, after ACA = year 2014. Medicaid expansion states: AR, AZ, CT, DC, IA, KY, MD, MA, MI, MN, NV, NJ, NM, NY, OH, OR, WV. Nonexpansion states: AL, FL, GA, IN, LA, MS, MO, NE, NC, OK, PA, TN, TX, UT, VA, WI. States that provide adult Medicaid dental benefits: AR, CT, DC, IN, IA, KY, MA, MI, MN, NE, NJ, NM, NY, NC, OH, OR, PA, WI. States without adult Medicaid dental benefits: AL, AZ, FL, GA, LA, MD, MS, MO, NV, OK, TN, TX, UT, VA, WV.
Abbreviation: ACA, Affordable Care Act.
Figure 1.
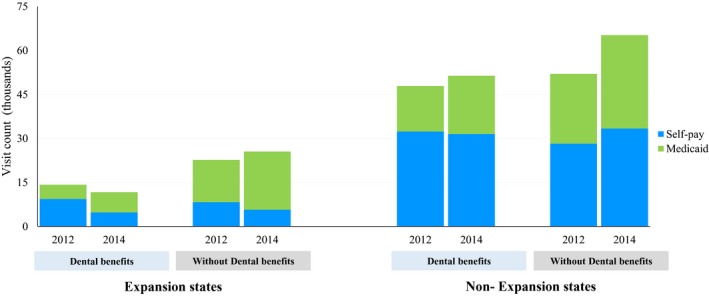
Changes in emergency department dental visits counts by health insurance status [Color figure can be viewed at wileyonlinelibrary.com]
Note. Study sample limited to adults aged 19‐64 yrs with income within the first income quartile calculated for median household income for patient’s ZIP code. Medicaid expansion states: AR, AZ, CT, DC, IA, KY, MD, MA, MI, MN, NV, NJ, NM, NY, OH, OR, WV. Nonexpansion states: AL, FL, GA, IN, LA, MS, MO, NE, NC, OK, PA, TN, TX, UT, VA, WI. States that provide adult Medicaid dental benefits: AR, CT, DC, IN, IA, KY, MA, MI, MN, NE, NJ, NM, NY, NC, OH, OR, PA, WI. States without adult Medicaid dental benefits: AL, AZ, FL, GA, LA, MD, MS, MO, NV, OK, TN, TX, UT, VA, WV
3.3. Payment source for ED dental visits
Table 3 presents differences‐in‐differences estimates for changes in Medicaid coverage and self‐pay/uninsured for ED dental use using individual‐level data. Medicaid expansion was associated with a significant 21.06 percentage‐point increase (95% CI 13.45, 28.67, P < .01) in Medicaid coverage. Meanwhile, the expansion was associated with a significant reduction in the rate of self‐pay/uninsured (−20.21 percentage points; 95% CI, −27.36, −13.07, P < .01). This reduction was larger in magnitude in states that provide adult dental benefits (−21.23 percentage points; 95% CI, −31.22, −11.24, P < .01) compared to states without adult dental benefits (−14.10 percentage points; 95% CI, −16.97, −11.23, P < .01).
Table 3.
Changes in insurance coverage for emergency department dental visits
| Unadjusted proportion % (95% CI) | Differences‐in‐differences | |||||
|---|---|---|---|---|---|---|
| Medicaid expansion states | Nonexpansion states | Net change after expansion % (95% CI) | ||||
| Before ACA | After ACA | Before ACA | After ACA | Unadjusted estimate | Adjusted estimatea | |
| Medicaid coverage | ||||||
| Full sample | 40.58 (40.14, 41.02) | 55.56 (55.12, 56.01) | 30.83 (30.58, 31.09) | 34.07 (33.83, 34.31) | 11.75 (7.01, 16.49)** | 21.06 (13.45, 28.67)** |
| States with dental benefits | 25.08 (24.47, 25.70) | 41.30 (40.56, 42.05) | 25.70 (25.35, 26.05) | 30.14 (29.80, 30.50) | 11.77 (1.90, 21.64)* | 18.19 (7.54, 28.84)** |
| States without dental benefits | 51.16 (50.58, 51.74) | 63.14 (62.61, 63.67) | 35.46 (35.09, 35.82) | 37.09 (36.76, 37.41) | 10.35 (8.81, 12.00)** | 17.20 (13.58, 20.82)** |
| Self‐pay/uninsured | ||||||
| Full sample | 37.20 (36.76, 37.63) | 21.76 (21.39, 22.13) | 47.61 (47.33, 47.88) | 42.76 (42.51, 43.01) | −10.59 (−17.86, −3.32)** | −20.21 − (−27.36, −13.07)** |
| States with dental benefits | 48.68 (47.98, 49.39) | 28.48 (27.80, 29.17) | 53.66 (53.27, 54.06) | 47.82 (47.44, 48.20) | −14.36 (−25.67, −3.04)* | −21.23 (−31.22, −11.24)** |
| States without dental benefits | 29.35 (28.82, 29.88) | 18.18 (17.76, 18.61) | 42.16 (41.78, 42.53) | 38.88 (38.55, 39.20) | −7.89 (−11.23, −4.54)** | −14.10 (−16.97, −11.23)** |
Sample limited to adults aged 19‐64 yrs with income within the first income quartile calculated for median household income for patient’s ZIP code.Medicaid expansion states: AR, AZ, CT, DC, IA, KY, MD, MA, MI, MN, NV, NJ, NM, NY, OH, OR, WV. Nonexpansion states: AL, FL, GA, IN, LA, MS, MO, NE, NC, OK, PA, TN, TX, UT, VA, WI. States that provide adult Medicaid dental benefits: AR, CT, DC, IN, IA, KY, MA, MI, MN, NE, NJ, NM, NY, NC, OH, OR, PA, WI. States without adult Medicaid dental benefits: AL, AZ, FL, GA, LA, MD, MS, MO, NV, OK, TN, TX, UT, VA, WV.
Abbreviations: ACA, Affordable Care Act; CI, confidence interval.
Model adjusted for age, sex, race, rural residence, state‐year unemployment rate, and number of dentists per capita in each state.
Significant (P < .05); **(P < .01).
3.4. Sensitivity analysis
The total number of ED visits for traumatic dental conditions (29 579 visits) was much lower than for nontraumatic conditions (359 411 visits). Findings from the subgroup analyses by type of visit were largely similar to our main analysis (Table S1). Medicaid expansion was associated with increased ED utilization for both traumatic and nontraumatic conditions, except in states that expanded Medicaid and offer dental benefits. In the latter states, ED dental visits fell from 18 229 to 15 694 with a net difference of 2535 (−13.9 percent) for nontraumatic conditions and fell from 1885 to 1446 with a net difference of 439 (−23.3 percent) for traumatic conditions. In addition, the expansion significantly increased Medicaid coverage for nontraumatic conditions (21.30 percentage points; 95% CI, 13.60, 29.00, P < .01) and traumatic conditions (19.01 percentage points; 95% CI, 12.19, 25.84, P < .01), while significantly decreasing the self‐pay/uninsured rates for ED use for both subgroups (nontraumatic conditions: −20.36 percentage points; 95% CI, −27.50, −13.22, P < .01 and traumatic conditions: −19.92 percentage points; 95% CI, −27.00, −12.83, P < .01) (Table S2).
Visual inspection of unadjusted monthly trends for study outcomes does not show any obvious divergence in parallel trends for ED visit rates or coverage type (Figure S2). We also conducted a placebo differences‐in‐differences test using the pre‐reform period to formally test these trends. We used the second half of 2012 as a placebo treatment period to test for changes in Medicaid coverage and self‐pay/uninsured for ED dental use, compared to the first half of 2012. The placebo expansion demonstrated a small and nonsignificant changes in Medicaid coverage (−0.89 percentage points; 95% CI, −1.87, 0.09) and self‐pay/uninsured rate (0.40 percentage points; 95% CI, −1.12, 1.91) in the 2nd half of 2012. These results offer support for our study design.
In our falsification sample of adults aged 65 years and older, we found an increase in ED utilization in three state groups, with a modest decrease in states that expanded Medicaid and provide adult dental benefits from 733 to 685 and a net difference of 48 (−6.5 percent) (Figure S3 and Tables S3 and S4). This decline represents roughly one‐third of the ED visit reduction (−18.0 percent) we detected in these states among nonelderly adults with Medicaid or self‐pay. As for changes in payment source, the ACA expansion was associated with no significant changes in Medicaid coverage (0.00 percentage points; 95% CI, −1.17, 1.18) or self‐pay/uninsured (−0.06 percentage points; 95% CI, −1.30, 1.19) for ED dental use among elderly adults (Table S5).
4. DISCUSSION
In this study, we took advantage of a natural policy experiment to examine the effect of Medicaid expansion coverage on ED utilization for dental conditions. Our findings suggest that Medicaid expansion led to an overall increase in ED utilization for dental care in states that expanded but without dental coverage, while dental ED visits declined in states that expanded Medicaid and provide adult dental benefits. We also found that the expansion increased Medicaid coverage for ED dental visits and reduced self‐pay/uninsured status, as expected. Taken together, our findings indicate that there is a potential for important synergy between expanded insurance coverage and dental benefits in reducing ED visits for dental care.
Our study is consistent with findings from previous research indicating that ED utilization in general—and not just related to dental care—has generally been increasing.5, 23, 24 However, the evidence regarding the impact of insurance coverage on overall ED utilization is mixed.25 For example, a recent review 25 on the topic referenced the 2006 Massachusetts health reform that resulted in decreased reliance on ED for young adults after insurance expansion.26 On the other hand, the Oregon Health Insurance Experiment (a randomized study of Medicaid) detected a significant increase in ED use.27 Among factors that could explain this heterogeneity are geographic and demographic differences across states, as well as variations in the characteristics of patients’ population who are utilizing the ED for their medical care.25 Our findings are also consistent with numerous prior studies showing major coverage gains after the ACA expansion.9, 15
But these prior studies focus on all ED visits, while here we focus on dental ED visits. Prior research in this narrower area has been primarily based on the experience of single states and often simple pre‐post designs without a comparison group. For example, in Kentucky, which provides adult dental coverage, Medicaid expansion was associated with an increased use of ED for dental care.15 Meanwhile, in California and Massachusetts, eliminating Medicaid adult dental benefits was associated with a substantial increase in ED visits for dental conditions.16, 17 Similarly in Oregon, the Medicaid expansion lottery experiment doubled ED dental visits.18 Our study builds on previous findings that examined ED dental use and makes a contribution to the literature by using a quasi‐experimental design and examining both Medicaid expansion and state‐level variations in the extent of dental care covered by Medicaid. Our findings demonstrate that Medicaid expansion has increased ED dental use except in expansion states that also provide dental coverage.
Our study provides insights on utilization patterns for dental care. The Medicaid expansion appears to have increased the ability of patients to get dental care, but in states not covering dental services in Medicaid much of this care may occur in the ED. However, the cost of ED visits for dental treatment is high and given that most patients will only receive palliative care for nonurgent conditions,28, 29 efforts should be directed to reduce preventable ED dental visits and steer those cases to outpatient dental clinics. A previous study showed that dental care use increased in states that expanded Medicaid and provide dental benefits.13 Therefore, the decrease in ED dental use in states that provide adult dental benefits raises the possibility that low‐income adults are more likely to be receiving dental care in outpatient settings. However, further research needs to assess changes in utilization at outpatient clinics after the ACA expansion to complement our analysis and to evaluate to what extent increased dental coverage offsets costs of dental ED visits.
4.1. Limitations
We analyzed data from the first year after the implementation of the ACA; however, coverage gains continued to increase in the following years and more states adopted the law. Thus, our results capture the early effect of Medicaid expansion and may have underestimated the effect of the expansion on ED dental use. Future studies are needed to assess the national and long‐term effects of the full implementation of the ACA on ED utilization for receiving dental care.
In addition, difference‐in‐differences analysis relies on the assumption that the control and treatment groups are exchangeable but for the intervention. Our study did not include pre‐expansion data from before 2012, and therefore, we were not able to test the assumption that pre‐expansion trends in ED visits were, in fact, parallel. Instead, we used monthly observations in year 2012 to test for differences in trend between expansion and control states, and our findings show no significant differential changes prior to 2014 by Medicaid expansion status. Our falsification test among the elderly provides additional evidence along these lines. We found a 18 percent drop in ED dental visits for the Medicaid and self‐pay among adults aged 19‐64 years old in expansion states that offer adult dental benefits, compared to a 6.5 percent decrease in ED visits for elderly adults (across all payers) in those states. Thus, our falsification testing using elderly adults suggests that a portion of the decline we are observing may be due to factors other than the Medicaid expansion that also affected elderly adults, though this appears to account for less than half of our overall estimate.
There are wide variations in the way ED dental visits are defined in previous research. In this study, we included ED visits due to any dental‐related condition. The SEDD dataset does not include any ED visits that lead to hospitalizations, and therefore, analyses of ED traumatic dental visits may be subject to bias. Nevertheless, we presented findings from this subgroup analysis to allow comparisons with previous research that focused primarily on nontraumatic conditions.
Finally, we lacked information about individuals’ income, instead relying on the zip codes of individual residence as a proxy for Medicaid eligibility, which means our results are likely biased toward the null due to measurement error.
5. CONCLUSIONS
While the ACA’s Medicaid expansion led to increased coverage gains among patients visiting the ED for dental conditions, our study suggests that the combination of Medicaid expansion and dental coverage for adults may reduce the need for emergency dental care, potentially through improved access to outpatient dental services.
CONFLICTS OF INTEREST
The authors declare no competing interest.
AUTHOR CONTRIBUTIONS
HW Elani, BD Sommers, and I. Kawachi contributed to the conception and design of the study, data interpretation, revised, and approved the final version of the article. HW Elani conducted the analysis and drafted the manuscript. BD Sommers oversaw the analysis.
HUMAN PARTICIPANT PROTECTION
This study used deidentified data and was determined to be “not‐human subjects research” by the institutional review board of the Harvard Faculty of Medicine.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: HW Elani is supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number K99MD012253. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Purchase of SEDD data was supported by Harvard School of Dental Medicine.
The interpretations, conclusions, and/or opinions presented as a result of this analyses of the SEDD data sets are solely the interpretations, conclusions, and/or opinions of the authors, and do not constitute the findings, policies, or recommendations of the US Government, the US Department of Health and Human Services, or AHRQ.
The authors would like to thank Dr Nalton Ferraro and the Harvard School of Dental Medicine Initiative to Integrate Oral Health and Medicine for their support of this research.
Elani HW, Kawachi I, Sommers BD. Changes in emergency department dental visits after Medicaid expansion. Health Serv Res. 2020;55:367–374. 10.1111/1475-6773.13261
REFERENCES
- 1. Dieleman JL, Squires E, Bui AL, et al. Factors associated with increases in US health care spending, 1996–2013. JAMA. 2017;318(17):1668‐1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bamezai A, Melnick G, Nawathe A. The cost of an emergency department visit and its relationship to emergency department volume. Ann Emerg Med. 2005;45(5):483‐490. [DOI] [PubMed] [Google Scholar]
- 3. ADA . Emergency Department Visits for Dental Conditions – A Snapshot. ADA American Dental Association. Health Policy Institute Infographics, 2018;https://www.ada.org/~/media/ADA/Science%20and%20Research/HPI/Files/HPIgraphic_0218_2.pdf?la=en. Accessed May 08, 2019.
- 4. Wall T, Vujicic M. Emergency Department Use for Dental Conditions Continues to Increase. ADA American Dental Association. Health Policy Institute Research Brief, 2015; http://www.ada.org/~/media/ADA/Science%2520and%2520Research/HPI/Files/HPIBrief_0415_2.ashx. Accessed July 18, 2017. [Google Scholar]
- 5. Seu K, Hall K, Moy E. Emergency department visits for dental‐related conditions, 2012; https://www.hcup-us.ahrq.gov/reports/statbriefs/sb143.pdf. Accessed February 19, 2019. [PubMed] [Google Scholar]
- 6. Vujicic M, Buchmueller T, Klein R. Dental care presents the highest level of financial barriers, compared to other types of health care services. Health Aff (Millwood). 2016;35(12):2176‐2182. [DOI] [PubMed] [Google Scholar]
- 7. GAO . MEDICAID: States Made Multiple Program Changes, and Beneficiaries Generally Reported Access Comparable to Private Insurance. In: Office USGA , ed. Washington, DC: GAO; 2012. [Google Scholar]
- 8. KFF . Key Facts about the Uninsured Population, 2018; https://www.kff.org/uninsured/fact-sheet/key-facts-about-the-uninsured-population/. Accessed February 19, 2019. [Google Scholar]
- 9. Sommers BD, Gunja MZ, Finegold K, Musco T. Changes in self‐reported insurance coverage, access to care, and health under the affordable care act. JAMA. 2015;314(4):366‐374. [DOI] [PubMed] [Google Scholar]
- 10. Sommers BD, Baicker K, Epstein AM. Mortality and access to care among adults after state Medicaid expansions. N Engl J Med. 2012;367(11):1025‐1034. [DOI] [PubMed] [Google Scholar]
- 11. Hinton E, Paradise J. Access to Dental Care in Medicaid: Spotlight on Nonelderly Adults. 2016; Mar 17, 2016; http://kff.org/medicaid/issue-brief/access-to-dental-care-in-medicaid-spotlight-on-nonelderly-adults/. Accessed April 27, 2016. [Google Scholar]
- 12. Medicaid .gov. Medicaid State Plan Amendments. https://www.medicaid.gov/state-resource-center/medicaid-state-plan-amendments/index.html. Accessed March 13, 2019. [Google Scholar]
- 13. Nasseh K, Vujicic M. Early Impact of the affordable care act’s medicaid expansion on dental care use. Health Serv Res. 2017;52:2256–2268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Singhal A, Damiano P, Sabik L. Medicaid adult dental benefits increase use of dental care, but impact of expansion on dental services use was mixed. Health Aff (Millwood). 2017;36(4):723‐732. [DOI] [PubMed] [Google Scholar]
- 15. Chalmers N, Grover J, Compton R. After medicaid expansion in kentucky, use of hospital emergency departments for dental conditions increased. Health Aff (Millwood). 2016;35(12):2268‐2276. [DOI] [PubMed] [Google Scholar]
- 16. Singhal A, Caplan DJ, Jones MP, et al. Eliminating Medicaid adult dental coverage in California led to increased dental emergency visits and associated costs. Health Aff (Millwood). 2015;34(5):749‐756. [DOI] [PubMed] [Google Scholar]
- 17. Neely M, Jones JA, Rich S, Gutierrez LS, Mehra P. Effects of cuts in Medicaid on dental‐related visits and costs at a safety‐net hospital. Am J Public Health. 2014;104(6):e13‐e16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baicker K, Allen HL, Wright BJ, Taubman SL, Finkelstein AN. The effect of medicaid on dental care of poor adults: evidence from the oregon health insurance experiment. Health Serv Res. 2018;53(4):2147‐2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. HCUP State Emergency Department Databases (SEDD) . Healthcare Cost and Utilization Project (HCUP). Rockville, MD: Agency for Healthcare Research and Quality; 2012, 2014. [Google Scholar]
- 20. KFF . Summary of the Affordable Care Act, 2017; http://files.kff.org/attachment/Summary-of-the-Affordable-Care-Act. Accessed February 19, 2019. [Google Scholar]
- 21. CDC . Centers for Disease Control and Prevention. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD‐9‐CM). https://www.cdc.gov/nchs/icd/icd9cm.htm. Accessed October 17, 2018. [Google Scholar]
- 22. Karaca‐Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health Serv Res. 2012;47(1 Pt 1):255‐274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Okunseri C, Okunseri E, Thorpe JM, Xiang Q, Szabo A. Patient characteristics and trends in nontraumatic dental condition visits to emergency departments in the United States. Clin Cosmet Investig Dentist. 2012;4:1‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. KFF . Hospital emergency room visits per 1,000 population by Ownership Type. https://www.kff.org/other/state-indicator/emergency-room-visits-by-ownership/?activeTab=graph%26currentTimeframe=0%26startTimeframe=17%26selectedDistributions=total%26selectedRows=%257B%2522wrapups%2522:%257B%2522united-states%2522:%257B%257D%257D%257D%26sortModel=%257B%2522colId%2522:%2522Location%2522,%2522sort%2522:%2522asc%2522%257D. Accessed February 19, 2019. [Google Scholar]
- 25. Sommers BD, Simon K. Health insurance and emergency department use ‐ a complex relationship. N Engl J Med. 2017;376(18):1708‐1711. [DOI] [PubMed] [Google Scholar]
- 26. Miller S. The effect of insurance on emergency room visits: an analysis of the 2006 Massachusetts health reform. J Public Econ. 2012;96:893‐908. [Google Scholar]
- 27. Finkelstein AN, Taubman SL, Allen HL, Wright BJ, Baicker K. Effect of Medicaid coverage on ED Use — further evidence from Oregon’s experiment. N Engl J Med. 2016;375(16):1505–1507. [DOI] [PubMed] [Google Scholar]
- 28. Davis EE, Deinard AS, Maiga EW. Doctor, my tooth hurts: the costs of incomplete dental care in the emergency room. J Public Health Dent. 2010;70(3):205‐210. [DOI] [PubMed] [Google Scholar]
- 29. Darling BG, Singhal A, Kanellis MJ. Emergency department visits and revisits for nontraumatic dental conditions in Iowa. J Public Health Dent. 2016;76(2):122‐128. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


