Abstract
Objectives
To determine the effectiveness of culturally tailored education on attendance at breast and cervical cancer screening among ethnic minority women.
Data Sources
Systematic database searches in Ovid MEDLINE, ProQuest, PubMed, PsycINFO, and Cochrane CENTRAL.
Study Design
Randomized controlled trials (RCTs) of culturally tailored educational interventions to ethnic minority women in Western countries were investigated for a meta‐analysis. RCTs that assessed attendance at mammography or the Papanicolaou test (Pap test) were eligible for inclusion.
Data Collection Methods
Study characteristics and results were extracted separately. Independent raters assessed risk of bias by using Cochrane Collaboration's tool.
Principal Findings
Seven RCTs (n = 4246) were included in the meta‐analysis of mammography attendance, and four RCTs (n = 1750) were included in the meta‐analysis of Pap test attendance. The effect of culturally tailored educational interventions on attendance at mammography was an increase of 18 percent (RR = 1.18, 95% CI, 1.09‐1.28, P < .001), with low heterogeneity (I 2 = 30.0, P = .237), and a 54 percent increase at the Pap test (RR = 1.54, 95% CI, 1.14‐2.09, P = .005), with substantial heterogeneity (I 2 = 75.9%, P = .001).
Conclusions
Interpreted within the limitations set by the low number of studies and substantial heterogeneity for the Pap test, findings from the current meta‐analyses indicate that culturally tailored educational interventions may increase attendance of ethnic minority women at breast and cervical cancer screenings. There is a need for more studies, in particular RCTs conducted outside the United States, to determine if such findings are similar in other countries.
Keywords: ethnic groups, health education, mammography, meta‐analysis, Papanicolaou test
What this study adds.
What is already known on this topic
Attendance of ethnic minority women for mammography and the Papanicolaou (Pap) test is low in the United States, Europe, Canada, and Australia.
Culturally tailored educational interventions can use linguistically appropriate methods to increase knowledge about cancer and screening and can address common cultural and religious barriers to screening.
What this study adds
Culturally tailored education increased attendance at mammography by 18 percent among ethnic minority women.
For Pap test attendance, an increase of 54 percent was found, but the substantial heterogeneity calls for careful judgment when interpreting the results.
1. INTRODUCTION
Breast and cervical cancer screening tools can detect cancer at early stages, when treatment is more effective and likely to succeed.1 Public cancer screening programs using mammography and the Papanicolaou (Pap) test have successfully decreased breast and cervical cancer mortality in Western countries over the past decades.1 However, ethnic minority women have low participation rates in breast and cervical cancer screening in the United States, Europe, Canada, and Australia.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Cancer causes extreme suffering for each woman and her family. In addition, the economic impact of cancer is significant and increasing, with a total annual economic cost of US$1.16 trillion in 2010,14 and the treatment of breast and cervical cancer is more expensive than the cost of prevention and early detection.15 Considerable efforts have been invested in reducing breast and cervical cancer incidents and mortality by increasing screening rates. However, disparities in screening rates continue to exist among certain racial and ethnic minority groups.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13
Previous studies have identified several culturally specific barriers to breast and cervical cancer screening among ethnic minority women living in Western countries.16, 17, 18, 19, 20, 21, 22, 23, 24, 25 Low linguistic proficiency, insufficient knowledge about cancer and screening programs, and low health literacy are found to be barriers. The same goes for cultural and religious barriers, such as false religious beliefs (fatalism), confidence in local and conventional curers, women's roles, and sexual issues.16, 17, 18, 19, 20, 21, 22, 23, 24, 25 Educational interventions aim to influence individuals' physical, intellectual, and moral development through training and education.26 The educational interventions for ethnic minority women must be culture‐specific, because women's behaviors and understandings of disease and symptoms are products of their social and cultural contexts, cultural beliefs, life experiences, and socioeconomic factors.27 Women in similar cultural groups generally share common knowledge, beliefs, and attitudes that fundamentally affect their behaviors.27
In the last decades, randomized controlled trials (RCTs) have investigated whether interventions can increase screening participation rates among ethnic minority women. Previous systematic reviews and meta‐analyses have explored the effects of different types of interventions to promote breast and cervical cancer screening among minority women.28, 29, 30, 31, 32, 33 Two meta‐analyses had several methodological and clinical limitations.28, 29 One such limitation is that the meta‐analyses included primary studies with samples of up to 60 percent Caucasian women, without presenting separate results for participants with other ethnic origins. Because the ethnicity of participants lost to follow‐up was not reported in the primary studies, it is impossible to determine whether the findings were representative for ethnic minority women. In addition, the meta‐analyses failed to report risk‐of‐bias assessment and forest plots of the findings.28, 29 These flaws invite for a meta‐analysis following established procedures in order to avoid spin citation of results that lack empirical research evidence.
It has been claimed that access‐enhancing interventions produce the best results for increasing attendance at breast and cervical cancer screening, followed by education, individual counseling, and letters or other reminders.28, 29 In clinical practice, providing education is easier to implement and has far lower financial costs, compared to increasing the availability of mammography equipment worldwide. The two previous meta‐analyses investigated strategies to improve breast and cervical cancer screening among ethnic minorities in the United States, but low participation at cancer screening among ethnic minority women is a significant problem in Europe, Canada, and Australia as well.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 Therefore, the scope of the current meta‐analysis was to determine whether culturally tailored educational interventions increase attendance at mammography and the Pap tests among ethnic minority women in Western countries.
2. METHODS
Cochrane collaboration guidelines on conducting systematic reviews,34 Center for Review and Dissemination's guidelines for undertaking reviews in health care,35 and PRISMA guidelines36 were followed through the entire review process.
2.1. Eligibility criteria
Eligibility of randomized controlled trials (RCTs) was based on following inclusion criteria: Participants were women >18 years of Asian, African, Hispanic, or Oceanian (except Australia and New Zealand) origin living in a Western country (defined as Europe, the United States, Canada, Australia, and New Zealand). Educational interventions consisted of verbal teaching (one‐on‐one or in groups), written material, video or media, or a combination of these interventions and were given by trained lay health workers or health care professionals. Educational intervention was operationalized and defined as a new program, course, curriculum, or pedagogical technique that seeks to reform an older system or practice.26 Educational interventions were culturally tailored to the targeted group. Outcome of interest was screening attendance at mammography and/or the Pap test at baseline and follow‐up, self‐reported from the participants or collected from medical records.
Studies were excluded if the educational part had been but one element of a multilevel intervention program or if educational efforts had been combined with assisted navigation, as effects could not then be attributed to the educational intervention alone.
2.2. Search strategies
Comprehensive systematic literature searches were conducted in Ovid MEDLINE, ProQuest, PubMed, PsycINFO, and Cochrane CENTRAL. Our search strategy and PICO form included relevant keywords and thesaurus, such as “ethnic group,” “immigrant,” “women,” “education,” “teaching,” “intervention,” “screening,” “mammography,” and “Papanicolaou test.” Experts in database searches critically assessed the search strategy before the searches were conducted in May 2017, with an update in May 2018. The searches included records from inception to present and had no limits regarding languages. References of retrieved articles were also scanned for additional studies of interest. We also systematically examined all articles included in the two previous meta‐analyses. Details of the search strategies are available in Appendix S1.
2.3. Study selection
All titles and abstracts were scrutinized by the first author (TB), and records that obviously did not meet the inclusion criteria were excluded. The causes for exclusion were documented in an evidence table and reviewed by the third author (SB). All excluded records were assessed jointly for a final decision. The remaining records were read in full text and assessed separately by the two reviewers (TB, SB). Any discrepancies between the two reviewers were solved by consensus decision. Articles with insufficient information were excluded. To ensure transparency in the selection of studies, detailed information of excluded studies and cause of exclusion is available.
2.4. Data extraction
All extracted data from each study were documented in an evidence table inspired by Botella and Gambara.37 The two reviewers independently coded characteristics, with a 92 percent level of agreement. Because the included studies reported their findings in different ways, the data were converted into a common format. In order to reduce risks of errors, all results were extracted and controlled several times. First, one reviewer (TB) extracted and converted the results two separate times. Then, the two sets of extracted data were compared. Finally, TB and SB studied all extracted data for accuracy and calculated the converted data a third time. Discrepancies were resolved by discussion and recalculation. Researchers from two primary studies were contacted in order to obtain missing or additional data, but none responded.
2.5. Assessing the risk of bias
The Cochrane Collaboration tool was used to assess the risk of bias.38 Included studies were assessed independently by the first and third authors, and any disagreement was resolved by discussion. The level of agreement prior to consensus discussions was very good, with an intraclass correlation coefficient (ICC, two‐way random‐effects model, absolute agreement, single measure reliability) of 0.79 (95% CI, 0.67‐0.86).
2.6. Statistical analysis
The current meta‐analysis was conducted in Stata SE release 16. A significance level of P = .05 and 95% confidence interval (CI) were used. The effect measure was risk ratio (RR). Risk difference (RD) might be the natural choice in meta‐analysis of RCTs with binary outcomes,39 but ratio‐based effect measures have greater stability over different risk groups than difference‐based measures.39 Analyses with both a random‐effects and a fixed‐effects model were run to test the stability over the models. For this study, the random‐effects model was chosen. In such a model, the between‐study variation must be estimated. The restricted maximum likelihood estimate (REML) is usually preferred to the simpler DerSimonian‐Laird (D + L) pooled estimate.40 The forest plot presents the effect estimates of the included studies, with the overall effect size, with REML estimation of the between‐study variation. For the fixed‐effects model, the overall effect was calculated with the Mantel‐Haenszel (M‐H) pooled estimate.40
Statistical heterogeneity was examined using I 2 statistics with its P‐value, as recommended for meta‐analyses.41 The I 2 statistic measures the percentage of total variation in study results that is due to heterogeneity. I 2 < 40 percent indicates low heterogeneity, values indicate 30‐60 percent moderate heterogeneity, and values 50‐90 percent may indicate substantial heterogeneity, while I 2 over 75 percent is defined as considerable. We also used L'Abbé plots to analyze heterogeneity of the effect measure.39
Publication bias was assessed by visual examination of funnel plots and the Harbord test to examine and interpret asymmetry.42, 43 This test is recommended for meta‐analyses of RCTs with binary outcomes. Although the funnel plot and the Harbord test may have undesirable properties in detecting asymmetry, they provide valuable information.42, 43
3. RESULTS
3.1. Search results
The electronic database search identified 207 records (Appendix S2). Scanning references identified 41 studies of interest. Sixty‐eight records were duplicates. Of 146 records, five RCTs measured mammography attendance,44, 45, 46, 47, 48 two measured Pap test attendance,49, 50 and two measured both51, 52 (Figure 1).
Figure 1.
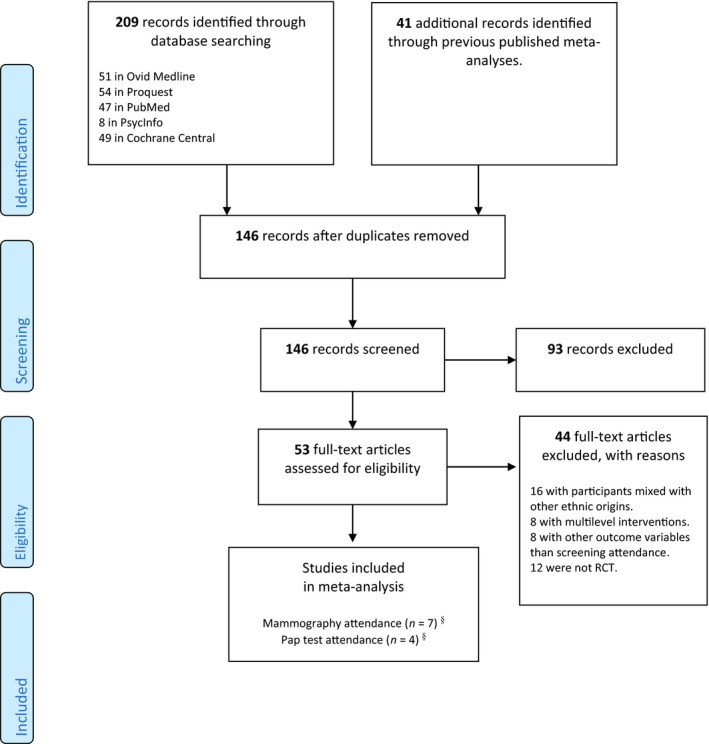
Flow diagram. §Two studies measured both mammography and Pap test attendance and were included in both meta‐analyses. [Color figure can be viewed at wileyonlinelibrary.com]
3.2. Characteristic of the included studies
The seven RCTs that measured mammography attendance included 4246 participants. All studies were conducted in the United States and published between 2003 and 2014. Participants were Asian (3), African American (2), Hispanic (1), and Polynesian (1). Sample sizes ranged from 344 to 984. All RCTs used self‐reported data. Follow‐up ranged from two to 15 months, with four trials conducting follow‐up at 6 months. The educational interventions were theory‐based, and six RCTs were based on the health belief model alone or in combination with other theories. In five RCTs, the educational interventions consisted of verbal education in groups or one‐on‐one; three of these RCTs combined verbal education with written information. The education was provided through lay health workers (2), video (2), and professionals (2).
The four RCTs measuring Pap test attendance included 1750 participants with Hispanic (3) and Asian (1) origins. The studies were conducted in the United States and published between 2003 and 2013. Sample sizes ranged from 120 to 613. Outcome was collected through self‐reported data, and follow‐up ranged from two to 12 months. The educational interventions consisted of verbal education in groups, and two combined verbal education with written information. Lay health workers provided the education in three RCTs. The educational interventions in three RCTs were based on the health belief model alone or in combination with other theories. Characteristics of the included RCTs are described in Table 1.
Table 1.
Table of characteristics
| Author (Year) | N | Sample completed (intervention/ control) | Population, ethnicity | Intervention | Cultural tailoring | Educator | Theoretical framework | Control group | Follow‐up months |
|---|---|---|---|---|---|---|---|---|---|
| Mammography attendance | |||||||||
| Champion et al (2006) | 344 | 299 (243/56) | African Americans | Three study arms: (a) educational 20‐min video; (b) a 40‐min interactive computer‐assisted instruction program. The targeted videotape was a linear version of the computer program. (c) Control group | The interventions were developed using input from community‐based focus groups of African American women who reviewed scripts for sociocultural appropriateness, acceptability, and understandability. The program used African American women (storytellers, media celebrity, physician, and minister) to educate and to demonstrate a mammography procedure | Video | HBMa, TTMb, extended parallel process model | Written material | 6 |
| Lee et al (2014) | 428 | 395 (195/200) | Korean immigrants in the United States | Educational 30‐min DVD, a 10‐min group discussion session after video with PowerPoint presentation, and a homework discussion couple activity | The education program used a Korean‐language DVD with a Korean American physician to address facts and culture‐specific beliefs that prevent Korean American women from receiving screening. The homework discussion activity aimed to increase support provided by Korean American husbands for their wives | HBMa, Klein‐man's model of illness | Diet information | 6,15 | |
| Mishra Shiraz et al (2007) | 809 | 775 (391/384) | Samoan in the United States | Educational booklets, skill building and behavioral exercises, and interactive group discussion sessions | Educational materials in English and Samoan language, with Samoan artwork, scenery, and pictures of Samoans. Samoan health educators held educational sessions in Samoan language, addressing culture‐specific myths and beliefs. Role‐play and skill building with cultural and religious considerations | Lay health workers | HBMa, Freire's empowerment pedagogy | Usual care | 8 |
| Sadler et al (2011) | 984 | 232 (112/120) | African Americans | Breast cancer education‐session offered in beauty salons. Posters and literature were displayed throughout the salons and cosmetologists used synthetic breast models to show clients how a lump feels. | Cosmetologists were trusted members of the African American society and located in their local community. The cosmetologist received individual training from an African American storyteller, an integral element in African culture. The salon had posters, brochures, and magazines with African American women (eg, black celebrities with cancer) | Trained beauty cosmetologist | HBMa | Diabetes education | 6 |
| Wang et al (2012) | 664 | 571 (378/193) | Chinese Americans | Three study arms: (a) culturally target video including a Chinese soap opera–style story and recommendations from a Chinese physician; (b) genetic video with a general soap opera story with recommendations from a physician. (c) Control group | The culturally target video in soap opera style had a Chinese breast cancer survivor celebrating her birthday with friends. The female physician was Chinese. The video was in Mandarin, dubbed in Cantonese, with Chinese and English subtitles. The generic video showed multiethnic women discussing cancer at lunch break, with an American physician, talking in English, dubbed in Mandarin and Cantonese with Chinese and English subtitles | Video | HBMa | Fact sheet via mail | 6 |
| PAP test attendance | |||||||||
| Byrd et al (2013) | 613 | 513 (380/133) | Mexican Americans | Four study arms: (a) the full AMIGA program: video and flip chart with information, including games, activities, and a set of cards; (b) the AMIGA program without the video; (c) the AMIGA program without the flip chart. The 3 interventions included written information. (d) Control group | The intervention was developed by researchers, community members, and lay health workers with Hispanic origins and of similar socioeconomic status as the participants. Bicultural and bilingual lay health workers tested and validated the educational material. Education was given in Spanish or English, and addressed common myths, barriers and beliefs about cervical cancer and screening among Hispanics | Lay health workers | HBMa, TTMb, social cognitive theory | Usual care | 6 |
| O'Brien et al (2010) | 120 | 70 (34/36) | Hispanics in the United States | Two 3‐h workshops, followed by education and pamphlets | Education program designed especially for Hispanic women, addressing common myths and barriers and epidemiology of cervical cancer in Hispanics. Questionnaires, education, and follow‐up in Spanish | Lay health workers | HBMa | Usual care | 6 |
| Mammography and pap test attendance | |||||||||
| Jandorf et al (2008) | 487 | 250 (151/99) | Latinas in the United States | Open health education meetings at local venues (eg, churches, homes, schools), with educational presentations and narrative communication from cancer survivors | The intervention was based on focus group findings with Latina breast cancer survivors, community gatekeepers and local clergy. The education provided specific cultural information and beliefs that resulted in a unique educational program for Latinos | Lay health workers and staff members | Diabetic education program | 2 | |
| Maxwell et al (2003) | 530 | 447 (213/234) | Filipino Americans | Educational group sessions in 60‐90 min and information packages to take home | Several components of the study were based on recommendations of Filipino community partners. Information and questionnaires were given in Tagalog and English. All health educators were born and raised Philippines and fluent in both English and Tagalog. The education was provided by a female Filipino health professional. Traditional Filipino snacks were served | Physicians and nurses | HBMa, adherence model | Physical activity module | 12 |
The health belief model.
The transtheoretical model.
3.3. Risk of bias
Among the mammography attendance RCTs, one RCT was assessed to have high risk of bias, two to have moderate risk of bias, and four to have low risk of bias. Among the included RCTs measuring Pap test attendance, one was assessed to have moderate risk of bias and three to have low risk (Table 2).
Table 2.
Risk of bias
| Author (Year) | Selection bias | Performance bias | Detection bias | Attrition bias | Reporting bias | |
|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Blinding of participants and personnel | Blinding of outcome assessment | Incomplete outcome data | Selective reporting | |
| RCTs measuring mammography attendance | ||||||
| Champion et al (2006) | 1 | 2 | 2 | 0 | 2 | 0 |
| Jandorf et al (2008) | 0 | 0 | 2 | 0 | 2 | 0 |
| Lee et al (2014) | 0 | 1 | 2 | 0 | 1 | 0 |
| Maxwell et al (2003) | 1 | 1 | 2 | 0 | 0 | 0 |
| Mishra Shiraz et al (2007) | 1 | 1 | 2 | 0 | 1 | 0 |
| Sadler et al (2011) | 1 | 1 | 2 | 0 | 1 | 0 |
| Wang et al (2012) | 1 | 1 | 2 | 0 | 0 | 0 |
| RCTs measuring Pap test attendance | ||||||
| Byrd et al (2013) | 0 | 1 | 2 | 0 | 0 | 0 |
| Jandorf et al (2008) | 0 | 0 | 2 | 0 | 2 | 0 |
| Maxwell et al (2003) | 1 | 1 | 2 | 0 | 0 | 0 |
| O'Brien et al (2010) | 1 | 1 | 2 | 0 | 1 | 0 |
3.4. Effectiveness of culturally tailored educational interventions on attendance at mammography
The overall REML risk ratio (RR) for mammography was 1.18 (95% CI, 1.09‐1.28, P < .001) with low heterogeneity (I 2 = 30.0, P = .237). The forest plot shows the individual and overall effects with random‐effects model (Figure 2). The corresponding results for the fixed‐effects model, with the overall M‐H estimate, are 1.17 (95% CI, 1.09‐1.26, P < .001) (results not shown).
Figure 2.
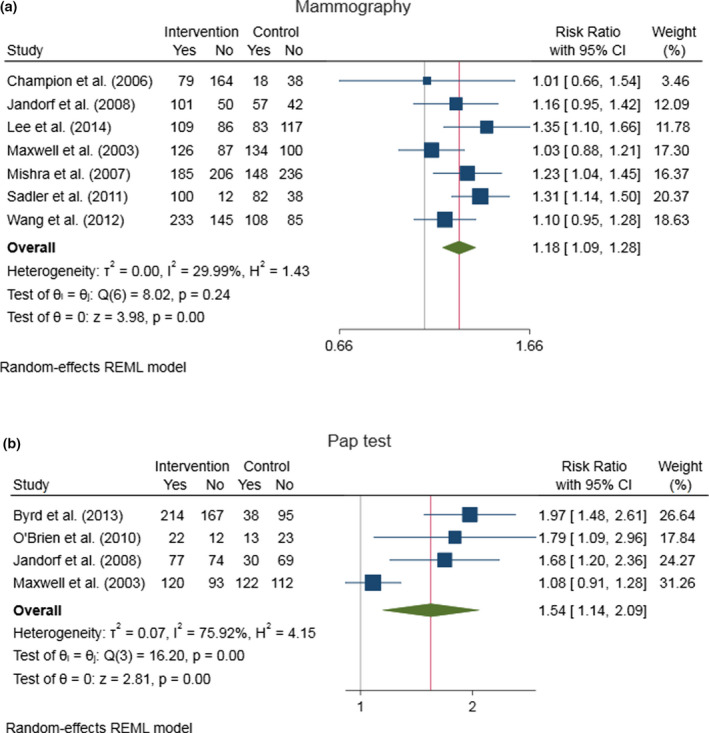
Forest plot. The square data markers indicate risk ratios (RRs) from primary studies, with sizes reflecting the statistical weight of the study using random‐effects model. The horizontal lines indicate 95% CIs. The diamonds data markers represent the overall RR and 95% CI with random‐effects model, with the overall effect estimated by the restricted maximum likelihood estimate (REML). Heterogeneity was estimated using I2 statistics. The vertical lines through the diamonds show the summary effect estimate, next to the line of no effect (RR = 1) [Color figure can be viewed at wileyonlinelibrary.com]
We explored the heterogeneity by visual examination of L'Abbé plots (Appendix S3). The information about the heterogeneity contained in the forest plots was confirmed in the L'Abbé plot. Comparing the L'Abbé plot with RD and RR as effect measures, we observed less variability for RR (results not shown). Publication bias was assessed by visual examination of a funnel plot (Figure 3). Funnel plot asymmetry was explored by the Harbord test, and no statistically significant asymmetry was found (P = .649). With a small number of studies, it is difficult to identify publication bias.
Figure 3.
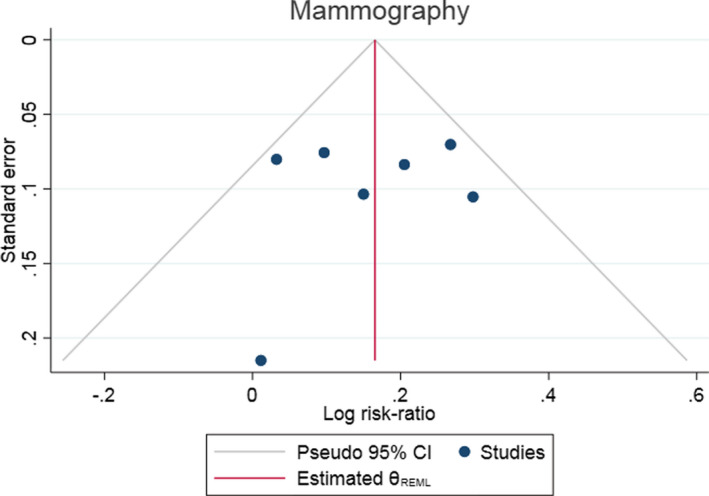
Funnel plot. Funnel plots for the meta‐analysis of the effects of educational interventions on attendance at mammography. Circles indicate included studies. The effect estimates are on the x‐axis and standard error estimates on the y‐axis. The scale of the y‐axis is reversed, so that studies with low precision are placed at the bottom. Studies with greater precision and large N are at the top of the plot. Asymmetry of the plot can indicate publication bias [Color figure can be viewed at wileyonlinelibrary.com]
3.5. Effectiveness of culturally tailored educational interventions on attendance at the Pap test
RR for the Pap test was 1.54 (95% CI, 1.14‐2.09, P = .005), with substantial heterogeneity (I 2 = 75.9%, P < .001). Figure 2 shows the forest plot with the individual and overall effects with random‐effects model. The corresponding results for the fixed model with the overall M‐H estimate were 1.45 (95% CI, 1.27‐1.65, P < .001) (results not shown).
The forest and L'Abbé plots confirmed that the effect measure for the Maxwell et al (2013) study differs significantly from the other included studies. When we deleted this study from the meta‐analysis, we found an increased effect of 84 percent, RR = 1.84 (95% CI, 1.50‐2.24, P < .001), with I 2 = 0.00%, P < .783). Because I 2 is calculated from a Cochran's Q value of 0.49, and this is less than the number of studies minus one, I 2 is negative, and therefore converted to zero.39 Due to the low number of studies of the Pap test, no funnel plot was made.
Both the analyses of mammography and the Pap test included results from Jandorf et al51 and Maxwell et al52 There may be dependence between attendance of mammography and the Pap test. Since there was no information about the sample size for those attending both mammography and the Pap test, we were unable to estimate the dependence. We have assumed that the dependence is only minor and have estimated effect sizes and test statistics under standard assumptions of independent samples.
4. DISCUSSION
The meta‐analyses in the current systematic review indicate that culturally tailored educational interventions may increase attendance at mammography and the Pap tests among ethnic minority women. These results are consistent with previous reviews that have found that theory‐based and tailored interventions increased screening attendance.28, 29, 30 The aim of early detection is to reduce mortality and other serious consequences of advanced disease.14 In settings where early detection and basic treatment are available and accessible, the 5‐year survival rate for early localized breast cancer exceeds 80 percent.53 As a result of public screening programs in Western countries, cervical cancer rates have decreased by as much as 65 percent over the past 40 years.1 Cancer is a major global health problem, responsible for 8.8 million deaths in 2015, and the number of new cancer cases is expected to rise by about 70 percent over the next two decades.1 The unabated rise of incidence rates among some of the racial and ethnic groups is of particular concern.54
Racial and ethnic disparities in breast and cervical cancer incidence and screening attendance are evident in the United States.54, 55 As well, immigrants in Europe, Australia, and Canada have low levels of participation in screening programs.2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 At the same time, studies have found that groups of immigrant women, more often than other women, have late‐stage cancer when they are diagnosed, a diagnosis associated with a higher rate of mortality,56, 57 and immigrant women have reported cultural, religious, and linguistic barriers to participation at cancer screening programs in their host countries.16, 19, 20, 23 Currently, the number of migrants worldwide has reached 250 million and grows at a rate greater than the rate of growth of the world's population, and high‐income countries host almost two‐thirds of all immigrants.58 Taking into consideration, therefore, the large number of affected women, implementation of effective educational interventions that are relatively inexpensive can potentially reduce disease, illness, and mortality among women worldwide.
Culturally tailored educational interventions in the current study contained theory‐based group education, individual counseling, and education provided by local lay health workers or professionals and were combined with linguistic tailored brochures, video, and media campaigns. Culturally relevant strategies, such as relevant graphics, role models, and narrative storytelling from cancer survivors from the target populations, were integrated into the programs. These types of interventions are often referred to as “complex,” because the constituent parts may act both independently and interdependently. Thus, defining the “active ingredient” can be less straightforward than in other research topics.35 Hence, it appears that the most significant clinical issue is to consider what types of intervention work best in a particular setting and for a particular population group. Evaluation of public health interventions is usually complex, as multiple interventions, outcomes, participants, settings, and stakeholders are often necessary components. Success invariably depends on health and on social and economic contexts that have a wide‐reaching and sustainable impact on peoples' lives.35 Because of this complexity, no single evaluation method is likely to be appropriate, and a range of different study designs are used.35 Indeed, all these differences contribute to the complexity and, thus, heterogeneity at the synthesis stage.35 In the current systematic review, the intervention effect on mammography attendance had low heterogeneity, whereas the impact of intervention on attendance at the Pap tests generated substantial heterogeneity, mainly due to one study. Subgroup analyses can be used to explore the heterogeneity and aid the evaluation of differential impacts across groups and in assessing inequalities.35 Unfortunately, the data in the current study did not have sufficient statistical power to analyze differences and similarities between ethnic minority groups, types of educational interventions, or socioeconomic factors, such as education level, household income, and previous screening history. Thus, careful judgment is needed when interpreting the results.
The results in the current study indicate that education with theory‐based instructions, culturally relevant materials, and linguistically appropriate methods may be effective in enhancing cancer screening attendance. Linguistically appropriate approaches have been used for decades as culturally sensitive intervention strategies to enhance participants' understanding.59 Diverse aspects of culture can be incorporated into an intervention, both superficially, through the use of graphics and features relevant to the target population, and more deeply, through the integration of social and cultural values. Still, culture is a comprehensive social phenomenon that includes knowledge, attitudes, experience, belief, values, and religion for a group of people.60 As well, culture is not static.60 Thus, culturally tailored interventions may not necessarily adequately address all aspects of participants' cultural characteristics. Knowing participants' characteristics and preferences is required in order to choose suitable health education materials.30
4.1. Strengths
A broad range of search terms, combined with multiple complementary electronic databases supplemented with hand searches, contributed to a highly sensitive and thorough literature search. The strict and operationalized eligibility criteria, including exclusively RCTs with a study population consisting of only ethnic minority women, allowed us to split the results into two meta‐analyses. Independent reviewers performed study selection, data extraction, and risk‐of‐bias assessment. Only one RCT was assessed as having a high risk of bias. Data were converted into a common format and controlled multiple times to reduce the risk of error. This resulted in high interrater absolute agreement, and in cases of doubt, consensus decisions were used as quality control. In addition, we collaborated with experts in database literature searches, and one of the authors (PL) is an expert in statistical methods for meta‐analysis.
4.2. Limitations
The target of the current meta‐analysis was RCTs conducted in Western countries. However, as all the included RCTs were conducted in the United States, the findings may not be generalizable to other Western countries. This is unfortunate, because there are more immigrants in Europe than in the United States,58 and the low participation rates in preventive screening among immigrant women are also a significant problem in Europe, Canada, and Australia. Hence, future research may want to examine the effectiveness of educational interventions among ethnic minority women outside of the United States.
All RCTs measured outcome by self‐reported data. There is always a risk of bias in designs that rely entirely on self‐report as a source of information for the outcome variable. Two studies validated some of their self‐report data with medical records. Unfortunately, due to the insufficient amount and low quality of the data, it was not possible to synthesize these data. We recommend that future researchers make strong efforts to obtain data from medical records in order to validate their self‐reported data.
Although we constructed a structured and accurate search strategy and carried out comprehensive searches in five databases, only seven RCTs met the inclusion criteria for mammography attendance, and four RCTs, for Pap test attendance. Even though there were no restrictions regarding language, only Anglophone trials were identified. There may be RCTs that our search failed to identify.
The current meta‐analysis showed substantial heterogeneity for Pap test attendance. Due to the low amount of RCTs and insufficient information published in the primary study reports, we were unable to explore the heterogeneity through subgroup analyses, such as differences and similarities between ethnic minority groups, types of educational interventions, or socioeconomic factors. Thus, we call for careful judgment when interpreting this result.
The current meta‐analysis included women of Asian, African, Hispanic, or Oceanian origin. However, ethnic minority women are a heterogeneous group with many differences, and the women in these studies represented diverse ethnic origins. All reviewers are recommended to use operationalized definitions,35 but a major problem is the inconsistent use and wide variation in the definitions of ethnic minorities and migrants used in empirical studies. For example, there is not even a universally accepted definition for migrant at the international level.61 To research and analyze accurately something like the immigrant phenomenon—or, more specifically, the phenomenon of various ethnic minority women and their relationship to their health care—then clear and consistent terminology needs to be agreed upon for conducting and reporting studies.
5. CONCLUSION
Interpreted within the limitations set by the low number of studies and substantial heterogeneity for the Pap test studies, findings from the current meta‐analyses indicate that culturally tailored educational interventions may increase attendance at breast and cervical cancer screening among ethnic minority women. RCTs conducted outside of the United States are needed to examine whether our findings are similar for ethnic minority women in other Western countries. To inform clinical practice, more research is required to determine which educational approaches and settings are the most effective for increasing participation in cancer screening.
CONFLICT OF INTEREST
The authors have no conflict of interest.
Supporting information
ACKNOWLEDGMENT
Joint Acknowledgment/Disclosure Statement: Writing of the article was funded by Research and Development Unit, Møre and Romsdal Hospital Trust.
Brevik TB, Laake P, Bjørkly S. Effect of culturally tailored education on attendance at mammography and the Papanicolaou test. Health Serv Res. 2020;55:457–468. 10.1111/1475-6773.13271
Funding information
This work was supported by the Møre and Romsdal Hospital Trust.
REFERENCES
- 1. Torre LA, Bray F, Siegel RL, Ferlay J, Lortet‐Tieulent J, Jemal A. Global cancer statistics, 2012. CA: A Cancer J Clin. 2015;65(2):87–108. [DOI] [PubMed] [Google Scholar]
- 2. Bhargava S, Moen K, Qureshi SA, Hofvind S. Mammographic screening attendance among immigrant and minority women: a systematic review and meta‐analysis. Acta Radiol. 2018;59(11):1285‐1291. [DOI] [PubMed] [Google Scholar]
- 3. Ahmed AT, Welch BT, Brinjikji W, et al. Racial disparities in screening mammography in the United States: a systematic review and meta‐analysis. J Am College Radiol. 2017;14(2):157‐165. [DOI] [PubMed] [Google Scholar]
- 4. Aminisani N, Armstrong BK, Canfell K. Cervical cancer screening in Middle Eastern and Asian migrants to Australia: a record linkage study. Cancer Epidemiol. 2012;36(6):394‐400. [DOI] [PubMed] [Google Scholar]
- 5. Azerkan F, Sparén P, Sandin S, Tillgren P, Faxelid E, Zendehdel K. Cervical screening participation and risk among Swedish‐born and immigrant women in Sweden. Int J Cancer. 2012;130(4):937‐947. [DOI] [PubMed] [Google Scholar]
- 6. Berens E‐M, Stahl L, Yilmaz‐Aslan Y, Sauzet O, Spallek J, Razum O. Participation in breast cancer screening among women of Turkish origin in Germany – a register‐based study. BMC Women's Health. 2014;14(1):24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bhargava S, Tsuruda K, Moen K, Bukholm I, Hofvind S. Lower attendance rates in immigrant versus non‐immigrant women in the Norwegian Breast Cancer Screening Programme. J Med Screen. 2017;25(3):155‐161. [DOI] [PubMed] [Google Scholar]
- 8. Campari C, Fedato C, Iossa A, et al. Cervical cancer screening in immigrant women in Italy: a survey on participation, cytology and histology results. Eur J Cancer Prev. 2016;25(4):321‐328. [DOI] [PubMed] [Google Scholar]
- 9. Møen KA, Kumar B, Qureshi S, Diaz E. Differences in cervical cancer screening between immigrants and nonimmigrants in Norway: a primary healthcare register‐based study. Eur J Cancer Prev. 2017;26(6):521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Woltman KJ, Newbold KB. Immigrant women and cervical cancer screening uptake: a multilevel analysis. Can J Public Health. 2007;98(6):470–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lofters AK, Moineddin R, Hwang SW, Glazier RH. Low rates of cervical cancer screening among urban immigrants: a population‐based study in Ontario, Canada. Med Care. 2010;48(7):611–618. [DOI] [PubMed] [Google Scholar]
- 12. Vahabi M, Lofters A, Kumar M, Glazier RH. Breast cancer screening disparities among urban immigrants: a population‐based study in Ontario, Canada. BMC Public Health. 2015;15(1):679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Vermeer B, Van den Muijsenbergh ME. The attendance of migrant women at the national breast cancer screening in the Netherlands 1997–2008. Eur J Cancer Prev. 2010;19(3):195‐198. [DOI] [PubMed] [Google Scholar]
- 14. Stewart B, Wild CP. World Cancer Report 2014. International Agency for Research on Cancer. Geneva, Switzerland: WHO; 2017. [Google Scholar]
- 15. Knaul FM, Arreola‐Ornelas H, Atun R, et al. Investing in Cancer Care and Control. Boston, MA: Harvard University, Harvard Global Equity Initiative; 2012. [Google Scholar]
- 16. Grandahl M, Tydén T, Gottvall M, Westerling R, Oscarsson M. Immigrant women's experiences and views on the prevention of cervical cancer: a qualitative study. Health Expect. 2015;18(3):344‐354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Rajaram SS, Rashidi A. Minority women and breast cancer screening: the role of cultural explanatory models. Prev Med. 1998;27(5):757‐764. [DOI] [PubMed] [Google Scholar]
- 18. Johnson CE, Mues KE, Mayne SL, Kiblawi AN. Cervical cancer screening among immigrants and ethnic minorities: a systematic review using the Health Belief Model. J Low Genit Tract Dis. 2008;12(3):232‐241. [DOI] [PubMed] [Google Scholar]
- 19. Gele AA. Barriers and facilitators to cervical cancer screening among Pakistani and Somali immigrant women in Oslo: a qualitative study. International Journal of Women's Health. 2017;9:487‐496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Leinonen MK, Campbell S, Ursin G, Tropé A, Nygård M. Barriers to cervical cancer screening faced by immigrants: a registry‐based study of 1.4 million women in Norway. Eur J Pub Health. 2017;27(5):873‐879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kwok C, White K, Roydhouse JK. Chinese‐Australian women's knowledge, facilitators and barriers related to cervical cancer screening: a qualitative study. J Immigr Minor Health. 2011;13(6):1076. [DOI] [PubMed] [Google Scholar]
- 22. Møen KA, Terragni L, Kumar B, Diaz E. Cervical cancer screening among immigrant women in Norway‐ The healthcare providers’ perspectives. Scand J Prim Health Care. 2018;36(4):415‐422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Anaman‐Torgbor JA, King J, Correa‐Velez I. Barriers and facilitators of cervical cancer screening practices among African immigrant women living in Brisbane, Australia. Eur J Oncol Nurs. 2017;31:22‐29. [DOI] [PubMed] [Google Scholar]
- 24. Azami‐Aghdash S, Ghojazadeh M, Gareh Sheyklo S, et al. Breast cancer screening barriers from the womans perspective: a meta‐synthesis. Asian Pac J Cancer Prev. 2015;16(8):3463‐3471. [DOI] [PubMed] [Google Scholar]
- 25. Marlow LA, Waller J, Wardle J. Barriers to cervical cancer screening among ethnic minority women: a qualitative study. J Fam Plann Reprod Health Care. 2015;41:248‐254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. IGI‐Global . What is Educational Education; 2018; https://www.igi‐global.com/dictionary/educational‐intervention/33094. Accessed August 15, 2017. [Google Scholar]
- 27. Kleinman A. The Illness Narratives. Suffering, Healing & the Human Condition. New York: Basic Bookism; 1988. [Google Scholar]
- 28. Han HR, Kim J, Lee JE, et al. Interventions that increase use of Pap tests among ethnic minority women: a meta‐analysis. Psycho‐oncology. 2011;20(4):341‐351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Han H‐R, Lee J‐E, Kim J, Hedlin HK, Song H, Kim MT. A meta‐analysis of interventions to promote mammography among ethnic minority women. Nurs Res. 2009;58(4):246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Chan DN, So WK. A systematic review of randomised controlled trials examining the effectiveness of breast and cervical cancer screening interventions for ethnic minority women. Eur J Oncol Nurs. 2015;19(5):536‐553. [DOI] [PubMed] [Google Scholar]
- 31. Corcoran J, Dattalo P, Crowley M. Interventions to increase mammography rates among US Latinas: a systematic review. J Women's Health. 2010;19(7):1281‐1288. [DOI] [PubMed] [Google Scholar]
- 32. Corcoran J, Dattalo P, Crowley M. Cervical cancer screening interventions for US Latinas: a systematic review. Health Soc Work. 2012;37(4):197‐205. [DOI] [PubMed] [Google Scholar]
- 33. Masi CM, Blackman DJ, Peek ME. Interventions to enhance breast cancer screening, diagnosis, and treatment among racial and ethnic minority women. Med Care Res Rev. 2007;64(5):195S‐242S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Vol. 4 Hoboken: John Wiley & Sons; 2011. [Google Scholar]
- 35. Center for Reviews and Dissemination . Systematic Reviews. CRD Guidance for Undertaking Reviews in Health Care. University of York. York, UK: York Publishing Services Ltd; 2009. [Google Scholar]
- 36. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264‐269. [DOI] [PubMed] [Google Scholar]
- 37. Botella J, Gambara H. Doing and reporting a meta‐analysis. Int J Clin Health Psychol. 2006;6(2):425‐440. [Google Scholar]
- 38. Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fagerland MW. Evidence‐based medicine and systematic reviews In: Laake P, Benestad HB, Olsen BR, eds. Research in Medical and Biological Sciences. Oxford, UK: Elsevier Ltd.; 2015:431‐461. [Google Scholar]
- 40. Fagerland M, Lydersen S, Laake P. Statistical Analysis of Contingency Tables. Boca Raton: Chapman & Hall/CRC; 2017. [Google Scholar]
- 41. Guyatt GH, Oxman AD, Kunz R, et al. guidelines: 7. Rating the quality of evidence—inconsistency. J Clin Epidemiol. 2011;64(12):1294‐1302. [DOI] [PubMed] [Google Scholar]
- 42. Harbord RM, Egger M, Sterne JA. A modified test for small‐study effects in meta‐analyses of controlled trials with binary endpoints. Stat Med. 2006;25(20):3443‐3457. [DOI] [PubMed] [Google Scholar]
- 43. Sterne JAC, Sutton AJ, Ioannidis JPA, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta‐analyses of randomised controlled trials. BMJ. 2011;343. [DOI] [PubMed] [Google Scholar]
- 44. Champion VL, Springston JK, Zollinger TW, et al. Comparison of three interventions to increase mammography screening in low income African American women. Cancer Detect Prev. 2006;30(6):535‐544. [DOI] [PubMed] [Google Scholar]
- 45. Lee E, Menon U, Nandy K, et al. The effect of couples intervention to increase breast cancer screening among Korean Americans. Oncol Nurs Forum. 2014;41(3):185‐193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Mishra Shiraz RB, Cathrine C, Cindy C, Pat L, Claudia B. Results of a randomized trial to increase mammogram usage among Samoan woman. Cancer Epidemiol Biomark Preven. 2007;12:2594‐2604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Sadler GR, Ko CM, Wu P, Alisangco J, Castaneda SF, Kelly C. A cluster randomized controlled trial to increase breast cancer screening among African American women: the black cosmetologists promoting health program. J Natl Med Assoc. 2011;103(8):735‐745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Wang JH, Shwartz MD, Brown RL, et al. Results of a randomized controlled trial testing the efficacy of a culturally‐targeted and a generic video on mammography screening among Chinese‐American immigrants. Cancer Epidemiol Biomark Prev. 2012;21(11):1923‐1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Byrd TL, Wilson KM, Smith JL, et al. AMIGAS: a multicity, multicomponent cervical cancer prevention trial among Mexican American women. Cancer. 2013;119(7):1365‐1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. O'Brien MJ, Halbert CH, Bixby R, Pimentel S, Shea JA. Community health worker intervention to decrease cervical cancer disparities in Hispanic women. J Gen Intern Med. 2010;25(11):1186‐1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Jandorf L, Bursac Z, Pulley L, Trevino M, Castillo A, Erwin DO. Breast and cervical cancer screening among Latinas attending culturally specific educational programs. Prog Community Health Partnersh: Res Educ Action. 2008;2(3):195‐204. [DOI] [PubMed] [Google Scholar]
- 52. Maxwell AE, Bastani R, Vida P, Warda US. Results of a randomized trial to increase breast and cervical cancer screening among Filipino American women. Prev Med. 2003;37(2):102‐109. [DOI] [PubMed] [Google Scholar]
- 53. World Health Organization . WHO Position Paper on Mammography Screening. Geneva, Switzerland: WHO; 2014. [PubMed] [Google Scholar]
- 54. Liu L, Zhang J, Wu AH, Pike MC, Deapen D. Invasive breast cancer incidence trends by detailed race/ethnicity and age. Int J Cancer. 2012;130(2):395‐404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359‐E386. [DOI] [PubMed] [Google Scholar]
- 56. Latif F, Helgeland J, Bukholm G, Bukholm IRK. Ethnicity differences in breast cancer stage at the time of diagnosis in Norway. Scand J Surg. 2015;104(4):248‐253. [DOI] [PubMed] [Google Scholar]
- 57. Jack R, Davies E, Møller H. Breast cancer incidence, stage, treatment and survival in ethnic groups in South East England. Br J Cancer. 2009;100(3):545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. United Nations DoEaSA, Population Division . International Migration Report 2017: Highlights. New York, NY: United Nations DoEaSA, Population Division; 2017. [Google Scholar]
- 59. Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethn Dis. 1999;9(1):10‐21. [PubMed] [Google Scholar]
- 60. Samovar LA, Porter RE, McDaniel ER, Roy CS. Communication Between Cultures. Toronto, ON: Nelson Education; 2017. [Google Scholar]
- 61. Hannigan A, O'Donnell P, O'Keeffe M, MacFarlane A. How do Variations in Definitions of “Migrant” and Their Application Influence the Access of Migrants to Health Care Services? Copenhagen: WHO Regional Office for Europe; 2016. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


