The growing adoption of the electronic health record (EHR) brings new opportunities to improve physician decision-making towards higher value care.1 Default options, or the conditions that are set into place unless an alternative is actively chosen, have been shown to influence decisions in many contexts.2 However, the effectiveness of different ways of implementing defaults has not been systematically examined in healthcare, and many people may assume that this is a ‘one size fits all’ type intervention in which simply changing the default will always have the same effect.2 In prior work, changing the design of EHR medication display defaults for internal medicine physicians increased generic prescribing by 5.4 percentage points.3 In that intervention, the process of searching for a brand name medication changed from displaying a list of brand name options followed by their generic-equivalents to displaying only generic-equivalent options. To view brand names, a physician had to click on another tab. In November 2014, the University of Pennsylvania Health System (UPHS) implemented a different change in EHR defaults among all specialties across the entire health system. Instead of changing display defaults, an opt-out checkbox labeled “dispense as written” was added and if left unchecked the generic-equivalent was prescribed. The objective of this study was to evaluate the impact of this intervention on physician prescribing behaviors.
METHODS
Monthly prescription data from all UPHS outpatient clinics between January 2014 and June 2015 were obtained using Clarity, an EPIC reporting database. We included new prescriptions for oral medications often prescribed for 10 common medical conditions. Medications without an available generic-equivalent and combination pills were excluded. The University of Pennsylvania Institutional Review Board deemed the study exempt.
Generic prescribing rates were compared between the pre-intervention period (January to October 2014) and the post-intervention period (December 2014 to June 2015) using chi square tests. A difference-in-differences approach was used to test whether levothyroxine, a medication known to often have different levels of thyroid hormone than its brand name formulation,4 had a different change in trend than other medications with similar baseline generic prescribing rates. Hypothesis tests were two-sided with a significance level of P < 0.05. Analyses were conducted using Stata (StataCorp, Version 12).
RESULTS
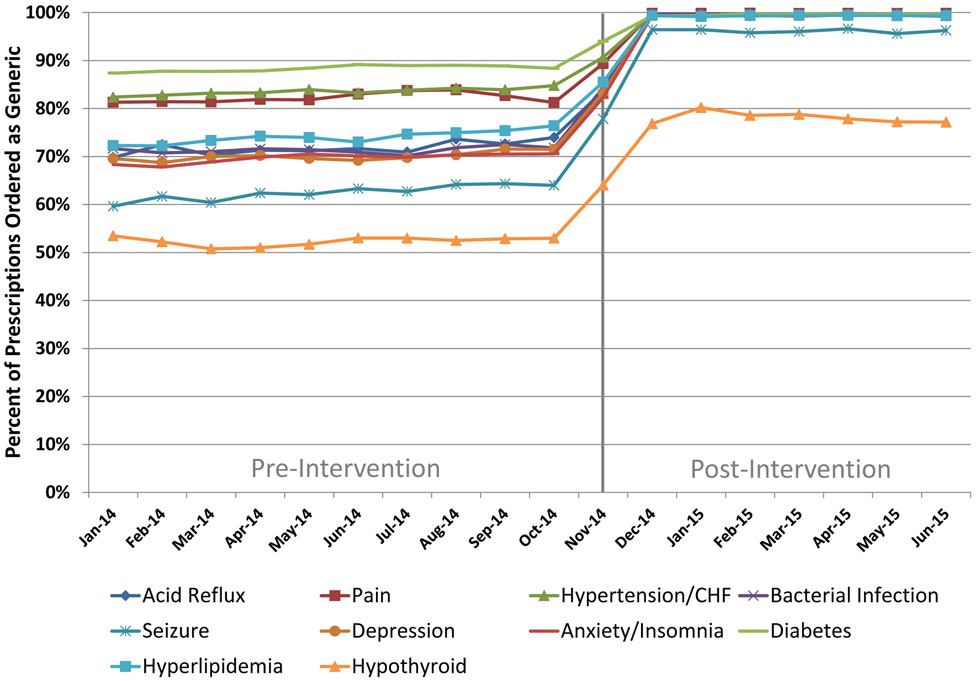
The overall generic prescribing rate increased significantly from 75.3% (611,068/811,561) during the 10-month pre-intervention period to 98.4% (644,587/655,011) during the 7-month post-intervention period (P < 0.001) (Figure). Compared to other medications with similar baseline generic prescribing rates, there was less of an increase for levothyroxine representing a greater proportion of opt-outs (Adjusted Difference-in-Difference: −15.6 percentage points, 95% Confidence Interval: −16.4, −14.8, P < 0.001) (Table).
Figure. Percentage of Medications Prescribed as Generic by Drug Class and Month.
Data presented is percent of medications prescribed as generic by month from January 2014 to June 2015 for each of the represented drug classes. Vertical grey line represents the intervention in mid-November.
TABLE.
Change in Levothyroxine Generic Prescribing Rate Over Time Relative to Medications with Comparable Baseline Rates
| Medication | Pre-Intervention (% Generic) |
Post-Intervention (% Generic) |
Difference (% Generic) |
|---|---|---|---|
| Atorvastatin | 65.4 | 99.1 | 33.7 |
| Divalproex | 37.4 | 90.6 | 53.2 |
| Levofloxacin | 34.3 | 99.8 | 65.5 |
| Lamotrigine | 45.2 | 91.4 | 46.2 |
| Levetiracetam | 38.2 | 92.3 | 54.1 |
| Zolpidem | 64.7 | 98.8 | 34.1 |
| Overall | 57.6 | 98.2 | 40.6 |
| Levothyroxine | 52.5 | 77.9 | 25.4 |
| Adjusted Difference-in-Difference | −15.6 | ||
| 95% Confidence Interval | (−16.4, −14.8) | ||
| P-Value | < 0.001 | ||
Represents linear probability regression model estimate for change in the trend of levothyroxine from the pre-intervention period to the post-intervention period relative to the change in trend of all other medications presented over the same time period
DISCUSSION
Using generic medications has been associated with higher adherence and improved clinical outcomes.5 Yet, brand name medications are often prescribed when generic-equivalents exist leading to unnecessary costs.6 The 23.3 percentage point generic prescribing increase in this study compares favorably with the 5.4 percentage point increase in prior work.3 The opt-out rate for generic levothyroxine was 22.1% after the intervention, compared to <2% among other medications, likely reflecting physicians’ recognition that generic and brand name levothyroxine may differ in formulation.4 This provides a real-world illustration of what has heretofore been an hypothesis in the healthcare context: that the effectiveness of defaults in changing behavior is appropriately mitigated in the setting of strongly held preferences.2 Our results are limited to one health system and in some settings our intervention may be less impactful than it appears because brand name prescriptions are often converted to generics at pharmacies before dispensing. Nonetheless, our findings indicate that the manner in which default options are designed and implemented has an important influence on their effectiveness for changing physician behavior.
ACKNOWLEDGEMENTS
This work was funded in part by a grant from the National Institute on Aging, P30AG034546. Dr. Patel had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Dr. Volpp is a principal at the behavioral economics consulting firm, VAL Health. Dr. Volpp also has received consulting income from CVS Caremark and research funding from Humana, CVS Caremark, Discovery (South Africa), Hawaii Medical Services Association, and Merck, none of which are related to the work described in this manuscript.
REFERENCES
- 1.Patel MS, Volpp KG. Leveraging insights from behavioral economics to increase the value of health-care service provision. J Gen Intern Med. 2012;27:1544–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halpern SD, Ubel PA, Asch DA. Harnessing the power of default options to improve health care. N Engl J Med. 2007;357(13):1340–4. [DOI] [PubMed] [Google Scholar]
- 3.Patel MS, Day S, Small DS, Howell JT, Lautenbach GL, Nierman EH, Volpp KG. Using Default Options Within the Electronic Health Record to Increase the Prescribing of Generic-Equivalent Medications: A Quasi-experimental Study. Ann Intern Med. 2014;161:S44–S52. [DOI] [PubMed] [Google Scholar]
- 4.Hennessey JV. Generic vs name brand L-thyroxine products: interchangeable or still not? J Clin Endocrinol Metab. 2013;98(2):511–4. [DOI] [PubMed] [Google Scholar]
- 5.Gagne JJ, Choudhry NK, Kesselheim AS, Polinski JM, Hutchins D, Matlin OS, Brennan TA, Avorn J, Shrank WH. Comparative Effectiveness of Generic and Brand-Name Statins on Patient Outcomes: A Cohort Study. Ann Intern Med. 2014;161(6):400–407. [DOI] [PubMed] [Google Scholar]
- 6.Gellad WF, Donohue JM, Zhao X, Mor MK, Thorpe CT, Smith J, Good CB, Fine MJ, Morden NE. Brand-name prescription drug use among Veterans Affairs and Medicare Part D patients with diabetes: a national cohort comparison. Ann Intern Med. 2013;159(2):105–14. [DOI] [PMC free article] [PubMed] [Google Scholar]