Abstract
Hungarian obstetrician Ignac Semmelweis (1818–1865) was one of the earliest clinical investigators of modern medical science. In nineteenth century Europe, puerperal fever (childbed fever) was a major clinical and public health problem with very high maternal mortality. It was thought to be caused by miasma, epidemicity, or the Will of Providence. Apart from bloodletting, there was no cure for it. Semmelweis cared for the childbed fever women during their illness, and when they died, he did autopsies on them. Astute clinical observations and logical reasoning goaded Semmelweis to suspect the role of “unholy” hands of “holy” physicians in the transmission of puerperal fever. He enforced a hand-washing policy for physicians. Those with unwashed hands were disallowed into labor room. The hand-washing practice for 1 year led to unprecedented decrease in maternal mortality. It enabled Semmelweis to establish a strong, specific, temporal causal association between unclean hands and puerperal fever. Although not accepted during his lifetime, this causal hypothesis contributed significantly to the understanding of etiopathophysiology of not only puerperal fever but also many other communicable diseases. Clinical hand washing, since then, has prevented millions of deaths of humankind. In the present times too, his idea of hand hygiene plays a central role in COVID-19 pandemic management. Authors present a brief account of life and work of this maverick genius, who was born “too early in the darkness.” He is also called the “Father of infection control” and “Savior of mothers.”
Keywords: Puerperal fever , Childbed fever, Hand hygiene, COVID-19 pandemic
Life and Work
Born in Hungary in 1818, Semmelweis (Fig. 1) graduated from Vienna Medical School in 1844. He specialized in obstetrics and worked in Vienna General Hospital [1]. In nineteenth century Europe, childbed fever (puerperal fever) was an important clinical and public health problem, with very high maternal mortality. It was thought to be caused by “miasma,” epidemicity or by the Will of Providence. Apart from bloodletting, there was no cure for it [2]. Semmelweis cared for these women during their illness, and when they died, he did autopsies on them. He tried to correlate the autopsy findings to clinical symptomatology through secondary data analysis of maternal death records.
Fig. 1.
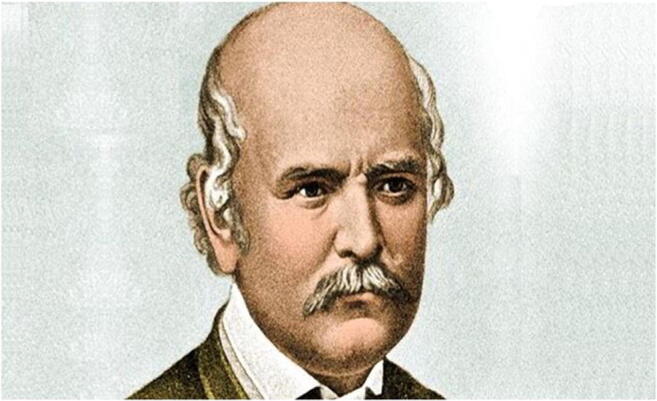
Ignac Semmelweis (1818–1865)
The hospital had two maternity clinics [3]. In first clinic, all deliveries were by physicians and medical students, and in second clinic, all were by midwives. Maternal mortality in the first clinic was unexpectedly higher, 16% compared with 7% in the second clinic. In the first clinic, physicians and medical students started their day by doing autopsies on women who had died on the previous night. From the autopsy room, they proceeded directly to labor room, with no cleaning of their hands, and delivered babies for the rest of the day (surgical gloves were not invented yet; all clinical procedures were done with bare hands). Midwives of the second clinic never conducted autopsies.
During this time, Semmelweis’ friend and colleague Kolletschka died due to overwhelming wound infection of an accidental laceration sustained during one of childbed fever autopsies. Kolletschka’s autopsy findings were similar to those in childbed fever women. Semmelweis suspected a common link between these deaths. He hypothesized that certain “death particles” from body tissues of deceased, stuck to the hands of physicians and medical students during autopsies; their unclean hands carried and transferred these particles to women in labor. Presumably these particles caused childbed fever deaths. Adequate hand washing by physicians and medical students might reduce the transmission of these death particles. He designed and implemented a hand-washing policy for physicians and medical students. Before they entered labor room, they were forced to brush under their fingernails and wash their hands in chlorine water till the skin became dry and cadaveric smell was gone. At the end of 1 year, mortality rate in the first clinic dropped to 2.4%, a rate similar to that seen in the second clinic [4].
Semmelweis thus established causality of childbed fever by demonstrating a strong, specific temporal association with unclean hands in 1847, without even knowing about the exact etiological agent. But to Semmelweis’ seniors, this association seemed implausible and incoherent. They doubted the existence of death particles and rejected the idea of their transmission through “unholy” hands of “holy” physicians.
Semmelweis with his undiplomatic behavior made more professional enemies than friends in Vienna and had to leave for Budapest to work in a city hospital for the rest of his life. Semmelweis published a book “Etiology, the concept, and the prevention of puerperal fever” in 1860, after 13 years of his study. The book had an unwelcome response; it was criticized for poor language and unprofessional writing style. Semmelweis could not tolerate the criticism and suffered with bouts of depression, rage, paranoia, and forgetfulness. He ended up in a mental asylum and died in 1865 [5].
Semmelweis’ contribution was recognized 20 years after his death as the medical world became more receptive and wiser after germ theory of disease by Louis Pasteur and concept of antisepsis by Joseph Lister. He was hailed as the “Father of hand hygiene,” the “Father of infection control,” and “Savior of mothers.”
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
Footnotes
The original version of this article was revised: The article “Ignac Semmelweis—Father of Hand Hygiene”, written by Uvi Tyagi and Kailash Chander Barwal, was originally published in SpringerLink on 21 May 2020 with open access.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
6/27/2020
The article ���Ignac Semmelweis���Father of Hand Hygiene���, written by Uvi Tyagi and Kailash Chander Barwal, was originally published electronically on the publisher���s internet portal (currently SpringerLink) on 21 May 2020 with open access.
References
- 1.Ignaz Semmeweis, Wikipedia
- 2.Semmelweis (2001), US/Austria, Belvedere Film, director: Jim Berry, producers: Robert Dassanowsky and Elfi von Dassanowsky
- 3.Nuland SB. Sherwin B Nuland (ed) doctors- the biography of medicine. 2. New York: Vintage; 1995. The germ theory before germs; pp. 238–262. [Google Scholar]
- 4.Gordis L. The epidemiological approach to disease and intervention. In: Gordis L, editor. Epidemiology,5th edn. Saunders: Elsevier; 2014. pp. 8–11. [Google Scholar]
- 5.That Mothers might live (1938) US, MGM, director: Fred Zinnemann, Oscar for the best short film


