Abstract
Background: Symptoms of anxiety, depression, and cancer-related fatigue are commonly associated with cancer. Cancer patients increasingly use complementary and alternative treatments, such as yoga, to cope with psychological and physical impairments. In the present article, long-term changes of anxiety, depression, and fatigue in cancer are examined 6 months after a yoga intervention. Method: We used an observational design based on a randomized controlled study in cancer patients with mixed diagnoses to evaluate long-term changes of symptoms of anxiety, depression, and fatigue 6 months after the end of yoga therapy. We measured anxiety symptoms with the Generalized Anxiety Disorder scale (GAD-7), depressive symptoms with the Patient Health Questionnaire–2 (PHQ-2), and fatigue with the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire–Fatigue Scale (EORTC QLQ-FA13). Yoga therapy was provided in yoga classes of 60 minutes each once a week for 8 weeks in total. The exercises provided contained both body and breathing activities as well as meditation. Results: A total of 58 patients participated in the study. Six months after the end of yoga therapy, symptoms of anxiety, depression, and fatigue were significantly reduced compared with baseline. However, symptoms of anxiety and fatigue slightly increased during the follow-up period, whereas symptoms of depression remained stable. Conclusion: Our results are promising and support the integration of yoga interventions in supportive cancer treatment concepts but should be confirmed by randomized controlled trials. Long-term effects of yoga therapy on cancer patients should be the subject of further research.
Keywords: cancer, oncology, anxiety, depression, fatigue, yoga, supportive care
Introduction
In Germany, around 50% of the population face a cancer diagnosis in the course of their lifetime.1 According to recent data, half a million people develop cancer every year. Demographic change and widely used screening methods will lead to an increase of 20% of cancer incidences until 2030.1 For this reason, medical care of cancer patients is a very important task of our health care system.
Coping with a life-limiting disease is very challenging and often occurs together with anxiety and depressive symptoms.2-8 The prevalence of anxiety disorders and depression is much higher in cancer patients than in healthy individuals.5,9 Besides anxiety and depression, cancer-related fatigue is one of the most frequent symptoms in cancer patients.10 More than 50% of the patients are affected by fatigue during or after their treatment.11 These cancer-related symptoms could lead to a reduction of quality of life, reduction of treatment adherence, and even worse survival than in not-affected patients.12,13 Accordingly, cancer-related psychological and physical impairments have to be considered in cancer treatment concepts.
In order to cope with these symptoms, 35% to 50% of all cancer patients use complementary and alternative medicine (CAM).14-16 In recent years, a steady rise of CAM use has been observed. Yoga, as a prime example of CAM, is a promising mind-body intervention, which is performed, with increasing demand, as a supportive therapy in oncological care. Concurrently, yoga has become an interesting topic of research.16 To date, most researchers have focused on short-term effects of yoga therapies on psychological and physical symptoms in cancer patients. Previous meta-analyses and reviews suggest that yoga might lead to a reduction of anxiety and depressive symptoms immediately after the intervention.17-24 Short-term effects on fatigue have also been found in several reviews and meta-analyses.19,21,23,25-27 However, there is a lack of understanding of how long the benefits of a yoga intervention might last. With regard to anxiety, 4 small studies could not find any group differences between intervention and control groups at follow-up examinations.28-31 Depressive symptoms were measured in 7 randomized controlled trials (RCTs) including long-term follow-ups, but again, no significant group differences were found 3 to 6 months after yoga therapy.28-34 It is worth noting that anxiety and depressive symptoms were merely studied in secondary analyses. Trials that analyzed changes of fatigue showed inconsistent results concerning long-term effects of yoga interventions.28-36 Therefore, the aim of this study was to evaluate the long-term changes of anxiety, depression, and fatigue in patients with mixed tumor diseases after yoga therapy, using a prospective, observational design.
Methods
Design
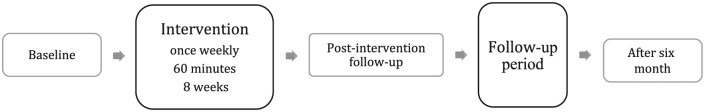
This observational study is based on a randomized, controlled intervention study, which was performed at the University Hospital of Würzburg, Germany, Comprehensive Cancer Center Mainfranken. The Ethical Committee of Würzburg approved the study on July 26, 2014. Cancer patients with different tumor entities were included consecutively. The inclusion criteria were presence of a tumor disease, age of 18 or older, and working knowledge of German language. The recruitment was carried out on the basis of informatory presentations provided by the Comprehensive Cancer Center Mainfranken, which were held every 3 months. Furthermore, the Psycho-oncological Service of the University Hospital of Würzburg addressed cancer patients in person. Eligible patients were briefed both personally and by an information sheet before they gave written consent to participate in the study and external randomization took place. Yoga therapy consisted of weekly classes of 60 minutes each over a period of 8 weeks. During these 8 weeks, participants of the control group did not receive any yoga therapy but were offered yoga therapy thereafter. Every participant completed questionnaires at baseline, before and after yoga therapy, and 6 months after the end of yoga therapy (Figure 1). By providing yoga therapy to the control group after their waiting time ended, comparing the intervention group with the waiting-list control group was limited to the period before the waiting-list control group started yoga therapy. Consequently, for this secondary study on long-term effects, we combined the intervention and control groups because both received yoga therapy.
Figure 1.
Observational one-group pre-post design.
Intervention
Yoga treatment was conducted in groups of 10 to 12 patients. Yoga classes started with a relaxation and a short conversation about the participants’ mental and physical condition. Afterward, several exercises of gentle Hatha Yoga, inspired by John Kabat-Zinn,37 were carried out. This was always done in the same sequence, under supervision, and with correction, if necessary. The exercises were then followed by a meditation at the end of the session. Each participant also received a CD and a printed manual to motivate training at home.
Measures
We used the reliable and valid self-reported Generalized Anxiety Disorder scale (GAD-7) to measure the intensity of various anxiety symptoms.38 GAD-7 has 7 items that refer to the period of the past 2 weeks and can be answered with “Not at all” (0 points), “On individual days” (1 point), “More than half the days” (2 points), or “Nearly every day” (3 points). By summing up these items, the total score of the GAD-7 may range from 0 to 21, with higher values indicating more severe anxiety symptoms.
To determine symptoms of depression, the reliable, valid, and sensitive Patient Health Questionnaire–2 (PHQ-2) was used.39,40 This is a shortened version of the Patient Health Questionnaire–9. It consists of the 2 core symptoms of a depressive episode: depressed mood and loss of interest as well as pleasure in routine activities during the past 2 weeks. The answer options are the same as in the GAD-7. Consequently, the total score may range from 0 to 6 with higher values indicating more severe depressive symptoms.
Cancer-related fatigue was assessed using the dependable questionnaire EORTC QLQ-FA13 (European Organization for Research and Treatment of Cancer Quality of Life Questionnaire–Fatigue Scale).41 This questionnaire measures 3 dimensions of fatigue, emotional, physical, and cognitive fatigue, with 13 items. Response options are “not at all” (1), “a little” (2), “quite a bit” (3), and “very much” (4). Scores are transformed to a scale ranging from 0 to 100. Higher values indicate more severe fatigue symptoms.
Furthermore, we designed a questionnaire to assess information about maintained yoga exercise after the end of yoga therapy. In addition to the main question whether patients continued to practice yoga or not, they were asked if they practiced on their own or with an instructed group. Moreover, we assessed the frequency and duration of yoga exercise. Additionally, the questionnaire included possible reasons why patients continued to practice yoga or why they decided to quit. Possible answers to choose from were, for example, “If I practice yoga, I feel less tired” or “Yoga helps me to better cope with anxiety concerning my tumor disease.” Given reasons why somebody stopped to practice were, for example, “Without professional instruction, I am not motivated to practice yoga” or “I stopped practice because I did not benefit from yoga therapy.”
Statistical Analysis
Data analysis was carried out using IBM SPSS Statistics Version 22. We used paired t tests to analyze changes between baseline and follow-up. We present standardized effect sizes (SES) and 95% confidence intervals (CIs) to demonstrate changes of symptoms of anxiety, depression, and fatigue in the course of the 6-month follow-up period. Furthermore, to analyze a potential link between maintained yoga practice and symptoms of anxiety, depression, and fatigue, the Mann-Whitney U test for independent samples was performed. P < .05 was considered significant.
Results
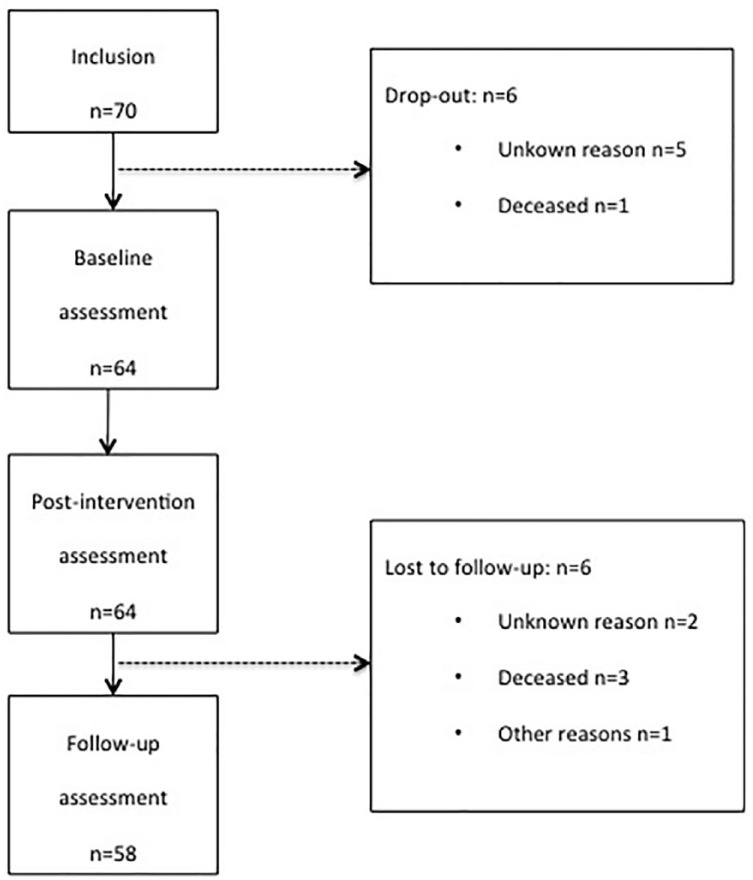
Seventy patients were included. As the number of dropouts (n = 6) and lost to follow-up (n = 6) amounted to 12 persons in total, the data of 58 patients were available for our analyses. The reasons for a dropout remained unknown regarding 5 participants, whereas 1 patient died during the study period. The cause for loss to follow-up was unknown for 2 persons, 3 patients died during the follow-up period, and 1 person stopped participation because of physical problems (Figure 2).
Figure 2.
Patient flow.
A total of 58 patients participated in the study (Table 1). Fifty-two (90%) of the patients were women. The average age was 58 years (SD = 11.97, range 24-80 years), and 62% were married. All patients were German. Ninety percent of the participants had secondary and higher education, which means that they finished either middle/junior high school or academic high school. The most common tumor diagnosis was breast cancer (55%), followed by lymphoma/leukemia (10%), colorectal cancer (7%), and ovarian/endometrial cancer (7%; Table 2). The average time span since primary diagnosis was 24 months. About one tenth of patients had a recurrence, and in one fifth of the patients, metastases were diagnosed.
Table 1.
Sociodemographic Data (n = 58).
| Age | |
| Years, mean (SD) | 58.19 (11.97) |
| Age range | 24-80 |
| Gender, n (%) | |
| Female | 52 (90) |
| Male | 6 (10) |
| Marital status, n (%) | |
| Married | 36 (62) |
| Single | 11 (19) |
| Divorced | 9 (16) |
| Widowed | 2 (3) |
| Living in a relationship, n (%) | 42 (72) |
| Nationality, n (%) | |
| German | 58 (100) |
| Others | 0 (0) |
| Highest graduation, n (%) | |
| Less than junior (<10 years; basic secondary school) | 6 (10) |
| Junior (10 years; middle-level secondary school) | 32 (55) |
| Senior (high school graduate) | 20 (35) |
Abbreviation: SD, standard deviation.
Table 2.
Disease-Related Baseline Data (n = 58).
| Tumor entity, n (%) | |
| Breast cancer | 32 (55) |
| Lymphoma/leukemia | 6 (10) |
| Colorectal cancer | 4 (7) |
| Ovarian/endometrial cancer | 4 (7) |
| Prostatic cancer | 3 (6) |
| Malignant melanoma | 2 (3) |
| Malignomas of bones/joints/muscles | 2 (3) |
| Central nervous system tumors | 2 (3) |
| Pancreatic cancer | 1 (2) |
| Renal cell carcinoma | 1 (2) |
| Malignomas of head and neck | 1 (2) |
| Relapse, n (%) | |
| Yes | 5 (9) |
| No | 50 (86) |
| Missing | 3 (5) |
| Time since diagnosis, n (%) | |
| Up to 1 month | 2 (3) |
| Up to 2 months | 2 (3) |
| Up to 3 months | 1 (2) |
| Up to 6 months | 6 (10) |
| Up to 1 year | 9 (16) |
| Up to 2 years | 14 (24) |
| About 3 years | 5 (9) |
| About 5 years | 5 (9) |
| About 10 years | 8 (14) |
| About 15 years | 4 (7) |
| Missing | 2 (3) |
| Metastases, n (%) | |
| Yes | 11 (19) |
| No | 43 (74) |
| Missing | 4 (7) |
| Relapse, n (%) | |
| Yes | 50 (86) |
| No | 5 (9) |
| Missing | 3 (5) |
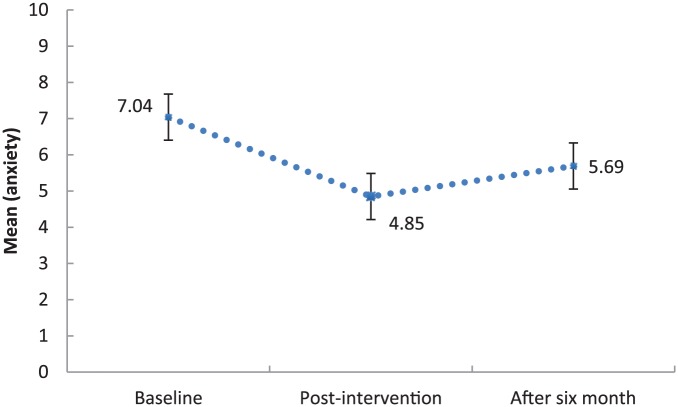
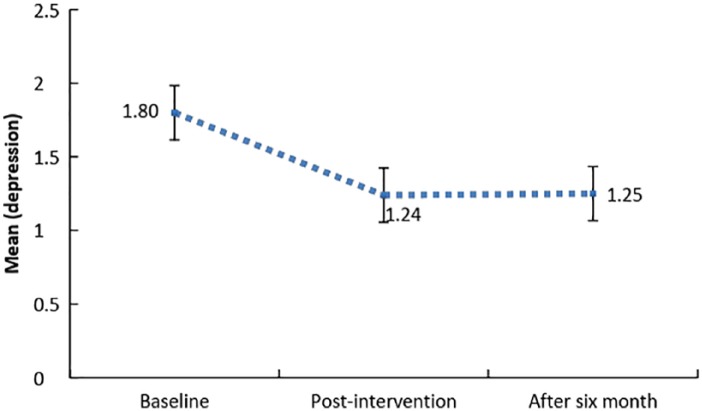
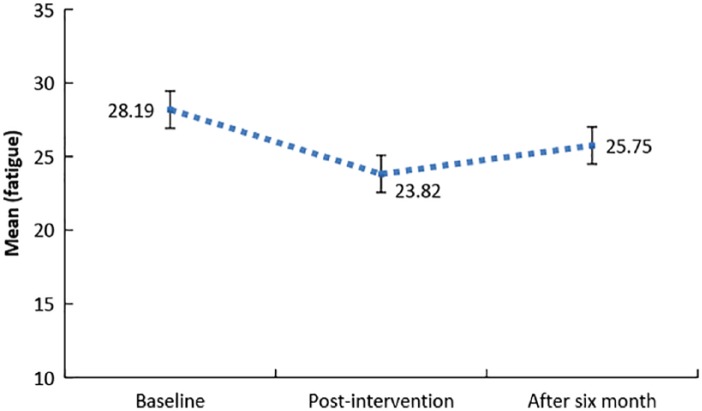
Compared with baseline values, anxiety, depression, and fatigue values were significantly lower at the follow-up time point after 6 months (Figures 3-5 and Table 3). These results suggest long-term improvement of symptoms of anxiety, depression, and fatigue in the course of a yoga therapy. During the follow-up period between the end of yoga therapy and 6 months later, we found a small time effect on anxiety (SES = 0.22, 95% CI = −0.03 to 0.47) and fatigue (SES = 0.27, 95% CI = −0.05 to 0.50), which indicates a slight, nonsignificant increase of symptoms. Regarding depression, no time effect was found during the follow-up period (SES = 0.01, 95% CI = −0.11 to 0.13; Figures 3-5 and Table 4).
Figure 3.
Symptoms of anxiety in the course of the study (n = 55; error bars indicate standard error of the mean).
Figure 4.
Symptoms of depression in the course of the study (n = 55; error bars indicate standard error of the mean).
Figure 5.
Symptoms of fatigue in the course of the study (n = 55; error bars indicate standard error of the mean).
Table 3.
Within-Group Change of Symptoms of Anxiety, Depression, and Fatigue From Baseline to 6-Month Follow-up.
| Variables | n | T1 | T3 | P | SES | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Anxiety | 58 | 6.94 | 4.09 | 5.66 | 3.69 | .013 | −0.31 | −0.56 to −0.06 |
| Depression | 58 | 1.78 | 1.33 | 1.26 | 1.26 | .001 | −0.39 | −0.62 to −0.16 |
| Fatigue | 58 | 28.30 | 8.29 | 25.69 | 8.03 | .006 | −0.31 | −0.54 to −0.09 |
Abbreviations: T1, baseline; T3, follow-up time point after 6 months; M, mean; SD, standard deviation; SES, standardized effect size; CI, confidence interval.
Table 4.
Within-Group Change of Symptoms of Anxiety, Depression, and Fatigue From Post-Intervention to 6-Month Follow-up.
| Variables | n | T2 | T3 | P | SES | 95% CI | ||
|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | |||||
| Anxiety | 55 | 4.85 | 3.80 | 5.69 | 3.72 | .083 | 0.22 | −0.03 to 0.47 |
| Depression | 55 | 1.24 | 1.02 | 1.25 | 1.29 | .900 | 0.01 | −0.11 to 0.13 |
| Fatigue | 55 | 23.82 | 7.10 | 25.75 | 8.10 | .028 | 0.27 | −0.05 to 0.50 |
Abbreviations: T2, post-intervention time point; T3, follow-up time point after 6 months; M, mean; SD, standard deviation; SES, standardized effect size; CI, confidence interval.
Sixty-nine percent of the participants continued to practice yoga after the intervention. Most patients (78%) reported practicing on their own. One third continued to attend instructed yoga classes. The majority of patients practiced less than 45 minutes once to twice per week. The most popular reasons for continuing yoga were reduction of tiredness (82%) and gain of fitness (97%). Furthermore, more than half of the subjects reported continuing because yoga helped deal with anxiety and concerns regarding the future. The main reason not to continue with yoga, reported by 31%, was the lack of professional instruction after the intervention (94%). However, we found no significant relation between the maintenance of yoga practice and symptoms of anxiety (P = .33), depression (P = .19), and fatigue (P = .13).
Discussion
In this observational study, we found a long-term improvement of symptoms of anxiety, depressive symptoms, and fatigue after a yoga intervention in cancer patients with mixed diagnoses. Compared with baseline, anxiety, depression, and fatigue were reduced significantly 6 months after the yoga intervention. However, anxiety and fatigue slightly increased after the end of yoga therapy, whereas depressive symptoms remained stable during the follow-up period after treatment completion. Moreover, maintenance of yoga practice was reported by 69% of the subjects. Most participants reported subjective benefit although no link between maintenance and outcomes was observed.
To date, 4 RCTs investigated long-term effects of yoga therapy on anxiety in cancer patients.28-31 However, none of the trials analyzed change of anxiety in the course of time. No evidence of long-term effects was found. Nonetheless, these negative results have to be questioned. Small study samples, selection bias, and low adherence might have distorted the results. In contrast to these findings, our results indicate long-term improvements of anxiety in the course of yoga therapy.
A small one-armed pilot study reported a significant reduction of depression and fatigue from baseline to 3-month follow-up.36 Two RCTs with breast cancer patients confirmed the long-term reduction of fatigue as an effect of a yoga intervention by demonstrating significant group differences.29,33 Another RCT with 181 breast cancer patients found that depression and fatigue increased during 3 months of follow-up but did not reach baseline levels.32 Furthermore, significant long-term group differences were reported for fatigue but not for depression.32 In only one study, with 163 breast cancer patients, a 6-month follow-up was conducted. Significant group differences for fatigue immediately posttreatment were not found 6 months later, though depressive symptoms were not significantly different between groups at any time.34 To conclude, our results of a significant reduction of fatigue and depressive symptoms between baseline and follow-up are in line with previous research. Still, a causal connection to yoga therapy could not be demonstrated in previous RCTs. Moreover, regarding fatigue, results about long-term group differences were inconsistent.
Most trials included only one tumor entity (especially breast cancer), offered different yoga styles and different length as well as frequency of yoga classes, and were designed as a RCT. Furthermore, different assessment instruments were used in the individual studies. Consequently, making comparisons with our results is difficult, and further research is needed to clarify the inconsistent state of research. Possible long-term effects on anxiety, depression, and fatigue should be investigated in larger studies with active control groups and symptomatic patients with a cancer diagnosis other than breast cancer. Besides clinical trials, research on symptom physiology and biologic mechanisms of response would help better understand the effects of yoga therapies.
Strengths and Limitations
Strengths of this study include excellent adherence with minimal attrition and a loss to follow-up of only 10%. Additionally, this is the first study, to our knowledge, with a 6-month follow-up investigating long-term changes of anxiety, depression, and fatigue after yoga therapy in cancer patients. Further research on long-term effects is definitely needed.
This study was based on an observational design, lending our results less credibility than do studies with a control group. To ensure high compliance with the study in the control group in our primary RCT, yoga therapy was offered to the control group after their waiting time. Thus, this investigation on long-term changes was carried out with methodological limitations. Most important, positive changes of anxiety, depression, and fatigue cannot be causally attributed to yoga therapy. Spontaneous recovery of symptoms, remission or progression of tumor disease, social support, physical activity, and other concurrent treatments may have been confounding variables. Furthermore, the number of participants was relatively small. With a greater number of subjects, higher statistical power could have been achieved. Another limitation is that elevated levels of symptoms of anxiety, depression, and fatigue were not used as part of the inclusion criteria, and therefore, these symptoms had less room to decrease.33 Accordingly, the potential of yoga might be even higher than our data reflect when provided to highly distressed patients. Further studies should employ a larger number of participants and only patients with an increased level of symptoms.
As already mentioned, many of the published studies were restricted to breast cancer patients. Thus, the inclusion of different tumor entities is a strength of our study because current publications of research on tumor entities other than breast cancer are rare but needed.18 In our study, about half of the patients were breast cancer patients but the other half of patients were diagnosed with other cancers. Subgroup analyses should be carried out but are limited by our sample size. However, the high percentage of breast cancer patients restricts the generalizability to patients with other cancers. Other limitations concerning the study population are acknowledged. With a share of 90% of women, a conclusion as to effects in men is not possible. The high level of participation of women with breast cancer reflects the generally higher tendency of women as well as breast cancer patients to use alternative medicine.42-45 In addition, women seem to have more positive beliefs about yoga than men46 and thus are more likely to participate. A positive attitude toward yoga therapy could have biased the results.47 Moreover, generalizability is limited by the fact that many participants had high school education. This may result from the fact that higher educated people are more likely to use CAM.14,44,45 Last, the therapy period lasted 8 weeks. Although effects were achieved during this time and long-term changes could be found, a more extensive therapy with a higher frequency of yoga classes might have produced larger effects and long-term changes.19,32
Conclusion
To conclude, our results suggest positive changes of anxiety, depression, and fatigue in the long term after a yoga therapy. In addition, 69% of patients reported subjective benefits, which led to maintenance of yoga practice. Our results are promising and support the integration of yoga interventions in supportive cancer treatment concepts but should be confirmed by RCTs. Long-term effects of yoga therapy on cancer patients should be the subject of further research.
Acknowledgments
We thank Prof Dr Hermann Faller of the University of Würzburg for his great support with planning our study and statistical analysis and for the supervision of this article. Furthermore, we want to thank the Comprehensive Cancer Center Mainfranken for supporting this study and the Center of Palliative Care for providing the location for the yoga therapy.
Footnotes
Authors’ Note: This article is based on the first author’s doctoral dissertation at the University of Würzburg.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Robert-Koch-Institut; die Gesellschaft der epidemiologischen Krebsregister in Deutschland e.V. Krebs in Deutschland 2011/2012. 10 aufl. Berlin, Germany: Robert-Koch-Institut; 2015. [Google Scholar]
- 2. Roth AJ, Massie MJ. Anxiety and its management in advanced cancer. Curr Opin Support Palliat Care. 2007;1:50-56. [DOI] [PubMed] [Google Scholar]
- 3. Roy-Byrne PP, Davidson KW, Kessler RC, et al. Anxiety disorders and comorbid medical illness. Gen Hosp Psychiatry. 2008;30:208-225. [DOI] [PubMed] [Google Scholar]
- 4. Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160-174. [DOI] [PubMed] [Google Scholar]
- 5. Mehnert A, Brähler E, Faller H, et al. Four-week prevalence of mental disorders in patients with cancer across major tumor entities. J Clin Oncol. 2014;32:3540-3546. [DOI] [PubMed] [Google Scholar]
- 6. Vehling S, Koch U, Ladehoff N, et al. Prevalence of affective and anxiety disorders in cancer: systematic literature review and meta-analysis [in German]. Psychother Psychosom Med Psychol. 2012;62:249-258. [DOI] [PubMed] [Google Scholar]
- 7. Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19-28. [DOI] [PubMed] [Google Scholar]
- 8. Kusch M, Labouvie H, Hein-Nau B. Klinische Psychoonkologie. Berlin, Germany: Springer; 2013. [Google Scholar]
- 9. Hartung TJ, Brähler E, Faller H, et al. The risk of being depressed is significantly higher in cancer patients than in the general population: prevalence and severity of depressive symptoms across major cancer types. Eur J Cancer. 2017;72:46-53. [DOI] [PubMed] [Google Scholar]
- 10. Berger AM, Mooney K, Alvarez-Perez A, et al. ; National Comprehensive Cancer Network. Cancer-related fatigue, version 2.2015. J Natl Compr Canc Netw. 2015;13:1012-1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mehnert A, Hartung TJ, Friedrich M, et al. One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology. 2018;27:75-82. [DOI] [PubMed] [Google Scholar]
- 12. Curt GA. The impact of fatigue on patients with cancer: overview of FATIGUE 1 and 2. Oncologist. 2000;5(suppl 2):9-12. [DOI] [PubMed] [Google Scholar]
- 13. DiMatteo MR, Haskard-Zolnierek KB. Impact of depression on treatment adherence and survival from cancer. In: Kissane DW, Maj M, Sartorius N, eds. Depression and Cancer. Oxford, England: Wiley-Blackwell; 2011:101-124. [Google Scholar]
- 14. Fouladbakhsh JM, Stommel M. Gender, symptom experience, and use of complementary and alternative medicine practices among cancer survivors in the US cancer population. Oncol Nurs Forum. 2010;37:E7-E15. [DOI] [PubMed] [Google Scholar]
- 15. Horneber M, Bueschel G, Dennert G, Less D, Ritter E, Zwahlen M. How many cancer patients use complementary and alternative medicine: a systematic review and metaanalysis. Integr Cancer Ther. 2012;11:187-203. [DOI] [PubMed] [Google Scholar]
- 16. Molassiotis A, Fernadez-Ortega P, Pud D, et al. Use of complementary and alternative medicine in cancer patients: a European survey. Ann Oncol. 2005;16:655-663. [DOI] [PubMed] [Google Scholar]
- 17. Hardörfer K, Jentschke E. Effect of yoga therapy on symptoms of anxiety in cancer patients. Oncol Res Treat. 2018;41:526-532. [DOI] [PubMed] [Google Scholar]
- 18. Lin KY, Hu YT, Chang KJ, Lin HF, Tsauo JY. Effects of yoga on psychological health, quality of life, and physical health of patients with cancer: a meta-analysis. Evid Based Complement Alternat Med. 2011;2011:659876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Buffart LM, van Uffelen JG, Riphagen II, et al. Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer. 2012;12:559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cramer H, Lange S, Klose P, Paul A, Dobos G. Yoga for breast cancer patients and survivors: a systematic review and meta-analysis. BMC Cancer. 2012;12:412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Stan DL, Collins NM, Olsen MM, Croghan I, Pruthi S. The evolution of mindfulness-based physical interventions in breast cancer survivors. Evid Based Complement Alternat Med. 2012;2012:758641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. D’Silva S, Poscablo C, Habousha R, Kogan M, Kligler B. Mind-body medicine therapies for a range of depression severity: a systematic review. Psychosomatics. 2012;53:407-423. [DOI] [PubMed] [Google Scholar]
- 23. Danhauer SC, Addington EL, Sohl SJ, Chaoul A, Cohen L. Review of yoga therapy during cancer treatment. Support Care Cancer. 2017;25:1357-1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Galliford M, Robinson S, Bridge P, Carmichael M. Salute to the sun: a new dawn in yoga therapy for breast cancer. J Med Radiat Sci. 2017;64:232-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Mishra SI, Scherer RW, Snyder C, Geigle P, Gotay C. Are exercise programs effective for improving health-related quality of life among cancer survivors? A systematic review and meta-analysis. Oncol Nurs Forum. 2014;41:E326-E342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Cramer H, Lange S, Klose P, Paul A, Dobos G. Can yoga improve fatigue in breast cancer patients? A systematic review. Acta Oncol. 2012;51:559-560. [DOI] [PubMed] [Google Scholar]
- 27. Hilfiker R, Meichtry A, Eicher M, et al. Exercise and other non-pharmaceutical interventions for cancer-related fatigue in patients during or after cancer treatment: a systematic review incorporating an indirect-comparisons meta-analysis. Br J Sports Med. 2018;52:651-658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cohen L, Warneke CW, Fouladi RT, Rodriguez MA, Chaoul-Reich A. Psychological adjustment and sleep quality in a randomized trial of the effects of a Tibetan yoga intervention in patients with lymphoma. Cancer. 2004;100:2253-2260. [DOI] [PubMed] [Google Scholar]
- 29. Cramer H, Rabsilber S, Lauche R, Kümmel S, Dobos G. Yoga and meditation for menopausal symptoms in breast cancer survivors—a randomized controlled trial. Cancer. 2015;121:2175-2184. [DOI] [PubMed] [Google Scholar]
- 30. Chandwani KD, Thornton B, Perkins GH, et al. Yoga improves quality of life and benefit finding in women undergoing radiotherapy for breast cancer. J Soc Integr Oncol. 2010;8:43-55. [PubMed] [Google Scholar]
- 31. Cramer H, Pokhrel B, Fester C, et al. A randomized controlled bicenter trial of yoga for patients with colorectal cancer. Psychooncology. 2016;25:412-420. [DOI] [PubMed] [Google Scholar]
- 32. Kiecolt-Glaser JK, Bennett JM, Andridge R, et al. Yoga’s impact on inflammation, mood, and fatigue in breast cancer survivors: a randomized controlled trial. J Clin Oncol. 2014;32:1040-1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Bower JE, Garet D, Sternlieb B, et al. Yoga for persistent fatigue in breast cancer survivors: a randomized controlled trial. Cancer. 2012;118:3766-3775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chandwani KD, Perkins G, Nagendra HR, et al. Randomized, controlled trial of yoga in women with breast cancer undergoing radiotherapy. J Clin Oncol. 2014;32:1058-1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL. Yoga of awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Support Care Cancer. 2009;17:1301-1309. [DOI] [PubMed] [Google Scholar]
- 36. Bower JE, Garet D, Sternlieb B. Yoga for persistent fatigue in breast cancer survivors: results of a pilot study. Evid Based Complement Alternat Med. 2011;2011:623168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kabat-Zinn J. Die MBSR Yogaübungen: Stressbewältigung durch Achtsamkeit. 4 aufl. Freiburg im Breisgau, Germany: Arbor; 2015. [Google Scholar]
- 38. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166:1092-1097. [DOI] [PubMed] [Google Scholar]
- 39. Lowe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58:163-171. [DOI] [PubMed] [Google Scholar]
- 40. Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41:1284-1292. [DOI] [PubMed] [Google Scholar]
- 41. Weis J, Arraras JI, Conroy T, et al. Development of an EORTC quality of life phase III module measuring cancer-related fatigue (EORTC QLQ-FA13). Psychooncology. 2013;22:1002-1007. [DOI] [PubMed] [Google Scholar]
- 42. Adams M, Jewell AP. The use of complementary and alternative medicine by cancer patients. Int Semin Surg Oncol. 2007;4:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Wanchai A, Armer JM, Stewart BR. Complementary and alternative medicine use among women with breast cancer: a systematic review. Clin J Oncol Nurs. 2010;14:E45-E55. [DOI] [PubMed] [Google Scholar]
- 44. Cramer H. Yoga in Germany—results of a nationally representative survey [in German]. Forsch Komplementmed. 2015;22:304-310. [DOI] [PubMed] [Google Scholar]
- 45. Garland SN, Valentine D, Desai K, et al. Complementary and alternative medicine use and benefit finding among cancer patients. J Altern Complement Med. 2013;19:876-881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Sohl SJ, Schnur JB, Daly L, Suslov K, Montgomery GH. Development of the beliefs about yoga scales. Int J Yoga Therap. 2011;(21):85-91. [PMC free article] [PubMed] [Google Scholar]
- 47. Mackenzie MJ, Carlson LE, Ekkekakis P, Paskevich DM, Culos-Reed SN. Affect and mindfulness as predictors of change in mood disturbance, stress symptoms, and quality of life in a community-based yoga program for cancer survivors. Evid Based Complement Alternat Med. 2013;2013:419496. [DOI] [PMC free article] [PubMed] [Google Scholar]