Abstract
Objective
The aim of this study was to elucidate the cognitive processes involved in surgical procedures from the perspective of different team roles (surgeon, anesthesiologist, and perfusionist) and provide a comprehensive compilation of intraoperative cognitive processes.
Summary Background Data
Nontechnical skills play a crucial role in surgical team performance and understanding the cognitive processes underlying the intraoperative phase of surgery is essential to improve patient safety in the operating room (OR).
Methods
A mixed-methods approach encompassing semistructured interviews with 9 subject-matter experts. A cognitive task analysis was built upon a hierarchical segmentation of coronary artery bypass grafting procedures and a cued-recall protocol using video vignettes was used.
Results
A total of 137 unique surgical cognitive processes were identified, including 33 decision points, 23 critical communications, 43 pitfalls, and 38 strategies. Self-report cognitive workload varied substantially, depending on team role and surgical step. Aweb-based dashboard was developed, providing an integrated visualization of team cognitive processes in the OR that allows readers to intuitively interact with the study findings.
Conclusions
This study advances the current body of knowledge by making explicit relevant cognitive processes involved during the intraoperative phase of cardiac surgery from the perspective of multiple OR team members. By displaying the research findings in an interactive dashboard, we provide trainees with new knowledge in an innovative fashion that could be used to enhance learning outcomes. In addition, the approach used in the present study can be used to deeply understand the cognitive factors underlying surgical adverse events and errors in the OR.
Keywords: cardiac surgery, cognitive processes, cognitive task analysis, nontechnical skills
Patients undergoing cardiac surgery are inserted into a high-risk sociotechnical system that involves multiple specialized health professionals interacting with each other and with several technological devices to perform complex tasks. Contributing to the complexity of the cardiac surgery operating room (OR), patients often present multiple comorbidities and severe cardiovascular conditions, imposing significant challenges to the OR team.1,2 Despite a considerable improvement in safety and patient outcomes in the past 2 decades, the incidence of operative errors leading to adverse events among cardiac surgery patients continues to be high, with some studies reporting 12% of these patients presenting adverse events during hospitalization, compared to 3% among all surgical specialties.3 Importantly, these studies have found that more than half of surgical adverse events are preventable.4,5
Among the many factors that contribute to errors in surgery, there is a solid body of evidence showing that preventable surgical errors are often not related solely to knowledge and/or technical skills, but represent suboptimal performance in cognitive (eg, decision-making, situational awareness) and social (eg, teamwork, communication) nontechnical skills.6,7,8 At the individual surgeon level, cognitive factors, such as attention switching, cognitive load, and reasoning biases, are certainly relevant contributors of human errors in the OR that can lead to avoidable adverse events.9,10,11 Nonetheless, as a highly coordinated multiplayer endeavor, cardiac surgery relies on cognitive mechanisms that are better understood at a team level. In fact, previous research has employed the framework of “distributed cognition” which has the activity system (eg, coordination between different team members) as the unit of cognitive analysis rather than the individual, allowing the investigation of how cognitive resources and task demands are managed and distributed throughout the OR team.12 Despite playing a crucial role in team performance, the cognitive processes underlying the intraoperative phase of cardiac surgery are still not well understood.
Cognitive task analysis (CTA) is a structured mixed-methods approach from the behavioral sciences, used to capture the knowledge and cognitive processes that experts use to perform complex tasks, such as decision-making, problem-solving, and critical thinking.13 Previous literature has shown that experts, when describing routine activities, tend to skip certain procedural steps owing to the fact that many of these steps are performed in an automated way.14 This is especially true for complex and long procedures, such as cardiac surgery, where concurrent tasks are executed by multiple team members in a highly coordinated level. CTA allows for the elucidation of common cognitive processes, such as decision-making and critical communications, that are context-specific and form the basis for expertise, but are not easily measured using other approaches. Making these processes explicit may provide a unique opportunity for surgeons, trainees, and other surgical team members to enhance their learning experience, gaining a more comprehensive understanding of the surgical operation, beyond simple procedural task segmentation.15,16
The primary aim of this study was to elucidate the cognitive processes involved in surgical procedures from the perspective of different team roles: surgeon, anesthesiologist, and perfusionist. This provides a comprehensive compilation of intraoperative decision points, critical communications, pitfalls, problem-solving/prevention strategies, and cognitive demands related to operative surgery. A secondary aim was to present this comprehensive analysis in an interactive visual analytics dashboard for ease of interpretation and application. For this study, we chose coronary artery bypass grafting (CABG) procedures, as this is one of the most commonly performed major surgical procedures in the United States, with approximately 400,000 operations every year.17
METHODS
Study Setting and Participants
This study was carried out at the VA Boston Healthcare System (West Roxbury campus), a tertiary teaching hospital affiliated with Harvard Medical School, located in Boston, MA. A research protocol was approved by the local Institutional Review Board and all participants (patient and OR staff) completed an informed consent. One patient undergoing an On-Pump CABG procedure was included and the video recording of this procedure was used to create a series of video vignettes. A total of 9 expert OR team members: cardiac surgeons (n = 3), perfusionists (n = 3), and cardiac anesthesiologists (n = 3) elected to participate, with sample size selected based on previous studies indicating that 3 to 5 subject-matter experts are needed to complete a CTA protocol involving surgical procedures.15,16,17
Procedure
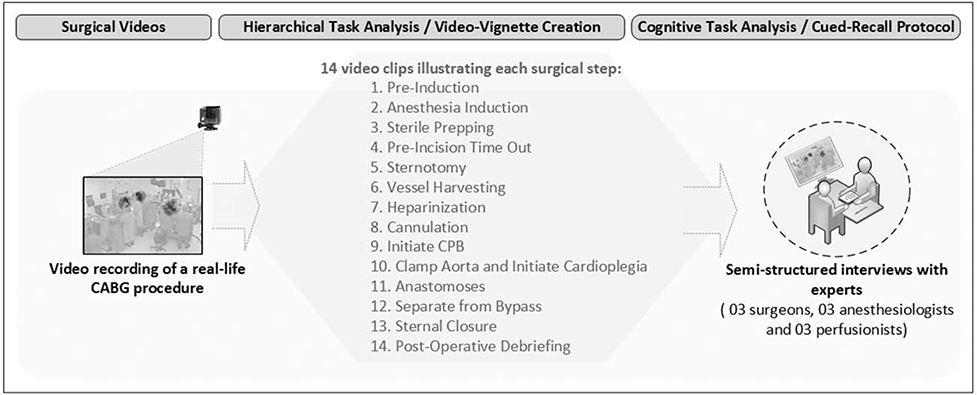
A summary workflow of the methodological approach and procedures carried out during this study is displayed in Figure 1.
FIGURE 1.
Methodological approach.
Video Recording and Editing Procedures
Two cameras (GoPro Hero 4) were set up with a wide and a narrow field of view to record audio and video of an entire CABG surgery from patient OR arrival until departure. As a result of a previous hierarchical task analysis (HTA),19,20 video of a CABG procedure was decomposed into 14 steps, including a total of 65 descendant substeps, covering the intraoperative phase from arrival of the patient into the OR until departure to ICU. Informed by this HTA, we edited the recording to create 14 video vignettes illustrating each CABG step. These video vignettes were used to develop a cued-recall protocol21 and to guide the semistructured interviews with subject-matter experts.
Cognitive Task Analysis
Previous research from our team on surgical process modeling20,22 has used HTA23 to decompose the intraoperative phase of CABG procedures into a 2-level hierarchical view, including surgical steps and substeps. Built upon this hierarchical segmentation, we appliedaCTAmethod24 inwhichahumanfactorsresearcherconducted in a private office individual semistructured interviews with subject-matter experts from different OR roles (surgeons, perfusionists, and anesthesiologists) to elucidate the cognitive processes involved during the intraoperative phase of CABG. The interviews with subject-matter experts were audio-recorded and used for analysis. To minimize recall bias and allow accurate capture of intraoperative cognitive processes during the CTA, we used a cued-recall protocol21 based on video vignettesrecordedfromareal-lifeprocedure.Avideovignetteisashort video clip that aims to trigger recall of events in a more effective way than only providing written or verbal cues to participants.25
During the semistructured interviews, each CABG step (with substeps) and its correspondent video vignette were displayed on a laptop monitor in sequence (step 1 through step 14) to each subject-matter expert, individually. After each CABG step, the interviewer asked a series of questions to explore 5 distinct intraoperative cognitive processes: decision-making, critical communications, pitfall identification, problem prevention/solving strategies, and perceived cognitive workload. These specific processes were chosen based on previous research that developed a universal framework to define and measure intraoperative performance, guiding behaviors in the OR.11 The authors of this study found that decision-making for both expected and unexpected intraoperative scenarios, coordination of operative steps and tasks (through team communication), and deviation from the expected course of the operation are the most relevant advanced cognitive skills which, in conjunction with other domains of intraoperative performance, are moderated by task complexity, mental workload, and knowledge integration.
To standardize the interview process and to guarantee that participants would identify and describe the specific cognitive processes that we intended to explore, we asked all interviewees the same questions to generate specific responses regarding each of the cognitive processes above for each surgical step in sequence. Step by step, we asked participants to “Identify and describe all moments in which you need to make a decision during this step” to explore decision points; “Identify and describe critical communications that occur during this step” to explore critical communications; “What problems may occur during this step?” to explore pitfalls; “What strategies do you use to solve and/or prevent problems during this step?” to explore problem prevention/solving strategies. The interviewer also used follow-up questions to explore the factors that are considered in each decision point (eg, “Which factors do you consider when making this decision?”) and which team members are involved in each critical communication (eg, “Who are the team members involved in this communication?”). Perceived cognitive workload was assessed by asking experts to report their usual mental demand (“How mentally demanding is this step for you?”), during each surgical step using a visual analogue scale from 1 (minimum demand) to 100 (maximum demand).
Data Analysis and Visualization Dashboard
A physician with expertise in human factors reviewed all interview recordings and created an extensive and inclusive list of intraoperative cognitive processes. All cognitive elements (decision points, critical communications, pitfalls, problem prevention/solving strategies, and perceived cognitive workload) mentioned by the interviewees were entered into a spreadsheet (Excel 2016). To maintain inclusivity, no selection process was used to filter responses, and all answers to the standardized interview questions were reported in the results. This is a common technique used by CTA methods to generate an inclusive and exhaustive list of cognitive elements.18 As we used a step-by-step interview workflow (step 1 through 14, in sequence), the cognitive elements reported by participants were already related to each surgical step. The number of interviewees (percentage from total) who mentioned each specific cognitive process was also reported.
To facilitate data visualization and exploring, we developed a web-based interactive dashboard that can be assessed online, allowing readers to interact with the study findings. For this purpose, we used a visual analytics software system (Tableau 2018.1) linked to a dataset stored in xlxs format (Excel 2016). The cognitive workload scores for each CABG step were averaged across each OR role and the entire OR team.
RESULTS
A total of 9 interviews were conducted with cardiac surgery subject-matter experts, generating a total of 16hours and 3 minutes of audio data. Subject-matter experts’ demographic characteristics are shown in Table 1.
TABLE 1.
Subject-Matter Experts’ Characteristics
| Surgeons | A nest hesiol ogists | Perfusionists | |
|---|---|---|---|
| (N = 3) | (N = 3) | (N = 3) | |
| Age, y | 56.3 | 43.0 | 45.7 |
| Sex (male/female) | 2/1 | 2/1 | 3/0 |
| Experience, y* | 23.7 | 9.3 | 19.0 |
| Number of CABGs* | 1967 | 700 | 1200 |
Since cardiac surgery training was completed.
The CTA based on cognitive interviews with subject-matter experts identified 137 unique surgical cognitive processes, including 33 decision points, 23 critical communications, 43 pitfalls, and 38 strategies. Table 2 shows the cognitive processes categorized according to each of the 14 CABG top-level steps. The percentage of subject-matter experts who mentioned a specific cognitive element during interviews (mentioning rate) is shown in eTable (supplemental material, http://links.lww.com/SLA/B708)). Interestingly, safety checklist “sign in” during Step 1—pre-induction was reported within 2 different cognitive processes: critical communication and problem prevention/solving strategy, as they appeared as answers to different questions: “Identify and describe critical communications that occurduring this step” and “What strategies do you use to solve/ prevent these problems,?”. In fact, communication during the safety checklist is critical and this is a recognized strategy to prevent errors in the OR.
TABLE 2.
Cognitive Processes During CABG Procedures
| Surgical Step | Decisions (D) | Critical Communications (C) | Pitfalls (P) | Strategies (S) |
|---|---|---|---|---|
| Step 1. Preinduction | D1. What type/size of cannulas will be used? D2. Will BIS and/or fNIRS monitors be used? D3. Will the radial artery be used? D4. Which cardioplegia cannulation and solution will be used? D5. Will the Swan-Ganz be used? D6. Which vein harvesting technique will be used? (open vs endoscopic) D7. Which drugs will be used for anesthesia? D8. Which antibiotics will be administered? |
Cl. Using safety checklist “sign in” | P1. Select wrong cannulas P2. Peifonn wrong procedure or in the wrong patient |
S1. Double check (verbally) cannula choices S2. Know in advance surgeon’s preference S3. Use safety checklist “sign in” S4. Know in advance the level of expertise from all team members |
| Step 2. Anesthesia induction | D9. Should the surgical team stay in the OR during induction? D10. In which moment should the surgical team be called if clinical deterioration during induction? D11. In case of arterial puncture during central line placement, should the surgeiy be cancelled? D12. Will TEE be used? |
C2. Managing patient with clinical deterioration during induction | P3. Clinical deterioration during induction P4. Equipment problems (eg, disconnected gas line, monitor cables not working) P5. Difficulty/complications during OTI, CL, and AL placement |
S5. Prime CPB and test system in advance S6. Use US-guided venous/ arterial catheterization |
| Step 3. Sterile prepping | C3. Setting up CPB lines | P6. Suction lines set up in reverse flow P7. Presence of air in the circuit P8. Sterile field contamination during lines set up or during TEE P9. Inappropriate patient positioning |
S7. Test circuit flow direction with saline S8. Remove bubbles from lines S9. Use closed-loop communication during lines set up S10. Use color code to connect lines S11. Use CPB checklist S12. Have a second perfusionist to help |
|
| Step 4. Preincision time out | D13. Does the patient need blood transfusion before surgery start? | C4. Using safety checklist (“time out”) C5. Running laboratory tests (Hb/Ht, platelets, gas, ACT) and calculating heparin dose |
P10. Blood products or special medications (eg, alternative anticoagulants) are not in the OR P11. Lines disconnection during bypass machine moving P12. Detect new findings during TEE |
S13.Repeat lab test if unexpected results S14. Re-check line connections S15.Use “time out” checklist S16.Use “crisis” checklist if needed S17.Check materials/equipment in advance |
| Step 5. Sternotomy | D14. Which tasks can be performed by the Surgical Fellow? D15. Does the patient need additional analgesia/sedation? |
C6. Stopping and restarting ventilation during sternotomy | P13. Problems with the saw (eg, battery, blade) P14. Accidental injuries involving adjacent vessels |
|
| Step 6. Vessel harvesting | D16. Are alternative conduits needed? D17. Can the perfusionist leave the OR? |
C7. Discussing quality of conduits and alternative options for harvesting | P15. Conduits do not present good quality P16. Injury the LIMA P17. Divide the LIMA before heparinization P18. Absorption of C02 during endoscopic vein harvest |
|
| Step 7. heparinization | D18. What is the ACT range to proceed with cannulation? D19. What should be done in case of heparin resistance? |
C8. Confirming heparin dose and heparin administration C9. Running subsequent ACT tests and reaching ACT target |
P19. Delay to take blood samples for ACT test after heparin administration P20. Heparin resistance P21. Proceeding to cannulation before ACT on target |
S18.Use a timer to monitor interval between ACT tests S19.Use “crisis” check list for heparin resistance S20.Check patient’s previous history (heparin use, interferences with ACT test) S21.Confirm ACT range safe for cannulation S22.Maintain pump sucker always prepared for use S23.Use closed-loop communication during heparinization S24.Write the target ACT and Heparin dose in the whiteboard S25.Clamp off cardiotomy reservoir until adequate ACT and lines are divided |
| Step 8. cannulation | D20. Which aorta site will be cannulated? | C10. Coordinating arterial and venous lines clamping C11. Managing patient’s blood pressure before cannulation |
P22. Patient presents hypotension during cannulation P23. Presence of air in cannulas/lines P24. Cannulas misplaced or coming out P25. Aorta dissection |
S26. Double check presence of air in cannulas/lines S27. Use closed-loop communication during lines clamping and blood pressure management |
| Step 9. initiate CPB | D21. Will retrograde autologous priming (RAP) be used? D22. Which hypothermia strategy will be used? D23. Does the patient need blood transfusion during RAP/CPB? D24. Will continuous positive airway pressure (CPAP) be used during CPB? |
Cl2. Initiating CPB Cl3. Managing temperature control |
P26. Hypotension during RAP and/or heart manipulation P27. CPB Full flow is not achieved P28. Ventilator is turned off earlier or later than expected P29. Low cerebral oxygen saturation |
S28.Having a second perfusionist during CPB initiation S29.Double check cannulas, lines and connections before CPB S30.Visually check the lungs for absence of ventilations S31.Keep ventilator turned on until perfusionist announces “full flow” |
| Step 10. Clamp aorta and deliver cardioplegia | D25. Which cardioplegia delivery strategy will be used? D26. Which aortic clamping technique will be used? |
Cl4. Managing CPB flow and cardioplegia delivery during cross-clamp Cl5. Delivering cardioplegia and confirming absence of electrical activity |
P30. Misplacement of aorta clamp P31. Ventricle distention caused by cardioplegia solution P32. Cardioplegic arrest is delayed or not achieved P33. Opened lines and/or connections |
S32.Test circuits and flow direction in advance S33.Ask other OR team members to be quiet during critical communications S34. Observe nonverbal cues that indicate next steps (eg, scrub nurse handling clamp to surgeon means that the next step is aorta clamping) |
| Step 11. Anastomoses | D27. Is an additional dose of cardioplegia needed? | Cl6. Managing CBP flow during removal of aorta cross clamp Cl7. Checking distal anastomoses for bleeding |
P34. Reduction in venous return due to heart manipulation P35. Excessive blood in the coronary arteries P36. Bleeding at distal anastomoses |
S35.Check vent lines S36.Use of blower-mister device |
| Step 12. Separate from bypass | D28. What is the best site for distal anastomoses? D29. Does the patient need blood transfusion? D30. When should CPB be terminated? D31. When protamine should be administered? D32. Does the patient need inotropic and/or vasoactive drugs? |
Cl8. Restarting ventilation and weaning from bypass Cl9. lerminating CPB C20. Administering protamine |
P37. Delay for restarting ventilation P38. Low cardiac output P39. Wrong protamine administration (dose and/or time) P40. Atrial or ventricular fibrillation P41. Lungs are not re-expanding P42. Protamine reaction |
S37. Closed-loop communication between surgeon, anaesthesiologist, and perfusionist |
| Step 13. Sternal closure | D33. Will blood volume collected in the cell saver be used? | C21. Confirming patient hemostasis C22. Verifying final sponge- sharp-instrument count |
P43. Patient bleeding | S38. Repeat ACT test and observe bleeding |
| Step 14. Postoperative debriefing | C23. Confirming procedure, complications, and review kev concerns for recovery | |||
ACT indicates activated clotting time; AI, arterial line; BIS, bispectral index monitor; CL, central line; CPB, cardiopulmonary bypass; fNIRS, functional near-infrared spectroscopy; Hb, hemoglobin; Ht, hematocrit; LIMA, left internal mammary artery; OTI, orotraqueal intubation; RAP, retrograde autologous priming; TEE, transesophageal echocardiography.
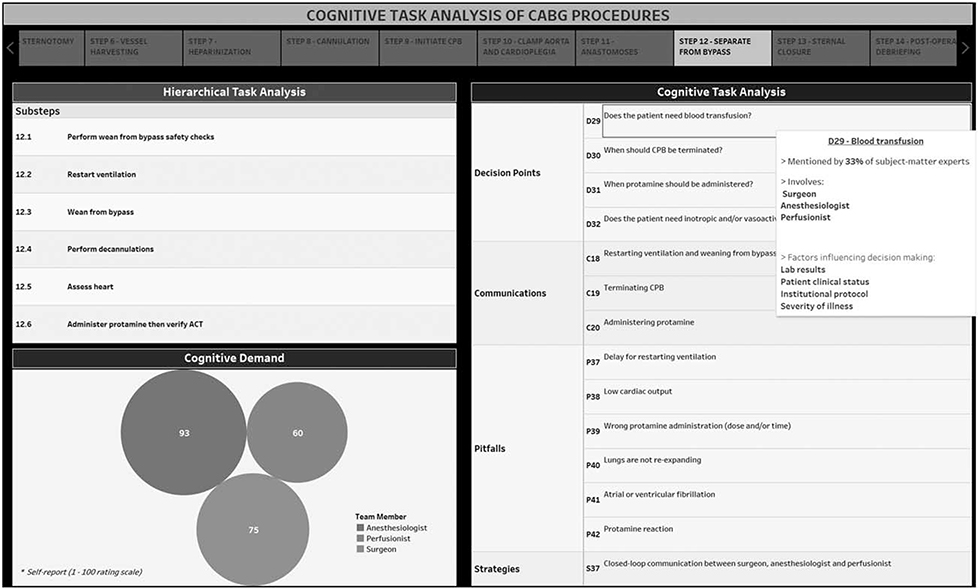
Perceived cognitive workload varied substantially, depending on OR role and surgical step. The CABG steps imposing the highest cognitive demand to the surgical team were: “separate from bypass,” “anastomoses,” and “cannulation”. The steps imposing the lowest cognitive demand were “Sterile Prepping” and “Sternotomy” (Figure 2).
FIGURE 2.
Self-reported cognitive load across different team members and CABG steps.
The interactive dashboard (https://public.tableau.com/profile/cognitus#!/vizhome/CognitiveTaskAnalysis-CABG/CTA) provides an integrated visualization of team cognitive processes in the OR. It presents specific decision points, critical communications, potential problems, and problem-solving/prevention strategies along with perceived cognitive workload for each of the 14 steps of CABG. The web-based application of this dashboard enables surgeons and educators to interact with the data and explore expert cognitive processes while navigating through the surgical workflow. By clicking on each element of the dashboard, additional information is displayed, including mentioning rate, which team members are usually involved in each process and, for decision points, which factors influence decision-making (Fig. 3).
FIGURE 3.
Web-based interactive dashboard for exploring intraoperative cognitive processes during CABG.
DISCUSSION
In the present study, we conducted a comprehensive cognitive task analysis to elucidate the cognitive processes involved during the intraoperative phase of CABG procedures, from the perspective of surgeons, anesthesiologists, and perfusionists. The study findings yield a compilation of decision points, critical communications, pitfalls, problem solving/prevention strategies and related cognitive demands for each of the 14 steps of CABG. Additionally, an online visual analytics dashboard was developed, displaying the hierarchical segmentation of the surgical operation into steps and substeps and allowing the reader to explore the data in an interactive way.
To our knowledge, this is the first study that explores, from a team perspective, both the hierarchical segmentation and the cognitive processes involved during the entire intraoperative phase of a complex surgical procedure. Previous research has used both hierarchical and cognitive task analysis to model surgical tasks and procedures, providing a framework upon which most of the current surgical teaching and assessment methodologies are built23,26,27. In fact, most of the current instructional designs predominant in surgical education provide specific step-by-step models to develop learners’ competence in surgical technical skills.23,27,28 Although the hierarchical nature of these models supports a high level view of task decompositions and provides detailed specifications of how surgeons should execute certain surgical steps, these models are often focused on developing surgeons’ psychomotor skills29,30 and do not thoroughly capture the variety of cognitive processes entailed during complex team-based surgical procedures.31,32 For instance, our results showed that the “separate from bypass” step, besides having 6 substeps, involves 5 decision points and 3 critical communications, imposing high cognitive demands for the entire team. The decision point related to when the CPB should be terminated was mentioned by 100% of the subject-matter-experts and involves surgeon, anesthesiologist, and perfusionist.
The findings of our study evidence the myriad of cognitive processes underpinning the practice of cardiac surgery, highlighting the high complexity and the crucial role of nontechnical skills, such as teamwork, interpersonal communication, and task management on optimal surgical performance. For instance, among the 38 strategies provided by experts to prevent or solve problems during CABG, closed-loop communication, use of checklists, and cross-checking were recurrent strategies reported in the CTA. The study findings can inform current surgical education initiatives toward incorporating these cognitive elements into the curriculum and competence assessment approaches in cardiac surgery. Moreover, as many of these cognitive elements are not unique for cardiac surgery, reflecting common human cognitive capabilities required for operative surgery, a similar framework can be used for thoroughly describing and understanding other surgical procedures, especially those involving complex team-based tasks.
As a preoperative teaching tool, our findings can be used to inform simulation-based curricula and scenario creation in cardiac surgery. The CABG process model (steps/substeps) and its specific cognitive processes can be used for monitoring performance, supporting decision-making, and identifying critical communications and their impact on surgical complications and patient outcomes.
In accordance with previous literature, our results show that self-reported cognitive workload is not uniformly distributed across distinct surgical steps and OR team roles. Different from these previous studies, we also described the decisions points, critical communications, and potential problems that are related to those varied levels of cognitive demand. During the “anastomoses” step, for example, surgeons reported the highest cognitive workload. This step requires a vast amount of attentional resources from surgeons and a potential problem that may occur is bleeding at distal anastomosis. However, anesthesiologists and perfusionist reported low to moderate workload during the “anastomosis” step. The same asymmetry on cognitive demand happens during the “induction” step in which anesthesiologists reported a high cognitive workload, with potential problems related to orotracheal intubation and central line placement, whereas surgeons and perfusionists reported low workload. Future research measuring cognitive workload in the surgical setting can use a similar approach to incorporate context-specific information into their measurement models. As there are multiple factors leading to cognitive overload and consequent performance deterioration during surgery, the elucidation of the underlying cognitive processes may provide additional insights for the development of mitigation and prevention strategies aiming to improve patient safety.33,34
Future initiatives can use this approach to review videos from surgical cases where adverse events occurred, and better understand the cognitive factors that contributed to errors in the OR. Current methods, such as root cause analysis, document review, and voluntary reporting systems are not able to capture these cognitive elements in a standardized and comprehensive manner.35,36 Surgical safety reviews of CABG procedures, for example, can investigate the cognitive processes involvedin a specific error or adverse event in the OR, based on the specific CABG step and cognitive elements, as informed by our findings.
The results of our study can also inform real-time strategies to improve patient safety in the OR. In fact, workflow segmentation through surgical process modeling and cognitive analysis of team-based tasks are being used to inform the design and development of intraoperative cognitive guidance systems, such as Smart checklists and decision support systems in the OR.20,37,38 By understanding the cognitive demands imposed by specific tasks on specific team members, technology-enabled guidance systems may offer clinical support tailored to specific task demands and OR roles.
Limitations
This study presents some limitations that are relevant for the interpretation of our results. First, the clinicians included in the interviews were from a single institution, limiting the generalizability of our findings. The subject-matter experts involved had many years of expertise, bringing experiences from other institutions, but future studies could include several institutions in the cognitive task analysis to replicate the findings here and potentially capture a wider range of practices that may vary across different hospitals. Although we captured expertise from multiple providers and different roles, nurses were not involved. They play an importantroleinthecardiacORandmaybringdifferentperspectivesfrom those already reported in our study so future studies should seek to include them.
Although the selection of the specificcognitive processes to be explored during the CTA was based on a previous framework, it is important to point out that there are other cognitive processes that also play an important role in surgery, such as psychomotor skills, situational awareness, and stress management.11 Future studies can further explore these other processes.
A limitation related to the CTA method of including all mentioned cognitive elements (inclusive and exhaustive list) is the fact that some processes were mentioned by only 1 expert (11%), whereas other elements were mentioned by all experts (100%) and, therefore, they may not be equally relevant to the specific surgical step under which they were reported.
Another limitation is the fact that the anesthesiologists included in the interview protocol were less experienced than perfusionists and surgeons, and it may have influenced their self-reported cognitive demands. The difference in cognitive demands across team members reported in our study may not be role-dependent. Future studies should continue including a heterogeneous sample of participants, as a wide range of experience levels will enrich study findings with different perspectives and enhance ecological validity. However, it is important to ensure that this heterogeneity in experience is not cofounded with role.
Novelty
A novel aspect of our study involved the use of video vignettes created from real-life cardiac surgeries, facilitating experts’ recall and allowing a deeper exploration of clinicians’ cognitive processes compared to traditional CTA methods. Recent research has suggested use of operative videos as a key component of surgical quality improvement.39 Another innovative aspect is the interactive online dashboard, which enables the reader to navigate through the study findings using an integrative and fluid interface, opening access to the results of our research for broad application.
CONCLUSIONS
This study advances the current body of knowledge by elucidating, for the first time, 137 relevant cognitive processes involved during the intraoperative phase of cardiac surgery from the perspective of multiple OR team members. By displaying the research findings in an interactive dashboard, we provide trainees with new knowledge in an innovative fashion that could be used to enhance learning outcomes. In addition, the approach used in the present study can be used to deeply understand the cognitive factors underlying surgical adverse events and errors in the OR, contributing to the development of mitigation and prevention strategies toward improving surgical patient safety.
Supplementary Material
Acknowledgments
This study was funded by the National Heart, Lung, and Blood Institute (NHLBI) of the National Institutes of Health under award 1R01HL126896-01A1. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies.
Footnotes
The authors report no conflict of interests.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Wahr JA, Prager RL, Abernathy JH 3rd, et al. Patient safety in the cardiacoperating room: human factors and teamwork: a scientific statement from the American Heart Association. Circulation. 2013;128:1139–1169. [DOI] [PubMed] [Google Scholar]
- 2.Sanchez JA, Ferdinand FD, Fann JI. Patient safety science in cardiothoracicsurgery: an overview. Ann Thorac Surg. 2016;101:426–433. [DOI] [PubMed] [Google Scholar]
- 3.Gawande AA, Thomas EJ, Zinner MJ, et al. The incidence and nature ofsurgicaladverseeventsinColoradoandUtahin1992.Surgery.1999;126:66–75. [DOI] [PubMed] [Google Scholar]
- 4.Martinez EA, Shore A, Colantuoni E, et al. Cardiac surgeryerrors: results fromthe UK National Reporting and Learning System. Int J Qual Health Care. 2011;23:151–158. [DOI] [PubMed] [Google Scholar]
- 5.Gurses AP, Kim G, Martinez EA, et al. Identifying and categorising patientsafety hazards in cardiovascular operating rooms using an interdisciplinary approach: a multisite study. BMJ Qual Saf. 2012;21:810–818. [DOI] [PubMed] [Google Scholar]
- 6.Flin R, Youngson GG, Yule S. Enhancing Surgical Performance: A Primer in Non-Technical Skills. CRC Press; 2015, Available at: https://market.android.com/details?id=book-HhUqCgAAQBAJ. [Google Scholar]
- 7.Gawande AA, Zinner MJ, Studdert DM, et al. Analysis of errors reported bysurgeons at three teaching hospitals. Surgery. 2003;133:614–621. [DOI] [PubMed] [Google Scholar]
- 8.Christian CK, Gustafson ML, Roth EM, et al. A prospective study of patientsafety in the operating room. Surgery. 2006;139:159–173. [DOI] [PubMed] [Google Scholar]
- 9.Zhang J, Patel VL, Johnson TR, et al. A cognitive taxonomy of medical errors.J Biomed Inform. 2004;37:193–204. [DOI] [PubMed] [Google Scholar]
- 10.Boquet AJ, Cohen TN, Reeves ST, et al. Flow disruptions impacting thesurgeon during cardiac surgery: defining the boundaries of the error space. Perioperative Care and Operating Room Management. 2017;7:1–6. [Google Scholar]
- 11.Madani A, Vassiliou MC, Watanabe Y. What are the principles that guidebehaviors in the operating room? Ann Surg. 2016;265:255–267. [DOI] [PubMed] [Google Scholar]
- 12.Hazlehurst B, McMullen CK, Gorman PN. Distributed cognition in the heartroom: how situation awareness arises from coordinated communications during cardiac surgery. J Biomed Inform. 2007;40:539–551. [DOI] [PubMed] [Google Scholar]
- 13.Salvendy G Handbook of Human Factors and Ergonomics. John Wiley & Sons; 2012, Available at: https://market.android.com/details?id=bookWxJVNLzvRVUC. [Google Scholar]
- 14.Hoffman RR, Shadbolt NR, Mike Burton A, et al. Eliciting knowledge fromexperts: a methodological analysis. Organ Behav Hum Decis Process. 1995;62:129–158. doi: 10.1006/obhd.1995.1039. [DOI] [Google Scholar]
- 15.Sullivan ME, Ortega A, Wasserberg N, et al. Assessing the teaching ofprocedural skills: can cognitive task analysis add to our traditional teaching methods? Am J Surg. 2008;195:20–23. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan ME, Yates KA, Inaba K, et al. The use of cognitive task analysis toreveal the instructional limitations of experts in the teaching of procedural skills. Acad Med. 2014;89:811–816. [DOI] [PubMed] [Google Scholar]
- 17.Alexander JH, Smith PK. Coronary-artery bypass grafting. N Engl J Med. 2016;374:1954–1964. [DOI] [PubMed] [Google Scholar]
- 18.Smink DS, Peyre SE, Soybel DI, et al. Utilization of a cognitive task analysisfor laparoscopic appendectomy to identify differentiated intraoperative teaching objectives. Am J Surg. 2012;203:540–545. [DOI] [PubMed] [Google Scholar]
- 19.Dias RD, Osterweil LJ, Riccardi G, et al. Development of an interactivedashboard to analyze cognitive workload of surgical teams during complex procedural care. IEEE Int Interdiscip Conf Cogn Methods Situat Aware Decis Support. 2018;2018:77–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Avrunin GS, Clarke LA, Osterweil LJ, et al. Experience modeling andanalyzing medical processes. In: Proceedings of the, ACM., International Conference on Health Informatics—IHI., ‘10., 2010., doi: 10.1145/1882992.1883037. [DOI] [Google Scholar]
- 21.White MR, Braund H, Howes D, et al. Getting inside the expert’s head: ananalysis of physician cognitive processes during trauma resuscitations. Ann Emerg Med. 2018;72:289–298. [DOI] [PubMed] [Google Scholar]
- 22.Avrunin GS, Clarke LA, Conboy HM, et al. Toward improving surgicaloutcomes by incorporating cognitive load measurement into process-driven guidance. Softw Eng Healthc Syst SEHS IEEE ACM Int Workshop. 2018;2018:2–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sarker SK, Chang A, Albrani T, et al. Constructing hierarchical task analysis insurgery. Surg Endosc. 2007;22:107–111. [DOI] [PubMed] [Google Scholar]
- 24.Clark R Cognitive task analysis for expert-based instruction in healthcare. In: In: Handbook of Research on Educational Communications and Technology; 2013. 541–551. [Google Scholar]
- 25.Hurtubise L, Martin B, Gilliland A, et al. To play or not to play: leveraging video in medical education. J Grad Med Educ. 2013;5: 13–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wingfield LR, Kulendran M, Chow A, et al. Cognitive task analysis: bringing olympic athlete style training to surgical education. Surg Innov. 2015;22:406–417. [DOI] [PubMed] [Google Scholar]
- 27.Clark RE, Pugh CM, Yates KA, et al. The use of cognitive task analysis toimprove instructional descriptions of procedures. J Surg Res. 2012;173: e37–e42. [DOI] [PubMed] [Google Scholar]
- 28.Nazari T, Vlieger EJ, Dankbaar MEW, et al. Creation of a universal languagefor surgical procedures using the step-by-step framework. BJS Open. 2018;2:151–157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yeung C, McMillan C, Saun TJ, et al. Developing cognitive task analysisbased educational videos for basic surgical skills in plastic surgery. J Surg Educ. 2017;74:889–897. [DOI] [PubMed] [Google Scholar]
- 30.Hashimoto DA, Axelsson CG, Jones CB, et al. Surgical procedural mapscoring for decision-making in laparoscopic cholecystectomy. Am J Surg. 2019;217:356–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moorthy K Objective assessment of technical skills in surgery. BMJ. 2003;327:1032–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sarker SK, Hutchinson R, Chang A, et al. Self-appraisal hierarchical taskanalysis of laparoscopic surgery performed by expert surgeons. Surg Endosc. 2006;20:636–640. [DOI] [PubMed] [Google Scholar]
- 33.Thiels CA, Lal TM, Nienow JM, et al. Surgical never events and contributinghuman factors. Surgery. 2015;158:515–521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cohen, Tara N, Sarah E, et al. Using HFACS-healthcare to identify systemicvulnerabilities during surgery. Am J Med Qual. 2018;33:614–622. [DOI] [PubMed] [Google Scholar]
- 35.Website. Institute of Medicine (US) Committee on Data Standards for PatientSafety; Aspden P, Corrigan JM, Wolcott J, et al. , editors. Patient Safety: Achieving a New Standard for Care. Washington (DC): National Academies Press (US); 2004. 6, Adverse Event Analysis. Available at: https://www.ncbi.nlm.nih.gov/books/NBK216102/. Accessed February 7, 2019. [PubMed] [Google Scholar]
- 36.Chung KC, Kotsis SV. Complications in surgery. Plast Reconstr Surg. 2012;129:1421–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jalote-Parmar A, Badke-Schaub P, Ali W, et al. Cognitive processes asintegrative component for developing expert decision-making systems: a workflow centered framework. J Biomed Inform. 2010;43:60–74. [DOI] [PubMed] [Google Scholar]
- 38.Tarola CL, Hirji S, Yule S, et al. Cognitive support to promote shared mentalmodels during safety-critical situations in cardiac surgery. 2018 IEEE Conf Cogn Comput Asp Situat Manag CogSIMA (2018). 2018;2018:165–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dimick JB, Scott JW. Avideo is worth a thousand operative notes. JAMA Surg. 2019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.