Abstract
Emerging evidence suggests that patients with coronavirus disease 2019 (COVID-19) are at risk of thromboembolic complications, including ischemic strokes. We present a case illustrating the value of CT perfusion to identify acute small subcortical infarcts in a patient with COVID-19 admitted to an intensive care unit for bilateral pneumonia and pulmonary embolism presenting with sudden right limb weakness.
Keywords: Thalamic stroke, COVID-19, CT perfusion, Perforating artery stroke
Case presentation
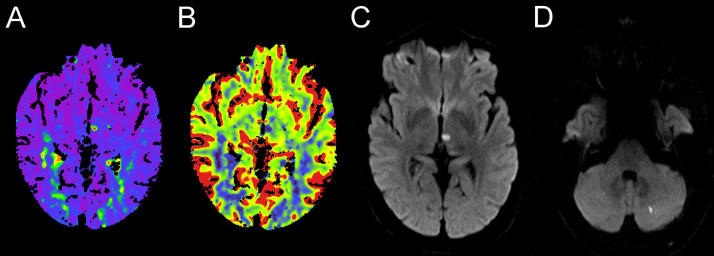
A previously healthy 50-year-old man was admitted to an intensive care unit (ICU) for COVID-19 with bilateral pneumonia that required non-invasive ventilation and vasoactive assistance. Pharmacologic therapy included hydroxychloroquine, antiretrovirals, wide spectrum antibiotics and prophylactic anticoagulation with low dose molecular weight heparin, which was discontinued despite having subsegmental pulmonary embolism on chest CT-angiogram due to severe upper gastrointestinal bleeding. Two days later the patient had sudden right facial palsy with mild ipsilateral limb weakness, and the stroke code protocol was activated. Neither nonenhanced CT nor CT-angiography showed acute ischemic lesions or proximal vascular occlusions. The perfusion maps showed a small focal hypoperfusion in the paramedian perforating vascular territory supplying the left medial thalamus (Figure 1 A and B). This acute ischemic lesion was confirmed in a 1.5T brain MRI study acquired 48 hours later, which also showed other 2 punctate acute ischemic lesions in each cerebellar hemisphere (Figure 1C and D). Intravenous thrombolysis was contraindicated due to the recent digestive bleeding, but considering the high thromboembolic risk in a patient with recent pulmonary embolism and ischemic stroke, anticoagulation therapeutic doses of unfractionated heparin were initiated, and an inferior vena cava filter was placed. The patient recovered from neurological deficits within 24 hours.
Figure 1.
CT perfusion maps show a typical pattern of hypoperfusion the left paramedian thalamic artery characterized by a focal delay in time to drain maps (A) and a decreased cerebral blood flow (B). The MRI at 24 hours confirmed in the diffusion-weighted imaging a small ischemic lesion in the corresponding thalamic area (C) and showed other 2 small ischemic lesions in bilateral posterior inferior cerebellar artery territories (D).
Discussion
Patients presenting with focal neurological deficits on ICUs often lack a thorough neurological examination, and stroke mimics are more difficult to rule out in such complex patients. Different neurological complications such as encephalopathy, seizures, and stroke have been recently reported in patients with COVID-19.1 Patients with severe COVID-19 infection present a deep proinflammatory state and endothelial dysfunction leading to hypercoagulability and thromboembolic complications, including stroke.2 Recent small series of patients with severe COVID-19 infection reported different radiological patterns in patients with ischemic stroke, including large vessel occlusions and small cortical infarcts.1 , 3, 4, 5 However, occlusions in the territories of deep perforating arteries have not been described before to our knowledge. The incidence of such small infarcts may be underestimated in patients with complex management in ICUs.
CT perfusion studies not only provide an estimation of viable and damaged tissue in the ischemic tissue,6 but also may unmask distal or deep perforating artery occlusions despite normal findings on nonenhanced CT and CT-angiography,7 or show non-vascular perfusion patterns suggesting stroke mimics.8 This case illustrates the value of CT perfusion to identify an acute ischemic stroke in a patient with COVID-19 and normal nonenhanced CT and CT-angiography. The finding on MRI of multiple ischemic lesions within distant arterial territories suggests a thromboembolic etiology or a prothrombotic state rather than atherosclerotic small vessel disease.9 Anticoagulant therapy has been recommended in such patients with a pro-thrombotic state,2 but its efficacy in non-critical patients should be tested in randomized trials.
In conclusion, CT perfusion studies may be useful to identify small ischemic lesions and assist physicians in the early therapeutic management including intensive care in patients with suspected stroke and COVID-19. The incidence and pathophysiology of stroke in patients with COVID-19 should be investigated in large prospective cohorts.
Declaration of Competing Interest
None
Acknowledgments
Acknowledgment
We thank all the health care workers at Hospital Clínic for the great efforts during COVID-19 pandemic.
Funding
SR receives funding from the Institute of Health Carlos III, with a Grant for Health Research (CM18/00116).
Footnotes
This work was performed in: Department of Neurology, Hospital Clínic, Barcelona.
References
- 1.Mao L., Jin H., Wang M. Neurologic Manifestations of Hospitalized Patients With Coronavirus Disease 2019 in Wuhan, China. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.1127. [published online ahead of print, 2020 Apr 10] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hess D.C., Eldahshan W., Rutkowski E. COVID-19-Related Stroke. Transl Stroke Res. 2020:1–4. doi: 10.1007/s12975-020-00818-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Helms J., Kremer S., Merdji H., Clere-Jehl R., Schenck M., Kummerlen C. Neurologic Features in Severe SARS-CoV-2 Infection. N Eng J Med. 2020 doi: 10.1056/NEJMc2008597. NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Avula A., Nalleballe K., Narula N. Brain Behav Immun. 2020 doi: 10.1016/j.bbi.2020.04.077. S0889-1591(20)30685-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oxley T.J., Mocco J., Majidi S. Large-Vessel Stroke as a Presenting Feature of Covid-19 in the Young. N Engl J Med. 2020 doi: 10.1056/NEJMc2009787. NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Konstas A.A., Goldmakher G.V., Lee T.Y., Lev M.H. Theoretic basis and technical implementations of CT perfusion in acute ischemic stroke, part 2: technical implementations. AJNR Am J Neuroradiol. 2009;30(5):885–892. doi: 10.3174/ajnr.A1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rudilosso S., Urra X., San Román L. Perfusion Deficits and Mismatch in Patients with Acute Lacunar Infarcts Studied with Whole-Brain CT Perfusion. AJNR Am J Neuroradiol. 2015;36(8):1407–1412. doi: 10.3174/ajnr.A4303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Cauwenberge M.G.A., Dekeyzer S., Nikoubashman O., Dafotakis M., Wiesmann M. Can perfusion CT unmask postictal stroke mimics? A case-control study of 133 patients. Neurology. 2018;91(20):e1918–e1927. doi: 10.1212/WNL.0000000000006501. [DOI] [PubMed] [Google Scholar]
- 9.Regenhardt R.W., Das A.S., Lo E.H., Caplan L.R. Advances in Understanding the Pathophysiology of Lacunar Stroke: A Review. JAMA Neurol. 2018;75(10):1273–1281. doi: 10.1001/jamaneurol.2018.1073. [DOI] [PMC free article] [PubMed] [Google Scholar]