Hospitals around the world are ramping up their services to accommodate patients infected with severe acute respiratory distress syndrome coronavirus 2 (SARS-CoV-2). Although healthcare workers (HCW) are at significant risk for infection with SARS-CoV-2, the deficit of personal protective equipment (PPE) to protect HCWs from infection has been a major recurring concern. Recommendations for the use of personal protective equipment to protect against SARS-CoV-2 exposure by HCWs were recently published by the World Health Organization and the US Centers for Disease Control and Prevention. For aerosol-generating procedure, N95 respirators, eye protection, isolation gowns, and gloves were recommended. Coveralls, boots with a cover, and hair coverings were not part of the recommended protective clothing [1].
The World Health Organization (WHO) has classified cardiopulmonary resuscitation (CPR) as an aerosol-generating procedure [2]. The center for disease control (CDC) along with American Heart Association (AHA) has issued recommendations for CPR, endotracheal intubation, and noninvasive ventilation to minimize aerosol generation and protect the HCW [3]. Some of these recommendations especially for CPR include holding chest compression during intubation and trying to establish airway early in the resuscitation to minimize aerosol generation. Barrier enclosures have been previously described to minimize contamination of HCW during aerosol generating procedures [4]. However, no such modality has been described to protect HCWs while performing CPR. Here we describe a model to lower contamination by aerosol of HCWs during simulated CPR.
1. Method
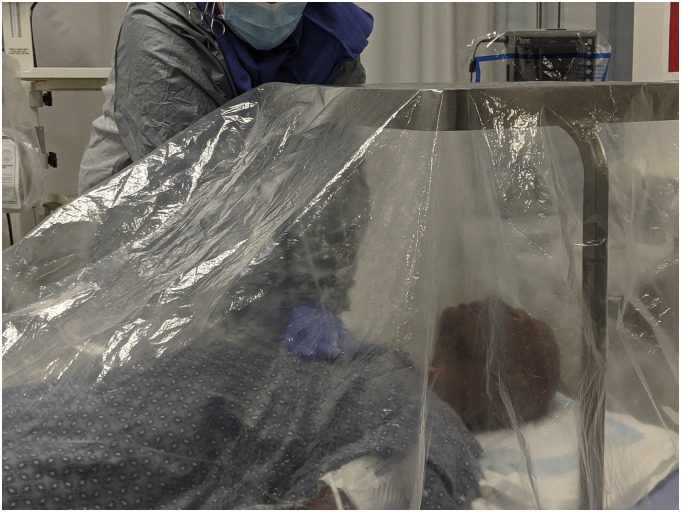
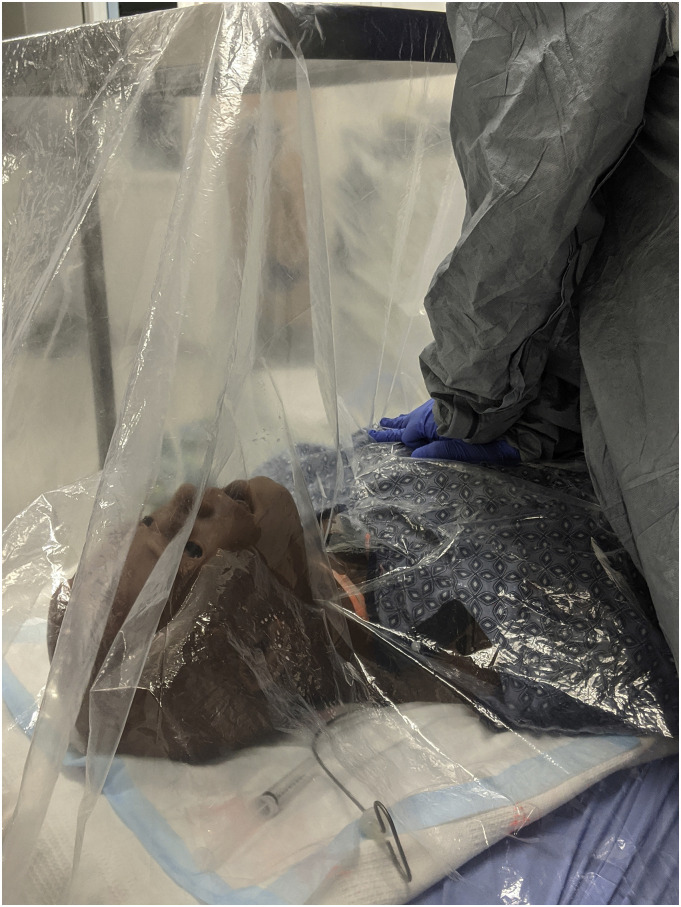
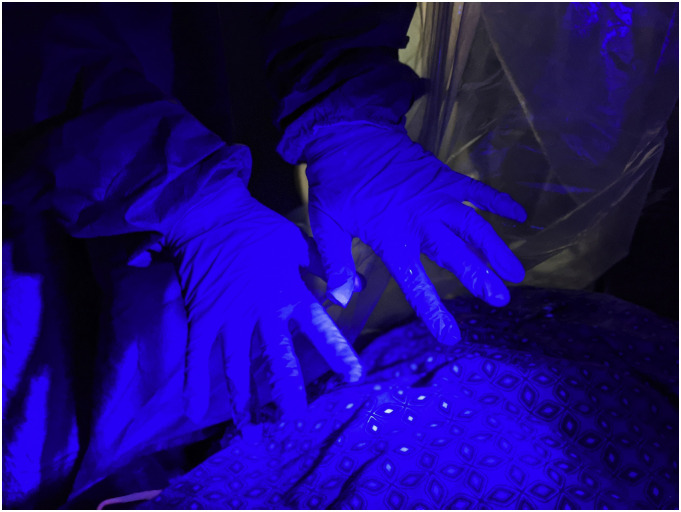
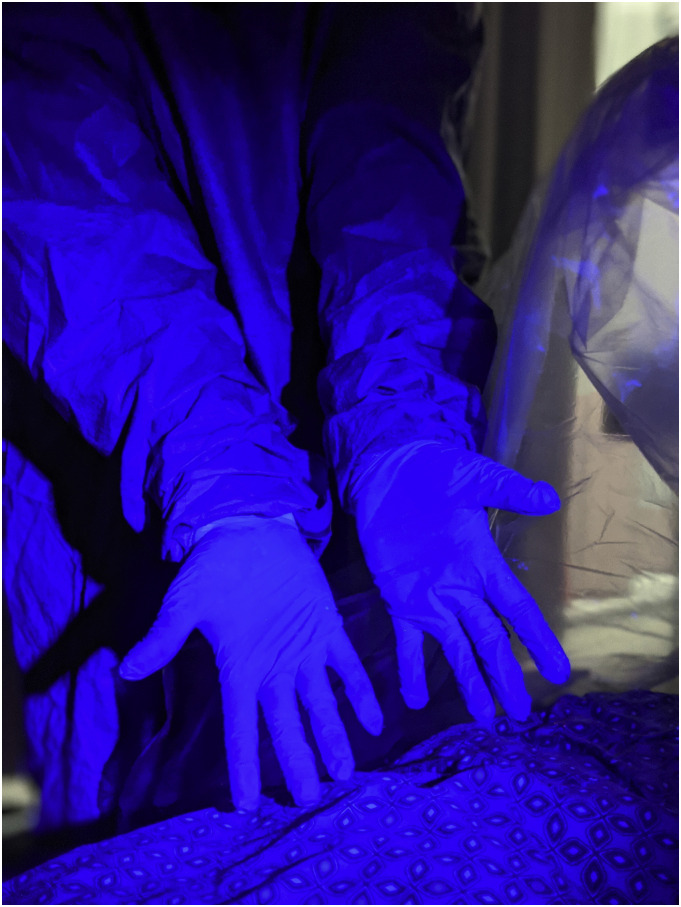
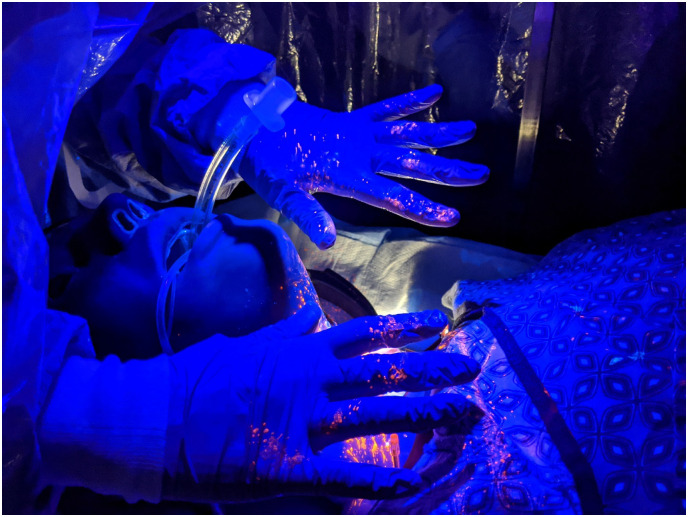
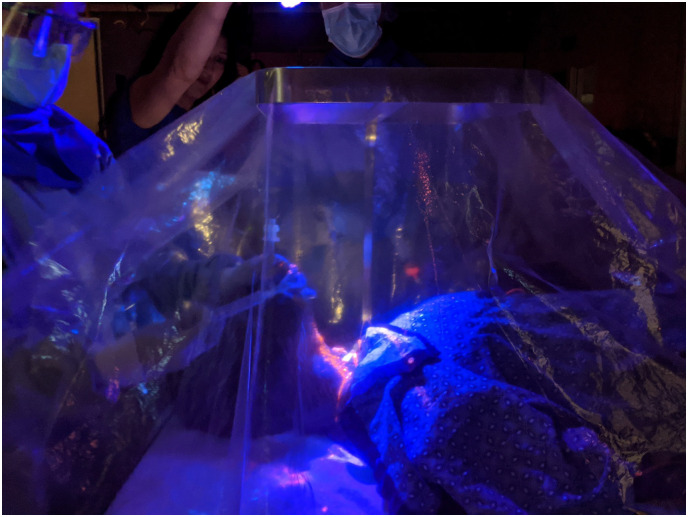
The barrier used is Mayo stand with transparent plastic sheet. We used clear plastic shower liner (70 inchin. x 72 in.) covering the simulated patient. We pulled the mayo stand as shown in figure over the head of the patient, adjusted the height of the stand, and covered it with the plastic sheet to fully enclose the mouth and face of the patient before we started the CPR. In our simulation, the person performing chest compression was stationed to the right side of the manikin ‘victim’ who is not intubated. The model simulates the beginning of cardiac arrest resuscitation before a definitive airway is established. The HCW performing chest compression is donned in appropriate PPE as per CDC guidelines. Glow germ™ was used to simulate aerosols during the CPR.
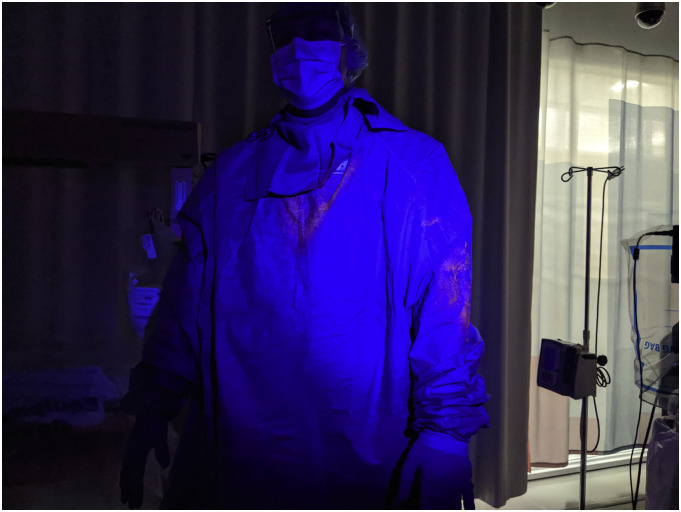
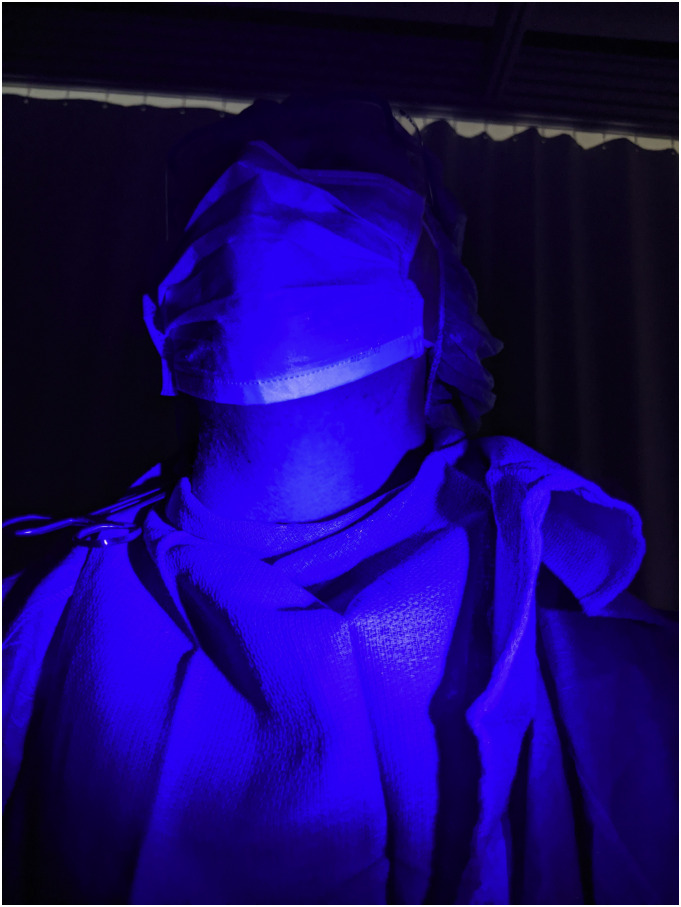
We performed this simulation with and without barrier and took photographs of HCW illuminated by ultraviolet light to assess the visible level of contamination with the fluorescent aerosolized particles.
2. Results
UV light illuminated images below demonstrate exposure to HCW using complete PPE as per CDC and WHO guidelines with and without the barrier described previously. Fig. 1 : Draped Mayo stand barrier during CPR. Fig. 2 shows barrier stand and HCW performing CPR with barrier sheet on to decrease contamination from any generated aerosol. Fig. 3, Fig. 4, Fig. 5, Fig. 6 show dispersion of aerosols on the PPE of the HCW performing CPR without barrier enclosure. Fig. 7, Fig. 8 show minimal contamination of HCW with aerosols when barrier stand and cover were used during CPR.
Fig. 1.
Mayo stand with plastic drape decreasing aersol exposure to HCW performing CPR.
Fig. 2.
Mayo stand with plastic drape decreasing aersol exposure to HCW performing CPR.
Fig. 3.
Dispersion of aerosols on the PPE of the HCW performing CPR without barrier enclosure.
Fig. 4.
Dispersion of aerosols on the PPE of the HCW performing CPR without barrier enclosure.
Fig. 5.
Dispersion of aerosols on the PPE of the HCW performing CPR without barrier enclosure.
Fig. 6.
Dispersion of aerosols on the PPE of the HCW performing CPR without barrier enclosure.
Fig. 7.
Minimal contamination of HCW with aerosols when barrier stand and cover were used during CPR.
Fig. 8.
Minimal contamination of HCW with aerosols when barrier stand and cover were used during CPR.
3. Discussion
Despite personal protective equipment, fluorescent markers were found on the uncovered areas of neck, skin and hair of the HCW providing resuscitation to a simulated SARS-CoV-2 patient without barrier enclosure. The findings suggest that the current recommendations for personal protective equipment may not fully prevent exposures while performing CPR. Clothing that covers all skin and hair may further diminish exposure risk.
However using a simple barrier stand with barrier sheet can significantly decrease aerosol dispersion in the air and onto the healthcare workers, potentially better protecting them from significant exposure.
Inhalation of aerosols and exposure risks associated with doffing were not evaluated. The simulated healthcare setting and the surrogate measures of exposure are the primary limitations. Because this was a mannikin simulation, it is uncertain how the results may translate to actual patient care.
ADDENDUM
The barrier enclosure mentioned in our publication, using mayo stand and plastic sheet, can also be used to assist health care workers (HCW) during manual bagging and intubation along with CPR. We performed simulation with HCW performing intubation using video laryngoscopy initially without the barrier enclosure and later with the barrier enclosure as mentioned. The HCW performing chest compression is done in appropriate PPE as per CDC guidelines. Glo germ ™ was used to simulate aerosols during the intubation
.
Additional images attached. Image 10 showing aerosol dispersion on HCW post intubation using video laryngoscopy without using our barrier enclosure. Fig 11 shows HCW performing intubation using barrier enclosure and Fig 12 shows aerosol dispersion post intubation limited to hands pf HCW but protecting them otherwise.
Our novel technique of stand and sheet can thus be used for intubation and chest compression while protecting HCW from significant aerosol exposure.
In addition we want to add the attached 3 photos
.
References
- 1.World Health Organization . 2020. Rational use of Personal Protective Equipment for Coronavirus Disease 2019 (COVID-19). Published February 27. Accessed March 21, 2020. https://apps.who.int/iris/bitstream/handle/10665/331215/WHO-2019-nCov-IPCPPE_use-2020.1-eng.pdf. [Google Scholar]
- 2.Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. World Health Organization (WHO); 2020. website. https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations. Published March 29, 2020. Accessed April 3. [Google Scholar]
- 3.Coronavirus Disease 2019 (COVID-19): Interim Infection Prevention and Control Recommendations for Patients with Suspected or Confirmed Coronavirus Disease 2019 (COVID-19) in Healthcare Settings. Centers for Disease Control and Prevention (CDC); 2020. website. https://www.cdc.gov/coronavirus/2019-ncov/infection-control/control-recommendations.html. Last reviewed April 1, 2020. Accessed April 3. [Google Scholar]
- 4.Canelli R., Connor C.W., Gonzalez M., Nozari A., Ortega R. Barrier enclosure during endotracheal intubation [published online ahead of print, 2020 Apr 3] N Engl J Med. 2020 doi: 10.1056/NEJMc2007589. (NEJMc2007589) [DOI] [PMC free article] [PubMed] [Google Scholar]