Abstract
This paper extends the growing research on the impact of gender equity on public health outcomes using the ongoing Covid-19 pandemic as its research setting. Specifically, it introduces a conceptual model incorporating the impact of gender equity and human development on women’s representation in legislature and public health expenditure, and their combined impact with human environment (population density, aging population and urban population) on important public health outcomes in the Covid-19 context, including the total number of tests, diagnosed, active and critical cases, and deaths. Data from 210 countries shows support for many of the hypothesized relationships in the conceptual model. The results provide useful insights about the factors that influence the representation of women in political systems around the world and its impact on public health outcomes. The authors also discuss implications for public health policy-makers to ensure efficient and effective delivery of public health services in future.
Keywords: Covid-19, Gender equity, Human development, Human environment, Public health expenditure, Public health outcomes
1. Introduction
The unprecedented devastation caused by the ongoing Covid-19 pandemic has aroused public attention on the need for a proper public health policy (Herper, 2020, King, 2020), especially due to the disproportionately large number of infected cases and deaths in the developed countries, led by the United States, followed by Spain, Italy, France, Germany, the United Kingdom and others (Worldometers, 2020). As the debates continue to fix the responsibility for the birth and spread of this deadly virus and the lack of readiness to handle its disastrous impact (Patterson, 2020, Qato, 2020, Smakaj, 2020), public health experts seem to mainly view it through the lens of medicine, epidemiology, and health science disciplines. However, public health is an interdisciplinary subject that involves social sciences, public policy, public education, economics, and management (Jambroes et al., 2014, Tulchinsky and Varavikova, 2014). Hence, a failure to have a proper public health policy may not only lead to a huge loss of human lives; it can also shatter the economy, expose the incompetence of the public bodies including the governments and political leaders, and weaken the confidence of the general public (United Nation, 2020).
In this context, gender equity is recognized as an important factor to influence the quality of public healthcare systems and their outcomes (WHO, 2017). Although women are underrepresented in leadership positions in healthcare, their significance in other leadership positions cannot be underestimated, as evident from the growing numbers of women CEOs, politicians, and heads of governments (Mayer & Oosthuizen, 2020). Women leaders are strong advocates for immunization programs, education and equal employment opportunities (Beaman, Duflo, Pande, & Topalova, 2012). Women senators lobbied for the Breast and Cervical Cancer Mortality Prevention Act in the US (Lee et al., 2014). Gender equity also has positive effects on firm performance and governance (Post & Byron, 2015).
This paper extends the growing research on the impact of gender equity by exploring its impact on public health outcomes using the ongoing Covid-19 pandemic as its research setting. The authors begin with an extensive review of the relevant literature to develop a conceptual model and specific hypotheses about the impact of gender equity and human development on women’s representation in legislature and public health expenditure, and the combined impact of public health expenditure along with human environment (population density, aging population and urban population) on important public health outcomes in the Covid-19 context, including the total number of tests, diagnosed, active and critical cases, and deaths. The authors use the data from 210 countries to find support for many hypotheses. The results provide useful insights about the factors that influence the representation of women in political systems around the world and its impact on public health outcomes. The authors also discuss implications for public health policy-makers to ensure efficient and effective delivery of public health services in future.
2. Conceptual background and hypotheses
2.1. Public health
Winslow (1920; p. 30) defines public health as “the science and art of preventing disease, prolonging life, and promoting physical health and efficiency through organized efforts for the sanitation of the environment, the control of community infections, the education of the individual in principles of personal hygiene, the organization of medical and nursing service for the early diagnosis and preventive treatment of disease, and the development of the social machinery which will ensure to every individual in the community a standard of living adequate for the maintenance of health”. In other words, public health is not just about medical science of epidemiology, diagnosis, and cure, and it is also linked to social science, which includes politics, management, welfare, and public policy.
2.2. Public health and gender equity
Past research shows significant psychological and cognitive differences in personality, values, and concerns between women and men. For example, women tend to be more cautious (Lundeberg, Fox, & Punćochaŕ, 1994), risk-averse (Agnew et al., 2008, Byrnes et al., 1999), and fatalistic (Pandey & Jain, 2017) than men. Women put more emphasis on risk attributes (e.g., possibility of loss) in investment decisions than men (Olsen & Cox, 2001) and perceive more risk in traffic and environmental hazards (Dejoy, 1992, Fllyn et al., 1994). Besides being risk averse, women are also loss averse (Brooks & Zank, 2005). In addition, there is a difference in risk-taking behavior between female and make leaders for the decisions making for themselves and their groups. Ertac and Gurdal (2012) show male leaders take more risk for the decisions made for their own and the groups than male non-leaders. On the contrary, female leaders take less risk on behalf of a group which is lower than that taken individually. These differences in over-confidence and risk aversion levels between females and males make females to be more cautious and take less risk in making decisions. Hence, the authors hypothesize as follows:
H1
Gender equity has a positive effect on, (a) representation of women in legislature, and (b) public health expenditure.
2.3. Public health and human development
Past research shows that public health outcomes are influenced by indicators of human development, such as education (Ross & Wu, 1995), employment, income disparity etc. because these variables impact the access to public health infrastructure and general health of populations. Human development is related to health condition. Education level and economic condition are factors influencing health status. The well-educated are less likely to have economic hardship. They also have a greater sense of healthiness and healthier behaviors such as less/no smoking, more physical exercise, and medical check-ups to improve their health. The wealthier people with higher income have greater purchasing power for healthier lifestyle (healthy food, better nutrition, more protected medical insurance). Ross and Wu (1995) find education level has positive effect on health through work and economic condition, social-psychological resources, and health lifestyle. Hence,
H2
Human development has a positive effect on, (a) representation of women in legislature, and (b) public health expenditure.
H3
Representation of women in legislature has a positive effect on public health expenditure.
2.4. Public health expenditure and Covid-19 outcomes
At the time of writing this paper, more than 4.2 million cases of Covid-19 have been diagnosed worldwide, with about two-third of these cases still active and about 290,000 deaths (Worldometers (2020) (2020), 2020). Most recent studies examine these outcomes from a medical or therapeutic perspective (e.g., Murthy, Gomersall, & Fowler, 2020) despite much debate in media on the role of public policy makers, politicians, and general public in the spread of this virus. Past research shows a positive link between public health expenditure and its outcomes (Kim & Lane, 2013), such as infant mortality and life expectancy rates (Nixon & Ulmann, 2006). Hence, it would be expected that greater expenditure on public health infrastructure such as hospitals, ICU facilities and equipment such as ventilators, personal protection equipment (PPE) such as face masks and gowns, and healthcare professionals, would help deliver positive results in the battle against Covid-19. Hence, the authors hypothesize direct effects of public health expenditure on the various Covid-19 outcomes as follows:
H4
Public health expenditure has a positive effect on the total number of Covid-19 (a) tests, (b) diagnosed, (c) active, and (d) critical cases, and (e) a negative effect on the number of deaths.
2.5. Public health and human environment
Human environment, which consists of elements such as population density, urbanization, and age structure, is a major factor influencing public health. World Health Organization reports the negative impact of high population density and urbanization on mental and physical health (WHO, 2020, WHO, 2020b). Rapid urbanization in most countries in the last few decades has led to inadequate housing, congested public transport, poor hygiene, and high pollution level (air, water, and noise), which results in physical and mental health problems (WHO, 2020b). In fact, infectious diseases and epidemics (e.g., tuberculosis, pneumonia) are also more likely to happen in densely populated and urban areas (WHO, 2020, WHO, 2020b). As higher population density is expected to lead to more active transport, more perceived stress and smoking, it has negative effects on mortality (Beenackers, Groeniger, Kamphuis, & Van Lenthe, 2018) and health conditions (Greiner, Li, Kawachi, Hunt, & Ahluwalia, 2004). Similarly, age structure of a population affects the social (e.g., social protection), economic (e.g., labor force), and health (e.g., healthcare for elderly) systems and policies of a country. The functioning of the immune system declines with age, which influences the physical strength of the elderly to respond to infection. There is a negative relationship between physical health condition and age (Ma et al., 2009, Sun et al., 2011). Hence, as follows:
H5
Number of tests for Covid-19 are influenced positively by (a) population density, (b) aging population, and (c) urban population.
H6
Number of deaths due to Covid-19 are influenced positively by (a) population density, ((b) aging population, and (c) urban population.
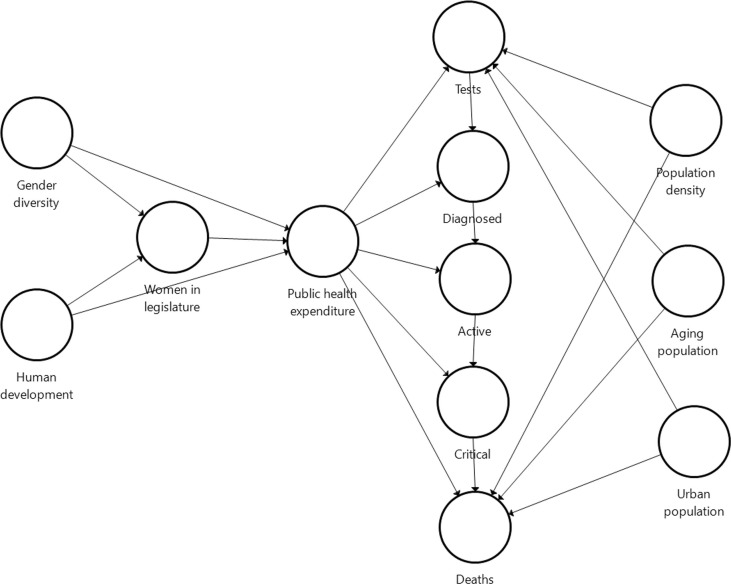
Fig. 1 shows the conceptual model summarizing all these hypotheses.
Fig. 1.
Conceptual model.
3. Methodology
This paper uses publicly reported indicators to operationalize all the constructs. All the measures for gender equity, women in legislature, human development, public health expenditure and human environment are from the year 2018 or earlier; whereas all the public health outcomes related to Covid-19 are the current figures. This temporal separation between the predictor and outcome variables helps eliminate any concerns about endogeneity or reverse causality (Mertens, Pugliese, & Recker, 2017). Moreover, all the measures are either indices or ratios, to avoid confounds due to any other between-country differences. Table 1 shows the sample profile using three levels for each characteristics.
-
•
Gender equity. Reversed score for Gender Inequality Index, which is a composite index ranking countries in terms of gender gap with three dimensions: reproductive health, empowerment, and labor market participation (UNDP, 2020).
-
•
Women in Legislature. Percentage of females elected to the legislative body of a country (World Bank (2020) (2020), 2020).
-
•
Human development. Human Development Index (UNDP, 2020) is a composite index ranking countries in terms of human development based on three dimension indices, life expectancy index, education index, and income index.
-
•
Public health expenditure. Current expenditure on public health by a country as a percentage of its GDP (UNDP, 2020).
-
•
Public health outcomes. Five indicators related to Covid-19 pandemic (Worldometers (2020) (2020), 2020), including (a) number of tests performed to diagnose a Covid-19 case, (b) number of diagnosed cases (patients diagnosed with Covid-19 infection), (c) number of active cases (currently infected patients), (d) number of critical cases (those in serious condition e.g., admitted to ICU), and (e) number of people dead due to Covid-19. All these indicators are divided by the country’s population to avoid any possible confound due to the wide variation in the size of populations for the countries in the sample.
-
•
Human environment. Three indicators reported by UNDP (2020). Population density is the number of people (in millions) per square kilometer. Population above 65 years (%) is the ratio of people above the age of 65 years to the total population. Urban population (%) is the proportion of population living in urban areas.
Table 1.
Sample profile (N = 210).
| Sample characteristics | No. of Countries | %age | Sample characteristics | No. of Countries | %age |
|---|---|---|---|---|---|
| Gender Inequality Index | Active cases per million population | ||||
| <0.25 | 53 | 34.2% | <100 | 115 | 54.8% |
| 0.25–0.50 | 63 | 40.6% | 100–500 | 57 | 27.1% |
| >0.50–0.75 | 39 | 25.2% | >500 | 38 | 18.1% |
| Human Development Index | Critical cases per million population | ||||
| <0.50 | 20 | 11.6% | <20 | 101 | 77.7% |
| 0.50–0.75 | 67 | 39.0% | 20–50 | 15 | 11.5% |
| >0.75 | 85 | 49.4% | >50 | 14 | 10.8% |
| Women in Legislature (%) | Deaths per million population | ||||
| <20% | 70 | 40.0% | <20 | 124 | 77.5% |
| 20–40% | 88 | 50.3% | 20–100 | 25 | 15.6% |
| >30% | 17 | 9.7% | >100 | 11 | 6.9% |
| Public health expenditure (% of GDP) | Population density (per Sq. Km.) | ||||
| <5% | 50 | 29.8% | <100 | 111 | 53.4% |
| 5–10% | 100 | 59.5% | 100–500 | 75 | 36.1% |
| >10% | 18 | 10.7% | >500 | 22 | 10.6% |
| Tests per million population | Population above 65 (%) | ||||
| <1000 | 52 | 34.9% | <10% | 111 | 64.9% |
| 1000–5000 | 50 | 33.6% | 10–20% | 48 | 28.1% |
| >5000 | 47 | 31.5% | >20% | 12 | 7.0% |
| Diagnosed cases per million population | Urban population (%) | ||||
| <100 | 106 | 50.5% | <50% | 57 | 32.4% |
| 100–500 | 56 | 26.7% | 50–75% | 65 | 36.9% |
| >500 | 48 | 22.9% | >75% | 54 | 30.7% |
Note: Total number of countries for each characteristics is subject to availability of data.
4. Data analysis and results
The authors use path analysis with SmartPLS 3.0 to test all the hypotheses because they have a relatively small sample (N = 210) of secondary data with many ratios and other artifacts that may not be normally distributed and their conceptual model is quite complex with many construct and relationships (Hair, Risher, Sarstedt, & Ringle, 2019). All the VIF (Variance Inflation Factor) values are less than the recommended cut-off value of three, hence multi-collinearity is not a concern (Hair et al., 2019). Next, R-square values are high for many outcome variables (e.g., number of tests = 0.13, diagnosed cases = 0.28, and deaths = 0.45), hence the model explains a significant proportion of variance in these variables. High values of the blindfolding-based cross-validated redundancy measure Q2 also confirm the predictive accuracy of the PLS path model (Hair et al., 2019). Finally, a low SRMR (0.054) and high NFI (0.86) also show a good model-fit in view of the many missing values in the dataset.
Table 2 shows the correlations and descriptive statistics for all the variables and Table 3 reports the results of the path analysis. First, gender equity has significant positive effects on women in legislature (β = 0.49, p < .001) and public health expenditure (β = 0.25, p < .01), hence both H1a and H1b are supported. Next, human development has an unexpected negative effect on women in legislature (β = −0.21, p < .001) and a non-significant positive effect on public health expenditure (β = 0.10, p > .30), however women in legislature has a significant positive effect on public health expenditure (β = 0.23, p < .001), hence H2a and H3 are supported but not H2b. Public health expenditure has a positive effect on the number of diagnosed (β = 0.17, p < .05) and critical (β = 0.20, p < .01) cases but no significant effect on the other outcomes (number of tests, active cases and deaths), hence H4b and H4d are supported but not H4a, H4c, and H4e. Finally, both aging population (β = 0.24, p < .05) and urban population (β = 0.22, p < .01) have significant positive effects on the number of tests but only urban population has a significant positive effect on number of deaths (β = 0.12, p < .05), hence only H5b, H5c, and H6c are supported and not the remaining hypotheses.
Table 2.
Correlations and descriptive statistics.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
1.00 | |||||||||||
|
0.80** | 1.00 | ||||||||||
|
0.37** | 0.15 | 1.00 | |||||||||
|
0.41** | 0.32** | 0.34** | 1.00 | ||||||||
|
0.50** | 0.44** | 0.13 | 0.15 | 1.00 | |||||||
|
0.56** | 0.43** | 0.24** | 0.36** | 0.32** | 1.00 | ||||||
|
0.54** | 0.41** | 0.23** | 0.33** | 0.23** | 0.96** | 1.00 | |||||
|
0.44** | 0.33** | 0.25** | 0.41** | 0.21* | 0.85** | 0.85** | 1.00 | ||||
|
0.41** | 0.34** | 0.23** | 0.38** | 0.20* | 0.84** | 0.83** | 0.89** | 1.00 | |||
|
0.14 | 0.18* | −0.02 | −0.04 | 0.04 | 0.10 | 0.10 | 0.08 | 0.02 | 1.00 | ||
|
0.77** | 0.63** | 0.31** | 0.53** | 0.40** | 0.54** | 0.50** | 0.39** | 0.39** | 0.06 | 1.00 | |
|
0.61** | 0.60** | 0.13 | 0.30** | 0.37** | 0.35** | 0.36** | 0.29** | 0.26** | 0.21** | 0.47** | 1.00 |
| Mean | 0.35 | 0.72 | 23.59 | 6.55 | 10,060 | 586 | 406 | 22 | 31 | 482 | 8.50 | 60.12 |
| Standard deviation | 0.19 | 0.15 | 12.11 | 2.62 | 30,047 | 1405 | 1025 | 53 | 104 | 2164 | 7.14 | 22.81 |
***p < .001.
p < .05.
p < .01.
Table 3.
Path analysis (SmartPLS 3.0) output.
| Hypothesized relationship | Standardized Beta coefficient | Result |
|---|---|---|
| H1a: Gender equity → Women in legislature | 0.49*** | Supported |
| H1b: Gender equity → Public health expenditure | 0.25** | Supported |
| H2a: Human development → Women in legislature | −0.21* | Not supported |
| H2b: Human development → Public health expenditure | 0.10 | Not supported |
| H3: Women in legislature → Public health expenditure | 0.23*** | Supported |
| H4a: Public health expenditure → Number of tests | −0.08 | Not supported |
| H4b: Public health expenditure → Number of diagnosed cases | 0.17* | Supported |
| H4c: Public health expenditure → Number of active cases | −0.01 | Not supported |
| H4d: Public health expenditure → Number of critical cases | 0.20*** | Supported |
| H4e: Public health expenditure → Number of deaths | 0.08 | Not supported |
| H5a: Population density → Number of tests | −0.02 | Not supported |
| H5b: Aging population → Number of tests | 0.24** | Supported |
| H5c: Urban population → Number of tests | 0.22** | Supported |
| H6a: Population density → Number of deaths | −0.01 | Not supported |
| H6b: Aging population → Number of deaths | 0.08 | Not supported |
| H6c: Urban population → Number of deaths | 0.12* | Supported |
p < .05.
p < .01.
p < .001.
5. Discussion and implications
Health experts argue that women should be involved in all stages of public health management, including planning, decision-making, and emergency response systems, because they account for about half the world’s population and are the primary care-giver for the young, the elderly, and sick people in most households and healthcare facilities (WHO, 2017). However, despite these calls, women continue to be under-represented in top national and global healthcare organizations (WHO, 2017) and even government and legislatures (UNDP, 2020). This paper addresses these calls for greater representation of women in leadership roles by exploring the impact of gender equity on public health outcomes during the ongoing Covid-19 pandemic. Using publicly available data for 210 countries, the authors analyze the impact of gender equity and human development on women’s representation in legislature and public health expenditure, and the impact of public health expenditure and human environment (population density, aging population and urban population) on Covid-19 outcomes (number of tests, diagnosed, active and critical cases, and deaths).
The results show a clear evidence of the importance of women’s role in managing public health outcomes, with the strong positive effects of gender equity and the proportion of women in legislature on public health expenditure, which in turn shows significant impact on the number of diagnosed and critical cases but not on the number of deaths. However, the unexpected negative effect of human development on women in legislature and no significant effect on public health expenditure suggests a relook at the definition of human development. Moreover, the lack of any significant impact of public health expenditure on the number of tests or deaths may indicate possible mismanagement of public health systems due to unclear policies and priorities in many countries during this crisis, which has already led to calls for improvement in future (Patterson, 2020, Qato, 2020). Both aging population and urban population have significant positive effects on the number of tests but only urban population has a positive effect on the number of deaths, which is not surprising as these two population segments have been the worst hit by the Covid-19 outbreak so far (Keil, Connolly, & Ali, 2020). Interestingly, population density has no impact on the number of tests or deaths, which suggests some biases in the way these tests are being conducted and the deaths are being reported (Kwiatkowski & Nadolny, 2020).
There is growing evidence that the COVID-19 crisis impacts men and women in different ways, including healthcare workers, patients, their family members and the society at large; and therefore, the measures to address this crisis and its outcomes should take these gender differences into account (Linde and Gonzalez, 2020, Papp and Hersh, 2020). For example, women tend to be more vulnerable at home and in the workplace, due to which they are more likely to suffer the economic impact of Covid-19 crisis (Linde & Gonzalez, 2020). Moreover, women comprise 70% of the global healthcare workforce and their experiences during the COVID-19 pandemic are significantly different to those of their male counterparts, especially due to the unique risks and vulnerabilities faced by women due to “deep-rooted inequalities and traditional gender roles” (Papp & Hersh, 2020). Therefore, public health agencies and policy makers need to look at the COVID-19 pandemic through a gender lens in order to identify and implement the most effective policy responses.
All the issues identified in this paper, such as under-representation of women in leadership positions, possible mismanagement of public health systems and inconsistent or incorrect reporting of the public health outcomes in this context, need to be addressed not only for a quick economic recovery in the aftermath of this Covid-19 crisis but to also prevent and manage such disasters in future. Clearly, Covid-19 has revealed the vulnerabilities of the modern civilization and economic systems, wherein the so-called developed countries account for most of the diagnosed cases and deaths, although it is still early days and we need to wait to see its impact on the less developed countries in Asia, Africa and Latin America, before we can make a full assessment and recommendations, especially about the role of gender equity in managing this crisis.
Biographies
Tak Yan Leung (PhD) is an Associate Professor of Accounting at the LSK School of Business & Administration, Open University of Hong Kong. Her research interests include corporate finance, corporate governance, and executive compensation. She has won a number of competitive research grants and published articles in a several top international journals, including Academy of Management Journal, Accounting and Finance, International Review of Economics and Finance, International Review of Accounting, Banking and Finance, Journal of Corporate Finance, British Journal of Management, Journal of Empirical Finance, International Business Review, among others. She serves as a member of the Editorial Review Board of the Journal of Business Research.
Piyush Sharma (PhD) is a Professor of Marketing at Curtin University, Australia. He serves as the Regional Editor (Asia) for Journal of Knowledge Management, Associate Editor (Marketing and International Business) for Journal of Business Research and Senior Editor (Marketing) for International Journal of Emerging Markets. He is also a member of the Editorial Review Boards of the Journal of the Academy of Marketing Science, Journal of International Business Studies, Journal of Service Research, European Journal of Marketing, and Journal of Service Theory and Practice, among others. His research appears in the Journal of International Business Studies, Journal of the Academy of Marketing Science, Journal of Service Research, International Journal of Research in Marketing, Journal of Business Research, Industrial Marketing Management, Psychology & Marketing, European Journal of Marketing, Journal of Service Management, Journal of Service Theory and Practice, Journal of Services Marketing, Journal of Marketing Management, Journal of Advertising, and Journal of Retailing and Consumer Services, among others.
Pattarin Adithipyangkul (PhD) is a lecturer in the School of Accounting, Curtin University. Her research interests include corporate governance, executive compensation, family business, and agency theory. She has published in journals such as Journal of Contemporary Accounting and Economics, Australian Accounting Review, Asia Pacific Journal of Management, and Chinese Economy.
Peter Hosie (PhD) is a Senior Human Capital Consultant with Helix Management based in Perth, Australia. He is a Fellow of the Australian Human Resource Institute and has held academic and policy development positions with universities in Australia, United Arab Emirates and Austria. He has over 120 publications, including journal articles, conference papers, book chapters, books and monographs. His research appears in a diverse range of journals, including International Journal of Human Resource Management, International Journal of Manpower. Journal of Services Marketing, Asia Pacific Journal of Human Resources, Personnel Review, International Journal of Workplace Health Management, European Business Review, and Asia Pacific Journal of Management, among others.
Contributor Information
T.Y. Leung, Email: tyleung@ouhk.edu.hk.
Piyush Sharma, Email: Piyush.Sharma@curtin.edu.au.
Pattarin Adithipyangkul, Email: P.Adithip@curtin.edu.au.
Peter Hosie, Email: pjhosie@outlook.com.
References
- Agnew J.R., Anderson L.R., Gerlach J.R. Who chooses annuities? An experimental investigation of the role of gender, framing, and defaults. American Economic Review: Papers & Proceedings. 2008;98(2):418–422. [Google Scholar]
- Beaman L., Duflo E., Pande R., Topalova P. Female leadership raises aspirations and educational attainment for girls: A policy experiment in India. Science. 2012;335(6068):582–586. doi: 10.1126/science.1212382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beenackers M.A., Groeniger J.O., Kamphuis C.B.M., Van Lenthe F.J. Urban population density and mortality in a compact Dutch city: 23-year follow-up of the Dutch GLOBE study. Health & Place. 2018;53:79–85. doi: 10.1016/j.healthplace.2018.06.010. [DOI] [PubMed] [Google Scholar]
- Brooks P., Zank H. Loss averse behavior. Journal of Risk and Uncertainty. 2005;31(3):301–325. [Google Scholar]
- Byrnes J.P., Miller D.C., Schafer W.D. Gender differences in risk taking: A meta-analysis. Psychological Bulletin. 1999;125(3):367–383. [Google Scholar]
- Dejoy D.M. An examination of gender differences in traffic accident risk perception. Accident Analysis & Prevention. 1992;24(3):237–246. doi: 10.1016/0001-4575(92)90003-2. [DOI] [PubMed] [Google Scholar]
- Ertac S., Gurdal M.Y. Deciding to decide: Gender, leadership and risk-taking in groups. Journal of Economic Behavior & Organization. 2012;83(1):24–30. [Google Scholar]
- Fllyn J., Slovic P., Mertz C.K. Gender, race, and perception of environmental health risk. Risk Analysis. 1994;14(6):1101–1108. doi: 10.1111/j.1539-6924.1994.tb00082.x. [DOI] [PubMed] [Google Scholar]
- Greiner K.A., Li C., Kawachi I., Hunt D.C., Ahluwalia J.S. The relationships of social participation and community ratings to health and health behaviors in areas with high and low population density. Social Science & Medicine. 2004;59(11):2303–2312. doi: 10.1016/j.socscimed.2004.03.023. [DOI] [PubMed] [Google Scholar]
- Hair J.F., Risher J.J., Sarstedt M., Ringle C.M. When to use and how to report the results of PLS-SEM. European Business Review. 2019;31(1):2–24. [Google Scholar]
- Herper, M. (2020). The coronavirus exposes our health care system’ weaknesses. We can be stronger. March 2, 2020. https://www.statnews.com/2020/03/02/the-coronavirus-exposes-our-health-care-systems-weaknesses-we-can-be-stronger/.
- Jambroes M., Nederland T., Kaljouw M., van Vliet K., Essink-Bot K., Ruwaard M.-L. A new concept of health – implications for public health policy and practice: A Qualitative analysis. The Lancet. 2014;384(Special Issue):39. [Google Scholar]
- Keil, R., Connolly, C., & Ali, S. H. (2020). Outbreaks like coronavirus start in and spread from the edges of cities. The Conversation, 18th February, 2020.
- Kim T.K., Lane S.R. Government health expenditure and public health outcomes: A comparative study among 17 countries and implications for US health care reform. American International Journal of Contemporary Research. 2013;3(9):8–13. [Google Scholar]
- King, J. S. (2020). Covid-19 and the need for health care reform. The New England Journal of Medicine, April 17, 2020, 10.1056/NEJMp2000821. [DOI]
- Kwiatkowski, M. & Nadolny, T. L. (2020). At least 2,300 nursing homes have coronavirus cases and the reality is likely much worse. USA Today, 13th April, 2020.
- Lee N.C., Wong F.L., Jamison P.M., Jones S.F., Galaska L., Brady K.T.…Townsend G.-A.S. Implementation of the national breast and cervical cancer early detection program: The beginning. Cancer. 2014;120(S16):2540–2548. doi: 10.1002/cncr.28820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linde, A. & Gonzalez, A. (2020). The Pandemic’s Gender Imperative, Project Syndicate, 8th May, 2020. https://www.project-syndicate.org/commentary/covid19-pandemic-gender-differences-by-ann-linde-and-arancha-gonzalez-2020-05.
- Lundeberg M.A., Fox P.W., Punćochaŕ J. Highly Confident but Wrong: Gender Differences and Similarities in Confidence Judgments. Journal of Educational Psychology. 1994;86(1):114–121. [Google Scholar]
- Ma W.M.H., Harrison M.B., Coo H., Friedberg E., Buchanan M., VanDenKerkhof E.G. Associations between chronic disease, age, and physical and mental health status. Chronic Diseases in Canada. 2009;29(2):108–116. [PubMed] [Google Scholar]
- Mayer C.H., Oosthuizen R.M. Concepts of creative leadership of women leaders in 21st century. Creativity Studies. 2020;13(1):21–40. [Google Scholar]
- Mertens W., Pugliese A., Recker J. Springer; Cham: 2017. Causality: Endogeneity Biases and Possible Remedies. In Quantitative Data Analysis; pp. 99–134. [Google Scholar]
- Murthy S., Gomersall C.D., Fowler R.A. Care for critically ill patients with COVID-19. Journal of American Medical Association. 2020;323(15):1499–1500. doi: 10.1001/jama.2020.3633. [DOI] [PubMed] [Google Scholar]
- Nixon J., Ulmann P. The relationship between health care expenditure and health outcomes. The European Journal of Health Economics. 2006;7(1):7–18. doi: 10.1007/s10198-005-0336-8. [DOI] [PubMed] [Google Scholar]
- Olsen R.A., Cox C.M. The influence of gender on the perception and response to investment risk: The case of professional investors. The Journal of Psychology and Financial Markets. 2001;2(1):29–36. [Google Scholar]
- Pandey J., Jain U. Worldviews and perceptions of environmental problems. Psychological Studies. 2017;62(3):250–260. [Google Scholar]
- Papp, S. & Hersh, M. (2020). A Gender Lens for COVID-19, Project Syndicate, 27th March, 2020. https://www.project-syndicate.org/commentary/covid19-response-requires-a-gender-lens-by-susan-papp-and-marcy-hersh-2020-03.
- Patterson, R. N. (2020). How to reform healthcare after Covid-19. April 20, 2020, https://thebulwark.com/how-to-reform-healthcare-in-the-wake-of-covid-19/.
- Post C., Byron K. Women on boards and firm financial performance: A meta-analysis. Academy of Management Journal. 2015;58(5):1546–1571. [Google Scholar]
- Qato, D. (2020). Our public health infrastructure is losing a fight with capitalism. Jacobin Magazine, 20th March, 2020. https://www.jacobinmag.com/2020/03/coronavirus-public-health-infrastructure-capitalism-epidemiology.
- Ross C.E., Wu C. The links between education and health. American Sociological Review. 1995;60(5):719–745. [Google Scholar]
- Smakaj, B. (2020). Covid-19 and the need for deep EU reform. https://www.euractiv.com/section/future-eu/opinion/covid-19-and-the-need-for-deep-eu-reform/.
- Sun S., Chen J., Johannesson M., Kind P., Xu L., Zhang Y., Burström K. Population health status in China: EQ-5Q results, by age, sex and socio-economic status, from the National Health Services Survey 2008. Quality of Life Research. 2011;20(3):309–320. doi: 10.1007/s11136-010-9762-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tulchinsky T.H., Varavikova E.A. Elsevier, Academic Press; San Diego: 2014. The New Public Health. [Google Scholar]
- UNDP (2020). Global Human Development Indicators, United Nations Development Programme Human Development Reports, New York, USA.
- United Nation (2020). Everyone included: Social impact of Covid-19. https://www.un.org/development/desa/dspd/everyone-included-covid-19.html.
- Winslow C.E.A. The untilled fields of public health. Science. 1920;51(1306):23–33. doi: 10.1126/science.51.1306.23. [DOI] [PubMed] [Google Scholar]
- WHO (2017). Statement by Dr Zsuzsanna Jakab, WHO Regional Director for Europe, for International Women’s Day, World Health Organization, www.euro.who.int/en.
- WHO (2020a). Population density – A growing concern, Health situation and trend assessment, World Health Organization South East Asia, http://origin.searo.who.int/.
- WHO (2020b). Urban health. World Health Organization, https://www.who.int/health-topics/urban-health.
- World Bank (2020). World Bank Open Data, https://data.worldbank.org/.
- Worldometers (2020). https://www.worldometers.info/coronavirus (accessed 30 April, 2020).