Abstract
The COVID-19 outbreak has become a pandemic that is threatening global health. The typical clinical manifestations were fever, cough, dyspnea, and myalgia or fatigue. Digestive symptoms such as nausea, vomiting, diarrhea, abdominal pain usually accompany respiratory symptoms. However gastrointestinal bleeding as the first symptom is not reported. Here we reported a case of COVID-19 with gastrointestinal bleeding as the initial symptom to the emergency department with a real-time reverse transcriptase polymerase chain reaction test positive, and normal thorax tomography. The case demonstrate that; clinicians should be alerted to patients about COVID-19 when referring to atypical symptoms and every patient undergoing endoscopy should be considered potentially infected or can infect others.
Keywords: COVID-19, Emergency, Endoscopy, Gastrointestinal bleeding
Introduction
The typical clinical presentation of Coronavirus disease (COVID-19) is often fever, dyspnea, cough, myalgia, and fatigue [1]. Digestive symptoms such as nausea, vomiting, diarrhea, abdominal pain are in the range of 2-18.6%, and they usually accompany respiratory symptoms [2], [3]. However, the incidence of the digestive symptoms in critical patients is up to 36-50.5% [2], [4]. Gastrointestinal system (GIS) bleeding is rare and is frequently seen in critical intensive care patients [4], [5]. In this case, we wanted to present a COVID-19 patient who was admitted to the emergency department with dyspnea, abdominal pain, and diarrhea and was diagnosed with gastrointestinal bleeding, with a real-time reverse transcriptase polymerase chain reaction (RT-PCR) test positive, and normal thorax tomography. In the literature, gastrointestinal bleeding has not been reported as the first symptom of presented to the emergency department in patients with COVID-19 positive. This case is the first case reported in the literature.
Case report
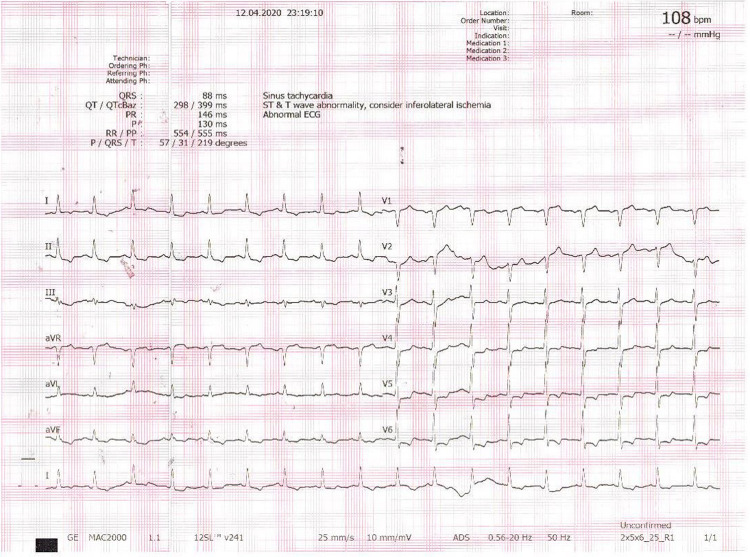
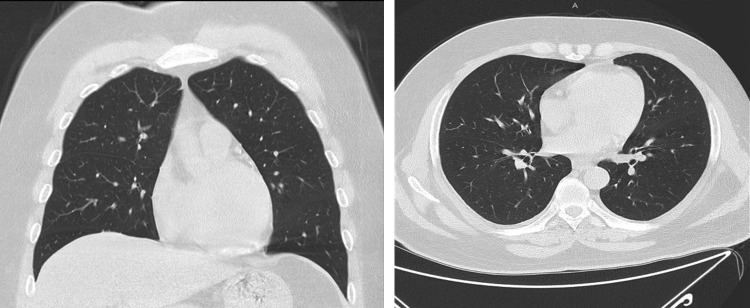
A 53 year old male patient with a medical history of hypertension, diabetes mellitus, and chronic renal failure presented to emergency department with epigastric pain, diarrhea, and dyspnea. The patients stated that he presented to the emergency department due to dyspnea and epigastric pain two days before this application, and a nasal swab was taken for COVID-19, and symptomatic treatment was initiated. The patient presented to the emergency department again since his complaints did not regress, and he also had diarrhea started. The patient stated that he had no fever or cough. He had dyspnea, palpitation, and black stool. He had no recent travel outside of the state or internationally, no contact with COVID-19 (+) patient. He had no drug usage in his history except for the use of acetylsalicylic acid. The vital signs were blood pressure: 130/100 mmHg, pulse: 108 beats.min−1, O2 saturation: 99%, respiration rate: 18 min−1, Glasgow Coma Score: 15 (G4M6S5). The heart was rhythmic and tachycardic, sinus tachycardia and ischemia in the inferolateral derivation were recorded on the electrocardiogram. (Fig. 1 ) No abnormality was found on the patient's cardiopulmonary or respiratory examination. He had epigastric tenderness in the abdominal examination. Melena was present in his rectal examination. The laboratory values when the patient presented to the emergency department and the follow-up values are shown in Table 1 . The patient had anemia and an increase in WBC, BUN, creatinine, LDH, glucose, procalcitonin, highly sensitive Troponin I values. (Laboratory tests of 5 months ago Hb: 14.2 g/dl, creatinine: 1.87 mg/dl). It was learned that the COVID-19 RT-PCR test, which was taken two days ago, was positive. No abnormal findings were present on thorax tomography. (Fig. 2 )
Figure 1.
Electrocardiogram showing sinus tachycardia and ischemia in the inferolateral derivation on admission, pulse: 108 beats.min−1.
Table 1.
Blood test findings.
| Blood Parameter | On Admission | Day 1 | Day 2 | Day 7 |
|---|---|---|---|---|
| WBC (103 μL) | 13.8a | 11.4a | 9.7 | 9.9 |
| Hemoglobin (g/dl) | 8.3a | 7.2a | 10.3a | 9.9a |
| Hematocrit (%) | 25.4a | 22.3a | 31.1a | 28.7a |
| Platelet (103 μL) | 232 | 241 | 253 | 252 |
| Lymphocyte (103 μL) | 2.8 | 3.1 | 2.2 | 2.8 |
| Glucose (mg/dl) | 210a | 132a | 111a | 109a |
| Urea (mg/dl) | 209a | 132a | 119a | 109a |
| Creatinine (mg/dl) | 2.31a | 2.28a | 2.56a | 2.36a |
| Alanine transferase (IU/L) | 27 | 31 | 30 | 29 |
| Aspartate transferase (IU/L) | 35 | 36 | 33 | 31 |
| Sodium (mmol/L) | 134 | 135 | 139 | 137 |
| Potassium (mmol/L) | 5.15 | 4.99 | 4.95 | 5.03 |
| Amylase (IU/L) | 70 | 65 | 84 | 53 |
| Total Bilirubin (mg/dl) | 0.42 | 0.52 | 0.65 | 0.37 |
| Direct Bilirubin (mg/dl) | 0.09 | 0.12 | 0.14 | 0.09 |
| Ferritin (μg/L) | 69.1 | 319.7 | 218 | 133.9 |
| Lactate Dehydrogenase (IU/L) | 269a | 331a | 273a | 237 |
| Creatine Kinase (IU/L) | 248a | 243a | 260a | 234a |
| Procalcitonin (μg/L) | 0.56a | 0.18a | 0.08a | 0.06 |
| D-Dimer (μg/L) | 337 | 482 | 1320a | 338 |
| CK-MB (μg/L) | 11.9a | 5.3 | 3.4 | 2.1 |
| High Sensitivity Troponin I (ng/L) | 150a | 70 | 5 | 4 |
| aPTT (sec) | 21.3a | 21.4a | 21.6a | 23.1a |
| PTZ (sec) | 17a | 16.8a | 16.3a | 17.2a |
| INR | 1.42a | 1.40a | 1.37a | 1.45a |
| Fibrinojen (mg/dl) | 460.2a | 414.74a | 509.62a | 370.82a |
WBC: White blood cell; CK-MB: Creatinine kinase- Myocardial band; aPTT: Activated partial thromboplastin time; PTZ: Prothrombin time; INR: International Normalized Ratio
Value other than reference values.
Figure 2.
CT scan of the chest showing normal lung on admission.
The patient was hospitalized in the private, isolated service. Pantoprazole infusion was initiated for gastrointestinal system bleeding. Hydroxychloroquine 2 × 400 loading and 2 × 200 maintenance treatments were given for five days for COVID-19 treatment. When hemoglobin level decreased to 7.2 g/dl in the control hemogram, patient had 3 units of red blood cell transfusion. The ejection fraction was 55% on the patient's echocardiography. There was no segmental and global wall motion abnormality. In his follow-up, his cardiac enzymes regressed, and his ECG did not change. Hemoglobin values did not decrease after transfusion. The patient was discharged on the 7th day of hospitalization with the recommendation of 14 days of home isolation. The nasal swab sample, which was taken 14 days after his first application, was negative.
Discussion
Although COVID-19 patients frequently apply with the findings of the respiratory system, recent studies point out that the findings of the gastrointestinal system are also significantly observed [2], [4]. In a multicentre study in which the frequency of digestive system findings was investigated in patients with COVID-19 and 204 patients were included, GIS findings were found in 50.5% of the hospitalized patients, and the most common symptom (78.6%) was reported as a lack of appetite. However, more specific GIS symptoms such as diarrhea in 34%, vomiting in 3.9%, and abdominal pain in 1.9% were also detected. While 47.6% of patients with GIS symptoms had both GIS symptoms and respiratory symptoms, 2.9% (n = 6) were found to have only GIS specific symptom [2]. Our case had both dyspnea and abdominal pain with diarrhea. However, what made the case different was the condition considered as diarrhea was GIS bleeding. Because most COVID-19 GIS bleeding cases in the literature are critical ill patients [4], [5]. GIS bleeding can occur due to primary or secondary reasons. There may be gastrointestinal mucosal cell damage due to virus invasion or tissue hypoxia caused by long-term hypoxemia. It may also be due to existing coagulopathy in patients who developed multiple organ failure. Steroid, corticosteroid which used in treatment and heparin, or salicylic acid used in prophylaxis of intravascular thrombosis may also cause bleeding [4]. It is difficult to say precisely whether gastrointestinal bleeding observed in our case is due to salicylic acid or COVID-19. This finding can be either coincidental or may be the result of mucosal damage caused by salicylic acid and physiological stress affecting the digestive system mucosa.
COVID-19 damages the digestive system both directly and via inflammatory response and indirectly by viral invasion. COVID-19 has been shown to use Angiotensin-Converting enzyme II (ACE II) receptor for entry into the cell [6]. ACE II is highly expressed in type II alveolar cells of the lung and epithelial cells of the gastrointestinal system [7]. At autopsy of a patient who died due to COVID 19, histologically degeneration, necrosis, and varying degrees of mucosal spillage were detected in the gastrointestinal mucosa [8]. In the staining of pathology specimens for ACE II, positive areas were detected in gastric cytoplasm, intestinal epithelial cells, and more rarely in esophageal squamous epithelial cells. Also, viral nucleocapsid protein was detected in the duodenal and rectal glandular epithelial cells in the gastric cytoplasm [9]. This finding can be an indication of a direct virus attack on the digestive system [4]. Angiotensin II has a strong vasoconstrictor effect and a proinflammatory effect [10]. The chain reaction of inflammatory factors and viremia can damage the digestive system [2]. In our case, Angiotensin II and direct virus attack may have helped initiate this necrosis and degeneration in the gastrointestinal mucosa, causing ulceration and bleeding.
When performing aerosol-producing procedures, such as upper gastrointestinal tract endoscopy, aerosolization of viral particles may occur when the endoscope passes through the pharynx [11]. Health professionals are advised to do this in negative pressure rooms, using appropriate personal protective equipment and N95 masks [12]. Besides, the American Gastroenterology Association (AGA) recommends rapid testing before the procedure, if possible, for any patient undergoing an GIS endoscopic procedure. Every patient undergoing endoscopy should be considered potentially infected or can infect others [13]. In our case, the absence of fever, cough, and thorax tomography findings may have led to the missing of the patient's diagnosis. However, because our hospital is a pandemic hospital, a sample of the nasopharyngeal swab is taken for RT-PCR from every patient considered as a suspicious case. The sampling of this patient two days ago prevented contamination during hospitalization or possible interventional procedures. Since the hemoglobin values did not decrease, and the stool color turned yellow after blood transfusion, endoscopy was not performed. Emergency coronary angiography was not performed since our patient tended to fall in the cardiac markers, no change in ECG findings, and no abnormal findings were detected on echocardiography. Medical treatment was given. The patient was called for cardiology and gastroenterology outpatient control two weeks after discharge. If there is no urgent problem, the endoscopy procedure is planned for to 8 weeks later with the recommendation of AGA13.
Conclusion
Clinicians’ frequent examination of respiratory symptoms in the differential diagnosis of COVID-19 patients may cause delays in diagnosis and undesired infections in patients presenting with gastrointestinal system findings alone. Clinicians should be alerted to patients when referring to atypical symptoms. This condition is important both for the early diagnosis and treatment of patients and for preventing possible contamination, and for preventing invasive procedures without wearing personal protective equipment and preventive measures.
Funding
None.
Informed consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Disclosure of interest
The authors declare that they have no competing interest..
Author contributors
All authors read the manuscript and agreed to the content and data. All authors played a significant role in the paper.
Acknowledgements
None.
References
- 1.Huang C., Wang Y., Li X., et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. The Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pan L., Mu M., Yang P., Sun Y., Wang R., et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol. 2020;115:766–773. doi: 10.14309/ajg.0000000000000620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wang D., Hu B., Hu C., et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA. 2020 doi: 10.1001/jama.2020.1585. published online Feb 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tian Y., Rong L., Nian W., He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843–851. doi: 10.1111/apt.15731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yang X., Yu Y., Xu J., Shu H., Xia J., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30079-5. pii: S2213-2600(20)30079-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu F., Zhao S., Yu B., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020 doi: 10.1038/s41586-020-2008-3. Published online Feb 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang H, Kang Z, Gong H. et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. BioRxiv 927806. Post online Jan 31. https://doi.org/10.1101/2020.01.30.927806.
- 8.National Health Commission of the People's Republic of China. Guidance on coronavirus disease 2019 (COVID-19), China (Vision 7) (in Chinese). Published online March 3. http://www.gov.cn/zhengce/zheng ceku/2020-03/04/conte nt_54867 05.htm.
- 9.Xiao F., Tang M., Zheng X., Liu Y., Li X., Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.02.055. Published online Mar 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klempin F., Mosienko V., Matthes S., Villela D.C., Todiras M., Penninger J.M., et al. Depletion of angiotensin-converting enzyme 2 reduces brain serotonin and impairs the running-induced neurogenic response. Cell Mol Life Sci. 2018;75:3625–3634. doi: 10.1007/s00018-018-2815-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnston E., et al. Risk of bacterial exposure to the endoscopist's face during endoscopy. Gastrointestinal endoscopy. 2019;89(4):818–824. doi: 10.1016/j.gie.2018.10.034. [DOI] [PubMed] [Google Scholar]
- 12.Sehulster L.M., Chinn R.Y.W., Arduino M.J., Carpenter J., et al. American Society for Healthcare Engineering/American Hospital Association; Chicago IL: 2004. Guidelines for environmental infection control in health-care facilities. Recommendations from CDC and the Healthcare Infection Control Practices Advisory Committee (HICPAC) [Google Scholar]
- 13.Sultan S., Lim J.K., Altayar O., Davitkov P., Feuerstein J.D., Siddique S.M., Falck-Ytter Y., El-Serag H.B., on behalf of the AGA AGA institute rapid recommendations for gastrointestinal procedures during the COVID-19 Pandemic. Gastroenterology. 2020 doi: 10.1053/j.gastro.2020.03.072. [DOI] [PMC free article] [PubMed] [Google Scholar]