Abstract
The number of cases of the coronavirus-induced disease-2019 (COVID-19) continues to increase exponentially worldwide. In this crisis situation, the management of ST-segment elevation myocardial infarction (STEMI) is challenging. In this review, we outline the risks and benefits of primary PCI vs. thrombolysis for STEMI. While thrombolysis may seem like a good choice, many patients have a contraindication and could end up using more resources. Also, with a high probability of the angiogram showing non-obstructed coronary arteries during acute infections, primary PCI should be the preferred strategy.
Abbreviations: ED, Emergency Department; EKG, Electrocardiogram; EMS, Emergency Medical Services; PCI, Primary percutaneous coronary intervention; STEMI, ST-segment elevation myocardial infarction
Keywords: STEMI, COVID-19, Primary percutaneous coronary intervention, Fibrinolytics
Highlights
-
•
During the COVID-19 pandemic, management of STSTEMI is challenging.
-
•
Many patients have a contraindication to thrombolysis and end up using resources with this treatment.
-
•
There is a high probability that an infected patient will show a normal angiogram.
-
•
Primary PCI should be the preferred strategy in STEMI patients, with precautions.
1. Introduction
After the first discovery of coronavirus-induced disease-2019 (COVID-19) in Wuhan, China, the number of cases increased exponentially worldwide [1]. Several measures were undertaken by the government to limit the spread of COVID-19, including social distancing, avoidance of travel, closure of nonessential businesses (restaurants, retail stores, sporting events, etc.), and quarantine for infected patients or those with symptoms. In addition, most health-care facilities in the United States canceled elective surgeries, limited visitors, and transitioned ambulatory clinic visits to televisits to help limit the community spread and to “flatten the curve.” In this crisis situation, optimal management of acute cardiac conditions such as ST-segment elevation myocardial infarction (STEMI) is challenging.
Management of STEMI involves multiple levels of care from Emergency Medical Services (EMS) personnel, emergency department (ED) physicians and nurses, the cardiac catheterization laboratory team, interventional cardiologists, and cardiac intensive care unit team. Over the years, the mortality rate for STEMI has decreased not only because of the introduction of primary percutaneous coronary intervention (PCI) but also because of improved performance of all personnel involved in STEMI care before and after PCI [2]. From the patient making a call to 911, arrival of EMS, and transfer of the patient to the catherization lab, the entire system has been made more efficient, such as decreasing the “door-to-balloon time” [2]. However, during this pandemic, every link in this management chain will be affected.
STEMI patients with active symptoms may present late to the hospital, as they fear that seeking medical attention will result in an increased exposure to the infection. Recently, cardiologists all over the world have seen a decrease of STEMI patients during this pandemic [3]. In addition, once the patient does present, there may also be delay due to the infection-control measures employed by EMS, ED, and catherization lab personnel to prevent the spread of the infection to themselves and other patients. A recent analysis by Tam et al. [4] at a STEMI center in Hong Kong, China, showed that patients presenting with STEMI have a delay in all three important aspects of care (symptom onset to first medical contact, door to device, and catheterization lab arrival to device). The duration for all of these components of STEMI care was higher than regular on/off hours. Their analysis demonstrated that well-built systems of care for STEMI management can easily be disrupted during this pandemic.
However, it is important for physicians and the community to know that delay in treatment increases mortality in STEMI patients both with and without hemodynamic instability. An analysis from the German prospective, multicenter Feedback Intervention and Treatment Times in ST-Elevation Myocardial Infarction (FITT-STEMI) trial shows that every 10 min in treatment delay resulted in 3.31 additional deaths in 100 PCI-treated patients [5]. The notion of “time is muscle” should still be remembered in these tough times. Recently, the Society for Cardiovascular Angiography and Interventions (SCAI) [6] and the Canadian Association of Interventional Cardiology [7] published guidelines for the management of procedures in the cardiac catheterization laboratory. Both sets of guidelines recommend considering thrombolytics at either physician discretion or in low-risk patients. In this review, we discuss the risks vs. benefits of primary PCI and thrombolytics, how the cardiac catheterization laboratory team should be prepared, and what treatment options should be considered in this crisis situation.
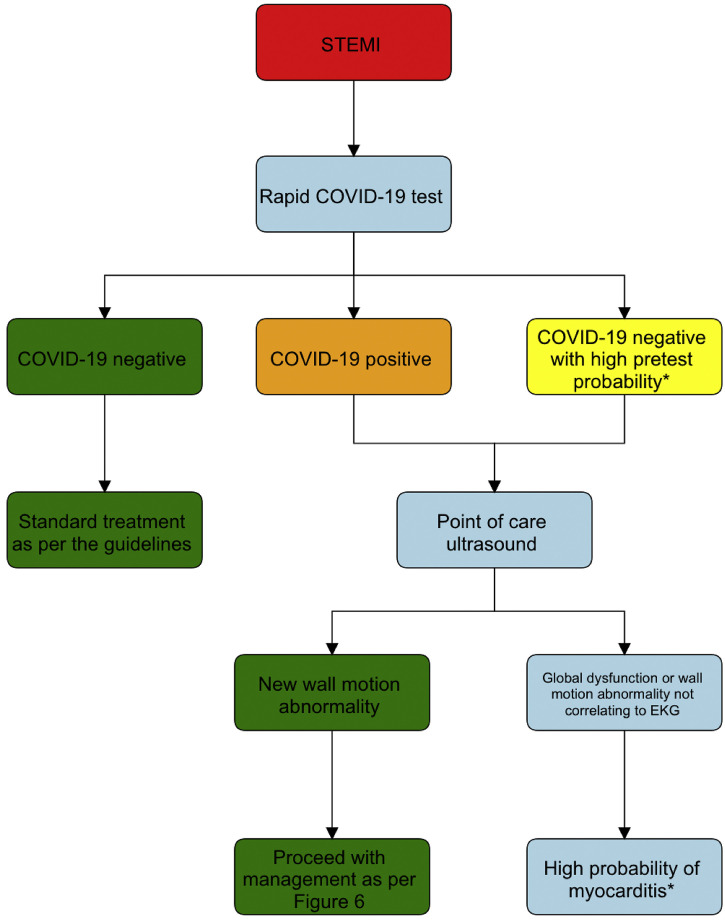
2. Initial assessment of STEMI patients during pandemic
In the era of the COVID-19 pandemic, it is important to quickly assess whether a patient presenting with STEMI is or is not infected with COVID-19. The initial management of STEMI patients is outlined in Fig. 1 . The bedside diagnosis of COVID-19 is difficult, and if available, molecular point-of-care rapid portable tests of COVID-19 should be performed using Abbott ID Now (Abbott, IL), which can give results in 5 min [8]. However, if rapid testing is not available, primary PCI should be performed as if the patient is COVID-19-positive, irrespective of the test results. Electrocardiogram (EKG) and computed tomography (CT) of the lungs done routinely should be carefully evaluated to rule out pericarditis and other non-cardiac causes of chest pain. Rapid measurement of cardiac troponins can be used to differentiate STEMI from myocarditis, as STEMI has a feature of dynamic change. Also, the CT scan can be evaluated for three major classic features of COVID-19: ground-glass opacity, consolidation, and bilateral pulmonary infiltration with reticular patterns. Point-of-care ultrasound, rather than the standard transthoracic echocardiogram, can be used to evaluate for a new wall-motion abnormality, as there is a risk of exposing the cardiac sonographer to COVID-19. Global left ventricular dysfunction or a wall-motion abnormality not correlating to the EKG is likely caused by myocarditis rather than STEMI. Patients with a new wall-motion abnormality and EKG evidence of a STEMI should be promptly managed as per the proposed algorithm.
Fig. 1.
Initial management of STEMI during COVID-19 pandemic.
*In these patients, thrombolysis should be avoided. If available, cardiac magnetic resonance imaging can be done to evaluate for myocarditis. If in doubt, coronary angiogram should be performed rather than thrombolysis.
STEMI - ST-segment elevation myocardial infarction.
3. Thrombolytics vs. primary PCI for STEMI
Current guidelines [9,10] recommend prompt reperfusion with primary PCI with a door-to-balloon time of 90 min if the patient presents to a PCI-capable hospital. If a patient presents to a non-PCI-capable hospital, emergent transfer to a PCI-capable hospital should be performed within 120 min of arrival. If the timeline cannot be achieved, thrombolysis should be performed within the first 30 min of arrival. Symptomatic, unstable patients should be urgently transferred to a PCI-capable hospital even after thrombolysis administration.
While similar protocols can be followed even during this pandemic in COVID-19-negative patients, it is rather challenging in a COVID-19-positive patient or a COVID-19 patient under investigation. Delays happen for various reasons, including infection precautions by the staff and physicians, delay in patient presentation, and short staff at hospitals. Fig. 2, Fig. 3 outline risks vs. benefits in treating STEMI patients with thrombolysis vs. primary PCI during the COVID-19 pandemic.
Fig. 2.
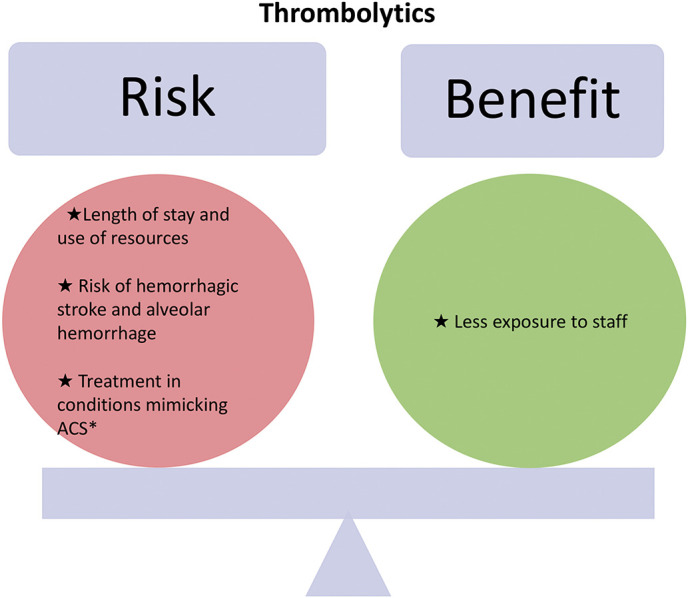
Risks vs. benefits of treating STEMI with thrombolysis during COVID-19.
*Myocarditis, pericarditis, takotsubo cardiomyopathy.
STEMI - ST-segment elevation myocardial infarction.
ACS - Acute coronary syndrome.
Fig. 3.
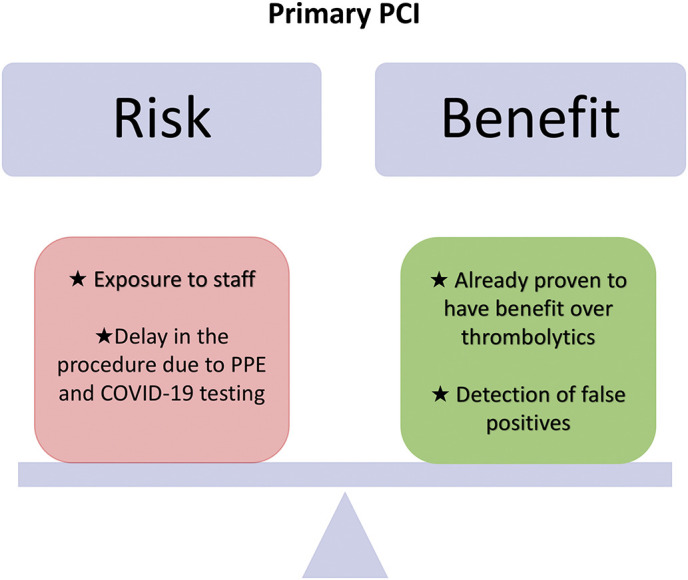
Risks vs. benefits of treating STEMI with primary percutaneous coronary intervention during COVID-19.
STEMI - ST-segment elevation myocardial infarction
PCI - Percutaneous coronary intervention.
PPE - Personal protective equipment.
Currently, there are no published studies evaluating different STEMI treatment strategies during a pandemic. A protocol was recently published from Sichuan Provincial People's Hospital by Zeng et al. [11] describing the use of thrombolysis in STEMI patients if the onset of symptoms was <12 h and proceeding with PCI only after the patient had tested negative for COVID-19. The authors also recommended that the risk of spreading the infection vs. the benefit of performing PCI should be carefully evaluated, and in unstable patients, conservative treatment should be followed until the resolution of pneumonia. However, this approach cannot be readily followed for multiple reasons.
-
1.
Many patients have contraindications for thrombolysis [2] (previous stroke or hemorrhagic stroke, active bleeding, elderly, multi-organ failure [liver and kidney damage] due to cytokine storm in COVID-19 patients [12]).
-
2.
Inability to identify acute coronary mimics, i.e., no culprit lesions despite STEMI findings on EKG, and increased prevalence of takotsubo, myopericarditis, and possibly even spontaneous coronary artery dissection during acute infections [13,14].
-
3.
Increased utilization of resources because of increased length of stay and complications arising from thrombolytics. In an analysis of 29,190 STEMI patients from 229 hospitals participating in the Get With the Guidelines—Coronary Artery Disease (GWTG-CAD) database, in-hospital mortality (fibrinolytics 4.6% vs. primary PCI 3.3%, p = 0.001), length of stay (fibrinolytics 4 days vs. primary PCI 3 days, p < 0.001), and length of stay >4 days (fibrinolytics 39% vs. primary PCI 28%, p < 0.0001) were significantly higher in the group in which thrombolytics were used [15].
-
4.
The use of intensive care unit rooms for close monitoring after thrombolytic administration, which can be used for other sick patients.
-
5.
A recent study showed that about 31% of symptomatic patients with COVID-19 can go into acute respiratory distress syndrome [12], and there is an increased risk of alveolar hemorrhage with thrombolytics [16].
A recent study from New York City shows that there is a high prevalence of non-obstructive disease with high mortality (72%). However, only half of the patients underwent coronary angiography [17]. In another study from Italy on 28 COVID-19 patients with STEMI, all of them underwent coronary angiography and none was treated with fibrinolysis. Out of 28 patients, 61% had a culprit lesion, and about 40% did not have obstructive coronary artery disease [18].
Cardiac involvement in the clinical course of COVID-19 infection is common [19]. Zhou et al. showed that 17% of patients had acute cardiac injury [12]. There have been several case reports [[20], [21], [22]] of patients with viral infections and acute myocarditis noted to have STEMI on the EKG. While cardiac magnetic resonance imaging (MRI) can accurately distinguish infectious myocarditis from other etiologies, it is often not available readily at all institutions. Thrombolysis in this group of patients with myocarditis and non-obstructive coronary arteries would be deleterious.
Given all of these problems, we recommend primary PCI. There is longstanding and strong evidence of the proven benefit with primary PCI [2,15]. The two major problems are potentially exposing the catheterization laboratory team and EMS personnel to the infection and delay in delivering care.
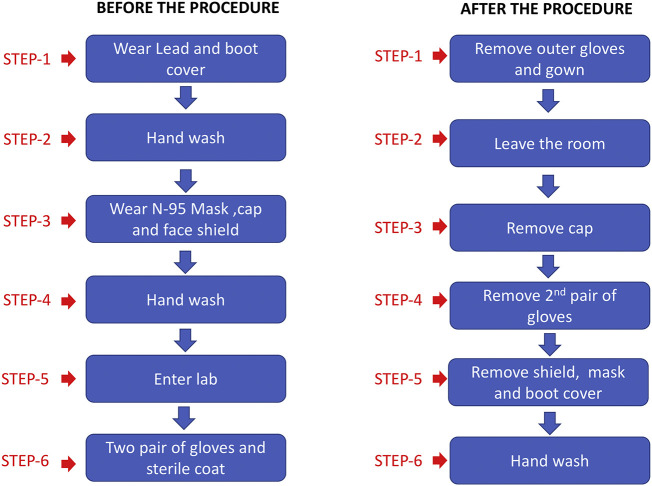
4. Preparation of cardiac catheterization laboratories
The risk of infection can be reduced if important steps are followed in all laboratories as proposed by the American College of Cardiology's Interventional Council and SCAI [23]. First and foremost, training of catheterization lab personnel on how to use personal protective equipment is critical. The six steps of “donning” and “doffing” (Fig. 4 ) should be followed by everyone in the catheterization lab. Other important steps that need to be followed by the catheterization lab are:
-
-
Allocating resources, i.e., always having a team as a backup and avoiding having two interventionalists in one procedure.
-
-
Training EMS personnel on infection control measures when transferring the patient to either the ED or the catheterization laboratory.
-
-
Designating one or two catheterization laboratory rooms exclusively for these patients and removing most supplies to avoid cross-contamination.
-
-
Performing deep cleaning after every procedure.
-
-
Cohorting COVID-19 patients.
-
-
Avoiding endotracheal intubation because of the use of positive pressure ventilation in all catheterization labs, as it might increase aerosolization. There should be a low threshold to perform endotracheal intubation for respiratory support in patients with borderline respiratory status or hemodynamic compromise to avoid “emergent” intubation in the catheterization laboratory.
Fig. 4.
Six rules of “donning” and “doffing” personal protective equipment.
If a patient is already transferred to a floor or unit and needs another procedure such as right heart catheterization, pulmonary artery catheter placement, intra-aortic balloon pump, extracorporeal membrane oxygenation, pericardiocentesis, or temporary transvenous pacemaker, it should be done at the bedside rather than in the catheterization lab.
If these steps are not followed, the risk of exposing the staff outweighs any benefit of primary PCI. Also, as the prevalence of COVID-19 increases in the community with an increase in asymptomatic carriers [24], every patient presenting to the catheterization lab should be considered COVID-19-positive until proven otherwise. Finally, every effort should be made to centralize COVID-19-trained catheterization laboratories and primary PCI care; if possible, STEMI cases should be taken by EMS or transferred to that facility. If we follow all of these precautions, delay in STEMI care should decrease even during this pandemic.
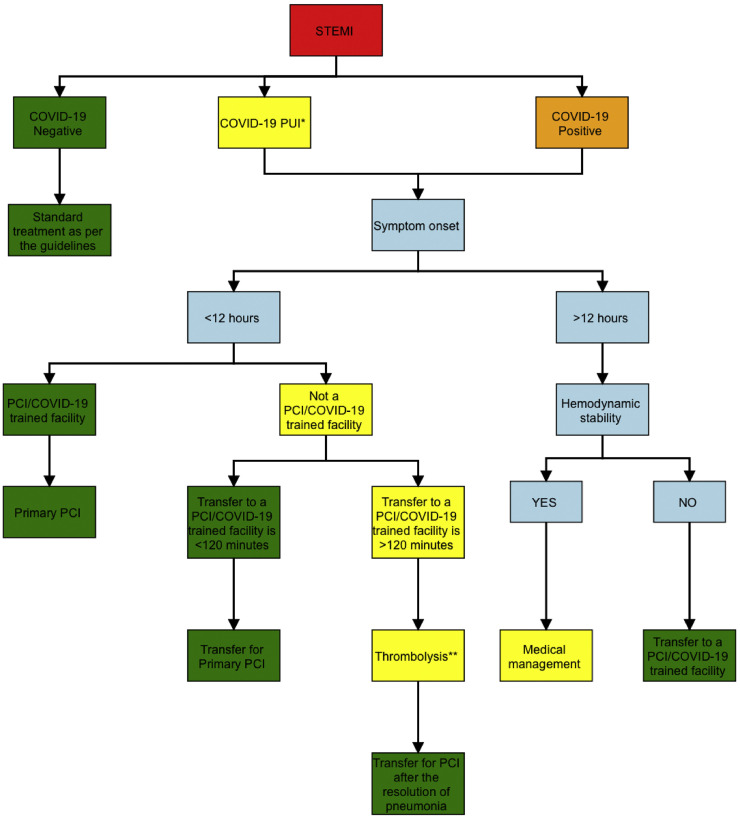
5. Proposed treatment algorithm for management of STEMI during COVID-19
We propose the following treatment algorithm for STEMI during COVID-19 (Fig. 5 ). If a patient is COVID-19-negative, standard treatment as per the guidelines should be followed. Both COVID-19 patients under investigation and COVID-19-positive patients should be treated similarly, as there could be a delay in test results, which can be harmful in STEMI patients. Only patients with symptom onset of <12 h should be evaluated for either thrombolytics or primary PCI. If a patient presents to a COVID-19-trained and PCI-capable facility, primary PCI should be performed. All the infection precaution steps should be followed by the team, and every effort should be made to achieve ideal door-to-balloon times. If a patient presents to a non-COVID-19-trained lab or a non-PCI-capable hospital and the transfer to a COVID-19-trained/PCI-capable facility can happen within 120 min, it should be initiated. However, if the transfer cannot happen within 120 min, thrombolysis should be performed, and concomitant medical management with aspirin, clopidogrel, heparin, or enoxaparin should be followed, as per the guidelines [9,10]. Before thrombolysis is administered, acute coronary syndrome mimics should be ruled out by careful evaluation of the EKG to rule out myopericarditis, and point-of-care ultrasound should be used to evaluate for new wall-motion abnormality. Signs of delayed myocardial enhancement on cardiac CT acquired after the iodinated contrast can be helpful [25,26], and this can be considered in facilities with no cardiac MRI. All unstable patients after thrombolysis should promptly be transferred to COVID-19-trained catheterization labs, and stable patients should be transferred after the resolution of pulmonary symptoms.
Fig. 5.
Treatment algorithm for management of STEMI during COVID-19.
*COVID-19 person under investigation: Any patient with fever or cough or shortness of breath with an elevated biomarker (C-reactive protein or lactate dehydrogenase) but a negative rapid COVID-19 test.
** Rule out ACS mimics before administering thrombolysis such as myocarditis, takotsubo cardiomyopathy, or pericarditis by careful evaluation of EKG and point-of-care ultrasound.
STEMI - ST-segment elevation myocardial infarction.
PCI - Percutaneous coronary intervention. PUI - Patient under investigation.
6. Conclusion
Treatment of STEMI patients during a pandemic is challenging. While thrombolysis can potentially be a good choice, many patients have a contraindication, and if thrombolysis is given, it would end up using more resources in these finite hospital settings. Also, with the high probability of the coronary angiogram showing normal coronary arteries during acute infections and pandemics, it is imperative for physicians to use primary PCI as the initial preferred strategy in these stressful situations rather than blindly choosing thrombolytics. Non-invasive diagnostic testing may be useful to differentiate true STEMIs from mimics. In addition, training of cardiac catheterization personnel on how to use personal protective equipment is crucial to limit the risk of acquiring infection.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
Ron Waksman – Advisory Board: Amgen, Boston Scientific, Cardioset, Cardiovascular Systems Inc., Medtronic, Philips, Pi-Cardia Ltd.; Consultant: Amgen, Biotronik, Boston Scientific, Cardioset, Cardiovascular Systems Inc., Medtronic, Philips, Pi-Cardia Ltd.; Grant Support: AstraZeneca, Biotronik, Boston Scientific, Chiesi; Speakers Bureau: AstraZeneca, Chiesi; Investor: MedAlliance.
Gary S. Mintz - Honoraria from Boston Scientific, Philips, Terumo, and Medtronic.
All other authors – None.
References
- 1.CDC. COVID-19 updates. Available athttps://www.cdc.gov/coronavirus/2019-ncov/cases-updates/summary.html. Accessed on April 6th 2020.
- 2.Granger C.B., Bates E.R., Jollis J.G., Antman E.M., Nichol G., O’Connor R.E. Improving care of STEMI in the United States 2008 to 2012. J Am Heart Assoc. 2019;8 doi: 10.1161/JAHA.118.008096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.De Filippo O., D’Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tam C.-C.F., Cheung K.-S., Lam S., Wong A., Yung A., Sze M. Impact of coronavirus disease 2019 (COVID-19) outbreak on ST-segment–elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scholz K.H., Maier S.K.G., Maier L.S., Lengenfelder B., Jacobshagen C., Jung J. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J. 2018;39:1065–1074. doi: 10.1093/eurheartj/ehy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Szerlip M., Anwaruddin S., Aronow H.D., Cohen M.G., Daniels M.J., Dehghani P. Considerations for cardiac catheterization laboratory procedures during the COVID-19 pandemic perspectives from the Society for Cardiovascular Angiography and Interventions Emerging Leader Mentorship (SCAI ELM) Members and Graduates. Catheter Cardiovasc Interv. 2020;96:586–597. doi: 10.1002/ccd.28887. [DOI] [PubMed] [Google Scholar]
- 7.Wood D.A., Sathananthan J., Gin K., Mansour S., Ly H.Q., Quraishi A.U. Precautions and procedures for coronary and structural cardiac interventions during the COVID-19 pandemic: guidance from Canadian Association of Interventional Cardiology. Can J Cardiol. 2020;36:780–783. doi: 10.1016/j.cjca.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Detect COVID-19 in as little as 5 minutes. Available at https://www.abbott.com/corpnewsroom/product-and-innovation/detect-covid-19-in-as-little-as-5-minutes.html. Accessed on April 6, 2020.
- 9.Ibanez B., James S., Agewall S., Antunes M.J., Bucciarelli-Ducci C., Bueno H. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 10.O’Gara P.T., Kushner F.G., Ascheim D.D., Casey D.E., Jr., Chung M.K., de Lemos J.A. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–e425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 11.Zeng J., Huang J., Pan L. How to balance acute myocardial infarction and COVID-19: the protocols from Sichuan Provincial People’s Hospital. Intensive Care Med. 2020;46:1111–1113. doi: 10.1007/s00134-020-05993-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yerasi C., Koifman E., Weissman G., Wang Z., Torguson R., Gai J. Impact of triggering event in outcomes of stress-induced (Takotsubo) cardiomyopathy. Eur Heart J Acute Cardiovasc Care. 2017;6:280–286. doi: 10.1177/2048872616633881. [DOI] [PubMed] [Google Scholar]
- 14.Wang K., Asinger R.W., Marriott H.J. ST-segment elevation in conditions other than acute myocardial infarction. N Engl J Med. 2003;349:2128–2135. doi: 10.1056/NEJMra022580. [DOI] [PubMed] [Google Scholar]
- 15.Hira R.S., Bhatt D.L., Fonarow G.C., Heidenreich P.A., Ju C., Virani S.S. Temporal trends in care and outcomes of patients receiving Fibrinolytic therapy compared to primary percutaneous coronary intervention: insights from the get with the guidelines coronary artery disease (GWTG-CAD) registry. J Am Heart Assoc. 2016;5 doi: 10.1161/JAHA.116.004113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Narayanan S., Thulaseedharan N.K., Subramaniam G., Panarkandy G., Arathi N. Pulmonary alveolar hemorrhage following thrombolytic therapy. Int Med Case Rep J. 2017;10:123–125. doi: 10.2147/IMCRJ.S129087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bangalore S., Sharma A., Slotwiner A., Yatskar L., Harari R., Shah B. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stefanini G.G., Montorfano M., Trabattoni D., Andreini D., Ferrante G., Ancona M. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141:2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Inciardi R.M., Lupi L., Zaccone G., Italia L., Raffo M., Tomasoni D. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5:819–824. doi: 10.1001/jamacardio.2020.1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shahid M., Hoey E., Basavarajaiah S. Acute myocarditis and ST-segment elevation. Am J Cardiol. 2016;118:1605–1608. doi: 10.1016/j.amjcard.2016.08.031. [DOI] [PubMed] [Google Scholar]
- 21.Ang K.P., Quek Z.Q., Lee C.Y., Lu H.T. Acute myocarditis mimicking ST-elevation myocardial infarction: a diagnostic challenge for frontline clinicians. Med J Malaysia. 2019;74:561–563. [PubMed] [Google Scholar]
- 22.Park S.C., Crane I.M., Pal K., Cagnina R.E. Rabies encephalitis with myocarditis mimicking ST-elevation myocardial infarction. Open Forum Infect Dis. 2019;6(ofz260) doi: 10.1093/ofid/ofz260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Welt F.G.P., Shah P.B., Aronow H.D., Bortnick A.E., Henry T.D., Sherwood M.W. Catheterization laboratory considerations during the coronavirus (COVID-19) pandemic: from the ACC’s Interventional Council and SCAI. J Am Coll Cardiol. 2020;75:2372–2375. doi: 10.1016/j.jacc.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bai Y., Yao L., Wei T., Tian F., Jin D.Y., Chen L. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brooks M.A., Sane D.C. CT findings in acute myocarditis: 2 cases. J Thorac Imaging. 2007;22:277–279. doi: 10.1097/RTI.0b013e31803ecefa. [DOI] [PubMed] [Google Scholar]
- 26.Trobs M., Brand M., Achenbach S., Marwan M. Ultra-low dose comprehensive cardiac CT imaging in a patient with acute myocarditis. J Cardiovasc Comput Tomogr. 2014;8:475–476. doi: 10.1016/j.jcct.2014.09.001. [DOI] [PubMed] [Google Scholar]