Abstract
The emergence and continued evolution of the transporter field has caused reevaluation and refinement of the original principles surrounding drug disposition. In this paper, we emphasize the impact that transporters can have on volume of distribution and how this can affect the other major pharmacokinetic parameters. When metabolic drug-drug interactions or pharmacogenomic variance change the metabolism of a drug, the volume of distribution appears to be unchanged while clearance, bioavailability, and half-life are changed. When transporters are involved in the drug-drug interactions or pharmacogenomic variance, the volume of distribution can be markedly affected causing counterintuitive changes in half-life. Cases are examined where a volume of distribution change is significant enough that although clearance decreases, half-life decreases. Thus, drug dosing decisions must be made based on CL/F changes, not half-life changes, as such volume of distribution alterations will also influence the half-life results.
Keywords: Transporters, Volume of Distribution, Clearance, Half-Life, Mean Residence Time
INTRODUCTION: THE USES OF PHARMACOKINETICS AND THE BASIC PARAMETERS
For many years, we have taught the therapeutic triangle as depicted in Fig. 1. We define pharmacodynamics as describing what the drug does to the body. Pharmacokinetics is the inverse describing what the body does to the drug (1–3). Pharmacokinetics, which relates the dose of a drug to the concentration in the body at some site has two potential uses: a) as a tool in therapeutics and b) as a tool in defining drug disposition. Pharmacokinetics can be described in terms of four basic characteristics: clearance, half-life, volume of distribution and bioavailability. How one employs these four basic parameters depends upon whether pharmacokinetics is used a tool in therapeutics or as a tool in defining drug disposition.
Fig. 1.
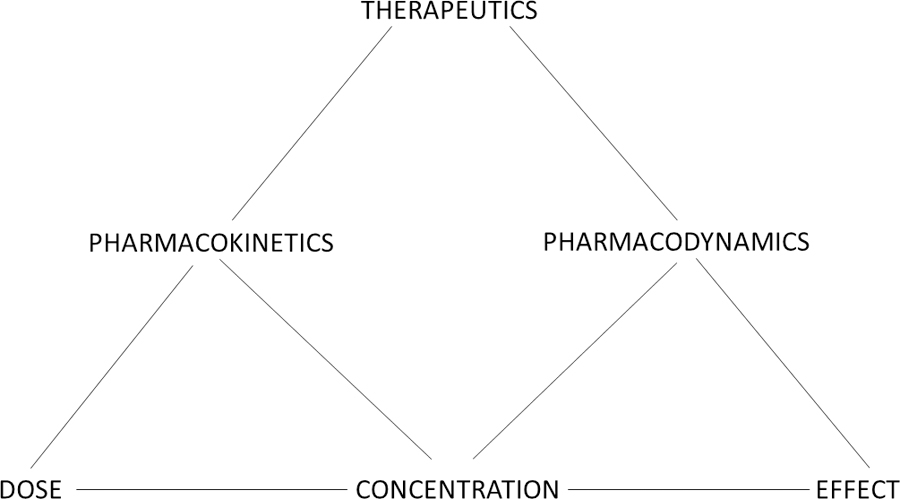
The therapeutic triangle.
When pharmacokinetics is used as a tool in therapeutics, clearance (CL) dictates the dosing rate (mass/time), modified by bioavailability (F) when the route of administration is not directly into the systemic circulation as for an intravenous dose. That is, as given in Equation 1 the exposure of the patient to the drug as measured by the area under the systemic concentration time curve (AUC) is the available dose (F·D) divided by clearance.
| (1) |
When pharmacokinetics is used as a tool in characterizing drug disposition, clearance is a measure of the body’s ability to eliminate the drug and bioavailability is a measure of the fraction of the drug dose that reaches the systemic circulation as a function of absorption limitations, intestinal metabolism and first-pass hepatic loss.
When pharmacokinetics is used as a tool in therapeutics, half-life dictates the dosing interval. For example, if in Eq. 1 the dosing rate was determined to be 1,440 mg/day, knowledge of the therapeutic window from a pharmacodynamic evaluation would lead to giving the drug 1,440 mg once a day, 720 mg twice a day, 360 mg every six hours or an infusion of 1 mg/min for 24 hours, all being equivalent dosing rates. Knowledge of the half-life and the therapeutic window would help in the selection of dose and dosing interval, knowing that if the drug were dosed every half-life, accumulation upon multiple dosing would only be 2-fold that found for the first dose and the peak-to-trough ratio would also be 2. In contrast, when pharmacokinetics is used as a tool in characterizing drug disposition half-life is much less useful since it is a dependent variable reflecting both clearance, a measure of the body’s ability to eliminate drug, and volume of distribution, the theoretical space available into which the drug may distribute. That is, as given in Eq. 2, the total body half-life at steady state (t1/2,steady state) divided by the logarithm of 2 yields the mean residence time (MRT), which equals volume of distribution steady state (Vss) divided by clearance (4):
| (2) |
where the t½ value reflects a single overall half-life for the drug that will predict accumulation of drug in the body at steady-state following multiple intravenous bolus doses. The relationship between terminal half-life and MRT, which has been evaluated in detail by Sobol and Bialer (5), cannot be described by Eq. 2. Here we address small molecule pharmacokinetics, Mager and Jusko (6) have discussed the potential disconnect between CL, Vss and terminal half-life for macromolecules.
RECOGNITION OF CHANGES IN VOLUME OF DISTRIBUTION AND THEIR RELEVANCE
In general, most predictions of the effects of disease states, pharmacogenomic variance and drug-drug interactions have ignored the volume term in Eq. 2 with the expectation that when clearance decreases half-life will get longer and when clearance increases half-life will get shorter. This appears to be a reasonable omission for drug-drug interactions and pharmacogenomic variants related to metabolism changes, since as we have recently reported (7), we are not aware of any clinically significant changes in drug volume of distribution that result from metabolic changes only. However, this may not be true for disease state changes. As early as 1975, Klotz et al. (8) showed that the change in diazepam half-life with age was independent of clearance changes. We reported this importance of evaluating volume of distribution changes on half-life as early as 1985 in our Goodman and Gilman chapter (2).
TRANSPORTER INTERACTIONS CAN MARKEDLY CHANGE VOLUME OF DISTRIBUTION
This general belief in the inverse relationship between clearance and MRT (or whole body half-life) became established in pharmacokinetics long before the importance of drug transporters on drug disposition was recognized. In our recent paper discussing the theory and critical analyses of the extended clearance concept following oral and intravenous dosing (9) we reviewed the published studies from our laboratory beginning in 2007 in which OATP substrates were orally dosed to humans under control conditions and when a single intravenous dose of rifampin was administered concomitantly to inhibit hepatic uptake of the substrate. Results from those oral dosing studies of atorvastatin (10), glyburide (11) and rosuvastatin (with both White and Asian subjects wild-type for both OATP1B1 and BCRP) (12) are summarized in Table I. The values given are the ratios of the pharmacokinetic parameters in the rifampin phase when the victim drug is orally dosed concomitantly with a single IV rifampin dose to inhibit hepatic uptake transporters divided by the measurement in the control phase in the absence of rifampin. Since these three drugs are all substrates of OATPs and rifampin is a potent inhibitor of OATPs, we would expect the area under the curve to increase with concomitant IV rifampin dosing as the victim drug is inhibited from entering the hepatocytes by rifampin. The clearance ratios are just the inverse of the AUC ratio. That is, changes in transporter activity can change clearance independent of metabolic elimination processes (9) as we show with the relevant equations in the last section of this tutorial in explaining the Table I glyburide results with and without induction.
Table I.
Ratio of pharmacokinetic parameters (IV rifampin phase/control phase)
| Drug | |||||
|---|---|---|---|---|---|
| Atorvastatin | 7.7 | 0.14 | 0.056 | 0.44 | 0.39 |
| Rosuvastatin (Whites) | 3.6 | 0.27 | 0.082 | 0.30 | 0.63 |
| Rosuvastatin (Asians) | 3.2 | 0.30 | 0.103 | 0.33 | 0.59 |
| Glyburide (noninduced) | 2.2 | 0.45 | 0.32 | 0.71 | 0.77 |
| Glyburide (induced) | 2.2 | 0.45 | 0.43 | 0.96 | 0.91 |
In the last two columns of Table I the terminal half-life and MRT ratios are given. Here we see the counterintuitive result from what would be expected. Intravenous rifampin following oral dosing of these OATP substrates causes AUC to increase and clearance to decrease, but half-life and MRT get shorter, not longer. When CL/F is decreased in the presence of rifampin in Table I, half-life and MRT are never increased, the outcome expected for inhibition of hepatic uptake. The half-life and MRT ratios differ slightly since MRT considers the whole body for these multicompartment drugs whereas the terminal half-life reflects the systemic concentrations following cessation of dosing. What is the reason for these counterintuitive results? These outcomes result from the fact that when transporters play a significant role in drug disposition, volume of distribution changes can be different than clearance changes, as first noted by our laboratory (13), since transporters are not only present in the liver but in many organs of the body, and thus when transporters are inhibited distribution will change in a differential manner from hepatic clearance. Thus, the magnitude of change in terminal half-life and MRT is not predicted by changes in clearance alone, due to significant changes in volume of distribution. As seen for atorvastatin, when CL/F decreases 86% with concomitant rifampin dosing, Vss/F decreases 94.4%, resulting in a 61% decrease in terminal half-life and a 56% decrease in MRT. Similarly, a large discontinuity between the clearance and Vss ratios is observed for rosuvastatin in Asians and Whites resulting in a 37 to 41% decrease in terminal half-life and a 67 to 70% decrease in MRT. Glyburide, studied in both induced and non-induced states, showed a 55% decrease in CL/F for both conditions, however Vss/F also decreased 57% (induced) and 68% (non-induced), resulting in no change in terminal half-life and MRT for the induced condition, and only a 23% and 29% change in terminal half-life and MRT for the non-induced condition. These changes cannot be attributed to differences in bioavailability since this term is in both the clearance and volume ratio relationships (Eq. 2).
Lesson to be learned:
When transporters are significantly involved in drug disposition, changes in transporter activity due to drug-drug interactions, pharmacogenomic variance and disease states can result in differential changes in clearance and volume of distribution that result in discordance of changes between clearance and half-life, even to the point that half-life decreases when clearance decreases. The role of volume of distribution changes should not be ignored, since even significant changes in AUC or clearance may not be quantitatively reflected in MRT or terminal half-life due to a more significant change in volume of distribution. Alterations in the amount of drug dosed should be based on AUC (CL/F) changes, although dosing interval may also require changes based on half-life for drugs exhibiting narrow therapeutic indices.
VOLUME OF DISTRIBUTION CHANGES DUE TO TRANSPORTER INTERACTIONS MAY BE EQUAL IN MAGNITIUDE TO CLEARANCE CHANGES AND WILL NOT RESULT IN HALF-LIFE CHANGES
Our glyburide data would suggest that there may not always be a differential effect of transporter inhibition on clearance and volume of distribution. In that study (11), concomitant intravenous dosing of 600 mg rifampin following a single 10 mg oral dose of glyburide versus a control single oral dose of glyburide caused AUC to increase 2.2-fold. These same subjects were then reexamined when enzymes were induced by multiple rifampin dosing, again yielding the same increase in AUC with concomitant IV dosing of rifampin, highlighting that the magnitude of change resulting from the transporter interaction is unaffected by metabolic enzyme induction. The scientific explanation for this outcome is addressed the last section of the tutorial. In our glyburide study, no significant differences are seen between induced and non-induced conditions for the Vss/F, MRT and t1/2,z values. Since volume of distribution and clearance decreased by concomitant IV dosing of rifampin to similar degrees in the induced state, there are minimal changes in the observed MRT and terminal half-life.
Lesson to be learned:
a) Not all transporter activity changes will lead to differential CL and Vss changes; b) the extent of drug-drug uptake transporter interactions will be the same independent of changes in metabolic interactions (i.e., induced versus non-induced conditions) as will be shown subsequently in the AUC/Doseoral equation.
METABOLIC INTERACTIONS DO NOT APPEAR TO CHANGE VOLUME OF DISTRIBUTION BUT ANALYSIS OF ORAL DOSING PHARMACOKINETICS IS CHALLENGING DUE TO POTENTIAL BIOAVAILABILITY CHANGES
Although most clinically relevant pharmacokinetic changes due to drug interactions, pharmacogenomic variance and disease states are observed following oral drug dosing, much of the theory taught to clinicians and drug development scientists is based on intravenous drug dosing. We address this issue in more detail in the following section. Analysis of a 1998 study (14) of the effect of clarithromycin dosing on oral and IV midazolam pharmacokinetics illustrates the difficulties one encounters when only oral drug-drug interaction data are available. Midazolam, a Class 1 BDDCS drug where no clinically significant transporter effects would be expected or observed, is a substrate of CYP3A4, an enzyme inhibited by clarithromycin. As shown in Table II, with concomitant clarithromycin dosing, IV midazolam AUC increases 2.7-fold, which is also observed for the change in the terminal half-life (2.7-fold) and MRT (3-fold), since Vss and V1 (volume of distribution for the central compartment) did not change significantly (ratios of 1.1 and 1.0, respectively) as we expect for metabolic drug interactions (7). However, when the clarithromycin oral midazolam drug interaction is evaluated AUC increases 7.1-fold, CL/F decreases to 0.14 and Vss/F decreases to 0.35. Here again there is a discontinuity between the CL/F and Vss/F ratios so that the changes in half-life (2.6-fold) and MRT (2.7-fold) are quite different than that observed for AUC or CL/F. This is a result of the marked effect of clarithromycin on bioavailability where the ratio increases 2.4-fold, primarily as a function of gut bioavailability (FG) increasing 2.0-fold versus the hepatic first-pass increase in bioavailability (FH), which only increases 1.2-fold (14). However, we only know these changes in F because an IV drug interaction study was also carried out, not the usual information available for an oral interaction study.
Table II.
Ratios of midazolam blood pharmacokinetic parameters with/without 7 days of clarithromycin dosing
| IV Midazolam Ratios | Parameter | Oral Midazolam Ratios |
|---|---|---|
| 2.7 | AUC | 7.1 |
| 1.3 | Cmax | 3.3 |
| 0.37 | CL CL/F F, FH, FG |
0.14 2.4, 1.2, 2.0 |
| 1.1 1.0 |
Vss Vss/F V1 |
0.35 |
| 2.7 | t½terminal | 2.6 |
| 3.0 | MRT | 2.5 |
AUC, CL, F and t1/2terminal values as reported by Gorski et al. (12) using weight corrected values for AUC and CL; Cmax, Vss, V1 and MRT determined from digitized data from figures of average concentration time curves.
Other interesting results are seen in Table II, reflecting points raised in our recent paper (7), “Understanding drug-drug interactions and pharmacogenomic changes in pharmacokinetics for metabolized drugs”. First, maximum concentration (Cmax) ratios are markedly less affected by enzyme inhibition than AUC ratios. As we previously pointed out (9), AUC for both single and multiple drug doses accurately reflect the change in clearance and bioavailability. At steady-state, Cmax changes will approximate AUC changes, but following a single dose under inhibited conditions the Cmax ratio will be markedly less if accumulation occurs with multiple dosing, since Cmax observed at steady-state is greater than the single dose Cmax due to accumulation. Secondly, as we previously pointed out (5), a significant difference between the AUC ratio and the half-life ratio following oral dosing indicates a marked first pass loss condition. Here, for midazolam, a relatively low hepatic extraction ratio drug where the FH ratio is only 1.2, the marked difference between the AUC and half-life ratios is primarily a function of FG (ratio = 2.0) for this CYP3A substrate.
Lesson to be learned:
Following oral dosing, drug-drug interactions and pharmacogenomic variance can also frequently lead to differential clearance and half-life changes, but for variations due to metabolism alone, half-life will never decrease when clearance decreases. These differential changes result from changes in FH and FG. First dose Cmax ratios for the victim drug may be markedly different than the AUC ratio.
CHANGES IN HALF-LIFE SHOULD NOT BE USED IN MAKING ORAL DRUG DOSING DECISIONS FOR DRUG-DRUG INTERACTIONS AND PHARMACOGENOMIC VARIANCE OUTCOMES
In Table I we demonstrated how transporter effects could change volume of distribution differentially from clearance and thus showing why making drug dosing adjustments based on half-life would be inappropriate. Here we show that when only oral data is available, drug dosing decisions should never be made based on changes in half-life whether or not there are transporter interactions. The oral midazolam results in Table II point out the unfortunate confounding aspects of the recent publication of Jelliffe and Bayard in this journal (15). These authors argue that both clearance and elimination rate constant approaches are mathematically proven equally valid in “training clinical pharmacokineticists and physicians to manage drug therapy optimally for patients under their care in their everyday practice”. However, that analysis was based on equations for a drug following a one compartment pharmacokinetic model for intravenous dosing. One can readily see from the oral midazolam ratios in Table II that clearly the CL/F parameter, the inverse of the AUC ratio, is the relevant value clinicians must consider in adjusting midazolam doses with concomitant clarithromycin administration. Measuring the half-life change would provide no clinically useful information with respect to drug dose. Knowing that clearance and elimination rate constant approaches are equally valid as claimed by Jelliffe and Bayard (15) for IV dosing when a drug follows one-compartment pharmacokinetics provides clinicians with no useful information. The use and devising of pharmacokinetic theoretical analyses using a one- compartment model following IV dosing continues to plague the rational understanding of pharmacokinetic principles in drug dosing and the use of pharmacokinetics as a tool in defining drug disposition. As we noted in 2008 (16), all of the equations utilized to predict drug accumulation in the literature and in pharmacokinetic textbooks do not provide the correct numbers since they are all based on IV drug dosing for a drug following a one compartment model.
Lesson to be learned:
Theoretical pharmacokinetic analyses based only on intravenous drug dosing can be very misleading when observing data following oral dosing. Drug dosing decisions and recommendations for drug dosing changes (i.e. the dosing rate) must be based on CL/F (the inverse of AUC) changes, not half-life (rate constant) changes.
PERSPECTIVE: INCORPORATING TRANSPORTER EFFECTS IN DEFINING DRUG PHARMACOKINETICS IS ONLY CONSISTENT WITH THE WELL-STIRRED MODEL OF HEPATIC ELIMINATION
Transporters have also changed basic pharmacokinetic understanding with respect to models of hepatic elimination. Transporters have been incorporated into hepatic clearance models via the extended clearance concept as we recently reviewed (9). It is well recognized that the extended clearance concept as used in pharmacokinetics assumes that hepatic elimination is described by the well-stirred model (17–23), but it is not clearly indicated why this must be so. Solving for the change in the total amount of drug within the hepatocyte (AH) with time is given by
| (3) |
where PSinf,int for basolateral influx (inf) and efflux (eff) into and out of the hepatocyte, respectively, are the intrinsic membrane passage clearances that are composed of both active intrinsic transporter clearances as well as passive intrinsic diffusional processes; fu values are fraction unbound in the blood (B) and in the hepatocyte (H), respectively; CLH,int parameters are the intrinsic clearances for irreversible drug removal from the hepatocyte via metabolism (CLH,int,met) and biliary clearance (CLH,int,bil); C values are total drug concentrations driving basolateral efflux, metabolism and biliary excretion in the liver and the blood concentration driving influx as indicated by the subscripts. We have differentiated the three driving force concentrations within the liver since one would not expect that the concentration in the liver at the basolateral border driving efflux was necessarily the same as the concentration at the apical border driving biliary excretion nor the average concentration within the liver driving metabolism. This differentiation of concentrations within the hepatocyte/liver is inherent when clearance is defined in terms of the parallel tube or axial dispersion models. However, this conundrum of differential concentrations can be solved by assuming the well-stirred model where all concentrations within the hepatocyte/liver are equivalent as given in Eq. 4.
| (4) |
At steady state where the left hand sides of Eqs. 3 and 4 become zero, then using the well-stirred model, the liver clearance can be calculated as we (9) and others (17–23) have shown yielding Eq. 5.
| (5) |
and following oral dosing (9) leading to Eq. 6
| (6) |
It is Eq. 6 that explains the glyburide AUC results in Table I, where inhibiting hepatic uptake (PSinf,int) by dosing intravenous rifampin causes the same change in AUC under induced and noninduced conditions independent of the other parameters in Eq. 6 (particularly FG and CLH,int) when metabolism is induced by continuous rifampin dosing.
Although it is well recognized that when transporters are included in the derivation of organ clearance this is only consistent with the well-stirred model, investigators and particularly the physiologic based pharmacokinetic (PBPK) model programs define clearance within the organ using the axial dispersion model. This is incorrect and unjustified. As we recently noted (9) the recognition that the extended clearance concept is derived from the well-stirred model explains why PBPK models function best with multiple (often 5) consecutive liver compartments when hepatic availability is low. Each well-stirred model compartment can only decrease concentrations by a single step, since there is no incremental metabolism in the well-stirred model in contrast to the parallel tube and axial dispersion models. However, the incremental process can be mimicked by this series of consecutive well-stirred model steps utilized in the PBPK models as recently analyzed by Li et al. (24).
Lesson to be learned:
Models incorporating the possibility of transporter effects, including PBPK models, are only consistent with the well-stirred model, and this model of organ elimination does an adequate job of allowing investigators to use various approaches to predict drug-drug, pharmacogenomic variance and disease state changes in drug pharmacokinetics.
CONCLUSIONS
The recognition of the importance of transporters with respect to drug disposition has led to further refinements in the pharmacokinetic interpretation of drug disposition. It appears that metabolic drug-drug interactions and pharmacogenomic variance affecting metabolism of drugs only effects clearance, bioavailability and half-life with volume of distribution being unchanged. However, when transporters are an important aspect of drug disposition, drug-drug interactions and pharmacogenomic variance can also result in differential marked changes in volume of distribution, thereby affecting half-life to the extent that counterintuitive outcomes can result where decreased clearance can result in a faster rather than a slower half-life. This is crucial to recognize as examining only MRT or terminal half-life changes may mask significant CL/F or AUC changes due to an equally significant volume of distribution change. The lessons learned in this tutorial came about after we recognized that transporter drug-drug interactions (DDIs) can result in changes in volume of distribution in addition to clearance, but that this was not true when DDIs were only metabolic. Analysis of oral dosing pharmacokinetic interaction studies (in the absence of IV interaction data) can potentially be misleading if changes in bioavailability are not properly recognized. It is also important to note that models incorporating such transporter effects are only consistent with the well-stirred model of hepatic disposition.
AKNOWLEDGEMENTS
This work was supported in part by a Mary Ann Koda-Kimble Seed Award for Innovation. Dr. Benet is a member of the UCSF Liver Center supported by NIH grant P30 DK026743. Dr. Bowman was supported by the National Science Foundation Graduate Research Fellowship Program (Grant 1144247) and a Pharmaceutical Research and Manufacturers of America Foundation Pre-doctoral Fellowship in Pharmaceutics. Ms. Sodhi was supported in part by an American Foundation for Pharmaceutical Education Predoctoral Fellowship and NIGMS grant R25 GM56847.
Footnotes
COMPLIANCE WITH ETHICAL STANDARDS
Conflict of Interest The authors declare that they have no conflicts of interest to disclose.
REFERENCES
- 1.Benet LZ. Pharmacokinetics: Basic principles and its use as a tool in drug metabolism In: Mitchell JR, Horning MG, editors. Drug Metabolism and Drug Toxicity. New York: Raven Press; 1984. p. 199–211. [Google Scholar]
- 2.Benet LZ, Sheiner LB. Introduction; Pharmacokinetics: The dynamics of drug absorption, distribution, and elimination In: Gilman AG, Goodman LS, Rall TW, Murad F, editors. The Pharmacological Basis of Therapeutics. Seventh Edition. New York: Macmillan Publishing Company; 1985. Chapter 1, p. 1–34. [Google Scholar]
- 3.Benet LZ. Introductory lecture, “Pharmacokinetics for Pharmaceutical Scientists”, UCSF one week course first taught February 1986 and continuously each year since.
- 4.Benet LZ, Galeazzi RL. Noncompartmental determination of the volume of distribution steady-state. J Pharm Sci 1979;68:1071–4. [DOI] [PubMed] [Google Scholar]
- 5.Sobol E, Bialer M. The relationships between half-life (t1/2) and mean residence time (MRT) in the two-compartment open body model. Biopharm Drug Dispos 2004;25:157–62. [DOI] [PubMed] [Google Scholar]
- 6.Mager DE, Jusko WJ. General pharmacokinetic model for drugs exhibiting target-mediated drug disposition. J Pharmacokinet Pharmacodyn 2001;28:507–32. [DOI] [PubMed] [Google Scholar]
- 7.Benet LZ, Bowman CM, Koleske ML, Rinaldi CL, Sodhi JK. Understanding drug–drug interaction and pharmacogenomic changes in pharmacokinetics for metabolized drugs. J Pharmacokinet Pharmacodynam 2019;46:155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klotz U, Avant GR, Hoyumpa A, Schenker S, Wilkinson GR. The effects of age and liver disease on the disposition and elimination of diazepam in adult man. J Clin Invest 1975;55:347–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benet LZ, Bowman CM, Liu S, Sodhi JK. The extended clearance concept following oral and intravenous dosing: theory and critical analyses. Pharm Res 2018;35:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lau YY, Huang Y, Frassetto L, Benet LZ. Effect of OATP1B transporter inhibition on the pharmacokinetics of atorvastatin in healthy volunteers. Clin Pharmacol Ther 2007;81:194–204. [DOI] [PubMed] [Google Scholar]
- 11.Zheng HX, Huang Y, Frassetto LA, Benet LZ. Elucidating rifampin’s inducing and inhibiting effects on glyburide pharmacokinetics and blood glucose in healthy volunteers: unmasking the differential effects of enzyme induction and transporter inhibition for a drug and its primary metabolite. Clin Pharmacol Ther 2009;85:78–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wu H-F, Hristeva N, Chang J, Liang X, Li R, Frassetto L, Benet LZ. Rosuvastatin pharmacokinetics in Asian and white subjects wild type for both OATP1B1 and BCRP under control and inhibited conditions. J Pharm Sci 2017;106:2751–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grover A, Benet LZ. Effects of drug transporters on volume of distribution. AAPS J 2009;11:250–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gorski JC, Jones DR, Haehner-Daniels BD, Hamman MA, O’Mara EM, Hall SD. The contribution of intestinal and hepatic CYP3A to the interaction between midazolam and clarithromycin. Clin Pharmacol Ther 1998;64:133–43. [DOI] [PubMed] [Google Scholar]
- 15.Jelliffe R, Bayard D. New perspectives in clinical pharmacokinetics-1: the importance of updating the teaching in pharmacokinetics that both clearance and elimination rate constant approaches are mathematically proven equally valid. AAPS J 2018;20:36. [DOI] [PubMed] [Google Scholar]
- 16.Sahin S, Benet LZ. The operational multiple dosing half-life: a key to defining drug accumulation in patients and to designing extended release dosage forms. Pharm Res 2008;25:2869–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sirianni GL, Pang KS. Organ clearance concepts: new perspectives on old principles. J Pharmacokinet Biopharm 1997;25:449–70. [DOI] [PubMed] [Google Scholar]
- 18.Webborn PJH, Parker AJ, Denton RL, Riley RJ. In vitro-in vivo extrapolation of hepatic clearance involving active uptake: theoretical and experimental aspects. Xenobiotica 2007;37: 1090–109. [DOI] [PubMed] [Google Scholar]
- 19.Camenisch G, Umehara K. Predicting human hepatic clearance from in vitro drug metabolism and transport data: a scientific and pharmaceutical perspective for assessing drug-drug interactions. Biopharm Drug Dispos 2012;33:179–94. [DOI] [PubMed] [Google Scholar]
- 20.Barton HA, Lai Y, Goosen TC, Jones HM, El-Kattan AF, Gossed JR, Lin J, Varma MV. Model-based approaches to predict drug-drug interactions associated with hepatic uptake transporters: preclinical, clinical and beyond. Expert Opin Drug Metab Toxicol 2013;9:459–72. [DOI] [PubMed] [Google Scholar]
- 21.Varma MV, Steyn SJ, Allerton C, El-Kattan AF. Predicting clearance mechanism in drug discovery: extended clearance classification system (ECCS). Pharm Res 2015;32:3785–802. [DOI] [PubMed] [Google Scholar]
- 22.El-Kattan AF, Varma MVS. Navigating transporter sciences in pharmacokinetics characterization using the extended clearance classification system. Drug Metab Dispos 2018;46:729–39. [DOI] [PubMed] [Google Scholar]
- 23.Patilea-Vrana G, Unadkat JD. Transport vs. metabolism: what determines the pharmacokinetics and pharmacodynamics of drugs? Insights from the extended clearance model. Clin Pharmacol Ther 2016;100:413–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Li Z, Di L, Maurer TS. Theoretical considerations for direct translation of unbound liver-to-plasma partition coefficient from in vitro to in vivo. AAPS J 2019;18;21:43. [DOI] [PubMed] [Google Scholar]


