Abstract
Objective: We compared screening methods for asymptomatic venous thromboembolism (VTE) in patients with acute spine and spinal cord injuries (SCI). Patients were screened by D-dimer monitoring alone (DS group) or by D-dimer monitoring combined with ultrasonography (DUS group).
Design: Prospective cohort study.
Setting: One department of a university hospital in Japan.
Participants: 114 patients treated for acute SCI between 2011 and 2017.
Interventions: N/A.
Outcome Measures: D-dimers were measured upon admission and 1, 3, 5, 7, and 14 days thereafter. DUS-group patients also underwent an ultrasound 7 days after admission. If ultrasonography indicated deep venous thrombosis (DVT), or if D-dimer levels increased to ≥ 10 µg/mL, the patient was assessed for VTE, including DVT or pulmonary embolism (PE), by contrast venography. We analyzed the incidence of VTE detected in the DS and DUS groups.
Results: In the DS group, D-dimers were elevated (≥ 10 µg/mL) in 15 of 70 patients (21.4%), and 9 of the 15 had asymptomatic VTE (12.9%, DVT 11.4%, PE 5.7%). In the DUS group, one patient developed VTE on day 4, and D-dimers were elevated in 13 of 43 patients (30.2%), ultrasonography indicated DVT in 12 patients (27.9%), and asymptomatic VTE was diagnosed in 12 patients (27.9%, DVT 27.9%, PE 4.7%). The DUS group had a higher incidence of DVT (P = 0.002) and VTE (P = 0.042) than the DS group.
Conclusions: Combined D-dimer and ultrasound screening in patients with acute SCI improved the detection of VTE, including PE, compared with D-dimer screening alone.
Keywords: Spinal cord injury, Venous thromboembolism, D-dimer test
Introduction
Venous thromboembolism (VTE), which includes deep venous thrombosis (DVT) and pulmonary embolism (PE), is common in patients with acute spinal cord injuries (SCI). VTE has been reported at rates of 12−64% when diagnosed on clinical criteria alone.1 VTE accounts for 9.7% of the deaths occurring during the first year after SCI.1 Although contrast venography is the gold standard for diagnosing VTE, it is not suitable for the routine screening of asymptomatic patients, due to potential complications, technical issues, expense, and invasiveness.2 D-dimer, a fibrin degradation product, is a small protein fragment found in the blood after a blood clot is degraded by fibrinolysis.3 Although D-dimer testing shows promise for VTE screening,1,3–6 studies showed that D-dimer screening had low sensitivity and specificity after hip replacement, indicating that the D-dimer level alone is not sufficient to detect and diagnose DVT.7,8 Ultrasonography is the primary non-invasive method for investigating suspected DVT of the femoral vein and popliteal vein.5 Standard ultrasound showed relatively high sensitivity for proximal (more than 90%) or below-the-knee DVT (around 60%) in a systematic review and meta-analysis and meta-regression of diagnostic cohort studies.9 In this study, we screened patients with acute SCI by D-dimer testing only or by a combination of D-dimer and ultrasound. Indications of VTE, including PE, were investigated by contrast venography. We hypothesized that combined D-dimer and ultrasound screening would reduce the false negatives for VTE.
Materials and methods
Subjects
This prospective study included 114 patients (84 men and 30 women) who were treated for acute SCI between January 2011 and April 2017, and were admitted to our hospital immediately after injury. The average age when admitted was 60.2 years (range 17–89). Of the 114 patients, 56 were treated surgically within 1 week after injury and 58 received conservative therapy. On the American Spinal Injury Association (ASIA) Impairment Scale (AIS), there were 16 A, 10 B, 32 C, 16 D, and 40 E cases. There were 71 cervical, 14 thoracic, and 20 lumbar injuries, and 9 patients with both cervical and thoracic injuries. There were 30 patients with injuries in addition to SCI. None of the patients were using anticoagulants before the injury.
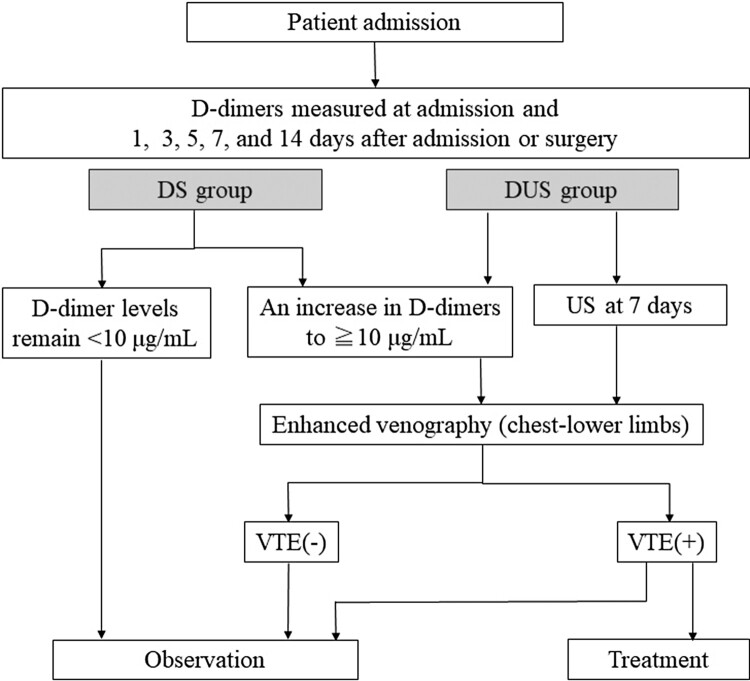
VTE screening protocol (Fig. 1)
Figure 1.
Prospective VTE-screening protocol. Patients whose D-dimer levels rose to ≥ 10 μg/mL during the acute recovery period, or whose ultrasound showed indications of DVT at 7 days post-injury, were screened immediately for VTE by contrast venography. Results were interpreted by radiologists in our hospital, and patients with VTE were treated as appropriate.
The D-dimer screening (DS) group consisted of patients who were admitted from January 2011 to January 2015; these patients were screened prospectively for VTE by measuring the D-dimer level at admission and at 1, 3, 5, 7, and 14 days after admission (or surgery). The combination screening (DUS) group consisted of patients admitted from February 2015 to April 2017; these patients were tested prospectively for VTE by D-dimer monitoring (as for the DS group) plus ultrasound screening conducted 7 days after admission (or surgery) by an experienced examiner using a Prosound Alpha-7 (Aloka, Tokyo). The ultrasound examiner was blinded to the results of the D-dimer testing. The DS-group patients gave informed consent for inclusion in a study using D-dimer screening alone beginning in January 2011. The DUS group patients gave informed consent for inclusion in a study using combination screening beginning in February 2015. All patients used elastic stockings and pneumatic compression foot/calf pumps (Kendal SCD EXPRESS, Dublin, Ireland) after admission to prevent VTE, and all patients started rehabilitation therapy immediately after admission or surgery. Patients were observed carefully for VTE symptoms such as chest pain, dyspnea, tachypnea, tachycardia, and decrease in blood pressure (for PE), and calf swelling, pain, skin-color change, and calf cramps (for DVT).1 Patients whose D-dimer level first reached 10 µg/mL at each time point after admission or whose ultrasound results indicated DVT were immediately assessed by contrast venography (computed tomography: CT) from the lower limbs to the chest using a Discovery HD 750 (GE Healthcare, Waukesha, WI). The results were interpreted by radiologists in our hospital. Patients diagnosed with VTE were examined by a vascular surgeon to see whether they needed anticoagulant treatment. Patients who were mobile and were diagnosed with PE or DVT were treated with heparin, warfarin, or edoxaban as deemed appropriate by a vascular surgeon. Elastic stockings and foot/calf pumps were removed if VTE was diagnosed.
Measurement of D-dimer levels
D-dimer levels were measured as described elsewhere.3 Briefly, a sample of venous blood was subjected to a latex immunoassay using an anti-human D-dimer antibody (Liatest D-dimer, Stago Inc., New Jersey, USA) and the STA-Liatest D-dimer assay, which has a detection limit of 0.4 µg/mL.
Statistical analysis
Data input and statistical calculations were performed using SPSS ver.12.0J (SPSS Inc., Chicago, IL, USA). D-dimer values and age were compared between DS and DUS patients and between VTE and non-VTE patients by the Mann-Whitney U-test. The sex, AIS score, injury level, additional injury, surgery, and incidence of VTE in the DS and DUS groups were analyzed by Chi-square test. Values were expressed as means ± S.D. P values < 0.05 were considered statistically significant.
Results
Characteristics of the DS and DUS groups (Table 1)
Table 1. Patient characteristics in the DS and DUS groups.
| DS group (n = 70) | DUS group (n = 44) | P value | |
|---|---|---|---|
| Age | 59.7 ± 18.8 | 65.4 ± 15.2 | 0.096 |
| Sex(men: women) | 49:21 | 35:9 | 0.284 |
| OS | 11.4% (8) | 31.8% (14) | 0.013* |
| Bony injury | 82.9% (58) | 40.9% (18) | 0.001* |
| AIS score | |||
| A | 10% (7) | 20.5% (9) | 0.259 |
| B | 5.7% (4) | 13.6% (6) | 0.181 |
| C | 27.1% (19) | 30.2% (13) | 0.673 |
| D | 17.1% (12) | 2.3% (4) | 0.278 |
| E | 40% (28) | 27.3% (12) | 0.232 |
| Injury level | |||
| Cervical | 58.6% (41) | 68.2% (30) | 0.328 |
| Thoracic | 10% (7) | 15.9% (7) | 0.389 |
| Lumber | 22.9% (16) | 9.1% (4) | 0.078 |
| Combined | 8.6% (6) | 6.8% (3) | 0.517 |
| Additional injury | 25.7% (18) | 27.3% (12) | 0.538 |
| Surgery | 53.3% (38) | 40.9% (18) | 0.183 |
*Chi-square-test, P < 0.05.
AIS, ASIA impairment scale; OS, spinal ossification.
Although there were no significant differences between the DS and DUS groups in age, sex, AIS, injury level, additional injuries, or surgery, the DUS group had a significantly higher percentage of patients with bony injury (P = 0.001) or spinal-ligament ossification (P = 0.013).
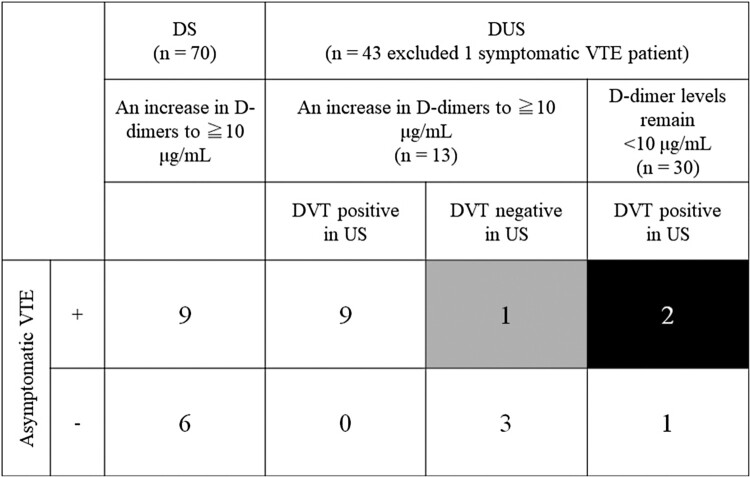
Screening results (Fig. 2 and Table 2)
Figure 2.
VTE screening results. In the DS group, 9 of the 15 patients (66.7%) whose D-dimer levels increased (to ≥ 10 µg/mL) were diagnosed with VTE by contrast venography. In the DUS group, one patient developed symptomatic VTE on day 4, and 12 of the other 43 patients (27.9%) were diagnosed with asymptomatic VTE by contrast venography. Ultrasound screening indicated DVT in 3 of the 30 DUS-group patients whose D-dimer levels remained under 10 µg/mL; 2 of the 3 patients were diagnosed with VTE by contrast venography (black box). Ultrasound results did not indicate DVT for one of the 13 patients with elevated D-dimers (gray box); in this patient, VTE was detected by contrast venography.
Table 2. Asymptomatic VTE in the DS and DUS groups.
| DS group (n = 70) | DUS group (n = 43) | P value | |
|---|---|---|---|
| D-dimer elevation (to ≥ 10 μg/mL) | 21.4% (15) | 30.2% (13) | 0.370 |
| 1 day | 0 case | 0 case | – |
| 3 days | 4 cases | 2 cases | – |
| 5 days | 3 cases | 5 cases | – |
| 7 days | 3 cases | 4 cases† | – |
| 14 days | 5 cases | 2 cases | – |
| DVT-positive US | – | 27.9% (12) | – |
| Asymptomatic DVT | 11.4% (8) | 27.9% (12) | 0.022* |
| Asymptomatic PE | 5.7% (4#) | 4.7% (2#) | 0.597 |
| Asymptomatic VTE | 12.9% (9) | 27.9% (12) | 0.042* |
| Incidence of AIS A in VTE cases | 66.7% (6/9) | 33.3% (4/12) | – |
| Treatment for VTE | 44.4% (4/9) | 83.3% (10/12) | 0.790 |
*Chi-square-test, P < 0.05; #A case of PE only; †Three of 4 cases were positive for VTE on ultrasound (US) at 7 days.
The DUS group included one case of symptomatic PE in a 17-year-old male who was admitted with a cervical SCI with bony fracture after a fall. He was AIS A when admitted. He was treated surgically and was given elastic stockings and A-V foot pumps to prevent VTE after admission, and he began rehabilitation immediately. He began having difficulty breathing 4 days after surgery. He was immediately evaluated by contrast venography from the lower limbs to the chest, and the results were interpreted by radiologists at our hospital. Symptomatic PE in the right chest was diagnosed, and he was treated with the anticoagulant heparin.
In the DS group, D-dimer elevation (to ≥ 10 µg/mL) was first detected in 15 of the 70 patients (21.4%) during the acute recovery phase: in 4 patients at 3 days after admission, in 3 at 5 days, in 3 at 7 days, and in 5 at 14 days. VTE was diagnosed in 9 of these 15 patients by contrast venography (VTE 27.3%; DVT 27.3%; PE 3.5%), and 4 of the 9 were treated with heparin only.
In the DUS group, D-dimer elevation was first detected in 13 of the 43 patients (30.2%) during the acute recovery phase: in 2 patients at 3 days after admission, in 5 at 5 days, in 4 at 7 days, and in 2 at 14 days. Ultrasound screening indicated DVT in 12 of the 43 patients (27.9%). Of these 12 patients, 3 did not have detectable D-dimer elevation at any time point, 5 had D-dimer elevation first detected on day 5 after admission, 3 on day 7, and 1 on day 14. Ultrasound screening on day 7 indicated DVT in 4 cases, of which 3 were diagnosed as DVT by contrast venography. All patients with elevated D-dimers or positive indications of VTE on ultrasound were examined by contrast venography, and 12 were found to have asymptomatic VTE (VTE 27.9%, DVT 27.9%, PE 4.7%). Of the 12 patients with VTE, 10 were treated with an anticoagulant (heparin, warfarin, or edoxaban). Of the 30 patients whose D-dimer levels stayed below 10 µg/mL, ultrasound indicated DVT in 3 patients, of whom 2 were diagnosed with VTE by contrast venography. Of the 13 patients with elevated D-dimers, ultrasound indicated DVT in all but one (Fig. 2). The incidence of DVT and VTE was significantly higher in the DUS than in the DS group (P = 0.022 and 0.042). The percentage of AIS A patients among the VTE cases was 66.7% in the DS group and 33.3% in the DUS group. Patients treated with anticoagulants did not show any side effects.
D-dimer values in the DS and DUS groups (Table 3)
Table 3. D-dimer testing in the DS and DUS groups.
| D-dimer | DS group (n = 70) | P value | DUS group (n = 44) | P value | ||
|---|---|---|---|---|---|---|
| VTE+(n = 9) | VTE−(n = 61) | VTE+(n = 13) | VTE−(n = 31) | |||
| At admission | 17.6 ± 26.9 | 13.1 ± 24.6 | 0.191 | 11.3 ± 12.4 | 9.6 ± 21.5 | 0.136 |
| 1 day | 9.3 ± 5.5 | 5.9 ± 8.4 | 0.035* | 5.9 ± 2.9 | 4.8 ± 8.7 | 0.022* |
| 3 days | 10.2 ± 8.2 | 3.9 ± 4.2 | 0.002* | 6.7 ± 4.4 | 2.2 ± 2.2 | <0.001* |
| 5 days | 12.1 ± 5.3 | 4.2 ± 3.7 | 0.001* | 9.3 ± 5.5 | 3.0 ± 2.5 | <0.001* |
| 7 days | 11.9 ± 7.2 | 4.3 ± 3.3 | 0.001* | 13.5 ± 8.2 | 3.3 ± 2.7 | <0.001* |
| 14 days | 10.1 ± 3.7 | 3.7 ± 3.4 | <0.001* | 7.1 ± 5.3 | 3.1 ± 2.6 | 0.004* |
*Mann-Whitney U-test, P < 0.05. Data are shown as mean ± S.D.
In the DS and DUS groups, the D-dimer levels did not differ significantly between the VTE and non-VTE patients at admission. However, D-dimers were significantly higher in the VTE than in the non-VTE patients on day 1 and thereafter.
Discussion
We screened for asymptomatic VTE in patients with acute SCI using D-dimer testing only or a combination of D-dimer testing and ultrasound, and compared the results of the two methods. VTE was diagnosed by contrast venography. The combination screening detected significantly more cases of asymptomatic VTE than did D-dimer screening alone.
Asymptomatic VTE is particularly common in SCI,10 due in part to two important factors.3 First, sensitivity to pain, one of the clinical manifestations of DVT, is reduced in SCI patients. Second, autonomic function is impaired in patients with SCI, so the body’s reaction to vasculitis and subsequent lower-limb edema is reduced. The frequency of VTE in untreated individuals with SCI, based on diagnosis solely by clinical criteria, has been reported to be 12−64%.1 We found a 12.9% prevalence of asymptomatic VTE in the DS group and 27.9% in the DUS group. These relatively low rates might have resulted from the preventative care (elastic stockings and A-V foot/calf pumps) provided for all patients.
A systematic review reported that the risk for VTE is greatest during the first 2 weeks after injury and that fatal PE is rare after 3 months post-SCI,1 and proposed weekly VTE screening for 13 weeks after SCI.1 Wada et al. screened 1043 patients for DVT by D-dimer testing and compression ultrasound upon admission to a rehabilitation facility,3 and adopted a D-dimer cutoff of 3.0 µg/mL. They found and treated DVT in 15 patients (1.4%). Matsumoto et al. investigated the incidence of VTE in SCI patients screened by D-dimer, and reported that the D-dimer value on VTE occurrence was 14.6 ± 13.5 μg/ml (2.78-44.3).4 Masuda et al. screened 268 patients with acute traumatic cervical SCI for DVT by weekly D-dimer testing until 1 month after injury, plus ultrasound every 2 weeks,6 and detected DVT in 22 patients (10.4%). They suggested that the optimal timing for D-dimer screening was 2 weeks after injury, with an optimal threshold of 16 μg/dL for diagnosing DVT. However, it is difficult to adopt a cutoff point in acute SCI due to traumatic changes. In DVT patients, PE needs to be diagnosed by contrast venography. In fact, we generally found high D-dimer levels at admission (Table 3). In our study, the addition of ultrasound increased the proportion of patients detected as having asymptomatic VTE from 10 to 12 of the 43 patients in the DUS group. This difference represented a 4.1% increase in the absolute rate of detection, which was not a statistically significant difference in the proportion. Nevertheless, our results highlight the importance of combination screening by D-dimer testing and ultrasound, and of diagnosing by contrast venography if the D-dimer levels begin to rise after the patient is admitted to the hospital.
The most serious complication of DVT is PE, which has a mortality rate of 2.5−4.7%.11,12 The American College of Chest Physicians recommends starting thromboprophylaxis with low-molecular-weight heparin for all patients with acute SCI once primary hemostasis is evident.13 Evidence indicated that screening could potentially detect asymptomatic DVT in 9.4% or more individuals who underwent thromboprophylaxis with low-molecular-weight heparin during the acute recovery stage after SCI.14 Although pharmacologic prophylaxis is recommended in the Consortium for Spinal Cord Medicine’s Clinical Practice Guideline on VTE prophylaxis, 3rd edition (2016) in the United States, the Japanese Orthopaedic Symptomatic VTE Prevention Guideline (2017) does not recommend that all SCI patients, including those with hematoma or additional injury, receive pharmacological prophylaxis. We found asymptomatic PE cases in our study; these patients were treated with anticoagulants immediately. Our results showed that additional screening by enhanced CT is important for detecting possible PE.
This study had the following limitations. First, we did not examine CTs with enhancement for all patients, so asymptomatic VTE could have gone undetected in patients who did not have elevated D-dimers and were not screened by ultrasound. Second, this study compared two different populations and included AIS E patients, who lacked neurological findings. However, 8 of the AIS E patients had another injury, such as a head, chest, or extremity injury, that required bed rest, and thus had a high risk of VTE. Therefore, we included the AIS E patients. Third, it is possible that some patients had VTE when they were admitted. Fourth, the patients in this study were not randomly but sequentially allocated to the study groups. Despite these limitations, our study indicates the advisability of screening patients with SCI by repeated D-dimer testing combined with ultrasound.
Conclusion
Combined D-dimer and ultrasound screening in patients with acute SCI improved the detection of VTE, including PE, compared with D-dimer screening only.
Abbreviations
VTE, venous thromboembolism; DVT, deep venous thrombosis; PE, pulmonary embolism; SCI, spinal cord injury; AIS, American Spinal Injury Association (ASIA) Impairment Scale
Acknowledgements
We thank Drs. A. Ono, T. Numasawa, K. Kowatari, T. Tanaka, T. Sawada, and T. Shiozaki for their support and technical assistance.
Disclaimer statements
Contributors None.
Funding This study was supported by a Hirosaki University Grant for Distinguished Researchers (FY2017).
Conflict of interest None of the authors has any potential conflict of interest.
Declaration of interest None.
References
- 1.Furlan JC, Fehlings MG.. Role of screening tests for deep venous thrombosis in asymptomatic adults with acute spinal cord injury: an evidence-based analysis. Spine 2007;32(17):1908–16. doi: 10.1097/BRS.0b013e31811ec26a [DOI] [PubMed] [Google Scholar]
- 2.Kelly J, Rudd A, Lewis RR, Hunt BJ.. Screening for subclinical deep-vein thrombosis. QJM 2001;94(10):511–9. doi: 10.1093/qjmed/94.10.511 [DOI] [PubMed] [Google Scholar]
- 3.Wada M, Iizuka M, Iwadate Y, Yamakami I, Yoshinaga K, Saeki N.. Effectiveness of deep vein thrombosis screening on admission to a rehabilitation hospital: a prospective study in 1043 consecutive patients. Thromb Res 2013;131(6):487–92. doi: 10.1016/j.thromres.2013.04.022 [DOI] [PubMed] [Google Scholar]
- 4.Matsumoto S, Suda K, Iimoto S, Yasui K, Komatsu M, Ushiku C, et al. Prospective study of deep vein thrombosis in patients with spinal cord injury not receiving anticoagulant therapy. Spinal Cord 2015;53(4):306–9. doi: 10.1038/sc.2015.4 [DOI] [PubMed] [Google Scholar]
- 5.Becker DM, Philbrick JT, Bachhuber TL, Humphries JE.. D-dimer testing and acute venous thromboembolism. A shortcut to accurate diagnosis? Arch Intern Med 1996;156(9):939–46. doi: 10.1001/archinte.1996.00440090029004 [DOI] [PubMed] [Google Scholar]
- 6.Masuda M, Ueta T, Shiba K, Iwamoto Y.. D-dimer screening for deep venous thrombosis in traumatic cervical spinal injuries. Spine J 2015;15(11):2338–44. doi: 10.1016/j.spinee.2015.06.060 [DOI] [PubMed] [Google Scholar]
- 7.Chen CJ, Wang CJ, Huang CC.. The value of D-dimer in the detection of early deep-vein thrombosis after total knee arthroplasty in Asian patients: a cohort study. Thromb J 2008;6:5. doi: 10.1186/1477-9560-6-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shiota N, Sato T, Nishida K, Matsuo M, Takahara Y, Mitani S, et al. Changes in LPIA D-dimer levels after total hip or knee arthroplasty relevant to deep-vein thrombosis diagnosed by bilateral ascending venography. J Orthop Sci 2002;7(4):444–50. doi: 10.1007/s007760200077 [DOI] [PubMed] [Google Scholar]
- 9.Goodacre S, Sampson F, Thomas S, van Beek E, Sutton A.. Systematic review and meta-analysis of the diagnostic accuracy of ultrasonography for deep vein thrombosis. BMC Med Imaging 2005;5:663. doi: 10.1186/1471-2342-5-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johns JS, Nguyen C, Sing RF.. Vena cava filters in spinal cord injuries: evolving technology. J Spinal Cord Med 2006;29(3):183–90. doi: 10.1080/10790268.2006.11753873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Merli GJ, Crabbe S, Paluzzi RG, Fritz D.. Etiology, incidence, and prevention of deep vein thrombosis in acute spinal cord injury. Arch Phys Med Rehabil 1993;74(11):1199–205. [PubMed] [Google Scholar]
- 12.Rossi EC, Green D, Rosen JS, Spies SM, Jao JS.. Sequential changes in factor VIII and platelets preceding deep vein thrombosis in patients with spinal cord injury. Br J Haematol 1980;45(1):143–51. doi: 10.1111/j.1365-2141.1980.tb03819.x [DOI] [PubMed] [Google Scholar]
- 13.Geerts WH, Pineo GF, Heit JA, Bergqvist D, Lassen MR, Colwell CW, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004;126(3 Suppl):338S–400S. doi: 10.1378/chest.126.3_suppl.338S [DOI] [PubMed] [Google Scholar]
- 14.Green D, Lee MY, Ito VY, Cohn T, Press J, Filbrandt PR, et al. Fixed- vs adjusted-dose heparin in the prophylaxis of thromboembolism in spinal cord injury. JAMA 1988;260(9):1255–8. doi: 10.1001/jama.1988.03410090087036 [DOI] [PubMed] [Google Scholar]