Abstract
Objective
This article presents additional strategies to the medical professional and support tactics to keep both the health care provider and patient as safe as possible during the COVID-19 pandemic.
Observations
Follicular conjunctivitis has been reported as an early sign of infection or during hospitalization for severe COVID-19 disease. It has been confirmed that COVID-19 is transmitted through both respiratory droplets and direct contact. Another possible route of viral transmission is entry through aerosolized droplets into the tears, which then pass through the nasolacrimal ducts and into the respiratory tract. For nonemergent care, eye care providers should use telehealth. Eye care providers should prioritize patient care in order of absolute necessity, such as sudden vision loss, sudden onset flashes and floaters, and eye trauma. In those cases, exposure should be minimized. The close proximity between eye care providers and their patients during slit-lamp examination may require further precautions, such as shields, barriers, and mask use to lower the risk of transmission via droplets or through hand to eye contact.
Conclusions
All nonemergent eye care appointments should be delayed or conducted remotely. For emergent in-person appointments, careful and appropriate adherence to Centers for Disease Control and Prevention recommendations may minimize exposure for both the health care provider and patient.
Amid the COVID-19 pandemic, eye care professionals should be aware of important guidelines and consider using telehealth to keep both the health care provider and patient as safe as possible. This article is intended to give an update on the ever-changing landscape of eye care due to COVID-19. The Centers for Disease Control and Prevention (CDC) recommends that health care facilities and clinicians delay all elective ambulatory provider visits.1 In addition, the American Academy of Ophthalmology (AAO) recommends that all ophthalmologists cease providing any treatment other than urgent or emergent care.2 Our goal is to equip the eye care provider with the best practice guidelines for seeing urgent and emergent eye conditions.
COVID-19 is caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and its symptoms range from mild to severe respiratory illness, fever, cough, fatigue, and shortness of breath.1 Diarrhea is common early on with infection and loss of taste and smell have also been reported.1 Follicular conjunctivitis has also been reported, either as an early sign of infection or during hospitalization for severe COVID-19 disease.2–4 The incubation period of COVID-19 falls within 2 to 14 days according to the CDC.5
It has been confirmed that COVID-19 is transmitted through both respiratory droplets and direct contact. Another possible route of viral transmission is entry through aerosolized droplets into the tears, which then pass through the nasolacrimal ducts and into the respiratory tract.6
PREPARATIONS PRIOR TO OFFICE VISIT
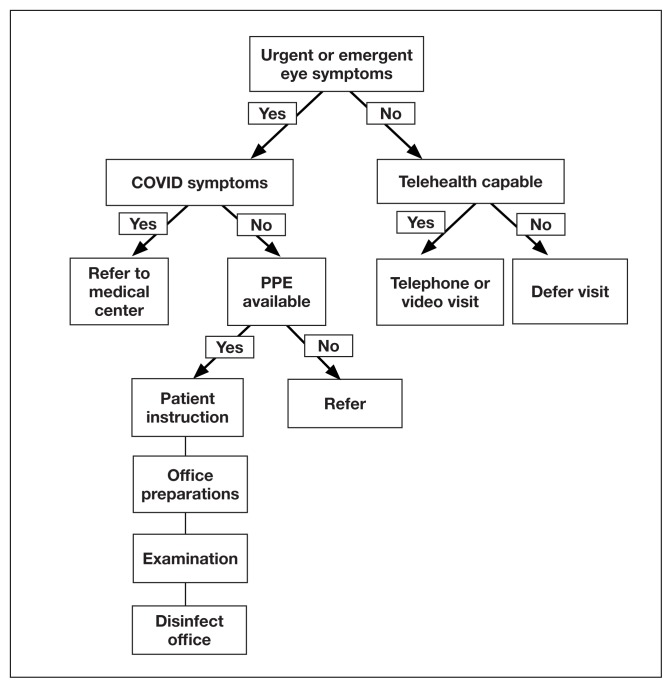
It is essential for the eye care provider to prioritize patient care in order of absolute necessity, such as sudden vision loss, sudden onset flashes and floaters, and eye trauma. In cases of potentially sight threatening pathology, it is in the best interest of the patient to conduct a face-to-face appointment. Therefore, it is important to implement new guidelines and protocols as we continue to see these patients (Figure 1).
FIGURE 1.
Summary of Primary Recommendations
Abbreviation: PPE, personal protective equipment.
Need to Know.
The American Academy of Ophthalmology (AAO) and Centers for Disease Control and Prevention recommend protection for the mouth, nose, and eyes when caring for patients potentially infected with SARS-CoV-21,2;
The AAO issued guidance recommending all eye doctors to suspend routine eye examinations, providing only urgent or emergent care2; and
Reports suggest mild follicular conjunctivitis easily transmitted by aerosol contact with conjunctiva or hand to eye contact.2–4
Prior to the patient entering the medical facility, measures should be implemented to minimize exposure risk. This can be done over the telephone or at vehicle entrance screening stations. The triage technician answering the telephone should have a script of questions to ask. The patient should be instructed to come into the office alone unless, for physical or mental reasons, a caregiver is required.
SARS-COV-2 SCREENING QUESTIONS
Preparedness through risk mitigation strategies are recommended with a targeted questionnaire and noncontact temperature check at the clinic or hospital entrance. Below are some general questions to further triage patients exposed to SARS-CoV-2.
Do you have fever or any respiratory symptoms?
Do you have new or worsening cough or shortness of breath?
Do you have flulike symptoms?
Have you been in close contact with someone, including health care workers, confirmed to have the COVID-19?
If the patient answers yes to any of the above questions, the CDC urges health care providers to immediately notify both infection control personnel at your health care facility and your local or state health department.1,2 In regions currently managing significant outbreaks of COVID-19, the AAO recommends that eye care providers assume that any patient could be infected with SARS-CoV-2 and to proceed accordingly.2 If urgent eye care is needed, a referral call should be made to a hospital or center equipped to deal with COVID-19 and urgent eye conditions. When calling the referral center, ensure adequate staffing and space and relay all pertinent information along with receiving approval from the treating physician.
FACE-TO-FACE OFFICE VISITS
Once it has been determined that it is in the best interest of the patient to be seen in a face-to-face visit, the patient should be instructed to call the office when they arrive in the parking lot. The CDC recommends limiting points of entry upon arrival and during the visit.1 As soon as an examination lane is ready, the patient can then be messaged to come into the office and escorted into the examination room.
An urgent or emergent ophthalmic examination for a patient with no respiratory symptoms, no fever, and no COVID-19 risk factors should include proper hand hygiene, use of personal protective equipment (PPE), and proper disinfection. Several studies have documented SARS-CoV-2 infection in asymptomatic and presymptomatic patients, making PPE of the up most importance.2,7,8 PPE should include mask, face shield, and gloves. Currently, there are national and international shortages on PPE and a heightened topic of discussion concerning mask use, effectiveness with extended wear, and reuse. Please refer to the CDC and AAO websites for up-to-date guidelines (Table).1,2 According to the CDC, N95 respirators are restricted to those performing or present for an aerosol-generating procedure.9
TABLE.
Resources for COVID-19 Updates
| Centers for Disease Control and Prevention | www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html |
| World Health Organization | www.who.int/emergencies/diseases/novel-coronavirus-2019 |
| National Institutes of Health | www.nih.gov/health-information/coronavirus |
| US Department of Veterans Affairs | www.publichealth.va.gov/n-coronavirus |
| American Academy of Ophthalmology | www.aao.org/coronavirus |
| American Optometric Association | www.aoa.org/coronavirus |
It is recommended that the eye care provider should only perform necessary tests and procedures. Noncontact tonometry should be avoided, as this might cause aerosolization of virus particles. The close proximity between eye care providers and their patients during slit-lamp examination may require further precautions to lower the risk of transmission via droplets or through hand to eye contact. The patient should be advised not to speak during the examination portion and the AAO also recommends a surgical mask or cloth face covering for the patient.2 An additional protective device that may be used during the slit-lamp exam is a breath shield or a barrier shield (Figures 2 and 3).2 Some manufacturers are offering clinicians free slit-lamp breath shields online.
FIGURE 2.
Stock Protective Breath Shield Provided by the Manufacturer Haag-Streit
FIGURE 3.
Self-Engineered Barrier Shield
INFECTION PREVENTION AND CONTROL MEASURES
Last, once the patient leaves the examination room, it should be properly disinfected. A disinfection checklist may be made to ensure uniform systematic cleaning. Alcohol and bleach-based disinfectants commonly used in health care settings are likely very effective against virus particles that cause COVID-19.10 During the disinfection process, gloves should be worn and careful attention paid to the contact time. Contact time is the amount of time the surface should appear visibly wet for proper disinfection. For example, Metrex CaviWipes have a recommended contact time of 3 minutes; however, this varies depending on type of virus and formulation, check labels or manufacturers’ websites for further directions.10 Also, the US Environmental Protection Agency has a database search available for disinfectants that meet their criteria for use against SARS-CoV-2.11
In an ever-changing environment, we offer this article to help equip providers to deliver the best possible patient care when face-to-face encounters are necessary. Currently nonurgent eye care follow-up visits are being conducted by telephone or video clinics. It is our goal to inform fellow practitioners on options and strategies to elevate the safety of staff and patients while minimizing the risk of exposure.
Footnotes
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the US Government, or any of its agencies.
References
- 1.Centers for Disease Control and Prevention. Coronavirus disease 2019 (COVID-19): for healthcare professionals. [Accessed April 13, 2020]. https://www.cdc.gov/coronavirus/2019-nCoV/hcp/index.html. Updated April 7, 2020.
- 2.American Academy of Ophthalmology. Important coronavirus context for ophthalmologists. [Accessed April 13, 2020]. https://www.aao.org/headline/alert-important-coronavirus-context. Updated April 12, 2020.
- 3.Zhou Y, Zeng Y, Tong Y, Chen CZ. Ophthalmologic evidence against the interpersonal transmission of 2019 novel coronavirus through conjunctiva [preprint] [Accessed April 13, 2020]. . Published February 12, 2020. [DOI]
- 4.Lu CW, Liu XF, Jia ZF. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395(10224):e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Symptoms of coronavirus. [Accessed April 13, 2020]. https://www.cdc.gov/coronavirus/2019-ncov/symptoms-testing/symptoms.html. Updated March 20, 2020.
- 6.van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N Engl J Med. 2020 doi: 10.1056/NEJMc2004973. NEJMc2004973. [Published online ahead of print, March 17, 2020] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kimball A, Hatfield KM, Arons M, et al. Asymptomatic and Presymptomatic SARS-CoV-2 Infections in Residents of a Long-Term Care Skilled Nursing Facility - King County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69(13):377–381. doi: 10.15585/mmwr.mm6913e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) [published online ahead of print, 2020 Mar 16] Science. 2020 doi: 10.1126/science.abb3221. eabb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for patients with suspected or confirmed coronavirus disease 2019 (COVID-19) in healthcare settings. [Accessed April 13, 2020]. https://www.cdc.gov/coronavirus/2019-ncov/hcp/infection-control-recommendations.html. Updated April 9, 2020.
- 10.Centers for Disease Control and Prevention. Cleaning and disinfection for households interim recommendations for U.S. households with suspected or confirmed coronavirus disease 2019 (COVID-19) [Accessed April 13, 2020]. https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/cleaning-disinfection.html. Updated March 28, 2020.
- 11.US Environmental Protection Agency. Pesticide registration: List N: disinfectants for use against SARS-CoV-2. [Accessed April 13, 2020]. https://www.epa.gov/pesticide-registration/list-n-disinfectants-use-against-sars-cov-2. Updated April 10, 2020.