Abstract
Introduction:
Human papillomavirus (HPV) is the most prevalent sexually transmitted infection that leads to nearly all cervical cancers in the United States (U.S.), which could be prevented with the HPV vaccine. Korean American women experience a high burden of cervical cancer, but little is known about their awareness, knowledge, attitudes, sociocultural factors and social network/support related to intention to obtain the HPV vaccine.
Methods:
This study reports baseline characteristics of 104 Korean American college women aged 18–26 and who have not been previously vaccinated against HPV, as part of a pilot randomized controlled trial testing feasibility, acceptability, and preliminary effectiveness of an HPV storytelling intervention. Data were analyzed including descriptive statistics, bivariate analysis, and multivariate logistic regression. Multivariate logistic regression was performed to understand the relationship between independent predictors of intention to receive HPV vaccination.
Results:
Overall, 34.6% of participants intended to obtain the vaccine. Positive predictors of intention to receive HPV vaccine were: years in the U.S., academic major, awareness of HPV and HPV vaccine, knowledge, and HPV recommendation by healthcare provider and parents. The multivariate logistic model showed that intention to receive the HPV vaccine was significantly associated with HPV vaccine recommendation by parents (OR=4.58, 95% CI, 1.37–15.36) and knowledge (OR=1.11, 95% CI, 1.11–1.22).
Conclusion:
These findings suggest a need for development of interventions that are not only culturally tailored but also acculturation-sensitive to promote HPV vaccination among Korean American college women. This may play a significant role in cervical cancer prevention among Korean American college women.
Keywords: HPV vaccination, awareness, knowledge, attitudes, Korean American college women
Introduction
The prevalence of cervical cancer has decreased significantly (by 75%) in the past 40 years as a result of the increased use of cervical cancer screening (Adegoke, Kulasingam & Virnig, 2012; Ward et al., 2012). However, some subgroups of Asian American women are disproportionately affected by cervical cancer. For instance, cervical cancer incidence and mortality are substantially greater in Korean American women (11.9 per 100,000) and Vietnamese women (18.9 per 100,000), than non-Hispanic white women (7.1 per 100,000) in the United States (U.S.) (Wang, Carreon, Gomez & Devesa, 2010). Although subgroup differences in the incidence rates of cervical cancer among Asian Americans has been observed, there are no population-based data that examine subgroup differences in primary prevention of cervical cancer, human papillomavirus (HPV) vaccine among Asian American subgroups.
HPV is the most prevalent sexually transmitted infection in the United States (U.S.) leading to nearly all-cervical cancers (Centers for Disease Control and Prevention [CDC], 2015; World Health Organization [WHO], 2016). HPV vaccines are designed to prevent the most common types of HPV that cause cervical cancer. HPV vaccine is most effective in preventing cancers when it is given before individuals become sexually active (Hildesheim et al., 2007). In the U.S., the average age of sexual initiation is 17 years for women (Cavazos-Rehg et al., 2009). However, there is a substantial difference in age of sexual initiation by race/ethnicity. For example, Asian American females were reported to experience sexual initiation by age 17 at a considerably lower rate (28%) than Caucasian (58%), African American (55%), and Hispanic females (41%) (Lee et al., 2010). Additionally, the average age of sexual initiation among Korean American women was 24 years (Lee et al., 2010). Therefore, the importance of HPV vaccination continues to be critical for emerging adult women who missed early immunization and are becoming sexually active.
In recent decades, Korean American women were consistently identified as the least likely Asian sub-group to receive cervical cancer screenings (Choi, Heo, Song & Han, 2016; Fang et al., 2017; Han et al., 2017; Lee et al., 2014; Tung, Lu, Granner, & Sohn, 2017). Our earlier qualitative study explored young Korean American women’s awareness of HPV infection and HPV vaccination and attitudes toward HPV prevention. This study found that there were considerable misunderstandings about HPV and the HPV vaccine and social and cultural barriers to HPV vaccination among Korean American women. The current study is built upon the qualitative study with the aim to assess Korean American college women’s awareness, knowledge, and attitudes toward HPV vaccination in a larger sample.
Methods
Design
This study was part of an experimental study, “I want to know more about the HPV vaccine” that evaluated preliminary effectiveness of an HPV intervention (Kim, 2017). The present study reports baseline characteristics of Korean American college women aged 18–26 who have not been previously vaccinated against HPV. Ethical approval for the procedures of this study was obtained from the University of Massachusetts Boston Institutional Reviewed Board (IRB).
Study setting
A short eligibility screening survey, informed-consent form, and the survey measures were uploaded into the Qualtrics Survey Tool (http://www.qualtrics.com/). Qualtrics is an online service that allows researchers to design an online research instrument with minimal investment of time or effort and without extensive programming experience.
Participants
Participants were recruited from August to October 2016 through word-of-mouth by Korean American student associations, churches, and researchers in the Northeastern U.S., and social media, such as Facebook, KakaoTalk (a Korean social networking service), and Korean American community websites. The eligibility criteria included: (1) current female undergraduate or graduate students; (2) self-identifying as Korean American.; (3) being 18–26 years; (4) residing in the Northeastern U.S.; (5) can speak or read English; and (6) self-reporting as not having yet been vaccinated against HPV.
Procedures
Individuals interested in the study were directed to enter the study website (http://www.hpveducation.org) to take the eligibility screening survey. An online survey link that included an informed consent and an online survey was sent to eligible participants via email. All participants were asked to sign the online consent form if they agreed to participate in the study. After providing informed consent, participants took a 10- to 15-minute baseline survey. Individuals who completed the survey received a $20 Amazon gift certificate in recognition of their time.
Survey Measures
A culturally relevant survey was developed based on the findings of a qualitative study which targeted Korean American college women (Kim et al., 2017) and a literature review using constructs of a situation-specific theory. This survey measured: (1) sociodemographic and acculturation (5 items), (2) sexual behavior and prevention behavior (4 items), (4) HPV vaccine recommendations (4 items), (5) awareness of HPV and HPV vaccine (3 items), (6) knowledge about HPV (16items; α = 0.91), the HPV vaccine (8 items; α = 0.82), and cervical cancer (8 items; α=0.81), and (6) attitudes toward HPV vaccine, (a) perceptions of HPV vaccine (cognitive dimension of attitude) (9 items; α=0.78), (b) feelings about getting the HPV vaccine (affective dimension of attitude) (10 items; α=0.75), and (c) intention to receive the HPV vaccine (conative dimension of attitude) (Kim, 2017; Kim, Lee, Kiang, & Kim, 2017). All knowledge and attitudes responses were given as “yes,” “no,” and “I don’t know.” As in previous studies, the option to respond “don’t know” was added in addition to “yes” and “no” responses because of the concern that a forced-choice rating of “yes” or “no” might bias the results by not distinguishing between respondents who were misinformed or uninformed about HPV, the HPV vaccine, and cervical cancer (Kim et al., 2017; Lee et al., 2013). Best psychometric practice includes a “don’t know” option when respondents are asked questions about their perceptions and feelings and when the respondents would have inadequate knowledge or insufficient familiarity to have formed an opinion about the topic. Furthermore, adding a “don’t know” option increases the accuracy of responses (Albaum et al., 2011; Dolnicar & Bettina, 2014). The preliminary qualitative study also pointed to the importance of “don’t know” options in questionnaires since the majority of Korean American college women had little knowledge about HPV and the HPV vaccine (Kim et al., 2017).
An overall knowledge score of HPV, HPV vaccine, and cervical cancer was calculated as the sum of correct answers. If the answer was correct, one point was given. If the answer was incorrect or “I don’t know,” zero points were given. An overall score of perceptions about the HPV vaccine and feelings about getting the HPV vaccine were calculated as the sum of positive responses. If the response was positive toward HPV vaccine, one point was given. If the response was negative or “I don’t know,” zero points were given. The outcome variable is intention to receive HPV vaccine which was dichotomized as follow: 0 = no intention to receive the HPV vaccine and 1 =intention to receive the HPV vaccine.
Statistical Analysis
All analyses were performed using SPSS Statistics software version 23 (IBM, Armonk, NY, USA). Prior to the analysis, the data were cleaned using exploratory data analysis (Pallant, 2013). Data were analyzed including descriptive statistics, bivariate analysis and multivariate logistic regression.
Descriptive statistics
Descriptive statistics was used to examine the sociodemographic and acculturation characteristics, sexual and prevention behavior, HPV vaccine recommendations, awareness of HPV and HPV vaccine, knowledge about HPV, the HPV vaccine, and cervical cancer, and attitudes toward HPV vaccine.
Bivariate analysis
Bivariate trend analysis was utilized to identify which variables have association with intention of HPV vaccination individually using Chi-Square or ANOVA test analysis as appropriate to assess statistical significance (p<0.05). Trend analysis was performed using the linear-by-linear association Chi-square statistic.
Multivariate logistic regression analysis
Multivariate logistic regression analysis was performed to understand the relationship between independent predictors of intention to receive HPV vaccination. Variables with a p-value less than 0.05 in the bivariate analysis were added for multivariate logistic regression analysis. The statistically significant level in the multivariable logistic regression analysis was set at p<0.05 (Pallant, 2013).
Results
Sociodemographic Characteristics
The mean age of the participants was 21.7 (SD = 2.3). Of the 104 participants, the majority of participants (77.9%) were born in South Korea, with 32.1% of participants immigrating or migrating to the U.S. after the age of 18 years; 38.5% reported being international (non-immigrant) students. More than half of the participants reported speaking Korean and English about equally well (52.9%) and identified themselves as more Korean than American or Completely Korean (61.5%) (Table 1). Of all participants, 34.6% were in a relationship.
Table 1.
Sociocultural and acculturation characteristics of 104 Korean college women
| Sociodemographic | N (%) or M ± SD |
Acculturation | N(%) |
|---|---|---|---|
| Age (range: 18–26) | 21.7 ± 2.34 | Nativity (n=102) | |
| International studenta | 39 (48.1) | South Korea | 81 (79.4) |
| Degree Program (n=100) | USA | 21 (20.6) | |
| Undergraduate | 76 (76.0) | Age Moved to the U.S. (n=81)a | |
| Graduate or other | 24 (24.0) | 18 years or older | 26 (32.1) |
| Major | Associate with in the community | ||
| Health-related | 40 (38.5) | Mostly or Almost exclusively Koreans | 59 (56.8) |
| Health Insurance | About equally Korean and non-Korean groups | 38 (36.5) | |
| College/University Plan | 48 (46.2) | Mostly non-Korean groups | 7 (6.8) |
| Other | 53 (51.0) | Preferred language | |
| No health insurance | 3 (2.9) | Mostly Korean, some English or Korean only | 32 (30.7) |
| Religion (n=103) | Korean and English about equally well | 55 (52.9) | |
| Buddhist | 4 (3.9) | Mostly English, some Korean | 17 (16.3) |
| Catholic/Protestant | 78 (75.7) | Cultural identity | |
| None | 21 (20.4) | More Korean than American or Completely Korean | 64 (61.5) |
| Relationship status | Equally Korean and American | 27 (26.0) | |
| In a relationship | 36 (34.6) | More American than Korean | 13 (12.5) |
Note: M=mean, SD=standard deviation
=participants who were born in South Korea (n=81)
Sexual and Prevention Behavior
Fifty percent of the participants reported they felt stressed “always” or “very often” during the past month, and 37.5% felt depressed “sometimes.” As shown in Table 2, 38.5% of participants reported they had sexual intercourse and the mean age of first sexual experience was 19.2 (SD = 2.37). Among those who aged 21 and over (n=55), none of the participants reported they had had a Pap smear. Of all respondents, only 9.6% reported they had been tested for STIs and none of the participants reported they had ever been diagnosed with HPV.
Table 2.
General health and sexual health and prevention behavior of 104 Korean college women
| Variable | N (%) or M ± SD |
|---|---|
| Felt stressed during the past month | |
| Always/Very often | 52 (50.0) |
| Felt depressed during the past month | |
| Always/Very often | 20 (19.2) |
| Have you ever had sexual intercourse (Yes) | 40 (38.5) |
| Age of first sex (n=26; range: 13–24) | 19.2 ± 2.37 |
| Have you ever had a Pap Test (Yes) (n=55; age≥21) | 0 |
| Have you ever been tested for STIs (Yes) | 10 (9.6) |
Note: HPV= human papillomavirus, STI= sexually transmitted infection, M= mean, SD= standard deviation
Awareness of HPV and HPV Vaccine
As presented in Table 5, nearly half of the participants (48.1%) had heard of HPV either in English or Korean. Most participants were more familiar with the term “cervical cancer vaccine” than HPV vaccine or Gardasil (66.3%). Of those who were aware of the term “cervical cancer vaccine” (n=69), 26.1% of participants reported that they had not heard of HPV vaccine or Gardasil before.
Table 5.
Bivariate analysis for the association between intention to receive HPV vaccination and awareness, recommendation, knowledge, and attitudes toward HPV Vaccine of 104 Korean college women
| Intention to receive HPV vaccine | ||||
|---|---|---|---|---|
| Yes (n=36) | No/Don’t know (n=68) | Total (n=104) | p-value | |
| N (%) or M ± SD | ||||
| Years in the U.S. | ||||
| 0–5 years | 19 (52.8) | 17 (25.4) | 36 (35.0) | 0.020 |
| More than 6 years | 11 (30.6) | 35 (52.2) | 46 (44.7) | |
| US-born | 6 (16.7) | 15 (22.4) | 21 (20.4) | |
| Awareness | ||||
| Heard of HPV | 22 (61.1) | 28 (41.2) | 50 (48.1) | 0.053 |
| Heard of HPV vaccine or Gardasil | 26 (72.2) | 28 (41.2) | 54 (51.9) | 0.003* |
| Cervical cancer vaccine | 32 (88.9) | 37 (54.4) | 69 (66.3) | 0.000* |
| Recommended by: | ||||
| Healthcare provider | 13 (36.1) | 10 (14.7) | 23 (22.1) | 0.012* |
| Parents Friends School |
18 (50.0) 9 (25.0) 8 (22.2) |
7 (10.3) 6 (8.8) 3 (4.4) |
25 (24.0) 15 (14.4) 11 (10.6) |
0.000* 0.025* 0.005* |
| Attitudes toward HPV Vaccine (range: 0–19) |
10.49 ± 3.6 | 10.53 ± 4.9 | 10.5 ± 4.51 | 0.957 |
Note: HPV= human papillomavirus, HPV= human papillomavirus, M= mean, SD= standard deviation,
*p<0.05
HPV Recommendations
Only 22.1% of participants reported that a health care provider had recommended they receive the HPV vaccine. Twenty-four percent received recommendations for HPV vaccination from parents, 14.4% from friends, and 10.6 % from school (Table 3).
Table 3.
Knowledge about HPV, HPV vaccine and cervical cancer among 104 Korean Female College Students
| HPV Knowledge (range: 0–16)a | N (%)* |
| HPV is common (T) | 30 (28.8) |
| There are many types of HPV (T) | 41 (39.4) |
| HPV infects both men and women (T) | 51 (49.0) |
| You can get HPV from having sex (T) | 69 (66.3) |
| You can get HPV from person to person just by skin-to-skin (T) | 15 (14.4) |
| You can get HPV from being unclean (F) | 47 (45.2) |
| You can get HPV from toilet seats (F) | 49 (47.1) |
| You can get HPV from hugging or holding hands (F) | 77 (74.0) |
| You can get HPV from having a family history of HPV (F) | 27 (26.0) |
| You can get HPV from sharing food or utensils (F) | 68 (65.4) |
| HPV can cause genital warts (T) | 55 (52.9) |
| HPV can cause cancer in men (T) | 36 (34.6) |
| HPV can cause cancer in women (T) | 75 (72.1) |
| Most people with HPV have no visible signs or symptoms (T) | 49 (47.1) |
| There is any treatment for HPV (F) | 9 (8.7) |
| Condoms can fully protect against HPV (F) | 54 (51.9) |
| HPV Vaccine (range: 0–8)b | |
| The HPV vaccine is safe (T) | 51 (49.0) |
| The HPV vaccine can protect you against HPV (T) | 59 (56.7) |
| The HPV vaccine can protect against all STIs (T) | 69 (66.3) |
| The HPV vaccine prevents cervical cancer (T) | 34 (32.7) |
| The HPV vaccine is for women (T) | 81 (77.9) |
| The HPV vaccine is for men (T) | 40 (38.5) |
| Aged 11–17 years can receive the HPV vaccine (T) | 41 (39.4) |
| Aged between 18–26 years can receive the HPV vaccine (T) | 83 (79.8) |
| How many shots are required to fully be vaccinated against HPV? Three (T) | 42 (40.4) |
| Cervical Cancer is…(range: 0–8)c | |
| caused by HPV (T) | 39 (37.5) |
| caused by sexual contact (T) | 53 (51.0) |
| is caused by smoking (T) | 19 (18.3) |
| is common in women aged 25–35 years (T) | 54 (51.9) |
| is common in women after menopause (T) | 24 (23.1) |
| is common among Korean/Korean American women (T) | 24 (23.1) |
| is common among Caucasian women (F) | 13 (12.5) |
| Cervical cancer runs in the family (F) | 24 (12.5) |
Note:Corrected answers are presented as frequency and percentage.
= (Mean= 7.2, SD=1.03)
=(Mean= 3.8, SD=2.12)
=(Mean= 2.4, SD=1.81)
Knowledge about HPV, HPV Vaccine, and Cervical Cancer
Knowledge about HPV, HPV vaccine, and cervical cancer is presented in Table 3. Among 104 participants, 33.3% thought HPV could cause cancer in men, 28.8% of respondents thought that HPV was common, 18.5% thought that HPV was not hereditary, only 9.3% thought that HPV can be transmitted by skin-to-skin contact, and 3.7% thought that there is no treatment for the HPV itself. Only one third of participants (32.7%) correctly answered that HPV vaccine prevents cervical cancer, 37% responded that men could receive the HPV vaccine, and 33.3% of participants correctly responded that three shots were required to fully be vaccinated against HPV. Interestingly, the majority of participants (75.9%) knew that anyone between 18 and 26 years of age can receive the HPV vaccine. However, only 38.9% knew that children and adolescents aged 11–17 years can receive the HPV vaccine. More than half of participants knew that cervical cancer is caused by sexual contact, while only 37.0% knew that cervical cancer is caused by HPV. Furthermore, only 16.7% knew that the risk for cervical cancer is higher in women who smoke, 16.7% knew that cervical cancer is common in women after menopause, and 16.7% knew that cervical cancer is common in Korean American women.
Attitudes Toward the HPV Vaccine
Perception of the HPV vaccine and feelings about HPV vaccination are presented in Table 4.
Table 4.
Perceptions and Feelings about Getting the HPV Vaccine among 104 Korean Female College Students
| Perceptions of getting HPV vaccinea | Feelings of getting HPV vaccineb | ||
|---|---|---|---|
| I did not get the HPV vaccine because… | N (%) | I worry because… | N (%) |
| I have never heard of it. | 29 (27.9) | of the side effects. | 51 (49.5) |
| I’m healthy. | 53 (50.9) | it costs too much. | 42 (49.5) |
| I’m too old. | 4 (3.9) | my insurance does not cover the cost. | 28 (27.5) |
| I’m too busy. | 50 (48.5) | I get scared of needles or injection. | 23 (22.5) |
| I have never had sexual intercourse | 34 (33.3) | I heard negative messages through social media or others. | 25 (24.3) |
| I’m sexually active. | 14 (13.7) | I’m not familiar with medical terminology. | 45 (43.7) |
| I have protected sex (e.g. condom). | 19 (18.6) | I’m not familiar with health care systems in the U.S. | 41 (40.2) |
| I’m not likely to get sexually transmitted infections. | 42 (41.2) | I don’t know where to get the HPV vaccine. | 32 (31.4) |
| I’m not likely to get genital warts or cervical cancer. | 40 (39.2) | it’s not easy to make an appointment for vaccination. | 30 (29.4) |
| there is a long wait time to see a health provider. | 33 (32.4) |
Note: = (Mean= 5.1, SD=2.32, range: 0–9)
=(Mean= 5.4, SD=3.0, range: 0–10)
Perceptions of the HPV vaccine (cognitive)
Nearly half of respondents (48.5%) reported being “too busy” as the reason why they did not get the HPV vaccine. Perceived likelihood of getting STIs (41.2%), genital warts, and cervical cancer (39.2%) was moderate. Of 104 participants, 41.2% perceived that they were not likely to get STIs and 39.2% perceived that they were not likely to get genital warts or cervical cancer.
Feelings about getting the HPV vaccine (affective)
Approximately half of the participants were worried about the side effects of the HPV vaccine (49.5%), the cost (49.5%), and not being familiar with either medical terminology (43.7%) or the health care system in the U.S. (40.2%) (Table 4).
Intention to get the HPV vaccine (conative)
Only 34.6% of participants reported they intended to get the HPV vaccine.
Bivariate Analysis of Intention to Receive HPV Vaccine
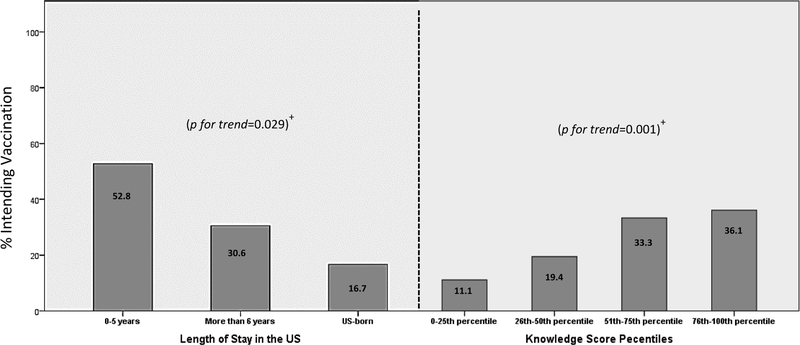
As presented in Table 5 and Figure 1, statically significant associations were observed between having intention to receive the HPV vaccine and years in the U.S. (χ2(2) = 7.873, p=0.02), heard of the HPV vaccine (χ2(1) = 9.088, p=0.003), heard of cervical cancer vaccine (χ2(2) = 12.53, p=0.000), HPV recommendation by health care provider (χ2(2) = 6.57, p<0.012), HPV recommendation by parents (χ2(2) = 21.02, p<0.000), and high level of knowledge about HPV, HPV vaccine, and cervical cancer (F (1,102) = 13.635, p<0.001) (Figure 1). However, Korean American college women’ relationship status (χ2(2) = 0.40, p=0.842), language preference (χ2(2) = 5.84, p=0.054), sexual experience (χ2(2) = 1.48, p<0.478), awareness of HPV (χ2(2) = 3.75, p=0.053), and perceptions and feelings toward getting HPV vaccine (F (1,100) = 0.003, p=0.957) were not significantly associated with intention to receive HPV vaccine.
Figure 1.
Characteristics associated with intention to receive HPV
Note:+Trend in proportions assessed with linear-by-linear association test.
Multivariate Logistic Regression Analysis
Due to the small sample size, we selected five variables (age, years in the U.S., major, awareness of cervical cancer vaccine, HPV recommendation by doctors and parents, and knowledge score) among other predictor variables. In the multiple logistic regression analysis, HPV recommendation by parents (OR=4.58, 95% CI, 1.37–15.36) and a high level of knowledge (OR=1.11, 95% CI, 1.11–1.22) were determined to be an independent predictor of intention to receive the HPV vaccine (Table 6).
Table 6.
Characteristics of 104 Korean college women and multivariate analysis of association between variables and intention to receive HPV vaccination
| Adjusted OR (95% CI) | p-value | |
|---|---|---|
| Age | 1.16 (0.92 – 1.45) | 0.216 |
| Year in the US | ||
| US-born | Ref. | 0.235 |
| 0–5 years | 3.47 (0.79 – 15.31) | 0.100 |
| More than 6 years | 1.63 (0.39 – 6.89) | 0.505 |
| Major | ||
| Health-related major | 2.40 (0.80 – 7.20) | 0.118 |
| Awareness | ||
| Heard of cervical cancer vaccine | 2.42 (0.58 – 10.07) | 0.226 |
| Recommendation | ||
| Doctor | 2.03 (0.588–7.07) | 0.268 |
| Parents | 4.58 (1.37–15.36) | 0.014* |
| Knowledge Score | 1.11 (1.11 – 1.22) | 0.025* |
Note. OR= odds ratio, CI=confidence interval, p<0.05
Discussion
In this study of 104 Korean American college women from six states in the Northeastern region, we found that most were not aware of the HPV vaccine and had low knowledge of HPV, HPV vaccine, and cervical cancer. These findings stand in contrast to the false assumption that college students have higher knowledge of health issues and health literacy because of their education (Kim et al., 2015). Participants were more familiar with the term “cervical cancer vaccine” (66.3%) than the term HPV vaccine or Gardasil (51.9%), which is consistent with other studies focusing on Korean or Korean American women (Kim et al., 2017; Kang & Kim, 2011). In Korea, the HPV vaccine is widely advertised as cervical cancer vaccine (자궁경부암 백신) (Kim et al., 2017). This can mislead Korean Americans to perceive that men cannot get the HPV vaccine or think that the HPV vaccine is a different vaccine than the cervical cancer vaccine. Further research should be more inclusive, including young adults from the Korean American community with diverse characteristics (e.g., male, non-college students) to provide HPV education in young Korean American adults.
The 2011–2015 National Health Interview Survey indicated that foreign-born Asian women had lower initiation of HPV vaccination compared to U.S.-born Asian women. However, the results of the present study showed that foreign-born Korean women had higher intention to receive the HPV vaccine than U.S. born. Although intention to receive HPV vaccination has been a strong predictor of HPV vaccination uptake in previous research (Allen et al., 2009; Bendik et al., 2011; Bynum et al., 2011; Patel et al., 2012; Patel et al., 2014; Ratanasiripong et al., 2013), the actual HPV vaccination behavior of foreign-born Korean college women may be different from their intention to receive HPV vaccination due to their unique social and cultural barriers to HPV vaccination. Unlike previous studies that have focused on majority populations, this study found a considerable number of Korean American college women worried about getting the HPV vaccine because they were not familiar with medical terminology and the health care system in the U.S. This suggests that Korean American college women may struggle with different cultural stressors or cultural conflict especially related to health care access than other college students (Ahn et al., 2008; Hovey et al., 2006; Kang et al., 2010). The findings of this study have recognized the need for emphasizing importance of increasing and educating young Korean Americans the importance and benefits of HPV vaccination. Moreover, it is critical to provide information about access to HPV vaccines (e.g. cost, insurance coverage, where to get the HPV vaccine) to facilitate HPV vaccination among foreign-born Koreans or Korean Americans.
Another unique finding of this study is that nearly half of respondents (48.5%) reported they did not get the HPV vaccine because they are too busy. This finding confirms the findings of our earlier qualitative study (Kim et al., 2017). One factor that could affect feeling too busy is that Korean American college students often experience high levels of stress caused by schoolwork and sociocultural-related situations (Gloria & Ho, 2003; Lee, Koeske & Sales, 2004; Miller et al, 2011). Consistent with previous studies, our results indicated that Korean American college women always or very often felt stressed (Alberta, & Ho, 2003; Lee, Koeske & Sales, 2004; Miller et al, 2011). The mindset of being busy and feeling stressed may influence their decision-making about receiving the HPV vaccine, leading to choices such as refusing or delaying receiving the HPV vaccine. There are few culturally relevant interventions about HPV and the HPV vaccine available in the U.S. for young Korean Americans. HPV vaccination strategies should include culturally and linguistically relevant education programs to facilitate HPV vaccination.
Participants reported a lack of recommendation by health care providers to receive the HPV vaccine. Health care providers have previously discouraged Korean American college students from getting the HPV vaccine because the healthcare providers were misinformed that “Korean or Asian women were less prone to cervical cancer” (Kim et al., 2017). HPV vaccine recommendations were strongly associated with HPV vaccine uptake among racial and ethnic minorities in previous studies (Cohen et al,2015; Ylitalo et al., 2013). Ironically however, some racial and ethnic minorities were less likely to receive a recommendation from health care providers (Cohen et al, 2015; Ylitalo et al., 2013). In future studies, HPV vaccine education efforts should target health care providers to increase HPV vaccination rates.
This study has limitations that may affect the generalizability of the findings. The participants in this study were restricted to inclusion criteria. However, the goal of this study was to identify knowledge in Korean American women that is often overlooked in American literature. Although we found statistically significant associations from the multivariate logistic regression analysis, it is important to confirm these findings with a larger study. Response bias is a possibility in self-administered surveys owing to misunderstanding of questions, wording of questions (e.g., negative/positive wording, direct/indirect questions, personal/impersonal wording), and social desirability bias. Studies indicated that Korean female college students have often been uncomfortable talking about the topic of sexual behavior or STI-related topics (Kim et al., 2017; Sohn & Park, 2012). To mitigate this bias and discomfort, respondents had the option to select “I don’t know” for questions concerning sexual behavior, screening behavior (i.e., Pap smear, HPV testing, STI testing), and relationship status.
Conclusion
This study presented the factors associated with intention to obtain HPV vaccination among unvaccinated Korean American college women. This study adds to the literature, offering potential avenues for intervention that have not previously been recognized to promote HPV vaccination among Korean American college students. Findings from this study suggest a need for developing HPV interventions that address the unique characteristics of Korean American college women, such as generational differences and the cultural barriers to health literacy in receiving HPV vaccination. This may play an important role in promoting HPV vaccination among Korean American college women.
Supplementary Material
Acknowledgements:
This study was funded by American Cancer Society (Grant Number: DSCN-129572).
Footnotes
Disclosure of Potential Conflicts of Interest:
No potential conflicts of interest were disclosed.
Conflict of interest: The authors declare that they have no conflict of interest
References
- Adegoke O, Kulasingam S, & Virnig B (2012). Cervical cancer trends in the United States: a 35-year population-based analysis. Journal of Women’s Health, 21(10), 1031–1037. 10.1089/jwh.2011.3385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn AJ, Park YS and Kim BSK (2008). Asian cultural values gap, cognitive flexibility, coping strategies, and parent-child conflicts among Korean Americans. Cultural Diversity and Ethnic Minority Psychology, 14(4), 353–363 [DOI] [PubMed] [Google Scholar]
- Albaum G, Wiley J Roster CA, & Smith SM (2011). Visiting item non-responses in Internet survey data collection. International Journal of Market Research, 53(5), 687–703. [Google Scholar]
- Allen J, Mohllajee A, Shelton R, Othus M, Fontenot H, & Hanna R (2009). Stage of adoption of the human papillomavirus vaccine among college women. Preventive Medicine, 48(5), 420–425. [DOI] [PubMed] [Google Scholar]
- Bendik M, Mayo R, & Parker V (2011). Knowledge, perceptions, and motivations related to HPV vaccination among college women. Journal of Cancer Education, 26(3), 459–464. doi: 10.1007/s13187-011-0200-8 [DOI] [PubMed] [Google Scholar]
- Bynum SA, Brandt HM, Friedman DB, Annang L, & Tanner A (2011). Knowledge, beliefs, and behaviors: Examining human papillomavirus-related gender differences among African American college students. Journal of American College Health, 59(4), 296–302. [DOI] [PubMed] [Google Scholar]
- Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Schootman M, Bucholz KK, Peipert JF, Sanders-Thompson V, Cottler LB, and Bierut LJ. (2009). Age of sexual debut among US adolescents. Contraception, 80(2), 158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention [CDC]. (2015). Epidemiology and prevention of vaccine-preventable diseases. E-book, the Pink Book, 13th ed. Washington DC: Public Health Foundation. [Google Scholar]
- Choi E, Heo GJ, Song Y, & Han H-R (2016). Community health worker perspectives on recruitment and retention of recent immigrant women in a randomized clinical trial. Family & Community Health: The Journal of Health Promotion & Maintenance, 39(1), 53–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen T, Legg JS, Hutchinson J, Levy J, & Bosher W (2015). Factors influencing HPV vaccine use among racially diverse female college students. Journal of Health Disparities Research & Practice, 8(2), 75–88. [Google Scholar]
- Dolnicar S & Grün B (2014). Including don’t know answer options in brand image surveys Improves data quality. International Journal of Market Research, 56(1) 33–50. [Google Scholar]
- Fang CY, Ma GX, Handorf EA, Feng Z, Tan Y, Rhee J, … Koh HS (2017). Addressing multilevel barriers to cervical cancer screening in Korean American women: A randomized trial of a community-based intervention. Cancer, 123(6), 1018–1026. 10.1002/cncr.30391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloria AM & Ho TA (2003). Environmental, social, and psychological experiences of Asian American undergraduates: examining issues of academic persistence. Journal of Counseling & Development, 81(1), 93–105, doi: 10.1002/j.1556-6678.2003.tb00230.x [DOI] [Google Scholar]
- Han H-R, Song Y, Kim M, Hedlin HK, Kim K, Ben Lee H, & Roter D (2017). Breast and cervical cancer screening literacy among Korean American women: a community health worker-led intervention. American Journal of Public Health, 107(1), 159–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hildesheim A, Herrero R, Wacholder S, Rodriguez AC, Solomon D, Bratti MC, Porras C (2007). Effect of human papillomavirus 16/18 l1 viruslike particle vaccine among young women with preexisting infection. Journal of the American Medical Associations, 298(7), 743–753. [DOI] [PubMed] [Google Scholar]
- Hovey JD, Kim SE, & Seligman LD (2006). The influences of cultural values, ethnic identity, and language use on the mental health of Korean American college students. Journal of Psychology, 140(5), 499–511. [DOI] [PubMed] [Google Scholar]
- Kang H, & Kim J (2011). Knowledge, attitudes of human papillomavirus vaccine, and intention to obtain vaccine among Korean female undergraduate students. Women & Health 51, no. 8: 759–776. [DOI] [PubMed] [Google Scholar]
- Kang H, Okazaki S, Abelmann N, Kim-Prieto C, & Lan S (2010). Redeeming immigrant parents: How Korean American emerging adults reinterpret their childhood. Journal of Adolescent Research, 25(3), 441–464. [Google Scholar]
- Kim M (2017). “I Want to Know More about the HPV Vaccine”: Stories by Korean American College Women. (Doctoral dissertation). Retrieved from https://scholarworks.umb.edu/doctoral_dissertations/372
- Kim M, Lee H, Kiang P, & Kim D (2017). Human Papillomavirus: A qualitative study of Korean American female college students’ attitudes toward vaccination. Clinical Journal of Oncology Nursing, 21(5), E239–E247. [DOI] [PubMed] [Google Scholar]
- Kim M, Lee H, Kiang P, Watanabe P, Torres MI, Halon P, Shi L, & Church DR (2015). Debunking the myth: low knowledge levels of HBV infection among Asian American college students. Asia-Pacific Journal of Oncology Nursing, 2(1), 1–16. 10.4103/2347-5625.152399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Chen L, Jung MY, Baezconde-Garbanati L, & Juon H-S (2014). Acculturation and cancer screening among Asian Americans: role of health insurance and having a regular physician. Journal of Community Health, 39(2), 201–212. 10.1007/s10900-013-9763-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee D, Koo Y, Yoon B, & Choi D (2010). Reproductive health characteristics of urban South Korean women. Gynecologic & Obstetric Investigation, 70(3), 154–159. [DOI] [PubMed] [Google Scholar]
- Lee H, Kiang P, Watanabe P, Halon P, Shi L, & Church DR (2013). Hepatitis B virus infection and immunizations among Asian American college students: infection, exposure, and immunity rates. Journal of American College Health, 61(2), 67–74. [DOI] [PubMed] [Google Scholar]
- Lee J, Koeske GF, & Sales E (2004). Social support buffering of acculturative stress: a study of mental health symptoms among Korean international students. International Journal of Intercultural Relations, 28(5), 399–414. doi: 10.1016/j.ijintrel.2004.08.005 [DOI] [Google Scholar]
- Miller MJ, Yang M, Farrell JA, & Lin L (2011). Racial and cultural factors affecting the mental health of Asian Americans. The American Journal of Orthopsychiatry, 81(4) 489–497. doi: 10.1111/j.1939-0025.2011.01118.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pallant J (2013). SPSS survival manual: a step by step guide to data analysis using IBM SPSS. Open University Press: Maidenhead, UK [Google Scholar]
- Patel A, Stern L, Unger Z, Debevec E, Roston A, Hanover R, & Morfesis J (2014). Staying on track: A cluster randomized controlled trial of automated reminders aimed at increasing human papillomavirus vaccine completion. Vaccine, 32(21), 2428–2433. 10.1016/j.vaccine. [DOI] [PubMed] [Google Scholar]
- Patel DA, Zochowski M, Peterman S, Dempsey AF, Ernst S, & Dalton VK (2012). Human Papillomavirus vaccine intent and uptake among female college students. Journal of American College Health, 60(2), 151–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ratanasiripong NT, Cheng A, & Enriquez M (2013). What college women know, think, and do about human papillomavirus (HPV) and HPV vaccine. Vaccine, 31(10), 1370–1376 [DOI] [PubMed] [Google Scholar]
- Sohn A& Park S (2012). HIV/AIDS Knowledge, Stigmatizing Attitudes, and Related Behaviors and Factors that Affect Stigmatizing Attitudes against HIV/AIDS among Korean Adolescents. Osong Public Health and Research Perspectives, 3(1), 24–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung W-C, Lu M, Granner M, & Sohn J (2017). Assessing perceived benefits/barriers and self-efficacy for cervical cancer screening among Korean American women. Health Care for Women International, 38(9), 945–955. [DOI] [PubMed] [Google Scholar]
- Wang SS, Carreon JD, Gomez SL, & Devesa SS (2010). Cervical cancer incidence among 6 Asian ethnic groups in the United States, 1996 through 2004. Cancer, 116(4), 949–956. 10.1002/cncr.24843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward KK, Shah NR, Saenz CC, McHale MT, Alvarez EA, & Plaxe SC (2012). Changing demographics of cervical cancer in the United States (1973–2008). Gynecologic Oncology, 126(3), 330–333. 10.1016/j.ygyno.2012.05.035 [DOI] [PubMed] [Google Scholar]
- World Health Organization [WHO]. (2016). Human papillomavirus (HPV) and cervical cancer, Fact Sheet No 380. Accessed 17 February 2016 http://www.who.int/mediacentre/factsheets/fs380/en/
- Ylitalo KR Lee H, and Mehta NK (2013). Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US national immunization survey. American Journal of Public Health, 103(1) 164–169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.