Abstract
The study objectives were to 1) evaluate the criterion validity and reliability of the Mi Band 2 wearable activity monitor to measure steps during a six-minute walk test (6MWT), a treadmill walking test at various speed (1.28 km/h, 1.92 km/h, and 2.88 km/h) and a stair climbing test; 2) assess the validity and reliability of the monitor to measure heart rate during rest and exercise. Fourteen participants (females: n = 8; mean age ± SD: 23 ± 4.2) completed the study. The mean body mass index was 22 ± 3.6. The majority (~92%) of the Mi Band met the standard of 5% absolute percent error for measuring steps during the 6MWT. However, the Mi Band underestimated steps at slower walking speeds (< 2.88 km/h). Mi Band showed good internal consistency during the six-minute walk test and stairs climb (ICC: 0.83). The validity and reliability of the Mi Band to measure heart rate may not be suited for clinical or research use. The Mi Band significantly underestimated heart rate during exercise. Overall, caution is required when interpreting the steps recorded (at slower speeds) and heart rate measurements.
Keywords: Activity monitor, step count, heart rate sensing, accuracy testing, test-retest reliability, wearable technology
INTRODUCTION
Regular physical activity is critical to maintaining good health and preventing chronic disease (25). The use of accelerometers and heart rate monitors found in wearable activity watches, also known as wearables or activity monitors, has become a common approach for quantifying daily physical activity, providing users with a method of tracking exercise intensity (using heart rate) and for setting activity goals in physical activity interventions (16, 17, 27, 28). These wearable activity monitors are small and lightweight and are assembled into portable bands that are worn on the wrist. Current wrist-worn wearable activity monitors typically range from $100–400, however, there is a new influx of relatively low-cost wearable monitors (about $30–50). These new devices allow the wearable wrist-worn technology to be a more accessible and cost-effective means to measure steps and heart rate and help participants improve their physical activity levels, health, and well-being (9, 14, 19, 27, 29). The Mi Band 2 (Xiaomi, Inc) is a clear example of this new wave of affordable physical activity monitoring devices. The Mi Band 2 is available for approximately $30 USD and has the capability to export the data collected for more detailed analysis, providing researchers a myriad of inexpensive methods to record and analyze physical activity in participant populations.
Mi Band 2 can record steps and heart rate for up to 20 days. This function makes it an ideal tool for tracking physical activity level for longer periods of time. The ability to track heart rate in real-time can be used to monitor exercise intensity. Thus, Mi Band 2 could be a useful tool for the general public, physical activity researchers and exercise professionals to track and monitor physical activity. However, the psychometric properties of the Mi Band 2 activity monitor have not been independently established. The study objectives were to 1) assess the criterion validity and to test the reliability of the Mi Band 2 in measuring steps during the six-minute walk test (6MWT), treadmill walk at various speeds, and stairs climbing; 2) evaluate the construct validity and test the reliability of the Mi Band 2 in measuring heart rate during rest and exercise conditions. We hypothesized that the Mi Band 2 would be valid and reliable in measuring steps and heart rate.
METHODS
Participants
This study was approved by the Research Ethics Board and it was carried out fully in accordance to the ethical standards of the Helsinki Declaration and standards of the International Journal of Exercise Science (18). Research participation was promoted using online advertisements and publicly displayed posters on university campus. Fourteen healthy adults over the age of 18 were recruited to participate in the study. All participants were recruited via research posters from May to September 2018. We obtained written informed consent from all research participants. Participants were able to withdraw from the experiment at any time during the study. Exclusion criteria included mobility impairment, inability to walk up and down 2 flights of stairs, and known heart conditions (e.g. irregular heartbeat, heart disease).
Protocol
Qualified participants were asked to visit our lab for one hour to complete the experimental protocol. Participants’ age, sex, height, weight, waist and hip circumferences, were recorded by a research assistant prior to completing the step and heart rate measurements. The participants were also asked to complete the Fitzpatrick Skin Scale (10) questionnaire.
The Mi Band device contains a tri-axial micro-electromechanical system accelerometer, which can detect motion in three planes: vertical, anterior-posterior, and medio-lateral. The validity and reliability of the Mi Band to measure steps were assessed during the 6MWT, treadmill walking, and stairs climbing. The participants completed a 6MWT test in a 30-meter indoor course that was marked on the floor using masking tape and highly visible cones (2). The participants wore a Mi Band 2 activity monitor on both their left and right wrists during the test in order to establish reliability measure. The research assistant recorded the number of steps shown on the screen of the Mi Band activity monitor prior to the start of the 6MWT. A second research assistant recorded a video of the participants performing the six-minute walk test to determine steps. At the end of the 6MWT, registered steps shown on the screen of the Mi Band monitor were recorded and the monitor was reset to zero in between participants. The criterion steps were determined after concluding the entire experimental procedure by having two research assistants counting the number of steps in the recorded video during the 6MWT.
After the 6MWT, participants were invited to complete the treadmill-walking test (Woodway, Waukesha, WI, USA) at three different velocities: 1.28 km/h (0.36m/sec), 1.92 km/h (0.53 m/sec), and 2.88 km/h (0.8 m/sec). Participants were instructed to walk as naturally as possible at each velocity stage and each stage lasted two minutes, totaling six minutes of walking on the treadmill. Step counts registered by each Mi Band (i.e. one on the left wrist and one on the right wrist), were shown on the monitor screen and recorded for each velocity stage. Similar to the 6MWT, a second research assistant recorded a video for the treadmill test and step counts were manually counted by two research assistants to determine criterion after concluding the entire experimental procedure.
Upon concluding the treadmill test, participants performed a stair-climbing test. The participants were required to climb and descend two flights of stairs three consecutive times. At the beginning of the test, the experimenter instructed each participant to stand stationary at the bottom of the stairwell and await the experimenter’s command to begin climbing the stairs. At the end of the test, the experimenter recorded the steps shown on the Mi Band monitor screen on the left and right wrist. A second research assistant recorded the video for the stair-climbing test and step counts were manually counted by two research assistants to determine criterion steps by a research assistant after concluding the entire experimental procedure.
The Mi Band device contains an optical heart rate measurement system designed to measure heart rate based on photoplethysmography (24). Photoplethysmography measures heart rate by evaluating skin perfusion based on refraction and absorption of mid-wavelength visible (i.e., green) light detected by a sensor held on the skin (13, 24). Upon completion of the step measurement, participants were invited to perform a protocol designed to evaluate the validity and reliability of the heart rate measured by the Mi Band 2 activity monitor. Construct validity of the heart rate was determined using a three-lead electrocardiogram (Biopac Systems Canada Inc.). Participants wore the Mi Band activity trackers on their right and left wrists in order to establish a reliability measure. We measured the participants’ heart rates during the supine position for two minutes, followed by two minutes of sitting upright in a comfortable chair. Afterwards, participants performed graded exercises on a cycle ergometer (Monark 828E Ergomedic) at 0.5, 1, 1.5, and 2 kpm peddling at 60 revolutions per minute (RPM). Each resistance stage lasted 2 minutes. Participants wore Mi Bands on both wrists to measure heart rate, which was recorded every 15 seconds at rest and throughout each test.
Statistical Analysis
All analyses were performed using SPSS (Version 21). Based on a previous study, an acceptable measurement error for wrist-worn activity wearable monitors is within ± 5% (22). We calculated absolute percent error and percent error (indicating the direction of the error) using the following formulas:
Absolute value from each was accepted as the absolute percent error.
Criterion validity of the Mi Band in measuring steps was assessed during the 6MWT, treadmill test and stair-climbing test. The difference in steps was computed (i.e., Mi Band steps-criterion) and compared to zero using sample t-tests in order to assess whether there was a significant difference between Mi Band steps and the criterion. Construct validity of the Mi Band in measuring heartrate was examined during a bike test. The difference in heart rate was calculated (i.e., Mi Band heart rate – ECG heart rate) and compared to zero using sample t-tests in order to assess whether Mi Band heart rate was significantly different from heart rate measured using ECG. Bland-Altman plots were also constructed to demonstrate the distribution of the individual scores around zero (3).
We used intra-class correlation coefficients (ICC) to evaluate reliability between the registered steps and heart rate worn on the left and right wrists during the various testing conditions. ICC values were interpreted as follows: poor = < 0.4, fair = 0.4 to 0.59, good = 0.6 to 0.74, excellent = > 0.75 (5). Linear regression analysis was used to examine whether skin color and BMI were associated with heart rate percent error. Walking speed for the 6MWT was calculated using the following equation: Walking speed (km/h) = (6 MWT / 6 minutes) × 60. A p-value of less than 0.05 was used to denote statistical significance for all analyses.
RESULTS
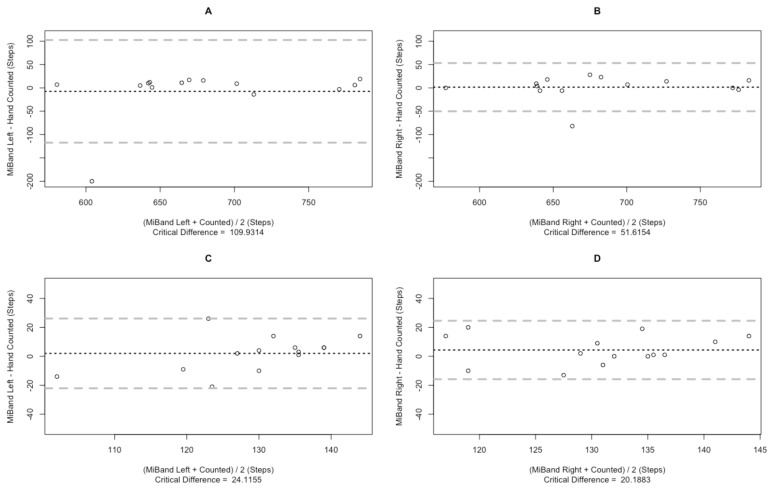
All recruited participants completed the study (n = 14; 8 females). Baseline characteristics are described in Table 1. During the 6MWT, the participants walked a mean distance of 528 ± 26.0m. The average walking speed during the 6MWT was 5.3 km/h and ranged from 4.2 km/h to 7.1 km/h. We observed no significant differences between criterion steps and the steps registered by the Mi Band wore on the left and right wrists during the 6MWT (p > 0.05). The Bland-Altman plot of the Mi Band during the 6MWT did not show a systematic error (Figure 1 A, B). The percent error for the Mi Band under 6MWT ranged from −28.4% to 2.6% and −11.7% to 4.2% (on the left and right wrist, respectively). Ninety-three percent of Mi Bands used during the 6MWT walking achieved less than ± 5% error. The intra-class correlation for the Mi Bands worn on the left versus the right wrists during 6MWT and stair-climbing was 0.83.
Table 1.
Baseline Characteristics (N=14; 8 Females).
| Mean | SD | Range | |
|---|---|---|---|
| Age | 23 | 4.2 | 18–32 |
| BMI | 22.3 | 3.6 | 18–31 |
| Waist (cm) | 78.1 | 11.5 | 63–109 |
| Hip/Waist Ratio | 0.89 | 0.08 | 0.81–1.03 |
| Skin Type | 2.6 | 1.1 | 1–4 |
Skin Type: 1 = always burns, never tans; 6 = Never burns (deeply pigmented dark brown to darkest brown)
Figure 1.
Bland-Altman plots depicting step measurement bias of the Mi Band during 6MWT and stairs climb: A) Mi Band worn on the left wrist during 6MWT; B) Mi Band worn on the right wrist during 6MWT; C) Mi Band worn on the left wrist during the stairs climb; D) Mi Band worn on the right wrist during the stairs climb; Solid horizontal lines = mean error score, dashed lines = 95% predicted intervals.
We did not observe a significant difference between criterion steps and the Mi Bands worn on either the left or right wrists (p > 0.05) during the stair-climbing test. However, only 50% of Mi Bands used during the stair walking achieved less than ± 5% error. The percent error for the Mi Band during the stair walking ranged from −9.7% to 18.4% and −15.7% to 23.6% for left and right wrists, respectively. The Bland-Altman plot of the Mi Band during the stair-climbing task was shown in Figure 1 C, D. The intra-class correlation for the Mi Band, worn on the left versus the right wrist during the stair-climbing, was 0.62 (Table 2).
Table 2.
Absolute Percent Error (APE) for measuring steps (n = 14).
| APE (% ± SD) | Range APE % Min-Max | Percent of monitors that under-estimated (%)a | Percent of monitors that over-estimated (%)a | |
|---|---|---|---|---|
| 6MWT | ||||
| Right Hand | 2.6 ±3.1 | 0.2–28 | 21 | 79 |
| Left Hand | 3.4 ±7.2 | 0.5–11.6 | 33 | 67 |
| Treadmill (1.28m/h) | ||||
| Right Hand | 86.5 ± 25.2 | 15.5–100 | 93 | 7 |
| Left Hand | 83.9 ± 29.6 | 10.1–100 | 93 | 7 |
| Treadmill (1.92m/h) | ||||
| Right Hand | 57.1 ± 36.7 | 3.5–100 | 86 | 14 |
| Left Hand | 41.3 ± 37.8 | 2.1–100 | 86 | 14 |
| Treadmill (2.88m/h) | ||||
| Right Hand | 8.6 ± 7.6 | 0.5–28.4 | 57 | 43 |
| Left Hand | 8.6 ± 6.4 | 1.8–24.7 | 38 | 61 |
| Stairs walking | ||||
| Right Hand | 8.0 ± 5.6 | 0.7–23.6 | 29 | 71 |
| Left Hand | 7.8 ± 6.4 | 0.7–18.4 | 25 | 75 |
Note.
Percent of monitors that under or over-estimated represents the number of monitors that under and over underestimated compared to criterion within each activity type.
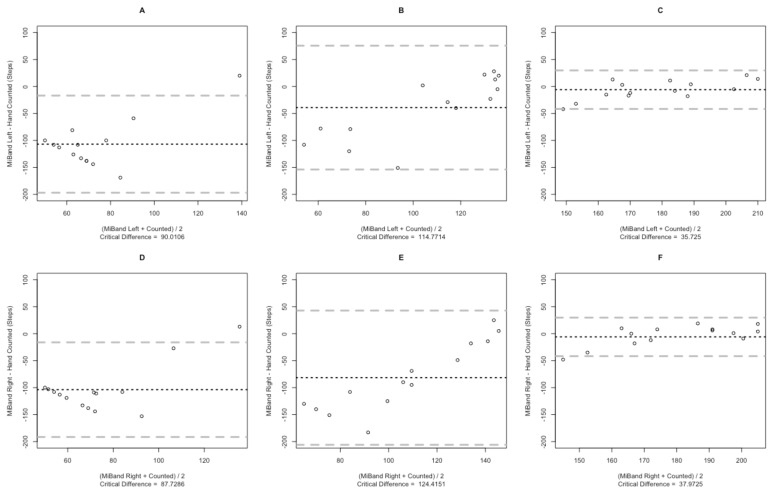
There was a significant difference between criterion steps and steps registered by the Mi Band worn on the left (p < 0.01) and right wrist (p < 0.01) during the treadmill testing at speeds of 1.28 km/h and 1.92 km/h (Table 2). However, there was no significant difference between criterion and the Mi Band during the treadmill test at 2.88 km/h (p > 0.05). The percent error for the Mi Band during the treadmill test at 2.88 km/h ranged from −24.7% to 10.7% and −28.4% to 10.7% for left and right wrists, respectively. However, only 36% of Mi Bands used during the treadmill test at 2.88 km/h achieved less than ± 3% error. The intra-class correlation for the Mi Band worn on the left versus the right wrist during the treadmill test at 1.28 km/h, 1.92 km/h, and 2.88 km/h were 0.96, 0.83, and 0.73, respectively. The Bland-Altman plot comparing the Mi Band and criterion steps during the treadmill test showed a greater systematic error during slower walking speeds (Figure 2).
Figure 2.
Bland-Altman plots depicting step measurement bias of the Mi Band during treadmill test: A) Mi Band worn on the left wrist during 1.28 km/h; B) Mi Band worn on the right wrist during 1.28 km/h; C) Mi Band worn on the left wrist during 1.92 km/h; D) Mi Band worn on the right wrist during 1.92 km/h; E) Mi Band worn on the left wrist during 2.88 km/h; F) Mi Band worn on the right wrist during 2.88 km/h. Solid horizontal line = mean error score, dashed lines = 95% predicted intervals.
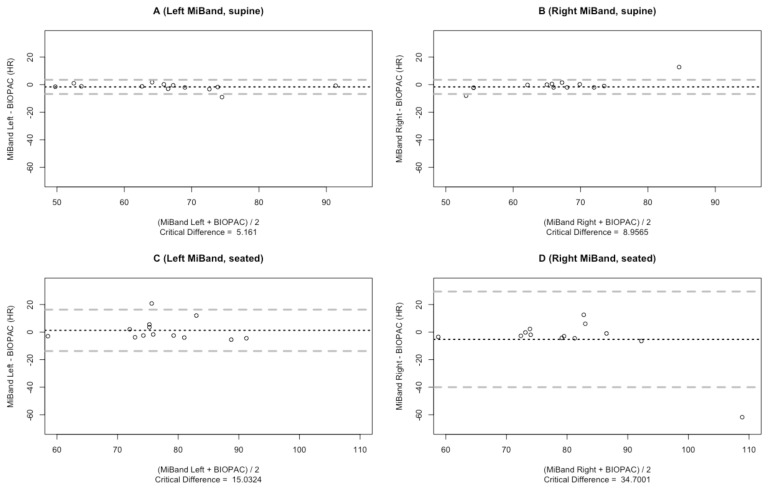
Heart Rate: The mean resting heart rate measured by the ECG during supine and seated positions, was 67 ± 3.5 and 75 ± 2.5 beats per minute (BPM). The mean heart rates measured by the ECG during cycling at 0.5, 1, 1.5, and 2.0 kpm were 92 ± 3.7, 104 ± 3.5, 114 ± 3.0, and 133 ± 3.0 BPM, respectively. During both supine and seated positions, we observed no significant differences between heart rates recorded from the ECG and the Mi Band worn on either the left (p > 0.05) or right wrist (p > 0.05) (see Figure 3 for Bland-Altman plot). However, a significant difference was observed between ECG recordings and heart rates measured by the Mi Band during all exercise conditions (p > 0.05).
Figure 3.
Bland-Altman plots depicting heart rate measurement bias of the Mi Band during rest conditions: A) Mi Band worn on the left wrist during supine; B) Mi Band worn on the right wrist during supine; C) Mi Band worn on the left wrist during seated position; D) Mi Band worn on the right wrist during seated position; Solid horizontal line = mean error score, dashed lines; 95% predicted intervals.
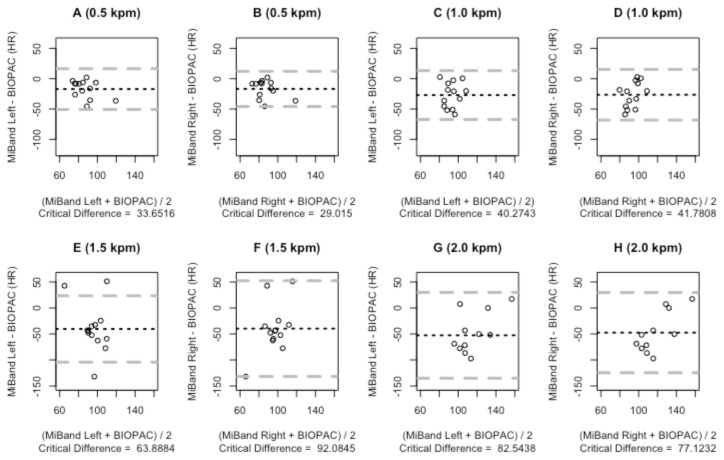
The percent error for the heart rate recorded by the Mi Band during the supine position ranged from −15.3% to 19.86% and −9.07% to 7.69% for left and right wrists, respectively. Meanwhile, the percent error for heart rates measured by the Mi Band during the seated position ranged from −10.0% to 7.46% and −24.1% to 6.4% for left and right wrists, respectively. The number of Mi Bands achieving less than ± 5% error when measuring heart rates during supine and seated positions was 62% and 57%, respectively. Mi Band devices tend to underestimate heart rate values during exercise conditions (Table 3). The ICCs for measuring heart rate using Mi Bands during rest (ICC: supine = 0.72; seated = 0.69) were higher compared with exercise conditions (ICC: Bike at 0.5 kpm = 0.47; Bike at 1.0 kpm = 0.66; Bike at 1.5 kpm = 0.67; and Bike at 2.0 kpm = 0.71). Bland-Altman plots showed a greater systematic error between the heart rate measured by Mi Band devices and the ECG during exercise conditions (Figure 4). Regression analysis did not show that heart rate percent error was significantly influenced by skin color or BMI (p > 0.05).
Table 3.
Absolute Percent Error (APE) for heart rate.
| APE% ±SE | Range APE % Min-Max | Percent of monitors that under-estimated (%)a | Percent of monitors that over-estimated (%)a | |
|---|---|---|---|---|
| Supine | ||||
| Right Hand | 5.5 ±1.9 | 0.5–14.6 | 53 | 64 |
| Left Hand | 4.7 ±0.83 | 1.0–9.1 | 31 | 69 |
| Sitting | ||||
| Right Hand | 10.8 ±5.8 | 0–35 | 46 | 53 |
| Left Hand | 10.0±4.5 | 0–10 | 39 | 62 |
| Bike (0.5kpm) | ||||
| Right Hand | 16.8 ±3.5 | 2.2–41.7 | 92 | 8 |
| Left Hand | 14.2±2.6 | 2.3–30.0 | 77 | 23 |
| Bike (1.0 kpm) | ||||
| Right Hand | 21.9 ±4.8 | 0.3–44.4 | 85 | 15 |
| Left Hand | 17.4 ±3.1 | 3.6–33.1 | 92 | 8 |
| Bike (1.5 kpm) | ||||
| Right Hand | 32.2 ±5.2 | 0.5–55.0 | 92 | 8 |
| Left Hand | 27.3 ±3.8 | 4.2–44.5 | 92 | 8 |
| Bike (2.0 kpm) | ||||
| Right Hand | 38.1 ±4.8 | 1.4–59.9 | 82 | 18 |
| Left Hand | 37.4 ±5.3 | 0.4–57.1 | 85 | 15 |
| Stairs walking | ||||
| Right Hand | 8.0 ±5.6 | 0.7–23.6 | 29 | 71 |
| Left Hand | 7.8 ±6.4 | 0.7–18.4 | 25 | 75 |
Note.
Percent of monitors that under or over-estimated represents the number of monitors that under and over underestimated compared to ECG within each activity type.
Figure 4.
Bland-Altman plots depicting heart rate measurement bias of the Mi Band during cycling: A) Mi Band worn on the left wrist during 0.5 kpm; B) Mi Band worn on the right wrist during 0.5 kpm; C) Mi Band worn on the left wrist during 1 kpm; D) Mi Band worn on the right wrist during 1 kpm; E) Mi Band worn on the left wrist during 1.5 kpm; F) Mi Band worn on the right wrist during 1.5 kpm. G) Mi Band worn on the left wrist during 2 kpm; H) Mi Band worn on the right wrist during 2 kpm. Solid horizontal line = mean error score, dashed lines = 95% predicted intervals.
DISCUSSION
The current study evaluated the validity and reliability of the Mi Band 2 wearable activity monitor to measure steps and heart rate. This is the first study to our knowledge to independently validate the Mi Band 2 wearable monitor. We found that the Mi Band 2 is suitable to measure steps but not heart rate. The majority (~92%) of the Mi Bands met the standard of 5% absolute percent error for measuring steps during the 6MWT, but only about two-thirds met the standard of 5% absolute error for measuring heart rate at rest. Overall, the Mi Band significantly underestimated steps at slower walking speeds as well as underestimated heart rate during exercise.
Decreased accuracy of the Mi Band during slower walking speeds may be due to its internal algorithms in detecting gait. The lower walking speeds may not be able to generate enough acceleration for the Mi Band algorithms to recognize that it is a step thus, underestimating the number of steps (26). This limitation of the Mi Band may be particularly limited in tracking activity levels in individuals with gait limitations, such as older adults. Previous validation studies of wearable activity monitors have also reported similar limitations (6, 8, 21, 23). For example, similar tri-axial accelerometer-based step monitors all have demonstrated that the accuracy of the activity monitors decreased at slower walking speeds between 3.2 and 4.5km/h (7, 9, 15). A recent study reported that the Fitbit Flex had −23% bias compared to criterion, and both the Fitbit Zip and Fitbit Flex had −26% bias at slower walking speeds (12). Results from these wearable devices must be interpreted with caution when measuring steps at a lower speed.
The Mi Band uses photoplethysmography to measure heart rate (1), however, this method does suffer from inaccurate measurement relative to gold standard measures (i.e., electrocardiography). Our results showed that the Mi Band tends to underestimate heart rate during exercise. Underestimation of heart rate measured by photoplethysmography has been previously reported (11). The heart rate percent error was the lowest during supine position. However, it is important to consider the practical and clinical significance of the mean difference from criterion. A 5% error of heart rate measurement can significantly influence exercise intensity. A previous study reported that heart rate recording accuracy may decrease with darker than lighter skin tones (24). We found that the heart rate percent error was not influenced by skin tones. However, future studies are warranted with a more diverse sample size.
The reliability of the Mi Band for measuring steps and heart rate was dependent on the activity. The Mi Band displayed lower reliability during walking on a flat surface (6MWT, treadmill) compared with climbing stairs. A potential reason for the lower ICC may be due to the fact that some of the participants were holding the railing when walking up and down the stairs. The acceleration detected by the Mi Band when a person holds onto the railing may be different from not holding on, thus the algorithms may not be able to detect steps appropriately. The lower reliability of the Mi Band 2 for measuring heart rate during exercise than at rest may be due to the fact that photoplethysmography does not directly measure heart rate but instead skin perfusion rate. Thus, the Mi Band may require better algorithms to measure changes in skin perfusion during exercise (1,13).
There were several limitations to the present study. First, our sample size is restricted to healthy adults; thus, this may limit the generalizability of our findings. Second, we assessed the Mi Band device under both rest and exercise conditions in controlled laboratory settings, but we did not measure the device’s accuracy and reliability in free-living conditions. Last, we measured reliability between devices worn on the left and right wrists, but we did not measure reliability over time.
In this study, we evaluated the validity and reliability of the Mi Band 2 to measure steps and heart rate at rest and during exercise conditions. This study has shown that the Mi Band 2 is a suitable tool to measure steps at a moderate pace in healthy adults. The accuracy and reliability of the Mi Band in measuring heart rate may not be suited for clinical or research use. Similar to other wearable activity monitors, the Mi Band device underestimates steps at lower speeds and underestimates heart rate during exercise.
ACKNOWLEDGEMENTS
Author Francisco Colino was supported by MITACS.
REFERENCES
- 1.Allen J. Photoplethysmography and its application in clinical physiological measurement. Physiol Meas. 2007;28(3):R1–39. doi: 10.1088/0967-3334/28/3/R01. [DOI] [PubMed] [Google Scholar]
- 2.ATS committee. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 3.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;327(8476):307–10. [PubMed] [Google Scholar]
- 4.Case MA, Burwick HA, Volpp KG, Patel MS. Accuracy of smartphone applications and wearable devices for tracking physical activity data. JAMA. 2015;313(6):625–6. doi: 10.1001/jama.2014.17841. [DOI] [PubMed] [Google Scholar]
- 5.Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–290. [Google Scholar]
- 6.De Cocker KA, De Meyer J, De Bourdeaudhuij IM, Cardon GM. Non-traditional wearing positions of pedometers: validity and reliability of the Omron HJ-203-ED pedometer under controlled and free-living conditions. J Sci Med Sport. 2012;15(5):418–24. doi: 10.1016/j.jsams.2012.02.002. [DOI] [PubMed] [Google Scholar]
- 7.Colley RC, Barnes JD, Leblanc AG, Borghese M, Boyer C, Tremblay MS. Validity of the SC-StepMX pedometer during treadmill walking and running. Appl Physiol Nutr Metab. 2013;38(5):520–4. doi: 10.1139/apnm-2012-0321. [DOI] [PubMed] [Google Scholar]
- 8.Diaz KM, Krupka DJ, Chang MJ, Peacock J, Ma Y, Goldsmith J, et al. Fitbit(R): An accurate and reliable device for wireless physical activity tracking. Int J Cardiol. 2015;185:138–40. doi: 10.1016/j.ijcard.2015.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Evenson KR, Goto MM, Furberg RD. Systematic review of the validity and reliability of consumer-wearable activity trackers. Int J Behav Nutr Phys Act. 2015;12:159. doi: 10.1186/s12966-015-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzpatrick TB. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124(6):869–71. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- 11.Gorny AW, Liew SJ, Tan CS, Müller-Riemenschneider F. Fitbit Charge HR wireless heart rate monitor: validation study conducted under free-living conditions. JMIR Mhealth Uhealth. 2017;5(10):e157. doi: 10.2196/mhealth.8233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Imboden MT, Nelson MB, Kaminsky LA, Montoye AHK. Comparison of four Fitbit and Jawbone activity monitors with a research-grade ActiGraph accelerometer for estimating physical activity and energy expenditure. Br J Sport Med. 2018;52(13):844–50. doi: 10.1136/bjsports-2016-096990. [DOI] [PubMed] [Google Scholar]
- 13.Jo E, Lewis K, Directo D, Kim MJ, Dolezal BA. Validation of biofeedback wearables for photoplethysmographic heart rate tracking. J Sports Sci Med. 2016;15(3):540–7. [PMC free article] [PubMed] [Google Scholar]
- 14.Liu S, Brooks D, Thomas SG, Eysenbach G, Nolan RP. Effectiveness of User- and Expert-Driven Web-based Hypertension Programs: an RCT. Am J Prev Med. 2018;54(4):576–83. doi: 10.1016/j.amepre.2018.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Liu S, Brooks D, Thomas S, Eysenbach G, Nolan RP. Lifesource XL-18 pedometer for measuring steps under controlled and free-living conditions. J Sports Sci. 2015;33(10):1001–6. doi: 10.1080/02640414.2014.981847. [DOI] [PubMed] [Google Scholar]
- 16.Liu S, Husband C, La H, Juba M, Loucks R, Harrison A, et al. Development of a self-guided web-based intervention to promote physical activity using the multi-process action control framework. Internet Interv. 2019;15:35–42. doi: 10.1016/j.invent.2018.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu S, Marques IG, Perdew MA, Strange K, Hartrick T, Weismiller J, et al. Family-based, healthy living intervention for children with overweight and obesity and their families: a ‘real world’ trial protocol using a randomised wait list control design. BMJ Open. 2019;9:e027183. doi: 10.1136/bmjopen-2018-027183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Navalta JW, Stone WJ, Lyons S. Ethical issues relating to scientific discovery in exercise science. Int J Exerc Sci. 2019;12(1):1–8. doi: 10.70252/EYCD6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nolan RP, Feldman R, Dawes M, Kaczorowski J, Lynn H, Barr SI, et al. Randomized Controlled Trial of E-Counseling for Hypertension: REACH. Circ Cardiovasc Qual Outcomes. 2018;11(7):e004420. doi: 10.1161/CIRCOUTCOMES.117.004420. [DOI] [PubMed] [Google Scholar]
- 20.Nolan RP, Liu S, Payne AYM. E-counseling as an emerging preventive strategy for hypertension. Curr Opin Cardiol. 2014;29(4):319–23. doi: 10.1097/HCO.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 21.Schneider PL, Crouter S, Bassett DR. Pedometer measures of free-living physical activity: comparison of 13 models. Med Sci Sport Exerc. 2004;36(2):331–5. doi: 10.1249/01.MSS.0000113486.60548.E9. [DOI] [PubMed] [Google Scholar]
- 22.Shcherbina A, Mattsson CM, Waggott D, Salisbury H, Christle JW, Hastie T, et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J Pers Med. 2017;7(2):3. doi: 10.3390/jpm7020003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Smith M, Powers M, Henderson O, Bodman T. Accuracy and Reliability of the FitBit ChargeTM Activity Tracker Among Older Adults. Oklahoma AHPERD. 2017;54(3):29–37. [Google Scholar]
- 24.Tamura T, Maeda Y, Sekine M, Yoshida M. Wearable photoplethysmographic sensors—past and present. Electronics. 2014;3(2):282–302. [Google Scholar]
- 25.Tremblay MS, Warburton DE, Janssen I, Paterson DH, Latimer AE, Rhodes RE, et al. New Canadian physical activity guidelines. Appl Physiol Nutr Metab. 2011;36(1):36–58. doi: 10.1139/H11-009. [DOI] [PubMed] [Google Scholar]
- 26.Tudor-Locke C, Williams JE, Reis JP, Pluto D. Utility of pedometers for assessing physical activity: construct validity. Sport Med. 2004;34(5):281–91. doi: 10.2165/00007256-200434050-00001. [DOI] [PubMed] [Google Scholar]
- 27.Wallen MP, Gomersall SR, Keating SE, Wisløff U, Coombes JS. Accuracy of heart rate watches: implications for weight management. PLoS One. 2016;11(5):e0154420. doi: 10.1371/journal.pone.0154420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang R, Blackburn G, Desai M, Phelan D, Gillinov L, Houghtaling P, et al. Accuracy of wrist-worn heart rate monitors. JAMA Cardiol. 2017;2(1):104–6. doi: 10.1001/jamacardio.2016.3340. [DOI] [PubMed] [Google Scholar]
- 29.Yang C-C, Hsu YL. A review of accelerometry-based wearable motion detectors for physical activity monitoring. Sensors. 2010;10(8):7772–88. doi: 10.3390/s100807772. [DOI] [PMC free article] [PubMed] [Google Scholar]