Abstract
Performing yoga in a heated environment (HY) is a popular exercise mode purported to improve range of motion (ROM), body composition, and aerobic fitness. The purpose of this investigation was to compare a session of HY to room temperature yoga (RTY) with regards to ROM, oxygen consumption, caloric expenditure, and biomarkers of acute stress and inflammation. Sixteen experienced yoga practitioners (F14, M2; 40 ± 11yr; 22.6 ± 1.8 kg/m2) completed a 1-hour standardized Bikram sequence in HY (105°F, 40°C) and RTY (74°F, 23.3°C) conditions (order of conditions randomized, humidity standardized at 40%). Intra-exercise metabolic gas exchange and heart rate (HR) was monitored using a metabolic cart. ROM measures were taken pre and post-exercise at the elbow, shoulder, hip, and knee. Cytokines interleukin 6,10 (IL-6, IL-10) and tumor-necrosis-factor alpha (TNF-α) were analyzed from blood samples collected pre- and 30-minutes post-exercise. Intra-exercise metabolic gas exchange and heart rate (HR) was monitored using a metabolic cart. Both bouts elicited similar acute changes in ROM although HY elicited a greater increase in hip abduction (RTYΔ° = 2.3 ± 1.3|HYΔ° = 6.6 ± 1.5; p < 0.05). Mean VO2, peak VO2, %VO2max, HR, and kcal expenditure did not differ between conditions. RER was lower during the HY (RTY = 0.95 ± 0.02| HY = 0.89 ± 0.02; p < 0.05) with a concomitant elevation in fat oxidation (RTY = 0.05 ± 0.01|HY = 0.09 ± 0.01, g·min−1; p < 0.05) and decrease in carbohydrate oxidation (RTY = 0.51 ± 0.04|HY = 0.44 ± 0.03, g·min−1; p < 0.05). Serum IL-6 was increased (15.5 ± 8.0-fold) following HY only (p < 0.05). HY does not significantly elevate aerobic energy cost compared to RTY but may acutely increase fat substrate utilization and hip ROM. Future studies remain needed to establish dose-response relationships for including HY or RTY into well-rounded fitness programs.
Keywords: Yoga, hot yoga, bikram yoga, range of motion, fitness
INTRODUCTION
Yoga is a popular exercise modality, with about 21 million adults in the U.S. having practiced it in 2015, and 31 million U.S. adults having practiced it at least once in their lifetime (44, 62). As an exercise modality, yoga has been reported to increase flexibility and range of motion as well as provide a low impact modality for body weight resistance and stability training (51). In recent years, the practice of performing yoga in heated environments (HY - hot yoga, Bikram Yoga) has become common with purported benefits of increased flexibility, general fitness, reduced systemic inflammation, improved body composition, reductions in blood pressure, muscular strength gain, and improvement in several psychological parameters related to mood and anxiety (28, 39, 57). Typically, HY sessions are performed in ambient temperatures ranging from 90–105° F (32 – 41°C), at a humidity level of 40%–70% (28, 57) depending on the type of practice.
Increased caloric expenditure as a result of physiologic adjustments to exercise in the heat is often used, in part, as a rational for performing HY (13). For example, during moderate-to-high intensity aerobic exercise (>~50%VO2max), an increase in energy expenditure at a given absolute workload has been observed to be caused by the added energy cost of maintaining oxygen delivery to working muscle while also shunting blood to the skin for thermoregulatory purposes (8, 42). Accordingly, increased ambient temperatures have been shown to increase heart rate, oxygen consumption, and perceived stress during steady state aerobic exercise (17, 25). Heated conditions have also been observed to influence substrate oxidation during exercise with the degree of influence being highly dependent on the level of training and heat acclimation (21, 35, 65). For example, untrained adults tend to be more likely to experience and increase in carbohydrate oxidation in heated (compared to thermoneutral) conditions as opposed to heat-acclimated trained individuals who have been observed to have either stable or gradual reductions in carbohydrate oxidation over time during prolonged exercise (41, 65). Conversely, under resting conditions, O’Hearn et al., 2016 (43) observed that heat exposure did not influence substrate oxidation rates or basal energy expenditure. The degree to which these adjustments may occur during yoga exercise is not well known. Boyd et al. 2018 (5) observed that compared to a single session of yoga performed at a thermonetural room temperature (Defined as 70–74°F / 21–23°C), HY was not found to significantly increase oxygen consumption but was found to elevate heart rate and perceived exertion. However, the sessions used in this investigation lasted for a period of 20-minutes and may not reflect common practices of yoga in heated environments that often range from 45-minute to 90-minute sessions (22, 44). In summary, although performing yoga is certainly not analogous to being at rest, a key question remains as to whether or not HY reaches sufficient exercise intensity thresholds to where heat may substantially influence caloric expenditure or substrate utilization fractions beyond performing yoga at room temperature.
HY has also been proposed to acutely increase range of motion (ROM) during exercise and yield greater chronic improvements in flexibility (57, 58). Regarding ROM, heat applied to muscles locally has been observed to increase both active and passive ROM (50). Therefore, it has been proposed that performing yoga under such conditions may provide a similar effect (57). However, while present literature indicates that yoga (in general) can chronically promote increases in flexibility, there is little evidence to suggest that the acute ROM responses to HY differ in comparison to yoga performed at room temperature (RTY).
Lastly, present data indicate that yoga (in general) may acutely and chronically reduce biomarkers of inflammation and increase markers of anti-inflammation in adults (32, 48). For example, experienced yoga practitioners have been observed to have a reduced increase in tumor-necrosis-factor alpha (TNF-α; a pro-inflammatory cytokine) following strenuous exercise compared to non-yoga practitioners as well as reductions in basal TNF-α and interleukin 6 (IL-6; chronic pro-inflammatory cytokine / acute metabolic myokine) (48, 61). In a recent review by Djalilova et al. 2019 (18), it was concluded that yoga may be a viable mode of exercise to reduce inflammation in healthy individuals as well as those with a variety of chronic conditions. Despite these findings, there is little data comparing the responses of HY to RTY with regards to acute alterations in systemic biomarkers of inflammation.
While previous data indicate that HY may provide some additional benefit to RTY, inconsistent reporting and lack of appropriate control data warrant further investigation. Therefore, the purpose of the present investigation was to compare the acute physiologic effects of a single hour long session of HY to a matched session of RTY with regards to aerobic intensity, caloric expenditure, resting hemodynamics, ROM, and biomarkers related to exercise stress and inflammation in experienced yoga practitioners. In light of previous literature, we hypothesized that compared to RTY, HY would not elevate exercise intensity enough to result in increased caloric consumption or cause perturbations in basal systemic inflammatory biomarkers, but that it would result in acute increases in ROM across four major joints (elbow, shoulder, hip, knee).
METHODS
Participants
Sixteen adults (F14, M2; 40 ± 11yr; 162.3 ± 1.9cm, 59.6 ± 6.7kg, 22.6 ± 1.8 kg/m2; VO2max 36.9 ± 7.6 ml•kg•min−1) who were experienced yoga practitioners (5.2 ± 2.6 h/wk of total yoga, 2.5 ± 1.9 h/wk of HY, 8.5 ± 1.1 years practiced) were recruited for this study. Specifically, participants were recruited who had been consistently practicing weekly yoga exercise for a period of over two years and who were familiar with all poses examined in the experimental yoga session based on a standardized Bikram yoga pose sequence (Figure 1, to follow). Prior to participation all participants were screened using a Bruce protocol (7) graded exercise stress test with ECG to assess VO2max and to confirm that participants were healthy enough to perform the exercise trials. Achievement of VO2max was established only under conditions whereby oxygen consumption plateaued with increasing workload, respiratory exchange ratio exceeded 1.2 (VCO2), RPE exceeded 17, and heart rate having to exceed >85% age-predicted maximum. For determining sample size, exercise VO2 and total caloric expenditure were used as our primary outcome variables. Data used for calculation were gathered from previous studies performed by our research team that utilized similar testing measures (27, 33, 34). For a power of 0.8(α = 0.05), a required sample size of 16 participants was calculated for a minimum detectible difference of either 3.5 mlO2·kg·min−1 (1 MET) or 20 kcals respectively.
Figure 1.
Yoga pose sequence performed during both HY and RTY sessions.
Protocol
At least one week following stress test screening, participants were asked to come to the laboratory to complete the first of two experimental yoga sessions. Participants were asked to not perform physical exercise as well as to match dietary intake (nutritional contents, and time of consumption) at least 72 hours prior to each experimental session using a 3-day dietary recall. On the morning of each experimental session, participants were also asked to arrive to the experimental session following a 4-hour fast (excluding water consumption). Consumption of caffeine and other stimulants was also not permitted prior to exercise during study days. During the experimental sessions participants completed a 1-hour standardized yoga exercise bout using a Bikram sequence (Figure 1, to follow) and synced to an instructional video (including instructing on pose sequence, technique, duration, and breathing) in both a heated (HY: 105°F, 40.5°C) and room temperature (RTY: 74°F, 23.3°C) condition on two separate laboratory visits (time of day controlled) separated by a minimum of 96 hours. Room temperature and humidity was monitored before, during, and after the experimental sessions to ensure that both remained stable. The order of the sessions (HY and RTY) were randomized. Humidity was standardized at 40%. Consumption of water or other fluids was not permitted during the exercise sessions. A trained laboratory technician manually assessed blood pressure before and immediately following exercise with subjects in a seated resting position.
Measures of oxygen consumption (VO2), carbon dioxide exhalation (VCO2), respiratory exchange ratio (RER: VCO2/VO2), heart rate, and caloric expenditure were continuously monitored using a calibrated mobile metabolic cart (Ultima, MGC Diagnostics, Saint Paul, MN, USA) during yoga bouts and for a period of 5-minutes with participants standing upright with the upper extremities at rest prior to exercise to confirm proper data recording and cart function.
Substrate oxidation was calculated from gas exchange measures recorded throughout the experimental session using the following standardized equations (31) under the assumption that protein oxidation was negligible during low intensity exercise:
Range of Motion (ROM): Measurements of passive ROM in the upper body (shoulder external & internal rotation, wrist flexion, elbow flexion, scaption, and forward flexion) and lower body (knee flexion, knee extension, hip flexion, hip internal & external rotation, and hip abduction) were taken before and immediately after each yoga session using validated orthopedic clinical techniques (3). Briefly, for each ROM measure, subjects were asked to remain relaxed while their limbs were manually placed whereby ROM was set as the farthest ROM achieved without perceived (indicated by the participants) active stretching elicited by the technician. At the point that each measurement position was reached, a single level digital image was recorded. ROM image analysis was performed independently by three trained members of the laboratory team (blinded to condition, HY/RTY) using digital protractor software (Screen Protractor, Version 4, Iconico®). The same two orthopedic physicians who provided procedures and training for performing ROM analysis also reviewed and provided final approval of ROM measures taken. Intra-observer analysis of agreement exceeded 0.8 for all measures indicating adequate agreement between reviewers.
Acute Post-Exercise Immune Response: Blood samples were taken immediately before and 30-minutes post-exercise in both the HY and RTY conditions using sterile phlebotomy procedures. Blood samples were drawn without stasis from an antecubital vein into Vacutainer tubes. In both instances, participants were seated in a phlebotomy chair at rest for a period of 15-minutes prior to sampling. Cytokine Analysis: Briefly, following 30 min of centrifugation at 1000 × g, serum was removed and stored at −80°C with Halt® protease inhibitor cocktail (Thermo Scientific®, MA, USA) for further analysis. Following collection of all study samples, serum concentrations of interleukin IL-6 (Marker of chronic inflammation, acute exercise stress, acute metabolic signaling), IL-10 (Marker of acute anti-inflammation), and tumor necrosis factor alpha (TNF-α, marker of chronic and acute inflammation) were quantified using established ELISA analysis techniques (59) via Quantikine high-sensitivity human immunoassay kits (R&D systems®, MN, USA) used according to the manufacturer’s protocol. All samples were analyzed in triplicate and randomized by plate by an experienced technician. Serum concentration values were normalized to internal standards provided in each kit by the manufacturer. Coefficients of variation for triplicate measures were as follows: IL-6 (9.2 ± 1.4%); IL-10 (8.6 ± 1.9%); TNF-α (8.9 ± 2.0%).
Statistical analysis was performed using SPSS® Statistics (Version 20, IBM Inc., Armonk NY). A 2(temperature) by 2(time) mixed-model ANOVA was used to detect differences between conditions (HY, RTY) for blood pressure, ROM and serum cytokine changes. Significant interactions detected by Type III tests of fixed effects were followed by a Bonferroni post hoc test for pairwise comparisons. A two-tailed paired samples t-test was used to compare metabolic measures recorded during exercise. Type I error was set at α = 0.05 for all comparisons. For all significant pairwise comparisons between conditions, a Cohen’s d statistic ([Mean1 – Mean2]/Pooled SD) for effect size was calculated whereby values were interpreted as follows: < 0.1, negligible (N); 0.1–0.3, small (S); 0.3–0.5, moderate (M); 0.5–0.7, large (L); > 0.7, very large (VL) (54).
RESULTS
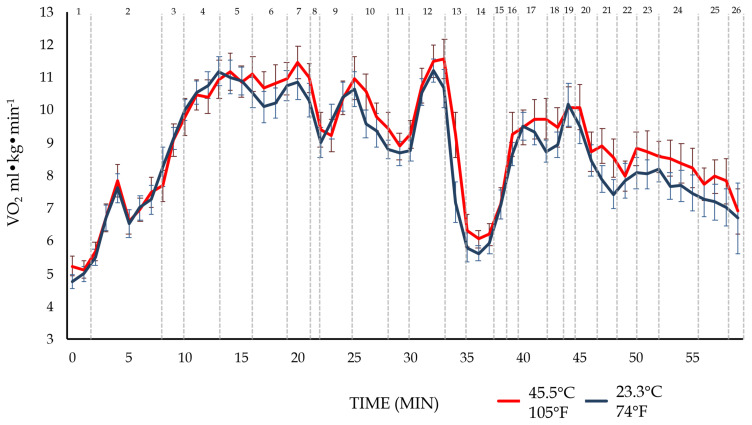
All exercise sessions were well tolerated by the participants. No differences were detected between conditions (HY or RTY) with regards to heart rate or gas exchange measures taken during the 5-minute pre-exercise collection period [Heart Rate, bpm (RTY: 84 ± 5|HY: 85 ± 5); VO2 ml·kg·min−1 (RTY: 4.8 ± 0.8|HY: 4.9 ± 1.6); RER (RTY: 0.83 ± 0.09|HY: 0.81 ± 0.08)]. An overview of oxygen consumption measured through the duration of the session is shown in Figure 2.
Figure 2.
Mean ± SEM time-course of oxygen consumption (VO2 ml·kg·min−1) during yoga exercise in heated (HY − 40.5°C / 105°F) and thermoneutral (RTY − 23.3°C / 74°F) conditions across all poses performed. Corresponding poses for each number listed across the top axis are shown in Figure 1.
Mean VO2, peak VO2, %VO2max, kcal expenditure, heart rate, and respiratory rate did not differ between conditions (Table 1, to follow). RER was observed to be reduced during the HY session compared to the RTY session (−0.06, p < 0.05). As a result, significant reductions in carbohydrate oxidation and an increase in fat oxidation was observed during HY compared to RTY (p < 0.05). Lastly, no significant changes were observed for pre-to-post session measures of blood pressure for either the HY or RTY sessions (Mean Arterial Pressure; RTY: Pre-85 ± 6, Post-85 ± 8 | HY: Pre-85 ± 6, Post-85 ± 7).
Table 1.
Mean cardio-metabolic responses to 1-hour of RTY and HY exercise.
| Independent Variable | RTY (74°F/23.3°C) | HY (105°F/41.5°C) | Effect Size d |
|---|---|---|---|
| VO2 (mean; ml·kg·min−1) | 8.6 ± 0.2 | 8.9 ± 0.3 | |
| Peak VO2 (ml·kg·min−1) | 14.5 ± 0.4 | 14.9 ± 0.5 | |
| %VO2max (mean) | 23.5% ± 1.3 | 25.3% ± 2.1 | |
| RER (mean; VCO2/VO2) | 0.95 ± 0.02 | 0.89 ± 0.02 # | 0.8 (VL) |
| Total Caloric Exp. (Kcal) | 151 ± 4 | 156 ± 7 | |
| CHO-OxR (mean; g·min−1) | 0.51 ± 0.04 | 0.44 ± 0.03 # | 0.6 (L) |
| Fat-OxR (mean; g·min−1) | 0.05 ± 0.01 | 0.09 ± 0.01 # | 0.9 (VL) |
| Heart Rate (mean; bpm) | 109 ± 8 | 113 ± 8 | |
| Respiratory Rate (mean; brpm) | 21 ± 4 | 21 ± 5 |
Note. Data are presented as means ± SEM for measures recorded continuously during the exercise bout.
Abbreviations: Oxygen consumption VO2; Peak oxygen consumption achieved during each bout; Respiratory Exchange Ratio –RER; Total Caloric Expenditure –Total Caloric Exp.; Carbohydrate Oxidation Rate –CHO-OxR; Fat Oxidation Rate –Fat-OxR; Heart Rate –beats per minute, Respiratory Rate –breaths per minute.
significant difference between conditions for gas exchange measures (p < 0.05).
Effect sizes interpreted as follows: 0–0.1 (Negligible, N); 0.1–0.3 (Small, S); 0.3–0.5 (Moderate, M); 0.5–0.7 (Large, L); > 0.7 (Very Large, VL).
Pre- and post-exercise Range of Motion measurements are shown in Table 2. Both conditions elicited similar acute increases in upper body ROM measures of which were primarily observed in the shoulder (p < 0.05). A small increase (1.7 ± 0.7°) in elbow extension was observed following the HY (p < 0.05) but not the RTY condition (Table 2).
Table 2.
ROM (Degrees) before and after 1-hour of RTY and HY exercise.
| ROM Measure | RTY (74°F/23.3°C) | HY (105°F/41.5°C) | ||||
|---|---|---|---|---|---|---|
| Pre | Post | Δ | Pre | Post | Δ | |
| Elbow | ||||||
| Flexion | 150.9 ± 1.0 | 150.6 ± 0.8 | −0.3 ± 0.6 | 151.2 ± 1.2 | 150.9 ± 1.1 | −0.3 ± 0.6 |
| Extension | 181.8 ± 1.7 | 183.4 ± 1.5 | 1.6 ± 0.9 | 181.8 ± 1.7 | 183.5 ± 0.7* | 1.7 ± 0.7 |
| Shoulder | ||||||
| ER 0° | 64.8 ± 2.7 | 68.5 ± 2.9* | 3.7 ± 1.1 | 63.3 ± 2.3 | 67.0 ± 3.1* | 3.7 ± 2.0 |
| IR Neutral | 48.8 ± 1.3 | 52.0 ± 2.0* | 3.3 ± 1.4 | 50.3 ± 2.3 | 54.5 ± 2.6* | 4.2 ± 1.4 |
| ER Neutral | 109.9 ± 1.9 | 113.0 ± 2.2* | 3.1 ± 1.1 | 110.0 ± 2.4 | 113.1 ± 2.9* | 3.1 ± 1.1 |
| Scaption | 148.3 ± 1.8 | 153.2 ± 1.6* | 4.9 ± 1.1 | 147.3 ± 2.4 | 150.9 ± 2.5* | 3.6 ± 1.1 |
| Flexion | 173.2 ± 1.7 | 176.0 ± 2.1* | 2.8 ± 1.1 | 175.8 ± 2.7 | 178.6 ± 2.9* | 2.8 ± 1.2 |
| Knee | ||||||
| Flexion | 18.3 ± 1.7 | 17.1 ± 1.3 | −1.1 ± 0.7 | 19.1 ± 1.7 | 18.2 ± 1.9 | −1.0 ± 0.8 |
| Extension | 181.8 ± 1.1 | 180.7 ± 1.0 | −1.0 ± 0.9 | 180.9 ± 0.7 | 180.9 ± 0.7 | −0.0 ± 0.5 |
| Hip | ||||||
| Flexion | 153.4 ± 1.3 | 156.06 ± 1.5* | 2.6 ± 0.7 | 152.4 ± 1.3 | 156.7 ± 1.3* | 4.2 ± 0.7(p=0.07) |
| IR | 32.6 ± 2.4 | 33.6 ± 2.5 | 1.0 ± 0.6 | 29.9 ± 2.4 | 30.7 ± 2.3 | 0.8 ± 1.1 |
| ER | 56.9 ± 1.9 | 58.6 ± 1.8 | 1.7 ± 0.8 | 56.9 ± 2.7 | 57.9 ± 2.3 | 1.0 ± 1.7 |
| Abduction | 79.8 ± 2.7 | 82.1 ± 2.3* | 2.3 ± 1.3 | 79.8 ± 3.4 | 86.5 ± 4.0* | 6.6 ± 1.5# |
Note. Data are presented as means ± SEM for ROM measures (degrees).
significant change from pre- to postexercise measures within condition.
significant difference between conditions for change(Δ) in ROM. (α = 0.05).
For hip ROM, both the HY and RTY conditions yielded increases in ROM for hip flexion and abduction (p < 0.05) with no change detected in internal or external rotation. Additionally, HY elicited a significantly greater increase in hip abduction (p < 0.05; Effect Size d = 0.8, VL) and trended (p = 0.07) towards a greater increase in ROM for hip flexion.
Data for serum cytokine responses to acute exercise are presented in Table 3. No post-exercise changes in serum TNF-α or IL-10 were observed under either condition. Serum IL-6 was significantly increased (15.5 ± 8.0-fold) following HY only compared to the RTY group where no changes were observed (p < 0.05; Effect Size d = 0.6, L).
Table 3.
Serum Cytokine Responses to Acute Exercise.
| Cytokines (pg/dL) | RTY (74°F/23.3°C) | HY (105°F/41.5°C) | ||||
|---|---|---|---|---|---|---|
| Pre | Post | Fold Δ | Pre | Post | Fold Δ | |
| IL-6 | 0.7 ± 0.3 | 0.9 ± 0.3 | 1.9 ± 1.0 | 0.9 ± 0.3 | 2.9 ± 0.8* | 15.5 ± 8.0# |
| IL-10 | 0.3 ± 0.1 | 0.3 ± 0.1 | < 0.1 | 0.3 ± 0.1 | 0.3 ± 0.1 | < 0.1 |
| TNF-α | 0.9 ± 0.1 | 0.9 ± 0.1 | < 0.1 | 08 ± 0.1 | 0.9 ± 0.1 | < 0.1 |
Note. Data are presented as means ± SEM as well as fold change (fold Δ) for serum cytokine concentration measures of interleukin 6&10 (IL-6, IL-10) as well as tumor necrosis factor alpha (TNF-α).
significant change from pre- to post-exercise measures within condition.
significant difference between conditions for fold change (fold Δ). (α = 0.05).
DISCUSSION
In the present investigation, we sought to compare the acute physiologic effects HY and RTY to with regards to aerobic intensity, caloric expenditure, resting hemodynamics, ROM, and biomarkers related to exercise stress and inflammation. In line with our hypothesis, performing the yoga session in a heated environment (HY) commonly used in hot yoga practice (105°F / 41.5°C) did not significantly increase the aerobic requirements or energy cost of exercise compared to performing the session at room temperature (RTY). Per our findings presented in Table 1, neither condition achieved VO2 or caloric consumption thresholds for improving aerobic fitness (26, 56) or producing chronic improvements in body composition (19). Notably however, our present results do suggest an increase in fat metabolism indicated by our measurements of gas exchange (Table 1) and acute alterations in IL-6 (Table 3). Somewhat contrary to our hypothesis, HY was observed to promote greater increases in ROM for only one of thirteen measures (Hip abduction, Table 2). In addition to previously reported physiologic and psychological benefits associated with yoga in general, these findings may be used to aid fitness practitioners to determine the best application for incorporating the practice of yoga into a well-rounded exercise program depending on individual health and fitness goals.
Overall, no statistical difference was observed between HY and RTY in terms of oxygen consumption or caloric expenditure (Table 1). This differs from other exercise modalities performed at higher intensities (greater %VO2max) in the heat where processes of thermoregulation (shunting of blood to the skin, increased sweat rate, and reduced plasma volume) require an increased energy cost to maintain core temperature while simultaneously providing working musculature with oxygen and nutrient delivery (11). While specific thermoregulatory processes were not the primary focus on this investigation, we find it likely that the low intensity nature of the particular yoga session used (< 30% VO2max) was insufficient to drive a thermoregulatory response to a degree that significantly influenced caloric expenditure under the heated conditions. However, acknowledging the limitations of the present study in regards to thermoregulatory measures, it is possible that under the heated conditions, participants modified their approach to performing the session to accommodate the heat stimulus as has been shown with other forms of exercise (23, 49, 55). In the present study, this may be indicated as participants operated at a reduced RER during exercise in the HY session compared to the RTY session. However, no other indications of physical pacing were observed as we did not observe any differences between sessions with regards to heart rate, respiratory rate, or pre-to-post exercise blood pressure measures (Table 1). Therefore, we presently conclude that the intensity of the exercise, involving primarily static yoga poses, was not sufficient to result in an elevated caloric expenditure in the heated environment. These results are in agreement with Boyde et al. 2018 (5) who observed similar results during a 20-minute HY bout and are in partial agreement with O’Hearn et al. 2016 (43) who determined that increased ambient temperature alone is not sufficient to increase energy expenditure at rest. While participants were not at rest during this investigation, the mean aerobic workload during the session was ~8.9 mlO2·kg·min−1(~2.5 METS) during the HY session which corresponds to light physical activity comparable to a slow walk (40).
Regarding the topics of exercise intensity and caloric expenditure as they pertain to health and fitness, the American College of Sports Medicine recommends that to improve aerobic fitness adults should exercise at an intensity of greater than 40–50% of VO2max for a period of at least 30 minutes per session and that those seeking to improve body composition or lose weight should seek to expend 300–400 kcals per bout (19). Durstine et al., 2002 (20) also recommended a minimum threshold of 1200–2200 kcals of exercise per week to induce favorable blood lipid changes. In the present investigation, participants expended an average of 151 ± 4 kcals during the RTY session and 156 ± 7 kcals during the HY session (Table 1). By comparison, performing steady state aerobic exercise at 50% VO2max (considered low-moderate intensity) in our present participant population would have yielded an expenditure of roughly 317 ± 19 kcals (~double) across the same timeline. Therefore, for those seeking improvements in aerobic fitness or weight reduction, a standardized hot yoga session, as performed in the present study, may not meet appropriate exercise intensity or volume thresholds as a stand-alone mode of exercise (even under heated conditions) compared to other modes of exercise performed across the same time span despite the modest changes in substrate utilization observed here indicated by RER differences between HY and RTY (Table 1).
Importantly, while there are some limitations to yoga, this type of exercise may benefit those seeking low-impact, low-intensity exercise options. Specifically, Yoga (RTY or HY) may serve as a way for recently sedentary individuals to transition to more intense exercise modalities (38) while simultaneously improving aspects of stability, mobility, and strength. For those who are highly trained, yoga has also been shown to provide an avenue of active recovery from more strenuous modalities of physical training (6, 52). It is also important to note that there are several modes of yoga that vary with regards to exercise intensity as well as overall physical and psychological focus (12). Therefore, it is of primary importance that individuals determine the degree to which a particular form of yoga fits their physical activity needs to achieve individual health, fitness, or performance goals within the framework of a well-rounded exercise or training program.
A commonly promoted aspect of performing yoga under heated conditions is that it increases achievable ROM and thus, promotes greater chronic increases in flexibility and mobility (57). The results of our investigation minimally support this claim, as a greater acute increase of hip abduction was observed (Table 2). These findings, to our knowledge, are the first to evaluate multi-joint ROM measures across all of the major joints before and after acute HY compared to RTY. Importantly, the magnitude of this finding should be viewed with caution as HY was only observed to elicit greater acute ROM changes compared to RTY in one of thirteen measures. Therefore, the clinical impact of these acute responses in a population of experienced practitioners may be limited. However, we acknowledge that for more novice practitioners, greater acute effects on ROM may have been observed. Presently, the appropriate dose-response relationship to elicit favorable changes in flexibility from the chronic practice of yoga or HY is not well established. We also caution the reader that the consideration of yoga as a low-impact activity may overshadow the potential risk of overtraining flexibility which has been previously linked to joint instability, hypermobility, and overuse injuries (1, 15). Bekhradi et al. 2018 (2) reported an injury prevalence of 1.18 injuries per 1000 yoga practice hours and that while the overall injury rates during yoga practice (7%) was low, injuries were primarily in the lower extremities. Therefore, in terms of flexibility, risk-to-benefit and dose-response investigations of HY and RTY remain needed. Based on the present findings, we conclude that for experienced / advanced practitioners who may have already achieved heightened levels of flexibility, the addition of a heated environment may only provide a minimal effect for acutely achieving greater ROM.
In the present study, we sought to determine the effects of both HY and RTY on common biomarkers associated with acute inflammation, muscle damage, and exercise stress (TNF-α & IL-6) as well as anti-inflammation commonly associated with exercise (IL-10) (45). Expectedly, neither the HY or RTY conditions yielded an immediate post-exercise change in TNF-α (Table 2) typically associated with higher intensities of muscle damaging exercise such as heavy resistance training (9, 45). Additionally, all study participants were experienced yoga practitioners who were accustomed to the types of exercise performed. Regarding the anti-inflammatory responses of IL-10, the lack of effect may be most reflective of neither session meeting an appropriate exercise stress threshold to elicit a response. Only the HY session was observed to produce a significant increase in IL-6 concentration (Table 2). IL-6 is often associated with chronic systemic and/or cardiovascular inflammation associated with conditions such as metabolic instability, diabetes, and obesity (24). However, during acute exercise, IL-6 also plays an important metabolic signaling role whereby its release from skeletal muscle contributes to an increase in lipolysis in the liver and adipose tissue (60). Notably, the changes in IL-6 observed here were mirrored by reduced RER and carbohydrate oxidation measures along with an increase in fat oxidation compared to RTY (Table 2). Such increases in IL-6 in response to heat stress have also been observed with other forms of exercise (63). Therefore, although the addition of a heated environment may not have significantly contributed to an increase in caloric expenditure, it may contribute to favorable metabolic adaptations over time. For example, acute pharmacologic or exercise induced increases in IL-6 have been observed to improve insulin sensitivity (46). Relating to the present investigation, Hunter et al. 2013 (29) observed improved glucose tolerance following an 8-week (3 days/week) Bikram yoga program in older obese adults. Such effects may be of particular benefit for previously sedentary individuals entering in to an exercise program. Although often considered to be a marker of chronic systemic inflammation, IL-6 has also been shown to play an acute anti-inflammatory role through inhibition of signaling, production, and release of inflammatory cytokines such as TNF-α, IL-1 when released form skeletal muscle during exercise (32, 46). This is mechanistically thought to assist in the differentiation between trauma and activity based immune system responses that also assist in chronic adaptation to exercise (43, 44). Of note, chronic practice of yoga (in general) has been previously associated with reductions in risk for cardiovascular disease, hypertension, and chronic inflammation (53). Therefore, future studies are required to confirm whether or not the chronic practice of HY (compared to RTY) contributes to greater improvements in metabolic function and to identify which populations may stand to gain the most benefit.
This investigation is not without limitations. First, the participants were largely experienced yoga practitioners and were mostly women. Further research will be needed determine the effects of HY compared to RTY across novice, clinical, and athletic populations. Next, the biomarkers examined (IL-6, IL-10, TNF-α) were only measured immediately before and 30-minutes following exercise due to logistical and budgetary restrictions. While a substantial amount of evidence exists demonstrating a time course of cytokine release with significant elevations observed within the first hour post-exercise, we do not discount that continued immune adjustments to exercise can persist for a much greater period of time >24h following exercise (45). There are also several pro-inflammatory and anti-inflammatory markers that were not assessed in this investigation. Cumulatively, the immune response to exercise is complex with a great deal of intramuscular and systemic signaling cross talk. Future investigations will be required to more fully investigate specific immune responses to RTY compared to HY. Despite these limitations, our finding that HY induced increases in IL-6 with paralleled alterations in substrate utilization remains intriguing. However, because of inherent limitations/assumptions using indirect calorimetry, additional studies may benefit from the utilization of doubly labeled water methodologies for more precise measurements of fuel substrate utilization during exercise (16). Within this investigation, we acknowledge the potential impact on pre-exercise nutrition with regards to substrate oxidation as well as other metabolic responses to acute exercise (64). For an applied approach, we had participants perform a 4h fast prior to exercise as opposed to a 10–12h fast often reported in the literature (4, 64) to more closely mimic the conditions that the participants in our study regularly exercise under. Additionally, similar metabolic focused studies involving acute exercise in heated and thermoneutral conditions have used similar standardized fasting timelines to those used in the present study (34–36). In this instance, subjects matched their initial dietary recall. Time of day for each session was also controlled. Therefore, while nutritional intake between participants was not standardized and remains a limitation, within-participant standardizing for comparison of caloric expenditure and substrate utilization was performed. However, we do acknowledge the limitations of dietary self-reporting. Finally, we only utilized a 5-minute pre-exercise collection period of heart rate and metabolic gas exchange with participants in a standing position prior to beginning exercise. Future investigations, depending on the independent variables of interest, may consider performing a rested state RMR prior to exercise to better confirm that resting metabolic conditions are the same prior to exercise trials.
While not the primary focus of this investigation, we acknowledge the potential interest in thermoregulatory processes in any investigation involving exercise performed at differing ambient temperatures. In the present study, none of our participants reported any symptoms of heat injury (confusion, dizziness, fainting, headache, cramping, nausea) (30), although these symptoms have been reported in the past with this type of yoga practice (37). Porcari et al. 2015 (47) also observed an increase in core body temperature of ~2–3°F under the same conditions (105°F, 40% humidity) used here. However, Camic et al. 2014 (10) observed that exercise induced increases in core temperature were similar between RTY and HY conditions. Regardless, for the experienced practitioners participating in the present study, we find it likely they may have already been acclimated to the HY study conditions. Whether or not changes in core temperature may have elicited the metabolic responses observed here with regards to substrate utilization remains a topic of further investigation. In general, for reasonably fit individuals with no known contraindications to exercise or thermoregulatory impairments we (and others, 12) suggest that hot yoga is likely safe as long as proper precautions such as adequate hydration and symptom monitoring are taken. However, as with other forms of exercise performed in the heat, a period of staged heat acclimation is warranted particularly for previously sedentary, overweight, or older individuals interested in performing this type of yoga (14).
Performing a one-hour session of yoga following a standardized Bikram sequence in a heated environment does not sufficiently increase aerobic intensity or caloric cost, nor does it achieve ACSM recommended aerobic or caloric thresholds for chronically improving VO2max or contributing to appreciable weight loss as a stand-alone mode of exercise. However, the addition of a heated environment may increase fat oxidization and contribute to favorable metabolic changes over time. Such responses may be of particular interest to obese or sedentary populations interested in beginning a well-rounded exercise program. In individuals who are already experienced in yoga practice, HY may result in greater acute increases in some aspects of ROM, although the effects appear to be limited. The degree to which this may be favorable in terms of general fitness is unknown. Lastly, further research is needed to determine the appropriate dose-response relationship of yoga to allow practitioners, therapists, and clinicians to make more educated decisions with regards to how it may best be incorporated into a comprehensive fitness program with specific training or therapeutic goals in mind.
ACKNOWLEDGEMENTS
The authors would sincerely like to thank Thomas Yetter, Tyler Heimdal, Brenda Hartman and the Houston Methodist Research Institute for facility and research staff support during this investigation.
REFERENCES
- 1.Beighton P, Grahame R, Bird H. Hypermobility of joints. Springer; 2012. Hypermobility in the performing arts and sport; pp. 125–149. [Google Scholar]
- 2.Bekhradi A, Wong D, Gerrie BJ, et al. Although the injury rate of yoga is low, nearly two-thirds of musculoskeletal injuries in yoga affect the lower extremity: a systematic review. J ISAKOS. 2018;3(4):229–234. [Google Scholar]
- 3.Blonna D, Zarkadas PC, Fitzsimmons JS, O’Driscoll SW. Validation of a photography-based goniometry method for measuring joint range of motion. J Shoulder Elbow Surg. 2012;21(1):29–35. doi: 10.1016/j.jse.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 4.Borack MS, Reidy PT, Husaini SH, et al. Soy-dairy protein blend or whey protein isolate ingestion induces similar postexercise muscle mechanistic target of rapamycin complex 1 signaling and protein synthesis responses in older men. J Nutri. 2016;146(12):2468–2475. doi: 10.3945/jn.116.231159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boyd CN, Lannan SM, Zuhl MN, Mora-Rodriguez R, Nelson RK. Objective and subjective measures of exercise intensity during thermo-neutral and hot yoga. Appl Physiol Nutr Metab. 2017;43(4):397–402. doi: 10.1139/apnm-2017-0495. [DOI] [PubMed] [Google Scholar]
- 6.Boyle CA, Sayers SP, Jensen BE, Headley SA, Manos TM. The effects of yoga training and a single bout of yoga on delayed onset muscle soreness in the lower extremity. J Strength Cond Res. 2004;18(4):723–729. doi: 10.1519/14723.1. [DOI] [PubMed] [Google Scholar]
- 7.Bruce RA, Kusumi F, Hosmer D. Maximal oxygen intake and nomographic assessment of functional aerobic impairment in cardiovascular disease. Am Heart J. 1973;85(4):546–562. doi: 10.1016/0002-8703(73)90502-4. [DOI] [PubMed] [Google Scholar]
- 8.Burke LM. Nutritional needs for exercise in the heat. Comp Biochem Physiol A Mol Integr Physiol. 2001;128(4):735–748. doi: 10.1016/s1095-6433(01)00279-3. [DOI] [PubMed] [Google Scholar]
- 9.Calle MC, Fernandez ML. Effects of resistance training on the inflammatory response. Nutr Res Pract. 2010;4(4):259–269. doi: 10.4162/nrp.2010.4.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Camic CL. Heart Rate and Core Temperature Responses During Basic Yoga Compared with those During Hot Yoga. Gundersen. 2014;113 [Google Scholar]
- 11.Casa DJ. Exercise in the heat. I. Fundamentals of thermal physiology, performance implications, and dehydration. J Athl Train. 1999;34(3):246. [PMC free article] [PubMed] [Google Scholar]
- 12.Cramer H, Ostermann T, Dobos G. Injuries and other adverse events associated with yoga practice: A systematic review of epidemiological studies. J Sci Med Sport. 2018;21(2):147–154. doi: 10.1016/j.jsams.2017.08.026. [DOI] [PubMed] [Google Scholar]
- 13.Cramer MN, Jay O. Biophysical aspects of human thermoregulation during heat stress. Auton Neurosci. 2016;196:3–13. doi: 10.1016/j.autneu.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 14.Daanen HAM, Racinais S, Périard JD. Heat acclimation decay and re-induction: a systematic review and meta-analysis. Sports Med. 2018;48(2):409–430. doi: 10.1007/s40279-017-0808-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dacci P, Amadio S, Gerevini S, et al. Practice of yoga may cause damage of both sciatic nerves: a case report. Neurol Sci. 2013;34(3):393–396. doi: 10.1007/s10072-012-0998-9. [DOI] [PubMed] [Google Scholar]
- 16.de Jonge L, DeLany JP, Nguyen T, et al. Validation study of energy expenditure and intake during calorie restriction using doubly labeled water and changes in body composition. Am J Clin Nutr. 2007;85(1):73–79. doi: 10.1093/ajcn/85.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Del Coso J, Hamouti N, Ortega JF, Mora-Rodriguez R. Aerobic fitness determines whole-body fat oxidation rate during exercise in the heat. Appl Physiol Nutr Metab. 2010;35(6):741–748. doi: 10.1139/H10-068. [DOI] [PubMed] [Google Scholar]
- 18.Djalilova DM, Schulz PS, Berger AM, Case AJ, Kupzyk KA, Ross AC. Impact of Yoga on Inflammatory Biomarkers: A Systematic Review. Biol Res Nurs. 2019;21(2):198–209. doi: 10.1177/1099800418820162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–471. doi: 10.1249/MSS.0b013e3181949333. [DOI] [PubMed] [Google Scholar]
- 20.Durstine JL, Grandjean PW, Cox CA, Thompson PD. Lipids, lipoproteins, and exercise. J Cardiopulm Rehab Prev. 2002;22(6):385–398. doi: 10.1097/00008483-200211000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Febbraio MA, Snow RJ, Hargreaves M, Stathis CG, Martin IK, Carey MF. Muscle metabolism during exercise and heat stress in trained men: effect of acclimation. J Appl Physiol. 1994;76(2):589–597. doi: 10.1152/jappl.1994.76.2.589. [DOI] [PubMed] [Google Scholar]
- 22.Field T. Yoga clinical research review. Complement Ther Clin Pract. 2011;17(1):1–8. doi: 10.1016/j.ctcp.2010.09.007. [DOI] [PubMed] [Google Scholar]
- 23.Flouris AD, Schlader ZJ. Human behavioral thermoregulation during exercise in the heat. Scan J Med Sci Sports. 2015;25:52–64. doi: 10.1111/sms.12349. [DOI] [PubMed] [Google Scholar]
- 24.Gabay C. Interleukin-6 and chronic inflammation. Arthritis Res Ther. 2006;8(2):S3. doi: 10.1186/ar1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Galloway S, Maughan RJ. Effects of ambient temperature on the capacity to perform prolonged cycle exercise in man. Med Sci Sports Exerc. 1997;29(9):1240–1249. doi: 10.1097/00005768-199709000-00018. [DOI] [PubMed] [Google Scholar]
- 26.Gormley SE, Swain DP, High R, et al. Effect of intensity of aerobic training on V̇O2max. Med Sci Sports Exerc. 2008;40(7):1336–1343. doi: 10.1249/MSS.0b013e31816c4839. [DOI] [PubMed] [Google Scholar]
- 27.Greene NP, Lambert BS, Greene ES, Carbuhn AF, Green JS, Crouse SF. Comparative efficacy of water and land treadmill training for overweight or obese adults. Med Sci Sports Exerc. 2009;41(9):1808–1815. doi: 10.1249/MSS.0b013e3181a23f7f. [DOI] [PubMed] [Google Scholar]
- 28.Hewett ZL, Cheema BS, Pumpa KL, Smith CA. The effects of Bikram yoga on health: critical review and clinical trial recommendations. Evid Based Complement Alternat Med Epub. 2015;2015 doi: 10.1155/2015/428427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hunter SD, Dhindsa M, Cunningham E, Tarumi T, Alkatan M, Tanaka H. Improvements in glucose tolerance with Bikram yoga in older obese adults: A pilot study. J Bodywork Movement Ther. 2013;17(4):404–407. doi: 10.1016/j.jbmt.2013.01.002. [DOI] [PubMed] [Google Scholar]
- 30.Jardine DS. Heat illness and heat stroke. Pediatr Rev. 2007;28(7):249. doi: 10.1542/pir.28-7-249. [DOI] [PubMed] [Google Scholar]
- 31.Jeukendrup AE, Wallis GA. Measurement of substrate oxidation during exercise by means of gas exchange measurements. Int J Sports Med. 2005;26(Suppl 1):S28–37. doi: 10.1055/s-2004-830512. [DOI] [PubMed] [Google Scholar]
- 32.Kiecolt-Glaser JK, Christian L, Preston H, et al. Stress, inflammation, and yoga practice. Psychosom Med. 2010;72(2):113. doi: 10.1097/PSY.0b013e3181cb9377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lambert BS, Greene NP, Carradine AT, et al. Aquatic treadmill training reduces blood pressure reactivity to physical stress. Med Sci Sports Exerc. 2014;46(4):809–816. doi: 10.1249/MSS.0000000000000167. [DOI] [PubMed] [Google Scholar]
- 34.Lambert BS, Shimkus KL, Fluckey JD, et al. Anabolic responses to acute and chronic resistance exercise are enhanced when combined with aquatic treadmill exercise. Am J Physiol Endo Metab. 2014;308(3):E192–E200. doi: 10.1152/ajpendo.00689.2013. [DOI] [PubMed] [Google Scholar]
- 35.Leites GT, Cunha GS, Chu L, Meyer F, Timmons BW. Energy substrate utilization with and without exogenous carbohydrate intake in boys and men exercising in the heat. J Appl Physiol. 2016;121(5):1127–1134. doi: 10.1152/japplphysiol.00535.2016. [DOI] [PubMed] [Google Scholar]
- 36.Lytle JR, Kravits DM, Martin SE, Green JS, Crouse SF, Lambert BS. Predicting Energy Expenditure of an Acute Resistance Exercise Bout in Men and Women. Med Sci Sports Exerc. 2019;51(7):1532–1537. doi: 10.1249/MSS.0000000000001925. [DOI] [PubMed] [Google Scholar]
- 37.Mace C, Eggleston B. Self-reported benefits and adverse outcomes of hot yoga participation. Int J Yoga Ther. 2016;26(1):49–53. doi: 10.17761/1531-2054-26.1.49. [DOI] [PubMed] [Google Scholar]
- 38.Moonaz SH, Bingham CO, Wissow L, Bartlett SJ. Yoga in sedentary adults with arthritis: effects of a randomized controlled pragmatic trial. J Rheumatol. 2015;42(7):1194–1202. doi: 10.3899/jrheum.141129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nakano J, Yamabayashi C, Scott A, Reid WD. The effect of heat applied with stretch to increase range of motion: a systematic review. Phys Ther Sport. 2012;13(3):180–188. doi: 10.1016/j.ptsp.2011.11.003. [DOI] [PubMed] [Google Scholar]
- 40.Nam GB. Exercise, heart and health. Korean Circ J. 2011;41(3):113–121. doi: 10.4070/kcj.2011.41.3.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Navalta JW, Stone WJ, Lyons TS. Ethical Issues Relating to Scientific Discovery in Exercise Science. Int J Exerc Sci. 2019;12(1):1–8. doi: 10.70252/EYCD6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Nielsen B, Savard G, Richter E, Hargreaves M, Saltin B. Muscle blood flow and muscle metabolism during exercise and heat stress. J Appl Physiol. 1990;69(3):1040–1046. doi: 10.1152/jappl.1990.69.3.1040. [DOI] [PubMed] [Google Scholar]
- 43.O’Hearn K, Tingelstad HC, Blondin D, Tang V, Filion LG, Haman F. Heat exposure increases circulating fatty acids but not lipid oxidation at rest and during exercise. J Therm Biol. 2016;55:39–46. doi: 10.1016/j.jtherbio.2015.11.002. [DOI] [PubMed] [Google Scholar]
- 44.Pate JL, Buono MJ. The physiological responses to Bikram yoga in novice and experienced practitioners. Altern Ther Health Med. 2014;20(4):12–18. [PubMed] [Google Scholar]
- 45.Pedersen BK, Akerstrom TC, Nielsen AR, Fischer CP. Role of myokines in exercise and metabolism. J Appl Physiol. 2007;103(3):1093–1098. doi: 10.1152/japplphysiol.00080.2007. [DOI] [PubMed] [Google Scholar]
- 46.Petersen A, Pedersen B. The role of IL-6 in mediating the anti inflammatory. J Physiol Pharmacol. 2006;57(Suppl 10):43–51. [PubMed] [Google Scholar]
- 47.Porcari JP, Steffen J. Heart rate and core temperature responses to Bikram yoga. Gundersen. 2015;8:3. [Google Scholar]
- 48.Rajbhoj PH, Shete SU, Verma A, Bhogal RS. Effect of yoga module on pro-inflammatory and anti-inflammatory cytokines in industrial workers of lonavla: a randomized controlled trial. J Clin Diagn Res. 2015;9(2):CC01. doi: 10.7860/JCDR/2015/11426.5551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ravanelli NM, Cramer MN, Molgat-Seon Y, Carlsen AN, Jay O. Do greater rates of body heat storage precede the accelerated reduction of self-paced exercise intensity in the heat? Euro J Appl Physiol. 2014;114(11):2399–2410. doi: 10.1007/s00421-014-2958-y. [DOI] [PubMed] [Google Scholar]
- 50.Robertson VJ, Ward AR, Jung P. The effect of heat on tissue extensibility: a comparison of deep and superficial heating. Arch Phys Med Rehabil. 2005;86(4):819–825. doi: 10.1016/j.apmr.2004.07.353. [DOI] [PubMed] [Google Scholar]
- 51.Ross A, Thomas S. The health benefits of yoga and exercise: a review of comparison studies. J Altern Complement Med. 2010;16(1):3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- 52.Ryba TV. The benefits of yoga for athletes: The body. Athl Ther Today. 2006;11(2):32–34. [Google Scholar]
- 53.Sawilowsky SS. New effect size rules of thumb. J Mod Appl Stat Methods. 2009;8(2):26. [Google Scholar]
- 54.Schlader ZJ, Stannard SR, Mündel T. Evidence for thermoregulatory behavior during self-paced exercise in the heat. J Therm Biol. 2011;36(7):390–396. [Google Scholar]
- 55.Swain DP, Franklin BA. VO2 reserve and the minimal intensity for improving cardiorespiratory fitness. Med Sci Sports Exerc. 2002;34(1) doi: 10.1097/00005768-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 56.Tracy BL, Hart CE. Bikram yoga training and physical fitness in healthy young adults. J Strength Cond Res. 2013;27(3):822–830. doi: 10.1519/JSC.0b013e31825c340f. [DOI] [PubMed] [Google Scholar]
- 57.Tran MD, Holly RG, Lashbrook J, Amsterdam EA. Effects of Hatha yoga practice on the health-related aspects of physical fitness. Prev Cardiol. 2001;4(4):165–170. doi: 10.1111/j.1520-037x.2001.00542.x. [DOI] [PubMed] [Google Scholar]
- 58.Turner-McGrievy GM, Wirth MD, Shivappa N, et al. Impact of a 12-month Inflammation Management Intervention on the Dietary Inflammatory Index, inflammation, and lipids. Clin Nutr. 2019;30:42–51. doi: 10.1016/j.clnesp.2019.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van Hall G, Steensberg A, Sacchetti M, et al. Interleukin-6 stimulates lipolysis and fat oxidation in humans. J Clin Endo Metab. 2003;88(7):3005–3010. doi: 10.1210/jc.2002-021687. [DOI] [PubMed] [Google Scholar]
- 60.Vijayaraghava A, Doreswamy V, Narasipur OS, Kunnavil R, Srinivasamurthy N. Effect of yoga practice on levels of inflammatory markers after moderate and strenuous exercise. J Clin Diagn Res. 2015;9(6):CC08. doi: 10.7860/JCDR/2015/12851.6021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vinoski E, Webb JB, Warren-Findlow J, Brewer KA, Kiffmeyer KA. Got yoga?: A longitudinal analysis of thematic content and models’ appearance-related attributes in advertisements spanning four decades of Yoga Journal. Body image. 2017;21:1–5. doi: 10.1016/j.bodyim.2017.01.006. [DOI] [PubMed] [Google Scholar]
- 62.Welc SS, Judge AR, Clanton TL. Skeletal muscle interleukin-6 regulation in hyperthermia. Am J Physiol Cell Physiol. 2013;305(4):C406–C413. doi: 10.1152/ajpcell.00084.2013. [DOI] [PubMed] [Google Scholar]
- 64.Westerterp KR. Diet induced thermogenesis. Nutri Metab. 2004;1(1):5. doi: 10.1186/1743-7075-1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yaspelkis B, Scroop G, Wilmore K, Ivy J. Carbohydrate metabolism during exercise in hot and thermoneutral environments. Int J Sport Med. 1993;14(01):13–19. doi: 10.1055/s-2007-1021139. [DOI] [PubMed] [Google Scholar]