Abstract
There is limited research on self-paced walking and whether healthy individuals reach perceived exertion- (RPE) and/or heart rate- (HR) based moderate intensities. Study purpose was to determine if achieved RPE and HR intensities during a self-paced walk are of equivalent magnitude and whether they reach the recommended moderate-intensity. Thirty participants completed a 15-minute self-paced walk. RPE and HR were measured every two minutes; each measure was ranked by intensity. Wilcoxon matched pairs test revealed no significant difference between the mean ranked RPE and %HRmax (2.4 ± 0.9, 2.3 ± 1.0, respectively, p = 0.365). Only 37.5% of time-matched RPE and %HRmax were the same intensity. A slight positive Spearman’s rho correlation (rs = 0.201, p = 0.002) was found. One-sample t-tests showed that RPE and %HRmax did not reach moderate intensity (p < 0.001). Individuals did not achieve moderate intensities when self-paced walking with varied RPE- and HR-based measures.
Keywords: Rating of Perceived Exertion, moderate-intensity, American College of Sports Medicine
INTRODUCTION
Walking is an exercise that can be completed at different intensities to accommodate for an individual’s level of fitness and goal for walking. It falls under the category of aerobic training which was shown to be the type of exercise that is chosen most often by women (40%) following a combination of exercise (42%) (22). More specifically, walking is the form of physical activity that is most often chosen by persons in the United States (21). Self-paced walking is characterized by the individual’s freedom to regulate the intensity of the exercise session (14). This type of walking allows the individual to walk at their own pace for the duration of the workout. Some important findings on self-paced exercise are that outdoor walking improves the intention to engage in additional exercise bouts (6) and that self-paced cycling may improve the achieved maximal oxygen consumption (VO2max) (12). While participation in physical activity is increasing, the adherence levels are still very low at only 6–8% among adolescents and less than 5% among adults (24). Having higher levels of adherence could help the individual meet the physical activity guidelines for the average adult.
In addition to adhering to an exercise program to achieve health benefits, the intensity of the physical activity also plays a role. While it has been determined that any exercise is good exercise, based on the 2018 Physical Activity Guidelines (PAG), it was still stated that moderate intensity physical activity should be the goal. The public health target range suggested in the 2008 Scientific Report was 500 to 1,000 metabolic equivalent (MET)-minutes of moderate-to-vigorous physical activity (or 150 to 300 minutes per week of moderate-intensity physical activity) (25). The 2018 Committee concurs with this target range (26). Moderate intensity exercise as defined by the American College of Sports Medicine (ACSM) is exercise at 64–76% of maximal heart rate, a perceived exertion (RPE) of 12–13, and 46–63% of VO2max (17). With the goal of adult Americans regarding physical activity being to exercise at moderate-to-vigorous level of physical activity each week, it is important to determine if self-paced walking is being used adequately to reach these goals by walking at a pace of at least moderate intensity.
The Borg Scale can be used to estimate exercise intensity (4). RPE is seen as one of the most convenient techniques for monitoring one’s level of exertion and is based on the subjective judgement of the individual’s biological cues and psychological and environmental variables (16). With the Borg Scale being easily obtained, many medical and fitness professionals can use RPE for their prescriptions based on the ACSM’s guidelines.
Exercise intensity can also be determined objectively by measuring the percentage of maximal heart rate (%HRmax) that the person is exercising. ACSM uses %HRmax to describe intensity by assigning intensity levels to each percentage from light to near maximal/maximal (17). The maximal heart rate itself can be measured or estimated when prescribing exercise (20, 28).
Scherr et al. researched the relationship between RPE scale and HR-based intensity during a maximal incremental exercise test on a treadmill or cycle ergometer (19). The authors used multiple factors to determine the subject’s metabolic and cardiac intensity level which were used in comparison to the RPE scale during each stage of the test. Their findings show that the RPE and HR relationship are of equivalent magnitude when determining exercise intensity. This research helps direct the study at hand as the purpose is to investigate whether this relationship holds true during self-paced walking.
The research thus far on self-paced walking intensity in healthy adults is limited. Dasilva et al. conducted a study on over ground self-paced walking where the participants had to begin walking at 1.1 m·s−1 for 2 minutes then could adjust their speed for the next three minutes (6). They were then given the opportunity to change their speed only at 5-minute increments throughout the test. Their RPE was taken every 5 minutes and HR collected every 30 seconds. The study showed that self-paced walking performed in a more naturalistic setting may lead to lower perception of exertion, but this data is limited in its generalizability due to the participants only changing speed at regulated intervals. Mauger et al. studied self-paced protocol versus traditional VO2max testing on a cycle. Their self-paced protocol told participants specific RPE’s to attain where they had to then choose a pace they believed matched the given exertion for each 2-minute segment of the test. The authors of this study acknowledged that this is not a fully self-paced protocol (12). The study at hand will allow the participants complete freedom over their walking speed by asking them to walk at a pace as if they were walking for exercise, making it truly self-paced for the entire 15-minute walk.
Given the increase in interest of self-paced walking and its link with exercise adherence, it is imperative to determine whether healthy adults meet the Physical Activity Guidelines’ recommendation for intensity based on RPE and heart rate during self-paced walking. Determining the relationship between HR and RPE is important because a person’s perception of their work rate will determine how hard they will work unless they have other sources of feedback (HR, speed, etc.). If a person’s perception matches their HR, then they can be more effective at meeting the suggested physical activity levels based on the guidelines. Therefore, the purpose of this study is to determine how perceived exertion and heart rate during a 15-minute self-paced walk compares to the Physical Activity Guidelines for Americans in 18–64-year-old adults. The questions to be answered are as follows: are the heart rate- and exertion-based intensities obtained of equivalent magnitude and do the %HRmax and RPE achieved during self-paced walking match the recommended intensities based on the Physical Activity Guidelines? Based on the ACSM guidelines, it is hypothesized that heart rate- and exertion-based intensities will be of equivalent magnitude and that the %HRmax and RPE achieved during self-paced walking will match the recommended moderate intensity.
METHODS
Participants
Considering the main variable was the ranked intensity on a 1–5 scale, an a priori power analysis was completed for estimated sample size. Assuming a normally distributed data set, a one-sample mean test with a moderate effect size of 0.5, standard power of 0.80, and alpha of 0.05, and two-tailed was used. Thirty-four participants were suggested. Thirty adults (14 males, 16 females) volunteered to participate. Participant characteristics are presented in Table 1. The study was approved by the local Institutional Review Board prior to recruitment. Informed consent was obtained from all individual participants included in the study. The ACSM’s Exercise Preparticipation Health Screening Questionnaire for Exercise Professionals was completed and analyzed to determine the status of each participant, requiring them to have no current cardiovascular, metabolic or renal diseases or symptoms related to those diseases (17). Further acceptance into the study required participants to be between the ages 18 and 64 years and be literate. Participation was stopped if they experienced any of these symptoms: chest discomfort with exertion; unreasonable breathlessness; dizziness, fainting, blackouts; ankle swelling; unpleasant awareness of a forceful, rapid or irregular heart rate; or burning or cramping sensations in lower legs when walking short distances. This research was carried out fully in accordance to the ethical standards of the International Journal of Exercise Science (13).
Table 1.
Participant characteristics.
| Characteristic | Mean ± Standard Deviation |
|---|---|
| Age (years) | 26.7 ± 12.2 |
| BMI* (kg·m−2) | 25.4 ± 5.0 |
| Estimated VO2 (ml·kg−1·min−1) | Male = 45.4 ± 5.2 |
| Female = 37.7 ± 8.0 | |
| Resting HR (b·min−1) | 72.4 ± 14.9 |
| 6MWT** Distance (m) | 612.2 ± 70.8 |
| Godin Weekly METs (strenuous + moderate) | 41.15 ± 26.1 |
BMI, body mass index;
6MWT, 6-minute walk test
Protocol
Once the participant was cleared to join the study, they were sent instructions to avoid strenuous exercise the day before and day of the test, avoid eating, drinking alcohol or caffeine and smoking at least one hour prior to test time, and to wear appropriate clothing and shoes for exercise. Each participant was seen individually on two separate days with at least 48 hours in between testing days. Day 1 consisted of a 6-minute walk test (6-MWT) and Day 2 involved a 15-minute self-paced walk on an indoor track.
HR and RPE data were collected at minutes 2, 4, 6, 8 10, 12, 14 and immediately upon termination of the 15-minute walk. Fifteen minutes was chosen based on several study findings related to the possible distance traveled, attitude and work rate. The 15-minute walk time was the minimal time for a 1-mile walk by Phase II rehab patients (8). Versus 30 minutes, 10 minutes of self-paced walking has resulted in better scores for intention, attitude and self-efficacy following exercise (9). It has also been noted that at 15-minutes of self-paced walking, individuals reached levels close to their ventilatory threshold, a level that if exceeded has been noted as having a negative effect on affective responses (18). It was our intention not to confound our results by eliciting such a psychophysiological response.
Day 1: Height and weight were measured. The participant was taught how to put on a heart rate chest strap and a heart rate watch was placed on their wrist (Polar H10 Transmitter and Polar V800 watch). The participant was asked to sit comfortably and read the instructions for Borg’s 15-point Rating of Perceived Exertion scale (4) and was given an opportunity to ask questions. Resting heart rate was recorded after 5 minutes, this HR was also used to ensure correct strap placement and signal strength accuracy.
The American Thoracic Society’s (ATS) 6-minute walk test has been used to successfully predict VO2max for the healthy population, allowing the recruitment of a healthy population and use of the ATS for VO2max prediction (5). Two cones were set up in a nearby hallway, 30 meters apart per the ATS Guidelines for the 6-minute walk test (3). We followed standard procedures outlined in the ATS statement with modifications made due to our 30 participants being of a healthy population (no source of oxygen, no pulse oximeter). The instructions were read to the participant prior to the walk, with an opportunity for questions. Each lap was measured and recorded according to the ATS statement. At the end of the 6-minute walk, participants were asked their RPE while being shown the scale for RPE familiarization. Their position from the cone was measured and combined with the lap count to calculate the total distance walked.
Estimated VO2max was calculated using the 6-MWT data that was obtained (6-minute walk distance, sex, resting heart rate, age) and the following equation: VO2max (mL·kg−1·min−1) = 70.161 + (0.023 × 6-MWT [m]) - (0.276 × weight [kg]) - (6.79 × sex, where m = 0, f = 1) - (0.193 × resting HR [beats per minute]) - (0.191 × age [y]) (5). Day 2: Upon arrival to the lab, participants were fitted for the heart rate chest strap and then sat down for two to five minutes to measure their resting heart rate and allow them to reread the instructions for the RPE scale. They were then led to the track where the following instructions were read to them:
“The objective of this walk is for you to walk at a pace that you would choose if you were walking for exercise for 15 minutes. You will be asked to report your RPE every 2 minutes and again at the end of the walk. You will begin when we start your watch and we will come to you to collect your RPE. We will also check your watch for your heart rate every 2 minutes and immediately upon termination of the walk. We will match your pace, so keep walking at your pace and we will catch up to you. Any questions?”
After any questions were answered, the heart rate watch and stopwatch were started and participants began walking. At the end of the walk, the participant’s heart rate watch and stopwatch were stopped and RPE immediately assessed for the final moments of the walk.
Heart rates for each 2-minute time point and the end of the 15-minute walk were converted to a %HRmax for each individual using the following equation: %HRmax = measured HR × (220 – individual’s age)−1 × 100. Use of HRmax estimates are accepted by ACSM, and furthermore, ACSM provides equations that can be used to estimate HRmax based on the population that you are testing; for the present study, Fox et al. 220 – age was utilized due to its population being a group of men and women of a wide age range (17).
A ranking system (Table 2) was created for %HRmax and RPE using the ACSM’s Guidelines for Exercise Testing and Prescription Table 6.1 (17). There are five intensity categories in Table 6.1. To create our ranking system, these intensity categories were ranked in order of 1, very light to 5, maximal. This ranking system was then applied to each RPE and %HRmax time point from the walk for all participants (240 total time points; eight time points per participant × thirty participants). For example, a 2-minute RPE of 11 and %HRmax of 50% would have ranks of 2 and 1, respectively. Next, a score was assigned for each RPE and %HRmax time point that were collected at the same time for a given participant. When a time point had an RPE and %HRmax of the same intensity rank, a score of 1 was assigned. A score of 0 was assigned if they were not the same intensity rank. Using the previous example, RPE of rank 2 and %HRmax of rank 1 would result in a score of 0 for that time point. Therefore, if every RPE and %HRmax measured at a particular time point for each of the thirty participants during the walk were of an equivalent intensity, based on the ranking system, a perfect score of 240 would be achieved, one point for each available data point.
Table 2.
Ranking of the ACSM intensity levels for RPE and %HRmax1
| Rank | Intensity | %HRmax | RPE |
|---|---|---|---|
| 1 | Very light | <57 | <9 |
| 2 | Light | 57–63 | 9–11 |
| 3 | Moderate | 64–76 | 12–13 |
| 4 | Vigorous | 77–95 | 14–17 |
| 5 | Near maximal to maximal | ≥96 | ≥18 |
ACSM’s Guidelines for Exercise Testing and Prescription 10th ed, Table 6.1, pg. 146
Once the total score was determined using the above method, an “equivalency percentage” was calculated by dividing this score by 240 (total number of time points) and multiplying by 100 [score × (240 total score possible)−1 × 100 = equivalency]. This quantified how well the study data points included intensity-equivalent, time-matched RPE and %HRmax values. If every time point had an RPE and %HRmax of the same intensity and rank, then the equivalency percentage would be 100%. If none of the RPE and %HRmax were of similar intensities, the percentage would be 0%.
Statistical Analysis
All data are presented as mean ± standard deviation. Thirty participants were included in this study. A Wilcoxon matched pairs test was used to determine if the heart rate- and exertion-based intensities obtained were equivalent. To determine the relationship between HR and RPE, a Spearman’s rho correlation was run. A one-sample Wilcoxon signed rank test was used to determine if the achieved %HRmax and RPE matched the recommended moderate intensity based on the physical activity guidelines. Physical activity guidelines moderate intensity activity is represented by a ranking of 3 based on our ranking system (Table 2). Significance was set a priori p ≤ 0.05. Statistical analyses were performed with SPSS 24.0 (IBM, New York) with effect sizes and post-hoc power calculated using G*Power (version 3.1.9.2, Heinrich-Heine-Universität, Düsseldorf, Germany). Effect sizes are reported as Cohen’s d using the mean ranking of 3, mean and standard deviation of rank for RPE and %HRmax as appropriate. Post-hoc power analysis was run using a Wilcoxon signed-rank test, two tails, calculated effect size, α error of 0.05 and reported as 1-β.
RESULTS
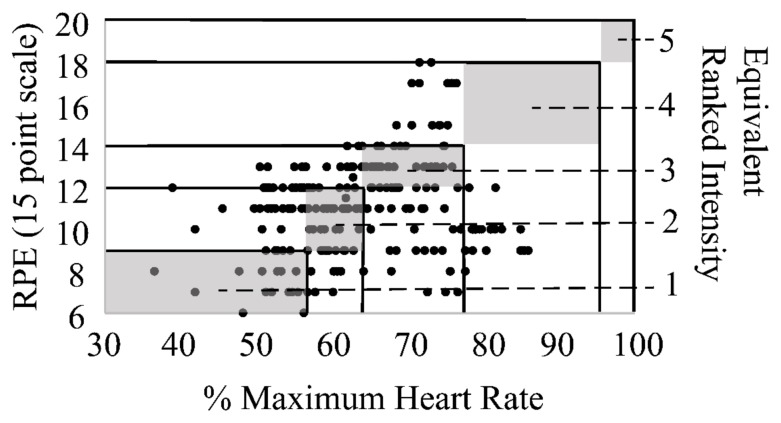
There was no significant mean difference found between RPE and %HRmax intensities (rank) based on the Wilcoxon matched pairs test (2.4 ± 0.9, 2.3 ± 1.0, respectively, p = 0.365); although, the Spearman’s rho correlation only shows a significant, small positive correlation between the two for intensity (rank) (rs = 0.201, p = 0.002) and the equivalency percentage between RPE and %HRmax was 37.5%. Furthermore, both the reported RPE and %HRmax magnitudes of the self-paced walk did not reach the physical activity guidelines recommended moderate intensity (ranking of 3) (p < 0.001, d = 0.67, 1-β = 0.93; p < 0.001, d = 0.70, 1-β = 0.95, respectively).
Figure 1 shows where the participants’ %HRmax and corresponding RPE fit into the intensity rankings in Table 2. Based on the data point density, it is apparent that most data points are not found inside of the boxes. To be exact, only 37.5% of the data points fall inside of the boxes.
Figure 1.
Intensity comparisons. Gray boxes represent equivalent intensities for RPE and % maximum heart rate based on ACSM Guidelines for Exercise Testing and Prescription 10th ed. Black dots represent single data points taken each two minutes of the self-paced walk for all participants.
DISCUSSION
The purpose of this self-paced walk study was to determine if healthy adults self-paced their walking exercise at an exertion level where the heart rate- and perceived exertion-based intensities are equal and if those intensities match the physical activity guidelines recommendation for daily exercise of moderate intensity. Participation in exercise is very low due to a low rate of initial engagement and the high rate of dropout (11). Breaking those barriers is essential to physical activity, but may be hard to do as exercising at the correct intensity may be harder than it seems.
The main testable hypothesis was to determine if the HR- and perceived exertion-based intensities from the self-paced walk were of equivalent magnitude. Equivalency of the %HRmax and RPE categories (Table 2) shows that as the HR increases during exercise, the exertion level experienced by the participant should increase accordingly. The results revealed that no significant mean difference between %HRmax and RPE’s intensity existed. This initial finding suggests that self-paced exercise does not alter the relationship between heart rate and RPE that is created when using ACSM Guidelines. Support for this finding comes from the significant correlation between RPE and %HRmax that exists. This result is important for clinicians who prescribe self-paced exercise to clients and patients as a means to improve exercise adherence while also continuing to use RPE or HR based intensities to keep track of their efforts. It should be noted, however, that the significant correlation was only slight. Correlation coefficients lower than 0.5 are generally thought to be useful for identifying non-chance relationships among variables, but not for predicting individual scores (27). While the correlation is significant, the further analysis of the results suggest that caution should be had when substituting between RPE and %HRmax, particularly in cardiovascular training or with conditions where limiting HR is necessary.
Easton and Williams conducted research on the RPE scale while placed on a cycle ergometer where the participant pedaled at an effort based on 3 different RPE levels for comparison to VO2max, HR, etc. They concluded RPE is a reliable reference for different levels of effort when comparing it to VO2max (7). They did note though that the HR and RPR correlations were lower than those found for VO2. This could direct future research in measuring VO2 for comparison to RPE during self-paced walking as HR has been shown here to not have a strong significant correlation with RPE. Although Dasilva et al. did not compare results specifically as the present study did, they did mark that their intensity reached during self-paced walking on the treadmill and overground walking was below ACSM’s recommended intensity which corresponds to the RPE values ranging from 8 to 11, also below the recommended intensity (6). This shows that there is a need for more data to test the correlation more thoroughly between RPE and %HRmax intensity during self-paced walking.
Additionally, despite the absence of a significant difference between mean RPE and %HRmax intensities, Figure 1 reveals a more evident, weak relationship between the two. Assuming the %HRmax is the more accurate method of determining exertion level, data points that are above or below the gray box reveal an over- or underreported RPE, respectively. This further exemplifies that RPE and HR during the self-paced walk are not of equivalent magnitude, only receiving an equivalency score of 37.5%. This evidence cautions practitioners against the suggestion that the intensities in Table 6.1 of the ACSM guidelines text are equivalent despite what might be an initial reaction to see them as such (17).
There is a noticeable slight upward trend between the RPE and %HRmax as the intensity increases (Figure 2); with the correlation between them being very slight. Noticeably, the ACSM-based RPE/%HRmax equivalency line and the linear regression line for the present data do not match. Figure 2 suggests that participants reported a relatively high RPE at the lower intensities and a relatively low RPE as intensities increased beyond moderate, when compared to their %HRmax. Some studies have concluded that the Borg RPE scale is more reliable as the work becomes more intense (7, 20). Smutok et al. further concludes that RPE provides a safe and reliable HR response when activity is above 80%HRmax (23). Although these statements have stated the higher intensity is most accurate for the substitution of RPE and %HRmax, the self-paced walking was important for the comparison of intensity level to the PAG. The present study tested participants at a self-paced exercise intensity, with most exercising at a light-moderate intensity, and saw great variability in the %HRmax versus RPE intensities, shown by the relatively large standard deviations and large amount of time points falling in different intensities seen in Figure 1. Based on these other studies, interchanging RPE and HR may be more reliable at higher rather than lower intensities showing a limitation to the study at hand which only tested self-paced walking which fell in the lower intensities. These data further supports the idea that RPE and %HRmax are not interchangeable in self-paced walking and that RPE may be overestimated at lower intensities and underestimated at higher intensities.
Figure 2.
Theorized and realized intensity correlations. Solid line represents the trendline for ACSM-based data. Dotted line represents the trendline for the study data.
The intensities of RPE and %HRmax during the self-paced walk did not match the recommended intensities for the physical activity guidelines. The results revealed that the mean RPE and %HRmax compared to the moderate intensity level of 3 were statistically different. In contrast, Williams et al. determined there was no significant difference between self-paced exercise intensity and prescribed intensity exercise measured when testing a group of predominately female overweight and obese individuals (28). Their prescribed intensity exercise was based on the ACSM’s guidelines for moderate intensity exercise based on a percentage of max heart rate, also using HRmax = 220-age. Major differences between that study and the present study were the testing environments and populations; Williams et al. participants were given instructions to exercise on their own time without supervision following a 6-month exercise promotion program. In addition to the different exercise protocol, the participants differed from the current study which included healthy men and women of a wide age range of BMI and fitness who did not engage in a 6-month structured program. This program may have been integral to those participants choosing to engage in a more intense level of physical activity.
The importance of the 220-age HRmax equation is due to the population size and limitations of the testing for this particular study, there are some studies that have successfully implemented the use of the same equation. It is important to note that although many studies use this equation, it is a limitation to the study. This equation only allows for an estimation of %HRmax based on age, while a true max test measures this variable directly. The error associated with this equation may have contributed to the difference between measured HR-based exercise intensity and the ACSM benchmark moderate intensity guideline.
RPE is a subjective measurement that the participants were thoroughly prepared to give during their self-paced walk after reading Borg’s RPE instructions and being given practice after the 6MWT, however, there are many factors that can affect the reported exertion level during exercise, two of those being fitness level and age. The fitness level of each individual varies depending on their exercise background, their job/hobbies, genetics, etc. According to Garcin et al., the individual’s level of fitness effects their perceived exertion for a given exercise intensity (10). They determined that lower level of fitness individuals perceived exercise as more strenuous than individuals of higher fitness levels. The Godin Leisure Time Questionnaire was shown by Amireualt and Godin to classify a person as an active person or an inactive person (2). This classification used calculated MET level from 15-minute bouts of strenuous and moderate exercise to classify a person as active or inactive. Any person with a MET sum of 24 or more was distinguished as active and below 24 was inactive. The participants in this study averaged a MET level of 41.15, with 70% of the participants over the 24 MET level; therefore, the study population is considered active. Age also effects the reported level of exertion from individuals with older adults underestimating their perceived exertion level (15). In light of these studies, the present data were separated into two categories based on age (≤ 25 and > 25 years), and again based on 3 fitness level categories (VO2peak < 40, 40 to 45, and > 45 ml·kg−1·min−1); no marked improvements in RPE and %HRmax equivalency % was seen for age (37.1% and 38.8%, respectively) or fitness (38.8%, 45.0% and 28.8%, respectively). Although the fitness level was considered active, the type of activity that the participants regularly participate in to be considered active could be different than walking for exercise, creating a limitation to the study due to their limited prior experience with walking for exercise.
Abbiss et al. also presented a valid point in their research on what the ratings of perceived exertion are actually measuring (1). They determined that it is difficult to determine if exertion or effort is properly being measured due to language differences, posed question when presenting the scale and user’s definition of these terms. Our instructions on reporting RPE consistently used “exertion” as the term and defined it as depending on “strain and fatigue in your muscles and on your feeling of breathlessness or aches in the chest”. However, it should be noted that in the final paragraph of the instructions it states, “it’s your own feeling of effort and exertion that’s important…” Additionally, throughout the explanation of how to use the scale, descriptions that are consistent with effort were also included, e.g. “17… he or she really has to push him- or herself..” This would be consistent with effort rather than exertion. These findings are in line with the concerns presented by Abbiss et al. Our study, with the lack of correlation between %HRmax and RPE, thus shows how RPE scale use for assessing exercise intensities during self-paced exercise may be improper, depending on the instructions given. The importance of continued research in RPE scale use for self-paced exercise is imperative.
This study has provided evidence that individuals may perceive their exertion level as harder than or easier than the HR-based intensity when self-pace walking. The intended intensity level may affect the relationship between RPE and HR. Overall, participants did not exercise at the recommended moderate intensity level based on RPE and HR. These findings suggest that self-paced walking as a modality of physical activity for meeting guidelines may result in intensities lower than intended. Practitioners who prescribe exercise for health should be aware of how each client or patient perceives their effort in relation to their heart rate response if self-paced walking is to be undertaken.
ACKNOWLEDGEMENTS
We would like to thank Marissa Frommeyer for all of the assistance she provided during data collection.
REFERENCES
- 1.Abbiss CR, Peiffer JJ, Meeusen R, Skorski S. Role of ratings of perceived exertion during self-paced exercise: What are we actually measuring? Sports Med. 2015;45:1235–1243. doi: 10.1007/s40279-015-0344-5. [DOI] [PubMed] [Google Scholar]
- 2.Amireault S, Godin G. The Godin-Shepard leisure-time physical activity questionnaire: Validity evidence supporting its use for classifying healthy adults into active and insufficiently active categories. Percept Mot Skills. 2015;120(2):604–622. doi: 10.2466/03.27.PMS.120v19x7. [DOI] [PubMed] [Google Scholar]
- 3.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 4.Borg G. An introduction to Borg’s RPE scale. New York: Mouvement Publications; 1985. [Google Scholar]
- 5.Burr JF, Bredin SS, Faktor MD, Warburton DER. The 6-minute walk test as a predictor of objectively measured aerobic fitness in healthy working-aged adults. Physician Sports Med. 2011;39(2):133–139. doi: 10.3810/psm.2011.05.1904. [DOI] [PubMed] [Google Scholar]
- 6.Dasilva SG, Guidetti L, Buzzachera CF, Elsangedy HM, Krinski K, De Campos W, Baldari C. Psychophysiological responses to self-paced treadmill and overground exercise. Med Sci Sports Exerc. 2010;43(6):1114–1124. doi: 10.1249/MSS.0b013e318205874c. [DOI] [PubMed] [Google Scholar]
- 7.Eston RG, Williams JG. Reliability of ratings of perceived effort regulation of exercise intensity. Br J Sports Med. 1988;22(4):153–155. doi: 10.1136/bjsm.22.4.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Faulkner J, Gerhard J, Stoner L, Lambrick D. Self-paced walking within a diverse topographical environment elicits an appropriate training stimulus for cardiac rehabilitation patients. Rehabilitation Res Prac. 2012:1–5. doi: 10.1155/2012/140871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Focht B. Affective responses to 10-minute and 30-minute walks in sedentary overweight women: Relationships with theory-based correlates of walking for exercise. Psychol Sport Exerc. 2013;14:759–766. [Google Scholar]
- 10.Garcin M, Mille-Hamard L, Billat V. Influence of aerobic fitness level on measured and estimated perceived exertion during exhausting runs. Int J Sports Med. 2004;25(4):270–277. doi: 10.1055/s-2004-819939. [DOI] [PubMed] [Google Scholar]
- 11.Lind E, Joens-Matre RR, Panteleimon E. What intensity of physical activity do previously sedentary middle-aged women select? Evidence of a coherent pattern from physiological, perceptual, and affective markers. Prev Med. 2005;40(4):407–419. doi: 10.1016/j.ypmed.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 12.Mauger AR, Sculthorpe N. A new VO2max protocol allowing self-pacing in maximal incremental exercise. Br J Sports Med. 2011;46(1):59–63. doi: 10.1136/bjsports-2011-090006. [DOI] [PubMed] [Google Scholar]
- 13.Navalta JW, Stone WJ, Lyons TS. Ethical Issues Relating to Scientific Discovery in Exercise Science. Int J Exerc Sci. 2019;12(1):1–8. doi: 10.70252/EYCD6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Oliveira BRR, Deslandes AC, Santos TM. Differences in exercise intensity seems to influence the affective responses in self-selected and imposed exercise: A meta-analysis. Front Psychcol. 2015;6(1105):1–9. doi: 10.3389/fpsyg.2015.01105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pincivero D. Older adults underestimate RPE and knee extensor torque as compared with young adults. Med Sci Sports Exerc. 2011;43(1):171–180. doi: 10.1249/MSS.0b013e3181e91e0d. [DOI] [PubMed] [Google Scholar]
- 16.Rejeski WJ. The perception of exertion: A social psychophysiological integration. Hum Kinetics J. 1981;3(4):305–320. [Google Scholar]
- 17.Riebe D, Ehrman JK, Liguori G, Magal M, editors. ACSM’s Guidelines for Exercise Testing and Prescription. 10th ed. Philadelphia, PA: Kluwer; 2017. [Google Scholar]
- 18.Rose EA, Parfitt G. Exercise experience influences affective and motivational outcomes of prescribed and self-selected intensity exercise. Scand J Med Sci Sports. 2012;22:265–277. doi: 10.1111/j.1600-0838.2010.01161.x. [DOI] [PubMed] [Google Scholar]
- 19.Scherr J, Wolfarth B, Christle J, Pressler A, Wagenpfeil S, Halle M. Associations between Borg’s rating of perceived exertion and physiological measures of exercise intensity. Eur J Appl Physiol. 2013;113:147–155. doi: 10.1007/s00421-012-2421-x. [DOI] [PubMed] [Google Scholar]
- 20.Scotson KR. The effect of prescribed and preferred intensity exercise on the relationship between self-efficacy and perceived exertion in older adults. Edith Cowan University; Australia: 2001. Retrieved from https://ro.ecu.edu.au/theses/1075. [Google Scholar]
- 21.Siegel P, Brackbill RM, Heath GW. The epidemiology of walking for exercise: Implications for promoting activity among sedentary groups. Am J Public Health. 1995;85(5):706–710. doi: 10.2105/ajph.85.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Silliman K, Rodas-Fortier K, Neyman M. A survey of dietary and exercise habits and perceived barriers to following a healthy lifestyle in a college population. Cal J Health Promot. 2004;2(2):10–19. [Google Scholar]
- 23.Smutok MA, Skrinar GS, Pandolf KB. Exercise intensity: Subjective regulation by perceived exertion. Arch Phys Med Rehabil. 1980;61:569–574. [PubMed] [Google Scholar]
- 24.Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T. Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 25.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 1st ed. Washington, D.C: U.S. Department of Health and Human Services; 2008. [Google Scholar]
- 26.U.S. Department of Health and Human Services. Physical Activity Guidelines for Americans. 2nd ed. Washington, D.C: U.S. Department of Health and Human Services; 2018. [Google Scholar]
- 27.Vincent WJ, Weir JP. Correlation and Bivariate Regression Statistics in Kinesiology. 4th ed. Illinois: Human Kinetics Publisher; 2012. [Google Scholar]
- 28.Williams DM, Dunsiger S, Miranda R, Jr, Gwaltney CJ, Emerson JA, Monti PM. Recommending self-paced exercise among overweight and obese adults: A randomized pilot study. Ann Behav Med. 2015;49(2):280–285. doi: 10.1007/s12160-014-9642-7. [DOI] [PMC free article] [PubMed] [Google Scholar]