Studies of infectious diseases have been limited by the lack of models that recapitulate normal cellular physiology and pathology. Developments in organotypic models have paved the road towards further studies of viral infections and host–virus interactions. For example, human intestinal organoids were efficiently used to study many viruses, such as rotavirus, norovirus, enterovirus 71, and human adenovirus.1
Mammalian airway organoids are complex three-dimensional structures characterised by different cellular composition and designed to mimic lung structures. Early research attempted to develop these organoids from different progenitor cells, including basal cells, secretory cells, and alveolar epithelial cells.2 In the past 5 years, scientists were able to generate mature lung organoids that contain basal, ciliated, and club cells. These organoids were used to study diseases such as cystic fibrosis and lung tumours, and infections.3 One study4 used airway organoids to look at viral replication, tissue tropism, and immune response to many human influenza A and avian viruses.
Fortunately, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus responsible for COVID-19, was isolated and propagated early on in the pandemic using numerous in-vitro models, such as Vero cells, Huh7 cells, and human airway epithelial cells. This isolation was enhanced after SARS-CoV-2 was isolated and propagated in TMPRSS2-expressing VeroE6 cells, indicating the vital role of TMPRSS2 serine protease in virus infectivity.5 Thus, in-vitro models are effective in the study of virus propagation, but they poorly recapitulate respiratory tract histology and function.
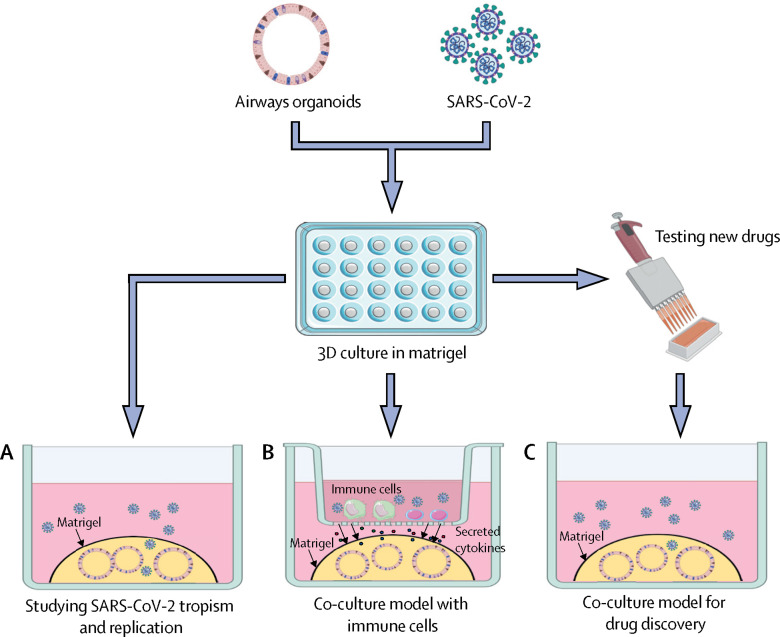
We recommend the use of human airway organoids as a model to study SARS-CoV-2 replication kinetics, tropism, and host response (figure ). Airway organoids can be generated using healthy lung tissue derived from patients undergoing surgical resection, and SARS-CoV-2 can be obtained from clinical specimens from patients who have tested positive. After the airway organoid is infected with SARS-CoV-2, immunofluorescence and electron scanning microscopes could be used to study the cytopathic effects of viral particles on different cell types. Furthermore, whole-genome sequencing and real-time quantitative PCR could determine viral replication kinetics and genetic alterations, and transcriptomic profiling could reveal the differential expression of genes related to viral infection. Additionally, flow cytometry enables the detection and quantification of different cell types before and after SARS-CoV-2 infection.
Figure.
Co-culture of airways organoids
Co-culture of airways organoids with SARS-CoV-2 could be used to study viral replication, tropism, and pathogenicity in addition to structural changes (A); study immune responses and cytokine release, recapitulate some pathological conditions such as cytokine release syndrome, and develop immunomodulatory drugs (B); and as a tool for antiviral drug discovery and development (C). Created using BioRender.com.
Angiotensin converting enzyme 2 and TMPRSS2 serine protease are highly expressed in human airway epithelia and airway organoids,6, 7 making models that use airway organoids suitable for the study of viral infectivity, since these proteins are thought to facilitate infection of cells.
Airway organoids could also be used in a co-culture model and be cultured with different immune cells. This co-culture model would enable the study of immunological responses to SARS-CoV-2. Moreover, genomic and transcriptomic profiling could reveal further signalling pathways involved in such immune responses. It is also possible to detect the secreted cytokines in response to SARS-CoV-2 infection and hence provide a model to recapitulate cytokine release syndrome seen in some patients with COVID-19.8 Moreover, a co-culture model could be used to explore the activity of immunomodulatory drugs.
Airway organoids could also be used to discover effective antiviral drugs to treat COVID-19. The potential activity of drug candidates could be predicted by several laboratory methods: real-time quantitative PCR can assess viral load, while immunofluorescence and electron microscopy can identify the number of cells that have been infected. Additionally, microarray analyses can identify the molecular mechanisms of investigational drugs and their possible cellular targets. Models using airway organoids could be invaluable to learn more about SARS-CoV-2 infectivity, replication kinetics, and host–virus interactions, an understanding of which will be key to help fight the current pandemic.
Acknowledgments
We declare no competing interests.
References
- 1.Ramani S, Crawford SE, Blutt SE, Estes MK. Human organoid cultures: transformative new tools for human virus studies. Curr Opin Virol. 2018;29:79–86. doi: 10.1016/j.coviro.2018.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barkauskas CE, Chung MI, Fioret B, Gao X, Katsura H, Hogan BLM. Lung organoids: current uses and future promise. Development. 2017;144:986–997. doi: 10.1242/dev.140103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sachs N, Papaspyropoulos A, Zomer-van Ommen DD. Long-term expanding human airway organoids for disease modeling. EMBO J. 2019;38:1–20. doi: 10.15252/embj.2018100300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hui KPY, Ching RHH, Chan SKH. Tropism, replication competence, and innate immune responses of influenza virus: an analysis of human airway organoids and ex-vivo bronchus cultures. Lancet Respir Med. 2018;6:846–854. doi: 10.1016/S2213-2600(18)30236-4. [DOI] [PubMed] [Google Scholar]
- 5.Matsuyama S, Nao N, Shirato K. Enhanced isolation of SARS-CoV-2 by TMPRSS2-expressing cells. Proc Natl Acad Sci USA. 2020;117:7001–7003. doi: 10.1073/pnas.2002589117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou J, Li C, Sachs N. Differentiated human airway organoids to assess infectivity of emerging influenza virus. Proc Natl Acad Sci USA. 2018;115:6822–6827. doi: 10.1073/pnas.1806308115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oudit GY, Imai Y, Kuba K, Scholey JW, Penninger JM. The role of ACE2 in pulmonary diseases—relevance for the nephrologist. Nephrol Dial Transplant. 2009;24:1362–1365. doi: 10.1093/ndt/gfp065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi Y, Wang Y, Shao C. COVID-19 infection: the perspectives on immune responses. Cell Death Differ. 2020;27:1451–1454. doi: 10.1038/s41418-020-0530-3. [DOI] [PMC free article] [PubMed] [Google Scholar]