Abstract
Background:
Recent studies indicate concussion increases risk of musculoskeletal injury in specific groups of patients. The purpose of this study was to determine the odds of anterior cruciate ligament (ACL) injury after concussion in a population-based cohort.
Methods:
International Classification of Diseases, 9th and 10th Revision (ICD-9, ICD-10) codes relevant to the diagnosis and treatment of a concussion and ACL tear were utilized to search the Rochester Epidemiology Project (REP) between 2000 and 2017. A total of 1,653 unique patients with acute, isolated ACL tears were identified. Medical records for cases were reviewed to confirm ACL tear diagnosis and to determine history of concussion within 3 years prior to the ACL injury. Cases were matched by age, sex, and REP availability date to patients without an ACL tear (1:3 match), resulting in 4,959 controls. The medical records of the matched control patients were reviewed to determine history of concussion.
Results:
39 patients with a concussion suffered an ACL injury up to 3 years after the concussion. The rate of prior concussion was higher in ACL-injured cases (2.4%) compared to matched controls with no ACL injury (1.5%). This corresponds to an odds ratio of 1.6 (95% CI 1.1-2.4; p=0.015).
Conclusions:
Although activity level could not be assessed, there are increased odds of ACL injury after concussion in a general population. Based on the evidence of increased odds of musculoskeletal injury after concussion, standard clinical assessments should consider concussion symptom resolution as well as assessment of neuromuscular factors associated with risk of injuries.
1. Introduction
An estimated 1.7 million people sustain a traumatic brain injury (TBI) annually in the United States and are the cause for an estimated 2.8 million emergency department visits.[1, 2] In particular, mild traumatic brain injuries (mTBI) are thought to be underreported and undercounted.[2] For example, it is estimated that between 1.6 million and 3.8 million sports-related concussions, a form of mTBI, occur each year in the United States.[3] Among athletes who sustain a concussion, a recent meta-analysis showed over two times greater odds of sustaining a lower extremity musculoskeletal injury than athletes without concussion.[4] A recent matched-cohort study among active duty soldiers showed an increased hazard of acute lower extremity injury after sustaining a concussion.[5] In further confirmation of these findings, another recent meta-analysis that included both military and athletic populations also confirmed over 2.5 times increased odds of all injuries after a concussion.[6] Therefore, with the high incidence of mTBI and concussion in both the general population and specific groups of athletes and soldiers, it is important to understand the sequelae after a concussion.
The recent data that relates concussion to an increased risk of musculoskeletal injury is in line with prior studies that point to neurologic risk factors in anterior cruciate ligament (ACL) injuries.[7-15] Of particular relevance, noncontact ACL injuries have been associated with lower neurocognitive function in non-concussed athletes, which suggested that neurocognitive differences may be associated with the loss of neuromuscular control and coordination errors leading to increased risk of ACL injury.[14] The incidence and rate of ACL injuries continues to increase, and results in approximately a $2 billion economic burden for the associated treatment and rehabilitation in the United States alone.[16, 17] Thus, it is important to identify potential factors that increase risk of an ACL injury, such as a previous injury like concussion. Previous injury is a known risk factor for ACL injury[12], but to date there is limited evidence that shows if history of a concussion increases risk for an ACL injury.
While the evidence for the relationship between concussion and musculoskeletal injury risk continues to grow, most studies to date have focused on specialized cohorts such as competitive athletes or soldiers. As such, their results may not be generalizable to a larger population. It is important to determine if the increased odds of injury after concussion is also present in a general population as concussion and/or musculoskeletal injuries can occur outside of elite athletic environments.[18] However, geographically-based epidemiological data are lacking to support previous findings of increased odds of musculoskeletal injury after concussion. Also, most studies have included any injury, or only limited the injuries to the lower extremity.[19-28] Given the increasing number of children who participate in athletics, and the increasing population of fitness enthusiasts, researchers should examine the general population-based odds of ACL injury after concussion.[16] Therefore, the current study sought to perform a population-based cohort study that relates concussion to a specific musculoskeletal injury known to be modulated by neuromuscular control. The general population is from a single geographic region that is generalizable to the larger population.[29] It was hypothesized that patients with a concussion have increased odds of ACL injury within three years after the concussion compared to patients without history of concussion. It is important to identify this relationship in order to make clinicians aware of potential sub-clinical threshold changes after concussion that lead to increased risk of musculoskeletal injury upon return to normal activities of daily living in the general population.
2. Methods
The Rochester Epidemiology Project (REP) is a medical record linkage system that provides access to complete medical records for all residents of Olmsted County, Minnesota, USA, regardless of the medical facility in which the healthcare was delivered.[29-32] The REP database has included over 6.1 million health records since its creation. This unique population-based data infrastructure allows for the complete determination and follow-up of all clinical diagnoses in a geographically defined community.[30] Moreover, REP epidemiological data have demonstrated generalizability to larger populations.[29] Institutional review board approval was obtained from both the Mayo Clinic and the Olmsted Medical Center. All patients provided general research authorization for use of their medical records at the time of medical care.
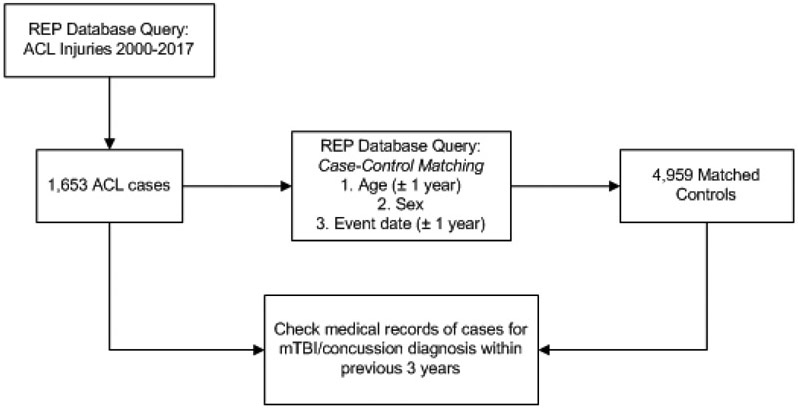
The REP database was queried for all occurrences of mTBIs, concussions, and ACL tears (based on International Classification of Diseases, 9th Revision [ICD-9], 10th Revision [ICD-10] diagnosis codes) from 2000 to 2017. Moderate and severe TBIs were excluded. While it would be preferable to match cases to controls by activity level, activity level is not consistently documented in the medical record; therefore, age was utilized as a surrogate for activity level (Table 1).[33] Records were included if evidence of an ACL tear (inclusive of grade I-grade III) existed based on clinical orthopedic examinations, arthroscopic examinations, magnetic resonance imaging (MRI), or operative reports of an ACL reconstruction.[33] The results yielded 1,653 patients in the defined population with an ACL injury (Figure 1). Roughly 81% of these patients had an ACL reconstruction, which aligns with previously published studies on this cohort.[34] These 1,653 patients were matched to Olmsted County residents identified in the REP database without an ACL diagnostic code in their medical record using a computerized matching algorithm. Each case was matched to three controls based on age (± 1 year, >99%), sex (exact, 100%), and event date (± 1 year, 100%), where the event date is the date of ACL injury for the cases or the REP availability date for the matched controls. A 1:3 case-control matching was performed to achieve sufficient statistical power,[35] which resulted in 1,653 ACL injury cases and 4,959 matched controls.[35]
Table 1:
Demographic comparison between ACL cases and matched controls with no ACL injury.
| ACL | Control | ||
|---|---|---|---|
| n (M/F) | 1,653 (924/729) | 4,959 (2,772/2,187) | |
| Number with concussions | 39 | 73 | |
| Age in years (SD) | 30.8 (13.1) | 30.7 (13.0) | |
ACL, anterior cruciate ligament; M, male; F, female; SD, standard deviation.
Figure 1:
Flow chart to identify ACL injury cases in the REP database, then identification of matched controls subjects. Both case and control medical records were checked for diagnosis of an mTBI or concussion within the three years prior to the event date. REP, Rochester Epidemiology Project.
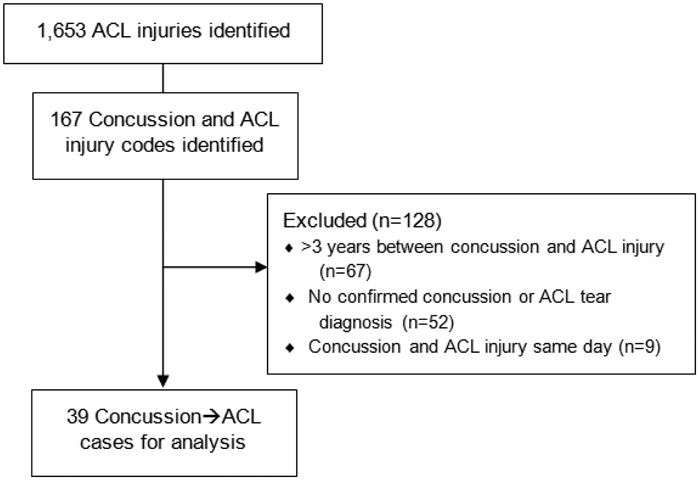
REP database query results for patients with both concussion and ACL diagnostic codes were searched for confirmation of an mTBI or concussion diagnosis. Two authors (ALM, MBS) reviewed all medical records to confirm the concussion diagnosis. A patient was included if their medical record contained documentation of an mTBI or concussion diagnosis by a doctor within three years prior to the ACL injury. Clinical diagnosis followed standard consensus statements for the respective time (e.g. Consensus Statement on Concussion in Sport: The 5th International Conference on Concussion in Sport, Berlin, October 2016).[36] Patients were excluded from analysis if the concussion and ACL injury event dates were the same or greater than three years apart to ensure all cases near the two year time point were captured. Previous studies have follow-up time frames that range from 90 days to two years post-concussion and have reported increased risk of injury after concussion within this timeframe.[19, 20, 23] In addition, a three year timeframe was selected to extend the current literature and to determine if increased risk of injury is longer than what previous studies have captured. The records of the matched controls were cross-referenced to verify whether an mTBI or concussion diagnosis was recorded in their medical record within three years prior to their match date. Matched controls were excluded if a moderate or severe TBI was documented within three years prior to their match date.
The data were summarized using means and standard deviations for continuous variables, and counts and percentages for categorical variables. The study was designed as a matched case-control study in which the outcome was defined as ACL injury and the exposure was defined as a concussion in the prior three years. The association of concussion and ACL injury was evaluated using logistic regression. The model was adjusted for age, sex, and year of ACL injury or control availability. Additional logistic regression models were generated for males and females separately, as well as by age groups. The results were summarized using odds ratios (OR) and reported with 95% confidence intervals. The association was considered significant if p ≤ 0.05 and the 95% confidence interval (CI) for the odds ratio did not contain 1. Assumptions were checked and model diagnostics were examined to verify model validity. All analyses were conducted using JMP 14 and SAS version 9.4 (SAS Institute, Inc., Cary, NC).
3. Results
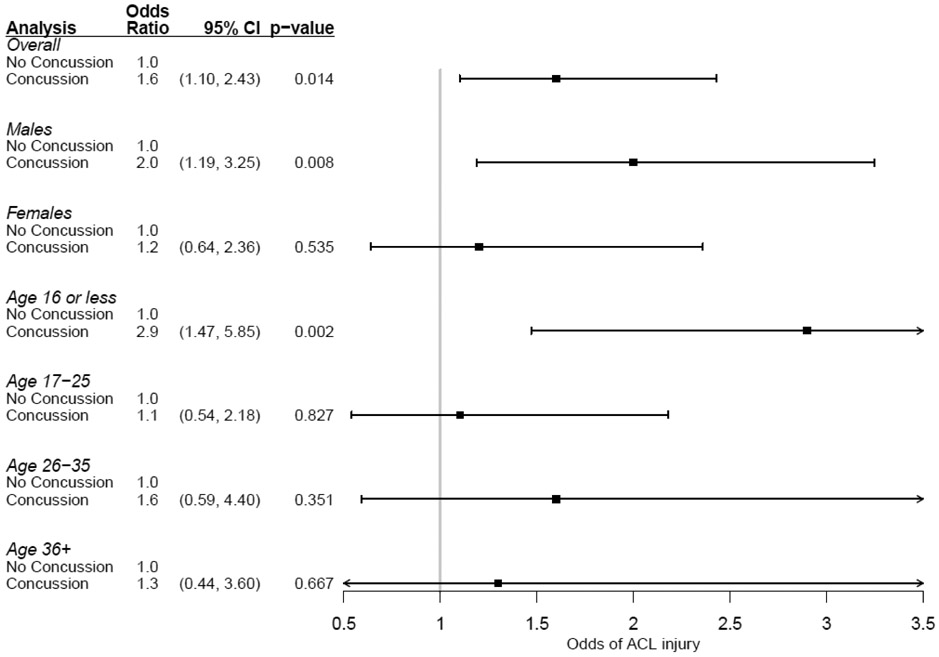
Each ACL case (n = 1,653) was matched to three healthy control subjects (n = 4,959) from the REP population database (Table 1). 56% of the ACL cases (n = 924) and matched control subjects (n = 2,772) were male. Within the time frame queried, there were 1,653 ACL injuries, of which 39 cases of ACL injury after a concussion were confirmed (Figure 2). 54% of ACL case concussions were attributed to a sporting mechanism compared to 48% of the control concussions (Figure 3). The average time between concussion and ACL Injury in the current cohort (n = 39) was 1.43 (± 0.9) years. The rate of prior concussion was higher in patients with an ACL injury (2.4%) compared to matched controls with no ACL injury (1.5%). This corresponds to an odds ratio of 1.6 (95% CI 1.1-2.4), p = 0.015, which indicates a significant association between concussion and subsequent ACL injury (Tables 2-3).
Figure 2:
Flow chart of ACL injury case identification and exclusion.
Figure 3:
Distribution of concussion mechanism between ACL cases and matched control subjects with no ACL injury. Undetermined was selected if the medical record gave no indication of how the concussion injury was sustained. Non-sporting mechanism included, but was not limited to, motor vehicle accidents, assault, and falls.
Table 2:
Adjusted logistic regression models for the overall group, and for sex-specific models.
| Adjusted logistic regression models | |||
|---|---|---|---|
| Group | Model Effects | Odds Ratio (95% CI) | p-value |
| Overall | Concussion | 1.6 (1.10, 2.43) | 0.014 |
| Age | 1.0 (1.00, 1.01) | 0.588 | |
| Sex | 1.0 (0.89, 1.12) | 0.999 | |
| Calendar year | 1.0 (0.99, 1.01) | 0.820 | |
| Males | Concussion | 2.0 (1.19, 3.25) | 0.0 08 |
| Age | 1.0 (1.00, 1.01) | 0.551 | |
| Calendar year | 1.0 (0.98, 1.01) | 0.809 | |
| Females | Concussion | 1.2 (0.64, 2.36) | 0.535 |
| Age | 1.0 (1.00, 1.01) | 0.836 | |
| Calendar year | 1.0 (0.98, 1.02) | 0.946 | |
Table 3.
Concussion and ACL injury.
| No concussion | Concussion | Odds Ratio (95% CI) | p-value | |
|---|---|---|---|---|
| ACL Injury (n=1653) | 1,614 (97.6%) | 39 (2.4%) | 1.6 (1.1, 2.4) | 0.014 |
| Control (n=4959) | 4,886 (98.5%) | 73 (1.5%) | Ref |
ACL, anterior cruciate ligament; CI, confidence interval.
Sex-specific analysis revealed that the rate of ACL injury was higher in concussed males (2.8%) than non-concussed males (1.5%), which corresponds to an odds ratio of 2.0 (95% CI 1.2-3.3; p = 0.008) (Table 2, Figure 4). The association between concussion and subsequent ACL injury was not significant in females, with an odds ratio of 1.2 (95% CI 0.6-2.4; p = 0.535). For age-group analysis, the association between concussion and subsequent ACL injury was significant only for the 16 years old and younger age group (OR = 2.9, 95% CI 1.5-5.9; p = 0.002) (Figure 4).
Figure 4:
Forest plot shows the odds ratio for the adjusted logistic regression models for the overall group, each sex-specific, and each age-group analyses.
4. Discussion
Previous studies have identified increased risk of lower extremity musculoskeletal injury in athletic and active military populations, but not specifically for ACL injuries, and not in a general population.[4, 5, 19-28] The current study confirms the hypothesis that there are increased odds of ACL injury after a concussion in a population-based cohort. The odds ratio of sustaining an ACL injury within three years after a concussion observed in this study (OR = 1.6, 95% CI 1.1-2.4) is consistent with prior reported statistics of any lower extremity injury after a concussion.[19-28] Given the substantial body of evidence that shows the majority of ACL injuries occur by a non-contact mechanism[37, 38] and that ACL rupture has been linked with altered neuromuscular control[10, 39], it follows that after a concussion the odds of an ACL injury are increased. The resultant neurocognitive and neuromuscular dysregulation from the concussion may contribute to the increased risk of lower extremity injury previously established[4, 40], and now specifically increased odds of ACL injury.
A three year window was selected for inclusion criteria for ACL injury after a concussion in the current study to extend the window of time previous studies have utilized to investigate the association between concussion and injury. Previous studies have follow-up time frames that range from 90 days to two years post-concussion and have reported increased risk of injury after concussion within this time frame.[19, 20, 23] The average time between concussion and ACL Injury in the current cohort (n = 39) was 1.43 (± 0.9) years, which falls within the range of the previous studies’ follow-up window. This suggests that the average time from concussion to lower extremity injury, and specifically ACL injury, is between six months and two years; accordingly, this is the time period that should be monitored closely.
As the research community and the media have focused on the effects of concussions, clinical emphasis has also focused on assessment of individuals for appropriateness for return to activity.[11, 12, 41-47] Players, parents, coaches, and physicians appropriately assess the risk of long-term neurologic deficits in consideration of return to sport after a concussion. Clinical (e.g. Standardized Assessment for Concussion [SAC], Sport Concussion Assessment Tool [SCAT]) and computer assessments (e.g. ImPACT, Cogstate) for concussion diagnosis and monitoring of concussion symptoms have been developed, but usually only assess mental status as well as cognitive and physical performance.[48-51] In addition, computerized neurocognitive testing can reveal deficits in mental function and processing (such as processing speed and reaction time); however, they may have limited utility if a patient-specific baseline score has not been established prior to injury.[48, 51]
Clinical neurological assessment is recommended to also include measures of sensorimotor, function, coordination, gait, and balance.[36] In a review on neuromuscular control deficits after concussion, divided attention was concluded to be a likely contributing factor to risk of future injury.[40] Alternatively, Eagle et al. postulate a direct perception theory, in which concussion dysregulates a “continuous perception-action coupling loop.”[52] This theory states that a concussion prevents an athlete (or in the current study, a member from the general population) from appropriately perceiving opportunities from physical action in the dynamic environment around them, thus increasing their risk of a new injury.[52] Accordingly, it was recommended that multifactorial assessments are used to assess patients’ readiness for return to play after a concussion.[40]
Concussion symptoms and severity vary between individuals, which confounds diagnosis and determination of physiological recovery.[53] However, it is clear from this study and others[4] that all concussed individuals are at an increased risk of lower extremity injuries, specifically injury to the ACL. Thus, consideration and assessment of neuromuscular control should be incorporated in addition to concussion symptom resolution for all patients, not specifically just athletes, who desire to return to activity. For example, clinical evaluations could incorporate a divided-attention component to a task (e.g. gait analysis, drop vertical jump) to assess neuromuscular control after a concussion.[40, 54, 55]
Research on athletes has highlighted post-concussive symptoms and changes in gait, balance, and biomechanics in athletic tasks.[40, 54, 56-59] Moreover, the current study will facilitate improved understanding of the epidemiological repercussions of mTBI beyond cognitive performance. Elite athletes, trainers, coaches, physicians and now parents, weekend-warriors, and laborers should take precautions in return-to-activity with the understanding that they are at increased risk for a major lower extremity musculoskeletal injury after concussion. Based on the current and previous evidence of increased risk of musculoskeletal injury after concussion, clinical assessments should consider concussion symptom resolution as well as neuromuscular risk factors associated with lower extremity musculoskeletal injuries and specifically acute ACL injuries. However, future research into appropriate screening and assessment of neuromuscular risk factors for ACL injury following a concussion is necessary to better understand the underlying cause of increased ACL injury risk.
The current study is not without limitations. First and foremost, while the REP database is comprehensive in its coverage of individuals within the defined geographic boundaries, the data is only as good as what is charted. While the diagnosis of ACL either by clinical exam, MRI imaging, or operative reports is reliable within the time frame of our study, the same cannot be said about concussion diagnosis. Awareness of concussion among the public, and the ability and willingness of clinicians to specifically diagnose it within the medical record, is unmeasurable and thus could be severely under reported–especially in cases of mTBI. In addition, concussion diagnosis was not standardized (e.g. a validated checklist). Clinical diagnosis by a doctor followed guidelines recommended from the appropriate consensus statement for concussion in sport.[36] Also, the current study did not match ACL cases by body mass index, activity level, or activity exposure as it was not contained within the medical record. This information could alter the perceived odds of sustaining an ACL injury after concussion, likely with an odds increase for higher body mass index, activity level, and athletic exposures. However, age is a surrogate for activity level as older individuals are less likely to be involved in competitive athletics and are typically more sedentary.[33] In addition, mechanism of ACL injury could not be included in analysis, as it was not reliably documented in the medical records. Consideration of ACL injury mechanism (contact vs. non-contact) may provide additional insight into how concussion affects ACL injury risk. Finally, the study could not account for previous injury or concussion sustained by individuals that was not documented in the REP and medical records.
5. Summary and Conclusions
In conclusion, in a geographical population the current study reported that all individuals have increased odds (1.6) of an ACL injury within three years post-concussion. While activity exposure or activity level after concussion could not be accounted for in the current study, the results of this study with a large sample size support the existing literature and further confirm an increased risk of musculoskeletal injury after a concussion.
Key Points:
This is the first study to identify increased odds of specifically an ACL injury within the three years following a concussion in a geographically-representative population. Increased risk of lower extremity musculoskeletal injuries after a concussion has previously been established in specific groups of athletes.
Clinicians should incorporate neuromuscular assessments as part of return-to-activity from a concussion for all patients, not just athletes.
Acknowledgments
Funding: Fellowship funding was provided by the Mayo Clinic Graduate School of Biomedical Sciences [ALM]. Funding for this research was received from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (R01AR55563 [TEH] and L30AR070273 [NDS]) and the National Institute of Children and Human Development (K12HD065987 [NDS]). This study was also made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under award R01AG034676.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Ethical Approval: Institutional review board approval was obtained from both the Mayo Clinic (IRB# 18-001196) and the Olmsted Medical Center (005-OMC-18) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with human participants performed by any of the authors. All patients provided general research authorization for use of their medical records at the time of medical care. All authors have no conflicts of interest to declare.
References
- 1.Faul M, Wald MM, Xu L, Coronado VG. Traumatic brain injury in the United States; emergency department visits, hospitalizations, and deaths, 2002-2006. 2010. [Google Scholar]
- 2.Taylor CA, Bell JM, Breiding MJ, Xu L. Traumatic Brain Injury-Related Emergency Department Visits, Hospitalizations, and Deaths - United States, 2007 and 2013. MMWR Surveill Summ. 2017. March 17;66(9):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Langlois JA, Rutland-Brown W, Wald MM. The epidemiology and impact of traumatic brain injury: a brief overview. The Journal of head trauma rehabilitation. 2006;21(5):375–8. [DOI] [PubMed] [Google Scholar]
- 4.McPherson AL, Nagai T, Webster KE, Hewett TE. Musculoskeletal Injury Risk After Sport-Related Concussion: A Systematic Review and Meta-analysis. Am J Sports Med. 2018. August 3:363546518785901. [DOI] [PubMed] [Google Scholar]
- 5.Kardouni JR, Shing TL, McKinnon CJ, Scofield DE, Proctor SP. Risk for lower extremity injury after concussion: a matched cohort study in soldiers. journal of orthopaedic & sports physical therapy. 2018;48(7):533–40. [DOI] [PubMed] [Google Scholar]
- 6.Reneker JC, Babl R, Flowers MM. History of concussion and risk of subsequent injury in athletes and service members: A systematic review and meta-analysis. Musculoskelet Sci Pract. 2019. July;42:173–85. [DOI] [PubMed] [Google Scholar]
- 7.Baumeister J, Reinecke K, Weiss M. Changed cortical activity after anterior cruciate ligament reconstruction in a joint position paradigm: an EEG study. Scandinavian journal of medicine & science in sports. 2008;18(4):473–84. [DOI] [PubMed] [Google Scholar]
- 8.Borotikar BS, Newcomer R, Koppes R, McLean SG. Combined effects of fatigue and decision making on female lower limb landing postures: central and peripheral contributions to ACL injury risk. Clinical biomechanics. 2008;23(1):81–92. [DOI] [PubMed] [Google Scholar]
- 9.DeAngelis A, Needle A, Kaminski T, Royer T, Knight C, Swanik C. An acoustic startle alters knee joint stiffness and neuromuscular control. Scandinavian journal of medicine & science in sports. 2015;25(4):509–16. [DOI] [PubMed] [Google Scholar]
- 10.DeMont RG, Lephart SM, Giraldo JL, Swanik CB, Fu FH. Muscle preactivity of anterior cruciate ligament-deficient and-reconstructed females during functional activities. Journal of athletic training. 1999;34(2):115. [PMC free article] [PubMed] [Google Scholar]
- 11.Hewett TE, Ford KR, Myer GD. Anterior cruciate ligament injuries in female athletes: Part 2, a meta-analysis of neuromuscular interventions aimed at injury prevention. The American journal of sports medicine. 2006;34(3):490–8. [DOI] [PubMed] [Google Scholar]
- 12.Hewett TE, Myer GD, Ford KR. Anterior cruciate ligament injuries in female athletes: Part 1, mechanisms and risk factors. The American journal of sports medicine. 2006;34(2):299–311. [DOI] [PubMed] [Google Scholar]
- 13.Swanik CB. Brains and sprains: the brain's role in noncontact anterior cruciate ligament injuries. Journal of athletic training. 2015;50(10):1100–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swanik CB, Covassin T, Stearne DJ, Schatz P. The relationship between neurocognitive function and noncontact anterior cruciate ligament injuries. The American journal of sports medicine. 2007;35(6):943–8. [DOI] [PubMed] [Google Scholar]
- 15.Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. The American journal of sports medicine. 2007;35(3):368–73. [DOI] [PubMed] [Google Scholar]
- 16.Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr., et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med. 2014. October;42(10):2363–70. [DOI] [PubMed] [Google Scholar]
- 17.Herzog MM, Marshall SW, Lund JL, Pate V, Spang JT. Cost of Outpatient Arthroscopic Anterior Cruciate Ligament Reconstruction Among Commercially Insured Patients in the United States, 2005-2013. Orthop J Sports Med. 2017. January;5(1):2325967116684776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tator CH. Concussions and their consequences: current diagnosis, management and prevention. CMAJ. 2013. August 6;185(11):975–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brooks MA, Peterson K, Biese K, Sanfilippo J, Heiderscheit BC, Bell DR. Concussion increases odds of sustaining a lower extremity musculoskeletal injury after return to play among collegiate athletes. The American journal of sports medicine. 2016;44(3):742–7. [DOI] [PubMed] [Google Scholar]
- 20.Burman E, Lysholm J, Shahim P, Malm C, Tegner Y. Concussed athletes are more prone to injury both before and after their index concussion: a data base analysis of 699 concussed contact sports athletes. BMJ open sport & exercise medicine. 2016;2(1):e000092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cross M, Kemp S, Smith A, Trewartha G, Stokes K. Professional Rugby Union players have a 60% greater risk of time loss injury after concussion: a 2-season prospective study of clinical outcomes. Br J Sports Med. 2016;50(15):926–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fino PC, Becker LN, Fino NF, Griesemer B, Goforth M, Brolinson PG. Effects of Recent Concussion and Injury History on Instantaneous Relative Risk of Lower Extremity Injury in Division I Collegiate Athletes. Clinical journal of sport medicine: official journal of the Canadian Academy of Sport Medicine. 2017. [DOI] [PubMed] [Google Scholar]
- 23.Herman DC, Jones D, Harrison A, Moser M, Tillman S, Farmer K, et al. Concussion may increase the risk of subsequent lower extremity musculoskeletal injury in collegiate athletes. Sports medicine. 2017;47(5):1003–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lynall RC, Mauntel TC, Padua DA, Mihalik JP. Acute lower extremity injury rates increase after concussion in college athletes. Med Sci Sports Exerc. 2015;47(12):2487–92. [DOI] [PubMed] [Google Scholar]
- 25.Lynall RC, Mauntel TC, Pohlig RT, Kerr ZY, Dompier TP, Hall EE, et al. Lower extremity musculoskeletal injury risk after concussion recovery in high school athletes. Journal of athletic training. 2017;52(11):1028–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Makdissi M, McCrory P, Ugoni A, Darby D, Brukner P. A prospective study of postconcussive outcomes after return to play in Australian football. The American journal of sports medicine. 2009;37(5):877–83. [DOI] [PubMed] [Google Scholar]
- 27.Nordstrom A, Nordstrom P, Ekstrand J. Sports-related concussion increases the risk of subsequent injury by about 50% in elite male football players. Br J Sports Med. 2014;48(19):1447–50. [DOI] [PubMed] [Google Scholar]
- 28.Nyberg G, Mossberg KH, Tegner Y, Lysholm J. Subsequent traumatic injuries after a concussion in elite ice hockey: a study over 28 years. Current Research: Concussion. 2015;2(3):109–12. [Google Scholar]
- 29.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012. February;87(2):151–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ, 3rd. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012. December;87(12):1202–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ 3rd, Pankratz JJ, Brue SM, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012. December;41(6):1614–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, 3rd, Rocca WA. Use of a medical records linkage system to enumerate a dynamic population over time: the Rochester epidemiology project. Am J Epidemiol. 2011. May 1;173(9):1059–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schilaty ND, Nagelli C, Bates NA, Sanders TL, Krych AJ, Stuart MJ, et al. Incidence of Second Anterior Cruciate Ligament Tears and Identification of Associated Risk Factors From 2001 to 2010 Using a Geographic Database. Orthop J Sports Med. 2017. August;5(8):2325967117724196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schilaty ND, Bates NA, Sanders TL, Krych AJ, Stuart MJ, Hewett TE. Incidence of Second Anterior Cruciate Ligament Tears (1990-2000) and Associated Factors in a Specific Geographic Locale. Am J Sports Med. 2017. June;45(7):1567–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hennessy S, Bilker WB, Berlin JA, Strom BL. Factors influencing the optimal control-to-case ratio in matched case-control studies. Am J Epidemiol. 1999. January 15;149(2):195–7. [DOI] [PubMed] [Google Scholar]
- 36.McCrory P, Meeuwisse W, Dvorak J, Aubry M, Bailes J, Broglio S, et al. Consensus statement on concussion in sport-the 5(th) international conference on concussion in sport held in Berlin, October 2016. Br J Sports Med. 2017. June;51(11):838–47. [DOI] [PubMed] [Google Scholar]
- 37.Boden BP, Sheehan FT, Torg JS, Hewett TE. Non-contact ACL injuries: mechanisms and risk factors. The Journal of the American Academy of Orthopaedic Surgeons. 2010;18(9):520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Griffin LY, Agel J, Albohm MJ, Arendt EA, Dick RW, Garrett WE, et al. Noncontact anterior cruciate ligament injuries: risk factors and prevention strategies. J Am Acad Orthop Surg. 2000. May-Jun;8(3):141–50. [DOI] [PubMed] [Google Scholar]
- 39.Ingersoll CD, Grindstaff TL, Pietrosimone BG, Hart JM. Neuromuscular consequences of anterior cruciate ligament injury. Clin Sports Med. 2008. July;27(3):383–404, vii. [DOI] [PubMed] [Google Scholar]
- 40.Howell DR, Lynall RC, Buckley TA, Herman DC. Neuromuscular Control Deficits and the Risk of Subsequent Injury after a Concussion: A Scoping Review. Sports Med. 2018. May;48(5):1097–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Asplund CA, McKeag DB, Olsen CH. Sport-related concussion: factors associated with prolonged return to play. Clinical Journal of Sport Medicine. 2004;14(6):339–43. [DOI] [PubMed] [Google Scholar]
- 42.Cantu RC. Posttraumatic retrograde and anterograde amnesia: pathophysiology and implications in grading and safe return to play. Journal of athletic training. 2001;36(3):244. [PMC free article] [PubMed] [Google Scholar]
- 43.Cantu RC. Return to play guidelines after a head injury. Clinics in sports medicine. 1998;17(1):45–60. [DOI] [PubMed] [Google Scholar]
- 44.Collins M, Lovell MR, Iverson GL, Ide T, Maroon J. Examining concussion rates and return to play in high school football players wearing newer helmet technology: a three-year prospective cohort study. Neurosurgery. 2006;58(2):275–86. [DOI] [PubMed] [Google Scholar]
- 45.Lovell M, Collins M, Bradley J. Return to play following sports-related concussion. Clinics in sports medicine. 2004;23(3):421–41. [DOI] [PubMed] [Google Scholar]
- 46.Sye G, Sullivan SJ, McCrory P. High school rugby players’ understanding of concussion and return to play guidelines. British journal of sports medicine. 2006;40(12):1003–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wasserman EB, Kerr ZY, Zuckerman SL, Covassin T. Epidemiology of sports-related concussions in National Collegiate Athletic Association athletes from 2009-2010 to 2013-2014: symptom prevalence, symptom resolution time, and return-to-play time. The American journal of sports medicine. 2016;44(1):226–33. [DOI] [PubMed] [Google Scholar]
- 48.Meehan WP 3rd, d'Hemecourt P, Collins CL, Taylor AM, Comstock RD. Computerized neurocognitive testing for the management of sport-related concussions. Pediatrics. 2012. January;129(1):38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Echemendia RJ, Meeuwisse W, McCrory P, Davis GA, Putukian M, Leddy J, et al. The Sport Concussion Assessment Tool 5th Edition (SCAT5): Background and rationale. Br J Sports Med. 2017. June;51(11):848–50. [DOI] [PubMed] [Google Scholar]
- 50.McCrea M Standardized Mental Status Testing on the Sideline After Sport-Related Concussion. J Athl Train. 2001. September;36(3):274–9. [PMC free article] [PubMed] [Google Scholar]
- 51.Farnsworth JL 2nd, Dargo L, Ragan BG, Kang M. Reliability of Computerized Neurocognitive Tests for Concussion Assessment: A Meta-Analysis. J Athl Train. 2017. September;52(9):826–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Eagle SR, Kontos AP, Pepping GJ, Johnson CD, Sinnott A, LaGoy A, et al. Increased Risk of Musculoskeletal Injury Following Sport-Related Concussion: A Perception-Action Coupling Approach. Sports Med. 2019. June 21. [DOI] [PubMed] [Google Scholar]
- 53.Kamins J, Bigler E, Covassin T, Henry L, Kemp S, Leddy JJ, et al. What is the physiological time to recovery after concussion? A systematic review. Br J Sports Med. 2017. June;51(12):935–40. [DOI] [PubMed] [Google Scholar]
- 54.Howell DR, Buckley TA, Lynall RC, Meehan WP 3rd. Worsening Dual-Task Gait Costs after Concussion and their Association with Subsequent Sport-Related Injury. J Neurotrauma. 2018. July 15;35(14):1630–6. [DOI] [PubMed] [Google Scholar]
- 55.Register-Mihalik JK, Littleton AC, Guskiewicz KM. Are divided attention tasks useful in the assessment and management of sport-related concussion? Neuropsychol Rev. 2013. December;23(4):300–13. [DOI] [PubMed] [Google Scholar]
- 56.Dubose DF, Herman DC, Jones DL, Tillman SM, Clugston JR, Pass A, et al. Lower Extremity Stiffness Changes after Concussion in Collegiate Football Players. Med Sci Sports Exerc. 2017. January;49(1):167–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Howell DR, Myer GD, Grooms D, Diekfuss J, Yuan W, Meehan WP, 3rd. Examining Motor Tasks of Differing Complexity After Concussion in Adolescents. Arch Phys Med Rehabil. 2018. September 5. [DOI] [PubMed] [Google Scholar]
- 58.Lynall RC, Blackburn JT, Guskiewicz KM, Marshall SW, Plummer P, Mihalik JP. Functional balance assessment in recreational college-aged individuals with a concussion history. J Sci Med Sport. 2018. November 6. [DOI] [PubMed] [Google Scholar]
- 59.Murray NG, Szekely B, Moran R, Ryan G, Powell D, Munkasy BA, et al. Concussion history associated with increased postural control deficits after subsequent injury. Physiol Meas. 2019. February 20;40(2):024001. [DOI] [PubMed] [Google Scholar]