1. Introduction
Exposure to poor socioeconomic conditions during childhood is a well-known risk for adult morbidity and mortality (Cohen et al., 2010; Taylor, 2010). One explanation for the social inequities in health is that children from impoverished backgrounds experience more cumulative and severe stressors, which take a toll on the body’s physiological systems (Brotman et al., 2007; Evans & Kim, 2010). Indeed, low-income children show signs of cardiovascular reactivity, such as elevated levels of arterial blood pressure and prehypertension (Evans & Kim, 2012; Lehman et al., 2009).
The family stress model is a useful conceptual framework with which to understand the mechanisms that link economic hardship to health (Conger & Conger, 2008). The family stress model asserts that poverty-related adversity contributes to children’s poor health by way of family conflict, harsh parent-child relations, and parent psychological distress (Conger & Donnellan, 2007). We apply the family stress model in the present study to examine the extent to which socioeconomic hardship in childhood leads to hypertension in young adulthood by means of across-time changes in family conflict, anxiety-depression, and high body mass. Each of these pathways is described below.
1.1. Socioeconomic Hardship, Family Conflict, and Poor Cardiovascular Health
Financial strain and economic insecurity are strongly associated with family tension and conflict (Kavanaugh et al., 2018; Neppl et al., 2016). Stressful family relations, as well as conflictual parent-child relations, have been linked directly with children’s high blood pressure and pre-hypertension (Clark & Armstead, 2000; Mak et al., 2019; Su et al., 2015). Family tensions derived from economic insecurity also relate to elevated levels of inflammation (Schreier et al., 2014), cortisol (Brown et al., 2019), and other neuroendocrine stress hormones in children (Brody et al., 2013; Taylor, 2010) -- all of which can contribute to high blood pressure (Pickering, 2007). Parental unemployment and job insecurity and their resultant income instability are also associated with family stress and conflict and children’s health problems (e.g., Hill et al., 2013; Schaller & Zerpa, 2019). The environmental aspects of poverty (substandard housing, crowding) are also stressful for children (Evans, 2004), with children exposed to such stressors experiencing frequent family conflict and elevated blood pressure (Evans & Kim, 2012). A chaotic home environment, or household disorganization and unpredictability which are more likely to occur in low-income families, also has been highlighted as mediating the link between poverty and children’s poor health (Brown et al., 2019; Evans et al., 2005; Schreier et al., 2014).
1.2. Socioeconomic Hardship, Psychological Distress, and Poor Cardiovascular Health
Psychological factors have been widely studied as mediating the socioeconomic-health connection in children (Miller et al., 2011) and adults (Cohen et al., 2007; Matthews & Gallo, 2011). Indeed, the chronic stress of living in poverty during childhood and adolescence can lead to anxiety and depression, which increase physiological arousal and can contribute to hypertension and cardiovascular disease in adulthood (Doom et al., 2016, 2017; Kavanaugh et al., 2018). Sustained elevated anxiety resulting from economic insecurity has been shown to disrupt bodily regulatory systems, altering the immune, metabolic, neuroendocrine, and autonomic nervous systems (Pickering, 2007; Suglia et al., 2018). When continued over time, such responses can lead to elevated blood pressure and hypertension (Spruill, 2010). Using a large longitudinal sample, Lehman et al. (2009) found that low socioeconomic status during childhood led to high blood pressure in adulthood through pathways of heightened anxiety and depression. Using the same sample, low childhood social class predicted a harsh and risky family environment, which led to poor cardiovascular health in adulthood by its effect on individuals’ depression and anger (Loucks et al., 2011). Evans and colleagues also found that low family income-to-needs ratio contributed to both children’s internalizing problems and high blood pressure (Evans & Cassells, 2014).
1.3. Socioeconomic Hardship, Overweight/Obesity, and Poor Cardiovascular Health
Children from low socioeconomic backgrounds are more likely to be overweight or obese (Lee et al., 2014; McLaren, 2007), which are known risks for high blood pressure (Lo et al., 2014). The most widely cited mechanism linking socioeconomic adversity to obesity is the body’s physiological reactions to stress, such that elevated cortisol levels and chronic arousal of the hypothalamic-pituitary-adrenal (HPA) axis lead to disruption in metabolic functioning resulting in overweight (Gundersen et al., 2010). Children with obesity are at an approximate 3-fold higher risk for hypertension than children without obesity, and risk of hypertension increases across the entire range of body mass and is not defined by a simple threshold effect (Sorof & Daniels, 2002). Studies support these links and have found that youth exposed to many cumulative economic stressors have both a high body mass and elevated blood pressure (Brody et al., 2013; Evans & Kim, 2012). General family stress and family financial strain also have been found to relate directly to childhood overweight and obesity (Garasky et al., 2009; Halliday et al., 2014).
1.4. The Present Study and Hypotheses
Drawing from the family stress model (Conger & Conger, 2008), we hypothesize that socioeconomic hardship during childhood will lead to hypertension in young adulthood by way of three central mediators: family conflict, anxiety-depression, and high body mass. We also incorporate Bronfenbrenner’s bioecological systems theory to clarify the ordering of relations among these variables (Bronfenbrenner & Morris, 2006). The bioecological framework contends that processes occur across successive layers of the environment – ranging from distal environmental factors to proximal social processes to individual socioemotional and physiological functioning - with each system or layer trickling down to affect health (McLaren & Hawe, 2005). We apply this framework to hypothesize that childhood socioeconomic hardship will contribute to family conflict, which will lead to anxiety-depression, which will contribute to high body mass, which will lead to hypertension. A large literature supports the link between family conflict and children’s psychological distress (e.g., Spies et al., 2011), and a recent literature review indicated robust relations between children’s psychological distress and obesity (Gundersen et al., 2011). Additionally, results of a meta-analysis showed that, among those 20 years of age and younger, depression was consistently related to subsequent overweight/obesity, while overweight/obesity was not related to subsequent depression (Luppino et al., 2010).
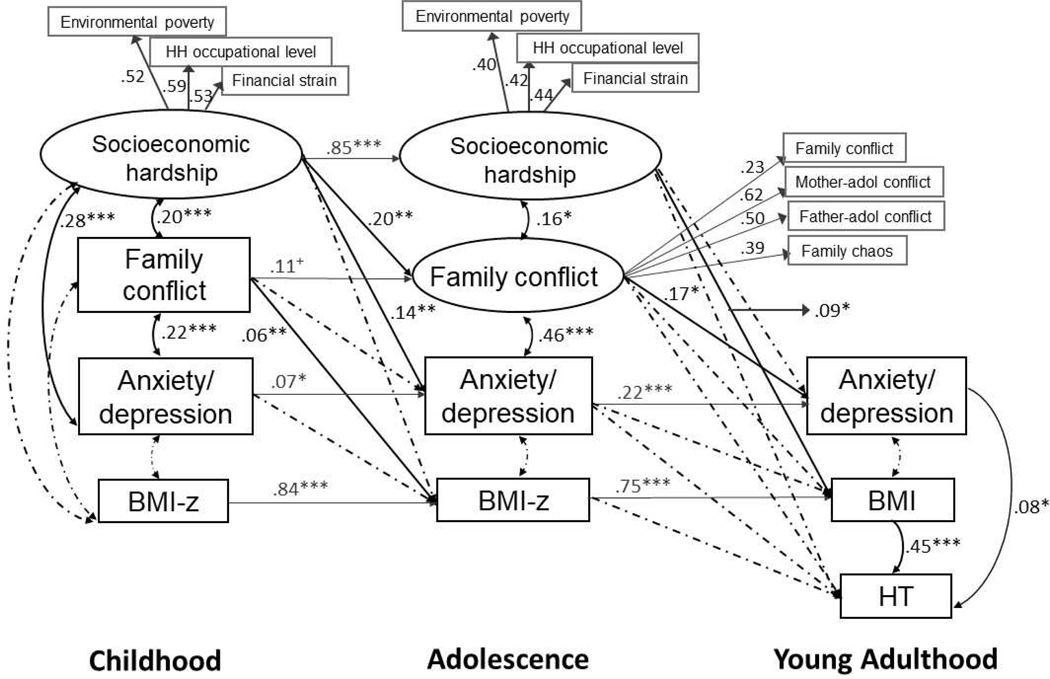
We use data from a longitudinal sample that had repeated measures of socioeconomic hardship and each mediator, allowing for tests of the hypothesized pathways across time (Figure 1). For example, we examine how socioeconomic hardship during childhood relates to family conflict in adolescence, which relates to anxiety-depression in young adulthood, which contributes to hypertension. We also test the extent to which socioeconomic hardship in childhood relates directly to anxiety-depression in adolescence and, separately, to body mass in adolescence, with each in turn, leading to hypertension in young adulthood.
Figure 1.
Model of the across-time associations among socioeconomic hardship, family conflict, anxiety-depression, body mass index (BMI), and hypertension (HT). Standardized coefficients are shown. Nonsignificant paths (shown as dashed lines) were included in the model. Within-time paths at adolescence were included but are not shown for sake of clarity; those not shown were nonsignificant. Model fit was: χ2 (156) = 340.53, CFI = .942, RMSEA = .034, SRMR = .038. N = 1,039. Analyses adjusted for sex, age, parent history of HT, and smoking status at young adulthood. +P < .06. *P < .05. **P < .01. ***P < .001.
2. Methods
2.1. Sample and Study Design
Data were from 1,039 participants of the Santiago Longitudinal Study (SLS) who were studied at childhood (M age 10 years), adolescence (M age = 15.6 years), and young adulthood (M age = 23.0 years). The SLS initially involved 1,790 Chilean infants who participated in a randomized-controlled iron-deficiency anemia preventive trial or neuromaturation study (Lozoff et al., 2003). Infants were recruited at 6 months (1991–1996) from community clinics serving predominantly working-class, low-to-middle income families. Eligible infants were healthy, full-term, singletons with birth weight ≥ 3.0 kg. At child age 10 and at adolescence, children’s mothers completed measures of family economic hardship and family conflict and, at child age 10, their child’s anxiety-depressive symptoms (Table 1). Assessments were completed at the Institute of Nutrition and Food Technology (INTA) at the University of Chile. At adolescence, children completed measures of their family dynamics, conflict with parents, and their anxiety-depressive symptoms. At young adulthood, participants completed a measure of their anxiety-depression, and blood pressure was measured in 1,039 participants. Analyses focused on these 1,039 participants. Height and weight were measured at each study time point.
Table 1.
Sample characteristics and descriptive statistics of study measures
| n | Mean or % | SD | Range | Rater | |
|---|---|---|---|---|---|
| Background characteristics | |||||
| †Sex (% female) | 1039 | 52% | Mother | ||
| Father education (years) | 1039 | 9.7 | 2.8 | 0 – 19 | Mother |
| Mother education (years) | 1039 | 9.5 | 2.7 | 1 – 17 | Mother |
| Father employed | 1039 | 93% | Mother | ||
| Childhood assessment | |||||
| †Age (years) | 969 | 10.0 | 0.1 | 10.0 – 10.7 | Mother |
| Environmental povertya | 882 | 15.1 | 4.7 | 6 – 41 | Mother |
| HH occupational level, stabilityb | 882 | 3.8 | 0.7 | 1 – 6 | Mother |
| Family financial strain | 875 | 2.0 | 1.4 | 0 – 4 | Mother |
| Family conflict | 875 | 0.6 | 0.8 | 0 – 5 | Mother |
| Anxiety-depression | 879 | 7.9 | 4.6 | 0 – 26 | Mother |
| BMI (kg/m2) | 877 | 19.4 | 3.3 | 13 – 34 | RNc |
| BMI-z score | 877 | 1.0 | 1.1 | −2.0 – 4.0 | |
| Adolescent assessment | |||||
| †Age (years) | 970 | 15.6 | 0.8 | 14 – 17 | Participant |
| Environmental povertya | 895 | 14.7 | 4.3 | 6 – 41 | Mother |
| HH occupational level, stabilityb | 895 | 3.8 | 0.7 | 1 – 6 | Mother |
| Family financial strain | 779 | 1.5 | 1.1 | 0 – 3 | Mother |
| Family conflict | 779 | 0.6 | 0.8 | 0 – 5 | Mother |
| Family chaos | 824 | 4.3 | 2.9 | 0 – 15 | Participant |
| Mother-adolescent conflict | 921 | 13.5 | 3.6 | 8 – 32 | Participant |
| Father-adolescent conflict | 839 | 12.2 | 3.5 | 8 – 32 | Participant |
| Anxiety-depression | 885 | 6.2 | 3.8 | 0 – 26 | Participant |
| BMI (kg/m2) | 971 | 23.0 | 4.3 | 14 – 45 | RNc |
| BMI-z score | 971 | 0.6 | 1.0 | −3.0 – 4.0 | |
| Young adulthood assessment | |||||
| †Age (years) | 1039 | 23.0 | 1.0 | 21 – 26 | Participant |
| †Parent hx HT | 870 | 48.3% | Participant | ||
| †Current smoker | 1038 | 42% | Participant | ||
| Anxiety-depression | 812 | 10.0 | 5.5 | 0 – 24 | Participant |
| BMI (kg/m2) | 1039 | 26.8 | 5.7 | 17 – 59 | RNc |
| Systolic BP (mmHg) | 1039 | 111.1 | 11.2 | 80 – 155 | RNc |
| Diastolic BP (mmHg) | 1039 | 69.0 | 7.5 | 50 – 100 | RNc |
| Normal BP | 768 | 73.9% | |||
| Elevated BP | 116 | 11.2% | |||
| HT stage 1 | 129 | 12.4% | |||
| HT stage 2 | 26 | 2.5% |
Note.
Denotes a covariate.
Higher scores reflect more impoverished living conditions.
Higher scores indicate lower occupational status and stability of household head.
RN = assessed by a research staff nurse. BMI = body mass index. HT = hypertension. BP = blood pressure.
All 1,790 children who participated at infancy were invited to participate at all subsequent study time points regardless of whether they missed an earlier assessment.
Individuals included in the current analyses were similar to those lost to follow-up in background characteristics (age, family size, environmental poverty, parent education, mother’s age at child’s birth, and body mass at all time points). However, those studied here were more likely to be female, to have lower levels of family conflict and anxiety-depression at adolescence, and less likely to have received iron supplementation as part of the infancy preventive trial (see Supplemental Table 1). (A flow chart of sample follow-up is shown in Supplemental Figure 1.) Approval for this study was obtained from the authors’ university Institutional Review Boards in the U.S. and Chile. Informed written consent was obtained from children’s parents at the age 10 and adolescent assessments; participants provided their own assent at childhood and adolescence and written informed consent at young adulthood. All study procedures were in accord with the Code of Ethics of the World Medical Association (World Medical Association, 2013).
2.2. Measures
Socioeconomic hardship
Environmental poverty.
Impoverished living conditions were indexed using the Graffar social class instrument, a measure of poverty often used in developing countries (Graffar, 1956). Six questions ask about the family’s living conditions (quality of house construction, crowding, access to an indoor kitchen, running water, indoor bathroom, frequency of garbage pickup), coded as 1 (optimal) to 6 (poor quality). The Graffar also asks about the family’s possession of five major commodities (refrigerator, washing machine, car, etc.), coded as 0 (present) or 1 (absent). The living condition score and possession count score were summed for a possible score range of 6 to 41, with higher scores indicating greater environmental poverty. Mothers completed identical versions of the Graffar when their child was age 10 and in adolescence.
Household head occupational level and stability.
The Graffar also asks about the household head’s occupational level and stability. Options ranged from professional, administrative, stable skilled, stable semi-skilled, sporadic unskilled, to unemployed, coded as 1 to 6, respectively, with higher scores indicating less skilled and less stable occupations.
Financial strain.
Mother ratings on the Social Readjustment Rating Scale (Holmes & Rahe, 1967) were used to assess family financial strain (4 items at child age 10, e.g., “the family has had . . . serious debts,” “serious financial hardship,” and 3 items at child’s adolescence, e.g., “the family has had . . . serious debts,” “experienced major or constant financial hardship ”). Items were coded as 0 (not present) or 1 (present) within the past year and summed, with higher scores indicating greater financial strain.
Family conflict
Family conflict.
Mother ratings on five items of the Social Readjustment Rating Scale (Holmes & Rahe, 1967) were used to assess family conflict (e.g., “serious family conflict,” “serious spousal conflict”). Items were coded as 0 (not present) or 1 (present) within the past year and summed, with higher scores indicating greater family conflict (range: 0 – 5). Identical items were analyzed at the childhood and adolescent time points.
Parent-adolescent conflict.
At adolescence, youth completed questions about the conflict in their relationships with their parents (8 items for mother, 8 for father) (e.g., “How often does your mother/father shout or yell at you?,” “insult or swear at you?”) (Ho et al., 2013). Response options ranged from 1 (never) to 4 (always). Cronbach’s coefficient alpha was .80 for items pertaining to mothers and .79 for items pertaining to fathers.
Family chaos.
At adolescence, youth completed the Chaos, Hubbub, and Order Scale (CHAOS), which involves 15 true/false statements (coded 1/0) measuring disorganization and confusion in the home (“It’s a real zoo in our home,” “It’s so noisy, you can’t hear yourself think in our home”) (Matheny et al., 1995). Items were summed, with higher scores reflecting a more chaotic home environment. Cronbach’s alpha of items within the study sample was .76.
Anxiety-depression.
Mothers completed the Spanish version of the Child Behavior Checklist (CBCL) when their child was 10 years old, of which 13 items assess children’s anxiety and depressive symptoms within the past 6 months (my child. . . “worries,” “is fearful,” “is nervous,” “is sad”) (Achenbach & Ruffle, 2000). Response options were 0 (never), 1 (somewhat or sometimes true), and 2 (very true or often true). At adolescence, youth completed the Youth Self Report (YSR; Achenbach, 1991) version of the CBCL, which has the identical items as the CBCL. At young adulthood, participants completed the Adult Self Report (ASR) version of the CBCL, which has 12 anxiety-depression items identical to those on the CBCL and YSR (Achenbach & Rescorla, 2003). Cronbach’s alphas were: .73 for the CBCL, .74 for the YSR, and .88 for the ASR.
Body mass index (BMI).
At each time point, participants’ lightly-clothed weight was measured by a research nurse at INTA to the neared 0.1 kg using a Seca scale. Height was measured to the nearest 0.1 cm, using a Holtain stadiometer. Two height and weight measures were taken, with a third measurement taken if the difference between the first two exceeded 0.3 kg for weight or 0.5 cm for height. At childhood and adolescence, measurements were converted to body mass index (BMI) z scores using the World Health Organization standards. At young adulthood, BMI was calculated from weight and height (kg/m2) and used for analyses.
Blood pressure, Hypertension (HT).
After 15 min at rest, systolic and diastolic blood pressures (SBP, DBP) were measured three times on the non-dominant arm using a standard mercury sphygmomanometer by trained clinical staff. The first measurement was discarded and the second two were averaged for analysis. Blood pressure (BP) was classified using the recent adult guidelines for systolic and diastolic BP (Whelton et al., 2018) as: normotensive: <120 mm Hg and < 80 mm Hg; elevated: 120–129 mm Hg and < 80 mm Hg; HT Stage 1: 130–139 mm Hg or 80–89 mm Hg; or HT Stage 2: > 140 mm Hg or ≥ 90 mm Hg. These categories were coded for analysis as: 0 (normal BP), 1 (elevated BP), 2 (HT stage 1), and 3 (HT stage 2).
2.3. Covariate Selection
The following were considered as covariates: participants’ sex (male = 1, female = 0), age, smoking status at young adulthood (none [0], occasional [1], regular [2]), parental history of HT (assessed by participant report at young adulthood, yes = 1; no = 0), and receipt of iron supplementation as part of the preventive trial (yes = 1, no = 0). Iron supplementation was not related to any of the model variables and thus, not considered further. All other covariates were retained in analyses.
2.4. Statistical Analysis
We conducted structural equation modeling using Mplus 8.2 to evaluate the pathways shown in Figure 1 (Muthén & Muthén, 2017). We first constructed latent factors within Mplus for select exogenous variables. A latent variable for socioeconomic hardship (at both childhood and adolescence) was indicated by scores of environmental poverty, household head occupational level and stability, and financial strain. A latent variable of family conflict during adolescence was indexed by four observed variables: mother-ratings of family conflict, and participant ratings of mother-adolescent conflict, father-adolescent conflict, and family chaos. As shown in Figure 1, the model included autoregressive paths and within-time correlations. In this case, the autoregressive paths function as a control for the across-time paths; such that, once the portion of variance at adolescence is shared with the variance of the childhood measure, the variance that remains is change from childhood to adolescence. Thus, a significant across-time path when autoregressive paths between repeated measures are included can be interpreted as the childhood predictor relating to change in the endogenous variable from childhood to adolescence. This approach strengthens inferences about the temporal and causal relations between constructs (Little et al., 2015). To rule out the possibility of feedback processes, in preliminary analyses we tested cross-lag relations from BMI to anxiety-depression, and from child anxiety-depression to family conflict at adolescence. All feedback paths were non-significant with small effect estimates (β’s < .03); thus, these paths were dropped from the model.
Model fit was evaluated using well-established guidelines (Kline, 2015) of the comparative fit index (CFI > .90), root mean square error of approximation (RMSEA < .05), and standardized root mean square residual (SRMR < .08). Analyses were conducted using maximum likelihood estimators, which are robust to non-normality. All cases were retained (N = 1,039) using the full information maximum likelihood method (FIML), which fits the model being tested directly onto the non-missing data for each participant (Muthén & Muthén, 2017) and has been shown to be superior to other missing data strategies (Raykov, 2005). Mediation was tested using the INDIRECT command within Mplus, which estimates indirect effects using the delta method of standard errors (Muthén, 2011). In line with recommendations by Selig and Preacher (2009) and others (Cole & Maxwell, 2003), we present the total indirect effects of each exogenous variable on hypertension. Total indirect effects are believed to provide valuable information regarding the degree to which an exogenous variable summarily indirectly influences an outcome (Cole & Maxwell, 2003).
3. Results
The mean household head occupational level for the current sample at the childhood assessment was 3.8 (Table 1, range 1 to 6), indicating that the average household head held a stable semi-skilled job (e.g., taxi driver). Environmental poverty was moderate, with most households having a separate kitchen and indoor running water and bathrooms. However, many families lived in small, crowded houses and did not have a car. Financial strain was relatively high, with approximately half of families experiencing significant debt and major or constant financial strain. At the childhood assessment, 40% of household heads were unemployed at some point during the previous year and 52% experienced unstable employment. At the young adult assessment, 11% of participants had elevated blood pressure, and approximately 15% had hypertension (Table 1). Significant associations among the indicators of socioeconomic hardship at childhood and, separately, at adolescence, and among the indicators of family conflict at adolescence indicate that the observed variables were measuring distinct but related aspects of each latent variable. (Correlations among all model variables are shown in Supplemental Table 2).
3.1. Latent Variables
The measurement model had good fit: χ2 (30) = 75.70, CFI = .941, RMSEA = .039, SRMR = .042. The factor loadings for the latent variables ≥ .23 (p < .001) (Figure 1).
3.2. Modeling Results
This study’s analytic model demonstrated good fit (Figure 1). Path coefficients (standardized and unstandardized regression coefficients, β and B, respectively) indicated that socioeconomic hardship in childhood and adolescence related within-time to family conflict (β = .20, B = .36, SE = .09, p <.001 and β = .16, B = .02, SE = .01, p <.05, respectively). Family conflict at both childhood and adolescence related strongly within-time to anxiety-depression (β = .22, B = .75, SE = .14, p <.001 and β = .46, B = .31, SE = .10, p <.001, respectively). Socioeconomic hardship in childhood also related directly to children’s anxiety-depression (β = .28, B = 3.13, SE = .60, p <.001). At young adulthood, both greater anxiety-depression and higher BMI were directly associated with hypertension (β = .08, B = .01, SE = .01, p <.05 and β = .45, B = .06, SE = .01, p <.001, respectively). There were five notable across-time paths: (1,2) socioeconomic hardship in childhood related to increases in family conflict and anxiety-depression at adolescence (β = .20, B = .02, SE = .01, p <.01 and β = .14, B = .21, SE = .08, p <.01, respectively); (3) family conflict in childhood related to increases in BMI at adolescence (β = .06, B = .08, SE = .02, p <.01); (4) socioeconomic hardship in adolescence related to increased BMI from adolescence to young adulthood (β = .09, B = .31, SE = .14, p <.05), and (5) family conflict during adolescence related to increased anxiety-depression from adolescence to young adulthood (β = .17, B = 4.82, SE = 2.26, p <.05). Coefficients for the covariates on hypertension were: age (β = .06, B = .04, SE = .02, p <.05), male sex (β = .27, B = .44, SE = .05, p <.001), parent history of hypertension (β = .06, B = .10, SE = .05, p <.05), and young adult smoking status (β = .001, B = .001, SE = .02, p = .99). The full model accounted for 23.3% of the variance in hypertension severity. It is of note that there were no significant paths from anxiety-depression to BMI at any time point. Post-hoc analyses ruled out the possibility that this null finding was due to a curvilinear relation, given that frequent anxiety and depression can lead to undereating in some individuals but overeating in others (Burke & Storch, 2015).
3.3. Indirect Effects
In this study, we hypothesized that socioeconomic hardship will lead to hypertension by way of family conflict, anxiety-depression, and high body mass. We also hypothesized a specific ordering, such that socioeconomic hardship will contribute to family conflict, which will lead to anxiety-depression, which will contribute to high body mass, which will lead to hypertension. Although the full mediational pathway was not supported by these data, several segments of this pathway reached significance. For example, childhood socioeconomic hardship related to hypertension via adolescent socioeconomic hardship and young adult BMI (Table 2; indirect effect estimate = .036, S.E. = .016). Adolescent socioeconomic hardship had an indirect effect on hypertension via young adult BMI (estimate = .042, S.E. = .018). The pathway from childhood socioeconomic hardship to hypertension as mediated by adolescent and young adult anxiety-depression approached statistical significance (estimate = .002, S.E. = .001). Other mediating pathways involved: childhood family conflict related to hypertension via adolescent and young adult BMI (estimate = .021, S.E. = .007), and childhood BMI related to hypertension via adolescent and young adult BMI (estimate = .281, S.E. = .030). Total indirect effect tests from each exogenous variable to hypertension indicated significant total indirect effects originating from family conflict and BMI in childhood, and from socioeconomic hardship, anxiety-depression and BMI in adolescence (Table 2).
Table 2.
Parameter Estimates of Indirect Effects on Hypertension
| Specific indirect effects | Est. | (SE) | P . |
|---|---|---|---|
| Socioeco hard C → socioeco hard A → BMI YA → HT | .036 | (016) | .025 |
| Socioeco hard A → BMI YA → HT | .042 | (018) | .021 |
| Socioeco hard C → anx-dep A → anx-dep YA → HT | .002 | (001) | .094 |
| Anx-dep A → anx-dep YA → HT | .018 | (.009) | .045 |
| Family conflict C → BMI A → BMI YA → HT | .021 | (.007) | .003 |
| BMI C → BMI A → BMI YA → HT | .281 | (.030) | .001 |
| BMI A → BMI YA → HT | .336 | (.035) | .001 |
| Total indirect effects* | Est. | (SE) | P . |
| Socioeco hard C | .211 | (168) | .209 |
| Family conflict C | .025 | (.009) | .007 |
| Anxiety-depress C | .004 | (.007) | .560 |
| BMI C | .263 | (.050) | .001 |
| Socioeco hard A | .044 | (.018) | .016 |
| Family conflict A | .012 | (021) | .570 |
| Anxiety-depress A | .033 | (.016) | .040 |
| BMI A | .336 | (.035) | .001 |
| Anxiety-depress YA | .012 | (013) | .332 |
| BMI YA | .449† | (.045) | .001 |
Note. Est. = standard estimate. SE = standard error. C = assessed at childhood. A = assessed at adolescence. YA = assessed at young adulthood. BMI = body mass index. HT = hypertension severity score. Socioeco hard = socioeconomic hardship latent variable. Anx-dep = anxiety-depression. Analyses adjusted for sex, age, parental history of hypertension, and young adult smoking status.
Total indirect effects are the sum of all possible indirect effects shown in Figure 1. Each childhood variable adjusted for all other childhood measures and included all possible downstream indirect paths. Each adolescent variable adjusted for all childhood measures, the other adolescent variables, and included all possible downstream paths. The young adult variables adjusted for all childhood and adolescent measures.
This is a direct effect as this variable had only a direct pathway to hypertension.
4. Discussion
Guided by the family stress model and bioecological systems theory, the present study examined how economic adversity in childhood trickles down to affect cardiovascular health in young adulthood. Three central mediators were studied, family conflict, psychological distress, and body mass. Findings indicate that childhood socioeconomic hardship related to hypertension primarily through its influence on increases in psychological distress and BMI over time. Family conflict during childhood also related to hypertension by way of increases in BMI. These and other findings are discussed below.
Socioeconomic hardship was highly stable from childhood to adolescence, with economic disadvantage at adolescence linked to greater increases in BMI from adolescence to young adulthood, which related to hypertension. Normally growing youth typically show decelerated growth during the transition to adulthood, as pubertal influences decline and skeletal growth subsides (Lee et al., 2011). Individuals who had large BMI increases during this transition, however, were at risk of elevated blood pressure and hypertension, likely reflecting the proximal impact of physiological mechanisms associated with high body mass that induce hypertension (e.g., sodium retention, extracellular-fluid volume, etc., Kotsis et al., 2010). Other studies have also shown that excessive and rapid weight gain are risk factors for hypertension (Huang et al., 1998; Masuo et al., 2000). The current results corroborate these earlier findings and point to childhood family economic conditions -- as early as age 10 -- as preceding meaningful BMI increases. These results call attention to the central role of BMI and BMI increase in understanding how childhood poverty relates to subsequent hypertension. This finding also echoes concerns about childhood overweight and obesity becoming increasingly important risk factors for early-onset hypertension, as rates of childhood obesity have recently risen to epidemic proportions (Flynn, 2013; Sorof & Daniels, 2002).
Results also showed that childhood socioeconomic hardship related to anxiety-depression in adolescence, which remained stable into young adulthood and contributed to hypertension. This pathway is consistent with the family stress model and highlights that children are aware of and can be negatively affected by their family’s economic instability (Conger & Conger, 2008). Socioeconomic disadvantage during childhood was strongly related to anxiety and depressive symptoms both in childhood and in adolescence, suggesting its long-lasting effects. A large literature has documented that chronic exposure to high physiological arousal that accompanies psychological distress can be damaging to bodily regulatory systems and lead to stress-related disease (Cohen et al., 2007; Miller et al., 2011 ; Suls & Bunde, 2005). However, several studies finding psychological pathways to hypertension have examined retrospective reports of child maltreatment or other severe forms of adversity (e.g., Su et al., 2015; Suglia et al., 2014, 2018). Current results demonstrate that psychological distress derived from parental job insecurity or family financial strain, for example, can also lead to elevated blood pressure.
Family conflict also had notable effects on hypertension, primarily through increases in BMI and anxiety-depression over time. Thus, the negative effects of childhood family conflict on health might be evident only at later points in development. There were also strong associations between family conflict and anxiety-depression (both within and across time), with anxiety-depression at young adulthood contributing to hypertension. This pathway highlights the integral connections between family functioning and mental and physical health and points to family-level origins of disease (Conger & Conger, 2008). In fact, a recent intervention that strove to strengthen family relationships showed significant reductions in individuals’ inflammation, affirming such associations (Miller et al., 2014).
Finally, support for the full mediation pathway was not found (i.e., from socioeconomic disadvantage to family conflict to anxiety-depression to BMI to hypertension). This might be due to the relatively small magnitude of effect sizes of the individual pathways coupled with the complexity of the model (i.e., sequentially testing two or three mediators). Insignificant indirect effects can occur in spite of significant individual pathways (as was the case in the current analyses) because of low power associated with the test of mediation (MacKinnon et al., 2007). When demands on power were reduced, such as when testing for mediation in segments of the pathway, some significant mediated pathways were found. Nevertheless, considering the absence of significant indirect effects for the full model, as well as the relatively modest effect sizes and the lack of a direct association between anxiety-depression and BMI (cited previously), one must be cautious when making conclusions about the cumulative process as outlined in the full model.
4.1. Limitations and Strengths
Certain study limitations are important for interpreting the findings. This study did not consider several health-related behaviors known to be associated with hypertension, such as physical activity, diet/nutrition, or alcohol consumption (Gee et al., 2012). We also did not analyze biological mediators, such as inflammation, cortisol, or HPA axis functioning (Pickering, 2007; Slopen et al., 2013). The absence of these and other factors known to relate to hypertension limited a more comprehensive understanding of how multiple risk factors interrelate to increase risk of hypertension. Participants in the current sample differed from those not followed up in young adulthood in that they were more likely to be female and had lower levels of family conflict and anxiety-depression at adolescence. We adjusted for sex in the analyses. However, there remains the possibility that processes contributing to hypertension might be different for individuals experiencing less family conflict or psychological distress. Another consideration is that all significant mediated pathways involved a variable measured at the same time as this study’s outcome. It is possible, though perhaps unlikely (Kotsis et al., 2010; Meng et al., 2012), that elevated blood pressure contributes to a higher BMI or higher anxiety-depression. Additionally, it is a study limitation that similar indicators of family conflict available at adolescence were not available at childhood so that across-time change in the latent variable of family conflict could be analyzed. This study also did not have assessments of participants’ family socioeconomic status nor family conflict at young adulthood. Thus, the significant pathways in the model are unadjusted for these variables and potentially confounded by the absence of these controls. In addition, the current sample was primarily low-to-middle class; thus, the relations found may not be generalizable to populations outside this socioeconomic range. Relatedly, the absence of truly impoverished families likely attenuated effects stemming from socioeconomic hardship. However, even within this working-class sample, significant relations were found from socioeconomic hardship to family conflict, anxiety-depression, and a higher body mass.
Study strengths are its use of multiple-wave longitudinal data, the use of parent and child reports in the assessment of study variables, the relatively large sample, good follow-up rates, and the inclusion of important covariates in the analyses, such as smoking status and family history. We also examined multiple aspects of socioeconomic disadvantage and family conflict, which we believe capture well the stressors and strains that arise from living in poverty (Evans, 2004) and are important for adult health (Cohen et al., 2007, 2010). All study participants were healthy as newborns and infants, thus there were no obvious early health problems confounding later health status. Participants’ blood pressure was objectively measured by clinical staff and we analyzed hypertension severity using the recent hypertension guidelines (Whelton, et al., 2018). The focus on hypertension in young adulthood is timely given the recent increased prevalence of pediatric hypertension (Rosner et al., 2013; Sharma et al., 2018) and that elevated blood pressure often only first becomes evident during young adulthood but itself carries significant cardiovascular risks (de Moraes et al., 2014). In addition, gradations in blood pressure levels are clinically significant given that hypertension reliably progresses in severity across time (Redwine & Faulkner, 2012) and risk of cardiovascular disease increases proportionately with rising blood pressure (Lewington et al., 2002).
5. Conclusions
Children from more economically disadvantaged families experienced higher levels of family conflict, which related to significant increases in anxiety-depression and body mass over time, both of which were directly linked to hypertension. Findings provide an understanding of how early-life adversity associated with socioeconomic disadvantage manifests as stress-related health problems in later life. Understanding the developmental pathways that begin in childhood and progress over time may be useful to prevention efforts so that modifiable risks can be targeted and minimized. Findings might facilitate clinical efforts to identify hypertension in children and adolescents and thereby reduce the risk of future cardiovascular events (Shonkoff et al., 2012). Encouraging findings are emerging in which early childhood investments addressing family relationships, good nutrition, and health care access substantially boost adult health (Campbell et al., 2014; Miller et al., 2014). Future research might also examine the potential benefit of targeting overweight/obesity and poor mental health that stem from childhood poverty. Such efforts might go a long way toward reducing the socioeconomic disparities in health.
Supplementary Material
Highlights.
Economic hardship related to hypertension through anxiety-depression and BMI.
Family conflict related to hypertension by way of a higher BMI.
BMI increase was a risk factor for early-onset hypertension.
Acknowledgments
Funding Acknowledgement: This work was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (R01-HD-033487; R03-HD-097295), and the National Heart, Lung, and Blood Institute (R01-HL-088530; T32-HL-079891–12).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Achenbach TM (1991). Manual for the youth self-report and 1991 profile. Burlington, VT: University of Vermont. [Google Scholar]
- Achenbach TM, & Rescorla LA (2003). Manual for the ASEBA adult forms and profiles. Burlington, VT: University of Vermont. [Google Scholar]
- Achenbach TM, & Ruffle TM (2000). The Child Behavior Checklist and related forms for assessing behavioral/emotional problems and competencies. Pediatrics in Review, 21, 265–271. 10.1542/pir.21-8-265 [DOI] [PubMed] [Google Scholar]
- Brody GH, Yu T, Chen YF, Kogan SM, Evans GW, Beach SR, … & Philibert, R. A. (2013). Cumulative socioeconomic status risk, allostatic load, and adjustment: A prospective latent profile analysis with contextual and genetic protective factors. Developmental Psychology, 49(5), 913–927. 10.1037/a0028847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U, & Morris PA (2006). The bioecological model of human development In Damon W & Lerner RM (Eds.) Handbook of Child Psychology Vol. 1: Theoretical Models of Human Development (5th ed.) Wiley: New York, pp. 793–828. [Google Scholar]
- Brotman DJ, Golden SH, & Wittstein IS (2007). The cardiovascular toll of stress. The Lancet, 370(9592), 1089–1100. 10.1016/S0140-6736(07)61305-1 [DOI] [PubMed] [Google Scholar]
- Brown ED, Anderson KE, Garnett ML, & Hill EM (2019). Economic instability and household chaos relate to cortisol for children in poverty. Journal of Family Psychology, 33(6):629–39. [DOI] [PubMed] [Google Scholar]
- Burke NL, & Storch EA (2015). A meta-analysis of weight status and anxiety in children and adolescents. Journal of Developmental & Behavioral Pediatrics, 36(3), 133–145. 10.1097/DBP.0000000000000143 [DOI] [PubMed] [Google Scholar]
- Campbell F, Conti G, Heckman JJ, Moon SH, Pinto R, Pungello E, & Pan Y. (2014). Early childhood investments substantially boost adult health. Science, 343(6178), 1478–1485. 10.1126/science.124842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, & Armstead C. (2000). Family conflict predicts blood pressure changes in African-American adolescents: A preliminary examination. Journal of Adolescence, 23(3), 355–358. 10.1006/jado.2000.0320 [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki Deverts D, Chen E, & Matthews KA (2010). Childhood socioeconomic status and adult health. Annals of the New York Academy of Sciences, 1186(1), 37–55. 10.1111/j.1749-6632.2009.05334.x [DOI] [PubMed] [Google Scholar]
- Cohen S, Janicki-Deverts D, & Miller GE (2007). Psychological stress and disease. JAMA, 298(14), 1685–1687. 10.1001/jama.298.14.1685 [DOI] [PubMed] [Google Scholar]
- Cole DA, & Maxwell SE (2003). Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. Journal of Abnormal Psychology 112(4), 558–577. 10.1037/0021-843X.112A558 [DOI] [PubMed] [Google Scholar]
- Conger RD, & Conger KJ (2008). Understanding the process through which economic hardship influences families and children In Crane DR & B Heaton T. (Eds.), Handbook of Families and Poverty. Sage, Thousand Oaks, CA, pp. 64–95. [Google Scholar]
- Conger RD, & Donnellan MB (2007). An interactionist perspective on the socioeconomic context of human development. Annual Review of Psychology, 58, 175–199. 10.1146/annurev.psych.58.110405.085551 [DOI] [PubMed] [Google Scholar]
- de Moraes ACF, Lacerda MB, Moreno LA, Horta BL, & Carvalho HB (2014). Prevalence of high blood pressure in 122,053 adolescents: A systematic review and meta-regression. Medicine, 93(27), e232–e241. https://dx.doi.org/10.1097%2FMD-.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doom JR, Gunnar MR, & Clark CJ (2016). Maternal relationship during adolescence predicts cardiovascular disease risk in adulthood. Health Psychology, 35, 3376–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doom JR, Mason SM, Suglia SF, & Clark CJ (2017). Pathways between childhood/adolescent adversity, adolescent socioeconomic status, and long-term cardiovascular disease risk in young adulthood. Social Science & Medicine, 188, 166–175. 10.1016/j.socscimed.2017.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW (2004). The environment of childhood poverty. American Psychologist, 59(2), 77–92. 10.1037/0003-066X.59.2.77 [DOI] [PubMed] [Google Scholar]
- Evans GW, & Cassells RC (2014). Childhood poverty, cumulative risk exposure, and mental health in emerging adults. Clinical Psychological Science, 2(3), 287–296. https://dx.doi.org/10.1177%2F2167702613501496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Gonnella C, Marcynyszyn LA, Gentile L, & Salpekar N. (2005). The role of chaos in poverty and children’s socioemotional adjustment. Psychological Science, 16(7), 560–565. [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kim P. (2010). Multiple risk exposure as a potential explanatory mechanism for the socioeconomic status-health gradient. Annals of the New York Academy of Sciences, 1186(1), 174–189. https://doi.org/ DOI: 10.1111/j.1749-6632.2009.05336.x [DOI] [PubMed] [Google Scholar]
- Evans GW, & Kim P. (2012). Childhood poverty and young adults’ allostatic load: The mediating role of childhood cumulative risk exposure. Psychological Science, 23(9), 979–983. [DOI] [PubMed] [Google Scholar]
- Flynn J. (2013). The changing face of pediatric hypertension in the era of the childhood obesity epidemic. Pediatric Nephrology, 28(7), 1059–1066. 10.1007/s00467-012-2344-0 [DOI] [PubMed] [Google Scholar]
- Garasky S, Stewart SD, Gundersen C, Lohman BJ, & Eisenmann JC (2009). Family stressors and child obesity. Social Science Research, 38(4), 755–766. 10.1016/j.ssresearch.2009.06.002 [DOI] [PubMed] [Google Scholar]
- Gee ME, Bienek A, Campbell NR, Bancej CM, Robitaille C, Kaczorowski J, … & Nolan RP (2012). Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension). The American Journal of Cardiology, 109(4), 570–575. 10.1016/j.amjcard.2011.09.051 [DOI] [PubMed] [Google Scholar]
- Graffar M. (1956). A method for social classification of population samples. Courier, 6, 455–459. [Google Scholar]
- Gundersen C, Mahatmya D, Garasky S, & Lohman B. (2011). Linking psychosocial stressors and childhood obesity. Obesity Reviews, 12(5), e54–e63. https://doi.org/-doi: 10.1111/j.1467-789X.2010.00813.x [DOI] [PubMed] [Google Scholar]
- Halliday JA, Palma CL, Mellor D, Green J, & Renzaho AMN (2014). The relationship between family functioning and child and adolescent overweight and obesity: A systematic review. International Journal of Obesity, 38(4), 480–493. 10.1038/ijo.2013.213 [DOI] [PubMed] [Google Scholar]
- Hill HD, Morris P, Gennetian LA, Wolf S, Tubbs C. (2013). The consequences of income instability for children’s well-being. Child Development Perspectives, 7, 85–90. 10.1111/cdep.12018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho M, Sanchez N, Maurizi LK, Bares CB, Grogan-Kaylor A, & Delva J. (2013). Examining the quality of adolescent-parent relationships among Chilean families. Child and Adolescent Social Work Journal, 30(3), 197–215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes TH, & Rahe RH (1967). The social readjustment rating scale. Journal of Psychosomatic Research, 11, 213–218. 10.1016/0022-3999(67)90010-4 [DOI] [PubMed] [Google Scholar]
- Huang Z, Willett WC, Manson JE, Rosner B, Stampfer MJ, Speizer FE, & Colditz GA (1998). Body weight, weight change, and risk for hypertension in women. Annals of Internal Medicine, 128(2), 81–88. [DOI] [PubMed] [Google Scholar]
- Kavanaugh SA, Neppl TK, & Melby JN (2018). Economic pressure and depressive symptoms: Testing the family stress model from adolescence to adulthood. Journal of Family Psychology 32(7), 957–965. https://dx.doi.org/10.1037%2Ffam0000462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2015). Principles and practice of structural equation modeling. Guilford Press, New York. [Google Scholar]
- Kotsis V, Stabouli S, Papakatsika S, Rizos Z, & Parati G. (2010). Mechanisms of obesity-induced hypertension. Hypertension Research, 33(5), 386–393. 10.1038/hr.2010.9 [DOI] [PubMed] [Google Scholar]
- Lee H, Andrew M, Gebremariam A, Lumeng JC, & Lee JM (2014). Longitudinal associations between poverty and obesity from birth through adolescence. American Journal of Public Health, 104(5), e70–e76. https://dx.doi.org/10.2105%2FAJPH.2013.301806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee H, Lee D, Guo G, Harris KM (2011). Trends in body mass index in adolescence and young adulthood in the United States: 1959–2002. Journal of Adolescent Health, 49(6), 601–8. 10.1016/j.jadohealth.2011.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehman BJ, Taylor SE, Kiefe CI, & Seeman TE (2009). Relationship of early life stress and psychological functioning to blood pressure in the CARDIA study. Health Psychology, 28(3), 338–346. 10.1037/a0013785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewington S, Clarke R, Qizilbash N, Peto R, & Collins R. (2003). Age-specific relevance of usual blood pressure to vascular mortality. The Lancet, 361(9366), 1391–1392. 10.1016/S0140-6736(03)13064-4 [DOI] [PubMed] [Google Scholar]
- Little TD, Deboeck P, & Wu W. (2015). Longitudinal data analysis In Fitzmaurice G, Davidian M. Verbeke G, & Molenberghs G. (Eds.), Emerging Trends in the Social and Behavioral Sciences: An Interdisciplinary, Searchable, and Linkable Resource: Chapman & Hall/CRC Press, Bacon Rouge FL, pp. 1–17. [Google Scholar]
- Lo JC, Chandra M, Sinaiko A, Daniels SR, Prineas RJ, Maring B, … & Adams KF (2014). Severe obesity in children: Prevalence, persistence and relation to hypertension. International Journal of Pediatric Endocrinology, March (1), 1–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loucks EB, Almeida ND, Taylor SE, & Matthews KA (2011). Childhood family psychosocial environment and coronary heart disease risk. Psychosomatic Medicine, 73(7), 563–571. https://dx.doi.org/10.1097%2FPSY.0b013e318228c820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lozoff B, De Andraca I, Castillo M, Smith J, Walter T, & Pino P (2003). Behavioral and developmental effects of preventing iron-deficiency anemia in healthy full-term infants. Pediatrics, 112, 846–854. [PubMed] [Google Scholar]
- Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, & Zitman FG (2010). Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Archives of General Psychiatry, 67(3), 220–229. 10.1001/archgenpsychiatry.2010.2 [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, & Fritz MS (2007). Mediation analysis. Annual Review of Psychology 58, 593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mak HW, Kim J, & Wang S. (2019). The role of parent-adolescent relationships in the development of (pre) hypertension in young adulthood in the U.S. Journal of Adolescent Health, 64(2), 258–264. 10.1016/i.iadohealth.2018.08.009 [DOI] [PubMed] [Google Scholar]
- Masuo K, Mikami H, Ogihara T, & Tuck ML (2000). Weight gain-induced blood pressure elevation. Hypertension, 35(5), 1135–1140. [DOI] [PubMed] [Google Scholar]
- Matheny AP Jr, Wachs TD, Ludwig JL, & Phillips K. (1995). Bringing order out of chaos: Psychometric characteristics of the confusion, hubbub, and order scale. Journal of Applied Developmental Psychology 16(3), 429–444. 10.1016/0193-3973(95)90028-4 [DOI] [Google Scholar]
- Matthews KA, & Gallo LC (2011). Psychological perspectives on pathways linking socioeconomic status and physical health. Annual Review of Psychology, 62, 501–530. 10.1146/annurev.psych.031809.130711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L. (2007). Socioeconomic status and obesity. Epidemiologic Reviews, 29(1), 29–48. 10.1093/epirev/mxm001 [DOI] [PubMed] [Google Scholar]
- McLaren L, & Hawe P. (2005). Ecological perspectives in health research. Journal of Epidemiology & Community Health, 59(1), 6–14. doi: 10.1136/jech.2003.018044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng L, Chen D, Yang Y, Zheng Y, & Hui R. (2012). Depression increases the risk of hypertension incidence: A meta-analysis of prospective cohort studies. Journal of Hypertension, 30(5), 842–851. doi: 10.1097/HJH.0b013e32835080b7 [DOI] [PubMed] [Google Scholar]
- Miller GE, Brody GH, Yu T, & Chen E. (2014). A family-oriented psychosocial intervention reduces inflammation in low-SES African American youth. Proceedings of the National Academy of Sciences, 111(31), 11287–11292. http://www.pnas.org/cgi/doi/10.1073/pnas.1406578111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller GE, Chen E, & Parker KJ (2011). Psychological stress in childhood and susceptibility to the chronic diseases of aging: Moving toward a model of behavioral and biological mechanisms. Psychological Bulletin, 137(6), 959–997. https://dx.doi.org/10.1037%2Fa0024768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen BO (2011). Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. Los Angeles, CA: Author. [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus user’s guide (Version 8). Los Angeles: Authors. [Google Scholar]
- Neppl TK, Senia JM, & Donnellan MB (2016). Effects of economic hardship: Testing the family stress model over time. Journal of Family Psychology, 30(1), 12−21. https://dx.doi.org/10.1037%2Ffam0000168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering TG (2007). Stress, inflammation, and hypertension. Journal of Clinical Hypertension, 9, 567–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov T. (2005). Analysis of longitudinal studies with missing data using covariance structure modeling with full-information maximum likelihood. Structural Equation Modeling, 12 (3), 493–505. 10.1207/s15328007sem1203_8 [DOI] [Google Scholar]
- Redwine KM, & Falkner B. (2012). Progression of prehypertension to hypertension in adolescents. Current Hypertension Reports, 14(6), 619–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosner B, Cook NR, Daniels S, & Falkner B. (2013). Childhood blood pressure trends and risk factors for high blood pressure: The NHANES experience 1988–2008. Hypertension, 62(2), 247–254. 10.1161/HYPERTENSIONAHA.111.00831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaller J, & Zerpa M. (2019). Short-run effects of parental job loss on child health. American Journal of Health Economics, 5(1), 8–41. 10.1162/ajhe_a_00106 [DOI] [Google Scholar]
- Schreier HM, Roy LB, Frimer LT, & Chen E. (2014). Family chaos and adolescent inflammatory profiles: The moderating role of socioeconomic status. Psychosomatic Medicine, 76(6), 460–467. doi: 10.1097/PSY.0000000000000078 [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, … & Committee on Early Childhood, Adoption, and Dependent Care. (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–e246. 10.1542/peds.2011-2663 [DOI] [PubMed] [Google Scholar]
- Selig JP, & Preacher KJ (2009). Mediation models for longitudinal data in developmental research. Research in Human Development, 6(2–3), 144–164. 10.1080/15427600902911247 [DOI] [Google Scholar]
- Sharma AK, Metzger DL, & Rodd CJ (2018). Prevalence and severity of high blood pressure among children based on the 2017 American Academy of Pediatrics Guidelines. JAMA Pediatrics, 172(6), 557–565. doi: 10.1001/jamapediatrics.2018.0223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slopen N, Goodman E, Koenen CK, & Kubzansky LD (2013). Socioeconomic and other social stressors and biomarkers of cardiometabolic risk in youth: A systematic review of less studied risk factors. PloS One, 8(5), e64418. DOI: 10.1371/journal.pone.0064418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorof J, & Daniels S. (2002). Obesity hypertension in children: A problem of epidemic proportions. Hypertension, 40(4), 441–447. 10.1161/01.HYP.-0000032940.33466.12 [DOI] [PubMed] [Google Scholar]
- Spies LA, Margolin G, Susman EJ, & Gordis EB (2011). Adolescents’ cortisol reactivity and subjective distress in response to family conflict: The moderating role of internalizing symptoms. Journal of Adolescent Health, 49(4), 386–392. doi: 10.1016/j.jadohealth.2011.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruill TM (2010). Chronic psychosocial stress and hypertension. Current Hypertension Reports, 12(1), 10–16. DOI 10.1007/s11906-009-0084-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steptoe A, Brydon L, & Kunz-Ebrecht S. (2005). Changes in financial strain over three years, ambulatory blood pressure, and cortisol responses to awakening. Psychosomatic Medicine, 67(2), 281–287. doi: 10.1097/01.psy.0000156932.96261.d2 [DOI] [PubMed] [Google Scholar]
- Su S, Wang X, Pollock JS, Treiber FA, Xu X, Snieder H, … & Harshfield GA (2015). Adverse childhood experiences and blood pressure trajectories from childhood to young adulthood: The Georgia stress and Heart study. Circulation, 131(19), 1674–1681. 10.1161/CIRCULATIONAHA.114.013104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Clark CJ, Boynton-Jarrett R, Kressin NR, & Koenen KC (2014). Child maltreatment and hypertension in young adulthood. BMC Public Health, 14(1), 1149–1155. http://www.biomedcentral.com/147-2458/14/1149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suglia SF, Koenen KC, Boynton-Jarrett R, Chan PS, Clark CJ, Danese A, … & Pratt CA (2018). Childhood and adolescent adversity and cardiometabolic outcomes: A scientific statement from the American Heart Association. Circulation, 137(5), e15–e28. 10.1161/CIR.0000000000000536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suls J, & Bunde J. (2005). Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin, 131(2), 260–300. 10.1037/0033-2909.131.2.260 [DOI] [PubMed] [Google Scholar]
- Taylor SE (2010). Mechanisms linking early life stress to adult health outcomes. Proceedings of the National Academy of Sciences, 107(19), 8507–8512. www.pnas.org/cgi/doi/10.1073/pnas.1003890107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, Way BM, & Seeman TE (2011). Early adversity and adult health outcomes. Development and Psychopathology, 23(3), 939–954. 10.1017/S0954579411000411 [DOI] [PubMed] [Google Scholar]
- Whelton PK, Carey RM, Aronow WS, et al. (2018). 2017 ACC/AHA/AAPA/ABC-/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of American College Cardiology 71, e13–e115. [DOI] [PubMed] [Google Scholar]
- Winning A, Glymour MM, McCormick MC, Gilsanz P, & Kubzansky LD (2015). Psychological distress across the life course and cardiometabolic risk. Journal of the American College of Cardiology, 66, 1577–86. 10.1016/jjacc.2015.08.021 [DOI] [PubMed] [Google Scholar]
- World Medical Association (2013). Declaration of Helsinki: Ethnical principles for medical research involving human subjects. JAMA, 310, 2191–2194. 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.