Abstract
Introduction:
Physical activity monitors, motivational text messages, personal calls, and group meetings, have proven to be efficacious physical activity interventions. However, individual participant response to these interventions varies drastically. A SMART design (sequential multiple assignment randomized trial) provides an effective way to test interventions that start with an initial treatment and then transition to an augmented treatment for non-responders. We describe a SMART to determine the most effective adaptive intervention to increase physical activity (steps, moderate-to-vigorous physical activity) and improve cardiovascular health among employed women who are not regularly physically active. The SMART uses combinations of four treatments: 1) enhanced physical activity monitor (Fitbit wearable activity monitor and mobile app with goal setting and physical activity prescription), 2) text messages, 3) personal calls, and 4) group meetings.
Methods:
Participants (N = 312) include women ages 18–70 employed at a large academic medical center. Women will be randomized to an initial intervention, either an enhanced physical activity monitor or enhanced physical activity monitor + text messaging. Non-responders to the initial intervention at 2 months will be randomized to either personal calls or groups meetings for the next 6 months. At 8 months, all participants will return to only an enhanced physical activity monitor until their final 12-month assessment.
Discussion:
Results of this study will add to the literature on improving physical activity in employed women. This study will identify effective interventions for women who respond to less intensive treatments, while maximizing benefits for those who need a more intensive approach.
Keywords: Women, Physical activity, Fitbit, SMART, Sequential multiple assignment randomized trial, Adaptive interventions
1. Introduction
Insufficient physical activity continues to be a risk factor for cardiovascular disease, which is a leading cause of death among women [1,2]. Despite this important fact, slightly over half of women in the United States continue to not meet aerobic physical activity guidelines [3]. Low levels of physical activity can be exacerbated by large amounts of sedentary behavior imposed in many worksites [4], which poses as a significant barrier as over 56% of women are employed [5]. Women also experience barriers to being more physically active outside of work including home demands, neighborhood safety, and health concerns [6–8]. Lower levels of self-efficacy, as well as needing different types of social support, can also affect physical activity in women [9–14].
Physical activity monitors, motivational text messages, behavioral group meetings and motivational personal calls have been tested in interventions to improve physical activity. Recent interventions using physical activity monitors (e.g. Fitbit) as a motivational tool for self-monitoring have shown promising results in increasing physical activity in women [15]. Another intervention with demonstrated physical activity efficacy includes motivational text messages coupled with physical activity monitors [16,17]. Women who fail to increase and maintain their physical activity with physical activity monitors alone or physical activity monitors coupled with text messages [18,19] may benefit from augmented treatment, including personal telephone calls that provide individual social support [20–22] and/or group meetings that provide peer social support [10,23]. While each intervention has proven efficacy, individual participant response to the intervention varies drastically.
Adaptive interventions specify a sequence of decision rules to determine why, how, and when treatment delivery should be changed based on patient characteristics or response to an initial treatment [24]. A sequential multiple assignment randomized trial (SMART) provides an effective way to test differential response to alternative treatment options that make up adaptive interventions. In a SMART design, researchers start with an initial intervention, and then change/augment it over time based on response to the initial treatment [24]. The SMART design was developed to allow researchers to build optimal adaptive interventions, and this design is rapidly gaining popularity and use among scientists. It is being tested with a wide spectrum of healthcare outcomes [25–27]. However only a small amount of studies with SMART trials have included physical activity as part of the intervention, and these have been weight loss studies [28–31].
The purpose of this paper is to describe the protocol of a sequential multiple assignment randomized trial (SMART) that will test adaptive interventions designed to improve physical activity (steps, moderate-to-vigorous physical activity) and improve cardiovascular health among working women who are not regularly physically active. The SMART uses combinations of four treatments: 1) enhanced physical activity monitor (Fitbit wearable activity monitor and mobile app with goal setting and physical activity prescription), 2) text messages, 3) personal calls, and 4) group meetings.
2. Methods
The study protocol and consent procedures have been approved by the Rush University Medical Center and the University of Illinois at Chicago Institution Review Boards. The trial protocol ( NCT03558828) is registered in ClinicalTrials.gov and the full study protocol is published in ClinicalTrials.gov, and the results will be published at that site upon completion of the trial.
2.1. Specific aims
This study aims to determine the most effective adaptive intervention (Fig. 1) combining four efficacious treatments (enhanced physical activity monitor, text messages, personal calls, group meetings) to increase physical activity (daily steps, minutes of moderate-to-vigorous physical activity/week) and improve cardiovascular health (aerobic fitness, body composition) among employed women who are not regularly physically active. This study also aims to assess treatment effects on intervention targets, which are personal and social determinants of health (benefits, barriers, self-efficacy, and social support). A sequential multiple assignment randomized trial (SMART) design [32] will address the following aims, hypotheses, and research question.
Fig. 1.
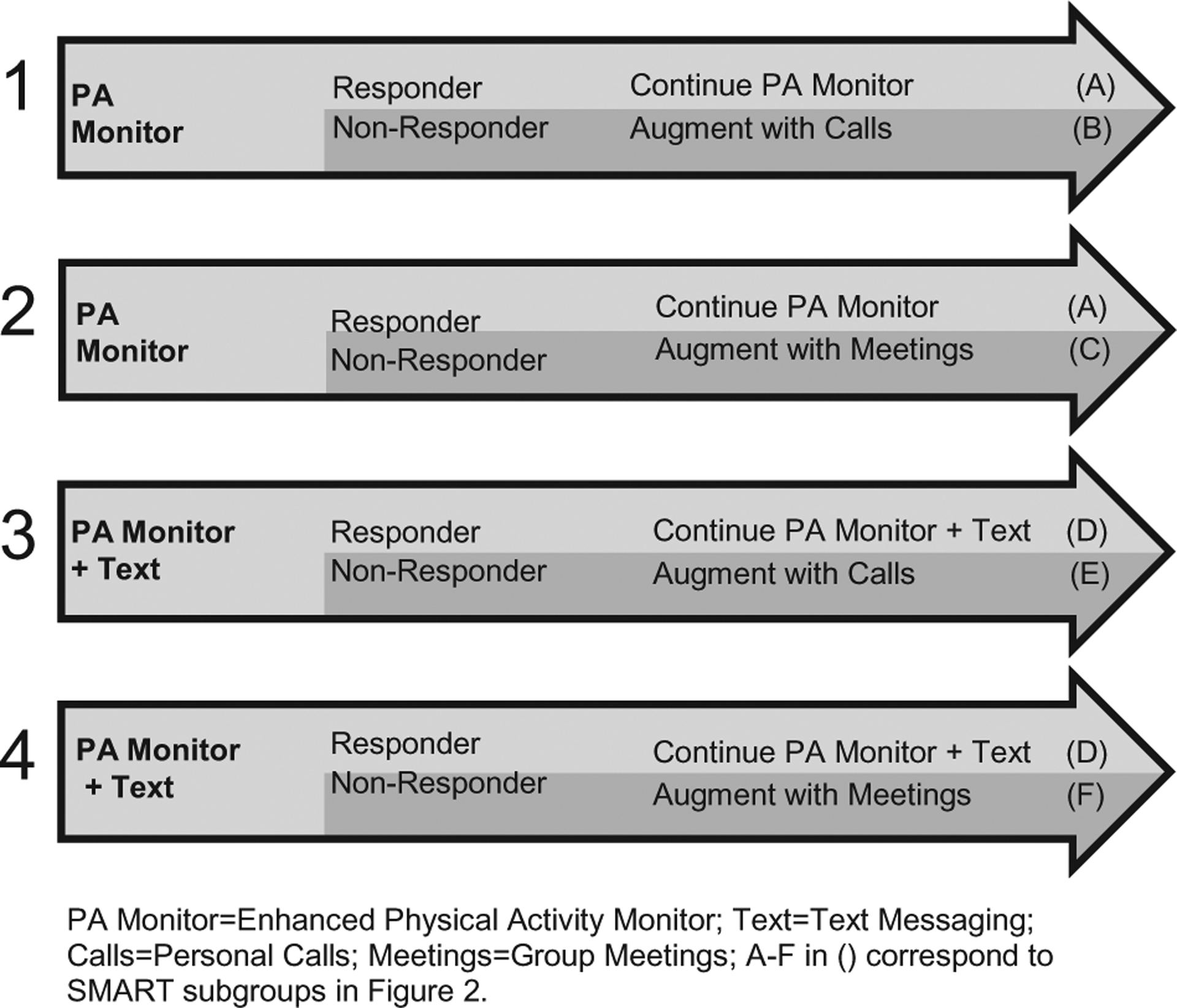
Four adaptive interventions.
2.1.1. Aim 1 (Primary)
Among non-responders to the initial treatments (physical activity monitor vs. physical activity monitor + text messages), compare the two augmented treatments: personal calls and group meetings. Aim 1 Hypothesis: Group meetings will be more effective than personal calls in improving physical activity and cardiovascular health after 34 and 50 weeks, among non-responders to the initial treatment.
2.1.2. Aim 2a (Secondary)
Compare the two initial treatments: enhanced physical activity monitor and enhanced physical activity monitor + text messages. Aim 2a Hypothesis: Participants who receive enhanced physical activity monitor + text messages as compared to those who receive enhanced physical activity monitor alone will show greater improvement in physical activity at the end of 8 weeks.
2.1.3. Aim 2b (Secondary)
Compare the four adaptive interventions embedded in the SMART on physical activity and cardiovascular health (Fig. 1). Aim 2b Hypothesis: Adaptive intervention #4 will be more effective than #1, #2, or #3 in improving physical activity and cardiovascular health after 34 and 50 weeks.
2.1.4. Aim 3 (Exploratory)
Identify mediators and moderators of the initial and augmented treatments on physical activity and cardiovascular health. Aim 3 Hypothesis: The intervention targets (benefits, barriers, self-efficacy, and social support) will mediate the effect of the initial and augmented treatments on physical activity (8, 34, and 50 weeks) and cardiovascular health (34 and 50 weeks). Aim 3 Research Question: Do characteristics of participants (prior physical activity, demographics, BMI, depression) and their environment (walkability, crime) moderate the effects of the initial and augmented treatments on physical activity and cardiovascular health?
2.1.5. Aim 4 (Cost-effectiveness)
Compare the cost-effectiveness of the four adaptive interventions from the societal perspective which includes both program costs and participant costs. Aim 4 Hypothesis: Adaptive intervention #4 will have the lowest cost per unit increase in physical activity and improvement in cardiovascular health, taking into account program and participant costs.
2.2. Study design
This study compares four adaptive interventions (Fig. 1). Each adaptive intervention consists of an initial treatment component (physical activity monitor or physical activity monitor + text messaging) followed by an augmented treatment (personal calls or group meetings) for those who do not respond to the initial treatment component. For ease of management, we limit the augmented treatments to only two of the four factorial combinations of personal calls and group meetings. We focus on personal calls only (least expensive) and group meetings (current standard). It is well-established that without an intervention, physical activity remains unchanged [33].
The combination of the two initial treatment components and the two augmented treatment components delivered to non-responders yields four adaptive interventions that will be evaluated in this study: (1) Start with enhanced physical activity monitor, augment with motivational personal calls for non-responders, and continue enhanced physical activity monitor for responders; (2) Start with enhanced physical activity monitor, augment with motivational group meetings for non-responders, and continue enhanced physical activity monitor for responders; (3) Start with enhanced physical activity monitor + text messaging, augment with motivational personal calls for non-responders and continue enhanced physical activity monitor + text messaging for responders; and (4) Start with enhanced physical activity monitor + text messaging, augment with motivational group meetings for non-responders and continue enhanced physical activity monitor + text messaging for responders.
A methodologically rigorous SMART design (Fig. 2) will be used to test these adaptive interventions. Participants will be randomly assigned to one of the two eight-week (early adoption phase) initial treatment components: a) enhanced physical activity monitor treatment only (wearable activity monitor and mobile app with goal setting and physical activity prescription), or b) enhanced physical activity monitor + motivational text messages treatment. Earlier work with the Women’s Lifestyle Physical Activity Program with a sample comprised of 67% Caucasian and 33% African American women showed that non-responders can be identified at eight weeks [23]. In that study, we found the median first lapse in prescribed walking (one week of not adhering to a walking goal) occurred at six weeks, and on average, Week 8 was the first week at which a three-week relapse (three lapsed weeks) could be identified [34]. These women were least likely to continue the program suggesting 8 weeks may be an optimal time to augment the treatment. Therefore, week 8 has been set as the decision point for women who have not met their physical activity step goal (i.e., non-responders).
Fig. 2.

SMART design of the physical activity study.
At week 8, the research team will remotely determine if participants are deemed responders or non-responders to their initial treatment assignment based on their daily wearable physical activity step count. In this study, a Fitbit is the type of physical activity monitor that is used [35]. If a participant a) fails to wear her Fitbit or does not have a valid day (i.e., wears the Fitbit a minimum of 3 of 7 days in weeks 6 to 8, with either 10 h of wear time for that day and/or exceeds her baseline step average for that day), and b) her average steps do not exceed the short-term goal of 600 steps above baseline average for two of the three weeks in weeks 6 to 8, she will transition to the non-responder group. Six hundred steps was derived from taking 20% of 3000 steps, the overall proposed increase of steps per day, and represents reasonable progress toward the goal of increasing by 3000 steps per day. Based on previously published step count data, counts per day have been classified as: < 5000 = “sedentary”; 5000–7499 steps = “low active”; 7500–9999 steps = “somewhat active”; 10,000–12,499 steps = “active”; and ≥12,500 steps = “high active” [36]. Adults in the U.S. take an average of 5117 steps per day [37]. Adding 3000 steps to 5117 steps per day would move an individual from the “low active” into the “somewhat active” category. Thus, each woman is given an overall goal to achieve by the end of the study, to increase her steps above her baseline by a minimum of 3000 steps per day, an increase that approximates 30 min of physical activity [38,39] at a moderate walking pace.
Non-responders to initial treatments will be randomly assigned to one of the two augmented treatments: a) personal calls, or b) group meetings for Weeks 9–34 (later adoption phase). Responders will continue with their original treatment for Weeks 9–34 (later adoption). During Weeks 35–50 (maintenance), all women will receive enhanced physical activity monitors only. Data collection will occur at baseline and at Weeks 9–10 (end of early adoption/post-initial intervention), 34–35 (end of later adoption/post-augmented intervention), and 51–52 (end of maintenance/follow-up). This design creates six subgroups, A through F (Fig. 2) that will be used to evaluate the four adaptive interventions (Fig. 1). The letters A through F in Figs. 1 and 2 show the link between the four adaptive interventions and the SMART design.
2.3. Participants
2.3.1. Setting
Participants are being recruited from employees at a large urban academic medical center in the Midwest. The recruitment setting for this study employs approximately 7577 females from diverse ethnic backgrounds: African American (24%), Asian (10%), Hispanic (14%), White (47%), and other ethnicities (5%). The mean age of employees is 39.97 years (SD = 19.22). In order to assure that our recruitment site has enough potential participants, we conservatively assumed that 24.7% of employed women at this worksite fail to meet aerobic physical activity guidelines, which is half the rate of the general population of women who fail to meet the guidelines [3]. Based on this conservative assumption, we estimate that we will have a pool of approximately 1870 women eligible for participation. This potential pool size allows for some of the women to either not be interested in participating, or not meet inclusion criteria.
2.3.2. Sample
Inclusion criteria are: (1) female employee at study site (the sample is limited to women due to the substantive findings, including our own [23,40] suggesting that women have a more favorable response when interventions are specifically designed for women) [41]; (2) aged 18 to 70; (3) able to speak/read English (because the second round of randomization includes the group meeting, which requires ≥6 participants and we cannot guarantee adequate numbers of same-language participants unless we limit the sample to English); (4) owners of a smart-phone with text messaging capability, (because of the wide use of smartphones and text messages [42], participants’ own smartphones will be used); (5) willing to receive motivational text messages at the proposed rate of 3 per week for 8 months (because participants need to decide ahead of time if they have a phone plan that is compatible with taking additional text messages without undue financial burden for themselves); (7) as verified by wearing an ActiGraph accelerometer for one week during the screening period, has an average of < 7500 steps per day; (8) desiring to be more physically active; (9) willing to be assessed for diabetes, as we will include participants who have Type 1 diabetes, or Type 2 diabetes with an A1C ≥ 9.0%, or have an A1C of ≥6.5% without a prior diabetes diagnosis, only if they have been given clearance by their health care provider [43]; and (9) without a disability that inhibits walking as determined by the PAR-Q & You (PA Readiness Questionnaire) [44]. If a participant has: (1) major signs/symptoms of pulmonary or cardiovascular disease;45and (2) systolic blood pressure (BP) ≥ 160 and/or diastolic BP ≥ 100 [45,46], they will require medical clearance from their healthcare provider before being able to continue in the study. If the participant does not receive medical clearance (i.e. their healthcare provider will not give them permission to participate in the study, or they do not follow-up with their healthcare provider to obtain medical clearance), they will be considered a screen failure.
2.3.3. Sample size
All power analyses were estimated using methods described by Oetting et al. [47] A net effect size of 0.41 was obtained by comparing 48-week change in self-reported moderate-vigorous physical activity for the group meetings only condition from the Women’s Lifestyle Physical Activity Program (d = 0.89) to the weighted average effect size from six telephone interventions reported in the literature (d = 0.48) [21,48]. Given d = 0.41, a α2-tailed = 0.01, pre-post correlation of r = 0.60, a sample size of 188 non-responders (280 participants and 67% non-response to the initial treatment), we will obtain a power of 0.80 for Aim 1. To account for attrition, we will over-sample by 10%, for a sample size of 312. These 312 participants will be divided into five waves of approximately 62 to 63 participants per wave. The initial sample size of 280 will afford power of 0.81 to detect an effect size of d = 0.27 for secondary Aim 2a (assuming α2-tailed = 0.05, and rpre-post = 0.60). For secondary Aim 2b, we will have an adequate sample size for a 90% probability of correctly choosing the best adaptive intervention, assuming an effect size of d = 0.30 for the difference between the best strategy and the next best strategy.
Staggering recruitment by waves will allow the research team adequate time to recruit, screen, and enroll participants into the study. Recruiting 60 or more participants into each wave will yield at least 30 participants randomized to each initial treatment condition. Of these participants recruited into each wave, we expect an average of one-third (n = 20 per initial treatment condition) to respond. Of the expected non-responders (n = 20 per initial treatment condition), half will be randomly assigned to personal calls (n = 20), and half randomly assigned to enhanced group meetings (n = 20).
2.3.4. Recruitment
This study will build on the successful recruitment strategies used in our prior studies [49–51]. We will use reactive strategies to recruit participants (i.e., women will be informed about the program, and those interested in participating will be contacted by study researchers). The strategies will include flyers, using recruitment posters on electronic and paper employee bulletin boards located near work areas, promoting the study in the main cafeteria area at meal times, and advertising in the worksite news portal. All strategies will include a brief description of the program, provide a phone number to call for further information, and provide a program email address. For ease of study recognition, we have worked with marketing at our university to develop a brand for the study, calling it Working Women Walking. The Working Women Walking logo will appear on all of our study materials.
2.3.5. Retention
For this study, we will use a number of successful retention strategies [49,50,52,53] similar to our preliminary studies, where we had 100% retention over 12 weeks in the Text4Walking program and 90% retention over 48 weeks in the Women’s Lifestyle Physical Activity Program. First, all research-related visits will be offered at the worksite on both daytime and evening shifts. Data collection appointment assessments will be split over several days. Participants will also have the option for research-related visits to be at a convenient location of their choosing (e.g., their home). Participants assigned to group meetings may use their phones for audio conferencing or Webex videoconferencing if they are unable to attend the group meeting in-person. We will identify multiple means of remaining in contact with participants including: work, home, and cell phone numbers (including text messages); home and email addresses. Participants will receive reminder telephone calls, text messages, and/or e-mails before data collection and group meetings.
2.4. Framework
Fig. 3 provides the framework that informs all components of the physical activity adaptive interventions. This framework is based on several key constructs of Bandura’s Social Cognitive Theory and Pender’s Health Promotion Model [9,10]. The intervention’s effect on physical activity and cardiovascular health outcomes is moderated by prior physical activity behavior, as well as personal factors. The intervention’s effect on physical activity and cardiovascular outcomes is mediated by intervention targets. Text messaging, personal calls and group meetings impact perceived benefits and barriers of physical activity, and self-efficacy. Group meetings also impact social support [54].
Fig. 3.
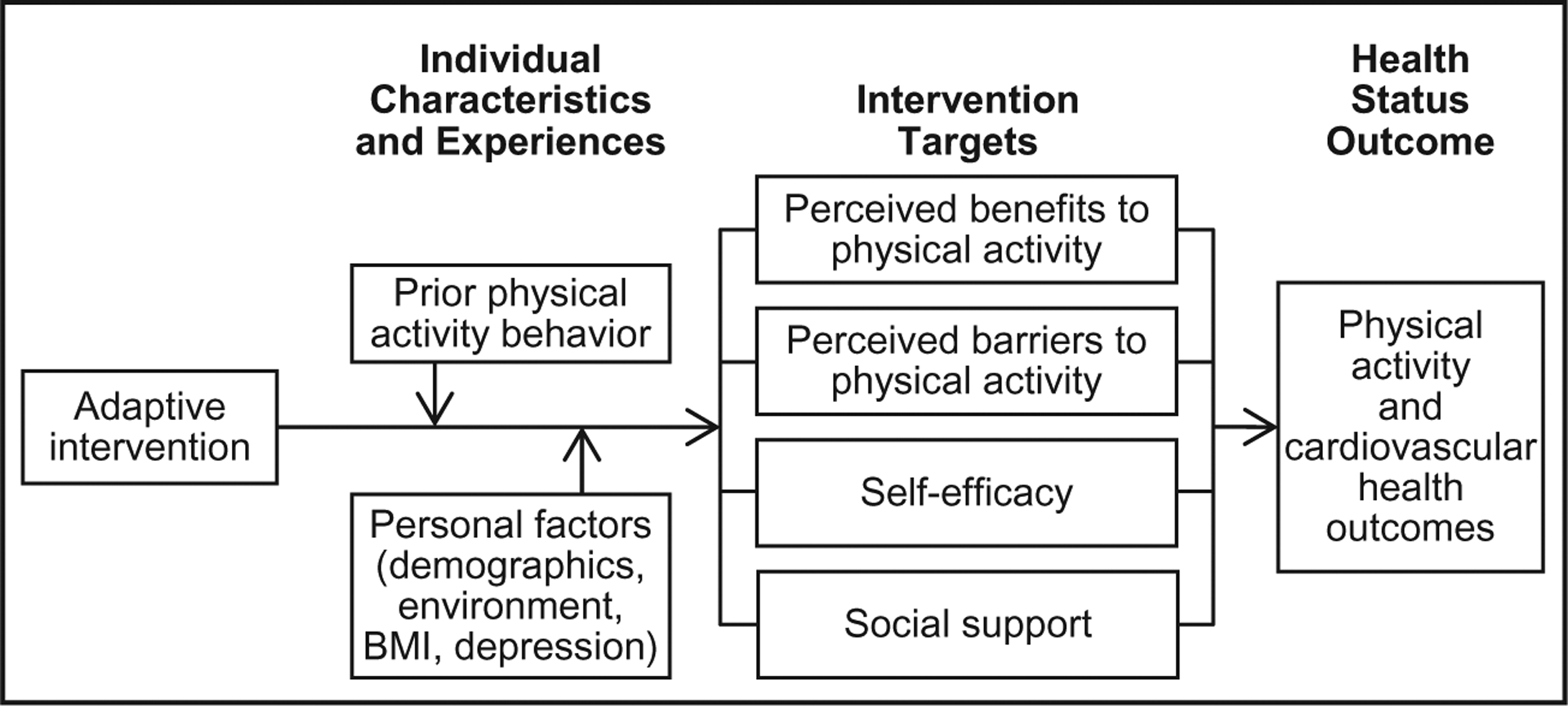
Framework for physical activity adaptive interventions.
2.5. Intervention
2.5.1. Enhanced physical activity monitor treatment
All women will receive an enhanced physical activity monitor treatment, which includes: 1) a Fitbit, wrist-based physical activity monitor (Charge 2 or Charge 3) and Fitbit mobile app for self-monitoring of daily physical activity; and 2) goal setting with a physical activity prescription. We will follow the physical activity prescription guidelines that were successfully used in our prior work [23]. First, steps walked per week and per day (step counts) are obtained from the Fitbit, which is distributed during initial eligibility screening and worn for one week prior to the start of the intervention [55]. The baseline step count per day is identified by averaging daily step counts over at least four days of valid data (see measures in Section 2.8). The overall goal is the baseline step count plus 3000 steps per day. To enhance self-efficacy, we will work with each woman to set an initial physical activity goal to gradually increase walking frequency, duration, and intensity [10,56] For activity progression, we first emphasize frequency (adding steps throughout the day), then duration (adding 10- to 30-minute bouts of physical activity), and finally intensity.
The initial step count goal will be entered electronically into the Fitbit mobile app, and the Fitbit is to be worn at all times while awake except during bathing and swimming [57]. The physical activity monitor and mobile app will allow women to self-monitor their walking steps, distance, and intensity. Fitbit data will be collected using the iCardia system [58]. Throughout the entire 12 months of the study, text message reminders will be sent to all of the participants every Monday morning to remind them to sync their Fitbit. In addition, the participants in the text message group will be given a step classification text message on Monday for the first 8 months of the study.
All participants will have a program orientation, which will include guidance on setting a physical activity goal, using motivational interviewing, and guidance using their Fitbit physical activity monitor and mobile app, as well as viewing a video that will give information related to self-monitoring their steps, and proper walking and stretching techniques. The participants will also receive a Participant Physical Activity Manual [23].
2.5.2. Motivational text messaging
In addition to the enhanced physical activity monitor half of the participants will also receive motivational text messages. Women who receive an enhanced physical activity monitor + motivational text messages treatment from Week 1 through Week 34 will participate in an initial brief motivational interviewing session to identify strategies to overcome barriers. Motivational interviewing will be used to elicit self-motivational statements that address the intervention targets of perceived benefits, perceived barriers, self-efficacy, and social support (Fig. 3) [9,10,59]. This is accomplished by prompting participants to explore and resolve their own barriers to physical activity. After this step, participants will be asked if they want to develop and write any of their own text messages as well as asked to select additional text messages from the Text4Walking database, that has over 250 established physical activity text messages that provide motivating messages to overcome specific physical activity barriers and encourage an individual to walk more [17,60].
2.5.3. Motivational personal calls
Motivational personal calls will be based on the model used in our successful Women’s Lifestyle Physical Activity Program [23]. The personal call treatment consists of five brief (approximately 10 min) motivational interviewing telephone calls, made by an interventionist, every two weeks during the first 10 weeks of late adoption, and four calls every three weeks for the following 14 weeks (total 10 personal calls in late adoption Weeks 11–34). Participants will be given feedback based on their step counts in the prior week in relation to their goal (obtained from iCardia). Using motivational interviewing, the interventionist will tailor the discussion to match the participant’s needs, experiences, barriers, motivation, and confidence. Suggestions for addressing problems will be provided after the participant has explored options and agreed to receive feedback [61].
2.5.4. Group meetings
Group meetings will be based on the model used in our prior research [23]. The group meeting treatment consists of five 45-minute group meetings held every four to six weeks during late adoption (Weeks 9–34). Due to the time needed to schedule, group meetings will start at Week 12. Group meetings will be led by a trained interventionist, held in a private conference room on the worksite property, and scheduled between the day and evening shift times. Women will be able to attend in person or by using their own phones for audioconferencing or Webex video conferencing [62] to interact and view group meeting materials.
These group meetings are targeted to address participant’s common barriers to physical activity, and identify benefits of physical activity [1,7]. The content for the first group meeting focuses on identifying realistic outcome expectations regarding the effects of physical activity, to ensure realistic short- and long-term goals. The second and third meetings address personal and environmental problems that can interfere with increasing physical activity. The fourth group meeting focuses on anticipating disincentives for physical activity and handling relapses. At the final group meeting, participants will share their experiences. Consistent with social cognitive theory [10], the group begins with a seven minute video of women role modeling (vicarious experience) by demonstrating skills, sharing experiences, and sharing approaches to problem solving and overcoming challenges pertinent to each group meeting. These videos were developed in our earlier work [23,40] and will be updated using a diverse group of women. Following the video, each group meeting will include a 30-minute group discussion facilitated by the interventionist to role model, provide guidance, and encourage participants to solve problems together.
2.6. Procedures
After an explanation of the study, interested women will be screened for inclusion criteria. Those who meet these criteria will be scheduled for a screening appointment. Screening appointments will be scheduled at the worksite either before or after work, on breaks, or at another time convenient to them. If a participant passes the screening process, she will be given instructions to wear two physical activity monitors for one week. She will wear a blinded Fitbit (settings adjusted so that the participant cannot see the step count on the device or mobile app or tape applied over screen) and an ActiGraph that is placed on the waist. If they have not worn their Fitbit and ActiGraph as instructed, they will be given an extra week to wear it. At a one-week follow-up visit, as determined by ActiGraph data, if the participant walked on average ≥ 7500 steps per day, they will be informed that they are too active to participate in the study. They will be given a copy of Step It Up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities. This Call to Action provides strategies to improve walking.
If they have walked on average < 7500 steps per day, baseline data collection will be gathered with questionnaires, and participants will complete a step fitness test [63]. Baseline step count per day will be established using the data from the initial week that the participant wore both the Fitbit and the ActiGraph. Participants will then be enrolled into the study and randomly assigned to one of the first two initial treatments. All women will have a program orientation appointment, lasting 60 to 75 min.
At the end of 8 weeks (decision point), the research team will determine if participants are responders or non-responders, determined by their daily step count synced to iCardia, and based on decision rules. At the Week 9 or 10 data collection appointment, assessment data will be obtained. If the participant is deemed a responder, she will be instructed to continue with her initial treatment. If she is deemed a non-responder, she will continue her initial treatment and be randomly assigned to one of the two augmented treatments. All participants will receive a new step goal at the end of Week 9 or10.
Randomization to the initial and augmented interventions will be conducted using the randomization module in REDCap. Because randomization will take place after participants have completed necessary research activities (i.e., baseline interview for initial randomization and collection of post-intervention accelerometer data for second randomization), we are unable to know the sample size for randomization at each step. Therefore, to minimize imbalance in sample sizes of the conditions, we will employ a block-randomization procedure at each step. Participants will be randomized in the order that they completed the preceding research activity.
To minimize ability to “guess” the next available condition, blocks of four and six will be randomly ordered and condition randomly ordered within block. The study statistician will be responsible for creating the randomization tables and uploading them into REDCap. Once in REDCap, all other research staff are blind to the randomization table; and, once randomized, REDCap blocks any effort to change/alter randomization status for a participant.
At the Week 35 or 36 data collection appointment, assessment data will be obtained. At this data collection assessment, all participants will return to only an enhanced physical activity monitor status. They will be instructed to continue to wear their physical activity monitor. All women participants receive a new step goal at the end of Week 35 or 36. At the Week 51 or 52 data collection appointment, final assessment data will be obtained. All participants will be allowed to keep their Fitbit devices. In total, participants will be compensated $160 for the four assessments.
2.7. Fidelity
Treatment fidelity, evidence that the intervention has been delivered as intended, will be monitored with the Behavior Change Consortium’s Model of Treatment Fidelity [64]. The Behavior Change Consortium recommended five different categories for incorporating treatment fidelity. Three focus on the study design, training, and treatment delivery. Two categories focus on treatment receipt of the intervention, and enactment [65,66].
2.7.1. Design
In the worksite, there is the potential for diffusion of intervention effects with person-level randomization. Although cluster-randomized trials are the ideal design to prevent diffusion of the interventions [18,67], the use of second person-level randomization for non-responders in the proposed SMART design precludes this approach. To address diffusion of the intervention in the proposed research, we will assess diffusion levels after completion of the intervention using a brief measure that identifies social interactions specific to the intervention in the worksite.
2.7.2. Training
To minimize contamination, separate research staff training will be held for each group of staff: (1) screening and baseline data collectors; (2) program orientation staff; (3) augmented treatment interventionists for the personal calls; and (4) augmented treatment interventionists for group meetings. These research staff groups are separate to minimize contamination across augmented treatments and minimize risk of differential treatment. Additional training in motivational interviewing will be held for the personal call treatment interventionists.
2.7.3. Delivery of the intervention
The technical performance of the enhanced physical activity monitor will be checked every week on iCardia. To prevent drift, all personal calls will be audiotaped and eight (four per intervention type) per wave randomly selected and assessed [68]. All group meetings will be audiotaped and Group Meeting 1 and a randomly selected Group Meeting from 2 to 5 (for each intervention type) per wave will be assessed for adherence and competence with the Breitenstein Fidelity Checklist which was modified for this study. Adherence will be measured with 10–14 items coded yes or no dependent on the interventionist following manualized instructions for a Group Meeting. Competence will be measured with 17 items that rate if the interventionist demonstrated specific competencies during Group Meetings [69]
2.7.4. Receipt of intervention
At the program orientation, a checklist will be used to evaluate behavioral competency regarding participant use of the physical activity monitor and step goal setting. For physical activity monitor use, we will use iCardia to track weekly physical activity monitor wear time, determined by the device’s capability to register heart rate. Daily Fitbit wear-time is automatically calculated by the iCardia system based on the incoming heart rate sensor data from the Fitbit devices. Fitbit Charge 2 uses photoplethysmography to measure continuous heart rate at a sampling frequency of ≤1 s. When a user removes the device from her wrist, there is no heart pulse recorded, which indicates “non-wear time”. Daily wear-time will be calculated by subtracting the total minutes of “non-wear time” from the total number of minutes per day (1440 min), with non-wear time defined as any interval with at least 60 consecutive seconds of non-recorded heart rate data. We will also track whether the physical activity monitor is registering steps.
For text messaging delivery, we will count the number of text messages sent. Satisfaction with the content and frequency of the text messaging system will be assessed with the Physical Activity Text Messaging Satisfaction Tool [70]. The personal call interventionists will enter the date and length of every personal call into the participant tracking database. The number of personal calls completed and participants contacted will be summed to obtain the dose. The group meeting interventionist will record group meeting attendance, distinguishing between in-person and remote attendance. The number of group meetings attended will be counted to obtain the dose. At the conclusion of the study period, participant satisfaction will be measured with the Overall Program Satisfaction Tool [71].
2.7.5. Enactment
Enactment (i.e., how well the participant can apply the treatment-related behavior skills) will be measured by checking iCardia to determine the number of weeks the participants wore their physical activity monitor for at least 10 h a day for a minimum of three days.
2.8. Measures
Measures for this study are categorized in Table 1 as individual characteristics and experiences, intervention targets, and health status outcomes, which include physical activity behavioral outcomes and cardiovascular health outcomes.
Table 1.
Study variables, measures, and reliability/validity.
| Aim variables | Measures, number of items | Reliability/validity |
|---|---|---|
| Individual characteristics and experiences | ||
| Demographics | Demographic Questionnaire [65] (age, gender, ethnicity, marital status, children, caregiver status, education, income, job) | - |
| Neighborhood environment | Neighborhood Environment Walkability Scale (NEWS; 28 items of respondents’ perceptions of characteristics in their neighborhoods that are conducive to walking) [66]. | Test-retest r = 0.58 to 0.80; criterion validity demonstrated [66] |
| Depression | Emotional Distress-Depression-Short Form 8b (8 items measuring depressive symptoms in past 7 days.) [67] | Cronbach’s alpha =0.91–0.98 [95]; construct validity demonstrated [96] |
| Intervention targets | ||
| Benefits/Barriers | Exercise Benefits/Barriers Scale (Revised for physical activity; 43 items about statements that relate to positive/negative physical activity ideas.) [68] | Cronbach’s alpha = 0.952; construct validity demonstrated [68] |
| Self-efficacy | McAuley’s Self-Efficacy for Overcoming Barriers to physical activity (17 items reflecting beliefs in ability to continue to be physically active in the face of barriers) [69] | Cronbach’s alpha = 0.94 in preliminary study [97,98] |
| Support | Social Support and Exercise Survey (Revised for physical activity; 13-item scale of family and friend support) [70] | Cronbach’s alpha = 0.61–0.84 and criterion-related validity demonstrated [70] |
| Health status outcomes | ||
| Physical activity behavioral outcomes | ||
| PA monitor | ActiGraph GT3X-BT accelerometer is to be worn during waking hours on the right hip, in line with the right armpit. Participants will need to wear the ActiGraph for a minimum of four 10-hour days, one of which is a weekend day [71,72]. | Intraclass correlation coefficient ranged from 0.95 to 0.99 and convergent validity demonstrated [71] |
| PA self-report lifestyle | International Physical Activity Questionnaire (IPAQ [73]; questions for days per week and hours and minutes per day of physical activity and walking and sitting time). | Spearman’s Rho = 0.80; criterion validity demonstrated with categorical estimates of sufficient physical activity [99] |
| Cardiovascular health outcomes | ||
| Aerobic fitness | Two-minute step test [58] can be performed in a small space using minimal equipment. Participants step in place to a predesignated height for 2 min [37]. | Correlation with treadmill r = 0.74; Concurrent validity with age [100] |
| Body composition BMI | Weight (lb)/height (in) [2] × 703. Weight to 0.20 lb., height to 0.25 in. [74] | Correlation with self-reported height and weight and BMI r = 0.97 and 0.89 [101] |
| Waist | Waist to 0.25 in. measured x2, the nearest at narrowest part of torso above umbilicus, below xiphoid [74] | Correlation with related cardiovascular and metabolic disease r = 0.48 and 0.61 [74] |
2.8.1. Individual characteristics and experiences
Individual characteristics and experiences will be assessed with three different measures. The Demographic Questionnaire [72] and the Neighborhood Environment Walkability Scale (NEWS73is obtained at baseline. Depression is assessed with the Emotional Distress-Depression-Short Form 8b [74], and is measured at baseline, post-initial intervention, post-augmented intervention, and follow-up.
2.8.2. Intervention targets
Intervention targets will be assessed with three different measures, each at the four time points of baseline, post-initial intervention, post-augmented intervention, and follow-up. Benefits and barriers will be assessed with the Exercise Benefits/Barriers Scale [75]. Self-efficacy will be measured with McAuley’s Self-Efficacy for Overcoming Barriers to physical activity [76]. Support is assessed with the Social Support and Exercise Survey, which was revised for physical activity [77].
2.8.3. Health status outcomes
To assess health status, measures will be used that examine both physical activity behavioral outcomes and cardiovascular health outcomes, and will be obtained at baseline, post-initial intervention, post-augmented intervention, and follow-up. While participants wear a Fitbit as part of the intervention, the primary measure of physical activity (number of steps/day, minutes of moderate/vigorous physical activity/week) will be assessed objectively with an ActiGraph [78,79]. As a secondary measure physical activity behavior will also be collected by self-report, with the International Physical Activity Questionnaire (IPAQ) - Long 7 Days Self-Administered has a set of 5 activity domains [80]. This self-reported physical activity data will be used for initial eligibility assessment and also to assess the relationship between self-reported and objectively reported physical activity on health outcomes.
Cardiovascular health outcomes will be assessed with several different measures. The primary measure of aerobic fitness (VO2max) will be assessed with the Two-minute step test, which requires the participant to step in place for two-minutes at a height half-way between the iliac crest and patella [63]. Secondary measures of body composition will be BMI (calculated from measures obtained with weight and height) [81], and waist circumference [82].
2.8.4. Data collection for cost-effectiveness analysis
Data for the cost-effectiveness analysis (Aim 4) will be obtained from study records and participant self-report. Program costs include the Fitbit equipment and database, text messages cost, staff time (calculated by an hourly wage) to write physical activity prescriptions for program orientation, and interventionists’ time to make motivational phone calls and lead group meetings. All participation will occur outside of work hours. Therefore all costs of participation are borne by the participants, and are primarily their opportunity costs, representing the value of their time spent in the intervention. These include program orientation attendance, and transportation if needed to and from program orientation. Dependent on the interventions that the participant is assigned to, time to review text messages, talk on personal calls, and attend group meetings, as well as transportation if needed to and from group meetings, will be assessed. There are no other direct (e.g. healthcare) or indirect (e.g. employer costs) associated with this intervention.
2.9. Data management
Several electronic resources will be used for data management. The Microsoft Access system will be used to manage participant recruitment, scheduling, consort report building, randomization, and tracking. The REDCap database will be used for data collection [83]. iCardia is hosted at the University of Illinois at Chicago, and will be used to remotely collect all Fitbit data generated by study participants, and to manage the delivery of text messages. iCardia is password-protected and hosted in a HIPAA-compliant server. iCardia provides researchers with a user-friendly dashboard that allows them to view each study participant’s physical activity data in the form of graphs, including battery level and time of last sync, and send personalized text-messages based on the incoming data [58,84]. All Fitbit data pertaining to steps and intensity of physical activity are exportable to Excel in a de-identified fashion (i.e. using random ID codes) for further statistical analysis. ActiLife software will be used to analyze the data from the ActiGraph monitors [85].
2.10. Data analysis plan
Statistical software programs SAS (v9.4) and R will be used for statistical analysis. Because multiple separate outcome measures are being evaluated in the primary aim, a two-tailed 0.01 significance level will be used for the statistical tests of these hypotheses. Secondary and exploratory aims will employ a standard two-tailed significance level of 0.05 for all statistical tests. All analyses will be performed on an intent-to-treat basis. A one-way analysis of variance will be conducted to look for potential diffusion effects. If significant differences are found, the estimated mean levels of diffusion will be used as weights in the efficacy analyses and cost analysis. Hypothesis testing will address four study aims.
2.10.1. Aim 1
Aim 1 is to compare the two augmented treatments used for non-responders, personal calls and group meetings, in improving physical activity and cardiovascular health after 35 and 50 weeks. This hypothesis will be tested using a multilevel analysis with time nested within participant (i.e., non-responders only). The hypothesis of the study is that the non-responders randomized to receive group meetings will demonstrate greater improvement in physical activity (device: number of steps/day, minutes of moderate/vigorous physical activity/week; cardiovascular fitness) compared to those randomized to receive personal calls. Secondary outcomes for Aim 1 are self-report life-style and occupational physical activity (minutes of moderate/vigorous physical activity per week), BMI, and waist circumference.
2.10.2. Aim 2a
Aim 2a is to compare enhanced physical activity monitor with and without text messages for improving the level of physical activity from baseline to 8 weeks. These analyses will parallel those used for Aim 1, but consider only two time points (baseline and 8 weeks) and include all participants. The hypothesis of the study is that those randomized to receive enhanced physical activity monitor + text messaging will demonstrate greater improvement in physical activity and cardiovascular health compared to those randomized to receive enhanced physical activity monitor alone.
2.10.3. Aim 2b
Aim 2 is to compare the four adaptive interventions in improving physical activity and cardiovascular health from baseline to 8, 34, and 50 weeks. The analysis is parallel to that described in Aim 1, except that the participants are not assigned to treatment based on simple randomization. Instead, they are screened on the basis of response status, and, once it has been ascertained that they did not respond to the initial treatment, they are randomly assigned to a treatment condition. Due to this design, the contrasts used to estimate the efficacy of these effects are nonorthogonal. The weights associated with the four interventions are then scored as a 4 for non-responder subgroups and 2 for responder subgroups. This is because responder subgroups are used twice in the design matrix (e.g., subgroup A is used in adaptive interventions 1 and 2; Figs. 2 and 3). The estimation of these models is then based on a weighted multilevel linear regression model that has terms for change over time, the initial treatment, the augmented treatment, the interaction between the two treatments, and the effects of baseline and time-varying characteristics [86]. The critical effect in this model is the time-by-adaptive-intervention interaction term. The null hypothesis is that there will be no interaction effect at all, while the alternative hypothesis is that adaptive intervention 4 (+ text messaging with group meetings [augmented for non-responders]) will produce the largest improvement rates.
2.10.4. Aim 3
Aim 3 will identify mediators and moderators of the initial and augmented treatments on physical activity and cardiovascular health. Using analytic models parallel to those for Aims 1 and 2, we will first test impact on intervention targets (benefits, barriers, self-efficacy, social support). Although we will test the impact of each treatment on all potential intervention targets, we anticipate variation in impact by treatment (e.g., initial treatment is less likely to impact social support). For intervention targets that are significantly impacted by treatment condition, we will test whether they serve as mediators of intervention effects on physical activity and health status outcomes using methods described by MacKinnon [87]. Moderation effects will be tested by adding moderator main effects and interactions of the moderators with condition and time. Significant moderator effects (i.e., significant moderator-by-time-by-treatment effects) will then be used to identify optimal intervention choices based on participant characteristics. For instance, participants with higher depression scores may respond more favorably to text messages than participants with lower depression scores. These optimal decision rules can then be cross-validated in future studies [88].
2.10.5. Aim 4
The cost-effectiveness analysis will be conducted from the societal perspective, including the program and participant costs. For the cost measurement, quantities of resources used and their associated prices will be collected for the program (either amounts paid or the value of the interventionist’s time), and participant (i.e., the value of the participant’s time to participate in the program). Program costs and participant costs will be calculated by summing their respective individual cost components, and these costs will be summed to calculate the total cost per participant.
For the effectiveness measurement, effectiveness will be measured using three measures of physical activity and cardiovascular health outcomes a)physical activity steps, b)moderate/vigorous physical activity, and c) aerobic fitness,). Cost-effectiveness will be evaluated by combining the mean total cost per participant with effectiveness (physical activity, cardiovascular health). We will calculate the incremental cost-effectiveness ratios (ICERs) for the four adaptive interventions: (1) enhanced physical activity monitor (initial) and enhanced physical activity monitor with personal calls (augmented); (2) enhanced physical activity monitor (initial) and enhanced physical activity monitor with group meetings (augmented); (3) enhanced physical activity monitor + text messaging (initial) and enhanced physical activity monitor+text messaging with personal calls (augmented); or (4) enhanced physical activity monitor+text messaging (initial) and enhanced physical activity monitor+text messaging with group meetings (augmented), such that the ICER = (Ci – Cj≠i)/(Ei – Ej≠i), where C denotes total cost and E denotes effectiveness. Effectiveness will be measured as the change in each outcome between baseline and study completion at 51–52 weeks. Subscript i denotes 1 of the 4 adaptive interventions, and subscript j denotes the comparison intervention group. We will calculate six sets of ICERs, one for each effectiveness measure; 95% confidence intervals will be calculated to evaluate the uncertainty in these results [89–91]. We will conduct one-way and multi-way sensitivity analyses for the key parameters to evaluate whether the ICERs are sensitive to plausible changes in their values. We will also plot acceptability curves based on varying threshold (willingness to pay) values for adherence and change in physical activity and cardiovascular health outcomes. Separate ICERs will be calculated from the program and participant perspectives.
2.11. Study limitations
Because this study is being conducted at a worksite, there is a possibility that participants who are in different interventions of the study will communicate with each other about the study. We believe this risk to be minimal because the physical activity monitor cannot be easily shared and the other treatments include individual tailoring. Despite this, we are monitoring diffusion of intervention across the groups. If we find significant differences in diffusion effects, we will adjust for this in the analysis. New waves do not start until the late adoption phase is completed or nearing completion for the previous wave, preventing temporal overlap of treatments. In addition, when women sign the study consent, they are informed of the type of interventions that they may be potentially randomized to receive. Given the second level of randomization into an augmented treatment if a woman is not active enough at 8 weeks (achieved < 600 daily steps above their daily baseline mean), it is a possibility that a participant would change their activity to be able to qualify for an augmented intervention. However we emphasize with all women at the beginning of the study, that it is important to try to achieve 600 or more daily steps above their average daily baseline mean.
3. Discussion
Walking provides a feasible and accessible way for most physically inactive working women to increase their physical activity. In 2017, the U.S. Surgeon General promoted walking, by publishing Step it up! The Surgeon General’s Call to Action to Promote Walking and Walkable Communities. The publication emphasized the many wonderful benefits of walking, and showcased walking as a realistic and feasible physical activity for the vast majority of Americans [92]. While walking is good for everyone, women already walk more for leisure in comparison to men [93]. This is important because it represents a physical activity gateway to obtain aerobic physical activity. After increasing frequency with walking (obtaining more steps), the next recommended step is to increase intensity by walking faster, as a way to obtain moderate-intensity physical activity, and therefore accrue aerobic physical activity for greater health benefits. In 2018, the 2nd edition of The Physical Activity Guidelines for Americans was published by the U.S. Department of Health and Human Services. The multiple benefits of physical activity were emphasized, and the 10-minute recommended bout of physical activity was eliminated, as it was recognized that benefits from physical activity can occur in very short bouts. Walking briskly, even for short periods of time, is one way to meet the recommended physical activity aerobic guidelines [1]. However, despite the strong recommendations to be physically active and the evidence that small amounts of physical activity are helpful in becoming healthier, many women continue to have challenges improving their physical activity.
When testing interventions with women to improve physical activity, specifically walking, a one-size fits all approach does not work for every woman. The SMART design allows for the researcher to deliver an intervention that takes into account if a participant is not responding to an initial treatment, and then add an augmented treatment as needed. In this study, a SMART trial will test which interventions alone or in combination with another intervention, work best to improve physical activity in working women [24,94]. In our study, increasing physical activity, as measured by daily steps is the main outcome. Responder and non-responder status, using decision rules is based on number of steps increased over baseline steps. Strengthening our study is obtaining ongoing step data from the Fitbit [57], and obtaining an objective measure of physical activity with an ActiGraph [79].
In conclusion, walking is a form of physical activity that the vast majority of Americans can safely engage in. The benefits of walking on a regular basis, with some of the walking being at a brisk pace, are well known. This study rigorously assesses which adaptive interventions work best for women ages 18 to 70. Using a SMART design, we will determine which of four adaptive interventions (combinations of physical activity monitor, text messaging, personal calls, and group meetings) best improves physical activity outcomes for employed women who are not regularly physically active. Results of this study will add to the body of literature on improving physical activity in employed women. This study will identify effective interventions that reduce costs and burden to women who respond to less intensive treatments, while maximizing benefits for those who need a more intensive approach.
Acknowledgements
We wish to thank Dr. Lola Coke, Mr. Peter Cummings, Dr. Louis Fogg, Dr. Diana Ingram, and Dr. Inbal Nahum-Shani for their assistance with this study protocol.
Funding
This work is funded by the National Institutes of Health, National Institute of Nursing Research R01 NR017635.
References
- [1].U.S. Department of Health and Human Services, Physical Activity Guidelines for Americans, 2nd edition, U.S. Department of Health and Human Services, Washington, D.C., 2018https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf, Accessed date: 8 June 2019. [Google Scholar]
- [2].Benjamin EJ, Virani SS, Callaway CW, et al. , Heart disease and stroke statistics-2018 update: a report from the American Heart Association, Circulation. 137 (12) (2018) e67–e492. [DOI] [PubMed] [Google Scholar]
- [3].National Center for Health Statistics. Health, united states, 2017: With special feature on mortality. Hyattsville, MD:; 2018. https://www.cdc.gov/nchs/data/hus/hus17.pdf. (Accessed June 8, 2019). [PubMed] [Google Scholar]
- [4].Buckley JP, Hedge A, Yates T, et al. , The sedentary office: an expert statement on the growing case for change towards better health and productivity, Br. J. Sports Med 49 (2015) 1357–1362. [DOI] [PubMed] [Google Scholar]
- [5].Bureau of Labor Statistics. Employment status of the civilian noninstitutional population by age, sex, and race,” Current Population Survey. https://www.bls.gov/cps/cpsaat03.htm. Updated 2019.
- [6].World Health Organization. Physical activity and women. http://www.who.int/dietphysicalactivity/factsheet_women/en/. Updated n.d.
- [7].Joseph RP, Ainsworth BE, Keller C, Dodgson JE, Barriers to physical activity among African American women: an integrative review of the literature, Women Health 55 (6) (2015) 679–699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Family Caregiver Alliance, Women and Caregiving: Facts and Figures, https://www.caregiver.org/print/240, (Updated 2015), Accessed date: 5 January 2016.
- [9].Pender N, Murdaugh L, Parsons MA, Health Promotion in Nursing Practice, 7th edition, Pearson, 2015. [Google Scholar]
- [10].Bandura A, Health promotion by social cognitive means, Health Educ. Behav 31 (2) (2004) 143–164. [DOI] [PubMed] [Google Scholar]
- [11].Maddison R, Pfaeffli L, Stewart R, et al. , The HEART mobile phone trial: the partial mediating effects of self-efficacy on physical activity among cardiac patients, Front. Public Health 2 (2014) 56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Buchholz SW, Factors that Affect Physical Activity Self-Efficacy in African American Women With Hypertension. [PhD], Wayne State University, Detroit, MI, 2003. [Google Scholar]
- [13].Oyibo K, Adaji I, Vassileva J, Social cognitive determinants of exercise behavior in the context of behavior modeling: a mixed method approach, Digit. Health 4 (2018) 2055207618811555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Edwards ES, Sackett SC, Psychosocial variables related to why women are less active than men and related health implications, Clin. Med. Insights Womens Health 9 (Suppl. 1) (2016) 47–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Cadmus-Bertram L, Marcus BH, Patterson RE, Parker BA, Morey BL, Use of the Fitbit to measure adherence to a physical activity intervention among over-weight or obese, postmenopausal women: self-monitoring trajectory during 16 weeks, JMIR Mhealth Uhealth 3 (4) (2015) e96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Buchholz S, Wilbur J, Ingram D, Fogg L. Physical activity text messaging interventions in adults: A systematic review. Worldviews on Evidence-Based Nursing. 2013;Early View. [DOI] [PubMed] [Google Scholar]
- [17].Buchholz SW, Ingram D, Wilbur J, et al. , Bilingual Text4Walking food service employee intervention pilot study, JMIR mHealth UHealth 4 (2) (2016) e68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Conn VS, Hafdahl AR, Moore SM, Nielsen PJ, Brown LM, Meta-analysis of interventions to increase physical activity among cardiac subjects, Int. J. Cardiol 133 (3) (2009) 307–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Kahn EB, Ramsey LT, Brownson RC, et al. , The effectiveness of interventions to increase physical activity. A systematic review, Am. J. Prev. Med 22 (4 Suppl) (2002) 73–107. [DOI] [PubMed] [Google Scholar]
- [20].Goode AD, Lawler SP, Brakenridge CL, Reeves MM, Eakin EG, Telephone, print, and web-based interventions for physical activity, diet, and weight control among cancer survivors: a systematic review, J. Cancer Surviv 9 (4) (2015) 660–682. [DOI] [PubMed] [Google Scholar]
- [21].Muller AM, Khoo S. Non-face-to-face physical activity interventions in older adults: a systematic review. Int. J. Behav. Nutr. Phys. Act 2014;11(1):35–5868–11–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Parra-Medina D, Wilcox S, Salinas J, et al. , Results of the heart healthy and ethnically relevant lifestyle trial: a cardiovascular risk reduction intervention for African American women attending community health centers, Am. J. Public Health 101 (10) (2011) 1914–1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Wilbur J, Miller AM, Fogg L, et al. , Randomized clinical trial of the women’s lifestyle physical activity program for African-American women: 24- and 48-week outcomes, Am. J. Health Promot (5) (2016) 333–345. [DOI] [PubMed] [Google Scholar]
- [24].Almirall D, Nahum-Shani I, Sherwood NE, Murphy SA, Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research, Transl. Behav. Med 4 (3) (2014) 260–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kidwell KM, Postow MA, Panageas KS, Sequential, multiple assignment, randomized trial designs in immuno-oncology research, Clin. Cancer Res 24 (4) (2018) 730–736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Kidwell KM, Hyde LW, Adaptive interventions and SMART designs: application to child behavior research in a community setting, Am. J. Eval 37 (3) (2016) 344–363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Meurer WJ, Seewald NJ, Kidwell K, Sequential multiple assignment randomized trials: an opportunity for improved design of stroke reperfusion trials, J. Stroke Cerebrovasc. Dis 26 (4) (2017) 717–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Sherwood NE, Butryn ML, Forman EM, et al. , The BestFIT trial: a SMART approach to developing individualized weight loss treatments, Contemp. Clin. Trials 47 (2016) 209–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Pfammatter AF, Nahum-Shani I, DeZelar M, et al. , SMART: study protocol for a sequential multiple assignment randomized controlled trial to optimize weight loss management, Contemp. Clin. Trials 82 (2019) 36–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Naar-King S, Ellis DA, Idalski Carcone A, et al. , Sequential multiple assignment randomized trial (SMART) to construct weight loss interventions for African American adolescents, J. Clin. Child Adolesc. Psychol (2015) 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Almirall D, Nahum-Shani I, Sherwood NE, Murphy SA, Introduction to SMART designs for the development of adaptive interventions: with application to weight loss research, Transl. Behav. Med 4 (3) (2014) 260–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Collins LM, Nahum-Shani I, Almirall D , Optimization of behavioral dynamic treatment regimens based on the sequential, multiple assignment, randomized trial (SMART), Clin. Trials 11 (4) (2014) 426–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Conn V, Hafdahl A, Cooper P, Brown L, Lusk S, Meta-analysis of workplace physical activity interventions, Am. J. Prev. Med 37 (4) (2009) 330–339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Wilbur J, Chandler P, Miller AM, Measuring adherence to a women’s walking program, West. J. Nurs. Res 23 (1) (2001) 8–24 (discussion 24–32). [DOI] [PubMed] [Google Scholar]
- [35].Diaz KM, Krupka DJ, Chang MJ, et al. , Fitbit(R): an accurate and reliable device for wireless physical activity tracking, Int. J. Cardiol 185 (2015) 138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Tudor-Locke C, Hatano Y, Pangrazi R, Kang M, Revisiting “how many steps are enough?”, Med. Sci. Sports Exerc 40 (7 Suppl) (2008) S537–S543. [DOI] [PubMed] [Google Scholar]
- [37].Bassett D, Wyatt H, Thompson H, Peters J, Hill J, Pedometer-measured physical activity and health behaviors in U.S. adults, Med. Sci. Sports Exerc 42 (10) (2010) 1819–1825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Marshall SJ, Levy SS, Tudor-Locke CE, et al. , Translating physical activity recommendations into a pedometer-based step goal: 3000 steps in 30 minutes, Am. J. Prev. Med 36 (5) (2009) 410–415. [DOI] [PubMed] [Google Scholar]
- [39].Slaght J, Senechal M, Hrubeniuk TJ, Mayo A, Bouchard DR, Walking cadence to exercise at moderate intensity for adults: a systematic review, J. Sports Med. (Hindawi Publ. Corp.) 2017 (2017) 4641203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Wilbur J, McDevitt JH, Wang E, et al. , Outcomes of a home-based walking program for African-American women, Am. J. Health Promot. 22 (5) (2008) 307–317. [DOI] [PubMed] [Google Scholar]
- [41].McSweeney JC, Rosenfeld AG, Abel WM, et al. , Preventing and experiencing ischemic heart disease as a woman: state of the science: a scientific statement from the American Heart Association, Circulation. 133 (13) (2016) 1302–1331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Pew Research Center, Mobile fact sheet, https://www.pewinternet.org/fact-sheet/mobile/, (Updated 2019), Accessed date: 14 September 2019.
- [43].American Diabetes Association, 2. classification and diagnosis of diabetes, Diabetes Care 39 (Suppl. 1) (2016) S13–S22. [DOI] [PubMed] [Google Scholar]
- [44].Canadian Society for Exercise Physiology, Par-Q & you (revised 2002), http://www.csep.ca/cmfiles/publications/parq/par-q.pdf.
- [45].American College of Sports Medicine, ACSM’s Guidelines for Exercise Testing and Prescription, 9th edition, Wolters Kluwer, Lippincott Williams and Wilkins, Philadelphia, 2014. [Google Scholar]
- [46].Canadian Society for Exercise Physiology, Canadian physical activity guidelines and Canadian sedentary behaviour guidelines, retrieved from http://www.csep.ca/cmfiles/guidelines/csep_guidelines_handbook.pdf, (Updated 2012), Accessed date: 7 April 2016.
- [47].Oetting AI, Levy JA, Weiss RD, Murphy SA, Shrout PE, Keyes KM, Ornstein K, Statistical methodology for a SMART design in the development of adaptive treatment strategies, in: Shrout PE, Keyes KM, Ornstein K (Eds.), Causality and Psychopathology: Finding the Determinants of Disorders and Their Cures, 2011, pp. 179–205. [Google Scholar]
- [48].Goode A, Reeves M, Eakin E, Telephone-delivered interventions for physical activity and dietary behavior change. An updated systematic review, Am. J. Prev. Med 42 (1) (2012) 81–88. [DOI] [PubMed] [Google Scholar]
- [49].Wilbur J, Buchholz SW, Ingram DM, Braun LT, Johnson TJ, Fogg L, Miller AM, Volgman AS, McDevitt J, Effectiveness, efficiency, durations, and costs of recruiting for an African American Women’s lifestyle physical activity program, Res. Nurs. Health 36 (5) (2013;October) 487–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Wilbur J, McDevitt J, Wang E, et al. , Recruitment of African American women to a walking program: eligibility, ineligibility, and attrition during screening, Res. Nurs. Health 29 (3) (2006) 176–189. [DOI] [PubMed] [Google Scholar]
- [51].Wilbur J, Miller AM, Chandler P, Recruitment and cardiovascular risk characteristics of African American and Caucasian midlife women, J. Cardiovasc. Nurs 15 (3) (2001) 88–104. [DOI] [PubMed] [Google Scholar]
- [52].Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA, A “SMART” design for building individualized treatment sequences, Annu. Rev. Clin. Psychol 8 (2012) 21–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Buchholz SW, Wilbur J, Schoeny ME, et al. , Retention of African American women in a lifestyle physical activity program, West. J. Nurs. Res 38 (3) (2015) 369–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Bennett JA, Mediator and moderator variables in nursing research: conceptual and statistical differences, Res. Nurs. Health 23 (5) (2000) 415–420. [DOI] [PubMed] [Google Scholar]
- [55].Alharbi M, Bauman A, Neubeck L, Gallagher R, Validation of Fitbit-flex as a measure of free-living physical activity in a community-based phase III cardiac rehabilitation population, Eur. J. Prev. Cardiol 23 (14) (2016) 1476–1485. [DOI] [PubMed] [Google Scholar]
- [56].Dishman R, Determinants of participation in physical activity, in: Bouchard C, Shepard T, Stephens J, Sutton J, McPherson B (Eds.), Vol Exercise, Fitness and Health, Human Kinetics, Champaign, IL, 1990, pp. 75–102. [Google Scholar]
- [57].Fitbit Charge HR. https://www.fitbit.com/chargehr. Accessed November 30, 2015.
- [58].Kitsiou S, Thomas M, Marai E, et al. , Development of an innovative mHealth platform for remote physical activity monitoring and health coaching of cardiac rehabilitation patients. Biomedical & Health Informatics, 2017 IEEE EMBS International Conference, 2017. [Google Scholar]
- [59].Emmons KM, Rollnick S , Motivational interviewing in health care settings. Opportunities and limitations, Am. J. Prev. Med 20 (1) (2001) 68–74. [DOI] [PubMed] [Google Scholar]
- [60].Buchholz SW, Ingram DM, Wilbur J, Pelt PP , Using photos to develop text messages to promote walking, J. Nurs. Scholarsh 45 (4) (2013) 380–387. [DOI] [PubMed] [Google Scholar]
- [61].Resnicow K, Jackson A, Braithwaite R, et al. , Healthy body/healthy spirit: a church-based nutrition and physical activity intervention, Health Educ. Res 17 (5) (2002) 562–573. [DOI] [PubMed] [Google Scholar]
- [62].Webex Cisco, Video Conferencing You Can Trust, https://www.webex.com/, (Updated 2019), Accessed date: 16 September 2019.
- [63].Rikli R, Jones CJ, Senior Fitness Test Manual, Human Kinetics, Champaign, Illinois, 2001. [Google Scholar]
- [64].Resnick B, Inguito P, Orwig D, et al. , Treatment fidelity in behavior change research: a case example, Nurs. Res 54 (2) (2005) 139–143. [DOI] [PubMed] [Google Scholar]
- [65].Bellg AJ, Borrelli B, Resnick B, et al. , Enhancing treatment fidelity in health behavior change studies: best practices and recommendations from the NIH behavior change consortium, Health Psychol. 23 (5) (2004) 443–451. [DOI] [PubMed] [Google Scholar]
- [66].Wilbur J, Schoeny ME, Buchholz SW, et al. , Women’s lifestyle physical activity program for African American women: fidelity plan and outcomes, J. Phys. Act. Health 13 (10) (2016) 1100–1109. [DOI] [PubMed] [Google Scholar]
- [67].To QG, Chen TT, Magnussen CG, To KG, Workplace physical activity interventions: a systematic review, Am. J. Health Promot 27 (6) (2013) e113–e123. [DOI] [PubMed] [Google Scholar]
- [68].Moyers T, Martin T, Manuel J, Miller W, Ernst D, Revised Global Scales: Motivational Interviewing Treatment Integrity 3.0 (MITI 3.0), University of New Mexico, Albuquerque, 2007. [Google Scholar]
- [69].Breitenstein S, Gross D, Garvey C, Hill C, Fogg L, Resnick B, Implementation fidelity in community-based interventions, Res. Nurs. Health 33 (2) (2010) 164–173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Gerber B, Stolley M, Thompson A, Sharp L, Fitzgibbon M, Mobile phone text messaging to promote healthy behaviors and weight loss maintenance: a feasibility study, Health Inform. J 15 (1) (2009) 17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Bear M, Bowers C, Using a nursing framework to measure client satisfaction at a nurse-managed clinic, Public Health Nurs. 15 (1) (1998) 50–59. [DOI] [PubMed] [Google Scholar]
- [72].Neighborhood Quality of Life Study, Neighborhood Quality of Life Study, http://www.drjamessallis.sdsu.edu/Documents/NQLS_S1.pdf, (Updated 2004), Accessed date: 19 April 2011.
- [73].Saelens B, Sallis J, Black J, Chen D, Neighborhood-based differences in physical activity: an environment scale evaluation, Am. J. Public Health 93 (9) (2003) 1552–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].National Institutes of Health, PROMIS® available instruments, http://www.nihpromis.org/measures/availableinstruments, (Updated 2015), Accessed date: 13 January 2016.
- [75].Sechrist KR, Walker SN, Pender NJ, Development and psychometric evaluation of the exercise benefits/barriers scale, Res. Nurs. Health 10 (6) (1987) 357–365. [DOI] [PubMed] [Google Scholar]
- [76].McAuley E, Jacobson L, Self-efficacy and exercise participation in sedentary adult females, Am. J. Health Promot 5 (3) (1991) 185–191. [DOI] [PubMed] [Google Scholar]
- [77].Sallis JF, Grossman RM, Pinski RB, Patterson TL, Nader PR, The development of scales to measure social support for diet and exercise behaviors, Prev. Med 16 (6) (1987) 825–836. [DOI] [PubMed] [Google Scholar]
- [78].McClain JJ, Craig CL, Sisson SB, Tudor-Locke C, Comparison of Lifecorder EX and ActiGraph accelerometers under free-living conditions, Appl. Physiol. Nutr. Metab 32 (4) (2007) 753–761. [DOI] [PubMed] [Google Scholar]
- [79].ActiGraph, ActiGraph wgt3x-bt, https://actigraphcorp.com/actigraph-wgt3x-bt/, (Updated 2019), Accessed date: 16 September 2019.
- [80].IPAQ Group. IPAQ - International Physical Activity Questionnaire. https://sites.google.com/site/theipaq/. Updated (n.d.).
- [81].Heyward VH, Advanced Fitness Assessment and Exercise Prescription, 5th ed., Human Kinetics, Champaign, IL, 2006. [Google Scholar]
- [82].National Institutes of Health, National Heart, Lung, and Blood Institute, NHLBI Obesity Education Initiative, North American Association for the Study of Obesity, The Practical Guide Identification, Evaluation, and Treatment of Overweight and Obesity in Adults, National Institutes of Health, Rockville, Maryland, 2000. [Google Scholar]
- [83].Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG, Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support, J. Biomed. Inform 42 (2) (2009) 377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Kitsiou S, Arena R, Kondos G, Gerber B , iCardia: a pilot mHealth technology for remote monitoring of physical activity and exercise (abstract), UIC College of Medicine Research Conference, University of Illinois at Chicago, April, 2016. [Google Scholar]
- [85].ActiGraph, ActiLife software, https://www.actigraphcorp.com/support/software/actilife/, (Updated 2019), Accessed date: 1 October 2019.
- [86].Nahum-Shani I, Qian M, Almirall D, et al. , Experimental design and primary data analysis methods for comparing adaptive interventions, Psychol. Methods 17 (4) (2012) 457–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [87].MacKinnon DP, Introduction to Statistical Mediation Analysis, Routledge, New York, 2008. [Google Scholar]
- [88].Nahum-Shani I, Qian M, Almirall D, et al. , Q-learning: a data analysis method for constructing adaptive interventions, Psychol. Methods 17 (4) (2012) 478–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [89].Polsky D, Glick HA, Willke R, Schulman K, Confidence intervals for cost-effectiveness ratios: a comparison of four methods, Health Econ. 6 (3) (1997) 243–252. [DOI] [PubMed] [Google Scholar]
- [90].Tambour M, Zethraeus N, Bootstrap confidence intervals for cost-effectiveness ratios: some simulation results, Health Econ. 7 (2) (1998) 143–147. [DOI] [PubMed] [Google Scholar]
- [91].Briggs AH, Wonderling DE, Mooney CZ, Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation, Health Econ. 6 (4) (1997) 327–340. [DOI] [PubMed] [Google Scholar]
- [92].U.S. Department of Health and Human Services. Step it up! the surgeon general’s call to action to promote walking and walkable communities. http://www.surgeongeneral.gov/library/calls/walking-and-walkable-communities/call-to-action-walking-and-walkable-communites.pdf. Updated 2015. [PubMed]
- [93].Pollard TM, Wagnild JM. Gender differences in walking (for leisure, transport and in total) across adult life: a systematic review. BMC Public Health 2017;17(1):341–017–4253–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Collins LM, Murphy SA, Strecher V, The multiphase optimization strategy (MOST) and the sequential multiple assignment randomized trial (SMART): new methods for more potent eHealth interventions, Am. J. Prev. Med 32 (5 Suppl) (2007) S112–S118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [95].Choi SW, Schalet B, Cook KF, Cella D, Establishing a common metric for depressive symptoms: linking the BDI-II, CES-D, and PHQ-9 to PROMIS depression, Psychol. Assess 26 (2) (2014) 513–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Marrie RA, Zhang L, Lix LM, et al. , The validity and reliability of screening measures for depression and anxiety disorders in multiple sclerosis, Mult. Scler. Relat. Disord 20 (2018) 9–15. [DOI] [PubMed] [Google Scholar]
- [97].Wilbur J, Reducing health disparity in African American women: Adherence to physical activity, (2009) RO1 NR04234($3110902).
- [98].Sallis JF, The development of self-efficacy scales for health-related diet and exercise behaviors, Health Educ. Res 3 (3) (1988) 283–292. [Google Scholar]
- [99].Craig CL, Marshall AL, Sjostrom M, et al. , International physical activity questionnaire: 12-country reliability and validity, Med. Sci. Sports Exerc 35 (8) (2003) 1381–1395. [DOI] [PubMed] [Google Scholar]
- [100].Chen H, Lin C, Yu L, Normative physical fitness scores for community-dwelling older adults, J. Nurs. Res 17 (1) (2009) 30–41. [DOI] [PubMed] [Google Scholar]
- [101].Kuczmarski MF, Kuczmarski RJ, Najjar M, Findings from the third national health and nutrition examination survey, 1988–1994, J. Am. Diet. Assoc 101 (1) (2001) 28–34 (quiz 35–6). [DOI] [PubMed] [Google Scholar]


