Abstract
The mental health of adult extremely low birth weight (ELBW) (<1000 g) survivors is poorer than their normal birth weight (NBW) peers. An understanding of the modifiable factors that affect this risk could provide targets for intervention. We set out to determine the extent to which a maternal history of mental health problems influenced mental health in ELBW and NBW offspring in adulthood. A total of 85 ELBW and 88 NBW individuals born between 1977 and 1982 in central west Ontario, Canada self-reported on internalizing (depression, anxiety) and externalizing (attention-deficit hyperactivity and antisocial) problems using the Diagnostic and Statistical Manual of Mental Disorders (DSM) scales of the Young Adult Self-Report at ages 22–26 and 30–35. They also reported on their mother’s maternal mental health using the Family History Screen. An interaction was found between birth weight status and maternal history of an anxiety disorder such that ELBW survivors showed a greater increase in internalizing scores than NBW participants at 22–26 (β = 10.27, p = 0.002) and at 30–35 years of age (β = 12.65, p = 0.002). An interaction was also observed between birth weight and maternal history of mood disorder, with higher externalizing scores in ELBW survivors than NBW adults at 22–26 (β = 7.21, p < 0.0001). ELBW adults appear to be more susceptible to the adverse mental health effects of exposure to maternal mood and anxiety disorders than those born at NBW. These links further highlight the importance of detecting and treating mental health problems in the parents of preterm survivors as a means of attempting to reduce the burden of psychopathology in this population.
Keywords: Mental disorders, risk, infant, extremely low birth weight, medical history taking, maternal
Introduction
The proportion of deliveries occurring preterm has increased significantly since the 1980s.1,2 Advances in neonatal care have substantially decreased premature mortality rates among preterm survivors, resulting in an increased number of these infants surviving into adulthood.3–5 As survival rates have increased, more attention has been paid to the longer term mental and physical health of those born preterm. This research suggests that a gradient of risk exists in these individuals such that those born smaller are more susceptible to a range of morbidities.6
Infants born at extremely low birth weight (ELBW; <1000 g) are the smallest and most vulnerable survivors of prematurity. In childhood, ELBW survivors have more health problems than those born at NBW. ELBW children have high rates of chronic conditions such as asthma and cerebral palsy when compared to NBW children, as well as more cognitive, academic, and motor problems, and reduced adaptive social functioning.7
Mental health problems are also more common in preterm survivors, including those born at ELBW, and these often first emerge in childhood and adolescence.8 By early adulthood, ELBW survivors are at greater risk for depression and anxiety relative to those born at NBW.8,9 They may also continue to have more difficulties with attention-deficit/hyperactivity disorder (ADHD) and social skills, but manifest fewer alcohol and drug use problems.10,11 However, not all individuals born preterm have mental health problems in adulthood, and it is important to understand this heterogeneity since it can help direct efforts aimed at early identification, prevention, and effective treatment.10
Why rates of mental disorders are increased in those born at ELBW is not entirely understood. In keeping with the developmental origins of health and disease (DOHaD) hypothesis, it has been suggested that exposure to significant adversity during gestation and/or early postnatal life can increase risk. Adaptations made by the fetus and infant in response to these adversities can affect stress response systems such as the hypothalamic–pituitary–adrenal axis,12 as well as those involved in emotional and cognitive processing,13 leading to increased susceptibility to mental disorders across the lifespan. Complicating matters further are studies that suggest that postnatal exposures that are easily observable by parents, teachers, and healthcare professionals like motor coordination problems14 and cognitive difficulties15,16 may have less impact than those that are less immediately obvious (e.g., childhood sexual abuse, psychiatric problems),17,18 because the former group are likely to receive additional social, educational, and medical support and intervention.
Studies of the mental health of ELBW survivors generally support a cumulative risk pattern,17,19,20 while relatively few are consistent with differential susceptibility theory in that those born at ELBW may be more or less vulnerable to mental illness depending on their unique biological sensitivity and subsequent exposures.21 Based on the cumulative risk model of psychopathology, one would expect that parental mental disorders would serve to further amplify the risk of mental health problems in ELBW survivors. Parental mental illness is not only associated with an increased genetic risk, but may influence the development of psychopathology via modeling and parenting, both which can be adversely affected by the stresses of raising a preterm-born infant/child.22,23 Goodman and Gotlib proposed an integrative model for the transmission of risk to children of mothers with depression; this included heritability, exposure to mother’s maladaptive behaviors and affect, exposure to stressful environments, and an innate dysfunction in offspring’s neuroregulatory mechanisms.23 This neuroregulatory dysfunction may be due to abnormal development caused by antenatal maternal depression, inadequate healthcare or other factors, and ties into the alterations seen in response to antenatal stress as part of the DOHaD model.
A parental history of depression or anxiety has been found to predict depression and anxiety in offspring in general population samples.24 Nomura and colleagues found that children born at less than 2500 g (low birth weight, LBW) had an increased risk of depression if a parent was diagnosed with major depressive disorder (though this study included only 20 LBW individuals).25 Moreover, Walshe et al. found an increased risk of psychiatric disorder in very preterm (<33 weeks gestational age) individuals who had a first degree relative with a history of psychiatric illness.26 However, they focused on how this affected risk within very low birth weight (VLBW) survivors only, and did not compare them to NBW controls.
It is important to point out that the impact of familial psychopathology on psychiatric risk in the most vulnerable preterm survivors (e.g., those born ELBW) is still lacking. Although paternal mental health contributes to child development, maternal mental health is often the central focus of developmental research; the primary reason being the assumption that the mothers’ involvement in daily childcare activities is greater than that of the fathers’.27 This is particularly true of the 1970s–1980s.28
Understanding the impact of a maternal history of mental disorders could aid in the prediction of mental health risk in preterm survivors, as well as provide targets for intervention that could optimize the health and quality of life of those born preterm. Given the immense costs associated with mental disorders and the negative impact they can have on the lives of prematurely born individuals and their families, identifying modifiable exposures that affect these risks is an important priority.
Using the oldest known prospectively followed cohort of ELBW survivors, the current study utilized the Family History Screen (FHS)29 to examine the moderating effect of birth weight status on the impact maternal depression or anxiety on the development and persistence of internalizing (depression and anxiety) and externalizing (antisocial, ADHD) problems in a cohort of ELBW survivors and normal birth weight (NBW) control participants in their 20s and 30s. We also investigated if these effects were amplified in ELBW adults.
Methods
Sample
The original ELBW sample consisted of 397 ELBW individuals born in central-west Ontario, Canada between 1977 and 1982. Of these infants, 179 survived to discharge, with 142 providing data at the 22–26 year visit and 100 at the 30–35 year follow-up. A group of 145 NBW individuals were matched with the ELBW participants on age, sex, and parental socioeconomic status as measured by self-reported household income when both groups were 8 years of age. Of these, 133 (93%) were available and provided data at the 22–26 year assessment and 89 at the 30–35 year follow-up. This study includes 85 ELBW participants and 88 NBW participants that completed the FHS at the 30–35 year visit. Data collection procedures regarding participant psychopathology for these visits are outlined in Boyle et al.9 and Van Lieshout et al.10
Measures
Predictor: maternal psychopathology
The FHS is a semi-structured interview used to assess symptoms of psychopathology among family members.29 For the purpose of the present study, we utilized the presence of any mood disorder (major depressive disorder or mania/hypomania) or any anxiety disorder (generalized anxiety disorder, agoraphobia, panic, social anxiety disorder, obsessive compulsive disorder) within the lifetime of the individual’s biological mother. This was reported on by the individual retrospectively, at the 30–35 year visit. Maternal mental health was chosen over paternal or combined parental health as at the time these infants were born, mothers had the primary role in child-rearing and therefore likely had the strongest effects on the development of offspring mental health.28 Following Diagnostic and Statistical Manual of Mental Disorders (DSM)-III-R criteria, the FHS has shown to be valid in identifying the aforementioned disorders as the κ coefficients for agreement between clinicians are as follows: 0.9 for any mood disorder and 0.7 for any anxiety disorder.29
Outcome: psychopathology at age 22–26 and age 30–35
Psychopathology was measured as a continuous concept using the Young Adult Self-Report (YASR).30 The YASR is a self-administered checklist comprised of 130 items (0, not true; 1, somewhat or sometimes true; and 2, very true or often true). To increase clinical relevance, we utilized those items and categories found to be consistent with diagnoses in the DSM-IV.31,32 This resulted in categories consistent with depressive, anxiety, avoidant personality, ADHD, and antisocial personality problems. These groups were collapsed into two broader categories: internalizing problems and externalizing problems. These two broader scales were chosen in order to optimize statistical power and because ELBW survivors were previously found to present with more internalizing problems than NBW control participants,9 and fewer externalizing problems.10 Internalizing problems included depressive, anxiety, and/or avoidant personality problems, while externalizing problems were antisocial personality and/or ADHD problems.
Birth variables
Infants’ sex, birth weight, and gestational age were recorded at birth and collected from their medical charts for ELBW individuals. For NBW controls, parents reported on these variables.
Covariates
Chronic health problems
Individuals with chronic health conditions are significantly more likely to develop psychiatric disorders,33 and preterm-born individuals are more likely to develop chronic health problems. Chronic health problems were defined as a count of chronic illnesses/conditions that persisted for at least 6 months and were taken from 24 categories of illnesses/conditions that included asthma, cardiovascular disease, and visual and hearing impairments. These were identified when participants were 12–16 years of age.
Emotional and behavioral problems at ages 12–16
Adolescent emotional and behavioral problems are commonly associated with concurrent psychopathology and can act as a confounder for outcomes specifically examined in adulthood.34 As this work aimed to show the impact of birth weight and maternal mental health on adult psychopathology specifically, we chose to adjust for this covariate in order to attempt to isolate their joint impact on psychopathology in adulthood. For example, this method has been used in several other studies of adult psychopathology in preterm survivors including those from Canada9,35 and Australia.36
Emotional and behavioral problems were measured at age 12–16 using the Ontario Child Health Study-Revised scales (OCHS-R).37 The items comprising these scales assess emotional–behavioral problems occurring in the previous 6 months (0, never or not true; 1, somewhat or sometimes true; and 2, very or often true). The OCHS-R scales contain psychiatric symptoms that are characteristic of the following DSM-III-R diagnoses: conduct disorder, oppositional disorder, ADHD, overanxious disorder, separation anxiety, and depression.37 In the YASR externalizing model, we adjusted for symptoms that were associated with conduct disorder, oppositional disorder, and ADHD as they are related to adult externalizing problems. In the YASR internalizing model, symptoms related to depression, overanxious disorder, and separation anxiety were controlled for as they are more predictive of later internalizing problems.
Intelligence quotient
Childhood intelligence quotient (IQ) is also associated with later psychopathology38 and is known to be reduced in preterm survivors.39,40 For this reason, we also chose to adjust statistically for this variable. All children completed the Wechsler Intelligence Scale for Children-Revised (WISC-R) at age 8.41 The subscales of the measure included verbal (similarities, mental arithmetic, and vocabulary) and performance (picture arrangement and block design). These items are then used to calculate an estimated IQ score, which has been shown to have a 0.96 correlation with the full-scale WISC-R-IQ.42
Informed consent
The study was given approval by the Ethics Committee of Hamilton Health Sciences, and the parents of all participants provided written consent prior for child and adolescent visits and the participants provided their own written consent for the two adult assessments (i.e., age 22–26 and 30–35).
Statistical analyses
Group differences between ELBW survivors and NBW control participants were analyzed using χ2 tests and Student’s t-tests. Associations between maternal mood or anxiety disorders and internalizing or externalizing problems of offspring at age 22–26 and 30–35 were examined using linear regression. All models were adjusted for sex, IQ at 8 years of age, chronic health problems at ages 12–16 as well as emotional problems at ages 12–16 for adult internalizing outcomes, and behavioral problems at ages 12–16 when predicting externalizing psychopathology in adulthood.
Effect modification by birth weight status was assessed through the addition of a multiplicative birth weight by maternal mood or anxiety disorder interaction term. Both models were then stratified by birth weight to examine associations with internalizing and externalizing among ELBW survivors and NBW control participants separately. All statistical tests were two-tailed with a significance level set at 0.05. Both complete case analysis and Markov chain Monte Carlo multiple imputation were conducted for all analyses. When pooling the estimates from 15 imputed datasets, the birth weight interaction no longer meets the arbitrary cutoff of statistical significance (Supplementary Table S1) for maternal anxiety disorder at 30–35 years, but does support the same directionality of the association using a complete case analysis. Using both approaches, the stratified models support the observation that ELBW infants show a heightened risk for psychopathology, and so the results of the complete case analysis are presented. Predictors of loss to follow-up were examined including birth weight status, sex, gestational age, teen emotional and behavioral problems, chronic health problems, and IQ (Supplementary Table S2).
Results
Sample characteristics can be found in Table 1. The mean (SD) age of ELBW individuals at the 22–26-year-old assessment was 23.30 (1.2) years and 23.61 (1.0) for the NBW group. At the 30–35-year-old assessment, the mean (SD) age of ELBW individuals was 32.06 (1.69) years and 32.50 (1.36) for the ELBW group (both p’s < 0.05). The ELBW survivors also had more chronic health problems 2.11 (1.69), and lower IQ scores 91.2 (15.9) at age 8 than the NBW group [0.89 (0.96), 103.8 (12.3)]. Additional analyses (Supplementary Table S2) examined participant attrition and indicated that at the 22–26 year sweep, ELBW individuals were significantly more likely to be lost to follow-up, as were those with fewer emotional problems in their adolescence. At age 30–35, males and ELBW individuals were significantly more likely to drop out of the study, as were those with more chronic health problems and participants with lower IQ. There were no differences between predictors of attrition between ELBW and NBW individuals.
Table 1.
Sample characteristics of the ELBW and NBW participants with a completed FHS*
| Sample characteristics | t (df) | p-value | ||
|---|---|---|---|---|
| Number of participants, n (%) | 85 (49.10) | 88 (50.90) | N/A | N/A |
| Gender, male, n (%) | 32 (37.60) | 34 (38.60) | N/A | N/A |
| Birth weight, M (SD) grams | 827.06 (132.74) | 3396.66 (468.96) | 49.39 (101.30) | 0.00 |
| Gestational age, M (SD) weeks | 27.02 (2.28) | 40 (0.00) | 52.39 (84) | 0.00 |
| WISC-R IQ score, M (SD)Measured at age 8 | 93.20 (15.20) | 106.45 (11.99) | 6.10 (139.8) | 0.00 |
| Teen emotional problems, M (SD)Identified at ages 12–16 | 4.58 (3.82) | 3.90 (4.07) | −1.09 (158) | 0.28 |
| Teen conduct problems, M (SD)Identified at ages 12–16 | 1.39 (2.76) | 1.55 (2.04) | 0.41 (157) | 0.68 |
| Chronic health problems, M (SD)Identified at ages 12–16 | 1.96 (1.54) | 0.99 (0.98) | −4.82 (132.60) | 0.00 |
| Maternal psychopathology | χ2 (df) | p-value | ||
| Maternal mood disorder, n (%) | 27 (15.10) | 28 (19.30) | 0.00 (1) | 0.99 |
| Maternal anxiety, n (%) | 12 (6.70) | 13 (9.00) | 0.03 (1) | 0.85 |
| 22–26-year follow-up | t (df) | p-value | ||
| Age, M (SD) years | 23.20 (1.13) | 23.59 (1.04) | 2.37 (171) | 0.02 |
| YASR internalizing, M (SD) | 13.65 (10.22) | 10.49 (8.25) | −2.24 (171) | 0.03 |
| YASR externalizing, M (SD) | 15.46 (6.84) | 15.72 (6.24) | 0.26 (171) | 0.80 |
| 30–35-year follow-up | t (df) | p-value | ||
| Age, M (SD) years | 32.05 (1.62) | 32.44 (1.33) | 1.73 (162.90) | 0.09 |
| YASR internalizing, M (SD) | 16.42 (12.84) | 11.81 (9.83) | −2.58 (149.80) | 0.01 |
| YASR externalizing, M (SD) | 5.78 (5.96) | 6.13 (5.88) | 0.38 (164) | 0.70 |
The bolded values indicate a significant p-value (p < 0.05).
The ELBW sample had significantly higher scores on the YASR internalizing scale at 22–26 years 12.9 (9.5) and at 30–35 years 16.79 (12.23) compared to the NBW cohort [10.3 (7.9), 11.55 (9.76)]. However, scores on the YASR externalizing scale were not significantly different between the ELBW and NBW cohorts at both adult time points. The two groups also did not differ on behavioral or emotional problems at age 12–16, or the prevalence of maternal mood or anxiety disorders.
Unadjusted raw associations between maternal psychopathology and offspring internalizing and externalizing problems at ages 22–26 and 30–35 are presented in Table 2. The raw results indicate that all interactions, with the exception of the interaction between maternal anxiety and externalizing behavior in mature adulthood, are significant. All raw significant main effects have medium to large effect sizes (0.49 < Cohen’s d < 1.23). However, these observations do not all hold true after the models were adjusted for the aforementioned covariates, suggesting that the covariates accounted for a certain degree of variance within the models. Adjusted models for the associations between maternal psychopathology and offspring internalizing and externalizing problems at ages 22–26 and 30–35 are presented in Table 3. Small to medium effects sizes were observed for all significant main effects (0.26 ≤ Cohen’s d ≤ 0.52).
Table 2.
Unadjusted regression analyses for influence of maternal psychopathology on internalizing and externalizing problems at 22–26 and 30–35 years in ELBW and NBW individuals*
| Unadjusted interaction | ELBW | NBW | |||||||
|---|---|---|---|---|---|---|---|---|---|
| p-value | β | p-value | Cohen’s d | β | p-value | Cohen’s d | |||
| Internalizing problems | 22–26-year follow-up | Maternal mood disorder | 0.00 | 8.65 | 0.00 | 0.89 | 7.82 | 0.00 | 1.01 |
| Maternal anxiety disorder | 0.00 | 11.67 | 0.00 | 1.23 | 3.76 | 0.13 | 0.41 | ||
| 30–35-year follow-up | Maternal mood disorder | 0.00 | 10.03 | 0.00 | 0.80 | 7.56 | 0.00 | 0.77 | |
| Maternal anxiety disorder | 0.04 | 14.14 | 0.00 | 1.20 | 6.89 | 0.02 | 0.6 | ||
| Externalizing problems | 22–26-year follow-up | Maternal mood disorder | 0.00 | 6.27 | 0.00 | 0.89 | 1.88 | 0.19 | 0.30 |
| Maternal anxiety disorder | 0.00 | 4.32 | 0.04 | 0.55 | 1.69 | 0.37 | 0.27 | ||
| 30–35-year follow-up | Maternal mood disorder | 0.01 | 3.02 | 0.03 | 0.49 | 2.04 | 0.14 | 0.34 | |
| Maternal anxiety disorder | 0.31 | 1.30 | 0.50 | 0.21 | 1.30 | 0.47 | 0.22 | ||
The bolded values indicate a significant p-value (p < 0.05).
Table 3.
Regression analyses for influence of maternal psychopathology on internalizing and externalizing problems at 22–26 and 30–35 years in ELBW and NBW individuals adjusted for health problems, IQ, and sex, as well as emotional problems for internalizing and teen conduct for externalizing problems*
| Adjusted interaction | ELBW | NBW | |||||||
|---|---|---|---|---|---|---|---|---|---|
| p-value | β | p-value | Cohen’s d | β | p-value | Cohen’s d | |||
| Internalizing problems | 22–26-year follow-up | Maternal mood disorder | 0.46 | 7.95 | 0.00 | 0.38 | 5.88 | 0.00 | 0.38 |
| Maternal anxiety disorder | 0.01 | 10.27 | 0.00 | 0.39 | 0.37 | 0.88 | 0.02 | ||
| 30–35-year follow-up | Maternal mood disorder | 0.21 | 8.24 | 0.01 | 0.33 | 4.97 | 0.02 | 0.26 | |
| Maternal anxiety disorder | 0.04 | 12.65 | 0.00 | 0.40 | 3.72 | 0.19 | 0.15 | ||
| Externalizing problems | 22–26-year follow-up | Maternal mood disorder | 0.01 | 7.21 | 0.00 | 0.52 | 0.85 | 0.52 | 0.07 |
| Maternal anxiety disorder | 0.37 | 3.89 | 0.11 | 0.19 | 2.54 | 0.13 | 0.17 | ||
| 30–35-year follow-up | Maternal mood disorder | 0.2 | 3.95 | 0.01 | 0.35 | 1.36 | 0.25 | 0.13 | |
| Maternal anxiety disorder | 0.52 | 2.28 | 0.25 | 0.15 | 1.43 | 0.33 | 0.01 | ||
The bolded values indicate a significant p-value (p < 0.05).
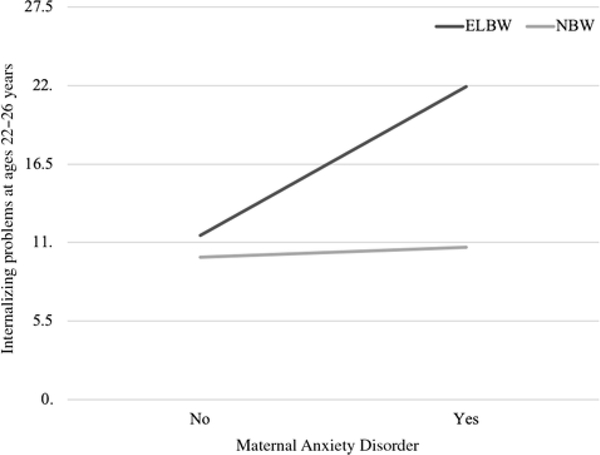
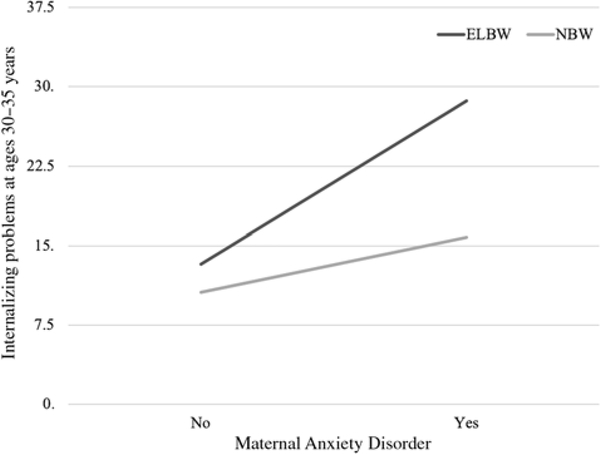
A statistically significant interaction was also found between birth weight group and any maternal anxiety disorder, associated with internalizing problems at both ages 22–26 (p = 0.01) and 30–35 (p = 0.04). Among ELBW survivors, the presence of a maternal anxiety disorder was associated with scores on the internalizing scale at age 22–26 that were 10.27 points higher on average than those whose mothers did not have an anxiety problem (p < 0.01) (see Fig. 1). This average difference increased to 12.65 points at 30–35 (p < 0.01) (see Fig. 2). Thus, ELBW children who are also exposed to maternal anxiety problems show heightened anxiety scores. Having a mother with an anxiety disorder numerically increased internalizing scores in NBW control participants, but these were small and not statistically significant (0.37 at 22–26 years and 3.72 at 30–35 years). A maternal history of an anxiety disorder did not influence externalizing problems in either the NBW or ELBW groups at either time point.
Fig. 1.
Effect of any maternal anxiety disorder on internalizing problems at 22–26 years (p = 0.01).
Fig. 2.
Effect of any maternal anxiety disorder on internalizing problems at 30–35 years (p = 0.04).
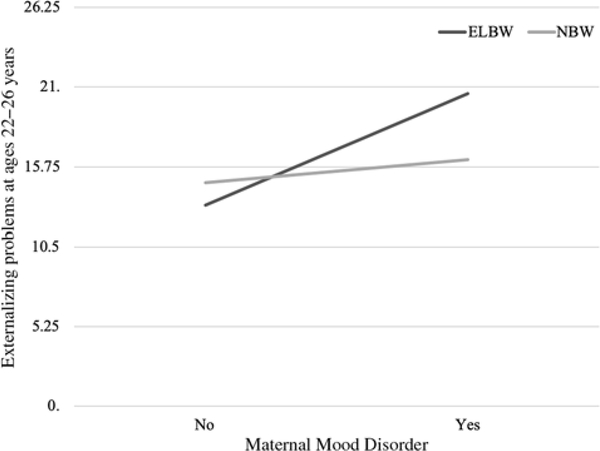
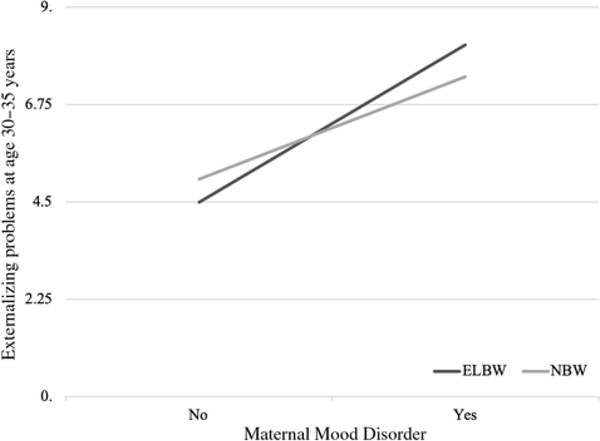
A statistically significant interaction was noted between birth weight status and maternal mood disorder with associated externalizing problems at age 22–26 (p = 0.007). ELBW survivors who had a mother with a mood disorder had externalizing scores that were 7.21 points (p < 0.05) higher than those who were not exposed (Fig. 3). While this interaction was not statistically significant at age 30–35 (Fig. 4), it was in the same direction as the 22–26-year-old finding.
Fig. 3.
Effect of any maternal mood disorder on externalizing problems at 22–26 years (p = 0.01).
Fig. 4.
Effect of any maternal mood disorder on externalizing problems at 30–35 years (p = 0.20).
There was, however, no statistically significant interaction between birth weight group and the presence of any maternal mood disorder for internalizing outcomes at either adult time point. A maternal history of a mood disorder was, however, associated with increased levels of internalizing problems in both ELBW and NBW individuals at 22–26 and 30–35 years of age.
Discussion
Despite the stresses associated with delivering and raising a preterm-born child, very few studies have examined whether birth weight moderates the impact of a maternal history of mental health problems on offspring psychopathology. Here, we report that the presence of a maternal anxiety disorder is associated with higher levels of symptoms of internalizing problems (i.e., depression and anxiety) in ELBW survivors in adulthood, an effect that is larger than for NBW controls. Likewise, ELBW survivors’ levels of externalizing problems in adulthood were higher than NBW participants in the presence of a maternal mood disorder, though this did not persist to 30–35 years. These findings suggest that preterm-born individuals may be more vulnerable to the effects mood and/or anxiety disorders in mothers and could provide a therapeutic target for reducing the rates and severity of certain mental health problems in adults born prematurely.
A few previous studies have explored outcomes of LBW survivors with a family history of mental illness. For example, Nomura et al. (2007) found an increased risk of depression if the parents of LBW infants were diagnosed with major depressive disorder.25 However, Nomura and colleagues examined the impact of parental depression specifically, and their study contained a small sample of 20 LBW individuals without a comparison group. Walshe et al. found that individuals born very preterm were at increased risk of psychiatric disorders, and that this risk was amplified if they had a first degree relative with a psychiatric disorder.26 However, this group did not have access to NBW control participants. Accordingly, the present study extends the extant literature by exploring the impact of maternal anxiety as well as depression in a group exposed to significant perinatal adversity and examining both internalizing and externalizing outcomes at two points across nearly a decade in adulthood.
Previous studies have noted increased rates of internalizing problems in ELBW survivors compared to NBW populations, with even higher levels in those with joint exposure to preterm birth and other perinatal adversities (e.g., being born small for gestational age, maternal exposure to antenatal corticosteroids).9,10 Previous reports also suggest that being exposed to certain postnatal adversities such as childhood sexual abuse18 also amplifies that already elevated risk of depression and anxiety in ELBW survivors.
As with the above findings, and in keeping with the cumulative risk hypothesis, the effects of perinatal adversity on psychopathology may be further amplified by a familial risk for mental disorders. This may be due to the combined effects of perinatal stress, genetic predisposition to mental illness, and/or a less than optimal rearing environment (e.g., maternal mental illness). Premature individuals may be more vulnerable not only to developing psychopathology because they are exposed to more risk factors, but risk factors for mental illness in adult life may have a bigger impact due to changes occurring during gestation that are aimed at adapting to the intrauterine environment. While these adaptations may be immediately beneficial to fetal development in utero, they may not translate into the postnatal environment, ultimately resulting in negative consequences later in life for ELBW survivors.43 These adaptations, which include epigenetic modifications and alterations in physiological regulatory systems such as the hypothalamus–pituitary–adrenal gland axis, may underlie this increased vulnerability to postnatal stressors.8,44
The first main finding of this study was that maternal anxiety disorders are associated with symptoms of internalizing problems in ELBW survivors in their early to mid-20s and 30s, more so than compared to NBW controls. That a maternal history of anxiety disorders leads to more internalizing problems in offspring is consistent with studies in general population samples, with effects as large or larger than maternal depression.22 This may be due to offspring exposure to the chronic nature of maternal anxiety compared to the more episodic course of maternal depression. Parenting may be of particular relevance to the mental health of preterm survivors given that they have multiple difficulties that can produce stress (e.g., physical illness, disability) and protective responses by their parents.19 Indeed, mothers of VLBW (<1500 g) infants have been shown to manifest high levels of postnatal anxiety, which have been linked with poorer cognitive development and more internalizing symptoms in offspring.45,46 Parental anxiety after the birth of preterm children may affect sensitive parenting and unintentionally lead to more overprotective parenting behaviors which can adversely affect development. This, in combination with the perinatal adversity many ELBW survivors face (and their accompanying biological changes), could help explain why internalizing symptoms were significantly higher in this group.
Our second main finding was that the presence of maternal mood disorder was associated with the risk of externalizing problems in adulthood more so in ELBW survivors than NBW, but only at ages 22–26. Letourneau et al. similarly found maternal depression was correlated to hyperactivity, aggression, and emotional problems in adolescents.47 Depression can significantly impact maternal parenting and has a negative impact on maternal–child interactions.48 Depressed mothers are shown to be more negative in play and less affectionate with their children, and they may also be more severe in parenting during adolescence.49–51 Harsh parenting in response to misbehavior can more often contribute to externalizing behaviors, normalizing aggression and violence.52 Parental warmth is also associated with decreases in externalizing behavior, the loss of this in the form of reduced maternal affection may have put ELBW survivors at greater risk.53 The lack of effect in the 30–35-year follow-up could be a result of the smaller sample size or very low levels of externalizing problems at this time point or that these individuals receiving more support or treatment. This may also be due to the normative reductions in externalizing problems seen in most people as they get older. Indeed, in the literature it is noted that externalizing problems often decrease into adulthood.54,55
This study is not without limitations. First, reports on maternal psychopathology in this study were made by offspring retrospectively, and despite the good psychometric properties of the FHS, this method is less ideal than formal psychiatric diagnoses, or even parental self-reports. It also does not specify the timing of maternal psychopathology in the child’s lifespan, or whether or not treatment was received. It could also be that we measured shared measurement variance between the FHS and YASR measures given they were completed by the same informant. Moreover, having a particular mental illness may have led to elevated rates of reporting that problem in family members.56 Additionally, only the impact of maternal psychopathology on offspring was examined in this study, given the more active role mothers had in child-rearing during the era in which these individuals were raised. This assumption implies that the interaction with birth weight status is more behavioral than genetic, even though both mechanisms are possible. Future studies should therefore attempt to examine the impact of both maternal and paternal psychopathology in order to more clearly delineate the source of these effects. Second, as expected with longitudinal studies, participant attrition resulted in a smaller sample size, which may have limited statistical power and our ability to detect statistically significant results. It is important to note that certain characteristics of the sample were predictive of attrition and these may have introduced additional bias. However, these predictors of loss to follow-up were adjusted for in our statistical analysis as a means of trying to reduce this bias. Additionally, it is important to note that this ELBW cohort is the oldest known prospectively followed cohort, and it may be some time before more recent cohorts are in a position to examine the questions addressed herein. Third, certain prenatal, neonatal, and postnatal data (i.e., APGAR scores and Bayley Scales of Infant and Toddler Development scores, medication use) were not obtained in both groups perinatally, and the role they may have played in the associations we described is not known. Finally, the ELBW cohort examined in this study was born in a time where preterm survival rates were lower and before the widespread use of surfactant, antenatal corticosteroids, and sophisticated diagnostic and therapeutic techniques to improve neonatal outcomes. Future studies should examine larger cohorts of ELBW survivors born after the introduction of these treatments to get an accurate representation of the challenges ELBW survivors being born today will face. It may also be of interest to examine if these challenges extend to VLBW (<1500 g) and LBW (<2500 g) survivors, which we were unable to do within our sample.
The results of this study suggest that ELBW survivors may be more sensitive to the adverse effects of exposure to maternal anxiety and mood problems in terms of adult mental health outcomes. Given the high levels of stress experienced by mothers of preterm infants, the elevated rates of mental health difficulties in these women, and the low cost of screening in this population, maternal mental illness may be a very important target for detection and intervention.57,58
Given associations between these problems and psychopathology in offspring, the treatment of maternal mental illness may be a valuable target as physicians and parents work to optimize the mental and physical health of preterm survivors across the lifespan.
Supplementary Material
Acknowledgements
The authors would like to thank the many participants and their families for their participation in this study.
Financial Support. This study was supported by the Canadian Institutes of Health Research grants CIHR: TMH-103145 (to L.A.S) and CIHR: MOP42536 (to S.S.), and a National Institute of Child Health and Human Development grant NICHD: 1-R01HD40219 (to S.S.).
Footnotes
Conflicts of Interest. None.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation, Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans and with the Helsinki Declaration of 1975, as revised in 2008, and have been approved by the institutional committee, Hamilton Integrated Research Ethics Board (HiREB).
Supplementary materials. For supplementary material for this article, please visit https://doi.org/10.1017/S2040174419000771
References
- 1.Langhoff-Roos J, Kesmodel U, Jacobsson B, Rasmussen S, Vogel I. Spontaneous preterm delivery in primiparous women at low risk in Denmark: population based study. BMJ. 2006; 332, 937–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Thompson JM, Irgens LM, Rasmussen S, Daltveit AK. Secular trends in socio‐economic status and the implications for preterm birth. Paediatr Perinat Epidemiol. 2006; 20, 182–187. [DOI] [PubMed] [Google Scholar]
- 3.Doyle LW. Evaluation of neonatal intensive care for extremely low birth weight infants in Victoria over two decades: I. Effectiveness. Pediatrics. 2004; 113, 505–509. [DOI] [PubMed] [Google Scholar]
- 4.Kusuda S, Fujimura M, Uchiyama A, Totsu S, Matsunami K. Trends in morbidity and mortality among very-low-birth-weight infants from 2003 to 2008 in Japan. Pediatr Res. 2012; 72, 531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Meadow W, Lee G, Lin K, Lantos J. Changes in mortality for extremely low birth weight infants in the 1990s: implications for treatment decisions and resource use. Pediatrics. 2004; 113, 1223–1229. [DOI] [PubMed] [Google Scholar]
- 6.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008; 371, 261–269. [DOI] [PubMed] [Google Scholar]
- 7.Hack M, Taylor HG, Drotar D, et al. Chronic conditions, functional limitations, and special health care needs of school-aged children born with extremely low-birth-weight in the 1990s. JAMA. 2005; 294, 318–325. [DOI] [PubMed] [Google Scholar]
- 8.Mathewson KJ, Chow HTC, Dobson KG, et al. Mental health of extremely low birth weight survivors: a systematic review and meta-analysis. Psychol Bull. 2017; 143, 347–383. [DOI] [PubMed] [Google Scholar]
- 9.Boyle MH, Miskovic V, Van Lieshout RJ, et al. Psychopathology in young adults born at extremely low birth weight. Psychol Med. 2011; 41, 1763–1774. [DOI] [PubMed] [Google Scholar]
- 10.Van Lieshout RJ, Boyle MH, Saigal S, Morrison K, Schmidt LA. Mental health of extremely low birth weight survivors in their 30s. Pediatrics. 2015; 135, 452–459. [DOI] [PubMed] [Google Scholar]
- 11.Hack M, Flannery DJ, Schluchter M, et al. Outcomes in young adulthood for very-low-birth-weight infants. N Engl J Med. 2002; 346, 149–157. [DOI] [PubMed] [Google Scholar]
- 12.Waxman JA, Van Lieshout RJ, Boyle MH, Saigal S, Schmidt LA. Linking extremely low birth weight and internalizing behaviors in adult survivors: influences of neuroendocrine dysregulation. Dev Psychobiol. 2015; 57, 486–496. [DOI] [PubMed] [Google Scholar]
- 13.Miskovic V, Schmidt LA, Georgiades K, Boyle M, MacMillan HL. Stability of resting frontal electroencephalogram (EEG) asymmetry and cardiac vagal tone in adolescent females exposed to child maltreatment. Dev Psychobiol. 2009; 51, 474–487. [DOI] [PubMed] [Google Scholar]
- 14.Poole KL, Schmidt LA, Missiuna C, et al. Childhood motor coordination and adult psychopathology in extremely low birth weight survivors. J Affect Disord. 2016; 190, 294–299. [DOI] [PubMed] [Google Scholar]
- 15.Dobson KG, Schmidt LA, Saigal S, Boyle MH, Van Lieshout RJ. Childhood cognition and lifetime risk of major depressive disorder in extremely low birth weight and normal birth weight adults. J Dev Orig Health Dis. 2016; 7, 574–580. [DOI] [PubMed] [Google Scholar]
- 16.Dobson KG, Ferro MA, Boyle MH, et al. Socioeconomic attainment of extremely low birth weight survivors: the role of early cognition. Pediatrics. 2017; 139, 2016–2545. [DOI] [PubMed] [Google Scholar]
- 17.Lund JI, Day KL, Schmidt LA, Saigal S, Van Lieshout RJ. Adult social outcomes of extremely low birth weight survivors of childhood sexual abuse. J Dev Orig Health Dis. 2016; 7, 581–587. [DOI] [PubMed] [Google Scholar]
- 18.Lund JI, Day KL, Schmidt LA, Saigal S, Van Lieshout RJ. Adult mental health outcomes of child abuse survivors born at extremely low birth weight. Child Abuse Negl. 2016; 59, 36–44. [DOI] [PubMed] [Google Scholar]
- 19.Day KL, Dobson KG, Schmidt LA, et al. Exposure to overprotective parenting and psychopathology in extremely low birth weight survivors. Child Care Health Dev. 2018; 44, 234–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Lieshout RJ, Boyle MH, Favotto L, et al. Impact of extremely low‐birth-weight status on risk and resilience for depression and anxiety in adulthood. J Child Psychol Psychiatry. 2018; 59(5), 596–603. [DOI] [PubMed] [Google Scholar]
- 21.Fortier P, Van Lieshout RJ, Waxman JA, et al. Are orchids left and dandelions right? Frontal brain activation asymmetry and its sensitivity to developmental context. Psychol Sci. 2014; 25, 1526–1533. [DOI] [PubMed] [Google Scholar]
- 22.Barker ED, Jaffee SR, Uher R, Maughan B. The contribution of prenatal and postnatal maternal anxiety and depression to child maladjustment. Depress Anxiety. 2011; 28, 696–702. [DOI] [PubMed] [Google Scholar]
- 23.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999; 106, 458–490. [DOI] [PubMed] [Google Scholar]
- 24.Milne BJ, Caspi A, Harrington H, et al. Predictive value of family history on severity of illness: the case for depression, anxiety, alcohol dependence, and drug dependence. Arch Gen Psychiatry. 2009; 66, 738–747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nomura Y, Wickramaratne PJ, Pilowsky DJ, et al. Low birthweight and risk of affective disorders & selected medical illness in offspring at high and low risk for depression. Compr Psychiatry. 2007; 48, 470–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Walshe M, Rifkin L, Rooney M, et al. Psychiatric disorder in young adults born very preterm: role of family history. Eur Psychiatry. 2008; 23, 527–531. [DOI] [PubMed] [Google Scholar]
- 27.Phares V, Duhig AM, Watkins MM. Family context: fathers and other supports In Children of Depressed Parents: Mechanisms of Risk and Implications for Treatment (eds. Goodman SH, Gotlib IH), 2002; pp. 203–225. American Psychological Association, Washington, DC. [Google Scholar]
- 28.Lamb ME, Tamis-LeMonda CS. The role of the father: an introduction In The Role of the Father in Child Development (ed. Lamb ME), 2004; pp. 1–31. John Wiley & Sons Inc., Hoboken, NJ. [Google Scholar]
- 29.Weissman MM, Wickramaraine P, Adams P. Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry. 2000; 57, 675–682. [DOI] [PubMed] [Google Scholar]
- 30.Achenbach TM. Manual for the Young Adult Self-report and Young Adult Behaviour Checklist, 1997. University of Vermont, Department of Psychiatry, Burlington, VT. [Google Scholar]
- 31.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed.), 1994. American Psychiatric Publishing, Inc., Arlington, VA. [Google Scholar]
- 32.Achenbach TM, Bernstein A, Dumenci L. DSM oriented scales and statistically based syndromes for ages 18 to 59: linking taxonomic paradigms to facilitate multitaxonomic approaches. J Pers Assess. 2005; 84, 49–63. [DOI] [PubMed] [Google Scholar]
- 33.Cadman D, Boyle M, Szatmari P, Offord DR. Chronic illness, disability, and mental and social well-being: findings of the Ontario Child Health Study. Pediatrics. 1987; 79(5), 805–813. [PubMed] [Google Scholar]
- 34.Hofstra MB, Van Der Ende JAN, Verhulst FC. Child and adolescent problems predict DSM-IV disorders in adulthood: a 14-year follow-up of a Dutch epidemiological sample. J Am Acad Child Adolesc Psychiatry. 2002; 41(2), 182–189. [DOI] [PubMed] [Google Scholar]
- 35.Young J, Savoy C, Schmidt LA, et al. Adult mental health outcomes of preterm survivors experiencing suicidal ideation in adolescence. Arch Suicide Res. 2019; 23, 163–174. [DOI] [PubMed] [Google Scholar]
- 36.Cheong JLY, Wark JD, Cheung MM, et al. Impact of extreme prematurity or extremely low birth weight on young adult health and well-being: the Victorian Infant Collaborative Study (VICS) 1991–1992 Longitudinal Cohort study protocol. BMJ Open. 2019; 9, e030345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Boyle MH, Offord DR, Racine Y, et al. Evaluation of the revised Ontario child health study scales. J Child Psychol Psychiatry. 1993; 34(2), 189–213. [DOI] [PubMed] [Google Scholar]
- 38.Koenen KC, Moffitt TE, Roberts AL, et al. Childhood IQ and adult mental disorders: a test of the cognitive reserve hypothesis. Am J Psychiatry. 2009; 166(1), 50–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Joseph RM, O’Shea TM, Allred EN, et al. Neurocognitive and academic outcomes at age 10 years of extremely preterm newborns. Pediatrics. 2016; 137(4), e20154343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cooke RWI. Are there critical periods for brain growth in children born preterm? Arch Dis Child Fetal Neonatal Ed. 2006; 91: F17–F20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wechsler D Manual for the Wechsler Intelligence Scale for Children, Revised, 1974. Psychological Corporation, San Antonio, TX. [Google Scholar]
- 42.Schuerger JM, Witt AC. The temporal stability of individually tested intelligence. J Clin Psychol. 1989; 45(2), 294–302. [Google Scholar]
- 43.Gluckman PD, Hanson MA. Developmental origins of disease paradigm: a mechanistic and evolutionary perspective. Pediatr Res. 2004; 56, 311–317. [DOI] [PubMed] [Google Scholar]
- 44.Lester BM, Conradt E, Marsit CJ. Epigenetic basis for the development of depression in children. Clin Obstet Gynecol. 2013; 56, 556–565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zelkowitz P, Na S, Wang T, Bardin C, Papageorgiou A. Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age. Acta Paediatr. 2011; 100, 700–704. [DOI] [PubMed] [Google Scholar]
- 46.Zelkowitz P, Papageorgiou A. Easing maternal anxiety: an update. Womens Health. 2012; 8, 205–213. [DOI] [PubMed] [Google Scholar]
- 47.Letourneau NL, Tramonte L, Willms JD. Maternal depression, family functioning and children’s longitudinal development. J Pediatr Nurs. 2013; 28, 223–234. [DOI] [PubMed] [Google Scholar]
- 48.Beck CT. The effect of postpartum depression on maternal-infant interaction: a meta-analysis. Nurs Res. 1995; 44, 298–304. [PubMed] [Google Scholar]
- 49.Murray L, Hipwell A, Hooper R. The cognitive developmental of 5-year-old children of postnatally depressed mothers. J Child Psychol Psychiatry. 1996; 37, 927–935. [DOI] [PubMed] [Google Scholar]
- 50.Stanley C, Murray L, Stein A. The effect of postnatal depression on mother-infant interaction, infant response to Still-face perturbation, and performance on an instrumental learning task. Dev Psychopathol. 2004; 16, 1–18. [DOI] [PubMed] [Google Scholar]
- 51.Leinonen JA, Solantaus TS, Punamaeki RL. Parental mental health and children’s adjustment: the quality of marital interaction and parenting as mediating factors. J Child Psychol Psychiatry. 2003; 44, 227–241. [DOI] [PubMed] [Google Scholar]
- 52.Catalano RF, Hawkins JD. The social development model: a theory of antisocial behavior In Cambridge Criminology Series. Delinquency and Crime: Current Theories (ed. Hawkins JD), 1996; pp. 149–197. Cambridge University Press, New York, NY. [Google Scholar]
- 53.Doyle AB, Markiewicz D. Parenting, marital conflict and adjustment from early- to mid-adolescence: mediated by adolescent attachment style? J Youth Adolesc. 2005; 34, 997–110. [Google Scholar]
- 54.Peterson IT, Bates JE, Dodge KA, Lansford JE, Pettit GS. Describing and predicting developmental profiles of externalizing problems from childhood to adulthood. Dev Psychopathol. 2015; 27, 791–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sampson RJ, Laub JH. Life-course desisters? Trajectories of crime among delinquent boys followed to age 70. Criminology. 2003; 41, 301–340. [Google Scholar]
- 56.Kendler KS, Silberg JL, Neale MC, et al. The family history method: whose psychiatric history is measured? Am J Psychiatry. 1991; 148, 1501–1504. [DOI] [PubMed] [Google Scholar]
- 57.Anderson C, Cacola P. Implications of preterm birth for maternal mental health and infant development. MCN Am J Matern Child Nurs. 2017; 42, 108–114. [DOI] [PubMed] [Google Scholar]
- 58.Wilkinson A, Anderson S, Wheeler SB. Screening for and treating postpartum depression and psychosis: a cost-effectiveness analysis. Matern Child Health J. 2017; 21, 903–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.