Purpose
To examine differences in students’ empathy in different years of medical school in a nationwide study of students of U.S. DO-granting medical schools.
Method
Participants in this cross-sectional study included 10,751 students enrolled in 41 of 48 campuses of DO-granting medical schools in the United States (3,616 first-year, 2,764 second-year, 2,413 third-year, and 1,958 fourth-year students). They completed a web-based survey at the end of the 2017–2018 academic year that included the Jefferson Scale of Empathy and the Infrequency Scale of the Zuckerman-Kuhlman Personality Questionnaire for measuring “good impression” response bias. Comparisons were made on empathy scores among students in different years of medical school using analysis of covariance, controlling for the effect of “good impression” response bias. Also, comparisons were made with preexisting data from students of U.S. MD-granting medical schools.
Results
A statistically significant decline in empathy scores was observed when comparing students in the preclinical (years 1 and 2) and the clinical (years 3 and 4) phases of medical school (P < .001); however, the magnitude of the decline was negligible (effect size =0.13). Comparison of findings with MD students showed that while the pattern of empathy decline was similar, the magnitude of the decline was less pronounced in DO students.
Conclusions
Differences in DO-granting and MD-granting medical education systems, such as emphasis on provision of holistic care, hands-on approaches to diagnosis and treatment, and patient-centered care, provide plausible explanations for disparity in the magnitude of empathy decline in DO compared with MD students. More research is needed to examine changes in empathy in longitudinal study and explore reasons for changes to avert erosion of empathy in medical school.
Empathy has been described as an element of professionalism in patient care.1 Empirical research shows that medical students’ empathy is positively associated with faculty’s ratings of their clinical competence.2 In addition, physician empathy is significantly associated with positive clinical outcomes in diabetic patients.3,4 Still, empathy is a vague concept and has been defined differently by behavioral and social researchers.5 However, in the context of patient care, clinical empathy has been defined as a predominantly cognitive (rather than an affective or emotional) attribute that involves an understanding of the experiences, concerns, and perspectives of the patient, combined with a capacity to communicate this understanding and an intention to help.5(p74),6 Consistent with this definition, in a systematic review of conceptualization of empathy in physicians, it was found that a great majority of researchers viewed empathy as a “cognitive” attribute (as opposed to a “feeling” or “affective” reaction).7
Background
Changes in empathy during medical school
Despite the importance of empathy in medical education and patient care, empirical evidence often suggests that empathy tends to erode as students progress through medical school.8–10 A decline in empathy during the clinical phase of medical education was first noticed in a longitudinal study8 by the Jefferson (currently Sidney Kimmel Medical College) research team in which the Jefferson Scale of Empathy (JSE) was administered at the beginning and the end of the third year of medical school when curriculum shifts from a preclinical to clinical phase of medical education.8 A second longitudinal study of erosion in empathy was undertaken by the same research team,9 in which 3 cohorts of medical students were followed up throughout medical school from orientation to graduation dates and completed the JSE 5 times (at the orientation and at the end of each year of medical school). The findings regarding decline in empathy were confirmed in all 3 cohorts in the third year of medical school, when ironically, empathy is most needed because of an increase in patient contacts.9 This was aptly reflected in the title of that publication: “The devil is in the third year.”9
A few review articles examined the issue of changes in empathy in physicians-in-training and other health professions students in the United States and abroad5(pp304–310) with mixed results. Colliver and his colleagues11 reviewed 11 studies (6 with medical students, 1 with dental students, and 4 with residents) and concluded that the decline of empathy during medical education has been greatly exaggerated. However, such a claim was not left unchallenged.12
By contrast, Neumann and her colleagues10 reviewed 18 articles (11 with medical students and 7 with residents) and concluded that empathy declined during the course of medical education, particularly during the clinical phase of medical education. Ferreira-Valente and colleagues13 reviewed studies published in English, Spanish, Portuguese, and French between 2009 and 2016 and selected 20 studies that met their inclusion criteria. Based on the magnitude of effect size of changes (estimated by the reviewers from published data), they did not offer a definitive conclusion about changes in empathy during medical school.13
With a few exceptions, the majority of studies on decline of empathy in medical school have been undertaken with samples from MD-granting medical schools. A large number of studies on decline in empathy in medical students are cross-sectional. A few published longitudinal studies of decline in empathy in students of MD-granting schools (hereafter, MD students) exist, but to our knowledge, no longitudinal study has been published on erosion of empathy in students of DO-granting schools (hereafter, DO students). A few cross-sectional studies on variation in empathy scores in DO medical students have reported no significant changes in empathy by year of schooling.14–16 A recent single-institution study with DO medical students by Rizkalla and Henderson17 reported a decline in JSE scores in the clinical phase of medical school, but the magnitude of decline was negligible. Decline in empathy has been more noticeable in studies in which the JSE was used,18,19 which can be attributed to the sensitivity of this instrument in detecting changes in empathic orientation toward patient care in physicians-in-training and those in practice.20
Because of differences in the DO-granting and MD-granting medical education systems and philosophies, it is worthwhile to explore differences in the pattern and magnitude of changes in empathy in DO and MD medical students. For example, osteopathic philosophy’s emphasis on provision of holistic care; hands-on approaches to diagnosis and treatment; and patient-centered, integrative, and collaborative care21,22 could result in a different pattern of empathic orientation in patient care among DO physicians-in-training. In addition, one may speculate that the educational goals in DO medical education regarding the importance of developing humanistic behavior, compassionate treatment, altruism, and empathy23 that are conducive to empathic orientation may reveal a different pattern and degree of changes in empathy among DO medical students.
The Project in Osteopathic Medical Education and Empathy
The Project in Osteopathic Medical Education and Empathy (POMEE) is a groundbreaking, nationwide, multi-institutional study in medical education, sponsored by the American Association of Colleges of Osteopathic Medicine (AACOM), in collaboration with the American Osteopathic Association, the Cleveland Clinic, and Sidney Kimmel Medical College at Jefferson. The POMEE was designed to use national samples of DO medical students at all levels of medical school education both to provide more definitive answers to the questions raised by medical educators on the assessment of empathy, its role, correlates, and variation in medical school, and to develop national norms of empathy scores for the first time in medical education research. We retrieved data for this study from the POMEE database, providing this unique opportunity to study empathy by year of schooling in national samples of DO medical students.
Study purpose
The purpose of this cross-sectional study was to examine variation in empathy scores in DO medical students in different years of medical school by using a validated measure of empathy, developed specifically for administration to medical students. We also sought to compare the pattern and magnitude of empathy score differences for DO medical students with previous findings for MD medical students.
Method
Participants
Participants were a national sample of 10,751 (out of a total 25,552) students in 41 of 48 campuses of colleges of DO-granting medical schools in the United States, representing 85% of all osteopathic college campuses in the country. Students in all 4 years of medical school participated in the study, with 3,616 (out of a total 7,197) first-year students (48% women, n = 1,738), 2,764 (out of 6,778) second-year students (50% women, n = 1,383), 2,413 (out of 6,683) third-year students (49% women, n = 1,180), and 1,958 (out of 4,894) fourth-year students (50% women, n = 970). We administered the study survey at the end of the 2017–2018 academic year at each college campus.
Study survey
We used a web-based survey that included questions about respondents’ demographic characteristics (age, gender, race/ethnicity), year of medical school education, specialty area of interest, plan to pursue a subspecialty, health care employment before medical school, and undergraduate major. The survey also included 2 scales: the JSE (S-Version) and the Infrequency Scale of the Zuckerman-Kuhlman Personality Questionnaire (ZKPQ).
Measuring clinical empathy with the JSE.
This scale is a 20-item, broadly used, and validated instrument for measuring clinical empathy in the context of health professions education and patient care.5(pp83–128) Items are answered on a 7-point Likert-type scale (1 = strongly disagree, 7 = strongly agree). Accumulated evidence from medical school student samples in the United States and abroad is available in support of psychometrics of the JSE.5(pp84–128, 276–286) For example, significant associations have been reported between medical students’ scores on the JSE and ratings of clinical competence in third-year core clerkships given by medical school faculty.2 Also, significant associations were observed between students’ JSE scores and ratings given by standardized patients in the objective structured clinical examination stations.24,25 More importantly, significant associations have been reported between physicians’ scores on the JSE and tangible clinical outcomes in diabetic patients in the United States3 and Italy.4
It has also been shown that medical students’ scores on the JSE are associated with personal qualities that are conducive to relationship building such as empathic concern and perspective taking26–39 in MD medical students and with personal accomplishment, orientation toward teamwork, and interprofessional collaboration in MD40 and DO medical students.15,36 Conversely, scores on the JSE yielded negative correlations with personal qualities that are detrimental to relationship building such as aggression hostility,29,41 and indicators of burnout such as depersonalization and emotional exhaustion,39,42,43 and neuroticism.44 In a recent study, using POMEE data, we reported strong evidence to support the measurement properties, underlying components, and latent variable structure of the JSE in a nationwide sample of first-year matriculants to osteopathic medical schools.45
Internal consistency reliability, determined by Cronbach’s coefficient alpha, in the United States and abroad is mostly reported in the 0.70s and 0.80s magnitudes,5(pp276–286) and stability of scores over time by test–retest reliability (in the 0.60s) has been reported in physicians,6 MD students,5 and DO students who participated in the POMEE.46 The aforementioned studies provide strong evidence for the validity and reliability of the JSE. The JSE has been translated into 57 languages and used by researchers in more than 80 countries.7 Because of its worldwide use and extensive psychometric support, the JSE has been recognized as the most researched instrument in medical education research47 and the most frequently used instrument for measuring empathy in medical education.7
Measuring attempts to make “good impression” responses.
Respondents to self-reported personality tests can manipulate their answers to produce good impressions. The attempt to present oneself in a more socially acceptable light is known as the “social desirability response set.” We used the Infrequency Scale of the ZKPQ48 to statistically control the effect of social desirability response set. This is a 10-item scale (true/false responses) developed to identify subjects with invalid records due to an exaggerated good impression response bias (a sample item: “I never met a person that I didn’t like”). Scores higher than 3 on this scale indicate questionable validity of the respondent’s record.48(p383) This scale has previously been used with medical students to detect and control for the tendency to make “good impression” responses.5,29
Procedures
The study survey evolved through several iterations and 2 pilot studies (alpha and beta) to improve its clarity and comprehensiveness, detect any possible bugs or crashes in the online administration, and explore the limits of the web-based product when using different desktop and mobile devices.
We arranged for 1 or 2 research coordinators from each participating college, at senior administrator or faculty level, to serve as a liaison or a contact between the participating colleges and research teams at the AACOM and Jefferson and to administer the web-based study survey at their college campuses. Research coordinators announced the project to students via email before administering the survey, described the importance of the project in advancing osteopathic education and patient care, and encouraged students to volunteer to participate. A similar message from the dean was included in the web-based survey. Students were also informed that they would have the option to receive their calculated empathy score, and literature on how to interpret their score, after completion of the project, if they entered their email address on the survey. The institutional review board (IRB) application for the project was submitted by the Jefferson team to the IRB of Thomas Jefferson University. An “exemption” status was granted (Control # 17E.112). All participating colleges submitted applications to their own IRBs and received approval related to human subjects research. With the exception of the voluntary option to enter email for receiving feedback, no personal identification information was solicited. All individual data were treated with strict confidentiality.
Statistical analyses
We used analysis of covariance to examine changes in the JSE scores. In this statistical model, score of the JSE served as the dependent variable, study groups (by year in medical school, preclinical versus clinical phases of medical school, gender, specialty interest) were the independent variables, and scores on the “good impression” scale served as the covariate. For comparisons of the JSE mean scores of the present study with those from a cross-sectional study of an allopathic medical school, we used a t test for independent samples. When sample sizes are large, negligible group differences or associations are likely to be statistically significant, even if practically unimportant. To determine the practical (clinical) significance of the statistically significant findings, we calculated the effect sizes and considered any effect size of 0.20 or less as negligible, thus practically unimportant regardless of statistical significance.49,50
Results
Response rates to the study survey were 3,616 out of 7,197 (50%) first-year students, 2,764 out of 6,778 (41%) second-year students, 2,413 out of 6,683 (36%) third-year students, 1,958 out of 4,894 (40%) fourth-year students, and 10,751 out of 25,552 (42%) of all DO students in all 4 years combined. To ensure that the study samples represented their respective populations, we compared each sample of first-, second-, third-, and fourth-year students with their respective national populations of all DO students in each year of medical school in the 2017–2018 academic year. Results showed that the study samples closely resembled their respective populations with regard to gender, age, and ethnicity. Detailed results have been reported elsewhere.50 Means and standard deviations of empathy scores for students in each year of medical school and summary results of statistical analyses are presented in Table 1.
Table 1.
Cross-Sectional Comparison of 10,751 Students’ Scores on the JSE by Year and by Clinical Phase, From a National Study of Empathy Across Medical School Years at 41 U.S. DO-Granting Medical Schools, 2017–2018
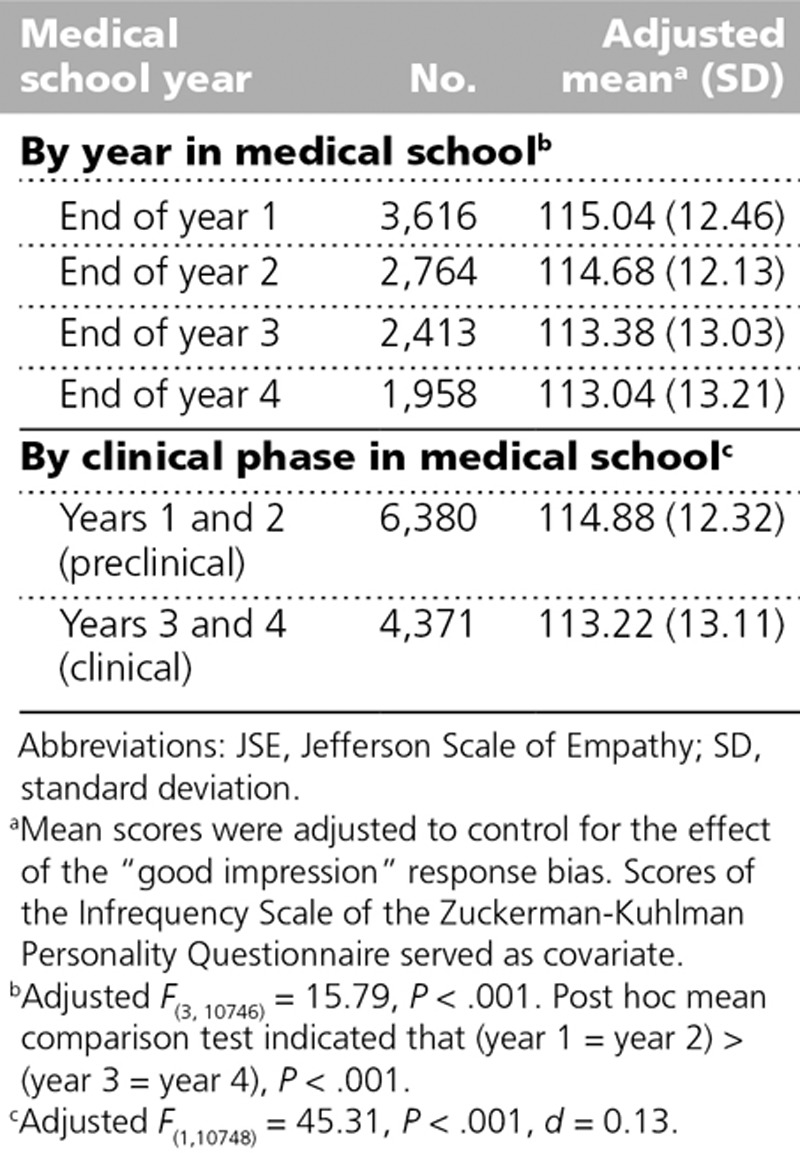
Analysis of covariance results indicated statistically significant differences in mean empathy scores by year of medical school (adjusted F(3,10746) = 15.79, P < .001). Post hoc mean comparison tests indicated that JSE scores did not significantly differ between students in years 1 and 2 of medical school (preclinical years). Also, we observed no significant difference between students in years 3 and 4 (clinical years). However, there was a statistically significant difference in empathy scores between students in years 1 and 2 combined, compared with those in years 3 and 4 combined. Therefore, we compared the 2 groups (preclinical versus clinical years of medical school education) on adjusted JSE mean scores. Means and standard deviations for the 2 groups of students in the preclinical and clinical phases of medical school education and summary results of analysis of covariance are presented in Table 1. As shown in Table 1, a significant decline in the JSE mean score was found in the clinical phase, compared with the preclinical phase of medical school education (adjusted F(1,10748) = 45.31, P < .001). However, such a magnitude of the difference is considered negligible and practically unimportant based on the effect size of 0.13.49,50 A similar pattern of findings was observed in DO students in a recent study at the Midwestern University/Chicago College of Osteopathic Medicine.17
There are 3 underlying components (factors) in the JSE: “perspective taking,” “compassionate care,” and “walking in patient’s shoes” in DO and MD medical students.5,45 In additional analyses, we compared factor scores in the preclinical and clinical phases of medical education. Results showed no practically significant differences on factor scores. We also examined mean empathy scores between individual college campuses. Within each study sample, the range of mean empathy scores across all participating campuses spanned no more than 10 or 12 points. A longitudinal multi-institutional research study could provide an answer to the question of whether differences in empathy scores at the beginning of medical school could contribute to the magnitude of decline as students progress through different years of schools.
Empathy change and gender
Higher JSE scores among women have been reported in a large number of studies of DO and MD students,2,5(pp 169–187),17,51–53 so we examined the pattern of empathy change by gender. Results are presented in Figure 1. As shown in the figure, women obtained higher empathy scores than men in all years of medical school (P < .001), with effect size estimates ranging from 0.40 to 0.47, which is in a moderate range. As shown in Figure 1, the pattern of changes was parallel for men and women.
Figure 1.
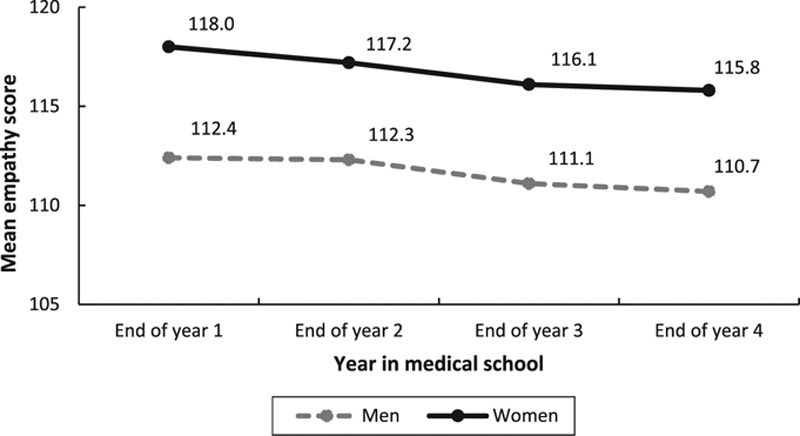
Comparison of scores on the JSE for men and women, from a national study of empathy across medical school years, 2017–2018. Participants were 10,751 students from 41 U.S. DO-granting medical schools. Mean empathy scores were adjusted to control for “good impression” response bias effects by using ANCOVA. Scores for the Infrequency Scale of the Zuckerman–Kuhlman Personality Questionnaire served as covariate. Results of ANCOVA indicated higher mean empathy scores for women compared with men. Year 1: Adjusted F(1,3574) = 192.7, P < .001. Year 2: Adjusted F(1,2728) = 116.2, P < .001. Year 3: Adjusted F(1,2375) = 96.3, P < .001. Year 4: Adjusted F(1,1933) = 76.9, P < .001. Abbreviations: JSE, Jefferson Scale of Empathy; ANCOVA, analysis of covariance.
Empathy change and specialty of interest
We also examined the pattern of change in the JSE scores in different years of medical school based on students’ reporting of the specialty they planned to pursue after graduation from medical school. Specialties chosen by fewer than 20 participants, specialties categorized as “other,” as well as the selection of “undecided” option, were excluded from the analysis. Results are depicted in Figure 2. As shown in Figure 2, students who planned to pursue “people-oriented” specialties (e.g., internal medicine, family medicine, psychiatry, pediatrics, etc.; n = 1,329, 1,190, 1,411, and 1,333 in years 1, 2, 3, and 4, respectively) obtained higher JSE scores in each year of medical school than those who planned to pursue “technology/procedure-oriented” specialties (e.g., anesthesiology, pathology, radiology, surgery, and surgical subspecialties, etc.; n = 705, 427, 495, and 273 in years 1, 2, 3, and 4, respectively), which is consistent with most published findings about medical students.5,29,53 Empathy score differences by specialty were statistically significant in each year (P < .001), and moderate in effect size magnitudes, ranging from 0.30 to 0.38 by schooling year.
Figure 2.
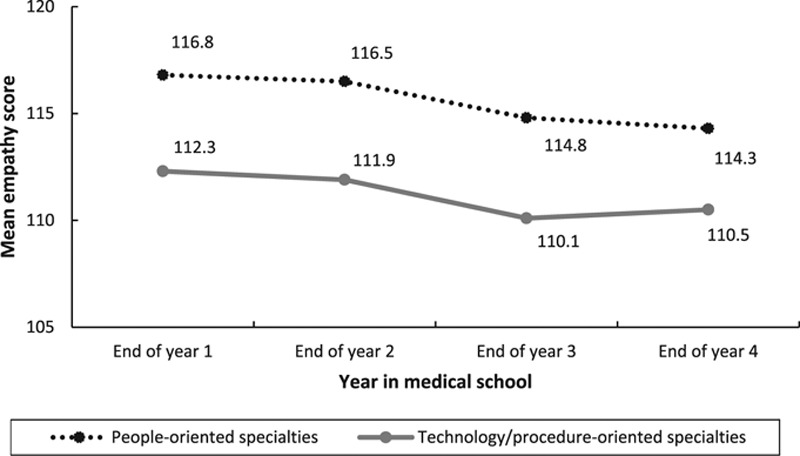
Comparison of scores on the JSE for students with different specialty interest, from a national study of empathy across medical school years, 2017–2018. Participants were 10,751 students from 41 U.S. DO-granting medical schools. Mean empathy scores were adjusted to control for “good impression” response bias effects by using ANCOVA. Scores of the Infrequency Scale of the Zuckerman–Kuhlman Personality Questionnaire served as covariate. Results of ANCOVA indicated higher mean empathy scores for students pursuing people-oriented (e.g., family medicine, psychiatry, pediatrics, etc.) compared with technology/procedure-oriented (e.g., pathology, radiology, surgery, etc.) specialties. Year 1: Adjusted F(1,2031) = 61.7, P < .001. Year 2: Adjusted F(1,1614) = 45.6, P < .001. Year 3: Adjusted F(1,1903) = 47.5, P < .001. Year 4: Adjusted F(1,1603) = 20.1, P < .001. Abbreviations: JSE, Jefferson Score of Empathy; ANCOVA, analysis of covariance.
Comparing changes in the JSE in this study with selected prior findings for MD students
We compared the JSE mean scores for students in each year of medical school in this study with corresponding mean scores reported by Chen and his colleagues in a cross-sectional study of MD students from Boston University School of Medicine.54 We chose the Chen et al study54 for comparison purposes because of key common features with our study, such as cross-sectional design, using the JSE medical student version, collection of data simultaneously at the end of the academic year from students in different years of medical school, and relatively good sample sizes. In their published study, Chen and colleagues reported JSE mean scores that were statistically adjusted for gender, age, educational debt, and specialty interest. In response to our request, Dr. Chen kindly provided us with unadjusted mean scores and standard deviations55 that we used in our comparisons reported in Table 2.
Table 2.
Comparisons of 10,751 DO Students’ and 486 MD Students’ Scores on the JSE by Year, From a National Study of Empathy Across Medical School Years at 41 U.S. DO-Granting Medical Schools, 2017–2018a
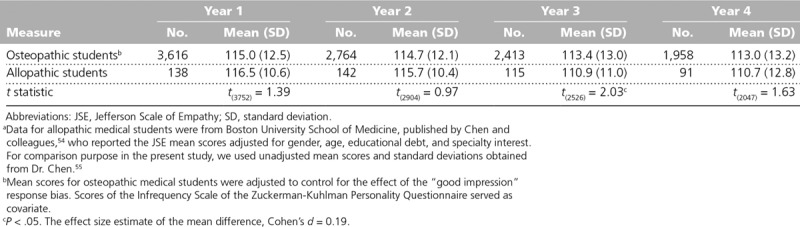
As shown in Table 2, no statistically significant difference was observed for the JSE mean scores in the first and second years of medical school when comparing DO and MD medical students. However, the JSE mean score for the third-year DO students was significantly higher than that in MD-granting medical schools (mean = 113.4 for DO and 110.9 for MD students; t(2526) = 2.03, P < .05, d = 0.19). A similar pattern of finding was observed for the fourth year of medical school, although the level of statistical significance did not reach the conventional level of significance (P < .05) in this year. These findings indicate that despite similarities in the pattern of decline of empathy scores between DO and MD students, the magnitude of decline in empathy starting in the third year is more pronounced among MD students. Within medical school systems, comparisons showed that the effect size of the decline in mean JSE scores between years 2 and 3 in DO and MD students were 0.10 and 0.45, respectively. Similarly, the effect sizes of the JSE mean empathy score decline in year 2 compared with year 4 for DO and MD students were 0.13 and 0.43, respectively. These findings indicate that the decline in empathy in MD students was more pronounced than that in DO students.
Discussion
This study benefits from 3 unique features. We collected data from national samples that represent all of U.S. DO students; we employed a well-established empathy-measuring instrument specifically developed for administration to medical students, with face and content validities and strong psychometric support in both MD and DO students; and we statistically controlled for “good impression” response bias to mitigate the effect of social desirability response set. This is, to our knowledge, the first time such an approach has been implemented in nationwide medical education research. Because of these advantages, our findings can provide more definitive answers to questions about correlates and outcomes of empathy in physicians-in-training with more confidence about their internal and external validities.56
Study limitations
One limitation of this study is a relatively low response rates (less than 50%) in samples of second-, third-, and fourth-year students. However, this limitation is mitigated by support for the representativeness of the samples based on some demographic variables.51 In addition, the well-known limitation of cross-sectional research in addressing changes over time restrains the validity of the findings. For example, we used different samples in different years of medical school, assuming that the baseline empathy scores were similar for students in different years. The assumption of equality of baseline empathy in different study groups has never been verified in any of the cross-sectional studies of medical students. A longitudinal research design is certainly more appropriate to examine changes in the same cohort of students as they progress through medical school. In particular, this could improve our understanding of contributing factors and features of medical education curricula that can avert the erosion of empathy. Student experiences, observations, and influences of the “hidden curriculum”57 in different years of medical school that can mediate empathic orientation toward patient care should be examined in longitudinal studies to develop remedies to enhance and sustain empathy as students progress through medical school education.
Concluding remarks
To our knowledge, this is the first and the only national cross-sectional study of changes of empathy in DO students. This study is poised to offer the most definitive insights to date into variation of student empathy, pattern of changes, and magnitude of differences by year of schooling in DO students in the United States. Thus, it lays the foundation for fruitful longitudinal research in the future. Although we found a similar pattern of decline in empathy scores from the preclinical to clinical phases of medical school education when comparing DO with MD students, the magnitude of standardized differences in empathy decline in the third year was substantially less pronounced in DO students.
Specific features of DO-granting medical education (e.g., hands-on osteopathic manipulative medicine, emphasis on holistic care, patient-centered approach, integrative and collaborative care, exhibition of compassionate treatment) and medical school characteristics can provide plausible explanations for the lesser erosion of empathy in the clinical phase of medical education in DO students. Indeed, a recent study of DO students reported by Rizkalla and Henderson17 provides empirical evidence for this proposition, showing that higher scores on the JSE are significantly associated with students’ interest and experience in osteopathic manipulative medicine and their belief in osteopathic philosophy. In another study with DO students,15 a significant correlation (r = 0.55, P < .01) was found between scores on the JSE and a measure of attitudes toward integrative patient care, which is a feature of osteopathic medical education.22 Findings of our study open a window to improve our understanding of changes in empathic orientation toward patient care, explore reasons for such changes, and address the role of medical education systems and student educational experiences in erosion of empathy in medical school in a longitudinal study design. We are currently undertaking such a nationwide longitudinal study in the second phase of the POMEE56 that can help to identify factors associated with decline in empathy in the clinical phase of medical education and avert the erosion of empathy in physicians-in-training.
Acknowledgments:
This study is part of an ongoing larger Project in Osteopathic Medical Education and Empathy (POMEE), sponsored by the American Association of Colleges of Osteopathic Medicine (AACOM), in collaboration with the American Osteopathic Association (AOA), the Cleveland Clinic, and the Sidney Kimmel Medical College of Thomas Jefferson University. The authors would particularly like to acknowledge those who made a significant contribution to this project’s success: Members of the AACOM team, especially Thomas Levitan, MEd, and Luke Mortensen, PhD, who were instrumental at the onset of this project in developing the survey instrument; Jefferson research team Daniel Z. Louis, MS, Vittorio Maio, MS, PSPH, Jon Veloski, MS, Niusha Jafari, MS, and Shira Carroll, BS; colleagues at the Jefferson Department of Information Services and Technology, Tracy Treadway, and Luke Kedziora, BS, who helped to prepare the web-based survey for online administration and correct computer glitches during pilot testing and afterward; and deans of participating colleges of osteopathic medicine and research coordinators from participating college campuses: Michael Becker, DO, Joe Bianco, PhD, Linda Boyd, DO, Joseph Brewer, PhD, Lisa Carroll, MD, Mark Clark, PhD, Karen Clayton, PhD, Glenn Davis, PhD, Robyn Dreibelbis, DO, Marti Echols, PhD, Kyle Henderson, PhD, Ana Maria Homs, PsyD, Sherri Howell, DO, Justina Hyfantis, PhD, Britt Johnson, PhD, LeAnn Jons-Cox, DO, Gretchen Lovett, PhD, Susan Mackintosh, DO, Elizabeth McClain, PhD, Edward Magalhaes, PhD, Patience Mason, MEd, Terrence Miller, PhD, Malcolm Modrzakowski, PhD, David Mokler, PhD, Bruce Newton, PhD, Lorree Ratto, PhD, Sean Reeder, DO, Tristan Reynolds, DO, Mireille Rizkalla, PhD, Raquel Malina Romanick, JD, Miko Rose, DO, Katherine Ruger, EdD, Amy Schlueter, MPA, Trish Sexton, DHEd, MS, Dana Shaffer, DO, Robert Sorrells, PhD, Vivian Stevens, PhD, Mary Ann Taylor, PhD, Clinton Whitson, MS, and Rynn Ziller, EdD. The authors are also thankful to Jennifer Wilson and Pamela Walter for editorial polishing of this article. And last but not least, special thanks to all of those thousands of osteopathic medical students in the academic year of 2017–2018 who made history in medical education research by voluntarily and willingly completing and submitting the online survey of this project.
Footnotes
Funding/Support: This study was funded by AACOM, AOA, and the Theodore F. Classen Chair of Osteopathic Research and Education at the Cleveland Clinic.
Other disclosures: None reported.
Ethical approval: The institutional review boards of Thomas Jefferson University and of all of the 41 participating colleges of osteopathic medicine approved this study as exempt.
References
- 1.Veloski J, Hojat M. Stern DT. Measuring specific elements of professionalism: Empathy, teamwork, and lifelong learning. In: Measuring Medical Professionalism. 2006Oxford, UK: Oxford University Press; [Google Scholar]
- 2.Hojat M, Gonnella JS, Mangione S, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002;36:522–527. [DOI] [PubMed] [Google Scholar]
- 3.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physicians’ empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86:359–364. [DOI] [PubMed] [Google Scholar]
- 4.Del Canale S, Louis DZ, Maio V, et al. The relationship between physician empathy and disease complications: An empirical study of primary care physicians and their diabetic patients in Parma, Italy. Acad Med. 2012;87:1243–1249. [DOI] [PubMed] [Google Scholar]
- 5.Hojat M. Empathy in Health Professions Education and Patient Care. 2016New York, NY: Springer International; [Google Scholar]
- 6.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Vergare M, Magee M. Physician empathy: Definition, components, measurement, and relationship to gender and specialty. Am J Psychiatry. 2002;159:1563–1569. [DOI] [PubMed] [Google Scholar]
- 7.Sulzer SH, Feinstein NW, Wendland CL. Assessing empathy development in medical education: A systematic review. Med Educ. 2016;50:300–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hojat M, Mangione S, Nasca TJ, et al. An empirical study of decline in empathy in medical school. Med Educ. 2004;38:934–941. [DOI] [PubMed] [Google Scholar]
- 9.Hojat M, Vergare MJ, Maxwell K, et al. The devil is in the third year: A longitudinal study of erosion of empathy in medical school. Acad Med. 2009;84:1182–1191. [DOI] [PubMed] [Google Scholar]
- 10.Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Acad Med. 2011;86:996–1009. [DOI] [PubMed] [Google Scholar]
- 11.Colliver JA, Conlee MJ, Verhulst SJ, Dorsey JK. Reports of the decline of empathy during medical education are greatly exaggerated: A reexamination of the research. Acad Med. 2010;85:588–593. [DOI] [PubMed] [Google Scholar]
- 12.Hojat M, Gonnella JS, Veloski JJ. Rebuttals to critics of studies of the decline of empathy. Acad Med. 2010;85:1812. [DOI] [PubMed] [Google Scholar]
- 13.Ferreira-Valente A, Monteiro JS, Barbosa RM, Salgueira A, Costa P, Costa MJ. Clarifying changes in student empathy throughout medical school: A scoping review. Adv Health Sci Educ Theory Pract. 2017;22:1293–1313. [DOI] [PubMed] [Google Scholar]
- 14.Kimmelman M, Giacobbe J, Faden J, Kumar G, Pinckney CC, Steer R. Empathy in osteopathic medical students: A cross-sectional analysis. J Am Osteopath Assoc. 2012;112:347–355. [PubMed] [Google Scholar]
- 15.Calabrese LH, Bianco JA, Mann D, Massello D, Hojat M. Correlates and changes in empathy and attitudes toward interprofessional collaboration in osteopathic medical students. J Am Osteopath Assoc. 2013;113:898–907. [DOI] [PubMed] [Google Scholar]
- 16.McTighe AJ, DiTomasso RA, Felgoise S, Hojat M. Effect of medical education on empathy in osteopathic medical students. J Am Osteopath Assoc. 2016;116:668–674. [DOI] [PubMed] [Google Scholar]
- 17.Rizkalla MN, Henderson KK. Empathy and osteopathic manipulative medicine: Is it all in the hands? J Am Osteopath Assoc. 2018;118:573–585. [DOI] [PubMed] [Google Scholar]
- 18.Smith KE, Norman GJ, Decety J. The complexity of empathy during medical school training: Evidence for positive changes. Med Educ. 2017;51:1146–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spatoula V, Panagopoulou E, Montgomery A. Does empathy change during undergraduate medical education?—A meta-analysis. Med Teach. 2019;41:895–904. [DOI] [PubMed] [Google Scholar]
- 20.Hojat M. Change in empathy in medical school. Med Educ. 2018;52:456–457. [DOI] [PubMed] [Google Scholar]
- 21.Carey TS, Motyka TM, Garrett JM, Keller RB. Do osteopathic physicians differ in patient interaction from allopathic physicians? An empirically derived approach. J Am Osteopath Assoc. 2003;103:313–318. [PubMed] [Google Scholar]
- 22.Noll DR, Ginsberg T, Elahi A, Cavalieri TA. Effective patient-physician communication based on osteopathic philosophy in caring for elderly patients. J Am Osteopath Assoc. 2016;116:42–47. [DOI] [PubMed] [Google Scholar]
- 23.National Board of Osteopathic Medical Examiners (NBOME). Fundamental Osteopathic Medical Competency Domains: Guidelines for Osteopathic Medical Licensure and the Practice of Osteopathic Medicine. Chicago, IL: National Board of Osteopathic Medical Examiners; https://www.nbome.org/docs/NBOME%20Fundamental%20Osteopathic%20Medical%20Competencies.pdf. Accessed December 30, 2019. [Google Scholar]
- 24.Berg K, Majdan JF, Berg D, Veloski J, Hojat M. A comparison of medical students’ self-reported empathy with simulated patients’ assessments of the students’ empathy. Med Teach. 2011;33:388–391. [DOI] [PubMed] [Google Scholar]
- 25.Berg K, Blatt B, Lopreiato J, et al. Standardized patient assessment of medical student empathy: Ethnicity and gender effects in a multi-institutional study. Acad Med. 2015;90:105–111. [DOI] [PubMed] [Google Scholar]
- 26.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson Scale of Physician Empathy: Development and preliminary psychometric data. Educ Psychol Meas. 2001;61:349–365. [Google Scholar]
- 27.Hojat M, Mangione S, Kane GC, Gonnella JS. Relationships between scores of the Jefferson Scale of Physician Empathy (JSPE) and the Interpersonal Reactivity Index (IRI). Med Teach. 2005;27:625–628. [DOI] [PubMed] [Google Scholar]
- 28.Costa P, de Carvalho-Filho MA, Schweller M, et al. Measuring medical students’ empathy: Exploring the underlying constructs of and associations between two widely used self-report instruments in five countries. Acad Med. 2017;92:860–867. [DOI] [PubMed] [Google Scholar]
- 29.Hojat M, Zuckerman M, Magee M, et al. Empathy in medical students as related to specialty interest, personality, and perception of mother and father. Pers Individ Dif. 2005;39:1205–1215. [Google Scholar]
- 30.Costa P, Alves R, Neto I, Marvão P, Portela M, Costa MJ. Associations between medical student empathy and personality: A multi-institutional study. PLoS One. 2014;9:e89254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arora S, Ashrafian H, Davis R, Athanasiou T, Darzi A, Sevdalis N. Emotional intelligence in medicine: A systematic review through the context of the ACGME competencies. Med Educ. 2010;44:749–764. [DOI] [PubMed] [Google Scholar]
- 32.Austin EJ, Evans P, Goldwater R, Potter V. A preliminary study of emotional intelligence, empathy and exam performance in first year medical students. Pers Individ Dif. 2005;39:1395–1405. [Google Scholar]
- 33.Kliszcz J, Nowicka-Sauer K, Trzeciak B, Nowak P, Sadowska A. Empathy in health care providers—Validation study of the Polish version of the Jefferson Scale of Empathy. Adv Med Sci. 2006;51:219–225. [PubMed] [Google Scholar]
- 34.Hong M, Bahn GH, Lee WH, Moon SJ. Empathy in Korean psychiatric residents. Asia-Pacific Psychiatry. 2011;3:83–90. [Google Scholar]
- 35.Brazeau CM, Schroeder R, Rovi S, Boyd L. Relationships between medical student burnout, empathy, and professionalism climate. Acad Med. 2010;85(10 suppl):S33–S36. [DOI] [PubMed] [Google Scholar]
- 36.Hojat M, Bianco JA, Mann D, Massello D, Calabrese LH. Overlap between empathy, teamwork and integrative approach to patient care. Med Teach. 2015;37:755–758. [DOI] [PubMed] [Google Scholar]
- 37.Hojat M, Michalec B, Veloski JJ, Tykocinski ML. Can empathy, other personality attributes, and level of positive social influence in medical school identify potential leaders in medicine? Acad Med. 2015;90:505–510. [DOI] [PubMed] [Google Scholar]
- 38.Pohl CA, Hojat M, Arnold L. Peer nominations as related to academic attainment, empathy, personality, and specialty interest. Acad Med. 2011;86:747–751. [DOI] [PubMed] [Google Scholar]
- 39.Hojat M, Vergare M, Isenberg G, Cohen M, Spandorfer J. Underlying construct of empathy, optimism, and burnout in medical students. Int J Med Educ. 2015;6:12–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hojat M, Spandorfer J, Isenberg GA, Vergare MJ, Fassihi R, Gonnella JS. Psychometrics of the scale of attitudes toward physician-pharmacist collaboration: A study with medical students. Med Teach. 2012;34:e833–e837. [DOI] [PubMed] [Google Scholar]
- 41.Hasan S, Al-Sharqawi N, Dashti F, et al. Level of empathy among medical students in Kuwait University, Kuwait. Med Princ Pract. 2013;22:385–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lamothe M, Boujut E, Zenasni F, Sultan S. To be or not to be empathic: The combined role of empathic concern and perspective taking in understanding burnout in general practice. BMC Fam Pract. 2014;15:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zenasni F, Boujut E, de Vaure CB, et al. Development of a French-language version of the Jefferson Scale of Physician Empathy and association with practice characteristics and burnout in a sample of general practitioners. Int J Pers Cent Med. 2012;2:759–766. [Google Scholar]
- 44.Xia L, Hongyu S, Xinwei F. Study on correlation between empathy ability and personality characteristics of undergraduate nursing students. Chin Nurs Res. 2011;32:2933–2935. [Google Scholar]
- 45.Hojat M, DeSantis J, Shannon SC, et al. The Jefferson Scale of Empathy: A nationwide study of measurement properties, underlying components, latent variable structure and national norm in medical students. Adv Health Sci Educ. 2018;23:899–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hojat M, Calabrese LH, Shannon SC, DeSantis J, Speicher M, Bragan L. Final Report: Project in Osteopathic Medical Education and Empathy. Submitted to the American College of Osteopathic Medicine. 2019. Philadelphia, PA; Sidney Kimmel Medical College at Philadelphia University + Thomas Jefferson University, Unpublished. [available from the authors on request]. [Google Scholar]
- 47.Colliver JA, Conlee MJ, Verhulst SJ, Dorsey JK. Rebuttals to critics of studies of the decline of empathy. Acad Med. 2010;85:1813–1814. [DOI] [PubMed] [Google Scholar]
- 48.Zuckerman M. DeRaad B, Perugini M. Zuckerman-Kuhlman Personality Questionnaire (ZKPQ): An alternative five-factor model. In: Big Five Assessment. 2002Seattle, WA: Hogrefe & Huber; [Google Scholar]
- 49.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 1987Hillsdale, NJ: Erlbaum. [Google Scholar]
- 50.Hojat M, Xu G. A visitor’s guide to effect sizes: Statistical significance versus practical (clinical) importance of research findings. Adv Health Sci Educ Theory Pract. 2004;9:241–249. [DOI] [PubMed] [Google Scholar]
- 51.Hojat M, Shannon SC, DeSantis J, Speicher MR, Bragan L, Calabrese LH. Empathy in Medicine National Norms for the Jefferson Scale of Empathy: A nationwide project in Osteopathic Medical Education and Empathy (POMEE). J Am Osteopath Assoc. 2019;119:520–532. [DOI] [PubMed] [Google Scholar]
- 52.Hojat M, Gonnella JS. Eleven years of data on the Jefferson Scale of Empathy-Medical Student Version (JSE-S): Proxy norm data and tentative cutoff scores. Med Princ Pract. 2015;24:344–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hojat M, Gonnella JS, Nasca TJ, Mangione S, Veloksi JJ, Magee M. The Jefferson Scale of Physician Empathy: Further psychometric data and differences by gender and specialty at item level. Acad Med. 2002;77(10 suppl):S58–S60. [DOI] [PubMed] [Google Scholar]
- 54.Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22:1434–1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chen D. Personal email communication from M. Hojat with D. Chen, July 6, 2012, and April 23, 2019.
- 56.Newton BW. Insights on the Nationwide Project in Osteopathic Medical Education and Empathy (POMEE). J Am Osteopath Assoc. 2018;118:e28–e32. [DOI] [PubMed] [Google Scholar]
- 57.Hafferty FW. Beyond curriculum reform: Confronting medicine’s hidden curriculum. Acad Med. 1998;73:403–407. [DOI] [PubMed] [Google Scholar]


