Abstract
A novel small enveloped RNA virus with the typical characteristic of the family to which it belongs, a crown, hence the name coronavirus, appeared in December 2019 in Wuhan, China, and subdued the world to its influence. The particular severity of the disease and higher mortality rates in patients with associated morbidities, including hypertension, obesity and diabetes, increases the concern over the consequences of this pandemic. In this review, the features of SARS-CoV-2 will be addressed, as well as the reasons why it poses a particular challenge to diabetic patients. We will also highlight the recent treatment strategies being explored to control this pandemic. Emerging evidence demonstrates that the correct management of diabetes in those patients infected with SARS-CoV-2 is of utmost importance for the viral disease progression, therefore, the importance of blood glucose control will also be addressed.
Keywords: ACE-2, ACE inhibitors, COVID-19, Diabetes, Glycemic control, SARS-CoV-2
1. SARS-CoV-2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), infected more than 3.5 million people in the world and was the cause of more than 250 thousand deaths in nearly 6 months (Dec-May) - data updated on 5th May [1]. This virus belongs to Nidovirales order, Coronaviridae family, Orthocoronavirinae subfamily and, according to its genomic characteristics, was classified in the Betacoronavirus genus. It is an enveloped virus with a single strand, positive-sense RNA genome, with a length of around 29.8 kb and a G + C content of 38% [2], [3]. Scanning electron microscopy images showed a 60–140 µm round or elliptic virus with frequently pleomorphic shape and distinctive spikes about 8 to 12 nm in length [4]. According to genomic sequencing, SARS-CoV-2 shares 89% homology with bat SARS-like-CoVZXC21, 82% with human SARS-CoV and around 50% with Middle East Respiratory Syndrome coronavirus (MERS-CoV) [2]. As all the other coronaviruses, SARS-CoV-2 comprises the four structural proteins E (envelope protein), M (membrane protein), N (nucleocapsid protein) and S (spike protein), as well as eight accessory proteins [5]. The spike surface glycoprotein plays an essential role by promoting the attachment of the virus to its receptor on host cells and may determine its host tropism and transmission ability. Receptor-binding domain (RBD) of S-protein from SARS-CoV-2 shares identical 3D structure with the RBD of S-protein from SARS-CoV, as well as 76.47% amino acid sequence homology [6]. In vitro and in vivo studies showed that angiotensin-converting enzyme 2 (ACE2) is the cellular receptor for SARS-CoV virus [7], [8]. The novel SARS-CoV-2 also binds to ACE2 [2], [9], [10], [11] with 10 to 20 times higher affinity than SARS-CoV does [12]. In addition, SARS-CoV-2 employs the cellular transmembrane serine protease 2 (TMPRSS2) for S protein priming, allowing internalization and replication in the host cells [11].
2. ACE2: Double edged sword for diabetic patients
ACE2 is a naturally occurring enzyme abundantly present in humans, mainly in the cell membrane of lung alveolar epithelial cells [13], [14], [15], [16] and enterocytes of the small intestine [15], which provide as entry routes for the SARS‐CoV infection and probably SARS-CoV-2. Additionally, ACE2 is also expressed by arterial and venous endothelial cells and arterial smooth muscle cells [15], cholangiocytes [17], testis [13], [14], pancreas [18], [19], in cardiovascular [13], [14], [16], renal [13], [14], [16], urothelial [16], mucosal [20] and gastrointestinal tissues [16], [21] in minor extent.
ACE2 is homologous to the firstly discovered ACE1, and both enzymes are part of the renin-angiotensin system (RAS), which has a crucial role in regulating blood pressure, maintaining electrolyte and fluid homeostasis for its potent vasoconstrictor/vasodepressor actions [22]. RAS is an enzymatic cascade starting with the cleavage of angiotensinogen by renin to form angiotensin (Ang) I. This peptide is then further metabolized by ACE1, which removes two amino acids at the C-terminal end to form the potent vasopressor peptide Ang II [23]. Ang II levels are endogenously regulated by the ACE2, which is a membrane-bound mono-carboxypeptidase that cleaves the terminal leucine and phenylalanine residues from Ang I and Ang II originating Ang 1–9 and Ang 1–7, respectively. The hexapeptide Ang 1–7 exerts a potent vasodilator, anti-fibrotic, anti-proliferation and anti-inflammatory effect via activation of its Mas receptor. Its effects counterbalance the ACE1-Ang II-ATR1 system [24].
On a similar manner, ACE1 inhibitor drugs (ACEIs) have an antihypertensive effect and substantially lower the risk of death, heart failure and stroke [25]. Patients with hypertension and diabetes benefit from the use of these drugs, since not only ACE2 is insensitive to blockade by ACE1 inhibitors, but also, the use of these inhibitor drugs increases the ACE2 gene expression and activity, probably due to an accumulation of Ang I [26]. ACE2 has been found to have protective effects against lung injury in different lung injury animal models [8], [27], [28]. Specifically, in diabetes, ACE2 seems to have a protective role in the progression of cardiovascular and renal complications and has been suggested as a potential therapeutic target for the management of diabetes and its complications [29], [30]. Studies in mice showed the role of ACE2 in the improvement of glycemia levels in mice with diabetes by direct effects in the pancreas [19], improving insulin sensitivity and glucose-mediated insulin release [31] and reduction of the risk of type 2 diabetes development [32].
The effect of diabetes in the expression of ACE2 is not well established. Studies in animal models of diabetes evidenced either an increased or reduced expression of ACE2 in renal tissues and pancreatic tissues, depending on the disease stage. On contrary, the levels of ACE2 in lung tissue of mice with diabetes seem to be lower when compared to renal and pancreatic tissues [29], [33]. Similarly, a study in non-obese diabetic (NOD) mouse model showed an increase of ACE2 in serum, liver and pancreas, but not in the lung [34]. A study performed in 2012 by Soro-Paavonen et al. showed increased serum ACE2 activity in type 1 Diabetes mellitus (DM) patients with vascular complications but not in those without complications [35].
It has been found that ACEIs and angiotensin II receptor blockers (ARBs) cause an overexpression of ACE2 in patients treated with these drugs [26]. In the study of Soro-Paavonen, patients treated with ACEIs had increased ACE2 activity, independently of the presence of vascular complications [35]. However, the expression of ACE2 mRNA was not measured. Expression levels of ACE2 have been associated with susceptibility to SARS-CoV and SARS-CoV-2 infection in different cell lines [7], [36], [37], therefore, raising the concern that patients being treated with ACEIs or ARBs could be at higher risk of infection and of associated morbidity and mortality after a SARS-CoV-2 infection, due to a higher expression of the virus’ entry gate in target tissues [38]. Nevertheless, conflicting information has been found on this topic and some data suggest that ACEIs and ARBs can have protective effects against lung injury [39]. With relatively few clinical studies on this matter, when compared to the pre-clinical studies in animal models, it may be erroneous to admit that the effects of RAS inhibitors on ACE2 expression are translatable to human physiology. Additionally the measurements of ACE2 plasma levels, performed in most studies, may not be a reliable indicator of ACE2 activity, since the full length protein is predominantly membrane bound [39]. Taking advantage of ACE2, SARS-CoV-2 gains access to the cells, however it has been shown that soon after infection ACE2 expression is rapidly downregulated [8]. Whether this effect is caused by the virus, to prevent ACE2 protective effects [28], or results from an indirect mechanism is not yet clear. It has been confirmed in some clinical studies that the long-term use of ACEIs or ARBs by patients is not associated with an increased risk of SARS-CoV-2 infection, neither of developing severe COVID-19 or even with a higher risk of in-hospital death [40], [41], [42]. All these studies highlight that the withdrawal of these medications is not recommended to prevent serious COVID-19, since these have well-known benefits in protecting the kidney and myocardium, [39] with the clinical decompensation caused by its removal potentially causing a more serious condition than the viral infection.
3. SARS-COV-2 on diabetes development and management: The importance of regulating blood glucose levels
The multi-organ damage is characteristic of SARS, nevertheless the major affected organs include the lungs, heart and kidney. The severity of disease progression and death predictor factors include old age, thrombocytopenia, severe hypoxia and hyperglycemia [43]. Hyperglycemia can also be a consequence of the SARS-CoV infection, due to the ACE2-dependent damage of pancreatic islets and exocrine tissue, as islet damage, elevation on fasting plasma glucose levels and diabetes development during hospitalization have all been reported [43]. Although the pancreas damage was transient to most patients, in some cases diabetes remained after 3-years follow-up [43]. In the case of SARS-CoV-2 the same transient damage in the pancreas has already been documented [44], and given its higher infectivity and affinity for the ACE2 receptor, there is increased concern relative to the complications caused by hyperglycemia, as well as the long-term effects of the infection on recovered patients.
Hyperglycemia is characteristic of diabetes, when this chronic metabolic disorder is left untreated, which leads to serious complications ranging from limb amputations, kidney failure, blindness or cardiovascular disease [45], [46]. This disorder may be caused by insufficient insulin production by the pancreas, resistance to insulin action or a mixture of both [46]. Therefore, as hyperglycemia underlies many of the complications developed in the disease course, a tight control of glucose blood levels in patients with diabetes is essential.
Since the beginning of COVID-19 outbreak, diabetes has been reported as one of the high-risk factors for rapid disease progression and bad prognosis of COVID-19 [47]. For instance, a retrospective cohort study with 191 Chinese patients infected with SARS-CoV-2 showed that 48% of the patients had a comorbidity, with diabetes representing 19% of those patients [48]. Another study showed that among 26 deaths due to SARS-CoV-2 in Wuhan, 42.3% had diabetes [49]. Also, a different cohort study analyzing 201 patients from Wuhan with confirmed COVID-19 pneumonia revealed that 10.9% of the patients had diabetes. They also observed that among the patients who developed acute respiratory distress syndrome (ARDS) (41.8% from the total cohort), more patients had comorbidities than those who did not develop ARDS, being diabetes the second most frequent comorbidity (19.0% in ARDS-patients versus 5.1% in non-ARDS patients) [50]. Furthermore, the largest case series of COVID-19 in China, reported by the Chinese Center for Disease Control and Prevention, showed that DM patients had higher mortality rates (7.3%) when compared to overall population (2.3%) in a total of 72,314 analyzed cases [51]. This comes as no surprise, as it is reported that people with diabetes demonstrate higher susceptibility to several infectious diseases, such as tuberculosis, pneumonia or influenza [52]. The underlying mechanisms are not completely understood and depend on the type of infection, but some hypotheses have been raised. Some possible explanations for DM being a high-risk factor for COVID-19 may be due to hyperglycemic environment, which is known to increase the virulence of some pathogens. Besides, it was also reported that phagocytosis and chemotaxis are impaired, the production of interleukins in response to infection is reduced, as well as the response of T cells and neutrophils [52], [53]. Overall, the immune response, which is vital to fight against COVID-19 infection, is impaired, especially in diabetic patients with poor blood glucose control.
Furthermore, several studies have shown that DM patients have a significant decrease in forced vital capacity (FVC) and forced expiratory volume in one second (FEV1), which are important indicators of lung function. This impaired pulmonary function was significantly associated with poorly controlled diabetes and consequently hyperglycemic levels [54], [55], [56]. Therefore, this reduced pulmonary capacity may also increase susceptibility to respiratory infections, possibly representing another factor in the myriad of events that might increase the vulnerability of DM patients towards COVID-19.
4. Therapeutics
In the absence of a specific antiviral drug, physicians are considering and trying lopinavir, ritonavir, interferon-1b, RNA polymerase inhibitor, remdesivir and tamiflu that were already reported for other diseases [57]. Inclusively, zinc oxide nanoparticles have also been considered, since they were shown to have inhibitory effects on H1N1 viral load [58]. Plus, vitamin C is also a good supplement for the immune system and has some preventive effects on pneumonia [59]. However, none of these have shown yet evidences of being beneficial for COVID-19.
As mentioned, it is suggested that therapeutics for diabetes and hypertension, namely ACEIs and ARBs, are responsible for upregulating ACE2. On the other hand, this is the functional receptor that SARS-CoV-2 uses as cellular entry [9]. In this sense, some authors hypothesize that these therapeutics may contribute for the increased infection and advice to discontinue ACEIs and ARBs, used in patients with diabetes or hypertension. However, there is no clear evidence in animals nor humans confirming this theory. Besides, ACE2 can also be increased by thiazolidinediones and ibuprofen, as well as exercise and dehydration. Plus, it was very recently published a Chinese study showing that transplantation of ACE2-mesenchymal stem cells improves the outcome of patients with COVID-19 pneumonia [60]. Some studies have actually already shown that overexpressed ACE2 plays a protective role in the lungs with SARS-CoV-2 infection, suggesting ARBs and ACEIs as therapy [61], [62]. As proof, in a preclinical study, authors injected animals with the spike glycoprotein of SARS-CoV, to cause a severe lung injury and verified that ACE2 is significantly downregulated. After treating them with ARB losartan, the severe acute lung injury was attenuated [8]. This evidence was supported by findings from China, where they showed that ACE2 blockade resulted in exacerbated lung damage and reduced animal survival after respiratory syncytial virus infection [28]. Actually, there is a comment from an Israel author, published in early March, proposing ARBs and ACEIs as a treatment for patients with COVID-19 infection to reduce the risk or severity of viral pneumonia [63]. However, when the coronavirus spike protein binds to ACE2, there is a downregulation of ACE2, which leads to an excessive accumulation of angiotensin II (vasoconstrictor, pulmonary inflammation, fibrosis, edema) and less ACE2 to convert it to angiotensin 1–7 (vasodilator, anti-proliferative, cytoprotective). The big question here is to know who wins this battle: the virus that binds to ACE2, which is upregulated in lungs, or the protective effects caused by the ACE2 upregulation. And this is not clarified yet. In this sense, European Medicines Agency (EMA) recommend that treatment with ARBs and ACEIs should be maintained in patients with diabetes and hypertension [64]. Patients who stop taking them may face more complications regarding kidney failure and increased mortality. Either way, as an alternative treatment, calcium channel blockers (CCBs) can be used, since they seem not to increase ACE2 expression and activity [65].
Commonly, and according to standard procedure, very sick patients should stop taking metformin and sodium-glucose transporter 2 inhibitors, due to their adverse side effects, as acidosis and fat metabolism [66]. In addition, the glucagon-like peptide receptor–1 analogues can also be stopped, since they may cause nausea, vomiting, and pioglitazone, among other side effects described elsewhere [67]. Plus, aromatase inhibitors should also be stopped since they reduce insulin sensitivity and insulin should be the only one used in acutely sick patients or with severe breathing disorders [68]. Only when recovered or stabilized, noninsulin therapy can be introduced.
Knowing that the virus infection is a multistep process, there are some possible targets to treat COVID-19. A strong candidate that could exert a potent antiviral effect is the anti-malaria chloroquine. It is described that the virus processing and internalization is facilitated by low pH and pH-dependent endosomal cysteine protease cathepsins [69]. Chloroquine becomes entrapped in membrane-enclosed low pH organelles and is rapidly protonated and concentrated in endosomes, interfering with their acidification. Hydroxychloroquine has been then considered for short-term treatment trials [70]. The antiviral activity of chloroquine combined with azithromycin against COVID-19 in vitro was recently reported. However, the authors found no evidence of a strong antiviral activity or clinical benefit of this combination for the treatment of hospitalized patients with severe COVID-19. Either way, ongoing randomized clinical trials with hydroxychloroquine should provide a definitive answer regarding the alleged efficacy of this combination and will assess its safety [71]. Also, amiodarone has the ability to interfere with the endocytic pathway, being suggested as a possible inhibitor of the SARS coronavirus [72]. After binding to ACE2, the virus requires the essential serine protease, TMPRSS2, for S protein priming. So, using TMPRSS2 inhibitors (e.g. camostat mesylate), already used to treat cancer and hepatitis, can be a possible or adjuvant therapy [73].
According to EMA, the potential treatments that are in clinical trials are: remdesivir (investigational), lopinavir/ritonavir (anti-HIV), chloroquine and hydroxychloroquine (anti-malaria and rheumatoid arthritis), systemic interferons as interferon beta (multiple sclerosis) and monoclonal antibodies with activity against components of the immune system [74]. Plus, all the diagnostics, treatments and vaccines considered for COVID-19 are summed up in Artis Ventures platform [75].
5. Conclusion
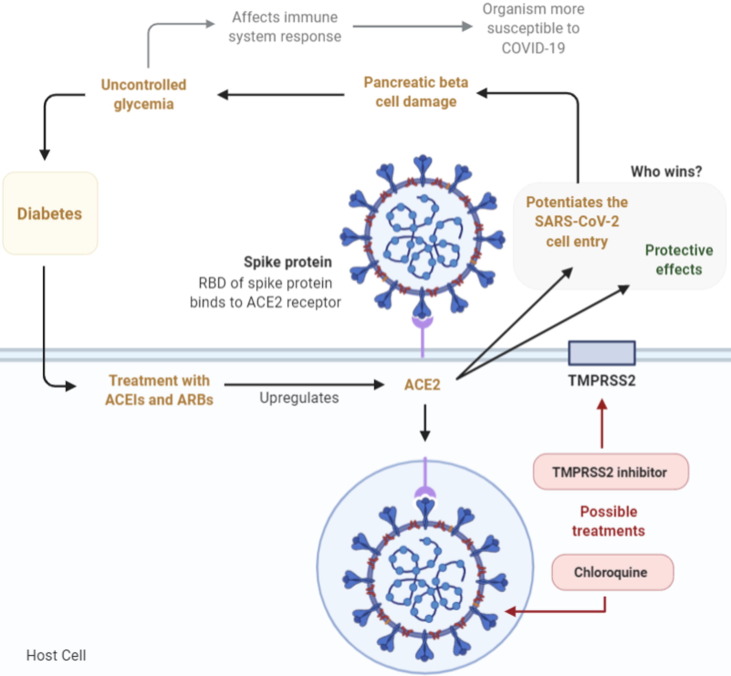
Overall, the chance of developing serious complications due to SARS-CoV-2 infection is higher in people with more health conditions associated. As discussed above, diabetes and all the complications associated with this disease, such as weakened immune response or hyperglycemia, present a higher risk for infected patients (Fig. 1 ). Not only for the COVID-19 progression, but also as a higher risk to develop secondary infections and therefore worsening of the health state. For those reasons, an effective and tight management of diabetes, specifically of glucose plasma levels, is extremely important in infected patients with diabetes. Additionally, while the use of ACEIs and ARBs in SARS-CoV-2 infected patients has raised some questions regarding their beneficial or harmful effects on disease progression, there is not enough evidence yet that allows drawing conclusions on this issue. Therefore, while care must be taken in the use of these drugs, their abrupt withdrawal is not recommended as it could lead to even more serious complications. Several strategies are being tested to control the COVID-19 pandemic and a better understanding of the SARS-CoV-2 effects on high-risk patients is fundamental to decrease the morbidities and mortality.
Fig. 1.
Schematic representation of SARS-CoV-2 internalization in the host cell and possible causes or effects of uncontrolled glycemia in viral infection. The virus may take advantage of physiopathological features of DM to trigger a more efficient infection, either by attaching to putatively overexpressed ACE2 in target organs of DM treated with ACEIs/ARBs or taking advantage of an underactive immune system characteristic of the disease. The viral mechanism of action affects diabetes, direct and indirectly, and can possible be treated by TMPRSS2 inhibitor or chloroquine, among other treatments previously mentioned. ACE2: angiotensin-converting enzyme 2; ACEI: ACE1 inhibitor drugs; ARBs: angiotensin II receptor blockers; RBD: receptor-binding domain; TMPRSS2: transmembrane serine protease 2.
Acknowledgments
Acknowledgments
This work was financed by FEDER - Fundo Europeu de Desenvolvimento Regional funds through the COMPETE 2020 - Operacional Programme for Competitiveness and Internationalisation (POCI), Portugal 2020, and by Portuguese funds through FCT - Fundação para a Ciência e a Tecnologia/ Ministério da Ciência, Tecnologia e Ensino Superior in the framework of the project PTDC/MED-OUT/30466/2017 and “Institute for Research and Innovation in Health Sciences” (FCT - UID/BIM/04293/2019). Cecília Cristelo, Cláudia Azevedo and Joana Marques would like to thank to Fundação para a Ciência e a Tecnologia (FCT), Portugal for financial support (SFRH/BD/139402/2018, SFRH/BD/117598/2016 and PD/BD/145149/2019, respectively).
Author Contributions
B.S. conceived the overall study design; C.C., C.A., J.M.M. and R.N. contributed equally in drafting the manuscript; all authors critically revised the manuscript.
Declarations of Competing Interest
None.
References
- 1.European Centre for Disease Prevention and Control. Situation Update Worldwide, as of 23 April 2020. 2020 [accessed May 5th, 2020]; https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases.
- 2.Lu R., Zhao X., Li J. Genomic Characterisation and Epidemiology of 2019 Novel Coronavirus: Implications for Virus Origins and Receptor Binding. The Lancet. 2020;395(10224):565–574. doi: 10.1016/S0140-6736(20)30251-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan J.F., Kok K.H. Genomic Characterization of the 2019 Novel Human-Pathogenic Coronavirus Isolated from a Patient with Atypical Pneumonia after Visiting Wuhan. Emerg Microbes Infect. 2020;9(1):221–236. doi: 10.1080/22221751.2020.1719902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhu N., Zhang D., Wang W. A Novel Coronavirus from Patients with Pneumonia in China, 2019. New Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wu A., Peng Y., Huang B. Genome Composition and Divergence of the Novel Coronavirus (2019-Ncov) Originating in China. Cell Host Microbe. 2020;27(3):325–328. doi: 10.1016/j.chom.2020.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu X., Chen P., Wang J. Evolution of the Novel Coronavirus from the Ongoing Wuhan Outbreak and Modeling of Its Spike Protein for Risk of Human Transmission. Sci China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li W., Moore M.J., Vasilieva N. Angiotensin-Converting Enzyme 2 Is a Functional Receptor for the Sars Coronavirus. Nature. 2003;426(6965):450–454. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kuba K., Imai Y., Rao S. A Crucial Role of Angiotensin Converting Enzyme 2 (Ace2) in Sars Coronavirus-Induced Lung Injury. Nat Med. 2005;11(8):875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wan Y., Shang J., Graham R., Baric R.S., Li F. Receptor Recognition by the Novel Coronavirus from Wuhan: An Analysis Based on Decade-Long Structural Studies of Sars Coronavirus. J Virol. 2020;94(7):e00127–e220. doi: 10.1128/jvi.00127-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tai W., He L., Zhang X. Characterization of the Receptor-Binding Domain (Rbd) of 2019 Novel Coronavirus: Implication for Development of Rbd Protein as a Viral Attachment Inhibitor and Vaccine. Cell Mol Immunol. 2020 doi: 10.1038/s41423-020-0400-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoffmann M., Kleine-Weber H., Schroeder S. Sars-Cov-2 Cell Entry Depends on Ace2 and Tmprss2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020;181:1–10. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wrapp D., Wang N., Corbett K.S. Cryo-Em Structure of the 2019-Ncov Spike in the Prefusion Conformation. Science. 2020;367(6483):1260–1263. doi: 10.1126/science.abb2507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tipnis S.R., Hooper N.M., Hyde R. A Human Homolog of Angiotensin-Converting Enzyme: Cloning and Functional Expression as a Captopril-Insensitive Carboxypeptidase. J Biol Chem. 2000;275(43):33238–33243. doi: 10.1074/jbc.M002615200. [DOI] [PubMed] [Google Scholar]
- 14.Donoghue M., Hsieh F., Baronas E. A Novel Angiotensin-Converting Enzyme-Related Carboxypeptidase (Ace2) Converts Angiotensin I to Angiotensin 1–9. Circ Res. 2000;87(5):E1–E9. doi: 10.1161/01.res.87.5.e1. [DOI] [PubMed] [Google Scholar]
- 15.Hamming I., Timens W., Bulthuis M.L. Tissue Distribution of Ace2 Protein, the Functional Receptor for Sars Coronavirus. A First Step in Understanding Sars Pathogenesis. J Pathol. 2004;203(2):631–637. doi: 10.1002/path.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zou X., Chen K., Zou J. Single-Cell Rna-Seq Data Analysis on the Receptor Ace2 Expression Reveals the Potential Risk of Different Human Organs Vulnerable to 2019-Ncov Infection. Front Med. 2020 doi: 10.1007/s11684-020-0754-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chai X., Hu L., Zhang Y. Specific Ace2 Expression in Cholangiocytes May Cause Liver Damage after 2019-Ncov Infection. bioRxiv. 2020 doi: 10.1101/2020.02.03.931766. [DOI] [Google Scholar]
- 18.Lau T., Carlsson P.O., Leung P.S. Evidence for a Local Angiotensin-Generating System and Dose-Dependent Inhibition of Glucose-Stimulated Insulin Release by Angiotensin Ii in Isolated Pancreatic Islets. Diabetologia. 2004;47(2):240–248. doi: 10.1007/s00125-003-1295-1. [DOI] [PubMed] [Google Scholar]
- 19.Bindom S.M., Hans C.P., Xia H., Boulares A.H., Lazartigues E. Angiotensin I-Converting Enzyme Type 2 (Ace2) Gene Therapy Improves Glycemic Control in Diabetic Mice. Diabetes. 2010;59(10):2540–2548. doi: 10.2337/db09-0782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu H., Zhong L., Deng J. High Expression of Ace2 Receptor of 2019-Ncov on the Epithelial Cells of Oral Mucosa. Int J Oral Sci. 2020;12(1):8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang H, Kang Z, Gong H, et al. The Digestive System Is a Potential Route of 2019-Ncov Infection: A Bioinformatics Analysis Based on Single-Cell Transcriptomes. bioRxiv, 2020: p. 2020.01.30.927806. https://doi.org/10.1101/2020.01.30.927806.
- 22.Colafella K.M.M., Bovée D.M., Danser A.H.J. The Renin-Angiotensin-Aldosterone System and Its Therapeutic Targets. Exp Eye Res. 2019;186 doi: 10.1016/j.exer.2019.05.020. [DOI] [PubMed] [Google Scholar]
- 23.Skeggs L.T., Jr., Kahn J.R., Shumway N.P. The Preparation and Function of the Hypertensin-Converting Enzyme. J Exp Med. 1956;103(3):295–299. doi: 10.1084/jem.103.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Iwai M., Horiuchi M. Devil and Angel in the Renin-Angiotensin System: Ace-Angiotensin Ii–At1 Receptor Axis Vs. Ace2–Angiotensin-(1–7)–Mas Receptor Axis. Hypertens Res. 2009;32(7):533–536. doi: 10.1038/hr.2009.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vickers C., Hales P., Kaushik V. Hydrolysis of Biological Peptides by Human Angiotensin-Converting Enzyme-Related Carboxypeptidase. J Biol Chem. 2002;277(17):14838–14843. doi: 10.1074/jbc.M200581200. [DOI] [PubMed] [Google Scholar]
- 26.Ferrario C.M., Jessup J., Chappell M.C. Effect of Angiotensin-Converting Enzyme Inhibition and Angiotensin Ii Receptor Blockers on Cardiac Angiotensin-Converting Enzyme 2. Circulation. 2005;111(20):2605–2610. doi: 10.1161/CIRCULATIONAHA.104.510461. [DOI] [PubMed] [Google Scholar]
- 27.Zou Z., Yan Y., Shu Y. Angiotensin-Converting Enzyme 2 Protects from Lethal Avian Influenza a H5n1 Infections. Nat Commun. 2014;5(1):3594. doi: 10.1038/ncomms4594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gu H., Xie Z., Li T. Angiotensin-Converting Enzyme 2 Inhibits Lung Injury Induced by Respiratory Syncytial Virus. Sci Rep. 2016;6:19840. doi: 10.1038/srep19840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tikellis C., Bialkowski K., Pete J. Ace2 Deficiency Modifies Renoprotection Afforded by Ace Inhibition in Experimental Diabetes. Diabetes. 2008;57(4):1018. doi: 10.2337/db07-1212. [DOI] [PubMed] [Google Scholar]
- 30.Batlle D., Soler M.J., Ye M. Ace2 and Diabetes: Ace of Aces? Diabetes. 2010;59(12):2994–2996. doi: 10.2337/db10-1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tocci G., Paneni F., Palano F. Angiotensin-Converting Enzyme Inhibitors, Angiotensin Ii Receptor Blockers and Diabetes: A Meta-Analysis of Placebo-Controlled Clinical Trials. Am J Hypertens. 2011;24(5):582–590. doi: 10.1038/ajh.2011.8. [DOI] [PubMed] [Google Scholar]
- 32.Abuissa H., Jones P.G., Marso S.P., O'Keefe J.H., Jr. Angiotensin-Converting Enzyme Inhibitors or Angiotensin Receptor Blockers for Prevention of Type 2 Diabetes: A Meta-Analysis of Randomized Clinical Trials. J Am Coll Cardiol. 2005;46(5):821–826. doi: 10.1016/j.jacc.2005.05.051. [DOI] [PubMed] [Google Scholar]
- 33.Ye M., Wysocki J., William J. Glomerular Localization and Expression of Angiotensin-Converting Enzyme 2 and Angiotensin-Converting Enzyme: Implications for Albuminuria in Diabetes. J Am Soc Nephrol. 2006;17(11):3067. doi: 10.1681/ASN.2006050423. [DOI] [PubMed] [Google Scholar]
- 34.Roca-Ho H., Riera M., Palau V., Pascual J., Soler M.J. Characterization of Ace and Ace2 Expression within Different Organs of the Nod Mouse. Int J Mol Sci. 2017;18(3) doi: 10.3390/ijms18030563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Soro-Paavonen A., Gordin D., Forsblom C. Circulating Ace2 Activity Is Increased in Patients with Type 1 Diabetes and Vascular Complications. J Hypertens. 2012;30(2):375–383. doi: 10.1097/HJH.0b013e32834f04b6. [DOI] [PubMed] [Google Scholar]
- 36.Hofmann H., Geier M., Marzi A. Susceptibility to Sars Coronavirus S Protein-Driven Infection Correlates with Expression of Angiotensin Converting Enzyme 2 and Infection Can Be Blocked by Soluble Receptor. Biochem Biophys Res Commun. 2004;319(4):1216–1221. doi: 10.1016/j.bbrc.2004.05.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jia H.P., Look D.C., Shi L. Ace2 Receptor Expression and Severe Acute Respiratory Syndrome Coronavirus Infection Depend on Differentiation of Human Airway Epithelia. J Virol. 2005;79(23):14614. doi: 10.1128/JVI.79.23.14614-14621.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fang L., Karakiulakis G., Roth M. Are Patients with Hypertension and Diabetes Mellitus at Increased Risk for Covid-19 Infection? Lancet Respirat Med. 2020;8(4) doi: 10.1016/S2213-2600(20)30116-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vaduganathan M., Vardeny O., Michel T. Renin-Angiotensin-Aldosterone System Inhibitors in Patients with Covid-19. New Engl J Med. 2020;382(17):1653–1659. doi: 10.1056/NEJMsr2005760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mancia G., Rea F., Ludergnani M., Apolone G., Corrao G. Renin-Angiotensin-Aldosterone System Blockers and the Risk of Covid-19. New Engl J Med. 2020 doi: 10.1056/NEJMoa2006923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reynolds H.R., Adhikari S., Pulgarin C. Renin-Angiotensin-Aldosterone System Inhibitors and Risk of Covid-19. New Engl J Med. 2020 doi: 10.1056/NEJMoa2008975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mehra M.R., Desai S.S., Kuy S., Henry T.D., Patel A.N. Cardiovascular Disease, Drug Therapy, and Mortality in Covid-19. New Engl J Med. 2020 doi: 10.1056/NEJMoa2007621. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 43.Yang J.-K., Lin S.-S., Ji X.-J., Guo L.-M. Binding of Sars Coronavirus to Its Receptor Damages Islets and Causes Acute Diabetes. Acta Diabetol. 2010;47:193–199. doi: 10.1007/s00592-009-0109-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Liu F, Long X, Zou W, et al. Highly Ace2 Expression in Pancreas May Cause Pancreas Damage after Sars-Cov-2 Infection. medRxiv, 2020: p. 2020.02.28.20029181. https://doi.org/10.1101/2020.02.28.20029181.
- 45.Rao Kondapally Seshasai S., Kaptoge S., Thompson A., Di Angelantonio E., Gao P., Sarwar N. New Engl J Med. 2014;364(9):829–841. doi: 10.1056/NEJMoa1008862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.World Health Organization Classification of Diabetes Mellitus. 2019:2019. [Google Scholar]
- 47.Guo W., Li M., Dong Y., Zhou H., Zhang Z., Tian C. Diabetes Is a Risk Factor for the Progression and Prognosis of Covid-19. Diabet Metab Res Rev. 2020 doi: 10.1002/dmrr.3319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fei Zhou T.Y. Ronghui Du, Guohui Fan, Ying Liu, Zhibo Liu, Jie Xiang, Yeming Wang, Bin Song, Xiaoying Gu, Lulu Guan, Yuan Wei, Clinical Course and Risk Factors for Mortality of Adult Inpatients with Covid-19 in Wuhan, China: A Retrospective Cohort Study. The Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Deng S.-Q. and Hong-Juan Peng, Characteristics of and Public Health Responses to the Coronavirus Disease 2019 Outbreak in China. J Clin Med. 2020;9(2):575. doi: 10.3390/jcm9020575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wu C., Chen X., Cai Y. Risk Factors Associated with Acute Respiratory Distress Syndrome and Death in Patients with Coronavirus Disease 2019 Pneumonia in Wuhan, China. JAMA Internal Med. 2020 doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu Z., McGoogan J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 52.Casqueiro J., Casqueiro J., Alves C. Infections in Patients with Diabetes Mellitus: A Review of Pathogenesis. Indian J Endocrinol Metabol. 2012 doi: 10.4103/2230-8210.94253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Peleg Y., Weerarathna T., McCarthy J.S., Davis T. Common Infections in Diabetes: Pathogenesis, Management and Relationship to Glycaemic Control. Diabet Metab Res Rev. 2007 doi: 10.1002/dmrr.682. [DOI] [PubMed] [Google Scholar]
- 54.McKeever T.M., Weston P.J., Hubbard R., Fogarty A. Lung Function and Glucose Metabolism: An Analysis of Data from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2005;161(6):546–556. doi: 10.1093/aje/kwi076. [DOI] [PubMed] [Google Scholar]
- 55.Yeh H.C., Punjabi N.M., Wang N.Y., Pankow J.S., Duncan B.B., Cox C.E. Cross-Sectional and Prospective Study of Lung Function in Adults with Type 2 Diabetes: The Atherosclerosis Risk in Communities (Aric) Study. Diabet Care. 2008 doi: 10.2337/dc07-1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Shah S.H., Sonawane P., Nahar P., Vaidya S., Salvi S. Pulmonary Function Tests in Type 2 Diabetes Mellitus and Their Association with Glycemic Control and Duration of the Disease. Lung India. 2013 doi: 10.4103/0970-2113.110417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gupta R., Ghosh A., Singh A.K., Misra A. Clinical Considerations for Patients with Diabetes in Times of Covid-19 Epidemic. Diabet Metab Syndrome. 2020;14(3):211–212. doi: 10.1016/j.dsx.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ghaffari H., Tavakoli A., Moradi A. Inhibition of H1n1 Influenza Virus Infection by Zinc Oxide Nanoparticles: Another Emerging Application of Nanomedicine. J Biomed Sci. 2019;26(1):70. doi: 10.1186/s12929-019-0563-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hemila H. Vitamin C Intake and Susceptibility to Pneumonia. Pediatr Infect Dis J. 1997;16(9):836–837. doi: 10.1097/00006454-199709000-00003. [DOI] [PubMed] [Google Scholar]
- 60.Leng Z., Zhu R., Hou W. Transplantation of Ace2 - Mesenchymal Stem Cells Improves the Outcome of Patients with Covid-19 Pneumonia. Aging and Disease. 2020;11(2):216–228. doi: 10.14336/AD.2020.0228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Sun M.L., Yang J.M., Sun Y.P., Su G.H. Inhibitors of Ras Might Be a Good Choice for the Therapy of Covid-19 Pneumonia. Chin J Tuberculosis Respirat Diseases. 2020;43(3):219–222. doi: 10.3760/cma.j.issn.1001-0939.2020.03.016. [DOI] [PubMed] [Google Scholar]
- 62.Li X.C., Zhang J., Zhuo J.L. The Vasoprotective Axes of the Renin-Angiotensin System: Physiological Relevance and Therapeutic Implications in Cardiovascular, Hypertensive and Kidney Diseases. Pharmacol Res. 2017;125(Pt A):21–38. doi: 10.1016/j.phrs.2017.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gurwitz D. Angiotensin Receptor Blockers as Tentative Sars-Cov-2 Therapeutics. Drug Dev Res. 2020 doi: 10.1002/ddr.21656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.European Medicines Agency. Ema Advises Continued Use of Medicines for Hypertension, Heart or Kidney Disease During Covid-19 Pandemic 2020 27/03/2020 [accessed April 3, 2020]; https://www.ema.europa.eu/en/news/ema-advises-continued-use-medicines-hypertension-heart-kidney-disease-during-covid-19-pandemic.
- 65.Murray K.M. Calcium-Channel Blockers for Treatment of Diabetic Nephropathy. Clin Pharm. 1991;10(11):862–865. [PubMed] [Google Scholar]
- 66.Hsia D.S., Grove O., Cefalu W.T. An Update on Sodium-Glucose Co-Transporter-2 Inhibitors for the Treatment of Diabetes Mellitus. Curr Opin Endocrinol Diabet Obes. 2017;24(1):73–79. doi: 10.1097/MED.0000000000000311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Filippatos T.D., Panagiotopoulou T.V., Elisaf M.S. Adverse Effects of Glp-1 Receptor Agonists. Rev Diabetic Stud. 2014;11(3–4):202–230. doi: 10.1900/RDS.2014.11.202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gibb F.W., Homer N.Z.M., Faqehi A.M.M. Aromatase Inhibition Reduces Insulin Sensitivity in Healthy Men. J Clin Endocrinol Metab. 2016;101(5):2040–2046. doi: 10.1210/jc.2015-4146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Perico L., Benigni A., Remuzzi G. Should Covid-19 Concern Nephrologists? Why and to What Extent? The Emerging Impasse of Angiotensin Blockade. Nephron. 2020:1–9. doi: 10.1159/000507305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Vincent M.J., Bergeron E., Benjannet S. Chloroquine Is a Potent Inhibitor of Sars Coronavirus Infection and Spread. Virol J. 2005;2:69. doi: 10.1186/1743-422x-2-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Molina J.M., Delaugerre C., Goff J.L. No Evidence of Rapid Antiviral Clearance or Clinical Benefit with the Combination of Hydroxychloroquine and Azithromycin in Patients with Severe Covid-19 Infection. Médecine et Maladies Infectieuses. 2020 doi: 10.1016/j.medmal.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stadler K., Ha H.R., Ciminale V. Amiodarone Alters Late Endosomes and Inhibits Sars Coronavirus Infection at a Post-Endosomal Level. Am J Respir Cell Mol Biol. 2008;39(2):142–149. doi: 10.1165/rcmb.2007-0217OC. [DOI] [PubMed] [Google Scholar]
- 73.Hoffmann M., Kleine-Weber H., Schroeder S. Sars-Cov-2 Cell Entry Depends on Ace2 and Tmprss2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell. 2020 doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.European Medicines Agency. Update on Treatments and Vaccines against Covid-19 under Development. 2020 [accessed April 6, 2020]; https://www.ema.europa.eu/en/news/update-treatments-vaccines-against-covid-19-under-development.
- 75.Bailey V., Guttendorf Z. Fight the Pandemic. 2020 [accessed April 6, 2020]; https://www.av.co/covid.