Abstract
We analyzed disease outcomes for patients with diabetes and laboratory-confirmed COVID-19 who were managed outpatient and followed by the Emory COVID-19 Virtual Outpatient Management Clinic (ECVOMC). The rate of hospitalization for patients with diabetes was double the overall rate of hospitalization for patients in the ECVOMC.
Keywords: Coronavirus, Telemedicine, Outpatient management
1. Introduction
With the emergence of coronavirus disease 2019 (COVID-19), diabetes mellitus has been identified as a risk factor for severe COVID-19 illness [1], [2]. However, the studies leading to the conclusion that diabetes is a risk factor for severe COVID-19 are based on limited data in hospitalized patients. In order to assess diabetes as a risk factor for hospitalization, we analyzed disease outcomes for outpatients with a diagnosis of Type 2 diabetes mellitus and laboratory-confirmed COVID-19 monitored by the Emory COVID-19 Virtual Outpatient Management Clinic (ECVOMC).
2. Materials and methods
The ECVOMC follows patients with laboratory-confirmed COVID-19 (PCR-positive nasopharyngeal swab) who are in isolation at home. On enrollment, the patient is evaluated by a physician or Advanced Practice Provider (APP) via audio-visual telemedicine and is assigned to a Risk Tier 1–3 (low, intermediate, or high risk, respectively) based on a clinical assessment of their risk for hospitalization, including symptom severity, age, or high-risk comorbidity [3]. A patient’s Risk Tier determines the frequency of follow-up telephone calls from the ECVOMC team member (registered nurse for Tiers 1 and 2, APP for Tier 3). The Risk Tier can be increased based on clinical worsening or can be downgraded if symptoms improve. Clinical follow-up continues until symptom improvement or the isolation period ends.
We conducted a retrospective chart review of all patients enrolled in the ECVOMC with a diagnosis of diabetes in their problem list, COVID testing by PCR between March 16 and April 24, 2020, and who had one or more follow-up phone calls after their initial telemedicine visit. Patient demographics, comorbidities, presenting symptoms, medications, and initial Risk Tier assignment were obtained. Data were collected for a minimum of two weeks after symptom onset.
3. Results
Sixty-five patients were identified, representing 12.4% of all patients enrolled in the ECVOMC. Forty-nine patients met inclusion criteria and sixteen were excluded: seven had been hospitalized and discharged prior to ECVOMC referral (to monitor their recovery), four did not follow-up due to symptom resolution or patient preference, and five were referred directly to the emergency department (ED) after initial ECVOMC contact.
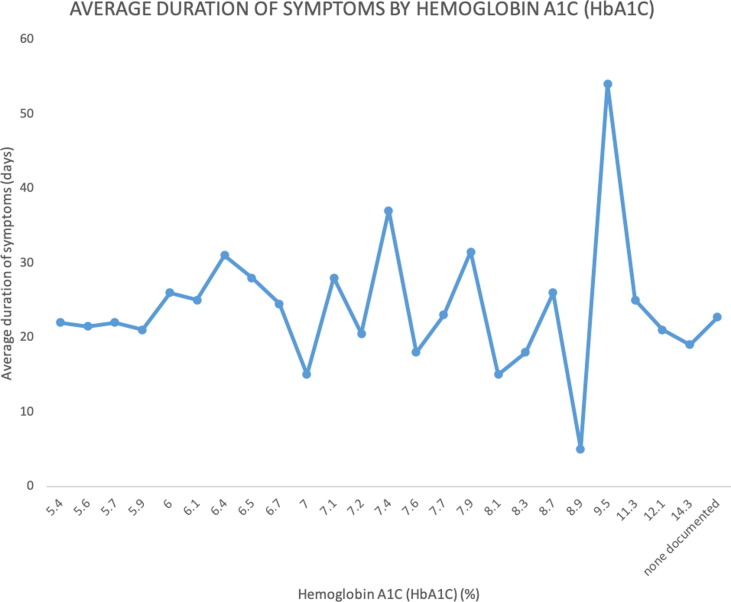
Patient characteristics are presented in Table 1 . The median age was 59 years. Most of the patients were female (73%). The majority of the cohort was African American (67%). The most common presenting symptoms were cough (n = 40) and fever (n = 27). On average, patients were managed for 13.8 days and received 13.2 calls. The average duration of illness, from symptom onset to ECVOMC discharge, was 23.7 days and did not correlate with HbA1C (Fig. 1 ). Four patients (8.2%) required in-person respiratory clinic assessments during enrollment. Five patients (10.2%) were hospitalized after an average of 2.4 days in ECVOMC. The hospitalization rate for all patients in ECVOMC is 5.1%, including those admitted to Emory hospitals or with documented admission to an outside hospital. Two patients died after hospital admission: (1) a 65-year-old male with obesity, hypertension, and most recent hemoglobin A1C (HbA1C) of 8.9% was referred to the ED after two days in ECVOMC and died after seven days in the hospital due to acute respiratory distress syndrome and cytokine storm; (2) a female, age > 90 years, with Alzheimer’s dementia was referred for inpatient hospice due to worsening respiratory symptoms and died after five days in the hospital.
Table 1.
Patient Characteristics.
| Variable | N = 49 |
|---|---|
| Median Age | 59 (Range: 30–94) |
| Median of most recent HbA1C | 7.2 (Range: 5.4–14.3) |
| Median BMI | 33.9 (Range: 21.5–63.9) |
| Median duration of symptoms (days) | 22 (Range: 5–54) |
| Median time from initial screening call to COVID testing (days) | 1 (Range: 0–7) |
| Median duration of program enrollment (days) | 14 (Range: 1–31) |
| Median number of follow-up calls | 12 (Range: 1–37) |
| Gender | |
| Male | 13 (27%) |
| Female | 36 (73%) |
| Race | |
| White or Caucasian | 7 (14%) |
| Black or African American | 33 (67%) |
| Asian | 2 (4%) |
| Other | 7 (14%) |
| Initial Risk Tier Assignment | |
| Low Risk | 6 (12%) |
| Intermediate Risk | 25 (51%) |
| High Risk | 18 (37%) |
| Presence of Comorbidities | |
| Hypertension | 38 (78%) |
| Obesity (BMI > 30) | 31 (63%) |
| Renal disease | 8 (16%) |
| Lung disease | 11 (22%) |
| Cardiac disease | 7 (14%) |
| Eye disease | 2 (4%) |
| Smoking Status | |
| Active Smoker | 2 (4%) |
| Former Smoker | 9 (18%) |
| Never Smoker | 38 (78%) |
| Diabetes medications | |
| Insulin | 15 (31%) |
| Metformin | 39 (80%) |
| Other oral medications | 20 (41%) |
| Total number of active medications | |
| 0 | 1 (2%) |
| 1–4 | 9 (18%) |
| 5–8 | 21 (43%) |
| 9+ | 18 (37%) |
| Hypertensive Medications | |
| CCB | 24 (49%) |
| ACE-I | 14 (29%) |
| ARB | 16 (33%) |
| Beta blocker | 15 (31%) |
| Thiazide | 19 (39%) |
| Presenting Symptoms | |
| Cough | 40 (82%) |
| Fever | 27 (55%) |
| Loss of smell or taste | 23 (47%) |
| Chills | 23 (47%) |
| SOB with exertion | 23 (47%) |
| Body aches | 22 (45%) |
| Headache | 18 (37%) |
| Diarrhea | 18 (37%) |
| Sinus congestion | 15 (31%) |
| Sore throat | 15 (31%) |
| Chest tightness | 12 (24%) |
| Dizziness when standing | 11 (22%) |
| SOB at rest | 11 (22%) |
| Joint pain | 7 (14%) |
| Nausea | 7 (14%) |
| Anorexia | 4 (8%) |
| Hyperglycemia | 4 (8%) |
| Abdominal Pain | 4 (8%) |
| Confusion | 4 (8%) |
| Wheezing | 3 (6%) |
| Rash | 0 (0%) |
ACE-I: angiotensin converting enzyme inhibitor; ARB: angiotensin receptor blocker; BMI: body mass index; CCB: calcium channel blocker; HbA1C: hemoglobin A1C; SOB: shortness of breath.
Fig. 1.
Average duration of symptoms in days by Hemoglobin A1C (HbA1C).
4. Discussion
In this study, we report the outcomes of our first 49 patients with diabetes managed outpatient in the ECVOMC. We found that the rate of hospitalization for patients with diabetes in ECVOMC was double the rate of hospitalization for all ECVOMC patients. These findings support prior reports describing increased risk of severe COVID-19 for individuals with diabetes [1], [2]. However, this study is notable for analyzing the outcomes of patients with diabetes who are managed outpatient as opposed to previous studies that looked at the hospitalized population.
We note that the rate of hospitalization in this study is low, despite the wide range of HbA1c and despite most patients having additional high-risk comorbidities (e.g. hypertension, obesity) [2]. This is likely due to our selecting a group for study that had been triaged and recommended for outpatient care. This is an important cohort, because the majority of patients with COVID-19 are well enough to remain home with telemedicine monitoring as the preferred approach [3]. The exclusion of patients immediately referred to the ED did not substantially impact number of patients in the study; around twelve percent of enrolled ECVOMC patients had diabetes, consistent with the prevalence of diabetes in the United States [4].
The time course to clinical worsening in our cohort was short; the five patients who were hospitalized were referred to the ED after only 2.4 days in the program. Additionally, the two patients who died after hospital admission were referred to the ED and hospitalized after one or two days in the program, faster than the patients who were hospitalized and recovered. HbA1C had no correlation with duration of symptoms, suggesting that length of illness may be independent of diabetes control. With a small sample size, we are unable to assess the potential role of HbA1c in predicting risk of hospitalization or death.
Our study was limited by small sample size due to limited testing availability and low event rate. We cannot determine risk factors for ED referral or hospitalization until larger cohorts of patients with diabetes are diagnosed with COVID-19 in the outpatient setting. The generalizability of our observations is limited by the telemedicine intervention inherent in ECVOMC enrollment. Finally, most patients were female, resulting in possible selection bias either in outpatient testing or in excluding hospitalized patients who tend to be male [5]. Outcomes may be affected by sex as a confounding variable, as females are known to develop less severe COVID-19 [5].
Current guidelines recommend that patients with diabetes and COVID-19 be considered for ED referral [6]. Our study demonstrates the appropriateness of assessment and management of this subgroup in an outpatient telemedicine program but supports categorization as “increased risk.” This report is hypothesis-generating and, after external validation with larger cohorts, may indicate that clinical guidelines for the management of these patients should be re-evaluated.
Declaration of Competing Interest
The authors declare no conflicts of interest.
Acknowledgments
Acknowledgements
The authors received no funding from an external source.
References
- 1.Guo W, Li M, Dong Y, et al. Diabetes is a risk factor for the progression and prognosis of COVID-19. Diab/Metabol Res Rev n/a(n/a):e3319. [DOI] [PMC free article] [PubMed]
- 2.Wang D., Hu B., Hu C. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Clinical Care Guidance. Coronavirus Disease 2019 (COVID-19) Web site. <https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-management-patients.html> Published 2020. Accessed May 12, 2020.
- 4.Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Department of Health and Human Services; 2020.
- 5.Grasselli G., Zangrillo A., Zanella A. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020 doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.College of Urgent Care Medicine and the American College of Emergency Physicians. Risk stratification guide for severity assessment and triage of suspected or confirmed COVID-19 patients (adults) in urgent care. In: American College of Emergency Physicians COVID-19 Field Guide. <https://www.acep.org/corona/covid-19-field-guide/triage/risk-stratification-and-triage-in-urgent-care/>: American College of Emergency Physicians; 2020.