Abstract
Introduction
The aim of the present study was to elucidate the foreseeable risk factors for suicidal ideation among Japanese perinatal women.
Methods
This cohort study was conducted in Nagoya, Japan, from July 2012 to March 2018. The Edinburgh Postnatal Depression Scale (EPDS) questionnaire was conducted at four time points: early pregnancy, late pregnancy, 5 days postpartum, and 1 month postpartum. A total of 430 women completed the questionnaires. A logistic regression analysis was performed using the presence of suicidal ideation on the EPDS as an objective variable. The explanatory variables were age, presence of physical or mental disease, smoking and drinking habits, education, hospital types, EPDS total score in early pregnancy, bonding, and quality and amount of social support, as well as the history of major depressive disorder (MDD).
Results
The rate of participants who were suspected of having suicidal ideation at any of the four time points was 11.6% (n=52), with the highest (n=25, 5.8%) at late pregnancy. For suicidal ideation, education level (OR: 1.19; 95% CI: 1.00–1.41; p=0.047), EPDS total points in the pregnancy period (OR: 1.25; 95% CI: 1.16–1.34; p < 0.000), a history of MDD (OR: 2.16; 95% CI: 1.00–4.79; p=0.049), and presence of mental disease (OR: 2.39; 95% CI: 1.00–5.70; p=0.049) were found to be risk factors for suicidal ideation. Age [odds ratio (OR): 0.88; 95% confidence interval (CI): 0.80–0.95; p=.002] and quality of social support (OR: 0.77; 95% CI: 0.60–0.99; p=.041) were found to be protective factors.
Conclusion
Based on these results, effective preventive interventions, such as increasing the quality of social support and confirming the history of depression, should be carried out in pregnant depressive women at the early stage of the perinatal period.
Keywords: major depressive disorder, harm avoidance, postpartum depression, suicidal ideation, self-harm
Introduction
Suicide prevention for expecting mothers is one of the most important problems in the field of perinatal mental health. A previous prospective cohort study reported that suicide was the leading cause of maternal death (8.7 per 100,000 women) in 2004–2015 in Tokyo, Japan (1). Maternal death rates (per 100,000 women) reported in countries other than Japan are as follows: 2.0 in the United States (2), 1.3 in Italy (3), 3.7 in Sweden (4), 5.9 in Finland (5), 2.6 in Canada (6), and 2.5 in the United Kingdom (7). Although the present survey is limited to Tokyo (1), the estimated suicide rate of perinatal women in Japan is higher than that in other countries.
Various psychosocial factors may be involved in maternal suicide. The following risk factors for maternal suicide have been reported: younger age (8, 9), unmarried (9), a history of family suicide, poverty (10), domestic violence (11), a history of abuse (12), racial issues (9, 13), regional isolation (9), anxiety (12, 14), suicidal ideation (15), a history of suicidal attempts (15), unexpected pregnancy (15), fetal and infant death (16), and mental disorders (14, 17, 18) such as major depressive disorder (MDD) (7, 8, 15, 19), bipolar disorder (19), and substance-related disorders (17).
In Japan, although general surveys on suicide have been widely conducted, research focusing on suicide among perinatal women is lacking. According to a Suicide Prevention Survey conducted in Japan in 2016 (20), young women had a high rate of experiencing suicidal ideation and suicide attempts. In that survey, the rates of women who had thoughts of suicidal ideation in their lifetime were reported to be 37.9 and 36.3% among those in their 20s and 30s, respectively, which translates to approximately 400,000 women among the total of 1,300,000 in that age range. In addition, about 200,000 women in their 20s and 30s have been estimated to have attempted suicide within the last year. According to a survey by the Ministry of Health, Labour and Welfare, the total number of suicides in 2018 among women in their 20s and 30s was 1,464 (21). About 40% of people who successfully committed suicide had attempted suicide at some point during their lifetime. Therefore, strategies such as introducing consultants for suicide prevention at a stage within suicidal ideation and providing psychosocial education for suicide prevention are frequently implemented in Japan. The need for similar activities for perinatal women has also been pointed out.
A number of studies have reported risk factors for suicidal ideation among perinatal women in countries other than Japan. A systematic review of 57 articles carried out by Gelaye et al. identified intimate partner violence, < 12 years of education, and MDD as risk factors for antenatal suicidal ideation (22).
A systematic review of 15 published research studies carried out by O'Connor et al. reported that women with a lower socioeconomic background and those who experience intimate partner violence are at increased risk for suicidal ideation (23). Ishida et al. examined the association between mental health problems in pregnant women and those in the postpartum period among 6,538 women aged 15–49 years in Paraguay, and reported that the risk for antenatal suicidal ideation was significantly higher when the pregnancy was unintended (24). They also reported that unintentionally pregnant women who had neither been in a union nor had a child were at a significantly higher risk for suicidal ideation compared with non-pregnant and non-postpartum women (24). Bodnar-Deren et al., who examined postnatal suicidal ideation among 1,073 mothers, reported that race/ethnicity, nativity, insurance, and language were significantly correlated with suicidal ideation at 3 weeks, 3 months, and 6 months postpartum (25). Sit et al. examined the associations between suicidal ideation among 628 depressed postpartum women and the following possible risk factors: experience of abuse as a child or adult, sleep disturbance, and anxiety symptoms (12). Sit et al. indicated that suicidal ideation among mothers was related to childhood physical abuse. They also reported that suicidal ideation among mothers with no history of childhood physical abuse was related to sleep disturbance and anxiety symptoms (12). Gelaye et al. also pointed out the urgent need for innovative approaches to improve the screening and detection of antepartum suicidal ideation, given that a substantial proportion of women with suicidal ideation do not meet the clinical thresholds for depression, and that the stress–diathesis model shows susceptibility to suicidal behavior independent of depressive disorders (22). Identifying the factors that cause suicidal ideation independent of depressive disorders is also desirable in Japan.
However, unfortunately, compared with death resulting from physical problems, suicide has not been emphasized as a reason for maternal death in Japan, and findings contributing to suicide prevention have been scarcely reported. Moreover, since suicide is affected by a country's economic status and cultural background, foreign survey results cannot be generalized to Japan.
We have been conducting a prospective cohort study on perinatal depression since 2004; we have found that approximately 32% of all participants show some depressive symptoms, as assessed by the Edinburgh Postnatal Depression Scale (EPDS) at any one of the following four time points: early pregnancy, late pregnancy, 5 days postpartum, and 1 month postpartum (26). Suicide has typically been strongly associated with a history of suicide attempts, and a strong association has been identified between suicide attempts and suicidal ideation (26).
The aim of the present study was to elucidate the foreseeable risk factors for suicidal ideation among perinatal women from the previous report to promote more effective suicide prevention measures.
Method
Design
The data in the present study were extracted from a prospective cohort study conducted in Nagoya, Japan from July 2012 to March 2018.
Participants
Participants were recruited during early pregnancy in a maternity class for psychological education about pregnancy and birth at individual facilities. This maternity class was provided by medical staffs for the prevention and early detection of postpartum depression and other mental disorders. At the end of the program, the study protocol was introduced, and applicants were invited to participate voluntarily in the study.
The following four hospitals participated in this prospective cohort study: one general hospital (Nagoya Teishin Hospital), two obstetrics and gynecology hospitals (Kaseki Hospital and Royal Bell Clinic), and one university hospital (Nagoya University Hospital). In Japan, obstetrics and gynecology hospitals mainly treat uncomplicated pregnant women. Pregnant women with complications are usually introduced into general or university hospitals. Perinatal women with severe complications are followed up at university hospitals, and scheduled hospitalization for birth is often performed. By contrast, general hospitals with a neonatal intensive care unit deal with emergency births.
The eligibility criteria were as follows: 1) pregnant female aged ≥20 years, 2) ability to read and write Japanese, 3) attended a gynecological checkup at one of the four hospitals.
Ethical Considerations
This study was approved by the ethics committees of Nagoya University Hospital. All study procedures were conducted in accordance with the Declaration of Helsinki and other relevant ethical guidelines. Written informed consent for participation was obtained from all participants.
Measurements
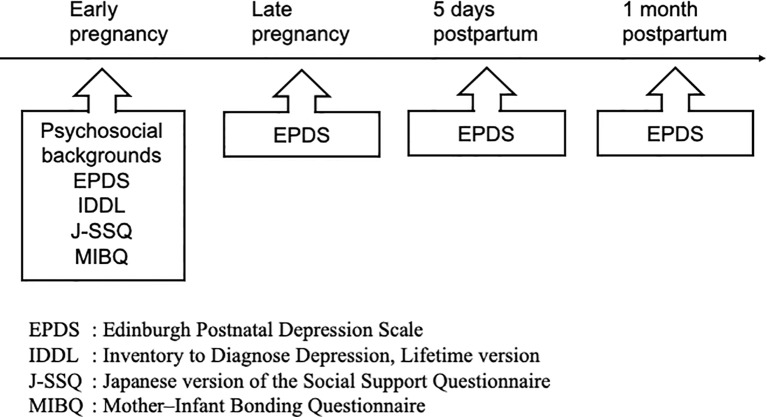
As shown in Figure 1, the participants' psychosocial backgrounds were evaluated at early pregnancy using a self-administered questionnaire with the following items: age, presence of physical and/or mental disease, smoking and drinking habits, years of schooling, number of childbirths, hospital types, bonding as assessed by the Mother–Infant Bonding Questionnaire (MIBQ), quality and amount of social support as assessed by the Japanese version of the Social Support Questionnaire (J-SSQ), and the presence of past depression from the Inventory to Diagnose Depression, Lifetime version (IDDL). In addition, the participants were asked to complete the EPDS at the following four time points: 1) early pregnancy, 2) late pregnancy, 3) 5 days postpartum, and 4) 1 month postpartum.
Figure 1.
Flowchart of the study.
The presence or absence of physical and/or mental disease was obtained from the participants using the questionnaire. When the participants answered “present,” they were asked to provide further details, i.e., what kind of diseases they were suffering from. As for smoking and drinking habits, the participants were asked whether these habits were present or absent. When the participants answered “present,” they were also asked to provide further details, i.e., changes in frequency and volume before and after pregnancy. The hospital types were determined whether the hospital has a Neonatal Intensive Care Unit (NICU).
Edinburgh Postnatal Depression Scale
The EPDS is a self-administered questionnaire designed by Cox et al. in 1987 (27) to screen for postpartum depression. It is composed of 10 items scored on a four-point Likert scale. In our cohort study, we clarified that the Japanese version of the EPDS, which was established by Okano et al. in 1996 (28), had a three-factor structure of depression, anxiety, and anhedonia (29, 30). We adopted the evaluation of suicidal ideation based on previous reports (8, 12, 31). Participants who had a score of ≥2 on the 10th item of the EPDS during at least one of the four periods were classified into the suicidal ideation group; the remaining participants were classified into the healthy group. Howard et al. (8) examined the validity of evaluating suicidal ideation using the 10th item of the EPDS in a study involving 4,150 women at 6 weeks postpartum. In their study, the definition of suicidal ideation for the 10th item of the EPDS (a score of ≥2) was compared with that used in the Clinical Interview Schedule-Revised (CIS-R) (≥2 of five items on the CIS-R suicidal ideation measurement) (32). As a result, 79% of the participants who were classified as having suicidal ideation using the CIS-R were found to have a score of ≥2 on the 10th item of the EPDS, and a moderate kappa statistic value of 0.42 was observed between these two variables. It should be noted that the CIS-R has been validated across cultures and is widely used for the assessment of common mental disorders (33, 34).
Inventory to Diagnose Depression, Lifetime Version
The IDDL is a self-administered questionnaire that assesses the history of MDD in accordance with the Diagnostic and Statistical Manual of Mental Disorders (DSM)-III (35). The IDDL is composed of 22 items scored on a five-point Likert scale. A score of ≥3 indicates having a specific symptom for items 5 and 6, while a score of ≥2 indicates having a specific symptom for the remaining 20 items. All 22 items on the IDDL are classified into two major and seven other symptoms according to the DSM-III criteria for MDD. If one of the items indicating each symptom is over the cutoff score, the symptom is judged to be present. The criteria for having a history of MDD were as follows: 1) having the cutoff score or higher for five or more of the 22 items, and 2) these items contain one or more items of the two major symptoms. The sensitivity and specificity of the IDDL are 74 and 93%, respectively (35). The sensitivity and specificity of the Japanese version of the IDDL used in the present study, which was validated by Uehara et al., are 83 and 97%, respectively (36).
Japanese Version of the Social Support Questionnaire
The 12-item Social Support Questionnaire (SSQ-12) was developed to assess social support using a total of 12 questions for number and satisfaction subscales (37). The SSQ-12 is composed of six items for satisfaction level scored on a six-point Likert scale, and six items for the amount of social support. The SSQ-12 is a revised and shortened version of the original SSQ (38), which was composed of 27 items. The Japanese version of the SSQ-12 used in the present study was validated by Furukawa et al. (39).
Mother–Infant Bonding Questionnaire
Maternal positive feeling to their infant was called bonding. The MIBQ was developed to assess maternal bonding. It is composed of nine items rated on a four-point Likert scale (40). Higher scores mean a stronger negative feeling toward a child. We validated the Japanese version of the MIBQ in a previous cohort study (41). Prepartum negative feeling to the fetus as called bonding failure have been reported to predict postpartum negative feeling to the infant (42). Further, mothers with high suicidality have been reported to be less sensitive and responsive to their infants' cues (43). Therefore, bonding during pregnancy was evaluated.
Statistical Analyses
With the presence or absence of suicidal ideation as an objective variable, this study was carried out using a logistic regression model with a forward selection procedure. The explanatory variables were: age, presence or absence of physical and/or mental disease, smoking and drinking habits, family income, years of schooling, EPDS total score in early pregnancy, bonding as assessed by the MIBQ, quality and amount of social support as assessed by the J-SSQ, and the presence of past depression as assessed by the IDDL. Listwise deletion methods were performed for missing values. The variance inflation factor (VIF) was calculated to evaluate multicollinearity. These explanatory variables were compared between groups based on the presence or absence of suicidal ideation. All statistical analyses were performed using IBM SPSS version 26.0 (IBM Japan, Tokyo, Japan.).
Results
Of 457 participants enrolled at early pregnancy [mean (M): 5.3 months, SD: 1.6 months] in the present study, 430 perinatal women were finally included in the analysis. The mean age of the participants was 33.0 years [standard deviation (SD): 4.7 years]. The mean years of schooling was 15.0 (SD: 2.0). The rates of nulliparous, primiparous, and those who had given birth two or three times were 81.8, 15.8, 2.0, and 0.5%, respectively. The current drinking and smoking rates were 9.8 and 2.8%, respectively. The prevalences of mental and physical disorders were 16.2 and 38.9%, respectively. The rate of participants who were suspected of having suicidal ideation at any of four time points was 13.0% (5.5, 5.8, 2.3, and 4.4% at early pregnancy, late pregnancy, 5 days postpartum, and 1 month postpartum, respectively). The mean EPDS total scores at early pregnancy, late pregnancy, 5 days postpartum, and 1 month postpartum were 5.3 (SD: 5.0; range: 0–29), 4.9 (SD: 4.8; range: 0–30), 5.5 (SD: 4.9; range: 0–26), and 5.8 (SD: 5.2; range: 0–25), respectively. The mean IDDL total score was 30.4 (SD: 16.8; range: 0–81). The ratio of participants who were suspected of having a history of MDD based on the IDDL was 29.5% (n=127). The mean MIBQ total score was 3.5 (SD: 3.5; range: 0–17). The mean amount and quality of social support according to the J-SSQ were 3.8 (SD: 2.1; range: 0–16) and 4.8 (SD: 1.4; range: 0–6), respectively. A comparison between the two groups divided by the presence or absence of suicidal ideation is shown in Table 1.
Table 1.
Comparison between groups (n=430) by presence or absence of suicidal ideation.
| Group 1 (n=379) | Group 2 (n=51) | p value | |
|---|---|---|---|
| Age (y) | 33.3 ± 4.6 | 31.6 ± 4.7 | .013 |
| Years of schooling | 15.0 ± 1.9 | 15.3 ± 2.10 | .250 |
| Nulliparous Primiparous Given birth twice Given birth three times |
82.3% 15.3% 1.8% 0.6% |
78.4% 17.6% 4.0% 0% |
.705 |
| Drinking rate | 9.0% | 17.6% | .053 |
| Smoking rate | 1.3% | 11.8% | <0.000 |
| Prevalence of mental disorders | 13.1% | 44.9% | <0.000 |
| Prevalence of physical disorders | 39.0% | 45.0% | .486 |
| EPDS at early pregnancy | 4.39 ± 3.95 | 11.55 ± 6.66 | <0.000 |
| EPDS at late pregnancy | 4.11 ± 4.03 | 10.27 ± 6.64 | <0.000 |
| EPDS at 5 days postpartum | 4.84 ± 4.32 | 9.73 ± 6.30 | <0.000 |
| EPDS at 1 month postpartum | 5.15 ± 4.52 | 10.53 ± 7.13 | <0.000 |
| History of MDD | 24.2% | 54.9% | <0.000 |
| IDDL | 28.39 ± 15.65 | 45.20 ± 17.35 | <0.000 |
| MIBQ | 3.19 ± 2.96 | 4.90 ± 5.37 | .084 |
| J-SSQ (support number) | 3.95 ± 2.16 | 3.20 ± 1.73 | .016 |
| J-SSQ (satisfaction level) | 4.90 ± 1.36 | 4.22 ± 1.35 | .001 |
EPDS, Edinburgh Postnatal Depression Scale; MDD, major depressive disorder; IDDL, Inventory to Diagnose Depression, Lifetime version; MIBQ, Mother–Infant Bonding Questionnaire; J-SSQ, Japanese version of the Social Support Questionnaire
Data are presented as the mean ± standard deviation (SD).
A t-test was used to compare age, years of schooling, and J-SSQ scores.
The chi-squared test was used to compare the number of children, drinking, and smoking rates, prevalence of mental and physical disorders, and rate of having a history of MDD.
The Mann–Whitney U test was used to compare EPDS, IDDL, and MIBQ scores.
No explanatory variable was excluded because the VIF was <5. As shown in Table 2, education level (OR: 1.19; 95% CI: 1.00–1.41; p=0.047), EPDS total points in the pregnancy period (OR: 1.25; 95% CI: 1.16–1.34; p < 0.000), a history of MDD (OR: 2.16; 95% CI: 1.00–4.79; p=0.049), and presence of mental disease (OR: 2.39; 95% CI: 1.00–5.70; p=0.049) were found to be risk factors for suicidal ideation. Age [odds ratio (OR): 0.88; 95% confidence interval (CI): 0.80–0.95; p=.002] and quality of social support (OR: 0.77; 95% CI: 0.60–0.99; p=.041) were found to be protective factors.
Table 2.
Forward stepwise logistic regression models.
| Covariates | Model 1: full model | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8: final model | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | OR | 95% CI | p Value | |
| Age | 0.89 | 0.81–0.97 | 0.008 | 0.89 | 0.81–0.97 | 0.008 | 0.89 | 0.81–0.97 | 0.008 | 0.89 | 0.81–0.97 | 0.008 | 0.89 | 0.81–0.97 | 0.006 | 0.89 | 0.81–0.97 | 0.006 | 0.88 | 0.81–0.96 | 0.005 | 0.88 | 0.80–0.95 | 0.002 |
| Years of schooling | 1.20 | 1.02–1.43 | 0.033 | 1.21 | 1.02–1.43 | 0.032 | 1.20 | 1.02–1.43 | 0.032 | 1.20 | 1.02–1.43 | 0.032 | 1.19 | 1.01–1.41 | 0.038 | 1.20 | 1.01–1.41 | 0.036 | 1.19 | 1.01–1.40 | 0.041 | 1.19 | 1.00–1.41 | 0.047 |
| The presence or absence of mental disease | 2.19 | 0.90–5.30 | 0.083 | 2.19 | 0.90–5.30 | 0.083 | 2.18 | 0.90–5.28 | 0.083 | 2.19 | 0.91–5.29 | 0.082 | 2.27 | 0.95–5.43 | 0.065 | 2.36 | 0.99–5.61 | 0.053 | 2.44 | 1.03–5.79 | 0.043 | 2.39 | 1.00–5.70 | 0.049 |
| A history of MDD | 2.26 | 1.01–5.08 | 0.048 | 2.25 | 1.01–5.04 | 0.048 | 2.26 | 1.01–5.05 | 0.046 | 2.26 | 1.01–5.05 | < 0.001 | 2.24 | 1.01–4.98 | 0.048 | 2.22 | 1.00–4.93 | 0.049 | 2.22 | 1.00–4.92 | 0.049 | 2.16 | 1.00–4.79 | 0.049 |
| Quality of social support | 0.75 | 0.58–0.99 | 0.041 | 0.75 | 0.58–0.99 | 0.040 | 0.75 | 0.58–0.98 | 0.037 | 0.75 | 0.57–0.97 | 0.028 | 0.75 | 0.57–0.97 | 0.028 | 0.75 | 0.58–0.97 | 0.028 | 0.74 | 0.57–0.96 | 0.025 | 0.77 | 0.60–0.99 | 0.041 |
| EPDS total point in the pregnancy period | 1.25 | 1.15–1.35 | < 0.00 | 1.25 | 1.15–1.35 | < 0.000 | 1.25 | 1.15–1.35 | < 0.000 | 1.25 | 1.16–1.35 | < 0.000 | 1.26 | 1.17–1.36 | < 0.000 | 1.26 | 1.17–1.36 | < 0.000 | 1.26 | 1.17–1.36 | < 0.000 | 1.25 | 1.16–1.34 | < 0.000 |
| Number of childbirths | 0.57 | 0.23–1.39 | 0.216 | 0.58 | 0.24–1.38 | 0.216 | 0.58 | 0.24–1.39 | 0.219 | 0.58 | 0.24–1.39 | 0.221 | 0.55 | 0.23–1.30 | 0.172 | 0.55 | 0.23–1.30 | 0.173 | 0.55 | 0.23–1.31 | 0.178 | |||
| Drinking habits | 1.65 | 0.49–5.58 | 0.420 | 1.63 | 0.49–5.38 | 0.425 | 1.63 | 0.49–5.40 | 0.421 | 1.66 | 0.51–5.47 | 0.403 | 1.90 | 0.63–5.78 | 0.257 | 1.93 | 0.63–5.87 | 0.247 | ||||||
| Hospital types | 1.19 | 0.74–1.93 | 0.479 | 1.19 | 0.74–1.91 | 0.485 | 1.19 | 0.74–1.91 | 0.471 | 1.20 | 0.74–1.91 | 0.462 | 1.20 | 0.75–1.93 | 0.445 | |||||||||
| Smoking habits | 1.77 | 0.37–8.55 | 0.475 | 1.80 | 0.38–8.51 | 0.458 | 1.78 | 0.38–8.34 | 0.464 | 1.74 | 0.37–8.19 | 0.481 | ||||||||||||
| Amount of social support | 0.97 | 0.79–1.20 | 0.781 | 0.97 | 0.79–1.20 | 0.768 | 0.97 | 0.79–1.20 | 0.767 | |||||||||||||||
| MIBQ total points in the pregnancy period | 1.01 | 0.92–1.11 | 0.863 | 1.01 | 0.91–1.11 | 0.866 | ||||||||||||||||||
| The presence or absence of physical disease | 0.95 | 0.44–2.01 | 0.904 | |||||||||||||||||||||
EPDS, Edinburgh Postnatal Depression Scale; MDD, major depressive disorder.
Discussion
The present study investigated the risk factors for suicidal ideation among perinatal women in Japan. The results indicated that higher education, more severe depressive symptoms in early pregnancy, a history of MDD, and presence of mental disease were significant risk factors, and that age and social support were significant protective factors.
Since the rate of suicidal ideation in early and late pregnancy was high, early intervention from the prenatal period is important. In the present study, the most important risk factors for suicidal ideation in the perinatal period in Japan were current and previous depressive symptoms.
In previous studies, age (8, 44) and social support (45) were reported to be protective factors that reduce suicidal ideation in pregnant women. However, since other confounding factors, such as economic status and unwanted pregnancies, may exist in the background, future research is needed to identify the exact role of these factors.
Meanwhile, in contrast to the present results, an association has been reported between fewer years of education and a higher rate of maternal suicide (46). In Japan, highly educated women are often forced to leave their jobs after childbirth because they cannot receive sufficient support to balance work and childbearing. The present results may reflect this situation.
This study had several limitations. First, it could have involved a selection bias because individuals who did not have any interest in mental health or a history of depressive illness may not have responded to the questionnaire, and therefore, would have been excluded from the analysis. In fact, the rate of participants who had a history of MDD as measured by the IDDL was quite high compared with previous reports (35, 36). Second, information regarding the presence or absence of mental illness was obtained from the questionnaire responses. Third, the definition of suicidal ideation in this study was based on that used in previous reports, as opposed to clinical diagnostic interviews by psychiatrists; such interviews should be conducted in future research.
In the present study, the rate of perinatal suicidal ideation was 13.0%. To our knowledge, this is the first study to investigate the rate of perinatal suicidal ideation in Japan. In previous reports from overseas, the rate of suicidal ideation during pregnancy has ranged from 2.6 to 22.8% (47–49), and that during the postpartum period from 6.16 to 14% (19, 49). The present result regarding the rate of perinatal suicidal ideation of 11.6% is within the range of these previous reports. This rate can vary greatly depending on the country, cultural differences, and evaluation methods. Since pregnancy and childbirth are not protective factors for suicidal ideation, further research is needed to help prevent suicide in perinatal women.
Based on the results of this study, effective preventive interventions, such as increasing the quality of social support and confirming the history of depression, should be carried out in pregnant depressive women at the early stage of the perinatal period.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethics committees of Nagoya University Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
SM, SG, AK, and NO conceived and designed the experiments. CK, YN, AY, TS, MM, MO, MS, and TO performed the experiments. CK, MA, and NO conducted the statistical analysis. CK, TI, BA, and NO wrote the paper. All authors contributed to and have approved the final manuscript.
Funding
Funding for this study was provided by research grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan; the Ministry of Health, Labour and Welfare of Japan; The Academic Frontier Project for Private Universities, Comparative Cognitive Science Institutes, Meijo University; the Core Research for Evolutional Science and Technology; Intramural Research Grant (21B‐2) for Neurological and Psychiatric Disorders from the National Center of Neurology and Psychiatry; the Specific Research Fund 2012 for East Japan Great Earthquake Revival by The New Technology Development Foundation, and the Japan Agency for Medical Research and Development; the Research and Development Grants for Comprehensive Research for Persons with Disabilities from Japan Agency for Medical Research and development, AMED (No. JP18dk0307077).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to express our gratitude to the staff members at Nagoya Teishin Hospital, Kaseki Hospital, Royal Bell Clinic and Nagoya University Hospital.
References
- 1. Takeda S, Takeda J, Murakami K, Kubo T, Hamada H, Murakami M, et al. Annual Report of the Perinatology Committee, Japan Society of Obstetrics and Gynecology, 2015: Proposal of urgent measures to reduce maternal deaths. J Obstetr Gynaecol Res (2017) 43:5–7. 10.1111/jog.13184 [DOI] [PubMed] [Google Scholar]
- 2. Palladino CL, Singh V, Campbell J, Flynn H, Gold KJ. Homicide and suicide during the perinatal period: findings from the National Violent Death Reporting System. Obstetr Gynecol (2011) 118:1056–63. 10.1097/AOG.0b013e31823294da [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Donati S, Senatore S, Ronconi A. Maternal mortality in Italy: a record-linkage study. BJOG: Int J Obstetr Gynaecol (2011) 118:872–9. 10.1111/j.1471-0528.2011.02916.x [DOI] [PubMed] [Google Scholar]
- 4. Esscher A, Essen B, Innala E, Papadopoulos FC, Skalkidou A, Sundstrom-Poromaa I, et al. Suicides during pregnancy and 1 year postpartum in Sweden, 1980-2007. Br J Psychiatry : J Ment Sci (2016) 208:462–9. 10.1192/bjp.bp.114.161711 [DOI] [PubMed] [Google Scholar]
- 5. Gissler M, Hemminki E, Lönnqvist J. Suicides after pregnancy in Finland, 1987-94: register linkage study. BMJ: Br Med J (1996) 313:1431–4. 10.1136/bmj.313.7070.1431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Grigoriadis S, Wilton AS, Kurdyak PA, Rhodes AE, VonderPorten EH, Levitt A, et al. Perinatal suicide in Ontario, Canada: a 15-year population-based study. Can Med Assoc J J Assoc Med Can (2017) 189:E1085–e1092. 10.1503/cmaj.170088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Khalifeh H, Hunt IM, Appleby L, Howard LM. Suicide in perinatal and non-perinatal women in contact with psychiatric services: 15 year findings from a UK national inquiry. Lancet Psychiatry (2016) 3:233–42. 10.1016/S2215-0366(16)00003-1 [DOI] [PubMed] [Google Scholar]
- 8. Howard LM, Flach C, Mehay A, Sharp D, Tylee A. The prevalence of suicidal ideation identified by the Edinburgh Postnatal Depression Scale in postpartum women in primary care: findings from the RESPOND trial. BMC Pregnancy Childbirth (2011) 11:57. 10.1186/1471-2393-11-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kim JJ, La Porte LM, Saleh MP, Allweiss S, Adams MG, Zhou Y, et al. Suicide risk among perinatal women who report thoughts of self-harm on depression screens. Obstetr Gynecol (2015) 125:885–93. 10.1097/AOG.0000000000000718 [DOI] [PubMed] [Google Scholar]
- 10. Huang H, Faisal-Cury A, Chan YF, Tabb K, Katon W, Menezes PR. Suicidal ideation during pregnancy: prevalence and associated factors among low-income women in Sao Paulo, Brazil. Arch Women's Ment Health (2012) 15:135–8. 10.1007/s00737-012-0263-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alhusen JL, Frohman N, Purcell G. Intimate partner violence and suicidal ideation in pregnant women. Arch Women's Ment Health (2015) 18:573–8. 10.1007/s00737-015-0515-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Sit D, Luther J, Buysse D, Dills JL, Eng H, Okun M, et al. Suicidal ideation in depressed postpartum women: Associations with childhood trauma, sleep disturbance and anxiety. J Psychiatr Res (2015) 66–67 95–104. 10.1016/j.jpsychires.2015.04.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gavin AR, Tabb KM, Melville JL, Guo Y, Katon W. Prevalence and correlates of suicidal ideation during pregnancy. Arch Women's Ment Health (2011) 14:239–46. 10.1007/s00737-011-0207-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Farias DR, Pinto Tde J, Teofilo MM, Vilela AA, Vaz Jdos S, Nardi AE, et al. Prevalence of psychiatric disorders in the first trimester of pregnancy and factors associated with current suicide risk. Psychiatry Res (2013) 210:962–8. 10.1016/j.psychres.2013.08.053 [DOI] [PubMed] [Google Scholar]
- 15. Newport DJ, Levey LC, Pennell PB, Ragan K, Stowe ZN. Suicidal ideation in pregnancy: assessment and clinical implications. Arch Women's Ment Health (2007) 10:181–7. 10.1007/s00737-007-0192-x [DOI] [PubMed] [Google Scholar]
- 16. Schiff MA, Grossman DC. Adverse Perinatal Outcomes and Risk for Postpartum Suicide Attempt in Washington State, 1987–2001. Pediatrics (2006) 118:e669–75. 10.1542/peds.2006-0116 [DOI] [PubMed] [Google Scholar]
- 17. Comtois KA, Schiff MA, Grossman DC. Psychiatric risk factors associated with postpartum suicide attempt in Washington State, 1992-2001. Am J Obstetr Gynecol (2008) 199:120.e1–5. [DOI] [PubMed] [Google Scholar]
- 18. Castro e Couto T, Brancaglion MY, Cardoso MN, Faria GC, Garcia FD, Nicolato R, et al. Suicidality among pregnant women in Brazil: prevalence and risk factors. Arch Women's Ment Health (2016) 19:343–8. 10.1007/s00737-015-0552-x [DOI] [PubMed] [Google Scholar]
- 19. Pope CJ, Xie B, Sharma V, Campbell MK. A prospective study of thoughts of self-harm and suicidal ideation during the postpartum period in women with mood disorders. Arch Women's Ment Health (2013) 16:483–8. 10.1007/s00737-013-0370-y [DOI] [PubMed] [Google Scholar]
- 20. Nippon Foundation : https://www.nippon-foundation.or.jp/en
- 21. Ministry of Health , Labor and Welfare of Japan: https://www.mhlw.go.jp/stf/seisakunitsuite/bunya/hukushi_kaigo/seikatsuhogo/jisatsu/ishikichousa.html
- 22. Gelaye B, Kajeepeta S, Williams MA. Suicidal ideation in pregnancy: an epidemiologic review. Arch Women's Ment Health (2016) 19:741–51. 10.1007/s00737-016-0646-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. O'Connor A, Geraghty S, Doleman DG, De Leo A. Suicidal ideation in the perinatal period: A systematic review. Ment Health Prev (2018) 12:67–75. 10.1016/j.mhp.2018.10.002 [DOI] [Google Scholar]
- 24. Ishida K, Stupp P, Serbanescu F, Tullo E. Perinatal risk for common mental disorders and suicidal ideation among women in Paraguay. Int J Gynaecol Obstetr (2010) 110:235–40. 10.1016/j.ijgo.2010.03.027 [DOI] [PubMed] [Google Scholar]
- 25. Bodnar-Deren S, Klipstein K, Fersh M, Shemesh E, Howell EA. Suicidal Ideation During the Postpartum Period. J Womens Health (Larchmt) (2016) 25:1219–24. 10.1089/jwh.2015.5346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Gunnell DJ, Peters TJ, Kammerling RM, Brooks J. Relation between parasuicide, suicide, psychiatric admissions, and socioeconomic deprivation. BMJ (1995) 311:226. 10.1136/bmj.311.6999.226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry: J Ment Sci (1987) 150:782–6. 10.1192/bjp.150.6.782 [DOI] [PubMed] [Google Scholar]
- 28. Okano S, Murata M, Masuji S, Tamaki R, Nomura J, Miyaoka H, et al. Reliability and validity of the Edinburgh postpartum depression scale (EPDS) in Japan. Arch Psychiatr Diagnost Clin Eval (1996) 7:525–33. [Google Scholar]
- 29. Kubota C, Inada T, Nakamura Y, Shiino T, Ando M, Aleksic B, et al. Factor structure of the Edinburgh Postnatal Depression Scale during the whole peripartum period: Results from a Japanese prospective cohort study. Sci Rep (2018) 8:17659. 10.1038/s41598-018-36101-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kubota C, Okada T, Aleksic B, Nakamura Y, Kunimoto S, Morikawa M, et al. Factor structure of the Japanese version of the Edinburgh Postnatal Depression Scale in the postpartum period. PloS One (2014) 9:e103941. 10.1371/journal.pone.0103941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Supraja TA, Thennarasu K, Satyanarayana VA, Seena TK, Desai G, Jangam KV, et al. Suicidality in early pregnancy among antepartum mothers in urban India. Arch Women's Ment Health (2016) 19:1101–8. 10.1007/s00737-016-0660-2 [DOI] [PubMed] [Google Scholar]
- 32. Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. psychol Med (1992) 22:465–86. 10.1017/S0033291700030415 [DOI] [PubMed] [Google Scholar]
- 33. Brugha TS, Bebbington PE, Jenkins R, Meltzer H, Taub NA, Janas M, et al. Cross validation of a general population survey diagnostic interview: a comparison of CIS-R with SCAN ICD-10 diagnostic categories. psychol Med (1999) 29:1029–42. 10.1017/S0033291799008892 [DOI] [PubMed] [Google Scholar]
- 34. Jordanova V, Wickramesinghe C, Gerada C, Prince M. Validation of two survey diagnostic interviews among primary care attendees: a comparison of CIS-R and CIDI with SCAN ICD-10 diagnostic categories. psychol Med (2004) 34:1013–24. 10.1017/S0033291703001727 [DOI] [PubMed] [Google Scholar]
- 35. Zimmerman M, Coryell W. The inventory to diagnose depression, lifetime version. Acta Psychiatr Scand (1987) 75:495–9. 10.1111/j.1600-0447.1987.tb02824.x [DOI] [PubMed] [Google Scholar]
- 36. Uehara T, Sakado K, Sato T, Sato S. The reliability and validity of the Japanese version of the inventory to diagnose depression lifetime version. Japanese J Psychiatr Treat (1995) 10:181–8. [Google Scholar]
- 37. Sarason IG, Sarason BR, Shearin EN, Pierce GR. A Brief Measure of Social Support: Practical and Theoretical Implications. J Soc Pers Relat (1987) 4:497–510. 10.1177/0265407587044007 [DOI] [Google Scholar]
- 38. Sarason IG, Levine HM, Basham RB, Sarason BR. Assessing social support: The Social Support Questionnaire. J Pers Soc Psychol (1983) 44:127–39. 10.1037/0022-3514.44.1.127 [DOI] [Google Scholar]
- 39. Furukawa TA, Harai H, Hirai T, Kitamura T, Takahashi K. Social Support Questionnaire among psychiatric patients with various diagnoses and normal controls. Soc Psychiatry Psychiatr Epidemiol (1999) 34:216–22. 10.1007/s001270050136 [DOI] [PubMed] [Google Scholar]
- 40. Robson KM, Kumar R. Delayed onset of maternal affection after childbirth. Br J Psychiatry : J Ment Sci (1980) 136:347–53. 10.1192/bjp.136.4.347 [DOI] [PubMed] [Google Scholar]
- 41. Ohara M, Okada T, Kubota C, Nakamura Y, Shiino T, Aleksic B, et al. Validation and factor analysis of mother-infant bonding questionnaire in pregnant and postpartum women in Japan. BMC Psychiatry (2016) 16:212. 10.1186/s12888-016-0933-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Rossen L, Hutchinson D, Wilson J, Burns L, O. C A, Allsop S, et al. Predictors of postnatal mother-infant bonding: the role of antenatal bonding, maternal substance use and mental health. Arch Women's Ment Health (2016) 19:609–22. 10.1007/s00737-016-0602-z [DOI] [PubMed] [Google Scholar]
- 43. Paris R, Bolton RE, Weinberg MK, depression P. suicidality, and mother-infant interactions. Arch Women's Ment Health (2009) 12:309–21. 10.1007/s00737-009-0105-2 [DOI] [PubMed] [Google Scholar]
- 44. Chen YY, Gunnell D, Lu CL, Chang SS, Lu TH, Li CY. Perinatal risk factors for suicide in young adults in Taiwan. Int J Epidemiol (2013) 42:1381–9. 10.1093/ije/dyt129 [DOI] [PubMed] [Google Scholar]
- 45. Wu CY, Stewart R, Huang HC, Prince M, Liu SI. The impact of quality and quantity of social support on help-seeking behavior prior to deliberate self-harm. Gen Hosp Psychiatry (2011) 33:37–44. 10.1016/j.genhosppsych.2010.10.006 [DOI] [PubMed] [Google Scholar]
- 46. Lysell H, Dahlin M, Viktorin A, Ljungberg E, D'Onofrio BM, Dickman P, et al. Maternal suicide – Register based study of all suicides occurring after delivery in Sweden 1974–2009. PloS One (2018) 13:e0190133. 10.1371/journal.pone.0190133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ. Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstetr Gynecol (2010) 116:1064–70. 10.1097/AOG.0b013e3181f60b0a [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Alhusen JL, Ray E, Sharps P, Bullock L. Intimate partner violence during pregnancy: maternal and neonatal outcomes. J Womens Health (Larchmt) (2015) 24:100–6. 10.1089/jwh.2014.4872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Lindahl V, Pearson JL, Colpe L. Prevalence of suicidality during pregnancy and the postpartum. Arch Women's Ment Health (2005) 8:77–87. 10.1007/s00737-005-0080-1 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.