Introduction
The coronavirus disease 2019 (COVID-19) pandemic has significantly financially impacted health care systems due to suspension of elective imaging and procedures. Washington state had passed its peak of hospital resource utilization in early April 2020, and the University of Washington Medicine is resuming elective imaging and procedures as stay-at-home orders are loosened. There are many factors to consider for the return of elective imaging. Many patients, especially elderly patients, may remain hesitant to return to imaging or hospital centers. There is a need to maintain or amplify safety measures to limit potential exposures. This article shares plans developed at the University of Washington Radiology to ensure patient and health care worker safety in the post-COVID environment.
Resumption of Elective Imaging and Procedures
As many communities and health care systems overcome the COVID-19 surge and resume routine elective imaging, it is important to maintain the precautions that reduced disease dissemination. In addition, many patients who may have actively chosen to delay their imaging may be hesitant to return to health care institutions, especially if they arrive to crowded waiting rooms. Despite large backlogs of postponed procedures and imaging, it is prudent to approach imaging with a slow ramp-up to keep safety measures in place that will protect patients and health care workers while also restoring patient confidence in their safety in the health care institutions. After resumption of elective imaging, reassessments every 2 weeks of hospital-related exposures can be considered, as well as assessment of infection rates throughout the community to assess whether elective outpatient imaging can continue.
Continuation of Safety Precautions
Exposure precautions for patients and health care workers should be maintained. This includes appropriate use of personal protective equipment, appropriate testing, and maintenance of social distancing practices [1].
Radiology health care worker protection policies should also be maintained. Maximizing distancing between workstations in the reading rooms, home interpretation, making available single workstation reading rooms, and daily health self-attestations should be considerations when possible [1,2].
Implementation of New Safety Protections
Implementation of novel approaches for limiting potential hospital exposures is needed. We are establishing online patient registration for imaging appointments at our outpatient imaging centers through our automated text messaging system to reduce the amount of time patients spend in waiting rooms to limit potential exposures. Patients will receive a text message 2 days before their examination with a link to an online registration form to be filled out that will include patient history sections, with links to screening forms and safety questionnaires that can be filled out online before they arrive, and directly uploaded to the technologists, instead of having to fill these forms out after arriving at the radiology front desk. Implementation of this sort of system would be beneficial outside of reducing patient exposures to COVID-19 as well to identify patients with contraindications to MRI or contrast beforehand and to be able to plan or redirect accordingly. When the patient arrives, there is a link in the text that, when clicked on, alerts the front desk staff of the patient’s arrival. Five to ten minutes before it is time for the patient to get prepared for his or her examination, a text alert is sent to the patient, and the patient comes to the imaging modality directly, bypassing the waiting room and front desk.
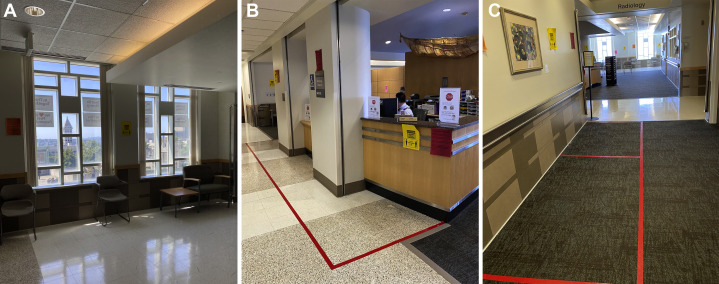
Reorganization of waiting rooms and patient flow should be considered for better observance of social distancing and reduced potential exposures. Removal of chairs to allow for at least 6-foot distances between seats is necessary (Fig. 1 a). Putting tape on the floor to demarcate appropriate distances from seating or staff desks can also be performed (Fig. 1b and 1c). Staggering appointments between imaging units of the same modality, or at outpatient imaging centers between modalities, to decompress waiting rooms and traffic in radiology should also be a consideration. In addition, one-way hallways throughout the radiology department, if possible, especially in high-traffic regions, can reduce potential exposures.
Fig 1.
Rearrangement of seating in the waiting room area is demonstrated, with 6-foot distance between chairs (a). Tape markings on the floor to indicate safe standing distance from the radiology front desk (b) and appropriate spacing between individuals waiting in line (c).
Elective procedures have been postponed in Washington state through May 18, 2020; however, some procedures, such as cancer therapeutic and diagnostic procedures, that could be delayed in mid-March have now become time-sensitive and must be scheduled. As we schedule these procedures, all patients that are undergoing aerosol-generating procedures [3] or will have moderate sedation, potential intubation, or open suction or are symptomatic are required to have severe acute respiratory syndrome coronavirus 2 reverse transcriptase polymerase chain reaction testing before the scheduled procedure. Patients undergoing aerosolizing procedures that incidentally test positive have their procedures performed under airborne or contact precaution if the procedure is deemed sufficiently urgent. For emergent procedures, a 2-hour rapid polymerase chain reaction test is employed. For those procedures that cannot be delayed 2 hours for the rapid polymerase chain reaction test, the procedure will be performed immediately under standard airborne or contact precaution.
Increased Imaging Access
Increasing imaging access is a goal of all radiology departments; however, in the post-COVID environment, the goal is not necessarily to increase imaging throughput but rather to increase gaps between studies to provide 10 to 15 min for appropriate equipment cleaning, to decompress waiting areas and hallways, and to increase patient confidence in the protection measures taken.
Increased access can be accomplished by extending imaging operation times into the evenings and weekends. In addition, shortening scanning block times, especially on MRI and CT, can help create gaps between studies for equipment cleaning time. We have shortened CT block times to 15 min through streamlined, efficient workflows. We have also shortened MRI to 15-min blocks for the most common MRI examinations performed, specifically most brain and spine MRI protocols, with other MRI scans fitting into 30-min scan times. This was accomplished through optimized workflows in addition to optimized protocols, using compressed sensing-sensitivity encoding [4] and 32-channel head coils to shorten brain MRI scan time without appreciable image quality loss. This process was started prior to the COVID-19 pandemic but was accelerated during the outbreak because of the anticipated need for increased efficiency. MRI brain tumor protocols were consolidated from five separate protocols into a single protocol. The earlier protocols ranged in scan time from 20 to 30 min, and the final single protocol scan time was reduced to 8.5 min of table time. In addition to the above acceleration approaches, we increasingly relied on isotropic 3-D sequences with multiplanar reconstructions in place of three-plane sequence acquisitions. Our ordering clinician partners and radiologists alike have expressed increased satisfaction with the new protocols compared with the old protocols.
Patient Communication
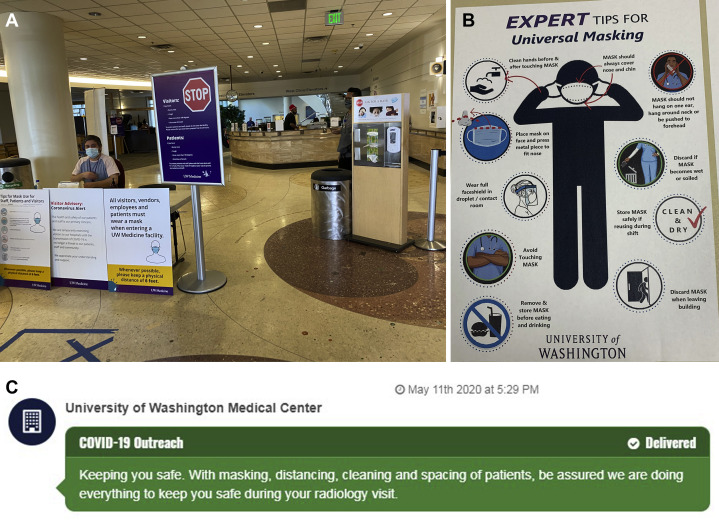
Patient anxiety and concern relating to COVID-19 may remain high, even after stay-at-home orders are lifted and elective imaging resumes. A survey of 700 individuals greater than 25 years of age from across the nation conducted by Revive Health on April 14, 2020 [5], determined that only 15% of patients would feel comfortable returning immediately to their hospitals for health care once stay-at-home orders were lifted; 36% only felt comfortable returning to hospitals after at least 3 months had passed after lifting of stay-at-home orders; 62% would only seek health care if faced with a very serious health condition. In addition, 56% expressed “a lot of concern” about getting sick from other patients. Hospitals and physicians are positioned to restore patient confidence regarding our health care systems and their ability to appropriately care for them. A second survey developed on March 30, 2020, polling likely the same cohort, found patient trust with local health experts (hospitals and physicians) at 81%, higher than national health experts, media, government officials, or employers. Only 30% were “very happy” with the communication they receive from their health care systems [6]. Considering this information, the University of Washington has adopted our patient texting system to communicate to patients the precautions we are taking in radiology to protect them from exposures. This includes the measures described previously relating to universal masking, hand hygiene, and focus on social distancing at all times in the hospital. We are also communicating these precautions with patients via e-mail and standard mail. We have posted signage throughout the radiology department as well as at the hospital entrances emphasizing the precautions to prevent exposures (Fig. 2 ).
Fig 2.
Hospital entrance checkpoint, with mask distribution, hand sanitizing station, and extensive signage communicating person protective measures (a). Example of one of the signs distributed throughout the radiology department communicating appropriate masking guidelines (b). Text message sent to patients assuring them that the health system is taking necessary precautions to protect patients (c).
Summary
In the post-COVID environment, patient and health care employee protections from potential exposures should be maintained to uphold the progress that has been made. In addition, patient anxieties persist regarding potential exposures within health care institutions. Considering these issues, it is important for radiology departments to maintain and improve upon the precautions and workflows that have been implemented. A slow ramp-up of outpatient imaging would better ensure these protections, as would innovative approaches to reduce potential exposures, and improved patient communication about precautions that are being taken in order to restore patient confidence.
Footnotes
Dr Linnau reports a grant from Healthineers and personal fees from Siemens Healthineers, outside the submitted work. The other authors state that they have no conflict of interest related to the material discussed in this article. All authors are employees of an academic institution. Dr Mossa-Basha, Vice Chair of Clinical Operations, Radiology Chief of Service, University of Washington and NWH Medical Centers, Medical Director of MRI, University of Washington School of Medicine, Seattle, Washington. Dr Linnau, Associate Radiology Chief of Service, Harborview Medical Center, University of Washington School of Medicine, Seattle, Washington. Dr Dushyant V. Sahani, Chair of Radiology, University of Washington School of Medicine, Seattle, Washington.
References
- 1.Mossa-Basha M., Medverd J., Linnau K. Policies and guidelines for COVID-19 preparedness: experiences from the University of Washington [E-pub ahead of print] Radiology. 2020 Apr 8:201326. doi: 10.1148/radiol.2020201326. [DOI] [PubMed] [Google Scholar]
- 2.Davenport M.S., Bruno M.A., Iyer R.S., Johnson A.M. ACR statement on safe resumption of routine radiology care during the Coronavirus Disease 2019 (COVID-19) pandemic. J Am Coll Radiol. 2020;17:839–843. doi: 10.1016/j.jacr.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Society of Interventional Radiology Aerosol generating procedures performed by interventional radiology clinical notification from the society of interventional radiology. https://www.sirweb.org/practice-resources/covid-19-resources/covid-19-clinical-notification-3-26-20/ Available at: Updated April 17 2020. Accessed May 5, 2020.
- 4.Vranic J.E., Cross N.M., Wang Y., Hippe D.S., de Weerdt E., Mossa-Basha M. Compressed sensing-sensitivity encoding (CS-SENSE) accelerated brain imaging: reduced scan time without reduced image quality. AJNR Am J Neuroradiol. 2019;40:92–98. doi: 10.3174/ajnr.A5905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Revive Health COVID-19 consumer survey findings report - part 3. https://www.thinkrevivehealth.com/covid-19/covid-19-consumer-survey-findings-report-part-3 Available at: Accessed May 5, 2020.
- 6.Revive Health COVID-19 consumer survey findings report - part 2. https://www.thinkrevivehealth.com/covid-19/covid-19-consumer-survey-findings-report-part-2 Available at: Accessed May 5, 2020.