Abstract
Introduction
Perceptions of health risks inform decisions about protective behaviors, but COVID-19 was an unfamiliar risk as it began to spread across the U.S. In the initial stage of the epidemic, authors examined perceived risks for COVID-19 infection and infection fatality and whether these risk perceptions were associated with protective behaviors. They also examined whether findings differed between later versus earlier responders.
Methods
Between March 10 and March 31, 2020, a cross-sectional online survey was conducted with a nationally representative U.S. sample (n=6,684). Half responded before March 13, 2020 (versus later). Participants assessed their risks of COVID-19 infection and infection fatality (0%–100%) which were transformed into quartiles (1–4). They reported their implementation of protective behaviors like handwashing and social distancing (yes/no). Analyses were conducted in April‒May 2020.
Results
Median perceived risk was 10.00% for COVID-19 infection and 5.00% for infection fatality, but respondents showed large disagreement. An increase of 1 quartile in perceived infection risk was associated with being 1.45 times (95% CI=1.33, 1.58) more likely to report handwashing, with perceived infection fatality risk showing no significant association. When predicting social distancing behaviors such as avoiding crowds, both quartile-based risk perceptions were significant (OR=1.24, 95% CI=1.17, 1.30 for infection and OR=1.19, 95% CI=1.13, 1.26 for infection fatality). Perceived COVID-19 infection risk, protective behaviors, and their relationship increased among later (versus earlier) responders.
Conclusions
Despite disagreements about the risks, people perceiving greater risks were more likely to implement protective behaviors—especially later (versus earlier) in March 2020. These findings have implications for risk communication.
INTRODUCTION
As coronavirus disease 2019 (COVID-19) spread across the U.S. in March 2020, people faced a new and unfamiliar health threat about which information was limited and changing. Although the outlook remains uncertain, COVID-19 has already caused far greater morbidity and mortality than other human coronaviruses such as severe acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome.1 To limit disease transmission, the Centers for Disease Control and Prevention have recommended protective behaviors such as hand hygiene and social distancing.2 Mass adoption of these behaviors is especially important when pharmacological interventions are not yet available.3 According to theories of decisions about health behavior, people who perceive greater risks are more motivated to implement protective behaviors.4, 5, 6 Hence, assessing associations between risk perceptions and protective behaviors has practical and theoretical relevance.
Links between perceived risks and protective behaviors have traditionally been studied for familiar risks like seasonal influenza.7 With emerging diseases like COVID-19, objective risk information is typically scarce, characterized by uncertainty, and subject to change. It is unclear how people perceive the risks or whether their initial risk perceptions inform their decisions about protective actions.8 Therefore, the objective of this study is to examine people's initial risk perceptions for COVID-19 infection and infection fatality, as well as associations of these initial risk perceptions with self-reported protective behaviors. Because the survey was completed between mid-to-late March 2020, the authors were able to add exploratory analyses to examine how risk perceptions, protective behaviors, and their associations varied as the initial stage of the epidemic unfolded.
METHODS
Study Sample
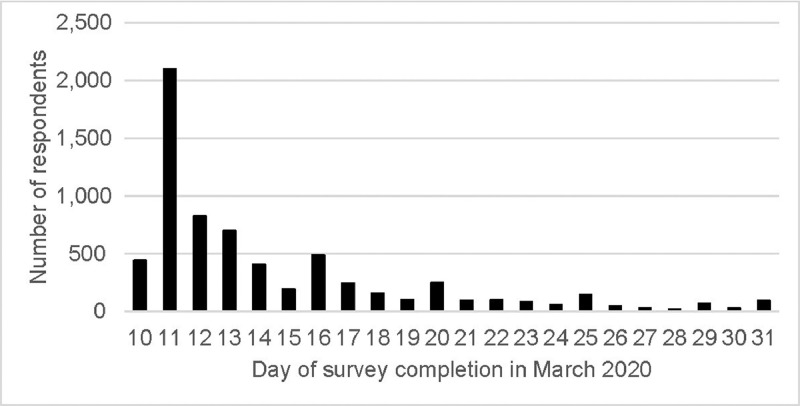
Data collection was approved by the University of Southern California's IRB, as part of the Understanding America Study (UAS). Since 2014, the UAS has been recruiting U.S. adults aged ≥18 years by mailing invitations to randomly selected U.S. addresses. If needed, interested individuals received Internet access and a computer or tablet. UAS members are regularly invited to participate in online surveys and receive about $20 per 30 minutes of survey time. Between March 10 and March 31, 2020, an online survey was conducted with 6,684 of 8,489 invited UAS participants (response rate=79%).9 Half completed the survey before (versus on or after) March 13, 2020 (Figure 1 ), when the White House issued a national emergency, the ban on European travel went into effect at midnight EDT, and several states announced school closures and bans of large gatherings.10, 11, 12 Table 1 shows how this sample compares with invited UAS participants who did not complete the survey and with the U.S. population.
Figure 1.
Number of respondents by survey day. Respondents could complete the survey between March 10‒31, 2020. Survey days were not randomly assigned. Half of respondents completed the survey before March 13, 2020, when the White House issued a national emergency, the ban on European travel went into effect at midnight EDT, and several states announced school closures and bans of large gatherings.10‒12
Table 1.
Demographic Characteristics of 2018 U.S. Population, Responders, and Nonresponders
| Demographic characteristic | 2018 U.S. population | Responders | Nonresponders | Test of difference between responders and nonresponders |
|---|---|---|---|---|
| At-risk age group ≥65 years | 16% | 20% (1,333 out of 6,684) | 20% (359 out of 1,798) | χ(1)=0.00, p=0.98 |
| Male | 49% | 48% (3,226 out of 6,684) | 49% (872 out of 1,799) | χ(1)=0.02, p=0.88 |
| African American | 13% | 12% (768 out of 6,684) | 14% (244 out of 1,799) | χ(1)=5.80, p=0.02 |
| Hispanic/Latinx | 18% | 16% (1,097 out of 6,684) | 18% (319 out of 1,799) | χ(1)=1.78, p=0.18 |
| Other minority | 9% | 9% (587 out of 6,684) | 8% (144 out of 1,799) | χ(1)=1.09, p=0.30 |
| White | 60% | 63% (4,232 out of 6,684) | 61% (1,092 out of 1,799) | χ(1)=4.18, p=0.04 |
| College degree | 32% | 34% (2,290 out of 6,684) | 32% (581 out of 1,805) | χ(1)=2.73, p=0.10 |
| Household income, median | $60,293 | $50,000–$59,000 | $50,000–$59,000 | M-W=6,003,157.50, p<0.001 |
| Below-median income | — | 45% (2,989 out of 6,684) | 52% (929 out of 1,790) | χ(1)=29.29, p<0.001 |
| Live in worst-hit state | 25% | 22% (1,482 out of 6,684) | 25% (458 out of 1,805) | χ(1)=8.26, p<0.01 |
Note: 2018 U.S. population statistics as reported by the U.S. Census Bureau (www.census.gov/quickfacts/fact/table/US/PST045218), with percent with college degree for population aged 25 and older. Worst-hit states at the time of the survey were California, Massachusetts, New Jersey, New York, and Washington. There were 6,684 responders and 1,805 nonresponders among the 8,489 invitees, but a few nonresponders had missing data for specific characteristics.
M-W, Mann-Whitney nonparametric test.
Measures
To assess experiences with COVID-19, participants were first asked: Has a doctor or another healthcare professional diagnosed you with the coronavirus (COVID-19)? and Do you think you have been infected with the coronavirus (COVID-19)? Response options were yes, no, and unsure. To assess perceived COVID-19 infection risk, participants were asked: On a scale from 0 to 100%, what is the chance that you will get the coronavirus in the next three months? To assess perceived infection fatality risk, participants were asked: If you do get infected with the coronavirus, what is the chance you will die from it? Both assessments were provided on a validated 0%–100% visual linear scale.7 Participants were also asked to report on protective behaviors: Which of the following have you done in the last seven days to keep yourself safe from coronavirus in addition to what you normally do? 2 Responses (yes or no) referred to behaviors recommended by the Centers for Disease Control and Prevention, including (1) washed hands with soap or used hand sanitizer several times per day; (2) avoided public spaces, gatherings, or crowds; (3) avoided contact with people who could be high-risk; and (4) canceled or postponed air travel for work and canceled or postponed air travel for pleasure, for which responses were combined. The UAS provided records of the survey completion date and respondent characteristics. The survey and data set are available from the UAS website.9
Statistical Analysis
Analyses were conducted with SPSS, version 26 in April‒May 2020. Post-stratification weights, generated through a raking algorithm, were used in all analyses to align the sample to the U.S. adult population, in terms of distributions for sex, race/ethnicity, age, education, and geographic location (more information is available at uasdata.usc.edu/page/Weights).
Before conducting the main analyses, the authors examined the percentage of participants who had been diagnosed with COVID-19 and the percentage who thought they had it. Descriptive statistics were computed, including medians and means (95% CIs) of respondents’ perceived COVID-19 infection and COVID-19 infection fatality risk. To examine disagreement between respondents, box plots were created for perceived risks (Figure 2 ), and t-tests were conducted to compare perceived risks between demographic groups (Table 2 ).
Figure 2.
Boxplot of perceived COVID-19 infection risk and perceived COVID-19 infection fatality risk. (a) Perceived COVID-19 infection risk. (b) perceived COVID-19 infection fatality risk. n=6,684. The box reflects the IQR. The black line in the box reflects the median. The whiskers reflect 1.5 × IQR. The circles reflect values outside 1.5 × IQR.
COVID-19, coronavirus disease 2019.
Table 2.
Differences in Risk Perceptions Between Demographic Groups
| Demographic characteristic | Respondents % (N) | Mean (SD) risk perception |
|
|---|---|---|---|
| COVID-19 infection | COVID-19 case fatality | ||
| Later responder (March 13‒31, 2020) | 50 (3,317) | 24.78 (23.96)*** | 15.05 (22.34) |
| Earlier responder (March 10‒12, 2020) | 50 (3,367) | 17.77 (21.25) | 15.29 (22.55) |
| At-risk age group ≥65 years | 20 (1,333) | 17.53 (20.08)*** | 22.81 (27.35)*** |
| Not at-risk age group <65 years | 80 (5,351) | 22.18, (23.47) | 13.26 (20.61) |
| Male | 48 (3,226) | 21.79 (22.91) | 14.28 (22.06)** |
| Female | 52 (3,458) | 20.74 (22.89) | 15.99 (22.77) |
| African American | 12 (768) | 15.42 (21.76)*** | 17.76 (23.63)** |
| Hispanic/Latinx | 16 (1,097) | 23.78 (25.28) | 13.90 (21.21) |
| Other minority | 9 (587) | 21.01 (23.44) | 14.77 (21.58) |
| White | 63 (4,232) | 22.02 (22.46) | 14.98 (22.59) |
| Below-median income | 54 (3,580) | 18.84 (22.12)*** | 18.59 (24.27)*** |
| Income ≥median | 46 (3,104) | 24.03 (23.48) | 11.23 (19.41) |
| College degree | 34 (2,290) | 24.63 (23.88)*** | 10.48 (18.51)*** |
| No college degree | 66 (4,394) | 19.49 (22.18) | 17.61 (23.89) |
| Live in worst-hit state | 22 (1,482) | 22.06 (24.16) | 14.96 (23.27) |
| Live in other state | 78 (5,202) | 21.02 (22.53) | 15.23 (22.21) |
Note: n=6,684; t-tests were conducted to examine differences between means. Significant differences are indicated on the first row for each group (***p<0.001; **p<0.01; *p<0.05). For race/ethnicity, the first 3 groups were compared with the white group. Median income was $50,000–$59,999. Worst-hit states at the time of the survey were California, Massachusetts, New Jersey, New York, and Washington.
To facilitate interpretation of the main analyses, investigators first examined the percentage of participants who engaged in each protective behavior. To answer the main research question about the relationship between risk perceptions and protective behaviors, authors conducted separate logistic regressions predicting each of the protective behaviors, including handwashing, avoiding crowds, avoiding contact with people who could be high risk, and canceling or postponing air travel. Because ORs for continuous scales with small units (such as the 0%–100% risk perception scales) can be difficult to interpret, these main logistic regressions were conducted with the quartile-based risk perceptions as predictors (Table 3 ). Specifically, respondents were divided into quartiles by perceived risk (or 4 similar-sized groups of respondents giving the lowest 25% to the highest 25% of responses). The authors also created graphs presenting the percentage of participants who reported protective behaviors by quartile of risk perception (Figure 3 ). Analogous logistic regressions with continuous risk perceptions yielded similar results (Table 4 ), as did Pearson correlations that did not include control variables (Table 5 ). In each of the reported logistic regressions, predictor variables were perceived infection risk and perceived infection fatality risk for COVID-19, while accounting for whether or not participants responded later (between March 13 and 31, 2020=1; between March 10 and 12, 2020=0); were in the at-risk group aged ≥65 years (yes=1, no=0); identified as male (yes=1, no=0); identified as African American (yes=1, no=0), Hispanic/Latinx (yes=1, no=0), or another minority (yes=1, no=0) versus white; had below-median income (yes=1; no=0); had a college degree (yes=1, no=0); and lived in one of the states that was worst hit at the time of the survey (California, Massachusetts, New Jersey, New York, or Washington=1; other state=0).
Table 3.
Logistic Regressions With Quartile-Based Risk Perceptions as Predictors
| Predictor variable | (1) Washed hands | (2) Avoided public spaces or crowds | (3) Avoided high-risk individuals | (4) Canceled or postponed travel |
|---|---|---|---|---|
| Perceived COVID-19 infection risk (1‒4) | 1.45 (1.33, 1.58)*** | 1.24 (1.17, 1.30)*** | 1.15 (1.09, 1.21)*** | 1.12 (1.06, 1.18)*** |
| Perceived COVID-19 infection fatality risk (1‒4) | 0.97 (0.90, 1.05) | 1.19 (1.13, 1.26)*** | 1.10 (1.05, 1.16)*** | 1.16 (1.10, 1.22)*** |
| Later responder (yes=1; no=0) | 2.02 (1.70, 2.39)*** | 3.33 (3.00, 3.71)*** | 2.81 (2.54, 3.12)*** | 3.01 (2.70, 3.36)*** |
| At-risk age group (yes=1; no=0) | 1.25 (1.02, 1.53) | 1.16 (1.02, 1.33)* | 1.07 (0.94, 1.22) | 0.93 (0.81, 1.07) |
| Male (yes=1; no=0) | 0.49 (0.42, 0.58)*** | 0.86 (0.77, 0.95)** | 0.83 (0.74, 0.92)*** | 0.89 (0.80, 0.99)* |
| African American (yes=1; no=0) | 2.04 (1.52, 2.73)*** | 1.44 (1.21, 1.70)*** | 1.70 (1.43, 2.02)*** | 2.15 (1.81, 2.55)*** |
| Hispanic/Latinx (yes=1; no=0) | 1.98 (1.51, 2.58)*** | 1.83 (1.57, 2.13)*** | 1.56 (1.35, 1.81)*** | 1.94 (1.68, 2.25)*** |
| Other minority (yes=1; no=0) | 1.28 (0.94, 1.74) | 2.07 (1.69, 2.52)*** | 1.97 (1.62, 2.40)*** | 2.20 (1.82, 2.65)*** |
| Below-median income (yes=1; no=0) | 0.70 (0.58, 0.83)*** | 1.14 (1.01, 1.28)* | 1.02 (0.91, 1.15) | 0.99 (0.88, 1.11) |
| College degree (yes=1; no=0) | 1.34 (1.10, 1.62)** | 1.43 (1.27, 1.62)*** | 1.05 (0.93, 1.18) | 1.63 (1.44, 1.84)*** |
| Live in worst-hit state (yes=1; no=0) | 1.35 (1.09, 1.67)*** | 1.18 (1.04, 1.34)* | 1.18 (1.04, 1.34)** | 1.33 (1.17, 1.51)*** |
| Later responder X perceived COVID-19 infection risk | 1.40 (1.18, 1.67)*** | 1.19 (1.07, 1.31)*** | 1.13 (1.03, 1.25)*** | 1.06 (0.96, 1.18) |
| Later responder X perceived COVID-19 infection fatality risk | 0.83 (0.71, 0.97)* | 0.92 (0.83, 1.02) | 1.01 (0.91, 1.11) | 1.04 (0.94, 1.15) |
Note: n=6,684. Boldface indicates statistical significance (***p<0.001; **p<0.01; *p<0.05). Later responders completed the survey on March 13‒31, 2020 and earlier responders on March 10‒12, 2020. At-risk age group was aged 65 years or older. Median income was $50,000–$59,999. Worst-hit states were California, Massachusetts, New Jersey, New York, and Washington. Interactions were added to the reported main effects in a separate model. Logistic regressions used post-stratification weights. Table 4 shows analogous models with continuous risk perceptions. Table 5 provides associated Pearson correlations.
COVID-19, coronavirus disease 2019.
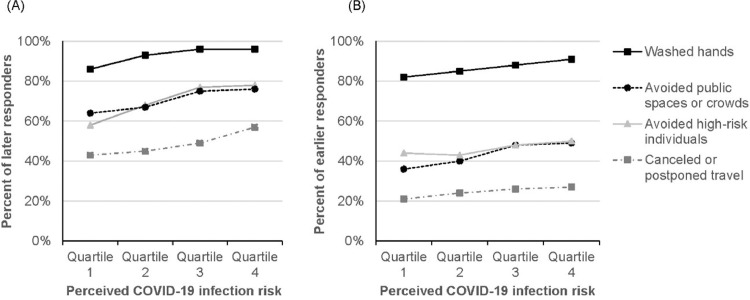
Figure 3.
Percent of respondents reporting each protective behavior by quartile of perceived COVID-19 infection risk and quartile of perceived COVID-19 infection fatality risk. (a) Quartiles reflect (1) 0%‒1.00% (n=1,730), (2) 1.01%‒10.00% (n=1,620), (3) 10.01%‒39.10% (n=1,665); and (4) 39.11%‒100.00% (n=1,670). (b) Quartiles reflect (1) 0%‒0.40% (n=1,687), (2) 0.41%‒5.00% (n=2,070), (3) 5.01%‒20.00% (n=1,289), and (4) 20.01%‒100.00% (n=1,638).
COVID-19, coronavirus disease 2019.
Table 4.
Logistic Regression Models With Continuous Risk Perceptions as Predictors
| Predictor variable | (1) Washed hands | (2) Avoided public spaces or crowds | (3) Avoided high-risk individuals | (4) Canceled or postponed travel |
|---|---|---|---|---|
| Perceived COVID-19 infection risk (0‒100) | 1.02 (1.01, 1.02)*** | 1.01 (1.01, 1.01)*** | 1.01 (1.01, 1.01)*** | 1.01 (1.00, 1.01)*** |
| Perceived COVID-19 infection fatality risk (0‒100) | 1.00 (1.00, 1.00) | 1.01 (1.01, 1.01)*** | 1.00 (1.00, 1.01)** | 1.01 (1.00, 1.01)*** |
| Later responder (yes=1; no=0) | 2.03 (1.71, 2.41)*** | 3.31 (2.98, 3.68)*** | 2.80 (2.53, 3.11)*** | 2.99 (2.67, 3.33)*** |
| At-risk age group (yes=1; no=0) | 1.25 (1.02, 1.54)* | 1.16 (1.01, 1.33)* | 1.08 (0.95, 1.23) | 0.95 (0.82, 1.10) |
| Male (yes=1; no=0) | 0.50 (0.42, 0.59)*** | 0.86 (0.77, 0.95)** | 0.83 (0.75, 0.92)*** | 0.89 (0.79, 0.99)* |
| African American (yes=1; no=0) | 1.89 (1.41, 2.52)*** | 1.38 (1.16, 1.63)*** | 1.07 (0.95, 1.20)*** | 2.14 (1.80, 2.53)*** |
| Hispanic/Latinx (yes=1; no=0) | 1.93 (1.48, 2.52)*** | 1.82 (1.56, 2.12)*** | 1.56 (1.34, 1.80)*** | 1.96 (1.69, 2.27)*** |
| Other minority (yes=1; no=0) | 1.26 (0.92, 1.71) | 2.06 (1.69, 2.51)*** | 1.97 (1.62, 2.39)*** | 2.20 (1.83, 2.66)*** |
| Below-median income (yes=1; no=0) | 0.69 (0.58, 0.82)*** | 1.10 (0.98, 1.24) | 1.07 (0.95, 1.19) | 0.93 (0.83, 1.05) |
| College degree (yes=1; no=0) | 1.36 (1.12, 1.65)** | 1.44 (1.27, 1.62)*** | 1.07 (0.95, 1.23) | 1.59 (1.41, 1.80)*** |
| Live in worst-hit state (yes=1; no=0) | 1.33 (1.08, 1.65)** | 1.15 (1.01, 1.31)* | 1.17 (1.03, 1.32)* | 1.30 (1.14, 1.48)*** |
| Later responder X perceived COVID-19 infection risk | 1.01 (1.00, 1.02)** | 1.01 (1.00, 1.01)** | 1.01 (1.00, 1.01)* | 1.00 (1.00, 1.01) |
| Later responder X perceived COVID-19 infection fatality risk | 0.99 (0.98, 1.00)** | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) |
Note: n=6,684. Boldface indicates statistical significance (***p<0.001; **p<0.01; *p<0.05). ORs for continuous risk perceptions are associated with only 1-unit change on the 0%‒100% scale. Later responders completed the survey on March 13‒31, 2020 and earlier responders on March 10‒12, 2020. At-risk age group was aged 65 years or older. Median income was $50,000–$59,999. Worst-hit states were California, Massachusetts, New Jersey, New York, and Washington. Interactions were added to the reported main effects in a separate model. Logistic regressions used post-stratification weights. Table 3 shows analogous models with quartile-based risk perceptions. Table 5 provides associated Pearson correlations.
COVID-19, coronavirus disease 2019.
Table 5.
Pearson Correlations of Risk Perceptions With Protective Behaviors
| Quartile-based risk perceptions (1‒4) |
Continuous risk perceptions (0‒100%) |
|||
|---|---|---|---|---|
| Protective behavior | COVID-19 infection | COVID-19 infection fatality | COVID-19 infection | COVID-19 infection fatality |
| Washed hands | 0.13*** | 0.03 | 0.11*** | 0.01 |
| Avoided public spaces or crowds | 0.17*** | 0.12*** | 0.16*** | 0.09*** |
| Avoided high-risk individuals | 0.11*** | 0.07*** | 0.11*** | 0.05*** |
| Canceled or postponed air travel | 0.11*** | 0.08*** | 0.12*** | 0.05*** |
Note: n=6,684. Boldface indicates statistical significance (***p<0.001). Pearson correlation between the 2 quartile-based risk perceptions: r =0.34 (p<0.001) and between the 2 continuous risk perceptions: r =0.21 (p<0.001).
COVID-19, coronavirus disease 2019.
In a final set of exploratory analyses, authors examined whether the findings differed between the 50% of respondents who completed the survey on or after (versus before) March 13, 2020, when the national emergency and the European travel ban were taking effect and school closures were being announced.10, 11, 12 This study used this dichotomous variable rather than a continuous variable for survey day because the number of respondents across survey days was highly skewed and dropped off substantially for later survey days (Figure 1). Authors computed t-tests to compare risk perceptions of later versus earlier responders. Chi-square tests compared reported protective behaviors of later versus earlier responders. This study also examined contributions of later versus earlier responding in the logistic regression models that predicted each protective behavior (Tables 3 and 4). To examine whether relationships between risk perceptions and protective behavior differed between later versus earlier responders, interactions between later versus earlier responding and each risk perception were added to logistic regressions predicting each protective behavior (Tables 3 and 4), and logistic regressions were run separately for later responders and earlier responders (Tables 6 and 7 ).
Table 6.
Logistic Regressions With Quartile-Based Risk Perceptions as Predictors for Later Versus Earlier Responders
| Later responders (March 13‒31, 2020) |
Earlier responders (March 10‒12, 2020) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictor variable | (1) Washed hands | (2) Avoided public spaces or crowds | (3) Avoided high-risk individuals | (4) Canceled or postponed travel | (1) Washed hands | (2) Avoided public spaces or crowds | (3) Avoided high-risk individuals | (4) Canceled or postponed travel |
| Perceived COVID-19 infection risk (quartile 1‒4) | 1.74 (1.51, 2.02)*** | 1.30 (1.20, 1.40)*** | 1.20 (1.11, 1.29)*** | 1.14 (1.06, 1.22)*** | 1.32 (1.19, 1.46)*** | 1.17 (1.09, 1.26)*** | 1.10 (1.03, 1.18)** | 1.09 (1.01, 1.18)* |
| Perceived COVID-19 infection fatality risk (0‒100) | 0.88 (0.77, 1.01) | 1.17 (1.08, 1.27)*** | 1.13 (1.05, 1.22)** | 1.18 (1.10, 1.26)*** | 1.02 (0.92, 1.12) | 1.20 (1.12, 1.29)*** | 1.08 (1.01, 1.15)* | 1.13 (1.04, 1.22)** |
| At-risk age group (yes=1; no=0) | 1.22 (0.84, 1.77) | 1.06 (0.86, 1.32) | 0.89 (0.73, 1.10) | 0.90 (0.74, 1.10) | 1.27 (1.00, 1.62) | 1.21 (1.02, 1.44)* | 1.21 (1.02, 1.43)* | 0.96 (0.78, 1.18) |
| Male (yes=1; no=0) | 0.52 (0.39, 0.70)*** | 0.80 (0.69, 0.95)** | 0.73 (0.63, 0.86)*** | 0.87 (0.75, 1.01) | 0.48 (0.39, 0.59)*** | 0.88 (0.76, 1.01) | 0.91 (0.79, 1.04) | 0.92 (0.78, 1.09) |
| African American (yes=1; no=0) | 2.18 (1.34, 3.53)** | 1.08 (0.84, 1.38) | 1.65 (1.27, 2.14)*** | 1.85 (1.47, 2.33)*** | 2.00 (1.39, 2.88)*** | 1.85 (1.47, 2.33)*** | 1.71 (1.36, 2.15)*** | 2.61 (2.03, 3.36)*** |
| Hispanic/Latinx (yes=1; no=0) | 1.41 (0.95, 2.09) | 2.06 (1.64, 2.60)*** | 1.49 (1.20, 1.85)*** | 1.83 (1.51, 2.22)*** | 2.63 (1.81, 3.81)*** | 1.68 (1.36, 2.07)*** | 1.64 (1.34, 2.02)*** | 2.11 (1.68, 2.66)*** |
| Other minority (yes=1; no=0) | 1.86 (0.96, 3.59) | 2.01 (1.44, 2.80)*** | 2.12 (1.53, 2.95)*** | 1.69 (1.30, 2.20)*** | 1.14 (0.80, 1.62) | 2.15 (1.67, 2.76)*** | 1.94 (1.51, 2.48)*** | 2.88 (2.22, 3.73)*** |
| Below-median income (yes=1; no=0) | 0.58 (0.43, 0.78)*** | 0.97 (0.82, 1.16) | 1.00 (0.84, 1.19) | 1.01 (0.86, 1.18) | 0.77 (0.62, 0.96)* | 1.29 (1.11, 1.51)** | 1.04 (0.89, 1.21) | 0.97 (0.81, 1.17) |
| College degree (yes=1; no=0) | 1.86 (0.96, 3.60)** | 1.71 (1.42, 2.06)*** | 1.27 (1.07, 1.52)** | 1.63 (1.38, 1.92)*** | 1.17 (0.93, 1.47) | 1.27 (1.08, 1.49)** | 0.90 (0.76, 1.05) | 1.63 (1.36, 1.96)*** |
| Live in worst-hit state (Yes=1; no=0) | 1.54 (1.04, 2.29)* | 1.09 (0.89, 1.33) | 1.18 (0.97, 1.44) | 1.44 (1.21, 1.71)*** | 1.29 (1.00, 1.66)* | 1.24 (1.05, 1.47)* | 1.17 (0.99, 1.39) | 1.20 (0.99, 1.45) |
Note: n=3,317 for later responders and n=3,367 for earlier responders. Boldface indicates statistical significance (***p<0.001; **p<0.01; *p<0.05). At-risk age group was aged 65 years or older. Median income was $50,000–$59,999. Worst-hit states were California, Massachusetts, New Jersey, New York, and Washington. Logistic regressions used post-stratification weights. Table 7 shows analogous models with continuous risk perceptions.
COVID-19, coronavirus disease 2019.
Table 7.
Logistic Regressions With Continuous Risk Perceptions as Predictors for Later Versus Earlier Responders
| Later responders (March 13‒31, 2020) |
Earlier responders (March 10‒12, 2020) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Predictor variable | (1) Washed hands | (2) Avoided public spaces or crowds | (3) Avoided high-risk individuals | (4) Canceled or postponed travel | (1) Washed hands | (2) Avoided public spaces or crowds | (3) Avoided high-risk individuals | (4) Canceled or postponed travel |
| Perceived COVID-19 infection risk (0‒100) | 1.03 (1.02, 1.03)*** | 1.01 (1.01, 1.02)*** | 1.01 (1.01, 1.01)*** | 1.01 (1.00, 1.01)*** | 1.01 (1.01, 1.02)*** | 1.01 (1.00, 1.01)*** | 1.01 (1.00, 1.01)*** | 1.01 (1.00, 1.01)** |
| Perceived COVID-19 infection fatality risk (0‒100) | 0.99 (0.99, 1.00) | 1.01 (1.01, 1.01)*** | 1.01 (1.00, 1.01)*** | 1.01 (1.00, 1.01)*** | 1.00 (1.00, 1.01) | 1.01 (1.00, 1.01)*** | 1.00 (1.00, 1.01) | 1.00 (1.00, 1.01) |
| At-risk age group (yes=1; no=0) | 1.26 (0.87, 1.84) | 1.03 (0.83, 1.23) | 0.89 (0.72, 1.09) | 0.91 (0.74, 1.11) | 1.25 (0.99, 1.60) | 1.23 (1.04, 1.46)* | 1.23 (1.04, 1.46)* | 0.98 (0.80, 1.20) |
| Male (yes=1; no=0) | 0.52 (0.39, 0.69)*** | 0.80 (0.68, 0.94)** | 0.73 (0.63, 0.86)*** | 0.87 (0.75, 1.00) | 0.49 (0.39, 0.60)*** | 0.88 (0.76, 1.02) | 0.91 (0.79, 1.04) | 0.92 (0.78, 1.09) |
| African American (yes=1; no=0) | 2.05 (1.26, 3.32)** | 1.01 (0.79, 1.29) | 1.58 (1.22, 2.05)** | 1.79 (1.42, 2.25)*** | 1.91 (1.32, 2.74)** | 1.78 (1.42, 2.24)*** | 1.69 (1.34, 2.01)*** | 2.59 (2.02, 3.33)*** |
| Hispanic/Latinx (yes=1; no=0) | 1.35 (0.92, 2.00) | 2.07 (1.64, 2.60)*** | 1.49 (1.20, 1.85)*** | 1.84 (1.52, 2.23)*** | 2.59 (1.79, 3.76)*** | 1.66 (1.35, 2.04)*** | 1.64 (1.34, 2.01)*** | 2.13 (1.69, 2.68)*** |
| Other minority (yes=1; no=0) | 1.84 (0.95, 3.55) | 2.00 (1.43, 2.78)*** | 2.11 (1.52, 2.93)*** | 1.68 (1.29, 2.19)*** | 1.13 (0.79, 1.62) | 2.14 (1.67, 2.75)*** | 1.94 (1.52, 2.49)*** | 2.89 (2.23, 3.74)*** |
| Below-median income (yes=1; no=0) | 0.57 (0.42, 0.77)*** | 0.94 (0.79, 1.12) | 0.99 (0.83, 1.17) | 1.01 (0.86, 1.18) | 0.75 (0.61, 0.94)* | 1.30 (1.11, 1.51)** | 1.05 (0.90, 1.22) | 0.98 (0.82, 1.18) |
| College degree (yes=1; no=0) | 1.91 (1.31, 2.78)** | 1.77 (1.47, 2.13)*** | 1.30 (1.09, 1.55)** | 1.64 (1.39, 1.93)*** | 1.19 (0.94, 1.49) | 1.27 (1.08, 1.49)*** | 0.89 (0.76, 1.04) | 1.62 (1.34, 1.94)*** |
| Live in worst-hit state (yes=1; no=0) | 1.52 (1.02, 2.26)* | 1.07 (0.87, 1.30) | 1.17 (0.96, 1.42) | 1.41 (1.19, 1.68)*** | 1.27 (0.99, 1.64) | 1.21 (1.02, 1.43)* | 1.16 (0.98, 1.37)** | 1.17 (0.97, 1.42) |
Note: n=3,317 for later responders and n=3,367 for earlier responders. Boldface indicates statistical significance (***p<0.001; **p<0.01; *p<0.05). ORs for continuous risk perceptions are associated with only 1-unit change on the 0‒100% scale. At-risk age group was aged 65 years or older. Median income was $50,000–$59,999. Worst-hit states were California, Massachusetts, New Jersey, New York, and Washington. Table 6 shows analogous models with quartile-based risk perceptions. Logistic regressions used post-stratification weights.
COVID-19, coronavirus disease 2019.
RESULTS
None of the participants had yet been diagnosed with COVID-19, although 0.3% were unsure. None of the participants thought they had been infected, although 6.9% were unsure. Median risk perceptions were 10.00% for perceived COVID-19 infection (mean=21.25, SD=22.90, 95% CI=20.70, 21.80) and 5.00% for perceived COVID-19 infection fatality (mean=15.17, SD=22.45, 95% CI=14.63, 15.71). Box plots revealed large disagreement between respondents about the emerging risks, although most perceived risks to be toward the lower end of the scale (Figure 2). Some of the disagreement in perceived risks likely reflected respondent characteristics (Table 2). As noted, this study controlled for these characteristics in subsequent analyses that answered the main research question about the relationship between risk perceptions and protective behaviors.
Of the 6,684 respondents, 90% reported handwashing, 58% avoiding high-risk individuals, 57% avoiding crowds, and 37% canceling or postponing travel. Although respondents showed large disagreement between the risks of COVID-19 infection (Figure 2), risk perceptions were generally associated with protective behaviors. In logistic regressions that took into account quartile-based risk perceptions as well as respondent characteristics, as their perceived risks of COVID-19 infection increased by 1 quartile, participants were 1.45 times (95% CI=1.33, 1.58) more likely to report handwashing (Table 3, Model 1). Reports of handwashing increased from 83% to 94% between the quartile of respondents perceiving the lowest risk for COVID-19 infection and the quartile reporting the highest risk for COVID-19 infection (Figure 3A).
In the logistic regressions that accounted for quartile-based risk perceptions and respondent characteristics, perceived COVID-19 infection fatality risk added little to predictions of handwashing (Table 3, Model 1). Handwashing only increased from 87% to 90% between the quartile of respondents perceiving the lowest risk for COVID-19 infection fatality and the quartile reporting the highest risk for COVID-19 infection fatality (Figure 3B).
When predicting social distancing behaviors such as avoiding public spaces or crowds, both risk perceptions were significant (OR=1.24, 95% CI=1.17, 1.30 for infection risk and OR=1.19, 95% CI=1.13, 1.26 for infection fatality risk) (Table 3, Model 2). Avoiding public spaces or crowds increased from 45% to 67% between the quartile of respondents perceiving the lowest risk for COVID-19 infection and the quartile reporting the highest risk for COVID-19 infection (Figure 3A). For infection fatality, the increase was from 46% to 63% (Figure 3B).
Median perceived risk for COVID-19 infection was 10.00% for the 50% of participants responding later (between March 13 and 31, 2020) and 5.00% for the 50% of participants responding earlier (between March 10 and 12, 2020). Indeed, t-tests confirmed that later respondents reported greater perceived risk for COVID-19 infection (mean=24.78, SD=23.96 vs mean=17.77, SD=21.25, t[6,682]=12.66, p<0.001). Medians for perceived COVID-19 infection fatality risk were 5.00% for both the earlier and later responders, revealing no significant difference (mean=15.05, SD=22.34 vs mean=15.29, SD=22.55, t[6,682]=0.43, p=0.15).
Additionally, later responders were more likely to implement each of the protective behaviors than earlier responders. Specifically, late responders showed greater likelihood of handwashing (93% vs 86%, chi-square[1]=96.74, p<0.001), avoiding public spaces or crowds (71% vs 43%, chi-square[1]=568.32, p<0.001), avoiding high-risk individuals (71% vs 46%, chi-square[1]=434.52, p<0.001), and canceling or postponing travel (49% vs 24%, chi-square[1]=449.25, p<0.001). Logistic regressions that took into account quartile-based risk perceptions and respondent characteristics found that later responders were approximately 2 to 3 times more likely to implement protective behaviors than earlier responders (Table 3). ORs in models with quartile-based risk perceptions (Table 3) varied between 2.02 (95% CI=1.70, 2.39) for handwashing and 3.33 (95% CI=3.00, 3.71) for avoiding public spaces or crowds.
Adding interactions between responding later versus earlier and risk perceptions to these logistic regressions (Tables 3 and 4) revealed that the association between perceived COVID-19 infection risk and protective behaviors was stronger for later responders (Tables 6 and 7). Possibly, earlier responders were still hesitating to act on their risk perceptions compared with earlier responders. This relationship held for all behaviors, except for canceling or postponing travel. For example, Figure 4A shows that handwashing increased with 10 percentage points (from 86% to 96%) for later respondents perceiving COVID-19 infection risk in the lowest (versus highest) quartile but with 9 percentage points (from 82% to 91%) for earlier respondents perceiving COVID-19 infection risk in the lowest (versus highest) quartile. Avoiding public spaces or crowds increased with 20 percentage points (from 58% to 78%) for later respondents reporting infection risk perceptions in the lowest (versus highest) quartile but with 13 percentage points (from 36% to 49%) for earlier respondents reporting COVID-19 infection risk perceptions in the lowest (versus highest) quartile. The interaction effect for handwashing may have been relatively smaller, owing to a potential ceiling effect in reported handwashing.
Figure 4.
Percent of later and earlier respondents reporting each protective behavior by quartile of perceived COVID-19 infection risk. Later responders completed the survey on March 13‒31, 2020 and earlier responders on March 10‒12, 2020. (a) Quartiles reflect (1) 0%‒1.00% (n=712), (2) 1.01%‒10.00% (n=735), (3) 10.01%‒39.09% (n=844), and (4) 39.10%‒100.00% (n=1,026). (b) Quartiles reflect (1) 0%‒1.00% (n=1,018), (2) 1.01%‒10.00% (n=885), (3) 10.01%‒39.09% (n=820), and (4) 39.10%‒100.00% (n=647).
COVID-19, coronavirus disease 2019.
Interactions between perceived COVID-19 infection fatality risk and later versus earlier responding were not significant in most of the logistic regression models predicting protective behaviors (Tables 3 and 4). Only in models predicting handwashing was this interaction significant, independent of whether risk perceptions were entered as continuous or quartile-based predictors. That is, risk perceptions of COVID-19 infection fatality risk were somewhat less strongly related to handwashing among participants who completed the survey later (Tables 6 and 7). Figure 4B shows that handwashing increased with 4 percentage points (from 83% to 87%) for the earlier respondents perceiving COVID-19 infection risk in the lowest (versus highest) quartile and with 1 percentage point (from 91% to 92%) for the later respondents perceiving COVID-19 infection risk in the lowest (versus highest) quartile. It is possible that this finding also reflected the aforementioned ceiling effect in the uptake of handwashing.
DISCUSSION
In March 2020, COVID-19 was still an emerging risk. In this nationally representative U.S. sample, none of the participants had yet been diagnosed with the disease or thought they had been infected. Participants showed large disagreements in their perceived risk for getting infected with COVID-19 and dying from it if they were to become infected. Yet, the findings suggest that the U.S. respondents were already acting on their risk perceptions of COVID-19 in mid-to-late March 2020. Generally, this study found greater reported implementation of protective behaviors to avoid COVID-19 among those who perceived greater COVID-19 infection risk and greater COVID-19 infection fatality risk. Participants’ decisions to implement most protective actions seemed to have been motivated by wanting to reduce their risk of COVID-19 infection and, less so, to reduce their risk of COVID-19 mortality. It is possible that the perceived COVID-19 infection risk had a stronger relationship with protective behaviors than perceived COVID-19 infection fatality risk, because COVID-19 was perceived to have severe consequences other than death, including serious illness and self-quarantine. By comparison, perceived infection risk was also more strongly correlated to intentions to get vaccinated than perceived infection fatality risk in a longitudinal study following its U.S. participants during the first year of the H1N1 epidemic.13
A cross-sectional study conducted during the initial stages of the SARS outbreak in the Netherlands reported similar effect sizes as the ones reported here for correlations between perceived SARS infection risk and reports of protective behaviors.14 By comparison, cross-sectional and longitudinal reports of correlations between perceived risk of infection with seasonal influenza and getting the influenza vaccine appeared to be somewhat higher than the correlations between risk perceptions and protective behaviors reported here.7 , 15 However, a cross-sectional study of risk perceptions for hypothetical pandemic influenza showed no significant correlations with protective behaviors in Asian or European regions that were not experiencing outbreaks at the time.16 These findings are in line with construal level theory of psychological distance, which posits that risks that are perceived as uncertain or further in the future may reduce willingness to act.17 At the early stages of the COVID-19 epidemic, it is possible that many people were still hesitant to act on their risk perceptions and preferred taking a wait and see approach—perhaps especially because social distancing can be perceived as difficult and costly.
This interpretation is also supported by the exploratory analyses of differences between later and earlier responders. Those analyses suggested that, as the epidemic started to unfold, reported risk perceptions and protective behaviors increased, and the relationship between perceived COVID-19 infection risk and most protective behaviors became stronger. Because survey days were not randomly assigned, it is possible that different people responded earlier or later. However, these findings held when accounting for respondent characteristics (Tables 3 and 4). A longitudinal study of H1N1 risk perceptions and intentions to vaccinate for H1N1 also found initial increases over the first few months of the epidemic but did not report on changes in the relationship between risk perceptions and protective behavior.13
Limitations
Like any study, this study had limitations. One limitation is that this cross-sectional study yielded only correlational findings and that survey days were not assigned randomly, which precludes causal conclusions. For example, correlations between risk perceptions and reported actions could reflect the effect of a third variable, such as risk messages that increased both. Another limitation is that behaviors were self-reported and may have reflected social desirability bias.18 Longitudinal studies are needed to understand how risk perceptions, protective behaviors, and their associations changed over time beyond the early stages of the epidemic.13 , 15 Over time, it is possible that people who take actions to protect themselves may subsequently perceive less COVID-19 risk. As an example, people who have received a seasonal influenza vaccination have been found to lower their perceived risk afterward.15 The analyses presented here included no measures of perceived uncertainty or timing of the risk, which would have been needed to further understand the role of psychological distance in hesitancy to act on initial risk perceptions. The analyses also included no measures of other factors that could have potentially motivated protective behaviors, such as perceptions of the chance of infecting others, social norms, the ability to implement protective behaviors and bear any associated costs, or the need to follow policymakers’ recommendations and stay-at-home orders.4, 5, 6
CONCLUSIONS
Even though people in the U.S. seemed to disagree about the risks associated with COVID-19 in the early stages of the epidemic, those perceiving greater risks were more likely to report that they implemented protective behaviors—and more so later (versus earlier) in March 2020. Research on psychological distance has suggested that people may be more willing to act if risks are presented as happening in the here and now and as real rather than hypothetical.17 To promote protective behaviors, communications may need to address risks, as well as other factors that (as noted previously) have been deemed relevant to behavior change,4, 5, 6 such as the perceived chance of infecting others, social norms, ability to implement protective behaviors and bear any associated costs, or the perceived need to follow policymakers’ recommendations and stay-at-home orders.
ACKNOWLEDGMENTS
Data collection was funded and conducted by the University of Southern California's Center for Economic and Social Research. The authors especially want to thank Marco Angrisani, Jill Darling, Tania Gutsche, and Arie Kapteyn for their help with this study. Wändi Bruine de Bruin was supported by the University of Southern California's Schaeffer Center for Health Policy and Economics as well as the Swedish Foundation for the Humanities and the Social Sciences (Riksbankens Jubileumsfond) Program on Science and Proven Experience “Science and Proven Experience.” The funders had no role in study design; collection, analysis, and interpretation of data; writing the report; and the decision to submit the report for publication. Our data collection as part of the Understanding America Study was approved as a Human Subjects research project by the University of Southern California (UP-14-00148).
Wändi Bruine de Bruin and Daniel Bennett designed the survey and wrote the manuscript; Wändi Bruine de Bruin analyzed the data.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.Park M, Thwaites RS, Openshaw PJM. COVID-19: lessons from SARS and MERS. Eur J Immunol. 2020;50(3):308–311. doi: 10.1002/eji.202070035. [DOI] [Google Scholar]
- 2.What you can do. Centers for Disease Control and Prevention. www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/get-ready.html. Updated May 8, 2020. Accessed June 3, 2020.
- 3.Bruine de Bruin W, Fischhoff B, Brilliant L, Caruso D. Expert judgments of pandemic influenza risks. Glob Public Health. 2006;1(2):178–193. doi: 10.1080/17441690600673940. [DOI] [PubMed] [Google Scholar]
- 4.Fischhoff B. Risk perception and communication. In: Fischhoff B, ed. Risk Analysis and Human Behavior. London, UK: Routledge; 2012:3–32. 10.4324/9780203140710. [DOI]
- 5.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Monogr. 1974;2(4):354–386. doi: 10.1177/109019817400200405. [DOI] [PubMed] [Google Scholar]
- 6.Rogers RW. A protection motivation theory of fear appeals and attitude change1. J Psychol. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- 7.Bruine de Bruin W, Carman KG. Measuring subjective probabilities: the effect of response mode on the use of focal responses, validity, and respondents’ evaluations. Risk Anal. 2018;38(10):2128–2143. doi: 10.1111/risa.13138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennett D, Chiang CF, Malani A. Learning during a crisis: the SARS epidemic in Taiwan. J Dev Econ. 2015;112:1–18. doi: 10.1016/j.jdeveco.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.University of Southern California; April 2, 2020. Understanding America Study March 2020 monthly survey.https://uasdata.usc.edu/index.php Updated. [Google Scholar]
- 10.Proclamation on declaring a national emergency concerning the novel coronavirus disease (COVID-19) outbreak. The White House. www.whitehouse.gov/presidential-actions/proclamation-declaring-nationalemergency-concerning-novel-coronavirus-disease-covid-19-outbreak/. Published March 13, 2020. Accessed June 3, 2020.
- 11.Proclamation—suspension of entry as immigrants and nonimmigrants of certain additional persons who pose a risk of transmitting 2019 novel coronavirus. The White House. www.whitehouse.gov/presidential-actions/proclamation-suspension-entry-immigrants-nonimmigrants-certain-additional-persons-pose-risk-transmitting-2019-novel-coronavirus/. Published March 11, 2020. Accessed June 2, 2020.
- 12.Yeung J, Berlinger J, Renton A, Wagner M, Hayes M, Rocha V. March 13 coronavirus news. CNN. March 13, 2020 www.cnn.com/world/live-news/coronavirus-outbreak-03-13-20-intl-hnk/h_b598bc1fba2dc834b255c7c58a3f8c84 [Google Scholar]
- 13.Gidengil CA, Parker AM, Zikmund-Fisher BJ. Trends in risk perceptions and vaccination intentions: a longitudinal study of the first year of the H1N1 pandemic. Am J Public Health. 2012;102(4):672–679. doi: 10.2105/AJPH.2011.300407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brug J, Aro AR, Oenema A, de Zwart O, Richardus JH, Bishop GD. SARS risk perception, knowledge, precautions, and information sources, the Netherlands. Emerg Infect Dis. 2004;10(8):1486–1489. doi: 10.3201/eid1008.040283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weinstein ND, Cuite CL, Herrington JE. Risk perceptions and their relation to risk behavior. Annals Behav Med. 2004;27:125–130. doi: 10.1207/s15324796abm2702_7. [DOI] [PubMed] [Google Scholar]
- 16.Sadique MZ, Edmunds WJ, Smith RD. Precautionary behavior in response to perceived threat of pandemic influenza. Emerg Infect Dis. 2007;13(9):1307–1313. doi: 10.3201/eid1309.070372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trope Y, Liberman N. Construal-level theory of psychological distance. Psychol Rev. 2010;117(2):440–463. doi: 10.1037/a0018963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kristiansen CM, Harding CM. The social desirability of preventive health behavior. Public Health Rep. 1984;99(4):384–388. www.jstor.org/stable/4627663 [PMC free article] [PubMed] [Google Scholar]