Abstract
Considering the population density, healthcare capacity, limited resources and existing poverty, environmental factors, social structure, cultural norms, and already more than 18,863 people infected, the community transmission of COVID-19 is happening fast. These exacerbated a complex fear among the public. The aim of this article is, therefore, to understand the public perception of socioeconomic crisis and human stress in resource-limited settings of Bangladesh during the COVID-19 outbreak.
The sample comprised of 1066 Bangladeshi participants. Principal component analysis (PCA) was considered to design a standardized scale to measure the mental stress and socioeconomic crisis, one-way ANOVA and t-test were conducted to perceive different demographic risk groups; multiple linear regression was applied to estimate the statistically significant association between each component, and classical test theory (CTT) analysis was applied to examine the reliability of each item according to the components to develop a composite score.
Without safeguarding the fundamental needs for the vulnerable ultra-poor group can undeniably cause the socioeconomic crisis and mental stress due to the COVID-19 lockdown. It has further created unemployment, deprivation, hunger, and social conflicts. The weak governance in the fragile healthcare system exacerbates the general public's anxiety as the COVID-19 testing facilities are centered around in the urban areas, a long serial to be tested, minimum or no treatment facilities in the dedicated hospital units for COVID-19 patients are the chief observations hampered along with the disruption of other critical healthcare services. One-way ANOVA and t-test confirmed food and nutritional deficiency among the vulnerable poorest section due to loss of livelihood. Also, different emergency service provider professions such as doctors, healthcare staff, police forces, volunteer organizations at the frontline, and bankers are at higher risk of infection and subsequently mentally stressed. Proper risk assessment of the pandemic and dependable risk communications to risk groups, multi-sectoral management taskforce development, transparency, and good governance with inter-ministerial coordination is required along with strengthening healthcare capacity was suggested to reduce mental and social stress causing a socioeconomic crisis of COVID-19 outbreak. Moreover, relief for the low-income population, proper biomedical waste management through incineration, and preparation for the possible natural disasters such as flood, cyclones, and another infectious disease such as dengue was suggested. Finally, this assessment process could help the government and policymakers to judge the public perceptions to deal with COVID-19 pandemic in densely populated lower-middle-income and limited-resource countries like Bangladesh.
Keywords: Psychology, COVID-19, Perception-based questionnaire, Principal component analysis (PCA), Linear regression model, Social panic, Social conflict
Psychology; COVID-19; Perception-based questionnaire; Principal component analysis (PCA); Linear regression model; Social panic; Social conflict.
1. Introduction
The World Health Organization (WHO) announced COVID-19 as a global pandemic on March 11, 2020. The disease has advanced into a pandemic, started with small chains of spreading, further culminating into larger chains of spread in many countries resulting in the widespread transmission consequently across the globe affecting all the continents (Anderson et al., 2020). The fatality case of COVID-19 risk is around 1% and that it can kill healthy adults, as well as the elderly people with, existing health problems (Gates, 2020). According to Worldometers (2020), 14 May 2020, with the total coronavirus cases rising to 4,490,958, and total deaths 301,616, USA is the worst affected country from the COVID-19 pandemic with 86,098 deaths. It took 67 days from the first reported of COVID-19 to reach 100,000 cases, 11 days for the second 100,000, and just four days for the third 100,000 (WHO, 2020a, WHO, 2020b). The accelerating spread of the COVID-19 and its outcomes around the world has led people to fear, panic, concern, and anxiety (Ahorsu et al., 2020), panic buying of surgical masks (Wang et al., 2020), stigma, depression, racism, and xenophobia. Besides, as there is no medication and vaccination yet, wrong use of disinfectant liquids, methyl alcohols, garlic, lemon tea is amongst the many misinformation to cure COVID-19. Moreover, the fear of infection, quarantine, social isolation, a lack of self-care even leads individuals to suicide. Predictably, any contagious epidemic outbreak has deleterious effects on individuals and society (Duan and Zhu, 2020).
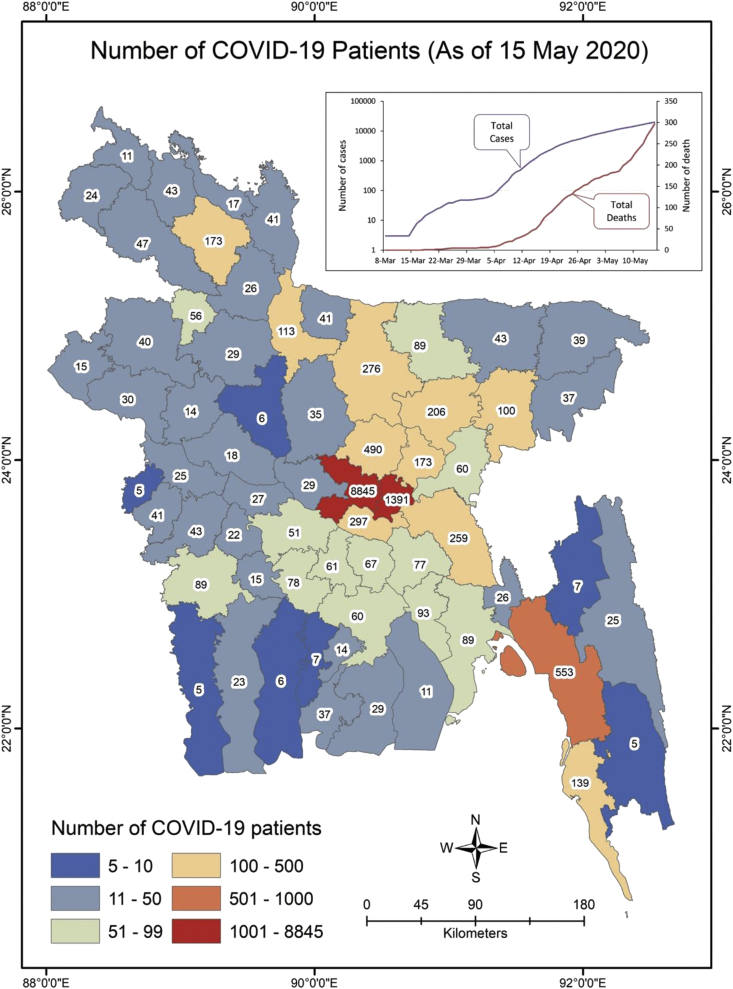
Institute of Epidemiology, Disease Control and Research (IEDCR) is the research institute under the Ministry of Health responsible for COVID-19 surveillance in Bangladesh, first confirmed the COVID-19 case on 7 March 2020, followed by a nationwide lockdown of all educational institutes, government and private offices, and industries from 26 March. The government of Bangladesh (GoB) deployed armed forces from 24 March to facilitate the social-distancing and prevention of the disease. Emergency healthcare services and law enforcement services were exempted from this announcement. Nevertheless, just after the announcement of lockdown, more than 11 million people left Dhaka to be in their home districts and commenced the risk of COVID-19 infection to the entire 64 districts in Bangladesh. On 15 May 2020, with 20,065 confirmed cases, 298 deaths (Figure 1) Bangladesh is within the top 30 affected country. With only 41 labs located in the urban areas, it is not easy to be tested for COVID-19 and often the tests are done after the patients had expired. Moreover, at present Bangladesh has 1,169 ICU beds, totalling to 0.72 beds/100,000 citizens. Of these 432 beds are in government hospitals and 737 in private hospitals. Likewise, there are only 550 ventilators in the country (IEDCR, 2020).
Figure 1.
Map of the study area showing number of COVID-19 confirmed patient (Data source: IEDCR).
Amidst the lockdown of the COVID-19 pandemic, Bangladesh also has been facing other epidemics of panic buying, social stigma, fear, and hatred. The primary healthcare treatments in the hospitals and private clinics were disrupted in the lockdown. Moreover, many emergency service providers such as frontline doctors, healthcare staffs, caregivers, police and armed forces, bankers and government authority were infected, isolated and even died. Private practitioners, clinics, and hospitals in suburban and rural areas were shut down due to the fear of infection. Moreover, the healthcare workers who have treated the patients and infected have been socially hatred and stigmatized. Besides, the deceased was even denied burial in the local graveyards which are basic human rights and, in most cases, handled by the government authority (TBS, 2020a). The price hike of the daily necessities was observed due to low supply and shopkeepers and suppliers stopped working fearing infection. Middle-income, lower-income and daily-wedge earners fell into a severe financial shortfall due to loss of jobs, incomes. With their last savings spent, they are plunged to be ultra-poor.
Considering the population density, environmental factors, social structure, cultural norms, healthcare capacity, and poverty in Bangladesh, it is certainly hard to lockdown millions of people. Besides, Bangladesh hosts the largest refugee camps in Cox's Bazar which is also about to embrace the COVID-19 pandemic, where, it will have catastrophic outcomes (Hopman et al., 2020). Despite the precautions taken by the government and other international aid bodies, on 14 May 2020, the Coronavirus cases were detected in Cox's Bazar Rohingya camps (TBS, 2020b). Moreover, miscommunication among the government ministries, policymakers, advisers and the country's apex trade organizations such as Federation of Bangladesh Chambers of Commerce and Industries (FBCCI) and the trade organization of the ready-made garment (RMG) manufacturers Bangladesh Garment Manufacturers and Exporters Association (BGMEA) led industry workers to return to the industrial districts due to the message of reopening at least two times first on 4th April and later on 11th April. To save their jobs, thousands of RMG workers travelled back to Dhaka and its surrounding districts on foot, in a truck, or covered vans without social distancing while ensuring further transmission. The district of Dhaka and its Upazilas Savar and Ashulia, Gazipur, Narayanganj, and Chittagong remained the highest infected clusters of COVID-19 infection (IEDCR, 2020). The latest extension period declared by the GoB is until 30 May 2020. Yet the RMG factories and other industrial operations resumed from 26 April 2020. Moreover, as the biggest Muslim festival Eid-Ul-Fitr approaches, mass people are gathering in the shopping centres despite the risk of spreading human transmission. It is utterly depicting the scenario of overlooking risks of the pandemic by unaware citizens while social anxiety and fear of the pandemic in concerned citizens. Both should be immediately dealt with by the Government along with the alliance groups with proper risk communication.
Moreover, the possibility of natural disasters such as tropical cyclones, flooding, and landslide preparedness, the rising of dengue fevers, and other infections are potentially overlooked. Furthermore, the consequences of disposal of used personal protective equipment (PPE) without proper treatment in the landfill will just arise more disease transmission and environmental disasters leaving the country at stake. In these circumstances, this study was therefore designed to analyze socioeconomic crisis and mental stress in resource-limited settings of Bangladesh due to the COVID-19 outbreak. This assessment might be useful for the government and policymakers of countries with a similar socioeconomic and cultural structure like Bangladesh.
2. Methodology
2.1. Study procedure
Considering the impact of COVID-19 outbreak in Bangladesh, this study identifies several relevant and possible items based on the country's situation analysis based on the print and electronic media, and literature review. We drafted the questionnaire considering demographic characteristics, individual mental health condition (MH), the health system in Bangladesh (HSB), governance and political issues (GPI), government decisions and impacts (GDI), socioeconomic issues (SEI), immediate emerging issues (IEI) and enduring emerging issues (EEI). A total of 49 items was considered in the drafted questionnaires to get people's perception of the COVID-19 outbreak in Bangladesh. Furthermore, expert consultation was considered to set and validate these 49 items.
Bangladesh has witnessed a boom in internet usage due to the fast-growing mobile internet and the government's push for digitalization. There are 99.428 million internet users in February 2020 according to the Bangladesh Telecommunication Regulatory Commission (BTRC, 2020). Google Form based online questionnaire was prepared to conduct the survey. An online database of target participants was prepared by reviewing the relevant websites and online social platforms of different groups in Bangladesh, considering their Bangladeshi citizenship, age above 18 years, current activities, occupation, social responsibilities, and engagement related to COVID19 response, socioeconomic sector, country-level planning, and policymaking. The prepared questionnaire with an introductory paragraph outlining the purpose of the study was shared through Email, Facebook, LinkedIn, and WhatsApp with selective and relevant people considering the purposive sampling method. The questionnaire survey was conducted from 28 March to 30 March 2020.
The inclusion of the respondents was different social groups like university faculty and scholars, Government officials, development worker or practitioner, doctors, engineers and technologists, youth leaders and students, businessmen and industry officials, banking and finance corporates, researchers, and others. The answers to the survey questionnaires are the voluntary basis. Data from 1082 respondents were collected via a nationwide online survey method, but following the removal of incomplete 16 questionnaires, 1066 were retained for this study. A five-point (1–5) Likert scale was employed to test whether each understands the statement descriptions that ranged from strongly disagree to strongly agree with the statements (Table S1).
2.2. Data analysis
Employing the Statistical Package for the Social Science (SPSS) v. 25.0, datasets were analyzed for Principal component analysis (PCA), one-way ANOVA and t-Test, multiple linear regression, and classical test theory (CTT). PCA is considered in this study to design a standardized scale to measure the socioeconomic crisis and mental stress in Bangladesh due to the COVID-19 outbreak. PCA is one of the population data reduction techniques that indicate each potentiality of variables and their significance level in a huge sample size. Before conducting the PCA, Kaiser-Maier -Olkin (KMO) and Bartlett's sphericity tests were applied to confirm the necessity of this analysis. The results of the KMO >0.5 (the KMO value was 0.903 in this research) and the significance of Bartlett's sphericity test at p < 0.01 verified our datasets to be fitted for the PCA (Islam et al., 2020). The number of factors chosen was based on the Kaiser's normalization principle, where the only factors with eigenvalues>1.0 were regarded. PCA results were used to find how many components are to be retained as well as how many items in each of those components are to be retained.
Furthermore, the test of association between each principal component and the demographic characteristic of the respondents were performed to see how people of different demographic status to perceive socioeconomic crisis and mental stress using the one-way ANOVA and t-test. Moreover, multiple linear regression was applied to estimate the statistically significant association between each component.
Classical Test Theory (CTT) analysis was applied to examine the reliability of each item according to the components to develop a composite score. Cronbach's alpha was employed to test the consistency and reliability of the factor loadings in this study (DeVellis, 1991). Descriptive statistics (e.g., Mean, Standard Deviation, Variance, Skewness, and Kurtosis) of respondents perceived socioeconomic crisis and mental stress was considered based on the developed composite score for the entire scale. The hierarchical cluster analysis (HCA) and Pearson's correlation coefficient was applied for identifying the relationships among all-composite items.
2.3. Ethics statement
The consent of participants was taken, and they remained anonymous. We have applied for the ethical clearance to the ethical clearance authority of Jahangirnagar University, Bangladesh. The studies involving participants of this questionnaire was reviewed by the Department of Public Health and Informatics and permit to conduct this study.
3. Results
3.1. Demographic information
According to the survey results, the ratio of male to female participants was 3:2, whereas the composition of age groups were 75.2% (18–30 years old), 16.7% (31–40 years old), 6.7% (41–50 years old), 1.1% (51–60 years old) and 0.3% (>60 years old), respectively. The young people responded more maybe because of their frequent access to the internet depending on the socioeconomic structure of Bangladesh. However, the average age of the participants (n = 1066) was 27.80 years (SD ± 10.05), and the participants had, on average, 12.5 years of formal education (SD ± 8.1). More than half of the participants were males (n = 661; 61.5%) and remaining (n = 405; 38.5%) females. Nearby, 60% of the youth group was mostly students as Bangladesh is a youth dividend country and they are the most dynamic groups of the society as well as dynamic on online platforms. The rest of the 40% were from various professions of doctors and health workers, civil service officials, non-government officials, teachers and scholars, policymakers, researchers, and businessmen (Table S1).
3.2. Relationships among demographic characteristics, socioeconomic components, and mental stress
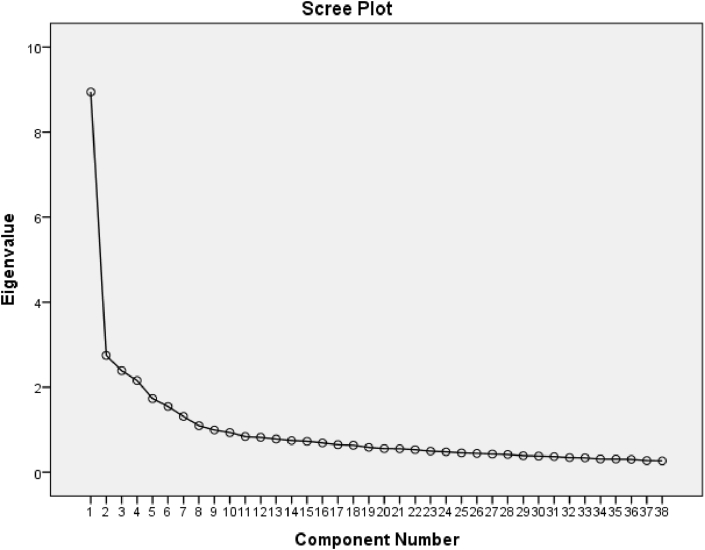
The scree plot (Figure 2) shows that a total of eight components can be retained (determined by components with eigenvalues greater than 1). Items with factor loadings (items loading on a component) less than 0.5 were omitted from the analysis and analysis repeated on the remaining items until a perfect scale was developed (Hair et al., 2014). We inspected the loadings of the items on each component and omitted a total of 12 items (have not met the 0.5-factor loading requirement) from the questionnaire. The scores of the items that loaded well on each component are represented in Table 1.
Figure 2.
Scree plots of the eigenvalues of PCA.
Table 1.
Retained items after principle component analysis.
| Sector | Items | PC1 | PC2 | PC3 | PC4 | PC5 | PC6 | PC7 | PC8 |
|---|---|---|---|---|---|---|---|---|---|
| Demographic characteristics | Age | 0.047 | -0.033 | -0.045 | 0.009 | -0.056 | 0.042 | -0.007 | 0.893 |
| Occupation | 0.019 | -0.027 | -0.001 | 0.057 | 0.031 | 0.027 | -0.017 | 0.883 | |
| Individual Mental health condition (MH) | I am most afraid of coronavirus recent outbreak in Bangladesh (MH1) | 0.112 | -0.005 | 0.029 | 0.24 | 0.758 | 0.074 | -0.057 | 0.034 |
| I am afraid of getting coronavirus (MH2) | 0.033 | 0.04 | 0.062 | 0.148 | 0.838 | 0.032 | -0.049 | 0.055 | |
| I am afraid of losing my life or my relatives' life due to this outbreak (MH3) | 0.055 | 0.063 | 0.076 | 0.13 | 0.788 | 0.074 | -0.091 | -0.06 | |
| All the news and numbers of COVID-19 in different media increasing my tension (MH4) | 0.117 | 0.114 | 0.097 | 0.049 | 0.624 | 0.086 | 0.039 | -0.046 | |
| Health system in Bangladesh (HSB) | There is a lack of trained doctors and health professional to deal with the COVID-19 (HSB1) | 0.651 | 0.03 | 0.099 | 0.011 | 0.034 | -0.014 | -0.022 | -0.042 |
| There is a lack of health facilities to combat the COVID-19 outbreak in Bangladesh (HSB2) | 0.74 | 0.079 | 0.103 | 0.214 | 0.092 | 0.215 | -0.079 | 0.05 | |
| There is a lack of health infrastructure to deal with COVID-19 (HSB3) | 0.745 | 0.068 | 0.144 | 0.202 | 0.099 | 0.111 | -0.056 | 0.026 | |
| There is a severe lack of bio-medical waste management facilities in Bangladesh (HSB4) | 0.683 | 0.11 | 0.138 | 0.21 | 0.055 | 0.229 | -0.077 | 0.022 | |
| There is a lack of COVID-19 testing facility in Bangladesh (HSB5) | 0.69 | 0.133 | 0.032 | 0.216 | 0.041 | 0.274 | -0.038 | -0.015 | |
| There is a lack of budget or financial support to response to this outbreak (HSB6) | 0.536 | 0.255 | 0.137 | -0.033 | 0.124 | -0.217 | 0.004 | 0.104 | |
| Governance and Political issues (GPI) | Bangladesh government can deal with this outbreak (GPI1) | -0.164 | 0.003 | -0.128 | 0.008 | -0.028 | 0.114 | 0.563 | -0.102 |
| Government is taking this outbreak seriously to deal with (GPI2) | -0.007 | -0.036 | -0.018 | -0.13 | -0.063 | 0.112 | 0.819 | 0.032 | |
| Government is taking proper decisions in the right time (GPI3) | -0.07 | -0.051 | 0.012 | -0.138 | -0.046 | -0.04 | 0.811 | 0.055 | |
| Government is involving other sector actors to combat the COVID-19 outbreak (GPI4) | 0.03 | -0.024 | 0.009 | -0.028 | -0.006 | 0.025 | 0.748 | -0.005 | |
| Government decisions and impacts (GDI) | Government need support from the people to reduce the impact of COVID-19 (GDI1) | 0.203 | -0.006 | 0.092 | 0.254 | 0.033 | 0.627 | 0.216 | -0.06 |
| Government need to formulate a policy and action plan and implement it immediately (GDI2) | 0.235 | 0.131 | 0.036 | 0.338 | 0.043 | 0.592 | 0.02 | -0.064 | |
| Shut down or lockdown of regular activities is a good decision to reduce the chance of infection of COVID-19 (GDI3) | 0.064 | 0.042 | 0.051 | 0.079 | 0.191 | 0.585 | 0.067 | 0.08 | |
| Shut down or lockdown or social distancing will have an economic and social impact in future (GDI4) | 0.051 | 0.362 | 0.333 | 0.005 | 0.04 | 0.513 | 0.082 | 0.094 | |
| The formal and informal business will be hampered (GDI5) | 0.075 | 0.376 | 0.387 | 0.003 | 0.023 | 0.543 | -0.032 | 0.14 | |
| Socio-economic issues (SEI) | Most of the poor people living in urban areas have to leave due to not having any options for income (SEI1) | 0.081 | 0.586 | 0.155 | 0.051 | 0.034 | 0.203 | 0.045 | -0.01 |
| Many people will lose their livelihood/jobs at a time (SEI2) | 0.016 | 0.681 | 0.192 | 0.171 | 0.056 | 0.163 | -0.053 | 0.101 | |
| There will be less supply of basic goods/products for daily use (SEI3) | 0.096 | 0.734 | 0.154 | 0.084 | 0.044 | -0.085 | 0 | -0.134 | |
| Price of most of the basic products will be higher than usual (SEI4) | 0.11 | 0.665 | 0.116 | 0.073 | 0.006 | 0.11 | -0.114 | -0.048 | |
| Poor people will suffer food and nutritional deficiency (SEI5) | 0.128 | 0.576 | 0.211 | 0.127 | 0.002 | 0.365 | -0.075 | -0.088 | |
| There is a chance of social conflict due to this outbreak (SEI6) | 0.119 | 0.62 | 0.128 | 0.12 | 0.126 | -0.103 | 0.016 | 0.051 | |
| Immediate emerging issues (IEI) | There is a chance of community transmission of COVID-19 in Bangladesh (IEI1) | 0.099 | 0.141 | 0.12 | 0.688 | 0.15 | 0.054 | -0.034 | 0.093 |
| A huge number of people will be infected (IEI2) | 0.072 | 0.141 | 0.13 | 0.701 | 0.279 | -0.014 | -0.084 | 0.03 | |
| There is a chance of not detecting most of the infected patients due to lack of health facilities leads to undermining the actual infected case (IEI3) | 0.218 | 0.13 | 0.144 | 0.661 | 0.066 | 0.23 | -0.185 | 0.017 | |
| There is a chance to increase in the number of death for not having proper health facilities (IEI4) | 0.233 | 0.105 | 0.244 | 0.694 | 0.125 | 0.228 | -0.092 | -0.027 | |
| Lack of bio-medical waste management facilities in Bangladesh will create more problem (IEI5) | 0.234 | 0.111 | 0.269 | 0.581 | 0.162 | 0.201 | -0.037 | -0.048 | |
| Enduring emerging issues (EEI) | If any disaster (flood, cyclone etc.) occur after the COVID-19 situation then it will create a double burden to the country (EEI1) | 0.199 | 0.123 | 0.548 | 0.299 | 0.056 | 0.215 | -0.073 | -0.013 |
| There is a chance of severe food scarcity due to these events (COVID-19 + Disasters) in the country (EEI2) | 0.165 | 0.227 | 0.648 | 0.147 | 0.103 | -0.119 | 0.028 | -0.14 | |
| High possibility of huge economical loss (EEI3) | 0.127 | 0.187 | 0.805 | 0.099 | 0.094 | 0.159 | -0.048 | 0.03 | |
| High possibility of increasing the poverty level (EEI4) | 0.091 | 0.296 | 0.732 | 0.169 | 0.088 | 0.123 | -0.039 | 0.003 | |
| High possibility of severe socio-economic and health crisis (EEI5) | 0.153 | 0.265 | 0.699 | 0.254 | 0.044 | 0.168 | -0.071 | 0.018 | |
| Varimax Rotation Sums of Squared Loadings | Eigenvalues | 3.275 | 3.265 | 3.126 | 3.012 | 2.58 | 2.436 | 2.389 | 1.736 |
| % of Variance | 8.852 | 8.824 | 8.45 | 8.14 | 6.974 | 6.584 | 6.456 | 4.692 | |
| Cumulative % | 8.852 | 17.676 | 26.125 | 34.265 | 41.239 | 47.823 | 54.28 | 58.971 |
Bold denotes significance at >0.5.
The loading scores were demarcated into three groups of weak (0.50–0.30), moderate (0.75–0.51), and strong (>0.75) respectively (Liu et al., 2003; Bodrud-Doza et al., 2016; Islam et al., 2017). The PC1 (First) elucidated 8.85% of the variance as it encompassed a confidence level of moderate positive loading, depicts the weakness of healthcare system in Bangladesh including lack of trained doctors and health professionals to deal with the COVID-19 (HSB1: 0.651); lack of health facilities to combat the COVID-19 outbreak in Bangladesh (HSB2: 0.74); lack of health infrastructure to deal with COVID-19 (HSB3:0.745); severe lack of biomedical waste management facilities in Bangladesh (HSB4: 0.683); lack of COVID-19 testing facility in Bangladesh (HSB5:0.69); and lack of budget or financial support to respond to this outbreak (HSB6:0.536). All the elements of the statement (HSB) showed moderate loading score revealing the fragility of the healthcare system of Bangladesh in dealing with COVID-19 pandemic, for instance very low ratio of intensive care unit (ICU) beds to population, limited or centralized COVID-19 testing facilities along with bias in selecting the test candidates, low test rate, lack or a substandard quality of personal protective equipment (PPE) for the caregivers, lack of institutional isolation units, and very poor coordination in health management systems, etc.
Afterwards, the PC2 (Second) elucidated 8.82% of the total variance, and it was moderately positive loaded with the socioeconomic issues (SEI), including the risk of poor people from urban areas forced to temporary migration while having no options for income along with the chance of inducing social conflicts due to this outbreak; restriction of basic supplies including foods; price hikes of commodities, losing jobs (SEI1-6: 0.576–0.734). However, weak but positively loaded socioeconomic issues such as shut down or lockdown or social distancing might have an economic and social impact in the future (GDI4; 0.362) along with the small formal and informal business will also be hampered. For example, small business will lose their regular customers due to shutting down their business (GDI5:0.376).
The PC3 (Third) explained 8.45% of the variance which was strong positive loaded with enduring emerging issues (EEI: 0.548 to 0.805). The major EEIs were stated here as occurring any further natural disasters such as flood and tropical cyclone (EEI1: 0.548) and their burden on food security (EEI2: 0.648), mounted economic loss (EEI3: 0.805) due to damages of business and industrial chains both locally and globally, these may put further stress as elevating poverty level (EEI4: 0.732) followed by a chance of inducing severe socioeconomic and health crisis (EEI5: 0.699).
Furthermore, PC4 (Fourth) elucidated 8.14% of the variance and was moderate positive loaded of immediate emerging issues (IEI: 0.581 to 0.701). This sector covered very important elements of COVID-19 pandemic in Bangladesh including the chance of community transmission (IEI1: 0.688), huge infection potentials (IEI2: 0.701), but this huge number of infection might not be reported due to lack of health facilities which ultimately undermine the actual cases (IEI3: 0.661), the lack of health facilities further trigger the chance of a high number of deaths due to infection (IEI4: 0.694), and the poor facility of biomedical waste management might be a risk factor for further virus transmission (IEI5: 0.581) through an unconventional pathway in Bangladesh.
While, PC5 (Fifth) explained 6.97% of the total variances, and it showed strong positive loadings with mental health issues (MH: 0.624 to 0.838) such as people are afraid of coronavirus recent outbreak in Bangladesh (MH1), fear of getting coronavirus infection (MH2), and afraid of losing life or relatives' life due to this outbreak (MH3) (MHI1-3:0.758-0.838); and a moderate positive loading of all the news and numbers of COVID-19 in different media increasing tension and anxiety (MH4: 0.624). This result indicates the mental health burden in Bangladesh due to COVID-19. Thus the question arises: What should be the role of the GoB during the global pandemic to safeguard its citizens?
The following PC6 (Sixth) might produce some indication regarding the question, which accounted for 6.58% of the variance. The PC6 was moderate but positively loaded of the government decision and impacts issues (GDI: 0.513 to 0.627), including the government need supports from the people to reduce the impact of COVID-19 (GDI1: 0.627) and also need to formulate a strong policy and action plan, and implement it immediately (GDI2: 0.592); also moderate positively loaded of the government decision and impact issues (GDI3-5: 0.513–0.585). These decisions were declared without a proper strategy of implementation and exit plan that might lead to huge mismanagement during the partial lockdown period in Bangladesh. This lack of coordination in policy formulation further linked with the PC7 (Seventh), elucidated 6.46% of the total variances and were strong positive loading of the government and political issues (GPI: 0.563 to 0.819). The loading elements were as follows: the capacity of dealing with the pandemic (GPI1: 0.563); seriousness in dealing with it (GPI2: 0.819); timely decision taking (GPI3: 0.811); involvement of other stakeholders properly (GPI4: 0.748). These are very crucial elements in terms of COVID-19 pandemic management, therefore failing to address this issue might produce huge aftermath. Finally, the PC8 (eighth) elucidated 4.692% of the total variances and strongly loaded with demographic characteristics such as age (0.893) and occupation (0.883).
3.3. Professional risk groups of socioeconomic crisis and mental stress
Results of t-Test and one-way ANOVA showed that all PCs exhibited a strong association among them except for PC7 (Governance and Political issues) and PC8 (demographic characteristics) (Table 2). However, a One-way ANOVA test between 35 items and the age and occupation of the participants were conducted which is presented in Table S2 and S3. A strong association between age and MH3, MH4, and EEI2 were found which represents that different age groups are afraid of getting coronavirus and losing their lives due to this outbreak. Also, climate change vulnerability and possible dengue outbreak in the country are creating mental stress among different age groups. Furthermore, a strong association between occupation and HSB1, SEI3, SEI5, and EEI2 represents that there is lack of trained health professional in the country, a supply of basic products will be reduced due to lockdown and fewer supplies, and poor people will suffer food and nutritional deficiency due to loss of livelihood. Also, different professions such as doctors, police, and banker are at higher risk of infection.
Table 2.
Test of association between each component and the demographic characteristic using T-test.
| t | df | Sig. (2-tailed) | Mean Difference | 95% Confidence Interval of the Difference |
||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| PC1 | 4.926 | 36 | 0 | 0.18881 | 0.1111 | 0.2665 |
| PC2 | 5.215 | 36 | 0 | 0.19492 | 0.1191 | 0.2707 |
| PC3 | 5.066 | 36 | 0 | 0.18757 | 0.1125 | 0.2627 |
| PC4 | 5.006 | 36 | 0 | 0.18278 | 0.1087 | 0.2568 |
| PC5 | 3.622 | 36 | 0.001 | 0.13649 | 0.0601 | 0.2129 |
| PC6 | 4.763 | 36 | 0 | 0.15951 | 0.0916 | 0.2274 |
| PC7 | 1.326 | 36 | 0.193 | 0.05481 | -0.029 | 0.1387 |
| PC8 | 1.472 | 36 | 0.15 | 0.05159 | -0.0195 | 0.1227 |
3.4. Strategy, actions and individual role in public wellbeing and socioeconomic crisis
The multiple linear regression model was applied to estimate the individual mental health condition (MH) performance in model 1 (Table 3). The results indicate that the independent variable MH2 and IEI3 was statistically significant and had a positive influence on MH1 (dependent Variable). From this model, it was found that coronavirus outbreak, lack of testing capacity undermining the actual cases with a lack of health facilities are inducing individual mental stress.
Table 3.
Estimated model of multiple regression.
| Model-1: Dependent Variable: MH1 (R = 0.991, R Square = 0.975) | |||||||
|---|---|---|---|---|---|---|---|
| Unstandardized Coefficients |
Standardized Coefficients |
t | Sig. | 95.0% Confidence Interval for B |
|||
| B | Std. Error | Beta | Lower Bound | Upper Bound | |||
| (Constant) | -0.009 | 0.02 | -0.453 | 0.669 | -0.06 | 0.042 | |
| MH2 | 0.897 | 0.055 | 0.976 | 16.179 | 0 | 0.754 | 1.039 |
| IEI3 | 0.17 | 0.065 | 0.157 | 2.597 | 0.048 | 0.002 | 0.338 |
|
Model-2: Dependent Variable: HSB6 (R=1, R Square= 1) | |||||||
| (Constant) | 0.085 | 0 | 3087.118 | 0 | 0.084 | 0.085 | |
| HSB1 | 0.86 | 0 | 0.893 | 2436.454 | 0 | 0.856 | 0.865 |
| GDI1 | -0.401 | 0 | -0.392 | -1583.19 | 0 | -0.404 | -0.397 |
| SEI1 | 0.73 | 0.001 | 0.633 | 1256.524 | 0.001 | 0.723 | 0.738 |
| SEI5 | -0.497 | 0.001 | -0.51 | -863.253 | 0.001 | -0.504 | -0.489 |
| GPI3 | -0.06 | 0 | -0.082 | -324.713 | 0.002 | -0.062 | -0.057 |
| HSB2 | -0.037 | 0 | -0.041 | -96.705 | 0.007 | -0.042 | -0.032 |
|
Model-3: Dependent Variable: GDI1 (R=1, R Square= 1) | |||||||
| (Constant) | 0.087 | 0 | 364.433 | 0.002 | 0.084 | 0.09 | |
| GDI2 | 0.712 | 0 | 0.707 | 2025.783 | 0 | 0.707 | 0.716 |
| GPI2 | 0.153 | 0 | 0.214 | 560.211 | 0.001 | 0.149 | 0.156 |
| SEI6 | -0.903 | 0.002 | -0.883 | -500.629 | 0.001 | -0.926 | -0.88 |
| SEI3 | 0.503 | 0.001 | 0.625 | 376.743 | 0.002 | 0.486 | 0.52 |
| GDI3 | 0.081 | 0 | 0.069 | 313.709 | 0.002 | 0.077 | 0.084 |
| EEI5 | 0.023 | 0 | 0.025 | 74.962 | 0.008 | 0.019 | 0.026 |
|
Modle-4: Dependent Variable: SEI5 (R=0.997, R Square= 0.993) | |||||||
| (Constant) | -0.076 | 0.014 | -5.529 | 0.005 | -0.114 | -0.038 | |
| SEI1 | 0.997 | 0.049 | 0.841 | 20.43 | 0 | 0.862 | 1.133 |
| GDI2 | 0.304 | 0.045 | 0.287 | 6.731 | 0.003 | 0.178 | 0.429 |
| EEI1 | 0.225 | 0.049 | 0.195 | 4.585 | 0.01 | 0.089 | 0.361 |
|
Model-5: Dependent Variable: IEI2 (R=1, R Square= 1) | |||||||
| (Constant) | -0.05 | 0 | -1261.6 | 0.001 | -0.05 | -0.049 | |
| IEI1 | 1.07 | 0 | 0.956 | 10993.03 | 0 | 1.068 | 1.071 |
| MH4 | 0.274 | 0 | 0.229 | 600.686 | 0.001 | 0.269 | 0.28 |
| GDI3 | -0.089 | 0 | -0.066 | -1241.36 | 0.001 | -0.09 | -0.088 |
| EEI4 | 0.042 | 0 | 0.042 | 887.841 | 0.001 | 0.041 | 0.043 |
| HSB1 | -0.023 | 0 | -0.021 | -422.45 | 0.002 | -0.024 | -0.022 |
| MH3 | 0.014 | 0 | 0.016 | 41.82 | 0.015 | 0.01 | 0.019 |
|
Model-6: Dependent Variable: EEI5 (R=0.996, R Square= 0.993) | |||||||
| (Constant) | -0.001 | 0.011 | -0.045 | 0.966 | -0.03 | 0.029 | |
| EEI4 | 0.623 | 0.076 | 0.645 | 8.23 | 0 | 0.428 | 0.818 |
| EEI1 | 0.46 | 0.094 | 0.383 | 4.889 | 0.005 | 0.218 | 0.702 |
For model 2, the results indicate that HSB1 and SEI1 had a positive impact whereas GDI1, SEI5, GPI3, HSB2 had a negative impact on HSB6. From this model, it is found that lack of budget or financial support has created constrained to COVID-19 response and created a scarcity of trained health professionals, which enforced to shut down the regular activities in the urban areas and poor people lose their income options. Due to this, people are suffering food and nutritional deficiency and the government is not getting proper support from the people to reduce the impact of the COVID-19 outbreak. Not having a proper response plan with the budget was not a good decision of the government, which created a lack of health facilities to combat this outbreak in Bangladesh.
For model 3, GDI2, GPI2, SEI6, SEI3, GDI3, and EEI5 were statistically significant and had a significant effect on GDI1. This model depicts the role of general people to assist the implementation of government actions against COVID-19 in Bangladesh such as the implementation of proper lockdown and social distancing, relief supports to the poor people, preventing potential socioeconomic burden, and ensuring the safeguard of the country.
For model 4, GDI2 and EEI1 were statistically significant and had a significant effect on SEI5. This means a strong coordinated strategy is warranted to tackle such unprecedented events as Bangladesh is one of the vulnerable countries in the world. Especially, the months from April to September is especially important in terms of natural disaster vulnerability in Bangladesh.
For model 5, IEI1, MH4, GDI3, EEI4, HSB1, MH3 were statistically significant and had a substantial effect on IEI2. This model can be suitable to explain the most potential risk factors for the negative impacts of COVID-19 pandemic in Bangladesh including mental health and poverty.
For model 6, EEI4 and EEI1 were statistically significant and had a significant effect on EEI5. This unprecedented chain of events could be a potential threat to the COVID-19 response and rehabilitation efforts by the GoB. However, there was significant evidence (R2= >0.97) that the independent variables in the proposed models adequately described in the influence of dependent variables (Table 3).
3.5. Descriptive overview of governance, perceived socioeconomic crisis and mental stress
CTT analysis was applied to examine the reliability of each item according to the components to develop a composite score. The Cronbach's alpha values varied from 0.719 to 0.839 (>0.70), indicating that a composite score for the entire scale can be generated to have a descriptive overview of respondents' perceived mental stress, and socioeconomic crisis (Table 4). On the scale of 1–5 (strongly disagree to strongly agree), for an individual mental health condition (MH), it was found that the composite mean is 4.04 ± 0.03 which represents that the participants are mentally stressed and afraid of COVID-19 outbreak in Bangladesh (Table 5). The source of such stresses and fears might be linked to factors such as fragile healthcare systems with poor management, low test rates, weak medical infrastructures, weakness in planning, and implementation of the COVID-19 response strategy by the GoB. The following further sectors results indicate the correctness of the claims as to the case of the health system in Bangladesh, with a mean of 4.47 ± 0.02 represents that the health systems in Bangladesh are very fragile to combat the COVID-19 spread in Bangladesh. The weak coordination is consenting to government political issues (GPI), with a mean of 2.63 ± 0.03 represents that the government is not taking a proper decision at the right time to reduce the effect of this pandemic. In summary, respondents had negative viewpoints about the government is taking a proper decision in the pandemic.
Table 4.
Cronbach's alpha value for composite score development.
| Cronbach's Alpha | N of Items | |
|---|---|---|
| Individual Mental health condition (MH) | 0.79 | 4 |
| Health system in Bangladesh (HSB) | 0.783 | 6 |
| Governance and Political issues (GPI) | 0.742 | 4 |
| Government decisions and impacts (GDI) | 0.719 | 5 |
| Socio-economic issues (SEI) | 0.78 | 6 |
| Immediate emerging issues (IEI) | 0.821 | 5 |
| Enduring emerging issues (EEI) | 0.839 | 5 |
Table 5.
Descriptive overview of respondents on psychosocial, and socio-economic crisis due to COVID-19 pandemic in Bangladesh.
| Mean | Std. Error of Mean | Median | Mode | Std. Deviation | Variance | Skewness | Kurtosis | Minimum | Maximum | |
|---|---|---|---|---|---|---|---|---|---|---|
| Individual Mental health condition (MH) | 4.04 | 0.03 | 4.25 | 5 | 0.83 | 0.69 | -1.04 | 0.94 | 1 | 5 |
| Health system in Bangladesh (HSB) | 4.47 | 0.02 | 4.67 | 5 | 0.61 | 0.37 | -2.28 | 7.93 | 1 | 5 |
| Governance and Political issues (GPI) | 2.63 | 0.03 | 2.50 | 2.25 | 0.91 | 0.83 | 0.29 | -0.38 | 1 | 5 |
| Government decisions and impacts (GDI) | 4.56 | 0.02 | 4.60 | 5 | 0.51 | 0.26 | -2.70 | 12.53 | 1 | 5 |
| Socio-economic issues (SEI) | 4.28 | 0.02 | 4.33 | 5 | 0.62 | 0.39 | -1.30 | 2.93 | 1 | 5 |
| Immediate emerging issues (IEI) | 4.44 | 0.02 | 4.60 | 5 | 0.61 | 0.37 | -1.75 | 5.11 | 1 | 5 |
| Enduring emerging issues (EEI) | 4.49 | 0.02 | 4.60 | 5 | 0.58 | 0.33 | -1.49 | 3.28 | 1 | 5 |
For government decisions and impacts (GDI), with a mean of 4.56 ± 0.02 represent that the government's decision to lock down the activities was right. Also, the lockdown of activities created economic impacts. Despite the huge future economic burden, the GoB took the challenge to implement partial lockdown in the country. However, this lockdown for a long time might not be carried out rather it become loosen day by day due to many socioeconomic factors and pressure from the industrial sectors in Bangladesh. With a mean value of 4.28 ± 0.02 for the socioeconomic issues (SEI) that represents the poor and marginalized people will suffer a lot due to the COVID-19 outbreak in Bangladesh. Besides, with a mean value of 4.44 ± 0.02 for the immediate emerging issues (IEI), it can be summarized as: the number of infections and death will increase due to the fragile heal care system and improper biowaste management. Some mismanagement in the industrial stakeholders and lack of coordination among the responsible national COVID-19 response committee already happened in Bangladesh. Furthermore, with a mean value of 4.49 ± 0.02 for enduring emerging issues (EEI), there is a change of sever health and socioeconomic crisis if climate change-induced disasters and dengue outbreak happen in the same year. For instance, the early flash flood might bring sufferings for the poor people and farmers of Bangladesh. Which in turn, puts excessive stress on the food security issue of the country.
The individual mental health (MH) had a statistically positive significant correlation with other issues (MH vs HSB, SEI, IEI, GDI, EEI) and their correlation values ranged from 0.205 to 426 while MH had a statistically negative significant correlation with GPI (r = -0.117, p < 0.01) (Table 6). The GPI had a statistically negative relationship with other issues (GPI vs SEI, IEI, EEI, MH) and their correlation values varied from -0.10 to -0.225 whereas the GPI had a significant positive relationship with GDI (r = 0.083, p < 0.01). The moderate significant correlation was observed between pairs e.g., SEI vs EEI (r = 0.561, p < 0.01), and EEI vs IEI (r = 0.527, p < 0.01). The weak positive significant correlation was identified between pairs such as HSB vs GDI (r = 0.384, p < 0.01), EEI vs GDI (r = 0.482, p < 0.01), and SEI vs HSB (r = 0.349, p < 0.01). These results indicate a diversified nature of the peoples' perception regarding the COVID-19 management and response in Bangladesh.
Table 6.
Correlation matrix of people's perception.
| MH | HSB | GPI | GDI | SEI | IEI | EEI | |
|---|---|---|---|---|---|---|---|
| MH | 1 | ||||||
| HSB | .254∗∗ | 1 | |||||
| GPI | -.117∗∗ | -.148∗∗ | 1 | ||||
| GDI | .235∗∗ | .384∗∗ | .083∗∗ | 1 | |||
| SEI | .205∗∗ | .349∗∗ | -.100∗∗ | .447∗∗ | 1 | ||
| IEI | .426∗∗ | .465∗∗ | -.225∗∗ | .475∗∗ | .390∗∗ | 1 | |
| EEI | .267∗∗ | .417∗∗ | -.124∗∗ | .482∗∗ | .561∗∗ | .527∗∗ | 1 |
Correlation is significant at the 0.01 level (2-tailed).
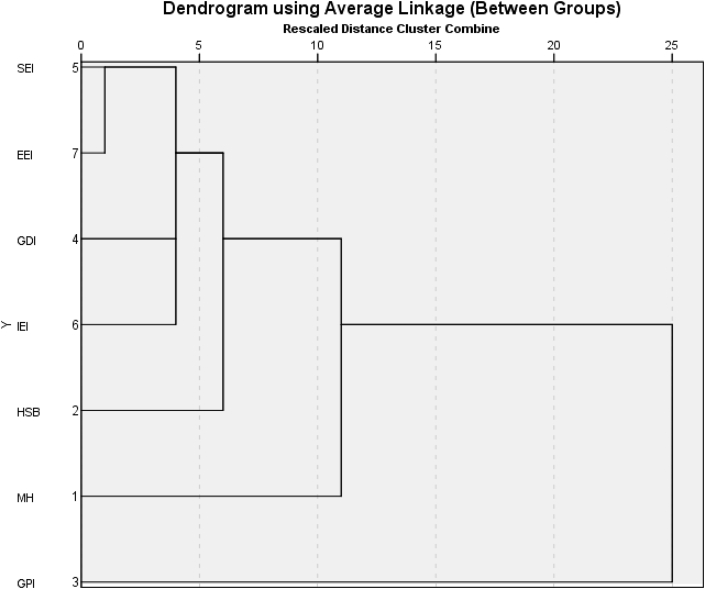
Further, the cluster analysis detected the total status of regional variations, and how socioeconomic and environmental crises influence further mental stress development (Figure 3). All the parameters were classified into two major groups: cluster-1(C1), and cluster-2 (C2). C1 composed of socioeconomic issues (SEI), enduring emergency issues (EEI), government decision and impact issue (GDI), immediate emergency issue (IEI), the health system in Bangladesh (HSB) and individual mental health (MH). C2 consisted of government political issues (GPI). It can be concluded that all the issues depend on governance and political aspects in Bangladesh.
Figure 3.
Dendrogram showing the clustering of people's perceptions on COVID-19 outbreak in Bangladesh.
4. Discussion
4.1. Strengthening healthcare system
The remarkable interferences and ventures in public health by the governmental authority can control a pandemic where good governance and good functional policy in the healthcare system exists. Tight lockdown, mass people quarantine, increased testing facilities, government stimulus packages, faster policy intervention and implementation have prevented COVID-19 virus from spreading transmission between humans in China, Hong Kong, South Korea, Vietnam, Taiwan, Singapore well to date, despite initial cases (Anderson et al., 2020; Zhang et al., 2020). The experiences gathered from across the globe, indicates that the patient-management decisions, early diagnosis, and rapid testing and detection are urgent in COVID-19 pandemic management (Binnicker, 2020). There is no doubt that the number of infections and death from COVID-19 increases where a fragile and corrupt healthcare system exists.
So far, the fatality rate due to the COVID-19 is 1.52% in Bangladesh (WHO, 2020a, WHO, 2020b). However, the reported case numbers are given by the Bangladesh Government certainly underestimates the actual number of infected persons given the shortages or unavailability of test kits (Ebrahim et al., 2020). The laboratory facilities for testing are only accessible in the urban areas and 33 testing laboratories are still a few numbers in a country of 165 million population. The fear of getting the virus-infected along with the administrative procedure of testing and reluctance of other private clinics and hospitals to admit patients is a sign of weak governance in the healthcare of Bangladesh. In this scenario, other critical care patients are denied admittances, negligence, and often left to die without treatments. After the detection of the first COVID-19 case in Bangladesh, at least 929 + death cases having COVID-19 like symptoms were reported in the different national daily newspapers until 10 May 2020, which is 3 times higher than the reported deaths by the GoB. This indicates a serious level of community transmission is occurring in Bangladesh.
Decentralization of testing and strengthening treatment facilities are therefore required for the healthcare systems to combat the pandemic and the treatment should reach in rural areas. The urban-rural disparity in the facilities should be reduced as the rural practitioners and healthcare workers are equally at the risk of the pandemic. Moreover, the administrative procedure of the deceased to burial put another confusion and religious fear in the minds of the common people as the victims to COVID-19 are buried without Muslim funeral procedures of baths and the presence of family members and relatives. In this scenario, it is imperative to deal with the peoples' fear and anxiety by the government. Proper information should be circulated to get the people out of confusion. Media partnerships should be created to prevent societal fear (Hopman et al., 2020).
4.2. Taking intervention in mental stress and social conflict counselling
By quick administrative action and raising awareness in individuals for social-distancing and stringent steps were taken to manage the spread of disease by cancelling thousands of activities of social gatherings in offices, clubs, classrooms, reception centres, transport services, travel restrictions, contact tracing leaving the countries in complete lockdown (Hopman et al., 2020; Cohen and Kupferschmidt, 2020). Yet weeks of being in isolation, quarantine, physical trauma creates further loneliness and anxiety and issues of a mental health crisis that have been mostly overlooked. At the individual level and the government level, proper risk communication is required. Special attention should be given to combat child and women abuse. Necessary action should be proposed for the post-recovery phase, suicide prevention, and mental health management (Duan and Zhu, 2020; Gunnell et al., 2020; Mamun et al., 2020). Several cases of suicide were reported due to the fear and stress of COVID-19 infection symptoms, job-loss, sudden fall to extreme poverty, economic crisis, hunger, and unable to cope with social hatred. This kind of traumatic situation should be dealt with immediately by the government through proper community counselling.
Small children are highly vulnerable to abuse if parent(s)/caregivers are quarantined. Moreover, with limited or no outdoor activities and no schooling makes them mentally stressed. Moreover, to maintain family hygiene in the pandemic, the burden just increases on the women along with her regular household activities. Likewise, it escalated family conflicts between men and women arising from physical and mental assault towards women. Students are also vulnerable to mental pressure as their education life is extended and posing an uncertain future caused by the pandemic. The Shutdown of all educational institutions may increase hatred and mentally depressed young which should be dealt with proper plans.
4.3. Backing up emergency service providers
In any successful governance, a competent early warning system and efficient analysis of the situation, interpretation, sharing, and use of relevant evidence and epidemiological knowledge is required (Gu and Li, 2020). In particular, epidemiological outcomes need to be informed on time so that they can be accurately evaluated and explained to the general people (Xiao and Torok, 2020). The low quality and an inadequate number of personal protective equipment (PPE) along with insufficient training to use PPE caused doctors and healthcare professionals infected across the country. Already 11% of the doctors and healthcare workers are infected with COVID-19. Moreover, members of Bangladesh police, armed forces, and rapid action battalion (RAB) along with other security agencies who have been jointly working to ensure social distancing across the country are at high risk of being infected. Already 914 members of security forces have been infected with several reported deaths. Besides, bankers, RMG factory workers, businessmen, shop keepers, daily wedge earners are at higher risk of infection.
4.4. Inclusive plan to protect the vulnerable communities amidst the pandemic and upcoming environmental disasters
Societies where underserved communities exist, they strongly fear government information and politics. The ultra-poor are often being left out of the relief program during the disasters. Public risk communications are therefore needed to let people know about the mental and social risk of elderly, children, people with special needs, disabled as they are susceptible to mental stress, and other disasters.
It should be mentioned here that government plans on pandemic control, risk alleviation, and social management must be as inclusive as possible. An inclusive commitment means responding to COVID-19 pandemic in a way that is sensitive to the most vulnerable communities, including ultra-poor, daily wedge earners, homeless people, unemployed, indigenous communities, immigrant communities, people with disabilities, and certain frontline healthcare workers and emergency responders. Prison centres, nursing homes, orphanages, homeless shelters, and refugee camps can be a focus for disease outbreaks; people in such settings often have inadequate access to basic healthcare and comorbidities that increase the risk of serious illness (Berger et al., 2020). Moreover, the government should take proper strategy to protect the agricultural farmers and their crops amidst the pandemic to strengthen the food security of the country and maintain the supply chain to consumers.
As a country of climate change vulnerability, there might be some additional risk factors of occurring natural disasters such as tropical cyclones, flash floods which may add further tolls for the country. Moreover, the shutdown of all kinds of business centres except groceries, pharmacies, and other daily necessities puts stress on the country's economy and financial burden. With RMG factories and other industrial production resumed from 26 April, another infectious outbreak of dengue along with critical level community transmission of coronavirus might have a cumulative/synergistic negative impact on the public health systems in Bangladesh. In this situation factory operation should be maintained with minimum social distancing; water, sanitation, and hygiene (WASH) kit; occupational health and safety guideline, and good healthcare management. BGMEA should be the monitoring body and draw safety protocols to protect the workers while maintaining public safety.
5. Concluding remarks
This perception-based study tried to visualize the mental stresses as well as the socioeconomic crisis due to the COVID-19 pandemic in Bangladesh. It can be undoubtedly established that mental stress due to the COVID-19 is because of the lockdown without ensuring the fundamental needs of the vulnerable ones. The weak governance in the healthcare systems and the facilities further exacerbates the general public's anxiety. The urban COVID-19 testing facilities, long serial to be tested, lowest facilities in the dedicated hospital units for COVID-19 patients hampered the other critical patients to get healthcare services. It was a good decision by the government to recruit 6000 doctors and nurses to combat this pandemic. The government needs to take decisions to implement testing facilities for both public and private clinical laboratories all over Bangladesh. As with the COVID-19 outbreak, other critical care patients and infectious diseases such as dengue testing are being affected and patients are being deprived. It is also timely steps that the government starts measures on dengue testing as well to all the COVID-19 patients.
However, numerous mental wellbeing and socioeconomic factors that have been identified in the study are already threatening public with fear and anxiety can be considered for the upcoming threat due to COVID-19 in Bangladesh are as follows; risk of community transmission, healthcare capacity, governance coordination and transparency, relief for the low-income population, proper biomedical waste management through incineration, and preparation for the possible natural disasters. The recommendations collected in the perception study can be summarized as to increase COVID-test rate and medical facilities. The strengthening and decentralization of the COVID-19 medical facilities and treatment are especially important for all 64 districts as the disease spread to entire Bangladesh. Besides, proper risk assessment and dependable risk communications, multi-sectoral management taskforce development, take care of biomedical waste, ensure basic supports to the people who need, and good governance was suggested to reduce mental and social stress causing a socioeconomic crisis of COVID-19 outbreak in Bangladesh. Finally, this assessment process could help the government and policymakers to judge the public perceptions in an emergency situation to deal with COVID-19 pandemic in densely populated lower-middle-income countries like Bangladesh.
Declarations
Author contribution statement
M. Shammi: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
M. Bodrud-Doza: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
A. R. M. Towfiqul Islam: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
M. Mostafizur Rahman: Conceived and designed the experiments; Performed the experiments; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors would like to acknowledge all the frontline doctors fighting this pandemic and all the researchers cited in the references. Also, the authors are gratefull to all the participants in this study.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
Supplementary Tables R1
References
- Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addiction. 2020 doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BTRC . 2020. Internet Subscribers in Bangladesh February, 2020.http://www.btrc.gov.bd/content/internet-subscribers-bangladesh-february-2020 [Google Scholar]
- Berger Z.D., Evans N.G., Phelan A.L., Silverman R.D. Covid-19: control measures must be equitable and inclusive. BMJ. 2020;368:m1141. doi: 10.1136/bmj.m1141. [DOI] [PubMed] [Google Scholar]
- Binnicker M.J. Emergence of a novel coronavirus disease (COVID-19) and the importance of diagnostic testing: why partnership between clinical laboratories, public health agencies, and industry is essential to control the outbreak. Clin. Chem. 2020 doi: 10.1093/clinchem/hvaa071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodrud-Doza M., Islam A.R.M.T., Ahmed F., Das S., Saha N., Rahman M.S. Characterization of groundwater quality using water evaluation indices, multivariate statistics and geostatistics in central Bangladesh. Water Sci. 2016;33(1):19–40. [Google Scholar]
- Cohen J., Kupferschmidt K. Countries test tactics in ‘war’ against COVID-19. Science. 2020;367(6484):1287–1288. doi: 10.1126/science.367.6484.1287. [DOI] [PubMed] [Google Scholar]
- DeVellis R.F. SAGE Publications; Newbury Park, CA: 1991. Scale Development: Theory and Applications. [Google Scholar]
- Duan L., Zhu G. Psychological interventions for people affected by the COVID-19 epidemic. Lancet Psychol. 2020;7(4):300–302. doi: 10.1016/S2215-0366(20)30073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebrahim S.H., Ahmed Q.A., Gozzer E., Schlagenhauf P., Memish Z.A. Covid-19 and community mitigation strategies in a pandemic. BMJ. 2020;368:m1066. doi: 10.1136/bmj.m1066. [DOI] [PubMed] [Google Scholar]
- Gates B. Responding to Covid-19 — a once-in-a-Century pandemic? N. Engl. J. Med. 2020:2003762. doi: 10.1056/NEJMp2003762. [DOI] [PubMed] [Google Scholar]
- Gu E., Li L. Crippled community governance and suppressed scientific/professional communities: a critical assessment of failed early warning for the COVID-19 outbreak in China. J. Chin. Govern. 2020:1–18. [Google Scholar]
- Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N.…Yip P.S.F. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychol. 2020 doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J.F., Black W.C., Babin B.J., Anderson R.E. Pearson Education limited; 2014. Multivariate Data Analysis. [Google Scholar]
- Hopman J., Allegranzi B., Mehtar S. Managing COVID-19 in low- and middle-income countries. JAMA. 2020 doi: 10.1001/jama.2020.4169. [DOI] [PubMed] [Google Scholar]
- IEDCR/DGHS/GoB . 2020. Coronavirus COVID-19 Dashboard; p. 2020.http://103.247.238.81/webportal/pages/covid19.php?fbclid=IwAR0fvp1tINehCpQfHn8c6lCqwqMmjNncdLdhNqYLIsMAhaSxD2nM4Jd043Y [Google Scholar]
- Islam A.R.M.T., Mamun A.A., Zahid A., Rahman M.M. Simultaneous comparison of modified-integrated water quality and entropy weighted indices: implication for safe drinking water in the coastal region of Bangladesh. Ecol. Indicat. 2020;113:106229. [Google Scholar]
- Islam A.R.M.T., Ahmed N., Bodrud-Doza M., Chu R. Characterizing groundwater quality ranks for drinking purposes in Sylhet district, Bangladesh, using entropy method, spatial autocorrelation index, and geostatistics. Environ. Sci. Pollut. Res. 2017;24(34):26350–26374. doi: 10.1007/s11356-017-0254-1. [DOI] [PubMed] [Google Scholar]
- Liu C.W., Lin K.H., Kuo Y.M. Application of factor analysis in the assessment of groundwater quality in a Blackfoot disease area in Taiwan. Sci. Total Environ. 2003;313(1-3):77–89. doi: 10.1016/S0048-9697(02)00683-6. [DOI] [PubMed] [Google Scholar]
- Mamun M.A., Siddique A.B., Sikder M.T., Griffiths M.D. Student suicide risk and gender: a retrospective study from Bangladeshi press reports. Int. J. Ment. Health Addiction. 2020 [Google Scholar]
- TBS . Archived Newspaper the Business Standard. 2020. Fear, Hatred and Stigmatization Grip Bangladesh amid Covid-19 outbreak.https://tbsnews.net/thoughts/fear-hatred-and-stigmatization-grip-bangladesh-amid-covid-19-outbreak-61129 [Google Scholar]
- TBS . Archived Newspaper the Business Standard. 2020. Coronavirus Cases Detected in Cox's Bazar Rohingya camps.https://tbsnews.net/coronavirus-chronicle/bangladesh-says-coronavirus-detected-rohingya-refugee-camp-81490?fbclid=IwAR024QrrPPYSK_9WzfaMpTHCJu7hemZ1UzFpAQaKnyBxyQ7QV-YoJOTQjGY [Google Scholar]
- Wang G., Zhang Y., Zhao J., Zhang J., Jiang F. Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet. 2020;395(10228):945–947. doi: 10.1016/S0140-6736(20)30547-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO . 2020. Coronavirus Disease 2019 (COVID-19) Situation Report 51.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 access [Google Scholar]
- WHO . 2020. Coronavirus Disease 2019 (COVID-19) Situation Report 63.https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200323-sitrep-63-covid-19.pdf?sfvrsn=b617302d_4 access [Google Scholar]
- Worldometers . 2020. COVID-19 Coronavirus Pandemic.https://www.worldometers.info/coronavirus/ [Google Scholar]
- Xiao Y., Torok M.E. Taking the right measures to control COVID-19. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30152-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Wang Z., Chang R., Wang H., Xu C., Yu X., Tsamlag L., Dong Y., Wang H., Cai Y. COVID-19 containment: China provides important lessons for global response. Front. Med. 2020 doi: 10.1007/s11684-020-0766-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Tables R1