Highlights
-
•
A Patient was treated with portal vein arterialization for iatrogenic occlusion of the hepatic artery after pancreatoduodenectomy.
-
•
Portal vein arterialization is an old surgical method, which could be helpful to reduce the failure-to-rescue rate of patients with a dearterialised liver.
-
•
Portal vein arterialization is a rare but safe technique to supply arterial blood to the liver.
Keywords: Liver surgery, Portal vein, Revascularisation, Arterialisation
Abstract
Introduction
Portal Vein Arterialization is a rare procedure for total de-arterialized livers to ensure arterial inflow to the liver.
Presentation of case
A 55-year-old male patient underwent pancreatoduodenectomy for chronic pancreatitis. One month after discharge the patient was re-admitted because of bleeding from a pseudoaneurysm of the ligated gastroduodenal artery. During radiological intervention a coil dislocated and a complete occlusion of the hepatic artery occurred. Extraction of the coil was not possible, therefore, the patient was transferred to our hospital for surgical revascularization. We performed a side-to-side running anastomosis between a branch of a mesenteric artery and the corresponding vein to supply arterial blood to the liver. The postoperative course was uneventful. Radiologic examinations showed a patent arterio-portal shunt.
Discussion
Portal vein arterialization might be a lifesaving procedure in complication management.
Conclusion
PVA is an old surgical method, which could be helpful to reduce the failure-to-rescue rate.
1. Introduction
The complete occlusion of the hepatic artery is a severe complication after pancreatic or liver resection. This can lead to liver necrosis or biliary ischemia with fatal liver failure. In some cases, the hepatic artery can anastomosed to the portal vein for arterial inflow into the liver [1,2]. Portal vein arterialization (PVA) serves as a salvage technique, when no other option for revascularization is available. However, a large variety of this technique is described in the literature [2]. In this case, we present a case of PVA after occlusion of the hepatic artery after pancreatoduodenectomy.
2. Case presentation
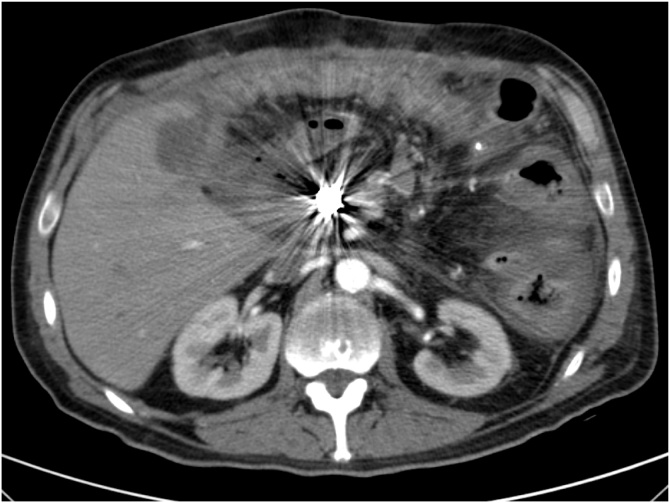
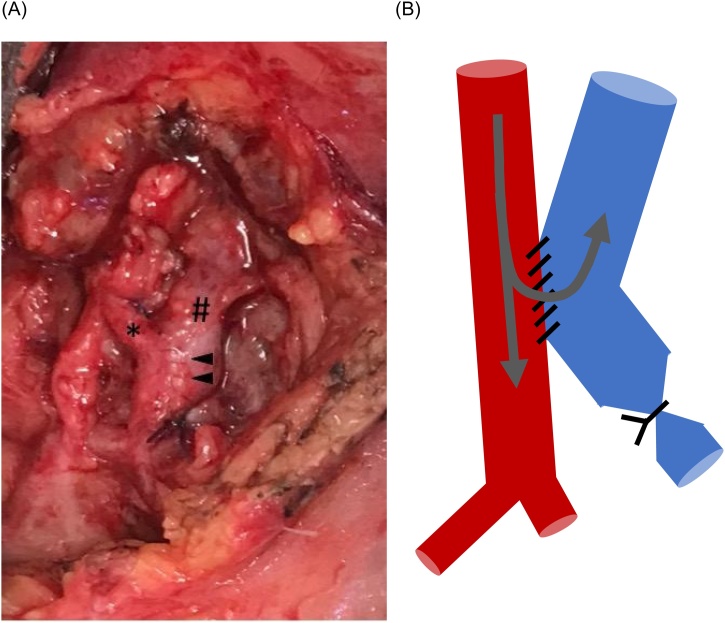
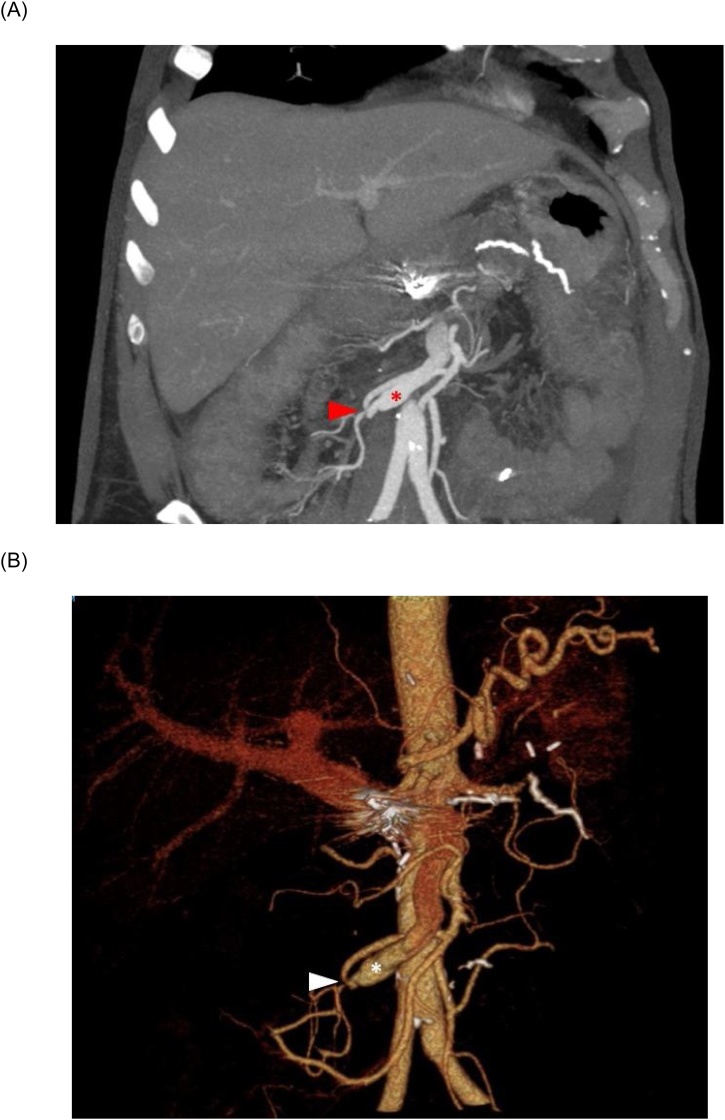
A 55-year-old male patient underwent pancreatoduodenectomy for chronic pancreatitis and stenosis of the pancreatic duct in a community hospital. A whipple’s pancreatoduodenectomy with end-to-side duct-to-mucosa pancreaticojejunostomy and portal vein reconstruction was performed [3]. During the postoperative course, the patient developed a pancreatic fistula grade B, which was treated conservatively. One month after discharge the patient was re-admitted to the same hospital with acute upper gastrointestinal bleeding. For hemodynamic stabilization the patient was intubated and afterwards an upper endoscopy was performed. A small bleeding was clipped. Because of the discrepancy between the hemorrhagic shock and the small bleeding, a CT-Scan was immediately performed. This revealed a pseudoaneurysm of the ligated gastroduodenal artery, which was coiled by an experienced interventional radiologist. During control angiography a persisting contrast filling of the aneurysm was seen, and therefore the aim was to place a second coil into the aneurysm. Accidently, the coil dislocated and a complete occlusion of the hepatic artery occurred (Fig. 1). An extraction of the coil was not possible and no other revascularization option was available. Therefore, the patient was transferred to our hospital for revascularization. The patient arrived intubated and was directly transferred to the operating room. The aim was to revasculate the hepatic artery with a vena saphena interponate graft, but unfortunately due to chronic inflammation the preparation of the surrounding tissue was of unacceptable risk and therefore the exposure of the hepatic artery was not performed. As an alternative, the arterialization of the portal vein was considered. After preparation of a small arterial mesenteric branch, we performed a side-to-side running anastomosis between the artery and corresponding vein (Fig. 2A + B). The anastomosed branch of the vein was proximally ligated to avoid arterial backflow towards the small bowel. Postoperatively the patient was extubated on the first postoperative day (POD). Doppler ultrasound controls revealed elevated portal flows. Coagulation parameters normalized within 2 days postoperatively and the ALAT peaked on the POD 1 (400 U/l). The postoperative course was uneventful. The patient suffered from a severe delirium, which required a complex medication and care. Therefore, the patient was discharged on 30th POD. An Angio-CT Scan showed patent arterio-portal shunt (Fig. 3).
Fig. 1.
CT Scan showing the dislocated coil occluding the hepatic artery.
Fig. 2.
(A) Portal vein arterialization between branches of the mesenteric artery (*) and vein (#). The arrowheads show the anastomosis. (B) Scheme of the anastomosis.
Fig. 3.
Arterial phase imaging showing patent arterio-portal shunt (arrow) and mesenteric vein (*): (A) CT Scan (B) 3D Reconstruction.
3. Discussion
Portal-vein arterialization (PVA) was originally developed for the treatment of portal hypertension [1]. Nowadays, PVA serves also as a rescue-procedure for revascularization in totally de-arterialized livers after HPB-procedures including transplantation [2]. This procedure comes along with a high mortality and a high incidence of portal hypertension [2]. An occlusion of the hepatic artery is a high risk of biliary ischemia or necrosis and liver necrosis with hepatic failure. However, this does not occur in all patients because of the development of arterial collaterals. Clinical findings or parameters, which allows a better decision about the need for revascularization, are rare. In our case, we assumed a high risk of liver necrosis, but it could be also possible that this procedure was not inevitable.
In conclusion, PVA is an old and almost forgotten surgical method. The aim of this case report is to commemorate this technique, which could be helpful to reduce the failure-to-rescue rate [4]. This Case Report has been reported in line with the SCARE criteria [5].
Declaration of Competing Interest
Nothing to declare.
Funding
Nothing to declare.
Ethical approval
No ethical approval was required for this case report.
Consent
Patient gave consent for publishing.
Author contribution
Tim Reese wrote the manuscript.
York von Rittberg critically reviewed the manuscript.
Karl J. Oldhafer critically reviewed the manuscript.
Registration of research studies
N/A.
Guarantor
Tim Reese.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Matzander U. Method and technic of pressure-adapted liver arterialization with portacaval anastomosis. Chirurg. 1974;45(May (5)):226. passim. [PubMed] [Google Scholar]
- 2.Bhangui P., Salloum C., Lim C., Andreani P., Ariche A., Adam R. Portal vein arterialization: a salvage procedure for a totally de-arterialized liver. The Paul Brousse Hospital experience. HPB (Oxford) 2014;16(August (8)):723–738. doi: 10.1111/hpb.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Romano G., Agrusa A., Galia M., Di Buono G., Chianetta D., Sorce V. Whipple’s pancreaticoduodenectomy: surgical technique and perioperative clinical outcomes in a single center. Int. J. Surg. 2015;21(September (Suppl. 1)):S68–71. doi: 10.1016/j.ijsu.2015.06.062. [DOI] [PubMed] [Google Scholar]
- 4.Nimptsch U., Krautz C., Weber G.F., Mansky T., Grützmann R. Nationwide in-hospital mortality following pancreatic surgery in germany is higher than anticipated. Ann. Surg. 2016;264(December (6)):1082–1090. doi: 10.1097/SLA.0000000000001693. [DOI] [PubMed] [Google Scholar]
- 5.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A., Orgill D.P., For the SCARE Group The SCARE 2018 statement: updating consensus surgical CAse REport (SCARE) Guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]