Abstract
Mature cystic teratoma (MCT) is a benign, slow-growing tumor and accounts for approximately 75% of mediastinal germ cell tumors. Patients with MCT are often asymptomatic when the tumors are small. Most of the symptoms are frequently related to compression of the mediastinal structures. We herein describe 3 adult cases of MCT. The patients were a 37-year-old man, a 35-year-old woman, and a 54-year-old woman. They were hospitalized with compression-related symptoms, such as chest pain, dyspnea, and cough. Findings from conventional chest radiograph, computed tomography (CT), magnetic resonance imaging were characterized. Conventional chest radiography still plays a major role in the initial evaluation of MCT, while CT remains the preferred modality for initial cross-sectional imaging evaluation of mediastinal lesions. However, thoracic magnetic resonance imaging provides more detailed and often definitive evaluation of mediastinal masses than CT because of its superior tissue characterization.
Keywords: Benign, Mature cystic teratoma, Mediastinal, Germ cell tumor
Introduction
Mediastinal germ cell tumors are relatively rare and account for approximately 10%-15% of mediastinal masses. Mediastinal mature cystic teratoma (MCT) is a benign histological variant of these tumors which consists of well-differentiated tissues originated from 2 or 3 germ cell layers [1]. Approximately, 53% of patients are asymptomatic and the teratomas are detected incidentally on standard chest radiograph. Symptoms are often produced when large tumors compress the surrounding structures [2]. Surgical resection is the main modality of treatment thus far. In the diagnosis of mediastinal teratomas, conventional chest radiograph still plays a major role for initial evaluation while computed tomography (CT) scan is significant for specifying the nature, location, and the relationship of the tumor to the other structures. In addition, it is beneficial in distinguishing tumors originating in the mediastinal areas from those that invade from lungs or other organs. Recently, ongoing developments in magnetic resonance imaging (MRI) are considered an adjunct to CT scan in the diagnosis of mediastinal lesions. MRI was more dominant than CT scan in evaluating the spread through the tumor capsule and adjacent structures infiltration by fat plane obliteration [3]. The purpose of this report is to characterize some imaging features of 3 cases of large mediastinal MCTs.
Case presentations
Patient 1
A 37-year-old man was admitted to our center with dyspnea on exertion for 2 months. The frontal chest X-ray showed an anomalous mass without radiographic evidence for gross calcification in the mediastinal area (Fig. 1a). Because the descending aortic border was not silhouetted, this mass was likely located in the anterior mediastinum. Chest CT with contrast was performed and demonstrated a cystic mass in the anterosuperior and middle mediastinum, with smooth edges, low density, and without apparent infiltration of adjacent organs. This mass was approximately 6 × 10 × 11 cm in size and contained calcifications and small foci of fat. Internally, the attenuation was slightly higher than that of simple fluid (Fig. 1b-d).
Fig. 1.
(Case 1) Mediastinal mature cystic teratoma in a 37-year-old man. Frontal chest radiography and CT scan images: (a) The frontal chest X-ray shows a noncalcified mediastinal mass. This mass arose from the anterior mediastinum because the descending aortic border was not silhouetted (arrow); (b) the axial plain view, (c) the coronal plain view, and (d) the sagittal plain view of the CT image shows a large heterogeneous cystic mass in the superior anterior mediastinum. Areas of soft tissue (arrow in c) and fat attenuation (arrow in b) are depicted within the mass.
In the MRI scans, opposed phase imaging showed a decreased signal intensity of microscopic intracellular lipid within the lesion (Fig. 2a and b). The axial T2 haste and axial T2 blade FS (Fig. 2c and d) imaging showed a large left anterior mediastinal mass with internal heterogeneous areas of signal intensity abnormality. The axial contrast-enhanced fat-suppressed T1-weighted and axial T1 FS subtraction images, obtained after administration of intravenous gadolinium-based contrast material, showed a lack of solid enhancement within the mass lesion (Fig. 2e and f).
Fig. 2.
(Case 1) Mediastinal mature cystic teratoma in a 37-year-old man. MRI findings: (a) In-phase and (b) opposed-phase MRI scans demonstrate a decrease in signal intensity on the opposed-phase images comparing with the in-phase images. The hypointensities on opposed-phase imaging reveals areas of microscopic intracellular lipid within the lesion. (c) Axial T2 haste and (d) axial T2 blade FS show the large left anterior mediastinal mass lesion causing an impression on the superior vena cava with internal heterogeneous areas of signal intensity abnormality. (e) Axial contrast-enhanced fat-suppressed T1-weighted MR image and (f) axial T1 FS subtraction, obtained after administration of intravenous gadolinium-based contrast material, show a lack of solid enhancement within the mass lesion.
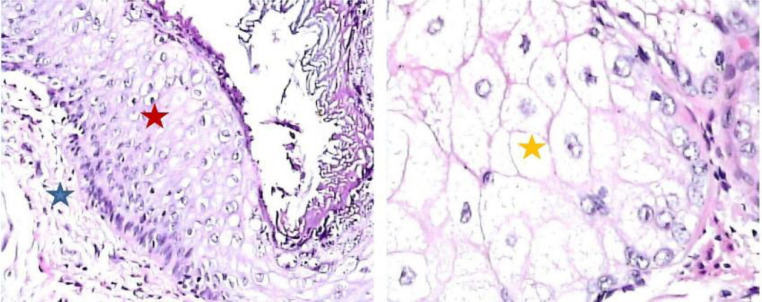
Mediastinal MRI showed a better definition of the lesions and a more accurate differential diagnosis. MRI was also used to evaluate the tumor relationship with other vital mediastinal structures for surgical planning. Surgical excision was successfully accomplished via a median sternotomy. The tumor was continuous to the left parietal pleura without cardiac, pulmonary, or vascular invasion. Macroscopic examination showed a predominantly cystic tumor, having a thin, sharply delineated wall filled with sebaceous material. Microscopically, the cyst wall was lined by glandular epithelium. Cartilage and smooth muscle were also evident (Fig. 3). The postoperative course was unremarkable and the patient was discharged on the eighth day. Follow-up chest radiography performed on day 1, day 8, and 1 year postoperatively showed no evidence of mediastinal tumor recurrence.
Fig. 3.
(Case 1) Hematoxylin and eosin-stained (original magnification, × 200) medium-power microscopic images showing the cartilage (blue star), smooth muscle (red star), and glandular epithelium (yellow star). (Color version of figure is available online.)
Patient 2
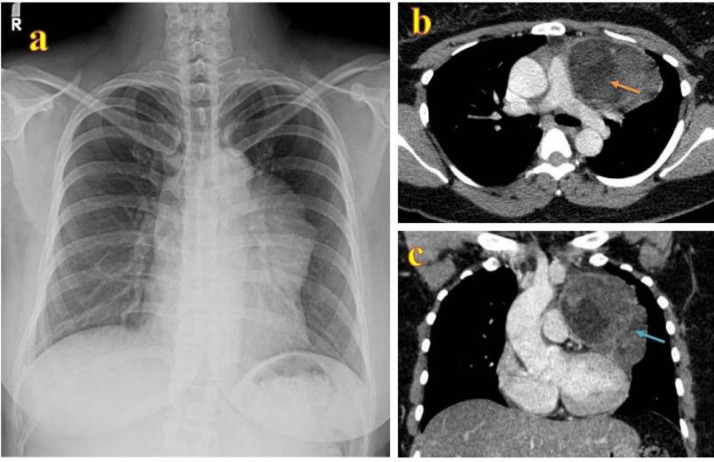
A 35-year-old female patient was transferred to our center with persistent cough and dyspnea for 1 month. Frontal chest X-ray showed a left anterior mediastinal mass. The descending aorta remained visible implying that the mass could not be posterior. The left hilar vessels remained visible (hilum overlay sign). Therefore, the mass could not be at the hilum. However, the absence of the upper left heart border silhouette implied that the mass must be anterior (Fig. 4a). Contrast-enhanced axial CT scan of the chest demonstrated a left anterior mediastinal mass approximately 7.5 × 8 × 10 cm in size, containing fat and soft tissue components (Fig. 4b and c). MRI confirmed a left anterior mediastinal mass with heterogeneous intensity on coronal T2 HASTE and peripheral, septal enhancement on coronal T1 vibe FS postcontrast (Fig. 5a and b). Regarding axial T1 in-phase and opposed-phase images, hypointensity areas in opposed-phase images demonstrated microscopic intracellular lipid in the lesion (Fig. 5c and d). Axial T1 vibe FS and axial T1 vibe FS subtraction images showed unenhanced proteinaceous fluid and homogenous enhanced soft tissue within the mass (Fig. 5e and f). The patient underwent surgical excision and no evidence of vascular invasion was noted. The major components of the tumor were fibrous connective tissue, squamous epithelium, and sebaceous gland (Fig. 6). The patient was discharged on the sixth day postoperatively. Follow-up radiography performed on day 1, day 14, and 9 months postoperatively showed no evidence of recurrent.
Fig. 4.
(Case 2) Mediastinal mature cystic teratoma in a 35-year-old woman. The frontal chest -X-ray and CT scan images: (a) Frontal chest X-ray showing the mass on the left anterior mediastinum. The descending aorta remains visible implying the mass cannot be posterior. The left hilar vessels remain visible (hilum overlay sign) implying the mass cannot be at the hilum. The upper left heart border silhouette is absent indicating the mass must be anterior. (b) Axial plain view and (c) coronal view of chest CT scan with contrast demonstrating a left anterior mediastinal mass containing fat (orange arrow) and soft tissue components (blue arrow). (Color version of figure is available online.)
Fig. 5.
(Case 2) Mediastinal mature cystic teratoma in a 35-year-old woman. MRI findings: (a) Coronal T2 HASTE and (b) Coronal T1 vibe FS postcontrast images confirming a left anterior mediastinal mass with heterogeneous intensity on T2W, peripheral and septal enhancement. (c) Axial T1 in-phase and (d) opposed-phase images showing hypointensity areas in opposed-phase image of microscopic intracellular lipid in the lesion. (e) Axial T1 vibe FS and (f) axial T1 vibe FS subtraction images showing unenhanced proteinaceous fluid and soft tissue enhancement (arrow) within the mass.
Fig. 6.
(Case 2) Hematoxylin and eosin-stained (original magnification, × 200) medium-power microscopic images demonstrating the fibrous connective tissue (blue star), squamous epithelium (red star), and sebaceous gland (yellow star). (Color version of figure is available online.)
Patient 3
A 54-year-old female patient vaguely presented with chest pain. Frontal chest X-ray revealed a large mass with the density of soft tissue and calcification on the right hemithorax. The mass was located by default in the anterior mediastinum because it obliterated the normal silhouette of the superior vena cava and right heart border. Hilar vessels could be seen through the mass (hilum overlay sign) (Fig. 7a). CT findings confirmed a well-defined and hypodense mass in the anterior mediastinum about 9 × 10 × 12 cm. The inner contents showed calcification and fat suggesting a teratoma (Fig. 7b and c). MRI revealed the following: coronal T2 HASTE image showed a complex, cystic anterior mediastinal mass; axial T2 HASTEIRM image showed a regular, thin-walled cystic anterior mediastinal mass with both fluid-like and nodular components (Fig. 8a and b). Axial T1 in-phase and opposed-phase images illustrated a microscopic intracellular lipid in the lesion (Fig. 8c and d). T1 vibe FS and T1 vibe FS subtraction images, after administrating gadolinium, noted a proteinaceous cystic anterior mediastinal mass without enhancement (Fig. 8e and f). Surgical incision was performed via median sternotomy and the tumor was successfully dissected without invasion of large mediastinal structures. Photomicrograph of the mature teratoma showing squamous epithelium and pseudostratified columnar epithelium (Fig. 9). The postoperative course was stable and the patient was discharged on the fifth day. Follow-up radiography performed 9 months postoperatively showed no evidence of recurrent.
Fig. 7.
(Case 3) Mediastinal mature cystic teratoma in a 54-year-old woman. Frontal chest radiograph and CT image: (a) Frontal chest X-ray demonstrating a large soft tissue density and calcification on the right side. The mass is located by default in the anterior mediastinum because it obliterates the normal silhouette of the SVC and right heart border. Hilar vessels can be seen through the mass (hilum overlay sign) (b) and (c) anterior hypodense well-defined right-sided mediastinal mass, with calcification (green arrow) and fat (orange arrow) within it, the appearance is highly suggestive of teratoma. (Color version of figure is available online.)
Fig. 8.
(Case 3) Mediastinal mature cystic teratoma in a 54-year-old woman. MRI findings: (a): Coronal T2 HASTE image demonstrating a complex cystic anterior mediastinal mass. (b): Axial T2 HASTEIRM image demonstrating a regular, thin-walled cystic anterior mediastinal mass with both fluidlike (green arrow) and nodular components (orange arrow). (c) Axial T1 in-phase and (d) opposed-phase images demonstrating microscopic intracellular lipid in the lesion (blue arrow). (e) T1 vibe FS and (f) T1 vibe FS subtraction images after the administration of gadolinium demonstrating a proteinaceous cystic anterior mediastinal mass without enhancement. (Color version of figure is available online.)
Fig. 9.
(Case 3) Hematoxylin and eosin-stained (original magnification, × 200) medium-power microscopic images showing the squamous epithelium (blue star) and pseudostratified columnar epithelium (red star). (Color version of figure is available online.)
Discussion
The most common site of extragonadal germ cell tumors is anterior mediastinum, especially in the area near or within the thymus gland. Mature teratoma is a benign, slow-growing type, and accounts for around 75% of mediastinal germ cell tumors [4]. Mature teratomas seldom manifest any clinical symptoms when they are small in size and do not compress the mediastinal structures. In the cases we have reported, all patients had clinical symptoms (dyspnea on exertion, cough, and chest pain), and MRI revealed that the tumors were large in size.
A frontal chest radiograph will show that, mediastinal mature teratomas often create an obtuse angle with the lungs, silhouette the cardiac borders, and demonstrate the hilum overlay sign. The hilar vessels are still visible through a mediastinal mass. This indicates the mass does not arise from the hilum. On a lateral chest radiograph, the mass can be compartmentalized into the anterior, middle, or posterior mediastinum. Masses that tend to obliterate the retrosternal clear space are in the anterior mediastinum [5]. Sometimes, calcification can be seen on a chest radiograph as in case 3 of this study.
Mediastinal mature teratomas are often well-defined on CT and show internal heterogeneous appearances owing to the presence of fat, fluid, soft tissue, or calcifications. Furthermore, these lesions can have an internal proteinaceous or hemorrhagic fluid component that has high density on noncontrast images. Intravenous contrast media enhance the soft tissue, peripheral and septal components [5,6]. In some reports of mediastinal teratomas imaged with CT, 53% involved calcifications, 65%-75% noted fat attenuation, and 85%-90% had areas of fluid attenuation [7]. The absence of fat cannot exclude a germ cell tumor from the differential diagnosis. The solid components in tumors can be the predictor of malignant risk. In this study, all 3 benign mature teratomas had the major components of fat, proteinaceous fluid, and some small areas of solid tissue. The hyperattenuating (up to 100 Hounsfield units) prevascular lesions on CT can be benign hemorrhagic, proteinaceous cysts, or necrotic solid lesions.
MRI is superior to CT in reliably distinguishing cystic from solid lesions [5]. On MRI, a cyst exhibits homogeneous hyperintensity on T2W images but variable intensity on T1W images due to its serous, proteinaceous, or hemorrhagic nature. A proteinaceous or hemorrhagic cyst shows high signal on T1W images. T1 vibe FS subtraction images can be useful in identifying the enhancement of a high-signal cyst [5,8].
Mature teratomas are the most common germ cell tumor of the mediastinum and may contain macroscopic and/or microscopic fat [9]. Macroscopic fat can be determined on both CT and MRI but microscopic intracellular fat is only detected on MRI [5]. On MRI, the combination of T1/T2-hyperintensity and saturation on fat-saturated MRI pulse sequences prove the existence of macroscopic or gross fat. A fat-fluid level within an anterior mediastinal mass is virtually diagnostic of a teratoma, indicating the existence of sebum. Besides, in- and opposed-phase chemical shift gradient echo imaging gives additional information regarding the figure of microscopic or intravoxel fat in teratomas [5,8].
A complication of teratomas may be rupturing into the pleural space or pericardium. Rupture of the teratoma can also be suspected if the wall of the lesion appears ruptured with associated effusions or lung consolidation [10,11]. No complication from these teratomas were noted in our series.
Conclusion
Mature cystic teratoma is an uncommon lesion in the mediastinum. This tumor is usually asymptomatic due to its slow growth rate and is often detected incidentally on chest X-ray. Despite CT remaining the modality of choice for initial cross-sectional imaging evaluation of mediastinal lesions, thoracic MRI provides more intimate and often definitive evaluation of mediastinal masses because of its superior tissue characterization.
Patient Consent
Written informed consent was obtained from the patients for the publication of this case report.
Footnotes
Acknowledgments: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing Interest: The authors declare that they have no conflict of interest regarding the publication of this case report.
References
- 1.Takeda S.-I., Miyoshi S., Ohta M., Minami M., Masaoka A., Matsuda H. Primary germ cell tumors in the mediastinum. Cancer. 2003;97(2):367–376. doi: 10.1002/cncr.11068. [DOI] [PubMed] [Google Scholar]
- 2.Lewis B.D., Hurt R.D., Payne W.S., Farrow G.M., Knapp R.H., Muhm J.R. Benign teratomas of the mediastinum. Surgery J Thorac Cardiovasc Surg. 1983;86(5):727–731. [PubMed] [Google Scholar]
- 3.Carter B.W., Betancourt S.L., Benveniste M.F. MR imaging of mediastinal masses. Top Magn Reson Imaging. 2017;26(4):153–165. doi: 10.1097/RMR.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 4.Moeller K.H., Rosado-de-Christenson M.L., Templeton P.A. Mediastinal mature teratoma: imaging features. AJR Am J Roentgenol. 1997;169(4):985–990. doi: 10.2214/ajr.169.4.9308448. [DOI] [PubMed] [Google Scholar]
- 5.Patel I.J., Hsiao E., Ahmad A.H., Schroeder C., Gilkeson R.C. AIRP best cases in radiologic-pathologic correlation: mediastinal mature cystic teratoma. Radiographics. 2013;33(3):797–801. doi: 10.1148/rg.333125088. [DOI] [PubMed] [Google Scholar]
- 6.Rosenzweig K.E., Chen C.P., SYom S. Leibel and Phillips textbook of radiation oncology. WB Saunders; 2010. Tumors of the lung, pleura, and mediastinum; pp. 737–771. edn. [Google Scholar]
- 7.Dhond A.P., Agrawal S.O., Sirmukaddam S.V., Srinath S., Roplekar P., Desai P.R. Mediastinal teratoma: a case report with review of literature. J Sci Soc. 2016;43:57. [Google Scholar]
- 8.Daye D., Ackman J.B. Characterization of mediastinal masses by MRI: techniques and applications. Appl Radiol. 2017;46:10–22. [Google Scholar]
- 9.Shameem M., Qaseem S.M.D., Siddiqui M.A., Shah N.N., Ahmad A. Mature mediastinal teratoma in adult. Respir Med CME. 2010;3(2):116–117. [Google Scholar]
- 10.Vieira R.D., Grimberg H., Uezumi K.K., Demarchi L.M.M., Tsutsui J.M., Lopes N.H.M. Teratoma of the mediastinum: a case report. J Med Case Reports. 2011;5(1):193. doi: 10.1186/1752-1947-5-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.No T.-H., Seol S.-H., Seo G.-W., Kim D.-I., Yang S.Y., Jeong C.H. Benign mature teratoma in anterior mediastinum. J Clin Med Res. 2015;7(9):726–728. doi: 10.14740/jocmr2270w. [DOI] [PMC free article] [PubMed] [Google Scholar]