Abstract
The presence of ipsilateral aneurysm in the stenosis of the internal carotid artery is determined by computed tomography angiography in 1.8%-3.2% of cases. The literature describes the most varied options for treating this pathology: isolated or alternate, and now the method of simultaneous endovascular treatment – carotid stenting and endovascular embolization of aneurysm – is gaining popularity. We presented a clinical case of treatment of 61 women with critical stenosis (90%) and tortuosity of the internal carotid artery in combination with ipsilateral saccular aneurysm of the anterior connecting artery. The uniqueness of this case lies in the fact that a hybrid approach has been applied in the treatment of pathology, not previously described in the literature. The case is highlighting the potential complexity of concomitant vascular cervical and cerebral pathology and the necessity of surgical and endovascular team interactions to choose the appropriate methods of treatment.
Keywords: Atherosclerosis, Carotid endarterectomy, Coil embolization, Saccular aneurysm
Introduction
According to literature in patients with hemodynamically significant lesions of precerebral arteries, 5% of cases have concomitant intracranial aneurysms, and in 1.8%-3.2% of case on the ipsilateral side [1], [2], [3]. Currently, in the absence of randomized studies, there are no definite clinical recommendations on the treatment choice in this group of patients [4], [5], [6].
Case report
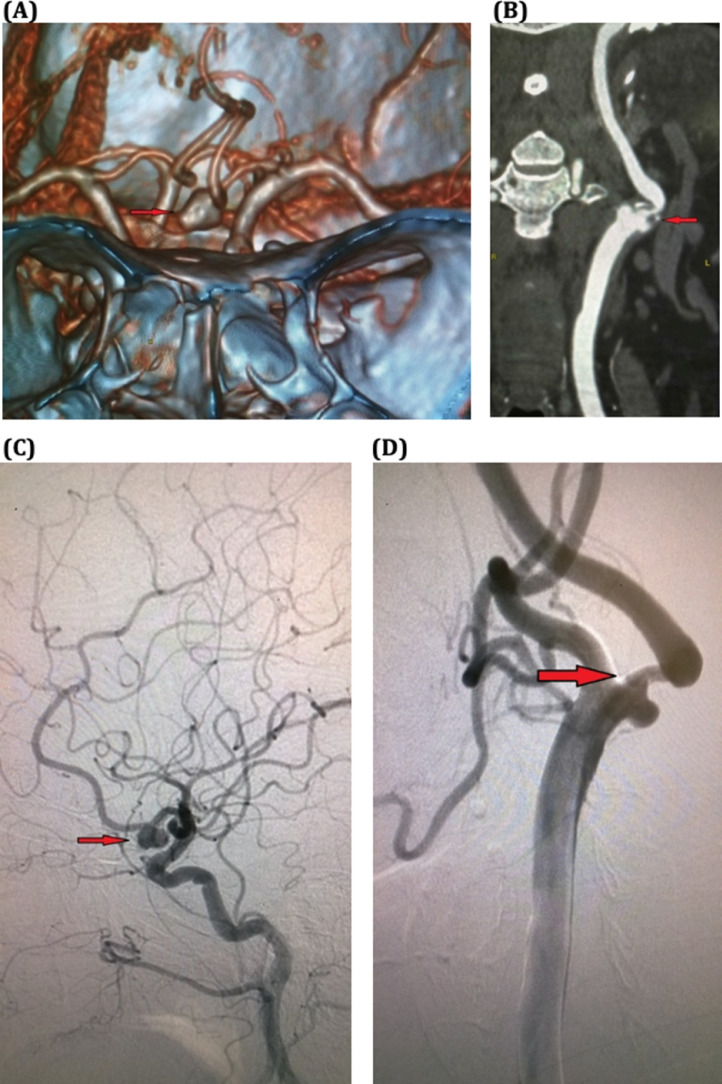
A 61-year-old female was admitted at the Department of Vascular Surgery with complaints of headache, tinnitus, dizziness, and unsteadiness of gait. According to duplex ultrasound, there was a high grade dense ulcerated stenosis of the left internal carotid artery (ICA) C1 segment with kinking into C2 and 340 cm/s systolic flow velocity. According to performed computed tomographyangiography (CTA), stenosis of the left ICA was 90% NASCET and 8.5 × 6.0 mm saccular aneurysm of the left anterior communicating artery (AComm) was incidentally found. Patient was prepared and transferred to the Cathlab, where direct cerebral angiography confirmed CTA findings (Fig. 1).
Fig. 1.
Diagnostic imaging. Acomm saccular aneurysm CT volume rendering (A); significant left internal carotid artery stenosis – CTA central line reconstruction (B); Acomm saccular aneurysm direct angiography (C); significant left internal carotid artery stenosis direct angiography (D). Acomm, anterior communicating artery; CT, computed tomography; CTA, computed tomography angiography.
Stenosis and aneurysm are independent pathologies. However, the possible presence of ipsilateral stenosis of the ICA did not lead to subarachnoid hemorrhage of such a large aneurysm. Due to the occurrence of subarachnoid hemorrhage in the early postoperative period, the first stage of an isolated ICA operation was dangerous.
Because of a complex calcific anatomy, dense atherosclerotic plaque with ulceration, a C-shaped kinking of the ICA, our team made the decision to perform a simultaneous hybrid procedure – CEA on the left ICA with subsequent AComm aneurysm coiling.
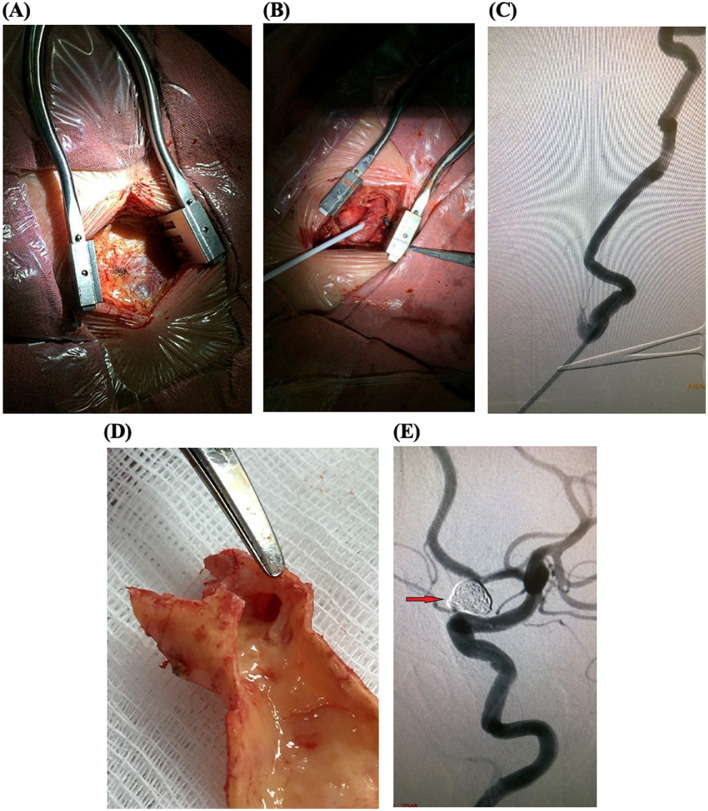
Under general anesthesia, a 5-cm incision was made on the middle side of the sternocleidomastoid muscle (Fig. 2). Common carotid artery, external carotid artery, ICA, and the upper thyroid artery were carefully identified, controlled with vessel loops, bypassed, and pinched by atraumatic clamps. About 5000 units of heparin were injected intravenously. Lumen of the CCA and ICA were opened and dense, ulcerated atherosclerotic plaque was removed, and the arteriotomy site was sewed with medpropilen 6/0 (Medrtonic, Minneapolis, Minnesote). Proximally to CCA bifurcation, femoral introducer Prelude 6F (Merit Medical, Salt Lake City, Utah) was inserted simultaneously with the clamps removal (Fig. 2). The ICA occlusion time was 12 minutes. Installation of the introducer through the purse string suture on the common carotid artery, then 0.014” Traxcess wire and Headway 17 micro catheter (Microvention, Terumo, Tokyo, Utah, Minnesote) were introduced into the aneurysm sac. The aneurysm was coiled with Axium 3D (Medtronic, Minneapolis, Minnesota) 8mm × 20cm, 7mm × 30cm and 2mm × 6cm. Control angiography showed completely excluded aneurysm sac, patent AComm and both anterior cerebral arteries with TICI 3 blood flow (Fig. 2). Total procedure time was 95 minutes.
Fig. 2.
Surgery and endovascular coiling. Incision (A); 6F sheath in the CCA (B); postendarterectomy angiography – patent ICA lumen without stenosis (C); ulcerated atherosclerotic plaque (D); coiled Acomm, Raymond-Roy occlusion classification 1 (E). Acomm, anterior communicating artery; CCA, common carotid artery; ICA, internal carotid artery.
The patient was extubated 30 minutes postop, transferred from the intensive care unit to the ward in 4 hours. Control ultrasound on the third day showed patent carotid reconstruction zone with linear blood flow velocity under 100 cm/s. The procedure and the postoperative period proceeded without complications. In our opinion, the simultaneous operation reduced the risks of any possible complications in a particular case to almost zero.
Discussion
According to the literature, the most frequently used treatment method for such concomitant pathology was CEA, followed by dynamic monitoring of the aneurysm [1,4,[7], [8], [9]]. Meta-analysis by Khan et al. in 2012 showed that from 141 observations 73.7% of patients’ undergone only ICA interventions (in 91.3% of them CEA). The methods of the rest alternated in different ways [1]. The percentage of ruptured intracranial aneurysms in the early and late postoperative periods after isolated CEA ranged from 0% to 5.3% [1,5]. However, in the vast majority of cases, the size of the aneurysms did not exceed 7 mm [3,10]. Currently, the most popular method of treatment of such pathology is simultaneous endovascular approach – CAS and aneurysm coiling. In some healthcare facilities, 2-stage treatment is preferred – CAS and after 3 weeks of careful blood pressure observation specialists perform aneurysm coiling [6]. In addition, in case of noncritical ICA stenosis and stable plaque, first-line aneurysm coiling is possible, with subsequent CAS in 1 month [11]. Taking into account ongoing neurological symptoms, high-grade carotid stenosis with complex anatomy, high risks of stroke as well as high risk of aneurysm rupture, especially in case of cerebral hemodynamics alterations after the CEA, our team including vascular and endovascular surgeons and anesthesiologist have refused total endovascular approach in favor of hybrid treatment. To perform this procedure, the presence of a specially equipped Cathlab or hybrid operating room is mandatory. A simultaneous operation does not require the exceptional skills of operating surgeons, but it facilitates the work of an endovascular surgeon, as the introducer is already directly inserted into the common carotid artery (this is especially important in patients with difficult anatomy of the brachiocephalic arteries). An ideal option when the surgeon combines both a vascular and endovascular surgeon, who can independently conduct such operations.
Conclusion
Due to the lack of evidence data in the setting of concomitant presence of the aneurysm and the stenosis of the ipsilateral ICA, the decision of treatment method should be made in a close interaction between the vascular and endovascular surgeon, neurosurgeon, and anesthesiologist. Based on the literature analysis and our experience, the hybrid approach with a simultaneous endarterectomy and ipsilateral intracranial aneurysm coiling is a safe and effective method of treating such pathology.
Footnotes
Competing interests: The authors declare no conflict of interests.
References
- 1.Khan U.A., Thapar A., Shalhoub J., Davies A.H. Risk of intracerebral aneurysm rupture during carotid revascularization. J Vasc Surg. 2012;56:1739–1747. doi: 10.1016/j.jvs.2012.07.027. [DOI] [PubMed] [Google Scholar]
- 2.Bouri S., Thapar A., Shalhoub J., Jayasooriya G., Fernando A., Franklin I.J. Hypertension and the post-carotid endarterectomy cerebral hyperperfusion syndrome. Eur J Vasc Endovasc Surg. 2011;41:229–237. doi: 10.1016/j.ejvs.2010.10.016. [DOI] [PubMed] [Google Scholar]
- 3.Kaçar Emre, Nas Ömer Fatih, Erdoğan Cüneyt, Hakyemez Bahattin. Single-stage endovascular treatment in patients with severe extracranial large vessel stenosis and concomitant ipsilateral unruptured intracranial aneurysm. Diagn Interv Radiol. 2015;21(6):476–482. doi: 10.5152/dir.2015.15092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Borkon M.J., Hoang H., Rockman C., Mussa F., Cayne N.S., Riles Th. Concomitant unruptured intracranial aneurysms and carotid artery stenosis: an institutional review of patients undergoing carotid revascularization. Ann Vasc Surg. 2014;28:102–107. doi: 10.1016/j.avsg.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 5.Siddiqui A., Vora N., Edgell R.C., Callison R.C., Kitchener J., Alshekhlee A. Rupture of a cerebral aneurysm following carotid endarterectomy. J Neurointerv Surg. 2012;4:27. doi: 10.1136/neurintsurg-2011-010091. [DOI] [PubMed] [Google Scholar]
- 6.Wajima D., Nakagawa I., Wada T., Nakase H. A trial for an evaluation of perianeurysmal arterial pressure change during carotid artery stenting in patients with concomitant severe extracranial carotid artery stenosis and ipsilateral intracranial aneurysm. Turk Neurosurg. 2017 doi: 10.5137/1019-5149.JTN.20418-17.0. [DOI] [PubMed] [Google Scholar]
- 7.Ladowski J.S., Webster M.W., Yonas H.O., Steed D.L. Carotid endarterectomy in patients with asymptomatic intracranial aneurysm. Ann Surg. 1984;200:70–73. doi: 10.1097/00000658-198407000-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ballotta E., Da Giau G., Manara R., Baracchini C. Extracranial severe carotid stenosis and incidental intracranial aneurysms. Ann Vasc Surg. 2006;20:5–8. doi: 10.1007/s10016-005-5438-3. [DOI] [PubMed] [Google Scholar]
- 9.Suh B.Y., Yun W.S., Kwun W.H. Carotid artery revascularization in patients with concomitant carotid artery stenosis and asymptomatic unruptured intracranial artery aneurysm. Ann Vasc Surg. 2011;25(5):651–655. doi: 10.1016/j.avsg.2011.02.015. [DOI] [PubMed] [Google Scholar]
- 10.Badruddin A., Teleb M.S., Abraham M.G., Taqi M.A., Zaidat O.O. Safety and feasibility of simultaneous ipsilateral proximal carotid artery stenting and cerebral aneurysm coiling. Front Neurol. 2010;1:120. doi: 10.3389/fneur.2010.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iwata T., Mori T., Tajiri H. Successful staged endovascular treatment of a symptomatic cervical carotid bifurcation stenosis coupled with a coincidental unruptured cerebral aneurysm in the carotid distal segment. AJNR Am J Neuroradiol. 2008;29:1948–1950. doi: 10.3174/ajnr.A1172. [DOI] [PMC free article] [PubMed] [Google Scholar]