Abstract
Objective
Restoring noncarious cervical lesions are challenging to clinical practice. This study aimed to compare the clinical performance/longevity of glass ionomer cements (GIC) and composite resins (CR) used for noncarious cervical lesions (NCCL) through a systematic review and meta-analysis (MA).
Data
Randomized and controlled clinical trials and nonrandomized clinical trials, which compared the clinical performance/longevity of CR and GIC (conventional and/or resin-modified) in the treatment of NCCL, were included.
Source
The methodological quality and risk of bias were evaluated using the Cochrane Collaboration tool. Seven MAs were performed considering (1) the clinical performance of the parameters in common: retention, marginal discoloration, marginal adaptation, secondary caries, color, anatomic form, surface texture and (2) a follow-up time of 12, 24 and 36 months. The prevalence of successful restorations and the total number of restorations per clinical parameter/follow-up time were used to calculate the relative risk (95% CI).
Study selection
After screening of the studies, 13 studies were used for quantitative synthesis. The risk difference (CI 95%, α, I2) between GIC and CR for anatomic form was 0.00 (-0.02, 0.02; p = 0.83; 0%); for color was -0.02 (-0.08, 0.04; p = 0.48; 80%); for surface texture was -0.02 (-0.06, 0.02; p = 0.31; 63%); for secondary caries was -0.00 (-0.01, 0.01; p = 0.87; 0%); for marginal discoloration was 0.01 (-0.01, 0.03; p = 0.23; 3%); for marginal adaptation was 0.01 (-0.01, 0.04; p = 0.34; 32%) and for retention was 0.07 (0.02, 0.12; p = 0.003; 76%).
Conclusion
GIC showed a clinical performance significantly higher than CR in regard to retention, whereas for the other parameters, GIC was similar to CR.
Clinical significance
NCCLs is increasingly prevalent among the population and this type of lesion causing defects in the tooth that affect not only aesthetics but also everyday habits, such as drinking, eating and teeth brushing, due to the sensitivity these lesions cause.
Keywords: Dentistry, Dental materials, Evidence-based medicine, Clinical research, Root caries, Glass ionomer cements, Composite resin
Dentistry; Dental materials; Evidence-based medicine; Clinical research; Root caries; Glass ionomer cements; Composite resin.
1. Introduction
Noncarious cervical lesions (NCCL) occur at the cementoenamel junction of the tooth, frequently starting at the outer surface and slowly and irreversibly progressing, without bacterial involvement [1]. NCCL are increasingly prevalent among the population due to the increase in life expectancy and worsening of these lesions with age, in addition to the high intake of acidic beverages by the population [1, 2, 3]. This type of lesion can occur due to erosion, abrasion, abfraction or a combination of these, causing defects in the tooth that affect not only aesthetics but also everyday habits, such as drinking, eating and teeth brushing, due to the sensitivity these lesions cause [2, 4, 5].
Thus, after diagnosis of the lesions, restorative treatment is usually necessary, combined with treatment of the causative factor [2, 6, 7]. Restorations, in addition to decreasing or ceasing sensitivity, avoid an increase in the affected area, accumulation of biofilm and the risk of developing carious lesions [1, 7]. The NCCL may exhibit an irregular or smooth disc-shaped appearance [6]. Therefore, the choice of restorative material is still a challenge due to the anatomy of lesions, the concentration of stress in the cervical region and dentinal sclerosis, which decreases the adhesion ability of the restorative material [1, 7, 8].
Composite resins (CR) are the materials most used in NCCL restoration because they have favorable aesthetic and mechanical properties [9]. In contrast, resins exhibit polymerization shrinkage and a high modulus of elasticity, causing stress due to occlusal forces [1, 7]. In the search for an alternative material to CR, studies have shown an increase in the choice of glass ionomer cements (GIC) because they have a modulus of elasticity similar to that of dentin and release fluoride. However, these materials have worse aesthetic properties because they are translucent and have fewer color options [1, 7]. GIC have less resistance to abrasion, increasing the surface roughness of these materials over time. Furthermore, due to the presence of reduced particles in CR, these materials have a smoother surface when compared to GIC [1].
In an attempt to improve the properties of GIC, resin-modified GIC have been developed, in which the functional monomers of photopolymerizable resins have been added. The addition of these components of the CR to the GIC brought improvements to their mechanical properties [6]. Other modifications have also been proposed, including the use of nanoparticles and use of thermo-light curing to improve the mechanical performance of GIC restorations [10, 11, 12]. However, very little is known about the clinical performance of those new-developed materials.
Due to the characteristics of the substrates, which are hyper-mineralized and with physiological and pathological dentin changes, the marginal integrity and retention of NCCL have always been a clinical challenge for professionals. Therefore, material of choice for restoring NCCL is a frequent doubt among clinicians. Given the above, summarized evidence on which material should be used for restoring NCCL is still necessary. The aim of this study was to assess, through a systematic review and meta-analysis (MA), the clinical performance/longevity of CR and GIC used in cases of NCCL. The null hypothesis was that there is no difference in clinical performance of any of the materials tested in NCCL.
2. Materials and methods
This systematic review and MA was registered in the PROSPERO database (registry CRD42018110230) and followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) guidelines (http://www.prisma-statement.org) [13]. The following question was asked: Is there a difference in the clinical performance of GIC and CR in NCCLs restorations?
2.1. Literature search strategy
Two examiners (IMB and ACMB) performed bibliographic searches independently in the following databases: PubMed (MEDLINE), Scopus, Web of Science and Cochrane Library. To locate unpublished or ongoing studies, PROSPERO was researched manually, with no restriction on the date of publication. The search strategy included changes in the keywords and was adapted to the rules of each database. MeSH terms and keywords related to noncarious cervical lesions, GIC and CR were used with Boolean operators (OR, AND) to combine the studies. There were no restrictions on the language or date of publication, and articles were searched until March 2020. Duplicate articles were identified, removed and considered as one study. The search strategy used in each database is shown in Table 1.
Table 1.
Search strategy according to the different databases assessed in the present study.
| Database | Strategy |
|---|---|
| PubMed | ((((((((((Root Caries [MeSH Terms]) OR Root Caries [Title/Abstract]) OR Cervical Cary [Title/Abstract]) OR Cervical Caries [Title/Abstract]) OR Non carious cervical lesion [Title/Abstract]) OR Non-carious cervical lesion [Title/Abstract]) OR Cervical lesion [Title/Abstract]) OR Cervical lesions [Title/Abstract])) AND (((((((Glass Ionomer Cements [MeSH Terms]) OR Glass Ionomer Cements [Title/Abstract]) OR Glass-Ionomer Cement [Title/Abstract]) OR Glass Ionomer Cement [Title/Abstract]) OR GIC [Title/Abstract]) OR GICs [Title/Abstract]))) AND ((((((((Composite resin [MeSH Terms]) OR composite resin [Title/Abstract]) OR Resin composite [Title/Abstract]) OR Composit resin [Title/Abstract]) OR Composit resins [Title/Abstract]) OR Resin composities [Title/Abstract]) OR Resin compomer [Title/Abstract])) |
| Scopus | (TITLE-ABS-KEY (“Root Caries”) OR TITLE-ABS-KEY (“Cervical Cary”) OR TITLE-ABS-KEY (“Cervical Caries”) OR TITLE-ABS-KEY (“Non carious cervical lesion”) OR TITLE-ABS-KEY (“Non-carious cervical lesion”) OR TITLE-ABS-KEY (“Cervical lesion”) OR TITLE-ABS-KEY (“Cervical lesions”)) AND (TITLE-ABS-KEY (“glass ionomer cements”) OR TITLE-ABS-KEY (“glass ionomer cements”) OR TITLE-ABS-KEY (“Glass-Ionomer Cement”) OR TITLE-ABS-KEY (“Glass Ionomer Cement”) OR TITLE-ABS-KEY (GIC) OR TITLE-ABS-KEY (GICs)) AND (TITLE-ABS-KEY (“Composite resin”) OR TITLE-ABS-KEY (“composite resin”) OR TITLE-ABS-KEY (“Resin composite”) OR TITLE-ABS-KEY (“Composit resin”) OR TITLE-ABS-KEY (“Composit resins”) OR TITLE-ABS-KEY (“Resin composities”) OR TITLE-ABS-KEY (“Resin compomer”)) |
| Web of Science | (TS=(“Root Caries”) OR TS=(“Cervical Cary”) OR TS=(“Cervical Caries”) OR TS=(“Non carious cervical lesion”) OR TS=(“Non-carious cervical lesion”) OR TS=(“Cervical lesion”) OR TS=(“Cervical lesions”)) AND (TS=(“glass ionomer cements”) OR TS=(“glass ionomer cements”) OR TS=(“Glass-Ionomer Cement”) OR TS=(“Glass Ionomer Cement”) OR TS=(GIC) OR TS=(GICs)) AND (TS=(“Composite resin”) OR TS=(“composite resin”) OR TS=(“Resin composite”) OR TS=(“Composit resin”) OR TS=(“Composit resins”) OR TS=(“Resin composities”) OR TS=(“Resin compomer”)) |
| Cochrane Library | ID Search Hits #1 Root Caries 408 #2 Cervical Caries 142 #3 Non carious cervical lesion 34 #4 Cervical lesion 582 #5 cervical lesions 1104 #6 #1 or #2 or #3 or #4 or #5 1825 #7 glass ionomer cements 802 #8 GIC 219 #9 Glass Ionomer Cement 595 #10 #7 or #8 or #9 1024 #11 Composite resin 2025 #12 Resin compomer 108 #13 #11 or #12 2036 #14 #6 and #10 and #13 64 |
2.2. Eligibility criteria
This review included randomized and controlled clinical trial studies and nonrandomized clinical studies comparing the clinical performance/longevity of CR and GIC (conventional and/or resin-modified) in the treatment of NCCL according to the following PICO strategy:
(P) - Problem: noncarious cervical lesion (NCCL);
(I) - Intervention: use of glass ionomer cement (GIC) (conventional and/or resin-modified);
(C) - Comparison: use of composite resin (CR);
(O) - Outcome: clinical performance/longevity of restorations, assessed as the presence of secondary carious lesions, marginal discoloration, marginal adaptation, color, surface texture, retention and anatomic form, according to the United States Public Health Service Home (USPHS)/Ryge and World Dental Federation (FDI) criteria. Item ‘O’ was not used in the search strategy to minimize the chances of missing articles.
Case reports, case series, in vitro studies, cohort studies, observational studies, literature reviews, letters to the editor and studies that did not meet the inclusion criteria were excluded. Also excluded were studies that evaluated the longevity of the materials used in the restorative treatment of dental carious lesions, including conventional cavity preparation (class I, II, III, IV) and root caries.
In addition, studies that used a sandwich restorative technique, studies in which the outcome was periodontal evaluation or performance of the adhesive system, studies that compared only GIC (chemical-activated versus light-activated) and studies that used only compomers and polyacid-modified resin as a restorative material were also excluded. For different studies that used the same samples, with the only difference being the evaluation time, the most recent study was used.
Reference management software (Mendeley Desktop, version 1.16.1, Mendeley Ltd., Elsevier Inc., NY, USA) was used for organizing the references and reading the titles and abstracts. After the duplicates were removed, two examiners (BMI and ACMB) classified the studies by reading the titles and abstracts. Articles that appeared to meet the inclusion criteria were analyzed in full, as well as articles in which the title and abstract did not contain sufficient information or the abstract was not available. After reading the selected articles in full, the results were compared. A third examiner (YWC) resolved any disagreement.
2.3. Data extraction
A spreadsheet was created to standardize the data to be extracted. In the spreadsheet, the following information was recorded: Authors, year, study design, sample size, intervention groups (including other restorative materials, when applicable), criteria used for clinical evaluation, number of losses to follow-up, evaluation time, outcomes (success rate based on the number of total restorations) and conclusion.
2.4. Assessment of the risk of bias in the studies
Two examiners (IMB and ACMB) independently assessed the risk of bias and the methodological quality of the selected studies by using the Cochrane Collaboration tool (http://handbook.cochrane.org) [14]. This tool is based on domains in which a critical evaluation of the risk of bias in intervention studies is performed for each domain. Seven domains are considered: (1) random sequence generation, (2) allocation concealment, (3) selective reporting, (4) blinding (participants and personnel), (5) blinding (outcome assessment), (6) incomplete outcome data and (7) other sources of bias. The criteria “Performance Bias (blinding of participants and personnel)” and “Detection Bias (blinding of outcome assessors)” were not considered key criteria due to the nature of the studies and the use of the restorative materials in question. Any disagreement during the assessment of risk of bias was resolved by consensus between the examiners, and when necessary, a third examiner (YWC) was consulted.
Each domain was evaluated according to the recommendations of the Cochrane Handbook, classifying the risk as “low” when there was low risk of bias, “high” when there as a high risk of bias and “unclear” when the information was insufficient or the question was left to the reader.
2.5. Meta-analysis (quantitative synthesis)
For MAs, the data were analyzed using the free software RevMan 5.3 (Review Manager v. 5, The Cochrane Collaboration; Copenhagen, Denmark). The MAs were performed according to each clinical parameter and were sub-grouped according to the follow-up time. The clinical parameters evaluated should follow the Ryge or USPHS criteria. Thus, seven MAs were conducted with data from 13 studies, where each MA was divided into two axes, considering clinical performance (assessed by the success rate, considering the Alpha + Bravo or Alpha only criteria, depending on how the data were reported in the articles) of the parameters in common: retention, marginal discoloration, marginal adaptation, secondary caries, color, anatomic form and surface texture and a follow-up time of 12, 24 and 36 months.
The data on the clinical parameters analyzed were dichotomized as “success” (based on the Alpha + Bravo or Alpha only criteria, depending on how the data were reported in the articles) or “failure” (Charlie criteria), according to the Modified USPHS Ryge Criteria for Direct Clinical Evaluation of Restoration [15].
One study [16] was not included in the MA because the criteria used was not reported and because of the 10-year evaluation period used. Similarly, other data obtained [14] were not used in the MA because they used FDI criteria for the evaluation. The data obtained in two articles [8, 17] were added because they evaluated the same sample at different evaluation times.
The prevalence of successful restorations and the total number of restorations per clinical parameter/follow-up time were used to calculate the risk difference, with a 95% confidence interval and statistical significance of 5%. Random-effects models were used, and heterogeneity was tested using the I2 index.
3. Results
3.1. Selection of studies
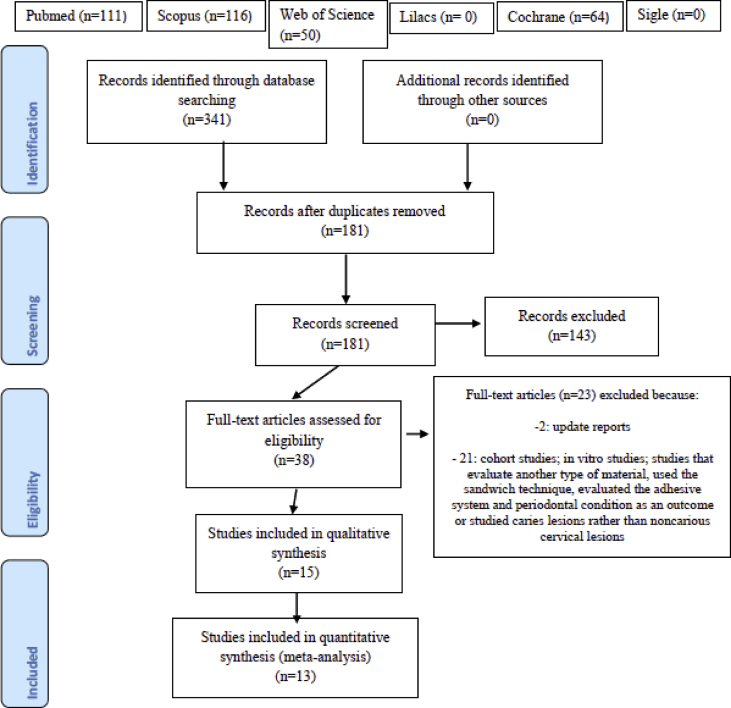
A total of 341 articles were initially identified, among which 181 were obtained after removal of duplicates. Of these, 46 articles remained as potentially eligible after careful reading of the titles and abstracts. After reading in full, 31 articles were excluded due to the type of study (cohort and in vitro), evaluation of other restorative material, the use of the sandwich technique, evaluation of the adhesive system and the periodontal condition as an outcome, evaluation of carious lesions instead of noncarious cervical cancer or because they were update reports. Thus, 15 articles remained for qualitative synthesis and 13 for quantitative synthesis (MAs) (Figure 1).
Figure 1.
Flow diagram of literature searches according to the PRISMA statement.
3.2. Characteristics of the articles included
The characteristics of the 15 studies included in the qualitative synthesis are listed in Table 2. Nine studies have an RCT split-mouth design [1, 5, 16, 18, 19, 20, 21, 22, 23], one study has an RCT parallel design [6] and five studies are split-mouth nonrandomized clinical trials [8,9,17,24,25,].
Table 2.
Data extraction from the included studies.
| Authors, Year | Study design | Sample size | Intervention groups | Evaluation criteria |
Lost to follow-up | Follow-up time | Results | Conclusion |
|---|---|---|---|---|---|---|---|---|
| Adeleke; Oginni. (2012) [18] | RCT (split-mouth design) | 336 lesions within 44 individuals | Resin-modified GIC n = 170; Composite resin n = 166 | USPHS | RC = 23; GIC = 26 (restorations) | 12 months | A + B: Retention: RC = 106/143, CIV = 131/144; Marg. Discoloration: RC = 105/105, CIV = 130/131; Marg. Adaptation: RC = 105/106, CIV = 131/131; Secondary caries: RC = 72/72, CIV = 117/117 | RMGIC demonstrated a higher retention rate than RC over a period of 12 months. |
| Brackett et al. (2003) [19] | RCT (split-mouth design) | 74 lesions within 24 individuals | Resin-modified GIC (Fuji II LC) n = 37; Composite resin (Z250) n = 37 | USPHS modified | RC = 10; GIC = 10 (restorations) | 12 months | A + B: Retention: RC = 26/31, CIV = 30/31; Color: RC = 26/26, CIV = 30/30; Marg Discoloration: RC = 26/26, CIV = 30/30; Secondary caries: RC = 26/26, CIV = 30/30; Anatomic Form: RC = 26/26, CIV = 30/30; Marg Adaptation: RC = 26/26, CIV = 30/30; Surface Texture RC = 26/26, CIV = 30/30; | No statistically significant difference was observed between the two restorative materials. Although not statistically compared, the RC restorations appear superior in color match to the RMGIC restorations. |
| 18 months | A + B: Retention: RC = 26/31, CIV = 30/31; Color: RC = 26/26, CIV = 30/30; Marg Discoloration: RC = 26/26, CIV = 30/30; Secondary caries: RC = 26/26, CIV = 30/30; Anatomic Form: RC = 26/26, CIV = 30/30; Marg Adaptation: RC = 26/26, CIV = 30/30; Surface Texture RC = 26/26, CIV = 30/30; | |||||||
| 24 months | A + B: Retention: RC = 22/27, CIV = 26/27; Color: RC = 22/22, CIV = 26/26; Marg Discoloration: RC = 22/22, CIV = 26/26; Secondary caries: RC = 22/22, CIV = 26/26; Anatomic Form: RC = 22/22, CIV = 26/26; Marg Adaptation: RC = 22/22, CIV = 26/26; Surface Texture RC = 22/22, CIV = 26/26; | |||||||
| Burgess et al. (2004) [9] | Nonrandomized clinical trial (split-mouth) | 120 lesions | Resin-modified GIC (Fuji II LC Improved) n = 30; Composite resin (Pertac III) n = 30; Composite resin (Synergy) n = 30; Compomer (Dyract AP) n = 30 | USPHS modified | 10% of the restorations were lost due to patients dropping out of the study. | 36 months | A + B: Retention: RC = 44/54, CIV = 24/27; Marg Discoloration: RC = 40/54, CIV = 21/27; Secondary caries: RC = 53/54, CIV = 27/27; Anatomic Form: RC = 48/54, CIV = 27/27; Marg Adaptation: RC = 17/54, CIV = 13/27; Surface Texture RC = 45/54, CIV = 17/27; | Pertac III and Fuji LC II Improved were significantly rougher than all other materials. Pertac III had significantly poorer marginal adaptation than other materials. |
| Celik; Tunac; Yilmaz. (2019) [1] | RCT (split-mouth design) | 134 lesions within 22 individuals | Resin-modified GIC (EQUIA Fil) n = 67; Composite resin (G-aenial) n = 67 | FDI criteria | RC = 13; GIC = 20 (restorations) | 12 months | Overall success rate: RC: 100%/Civ: 96% | The 3-year clinical performance of RC in NCCLs was better than that of GIC restorations. |
| 24 months | Overall success rate: RC: 100%/Civ: 91% | |||||||
| 36 months | Overall success rate: RC: 100%/Civ: 87% | |||||||
| De Oliveira et al. (2012) [20] | RCT (split-mouth design) | 124 lesions within 10 individuals | Resin-modified GIC (Fuji II LC) n = 40; Composite resin (Filtek Z350) n = 41; Primer + Resin-modified GIC (Scotch Bond Multi-Purpose + Fuji II LC) n = 43 | USPHS modified | 0 | 12 months | A + B: Retention: RC = 41/41 CIV = 38/40; Color: RC = 41/41, CIV = 38/40; Marg Discoloration: RC = 41/41, CIV = 38/40; Secondary caries: RC = 41/41, CIV = 38/40; Anatomic Form: RC = 41/41, CIV = 38/40; Marg Adaptation: RC = 41/41, CIV = 38/40 | The restorations performed with RMGIC and RC presented good clinical performance at 12 months. |
| Federlin et al. (1998) [21] | RCT (split-mouth design) | 48 lesions within 11 individuals | Resin-modified GIC (Fuji II LC) n = 16; Composite resin (Prisma TPH) n = 16; Compomer (Dyract) n = 16 | USPHS modified | 0 | 12 months | A + B: Color: RC = 15/15, CIV = 15/15; Marg Discoloration: RC = 15/15, CIV = 15/15; Secondary caries: RC = 15/15, CIV = 15/15; Anatomic Form: RC = 15/15, CIV = 15/15; Marg Adaptation: RC = 13/15, CIV = 15/15; Surface Texture: RC = 15/15, CIV = 15/15; Color: RC = 15/15, CIV = 15/15 | None of the materials studied revealed superiority over the other materials. |
| Franco et al. (2006) [17] | Nonrandomized clinical trial (split-mouth) | 70 lesions within 30 individuals | Resin-modified GIC (Vitremer) n = 35; Composite resin (Tetric Ceram) n = 35 | USPHS modified | RC = 8; GIC = 7 (restorations) | 12 months | A + B: Retention: RC = 30/35, CIV = 35/35; Marg Adaptation: RC = 30/30, CIV = 35/35; Marg Disc: RC = 30/30, CIV = 35/35; Anat Form: RC = 29/30, CIV = 35/35; Sec. Caries: RC = 30/30, CIV = 35/35 | After 5 years of evaluation, the clinical performance of RMGIC was superior to that of RC in restorations. |
| 24 months | A + B: Retention: RC = 26/33, CIV = 33/33; Marg Adaptation: RC = 26/26, CIV = 33/33; Marg Disc: RC = 26/26, CIV = 33/33; Anat Form: RC = 25/26, CIV = 33/33; Sec. Caries: RC = 26/26, CIV = 33/33 | |||||||
| 60 months | A + B: Retention: RC = 27/33, CIV = 27/28; Marg Adaptation: RC = 13/17, CIV = 23/27; Marg Disc: RC = 17/17, CIV = 27/27; Anat Form: RC = 15/17, CIV = 23/27; Sec. Caries: RC = 15/17, CIV = 27/27 | |||||||
| Hussainy et al. (2018) [6] | RCT (parallel design) | 101 lesions | Resin-modified GIC (Fuji II LC) n = 33; Composite resin (Filtek Z350 XT) n = 34; Polyacid-modified composite resin (Dyract Flow) n = 34 | USPHS | 0 | 12 months | A + B: Retention: RC = 32/34, CIV = 32/33; Marg Adaptation: RC = 32/34, CIV = 32/33; Marg Disc: RC = 32/34, CIV = 32/33; Color: RC = 32/34, CIV = 32/33; Sensitivity: RC = 32/34, CIV = 32/33 | RMGIC is superior regarding marginal adaptation and aesthetics for restoring NCCLs. |
| Matis; Cochran; Carlson. (1996) [16] | RCT (split-mouth design) | 120 lesions within 30 individuals | GIC (Ketac Fil) n = 60; GIC (Chelon Fil) n = 30; Composite resin (Cervident) n = 30 | Did not report the criteria | 12 individuals | 10 years | A + B: Retention: RC = 3/18, CIV = 46/54; Anat form: RC = 18/18, CIV = 45/54; Marg Adaptation: RC = 13/18, CIV = 44/54; Marg Disc: RC = 18/18, CIV = 52/54; Color: RC = 18/18, CIV = 51/54; Surface Texture: RC = 18/18, CIV = 53/54; Secondary caries: RC = 18/18, CIV = 54/54; Crazing: RC = 18/18, CIV = 45/54 | Glass ionomer materials are the restorative material of choice for abrasion/erosion lesions because of their long-term retention values. |
| Neo; Chew. (1996) [24] | Nonrandomized clinical trial (split-mouth) | 159 lesions within 18 individuals | GIC (Ketac-Fil) n = 50; Composite resin (Silux) n = 55; Sandwich technique (GIC: Ketac-Fil + RC: Silux) n = 54 | USPHS | 0 | 12 months | A + B: Retention: RC = 51/55, CIV = 50/50; Anat form: RC = 51/55, CIV = 50/50; Marg Adaptation: RC = 50/55, CIV = 48/50; Marg Disc: RC = 51/55, CIV = 50/50; Color: RC = 50/55, CIV = 47/50 | Lesions restored with RC exhibited the highest percentage of lost restorations. |
| 36 months | A + B: Retention: RC = 43/55, CIV = 48/50; Anat form: RC = 43/55, CIV = 47/50; Marg Adaptation: RC = 40/55, CIV = 47/50; Marg Disc: RC = 42/55, CIV = 47/50; Color: RC = 40/55, CIV = 43/50 | |||||||
| Onal; Pamir. (2005) [22] | RCT (split-mouth design) | 130 lesions within 30 individuals | Resin-modified GIC (Vitremer) n = 24; Composite resin (Valux Plus) n = 22; Polyacid-modified resin-based composites (Dyract AP) n = 46; Polyacid-modified resin-based composites (F2000) n = 38 | USPHS modified | RC = 2; GIC = 2 (restorations) | 12 months | A + B: Retention: RC = 20/20, CIV = 22/22; Anat form: RC = 20/20, CIV = 22/22; Marg Adaptation: RC = 20/20, CIV = 22/22; Marg Disc: RC = 20/20, CIV = 22/22; Color: RC = 20/20, CIV = 22/22; Surface RC = 20/20, CIV = 22/22; Secondary caries RC = 20/20, CIV = 22/22 | Vitremer, with its high retention rate, seems to be the most appropriate material for restoration of noncarious cervical lesions, although it does not have the aesthetic properties of resin-based composites. |
| 24 months | A + B: Retention: RC = 20/20, CIV = 22/22; Anat form: RC = 20/20, CIV = 22/22; Marg Adaptation: RC = 20/20, CIV = 22/22; Marg Disc: RC = 20/20, CIV = 22/22; Color: RC = 20/20, CIV = 22/22; Surface RC = 20/20, CIV = 22/22; Secondary caries RC = 20/20, CIV = 22/22 | |||||||
| Perdigão et al. (2012) [23] | RCT (split-mouth design) | 92 lesions within 33 individuals | Resin-modified GIC (Fuji II LC) n = 31; Resin-modified GIC (Ketac Nano) n = 30; Composite resin (Filtek Supreme Plus) n = 31 | USPHS modified | 14 restorations were unavailable for evaluation (RC = 4; GIC = 10) | 12 months | A: Retention: RC = 25/27, CIV = 51/51; Color: RC = 22/27, CIV = 41/51; Marginal Disc: RC = 22/27, CIV = 40/51; Sec. caries: RC = 25/27, CIV = 51/51; Wear: RC = 25/27, CIV = 50/51; Marginal Adaptation: RC = 23/27, CIV = 43/51; Postoperative sensitivity RC = 24/27, CIV = 49/51; Surface texture: RC = 25/27, CIV = 34/51 | The one-year retention rate was statistically similar for all adhesive materials. Nevertheless, enamel marginal deficiencies and color mismatch were more prevalent for Ketac Nano. The surface texture of Fuji II LC restorations deteriorated quickly. The survival rates were similar for the three types of restorations in NCCLs. |
| Popescu et al. (2016) [5] | RCT (split-mouth design) | 220 lesions within 45 individuals | Resin-modified GIC (Vitremer) n = 73; Composite resin (VersaFlo) n = 74; Sandwich technique (GIC: Vitremer + RC: VersaFlo) n = 73 | USPHS modified | 8 individuals (48 restorations) were unavailable for evaluation at 24 months | 12 months | A + B: Retention: RC = 58/58, CIV = 57/57; Color: RC = 56/58, CIV = 31/57; Marginal discoloration: RC = 51/58, CIV = 49/57; Marginal adaptation: RC = 51/58, CIV = 49/57; Anatomical form: RC = 58/58, CIV = 57/57; Sec. caries: RC = 0/58, CIV = 0/57 | |
| 18 months | A + B: Retention: RC = 57/58, CIV = 57/57; Color: RC = 51/58, CIV = 31/57; Marginal discoloration: RC = 37/58, CIV = 38/57; Marginal adaptation: RC = 40/58, CIV = 38/57; Anatomical form: RC = 58/58, CIV = 57/57; Sec. caries: RC = 0/58, CIV = 0/57 | |||||||
| 24 months | A + B: Retention: RC = 53/57, CIV = 54/57; Color: RC = 47/57, CIV = 31/57; Marginal discoloration: RC = 33/57, CIV = 32/57; Marginal adaptation: RC = 32/57, CIV = 32/57; Anatomical form: RC = 57/57, CIV = 57/57; Sec. caries: RC = 0/57, CIV = 0/57 | |||||||
| Powell; Johnson; Gordon. (1995) [25] | Nonrandomized clinical trial (split-mouth) | 116 lesions within 25 individuals | GIC (Ketac-Fil) n = 39; Composite resin (Silux Plus) n = 39; Sandwich technique (GIC: Vitrebond + RC: Silux Plus) n = 38 | USPHS modified | RC = 2; GIC = 2 (restorations) | 12 months | Clinically Acceptable: Color match: RC = 31/35, CIV = 31/34; Cavosurface Discoloration: RC = 34/35, CIV = 34/34; Surface Texture: RC = 35/35, CIV = 34/34; Sec caries: RC = 0/35, CIV = 1/34 | All the techniques resulted in restorations that were clinically acceptable for color match, marginal staining, surface texture, and caries development when evaluated at 3 years. |
| 24 months | Clinically Acceptable: Color match: RC = 35/38, CIV = 39/39; Cavosurface Discoloration: RC = 36/38, CIV = 39/39; Surface Texture: RC = 38/38, CIV = 39/39; Sec caries: RC = 5/38, CIV = 3/39 | |||||||
| 36 months | Clinically Acceptable: Color match: RC = 35/37, CIV = 35/37; Cavosurface Discoloration: RC = 31/37, CIV = 35/37; Surface Texture: RC = 37/37, CIV = 35/37; Sec caries: RC = 4/37, CIV = 2/37 | |||||||
| Santiago et al. (2010) [8] | Nonrandomized clinical trial (split-mouth) | 70 lesions within 30 individuals | Resin-modified GIC (Vitremer) n = 35; Composite resin (Tetric Ceram) n = 35 | USPHS modified | 2 individuals (4 restorations) were unavailable for evaluation at 24 months | 12 months | A + B: Retention: RC = 30/35, CIV = 35/35; Anat form: RC = 29/30, CIV = 35/35; Marg Adaptation: RC = 30/30, CIV = 35/35; Marg Disc: RC = 30/30, CIV = 35/35; Secondary caries RC = 30/30, CIV = 35/35 | RC showed an inferior clinical performance compared with RMGIC. In conclusion, in the present controlled clinical trial, the RMGIC showed a superior clinical effectiveness compared with the resin composite after 2 years of follow-up. |
| 24 months | A + B: Retention: RC = 26/33, CIV = 33/33; Anat form: RC = 25/26, CIV = 33/33; Marg Adaptation: RC = 26/26, CIV = 33/33; Marg Disc: RC = 26/26, CIV = 33/33; Secondary caries RC = 26/26, CIV = 33/33 |
The number of restorations ranged from 48 to 336, with the number of participants ranging from 10 to 44 in each study. In addition to the control group and the experimental group, eight studies had other groups that used other materials, such as compomers, polyacid-modified resin, primer with GIC or those using the sandwich technique (GIC as a base material + CR) [5, 6, 9, 20, 21, 22, 23, 24, 25].
The follow-up time ranged from 6 months to 10 years, and the data transcribed to the data extraction table (Table 2) included only results after 12 months of evaluation. The Modified USPHS criteria were the most widely used and were found in 13 studies. Only one study used the FDI criteria [1], and one study did not report the criteria used [16]. In all studies, with the exception of four, there were losses to follow-up during the follow-up period [6, 20, 21, 24].
3.3. Risk of bias of the included studies
To analyze the methodological quality of the studies, seven domains were evaluated that analyze various types of bias that can be found in randomized clinical trials, according to the Cochrane Collaboration tool.
Only four studies [1, 6, 16, 18] described in detail the method used for random sequence generation and allocation concealment, indicating low risk of bias. The other 11 studies did not describe in sufficient detail the method used for random sequence generation and allocation concealment and are therefore classified as “unclear risk of bias”. In some studies each patient received at least one restoration of each material evaluated [8, 9, 14, 17, 25]. Some authors was reported that the restorative materials were randomly assigned to the lesions, but they did not report the method [5, 19, 20, 21, 22, 23].
The selective reporting and incomplete outcome criteria had a low risk of bias for the 15 studies. Two studies were the only ones classified as “unclear risk of bias” for the criterion “Other sources of bias” because they did not inform the brand of the materials used and did not report age, teeth involved or study site [9, 18]. The other studies were classified as “low risk of bias” for this criterion. Regarding the blinding of participants, professionals and assessors involved in the research, these criteria were not considered key criteria due to the nature of the articles. The risk of bias in the 15 studies selected is shown in Table 3.
Table 3.
Quality assessment according to Cochrane Collaboration's.
|
Article |
Selection Bias |
Reporting Bias |
Performance Bias |
Detection Bias |
Attrition Bias |
Other Bias |
Total | |
|---|---|---|---|---|---|---|---|---|
| Random sequence generation | Allocation concealment | Selective reporting | Blinding (participants and personnel) | Blinding (outcome assessment) | Incomplete outcome data | Other sources of bias | ||
| Adeleke, Oginni. A (2012) [18] | low | low | low | low | low | low | unclear | 6 + |
| Brackett et al. (2003) [19] | unclear | unclear | low | low | low | low | low | 5 + |
| Burgess et al.(2004) [9] | unclear | unclear | low | low | low | low | unclear | 4 + |
| Celik; Tunac; Yilmaz. (2019) [1] | low | low | low | low | low | low | low | 7 + |
| De Oliveira et al. (2012) [20] | unclear | unclear | low | low | low | low | low | 5 + |
| Federlin et al. (1998) [21] | unclear | unclear | low | low | low | low | low | 5 + |
| Franco et al. (2006) and Santiago et al. (2010) [17,8] | unclear | unclear | low | low | low | low | low | 5 + |
| Hussainy et al. (2018) [6] | low | low | low | low | low | low | low | 7 + |
| Matis; Cochran; Carlson. (1996) [16] |
low | low | low | low | low | low | low | 7 + |
| Neo; Chew. (1996) [24] | unclear | unclear | low | low | low | low | low | 5 + |
| Onal; Pamir. (2005) [22] | unclear | unclear | low | low | low | low | low | 5 + |
| Perdigão et al. (2012) [23] | unclear | unclear | low | low | low | low | low | 5 + |
| Popescu et al. (2016) [5] | unclear | unclear | low | low | low | low | low | 5 + |
| Powell; Johnson; Gordon. (1995) [25] | unclear | unclear | low | low | low | low | low | 5 + |
| Total | 4 + | 4 + | 14 + | 14 + | 14 + | 14 + | 12 + | |
Risk of bias: low (+), high (-) or unclear (?).
3.4. Synthesis of results: meta-analysis
All MAs grouped only the data available for the clinical parameters in common, with follow-up times of 12, 24 and 36 months. Thus, each MA has a different number of studies. The data referring to the clinical parameters of the studies [9, 16, 23] that used different brands of the same materials were considered as only one data set.
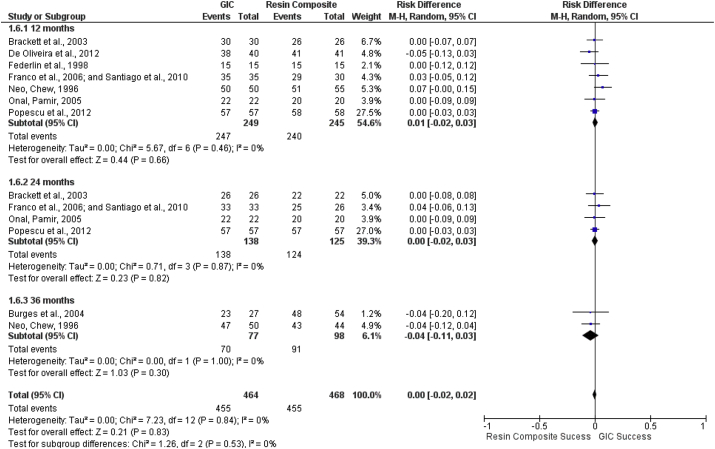
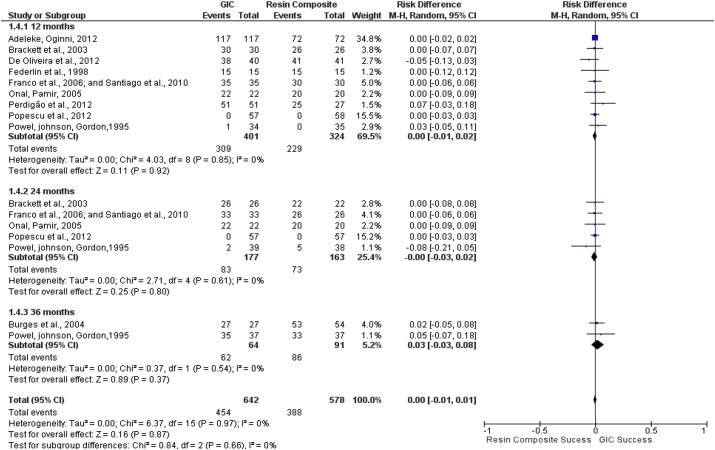
In the MA that analyzed the anatomic form (Figure 2), there was no significant difference between the two materials at any of the follow-up times and consequently in the final analysis. The risk difference (95% CI) for the anatomic form between GIC and CR was 0.00 (-0.02–0.02) (p = 0.83).
Figure 2.
Forest plot of the criterion anatomic form of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
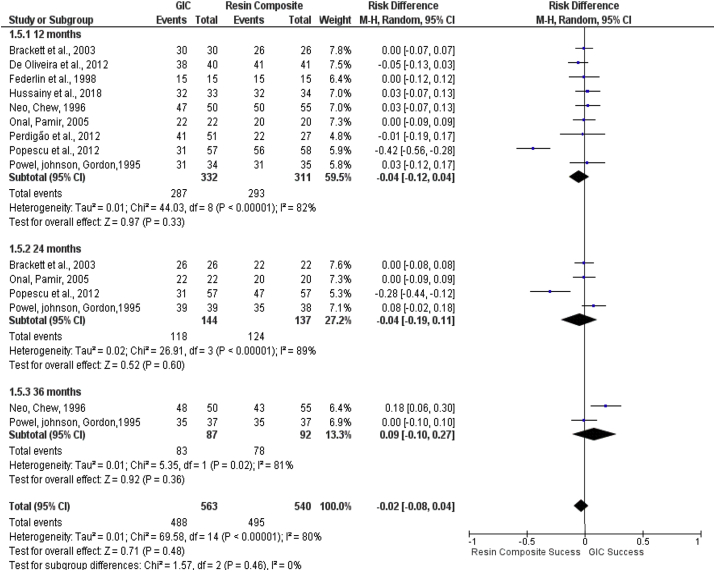
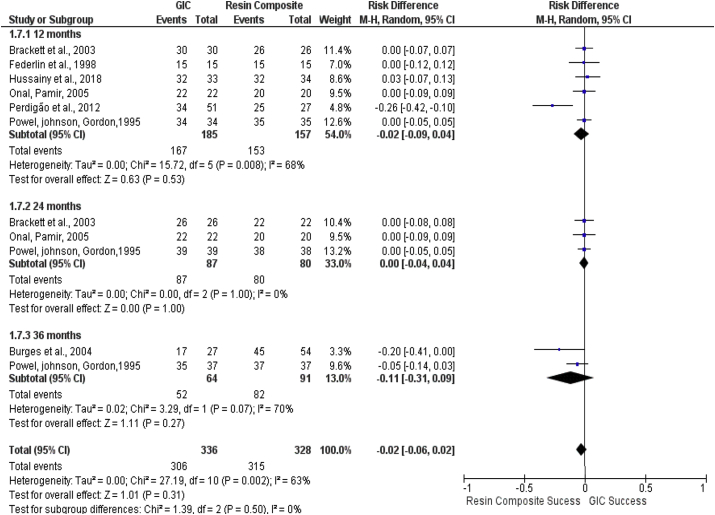
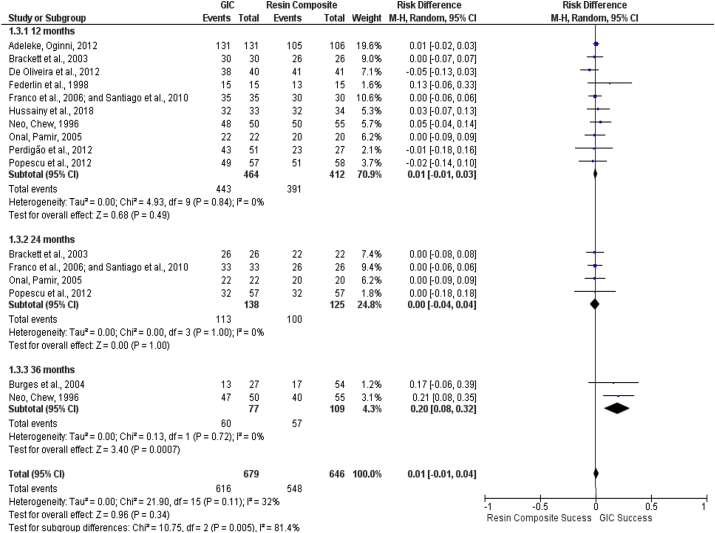
Evaluation of the parameters color (Figure 3), surface texture (Figure 4) and secondary caries (Figure 5) was performed and there was no difference in the behavior of the materials. The color and surface texture heterogeneity varied between 80 and 63%, and the risk difference (95% CI) was -0.02 (-0.08–0.04) (p = 0.48) and - 0.02 (-0.06–0.02) (p = 0.31), respectively. For the presence of secondary caries, the risk difference was 0, indicating low heterogeneity and risk difference (95% CI) of 0.00 (-0.01–0.01) (p = 0.87).
Figure 3.
Forest plot of the criterion color of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
Figure 4.
Forest plot of the criterion surface texture of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
Figure 5.
Forest plot of the criterion secondary caries of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
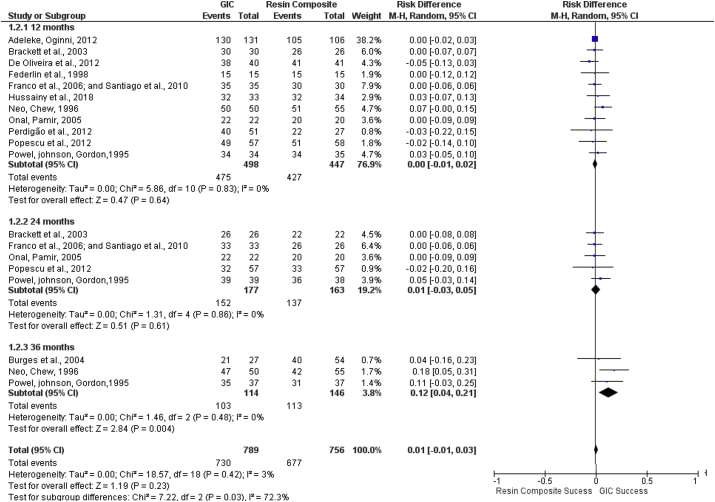
Regarding marginal discoloration (Figure 6) and marginal adaptation (Figure 7), only in the follow-up at 36 months was there a difference between the performance of the materials, with better results obtained from restorations with GIC, most likely due to the studies exhibiting a higher confidence interval at this follow-up time. However, in the final analysis, there was no difference between GIC and CR. The risk difference for marginal discoloration and marginal adaptation in the final analysis was 0.01 (-0.01–0.03) (p = 0.23) and 0.01 (-0.01–0.04) (p = 0.34), respectively, with low heterogeneity (3 and 32%).
Figure 6.
Forest plot of the marginal discoloration form of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
Figure 7.
Forest plot of the criterion marginal adaptation of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
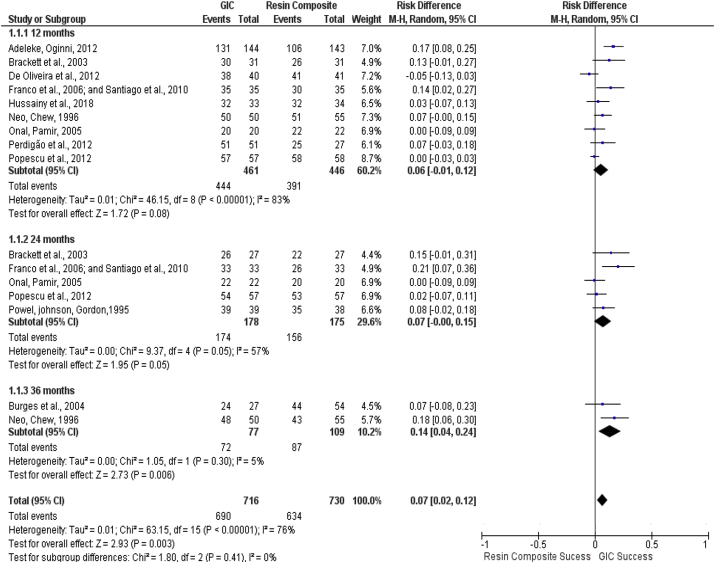
Regarding retention (Figure 8), GIC showed significantly better clinical performance than CR at the 36-month follow-up time and in the final analysis. The difference in clinical performance for retention (95% CI) in the final analysis between GIC and CR was 0.07 (0.02–0.12) (p = 0.003), and the heterogeneity obtained was considered high (76%). This was the only parameter in which one material showed superiority over another.
Figure 8.
Forest plot of the criterion retention of the NCCL restorations performed with glass ionomer cement and composite resin, subgrouped by the follow-up time at 12, 24 and 36 months. The blue squares indicate the mean of each study, and the error bars are the respective 95% confidence intervals. Black diamonds indicate the results of the subgrouped studies for a period of time, and the last diamond indicates the unified results of the three subgroups evaluated.
4. Discussion
Based on the articles included in this study, the results showed that the clinical performance of the analyzed materials (CR and GIC) was similar for most of the analyzed parameters (anatomic form, color, marginal discoloration, secondary caries, surface texture and marginal adaptation) in NCCLs. However, for the retention parameter, restorations performed with GIC presented significantly better clinical performance than those performed with CR. Seven MAs were conducted to independently evaluate each of these parameters in the follow-up periods at 12, 24 and 36 months. The difference in the adhesion mechanisms between the two materials may explain the better performance of GIC for retention than CR.
The chemical adhesion of GIC favors these results because degradation of the hybrid layer is still a clinical problem, and thus, the use of CR is not the best choice in NCCL restorations when considering the retention parameter [1, 17, 24]. The longevity of restorations determines one of the main evaluation criteria, therefore, resin-modified GIC are materials that can be indicated. The incorporation of light-cured resins improved its physical and mechanical properties.
As shown in the data extraction table (Table 2), of the 15 studies, five had a split-mouth nonrandomized clinical trial design, thus presenting an “unclear risk of bias” for the selection bias. Randomization is important because it allows the formation of balanced groups, avoiding biased allocation [14]. In studies that have a split-mouth design, allocation is likely more balanced, although randomization has not been used.
Three follow-up times (12, 24 and 36 months) were assessed to obtain more reliable results at different time points, because a time period of 12 months is a short time to evaluate adhesive materials; evaluation at longer follow-up times allows evaluation of the performance of the materials over time.
Only two studies used conventional GIC [16, 24] and thus, the results presented here on the performance of this type of material are more broadly applied to resin-modified GIC, likely due to its better aesthetic properties.
The criterion for the studies to be classified as eligible in this systematic review was that they should have a control group using CR and an experimental group using GIC (conventional or resin-modified). Studies that had a third group treated with another material in addition to the above two groups were included in the qualitative and quantitative synthesis; however, the third material was not taken into account.
The importance of the sandwich technique is noteworthy, and GIC is necessary to minimize the polymerization shrinkage that occurs with CR [24]. Although studies that used the sandwich technique as a control or experimental group were excluded from this review, studies in which there was an additional group and this group used this combination of materials remained eligible for inclusion in the review [5, 24, 25].
Most studies used the USPHS criteria, except for two. One of these studies used the FDI criteria, in which the restorations received a score of 1–5, where 1 to 3 means clinically acceptable and 4 or 5 represent failure, and the other study did not report the adopted criteria [1, 16]. The USPHS criteria evaluate restorations as follows: “Alpha” corresponds to excellent/acceptable restorations, “Bravo” corresponds to small but acceptable deviations, and “Charlie” corresponds to unacceptable restoration that can be repaired or restoration that needs to be replaced immediately [26]. Judgment of the parameters examined using this scale allows better comparability between studies in which restorations are clinically evaluated using standardized criteria [26]. According to the literature, the greatest problem in NCCLs is the retention factor [8, 17, 20, 24]. The lesions, in most cases, are small and shallow and contain dentinal tissue with sclerosis of the tubules, which is a tissue with higher mineral content that hinders adhesion. In addition, the location in the cervical region makes moisture control a challenge [1, 17, 24]. Thus, the clinical retention parameter evaluated in the studies showed differences when comparing the materials [16, 18, 20, 22, 24, 25].
The presence of sclerotic dentin causes total or partial obliteration of the dentinal tubules, thus the micromechanical adhesion of conventional/resin-modified GIC has shown better performance for the retention criterion.
The retention rate is one of the main indicators of the success of an NCCL restoration [5, 16, 22]. The MA that assessed retention identified GIC as superior to CR at the 36-month follow-up time point; however, the results of the final analysis corroborated those of the primary studies, indicating that GIC is superior to CR for the cited parameter [8, 16, 17, 18, 22, 24, 25]. Even with advances in adhesive techniques, the degradation experienced by the hybrid layer is still a clinical problem, and thus, CR is not the ideal material for NCCL restorations [17, 24].
The superiority of GIC in the retention of restorations can be attributed to the fact that materials with a low modulus of elasticity are more suitable for areas where there is a concentration of occlusal forces [22]. The combination of micromechanical adhesion mechanism and the addition of nanoparticles makes this material have better retentions rates [17].
CR has a higher modulus of elasticity than GIC, which is more sensitive to moisture and hydrolysis at the material/substrate interface [22, 24]. Additionally, several factors affect restorations, and the adhesive is considered an important factor to the longevity [7]. The location and size of the cavity also influence retention because most restorations that loosen are performed for small cavities [24].
The absence of enamel in the NCCLs contributes to deficient adaptation and pigmentation of the margins [6, 17]. The MA results obtained for the parameters marginal discoloration and alignment showed better performance for GIC at the 36-month follow-up time; however, in the final analysis, there was no difference, suggesting that the adhesive properties and the release of fluoride from GIC were equally satisfactory relative to the CR, and both materials had good sealing capacity.
The discoloration bothers the patients because it affects aesthetics. Due to the presence of filler particles, composite resins have a more homogeneous surface, but inadequate polymerization and sorption of oral fluids can explain the alteration of color [6]. The color stability of restorations is greatly influenced by correct polymerization in the case of resins and light-activated GIC because residual monomers undergo sorption of dyes and oral fluids and by satisfactory finishing and polishing [6, 20]. In only two studies, CR was superior [5, 19]. The remaining studies showed no difference in the color parameter, corroborating the results of the MA of this parameter, which showed no significant difference.
Anatomic form and surface texture are related to the adaptation of the material in the cavity and spaces that are formed during manipulation and/or insertion of the material [16]. These two parameters are also related to the wear resistance of the material [5, 22], and according to the MA, the two materials presented the same acceptance rate, which is related to their mechanical and physical properties.
With regard to heterogeneity, the retention (76%), color (80%) and surface texture (63%) MAs showed high heterogeneity. The MAs did not control the biases of each primary study individually. Therefore, in this case, the high heterogeneity can be attributed to the etiology of the lesions and differences in the teeth, the size of the lesions, the skill of the professional and/or evaluator and the commercial brand used because studies from 1995-2018 were included.
The similarity of the clinical materials tested in the present study indicates that both GIC and CR exhibit promising results. However, with regard to retention, GIC seems to be the more appropriate material. Results from this systematic review should be interpreted with care, since this summarized evidence included studies developed under different conditions. Some of the outcomes considered for this meta-analysis presented high heterogeneity, which suggests imprecision of the finding from previous studies.
Results from this meta-analysis are very similar to other recently published [27]. This previous report concluded that GIC presented better clinical performance than RC with regards to retention, whilst the surface texture was better for RC [27]. Differently, our study showed differences only for retention, in which GIC is favored. Similarly, included studies presented some unclear risk of evidence, which compromises the quality of evidence [27].
More recent clinical studies are likely to evaluate recent-launched products. However, little evidence is available for recent launched materials. Further well-designed clinical trials are necessary for evaluating the evidence of recently improved GIC and RC materials. This systematic review considered the whole variety of GIC and CR reported in the literature, unrespect of which brand was used. However, the results of this meta-analysis must be interpreted with care. Materials’ mechanical properties may vary significantly among the wide variety of GIC and RC. We are aware that recent GIC and RC have significantly improved, and improvement of clinical performance is expected. By considering retention as a key-factor for clinical success, mostly for NCCL, it is suggested that GIC restorations have better clinical performance/longevity than RC.
5. Conclusion
This systematic review showed a difference for only one clinical parameter, the retention of restorations. Among all the parameters evaluated in this study, the retention rates of resin-modified GIC were higher than composite resin restorations. The retention rate is the most important evaluation criteria, which is why Glass Ionomer Cements seem to be the most suitable material for restoring NCCL.
Declarations
Author contribution statement
I. Bezerra and A. Brito: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Y. Cavalcanti and L. Almeida: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
S. Sousa and B. Santiado: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
I. was supported by Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Finance Code 001, scholarship number: 1757970). A. Brito was supported by Conselho Nacional de Desenvolvimento Científico e Tecnológico (MSc Scholarship 130005/2018-5).
Competing interest statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Celik E.U., Tunac A.T., Yilmaz F. Three-year clinical evaluation of high-viscosity glass ionomer restorations in non-carious cervical lesions: a randomised controlled split-mouth clinical trial. Clin. Oral Invest. 2019;23:1473–1480. doi: 10.1007/s00784-018-2575-y. [DOI] [PubMed] [Google Scholar]
- 2.Loguercio A.D., Reis A., Barbosa A.N., Roulet J.F. Five-year double-blind randomized clinical evaluation of a resin-modified glass ionomer and a polyacid-modified resin in noncarious cervical lesions. J. Adhesive Dent. 2003;5:323–332. PMID: 15008339. [PubMed] [Google Scholar]
- 3.Rocha A.C., Da Rosa W.L.O., Cocco A.R., Da Silva A.F., Piva E., Lund R.-G. Influence of surface treatment on composite adhesion in noncarious cervical Lesions: systematic review and meta-analysis. Operat. Dent. 2018;43:508–519. doi: 10.2341/17-086-L. [DOI] [PubMed] [Google Scholar]
- 4.Moraschini V., Costa L.S., Santos G.O. Effectiveness for dentin hypersensitivity treatment of non-carious cervical lesions: a meta-analysis. Clin. Oral Invest. 2018;22:617–631. doi: 10.1007/s00784-017-2330-9. [DOI] [PubMed] [Google Scholar]
- 5.Popescu S.M., Tuculinã M.J., Manolea H.O., Mercut V., Scrieciu M. Randomized clinical trial of adhesive restorations in non carious cervical lesions. Key Eng. Mater. 2016;695:3–11. [Google Scholar]
- 6.Hussainy S.N., Nasim I., Thomas T., Ranjan M. Clinical performance of resin-modified glass ionomer cement, flowable composite, and polyacid-modified resin composite in noncarious cervical lesions: one-year follow-up. J. Conserv. Dent. 2018;21:510–515. doi: 10.4103/JCD.JCD_51_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Oz F.D., Kutuk Z.B., Ozturk C., Soleimani R., Gurgan S. An 18-month clinical evaluation of three different universal adhesives used with a universal flowable composite resin in the restoration of non-carious cervical lesions. Clin. Oral Invest. 2019;23:1443–1452. doi: 10.1007/s00784-018-2571-2. [DOI] [PubMed] [Google Scholar]
- 8.Santiago S.L., Passos V.F., Vieira A.H.M., Navarro M.F.L., Lauris J.R.P., Franco E.B. Two-Year clinical evaluation of resinous restorative systems in non-carious cervical lesions. Braz. Dent. J. 2010;21:229–234. doi: 10.1590/s0103-64402010000300010. [DOI] [PubMed] [Google Scholar]
- 9.Burgess J.O., Gallo J.R., Ripps A.H., Walker R.S., Ireland E.J. Clinical evaluation of four Class 5 restorative materials: 3-year recall. Am. J. Dent. 2004;17:147–150. [PubMed] [Google Scholar]
- 10.Moshaverinia M., Borzabadi-Farahani A., Sameni A., Moshaverinia A., Ansari S. Effects of incorporation of nano-fluorapatite particles on microhardness, fluoride releasing properties, and biocompatibility of a conventional glass ionomer cement (GIC) Dent. Mater. J. 2016;35:817–821. doi: 10.4012/dmj.2015-437. [DOI] [PubMed] [Google Scholar]
- 11.Gavic L., Gorseta K., Borzabadi-Farahani A., Tadin A., Glavina D., van Duinen R.N., Lynch E. Influence of thermo-light curing with dental light-curing units on the microhardness of glass-ionomer cements. Int. J. Periodontics Restor. Dent. 2016;36:425–430. doi: 10.11607/prd.2405. [DOI] [PubMed] [Google Scholar]
- 12.Gorseta K., Borzabadi-Farahani A., Moshaverinia A., Glavina D., Lynch E. Effect of different thermo-light polymerization on flexural strength of two glass ionomer cements and a glass carbomer cement. J. Prosthet. Dent. 2017;118:102–107. doi: 10.1016/j.prosdent.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 1.Moher D., Liberati A., Tetzlaff J., Altman D.G. The PRISMA group, preferred reporting Items for systematic reviews and meta-analyses : the PRISMA statement. PLoS Med. 2009;6:1–6. [PMC free article] [PubMed] [Google Scholar]
- 14.Higgins J.P.T., Altman D.G., Gotzsche P.C., Juni P., Moher D., Oxman A.D., Savic J., Schulz K.F., Weeks L., Sterne J.A.C. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:1–9. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bayne S., Schmalz G. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. Clin. Oral Invest. 2005;9:209–214. doi: 10.1007/s00784-005-0017-0. [DOI] [PubMed] [Google Scholar]
- 16.Matis B.A., Cochran M., Carlson T. Longevity of glass-ionomer restorative materials: results of a 10-year evaluation. Quintessence Int. 1996;27:373–382. PMID: 8941830. [PubMed] [Google Scholar]
- 17.Franco E.B., Benetti A.R., Ishikiriama S.K., Santiago S.L., Lauris J.R.P., Jorge M.F.F., Navarro M.F.L. 5-year clinical performance of resin composite versus resin modified glass ionomer restorative system in non-carious cervical lesions. Operat. Dent. 2006;31:403–408. doi: 10.2341/05-87. [DOI] [PubMed] [Google Scholar]
- 18.Adeleke, Oginni .A. Clinical evaluation of resin composite and resin-modified glass ionomer cement in non-carious cervical lesions. West. Afr. Coll. Surg. 2012;2:21–37. PMID: 25453001. [PMC free article] [PubMed] [Google Scholar]
- 19.Brackett W.W., Dib A., B Brackett M., A Reyes A., Estrada B.E. Two-year clinical performance of Class V resin-modified glass-lonomer and resin composite restorations. Operat. Dent. 2003;28:477–481. PMID: 14531590. [PubMed] [Google Scholar]
- 20.de Oliveira F.G., Machado L.S., Rocha E.P., de Alexandre R.S., Briso A.L.F., Mazza M.L.M.M., Sundfeld R.H. Clinical evaluation of a composite resin and a resin-modified glass-ionomer cement in non-carious cervical lesions: one-year results. Int. J. Clin. Dent. 2012;5:1–12. [Google Scholar]
- 21.Federlin M., Thonemann B., Schmalz G., Urlinger T. Clinical evaluation of different adhesive systems for restoring teeth with erosion lesions. Clin. Oral Invest. 1998;2:58–66. doi: 10.1007/s007840050046. 1998. [DOI] [PubMed] [Google Scholar]
- 22.Onal B., Pamir T. The two-year clinical performance of esthetic restorative materials in noncarious cervical lesions. J. Am. Dent. Assoc. 2005;136:1547–1555. doi: 10.14219/jada.archive.2005.0085. [DOI] [PubMed] [Google Scholar]
- 23.Perdigão J., Dutra-Corrêa M., Saraceni S.H.C., Ciaramicoli M.T., Kiyan V.H. Randomized clinical trial of two resin-modified glass ionomer materials: 1-year results. Operat. Dent. 2012;37:591–601. doi: 10.2341/11-415-C. [DOI] [PubMed] [Google Scholar]
- 24.Neo J., Chew C.L. Direct tooth-colored materials for noncarious lesions: a 3-year clinical report. Quintessence Int. 1996;27:183–188. PMID: 9063232. [PubMed] [Google Scholar]
- 25.Powell L.V., Johnson G.H., Gordon G.E. Factors associated with clinical success of cervical abrasion/erosion restorations. Operat. Dent. 1995;20:7–13. PMID: 8700767. [PubMed] [Google Scholar]
- 26.Hickel R., Roulet J.-F., Bayne S., Heintze S.D., Mjor I.A., Peters M., Rousson V., Randall R., Schmalz G., Tyas M., Vanherle G. Recommendations for conducting controlled clinical nt studies of dental restorative materials. J. Adhesive Dent. 2007;9(Suppl 1):121–147. doi: 10.1111/j.1875-595x.2007.tb00136.x. [DOI] [PubMed] [Google Scholar]
- 27.Boing T.F., de Geus J.L., Wambier L.M., Loguercio A.D., Reis A., Gomes O.M.M. Are glass-ionomer cement restorations in cervical lesions more long-lasting than resin-based composite resins? A systematic review and meta-analysis. J. Adhesive Dent. 2018;20:435–452. doi: 10.3290/j.jad.a41310. [DOI] [PubMed] [Google Scholar]