Abstract
Club drugs and alcohol abuse are prevalent among methadone maintenance treatment (MMT) patients. However, little is known about the association between these abuse and treatment outcomes among MMT patients. The aim of this study is to examine the prevalence of club drugs and alcohol abuse among MMT patientsand to investigate the associations between these abuse and treatment outcomes – drop-out and poor adherence. In this one-year cohort study conducting in Guangzhou, China, data including background characteristics, club drugs use in the last six months, alcohol use history and treatment-related information was collected. Cox regression analyses and log-binomial regression analyses were applied to identify the associations between these abuse and drop-out and poor adherence respectively. Thirty-seven participants (9.2%) admitted to the use of at least one type of club drugs in the last six months and eighty-eight (21.9%) were identified as alcohol abusers. Of all participants, 21.0% had dropped out of treatment and 27.7% exhibited poor adherence during the study period. Adjusting for significant background variables, use of at least one type of club drugs [hazards ratio (HR) = 1.90, 95% confidence Interval (CI) = 1.01–3.56] and use of methamphetamine in the last six months (HR = 2.26, 95%CI = 1.15–4.43) significantly predicted drop-out. Frequency of having six or more drinks on one drinking occasion when drinking [risk ratio (RR) = 1.87, 95% CI = 1.16–2.95] significantly predicted poor adherence. Our findings indicated that club drugs and alcohol abuse predicted drop-out and poor adherence among MMT patients. Early identification and intervention for the abuse should be taken into consideration when developing interventions tailored to improve treatment outcomes among MMT patients.
Keywords: Methadone maintenance treatment, drop-out, adherence, club drugs, alcohol
Introduction
Methadone maintenance treatment (MMT) is a substitution therapy for opioid addiction and has developed rapidly worldwide (Joseph, Stancliff & Langrod, 2000). Since 2004, China formally started MMT as a treatment programme and this initiative effectively curbed the spread of the HIV epidemic among drug users (Pang et al., 2007). In MMT, medication adherence is necessary to ensure the full effects (Jaremko, Sterling & Van Bockstaele, 2015). However, the requirement for long-term or even life-long daily attendance has led to poor adherence and high drop-out rates among MMT patients (Mattick, Breen, Kimber, & Davoli, 2014).
Studies consistently indicate that socio-demographic characteristics (e.g., age, sex and income), treatment-related characteristics (e.g., methadone dosage) and continued heroin use during treatment are associated with MMT drop-out and poor adherence (Cao et al., 2014; Proctor et al., 2015; White et al., 2014; Zhang et al., 2013). Drug users’ additive behaviours cluster with each other. Studies showed that multiple substance use, especially club drugs (e.g., methamphetamine and ketamine) and alcohol abuse, is popular among heroin users in recently years (Alam-mehrjerdi & Abdollahi, 2015; Dobler-Mikola et al., 2005; Wang et al., 2015). However, very few studies investigated the association between club drugs and alcohol abuse and treatment outcomes among MMT patients.
To fill this gap, this prospective cohort study aimed to investigate the prevalence of club drugs abuse and alcohol abuse among MMT patients in Guangzhou, and to assess how they predict drop-out and poor adherence among the patients during the one-year follow up period. We hypothesized that a significant proportion of MMT patients were using club drugs or alcohol; MMT patients exhibiting club drugs abuse or alcohol abuse would be more likely to drop out from MMT programme or to have poor treatment adherence.
Methods
Study participants
Participants of this prospective cohort study were recruited in August 2013 in four of the nine MMT clinics in Guangzhou city, and were followed up for a year. Eligible participants should be aged at least 18 years old, active heroin users prior to treatment, registered Guangzhou residents and could provide informed consents. Participants who intended to leave Guangzhou in the coming year were excluded. A total of 438 participants were approached, among whom 406 agreed to participate in the study and 401 finished the interview.
Measurements and outcomes
After informed consent, face-to-face interviews using structured questionnaires were conducted by trained interviewers. Data on socio-demographic characteristics, history of drug abuse and treatment-related characteristics were collected (Table 1). One statement was used to assess the abuse of club drugs: “Have you used any of the club drugs listed below in the last six months?” The studied club drugs included methamphetamine, ketamine, ecstasy, MaGu (methamphetamine and caffeine as main components), and triazolam, which are commonly used in China according to our literature review (Ding, He & Detels, 2013; Yang & Xia, 2010). A three-item Chinese version of the Alcohol Use Disorder Identification Test-Consumption (Ch-AUDIT-C) scale was used to measure alcohol abuse of MMT patients (Yip et al., 2015). Participants with a score ≥ 4 (male) or ≥ 3 (female) were identified as alcohol abusers (Delaney et al., 2014).
Table 1.
Background characteristics of all participants (n=401)
| n | % | |
|---|---|---|
| Socio-demographic characteristics | ||
| Sex | ||
| Male | 351 | 87.5 |
| Female | 50 | 12.5 |
| Age group | ||
| <40 | 117 | 29.2 |
| ≥40 | 284 | 70.8 |
| Education level attained | ||
| Primary or below | 98 | 24.4 |
| Junior high | 221 | 55.1 |
| Senior high or above | 82 | 20.5 |
| Current marital status | ||
| Single | 138 | 33.2 |
| Married or cohabitation | 215 | 53.6 |
| Divorced or other | 53 | 13.2 |
| Current employment status | ||
| No | 225 | 56.1 |
| Yes (full-time or part-time) | 176 | 43.9 |
| HIV infection status | ||
| No | 387 | 96.5 |
| Yes | 14 | 3.5 |
| Drug use history | ||
| Age of first drug use (years) | ||
| <20 | 85 | 21.2 |
| ≥20 | 316 | 78.8 |
| Ever injected drugs | ||
| No | 75 | 18.7 |
| Yes | 326 | 81.3 |
| Number of times of compulsory drug detoxification | ||
| 0 | 61 | 15.2 |
| 1–2 | 223 | 55.6 |
| ≥3 | 117 | 29.2 |
| Treatment-related characteristics | ||
| Duration of MMT(year) | ||
| 0 | 65 | 16.2 |
| 1–2 | 183 | 45.6 |
| ≥3 | 153 | 38.2 |
| Being transferred from other MMT clinics | ||
| No | 362 | 90.3 |
| Yes | 39 | 9.7 |
| Ever re-admitted to MMT | ||
| No | 355 | 88.5 |
| Yes | 46 | 11.5 |
| Average daily dose of methadone during the survey (mg/day) | ||
| <60 | 203 | 50.6 |
| ≥60 | 198 | 49.4 |
Participants’ daily treatment records since recruitment to August 31, 2014 were extracted from the MMT treatment information system. Drop-out was defined as not having visited the clinic for at least thirty consecutive days prior to the study’s completion date. We also used the outcome of poor adherence, which was defined as either being a drop-out case or having attended the MMT clinic for less than 50% of the follow-up period to cover intermittent MMT use cases.
Statistical analyses
Univariate Cox regression models were fitted to identify background variables that were associated with drop-out; variables with P<0.1 were used as candidates of a forward stepwise multivariate Cox regression model. Significant variables with P<0.05 were identified as potential confounders and were adjusted in another set of Cox regression models, using club drugs and alcohol abuse as independent variables respectively to predict drop-out. Similar approaches were applied using log-binomial regression models to predict poor adherence. Hazard Ratio (HR) and Relative risk (RR) with their 95% confidence intervals (CIs) were estimated. All P -values were two-sided. All statistical analyses were performed using the SAS software version 9.2 (SAS, Cary, NC).
Results
Background characteristics of study participants
Profiles of all participants are shown on Table 1. Thirty-seven participants (9.2%) admitted to the use of at least one type of club drugs in the last six months. The use rates of methamphetamine, MaGu, ketamine, triazolam and ecstasy in the last six months were 31 (7.7%), 8 (2.0%), 5 (1.2%), 4 (1.0%) and 4 (1.0%) respectively. Approximately half (47.6%) had ever consumed alcohol. Overall, eighty-eight (21.9%) participants exhibited alcohol abuse (male 22.2%, female 20.0%).
Incidence of drop-out and predictors
Eighty-four [21.0%; 95% CI: (17.1%, 25.3%)] participants dropped out from MMT during the study period. The estimated probabilities of dropping out were presented in Fig. 1. In multivariate Cox regression model, current marital status (divorced or other versus single: HR = 2.10, 95%CI = 1.13–3.89; P = 0.019; data not tabulated) and times of compulsory drug detoxification (three times or more versus never: HR = 0.36, 95%CI = 0.16–0.83; P = 0.017) were significant background preditors of drop-out. After adjusting for the two significant covariates, use of at least one type of club drugs in the last six months (yes versus no: HR = 1.90, 95%CI = 1.01–3.56; P = 0.047) and use of methamphetamine in the last six months (yes versus no: HR = 2.26, 95%CI = 1.15–4.43; P = 0.017) significantly predicted drop-out (Table 2).
Figure 1.
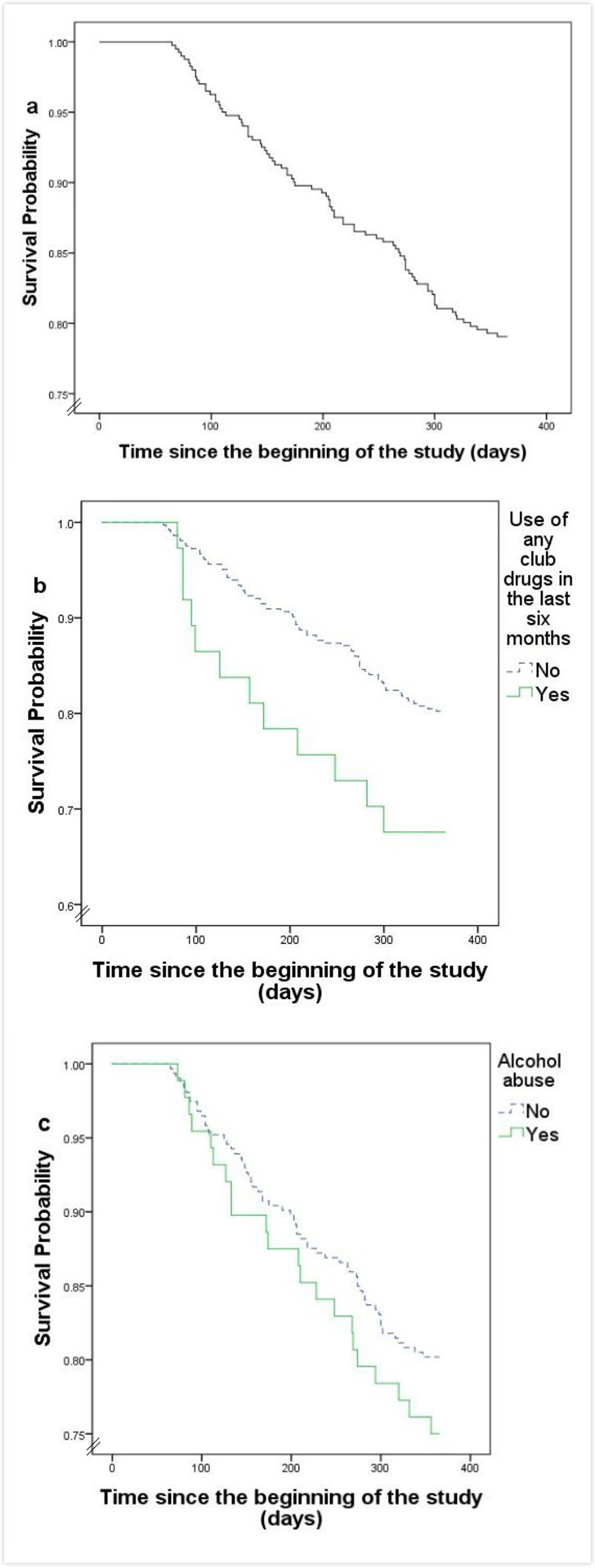
a The survival curve of all study participants.
b The survival curve of study participants grouped by club drugs abuse status.
c The survival curve of study participants grouped by alcohol abuse status.
Table 2.
Using club drugs and alcohol abuse to predict drop-out (Cox regression analyses, n=401)
| Univariate | Adjusted for significant background variablesa | ||||
|---|---|---|---|---|---|
| Row % | HR(95%CI) | P-value | HR(95%CI) | P-value | |
| Club drug abuse | |||||
| Use of any of the club drugs in the last six months | |||||
| No | 19.8 | 1.00 | 1.00 | ||
| Yes | 32.4 | 1.86 (1.01, 3.42) | 0.047 | 1.90 (1.01, 3.56) | 0.047 |
| Use of methamphetamine in the last six months | |||||
| No | 19.7 | 1.00 | 1.00 | ||
| Yes | 35.5 | 2.13 (1.13, 4.02) | 0.019 | 2.26 (1.15, 4.43) | 0.017 |
| Use of Ma Gu in the last six months | |||||
| No | 20.6 | 1.00 | 1.00 | ||
| Yes | 37.5 | 2.11 (0.67, 6.68) | 0.204 | 1.79 (0.55, 5.80) | 0.334 |
| Use of Triazolam Tablets in the last six months | |||||
| No | 20.9 | 1.00 | 1.00 | ||
| Yes | 25.0 | 1.26 (0.18, 9.06) | 0.817 | 1.51 (0.21, 10.97) | 0.684 |
| Use of ketamine in the last six months | |||||
| No | 21.0 | 1.00 | 1.00 | ||
| Yes | 20.0 | 0.97 (0.14, 6.98) | 0.977 | 0.91 (0.12, 6.78) | 0.926 |
| Use of ecstasy in the last six months | |||||
| No | 20.9 | 1.00 | 1.00 | ||
| Yes | 25.0 | 1.26 (0.18, 9.06) | 0.817 | 1.63 (0.22, 12.23) | 0.635 |
| Alcohol abuse | |||||
| Overdrinking | |||||
| No | 19.8 | 1.00 | 1.00 | ||
| Yes | 25.0 | 1.30 (0.80, 2.12) | 0.290 | 1.17 (0.72, 1.92) | 0.519 |
| Drinking frequency | |||||
| Never | 21.9 | 1.00 | 1.00 | ||
| At least once | 19.9 | 0.89 (0.58, 1.37) | 0.603 | 0.84 (0.54, 1.29) | 0.421 |
| Drinks on a typical day when drinking | |||||
| 1–2 drinks | 17.3 | 1.00 | 1.00 | ||
| ≥3 drinks | 24.2 | 1.50 (0.78, 2.88) | 0.229 | 1.38 (0.71, 2.69) | 0.335 |
| Frequency of having 6 or more drinks on 1 occasion when drinking | |||||
| Never | 16.2 | 1.00 | 1.00 | ||
| At least once | 27.8 | 1.85 (0.96, 3.56) | 0.067 | 1.94 (1.00, 3.78) | 0.051 |
Cox regression models adjusting for potential confounders (current marital status and number of times of compulsory drug detoxification), which predicted drop-out significantly at end of the study in a multivariate model (stepwise). HR: hazards ratio; CI: confidence interval.
Incidence of poor adherence and predictors
One hundred and eleven [27.7%; 95%CI: (23.4%, 32.3%)] participants exhibited poor adherence. In multivariate log-binomial regression model, being transferred from other clinics (yes versus no: RR = 1.96, 95%CI = 0.99–3.86; P = 0.049) was significantly associated with poor adherence. In Table 3, after adjusting for being transferred from other clinics, frequency of having six or more drinks on one drinking occasion significantly predicted poor adherence (at least once versus never: RR = 1.87, 95%CI = 1.16–2.95; P = 0.018).
Table 3.
Using club drugs and alcohol abuse to predict poor adherence (log-binomial analyses, n=401)
| Univariate | Adjusted for significant background variableb | ||||
|---|---|---|---|---|---|
| Row % | PR(95%CI) | P-value | RR(95% CI) | P-value | |
| Club drug abuse | |||||
| Use of any of the club drugs in the last six months | |||||
| No | 27.2 | 1.00 | 1.00 | ||
| Yes | 32.4 | 1.19 (0.68, 1.85) | 0.485 | 1.19 (0.68, 1.83) | 0.490 |
| Use of methamphetamine in the last six months | |||||
| No | 27.0 | 1.00 | 1.00 | ||
| Yes | 35.5 | 1.31 (0.74, 2.04) | 0.289 | 1.33 (0.75, 2.06) | 0.256 |
| Use of Ma Gu in the last six months | |||||
| No | 27.5 | 1.00 | 1.00 | ||
| Yes | 37.5 | 1.36 (0.40, 2.66) | 0.503 | 1.26 (0.37, 2.43) | 0.614 |
| Use of Triazolam Tablets in the last six months | |||||
| No | 27.7 | 1.00 | 1.00 | ||
| Yes | 25.0 | 0.90 (0.06, 2.66) | 0.906 | 0.95 (0.06, 2.82) | 0.955 |
| Use of ketamine in the last six months | |||||
| No | 27.8 | 1.00 | 1.00 | ||
| Yes | 20.0 | 0.72 (0.05, 2.30) | 0.715 | 0.57 (0.04, 1.87) | 0.538 |
| Use of ecstasy in the last six months | |||||
| No | 27.7 | 1.00 | 1.00 | ||
| Yes | 25.0 | 0.90 (0.06, 2.66) | 0.906 | 0.78 (0.05, 2.29) | 0.778 |
| Alcohol abuse | |||||
| Overdrinking | |||||
| No | 25.9 | 1.00 | 1.00 | ||
| Yes | 34.1 | 1.32 (0.91, 1.83) | 0.118 | 1.34 (0.93, 1.86) | 0.092 |
| Drinking frequency | |||||
| Never | 28.6 | 1.00 | 1.00 | ||
| At least once | 26.7 | 0.93 (0.68, 1.28) | 0.676 | 0.95 (0.69, 1.31) | 0.764 |
| Drinks on a typical day when drinking | |||||
| 1–2 drinks | 23.6 | 1.00 | 1.00 | ||
| ≥3 drinks | 32.3 | 1.37 (0.83, 2.19) | 0.201 | 1.35 (0.83, 2.16) | 0.214 |
| Frequency of having 6 or more drinks on 1 occasion when drinking | |||||
| Never | 21.3 | 1.00 | 1.00 | ||
| At least once | 38.9 | 1.82 (1.13, 2.89) | 0.011 | 1.87 (1.16, 2.95) | 0.018 |
Log-binomial regression models adjusting for potential confounders (transfer treatment), which predicted poor adherence significantly at end of the study in a multivariate model (stepwise). RR: relative risk; CI: confidence interval.
Discussion
This is one of the first studies using club drugs and alcohol abuse to predict drop-out and poor adherence among MMT patients. The findings (drop-out rate 21% and poor adherence rate 27.7%) were lower than those of other studies in China (drop-out rates ranging from 43% to 51.3%; poor adherence about 60%) (CHE et al., 2010; Gu et al., 2012; Lin, Hung, Peng, Chao, & Lee, 2015). It is possible as our study used a relatively broad definition of drop-out (30 days no MMT use) as compared to other studies (7 or 14 days no MMT use). Furthermore, our participants were current instead of newly recruited MMT users as in most other studies. Drop-out rates are known to be higher among patients in their first months of treatment (Strike et al., 2005).
In our study, patients who had used methamphetamine or any kind of club drugs in the last six months were 2.26 or 1.90 times more likely than others to drop out from MMT; patients who had six or more drinks during one drinking occasion for at least once were 1.87 times more likely than others to exhibit poor adherence. Drug users are in a context of syndemic of multiple risk behaviours (e.g., multiple substances use), psycho-social problems (e.g., depression, lacking of social support, social isolation) and diseases (e.g., HIV and HCV infection), which may lead to their poor coping ability and poor treatment compliance (González-Guarda, Florom-Smith & Thomas, 2011; Mizuno et al., 2015). The emergence of club drugs and alcohol abuse among MMT patients hence brings new challenges to current MMT programmes and highlights the needs for interventions (Shariatirad, Maarefvand & Ekhtiari, 2013).
In China, MMT clinics could service as a platform to reach drug users in community and provide holistic interventions incorporating multiple co-occuring conditions among MMT patients (Loeliger, 2016). MMT clinics could not only strengthen educational initiatives on the harm of club drugs and alcohol abuse, provide regular screening tests of club drugs and alcohol abuse, but also evaluate regularly patients’ physical and psycho-social status, and provide referral services (e.g., psychological treatment, AIDS treatment). Though there is a lack of manpower in medical staff to provide high quality comprehensive services in MMT clinics in China, there are also successful service models which incorporated methadone treatment with psycho-social services provided by social workers in MMT clinics (Gu et al., 2013; Lin et al., 2010).
There were several limitations of this study. Firstly, unidentified confounders might exist and confound the study’s conclusions. Secondly, the self-reported nature of club drugs use may result in bias due to the sensitivity of this topic. Thirdly, most of our participants have been on MMT for more than one year. Findings might not be applicable to newly-admitted MMT patients. Fourthly, the small sample size might result in potential sampling biases and limit the power to detect the predictive ability of some variables. Therefore, we should be careful about the generalizability of the findings. Lastly, our study involved only one city, limiting the generalizability of its findings.
In summary, our study has shown that club drugs and alcohol abuse are important problems in MMT clinics and may result in high drop-out rate and poor adherence without effective interventions. As MMT is the primary harm reduction programme controlling drugs abuse in China, holistic interventions to reduce club drugs and alcohol use among MMT patients are needed urgently. Further studies are required to evaluate evidence-based interventions that can improve treatment outcomes.
Acknowledgements:
The authors would like to thank all staff of the MMT clinics and all participants in the study.
Funding: This study was supported by the National Science and Technology Major Research Projects on Prevention and Control of Major Infectious Diseases (# 51000–41160002), NIH FIC Training Grant (# R25TW009345 and # R25TW009340).
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Alam-mehrjerdi Z, & Abdollahi M (2015). The Persian methamphetamine use in methadone treatment in Iran: implication for prevention and treatment in an upper-middle income country. DARU Journal of Pharmaceutical Sciences, 23(1). doi: 10.1186/s40199-015-0134-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao X, Wu Z, Rou K, Li L, Lin C, Wang C, … Li J (2014). Retention and its predictors among methadone maintenance treatment clients in China: A six-year cohort study. Drug and Alcohol Dependence, 145, 87–93. doi: 10.1016/j.drugalcdep.2014.09.776 [DOI] [PubMed] [Google Scholar]
- Che Y, Assanangkornchai S, McNeil E, Chongsuvivatwong V, Li J, Geater A, & You J (2010). Predictors of early dropout in methadone maintenance treatment program in Yunnan province, China. Drug and Alcohol Review, 29(3), 263–270. doi: 10.1111/j.1465-3362.2009.00157.x. [DOI] [PubMed] [Google Scholar]
- Delaney KE, Lee AK, Lapham GT, Rubinsky AD, Chavez LJ, & Bradley KA (2014). Inconsistencies between alcohol screening results based on AUDIT-C scores and reported drinking on the AUDIT-C questions: prevalence in two US national samples. Addiction Science & Clinical Practice, 9, 2. doi: 10.1186/1940-0640-9-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding Y, He N, & Detels R (2013). Circumstances of initiation into new-type drug use among adults in Shanghai: Are there differences by types of first new-type drug used? Drug and Alcohol Dependence, 131(3), 278–283. doi: 10.1016/j.drugalcdep.2012.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobler-Mikola A, Hattenschwiler J, Meili D, Beck T, Boni E, & Modestin J (2005). Patterns of heroin, cocaine, and alcohol abuse during long-term methadone maintenance treatment. Journal of Substance Abuse Treatment, 29(4), 259–265. doi: 10.1016/j.jsat.2005.08.002 [DOI] [PubMed] [Google Scholar]
- González-Guarda RM, Florom-Smith AL, & Thomas T (2011). A Syndemic Model of Substance Abuse, Intimate Partner Violence, HIV Infection, and Mental Health Among Hispanics. Public Health Nursing, 28(4), 366–378. doi: 10.1111/j.1525-1446.2010.00928.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu J, Lau JTF, Xu H, Zhong Y, Hao Y, Zhao Y, … Ling W (2013). A Randomized Controlled Trial to Evaluate the Relative Efficacy of the Addition of a Psycho-Social Intervention to Standard-of-Care Services in Reducing Attrition and Improving Attendance Among First-Time Users of Methadone Maintenance Treatment in China. AIDS and Behaviour, 17(6), 2002–2010. doi: 10.1007/s10461-012-0393-9 [DOI] [PubMed] [Google Scholar]
- Gu J, Xu H, Lau JT, Hao Y, Zhong Y, Fan L, …. Ling W (2012). Misconceptions predict dropout and poor adherence prospectively among newly admitted first-time methadone maintenance treatment clients in Guangzhou, China. Addiction, 107(9), 1641–1649. doi: 10.1111/j.1360-0443.2012.03859.x [DOI] [PubMed] [Google Scholar]
- Jaremko KM, Sterling RC, & Van Bockstaele EJ (2015). Psychological and physiological stress negatively impacts early engagement and retention of opioid-dependent individuals on methadone maintenance. Journal of Substance Abuse Treatment, 48(1), 117–127. doi: 10.1016/j.jsat.2014.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph H, Stancliff S, & Langrod J (2000). Methadone maintenance treatment (MMT): a review of historical and clinical issues. The Mount Sinai Journal of Medicine, New York, 67(5–6), 347–364. Retrieved from http://securingoursafety.org/wp-content/uploads/2013/08/Methadone-Maintenance-Treatment.pdf [PubMed] [Google Scholar]
- Lin C, Hung C, Peng C, Chao E, & Lee TS (2015). Factors Associated with Methadone Treatment Duration: A Cox Regression Analysis. PLoS One, 10(4), e123687. doi: 10.1371/journal.pone.0123687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin C, Wu Z, Rou K, Pang L, Cao X, Shoptaw S, & Detels R (2010). Challenges in providing services in methadone maintenance therapy clinics in China: Service providers’ perceptions. International Journal of Drug Policy, 21(3), 173–178. doi: 10.1016/j.drugpo.2009.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loeliger KB, Marcus R, Wickersham JA, Pillai V, Kamarulzaman A, & Altice FL (2016). The syndemic of HIV, HIV-related risk and multiple co-morbidities among women who use drugs in Malaysia: Important targets for intervention. Addictive Behaviours, 53, 31–39. doi: 10.1016/j.addbeh.2015.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattick RP, Breen C, Kimber J, & Davoli M (2014). Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. The Cochrane Database of Systematic Reviews, 2, D2207. doi: 10.1002/14651858.CD002207.pub4 [DOI] [PubMed] [Google Scholar]
- Mizuno Y, Purcell DW, Knowlton AR, Wilkinson JD, Gourevitch MN, & Knight KR (2015). Syndemic Vulnerability, Sexual and Injection Risk Behaviours, and HIV Continuum of Care Outcomes in HIV-Positive Injection Drug Users. AIDS and Behaviour, 19(4), 684–693. doi: 10.1007/s10461-014-0890-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pang L, Hao Y, Mi G, Wang C, Luo W, Rou K, … Wu Z (2007). Effectiveness of first eight methadone maintenance treatment clinics in China. AIDS, 21 Suppl 8, S103–S107. doi: 10.1097/01.aids.0000304704.71917.64 [DOI] [PubMed] [Google Scholar]
- Proctor SL, Copeland AL, Kopak AM, Hoffmann NG, Herschman PL, & Polukhina N (2015). Predictors of patient retention in methadone maintenance treatment. Psychology of Addictive Behaviours, 29(4), 906–917. doi: 10.1037/adb0000090 [DOI] [PubMed] [Google Scholar]
- Shariatirad S, Maarefvand M, & Ekhtiari H (2013). Methamphetamine use and methadone maintenance treatment: an emerging problem in the drug addiction treatment network in Iran. The International Journal on Drug Policy, 24(6), e115–e116. doi: 10.1016/j.drugpo.2013.05.003 [DOI] [PubMed] [Google Scholar]
- Strike CJ, Gnam W, Urbanoski K, Fischer B, Marsh DC, & Millson M (2005). Factors predicting 2-year retention in methadone maintenance treatment for opioid dependence. Addictive Behaviours, 30(5), 1025–1028. doi: 10.1016/j.addbeh.2004.09.004 [DOI] [PubMed] [Google Scholar]
- Wang R, Ding Y, Bai H, Duan S, Ye R, Yang Y, … He N (2015). Illicit Heroin and Methamphetamine Use among Methadone Maintenance Treatment Patients in Dehong Prefecture of Yunnan Province, China. PLoS One, 10(7), e133431. doi: 10.1371/journal.pone.0133431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White WL, Campbell MD, Spencer RD, Hoffman HA, Crissman B, & DuPont RL (2014). Patterns of abstinence or continued drug use among methadone maintenance patients and their relation to treatment retention. Journal of Psychoactive Drugs, 46(2), 114–122. doi: 10.1080/02791072.2014.901587 [DOI] [PubMed] [Google Scholar]
- Yang X, & Xia G (2010). Causes and consequences of increasing club drug use in China: a descriptive assessment. Substance Use & Misuse, 45(1–2), 224–239. doi: 10.3109/10826080903039827 [DOI] [PubMed] [Google Scholar]
- Yip BH, Chung RY, Chung VC, Kim J, Chan IW, Wong MC, …Griffiths SM (2015). Is Alcohol Use Disorder Identification Test (AUDIT) or its shorter versions more useful to identify risky drinkers in a Chinese population? A diagnostic study. PLoS One, 10(3), e117721. doi: 10.1371/journal.pone.0117721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang L, Chow EP, Zhuang X, Liang Y, Wang Y, & Tang C, et al. (2013). Methadone maintenance treatment participant retention and behavioural effectiveness in China: a systematic review and meta-analysis. PLoS One, 8(7), e68906. doi: 10.1371/journal.pone.0068906 [DOI] [PMC free article] [PubMed] [Google Scholar]


