Abstract
Background
The aim was to investigate if fatty acid profile and estimated desaturase activities; stearoyl CoA-desaturase (SCD), delta-5-desaturase and delta-6-desaturase (D5D; D6D), differ between individuals with metabolically healthy (MH) and unhealthy (MU) phenotypes. We also explored these associations according to BMI categories.
Methods
Men and women at moderately elevated risk of cardiovascular disease were included in this cross-sectional study (n = 321). If subjects met ≥4 out of 5 criteria (elevated triglycerides, total and LDL-cholesterol, HbA1c and low HDL-cholesterol), they were classified as MU (n = 52). If levels were within reference ranges for ≥3 of the same criteria, subjects were classified as MH (n = 150). Utilizing the entire population, a score ranging from 0 to 5 denoting the number of MU criteria met was computed. Estimated desaturase activities were calculated as product-to-precursor ratio of fatty acids in whole blood (SCD16 [16:1n7/16:0], SCD18 [18:1n9/18:0], D5D [18:3n6/18:2n6], D6D [20:4n6/20:3n6]).
Results
Individuals with MH had lower estimated SCD16 and SCD18 activities, whereas estimated D6D activity was higher compared to MU. Similar, SCD16 and SCD18 increased, whereas D6D decreased with increasing criteria of MU. Trends were similar across BMI categories.
Conclusions
This study supports the notion of estimated desaturase activities as possible novel biomarkers of metabolic health irrespectively of BMI.
Keywords: Fatty acids, Desaturases, Obesity, Metabolic disease, Stearoyl CoA desaturase, SCD1, D5D, D6D
Introduction
Cardiometabolic disorders, including type 2 diabetes (T2D) and cardiovascular disease (CVD) remain the major contributors to the global burden of disease [1]. Obesity is an important risk factor for cardiometabolic disorders, and is thus associated with insulin resistance, glucose intolerance and dyslipidemia [2]. However, not all obese individuals fit into this traditional phenotype, and a subgroup has been described with metabolically healthy (MH) obesity [3, 4]. Compared with metabolically unhealthy (MU) obesity, the MH obesity phenotype has a favorable lipid profile and a normal to slightly reduced insulin sensitivity, despite similar body mass index (BMI). Comparable patterns have been observed among individuals with overweight (BMI 25–30 kg/m2). Normal weight individuals (BMI 20–25 kg/m2) are generally considered MH, but MU normal weight individuals also exist [5, 6]. In an American population, about 2/3 were considered MU despite normal weight [7].
The fatty acid (FA) profile in the circulation is influenced by dietary and lifestyle factors [8, 9], and an unfavorable FA profile has been suggested to predict risk of T2D, CVD and the metabolic syndrome (MetS) [10–14]. Some FAs can be produced endogenously through de novo lipogenesis [15]. Stearoyl-CoA desaturase-1 (SCD1) is a rate-limiting enzyme in catalyzing the desaturation of monounsaturated fatty acids (MUFAs) from saturated fatty acids (SFAs). Delta-5-desaturase (D5D) and delta-6-desaturase (D6D) catalyze production of polyunsaturated fatty acids (PUFAs) (Table 1).
Table 1.
Stearoyl-CoA desaturase-1 (SCD1), Delta-5-desaturase (D5D) and Delta-6-desaturase (D6D) with purpose, precursor, product and estimated desaturase activity
| Desaturase enzyme name | Purpose | Precursor | Product | Estimated desaturase activity |
|---|---|---|---|---|
| SCD1 | Desaturation of monounsaturated fatty acids from saturated fatty acids | |||
| SCD16 | C16:0 (palmitic acid) | C16:1n7 (palmitoleic acid) | 16:1n7/16:0 | |
| SCD18 | C18:0 (stearic acid) | C18:1n9 (oleic acid) | 18:1n9/18:0 | |
| D6D | Desaturation of polyunsaturated fatty acids (PUFAs) | C18:2n6 (linoleic acid) | C18:3n6 (γ-linolenic acid) | 18:3n6/18:2n6 |
| D5D | Desaturation of polyunsaturated fatty acids (PUFAs) | C20:3n6 (dihomo-γ-linolenic acid) | C20:4n6 (arachidonic acid) | 20:4n6/20:3n6 |
An altered FA profile with a high proportion of C16:0 (palmitic acid) increased estimated SCD1 and D6D activities and decreased levels of C18:2n6 FA (linoleic acid) and estimated D5D activity have been associated with insulin resistance, CVD, obesity and development of MetS [16, 17]. Particularly the positive correlation between SCD1 activity, insulin resistance and fat mass has been observed both in animal models and in large human cohorts where SCD1 activity is estimated as product-to-precursor ratios in blood [17–19]. However, it is not known whether alterations in plasma FA profile and desaturase activity is associated with metabolic phenotypes independently of body mass. Hence, the objective of this study was to advance our understanding of the role of FA profile and estimated desaturase activities for the metabolic risk profile (MH and MU) in otherwise healthy subjects over different BMI categories.
Methods
Study population
The population was obtained from the Vascular lifestyle-Intervention and Screening in phArmacies (VISA)-study previously described in detail [20]. In short, a subset of 1318 individuals were screened and 582 with moderately elevated CVD risk participated in an 8-week randomized controlled trial (RCT) of lifestyle changes [21]. Of the 582 participants, 321 individuals were followed up one year after the RCT, and were accordingly included in the present cross-sectional study.
Subjects were ≥ 18 years and had BMI between 18.5 and 44.4 kg/m2. Importantly, despite moderately elevated risk factors for CVD, all subjects were free of CVD and did not use any medications known to affect serum levels of lipids, glucose, blood pressure or inflammatory markers. Subjects were characterized according to metabolic health phenotypes based mainly on the criteria of Karelis et al. [22]. Subjects were considered MH when fulfilling at least three of the following five criteria: fasting triglycerides < 1.7 mmol/l or < 2.1 mmol/l non fasting, total cholesterol < 5.2 mmol/L, low density lipoprotein-cholesterol (LDL-C) < 2.6 mmol/L, high density lipoprotein-cholesterol (HDL-C) > 1.3 mmol/L and hemoglobin Ab1c (HbA1c) < 5.7%. Subjects were considered MU when fulfilling at least four out of the five following criteria: triglycerides ≥1.7 mmol/L or ≥ 2.1 mmol/L (if not fasting), total cholesterol ≥5.2 mmol/L, LDL-C ≥ 2.6 mmol/L, HDL-C ≤ 1.3 mmol/L and HbA1c ≥5.7%. Using measured weight and height, BMI was calculated as weight (kg) divided by the square of height (m2). We defined normal weight, overweight and obese (BMI ≥ 30 kg/m2), according to the definition by World Health Organization [23]. To make use of data from the entire population, we computed a score based on criteria for MU ranging from 0 to 5 depending on the number of criteria met.
Anthropometric measures
Data collection was performed by pharmacy staff (pharmacists, technicians or nurses), in accordance with standard operational procedures [20]. Prior to the study, pharmacy staff completed a training program consisting of online e-learning courses and practical training. Subjects were weighed in light clothing without shoes using a digital scale. Height was measured with standing, erect posture and feet against the wall with a wall mounted height board. Blood pressure was measured twice after resting for about five minutes, using A&D Medical blood pressure Monitor™ Model US767Plus30 [21].
Biochemical measures
HbA1c, total cholesterol, HDL-C and triglycerides were measured by finger-pricks blood samples (Alere Afinion™AS100). At triglycerides > 7.34 mmol/L, HDL-C could not be measured. LDL-C was calculated using Friedewald’s formula. LDL-C was not calculated at triglycerides > 4.52 mmol/l. Non-HDL-C was calculated as total cholesterol – HDL-C [21].
Fatty acid composition in whole blood and desaturase estimation
FA profile was obtained from whole blood by using dried blood spots (DBS) (VITAS™ Analytical Services) [24]. DBS is a bio-sampling method where capillary blood, obtained by a finger-prick lancet, are dripped onto spots on filter collection cards (DBS card) [25]. The completed DBS card dried in room temperature for two to four hours before it was stored in an aluminium bag at 1–4 degrees Celsius until shipment to VITAS (Oslo, Norway) for analysis. Fatty acids methyl esters (FAME) were extracted from whole blood (plasma and cells) [26], and were analysed using Gas Chromatography – Flame Ionization Detector (GC-FID) after direct transmethylation. Whole blood FA profile was given in % FAME. The desaturase activities were estimated as the product-to-precursor ratios of FAs in whole blood according to the following: SCD1 = C16:1n7/C16:0 and C18:1n9/C18:0, hereafter referred to as SCD16 and SCD18, respectively. D5D = C18:3n6/C18:2n6 and D6D = C20:4n6/C20:3n6 (Table 1).
Questionnaires
From the validated, short food frequency questionnaire (FFQ), VISA-FFQ [27], we obtained data on intake of specific food groups and duration (minutes) and intensity (moderate and vigorous) of physical activity per week. Data on age, sex, smoking habits, marital status, ethnicity, educational level and income had been reported previously (− 52 weeks) through the baseline questionnaire [21].
Statistical analysis
Baseline characteristics were given as means ± standard deviations (SD) or median and 25th and 75th percentiles for continuous variables, and counts (%) for categorical variables. T-tests were used to assess differences in continuous variables, whereas Chi-Square tests were used for categorical variables. Non-normal variables were log-transformed before analysis.
Differences in FA profiles and estimated desaturase activities between the MU and MH groups were assessed using linear regression models adjusted for age and gender. Values are reported as estimated marginal means and corresponding 95% confidence intervals (CI). Furthermore, the association of FA profiles and estimated desaturase activities with increasing numbers of criteria for MU were investigated using linear regression adjusted for age and gender. We further explored whether trends were similar in BMI categories by adding an interaction term to the models (BMI × metabolic status) to assess whether the association of metabolic status with FA profiles depended on BMI. Finally, we used principal component analysis (PCA) to explore whether clusters of whole blood FAs were associated with MH and MU. All individual FAs were selected and normalized (scaled and centred) prior to PCA. Scree plots were examined and revealed three components explaining ~ 52% of the total variance in the dataset after application of varimax rotation. We proceeded with principal component (PC) 1 and PC2 and the computed PC scores were scaled and centred and given as z-scores. The PCA procedure was performed using the psych package for R. Linear regression was used to assess differences in PC1 and PC2 between MU and MH. A p-value of < 0.05 was considered statistically significant. We opted to not adjust for multiplicity due to the exploratory nature of the study. Statistical analyses were carried out using IBM SPSS version 23 and R version 3.6.3, using packages included in the “tidyverse” package selection, “psych” and “princomp”. Plots were made with the ggplot2 package for R.
Results
Metabolic health, fatty acid profile and estimated desaturase activities
Characterization of the participants is presented in Table 2. Of 321 subjects, 37.1% (n = 119) were categorized as normal weight, 40.2% (n = 129) were overweight and 22.7% (n = 73) were categorized as obese. Of these, 202 subjects met the criteria for MH and MU, and were subsequently categorized as MH (n = 150) or MU (n = 52). The individuals with MH phenotype were slightly younger (55.5 ± 14.8 years vs. 60.5 ± 12.1 years) and reported higher physical activity (median [25, 75th percentile]: 231 (79.3, 469) minutes vs. 114 (0, 247) minutes) than individuals with MU phenotype. There were no differences in blood pressure, gender, years of education, or prevalence of smokers between MH and MU subjects (Table 2).
Table 2.
Characteristics of metabolically healthy and unhealthy subjects
| Metabolically healthy (n = 150) | Metabolically unhealthy (n = 52) | P | |
|---|---|---|---|
| Demographics | |||
| Age, years (mean ± (SD)) | 55.5 ± 14.8 | 60.5 ± 12.1 | 0.017 |
| Men, n (%) | 34 (22.7) | 19 (36.5) | 0.132 1 |
| ≤ 13 years of schooling, n (%) | 77 (54.6) | 26 (51.0) | 0.854 1 |
| Smokers (daily or occasional), n (%) | 18 (12.3) | 5 (9.6) | 0.607 1 |
| Risk factors (mean ± (SD)) | |||
| BMI, kg/m2 | 26.6 ± 4.6 | 28.8 ± 4.5 | 0.003 |
| Total cholesterol, mmol/l | 6.2 ± 1.1 | 6.7 ± 1.0 | 0.012 |
| LDL-cholesterol, mmol/l | 3.8 ± 1.0 | 4.0 ± 0.9 | 0.073 |
| HDL-cholesterol, mmol/l | 1.9 ± 0.5 | 1.4 ± 0.4 | < 0.001 |
| NonHDL, mmol/l | 4.3 ± 0.9 | 5.2 ± 0.9 | < 0.001 |
| Triglycerides, mmol/l | 1.3 ± 0.5 | 2.9 ± 1.1 | < 0.001 |
| HbA1c, % | 5.4 ± 0.2 | 5.8 ± 0.4 | < 0.001 |
| Systolic BP, mmHg | 126.2 ± 16.1 | 126.6 ± 16.8 | 0.857 |
| Diastolic BP, mmHg | 79.5 ± 9.9 | 80.4 ± 10.1 | 0.567 |
| Physical activity, min/week2,3 | 231 (79.3, 469) | 114 (0, 247) | 0.002 |
Demographics as frequency [n (%)] and age were obtained 52 weeks prior to the present data collection. Risk factors are expressed as mean ± SD. P values from Student’s t-test. P is significant at 0.05 level. 1P value from Chi-square test. BMI, body mass index; BP, blood pressure; HbA1c, glycated hemoglobin A1c. 2Given as median (25th – 75th percentile). 3Mann-Whitney U test
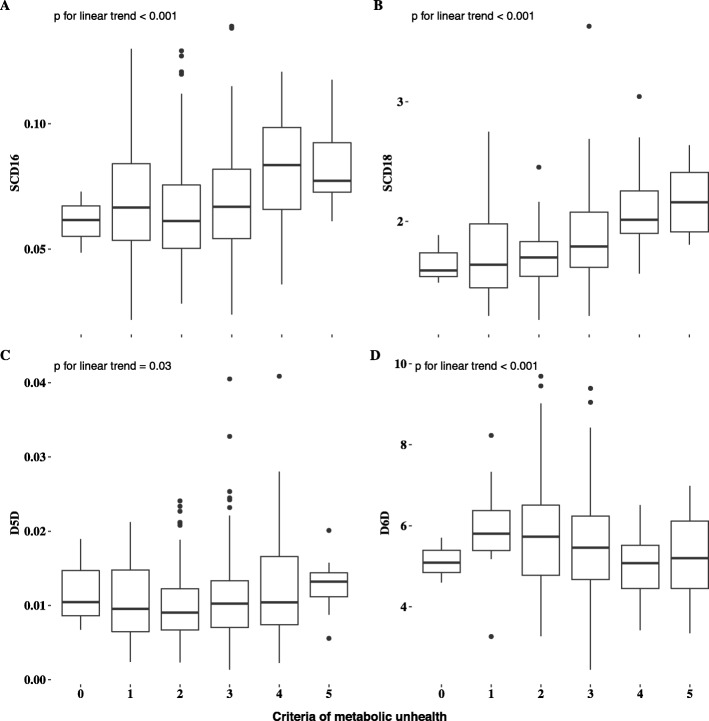
Of the FAs measured, C18:0 was higher, whereas C14:0 and C16:0 were lower in the MH group compared with MU group. Furthermore, the MH group had lower levels of total MUFAs, C16:1n7, C18:1n9 and estimated SCD16 and SCD18 activity compared to the MU group (P < 0.001 for all). Except for C18:3n3, total n6 FA, n3 FA and D6D, but not D5D, were significantly higher in the MH group (Table 3). We observed that estimated SCD16 and SCD18 activities (P for both < 0.001) increased with increasing number of criteria for MU (ranging 1–5). A clear decrease was observed for estimated D6D activity (P < 0.001) and a slight decrease was observed for estimated D5D activity with increasing number of criteria for MU (P = 0.03) (Fig. 1).
Table 3.
Fatty acid profile and estimated desaturase activity in metabolically healthy and unhealthy subjects
| Fatty acids, %FAME | Metabolically healthy (n = 150) | Metabolically unhealthy (n = 52) | P |
|---|---|---|---|
| C12:0 | 0.12 (0.1, 0.14) | 0.14 (0.12, 0.17) | 0.169 |
| C14:0 | 0.91 (0.85, 0.98) | 1.16 (1.06, 1.25) | < 0.001 |
| C15:0 | 0.25 (0.24, 0.26) | 0.25 (0.23, 0.26) | 0.658 |
| C16:0 | 21.51 (21.25, 21.78) | 22.35 (21.95, 22.76) | 0.001 |
| C17:0 | 0.35 (0.34, 0.36) | 0.33 (0.32, 0.35) | 0.049 |
| C18:0 | 11.79 (11.62, 11.96) | 10.98 (10.72, 11.24) | < 0.001 |
| C20:0 | 0.09 (0.08, 0.09) | 0.09 (0.09, 0.1) | 0.167 |
| SFA total | 35.03 (34.72, 35.34) | 35.3 (34.84, 35.77) | 0.323 |
| C16:1 n7 | 1.36 (1.26, 1.46) | 1.72 (1.57, 1.86) | < 0.001 |
| C18:1 n9 | 19.85 (19.45, 20.24) | 22.51 (21.9, 23.11) | < 0.001 |
| C18:1 c11 | 1.54 (1.49, 1.59) | 1.51 (1.44, 1.59) | 0.512 |
| C20:1 n9 | 0.26 (0.24, 0.27) | 0.24 (0.22, 0.26) | 0.221 |
| MUFA total | 23 (22.55, 23.45) | 25.98 (25.3, 26.66) | < 0.001 |
| SCD16 | 0.06 (0.06, 0.07) | 0.08 (0.07, 0.08) | < 0.001 |
| SCD18 | 1.7 (1.64, 1.75) | 2.08 (2, 2.16) | < 0.001 |
| D5D | 0.01 (0.01, 0.01) | 0.01 (0.01, 0.01) | 0.081 |
| D6D | 5.87 (5.65, 6.09) | 5.14 (4.8, 5.48) | < 0.001 |
| C18:2 n6 | 19.81 (19.34, 20.29) | 18.94 (18.22, 19.66) | 0.042 |
| C18:3 n6 | 0.2 (0.18, 0.22) | 0.22 (0.19, 0.24) | 0.257 |
| C18:3 n3 | 0.49 (0.46, 0.52) | 0.61 (0.56, 0.66) | < 0.001 |
| C20:3 n6 | 1.4 (1.35, 1.45) | 1.38 (1.31, 1.46) | 0.694 |
| C20:4 n6 | 8.03 (7.77, 8.29) | 7.01 (6.61, 7.4) | < 0.001 |
| C20:5 n3 | 1.48 (1.33, 1.63) | 1.06 (0.83, 1.29) | 0.002 |
| C22:5 n3 | 1.39 (1.34, 1.44) | 1.21 (1.13, 1.28) | < 0.001 |
| C22:6 n3 | 3.4 (3.25, 3.56) | 2.98 (2.74, 3.21) | 0.003 |
| PUFA total | 36.21 (35.63, 36.79) | 33.4 (32.52, 34.28) | < 0.001 |
| ω-3 total | 6.77 (6.46, 7.08) | 5.85 (5.37, 6.33) | 0.001 |
| ω-6 total | 29.44 (28.91, 29.98) | 27.55 (26.74, 28.35) | < 0.001 |
P values from linear regression models adjusted for age and sex. Values are estimated marginal means 95% confidence interval). P is significant at 0.05 level. SCD1, Stearoyl-CoA desaturase-1; D5D, delta-5-desaturase; D6D, delta-6-desaturase; SFA, saturated fatty acids; MUFA, monounsaturated fatty acids; PUFA, polyunsaturated fatty acids
Fig. 1.
Boxplots showing a) SCD16, b) SCD18, c) D5D and d) D6D activity indices accross metabolic health criteria
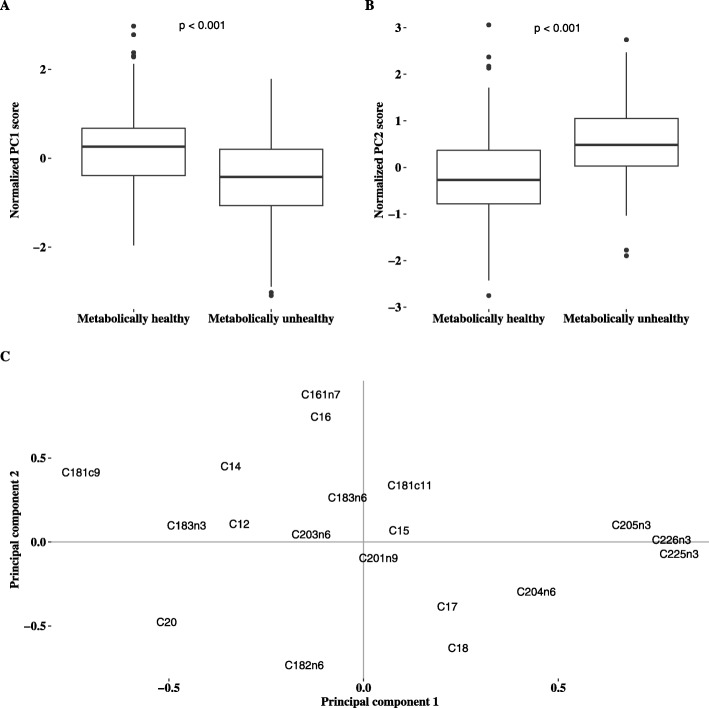
Principal component analyses
In order to explore whether clusters of FAs were different between the MH and MU groups, we performed PCA. All individual FAs were selected for analysis. PC1 and PC2 accounted for ~ 36% of the total variance in the dataset. Briefly, the FAs most positively correlated with PC1 were C20:5n3, C22:5n3 and C22:6n3 whereas C18:1n9 were strongly and inversely correlated with PC1. For PC2, the strongest positive correlations were observed for C16:0 and C16:1n7 and inverse correlations for C18:2n6 and C18:0. Compared with MH, individuals with MU had a lower mean z-score for PC1 and a higher mean z-score for PC2 as illustrated in Fig. 2.
Fig. 2.
a) Boxplot for principal component 1 score, b) boxplot for principal component 2 score aand c) correlation between the individual fatty acids and prinicpal component 1 and 2
Association of metabolic health phenotypes and estimated desaturases by BMI category
We further investigated the MU phenotypes according to BMI categories. Characteristics of MH and MU individuals by BMI group are presented in Additional file 1.
Of the overall population of individuals with obesity (including those between MU and MH), 46.6% (n = 34) were categorized as MH (corresponding to 10.4% of the total population) and 23.3% (n = 17) as MU. The corresponding prevalence of MH among the individuals with overweight were 40.3% (n = 52) and 17.8% MU (n = 23). Among those with normal weight, 53.8% (n = 64) were MH and 9.2% (n = 11) were MU. Parameters were generally similar except for the metabolic status classification criteria. Individuals with MH and obesity reported higher physical activity with median (25th–75th percentile) 150 min (0, 362) per week compared with 38 min (0, 126) for MU with obesity (P = 0.031). The FA profile and estimated desaturase activities were similar between MU and MH subjects in each BMI category and no interactions were observed in the regression models (Additional file 2). The association between numbers of criteria met for MU overall showed the same patterns in each BMI category as for the total population (Additional file 3).
Discussion
In a group of Norwegians with moderately elevated risk of CVD but non-medically treated, we found that estimated SCD16 and SCD18 activities increased with increasing number of criteria for MU, whereas estimated D5D and D6D activities appeared to decrease. Similar, some SFAs, total MUFA, estimated SCD16 and SCD18 were lower, whereas most PUFAs (both n3 and n6) and D6D were higher in MH than MU. These findings were also supported by results from PCA. Related findings were observed in subgroups according to BMI.
Findings from this study suggest that all of the investigated desaturases were related to metabolic health. The association between criteria for MU and desaturases was strongest for estimated SCD16 and SCD18 activities. In a subsample in the PREDIMED trial, estimated SCD16 but not SCD18 activity was increased in individuals with MetS [28]. Such an association may primarily be explained by obesity according to Warensjo et al. [12]. Additionally, findings from one large cohort study suggested that both SCD16 and SCD18 activities were associated with fat mass [18], further supporting that obesity can be a main driver of these associations. However, we observed associations between SCD activities and MU irrespectively of BMI subgroups. In line with our results, Lassale et al. found that individuals with a MU phenotype had higher risk of CVD than MH, irrespective of BMI [29]. One possible explanation for our findings could be different dietary intakes of SFAs, as estimated SCD16 activity has been shown to be higher after intervention with a diet high in SFA compared to a diet high in MUFA and PUFA [30, 31]. However, in the present study, we observed that intake of foods high in SFA did not differ between MH and MU (Additional file 4).
In addition to lower plasma levels of the SFAs C14:0 and C16:0, we also found lower levels of C16:1n7 and C18:1n9 in MH subjects, including MH obese compared with their MU counterparts. This finding corresponds to the lower levels of estimated SCD16 and SCD18 activities in MH, as endogen production of MUFAs is regulated by these desaturases [15].
MUFAs (C16:1 and 18:1) are major components of triglycerides, cholesterol esters and phospholipids, produced by de novo lipogenesis and carried in VLDL in the circulation [15]. This incorporation of MUFAs in VLDL, could partly explain the observed association between high levels of MUFAs and the MU phenotype, characterized by high levels of triglycerides, total cholesterol and LDL-C. Our findings are also supported by results from a NHANES survey where higher plasma concentration of SFAs and MUFAs were associated with increased levels of fasting plasma glucose and HbA1c [32]. The same pattern was found in the FINRISK study. Here, higher plasma levels of MUFAs in healthy, overweight subjects were associated with increased CVD risk, whereas higher levels of n6 FAs and docosahexaenoic acid (DHA) levels were associated with lower risk [33], in line with our study.
We found that the estimated activity of enzymes responsible for the desaturation of PUFAs, D6D and to some extent D5D activities, decreased with increasing numbers of criteria for MU. Both Zhao et al. and Mayneris-Perxachs et al. found that estimated D5D activity was inversely associated with metabolic dysregulation [28, 34], also in MH obese subjects [34]. The observed higher levels of estimated D6D in MH subjects in our study was therefore in contrast to other findings where D6D has been associated with increased risk of MetS and insulin resistance in individuals with overweight and obesity [28, 35]. The association has been suggested to be due to PUFA imbalance such as reduced n3/n6 FAs ratio [35]. However, the ratio in blood between n3 and n6 in the present study was not excessively high [35]. Neither where there any differences in dietary intake of fatty fish (high in n3 FA) between the MH and MU group.
Our findings suggests that SCD may influence the development of MU phenotype independently of fat mass and dietary intake. Consequently, other unmeasured metabolic markers could affect the association between SCD and MU phenotype. Genetics may play an important role, as several studies in rodents have shown that SCD16 deficient mice do not become overweight/obese or have metabolic disruptions even when fed a high fat diet [36]. In this regard, body fat distribution among subjects and across genders is another unmeasured factor that could have helped elucidated this results [37]. For instance, MH overweight and obese could have lower levels of visceral and ectopic fat [38, 39]. Furthermore, we observed MH to be more physically active than MU inn all BMI groups, indicating that lifestyle is likely to be important for metabolic health.
It is however possible that our study population is healthier than other populations. In total 10% defined as MH obese is among the highest prevalence independent of criteria used for metabolic health summarized by Liu et al. [40] and Wildman et al. [41]. Using BMI rather than waist circumference to define obesity often yields higher prevalence of MH obese [40]. Yet, other studies have found comparable prevalence of MH obese as the present study using ≥2 criteria for metabolic health [42]. Furthermore, subjects were enrolled in the present study based on background CVD risk and had previously attended an intervention study aiming at changing lifestyle behavior [21]. This might have influenced the study population and limiting the generalizability of results.
In line with this, we observed that in the present study, 9% (n = 13) of the MH were previously (1 year before) categorized as MU. This transition from MU to MH was due to favorable changes in diet, lifestyle and CVD risk factors previously described as long-term effects of participating in the VISA-study [21]. On another note, it has been suggested that MH overweight and obese phenotypes may be transient states, as individuals with MH overweight and obesity are still at increased risk of developing T2D and CVD compared to normal weight individuals [43]. FAs and desaturase activity indices could therefore be predictors of long-term development of metabolic disorders [12], such as a 10-year transition from MH to MU [34]. Hence, our results support that desaturases could be biomarkers of (future) metabolic health independent of BMI, although direction of association remains to be elucidated.
Strengths and limitations
The main strength of the study is the well-characterized sample of 321 individuals free of disease but at moderately increased risk of CVD who were originally recruited from the general population [20, 21]. Limitations includes lack of generalizability, as the study population had been previously included in an intervention study aiming at improving health. Furthermore, we note that due to the cross-sectional nature of the study, the direction of the associations reported is impossible to infer and no information on causality can be obtained.
Conclusion
We found that estimated SCD16 and SCD18 activities increased with increasing number of criteria for MU, and that estimated D6D activity and to some extent also D5D activity, decreased. The corresponding SFAs and PUFAs followed the patterns of the estimates activities of SCD16/SCD18 and D5D/D6D respectively. The findings persisted irrespectively of BMI. Hence, the study supports that these desaturases can be important novel biomarkers of metabolic health, although these analyses cannot answer whether the dysregulation of these desaturases are a cause or a consequence of lifestyle factors or genetics. This warrants further studies.
Supplementary information
Additional file 1. Characteristics of metabolically healthy and unhealthy normal weight, overweight and obese subjects.
Additional file 2. Fatty acid profile and desaturase ratios in metabolically healthy and unhealthy normal weight, overweight and obese subjects.
Additional file 3. Association of criteria for metabolic health and estimated desaturase activities in BMI categories.
Additional file 4. Diet and lifestyle for metabolically healthy (MH) and unhealthy (MU) participants stratified by body mass index (BMI).
Acknowledgements
We are grateful for all participants in the present study and the VISA-study. Our sincerely thanks to employees in Boots Norge AS for collecting both biochemical measurements and dried blood spot tests. Thanks to Kjersti W. Garstad and Lisa T. Mørch-Reiersen in Boots Norge AS and David R. Jacobs Jr. from University of Minnesota for significant contributions to study administration and to the design of the VISA-study. Thanks to Hege Berg Henriksen for assisting in development and processing of the questionnaire used to report physical activity level.
Abbreviations
- CVD
Cardiovascular diseases
- FA
Fatty acid
- HDL
High density lipoprotein
- HbA1c
Hemoglobin A1c
- LDL
Low density lipoprotein
- MetS
Metabolic syndrome
- MH
Metabolic healthy
- MU
Metabolic unhealthy
- MUFA
Monounsaturated fatty acids
- PUFA
Polyunsaturated fatty acids
- SCD1
Stearoyl CoA-desaturase 1
- SFA
Saturated fatty acids
- T2D
Type 2 diabetes
Authors’ contributions
KS, KR, VTH were responsible for study administration. KS, TO, TCNR, SMU, KBH, KR and VTH contributed to the conceptualization of the study. KS, TO, TCNR, KR and VHTH and were responsible for data curation, and TO and TCNR for the main data analysis. KS, TO and VHTH were responsible for writing the main manuscript text. All authors reviewed and approved the final manuscript.
Funding
We received funding from Wendel Jarlsbergs (distributed by the non-profit organization UNIFOR) for analysis of fatty acids and development of the VISA-FFQ questionnaire used to report diet and physical activity. We also previously received funding from Vita hjertego’ (Mills DA) for work with the VISA-FFQ.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The study was approved by the Regional Committee of Medical Ethics (ref. 2013/1660). Written informed consent for participation was obtained, and the study complied with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
TO and TCNR declare that they have no competing interests. KS reports grants from Mills DA (Vita hjertego’) relevant for the present paper, and grants from a pharmacy interest organization (Stiftelsen til fremme av. norsk apotekfarmasi), personal fees from MedXplore outside the submitted work. SMU has received research grants from Tine DA, Mills DA, Olympic Seafood, none of which are related to the content of this manuscript. KBH reports grants from Tine SA, Mills DA, Olympic Seafood, Amgen, Sanofi, Kaneka and personal fees from Amgen, Sanofi, Pronova, outside the submitted work. KR reports personal fees from MedXplore, Amgen, Mills DA, The Norwegian Medical Association, The Norwegian Directorate of Health, Sanofi, Takeda, Chiesi, Bayer and MSD, outside the submitted work. VHTH is a former employee at Mills AS and reports grants from Mills AS. She does not owns any stocks in the company, and the work performed in this paper was done after she left the company.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Svendsen, Karianne and Olsen, Thomas contributed equally and thus share first authorship
Contributor Information
Karianne Svendsen, Email: Karianne.svendsen@medisin.uio.no.
Thomas Olsen, Email: Thomas.olsen@medisin.uio.no.
Tove C. Nordstrand Rusvik, Email: tove.rusvik@gmail.com
Stine M. Ulven, Email: smulven@medisin.uio.no
Kirsten B. Holven, Email: k.b.holven@medisin.uio.no
Kjetil Retterstøl, Email: kjetil.retterstol@medisin.uio.no.
Vibeke H. Telle-Hansen, Email: vtelle@oslomet.no
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12944-020-01282-y.
References
- 1.Global Burden of Disease Mortality Causes of Death Collaborators Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544. doi: 10.1016/S0140-6736(16)31012-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ipsen DH, Tveden-Nyborg P, Lykkesfeldt J. Dyslipidemia: obese or not obese-that is not the question. Curr Obes Rep. 2016;5(4):405–412. doi: 10.1007/s13679-016-0232-9. [DOI] [PubMed] [Google Scholar]
- 3.Telle-Hansen VH, Halvorsen B, Dalen KT, Narverud I, Wesseltoft-Rao N, Granlund L, et al. Altered expression of genes involved in lipid metabolism in obese subjects with unfavourable phenotype. Genes Nutr. 2013;8(4):425–434. doi: 10.1007/s12263-012-0329-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Muñoz-Garach Araceli, Cornejo-Pareja Isabel, Tinahones Francisco. Does Metabolically Healthy Obesity Exist? Nutrients. 2016;8(6):320. doi: 10.3390/nu8060320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Caleyachetty R, Thomas GN, Toulis KA, Mohammed N, Gokhale KM, Balachandran K, et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J Am Coll Cardiol. 2017;70(12):1429–1437. doi: 10.1016/j.jacc.2017.07.763. [DOI] [PubMed] [Google Scholar]
- 6.Aung K, Lorenzo C, Hinojosa MA, Haffner SM. Risk of developing diabetes and cardiovascular disease in metabolically unhealthy normal-weight and metabolically healthy obese individuals. J Clin Endocrinol Metab. 2014;99(2):462–468. doi: 10.1210/jc.2013-2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Araujo J, Cai J, Stevens J. Prevalence of optimal metabolic health in American adults: National Health and nutrition examination survey 2009-2016. Metab Syndr Relat Disord. 2019;17(1):46–52. doi: 10.1089/met.2018.0105. [DOI] [PubMed] [Google Scholar]
- 8.Bjermo H, Riserus U. Role of hepatic desaturases in obesity-related metabolic disorders. Curr Opin Clin Nutr Metab Care. 2010;13(6):703–708. doi: 10.1097/MCO.0b013e32833ec41b. [DOI] [PubMed] [Google Scholar]
- 9.Vessby B, Gustafsson IB, Tengblad S, Boberg M, Andersson A. Desaturation and elongation of fatty acids and insulin action. Ann N Y Acad Sci. 2002;967:183–195. doi: 10.1111/j.1749-6632.2002.tb04275.x. [DOI] [PubMed] [Google Scholar]
- 10.Lankinen MA, Stancakova A, Uusitupa M, Agren J, Pihlajamaki J, Kuusisto J, et al. Plasma fatty acids as predictors of glycaemia and type 2 diabetes. Diabetologia. 2015;58(11):2533–2544. doi: 10.1007/s00125-015-3730-5. [DOI] [PubMed] [Google Scholar]
- 11.Kim OY, Lim HH, Lee MJ, Kim JY, Lee JH. Association of fatty acid composition in serum phospholipids with metabolic syndrome and arterial stiffness. Nutr Metab Cardiovasc Dis. 2013;23(4):366–374. doi: 10.1016/j.numecd.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 12.Warensjo E, Riserus U, Vessby B. Fatty acid composition of serum lipids predicts the development of the metabolic syndrome in men. Diabetologia. 2005;48(10):1999–2005. doi: 10.1007/s00125-005-1897-x. [DOI] [PubMed] [Google Scholar]
- 13.Tremblay AJ, Despres JP, Piche ME, Nadeau A, Bergeron J, Almeras N, et al. Associations between the fatty acid content of triglyceride, visceral adipose tissue accumulation, and components of the insulin resistance syndrome. Metab Clin Exp. 2004;53(3):310–317. doi: 10.1016/j.metabol.2003.10.011. [DOI] [PubMed] [Google Scholar]
- 14.Wang L, Folsom AR, Zheng ZJ, Pankow JS, Eckfeldt JH, Investigators AS. Plasma fatty acid composition and incidence of diabetes in middle-aged adults: the atherosclerosis risk in communities (ARIC) study. Am J Clin Nutr. 2003;78(1):91–98. doi: 10.1093/ajcn/78.1.91. [DOI] [PubMed] [Google Scholar]
- 15.Ferrier DR. In: Biochemistry. Sixth edition. Harvey RA, editor. 2014. [Google Scholar]
- 16.Riserus U, Willett WC, Hu FB. Dietary fats and prevention of type 2 diabetes. Prog Lipid Res. 2009;48(1):44–51. doi: 10.1016/j.plipres.2008.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warensjo E, Ohrvall M, Vessby B. Fatty acid composition and estimated desaturase activities are associated with obesity and lifestyle variables in men and women. Nutr mMetab Cardiovasc Dis. 2006;16(2):128–136. doi: 10.1016/j.numecd.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Vinknes KJ, Elshorbagy AK, Nurk E, Drevon CA, Gjesdal CG, Tell GS, et al. Plasma stearoyl-CoA desaturase indices: association with lifestyle, diet, and body composition. Obesity (Silver Spring, Md) 2013;21(3):E294–E302. doi: 10.1002/oby.20011. [DOI] [PubMed] [Google Scholar]
- 19.ALJohani AM, Syed DN, Ntambi JM. Insights into Stearoyl-CoA Desaturase-1 regulation of systemic metabolism. Trends Endocrinol Metab. 2017;28(12):831–842. doi: 10.1016/j.tem.2017.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Svendsen Karianne, Jacobs Jr David R, Røyseth Ida Tonning, Garstad Kjersti Wilhelmsen, Byfuglien Marte Gjeitung, Granlund Linda, Mørch-Reiersen Lisa T, Telle-Hansen Vibeke H, Retterstøl Kjetil. Community pharmacies offer a potential high-yield and convenient arena for total cholesterol and CVD risk screening. European Journal of Public Health. 2018;29(1):17–23. doi: 10.1093/eurpub/cky190. [DOI] [PubMed] [Google Scholar]
- 21.Svendsen K, Telle-Hansen VH, Morch-Reiersen LT, Garstad KW, Thyholt K, Granlund L, et al. A randomized controlled trial in Norwegian pharmacies on effects of risk alert and advice in people with elevated cardiovascular risk. Prev Med Rep. 2018;12:79–86. doi: 10.1016/j.pmedr.2018.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Karelis AD, Brochu M, Rabasa-Lhoret R. Can we identify metabolically healthy but obese individuals (MHO)? Diabetes Metab. 2004;30(6):569–572. doi: 10.1016/s1262-3636(07)70156-8. [DOI] [PubMed] [Google Scholar]
- 23.World Health Organization. Obesity and overweight 2018 [cited 2019 21.02]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.
- 24.Sakhi AK, Bastani NE, Ellingjord-Dale M, Gundersen TE, Blomhoff R, Ursin G. Feasibility of self-sampled dried blood spot and saliva samples sent by mail in a population-based study. BMC Cancer. 2015;15(1):265. doi: 10.1186/s12885-015-1275-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Edelbroek PM, van der Heijden J, Stolk LM. Dried blood spot methods in therapeutic drug monitoring: methods, assays, and pitfalls. Ther Drug Monit. 2009;31(3):327–336. doi: 10.1097/FTD.0b013e31819e91ce. [DOI] [PubMed] [Google Scholar]
- 26.Rise P, Eligini S, Ghezzi S, Colli S, Galli C. Fatty acid composition of plasma, blood cells and whole blood: relevance for the assessment of the fatty acid status in humans. Prostaglandins Leukot Essent Fat Acids. 2007;76(6):363–369. doi: 10.1016/j.plefa.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 27.Svendsen K, Henriksen HB, Ostengen B, Jacobs DR Jr, Telle-Hansen VH, Carlsen MH, et al. Evaluation of a short food frequency questionnaire to assess cardiovascular disease-related diet and lifestyle factors. Food Nutr Res. 2018;62. [DOI] [PMC free article] [PubMed]
- 28.Mayneris-Perxachs J, Guerendiain M, Castellote AI, Estruch R, Covas MI, Fito M, et al. Plasma fatty acid composition, estimated desaturase activities, and their relation with the metabolic syndrome in a population at high risk of cardiovascular disease. Clin Nutr (Edinburgh, Scotland) 2014;33(1):90–97. doi: 10.1016/j.clnu.2013.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Lassale C, Tzoulaki I, Moons KGM, Sweeting M, Boer J, Johnson L, et al. Separate and combined associations of obesity and metabolic health with coronary heart disease: a pan-European case-cohort analysis. Eur Heart J. 2018;39(5):397–406. doi: 10.1093/eurheartj/ehx448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Warensjo E, Riserus U, Gustafsson IB, Mohsen R, Cederholm T, Vessby B. Effects of saturated and unsaturated fatty acids on estimated desaturase activities during a controlled dietary intervention. Nutr Metab Cardiovasc Dis. 2008;18(10):683–690. doi: 10.1016/j.numecd.2007.11.002. [DOI] [PubMed] [Google Scholar]
- 31.Telle-Hansen VH, Larsen LN, Hostmark AT, Molin M, Dahl L, Almendingen K, et al. Daily intake of cod or salmon for 2 weeks decreases the 18:1n-9/18:0 ratio and serum triacylglycerols in healthy subjects. Lipids. 2012;47(2):151–160. doi: 10.1007/s11745-011-3637-y. [DOI] [PubMed] [Google Scholar]
- 32.Yu EA, Hu PJ, Mehta S. Plasma fatty acids in de novo lipogenesis pathway are associated with diabetogenic indicators among adults: NHANES 2003-2004. Am J Clin Nutr. 2018;108(3):622–632. doi: 10.1093/ajcn/nqy165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wurtz P, Havulinna AS, Soininen P, Tynkkynen T, Prieto-Merino D, Tillin T, et al. Metabolite profiling and cardiovascular event risk: a prospective study of 3 population-based cohorts. Circulation. 2015;131(9):774–785. doi: 10.1161/CIRCULATIONAHA.114.013116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao L, Ni Y, Ma X, Zhao A, Bao Y, Liu J, et al. A panel of free fatty acid ratios to predict the development of metabolic abnormalities in healthy obese individuals. Sci Rep. 2016;6:28418. doi: 10.1038/srep28418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Arshad Z, Rezapour-Firouzi S, Ebrahimifar M, Mosavi Jarrahi A, Mohammadian M. Association of Delta-6-Desaturase expression with aggressiveness of Cancer, diabetes mellitus, and multiple sclerosis: a narrative review. Asian Pac J Cancer Prev. 2019;20(4):1005–1018. doi: 10.31557/APJCP.2019.20.4.1005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bai Y, McCoy JG, Levin EJ, Sobrado P, Rajashankar KR, Fox BG, et al. X-ray structure of a mammalian stearoyl-CoA desaturase. Nature. 2015;524(7564):252–256. doi: 10.1038/nature14549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Frank AP, de Souza SR, Palmer BF, Clegg DJ. Determinants of body fat distribution in humans may provide insight about obesity-related health risks. J Lipid Res. 2019;60(10):1710–1719. doi: 10.1194/jlr.R086975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Karelis AD, St-Pierre DH, Conus F, Rabasa-Lhoret R, Poehlman ET. Metabolic and body composition factors in subgroups of obesity: what do we know? J Clin Endocrinol Metab. 2004;89(6):2569–2575. doi: 10.1210/jc.2004-0165. [DOI] [PubMed] [Google Scholar]
- 39.Primeau V, Coderre L, Karelis AD, Brochu M, Lavoie ME, Messier V, et al. Characterizing the profile of obese patients who are metabolically healthy. Int J Obes. 2011;35(7):971–981. doi: 10.1038/ijo.2010.216. [DOI] [PubMed] [Google Scholar]
- 40.Liu C, Wang C, Guan S, Liu H, Wu X, Zhang Z, et al. The prevalence of metabolically healthy and unhealthy obesity according to different criteria. Obesity facts. 2019;12(1):78–90. doi: 10.1159/000495852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wildman RP, Muntner P, Reynolds K, McGinn AP, Rajpathak S, Wylie-Rosett J, et al. The obese without cardiometabolic risk factor clustering and the normal weight with cardiometabolic risk factor clustering: prevalence and correlates of 2 phenotypes among the US population (NHANES 1999-2004) Arch Intern Med. 2008;168(15):1617–1624. doi: 10.1001/archinte.168.15.1617. [DOI] [PubMed] [Google Scholar]
- 42.Smith GI, Mittendorfer B, Klein S. Metabolically healthy obesity: facts and fantasies. J Clin Invest. 2019;129(10):3978–3989. doi: 10.1172/JCI129186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garcia-Moll X. Obesity and prognosis: time to forget about metabolically healthy obesity. Eur Heart J. 2018;39(5):407–409. doi: 10.1093/eurheartj/ehx535. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Characteristics of metabolically healthy and unhealthy normal weight, overweight and obese subjects.
Additional file 2. Fatty acid profile and desaturase ratios in metabolically healthy and unhealthy normal weight, overweight and obese subjects.
Additional file 3. Association of criteria for metabolic health and estimated desaturase activities in BMI categories.
Additional file 4. Diet and lifestyle for metabolically healthy (MH) and unhealthy (MU) participants stratified by body mass index (BMI).
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.