Abstract
Objective
Urinary retention caused by bladder clots can be frustrating because such blood clots are difficult to remove. We established a novel technique in which hydrogen peroxide is applied to evacuate bladder clots.
Methods
In this single-center retrospective study, we evaluated 31 patients with retention of blood clots in the bladder who underwent emergency evacuation using hydrogen peroxide.
Results
The patients comprised 17 men and 14 women with mean age of 61.2 years (range, 42–82 years). Hydrogen peroxide solution and a 20-Fr three-cavity Foley catheter with large-diameter side holes were used for manual bladder irrigation in all patients. The bladder blood clots were successfully removed in 27 patients. The remaining four patients could not tolerate the symptoms of urinary retention and had to resort to surgery.
Conclusion
Hydrogen peroxide solution for manual bladder irrigation can improve the efficiency of bladder blood clot evacuation. This is a simple and effective option for managing bladder clot retention.
Keywords: Hydrogen peroxide, clot evacuation, clot retention, bladder irrigation, Foley catheter, hematuria
Introduction
Bladder blood clot formation is a common emergency in urological practice. Severe hematuria can lead to blood clot formation in the bladder cavity and consequent urinary retention.1 Patients may develop pain if the clots cannot be evacuated in a timely manner. Manual bladder washout using a Foley catheter and syringe is the most common method of removing such blood clots. However, this method fails in some patients. Other methods of clot evacuation described in the literature include the use of improved flushing devices2–4 or changes in flushing fluid elements.5,6 However, these methods are complicated and not always effective. Open suprapubic clot evacuation has been adopted in certain cases. In 2006, Warlick et al.7 reported the successful use of hydrogen peroxide for the evacuation of blood clots from the bladder in two patients. We also found that when the hydrogen peroxide solution was mixed with the blood clot, the blood clot loosened and readily disintegrated.8 Hence, we attempted to use hydrogen peroxide solution for clot evacuation when traditional manual bladder irrigation failed, and the clinical outcomes were satisfactory.
Encouraged by the experience of Warlick et al.7 and our own results, we used hydrogen peroxide solution for bladder blood clot evacuation and continuous bladder irrigation after transurethral resection of the prostate.8 We herein share our experience of using hydrogen peroxide solution to remove blood clots from the bladder cavity.
Materials and methods
Patients
From January 2016 to June 2019, hydrogen peroxide solution was used in consecutive patients with bladder blood clot retention. Before the procedure, the bladder blood clots were evaluated by ultrasound (Figure 1). The volume was calculated as follows: 0.52 × anteroposterior diameter × up–down diameter × left–right diameter. Informed consent was obtained from all patients, and the study was approved by the Ethics Committee of the Second Affiliated Hospital of Soochow University.
Figure 1.
Ultrasound image of a patient with a large bladder clot.
Procedure
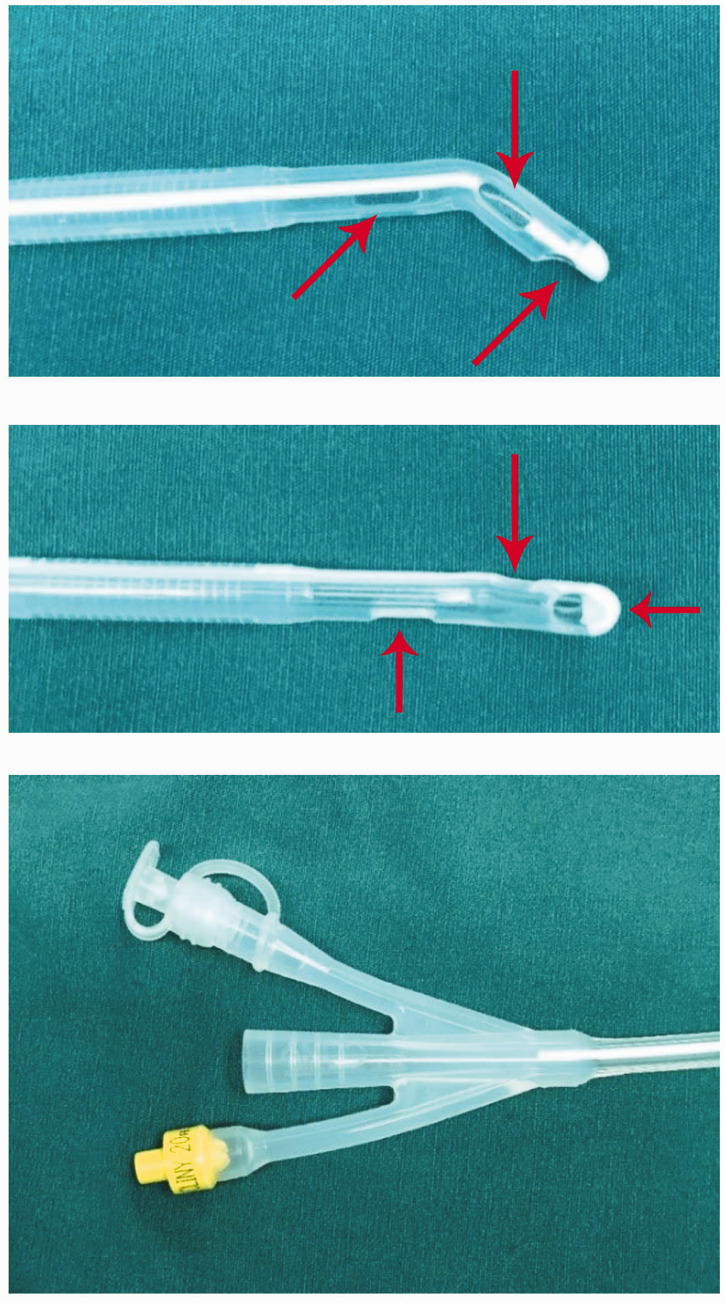
The materials used were 3% hydrogen peroxide solution, 0.9% saline solution, a 20-Fr three-cavity Foley catheter with large-diameter side holes, and an irrigation syringe. The irrigation fluid was a 1:5 mixture of 3% hydrogen peroxide solution and 0.9% saline solution. The Foley catheter used for the procedure is shown in Figure 2. It had three large holes at the tip, decreasing the chance of blockage during bladder irrigation. The irrigation syringe used for the procedure is shown in Figure 3. The tip of this device could tightly connect with the Foley catheter, and the other end of the irrigation device had a ring. These characteristics of the irrigation device reduced the fatigue of the manual procedure.
Figure 2.
Foley catheter with large side holes at the tip (arrows).
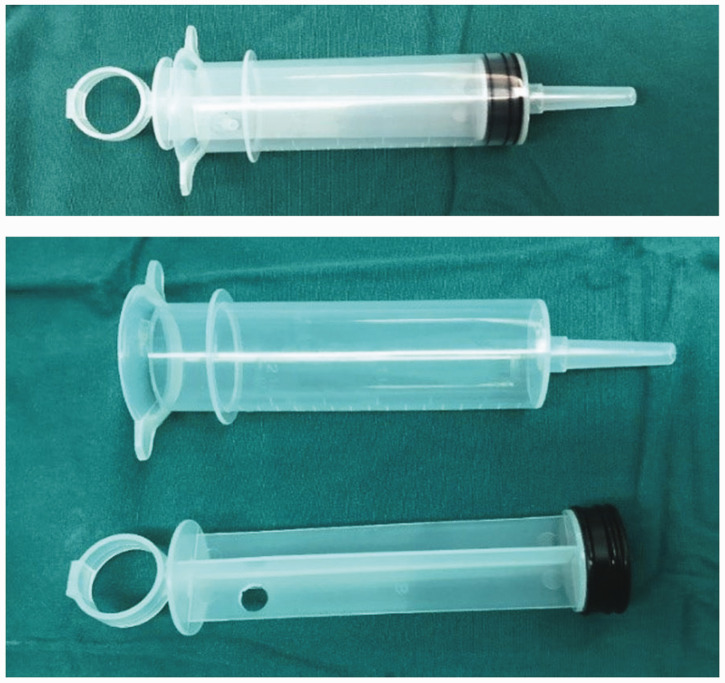
Figure 3.
Irrigation syringe.
For clot removal, the Foley catheter was indwelled into the urethra and bladder. In each cycle, 30 to 50 mL of irrigation fluid was injected into the bladder for about 30 s through the catheter using the irrigation syringe, maintained within the bladder for 3 to 5 minutes, and pulled back.
Results
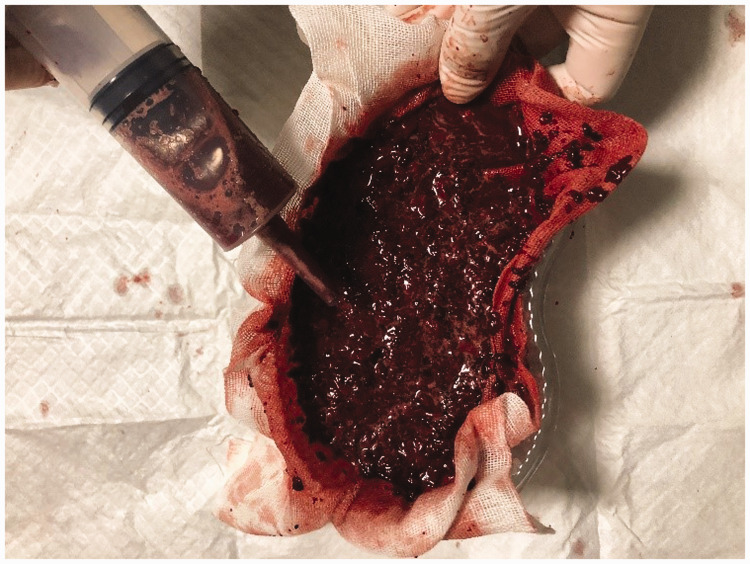
Thirty-one patients were included in this study. The blood clots were easily disrupted when mixed with hydrogen peroxide solution for 3 to 5 minutes. The clots were evacuated after 6 to 10 cycles of irrigation. Throughout this process, large blood clots became small fragments (Figure 4). The efficiency of manual bladder washout was greatly improved. The procedure was successful in 27 of the 31 patients. After three to five cycles of this manual bladder washout protocol in the other four patients, a few fragments of clots were evacuated. However, these patients could not tolerate the symptoms of urinary retention during the process and finally resorted to surgery. The mean manual bladder washout volume was 414.8 ± 115 mL. No procedure-associated complications occurred.
Figure 4.
Small blood clot fragments after manual bladder washout.
The patient demographics are provided in Table 1. The mean age of the patients was 61.2 ± 10.1 years (range, 42–82 years). As the table shows, the etiologies of the bladder blood clots were transurethral prostate resection (n = 7), photoselective vaporization of the prostate (n = 1), holmium laser enucleation of the prostate (n = 3), a bladder tumor (n = 4), transurethral resection of a bladder tumor (n = 3), percutaneous nephrolithotomy (n = 4), nephron-sparing surgery (n = 1), hemorrhagic nephritis (n = 2), and radiation cystitis (n = 6; prostate cancer in 4 and cervical cancer in 2). All patients with radiation cystitis had received external beam radiation therapy 3 to 10 years previously.
Table 1.
Patient characteristics and details of procedure.
| Parameters | Values |
|---|---|
| Number of patients | 31 |
| Sex | |
| Male | 17 (54.8) |
| Female | 14 (45.2) |
| Age, years | 61.2 ± 10.1 |
| Blood clot etiology | |
| TURP | 7 (22.6) |
| PVP | 1 (3.2) |
| HoLEP | 3 (9.7) |
| Bladder tumor | 4 (12.9) |
| TURBT | 3 (9.7) |
| PCNL | 4 (12.9) |
| NSS | 1 (3.2) |
| Hemorrhagic nephritis | 2 (6.5) |
| Radiation cystitis | 6 (19.4) |
| External beam radiation for prostate cancer | 4 (12.9) |
| External beam radiation for cervical cancer | 2 (6.5) |
| Size of clots, mL | 122.5 ± 39.7 |
| Time of procedure, minutes | 18.1 ± 5.4 |
| MBW volume, mL | 414.8 ± 115 |
Data are presented as n (%) or mean ± standard deviation.
TURP, transurethral prostate resection; PVP, photoselective vaporization of the prostate; HoLEP, holmium laser enucleation of the prostate; TURBT, transurethral resection of a bladder tumor; PCNL, percutaneous nephrolithotomy; NSS, nephron-sparing surgery; MBW, manual bladder washout.
Of the 27 patients who underwent successful clot evacuation, 25 completed the 6-month follow-up with no urinary irritation symptoms such as frequency, urgency, or dysuria. In 21 patients, the 6-month cystoscopy examination showed no abnormalities in the bladder cavity.
Discussion
In urological practice, a very common emergency that requires urgent therapy is hematuria. The causes of severe hematuria include surgical treatment of prostatic hyperplasia, urinary tract infection, a bladder tumor, percutaneous nephrolithotomy, and radiation cystitis. In this study, the main cause of the hematuria was surgical treatment of prostatic hyperplasia, including transurethral prostate resection (7/31, 22.6%), photoselective vaporization of the prostate (1/31, 3.2%), and holmium laser enucleation of the prostate (3/31, 9.7%). The second most common cause was a bladder tumor. When severe hematuria occurs, large numbers of blood clots accumulate in the bladder cavity, potentially leading to bladder tamponade and secondary acute urinary retention. Associated symptoms such as lower abdominal pain, restlessness, and elevated blood pressure may also occur. Bladder rupture can occur in rare cases. At this point, placement of an indwelling catheter is the primary treatment. However, the blood clots are very adhesive in the early stage, and catheters often become blocked. As a result, using an ordinary catheter is often ineffective in relieving the urinary tract obstruction and removing the blood clots.
Retention of blood clots in the bladder caused by severe hematuria must be treated on an emergency basis. If the etiology is clear, therapy should include treatment of the underlying cause and removal of the clot. If the etiology is unclear, identifying the cause is also important for evacuation of the clot. Therefore, appropriate clinical strategies are crucial in patients with bladder blood clots.
In general, manual bladder irrigation is a simple procedure involving the use of a syringe, a Foley catheter, and saline. Multiple factors may influence the effect of manual bladder washout, such as the catheter type and size, twisting/catheter manipulation, clot plus 1 L rule (i.e., the washout is not complete until 1 L of irrigation fluid has been returned with no further clot or dark hematuria), and others.9 The rate of catheter blockage is very high because of the adhesive property of blood clots. Therefore, the manual washing procedure is often time-consuming, exhausting, and inefficient, and patients’ suffering is prolonged. Additionally, the use of transurethral instruments such as cystoscopes and resectoscopes for blood clot evacuation usually requires operation under general anesthesia, which can lead to higher medical expenses and an increased frequency of patient movement. However, reducing the patient’s movement is crucial when blood clots originate from renal vessels; in such cases, interventional surgery for bleeding is inevitable. If the patient’s blood clots are resolved using a simple method, the doctor–patient trust relationship will be enhanced. In the present study, three of four patients who had been treated by percutaneous nephrolithotomy agreed to undergo embolization of the renal artery for bleeding. Therefore, exploring a treatment method that can solve the clinical problem of blood clot-induced bladder tamponade by simple manual bladder irrigation has great clinical value.
When the blood clots were mixed with hydrogen peroxide solution in the present study, we found that the severity of clot adhesion was reduced and that the clots became looser and more fragile. In clinical practice, 3% hydrogen peroxide is widely used as an antibacterial and disinfectant agent. It is used for wound debridement and can also be orally administered as a mouth rinse or tooth whitener.10 Its safety and effectiveness have been confirmed. Kalloo et al.11 and Lennon and Kalloo12 used hydrogen peroxide in patients with acute upper gastrointestinal bleeding and found that it could alter the characteristics of the blood clots. The authors presumed that hydrogen peroxide can enhance clot dissolution and endoscopic visualization in patients with acute upper gastrointestinal bleeding. These findings were supported in a similar report by Wu et al.13 These authors shared their experience of successfully using hydrogen peroxide for better visualization of the stomach and duodenum during acute upper gastrointestinal bleeding. Additionally, they provided evidence of minimal histological damage associated with hydrogen peroxide through histological analysis.
In urology, neither adherent nor mobilized bladder blood clots can be easily removed. Traditional catheter irrigation easily results in catheter blockage and is inefficient. Transurethral cystoscopy to remove blood clots is cumbersome, costly, and time-consuming. Thus, a simple and efficient method for removing bladder blood clots is urgently needed. In 2006, Warlick et al.7 used 0.15% to 0.30% hydrogen peroxide for blood clot evacuation in two patients and found that the clots were easily removed with no complications. A comparative clinical observation in our institute showed that using low-concentration hydrogen peroxide solution for continuous bladder irrigation after transurethral resection was superior to using normal saline.8 We found that using hydrogen peroxide solution for bladder irrigation reduced the catheter blockage rate and aggregation of blood clots in the bladder in patients who had undergone transurethral prostate resection. On this basis, using hydrogen peroxide to evacuate bladder clots was feasible. In our center, 31 patients with bladder blood clots underwent hydrogen peroxide bladder irrigation, and clot clearance was successful in 27 of these patients. The clinical symptoms caused by the bladder clots, such as frequent urination, urgency, and pain, were alleviated. The reason for procedure failure in the remaining four patients was not technical; rather, the failure was due to the patients’ low tolerance of urinary retention. At the 6-month follow-up, 21 patients underwent cystoscopy and no obvious abnormalities were found in the bladder mucosa.
In this study, use of the three-cavity Foley catheter with large-diameter side holes was also important. This catheter had three large holes at the tip to reduce blockage when removing tissue fragments. Another tool in the procedure was an irrigation syringe, as shown in Figure 2. This syringe could be tightly attached to the end of the Foley catheter, allowing less strenuous performance of manual bladder irrigation. Thus, bladder clot evacuation can be simplified by combining hydrogen peroxide solution with the two above-mentioned tools. Treatment using this method can be performed at the bedside and even in the emergency room. No adverse effects of hydrogen peroxide occurred during our procedure. Although the precise mechanism underlying decomposition of blood clots by hydrogen peroxide is unclear, we suggest that this method can be used for most bladder clots on an emergency basis.
Conclusion
Hydrogen peroxide may be helpful in weakening the adhesive property of bladder blood clots and promoting clot disruption. Thus, using hydrogen peroxide for bladder blood clot evacuation in patients with hematuria is a simple and effective method that can be used in an emergency.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
The present study was supported by the National Natural Science Foundation of China (grant no. 81773221 to Dr. J. Zhu), the Natural Science Foundation of Jiangsu Province (grant no. BK20161222 to Dr. J. Zhu), the Suzhou Science and Technology Planed Projects (grant nos. SYS201629 and SS201857 to Dr. J. Zhu), and the Grant for Key Young Talents of Medicine in Jiangsu (grant no. QNRC2016875 to Dr. J. Zhu).
ORCID iD
References
- 1.Ritch CR, Ordonez MA, Okhunov Z, et al. Pilot study of alteplase (tissue plasminogen activator) for treatment of urinary clot retention in an in vitro model. J Endourol 2009; 23: 1353–1357. DOI: 10.1089/end.2008.0513. [DOI] [PubMed] [Google Scholar]
- 2.Goel A, Dalela D. Mechanical suction for clot evacuation: experience with “suction bridge” for safe and effective clot removal. Int Urol Nephrol 2015; 47: 723–726. DOI: 10.1007/s11255-015-0962-8. [DOI] [PubMed] [Google Scholar]
- 3.Doersch KM, Navetta AF, Bird ET, et al. Case series: bladder clot evacuation using a prostate morcellation device. Can Urol Assoc J 2017; 11: E311–E314. DOI: 10.5489/cuaj.4219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Su YT, Huang KH, Chuang FC, et al. Use of an Ellik evacuator to remove tenacious bladder clots resulting from transvaginal oocyte retrieval: 2 cases and a literature review. Taiwan J Obstet Gynecol 2019; 58: 880–884. DOI: 10.1016/j.tjog.2019.05.033. [DOI] [PubMed] [Google Scholar]
- 5.Moharamzadeh P, Ojaghihaghighi S, Amjadi M, et al. Effect of tranexamic acid on gross hematuria: a pilot randomized clinical trial study. Am J Emerg Med 2017; 35: 1922–1925. DOI: 10.1016/j.ajem. 2017.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Bo J, Yangyang Y, Jiayuan L, et al. Evaluation of bladder clots using a nonsurgical treatment. Urology 2014; 83: 498–499. DOI: 10.1016/j.urology.2013.09.022. [DOI] [PubMed] [Google Scholar]
- 7.Warlick CA, Mouli SK, Allaf ME, et al. Bladder irrigation using hydrogen peroxide for clot evacuation. Urology 2006; 68: 1331–1332. DOI: 10.1016/j. urology. 2006. 08. 1090. [DOI] [PubMed] [Google Scholar]
- 8.Xu M, Xue BX, Yang DR, et al. [Low-concentration hydrogen peroxide solution for continuous bladder irrigation after transurethral resection of the prostate]. Zhonghua Nan Ke Xue 2018; 24: 345–348. [PubMed] [Google Scholar]
- 9.Clarebrough E, McGrath S, Christidis D, et al. CATCH-22: a manual bladder washout protocol to improve care for clot retention. World J Urol 2018; 36: 2043–2050. DOI: 10.1007/s00345-018-2346-z. [DOI] [PubMed] [Google Scholar]
- 10.Li Y. Biological properties of peroxide-containing tooth whiteners. Food Chem Toxicol 1996; 34: 887–904. [DOI] [PubMed] [Google Scholar]
- 11.Kalloo AN, Canto MI, Wadwa KS, et al. Clinical usefulness of 3% hydrogen peroxide in acute upper GI bleeding: a pilot study. Gastrointest Endosc 1999; 49: 518–521. [DOI] [PubMed] [Google Scholar]
- 12.Lennon AM, Kalloo AN. Hydrogen peroxide in upper gastrointestinal bleeding: a coming of age? Dig Dis Sci 2010; 55: 223–225. DOI: 10.1007/s10620-009-1078-8. [DOI] [PubMed] [Google Scholar]
- 13.Wu DC, Lu CY, Lu CH, et al. Endoscopic hydrogen peroxide spray may facilitate localization of the bleeding site in acute upper gastrointestinal bleeding. Endoscopy 1999; 31: 237–241. DOI: 10.1055/s-1999-13675. [DOI] [PubMed] [Google Scholar]