Abstract
Background
Exercise is a key component of physical health and quality of life for people living with dementia; however, challenges related to dementia symptoms and aging can make it difficult for people living with dementia to engage in exercise. While immersive virtual reality is showing increasing promise for exercise and rehabilitation applications, there is a lack of research regarding its use with people living with dementia.
Methods
Through participatory design with exercise therapists, kinesiologists, and people living with dementia, we designed two virtual reality environments (a farm and a gym) that were implemented on head-mounted displays to support five different upper-body exercises. Virtual reality and comparable human-guided exercises were tested with six people living with dementia. Both qualitative and quantitative measures were used, including reaching distance, distance traversed, and speed as well as feelings of enjoyment, engagement, interest, easiness, comfort, and level of effort.
Results
Participants’ subjective responses, motion, and fitness parameters all demonstrated comparable results between virtual reality and human-guided exercises. Therapists’ feedback also supported virtual reality exercise as an appropriate and engaging method for people living with dementia.
Conclusions
Collaborating with experts and people living with dementia throughout the design process resulted in an intuitive and engaging design. The results suggest that head-mounted virtual reality has promising potential to support physical activity for people living with dementia.
Keywords: Dementia, exergames, virtual reality, game design, participatory design, exercise motivation
Introduction
The average age of the world population is increasing due to longer lifespans and lower birthrates. In 2017, people 60 years and older comprised 13% of the population and is expected to increase to 21% by 2050.1 Aging research is now attracting considerable attention, with the particular focus on chronic adverse health conditions and related care for older adults. One such condition, dementia, encompasses wide range of chronic cognitive impairments and increases in prevalence with age. Earlier and more accurate diagnosis are resulting in a rise in dementia that is outpacing aging, from 50 million persons in 2017 to a predicted 132 million by 2050.1 Dementia is a major cause of disability and dependency in older adults and is the seventh leading cause of death.2
Dementia symptoms include impaired memory, path finding, decision-making, and language processing, all of which directly affect the quality of life for people living with dementia (PWD). Pharmacological treatments can be expensive, are not always effective, and may have adverse effects.3,4 Non-pharmacological interventions, however, can mitigate symptoms for many people and are an increasing focus of research.3
One intervention is physical activity, which has been shown to positively affect both physical5,6 and cognitive health.7–9 The exact impact of different types of exercise, especially aerobic, is undergoing investigation.10 For example, in one study, regular aerobic exercise led to improved cognitive abilities measured by Mini-Mental State Examination (MMSE) for PWD.11 The impact of other exercises such as cycling, walking, gait training, and balance have been also investigated in recent research, most of which conclude that physical activity has a positive impact on cognitive health.12,13 The enhancement of fitness parameters such as muscle strength and balance are another reported benefit of physical activity,14 which can help PWD have better functionality in performing their daily life activities. Physical activity promotes a wider range of positive impacts beyond physical and cognition for PWD, such as enhanced social health,15 reduced depression,16–18 and improved general mood.17
Despite the reported benefits of exercise for PWD, challenges related to dementia and aging make PWD less likely to engage to exercise, particularly in the later stages of the condition. The reported bidirectional relation of physical activity and brain health19 also shows that PWD are less successful in performing physical activity compared to older adults without dementia. Because most exercise programs in long-term care facilities for PWD are led by physical therapists in a group setting, impairments in language processing and task planning can make it difficult for PWD to join in. They may also be hampered by distractions and it is hard to move at their own pace. If PWD feel uncomfortable exercising in a group setting they are likely unmotivated to attend group exercise classes.
Virtual reality (VR)-based exercise is a new approach to complement the abilities of users in many health-related applications, especially rehabilitation.20 It can enable customizable exercise that can be done by individuals at their own pace. PWD can also experience activities that may be impossible or difficult in the real world, such as rowing a boat. Lastly, VR with tracking devices are able to quantitatively record motion parameters, which could enable further analysis and new clinical assessments. Different studies have used VR for PWD with different purposes,21 such as memory assessment and training,22–24 cognitive assessment,25 and navigation training and assessment.26 Traditionally, VR-based programs for physical activities for PWD employed interface devices such as touch screen,27,28 TV and PC,29 and Wii.30 Recently, head-mounted display VR (HMD-VR), which provides a fully immersive sense of the virtual world, is becoming increasingly available and affordable. It has been used for older adults targeting aspects such as executive functions and memory assessment;31 for PWD, the existing applications of HMD-VR have been limited to cognitive assessment.32,33 The use of VR in rehabilitation usually leverages a serious game to achieve a rehabilitation goal.34
While VR has been used in many applications related to the cognitive assessment of PWD, only a few studies investigated VR-based physical exercise. To our knowledge, no previous work has systematically designed and evaluated HMD-VR exercise programs for the specific purpose of engaging PWD in physical exercise. While HMD-VR is a portable and immersive technology with promising potential, there is a lack of studies evaluating it with PWD. Based on the literature, we expect that HMD-VR has the potential to support physical exercise for PWD, and the benefits may be comparable to therapist-led exercise in long-term care settings. We also expect that the fully immersive nature of HMD-VR can help PWD better engage in the exercise. This paper describes the co-design and evaluation of two HMD-VR-based games to engage PWD in outcomes-based exercise.
Objectives
The goal of this research was to investigate whether playing games and interacting with virtual objects in VR could be comparable alternative to (human) therapist-led exercise for PWD. Therefore, this research compared the use of HMD-VR to engage PWD in exercise with one-on-one therapist-led exercise. This was accomplished through two main objectives: (1) collaboration with exercise therapists and PWD to co-create HMD-VR-based exercise games for PWD and (2) a comparison study of HMD-VR versus therapist-led exercise.
Method
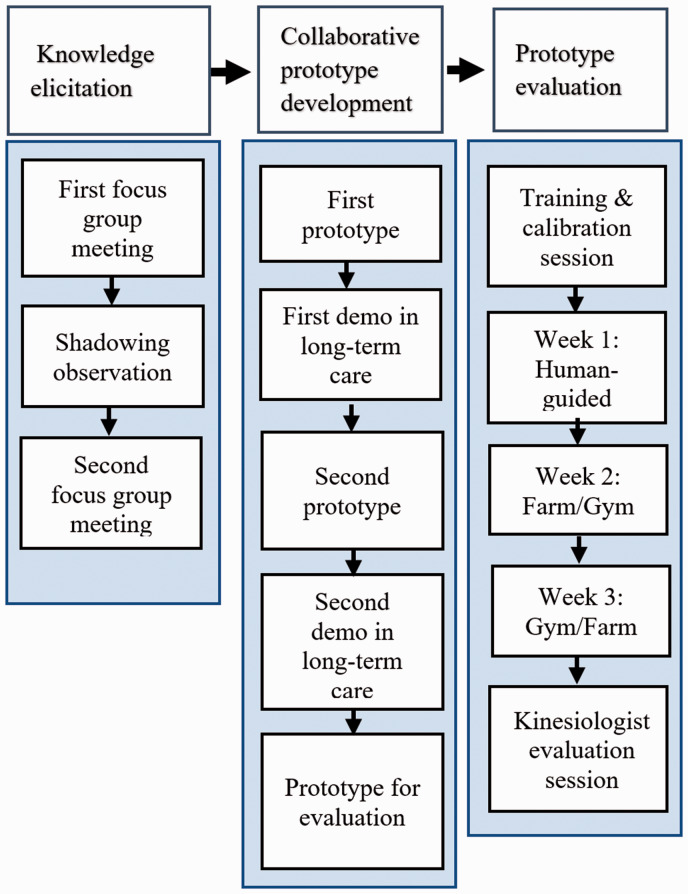
The study protocol is shown schematically in Figure 1 and has three main phases: (1) knowledge elicitation, 2) collaborative prototype development, and (3) prototype evaluation.
Figure 1.
Schematic of study protocol.
Knowledge elicitation
The design of any new technology for PWD must begin by gaining first-hand knowledge about their needs, wants, and abilities. Our knowledge elicitation phase incorporated two user experience design techniques: focus groups and shadowing observations. These were used to not only observe the characteristics of PWD but also to understand how they interact with people and objects in daily life. The first focus group meeting involved the University of Waterloo research team plus 25 kinesiologists and recreational therapists from Schlegel Villages (an organization of 19 long-term care and retirement communities across southern Ontario, Canada). We introduced a sample HMD-VR device and asked attendees for ideas of how they could envision this type of technology being helpful in supporting PWD. One therapist who showed particular interest in the project joined the research team to participate in the co-design process.
Following the first focus group, the research team from the University of Waterloo each conducted an 8-h shadowing observation session in a Schlegel Village long-term care center. The team members found opportunities to talk with residents and participate in their daily activities.
An important observation in this phase was the limited physical activity of most of the residents, despite available facilities and planned events. Following the shadowing observations, a second focus group was held with 12 kinesiologists, eight exercise therapists, and three PWD. The researchers presented two sample off-the-shelf VR programs, “Through the Ages: President Obama Celebrates America’s National Parks” and “NVIDIA VR Funhouse,” which were chosen to demonstrate the capabilities of HMD-VR and spark discussion regarding possible games for supporting exercise for PWD. Feedback from this meeting included all participants supporting the idea of using HMD-VR for exercise for PWD; however, concerns were raised about whether or not PWD would be comfortable using this technology for exercise, both from a physical and psychological perspective (i.e. primarily whether PWD might find the technology confusing or disorienting).
Collaborative prototype development
Setup and device
An Oculus Rift CV1 was selected as HMD-VR system. CV1 has two main components: a HMD and two handheld touch controllers. One advantage of CV1 is that its HMD provides a wide 110-degree field of view in the 3D virtual environment, which is close to one’s natural viewing angle. The high-resolution and high refresh rate of displays in CV1 is another advantage that provides users with better-quality images and motion of objects. To process and generate real-time game views for CV1, a personal (desktop) computer with 12GB of RAM, running Windows 7, and a NVIDIA GTX 1070 graphics card was used. The Unity3D game engine (version 5.6) was used for the game design.
Collaborative development
The research team (including the exercise therapist who joined the team from the first focus group) employed an iterative, collaborative approach to game design and usability testing. As outlined in Figure 1, there were two usability testing phases where we demonstrated our prototypes to kinesiologists, exercise therapists, and PWD. In the first usability test, nine kinesiologists and three PWD who tried the preliminary, low-fidelity games and gave feedback to the design team. We modified the games based on this feedback, prepared the new versions of the games and conducted Beta testing of these with two kinesiologists and three PWD before the main experiment.
Selecting appropriate motions for the exercise program for PWD in VR is crucial to ensuring the PWD engage in beneficial exercise activities. After discussions with exercise therapists and considering safety, we decided to focus on upper body motions, including hand, shoulder, and head motions, which could be performed in a seated position. These consultations resulted in five motions from daily exercise programs in long-term care that are considered to be beneficial for older adults (Table 1; left column).
Table 1.
Selected motions and corresponding game activities.
| Motion | Activity in farm game |
|---|---|
| Neck rotation | Watching a butterfly |
| Reaching over head | Lifting a box of apples |
| Reaching forward and straight | Sorting fruits in buckets |
| Reaching forward and across body | Sorting fruits in buckets |
| Rowing | Rowing a rowboat |
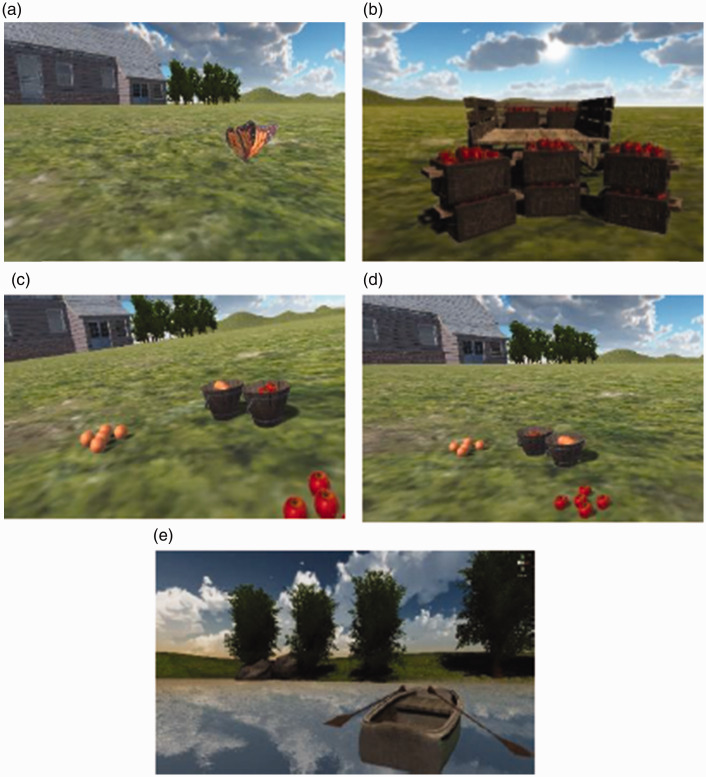
For VR games, two environments, a farm and a gym, were selected as they are gender neutral and many exercise-related activities can be simulated in them. They also represent environments that are familiar for most PWD living in Schlegel Villages, based on our consultation with therapists. For the farm environment, we selected five activities to elicit the desired motions (Table 1; right column). Figure 2 shows screenshots of the tasks designed for each activity in the farm environment.
Figure 2.
Activities used in the farm environment.
While the design of the farm tasks focused on matching exercise motions to natural activities, the design of the gym environment was intended to replicate therapist-led exercise in VR. For the gym environment, we designed an avatar to serve as the participant’s virtual exercise therapist and guide to the exercises from Table 1. The avatar’s motions were generated by the exercise therapist on our team and captured using Microsoft Xbox 360 Kinect. As requested by the therapists, the time of each activity in the virtual gym and virtual farm were kept to less than 5 min to avoid fatigue.
The VR programs were created with specific considerations for PWD.35 One important consideration was that the interactions with objects in virtual environments should be designed to be at the minimal level of complexity to make actions such as accessing/grabbing/and placing objects as easy as possible. For example, the boundary of sensitivity of interactions with any object in virtual environment were considered to be greater than the object’s boundary, such that participant could easily grab/place object by placing his/her hand close enough to the object. In addition, in contrast to design of many mass-market games, wrong actions and interactions with objects were minimized to prevent unnecessary confusion or distraction of participants from the main task. For example, software did not allow participants to put a type of fruit in a bucket assigned to another fruit type in the fruit sorting task. Also, a fruit could not be dropped when it had been grabbed by participant unless it was located on the top of the correct bucket.
The activities listed in were merged into the final software. During the transition between two activities, voice instructions were played to guide the participants, and the researcher changed the activities in the software program for the participants.
Voice instructions were recorded by our exercise therapist team member, synchronized with the tasks in the farm environment and the motions in the gym, and then integrated into the software. The software was designed to record hand and head positions during each activity from the hand controllers and HMD of the VR system at a sample rate of 90 Hz. Recorded positions were automatically saved in CSV files.
Calibration
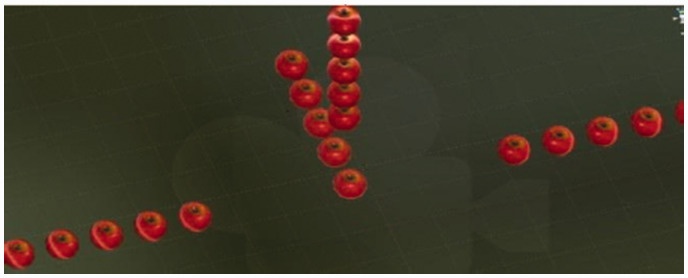
An important observation from the demos of prototypes design for sample PWD was the large variation of reaching distance amongst PWD because of confounding conditions, such as arthritis and stroke. Therefore, any design of VR games with the goal of exercise for PWD should take into account this variation by enabling customization to the movement abilities of the people using it. To this end, we designed and implemented a calibration game to extract the reaching distance of each participant. Figure 3 shows a snapshot of the calibration game, where the user reaches for target apples in four different directions: up, right, left, and front.
Figure 3.
Calibration game screenshot.33
The person’s customized maximum reaching distance was calibrated to the furthest apple that the person was able to reach in each direction. This distance was then used to automatically set the distance of objects in the farm environment so that the user could reach them. Figure 4 shows a person with dementia performing the calibration game.
Figure 4.
A person with dementia performing the calibration game.
Prototype evaluation
In this section, the details of the prototype evaluation including participant recruitment, data collection, and data analysis methods are discussed.
Participant recruitment
In collaboration with the staff of a long-term care residence we recruited eight participants. Table 2 summarizes the inclusion and exclusion criteria, which are reflective of PWD participating in an exercise program for PWD. For all potential participants, the Montreal Cognitive Assessment (MoCA) was administered to their gauge cognitive level. MoCA is a common test for screening cognitive impairments.36 The MoCA’s score ranges from 0 to 30 with higher values indicating higher cognitive function level. MoCA scores between 19 to 25 are identified as mild cognitive impairment. Participants who met our inclusion criteria (which included a MoCA score between 15 and 25) continued with the consent procedure. Of the eight initially identified potential participates, one of them decided not to participate and another one declined to continue after the first day of trials. Therefore, six participants were included in this study. Table 3 reports the demographics of these participants. The study has been reviewed and received ethics clearance through a University of Waterloo Research Ethics Committee (ORE# 22300). Participants provided written informed consent. The exercise therapist and the student researcher were both present in all the sessions to ensure participants were comfortable and safe.
Table 2.
List of the inclusion and exclusion criteria set.
| Inclusion criteria |
| 60 years and older |
| Able to communicate verbally in English |
| At least four years of education |
| Score between 15 and 25 on the MoCA |
| At level 1 (independent transfer) or level 2 (one-person transfer) on the Transfer Status Assessment Guide |
| Exclusion criteria |
| Moderate or severe cognitive impairment |
| Prone to motion sickness |
| Has hearing impairment |
| Any pre-existing conditions that would preclude the exercise activity as advised by neighborhood coordinator or exercise therapist |
| A history of epilepsy and/or seizures |
| Having a pacemaker (as per Oculus instruction manual) |
MoCA: Montreal Cognitive Assessment.
Table 3.
Participant demographics.
| Participant ID | Age | Gender | MoCA* |
|---|---|---|---|
| 1 | 92 | F | 15 |
| 2 | 92 | F | 15 |
| 3 | 87 | M | 19 |
| 4 | 91 | F | 18 |
| 5 | 77 | F | 18 |
| 6 | 82 | F | 20 |
| Average | 86.8 ± 6.2 | --- | 17.5 ± 2.1 |
*MoCA: Montreal Cognitive Assessment.
Study procedure
A within-subjects study was employed to assess PWD before and after exercise using VR games. To compare the impact of VR exercise games with therapist-led exercise, we considered three different exercise conditions as the independent variables: (1) exercise with the guidance of therapist (therapist-led), (2) exercise in a virtual gym, and (3) exercise on a virtual farm.
As depicted in the schematic of the study design in Figure 1, after the recruitment procedure, each participant attended in a short training session. The goal of the training session was to familiarize them with the VR technology and the designed environments. To this end, first the device setup, including HMD and touch controllers, was introduced to the participants, and then they tried a sample virtual environment (the fruit sorting scenario) for a short time. They also played our custom-built calibration game to extract reaching distance so the games could be calibrated to each individual by using this data to scale the position of objects (as a result range of motions) in 80% of max reach distance in the virtual games.
The evaluation portion of the study consisted of three weeks of trials. Each participant began with one week of therapist-led exercise led by the team’s exercise therapist. Participants were evenly and randomly assigned to one of the two virtual environments for the second week and then switched to the other VR environment in the third week. The motions, order of motions, and number of repetitions were fixed in all the three environments (therapist-led, gym, and farm). Participants performed each week’s designated task for five days of that week and each day the exercise session was about 20 min. All the sessions were video recorded for future analysis by the research team.
Data collection
Qualitative and quantitative methods were used to investigate the applicability of exercise delivery via VR-based games, as shown in Table 4. The qualitative evaluation methods recorded participants’ perceptions and exercise therapist’s impressions, while the quantitative methods were used to measure the motion and other physical parameters. We explain data collection methods in detail in the following subsections.
Table 4.
The evaluation methods used in this study.
| Measure | Type | Tools | Description |
|---|---|---|---|
| Participants’ questionnaire | Subjective rating | Paper-based 5-point Likert scale questionnaire | Feelings including enjoyment, easiness, comfort, enough workout, and engagement |
| Participant interview | Subjective comments | Verbal and note taking | Open-ended feedback, such as pros and cons and recommendations |
| Kinesiologists questionnaire | Subjective rating and comments | Paper-based questionnaire (5-point Likert scale and open-ended questions) | Feedback on selected activities, level of exercise, and recommendations |
| Exercise therapist observation | Subjective comments | Note taking | Feedback, any observation from exercise sessions |
| SFFA** | Quantitative and objective | Measuring tape | Physical measurement for estimating fitness of upper body |
| Shoulder circumduction | Quantitative and objective | Measuring tape | Shoulder flexibility |
| Motion Parameter | Quantitative and objective | Touch controller | Reaching distance, speed, and distance |
**SFFA: Schlegel Functional Fitness Assessment.
Self-reporting by participants: Two participant questionnaires were used; the first was used after each day’s activity and the second after finishing each week (each environment). The questions were constructed through consultation with exercise therapists, considering exercise engagement as the main goal. Daily questions asked were about subjective assessment of enjoyment and quality of workout using 5-point Likert scale questions. Weekly questionnaires asked about engagement, interest, ease, and comfort of participants working with each environment. Open-ended participant interviews were also conducted and recorded after each session to obtain general feedback and gain a deeper insight about how they perceived engaging in the exercise games. The answers of participants to the open-ended questions in the feedback forms in addition to the notes recorded in the interviews were used to capture the participants’ impressions. This feedback was also taken to reflect points that were important to the participants that may have been missed in the questionnaires.
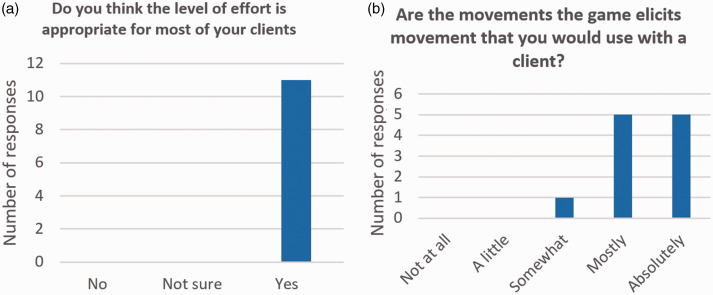
Expert feedback: Expert opinions about the game and user activity in the games was collected by recording our exercise therapist team member’s feedback during the experiment as well as feedback from 11 kinesiologists, who tried the game themselves at the end of the study. The exercise therapist on our team recorded all details of observations and thoughts that occurred during all days of the experiment. Kinesiologists used a questionnaire to record their opinions about the game and selected activities after they tried the games themselves.
Physical parameter measurements: Two types of physical measurements were used in this study: clinical physical measurements and motion parameters. The clinical physical measurements were gauged physical reaching distance of participants using two established methods: the Schlegel Functional Fitness Assessment (SFFA) and shoulder circumduction protocol. The SFFA is an evidence-based assessment measuring functional fitness for long-term care residents and consists of a short list of measurements including height, head-to-wall, reach downward, reach upward, and grip strength. The shoulder circumduction assessment measures length of acromion and shoulder circumduction using a flexible measuring tape. In addition to clinical physical measurements, motion parameters were recorded using sensor data obtained from the touch controllers and HMD of Oculus Rift CV1. The movement of the participants’ hand and head were measured during each session while participants played the game.
Data analysis
A statistical analysis (repeated measures ANOVA) of the answers to Likert scale questions from the daily and weekly questionnaires were used to explore participants’ perceptions of the three conditions.
From the evaluation methods described in the previous section, exercise therapist and kinesiologist feedback are considered to be very important as they are the experts in this field. Moreover, if shown to be effective, VR exergames would complement conventional therapy and could be a valuable assessment tool for professionals working with exercise for PWD. Therefore, the resulting design must also align with their needs if it is to be useful and accepted. The highlighted points in the answers were used to report the strength, weakness, suitability of design and selections, and possible suggestions for extension.
The quantitative measurements were statistically analysed using repeated measure ANOVA to compare exercise level and physical activity or abilities over the three weeks.37 The SFFA and shoulder circumduction as the clinical measurements were compared from the beginning of the experiment and after each week.
Results
The process of designing the games with PWD and therapists resulted in a list of design considerations for a VR-based exercise program for PWD, such as gameplay that requires no button presses, minimal cognitive complexity in tasks, high contrast of target objects, and targets being placed clearly within the field of view. The design considerations are summarized in Table 5 and more details are presented in our previous publications.35,38 One additional requirement of the design highlighted through our testing was the benefit of using audio instructions to give participants information about what they were supposed to do.
Table 5.
Design considerations for VR program for PWD.35
| Applying participatory design by consulting with specialists and involving PWD through the design process. |
| Keeping target object(s) of each activity in VR in the front view of participants. |
| Using no button or control from device(s). Try to implement interactions with body motions. |
| Using verbal instruction and prompts during and between activities in VR to guide participants. |
| Using high contrast tasks |
| Adjusting the required range of motion in each activity for each participant. Using calibration game is a suggestion to extract reaching distance of each participant. |
VR: virtual reality; PWD: people living with dementia.
With respect to subjective measures, as shown in Figure 5, participants indicated fairly high levels of enjoyment for both VR environments (both 3.80) that were comparable to therapist-led exercise (3.67); a statistical analysis using a repeated measure ANOVA showed no significant difference between conditions (F(2,10) = 0.727, p = 0.507, = 0.127). We also evaluated participants’ satisfaction with the amount of physical activity in each session using daily yes/no questions (Figure 6). In this evaluation, only two participants were not completely satisfied; one of them preferred to perform different motions instead of repetition of a specific motion and the other preferred more challenging tasks (as he had been a body builder).
Figure 5.
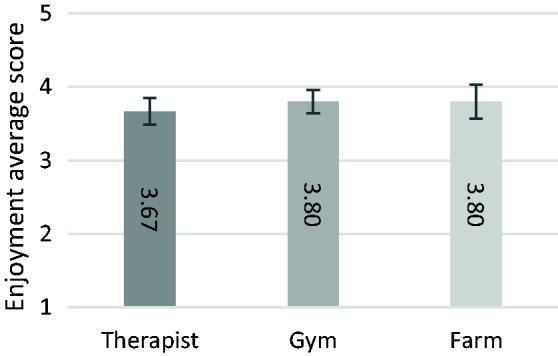
Participants’ self-rated level of enjoyment from daily activities in three environments measured by the 5-point Likert scale, where 5 is “loved it” and 1 is “hated it”.
Figure 6.
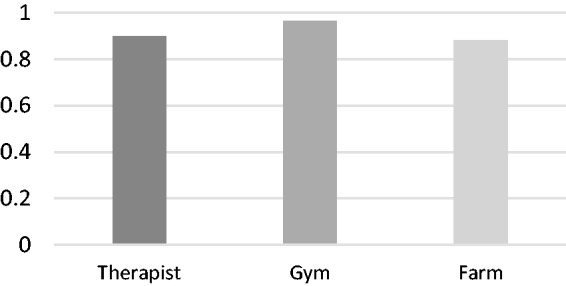
Participants’ self-rated perception of whether they got enough physical exercise in each environment. The scores were obtained from average values from the daily questionnaire where 0 represents feeling not enough workout and 1 means feeling enough workout.
Participants’ feelings of comfort, ease of use, engagement, and interest in each environment were evaluated by using 5-point Likert questions asked once a week, as shown in Figure 7. The ease of use levels for virtual environments were similar (4.17) to those for the therapist-led week (3.6) with no statistically significant difference (repeated measures ANOVA, F(2,8) = 2.364, p = 0.156, = 0.371).
Figure 7.
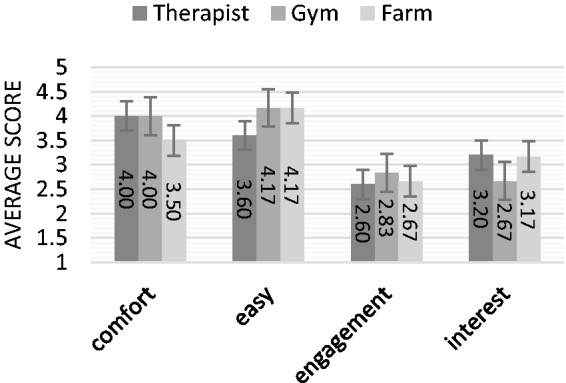
Participants’ responses to the after-scenario questionnaire to evaluate quality of their experience. Comfort, ease of use, and interest were measured using a 5-point scale, where 5 means “strongly agree” and 1 means “strongly disagree”. The engagement level was measured with a 4-point scale: 4 for “extremely engaged” and 1 for “not engaged at all”.
In the short interviews after each session, participants expressed their opinions about the exercise program and their activity on that day. The research team recorded all answers; some illustrative points are quoted in Table 6.
Table 6.
Representative quotes from participants regarding their impressions of the VR exergames.
| Quote | Participant # |
|---|---|
| “I love looking at the blue sky, the sky and switching the apples and rowing a boat which I really wasn't, yeah, look like that I was moving” | 4 |
| “I love rowing because it was relaxing, you know, when you are relaxing you are exercising” | 1 |
| “Good for everyone. rowing relaxing” | 1 |
| “Too easy. Engaging environment” | 6 |
| “It was a longer class today, rowing, … I could [keep] going” | 6 |
| “I think I could grab them fast, faster than what I did this before” | 4 |
| “I haven't been on water for a long time, so I don't know, but it's not bad, we can keep trying” | 4 |
| “That was nice. that's test for mental.” | 4 |
| “Too much repetition. more motion needed. everything was the same.” | 2 |
| “There wasn't that many apples” | 4 |
| “Wish it would be more challenging.” | 4 |
| "It's difficult to row to get nothing” | 6 |
VR: virtual reality.
The observations made by the exercise therapist during the experiment included valuable feedback from an expert perspective. The exercise therapist reported her observations regarding the participants’ performance and feeling such as:
“[one of the participants] talks to the system and answers it.”
“[Another participant after the first day] immediately grasped the oars and started rowing without waiting for the instructions”
“One of the participants verbalized what the butterfly was doing and followed the butterfly.”
The exercise therapists also reported progress in many cases, for example:
“[one of them] rowed longer today and seemed less frustrated”
“for a participant who had problem in the first day) … got first basket immediately; keeps putting hands too narrow but today did aim for top”
Based on the exercise therapist’s observations, she believed that the VR environments were successful in providing enjoyable activities with the goal of exercise, for example:
“Interesting to see that most residents do not recognize the parity of the movements between the three environments; furthermore, they don’t consider this as exercise”
In the dedicated session with 11 kinesiologists, we presented the game design and experiment setup. After they had tried the games, they completed a questionnaire asking about the appropriateness of the selected activities in the virtual environment and the level of exercise in the design. The results obtained from this survey are summarized in Figure 8.
Figure 8.
Kinesiologists’ feedback on the appropriateness of (a) the level and (b) type of exercise and movements selected in this study (n = 11).
The clinical measurements, including reaching upward, grip strength, and shoulder circumduction, were collected in four steps of the experiment and are reported in Figure 9.
Figure 9.
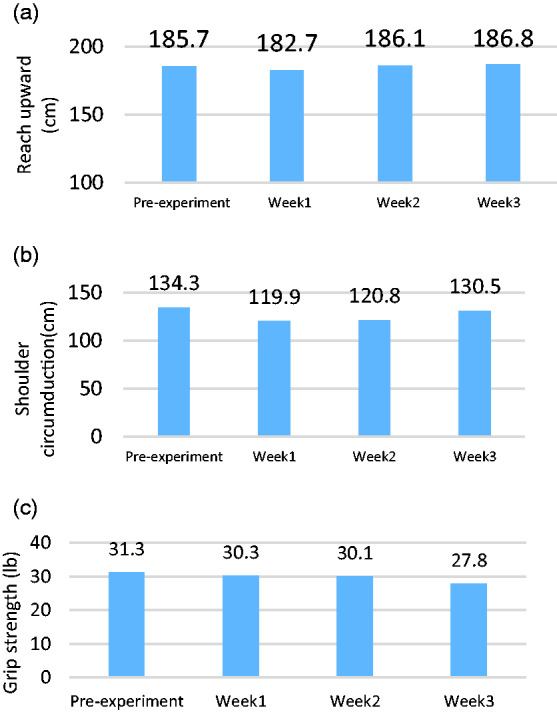
Reaching upward for both right (a) and left (b) hand for all six participants using a single measurement at the end of each week.
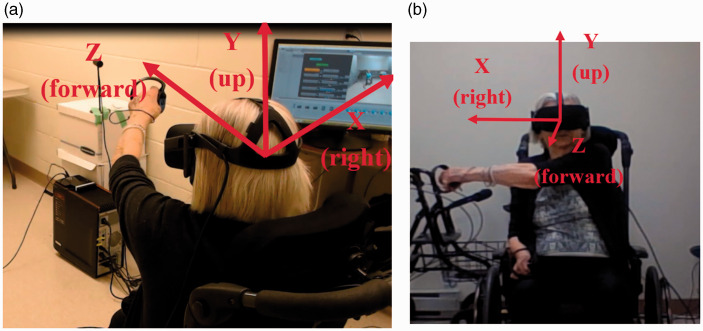
To measure the motion parameters, we fixed a three-dimensional coordinate system relative to the VR-system (Figure 10) that was used for all measurements. In Figure 10, the center of the coordinate system is the center of each participant’s head.
Figure 10.
Three-dimensional coordinate system introduced and used in the analysis of motion captured by sensor. The coordinate system has been shown in both view of back and front for a participant.39
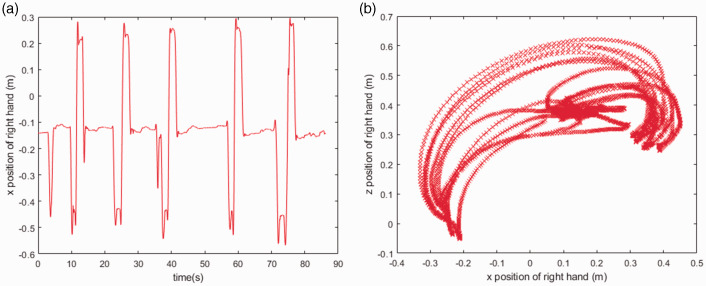
Figure 11(a) demonstrates tracking a left-hand movement in the x direction, of a user performing forward-cross reaching activity. The corresponding 2D tracking of the hand is shown in Figure 11(b). From the position of hands recorded during each activity, we extracted the motion parameters defined in the previous section.
Figure 11.
Example position data for a participant from the left hand for the reach forward-across reaching activity with (a) position of hand during the time and (b) range of motion in the x and z directions.39
Table 7 shows the average reaching distance in the X, Y, and Z directions for all participants in the three different environments and for four different activities. For each activity, only the direction of motion that was the target of the activity is displayed. For example, in the reaching overhead movement, the exercise is designed to produce a hand-stretching motion in the Y and Z directions.
Table 7.
Absolute reaching distance (cm) of participants in three dimensions of x, y, and z for different activities in three conditions (therapist, gym, and farm).
| Activity\Condition | Therapist |
Gym |
Farm |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Direction | X | Y | Z | X | Y | Z | X | Y | Z |
| Overhead | – | 114 | 58 | – | 60 | 47 | – | 61 | 55 |
| Forward straight | 51 | – | 51 | 85 | – | 55 | 89 | – | 52 |
| Forward across | 75 | – | 46 | 90 | – | 54 | 95 | – | 51 |
| Rowing | – | 33 | 53 | – | 42 | 61 | – | 41 | 48 |
An analysis of values reported in Table 7 show that the reaching distance in each direction was similar across different activities and for both therapist-led exercise and virtual reality exercise conditions. therapist-led with no statistically significant difference.
Another parameter extracted related to the motion data was the distance traversed by each participants’ hand. Table 8 shows the total distance in each condition. Participants appear to have similar levels of activity in terms of hand motion under the different conditions of the experiment.
Table 8.
Average traversed distance (m) by participants’ hand in different activities in three conditions.
| Activity\Condition | Therapist | Gym | Farm |
|---|---|---|---|
| Overhead | 14.43 | 10.24 | 11.48 |
| Forward straight | 16.35 | 17.94 | 18.72 |
| Forward across | 16.26 | 18.29 | 21.65 |
| Rowing | 62.23 | 63.23 | 54.59 |
The speed of motion in an activity measured by Oculus sensor can be compared in different environments. Table 9 shows the average speed of motion of participants in different activities and for three different environments. An analysis of speed values reported in Table 9 shows that speed in different environments was similar.
Table 9.
Average speed (m/s) of motion in each activity for the three different conditions.
| Activity\Condition | Therapist | Gym | Farm |
|---|---|---|---|
| Overhead | 0.22 | 0.23 | 0.26 |
| Forward straight | 0.14 | 0.27 | 0.23 |
| Forward across | 0.16 | 0.27 | 0.25 |
| Rowing | 0.18 | 0.27 | 0.25 |
Discussion
The goal of this research was to investigate whether an HMD-VR games-based exercise for PWD is a feasible approach as well as whether VR games can perform comparably to one-on-one therapist-led exercise.
The design techniques that we used in this study, such as focus groups, shadowing observation, and collaborative design, had many benefits. First, we obtained valuable feedback from experts throughout the design process. Second, by engaging PWD in intermediate testing of the prototype, we were better able to understand what aspects were working well and what needed to be changed.
The results of this study suggest that HMD-VR can indeed be used to engage PWD in exercise in a manner that is comparable to therapist-led exercise. All the participants completed the exercises using HMD-VR on all days and reported that they had an adequate workout in VR that was comparable to therapist-led exercise. There appeared to be no difficulties in using touch controllers to interact with objects in the games. The ease of use in working with VR games as reported in Figure 7 shows participants found exercising in VR as easy as human-guided exercise. The quotes recorded from the participants indicates they felt comfortable playing exercise games in VR. The exercise therapist observed very fast learning for all the participants, who were all first-time VR users. Taken together, these results give good support that HMD-VR exergames can be accessible and fun for PWD.
One concern raised by kinesiologists at the beginning of this study was whether PWD could use HMD-VR at all, considering that they had no experience with such technology and might find it complicated or confusing. The results of this study suggest that co-designing with ongoing input from therapists and PWD can result in HMD-VR games that are usable, relevant, and enjoyable for PWD. A key aspect of this study is to ensure the design of the game and gameplay support the abilities and needs of PWD, so as to make interaction easy, intuitive, and accessible.
The feedback of kinesiologists indicated they agreed with the selection of motion and activities for PWD. There was a positive feedback in the notes by the exercise therapists that were observed and recorded during the sessions, which suggests that the designed games and participants’ interactions exceeded the expectation of the exercise therapists. In addition to enabling a different modality of accessing exercise for PWD, the clinical measurement of fitness parameters and recording of motion parameters can show both participants’ engagement in the exercise and possible physical health improvements. While the fitness parameters tracked in this study showed no significant improvements, our sample size was small and the intervention period relatively short. However, our data suggests that HMD-VR is able to elicit a level of fitness similar to that of one-on-one therapist-led exercise, which is the present gold standard. Kinesiologists and exercise therapists confirmed that it is unlikely we would see any significant change in such a short (three weeks) exercise program in these measures; at the least, participants had the opportunity to engage in daily exercise. Future studies are needed to test VR exergames in long-term use.
Regarding the motion parameters extracted from sensor measurements such as reaching distance and traversed distance, as reported in Tables 7 and 8, the VR games appeared to work as well as therapist-led methods in engaging PWD to exercise. Our statistical analysis also showed no significant difference between the activities. Variations in the motion parameters such as the difference in Y-reaching distance in therapist-led exercise could be the result of the differences in simulating the same activities in therapist-led exercise and VR games. Participants appeared to traverse comparable distances while playing the games in VR and in a real exercise session and experienced a similar level of activity.
The above observations support the use of the VR-based exercise for PWD, as they enjoyed working in VR and had a similar level of exercise compared to therapist-led sessions.
As the motion parameters extracted for each user can be related to his/her fitness parameters, we investigated the correlation between clinical fitness measurement and motion parameters as reported in Table 10. According to this table, while grip strength is not correlated with any motion parameter, both Shoulder Circumduction and Reach Upward have a significant correlation (r > 0.8 or r > 0.9) with many motion parameters. It shows that the motion behaviors observed in the games are limited by individual motion capabilities. This suggests that motion parameters measured from the VR games might be used to estimate traditional clinical measurements of fitness.
Table 10.
Correlation between motion parameters and clinical measurements.
| Correlation coefficient | Grip strength (lb) | Shoulder circumduction (cm) | Reach upward (cm) |
|---|---|---|---|
| Grip strength (lb) | 1 | ||
| Shoulder circumduction (cm) | 0.664 | 1 | |
| Reach upward (cm) | 0.733 | .902* | 1 |
| Rowing ROM X | 0.037 | −0.477 | −0.636 |
| Cross ROM X | 0.209 | 0.81 | 0.728 |
| Straight ROM X | 0.372 | 0.769 | .868* |
| Overhead ROM X | 0.245 | 0.688 | 0.709 |
| Rowing ROM Y | 0.289 | 0.696 | 0.748 |
| Cross ROM Y | 0.345 | .837* | 0.806 |
| Straight ROM Y | 0.541 | .831* | .918** |
| Overhead ROM Y | 0.441 | .944** | .834* |
| Rowing ROM Z | 0.52 | 0.359 | 0.111 |
| Cross ROM Z | 0.484 | .911* | .932** |
| Straight ROM Z | 0.506 | .862* | .952** |
| Overhead ROM Z | 0.572 | .957** | .888* |
| Rowing distance | 0.601 | 0.727 | 0.55 |
| Cross distance | 0.461 | .856* | .874* |
| Straight distance | 0.602 | 0.804 | .971** |
| Overhead distance | 0.613 | .968** | .910* |
*p < 0.05.
**p < 0.01.
From the results of this study, the design appears to have been successful in promoting engagement in physical activity for PWD, which was the main goal in this work. The results showed that PWD can play the HMD-VR games and enjoy playing which involve having physical activity We hope that regularly using exercise games such as these, PWD could have better quality of life based on the reported benefits of physical activity for their both cognitive function and physical health. As this research represents proof-of-concept work, the level of impact will need to be validated through long-term use investigated in future studies with more games.
Methodological considerations
As this research was a proof-of-concept study, it employed a relatively small sample size that was recruited from the same long-term care facility, which may have introduced bias in the results. The diversity of interests and abilities of PWD highlight the need to involve more participants from different facilities to reach more substantial conclusions; this will be addressed in future work.
There are some recommendations for researchers who want to work on the design of the exercise program in VR for PWD. Collaborative design involving PWD in the design process as well as consulting with the kinesiologists and exercise therapists working with PWD can accelerate targeted development and hone applicability. In terms of game design, keeping visual targets in the virtual environment close to the center of field of view, providing verbal instructions, avoiding using buttons in interactions, preventing errors, using high contrast tasks, and customizing motions by using a calibration procedure were found to be key in enabling PWD to access and enjoy our HMD-VR games. It is also worth recognizing the diverse physical abilities and preferences of PWD in general; the activities in VR games might be preferred by some participants but not others, an important consideration in the success in any future game designs.
Conclusions
The results from this study support the feasibility of HMD-VR games for upper-body exercise for PWD. Participants enjoyed the VR exergames and physical assessment outcome measures from the VR conditions were similar to the therapist-led condition. This suggests that HMD-VR exergames have the potential to engage PWD as effectively as one-on-one therapists. Long-term tests with more participants and a greater variety of exercises and VR environments are needed to further investigate the impact of VR games in engaging PWD in exercise.
Acknowledgements
The authors thanks Schlegel Villages for the opportunity to run this study; in particular, the residents who participated in the development and evaluation as well as the kinesiologists and exercise therapists who shared their knowledge and experience. Special thanks to the exercise therapist on our team, Laura Domenicucci, who worked with the authors to identify the exercises, design the games, and run the prototype tests.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Guarantor
JB.
Contributorship
ME, SC, and JB conceived the study. Mentored by SC and JB, ME executed protocol development, gaining ethical approval, patient recruitment and data analysis as her MASc thesis research. ME wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research and publication of this article was supported by JB’s Schlegel Research Chair funds and SC and JB’s faculty start-up funds. The authors received no financial support for the authorship of this article.
ORCID iDs
Mazhar Eisapour https://orcid.org/0000-0002-5492-1556
Jennifer Boger https://orcid.org/0000-0001-6150-151X
References
- 1.World Health Organization. Dementia: Fact Sheet No. 362. 2017. WHO, https://www.who.int/en/news-room/fact-sheets/detail/dementia (accessed November 2018, 2017;2)
- 2.United Nation. World Population Prospects The 2017. Revision. 2017.
- 3.Fenney A, Lee TD. Exploring spared capacity in persons with dementia: What WiiTM can learn. Act Adapt Aging 2010; 34: 303–313. [Google Scholar]
- 4.Kavirajan H, Schneider LS. Efficacy and adverse effects of cholinesterase inhibitors and memantine in vascular dementia: A meta-analysis of randomised controlled trials. Lancet Neurol 2007; 6: 782–792. [DOI] [PubMed] [Google Scholar]
- 5.Potter R, Ellard D, Rees K, et al. A systematic review of the effects of physical activity on physical functioning, quality of life and depression in older people with dementia. Int J Geriatr Psychiatry 2011; 26: 1000–1011. [DOI] [PubMed] [Google Scholar]
- 6.Bossers WJR, van der Woude LH V, Boersma F, et al. A 9-week aerobic and strength training program improves cognitive and motor function in patients with dementia: a randomized, controlled trial. Am J Geriatr Psychiatry 2015; 23: 1106–1016. [DOI] [PubMed] [Google Scholar]
- 7.Öhman H, Savikko N, Strandberg TE, et al. Effect of physical exercise on cognitive performance in older adults with mild cognitive impairment or dementia: a systematic review. Dement Geriatr Cogn Disord 2014; 38: 347–365. [DOI] [PubMed] [Google Scholar]
- 8.Gallaway PJ, Miyake H, Buchowski MS, et al. Physical activity: a viable way to reduce the risks of mild cognitive impairment, Alzheimer’s disease, and vascular dementia in older adults. Brain Sci 2017; 7: 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cheng S-T, Chow PK, Song Y-Q, et al. Mental and physical activities delay cognitive decline in older persons with dementia. Am J Geriatr Psychiatry 2014; 22: 63–74. [DOI] [PubMed] [Google Scholar]
- 10.Kramer AF, Erickson KI. Capitalizing on cortical plasticity: influence of physical activity on cognition and brain function. Trends Cogn Sci 2007; 11: 342–348. [DOI] [PubMed] [Google Scholar]
- 11.Zheng G, Xia R, Zhou W, et al. Aerobic exercise ameliorates cognitive function in older adults with mild cognitive impairment: a systematic review and meta-analysis of randomised controlled trials. Br J Sport Med 2016; 50: 1443–1450. [DOI] [PubMed] [Google Scholar]
- 12.Perrochon A, Tchalla AE, Bonis J, et al. Effects of a multicomponent exercise program on spatiotemporal gait parameters, risk of falling and physical activity in dementia patients. Dement Geriatr Cogn Dis Extra 2015; 5: 350–360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Trautwein S, Scharpf A, Barisch-Fritz B, et al. Effectiveness of a 16-week multimodal exercise program on individuals with dementia: study protocol for a multicenter randomized controlled trial. JMIR Res Protoc 2017; 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Santana-Sosa E, Barriopedro MI, Lopez-Mojares LM, et al. Exercise training is beneficial for Alzheimer’s patients. Int J Sports Med 2008; 29: 845. [DOI] [PubMed] [Google Scholar]
- 15.Forbes D, Forbes SC, Blake CM, et al. Exercise programs for people with dementia. Cochrane Libr 2015; (4): CD006489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conradsson M, Littbrand H, Lindelöf N, et al. Effects of a high-intensity functional exercise programme on depressive symptoms and psychological well-being among older people living in residential care facilities: a cluster-randomized controlled trial. Aging Ment Health 2010; 14: 565–576. [DOI] [PubMed] [Google Scholar]
- 17.Eggermont LHP, Knol DL, Hol EM, et al. Hand motor activity, cognition, mood, and the rest–activity rhythm in dementia: A clustered RCT. Behav Brain Res 2009; 196: 271–278. [DOI] [PubMed] [Google Scholar]
- 18.Rolland Y, Pillard F, Klapouszczak A, et al. Exercise program for nursing home residents with Alzheimer’s disease: A 1-year randomized, controlled trial. J Am Geriatr Soc 2007; 55: 158–165. [DOI] [PubMed] [Google Scholar]
- 19.Loprinzi PD, Herod SM, Cardinal BJ, et al. Physical activity and the brain: a review of this dynamic, bi-directional relationship. Brain Res 2013; 1539: 95–104. [DOI] [PubMed] [Google Scholar]
- 20.Laver K, George S, Thomas S, et al. Cochrane review: virtual reality for stroke rehabilitation. Eur J Phys Rehabil Med 2012; 48: 523–530. [PubMed] [Google Scholar]
- 21.Dove E, Hons B, Astell AJ, et al. The use of motion-based technology for people living with dementia or mild cognitive impairment: A literature review. J Med Internet Res 2017; 19: e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allain P, Foloppe DA, Besnard J, et al. Detecting everyday action deficits in Alzheimer’s disease using a nonimmersive virtual reality kitchen. J Int Neuropsychol Soc 2014; 20: 468–477. [DOI] [PubMed] [Google Scholar]
- 23.Cherniack EP. Not just fun and games: Applications of virtual reality in the identification and rehabilitation of cognitive disorders of the elderly. Disabil Rehabil Assist Technol 2011; 6: 283–289. [DOI] [PubMed] [Google Scholar]
- 24.Man DWK, Chung JCC, Lee GYY. Evaluation of a virtual reality-based memory training programme for Hong Kong Chinese older adults with questionable dementia: A pilot study. Int J Geriatr Psychiatry 2012; 27: 513–20. [DOI] [PubMed] [Google Scholar]
- 25.Mendez MF, Joshi A, Jimenez E. Virtual reality for the assessment of frontotemporal dementia, a feasibility study. Disabil Rehabil Assist Technol 2015; 10: 160–164. [DOI] [PubMed] [Google Scholar]
- 26.Van Schaik P, Martyr A, Blackman T, et al. Involving persons with dementia in the evaluation of outdoor environments. CyberPsychology Behav 2008; 11: 415–424. [DOI] [PubMed] [Google Scholar]
- 27.Konstantinidis EI, Billis AS, Mouzakidis CA, et al. Design, implementation, and wide pilot deployment of FitForAll: An easy to use exergaming platform improving physical fitness and life quality of senior citizens. IEEE J Biomed Heal informatic 2014; 20: 189–200. [DOI] [PubMed] [Google Scholar]
- 28.Billis AS, Konstantinidis EI, Ladas AI, et al. Evaluating affective usability experiences of an exergaming platform for seniors. In: 2011 10th International workshop on biomedical engineering IEEE, 2011, pp.1–4.
- 29.McEwen D, Taillon-Hobson A, Bilodeau M, et al. Two-week virtual reality training for dementia: Single case feasibility study. J Rehabil Res Dev 2014; 51: 1069–1076. [DOI] [PubMed] [Google Scholar]
- 30.Higgins HC, Horton JK, Hodgkinson BC, et al. Lessons learned: Staff perceptions of the Nintendo Wii as a health promotion tool within an aged-care and disability service. Heal Promot J Aust 2010; 21: 189–195. [DOI] [PubMed] [Google Scholar]
- 31.Yeh SC, Chen YC, Tsai CF, et al. An innovative virtual reality system for mild cognitive impairment: Diagnosis and evaluation. In: 2012 IEEE-EMBS conference on biomedical engineering and sciences, Langkawi, 2012, pp.23–27.
- 32.Ijaz K, Ahmadpour N, Naismith SL, et al. An immersive virtual reality platform for assessing spatial navigation memory in predementia screening: Feasibility and usability study. JMIR Ment Heal 2019; 6: e13887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liappas N, Garc\’\ia-Betances RI, Teriús-Padrón JG, et al. Studying the technological barriers and needs of people with dementia: A quantitative study. In: 2018 IEEE international conference on pervasive computing and communications workshops (PerCom Workshops). Athens, Greece, 2018, pp.884–889.
- 34.Laver KE, Lange B, George S, et al. Virtual reality for stroke rehabilitation. Cochrane Database Syst Rev 2017; 11: CD008349. [DOI] [PMC free article] [PubMed]
- 35.Eisapour M, Cao S, Domenicucci L, et al. Participatory design of a virtual reality exercise for people with mild cognitive impairment. In: The ACM conference on human factors in computing systems Montreal, Canada: ACM SIGCHI, 2018.
- 36.Nasreddine ZS, Phillips NA, Bédirian V, et al. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc 2005; 53: 695–699. [DOI] [PubMed] [Google Scholar]
- 37.Eisapour M, Cao S, Domenicucci L, et al. Virtual reality exergames for people living with dementia based on exercise therapy best practices. Proc Hum Factors Ergon Soc Annu Meet 2018; 62: 528–532. [Google Scholar]
- 38.Eisapour M. Design and evaluation of virtual reality exergames for people living with dementia Thesis, University of Waterloo, Canada, 2018.
- 39.Eisapour M, Cao S, Boger JN. Game design for users with constraint: Exergame for older adults with cognitive impairment. In: 31st ACM user interface software and technology symposium Berlin; 2018.