Abstract
Background:
The basic health service is a fundamental right of every citizen. Appropriate use of medicine is an essential component for the quality of health. Drug use evaluation is a systematic and criteria-based drug evaluation, which ensures the appropriate use of the drug. The purpose of this study was to analyze the drug use situation in primary healthcare centers of Kathmandu valley.
Methodology:
A cross-sectional descriptive study was performed in all primary healthcare centers of Kathmandu valley. Six hundred prescriptions were analyzed retrospectively, choosing a simple random sampling method for prescribing indicators. One hundred twenty patients were interviewed for patient-care indicators, and health facility representatives were interviewed for health facility indicators. Drug use indicators developed by World Health Organization/International Network for Rational Use of Drugs were used with slight modification.
Result:
The average number of drugs per encounter was 2.6. The percentage of drugs prescribed by generic names and from the essential medicine list was 60% and 80.9%, respectively. The prescriptions encounters with antibiotics and injections were 58% and 4.2%, respectively. The average consultation and dispensing time were 3.6 min and 54.4 s, respectively. The percentage of drugs actually dispensed was 76.6%. Only half of the patients knew the correct dose of the dispensed drug and no adequate labeling at all. The majority of dispensers were intern nursing students (42%), and all prescribers were medical officers. Ten out of 12 primary healthcare centers had a copy of EML. The availability of key drugs in primary healthcare centers was incomplete (64.7%).
Conclusion:
The observed values for all World Health Organization indicators deviated from the optimal range. Patient care provided by health facilities was insufficient and thus an effective intervention program for the promotion of rational drug use practice is recommended.
Keywords: Drug use pattern, World Health Organization indicators, primary healthcare center, Nepal
Background
The basic health service is a fundamental right of every citizen. The health policy of Nepal 2014 aims to provide basic health services free of cost equipped with essential drugs, diagnostics, and skilled human resources.1 The government of Nepal declared to provide essential healthcare services to all people through primary healthcare centers (PHCs).2 PHCs make up an integral part of the country’s healthcare system. It serves as a basic primary health care provider at an electoral constituency level.
Medicine plays a vital element in the healthcare service. Patients observe medicines as an essential outcome of their visit. Appropriate use of medicine is essential to ensure the quality of health services received by patients.3,4 The appropriate use of medicine means patients receive medications appropriate to their clinical needs, in doses that meet their requirements for adequate time at the lowest cost.5 It is also one of the objectives of National Drug Policy 1995.6
Irrational use of drugs is common in all countries but relatively higher in developing countries, where routine monitoring of medicine use is weak.7–9 The common types of irrational use are too many medicines per patient, inappropriate use of antibiotics, overuse of injections when oral medication is more appropriate, and failure to use following clinical guidelines.8 The irrational use of medicine results in unnecessary adverse drug reactions (ADRs), increased patient expenses, antibiotic resistance, drug interaction, and ineffective treatment, which may lead to treatment failure.3 Conversely, the rational use of medicines can reduce global morbidity and mortality significantly.4
Previous studies among government health facilities showed insufficient patient-care services.9,10 They revealed irrational practices on the use of antibiotics, brand prescribing, and incomplete knowledge of patients regarding medicine use and incomplete access to prescribed medicine.9,10 Globally, more than 50% of all medicines are prescribed, dispensed, or sold inappropriately, and half of the patients do not take the prescribed drugs correctly. In addition, about one-third of the world population lacks access to essential medicine. However, 20%–40% of the health budget in developing countries is spent on medicine.5,11 The recent National health policy of Nepal also points to the challenge of providing primary health care programs, including qualitative, essential, and affordable medicine aspired by constitution.1
The World Health Organization (WHO) in collaboration with the International Network of Rational Use of Drugs (INRUD) developed a set of indicators to measure the performance of healthcare facilities in prescribing, patient care, and facility-specific aspects.12 WHO indicators are globally accepted methods, which have been used in more than 30 developing countries to study the appropriate use of the drug.3 In Nepal, limited studies have assessed drug use practices in primary health care settings to author’s knowledge. This study aims to assess drug use patterns using WHO/INRUD core indicators, additionally including prescriber and dispenser qualifications in PHCs of Kathmandu valley districts. This study is supposed to provide a basis to examine the status of the service provided by health facilities and to promote basic quality health services through the rational use of medicine.
Material and methods
Design and setting
This was a cross-sectional descriptive study carried out in PHCs of three districts (Kathmandu, Bhaktapur, and Lalitpur) in July 2018. There were 12 PHCs in these three districts. All the PHCs were selected for the study. These districts are located in the central part and the capital city of Nepal. Prescription indicators–related information was retrospectively studied from the recorded data, while the patient care and health facility indicators were prospectively collected at the time of visit.
Study population and sample size
The study population included all the PHCs of Kathmandu, Bhaktapur, and Lalitpur districts. There were seven PHCs in Kathmandu, two in Bhaktapur, and three in Lalitpur district. Altogether 12 PHCs were studied and evaluated. As per the WHO guidelines, the minimum recommended sample for retrospective prescription analysis is 600.12 Thus, for prescription-related studies, 600 prescriptions were analyzed retrospectively, meaning 50 prescriptions per PHC were randomly selected between May and June 2018. All prescription data were selected irrespective of age, gender, and disease. On a pre-study visit, retrieving the old manual data was found to be difficult and practically not possible; therefore, the recent 2 months of data were selected for the study. The retrospective method was used because the patient flow per day was very low (around 10). For patient-care-related indicators, patients visiting the PHCs were requested to take part in the study. All the patients interviewed were found to be visiting for the first time for their respective illness. One hundred twenty patients (10 patients per PHC), representing all age groups and diseases except pregnant women, were selected randomly and interviewed prospectively at the time of the visit. The sample number for patient care was calculated based on previous study and tentative patient visits per day.9 For facility-related indicators, the in-charge or representative of PHC present at the time of visit was interviewed for health facility–related study with prior consent.
Development of the questionnaires
The pre-designed form was prepared based on study objec-tives. The study questionnaires were prepared and conducted based on WHO/INRUD drug use indicators, which include prescribing, patient care, and health facility–specific indicators.12 The validation of the questionnaire was assured as the study used WHO/INRUD indicators which were widely used prior in Nepal and outside for similar study.3,9,11–13 The study instruments were initially pre-tested and consulted with senior pharmacist to ensure the validity of study. The slight modification was made under the patient-care indicators, including dispenser and prescriber qualifications (Annex-1 supplementary file).
Ethical consideration
The ethical approval was taken from the Nepal Health Research Council (Ref. No. 3125) before carrying out the study. The consent of the patient, medicine dispenser, and in-charge/representative of PHCs were taken before collecting data. The confidentiality of the data was maintained.
Process of data collection
The two authors were involved in data collection. The retrospective records of prescription and health facility data were collected from in-charge/representative of PHCs. Similarly, the data of patient-care indicators were noted by interviewing the patient.
Data management and analysis
Data were checked regularly for consistency and completeness after site visits. Microsoft Excel 2013 was used for data entry and analysis. WHO/INRUD methodology and formulas were applied for analysis.12 Descriptive statistics such as frequencies, mean, and percentages were measured. The optimal values were taken from the study of developing country for comparative study, which is shown in Table 1.3 The essential medicine list (EML) of Nepal 2016 and the free EML for health institutions issued in 2014 were used in the study.14,15 The results were presented in tabulated and pie chart form.
Table 1.
WHO indicators with their findings and optimal values.
| Prescribing indicators | Findings | Optimal value |
|---|---|---|
| Average number of drugs per encounter | 2.6 | 1.6–1.8 |
| Percentage of drugs prescribed by generic name | 60% | 100% |
| Percentage of encounters with an antibiotic prescribed | 58% | 20.0–26.8% |
| Percentage of encounters with an injection prescribed | 4.2% | 13.4–24.1% |
| Percentage of drugs prescribed from the list of essential drugs | 80.9% | 100% |
| Patient-care indicators | ||
| Average consultation time (minutes) | 3.6 | >10 |
| Average dispensing time (seconds) | 54.4 | >90 |
| Percentage of drugs actually dispensed | 76.6% | 100% |
| Percentage of drugs adequately labeled | 0% | 100% |
| Patient’s knowledge of correct dose | 50% | 100% |
| Health facility indicators | ||
| Availability of copy essential medicine list of Nepal 2016 | 83.3% | 100% |
| Availability of key drugs | 64.7% | 100% |
Operational definition
Antibiotics: Drugs, such as anti-bacterial agents, anti-infective dermatological drugs, anti-infective ophthalmological agents, and anti-diarrheal drugs like metronidazole, are considered as antibiotics in this study.
Key drugs: The key drugs under the health facility indicator refer to medicines designated by government for PHC in Nepal, to disseminate free of cost to patients.
Result
No indicators were aligning with optimal value. The average drug per prescription (2.6) and the antibiotic prescription (58%) were higher than the optimal value. In contrast, generic prescribing (60%), injection prescribing (4.2%), and prescribing from essential medicine (80.9%) were below the optimal value. The high deviation was seen in antibiotics, injections, and generic prescribing. The study showed at least one injection in 25 prescriptions (Table 1).
The patient consultation time to the prescriber and dispenser was very low. The average consultation time was found to be less than half (3.6 min) of optimal value (>10). Similarly, the average dispensing time was found to be low (54.4 s) compared to the optimal value (>90). The actual dispensing of the prescribed drug was 76.6%, which means around three drugs were dispensed out of four prescribed drugs. WHO recommended labeling was nil (0%), but the amount and frequency of drug administration were found to be labeled in primary packaging of 48% of dispensed medicine. Only half of the patients (50%) knew the correct dosing of the medicine they had been prescribed (Table 1).
More than half of PHCs (83.3%) were found to have an EML of Nepal. Out of 58 freely categorized drugs for PHCs, only 64.7% of drugs were found to be available at the time of the study. The maximum up to 48 and the minimum down to 25 medicines were found in PHCs. However, on average, 64.7% of medicines were available in PHCs (Table 1).
A total of 1559 drugs were prescribed to 600 patients. Out of 600 patients, about half of patients (43%) received three drugs in their prescriptions, and 31.2% of patients received two drugs in their prescriptions. Only one prescription was found to have no medicine. Among 58% of antibiotic prescribed prescriptions, single antibiotic per prescription was highest (48.5%) compared to two (8.7%) and three (0.8%) antibiotic per prescription. No antibiotics were prescribed in 252 (42%) prescriptions (Table 2).
Table 2.
Degree of medicine prescribed (n = 600).
| Number of medicine per prescription | Frequency (percentage) | Number of antibiotics per prescription | Frequency (percentage) |
|---|---|---|---|
| 0 | 1 (0.2) | 0 | 252 (42) |
| 1 | 73 (12.2) | 1 | 291 (48.5) |
| 2 | 187 (31.2) | 2 | 52 (8.7) |
| 3 | 258 (43) | 3 | 5 (0.8) |
| 4 | 71 (11.8) | ||
| 5 | 9 (1.5) | ||
| 6 | 1 (0.2) | ||
| Total | 600 (100) | Total | 600 (100) |
In all 12 PHCs, the medical officer was the only one involved in medicine prescribing practice.
The majority of dispensers were found to be intern students who are nursing students (42%) and intern health assistance (HA) students (8%). No pharmacy personnel were found in the dispensing practice (Figure 1).
Figure 1.
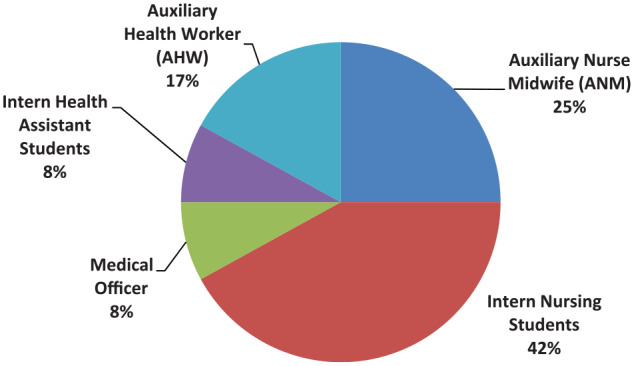
Dispenser qualification in PHCs of Kathmandu valley districts (n = 12).
A total of 96 different drug items and 18 antibiotics were prescribed in 600 prescriptions. The most commonly used medicine was acetaminophen, which is an analgesic and antipyretic agent, and ranitidine, which is an antiulcer agent. The most commonly used medicines belonged to EML of Nepal, and all were listed as free medicines for PHCs. Of the total 1559 drugs, 408 (26.2%) were antibiotics. The most commonly used antibiotic was amoxicillin followed by metronidazole and azithromycin. Except for only one ampicillin + cloxacillin, all antibiotics belonged to EML of Nepal (Table 3).
Table 3.
Frequently prescribed medicines (n = 1559) and antibiotics (n = 408).
| S. No. | Frequently prescribed medicine | Frequency (percentage) | S. No. | Frequently prescribed antibiotic | Frequency (percentage) |
|---|---|---|---|---|---|
| 1 | Acetaminophen | 217 (13.9) | 1 | Amoxicillin | 97 (23.8) |
| 2 | Ranitidine | 179 (11.5) | 2 | Metronidazole | 82 (20.1) |
| 3 | Amoxicillin | 97 (6.2) | 3 | Azithromycin | 63 (15.4) |
| 4 | Chlorpheniramine | 87 (5.6) | 4 | Ciprofloxacin | 63 (15.4) |
| 5 | Metronidazole | 82 (5.3) | 5 | Sulfamethoxazole + Trimethoprim | 34 (8.3) |
| 6 | Oral rehydration salt | 82 (5.3) | 6 | Cloxacillin | 29 (7.1) |
| 7 | Ibuprofen | 67 (4.3) | 7 | Cefixime | 16 (4) |
| 8 | Azithromycin | 63 (4) | 8 | Mupirocin | 6 (1.5) |
| 9 | Ciprofloxacin | 63 (4) | 9 | Ampicillin + Cloxacillin | 5 (1.2) |
| 10 | Vitamin B complex | 62 (4) | 10 | Amoxicillin + Clavulanic acid | 3 (0.7) |
Discussion
The prescribing pattern is a reflection of the quality of care delivered.4 The study revealed that the average number of drugs per encounter was 2.6, which was higher than the optimal value but lower than PHCs in Bangladesh (3.31), Pakistan (3.4), and Egypt (2.5).3,11,16 The maximum prescription (43%) contained three drugs, which is similar to PHCs in Madhya Pradesh, India, where maximum patients (37.3%) had three drugs.17 The study showed a maximum of six drugs per patient. This higher use of medicines may indicate a weaker health system prompting prescribers to combine more medicines to deliver the maximum clinical effect due to the absence of necessary medicine.4 This is probably due to a lack of prescriber skills in managing local illnesses or a lack of appropriate clinical guidelines. The lower use of drugs is desirable as it has a lower possibility of ADR, drug interaction, patient non-compliance, and economic burden. The in-depth study of patient’s therapeutic needs along with its unwanted consequences is to be analyzed to ensure quality and affordable services received by the patients.
The WHO strongly recommends prescribing in generic names as a safety precaution for patients because it identifies the drug clearly, enables better information exchange, and allows better communication between healthcare providers.16 However, generic prescribing was low (60%) compared to PHCs of Pakistan (71.6%), Egypt (95.4%), and Madhya Pradesh, India (60.9%) and higher compared to PHCs of Bangladesh (45.6%) and a recent study of Nepal (57.52%).3,10,11,16,17 In PHCs, 58 drugs were available for free as per government provision; therefore, whatever the brand name prescriber used in prescription, the medicines available in PHCs, of whichever brand name, are dispensed to the patient. Higher brand prescription in PHCs reflects the influence of pharmaceutical companies or prescriber’s higher faith in particular manufacturer products. Conversely, the medical council code and WHO manual on good prescribing strongly recommend prescribing in generic names.18,19 Therefore, low generic prescribing was a consequence of poor law and enforcement concerning generic prescribing from regulatory bodies.
The trend of antibiotic use was higher (58%) compared to PHCs of Bangladesh (49.1%) and Egypt (39.2%) but was lower than PHCs of India (67.5%).11,16,17 However, WHO indicates this value should be less than 30%.4 On the other hand, prescription containing single antibiotic was found higher (48.5%) compared to two (8.7%) and three (0.8%) antibiotics. Many studies assumed failure to determine the severity of illness or a lack of diagnostic facilities, free access to antibiotics in PHCs, and lack of appropriate policy and treatment guidelines as consequences of antibiotics overuse.4,9,20 PHCs lack equipped medical labs for antibiotic sensitivity studies, which promote the empirical use of antibiotics. The higher use of antibiotics can increase the possibility of antibiotic resistance, adverse effects, and frequent hospital admissions, which eventually increases the patients’ economic burden and need of high efficacious antibiotics for minor ailments; and hence the common antibiotics available free in PHCs would be useless.7 An effective mechanism has to be adapted to determine the actual need for antibiotics, and proper guidelines and education have to be introduced to ensure the quality of services the patient received.
The injection prescribed was low (4.2%). The result was far less than other studies conducted in PHCs of Pakistan (27.1%), PHCs of Bangladesh (13.6%), and optimal value (13.4%–24.1%).3,16 The lower uses of parenteral in PHCs signify the nature of patient’s illness and PHCs’ practice on parenteral prescribing. On the other hand, lower use of parenteral reduces the possibility of bloodborne diseases and cost of therapy.
The percentage of drugs prescribed from the EML was satisfactory (80.9%) compared to PHCs of other countries such as India (74.7%) and Bangladesh (62.6%), but lower compared to PHCs in Pakistan (93.4%) and Egypt (95.4%).3,11,16,17 However, it was low compared to the requirement (100%). The comparatively higher use of essential medicine available in PHCs indicates good utilization of resources available in PHCs as well as an inference that the access of medicines in PHCs is actually meeting the needs of patients. The use of EML must be promoted up to the maximum in PHCs as they are older, already tested in practice with established clinical use, and cost-effective than newer drugs.11
The average consultation time was 3.6 min, which was lower than an optimal value (>10 min) and PHCs of Egypt (7.1 min), but it was higher than PHCs of Pakistan (2.2 min).3,11 The study in Pakistan reported increasing workload as a reason for a short consultation time; but in our case, even though there was a lower patient flow, the consultation time was not high.3 Insufficient consultation time may lead to partial patient examination and consequent irrational therapy. Proper history collection, complete physical examination, appropriate health education, and good physician–patient interaction require sufficient consultation time.3 However, all the prescribers were medical officers, which is a good practice; but in their absence, auxiliary health workers take that role.
The average dispensing time was higher (54.36 s) compared to PHCs of Egypt (47.4 s) and Pakistan (38 s) but lower than an optimal value (>90 s).3,11The dispensing time was low even when the patient flow was very low. This insufficient dispensing time may reflect incomplete dissemination of essential information regarding medicine such as when to take medicine, medicine’s possible side-effects, and precautions to be taken. While checking the patient knowledge, only 50% (optimal value was 100%) of the patient knew about the number of drugs to be taken and the time of administration, which was 69% and 94% in PHCs in Pakistan and Egypt, respectively.3,11 Deficient information may result in incomplete knowledge which eventually may lead to failure of drug therapy and unwanted adverse drug events.3
Patient knowledge of the drug regimen can be improved with adequate labeling. However, WHO recommended drug-labeling practice was nil (0%) in our study, which is similar to the previous study of Health post of Nepal (0%) and PHCs of Egypt (0%), but it was 100% in PHCs of Pakistan.3,9,11 WHO recommends that each drug label should contain at least a patient’s name, drug name, and time of administration. However, the amount and frequency of drug administration were found to be labeled in 48% of dispensed medicine only. The study found that the majority of personnel involved in dispensing medicine were intern nursing students. Similarly, previous studies among community pharmacies and PHCs in Nepal also revealed higher non-pharmacy professionals in dispensary roles.10,21 This can be considered as the reason for low dispensing time, improper labeling, and patient knowledge in medicine. The lack of qualified health personnel was considered in resulting inadequate labeling of medications and insufficient time to counsel patients on the appropriate use of medicine like administration procedures, possible drug–food interactions, and side-effects.22 Pharmacists were considered expert healthcare personnel in advising patients on the rational use of medicine. They are essential in managing medicine-related issues to improve the appropriate use of medicines and eliminate medication errors. The lack of skill and knowledge of dispensers limits patient knowledge, which conclusively reflects in the low quality of services received by the patients.23
The percentage of drugs actually dispensed was 76.57 % (optimal value was 100%), while it was 90.9% and 95.9% in PHCs of Pakistan and Egypt, respectively.3,11 Access to medicine reflects the degree of services provided by the health care setting. Public confidence in the health system is suppressed when the medicines are not available.4 Medicine is a basic need for patients. The insufficient supply of medicine must be the result of a low percentage of actually dispensed medicine. The study found incomplete availability of drugs in PHCs. Only 64.65% of drugs were available. Patients visiting PHCs rely on drugs distributed at free of cost. The unavailability of designated free medicine in PHCs indicates the deprived basic healthcare service of the patient. The government aimed to promote an adequate supply of essential medicines at all levels of the government institution, whereas the study revealed insufficient and inadequate access to designated essential medicine in PHCs.6 The irregular and insufficient supply of medicine failed the goal of providing basic health care needs as a fundamental right of patients.24
A copy of EML was found to be present in 83.3% of PHCs (optimal value was 100%), while it was 100% in PHCs of Egypt and Pakistan.3,11 The study showed a satisfactory result as most of the PHCs had EML. The presence of EML in PHCs reflects the priority of health facility toward the use of essential medicine categorized to use in PHCs. WHO recommends adhering to a medicine listed in EML by the prescriber to ensure proper healthcare.11
A commonly used medicine reflects the medical situation of the patient to a very extent. The most commonly used medicines were acetaminophen and ranitidine. The overuse of nonsteroidal anti-inflammatory drugs (NSAIDs) reported causing serious effects on the gastrointestinal tract, cardiac, and renal system; thus, it should be used cautiously based on patient illness.25 The ranitidine use could be the reason for using analgesic-antipyretic agents or higher patients of gastroenteritis. Similarly, azithromycin, amoxicillin, and metronidazole were commonly prescribed antibiotics. These were commonly used in other PHCs as well.16 The most commonly used medicines were freely available in PHCs. On the contrary, the recent study carried out in the tertiary care hospital of Nepal showed pantoprazole, rabeprazole, and ibuprofen + acetaminophen as the most commonly prescribed drugs which are different, not available as free in PHCs, but belonged to the same category.26 It might be the result of different available resources and clinicians at the health facility.
Limitations
The study has a limitation of the short study period, small sample size for patient-care-related indicators, and limited in Kathmandu valley districts. The study reviewed retrospective data so there might be the limitation of information bias. The patient’s disease condition and age were not analyzed to examine the number and nature of the medicines prescribed. The optimal value was taken from a developing country, which may not be standard for comparison. These limitations may influence the generalization of the results obtained. However, despite this limitation, the findings of this study can help to understand basic health services focusing on the rational use of medicine in PHCs of Nepal.
Conclusion
All the WHO indicators were found to have deviated from the optimal value. Concerning prescribing indicators, antibiotic prescribing was found to have highly deviated comparatively. Conversely, the percentage of encounters with an injection prescribed was less. Generic prescribing was low. All the dispenser personnel were non-pharmacy, and intern students were also involved in dispensing, in fact, the majority of them, and patient consultation time was low along with poor patient knowledge about use of medicine they received. The designated essential medicines were not fully available in PHCs. The basic healthcare services in terms of medicine were very poor.
Recommendation
The study recommends immediate action toward the rational use of medicine and adequate access to required basic medicine needed to achieve universal health coverage. The qualified personnel along with sufficient consultation time are required to promote effective disease diagnosis and patient understanding of their role in treatment. The regulatory body must develop, implement, and monitor regulations to provide basic medicinal access from PHCs.
Supplemental Material
Supplemental material, Study_Questionnaire for Study on drug use pattern in primary healthcare centers of Kathmandu valley by Amrita Aryal, Asmita Dahal and Rajeev Shrestha in SAGE Open Medicine
Acknowledgments
The authors would like to thank all the patients and PHCs who contributed to the data collection and overall research conduction. The authors would also like to thank Mr Bijesh Mishra, PhD student, Oklahoma State University, USA, for his valuable suggestions in English language editing.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from ‘Ethical Review Board of Nepal Health Research Council (Approval No. 3125)’.
Informed consent: Verbal informed consent was obtained from patients and written informed consent was obtained from legally authorized representatives of study place before the study.
ORCID iD: Rajeev Shrestha  https://orcid.org/0000-0003-1822-3969
https://orcid.org/0000-0003-1822-3969
Supplemental material: Supplemental material for this article is available online.
References
- 1. Government of Nepal, Ministry of Health and Population, Department of Health Services. Annual Report Department of Health Services 2074/75 (2017/18), 1962, Kathmandu, https://dohs.gov.np/wp-content/uploads/2019/07/DoHS-Annual-Report-FY-2074-75-date-22-Ashad-2076-for-web-1.pdf [Google Scholar]
- 2. Jha N. Revitalizing primary health care and activities in Nepal. Heal Renaiss 2014; 11: 185–191. [Google Scholar]
- 3. Atif M, Sarwar MR, Azeem M, et al. Assessment of core drug use indicators using WHO/INRUD methodology at primary healthcare centers in Bahawalpur, Pakistan. BMC Health Serv Res 2016; 16(1): 684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ofori-Asenso R. A closer look at the World Health Organization’s prescribing indicators. J Pharmacol Pharmacother 2016; 7(1): 51–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. World Health Organization. The pursuit of responsible use of medicines: sharing and learning from country experiences, 2012, https://www.who.int/medicines/publications/responsible_use/en/
- 6. Government of Nepal. National Drug Policy, 1995, http://www.dda.gov.np/content/national-drug-policy-1995
- 7. Ofori-Asenso R, Brhlikova P, Pollock AM. Prescribing indicators at primary health care centers within the WHO African region: a systematic analysis (1995-2015). BMC Public Health 2016; 16: 724–016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mensa M, Tadesse T, Ayele A. Assessment of drug use pattern by using WHO core drug use indicators at public hospitals in Ethiopia. J Community Med Health Educ 2017; 07: 265–271. [Google Scholar]
- 9. Dahal P, Bhattarai B, Adhikari D, et al. Drug use pattern in primary health care facilities of Kaski district, Western Nepal. Sunsari Tech Coll J 2013; 1: 1–8. [Google Scholar]
- 10. Karki KB, Aryal KK, Gyawali P, et al. Quality of drugs and drug use patterns at different level of health care settings in Nepal, 2017, http://nhrc.gov.np/wp-content/uploads/2017/11/Final_Drug.pdf
- 11. Akl OA, El Mahalli AA, Elkahky AA, et al. WHO/INRUD drug use indicators at primary healthcare centers in Alexandria, Egypt. J Taibah Univ Med Sci 2014; 9: 54–64. [Google Scholar]
- 12. World Health Organization. How to investigate drug use in health facilities. Selected drug use indicators, 1993, https://www.who.int/medicines/publications/how-to-investigate_drug-use/en/
- 13. Lamichhane DC, Giri BR, Pathak OK, et al. Morbidity profile and prescribing patterns among outpatients in a teaching hospital in Western Nepal. Mcgill J Med 2006; 9(2): 126–133. [PMC free article] [PubMed] [Google Scholar]
- 14. Government of Nepal. Free essential drug for Health Institution, https://www.publichealthupdate.com/list-of-free-essential-drugs-for-health-institutions-nepal/
- 15. Ministry of Health. National list of essential medicines Nepal. 5th Rev. Government of Nepal, Ministry of Health and Population, Department of Health Services, 2016, http://apps.who.int/medicinedocs/documents/s23537en/s23537en.pdf [Google Scholar]
- 16. Momtaz H, Tomalika N, Mohsena M, et al. Morbidity and drug prescribing patterns at a rural primary health care center of Bangladesh. IMC J Med Sci 2019; 12: 50–56. [Google Scholar]
- 17. Bhartiy SS, Shinde M, Nandeshwar S, et al. Pattern of prescribing practices in the Madhya Pradesh, India. Kathmandu Univ Med J (KUMJ) 2008; 6(1): 55–59. [PubMed] [Google Scholar]
- 18. De Vries TPGM, Henning RH, Hogerzeil D, et al. Guide to good prescribing, 2000, p. 142, https://apps.who.int/iris/bitstream/handle/10665/59001/WHO_DAP_94.11.pdf
- 19. Nepal Medical Council. Nepal Medical Council Code of Ethics 2072, 2017, https://nmc.org.np/nmc-code-of-ethics
- 20. Otoom S, Culligan K, Al-Assoomi B, et al. Analysis of drug prescriptions in primary health care centres in Bahrain. East Mediterr Health J 2010; 16(5): 511–515. [PubMed] [Google Scholar]
- 21. Shrestha R, Ghale A. Study of good pharmacy practice in community pharmacy of three districts of Kathmandu valley, Nepal. Int J Sci Reports 2018; 4: 240. [Google Scholar]
- 22. Asif I. Irrational use of medicines—a threat to patient community, 2009, https://ezinearticles.com/?Irrational-Use-of-Medicines—A-Threat-to-Patient-Community&id=3144554
- 23. Hussain A, Ibrahim MIM. Qualification, knowledge and experience of dispensers working at community pharmacies in Pakistan. Pharm Pract (Granada) 2011; 9(2): 93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Government of Nepal. National Health Policy 2071, https://www.publichealthupdate.com/national-health-policy-2071-nepali-and-english-version/
- 25. Cryer B, Barnett MA, Wagner J, et al. Overuse and misperceptions of nonsteroidal anti-inflammatory drugs in the United States. Am J Med Sci 2016; 352(5): 472–480. [DOI] [PubMed] [Google Scholar]
- 26. Shrestha R, Prajapati S. Assessment of prescription pattern and prescription error in outpatient Department at Tertiary Care District Hospital, Central Nepal. J Pharm Policy Pract 2019; 12: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Study_Questionnaire for Study on drug use pattern in primary healthcare centers of Kathmandu valley by Amrita Aryal, Asmita Dahal and Rajeev Shrestha in SAGE Open Medicine


