Selected abstracts were presented as orals, MDT Diaries, The Cauldron and Gold Medal within the conference programme and the remaining accepted abstracts were presented as electronic posters.
Abstracts selected as Oral presentations
0131
Core-peripheral temperature difference assessed by thermal imaging and its association with illness severity in sepsis
Matt Charlton, Mark Sims, Tim Coats and Jonathan Thompson
Diagnostics Development Unit, University of Leicester, Leicester, United Kingdom
Abstract
Skin temperature and cutaneous temperature gradients are useful qualitative measures in the assessment of microcirculatory function and management of shock. Core-peripheral temperature difference (CPTD), has been demonstrated to be a potentially useful bedside measurement in children and adults, with gradients exceeding 5°C associated with poor peripheral perfusion and reduced cardiac output.1 Surface temperature of the inner canthus of the eye by infrared thermal imaging has been demonstrated to correlate with core body temperature with mixed results.2,3 Thermal nasal tip-to-canthal temperature difference has been shown to correlate with mortality in patients presenting to the emergency department, although the number of events in this study was low.4
Objective: To explore the association between CPTD assessed using thermal imaging and illness severity in patients with sepsis
Methods: Prospective observational cohort study (REC reference 16/NE/0168). Healthy adult staff members and patients were recruited in the Emergency Department and Intensive Care Unit at the Leicester Royal Infirmary. Participants were divided into three groups based on physiological measures and available laboratory investigations: healthy volunteers, sepsis and severe sepsis, as per the 2001 international sepsis definitions.5
All participants were provided a minimum of 30 minutes acclimatisation period to equilibrate to environmental temperature before image acquisition. A facial thermal image was then taken from a standard distance of 1 metre, using a FLIR T650sc long-wave infrared thermal imaging camera (FLIR Systems Inc.) focusing on the midface. Thermal tuning and image analysis were performed using FLIR Tools+ software with a minimum 9-pixel sample size in all regions of interest (inner canthus and nasal tip). CPTD was calculated by subtracting nasal tip temperature from the inner canthal temperature. Data were inputted to IBM SPSS Statistics (v24.0, IBM 2016) for analysis. Non-parametric data were analysed using the Kruskal-Wallis ANOVA and Mann-Whitney U tests for independent samples.
Results: 112 participants recruited between September 2016 and April 2018 (Table 1). Two were excluded from analysis because of inadequate image quality.
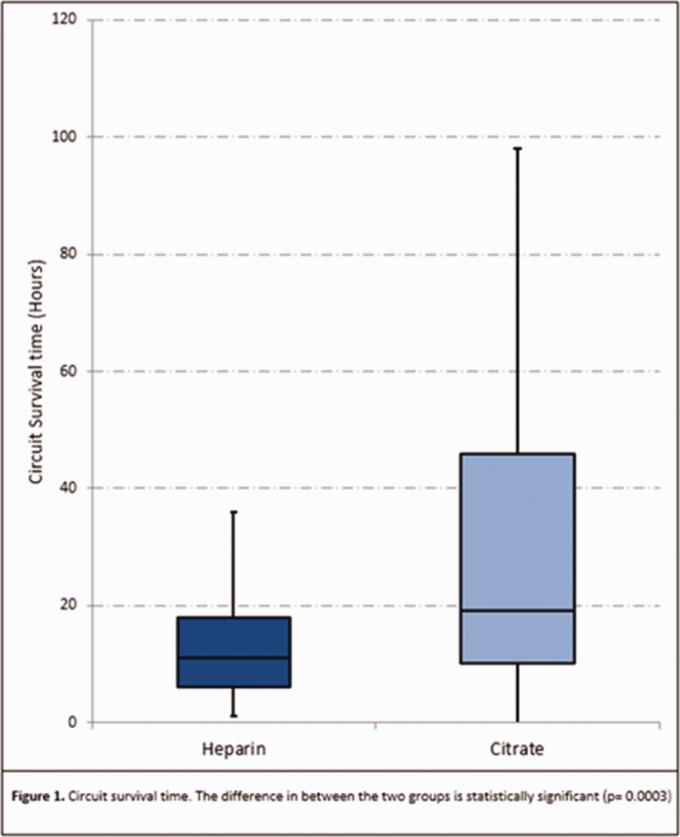
The median CPTD for healthy volunteers, sepsis and severe sepsis groups were 2.45°C, 2.5°C and 3°C respectively, with no statistically significant difference between the groups (p = 0.886) (Figure 1).
In those patients who died within 90-days of enrolment, the median CPTD was 3.5°C [1.65–8.2], compared with 2.4°C [1.3–6.6] in those patients who survived beyond 90-days (p = 0.253).
Conclusion: We found no obvious association between CPTD using infrared thermal imaging and illness severity in a heterogeneous group of patients with sepsis. Potential reasons include the accuracy with which inner canthal temperature predicts core body temperature, and the impact of non-standardised environments on the acquisition of thermal images.
This work was funded in part by a research grant from the NIAA/AAGBI.
Table 1.
Participant characteristics, presented as n (%) or median [IQR].
| Healthy (n = 40) | Sepsis (n = 34) | Severe Sepsis (n = 36) | |
|---|---|---|---|
| Male | 14 (35%) | 16 (47.1%) | 22 (61%) |
| Age (years) | 42 [31–50] | 69 [67–79] | 69 [62–78] |
| SOFA score | 4 [2–5] | 11 [7–13] | |
| 90-day mortality | 5 (14.7%) | 12 (33.3%) | |
| CPTD (°C) | 2.45 [1.55–6.4] | 2.5 [1.1–6.78] | 3.0 [1.45–6.65] |
0142
A qualitative exploration of staff perceptions of safety and missed care in adult intensive care (ICU)
Clare Leon-Villapalos, Mary Wells and Stephen Brett
Imperial College Healthcare NHS Trust, London, United Kingdom
Abstract
The ability to provide safe, patient-centred care depends on appropriately skilled and available personnel operating in staffing models that optimise their performance. Current staffing guidance in ICU.1 is largely based on staff:patient ratios, may not fully reflect the multi-professional nature of ICU care delivery and may be insensitive to the changing ICU population. Staff perceptions of safety and missed care are important organisationally2,3 and may contribute to stress and “burnout” in ICU staff. There has been limited exploration of these topics from a multi-professional perspective and in the context of critical care.
Objective: To explore multi-professional perceptions of safety and missed care in ICU.
We conducted qualitative, semi-structured interviews with ICU staff. Purposive sampling was used to recruit clinicians from different professions and levels of seniority, across three sites of a large NHS Trust. Interviews were digitally recorded and transcribed verbatim. Data were coded and analysed thematically, using NVivo vs 12.0 to manage data. United Kingdom Health Research Authority was obtained (Study ID 249248).
23 participants were recruited (14 nurses, 2 physiotherapists and 7 doctors).
Preliminary analysis suggests that perceptions of safety are shaped by staff experiences and views of the team they work with. Teamwork appears to mitigate against both the volume and acuity of patients; “100%. If we have a good team, we can probably take on anything”.
Important features of the team include; knowing one another, understanding the perspectives of different professions, organisational and clinical knowledge, and experience. The number of staff available in the team, particularly having a “float” nurse, was important to perceived safety, but was ascribed less importance than the composition of the team. Numbers of physiotherapy and nursing staff were, however, perceived to impact on the delivery of high-quality holistic care. Sufficient surveillance and support were also important for both junior and senior staff. This could be influenced by unit geography e.g. number of side-rooms. Senior staff felt care was unsafe when they could neither delegate nor provide sufficient support to their team.
Preliminary analysis suggests that staff perceptions of missed care are influenced by feelings of perfectionism and guilt, which in turn may impact on general perceptions of safety.
Staff primarily described missed care in terms of failing to provide comprehensive personal care, emotional support and rehabilitation. Despite believing these aspects of care to be important and feeling guilty when they were unable to provide them, staff frequently described them as “silly” or “basic”. Staff who described themselves as perfectionists tended to perceive a ‘safe’ day as one where “everything is done”.
Across all professions organisational measures and processes were not perceived to capture patient needs.
This study has revealed important influences on staff perceptions of safety and missed care in ICU. Findings suggest that there are factors, such as the nature and composition of the team, which are not wholly considered in current staff deployment models. Further research is needed to inform sensitive metrics which adequately reflect the reality of the ICU environment.
Funded by Imperial Healthcare Charity NIHR BRC
0331
Impact of Advanced Critical Care Practitioner led analgesia service in Critical Care Unit patients after multiple rib fractures
Nigel Manning1, Laura Beard2, Catherine Snelson3, Rajneesh Sachdeva4, Tony Whitehouse5, Mike Knowles6, Fang Gao Smith7 and Tonny Veenith5
1Advanced Critical Care Practitioner, Queen Elizabeth Hospital NHS foundation trust, Birmingham, Birmingham, United Kingdom
2Specialist Registrar in Anaesthetics, Queen Elizabeth Hospital NHS foundation trust, Birmingham, Birmingham, United Kingdom
3Consultant in Critical Care and Acute Medicine Clinical Service Lead Critical Care, Queen Elizabeth Hospital NHS foundation trust, Birmingham, Birmingham, United Kingdom
4Consultant in Anaesthesia, Queen Elizabeth Hospital NHS foundation trust, Birmingham, Birmingham, United Kingdom
5Birmingham acute care research group, Queen Elizabeth Hospital NHS foundation trust, Birmingham, Birmingham, United Kingdom
6Consultant in Critical Care, Anaesthetics and Acute Pain, Queen Elizabeth Hospital NHS foundation trust, Birmingham, Birmingham, United Kingdom
7Professor of Anaesthesia, University of Birmingham, Birmingham, United Kingdom
Abstract
Objective: This prospective longitudinal cohort study aimed to evaluate the effectiveness of Advanced Critical Care Practitioner (ACCP) led analgesia service, utilising a structured pain management pathway including Serratus Anterior Plane block, in patients admitted to a Critical Care Unit (CCU) following multiple rib fractures.
Background: Multiple rib fractures (MRF) are associated with significant morbidity and mortality.1 The morbidity following MRF is attributed to impaired cough, mobility, atelectasis, and pneumonia.2 Protocolised management to reduce inter-clinician variability for analgesia after MRF may reduce morbidity in CCU.3 Insertion of Serratus Anterior Plane blocks (SAPB) is easy and safe to perform. It can be inserted in patients with restricted mobility and haemodynamic instability where Epidural analgesia is contraindicated.4 In 2018, we introduced a protocolised analgesia pathway for patients with MRF, involving both conservative approaches with opioids and regional techniques including SAPB and Epidural. This is an ACCP led 24/7 service with cooperation of anaesthetic and Critical Care teams. This study intends to compare clinical outcomes from ACCP led analgesia service with the previous management without ACCPs.
Method: A prospective longitudinal cohort study from January 2017- January 2019 for all Critical Care patients, admitted to a single Major Trauma centre in the U.K., over 16 years old and with more than one rib fracture. We excluded pregnant and patients with penetrating injuries.
Data from 12 months of 2018 were compared to patients admitted in 12 months in 2017. The primary outcomes assessed were the length of the Critical Care (LOCCS) and overall hospital length of stay (LOS).
Results: Ninety-eight patients met the inclusion criteria in 2018 and were managed with the analgesic pathway with 79 patients in 2017. Their demographics did not differ (age, sex and Injury Severity Score- ISS) and mortality at 30 days was not significantly different. SAPB were utalised in over half of the group in 2018 (55 patients, 1 in 2017). A reduction in mean Critical Care length of mean stay, 11.1 days (S.D. ± 12.3) in 2017 compared to a mean 8.2 days (S.D. ± 9.1) in 2018. A mean LOS 27.8 days (S.D. ± 19.9) in 2017 compared to a mean of 23.2 days (S.D. ± 19.9) in 2018 was found, although not statistically significant (LOCCS p = 0.09, LOS p = 0.13).
Discussion: The study demonstrates the versatility, effectiveness and safety of ACCPs to provide such a service and their role in a diverse workforce. This pilot study suggests that there may be a reduction in the Critical Care and hospital length of stay in patients with MRF managed using a pain management pathway. A further multi-centre RCT is required to confirm these findings.
0361
SCARF: Supporting Community Recovery and Reducing Readmission Risk Following Critical Illness: From Research to Practice
Eddie Donaghy, James Marple, Jo Thompson and Tim Walsh
Anaesthesia, Critical Care and Pain Medicine, University of Edinburgh, Edinburgh, United Kingdom
Abstract
Introduction: Survivors of critical illness can experience multidimensional disabilities including physical, psychological and cognitive decline, social challenges and reduced quality of life. Approximately 25% experience an early unplanned acute hospital readmission within 90 days after discharge home.1 ICU survivors utilise around 50% more hospital costs than otherwise similar patients during the year after discharge.2 Recent research involving ICU survivors readmitted within 90 days of discharge highlighted multi-morbidity, polypharmacy, fragile social support, mobility and psychological problems prior to ICU admission increased readmission risk.3 Post-ICU re-admission prevention programs have not been widely studied or adopted despite these high rates of readmission.
Objective: To introduce a new integrated care pathway at the Royal Infirmary of Edinburgh for ICU survivors discharged to acute wards and identified as most ‘at risk’ of an early unplanned acute hospital readmission. Consequently, we secured funding for a 12 month Quality Improvement project.
Methods: Following our previous research findings, we (i) developed an ICU holistic needs screening tool to facilitate early identification of ICU survivors most ‘at risk’ readmission; (ii) introduced in-hospital holistic needs assessment to identify clinical and psychosocial needs of ‘at risk’ ICU survivors; (iii) provided patients and carers with information on potential after-effects of critical illness prior to discharge home; (iv) developed improved and quicker communication links between ICU discharge nurses and the ‘at risk’ ICU survivor’s GP, community pharmacist and community NHS multi-disciplinary support teams; (v) conducted telephone follow up of ‘at risk’ ICU survivors at 2 and 8 weeks after discharge home; (vi) conducted a quantitative evaluation of readmissions and a qualitative evaluation of patient/carer and health/social care professional experiences of the new ICU care pathway.
Results: Our newly introduced care pathway showed that a nurse-led simple screening tool (assessing multi-morbidity, polypharmacy, mobility, social support, and psychological issues) could be used to triage patients in ICU (‘SCARF positive’ versus ‘SCARF negative’). We found (i) SCARF positive patients comprised 23% of ICU survivors admitted over 12 months (ii) SCARF positive patients had prolonged hospitalisations and a 50% unplanned hospital readmission rate within 90 days (compared with 20% for SCARF negative patients). These particular patients had a high prevalence of social deprivation, substance misuse and mental illness. Evaluation with patients and carers, GPs, community pharmacists, and community health-social care staff was very positive. Process control methodology suggests a downward trend in all readmissions following ICU discharge over the intervention period (around 4% absolute; 15% relative reduction).
Conclusion: A targeted nurse led brief intervention to improve ICU survivors’ education prior to discharge home improves their awareness of the potential after-effects of critical illness. ICU survivors and carers valued the follow up phone calls. Community partners (GPs, community pharmacists and community health and social care teams) noted the benefits of early alerts of a patient’s admission to ICU and discharge from hospital. Reductions in 90 day early unplanned admissions were encouraging.
0363
Risk factors for ESRD following critical care
Paloma Ferrando-Vivas1, Lui G Forni2,3, Steve Harris4,5, Marlies Ostermann6, Manu Shankar-Hari6,7, Fergus J Caskey8,9, Kathryn M. Rowan1 and David Harrison1
1Intensive Care National Audit & Research Centre (ICNARC), London, United Kingdom
2Royal Surrey County Hospital NHS Foundation Trust, Guildford, United Kingdom
3University of Surrey, Guildford, United Kingdom
4University College London Hospitals NHS Foundation Trust, London, United Kingdom
5University College London, London, United Kingdom
6Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
7King's College London, London, United Kingdom
8North Bristol NHS Trust, Bristol, United Kingdom
9University of Bristol, Bristol, United Kingdom
Abstract
Introduction: The occurrence of acute kidney injury (AKI) is common among critically ill patients, associated with high mortality,1 and has been linked with subsequent end-stage renal disease (ESRD).2
Objectives: To use data linkage between routine data sources to estimate the rates of ESRD following critical care and identify predictors of ESRD.
Methods: Data from the ICNARC Case Mix Programme (CMP) were linked with the UK Renal Registry (UKRR), Hospital Episode Statistics (HES) and death registrations. Patients discharged alive from hospital between 1 April 2009 and 31 March 2016 were included in the analysis. Multiple admissions of the same patient and patients with pre-existing ESRD were excluded. The primary outcome was new receipt of renal replacement therapy (RRT) for ESRD, based on the date of diagnosis recorded in the UKRR database. Candidate predictors were chosen based on expert clinical opinion and availability in the linked datasets. The competing risk of death was accounted for using cause-specific Cox models and Fine-Gray regression models.
Results: After exclusions, a total of 598,603 patients admitted to 248 adult general critical care units in England participating in the CMP and discharged alive from hospital between 1 April 2009 and 31 March 2016 were included in the analysis. The median follow-up was 2.7 years (IQR 1.4 to 4.6 years) and 2,831 (0.48%) patients subsequently developed ESRD (incidence rate 1.52 per 1000 person-years; 95% CI 1.46 to 1.58). Key findings from the cause-specific Cox model included the following. Risk of RRT for ESRD decreased non-linearly with increasing age. Female gender (adjusted hazard ratio (HR) 1.30) and non-white ethnicities (HR 1.67-2.15) were associated with increased risk of ESRD. Those with chronic kidney disease (HR 4.11) or AKI (HR 1.72) during the previous 5 years or peripheral vascular disease (HR 1.29) or diabetes (HR 1.35) during the previous year were more likely to develop ESRD. In addition, receiving mechanical ventilation (HR 1.29), vascular surgery (HR 1.24) and nephrectomy (HR 1.92) were associated with increased risk of ESRD. By contrast, patients with severe liver disease (HR 0.81) and metastatic disease (HR 0.66) were less likely to receive RRT for ESRD. Increasing urine output was linearly associated with a decrease in the risk of developing ESRD (HR 0.89 per 500 ml/24h). Non-linear associations were observed between the risk of ESRD and creatinine, urea, sodium and blood lactate (modelled by restricted cubic splines; Figure). Each additional day of RRT in critical care was associated with a HR of 1.11. Harrell’s c-statistic for the model was 0.94, with an R2 of 0.985. Results for the Fine-Gray model were similar.
Conclusions: Rates of ESRD among survivors of critical illness are low, however a number of factors were identified that predispose to higher rates of ESRD, particularly relating to previous kidney disease, measures of kidney function and duration of RRT. Some apparent protective factors (e.g. increasing age, severe liver disease, metastatic disease) are likely to reflect patients with ESRD not referred for RRT.
Funding: NIHR HS&DR Programme (14/19/06)
Figure 1.
Cause-specific hazard ratios for non-linear physiological predictors.
Abstracts selected as MDT Diaires presentations
0060
“Thanks for taking time to sit with me and reflect on the death of my son"
Hywel Garrard
Salford Royal NHS Foundation Trust, Manchester, United Kingdom
Abstract
“Thanks for taking time to sit with me and reflect on the death of my son. The world needs more doctors like you.”
24th June 2019. That should have been the day that changed my practice. That was the day that the learning from excellence report arrived in my inbox. That wasn’t the day; neither was it several weeks earlier when I met the patient. The story ran deeper than that.
Recovering from his emergency surgery, whilst amid chemotherapy for a hematological malignancy; the patient had plenty to deal with.
None of this phased him; what was hurting more than the bone aches of chemo, or the belly ache of bowel surgery was the grief of losing his son.
Neither of us started out to talk about his son, but the door was ajar, and I gave him space to open it.
The way he found his lifeless body hanging. The way he had to cut him down. The way he had so much to live for. The way he wished he could have had a moment to talk him down. To talk him around. To show him the future he could have.
All I know is that the patient needed to talk. He needed someone to listen.
What I know is that we would never have talked like we did but for the day many months earlier that changed my practice.
That day wasn’t the funeral in the bleakness of early January. The cold morning with so many young mourners in black. The tears of friends, long out of touch, never imagining a reunion like this.
The day was the 11th of December. The day that changed my practice. The day my friend and former house mate took his own life.
Losing my friend made me face my own mental health, and like my physical health, I realised that keeping well is an active process. Kindness to yourself. Self-care, talking, listening and sharing emotions. Working on these habits have made me and kept me well.
This self-care and kindness are needed in critical care. If we’re well and have the emotional capacity, we can talk to our patients in a meaningful way. We can listen to their hopes and fears. Rather than ‘fixing’ only the physical problems we can offer a little humanity to help heal their emotional suffering.
The conversation with my patient can’t bring his son back, but I know having someone listen was a better medicine that any of the drugs we had on the ICU. He didn’t care for my qualifications, logbook or exams. He just wanted a human being to talk to. Someone to share with. That’s something we all need.
0174
MDT Diaries: Critical pain in intensive care
Yasser Al-Raweshidy
King's College Hospital NHS Foundation Trust, London, United Kingdom
Abstract
My first rotation as a fully registered General Medical Council doctor was in the Intensive Care Unit (ICU) at the Royal Marsden hospital. It was my first exposure to Critical Care.
I clerked in a young man in his 20s who was admitted directly from theatres to ICU. He had undergone an orchidectomy and exploratory laparotomy for a chemotherapy-resistant testicular tumour.
The patient arrived in pain. After administering a morphine bolus, I commenced him on a morphine Patient Controlled Analgesia, progressed to examine him and then went on to complete the electronic admission clerking.
The Intensive Care consultant in charge attended the unit and observed the patient to be in severe pain. Having identified that I was the doctor looking after him I was summoned to the patient’s bedside. There, I too observed the young man to be in distress from pain. The consultant proceeded by administering several morphine/ketamine boluses.
He made a passionate plea to request I stay at the bedside for as long as necessary to ensure the young man was comfortable, even if I had to spend all afternoon there. After 30 minutes the patient’s pain improved.
I just remember that, I at the time, felt so lucky that there was someone willing to educate me in human kindness and compassion in a non-judgement way. Never at any point was I made to feel guilty for ignoring this young man and instead deciding to focus on the admission clerking (something I was keen to complete promptly due to the expectation of further admissions).
The ICU can have a harsh industrial landscape to it. It is usually filled with incessantly bleeping equipment and all matter of bland grey or off-white looking devices delivering much needed life saving therapies. Contrast this with the softer environments of the hospital where walls can be adorned with art and light beams into walls though windows/doors. I think it can sometimes be all too easy to feel we too are part of this industrial machinery environment and as such our feelings towards our patients can become dehumanised. This is often compounded by the need to detach ourselves from the brutal realities of the ICU -the pain, suffering and extreme emotions that our patients and their families go through.
As an Intensive Care registrar coming towards the end of my training I look fondly back at this learning experience when my consultant made the effort to spend time with both me and my patient. To this day, I can recall several other small examples of compassionate care that this consultant demonstrated. I think that sometimes it can be the small traits and actions that we observe in others that motivate and drive us to aspire to be better clinicians. Indeed, although he doesn’t know it, that consultant was a major catalyst in driving me to pursue training in ICM. I look forward in the hope that, I too one day, will be able to inspire someone to embark on a career in Intensive Care.
0230
8 year old VVECMO patient – let's get up
Chloe Meehan
Royal Brompton Hospital, London, United Kingdom
Abstract
Who was it? An eight-year-old girl
What did they say? Unable to speak
Did you look at someone differently? All 7 other professionals in the room
On Sunday the 7th July an eight-year-old girl was admitted to our PICU, a young girl who was in school that week. She attended a local walk in centre presenting with very low saturations and a non-productive cough; she was blue lighted to her local hospital and started on oxygen therapy. Modes of oxygen delivery were escalated and when the young girl became too fatigued with worsening blood gases the decision was made to intubate and transfer to our PICU.
On arrival to our unit it quickly became apparent that conventional ventilation would not be sufficient. The decision to place the young girl on VVECMO was reached. This young girl was seen by my team from day 1; I was her lead physiotherapist.
I am lucky to have just rotated off the AICU unit where we routinely rehabbed our VVECMO patients; I had done my competencies. I was keen to keep this girl strong. I wanted her to get back to her swimming lessons with her two younger siblings as soon as possible. We saw this young girl daily for chest checks, stretches and repositioning, all the while telling her about the world outside, the heatwave, the thunderstorms, the number 1 in the charts, singing and playing silly music. No response. On the 22nd July, two weeks of being on VVECMO this young girl started to join in with our stretches and consistently react to our voices.
On the hottest day of the year, in full PPE and face masks we sat this young girl up. It was the first active rehabilitation VVECMO session undertaken in our PICU and I was leading it. In the room were two perfusionists, the consultant on this case, two ECMO nurses and three physiotherapists, it was an organised jumble of lines, tubes, cannulas and people.
1 young girl, 1 watching parent, 2 ECMO femoral cannulae, 8 medical professionals, 8 running infusions, 1 ETT – everyone was ready. Simple teamwork and simple instructions safely got this young girl sitting on the edge of the bed. We stayed there for ∼20 minutes. Tidal volumes and SpO2 improved. Passive stretches and proprioception work was carried out, explaining in eight-year-old language what we were doing.
Dad saw his little girl sit up.
The following day she was sat up on the edge of the bed again and 3 days later the ECMO was decannulated. A few days later she was sitting up waving to her parents, playing CandyCrush and sitting out in a wheelchair under a fluffy blue blanket. Soon she was standing, ETT still in place. She was acting somewhat like an eight-year-old girl again. Her story continues.
Early active rehabilitation isn’t possible without teamwork. I learned what it felt like to lead that team. The first active VVECMO rehab session went well, paving the way for many more to come.
0310
A simple “how are you?”
David Harvie
Queen Alexandra Hospital, Portsmouth, United Kingdom
Abstract
My recent experience of working as an ICU Registrar in a large tertiary Australian Hospital taught me something akin to the “hello my name is … campaign”. This campaign highlights “Introductions are about making a human connection. They begin therapeutic relationships and can instantly build trust in difficult circumstances.” (1) I learnt that human connections are vital in our everyday interactions.
On my first day at work in ICU in Australia holding the referral phone I was thrown off guard by the initial interaction from my Medical Registrar colleague; “Hello, how are you? how is your day going?” I was a bit shocked and confused. My initial response (in my head I may add, I am British after all!), was Why are you asking me this? You don’t care, just get on with your referral I’ve got work to do!
During my 2 years working there I began to enjoy this interaction. A brief, pleasant chat with your colleague from another department about how you are, rather than what I had been accustomed to, the aggressive bartering over who is going look after a patient! This small chat developed relationships with my colleagues from other departments. When it then came to discussing the referral, both parties were, in my opinion, able to communicate better. We know that good inter-professional communication influences quality of care and patient safety (2) and failure of interdisciplinary communication is linked to avoidable medical mishaps. (3)
This small change in my communication with other specialties became more apparent on my return to working in the UK. I noticed in my first week of work, that I was now automatically asking my colleagues, “How are you? how is it in ED today?” for example.
The response I was receiving initially was mainly of confusion and trepidation, but has started to be welcomed.
I think interaction for health professionals with ICU can sometimes be an unpleasant one. They are asked to refer to ICU and can be met with an ICU Registrar who is very busy, a bit stressed dealing with the some of the sickest patients in the hospital, whose response may be interpreted as somewhat aggressive in their questioning of why a patient is being referred. I subjectively have noticed that the change in my initial interaction, can then make the Doctor less defensive when making the referral and therefore communicate better for the interest of the patient.
Looking back, that first referral in a new hospital, and a simple question, “how are you? How is your day going?” has changed my practice for the better. I think it’s a simple step in helping breaking down the walls of ICU not building them up, allowing for potentially better care for the patients.
0335
ICU or Torture Chamber? How I learned to humanise the unit
Joanna Mann
University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
Abstract
A day in February 2019, which catapulted what was ‘voluntary supportive informal coffee mornings' for past Intensive Care Unit (ICU) Patients, sharing experiences of critical illness post hospital discharge; into what is now becoming a supported programme of educational development and moving towards a formal ‘Follow Up Service'.
So I met ‘Joan' and ‘Bill', returning to share her story of sepsis, starting from a ‘simple chest infection' that turned into a critical illness and long journey home, with her husband who witnessed everything unfold. This ‘coffee morning' allowed the ‘trauma' of being critically ill to be shared. Joan often referred to her life post retirement as ‘living the dream'. Now her only take on life is ‘living a nightmare … forever being crazy'. She is ‘so angry' with her body for becoming so ill. Her husband revealed he felt so ‘helpless and out of control' as he watched his wife going into a full body shutdown and then witnessing every moment, every decision … a ‘living hell', not knowing whether it meant he would be taking his wife home again or planning her funeral. Every bit of emotion showing whilst re-living their story, tears streaming down his face.
Joan ‘knew' she was dying. She remains psychologically disturbed having memories and nightmares; ‘spikes' being put into her, when lines were inserted and ‘things between her legs' – feeling violated. “If you were taken off the street and those things done to you, it would be called assault”, a perfect descriptor of how she feels.
After all this she hated hearing phrases on her road to home like ‘you'll be near normal' or ‘this is the best you'll get', the irony being she can't even look at herself in the mirror. Bill broke down into tears again, desperate to explain his feelings deeper. I could feel his pain but his wife would not let him because ‘nothing could change it or would help', because ‘what's done is done'. The isolation for them both, not being able to talk to anyone about their horrific ordeal, both lived in different ways and yet by chance, able to come and discuss this alone with health professionals who can appreciate their journey. An experience so powerful that it could make a difference in the future. How one couple's journey could transform care and change the future of post ICU rehabilitation.
So since this day, interventions on the unit have come into action: patient diaries, liaising with Outreach Team and providing support leaflets. A formal education package for all staff disciplines with continuing professional development hours for their portfolio by attending coffee mornings. Their story, used to develop research into staff reflection and the Chief Nurse developing a business case for a new service for the future. This one meeting could transform the care delivered in practice on admission to ICU, throughout hospital, on a coordinated rehabilitation pathway to home and beyond. A meeting on the surface so simple in action but so profound in its meaning for the future.
0407
Humanising Critical Care
Lucy Mires
Medway NHS Trust, Gillingham, United Kingdom
Abstract
Did you ever experience that ‘difficult patient’? Or maybe it was their family. You know the ones I’m talking about; the ones who are too anxious, too hostile or won’t engage. Every shift feels like another round in a boxing ring, leaving all those involved feeling both physically and emotionally exhausted. They ultimately become the patient/family no one wants to care for. I’m guessing that most of us within our clinical lifetimes will have experienced this situation to a greater or lesser extent. I wanted to share my experience of one such scenario with you, as ultimately it did change my practice and maybe it may even change yours.
The experience that I recount now involved a young patient and his mother. The patient himself I recall as being very unproblematic in nature; a young man with a terminal progressive degenerative neurological illness. Diagnosed in childhood, he was totally dependent for all his care needs. His mother was his longstanding carer and was undoubtedly an expert on all matters concerning her son. He was admitted to the ICU with a severe chest infection.
The relationship between the patient’s mother and the staff was always a tense one. There were issues regarding levels of involvement, trust and expectations from the offset. The relationship between the patient’s mother and the staff grew increasingly fraught as the patient grew increasingly sicker. I can remember finding all interactions with her extremely challenging, often confrontational with no resolution. Unfortunately the young man in question died. And it is what happened next, that really impacted upon my practice.
About a week after this young man’s death I received a phone call from his mother inviting the ICU staff to her son’s funeral. This invite came as a surprise regarding the nature of the relationship between her and the staff, and though normally I wouldn’t have considered attending a patient’s funeral, there was something about this situation that left me feeling that I should represent our team. I wanted to show that despite our differences we did genuinely care about her and her late son.
So, with some trepidation I attended the funeral, not knowing what to expect, anxious that I would somehow be faced with anger and blame. However, what confronted me was an insight into the life of a man I did not know, that metaphorically I had not met. A steady stream of videos and images played throughout that funeral of a young boy growing into a man. One who radiated with life and vitality. There throughout those images was his mother, smiling and encouraging. They both looked a world apart from the people I had encountered in the ICU.
My practice changed from that day. With every patient/family I encounter I remember that funeral, that family. I’m reminded that these people lived rich and complex lives; that they weren’t always sick. They are more than a sum of their illness. It helped me to prioritise the ‘care’ in Intensive Care, humanising the patient.
Abstracts selected as Cauldron presentations
0042
Champagne, Anyone?
Rachel Jones
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Three of the biggest threats in the ICU today (as identified by the NHS five year forward view1) are staff retention, long stay patient mental health and unsustainable staffing costs. All of these can be solved by purchasing arable land and establishing a winery and vineyard. We would make English Sparkling Wine from champagne grapes which would act both as a horticultural outlet for ICU patients and staff and a profitable option to help funding.
Horticultural therapy is a recognised discipline and can help both our patients and ourselves. Connecting with nature outside the four industrial walls of the ICU is proven to help with depression and anxiety.2
The ability to take patients to a purpose built outside space where they can feel the wind, the warmth of sunshine or hear the birdsong will revolutionise their recovery. Gardens are an established aspect of hospital development;3 this takes it one step further, transforming the garden into a business.
The staff could also benefit by using the space to engage with nature and de-stress. The vineyard and winery would offer sabbaticals to staff, with the opportunity to incorporate time within a phased return to work. The winery will have a space for meetings such as journal clubs or CPD which then can progress on as a space to build professional relationships outside of work
The final and most sustainable fact is that wine is a marketable product with a significant profit margin. English wine retails for £25/bottle and producers can be expected to get £15/bottle. With a small plot of four hectares we could produce 17440 bottles.4 With the addition of a professional vineyard manager and winemaker we would still make a profit of £189,000 from year five onwards. The first three years will be not be cropped due to fruit quality and will take 15 months of maturation before release meaning first production starts in year five. This would fund locum and agency staff to thus ensure staffing always meets the demand. This, in turn, would encourage staff retention and help avoid the increasing issues of staff burnout.
To conclude the 1 million US Dollar (£789,400 as of 4th July 2019) can solve the major threats to ICM. This is a fully costed opportunity that is also creates a legacy and sustained investment.
Table 1.
Break down of costs and projected profit.
| Viticultural Set Up | |
| 4 hectare of arable land | 50 k |
| 20000 vines (planting density 5000/ha) | 60 k |
| Training | 25 k |
| Planting | 10 k |
| Vineyard Manager (5y × 25k) | 125 k |
| TOTAL | 270 k |
| Vinification Set Up | |
| Building | 300 k |
| Equipment | 50k |
| Winemaker from Year 4 (32.5k × 2) | 65 k |
| Total | 685 k |
| Year 5 potential income | |
| 17440 bottles (4360/ha based on 2018 data) at £15/bottle | 262 k |
| Ongoing Costs | |
| Harvest labour | 15 k |
| Winemaker | 32.5 k |
| Vineyard Managed | 25 k |
| Profit | 189.5 k |
0150
Plan A is Bonefish Cay …
Charlie Pope
University Hospitals Bristol, Bristol, United Kingdom
Abstract
Burnout is becoming increasingly recognised by the intensive care community and is already alarmingly prevalent in our workforce. High mortality rates are blamed, but it unlikely this is the sole reason – one survey found burnout rates in ICU to be almost double those of palliative care (31% vs 16%).1 PTSD and depression affects a quarter of our workforce.1 Thirty-three percent of new nurses seek another job within a year.2 A different study found one in two ICU physicians will experience features of burnout, prompting us to ask the question “is it me, or you?”3 Trainees aren’t protected from burnout, with the results from the GMC training survey last year continuing this stark trend.4
The cost to the economy was estimated at £11.3 m (2013-14).1 The wider impact on safety, patient care and outcomes from strained professional relationships, negative working culture and incivility is difficult to quantify but likely to be significant.
When I heard about the generous donation of $1,000,000 it initially came as quite a surprise, but I soon saw it as an opportunity to improve team wellbeing.
Plan A is Bonefish Cay – an uninhabited Bahamian island without running water but nonetheless an absolute bargain (approx. $700,000). Local infrastructure needs work so $285,700 for a 1979 Cessna seaplane is necessary. Future investment will become available (£350 million per week from Boris…) for the clubhouse, marina and discotheque, so the last few dollars can go on swimwear.
Multidisciplinary team retreats to Bonefish Cay will provide huge opportunities for rest, relaxation, reflection and most importantly burnout prophylaxis.
After initial enquiries I received strongly worded correspondence from the NHS Counter Fraud Authority. Subsequently Plan B started to take shape…
I would employ a clinical psychologist ($55,000pa) who would share their time between patients, families and staff. Mental health issues would receive timely treatment, follow-up clinics would be offered, families could be supported and staff members could self-refer at any stage (counselling, debriefing difficult cases & Trauma Risk Management (TRiM) programmes5).
Wellbeing Champions would be tasked with encouraging good self-care through healthy lifestyles, mentoring, mindfulness, Schwartz rounds and sociable team days as a focus for developing resilient relationships with colleagues.
I would create a quiet space within the critical care unit, where staff and families could rest, away from alarms and clinical conversations – a garden would be an ideal space to contemplate critical events that occur on a daily basis and often get brushed off.
Staff wellbeing increases civility and civility saves lives. Civil work environments matter because they reduce errors, reduce stress and foster excellence.
One million dollars will create joy in work – more than just the absence of burnout – fostering a team of happy, healthy and productive people, impacting individual staff engagement and satisfaction, but also patient experience, quality of care, patient safety, and organizational performance.2 Who is going to look after our patients if we don’t look after ourselves? We need to start thinking about Staff Wellbeing as an important resource not a dispensable luxury.
0356
Is your house on fire yet?
Eleanor Damm
University Hospital of North Midlands, Stoke on Trent, United Kingdom
Abstract
We all know money is power – it is as ancient as human history. We will use our new found power to strongly encourage the hospital board to declare a climate emergency, aiming to be a carbon neutral trust as soon as possible, latest by 2030.
Climate breakdown is a global public health issue. It has a wide variety of effects –unpredictable weather patterns and extremes of temperature already take place, which are only set to worsen. Air pollution causes and exacerbates respiratory disease and cripples children’s lungs development.1 This is in addition to future predictions of mass migration to escape unliveable conditions.
As was highlighted again at the UN conference in March 2019, we must act now to avoid catastrophic and irreversible climate change.2
Critical care excels at attention to detail and as such is well placed to set an example and lead the hospital into a more sustainable and ecologically sound future.
We would appoint a Sustainability Consultant in ITU.
The first project to focus on will be waste segregation and disposal. The NHS currently only recycles 23% of its waste. Approximately 40% of anaesthetic waste could be reclassified as domestic waste/recycled with significant environmental and financial benefits.3,4
All waste should be seen as having potential material value. By reducing waste, we reduce carbon production, water consumption and air pollution impact from logistics.
By working closely with procurement and waste management, current practice will be examined, changed and audited for more sustainable options.
This includes drastic reduction of single use items, ranging from coffee cups in staff room to clinical equipment. It includes reducing use of plastic, and using recycled materials whenever possible. In addition, recycling options for materials used in healthcare will be investigated and set up, e.g. PVC and glass.
We would lobby drug and equipment companies to provide sustainable packaging such as recycled cardboard vial trays and we would lobby NHS England to prioritise sustainability across the NHS.
Recycling for common materials such as cans and cardboard will be made available in all staff and public areas.
Staff will be educated in appropriate waste disposal and appropriate bins will be made available.
Unadopted green spaces would be converted into wildlife friendly spaces and allotments for patients, staff and visitors to enjoy. Green spaces promote mental and physical health.5 Patients and staff would be encouraged to be involved in their upkeep as part of ITU rehabilitation. If successful the local organic produce could be used for patient meals. Set up wormery for food waste to reduce methane production.
On site green energy options such as rooftop solar panels or wind turbines would be reviewed to reduce our dependence on fossil fuel derived energy and after the initial outlay will reduce our ongoing energy outgoings.
Overall ITU will work towards a circular economy.
A million dollars won’t change the behaviour of a population but it can change a hospital. We have a moral duty to lead par example and set new standards. Let’s do it now.
0412
Anticipating intensive care admission – “Pre-ICU”
Eleanor C Richards
Royal London Hospital, London, United Kingdom
Abstract
Other specialties pave the way in anticipatory medicine. Emergency Medicine benefits from “admissions avoidance teams” whilst in anaesthesia, through “prehabilitation”, a patient can be pre-operatively optimised to improve surgical and postoperative outcomes. No clearly defined service exists for intensive care.
How often have you heard a clinician suggest “treat the cause, not the symptoms?” In intensive care, our clinical team faces increasing pressure in allocating resources between rising admissions. By creating a “Pre-ICU” department, we can target those patients who are on a downward trajectory towards a future intensive care admission. This will not only make the decision to admit such patients simpler, as there will be a clear Pre-ICU care plan in place, but also improve overall care for these patients.
Through the Pre-ICU department we would introduce patients to our role in the hospital before any intensive care admission and, following a “Pre-ICU Multidisciplinary Team” meeting, implement a Pre-ICU care plan. We would seek patients with risk factors for admission to intensive care, and intervene early.
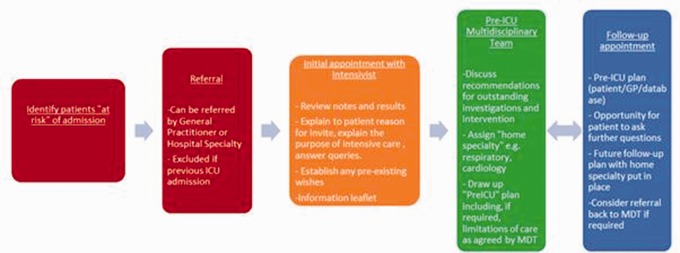
Following referral the patient would attend an appointment with an intensivist who would establish their background before presenting them to the Pre-ICU MDT, comprising intensivists as well as physicians with an interest in intensive care (ideally covering cardiology, respiratory, renal, neurology, gastroenterology and endocrine medicine). Figure 1 summarises the journey of a patient through the Pre-ICU department. The goal will be to draw up a Pre-ICU plan that not only outlines advice regarding any future admission but also puts in place strategies to avoid admission.
$1 million would fund establishment of the department, staffing costs and a database to collect information about MDT discussions. We hope to integrate each Pre-ICU plan into existing hospital systems so this information will be available at outpatient appointments and on attendance at the emergency department.
This investment would streamline ICU admissions for patients with predisposing risk factors. The goal is to reduce avoidable ICU admissions and improve care for chronic conditions. The MDT will foster better interactions between specialties, supporting patient care on the unit. Perhaps most importantly, the Pre-ICU would encourage understanding of the intensive care service in the general public and allow for patients to meet intensivists in a relaxed, elective setting.
0445
A Name Changer: The IPCU
Guy Parsons1,2
1Nuffield Department of Clinical Neurosciences, Oxford University, Oxford, United Kingdom
2Department of Critical Care, Milton Keynes University Hospital, Milton Keynes, United Kingdom
Abstract
‘Tis but thy name that is my enemy
Romeo and Juliet, Act II Scene ii
I would like a million dollars, please, for a re-brand. Not some corporate babble about seizing ‘low-hanging fruit’ for a ‘net-new’ approach based on ‘offline forward planning.’ Just a new sign for the door: The Intensive and Palliative Care Unit.
Names matter. From Montagues and Capulets to lymphatic tissue and Tourette’s we’re drawn to detail, to describe and delineate in essential terms the nub of a thing. But we’ve missed here, our current name tells only half the story. ICU hasn’t, it’s blinked, and some terminal essentials have escaped our fetish for Greek and Latin from nyx to matin.
So a new sign for the door and a new team too.
For the debilitating symptoms that start early and are often inadequately addressed whether patients are curative or non.1
For support with family care for stressed relatives when data is complex, communication valued and time hard won.2
For dignity in dying and quality in living, for decision making, explaining, pains taking, and should we carry on.
Let’s bring Palliative Care into the fold, not just for those that are dying but also for those that might grow old. A Specialist Nurse, a Palliative Care Consultant, an established and integrated team, not just ephemera. Because as much as we value our clinical skill, our scoring systems and prognostic tools, the modern ICU patient is a chimera and we’ve often been fooled.3
Critical care admissions in the last month of life are becoming more frequent.4 Traditional views on the ICU as a place to only support ‘good candidates’ with deranged physiology while awaiting resolution of underlying pathology are changing. An ageing and increasingly co-morbid population has seen ICUs admit older and sicker patients year-on-year. 23 years on from the profound disappointment of the SUPPORT project where prognostic information provision had no impact on end-of-life care quality how much further forward are we?
A new sign, a new team, and a nicer place to live. Away with bedside curtains as attractive as they are soundproof. Away with blank windowless walls. Bring in single rooms with natural light and noise control; treat the body and the soul. Make the hospital hospitable, recover humanity in the individual, we may only get one chance – who wants a horrid place to die?
So, a million dollars towards a new name, a new team, and a new unit layout please.
We’ll likely recoup some of the cost too – shorter lengths of stay, less organ support and fewer interventions have been found with palliative care integration alongside more proactive symptom control.5 Let’s challenge the perception of Critical Pare and Palliative Care as sequential rather than complementary and simultaneous. Let’s change our name to reflect our shared ideals and integrate Palliative Care on the IPCU.
For this alliance may so happy prove, To turn your households' rancour to pure love.
Romeo and Juliet, Act II Scene ii
Abstracts selected as Gold Medal presentations
0069
Establishing learning health systems in low and middle income countries
Abi Beane1,2,3, Anuja Abayadeera4, Gotabhaya Ranasinghe4, Arjen M Dondorp1,2, Rashan Haniffa1,2,3,5 and Constance Schultsze6
1Nuffield Department of Medicine, Oxford University, Oxford, United Kingdom
2Mahidol Oxford Tropical Medicine Research Unit, Bangkok, Thailand
3NICST, London, United Kingdom
4University of Colombo, Colombo, Sri Lanka
5University College London, London, United Kingdom
6Department of Global Health – AIGHD and Department of Medical Microbiology, Amsterdam UMC, University of Amsterdam, Amsterdam, The Netherlands
Abstract
Background: Poor quality of care is an important cause of excess mortality in LMICs.1 Learning health systems (LHS) embed knowledge generating processes to improve care in daily practice. However, quality improvement (QI) efforts in LMICs are hindered by an absence of granular data necessary for evaluation and limited opportunity for stakeholders to acquire the necessary skills.1 We hypothesised that a acute and critical care LHS can be established in LMIC settings.
Methods: A co-designed electronic surveillance platform to evaluate the quality of care using routinely available information was implemented across a network of LMIC acute and critical care facilities.2 Informed by data captured through the platform, domains of quality1 were evaluated; patient safety (Q1), timeliness (Q2), efficacy (Q3), equity (Q4), efficiency of care (Q5) and patient-centred outcomes (Q6). A community of practice was established to identify gaps in quality of care amenable to intervention.
Results: A clinician-led collaborative established Network for Improving Critical care Systems and Training (NICST). NICST’s platform captures routine data regarding organisation, processes and outcomes up to one-year following discharge.2 Networking 75 hospitals in South Asia and Sub-Saharan Africa, the platform has captured over 29,000 patient episodes since 2017. Examples of the quality evaluations enabled by the platform include:
1. Perioperative morbidity (POM) measures and quality of life (QoL, EQ5D-L) at 30 days following discharge for major laparotomy patients – incidence of one or more POMs at 72 hrs following surgery was 40.5%, with 40.1% of patients being commenced on new antibiotics (Q1,Q3). Median patient reported EQ5D-L was 0.84 [IQR 0.29], with 22.3% of patients reporting ongoing pain and anxiety post discharge (Q6).
2. Quality of care after acute myocardial infarction3 – the highest compliance was observed for antithrombotics during hospitalisation (79.1%) and continuous measure of patient satisfaction (76.1%) (Q6). The lowest compliance was for organisational structure and timeliness of reperfusion intervention (22.4%, Q5). Mean (SD) overall compliance as per composite quality indicator was 44% (0.07) (Q4). Predicted mortality at 3 days using the GRACE Score was 10.3% compared to observed mortality of 11.%.
3. Recognition of deteriorating patients- availability of vital signs on admission to hospital ranged from 91.0% (95% CI 90.52% to 91.40%) for heart rate to 23.9% (95% CI 23.29% to 24.60%) for oxygen saturation (Q1).4 Efficacy of Early Warning Score (EWS) to discriminate death on admission was less than 0.81 (AUROC) for all selected EWS (Q2,Q3,Q5). Positive predictive value to determine burden of triggering for frontline staff was low (10.44%) (Q4). Health care worker interviews revealed lack of formal triage, rigid team hierarchies and fear of blame as undermining the recognition of deteriorating patients (Q1,Q5).
NICST has facilitated international workshops in QI and research for over 100 LMIC delegates and provided fellowships for LMIC nationals seeking practical experience in education and QI.5 Data-driven interventions prioritised include: improving equity of access to AMI care, implementing human factors training into undergraduate medical education and implementation of an electronic vital signs platform.
Conclusion: An acute and critical care LHS can be established in LMICs.
0102
The REFLECT Study
Sarah Vollam1
1Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom
Abstract
Over 138,000 patients are discharged from Intensive Care Units (ICUs) in England, Wales and Northern Ireland each year.1 Of these, more than 8,000 then die before leaving hospital, five times the annual number of road traffic deaths in the UK.2 Most critical care research is focussed on improving survival to ICU discharge, with very few studies exploring subsequent in-hospital care. I have used a variety of research methods to examine post-ICU ward management.
I initially undertook a systematic review to identify the known factors associated with post-ICU mortality. Associated factors present at ICU discharge included abnormal bloods results, presence of tracheostomy and high nursing workload scores. The most frequently reported factor was out-of-hours discharge from ICU. I subsequently undertook a meta-analysis including data from 18 studies reporting the risk of out-of-hours discharge, comprising a total of 1,191,000 patients. This demonstrated a strong association with both post-ICU in-hospital mortality (RR 1.39 (95% CI 1.24, 1.57) p < 0.0001) and readmission to ICU (RR 1.30 (95% CI 1.19, 1.42), p < 0.001).3
The systematic review identified some risk factors for poor outcome but did not provide any insight into the underlying reasons, or mechanisms for improvement. To explore this further I undertook the NIHR-funded REFLECT study. This study used mixed methods to investigate care delivered to patients on general hospital wards in three NHS trusts, following ICU discharge (Wales REC 4 ref: 17/WA/0107).4
In REFLECT I led a retrospective case record review study of 300 patients across three NHS sites. I used an established ‘structured judgement review’ process previously used to investigate adverse events in general hospital populations. To explore this area of care from multiple perspectives I also conducted semi-structured interviews with 55 patients, relatives and staff about their experiences of post-ICU ward care. These interviews focused on identifying challenges of delivering care to these patients, including positive examples and suggestions for improvement. This work identified common characteristics of the post-ICU non-surviving population, the degree of ‘avoidability’ of these deaths and common problems in their care.
For each ‘problem in care’, I held a stakeholder meeting with representatives from each of the three study sites. At each meeting the Human Factors-based ‘Functional Resonance Analysis Method’ (FRAM)5 was used to map out care delivery in the target area of care, identifying challenges, facilitators and variations across sites.
The primary output of this body of work was identification of key areas of care delivery amenable to change. From this I am developing a complex intervention to improve post-ICU in-hospital survival, to be tested in a clinical trial. In addition, making changes to this area has the potential to improve both patient and staff experience.
The REFLECT study was funded by the National Institute for Health Research (NIHR) under its Research for Patient Benefit (RfPB) Programme (Grant Reference Number PB-PG-0215-36149). The views expressed are those of the author and not necessarily those of the NIHR or the Department of Health and Social Care. This work was also supported by the NIHR Biomedical Research Centre, Oxford.
0147
Understanding stress-driven genomic reprogramming and its consequences in critical illness
Alasdair Jubb1, Shelagh Boyle2, Robert Young3,4, David Hume5,6 and Wendy Bickmore2
1Division of Anaesthesia, Department of Medicine, University of Cambridge, Cambridge, United Kingdom
2MRC Human Genetics Unit, IGMM, University of Edinburgh, Edinburgh, United Kingdom
3MRC Human Gentics Unit, IGMM, University of Edinburgh, Edinburgh, United Kingdom
4Now at Usher institute, University of Edinburgh, Edinburgh, United Kingdom
5The Roslin Institute, University of Edinburgh, Edinburgh, United Kingdom
6Now at Mater Research Institute, University Of Queensland, Brisbane, Australia
Abstract
Each year there are >290,000 admissions to Intensive Care in England (1). Most patients survive, but many suffer long-term adverse physical and psychological consequences, which scale with severity of acute illness (2). We do not understand the causes for this, and hence have no effective treatments. My work aims to address the gaps in our knowledge of the biology underlying critical illness.
Critical illness triggers stress responses, including adrenal release of glucocorticoids (GC), and relatively high GC levels usually persist even in the prolonged phase. Mechanistically, GC interact with our DNA via a receptor protein (GR), altering gene expression. Differential expression of what are very similar sets of genes lead to phenotypic differences between individuals and species.
During my doctoral work I asked what are the differences in gene expression after exposure to GC between mice (a major model system for human disease) and humans? Macrophages are ubiquitous innate immune cells that express GR at high levels and play important roles in inflammation, resolution and repair arising from critical illness. I found limited overlap (10%) in the genes responsive to GC in human and mouse macrophages (3), but gene induction predominated in both species. I showed that the divergence is driven by differential GR binding to DNA at sites far from target genes. Gain and loss of GR binding sites between the species was not under positive selection. However, there was a strong signal for purifying selection at the few conserved sites, suggesting that these minority of sites have an evolutionarily important role. My results support cautious interpretation of murine data for humans but, equally, given the principlesof the response were the same in both species, for some questions mice remain a good model of GC biology.
How the distant GR binding events I (and others) have detected change gene expression is not known. Studies show that loops in the DNA can form between gene promoters and distal elements (4). In contrast, I found GC treatment of mouse macrophages induced very rapid (5 minutes) unfolding of DNA detectable by fluorescence in situhybridization (FISH) at loci associated with GR binding (5), which I have now replicated in using human macrophages. At conserved loci, inducible in both mouse and human macrophages (3), the structural reorganisation of DNA was sustained for at least 5 days following GC removal (5). Persistent genomic reprogramming, such as I measured in vitro, provides a plausible mechanism for the prolonged impact of the physiological stress of an ICU stay on survivors.
To pursue this hypothesis further, I am currently undertaking a comprehensive characterisation of GC- and critical illness-driven genomic reprogramming, focusing on both the observable consequences and the functionally important GR partner proteins. By these two paths, I aim to discover novel therapeutic targets for ongoing study, provide insight into the mechanisms of GR action, and ultimately drive improved outcomes for ICU patients.
This work was supported by the Wellcome Trust (097481/Z/11/Z), the MRC and BBSRC.
0165
A novel clinical monitor combining NADH fluorescence and tissue haemoglobin saturation to assess the adequacy of tissue perfusion
Chris Smart1, Mervyn Singer1 and Geoff Ward2
1University College London, London, United Kingdom
2In Tandem Designs, Warrnambool, Australia
Abstract
My project was to develop a novel device that simultaneously monitors mitochondrial redox state (via NADH fluorescence) and tissue microvascular oxyhaemoglobin saturation (StO2) via an implantable fibre-optic probe.
Nicotinamide dinucleotide hydride (NADH) is the reduced moiety of NAD and the principal electron carrier from Krebs’ cycle to electron transport chain. With progressive hypoxia [NADH] rises in a hyperbolic fashion, mirroring the rapidly stalling oxidative phosphorylation rate.1,2 NADH fluoresces under ultraviolet light excitation whereas its oxidised counterpart (NAD+) does not. Monitoring mitochondrial redox state (NADH:NAD+ ratio) via NADH fluorescence thus allows direct assessment of the adequacy of local oxygen supply to support aerobic respiration.3
NADH fluorescence was excited via a 340 nm LED, and StO2 was measured by a bespoke algorithm applied to diffuse reflectance from a pulsed white LED. The StO2 algorithm was proven accurate in phantom models using dilute solutions of soya emulsion, whole human blood, and yeast to function as an oxygen consumer. Solutions of NADH in soya emulsion were quantifiable down to ten micromolar.
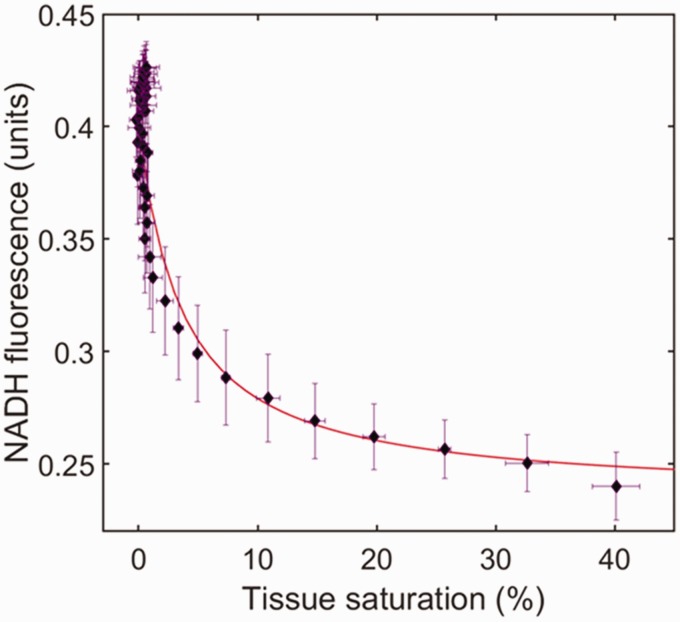
I performed various in vivo validation studies in rat models including aortic occlusion [Figure 1] and progressive haemorrhage-resuscitation (H-R) [Figure: 2]. After anaesthetic induction and arterial and venous cannulation, I implanted the fibreoptic probe into the vastus lateralis thigh muscle. For limb occlusion experiments I abruptly occluded the infrarenal aorta with a snare. For H-R studies, I withdrew 10% of estimated blood volume (66 ml/kg) at 15 minute intervals until cardio-respiratory arrest. The withdrawn blood was then returned, and the animal observed for 20 minutes then euthanised. NADH fluorescence, tissue HbO2 saturation, tissue PO2 and BP were recorded continuously with intermittent arterial blood gas analysis.
Initial tissue saturation varied from 50–70%, and the NADH fluorescence index from 0.15–0.22 units. Progressive leg ischaemia or hypoperfusion resulted in falls in tissue HbO2 saturation and tissue PO2 and increases in NADH fluorescence. Animals suffered cardiac arrest between 40–60% loss of EBV. Peri-arrest StO2 was universally near zero, with NADH fluorescence rising to between 0.34–0.42 units. Animals responding to resuscitation renormalized NADH, whereas non-survivors continued to increment [Figure 2].
In conclusion, I developed and then validated in vivo a monitor that can assess the relationship between tissue haemoglobin saturation and mitochondrial oxygen sufficiency. To my knowledge, these two modalities have never been combined onto any implantable scientific instrument. I demonstrated that quantitative monitoring of muscle NADH fluorescence and tissue oxyhaemoglobin saturation is useful in delineating tolerated limits in ischaemic states. Muscle StO2 values <10% and sustained NADH rises >0.35 units portend cardiovascular collapse. This device may have direct utility in shock states, both as a research tool and a real-time monitor.
Figure 1.
The hyperbolic relationship between StO2 and NADH fluorescence, obtained by the device during four aortic clamping events in an anaesthetised rat.
Figure 2.
Serial haemorrhage in non-survivor. 10% Estimated Blood volume withdrawn from arterial line at black arrows. Systolic blood pressure shown (Pink shade), Tissue saturation in pink, and NADH fluorescence in green. Unsuccessful resuscitation at red arrow predicted by poor NADH response.
Abstracts selected as ePoster presentations
0013
Haemophagocytic Lymphohistiocytosis – The Lethal Cytokine Storm: A Case Report
Luke Flower1, Richard Stratton1, Animesh Singh1, Rachel Westbrook1 and Jim Buckley1
1The Royal Free Hospital, London, United Kingdom
Abstract
Background: Haemophagocytotic Lymphohistocytosis (HLH) is a syndrome characterised by pathological immune dysfunction, with resultant cytokine storm and haemophagocytosis.1 If left untreated, it is almost always fatal.2 Despite this it is often misunderstood and under-diagnosed. It is therefore key intensivists are aware of this disease and include it in their differential when approaching critically unwell patients.
Case: A 47 year old gentleman presented with a 3–4 month history of worsening left sided facial pain, swelling and malaise, with nil improvement following a course of oral antibiotics. His medical history included a liver transplant in 2011 for primary sclerosing cholangitis, following which he was on long-term immunosuppression.
On admission he was treated as a presumed facial cellulitis with antibiotics and antifungals and a biopsy of the left maxillary sinus was performed.
He rapidly deteriorated, developing a severe AKI (creatinine > 1000), respiratory failure (PaO2/FiO2 ratio 13.3 kPa), liver failure (ALT and AST > 1000), cytopenia, coagulopathy (INR 1.9), intermittent pyrexia and circulatory collapse. He was transferred to ICU, intubated and ventilated, haemofiltered, started on inotropes and treated for presumed severe sepsis with multi-organ failure.
The patient’s EBV DNA level was measured at 5.8.106 copies/ml, with a ferritin of >78,000 micrograms/litre, raised triglycerides and LDH. These results, when combined with the clinical picture, led to the diagnosis of HLH. The patient was started on an interleukin-1 antagonist (Anakinra), methyl prednisolone and IVIG.
The biopsy of the patient’s sinus demonstrated an aggressive endo-nasal Natural Killer (NK)/T cell lymphoma. A liver biopsy was performed, which confirmed the presence of lymphoma with associated HLH. The lymphoma was felt to be a result of either his EBV viraemia or immune-suppression and the likely trigger of his HLH.
Following initiation of HLH treatment, the patient’s physiology improved significantly. Within 72 hours he no longer required inotropic support, and had halved his FiO2 and ventilatory requirements.
After initially being deemed too unwell for chemotherapy, following his physiological improvement, he was re-discussed and transferred to a tertiary oncology centre to commence treatment.
Conclusion: HLH is a life threatening condition, with an often non-specific and aggressive presentation. It is the result of an uncontrolled immune response, with excessive macrophage activation and cytokine production, coupled with reduced NK and cytotoxic lymphocyte function.2 The resultant cytokine storm and excess haemophagocytosis leads to multi-organ failure with pan-cytopaenia.
There appears to be a strong underlying genetic predisposition to the development of HLH when faced with a suitable trigger.3 The most common triggers include EBV and lymphoma. Clinical symptoms and biochemical signs can be both varied and non-specific,4,5.
Treatment is based on addressing the underlying cause and HLH specific treatments. These tend to revolve around controlling the immune dysfunction, usually involving interleukin-1 antagonists, anti-neoplastic agents and steroid treatment.
Without treatment, HLH is almost invariably fatal.2 As many clinicians know little about the disease, under-diagnosis is often the biggest barrier to treatment. It is therefore paramount that intensivists are aware of HLH, its possible presentations and the necessity of early diagnosis and effective treatment.
0014
Assessment of venous thromboembolism (VTE) risk and the provision of prophylaxis in the critical care unit
Patrick Barclay
Newcastle University, Newcastle, United Kingdom
Abstract
VTE cause 60,000 deaths a year in the UK, half of which are due to hospital admission.1 Endothelial injury, stasis of blood flow and hypercoagulability (Virchow’s triad) are the three components that are required for thrombosis. Sepsis, post surgery, trauma, heart and respiratory failure are all inherently pro thrombotic and common in intensive care. These initial risk factors are multiplied by the inherent nature and interventions found in critical care medicine. For example; vasopressors, central venous catheterisation and haemodialysis are common place, enhancing the patient’s hypercoagulable status. Immobility also largely contributes to blood stasis, increasing the risk of DVT tenfold.1
The incidence of asymptomatic DVT on admission to the intensive care unit (ICU) is as high as 5.5%, rising to 29% in those patients who did not receive thromboprophylaxis prior to ICU admission.1 Moreover, detecting DVT’s and PE’s pose their own challenge as the majority are clinically silent and present symptomatically without warning and often fatally. Even with adequate thromboprophylaxis, the critically ill patient still has a high risk of VTE, with 15% of patients found to have a DVT.1 Therefore, this makes the critically ill patient one of the highest at risk of venous thromboembolism (VTE), significantly increasing their morbidity and mortality.
The aim of the audit was to assess the compliance to NICE guideline NG89 (2018) standards 1–5, interventions for people admitted to critical care2 with a target compliance of 100%.
| Number | Standard |
|---|---|
| 1 | Assessment of VTE and bleeding |
| 2 | Provide pharmacological prophylaxis, unless contraindicated |
| 3 | Consider mechanical VTE prophylaxis unless contraindicated |
| 4 | Reassess VTE and bleeding risk daily |
| 5 | Adjustment of pharmacological prophylaxis based on renal function and weight |
Data was collected via a prospective analysis of patients admitted to the Intensive Care and High Dependency Units, achieved by scrutiny of patients’ bedside charts and notes by two observers. Analysis was subsequently performed to determine compliance with standards, recognising patient exclusion criteria in accordance with local unit guidelines.
| Standard | Compliance % |
|---|---|
| 1 | 62 |
| 2 | 98 |
| 3 | 53 |
| 4 | 48 |
| 5 | 100 |
50 consecutive patients (n = 50) were analysed.
The audit has shown evidence of good compliance with pharmacological prophylaxis with evaluation of renal function and BMI. However, there are deficiencies in initial assessment, mechanical techniques and documentation of their contraindications.
0016
Mortality of in-patient medical admissions to a DGH Critical Care Unit
Sunil Tailor1, Ademola Ademilua2, Omubo Davies1 and Roger Slater2
1Shrewsbury and Telford Hospital NHS Trust, Telford, United Kingdom
2Princess Royal Hospital, Telford, United Kingdom
Abstract
Increasing clinical demand and reorganisation of hospitals may result in “stable” medical in-patients being “cohorted” into hospital locations without ready access to critical care services on site.
The NEWS tool is recognised to provide warning of deterioration and a trigger for escalation of care.1
Current EWS tools perform well for predicting death and cardiac arrest within 48 hours, although the impact on in-hospital health outcomes and utilization of resources remains uncertain.2
In a retrospective case review, we examined the outcome of medical patients who had been hospital in-patients for more than 48 hours, whose condition deteriorated, requiring admission to our critical care unit (Princess Royal Hospital). The aim was to identify “red flag” observations for their deterioration and to measure mortality (overall: hospital +30-day) in this patient group.
During 2016–17 we identified 51 patients, of whom 39 patients were analysed because of a complete data set.
We classified 48% (19 patients) as hot: defined as having NEWS of 5 or more on one or more occasions in the 48-hours prior to ITU admission.
52% (21 patients) were classified as warm; defined as having NEWS no greater than 4 on one or more occasions in the 48 hr prior to ITU admission.
Red flag parameters (individual score of 3): respiratory rate: <8 or >25; SpO2 <91%; temp <35C; SBP < 90 or >220; HR < 40 or >131; AVPU: VPU.
• The most common predictive red flag indicator for ITU admission was a raised respiratory rate.
• 11 of the 39 patients did not score any red flag indicators. The mortality of this group was 33%.
• The mortality rate of 39 patients was 66%. The mortality for hot and warm classifications was 71% and 46% respectively.
• The majority (>80%) of patients were aged 51–80 years.
• The mean duration of ITU stay was 7.4 days (warm) vs 9.5 days (hot).
• Over the same time period, ICNARC data demonstrated that 80% of all admissions to the ITU were non-surgical; ITU and hospital mortality was 15.7% and 22.5% respectively.
• Medical inpatients with high NEWS of 5 or more during 48 hrs prior to ITU admission had very high 30 day mortality despite ITU care.
• 11 inpatients had no red flag indicators in the 48 hours prior to ITU admission despite their subsequent deterioration.
• There are significant resource implications in managing such patients.
• Care must be taken in defining stability in respect of medical in-patients in order to avoid later deterioration.
Limitations: not all patients could be analysed because of incomplete data.
0018
The use of high flow oxygen in ICU patients with Type 1 respiratory failure: A comparison of the use of high flow oxygen in patients across North West intensive care units
Salma Mahmoud1 and Rachel Markham2
1Lancaster Medical School, Lancaster, United Kingdom
2Royal Lancaster Infirmary, Lancaster, United Kingdom
Abstract
Introduction: In the past two decades, the development of high-flow oxygen therapy (HFOT) has led to its increased use in adult populations.1 HFOT allows warm and humified oxygen to be delivered up to a flow rate of 60 L/min.2 The therapy has a range of physiological advantages and it is generally well tolerated by patients.3
Large studies4 have shown promising results with HFOT use in patients with hypoxaemic respiratory failure. However, there is lack of high-quality research within the available evidence base. Currently, there are no national guidelines relating to HFOT use in critical care.
Objective: The aim of this audit was to determine whether local protocol exists in ICUs across the North West. The audit looked at the factors associated with decision-making and commencement of HFOT. A further aim of the audit was to use the data collected to devise a unified set of guidelines for HFOT use in ICU.
Methods: We used a standardized telephone questionnaire of 13 adult critical care units across the Lancashire and South Cumbria Critical Care Network, and Greater Manchester Critical Care and Major Trauma Network.
Questions asked were:
Does your ICU/Critical care unit have guidelines or protocol relating to starting patients on high-flow oxygen therapy?
Who makes the decision about the use of high-flow oxygen in ICU?
Does your ICU/Critical care unit have set starting flows and temperature?
Does your ICU/Critical care unit have protocol relating to switching patients from high-flow to NIV?
Does your ICU/Critical care unit have protocol relating to switching patients from high-flow to invasive ventilation?
Do you know if HFOT can be used outside of ICU?
Do you know what the main use for high-flow oxygen in your ICU is?
Results: All 13 centres utilised HFOT on ICU, however, 85% of hospitals do not have protocol for commencement of the therapy. 30% of the centres stated that it was a solely consultant or registrar-level decision, and the other hospitals had a more collaborative approach. Many hospitals set the flow rate of therapy based on patient parameters, but 46% of ICUs had a starting flow rate of 40 L/min. Only three hospitals limited the use of HFOT to ICU or high-dependency units, with the remaining hospitals using HFOT mainly on the respiratory wards, utilising a ward protocol.
Conclusion: This audit has highlighted the inconsistency and uncertainty surrounding HFOT use within ICU. There is clearly a gap in protocol and national guidance should be developed to ensure standardised use of high-flow in critical care patients.
| Frequency | % | |
|---|---|---|
| Guidelines | 2 | 15 |
| No guidelines | 11 | 85 |
| Consultant-led decision | 4 | 30 |
| MDT decision | 9 | 70 |
| No set starting flow rate | 7 | 54 |
| Starting flow rate of 40 L | 6 | 46 |
| Protocol for switching patients from HFOT to NIV or invasive ventilation | 0 | 0 |
0020
Identification of barriers and enablers towards performance of a Damage Control Surgery protocol amongst non-medical theatre staff at a Major Trauma Centre
william Francis-Smith1, Neil Roberts1, ed brittain1, samuel mcaleer2, kate holmes1 and paul moor1
1Derriford Hospital, Plymouth, United Kingdom
2royal cornwal hospitals NHS trust, Truro, United Kingdom
Abstract
Critically injured patients sometimes require immediate transfer to theatre for life-saving Damage Control Surgery (DCS). Achieving this in a timely fasion requires a complex pathway of behaviours amongst theatre staff ranging from obtaining and communicating critical patient details to identification and sourcing an appropriate theatre, trained staff and resources like blood and surgical kit. A ‘DCS protocol’ is in use to facilitate this at our hospital. However, case review reveals variable performance, with informal discussion suggesting multiple factors affecting this. Implementation science frameworks may be used to systematically analyse factors affecting clinical behaviour. This study uses the Theoretical Domains Framework (TDF) to identify barriers and enablers towards performance of the hospital’s DCS protocol and facilitate more effective performance improvement.
Paper questionnaire distributed to a purposive sample of all non-medical theatre staff (administrative, non-registered, band 5, band 6, band 7) for one week. Two questions for each of 14 TDF domains, addressing perceived importance and agreements with the domain as either a barrier or an enabler. Participants completed a 5-point Likert scale (1 = Very unimportant/strong barrier, 5 = Very important, strong enabler). Importance was compared using mean average. Agreement was described using a novel 2 × 2 graph to display concordance/discordance within participant groups. As a service improvement project, ethical approval was not required.
69 questionnaires were returned out of 200 distributed (35% response rate). Out of those completing demographic questions, 4 were administrative staff, 11 non-registered nursing, 39 Band 5/equivalent nursing, 10 Band 6, 4 Band 7. 20 responded as anaesthetic staff, 36 as surgical.
Domains perceived as most important for performing the DCS protocol were Skills and Resources (mean 4.1), closely followed by Beliefs about Consequences, Intentions, Social and Professional Role, and Knowledge (4.0). Domains perceived as less important were Behavioural Regulation (BR) (3.7), Emotion (3.4) and Reinforcement (3.0). There was some variation between staff groups, for example feedback-based domains (Reinforcement and BR) were more important for leadership groups (Band 6/7).
There was a wide spectrum of both concordant and discordant barrier and enabler domains. For example, Knowledge, Skills and Belief in Capabilities were important barriers for non-registered staff, along with Memory/Decisions/Attention, which was an enabler for other staff groups. Resources was a particularly discordant domain amongst non-registered and Band 5 s. Audit and feedback domains were strong enablers for Band 6/7 but barriers for others.
This study systematically identifies targets for improving performance of the DCS protocol at this trust, for example particular need to focus on capability-based domains for non-registered staff, a need to further investigate resource variation in Band 5 s, and a need to maintain good feedback about DCS cases for those in leadership roles. Other trusts could use this method to identify their own barriers and enablers towards effective DCS. The method may easily be applied to guide other performance improvement processes beyond DCS.
0021
Evaluation of maternal critical care provision in a UK tertiary intensive care unit
Stephen Glover1, Claire Hirst1, Eleanor Kehlenbeck1 and Kris Bauchmueller1
1Sheffield Teaching Hospitals, Sheffield, United Kingdom
Abstract
Despite generally low mortality rates in the obstetric population, there is increasing recognition that a multi-disciplinary approach is needed for the care of unwell women in pregnancy and the peri-partum period.1 Recent national guidance has outlined the cornerstones of high quality enhanced maternal critical care provision.2
We aimed to describe the obstetric critical care population in our institution, assess how our service compares against these new standards and where to focus further quality improvement work.
We conducted a retrospective review of all obstetric patients admitted to one of our general intensive care units (ICUs) between Jan 2013 and Nov 2018. Data on patient demographics, admission characteristics, critical care provision, outcomes and parent team input were extracted from the ICNARC database and MetaVision electronic patient record. Our trust has a split site configuration, with the Royal Hallamshire Hospital (RHH) ICU located close to the maternity unit and pulmonary hypertension centre, whilst the Northern General Hospital (NGH) ICU is co-located with the Emergency Department (ED) and Major Trauma Centre at another site across the city. Descriptive statistics were used and data expressed as median (range).
Overall, 143 patients were included in the study, 108 (76%) recently and 35 (24%) currently pregnant, 131 from RHH and 12 patients from NGH. 118 (83%) of admissions were for surgical reasons and 25 (17%) patients had a medical admission diagnosis. The majority (66%) of admissions were unplanned. The median age was 32 (18–49) and median APACHE 2 and SOFA scores on admission were 9 (0–27) and 4 (0–14). The leading reasons for ICU admission, severity of illness and respective length of stay on critical care are summarised in table 1. One patient died on ICU (splenic rupture), translating to an overall critical care mortality of 0.7%. Evidence of personal review by a Consultant anaesthetist, obstetrician or midwife was found in 40%, 29% and 15% of ICU days at RHH and 0%, 4% and 6% at NGH (only appropriate patients included).
Critically unwell obstetric patients present with diverse and complex pathology, mandating tailored levels of critical care input. Whilst overall mortality in our centre is very low in keeping with national data, there appears to be a significant lack of consistent daily senior anaesthetic, obstetric and midwifery input once patients are cared for on the ICU. Despite relatively limited patient numbers, the level of this additional specialist input was extremely low at the ICU remote from our maternity unit. Future quality improvement work should focus on creating an infrastructure that allows timely and regular multi-disciplinary care for our vulnerable critically ill maternal population.
Table 1.
Overview of different diagnostic groups amongst critically ill obstetric patients (median values expressed).
| Diagnosis category | No of patients (%) | APACHE-2 | ICU length of stay |
|---|---|---|---|
| Major obstetric haemorrhage | 38 (27) | 9 [6–18] | 2 [1–9] |
| Sepsis | 23 (16) | 11 [1–18] | 4 [1–16] |
| Pulmonary hypertension | 20 (14) | 7.5 [2–11] | 6 [1–21] |
| Cardiac disease | 12 (8) | 8.5 [5–27] | 2 [1–77] |
| Abnormally invasive placenta | 11 (8) | 11 [6–13] | 2 [2–3] |
| Respiratory failure | 9 (6) | 16 [7–27] | 2 [2–17] |
| Venous thromboembolism | 4 (3) | 7 [0–13] | 2.5 [1–3] |
| Pre–eclampsia | 4 (3) | 11.5 [9–14] | 2 [1–7] |
| Trauma | 3 (2) | 11 [8–14] | 4.5 [4–5] |
| Other | 19 (13) | – | – |
0022
The development of an ICU daily review proforma for medical trainees in improving quality of patient care
Arianne Ng1, David Hepburn2 and James Williams2
1Cardiff School of Medicine, Cardiff, United Kingdom
2Royal Gwent Hospital, Newport, United Kingdom
Abstract
Daily reviews are an integral part of the ICU process, and the clinical information is used to improve, or in some cases validate, the management plan, of patients. The introduction of an ICU review proforma was designed to mprove the data capture process and provide an important reference guide to ensure key and essential clinical details are not missed, e.g. delirium screening and RASS score. Furthermore, a standardised proforma should improve care processes as it ensures consistency in data capture amongst different clinicians, and potentially increases the productivity of the daily review process.
The project comprised of 3 distinct PDSA cycles: the development of the draft proforma, the trial of the draft proforma and finalisation of the proforma. A detailed retrospective audit of daily review documentation and face-to-face interviews with doctors and nurses, at ICU Royal Gwent Hospital, helped to identify the key and essential clinical information that should be captured during the daily review process. The draft proforma was subsequently developed and launched to ICU clinicians who trialled the proforma during their daily review round. Clinician feedback was collated via a questionnaire, and the proforma was revised and re-distributed. Further feedback from clinicians was obtained before finalising the proforma.
The detailed analysis of 53 randomly selected daily reviews, from 18 RGH ICU doctors, revealed that clinical information was consistently missed from daily reviews, e.g. thromboprophylaxis (96.2%), RASS score (90.6%) and checking of catheters, drains and lines (86.8%). There was also no documentation on prophylactic measures for pressure ulcers and eye care and CAM ICU score.
The ICU daily review proforma was designed to overcome the shortfall of information identified in the initial audit, as well as help clinicians capture key and essential data in a logical, complete, and consistent manner. Overall, 62% believed the new proforma was user-friendly and comprehensive, although, there were concerns that it may restrict freedom of thought. However, the overwhelming response from ICU clinicians was that, they believed, the proforma would be beneficial in helping teach trainees as it creates a platform where essential clinical information is consistently recorded in helping treat patients.
In summary, much information is not consistently documented in daily reviews, e.g. CAM ICU and RASS scores. It is recommended that the daily review proforma should be included as part of ICU induction training because it allows trainees understand the information requirements in the daily review, as established by consultants, and can be is a useful reference guide for medical trainees. This ensures that important information is routinely documented leading to comprehensive clinical records, improved communication and continuity of care between different clinicians reviewing the same patient.
0025
Early cardiovascular dysfunction drives in-hospital trauma deaths
Rich Carden1,2, David Lockey3 and Karim Brohi1,2
1Centre for Trauma Sciences, QMUL, London, United Kingdom
2Royal London Hospital, London, United Kingdom
3London's Air Ambulance, London, United Kingdom
Abstract
Improvements in trauma resuscitation practice have reduced the early in-hospital mortality from haemorrhage and its immediate sequelae. Early cardiovascular dysfunction (CVD) is a poorly understood and under-recognised major contributor to contemporary trauma deaths. The objective of this study was to demonstrate the prevalence and impact of CVD in a population of trauma patients without catastrophic TBI.
A review of data collected prospectively at a UK Major Trauma Centre from 2008–2018. Adult trauma patients over the age of 15 were included. CVD was defined as a score of 4 on admission or day 1 of admission using the cardiovascular component of the SOFA score.
Early CVD was more prevalent than any other single-system dysfunction assessed with the SOFA. All deaths with single organ failure in a SOFA domain other than cardiovascular had concurrent CVD. In predicting 28-day mortality, CVD had an AUROC of.882 (CI = .810–.955, p = 0.000), odds ratio of 57.2, and sensitivity and specificity of 86.7% and 89.7% respectively. Multiple regression analysis identified admission base deficit, admission systolic blood pressure and heart rate, increased age, blunt mechanism, increased injury severity score, and 24-hour crystalloid administration as strong predictors of developing CVD. These findings challenge the traditional view that post-injury MODS is driven predominantly by respiratory dysfunction.
CVD is a recognisable clinical phenotype that manifests early in the post-resuscitation phase, and is the earliest organ system to exhibit signs of dysfunction following critical injury. Future work should characterise this further, through both ultrasound and biomarker studies of the critically in
0026
Service Evaluation of Allied Health Professional Unmet Need in Critical Care
Nicola Williams, Jean Briggs, Helen Turner, Emma Leech and Linda House
Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
Abstract
Introduction: Critical illness can have catastrophic and often long-term consequences for survivors. Physical, cognitive and psychological impairments can result in reduced health-related quality of life which can persist for many years following hospital discharge. In recent years the importance of survivorship, or quality of survival, has been increasingly recognised. Early rehabilitation has been identified as improving outcomes, key to this is Allied Health Professionals (AHP) input into critical care. National guidance (NICE 83) and GPICS standards have highlighted the importance of AHP input into critical care.
Objective: The purpose of this evaluation was to identify the AHP unmet need on a single critical care unit.
Methods: The data was collected over an 8-week period on a daily basis using a questionnaire developed by all the AHP leads. This identified patients appropriate for AHP input, the type of interventions and if these were achieved. Inclusion criteria were patients who required AHP input during their admission. Exclusion criteria were elective post-operative patients on enhanced recovery pathways and patients admitted over weekend and discharged with no AHP input. Data was collected and reported in a descriptive and tabular format.
Results: 61 patients met the inclusion criteria for AHP input. 61 patients were identified as requiring Physiotherapy input, of these 61 patients received input. There were 432 opportunities for intervention of which 314 were completed identifying an 18% unmet need. 61 patients were identified as requiring Dietetic input, of these 59 patients received input. There were 222 opportunities for intervention of which 86 were completed identifying a 61% unmet need. 22 patients were identified as requiring Speech and Language Therapy input, of these 11 patients received input. There were 55 opportunities for intervention of which 12 were completed identifying a 78% unmet need. 43 patients were identified as requiring Occupational Therapy input, however currently there is no service provision into Critical Care. There were 166 opportunities for intervention of which none were completed identifying a 100% unmet need. 42 patients were identified as exhibiting psychological distress, however currently there is no Psychology service provision into Critical Care. There were 94 opportunities for psychological interventions of which none were completed identifying an 100% unmet need.
Conclusion: The evaluation identified unmet need for all AHP services onto the critical care unit. Physiotherapy was the most utilised service, however, both Dietetics and Speech and Language Therapy had limited input and identified high levels of missed opportunities for therapy input. Currently Occupational Therapy and Psychology have currently no service provision to critical care but have significant identified opportunities for input. These results indicate the lack of early rehabilitation support from AHP services for patients experiencing critical illness which may be limiting their functional, cognitive and psychological recovery.
0028
Quality Improvement: Critical Care Oxygen Prescribing
Rasmus Knudsen and Neil Allan
Pinderfields Hospital, Wakefield, United Kingdom
Abstract
Introduction: Oxygen therapy is received by 1 in 7 in-patients each day.1 Oxygen is considered a medicinal product and, although not a ‘prescription-only medicine’, does require thorough documentation to communicate its use for individual’s needs – namely target saturation. Usually, this is achieved via a prescription on a patient’s drug chart. British Thoracic Society Guidelines state that an oxygen target saturation range should be prescribed with an accompanying signature to all patients who are admitted to hospital.2
Objectives: To assess the compliance of the critical care unit at Pinderfield's General Hospital in having an active oxygen prescription for every patient. Having introduced a new oxygen prescription sticker to the existing drug charts.
Methods: Prospective audit of oxygen prescriptions per patient drug chart (s) per day for 10 consecutive working days. Data collection took place at one time-point per day. Data were collected on three parameters: target saturations, signature and date of prescription. Fields with handwriting that was illegible were considered to be incomplete.
The primary outcome will be complete active prescriptions, classified as having all three parameters adequately completed.
Results: 87 Prescription charts were assessed over the 10 days; for all of these, data were collected on all three parameters. Overall, 90.8% (79) of patients had a complete active prescription. Of prescriptions which were signed, none were missing target saturations and only 1 (1.3%) was missing the date of prescription.
Conclusion: The data shows that in the majority of cases (>90%), fully complete prescriptions were available for most patients on the critical care unit. Aided by the use of oxygen prescription stickers in the drug charts – not only prompting prescribers but allowing them to circle the target saturations that the patient require.
0029
How to waste a good orange cannula: Reduction in flow rates with assorted attachments and administration sets
Joanna Shak1 and Matthew Woods1
1University Hospitals of Leicester, Leicester, United Kingdom
Abstract
The 14G “orange” cannula in a large proximal vein is the gold standard “wide-bore venous access” for resuscitation. The rather impressive manufacturer quoted flow rates are determined using distilled water at 22oC at 100 kPa through 110 cm of tubing with 4 mm internal diameter. Commonplace practice is for various attachments and giving sets to be attached to the precious large bore cannula, and fluid resuscitation dripped through accordingly. This study aims to quantify the impact of various attachments on flow rates.
Full bags of 0.9% sodium chloride and 10% glucose solutions were suspended 1 metre over a flat surface and allowed to run freely for 1 minute via a standard or blood administration sets. Intravenous cannulae from 22G to 14G were tested. The reduction of flow rates caused by attachments were calculated, including three way tap, single needle free access port, back check valve, triple and double lumen extension sets and single lumen microbore T-piece extension sets.
Flow rates for 0.9% sodium chloride through a standard giving set through 22G to 14G cannulae yielded flow rates of 28mls−1 to 96mls−1, in contrast to the manufacturer quoted 36mls−1 to 343mls−1. (See Table)
The tested extensions caused flow reductions of up to 76%, maximal in narrow bore extensions in combination with wide bore giving set and less viscous fluid (See Figure).
Manufacturer quoted flow rates, tested under ideal conditions, can give a false sense of security. This experiment demonstrates that three-way taps and needle free extension devices provide minimal extra resistance. In contrast, extensions, particularly those with narrow bores, can reduce flow rate by up to 76%. Such impact on flow rates should be considered when choosing giving sets and extensions, especially in the resuscitation setting.
| Flow rate/mlmin-1 |
|||
|---|---|---|---|
| Blood giving set 0.9% NaCl | Standard giving set 0.9% NaCl | Standard giving set 10% glucose | |
| 14G | 209 | 96 | 65 |
| 14G + needle free connection device | 194 | 96 | 59 |
| 14G + three way tap | 211 | 95 | 63 |
| 14G + back check valve | 144 | 75 | 53 |
| 14G + 3 lumen extension | 104 | 63 | 49 |
| 14G + 2 lumen extension | 97 | 61 | 46 |
| 14G + 1 lumen T piece extension | 50 | 41 | 34 |
0030
Developing a culture of early identification of delirium combined with reducing sedation use in Critical Care Patients
Emma Jackson, Jason Cupitt and Rebecca Bell
Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
Abstract
Identification and treatment of delirium in Critical Care (CC) patients is notoriously poor. This Quality Improvement (QI) project aimed to facilitate earlier rehabilitation of patients through:
1 Improving CC staff knowledge of delirium
2 Improving detection of delirium
3 Reducing patient sedation levels
We surveyed nursing staff to explore barriers to identifying and managing delirium. Following identification of key areas, we introduced a novel delirium scoring system (TUFT), facilitated by the introduction of Raspberry PI technology. This assesses patients over an entire shift to give a final delirium score on which treatment is based. Alongside this system, we enforced prescribing of target RASS levels for each patient.
Our staff survey revealed the greatest barriers to reducing sedation were 1) poor staffing and 2) fear of self-extubation. The most common response to agitated patients was to increase sedation and/or analgesia. Nursing staff felt the initial delirium scoring system had no impact on patient care.
Under the initial CAM ICU delirium scoring system, we found that between 45–30% (Feb-March 2018) of patients had unknown delirium status. Following the introduction of TUFT scoring and regular feedback data from the novel Raspberry PI system, unknown delirium status statistics dropped to between 8–18% (April-May 2018). Combined with enforcement of RASS target prescription standards, compliance improved from 0% in Feb 2018 to a peak of 74% in April, with a slight reduction in May. Over this 4-month period, average RASS was reduced from −3 to 0.
While ongoing, this QI initiative shows that delirium detection can be significantly improved, and the unnecessary deep sedation of CC patients markedly reduced, with even a short period of dedicated and regular teaching and the introduction of minimally effortful health technologies.
0031
Drug Therapy in Delirium
Joseph Pick and Nabeel Amiruddin
Dudley Group Hospitals NHS Foundation Trust, Dudley, United Kingdom
Abstract
Delirium is an acute organic and reversible disturbance in cognitive function which frequently occurs in patients in Critical Care. Drug therapy remains part of the multimodal approach to delirium management and prevention. We conducted a retrospective analysis to evaluate how the choice of drug, dose and duration of course influenced a range of outcomes
We conducted a retrospective analysis of patients on the Intensive Care Unit at Russells Hall Hospital from our electronic patient record by including those who were CAM-ICU positive for on at least 2 occasions. The total dose and number of doses of melatonin, haloperidol and quetiapine were extracted and collated from our drug prescription and delivery record. In addition, we extracted the duration of dexmetomidine for each patient. The outcome variables chosen were, duration of delirium, length of stay on ICU and whether or not the patient survived to discharge to ward.
110 patients were included. Most patients received combinations of drug of the drugs chosen for analysis. Only 2 patients received quetiapine. There was a significant linear correlation between the total dose of melatonin and the number of CAM-ICU positive 12-hour period (p = 0.049) AND between the number of doses of melatonin and length of stay on ICU (p = <2 × 10–16). The latter correlation was far stronger that the former based on R-squared values (0.026 vs 0.52).
Melatonin is associated with a longer duration of delirum (based on CAM-ICU status) and length of Stay on ICU amongst the patients in our analysis compared to haloperidol and dexmetomidine. It is possible that the use of melatonin was a co-variant factor and the patients receiveing melatonin were sim ply sicker. However, in a comparison of ICNARC-model predicted in-hospital mortality, there was no difference between the patients receiving each drug.
We propose that a prospective randomised controlled trial should be conducted comparing melatonin to other drugs commonly used in delirium.
0032
Improving information-giving to critical care patients to guide post discharge rehabilitation: a quality improvement project
Dr. Sarah Elliott1, Armin Fardanesh2, Stavroula Stavropoulou – Tatla2 and Oliver Grassby2
1Medway Maritime Hospital, Gillingham, United Kingdom
2Kings College London, London, United Kingdom
Abstract
ICU survivors have a 1-year mortality rate of 30%, and a reduced quality of life associated with post-ICU syndrome; a triad of cognitive decline, physical weakness and psychiatric disorders. Early rehabilitation improves outcomes, leading to greater independence. The NICE CG83 guidelines instruct the provision of rehabilitation information to critical care patients on discharge. Currently, only a third of UK trusts meet these guidelines. Within 20 weeks, we aimed to achieve 100% patient and therapist satisfaction with the rehabilitation information given to patients at risk of physical morbidity on discharge from critical care at Medway Maritime Hospital. Critical care patient and therapist satisfaction was assessed using questionnaires at baseline and after each PDSA cycle. In PDSA1, a generalised rehabilitation information booklet was introduced including input from physiotherapy, occupational therapy, speech and language therapy and dietetics. In PDSA2, a personalised rehabilitation plan for pre-discharge completion by the therapists was added so to tailor rehabilitation plans to individual patient needs. A shift was observed in critical care patient satisfaction scores, indicating a significant change in the median from 20% at baseline to 70% after PDSA2. This was also reflected in the therapist satisfaction scores which increased significantly from 60% at baseline to 80% after PDSA2. The introduction of a generalised information booklet, supplemented with a personalised recovery plan, is an effective way of increasing critical care patient and therapist satisfaction with post-discharge rehabilitation information provision. This should translate to greater critical care patient engagement with rehabilitation and improved long-term outcomes. To further increase satisfaction, the addition of psychiatric input to the booklet is currently underway and the information booklet is given in conjunction with a follow up appointment.
0033
Whose Goal Is It Anyway? A Qualitative Analysis of Physiotherapists’ Perceptions Of Goal Setting in the ICU
Frances Wrack1, Bronwen Connolly2 and Evelyn J Corner1,3
1Department of Clinical Sciences, Brunel University London, Uxbridge, United Kingdom
2Wellcome-Wolfson Institute for Experimental Medicine, Queens University Belfast, Belfast, United Kingdom
3The Royal Brompton and Harefield NHS Trust, London, United Kingdom
Abstract
Quality of life after critical illness is a growing healthcare priority as intensive care unit (ICU) admissions continue to rise, whilst mortality rates decrease.1 Physical and cognitive sequelae from critical illness can cause lasting disability years after discharge.2 Consequently, implementation of National Institute for Health and Care Excellence (NICE) ‘Rehabilitation after critical illness in adults’3 has focussed on early rehabilitation for patients in ICU to minimise these life-changing effects. More recently NICE Quality Standards recommend engaging patients in goal-setting within 5 days of ICU admission to inform early rehabilitation programmes.4 However, with many psychological and physical complexities affecting communication with patients in ICU, combined with uncertain clinical prognoses, delirium, and patient anxiety, clinicians may face difficulties when negotiating rehabilitation goals with this population.
The objective of this study was to explore the perceptions and current experiences of qualified physiotherapists surrounding goal-setting in the adult ICU population.
An atheoretical qualitative study with a constructivist epistemology was conducted using focus groups to gain insight into the perceptions of qualified physiotherapists surrounding goal-setting in the ICU. Participants were recruited via advertisement on social media and snowball recruitment.
Focus groups were conducted at three different London university settings, were audio-recorded, and transcribed verbatim by the research team. An inductive thematic analysis was performed to identify emergent themes.
Fifteen physiotherapists, with 1–20 years' experience, working in specialist ICUs including neuro, cardiothoracic and trauma, participated in three focus groups. Three main themes emerged from the data; 1) ‘…it is a case of semantics’ represented the extensive ambiguity surrounding the terminology used when goal-setting, with treatment plans, familiar rehabilitation milestones, and weaning targets all used under the umbrella of the term ‘goal’. Two subordinate themes, ‘meaning’ and ‘ownership’, signified different values which physiotherapists placed on a goal, depending on the individuals’ interpretation of the meaning and whom the goal belonged to. 2) ‘If’ comprised of two subordinate themes, ‘unknown’ and ‘unpredictability’, and signified the many complexities facing patients during their volatile recovery, including medical setbacks, undetermined clinical prognoses and unrealistic expectations. 3) ‘From staying alive to living’ comprised of three subordinate themes; ‘surviving’, ‘step-by-step’ and ‘becoming human’. These reflected the transition an ICU patient undertakes when regaining autonomy during their recovery, and the different impact goal-setting can have in supporting this important time.
Goal-setting with this unique population is difficult due to the complexities of illness, challenges to patient engagement, and uncertainties regarding the clinical course. This study found that during different phases of recovery, goal setting can be used to support patients during the complex journey of recovery. During early phases of recovery, a paternalistic approach to goal setting, or assuring patients long term goals of hope helps give a sense of stability for the patient during a time of much ambiguity. In later stages of rehabilitation, therapists may use goals which recognise patients’ achievements, promoting feelings of self-efficacy and self-esteem, and use as motivation to continue their unique journey of recovery through ICU and beyond.
0034
Ongoing fluid management of sepsis following initial resuscitation – A survey of current practice across North West Intensive Care Units
Holly Newton1 and Rachel Markham2
1Lancaster Medical School, Lancaster, United Kingdom
2Royal Lancaster Infirmary, Lancaster, United Kingdom
Abstract
Introduction: Each year, over 19 million people develop sepsis, of these only half will recover fully. Current guidelines recommend immediate rapid fluid resuscitation to treat haemodynamic compromise.1 However, guidance for ongoing fluid management on the critical care unit is vague, with no specific end-point defined; despite emerging evidence that fluid overload is harmful, and that fluid restriction may improve prognosis.2
Objective: To investigate current practice of fluid management in sepsis across intensive care units in the north west of England.
Methods: Following ethical approval, we performed a standardised telephone audit of 20 adult intensive care units across the North West of England, all of whom agreed to participate in the survey.
Questions asked were:
1 Does your trust follow a protocol for initial fluid management of sepsis, if so which one?
2 Does your trust follow a protocol for ongoing ICU fluid management after the initial resuscitation? If so, what are they?
3 Does your unit have an end-point at which you would stop fluids e.g. based on blood pressure or urine output etc.?
4 What type of fluid does your trust tend to give?
5 Does your trust tend to give fluid boluses or continuous fluids?
Results: 18 out of 20 units followed a protocol for the initial fluid resuscitation of a patient with sepsis – generally the ‘Sepsis 6’. However, only nine units had an explicit guideline for ongoing fluid management. End-points for fluid replacement varied widely, ranging from physiological measurements to clinical judgement (Figure 1). All units utilised crystalloids for initial resuscitation. Seven units use predominantly fluid boluses for ongoing management, whilst 13 used a mixture of boluses and continuous fluids dependent upon the patients’ parameters.
Conclusions: Whilst the initial fluid resuscitation of a patient with sepsis is now embedded in clinical practice, this audit has demonstrated wide variability in the ongoing fluid management on the intensive care unit. Close attention to fluid balance and development of national guidelines could help to further reduce the mortality from sepsis.
| End-Point at which fluids are stopped | Frequency | Percentage (%) |
|---|---|---|
| Lactate Levels | 1 | 5 |
| Amount of fluid given | 1 | 5 |
| Clinical Judgement | 7 | 35 |
| BP and Urine Output | 7 | 35 |
| Fluid overload/Oedema | 2 | 10 |
| Cardiac Output Monitoring | 2 | 10 |
0037
The stigma revisited: characteristics and mortality of critically ill patients with a malignancy, a retrospective cohort study
Esther van der Zee1, Lianne Noordhuis1, Jelle Epker1, Nikki van Leeuwen1, Bas Wijnhoven1, Dominique Benoit2, Jan Bakker1,3,4,5 and Erwin Kompanje1
1Erasmus University Medical Center, Rotterdam, The Netherlands
2Ghent University Hospital, Ghent, Belgium
3New York University NYU Langone Medical Center, New York, The United States of America
4Columbia University Medical Center, New York USA, The United States of America
5Pontificia Universidad Católica de Chile, Santiago, Chile
Abstract
Introduction: The number of patients with a malignancy who require intensive care treatment has increased (1). Historically, patients with cancer were generally considered ineligible for intensive care treatment due to the unfavourable outcome (2, 3). Although Intensive Care Unit (ICU) survival of cancer patients has improved (4), literature suggest that healthcare professionals display implicit ‘cognitive biases’ towards cancer patients (5), potentially influencing (admission) decisions of (ICU) physicians.
Objective: The aim was to assess the mortality of critically ill patients with a current diagnosis of malignancy or a malignancy in their medical history admitted unplanned to the ICU, compared to a general unplanned ICU population.
Methods: We conducted a retrospective observational, single centre cohort study. The study population was defined as all patients with an active malignancy or a malignancy in their medical history admitted unplanned to our ICU during 1 year (January 1, 2017 to December 31, 2017). Complete remission (CR) was defined as no detectable malignancy and was determined by using the electronic database. We used an univariate and multivariate binary logistic regression analysis to identify factors independently associated with hospital mortality.
Results: During the study period, 2486 patients were admitted to our ICU, of which 702 patients (28.2%) with an active malignancy or a malignancy in the medical history. Two hundred and twenty-one (221) were admitted in an unplanned setting. Slightly more than half of the patients was admitted with an active malignancy (122, 55.2%). Hospital mortality was 43% (n = 95). Compared to our general ICU population, a significant difference was seen (29.6% vs 43%, p-value <0.001). The ICU- and 30-day mortality were 29.9% (n = 66) and 43.9% (n = 97). The ICU mortality of our study population showed no statistically significant difference compared to our general ICU population (29.9% vs. 23.8%, p-value 0.08. Only SOFA score (OR 1.15, 95% CI 1.05–1.26, p-value 0.003) and gender (OR 1.94, 95% CI 1.01–3.73, p-value < 0.05) were independently associated with mortality. The malignancy type (solid or hematologic malignancy) and status (active, CR < 1 year or CR > 1 year) were not associated with hospital mortality.
Conclusion: The majority of the patients in our study population survived the ICU admission. Therefore, the potential stigma and the biases concerning patients with a malignancy are not generally justified.
0038
Outcomes of Ventilated Patients following Reduced Tracheostomy Procedures
Nabeel Amiruddin1, David Stanley2 and Karim Salem2
1Dudley Group Hospitals NHS Foundation Trust, Dudley, United Kingdom
2The Dudley Group NHS Foundation Trust, Dudley, United Kingdom
Abstract
Background: Following the TracMan Study1 the practice of tracheostomy management has changed over time. At Russells Hall Hospital, Dudley, our rates of performing tracheostomies have decreased considerably. This could have had an impact on the duration of stay on ICU or duration of invasive ventilation.
Method: We conducted a retrospective analysis of ventilated patients and their length of stay and duration of ventilation varied over the time period in which tracheostomy insertion rates were falling by extracting all patients who received advanced ventilatory support for more than 1 day on our ICU using local ICNARC data. 1628 patients were included.
Results: There was a significant reduction in ICU length of stay and number of days of advanced respiratory support received over time between 1/1/2009 and 4/6/2019 (p = 1.59 × 10−6 and 1.88 × 10−8 respectively) but not hospital length of stay (p = 0.98).
Conclusions: The tracheostomy rates on the ICU at Russells Hall Hospital, Dudley had a negative correlated with the durations of both ICU stay of ventilated patients and advanced respiratory support. We believe that this is more likely to be due to multiple changes in practice such as improved sedation protocols including daily sedation holds as per BREATHE trial.2
0039
Severe hypercalcaemia in Intensive Care: An unusual cause
ZI HAO REUEL HENG1, Rhys Parry2, Omubo Davies2 and Roger Slater3
1Shrewsbury and Telford Hospitals NHS Trust, Telford, United Kingdom
2Shrewsbury and Telford Hospital NHS Trust, Telford, United Kingdom
3Princess Royal Hospital, Telford, United Kingdom
Abstract
Severe hypercalcaemia is defined as serum calcium > 3.5 mmol/l.
Major causes of hypercalcemia in adults include primary hyperparathyroidism, milk-alkali syndrome and malignant neoplasms. Neoplasms cause hypercalcaemia either by direct invasion (metastasis) or through factors that stimulate osteoclasts (Parathyroid Hormone related Peptide or PTHrP). Very rarely a benign tumour can be responsible. Clinical features of hypercalcaemia correlate with degree and rapidity of rise of serum calcium. Severe hypercalcaemia is associated with neurological, renal and gastrointestinal symptoms.
The differential diagnosis of the cause is determined by measuring parathyroid hormone (PTH) levels.
A 33-year-old woman 37/52 pregnant presented with epigastric pain, vomiting, proteinuria and hypertension and a deteriorating GCS (11/15). A CT head was normal. Blood showed hyperuricaemia and acute kidney injury. She was transferred to the operating room for caesarean section with suspected fulminating pre-eclampsia following a fall in GCS to 8. Immediately prior to general anaesthetic induction she had a generalized seizure. She was induced, intubated and commenced on IV magnesium and labetolol. Following successful delivery, a large pedunculated fibroid was noted on the left side of the uterus.
She was transferred to intensive care sedated, intubated and ventilated. Routine blood testing demonstrated severe hypercalcaemia, corrected serum calcium of 5.05 mmol/l.
PTH was at the lower limit at 1.3 pmol/l (normal range 1.3–7.6 pmol/l).
Treatment consisted of IV rehydration with 0.9% sodium chloride 4–6 litres in 24 hr, IV Pamidronate (a bisphosphonate) 60 mg over 2 hours. Over the next 3 days the serum calcium returned to normal.
A literature search uncovered 3 case reports of benign uterine leiomyomas having been the source of ectopic PTHrP leading to hypercalcaemia [1,2,3].
In this case, the uterine fibroid was presumed to have been the source of PTHrP. Unfortunately, direct measurement of PTHrP was not possible at the time of presentation.
In view of the fact that the calcium had returned to normal with medical treatment and post-delivery, it was decided to defer further surgery. The patient was successfully weaned from ventilatory support after 5 days. She was monitored and calcium remained within normal limits.
3/12 later the fibroid was removed. The histology showed a mitotically active smooth muscle leiomyoma.
Discussion: The clinical picture was strongly suggestive of severe hypercalcaemia associated with a uterine fibroid. The history did not reveal excessive calcium-containing antacids sufficient to cause hypercalcaemia.
A hypercalcaemic crisis can occur during pregnancy; women are most prone during the immediate postpartum period when dehydration and an abrupt decrease in placental transport of calcium to the foetus coexist.
Severe hypercalcaemia can rarely produce seizures, the mechanism is thought to be due to cerebro-vasospasm.
Conclusion: Uterine leiomyoma can rarely be a cause of hypercalcaemia in the critically ill obstetric patient. Severe hypercalcaemia can present in a similar manner to pre-eclampsia, and can worsen pre-eclampsia. Intensivists need to be aware of this condition.
0040
EarLy Exercise in blunt Chest wall Trauma: a feasibility trial (ELECT Trial)
Ceri Battle1, Claire O'Neill2, Kym Thorne2 and Hayley Hutchings2
1Morriston Hospital, Swansea, United Kingdom
2Swansea Trials Unit, Swansea, United Kingdom
Abstract
Historically, analgesia and chest physiotherapy have been advocated as the primary methods of managing a patient with blunt chest wall trauma, with the main aim of reducing the acute risk of the development of potentially fatal pulmonary complications. What remains unknown, is the best management for addressing the longer-term complications, specifically chronic pain and disability. We aim to establish the feasibility of a future definitive parallel RCT comparing the use of early thoracic and shoulder girdle exercise for the management of blunt chest wall trauma patients versus normal care. This feasibility trial will have two primary objectives: 1) To assess the sample size requirements and attrition rates for a full randomised control trial and recruitment period needed to achieve this target; 2) To test the feasibility and acceptability of the proposed trial methods; including the parallel randomised controlled design, the recruitment and consent processes, and collection of the proposed outcome measures at pre-specified time points.
This feasibility interventional study, will be single-centred, at Major Trauma Unit in Wales. All patients with isolated blunt chest wall trauma who are admitted for 24 hours or more will be included, over a three month period in 2019, with an additional three month follow-up period. Patients will be included in the trial if they have isolated blunt chest wall trauma and can complete the exercises and surveys. Patients with other injuries that could contribute to on-going pain and disability will be excluded. Patients allocated to the intervention group, will receive standard care, in addition to a programme of thoracic / shoulder girdle exercises (delivered by the physiotherapist who would routinely manage the patient as part of standard care). This programme will be continued by the patient, three times per day, for seven days post-assessment. The exercise programme will consist of shoulder active range of movement exercises trunk active side-flexion, rotation, forward flexion and extension range of movement exercises (all within limits of pain). The control group will receive standard care only. At baseline and at three months post recruitment, participants will be asked to complete the EQ5D-5 L / Brief Pain Inventory, in order to assess appropriateness of the outcome measures and potential difficulties in follow-up. Participants in the intervention group will be asked to record compliance with the exercise programme, using a pre-designed proforma. Participants will be invited to attend a focus group at the end of the data collection period, the purpose of which will be to discuss the acceptability of the trial by the patients, with particular attention to the exercise programme.
Pre-set trial feasibility criteria will be assessed using a traffic light system (in which green means the target was achieved, amber means the target was not achieved but progression is possible with some minor protocol modifications, and red means progression to a full trial is not possible).
Wales REC 6 has approved the trial. Health and Care Research Wales are funding this trial (Pathway to Portfolio Grant).
0041
Electronic Alerts—making the most of your Clinical Information System to manage Acute Respiratory Distress Syndrome (ARDS)
Moon-Moon Majumdar and Alexander Trimmings
East Sussex Healthcare NHS Trust, Hastings, United Kingdom
Abstract
In 2016, the international multi-centre LUNGSAFE1 trial demonstrated that ARDS is under-recognized and undertreated by clinicians. In 2018 the Faculty of Intensive Care Medicine (FICM) and the Intensive Care Society (ICS) released Guidelines on the Management of Acute Respiratory Distress Syndrome2which provides an evidence-based framework to manage adult patients with ARDS. Intensive care information systems are used to prescribe drugs, document medical plans and collate information but could potentially be utilised further to prompt healthcare professionals. This audit looks at a novel way of improving compliance with national ARDS guidelines.
Objectives:
1 To assess local adherence to FICM/ICS guidelines for management of ARDS
2 To implement an electronic alerting system to aid clinicians
Standards:
• Use of lower tidal volumes (VT) ≤6mls/kg ideal body weight
• Use of plateau pressure (PP) ≤30cmH2O
• Prone positioning for ≥12 hours/day in suitable patients with PaO2/FiO2 ratio (PFR)<150 mmHg (<20 kPa)
The audit was carried out in a 19-bed mixed general medical/surgical critical care unit split across two sites. IntelliSpace Critical Care & Anaesthesia information system (ICCA) was used to search for patients admitted with respiratory failure/post-cardiac arrest/multi-organ failure to Intensive Care (ICU) over the period May—November 2018. 39 patients identified. 15 patients were excluded (never ventilated, insufficient data, PFR > 300 mmHg, cardiac failure contributing to diagnosis). Final total 24. The initial audit results were presented at local governance meetings and teaching sessions for ICU doctors and nurses. Following this, we implemented an electronic alerting system on ICCA. This comprised three real-time yellow banner alerts on the screen in response to certain triggers: 1) “consider diagnosis of ARDS” if an intubated patient’s PFR falls below 300 mmHg 2) “review ventilation” for a patient ventilated with VT > 8mls/kg 3) “consider proning” if an intubated patient has a PFR < 150 mmHg. Re-audit 'cycle 2' was carried out with the same search criteria over the period May—July 2019. 29 patients identified. 16 patients excluded. Final total 13.
Cycle 1: ARDS was formally diagnosed in 12% of our ventilated ICU admissions (LUNGSAFE demonstrated ARDS prevalence of 23.4% in patients requiring mechanical ventilation). In 50% of cases “tidal volume of less than 6 mls/kg”, “lung protective” or “ARDSnet ventilation” was mentioned in the Doctors’ plan. On average over all 4 time points analysed (1, 12, 24 and 36 hours post intubation) patients were ventilated at <8mls/kg 53% of the time and at ≤6 mls/kg just 6% of the time. Just 1/8 of potentially appropriate patients were proned. Good adherence to a PP ≤ 30 cmH2O.
Cycle 2: ARDS was formally diagnosed in 15%. In 69% of cases “tidal volume of less than 6mls/kg”, “lung protective” or “ARDSnet ventilation” was mentioned in the Doctors’ plan. Patients were ventilated at <8mls/kg 73% of the time (averaged across all 4 time-points) and at ≤6mls/kg 12% of the time. 0/6 potentially appropriate patients were proned. Good adherence to a PP ≤ 30cmH2O.
In conclusion, electronic alerting along with an educational drive helped to improve ventilation compliance. However it did not improve documentation of ARDS as a diagnosis, or decision to prone. We have now incorporated 'suspected ARDS' into the daily safety huddle to raise awareness and complement changes to ICCA.
0043
Phenotypic plasticity in critical care: lessons from the ICNARC database
Jeronimo Moreno-Cuesta1, Antony Perera1, Marcos Rodrigues2, Alex Shenfield2 and Mervyn Singer3
1North Middlesex University Hospital, London, United Kingdom
2Sheffield Hallam university, sheffield, United Kingdom
3University College London, London, United Kingdom
Abstract
Background: Critical illness is a non-specific and (usually) maladaptive stress response to an insult (1). Individual patients may survive despite the odds or die unexpectedly. Unexpected deaths (UD) are those who die before being discharged from hospital despite having an estimated risk of death (ROD) <20% using the ICNARC risk model 2013. Correspondingly, patients who survive despite a ROD > 80% can be classified as Unexpected Survivors (US) or Extremophiles. Ordinary Survivors (OS) are those with a ROD < 20% who survive their hospital stay, whereas Ordinary Deaths (OD) are those with a ROD > 80% who die.
Objectives: Our aim is to describe different phenotypic profiles in intensive care patients, particularly those patients that against statistical odds unexpectedly survive (extremophiles) or die (2)
Methods: A random sample (N = 400 for each group, total 1600) was drawn from the ICNARC Case Mix Program database of patients admitted to UK intensive care. Comparisons were performed between survivors (OS vs US), deaths (OD vs UD), patients at high risk of death (US vs OD), low risk of death (OS vs UD), and within US and UD groups. A two-tailed p value <0.005 was considered significant (3).
Results: US were typically male and older than OS (p < 0.001) whereas UD were younger than OD (p < 0.001). During the first 24 hours of admission US patients had significantly higher blood lactate than OS (p < 0.001) while UD patients had significantly lower lactates than OD (p < 0.001). Patients in the US and UD groups had significant longer ICU length of stays (p < 0.005) than OS. The probability of survival within groups at high risk of death was directly related to a lower ICNARC score and blood lactate levels over the first 24 h of admission, and a higher requirement for advanced cardiovascular and respiratory support (c-index 0.752). The probability of dying within groups at low risk of death was directly related to higher APACHE II and ICNARC scores and to the need for advanced cardiovascular or respiratory support (c-index 0.776).
Conclusion: Extremophiles in intensive care are typically elderly males. Lactate levels are not associated with exceptional survival or demise. Characterization of extreme phenotypes could contribute to our understanding of survival in critical illness.
0044
Current use of Animal Assisted Therapy in Critical Care throughout the United Kingdom and the development of a set of National Guidelines
Emma Jackson1, Sarah Anderson2, Simon Riley-Fuller2, James Evans2, Kate Tantam3 and Lyndsey Uglow4
1Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
2Leeds Teaching Hospital NHS Trust, Leeds, United Kingdom
3University Hospitals Plymouth NHS trust, Plymouth, United Kingdom
4University Hospital Southampton FT, Southampton, United Kingdom
Abstract
Animal Assisted Therapy (AAT) has been shown to reduce anxiety, pain and fear. There is increasing use of AAT particularly in the Critical Care environment. There is limited evidence and guidelines on how to make AAT accessible in a safe and controlled manner to these patients.
A National meeting was held in London coordinated by the Leeds Teaching Hospitals who sent out invites to 21 Critical Care Units using AAT to attend. We had representatives from 14 different hospitals; including animal handlers, physicians, nursing, patient experience staff, quality improvement lead and occupational therapists. We discussed current use of AAT, barriers to implementation, infection prevention and potential to determine a national set of guidelines.
There was a wide range of AAT from ‘meet and greet style’, use in follow up and outreach for Critical Care patients and targeted therapy for functional movements. Several hospitals had internal policies already in place for the use of AAT in Critical Care providing robust internal measures and this is reflected in positive reference to AAT in CQC reports., with others using the Royal college of nursing ‘Working with Dogs in Healthcare settings’ as a guide.
There was wide discussion on the varying views held by infection control teams on the use of AAT and the importance of adhering to the strict infection prevention on visits. This also highlighted a potential lack of knowledge of how much work goes on behind scenes by the animal’s handler before and after the visit in order to protect both the patient and the animal.
There was consensus about the importance of accountability and being able to have a set of standards which AAT can be held up to. There was use of a log of patients visited by the animal on which day, this had been extended in some hospitals to a more formal referral system.
Each hospital had a wide variety in inclusion and exclusion criteria for the use of AAT in Critical Care. Some of the more common exclusion criteria included patients that are: in isolation, barrier-nursed, immunosuppressed, allergic, phobic, affected by hyperactive delirium, and patients who declined a visit from AAT.
There is great enthusiasm, nationally, about the use of AAT in Critical Care. This needs to be balanced with protecting patients, staff, handlers and the animals. This could be provided in the format of a set of national guidelines specifically aimed at the use of AAT in Critical Care. This would be based on an amalgamation of current local guidelines plus consultation by appropriate bodies.
There is a need to collect data to show that AAT is beneficial for our patients, this could include assessment of how regularly AAT is used in Critical Care before moving on to a measurable target such as pain scores or reduction in psychological distress.
We are currently working towards creating a set of National Guidelines with the target of launching them by the end of 2020 with the support of ICS and long-term aim of inclusion into GPICS.
0046
Critical analysis of low vs high dose anti snake venom regimen in neuroparalytic snake bite patients
Avinash Agrawal, Suhail Sarwar Siddiqui, Sulekha Saxena, Shuchi Agrawal and Ashwin Yadav
King George's Medical University, Lucknow, India
Abstract
Introduction & Objectives: The optimal anti-snake venom (ASV) dose required to treat neuroparalytic snake envenomation is not well known. low-dose ASV (100 ml iv stat followed by 100 ml 6 hourly till all symptoms disappear) may be as efficacious as the high-dose regimen (200 ml iv stat followed by 100 ml 6 hourly till all symptoms disappear), but a direct comparison of the regimens is not available. The objective of this study was to test the efficacy of low-dose ASV regimen against the high-dose regimen.
Methods: Our study is retrospective observational study at an ICU of tertiary care Hospital. After taking ethical approval, we have done analysis of data of the neuroparalytic snakebite patients requiring mechanical ventilation support over a period of 2 years (June 2014 to May 2916), data of total 112 adult patients with neuroparalytic snakebite patients (requiring mechanical ventilation support) were evaluated. Patients were given either low-dose ASV or high-dose ASV regimen as per advice of primary physician. The primary outcome i.e. mortality, and secondary outcome like time to complete recovery of symptoms, duration of mechanical ventilation and total dose of ASV were compared.
Results: Most patients were males (79 vs 33). The primary outcome i.e. mortality was not statistically different between two groups (p- 0.671). In terms of progression of neuroparalysis, and occurrence of Ventilator Associated Pneumonia (VAP) and ASV reactions, there was no statistically significant difference between two groups. Duration of mechanical ventilation or number of ventilatory days (ACV + PSV) was significantly less with High-dose regimen (p- <0.001)). Total dose of ASV requirement was not statistically significant between two groups (p- 0.637).
Conclusions: In our study, we observed that the high- dose ASV regimen was more effective for neuroparalytic (requiring mechanical ventilatory support) snakebites patients in terms of reduction in number of ventilatory days. However, larger randomized controlled trial are needed for definitive conclusions.
0047
I’m a new ICU Doc, get me out of here! The use of an interactive Escape Room format to facilitate junior doctor induction
Anthony Cochrane1, Nicholas Bolton1 and Osian Howarth2
1St Helens and Knowsley Teaching Hospital NHS Trust, Whiston, United Kingdom
2St Helens and Knowsley Teaching Hospitals NHS Trust, Whiston, United Kingdom
Abstract
Background: Junior doctors rotate between hospitals and departments on a frequent basis and need to be able to provide safe and effective care from the first day in their new rotation. Good, timely local induction helps with this, however junior doctors are still required to familiarise themselves with a large amount of information, in a new environment whilst working with a new team. Trainee feedback on our induction process is that it is adequate, but whilst it is felt to be comprehensive we were concerned that it had become impersonal and risked information overload. We wanted to improve knowledge retention and promote team building.
Escape Rooms are immersive adventure puzzle games that have increased in popularity over the past decade. Players solve puzzles to solve codes used to unlock a series of boxes within a fixed time frame to ‘escape’ the room. They have previously been used in secondary education1, nursing2 and medical student3 teaching. We designed a medical escape room based on a fictional patients admission to intensive care.
Methods: This low fidelity scenario runs inside an ICU side room on the second day of the junior doctors placement after formal induction on the first day. This clinical setting helps familiarise junior doctors with the bed space, paperwork and ICU geography and they work together to find clues, interpret clinical data, and calculate risks to safely guide the admission of a patient with type 1 respiratory failure to the intensive care unit. These clues help unlock a series of four boxes to move the scenario forward with a maximum of 1 hour to 'break out'.
The tasks and clues reinforce both factual information (scoring systems, drug doses, extensions and bleeps) and attitudes (MDT working, consultant support, human factors and fatigue)
After the session a short debrief is held to clarify issues with either the game itself or any points about induction or the unit which are unclear.
Results:
Trainees found the session engaging, enjoyable and useful.
Conclusion: This novel approach to induction has been well received by our trainees, currently we have evaluated learners reaction and satisfaction, in future we would like to assess the higher levels of Kirkpatrick’s evaluation model by accessing knowledge retention and behavioural change.
| Infomation type | Examples |
|---|---|
| Data interpretation | Safe confirmation of an NG tube on Chest X ray, Arterial Blood Gas analysis |
| Risk score calculation | NEWS2 score, A-a gradient, P:F ratio |
| Sources of help and support | Discussion with the ICU consultant, contact details for Critical Care Outreach and Anaesthetic teams |
| Admission routine | Contacting nurse in charge, unit telephone extensions, admission paperwork and ICNARC data collection |
| Safe prescribing | ICU drugs, VTE prophylaxis, stress ulcer prophylaxis and laxative prescription |
| Physiology | Create a model lung using bottles, balloons and straws, calculate a lung protective tidal volume using ulnar length |
| Human factors and tiredness | AAGBI fatigue guidelines and location of on call rooms |
| Location of critical equipment | Cardiac Arrest trolley and Difficult Airway trolley |
| Mean score (out of 10) | |
|---|---|
| Usefulness | 9 |
| Content | 9.5 |
| Relevance | 9.25 |
| Overall experience | 10 |
0048
Challenges in the temperature management of critically ill patients with major burn injuries
Jennifer Driver1, Alexandra Fielding2, Randeep Mullhi3, Elizabeth Chipp3, Dr Barbara Torlinska1 and Tomasz Torlinski3
1College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2Leicester Royal Infirmary, University Hospitals of Leicester, Leicester, United Kingdom
3Queen Elizabeth Hospital, University Hospitals Birmingham UHB NHS, Birmingham, United Kingdom
Abstract
Background: Patients with major burns lose the ability to maintain their core temperature. They compensate for this by increasing their metabolic rate.1,2 The hypermetabolic response is accepted to be a result of resetting the central hypothalamic temperature.2
Guidelines at University Hospitals Birmingham (UHB) recommend the maintenance of a core body temperature in the range 38.5 ± 1°C in patients with major burns.3 The International Society for Burn Injury (ISBI) guidelines mandate maintaining the core temperature above 36°C.4
Methods: This retrospective audit reviewed adult patients admitted with major burns (TBSA ≥ 20%) to the Intensive Care Unit (ICU) in a two year period. The main objectives were to determine:
• The proportion of patients that maintained their temperature in the range 37.5–39.5°C (UHB standard)3 or above 36°C(ISBI standard)4 for the first 48 hours post admission and during the entire ICU stay
• The average core temperature of patients returning from theatre
• The ability to maintain a differential of ≤2°C between core and peripheral temperature in the first 48 hours
Results:
Core temperature was within the UHB standard range 78% of the time and above the ISBI standard 97% of the time whilst on ICU. In the first 48 hours this was 69% and 95% respectively.
Within the first 48 h on ICU, none of the patients had their temperature fully maintained within the UHB range and in 16 patients (67%) it dropped below 36°C at least once.
Encouragingly, the audit showed that hypothermia was avoided in almost all patients returning from theatre (96%). However, patients with higher r-Baux score were more likely to have lower body temperature upon their return (-0.1°C per 10 points r-Baux, 95%CI: −0.001, −0.2, p = 0.04).
The mean core-peripheral temperature gap during the first 48 h on ICU was 1.65°C ± 1.26 and varied from −2.5 to 7.8. There were 7 patients (29%) with an average temperature gap >2°C. A higher temperature gap was associated with TBSA > 50% (OR = 8.0; 95%CI: 1.0–66.5, p = 0.05). Death was not associated with a temperature gap >2°C. However, in survivors, the mean temperature gap of >2°C was associated with significantly longer stay on ICU (median 25.7 days (95% CI: 18.7–32.8) vs. 13.8 days (10.3–17.2) in those with ≤2°C, p = 0.01).
Conclusion: UHB standards were achieved the majority of the time whilst the more liberal ISBI standards were achieved in almost all patients. During the first 48 hours increased core–peripheral gap is associated with increased length of ICU stay. Patients with higher r-Baux score have a lower temperature on return from theatre. These findings highlight the difficulties in managing temperature in major burns.
| Number of patients | 24 |
| Age (years) | 41.6 (16.2, 17–74)* |
| Male Sex | 17 (70.8%) |
| Total Body Surface Area (TBSA) | 42.7% (16.5, 20–83)* |
| Inhalational Injury | |
| Yes | 15 (62.5%) |
| No | 9 (37.5%) |
| Revised Baux Score (r-Baux) | 95 (25, 50–142)* |
| Number of surgical procedures | 6.3 (6.3, 1–18)* |
* Mean (SD, range)
0049
Audit of glycaemic control in a general intensive care unit
Lee Warburton
General Intensive Care Unit, University Hospital Southampton, Southampton, United Kingdom
Abstract
Poor glycaemic control is associated with worse outcomes in critically ill patients.1 Hyperglycaemia is an issue even in non-diabetic critically ill patients due to stress hyperglycaemia. The NICE-SUGAR trial suggests a blood glucose (BM) target of between 6 – 10 mmol/L and intervening with IV insulin to achieve this.2 This target has been adopted for intensive care patients by many medical societies such as the Joint British Diabetes Societies – Inpatient Care Group (JBDS-IP).3 Good glycaemic control also forms a core part of many intensive care supportive care checklists such as the FAST HUG checklist.4 We audited glycaemic control among patients on general intensive care. We defined good glycaemic control as BMs in keeping with the JBDS-IP target of 6–10 mmol/L and appropriate action as commencing a variable rate insulin infusion (VRII) for hyperglycaemia.
We performed a retrospective audit of the first 50 patients admitted to GICU from 15/10/18 onwards. We recorded the first 24 hours of data from the electronic health records (EHR). Patients were excluded if they stayed less than 24 hours, they were admitted for a diabetic emergency (DKA, HHS or Hypoglycaemia), or treatment had been changed to a palliative intent within the first 24 hours. Age, gender, diabetic status, BMs (mean/median/frequency/max), glycaemic targets set (if any), time BM > 10 mmol/L, time to intervention (if any), and hypoglycaemic events were all collected. A note was made of any other events to help guide future interventions. The audit was repeated from 28/11/18 onwards on 50 further patients, after an intervention in the form of a teaching session to medical staff emphasising the importance of glycaemic control and when to start a VRII.
In the pre-intervention group, 16/50 (32%) of patients had hyperglycaemia (8 non-diabetic). 6 patients had an appropriate intervention (VRII) but 1 patient developed hypoglycaemia. 9 patients had no action to hyperglycaemia, 5 of these for more than one BM measurement. 1 patient had hyperglycaemia actively tolerated as part of their clinical targets. In the post-intervention group, 22/50 (44%) of patients had hyperglycaemia (15 non-diabetic). 11 patients had an appropriate intervention (VRII) started but 2 patients had problems; 1 had worsening hyperglycaemia and 1 developed hypoglycaemia. 1 patient had their NG feed stopped as an inappropriate intervention. 10 patients had no action to hyperglycaemia, 6 of these for more than one BM measurement.
We found many patients developed hyperglycaemia in the first 24 hours, most notably more non-diabetics developed hyperglycaemia than diabetics. The most common response to hyperglycaemia was inaction. Another issue was related to inadequate monitoring of blood sugars on IV insulin leading to hypoglycaemia. Education directed at medical staff showed no appreciable difference in behaviour surrounding glycaemic control. Future priorities that have been identified are the development of an official glycaemic control policy, education of nursing staff (who are perhaps better placed to intervene), and modifications to the EHR to nudge clinicians towards intervention in hyperglycaemia.
0050
The South West Experience of High Flow Nasal Cannula Oxygen
Rachel Jones, Hazel Morrison and Alexandra Dipper
PRISM Trainee Research Network, South West, United Kingdom
Abstract
Introduction and Objectives: High flow nasal cannula (HFNC) oxygen is increasingly used to deliver higher concentrations of humidified oxygen to patients than conventional oxygen therapy. The majority of evidence for using HFNC comes from intensive care (ICU) environments. It is increasingly being used outside of this setting, with limited comparative data. We sought to evaluate outcomes for adult patients commenced on HFNC across the South West region.
Methods: Prospective data was collected by the PRISM trainee research group on all adult patients admitted to medicine (9 centres) and ICU (4 centres) and commenced on HFNC across the South West region. The first data collection period ran for 14 days in November 2018 and a second period of 28 days ran during February/March 2019. We looked at indications, treatment escalation trends and mortality.
Results: 109 (43 medical, 77 ICU) patients were started on HFNC oxygen. Age range was 21–91 (mean 62 years). Table 1 outlines the primary diagnosis.
86% of medical patients and 99% ICU patients had an escalation status recorded prior to commencing HFNC. The 30-day mortality was 37% for medical patients and 27% for ICU patients (p-value 0.26). At the point of HFNC commencing on a ward 13/25 (54%) patients who were deemed suitable for escalation were referred to ICU. Rescue intubation was required for 20/77 (26%) ICU patients and 3/25 (12%) medical patients. 17% of ICU patients used HFNC as a step down from mechanical ventilation.
Conclusions: This is a unique prospective review of both ICU and medical patients in one region. Overall mortality rates for those requiring HFNC in our population are similar to those reported for patients requiring acute NIV.1 The difference in 30-day mortality between ward and ICU is not statistically significant, although different indications can be seen for HFNC use. The need for HFNC in acute hypoxaemic respiratory failure indicates significant underlying pathology and should prompt consideration of an ICU review for optimization of care where appropriate.
Table 1.
Primary Diagnosis of Patients started on HFNC.
| Primary Diagnosis | Medical Cohort number (%) | ITU Cohort number (%) |
|---|---|---|
| Pneumonia | 23 (53) | 37 (49) |
| Pulmonary Oedema | 6 (14) | 2 (2) |
| Viral Pneumonitis | 4 (9) | 8 (11) |
| Interstitial Lung Disease | 3 (7) | 5 (7) |
| Pulmonary Embolism | 2 (5) | 2 (2) |
| Other | 5 (12) | 22 (29) |
0054
Sertraline Induced Hypersensitivity Pneumonitis
Gursharan Virdee, John Bleasdale, Ikramullah Mohammed and Emma Graham-Clarke
Sandwell and West Birmingham NHS Hospitals., Birmingham, United Kingdom
Abstract
Hypersensitivity Pneumonitis (HP), also known as extrinsic allergic alveolitis is a granulomatous, non-IgE mediated hypersensitivity reaction of the alveoli and distal bronchioles presenting as an acute, sub-acute or chronic condition. It is most commonly associated with exposure to extrinsic allergens (e.g. avian dust, mould and tobacco) and medications including anti-arrhythmics (e.g amiodarone), cytotoxics (e.g.methotrexate) and anti-epileptics (e.g. carbamazepine). Individuals diagnosed with this condition can present with severe hypoxia and respiratory depression. The fundamental principle of management is to remove the causative allergen. Evidence implicating selective serotonin re-uptake inhibitors as a causative agent is limited, and this case report describes a rare clinical presentation of HP associated with sertraline, how it was diagnosed and subsequently treated.
On the 31st July 2018, a 47-year old Caucasian female (78 kg) presented to the Accident & Emergency (A&E) department with shortness of breath, right-sided pleuritic chest pain and a productive cough. Her previous medical history revealed she suffered from severe depression and gastroesophageal reflux disorder, was a non-smoker and had no known drug allergies. Her current medications included lansoprazole 30 mg once daily (OD) and sertraline 200 mg OD, which was initiated by her General Practitioner in June 2015 at 100 mg OD and had been increased to 200 mg OD two weeks prior to admission after worsening of her depression.
Clinical examination revealed signs of systemic infection (tachycardia, hypotension, pyrexia and hypoxia (SpO2 = 96% on 28%)), a red blanching rash on her abdomen, and a high national early warning score (NEWS) of 10. Due to her clinical presentation, a preliminary diagnosis of community acquired pneumonia was made and benzylpenicillin (1.2 g) and clarithromycin (500 mg) were prescribed. Her condition declined and she was admitted to the critical care unit for sixty days.
A Computed Tomography Thorax and Pulmonary Angiography (CPTA) was completed and though a pulmonary embolus was excluded it clearly demonstrated ground-glass changes in her lung parenchyma consistent with acute respiratory distress syndrome (ARDS). This was confirmed with High-Resolution Computed Tomography (HRCT). A chest radiograph revealed diffuse worsening of interstitial infiltrates with new lobar pneumonia. In addition, microbiology/serology tests were all undertaken and were all negative.
After exhausting all other possible causes of HP and interstitial lung disease (ILD), the possibility of this being an adverse drug reaction was considered. Sertraline was identified as a possible cause of HP following a literature review that included some limited case reports of an association with HP1,2,3,4,5. During a morning ward round one of the authors (GV) suggested sertraline as a cause of HP and after a literature review the sertraline was stopped (26th September 2018), following consultation with the psychiatry team.
This resulted in a remarkably prompt improvement of respiratory function. Respiratory rate, FiO2, PaCO2 and oxygen saturation (>90%) all started to improve within a few days. She was weaned from the ventilator and her tracheostomy removed on the 2nd October 2018 and discharged home on 8th October.
In conclusion, this case report highlights the importance of recognising drug-induced respiratory conditions, particularly in a critical care setting.
0057
High-fidelity simulation as an education tool in Intensive Care
Manoj Wickramasinghe1, Philip Antill2, David Moir2, Claire Tordoff2 and James Beck2
1Leeds Teaching Hospitals NHS, Leeds, United Kingdom
2Leeds Teaching Hospitals NHS trust, Leeds, United Kingdom
Abstract
Simulation was introduced to anaesthesia and critical care through successes seen in the aviation industry. Since then the use of simulation-based education has increased exponentially. Simulation, which is in line with the constructivist theory of experiential learning, aims to teach the application of knowledge and skills as well as test non-technical skills.1 Advances in technology has brought about the change from low-fidelity to high-fidelity simulators. The Faculty of Intensive Care Medicine are increasingly advocating and recognising Simulation based education.2 In Leeds Teaching Hospital Trust we have set up a multi-disciplinary high-fidelity simulation course.
• Application of knowledge and skills in rare and common emergencies
• Exploring and increasing awareness of human factors
• Improving communication skills
• 1 day course with 4 doctors in Intensive care and 8 band 5/6 nurses
• Dedicated simulation faculty including senior nurses, simulation fellow, registrars and consultants with interests and experience in simulation
• Simulation and observation room with high-fidelity SimMan and video footage
• Simulation scenario template including scenario progression
• Formalised debrief session splitting nursing and medical learning objectives separately following by a whole group MDT discussion about non-technical skills and human factors
• Six 20 minute scenarios with 40 minute debriefs throughout day
• The course ends with feedback followed by certificates awarding 5 CPD points
• Excellent feedback received from candidates (Table 1)
• Feedback included the ‘realness’ of the scenarios
• Candidates enjoyed the opportunity to work in a ‘multi-disciplinary team’
• Candidates founded the debriefing session as a particularly useful part of the day and felt it was ‘non-threatening’
A one-day high-fidelity simulation course designed for Intensive Care staff has been well received. Themes in the feedback included the benefit of working in a multi-disciplinary team within a simulation scenario, high environmental and emotional fidelity, and constructive feedback. The feedback for the Leeds Intensive Care Simulation Course suggests and supports the growing body of evidence showing the benefits of Simulation-based education in Intensive Care.3
Table 1.
Feedback from candidates for LICS course.
| Poor | Below average | Average | Above Average | Excellent | |
|---|---|---|---|---|---|
| Introduction | 20% | 80% | |||
| Relevance | 7% | 93% | |||
| Learning outcomes | 11% | 89% | |||
| Debriefing | 9% | 91% | |||
| Overall rating | 2% | 7% | 91% |
0058
Evaluation of the optimal physiotherapy-led mobilisation on critical care following the implementation of a mobility guideline
Nicola Williams, David Seddon and Simon Barden
Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
Abstract
Introduction: Every patient on critical care should be assessed daily for the potential to begin functional rehabilitation including mobilisation. Levels of agitation and sedation, as measured by the Richmond Agitation and Sedation Score (RASS) and consciousness measured by the Glasgow Coma Scale (GCS), can impact on the type of activity delivered by physiotherapy. A new mobility guideline was initiated on the general intensive care unit (ICU) to maximise patient rehabilitation within the limitations of their RASS score.
Objective: The purpose of this evaluation is to establish whether the maximum level of rehabilitation/mobility was safely performed within each patient’s physical, medical and cognitive abilities.
Methods: A one day data collection point was taken on four consecutive months where every patient was assessed for the following: RASS/GCS at time of physiotherapy, contraindications to rehabilitation, highest level of rehabilitation delivered as per the mobility guideline, the type of rehabilitation/mobility performed and any comments. Data for contraindications to mobilisation, non-compliance, partial compliance and full compliance with mobilisation was collected and reported in a descriptive and tabular format.
Results: In November 40% of patients were contraindicated for mobilisation, 40% non-compliance and 20% partial compliance identifying that no patients achieved their target level of mobility. In December 38% of patients were contraindicated for mobilisation, 12% non-compliance and 50% full compliance identifying half the patients achieved their target level of mobility. In January 15% of patients were contraindicated for mobilisation, 15% non-compliance, 15% partial compliance and 55% full compliance identifying over half the patients achieved their target level of mobility. In February 35% of patients were contraindicated for mobilisation, however, 65% of patients were fully compliant identifying further improvement in patients achieving their target level of mobility.
Conclusions: As the mobility guideline was implemented, considering the patients RASS/GCS, there was an improvement in the proportion of patients mobilised by physiotherapy to the maximum level indicated. Thus, causing the proportion of patients who did not receive appropriate mobilisation to reduce. This enhanced mobilisation also appeared to impact on sedation levels which progressively reduced during the 4 month data collection period. Implementing a mobility guideline seems to improve the maximum achievable level of rehabilitation. Sedation level, as measured by the RASS, or degree of consciousness, as measured by GCS, can limit the type of mobility possible but this does not need to be a barrier to mobility or patient’s rehabilitation.
0061
The management of sepsis at Amrita Institute of Medical Sciences and Research Centre (AIMS), a tertiary care centre in Kerala, India: a re-audit
Rosanna Stopford1, Craig Cadwallader2, Sanjeev Singh3, Vidya Menon3 and Sam George1
1George Eliot Hospital, Nuneaton, United Kingdom
2University Hospital Coventry and Warwickshire, Coventry, United Kingdom
3Amrita Institute of Medical Sciences and Research Centre, Kochi, India
Abstract
Sepsis is a major cause of mortality worldwide.1 Implementation of sepsis management bundles has been associated with reduced mortality but the compliance with these bundles varies across regions. Research from India suggests that compliance with bundles is poor.2,3
Following identification of a septic patient, the Surviving Sepsis Campaign (2016) recommends that within 3 hours (i). blood cultures are obtained prior to administration of antibiotics, (ii). broad spectrum antibiotics administered, (iii). lactate measured and iv. 30 ml/kg crystalloid given for hypotension or lactate ≥4 mmol/l.4 The 6-hour bundle relates to severe sepsis/septic shock and patients requiring escalation to the intensive care unit (ICU) and advises that within 6 hours i. vasopressors should be administered for hypotension (refractive to fluid resuscitation) to maintain MAP ≥65 and ii. CVP and ScvO2 measured when arterial hypotension persists despite volume resuscitation or if initial lactate ≥4 mmol/l and iii. lactate remeasured (if initially raised).4
This audit aimed to i. establish adherence to the 3- and 6-hour bundles as set out by the SSC at AIMS; ii. compare current practice against the previous audit in 2016 and iii. identify areas for improvement. A prospective re-audit was conducted in April 2018 as part of a Warwick Medical School student elective. In Accident and Emergency, adult patients meeting SIRS or qSOFA criteria were identified from medical records. Compliance with the 3- and 6-hour management bundles was recorded.
Eighty patients were included in this audit. The 3-hour bundle was completed within 3 hours in 32 (40%) patients and exceeded 3 hours in 43 (53.8%) patients. The 3-hour bundle was not completed in 5 (6.3%) patients. In the first 3 hours, 65 (81.3%) patients had a lactate measured, 64 (80%) patients had blood cultures taken before antibiotics were given and 46 (57.5%) received antibiotics. All patients (n = 12, 100%) requiring fluid resuscitation, received fluids within 3 hours.
Of 11 patients requiring ICU admission, there was a trigger for escalation in all patients. Three patients (27.3%) received all components of the 6-hour bundle within the required time. Lactate was re-measured (where appropriate) and fluid status reassessed in all patients. Two patients (40%) out of 5 with persistent hypotension received vasopressor support after 6 hours. The 2016 audit reported compliance of 23.6% (40% in 2018) to the 3-hour bundle and 66.7% (27.3% in 2018) to the 6-hour bundle.
Despite greater adherence to the 3-hour bundle since 2016, compliance remains suboptimal. The proactive management at AIMS took significant steps in healthcare education following the 2016 audit but reported difficulties related to high staff turnover, particularly nursing staff. Delays were also attributed to the formalities of payment. Recommendations included further healthcare education, the introduction of the NEWS score for early identification of the deteriorating patient and providing the first dose of antibiotics without procuring financial clearance. Although there is still room for improvement, the global literature highlights significantly poorer adherence to the bundles than those we describe and data for India is scarce.5 AIMS sets a new benchmark for the nation.
0062
Rheumatoid associated Cardiac Tamponade: An unusual cause of type 1 respiratory failure
Linda Skelly1, Tim Furniss1,2 and Laura Langton1
1Warrington Hospital, Warrington, United Kingdom
2Health Education England (North West), Merseyside, United Kingdom
Abstract
Background: Rheumatoid Arthritis (RA) is a chronic inflammatory disease, which affects approximately 1% of the population in the United Kingdom.1 Typically, RA affects the joints by causing an inflammatory synovitis predominantly within the peripheral joints, however it can also have systemic involvement such as pericarditis, pleuritis, interstitial lung disease and vasculitis.2 RA has been shown through echocardiographic studies to cause pericardial effusion in 50% of patients with nodules and, 15% of those without nodules, however <10% of patients are clinically symptomatic.3 There have been only very few documented cases cardiac tamponade associated with RA4 or disease modifying therapies such as Methotrexate.
Case Presentation: We report the case of a 43 year old male patient with a past medical history of seropositive RA and recurrent deep vein thromboses. The patient attended the emergency department with a four-week history of progressively worsening central pleuritic chest pain and tachypnoea associated with fevers. He had been initiated on methotrexate for RA four weeks earlier but this had been discontinued prior to admission due to concerns this was causing his chest pain. On examination, he appeared grey and clammy, was tachycardic and tachpynoeic with a type 1 respiratory failure on blood gas analysis. ECG demonstrated sinus tachycardia and chest x-ray showed an enlarged heart with left sided pulmonary consolidation. Initial bedside echocardiography identified a moderate pericardial effusion, but with no evidence of compromise and blood pressure had improved following a single fluid bolus; an initial diagnosis of chest sepsis was made and the patient was referred to critical care for respiratory support. Subsequent CT chest showed evidence of massive pericardial effusion and associated collapse of the left lung.
The patient began to develop cardiovascular instability concerning for evolving tamponade. Due to anticoagulation with apixaban (for previous thromboses), prothrombin complex concentrate was transfused in an attempt to reverse anticoagulation prior to emergency pericardiocentesis.
Ultrasound guided pericardiocentesis drained one litre of haemoserous fluid. Cardiovasular recovery was immediate with respiratory recovery over the next 24 hours. The patient was discharged from critical care at 96 hours and home after five days. Repeat echocardiogram two weeks later showed no evidence of recurrence of the pericardial effusion but did show biventricular impairment due to atrial fibrillation.
Conclusion: In this case, due to the high inflammatory markers and recent diagnosis of RA, an inflammatory cause of pericardial effusion was felt most likely, although differentials included malignancy, medication (such as Methotrexate), infective, hypothyroidism and collagen vascular disease. Cardiac tamponade resulting from RA-induced pericardial effusion is a rare but life-threatening complication which may present at any stage of the disease process, and is treated with pericardiocenteis. Cardiac tamponade may present atypically, insidiously with mass effect causing respiratory failure prior to cardiovascular collapse. Bedside echo therefore continues to be an essential tool in the evaluation of the critically ill patient.
0063
Choosing the size of tracheostomy tube for adults in UK intensive care units: how do we do it?
Helen Newman1, Anna-Liisa Sutt2,3,4 and Sarah Wallace5,6
1Speech & Language Therapy, Royal Free London NHS Foundation Trust, Barnet, United Kingdom
2Speech & Language Therapy, Barts Health NHS Trust, London, United Kingdom
3Critical Care Research Group, The Prince Charles Hospital, Brisbane, Australia
4Northside Medical School, University of Queensland, Brisbane, Australia
5Wythenshawe Hospital, Manchester University NHS Foundation Trust, Manchester, United Kingdom
6Chair RCSLT Tracheostomy Clinical Excellence Network, London, United Kingdom
Abstract
Background: Each year 12000 people in the UK receive a tracheostomy tube (TT) (1). TTs bring lifesaving benefits to patients, such as facilitating mechanical ventilation (MV), weaning from MV, providing a patent airway, and allowing access to remove pulmonary secretions (2). There are important risks associated with their use, however. The wrong size TT can lead to difficulty ventilating patients, accidental dislodgement, tracheal stenosis, tracheomalacia and the inability to communicate with concomitant psychosocial burden (1,3). Guidance on type of TT to use exists (2,4), however, there is currently little specific guidance on how to select the size of TT for adults. Anecdotally practice varies widely between sites. This study aimed to investigate current TT-size selection practices in the UK.
Methods: Data were collected at the Royal College of Speech and Language Therapists Tracheostomy Clinical Expert Network meeting in London, UK, in May 2019 using Mentimeter online voting software. Smaller data sets were collected in June 2019 from ICU-based doctors and nurses. Descriptive statistics were used to analyse the survey findings.
Results: Eighty-six clinicians completed the survey: 64 therapists (62 speech and language therapists, 2 physiotherapists); 14 doctors and 8 nurses. Differences were found between factors reportedly being used in practice to decide TT size versus factors clinicians reported should be used (see Table 1). 'What is in stock/closest to hand’ was a common factor used in decision-making (therapists and nurses 66%; doctors 33%). ‘Gender’ was the most frequently considered factor by doctors. All groups reported ‘patient size’ was and should be considered. Tracheal diameter was rarely mentioned as a factor used in practice (three respondents). Dimensions of TTs were compared on average 54% of the time when switching between brands. The frequency of marking optimal positions of adjustable flange TTs was 45%. Use of TTs without an inner cannula was less frequent (18%). The most commonly used TT brand was Portex (68%) followed by Tracoe Twist (63%) and Shiley (32%). Fifteen respondents reported a maximum TT inner diameter of less than 8 mm at their place of work. Twenty reported a minimum outer diameter of 10 mm or higher. Downsizing TTs was common and occurred twice as frequently as upsizing.
Conclusions: There is variation in UK practices relating to TT size selection. Factors that clinicians feel should be used to guide decisions are not always used in practice. Factors that are used are often subjective, non-specific or non patient-related. The range of TT sizes used at some sites may be inadequate and place some patients at risk. Future research should seek to provide evidence regarding which factors are valid in TT size decisions and has the potential to have an impact on tracheostomised patients’ physical and psychological outcomes.
Table 1.
Factors clinicians reported were or should have been used in TT size decisions.
| Frequency ranking | Used in practice | Should be used |
|---|---|---|
| 1 | Patient size | Patient size |
| 2 | Gender | Anatomy/trachea size |
| 3 | Availability/What's in the cupboard | Weaning |
| 4 | Consultant preference | Gender |
| 5 | Neck size | Secretions |
0066
Aneurysmal Subarachnoid haemorrhage (SAH) – Time for up-to-date clinical practice guidelines
Swapnil Patharekar1,2 and Sandeep Gudibande1,3
1Royal Preston Hospital, Preston, United Kingdom
2specilaity doctor in critical care, Preston, United Kingdom
3consultant in critical care, Preston, United Kingdom
Abstract
Background: SAH resulting from rupture of a Berry aneurysm is a condition associated with significant mortality and morbidity. Occurrence of delayed cerebral ischaemia (DCI) is one of the main reasons for unfavourable outcomes. Multiple strategies exist to prevent and manage DCI, most of which are based on low-quality evidence, except for beneficial effects of nimodipine. Fluid management remains a controversial area for this subset of patients. American Heart Association guidelines in 2012 suggested maintenance of euvolemia to prevent DCI.1 It is well known that fluid overload is harmful in critically ill patients. However, often patients receive excessive intravenous crystalloids in order to increase the mean arterial blood pressure (MAP). Our local guidelines suggest fluid input of 3 litres/24 hours in patients at high risk of DCI as well as in patients with established DCI. The rationale is to avoid hypovolemia and subsequent low cerebral perfusion pressure (CPP).
Objective: The main objective was to review fluid balance in patients admitted to critical care with aneurysmal SAH.
Materials and methods: We reviewed clinical records from 25 patients with SAH from march to October 2018. We recorded their daily and 72 hour fluid balance in addition to their demographics and clinical characteristics.
Results: We found 56% of patinets were SAH grade 1 and 2. While rest 44% were SAH grade 3,4 and 5. We found that nearly 75% of patients were in positive fluid balance at the end of 72 hours from admission to critical care, ranging from 503 ml to 5750 ml with an average positive balance of 2500 ml.
Of the remaining 25% of patients who were in negative fluid balance, one patient had diabetes insipidus.
Vasospasm (clinical and confirmed by Transcranial Doppler) occurred in 5 patients in positive fluid balance group and 3 patients in negative balance group Day 1, 2 and 3 average fluid balance were 2.5 ml, 1287 ml and 656 ml respectively.
Conclusions: Our audit demonstrated that most patients admitted to critical care with any grade of aneurysmal SAH, gradually become fluid overloaded over the first 72 hours of admission.
It also does not seem to prevent DCI for which it is mainly advocated. We appreciate that the small number of patients in our audit questions the validity of this particular conclusion. However, there is evidence that hypervolemia in these patients neither prevents DCI or has any role in its treatment.2 A recent trial did not find any benefit by augmenting MAP in these patients.3 In light of new scientific evidence in this field, new clinical practice guidelines are urgently needed with particular emphasis on cardiovascular management of this cohort of patients. Ongoing work will result in publication of guidelines in February 2021 by National institute of clinical excellence (NICE). It is hoped that issues such as volume status assessment and management, advanced cardiac output monitoring and augmented blood pressure are addressed in these guidelines.
0067
A multi-disciplinary Emergency Department RSI simulation programme: improving the safe application of RSI checklists and action cards
Brendan Spooner, David Balthazor, Tom Hawthorne, Ged Doyle and Richard Browne
University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Introduction: At least 1 in 4 major airway complications occurs in the ED or ICU and the majority during RSI (rapid sequence induction).1 Complications from RSI in ED are as high as 12%2 and consequently checklists for ED RSIs have been recommended.1 Education and training are essential to ensure the appropriate use and maximal benefit of an RSI checklist.3 This may reduce complications and improve patient safety.3 An ED RSI checklist/action card was introduced locally (see figure 1), however practical experience of its use is hard to gain safely.
Objective: To introduce a simulation programme that provides multidisciplinary team (MDT) exposure to the ED RSI checklist/action card in a safe and non-threatening environment.
Method: A high fidelity, real-time, MDT ED RSI simulation programme was introduced. Candidates have included intensive care doctors, anaesthetists, ED nurses and ACCPs. Faculty are ICU doctors, senior ED nurse educators, ACCPs and ED ODPs (operating department practitioners). Sessions run in a simulation centre for 4 hours every 6 weeks. Each session would typically include 2–4 ICU registrars and 6–9 ED nurses. The session includes a lecture on RSI, airway assessment (see figure 2), checklist/action cards; followed by 3 simulations of ED patients needing RSI. Simulations use manikins with real time observations. A doctor would work with 3 ED nurses and an ED medical team leader (faculty) for a 20 minutes simulation with 40 minutes for debrief. Qualitative and quantitative feedback is collected.
Results: Over 15 courses, 134 candidates have attended including 67 trained nurses (department size is approximately 100) and 35 doctors who might lead an ED RSI. Feedback has been excellent with 99.2% of candidates rating the course as good or excellent. Over 80% of candidates rated the content, faculty and course as excellent. 95% rated the resources and sim set up as good or excellent. 100% of candidates felt that course was relevant to them. In free text responses many candidates praised the MDT format and length of the detailed debrief, as well as comments about increased confidence with RSI. Informal feedback from the ED education team found that ED nurses felt more confident assisting for RSIs and this has led to an increased perception of good teamworking amongst the ED RSI team.
Conclusion: The introduction of an ED RSI simulation programme has received excellent feedback. By giving staff exposure to the complex skills needed to successfully perform ED RSI, it is hoped patient safety will be improved.
Figure 1.
ED RSI checklist/action card.
0068
The use of aquatic physiotherapy in the rehabilitation of the critical care population
Susan Calvert1, Matthew Quint1, Laura Papineau2 and Claire Jeffries2
1Academic Department of Critical Care, Portsmouth Hospitals NHS Trust, Portsmouth, United Kingdom
2Solent NHS Trust, Portsmouth, United Kingdom
Abstract
Guillain Barre is a demyelinating polyneuropathy which can lead to profound muscle weakness and respiratory failure thus can result in an extended Critical Care stay. Interventions during the plateau phase are focussed on maintenance and avoidance of secondary complications. During this phase, where the patient experiences feelings of loss of control and high levels of dependency on those around them, psychological symptoms such as depression and anxiety can be the most difficult to manage due to the inability to predict the recovery process.
To offer a Critical Care patient in the plateau phase of GBS a novel rehabilitation strategy of aquatic physiotherapy. This approach could provide a different sensory experience and a supportive (gravity eliminated) environment to improve physical and psychological health.
An extensive risk assessment and planning process was completed between the hydro and critical care therapists utilising guidance from the Aquatic Therapy Association of Chartered Physiotherapists. An appropriate number and skill-mix of staff members was arranged (this included 2 aquatic therapy specialists, 1 critical care therapist to manage the airway in the water, an airway trained doctor and 2 hydrotherapy technicians skilled in emergency pool evacuation); essential and back-up equipment was sourced and stored in plastic boxes to protect it from water damage. On initiating the planning process, the patient was ventilated via a tracheostomy. Two days prior to the planned session, the patient had been weaned off his ventilator but still had the tracheostomy as his primary airway. Evaluation was achieved by measurement of range of movement and patient feedback.
Th patient successfully completed a 15 minute introductory hydrotherapy assessment session with no adverse incidents. He was able to demonstrate a greater range of active movement in the water than had been possible on land. The patient reported a sense of freedom and thoroughly enjoyed the session. He went on to be decannulated and aquatic physiotherapy was continued as part of his rehabilitation program.
Aquatic physiotherapy based rehabilitation proved useful in this case. The value of this approach in the wider critical care population requires further formal assessment of the safety and potential benefits vs risks.
0071
A Silent World. Patients’ and carers experiences of an unplanned percutaneous dilatational tracheostomy (PDT) during the critical care episode: a qualitative study
Emma Addie1, Mary Cooke2 and Ged Dempsey3
1The University of Liverpool, Liverpool, United Kingdom
2The University of Manchester, Manchester, United Kingdom
3Aintree University Hospital NHS Foundation Trust, Liverpool, United Kingdom
Abstract
Introduction: Placement of percutaneous dilatational tracheostomy (PDT) has become common practice in critical care, with long-term mechanical ventilation being the most frequent indication. It is believed to reduce dead-space, decrease airway resistance, improve the removal of secretions, decrease the risk of aspiration and allows the patient to be conscious; PDT is also perceived to improve patient comfort. The purported benefits of PDT in critical care are well documented, but there is a disparity in the supporting evidence base. It remains uncertain as to what impact this intervention has on holistic perspectives of a critically ill patient and their carers; which is pertinent to patient experience and recovery.
Objectives: We aimed to explore the lived experience of PDT from a patient and carer perspective; intending to synthesise emotional effects of clinical outcomes, leading to a comprehensive understanding of varied experiences.
Methods: An interpretive phenomenological approach was used to inform sampling, indepth data collection and data analysis. Participants were identified post discharge from Aintree University Hospital NHS trust, prior to attending a critical care follow up clinic. A purposive sample of nine participants were recruited to the study, – six patients and three carers – who had experienced PDT during the critical care episode. Semi-structured interviews were conducted with the patient and/or carer, and were completed individually or as a dyadic interview. An in-depth inquiry illustrated, informed and understood experiences firmly anchored in participant stories. Data collection and analysis were undertaken simultaneously, so recruitment ceased when data saturation was achieved, for the development of the emerging concepts.
Results: A non-formal, inductive approach to data analysis was undertaken; which is indicative to interpretive phenomenology. As the data was coded, themes and essences were established, identifying three key themes of: a silent world, coping with communication, interactions with staff. Five sub themes of: initial memories, awareness and understanding, suction and blockages, nil by mouth, visualisations and hallucinations and perceptions of removal also became apparent.
Conclusion: Whilst patients accept tracheostomy as a treatment during critical illness, it is evident that patients do not find tracheostomy comfortable; the physical and psychological consequences of tracheostomy are tolerated to overcome critical illness. The findings suggest a disparity of care in the holistic sense, demonstrating capability and expertise in the physical management of PDT, but delivered with an absence of therapeutic association. Acknowledgement that patients and carers are faced with the unknown with PDT is essential; the fostering of meaningful, therapeutic relationships grounded in holistic care could lead to empowerment, and the ability to cope with illness, treatments and environment. Therefore, future study is warranted in this area to further understand how clinical decisions such as PDT insertion are made to enhance to patient centred care.
0072
An Assessement of the Management and Outcomes of Decompensated Cirrhosis in an Adult Critical Care Unit
James McCulloch1, Matthew Frise1 and Andrew Chadwick1
1The Royal Berkshire Hopsital, Reading, United Kingdom
Abstract
Introduction: Decompensated cirrhosis is a common medical presentation with a high mortality.1 It is defined as a patient with cirrhosis presenting with an acute deterioration in liver function. It normally manifests as jaundice, hepatic encephalopathy or gastrointestinal bleeding. Frequently there is a precipitating cause, and this must be investigated for. Historically, care for patients in the UK with decompensated cirrhosis has been suboptimal.2
Objectives: To assess the management and outcomes of patients presenting with decompensated cirrhosis in a large UK district general hospital before and during their critical care admission. We assessed compliance to the decompensated cirrhosis care bundle from the British Society of Gastroenterology (BSG).
Methods: We undertook a retrospective audit of patients admitted to the ICU with decompensated cirrhosis over 1 year (n = 13). Electronic records were assessed for their care within the following themes; investigations for decompensated cirrhosis, management of alcohol related complications, management of spontaneous bacterial peritonitis, management of gastrointestinal bleeding, management of hepatic encephalopathy and VTE prophylaxis. Further demographic and outcome data were collected.
Results: Most patients admitted to ICU with decompensated cirrhosis had alcohol related cirrhosis (85%). The most common manifestation of decompensation was variceal bleeding (38%) followed by hepatorenal syndrome (31%). Nine patients (69%) died in hospital, with six (41%) dying in ICU.
Investigating decompensated cirrhosis
5 patients (38%) had abdominal imaging to diagnose ascites requested within 24hours of admission. 5 patients (38%) had no blood cultures taken prior to ICU and 4 of these patients had no blood cultures sent within 24hours of ICU admission. Ten patients had ascites with 3 having an ascitic tap prior to ICU.
Management of alcohol related complications
31% of patients with a current alcohol history were not prescribed Pabrinex.
Management of spontaneous bacterial peritonitis
One patient had confirmed SBP and they were prescribed the correct antibiotics and intravenous human albumin solution.
Management of Gastrointestinal Bleeding
In all six cases of variceal haemorrhage terlipressin was prescribed with five patients also prescribed prophylactic antibiotics. All patients received an endoscopy within 24hours of presentation with 5 taken for endoscopy within 12hours. However, only a third of patients were administered vitamin K and half given FFP when indicated.
Management of Hepatic Encephalopathy
12 patients had hepatic encephalopathy and were prescribed lactulose. 39% had a CT brain to exclude other causes of decreased conscious level.
Venous Thromboembolism Prophylaxis
Three patients were prescribed LMWH with the all others having justified contraindications such as active bleeding.
Conclusion: Care for the critically unwell patient with decompensated cirrhosis is complex; moreover, they are a young patient population with a high mortality. To ensure high quality care the BSG has developed a clear bundle of best practice. Our results demonstrate varied compliance with this. In part this is due to a lack of awareness of the bundle, but also the complex nature of this population requiring a high number of investigations and actions. We will aim to present both our audit data collected here and the results of our ongoing education programme.
0073
A comparison of the use of the Intensive Care Psychology Assessment Tool with general and neuro intensive care patients
Stephanie Ashton1, Christopher Lambert2 and Jacobus Preller2
1Cambridgeshire and Peterborough NHS Foundation Trust, Cambridge, United Kingdom
2Addenbrooke's Hospital, Cambridge, United Kingdom
Abstract
The Intensive Care Psychology Assessment Tool (IPAT) is the only assessment tool which has been validated for use with intensive care patients. As part of an initial comprehensive development process, Wade et al. (2014) produced a measure with good psychometric properties for identifying patients suffering psychological distress whilst in the ICU, and promising properties for identifying risk of post-ICU depressive, anxiety and trauma related problems (Ibid. pp). From this initial work a cut-off point of 7 or higher has been established as indicative of in-ICU distress, and heightened risk of post-Hospital psychological disorders. However, its validation process did not include neuro-intensive care patients, a group similarly at risk of experiencing psychological distress (Kelly et al. 2016). As such it remains an open question as to the validity of using the IPAT with this patient group.
This study compares IPAT data from a general intensive care population with that from a neuro-intensive care population. Its subsequent predictive power regarding is analysed for each group.
IPAT measurements taken over an 18-month period on the ICU and Neuro Critical Care Unit (NCCU) of Addenbrooke’s Hospital were compared and descriptive statistics produced. Unpaired T-tests were used to compare the IPAT data from each patient group. The predictive capacity for each was further investigated using Fisher’s exact test in sub-samples comparing the association between IPAT risk prediction and subsequent measures of depression, anxiety and PTSD risk.
The unpaired T-test indicated that the IPAT scores taken on ICU were significantly higher (M = 7.73, SD = 4.22) than those taken on NCCU (M = 5.77, SD = 4.36), t = 4.1884, p < 0.0001.
| Descriptive Statistics: | |||
|---|---|---|---|
| On ICU | On NCCU | Overall | |
| Number of IPATs completed | 158 | 178 | 336 |
| Number of IPATs not completed (refused, patient too unwell, etc.) | 5 | 13 | 18 |
| Mean average of IPAT score | 7.73 | 5.769 | 6.69 |
| Median IPAT score | 8 | 5 | 6 |
| Number of IPATs scoring 7 or above | 92 | 63 | 155 |
| Mean average score for IPATs scoring 7 or above | 10.576 | 10.66 | 10.61 |
| Number of IPATs scoring 6 or below | 66 | 115 | 181 |
| Number of IPATs scoring between 7 and 13 | 77 | 49 | 126 |
| Number of IPATs scoring between 14 and 20 | 15 | 14 | 29 |
| Fisher’s exact test | ||
|---|---|---|
| Condition | Former ICU patients | Former NCCU patients |
| IPAT v HADS_Anxiety | N = 29, P = 0.3383 | N = 18, P = 0.2507 |
| IPAT v HADS_Depression | N = 29, P = 1.0 | N = 18, P = 0.6305 |
| IPAT v PAS_PTSD | N = 20, P = 1.0 | N = 15, P = 0.2821 |
The results could suggest the IPAT is more sensitive to detecting psychological distress in patients on ICU than those on NCCU. This is possibly because the psychometric properties of this measure were not developed using NCCU patients, and it thus may miss some of this group’s important early risk factors.
Analysis of the contingency tables did not indicate any significant association between IPAT score on either unit and subsequent risk of psychopathology. This might be because data was only available from a subsequently treated sub-group rather than the entire original sample. As such it’s not possible to comment from these results on the relative predictive value of the IPAT with either patient group.
These results are critically discussed.
0075
Evaluation of the use of Neuron Specific Enolase as a biomarker of Severe Brain Injury in multimodal Neuroprognostication
Siobhan Stacey1, David Hepburn2, Katy McGillian1 and Megan Prosser1
1Cardiff University, Cardiff, United Kingdom
2Aneurin Bevan University Health Board, Newport, United Kingdom
Abstract
Due to the complicated nature of severe brain injury, forming a prognosis can be difficult and major decisions need to be based on the patient’s prognosis, such as the decision to withdraw life sustaining treatment (WLST). Therefore, there is an increased importance placed on best practice in neuroprognostication. This helps to guide further care, provide the best outcome for these patients and minimise distress to families. Neuron specific enolase is an enzyme released in brain injury1,2 and is currently used as a quantitative biomarker of brain injury3 to identify potential survivors and to ensure that life sustaining treatment is not withdrawn in these cases.
The study aimed to evaluate the role of NSE in multimodal neuroprognostication, the number of modalities used and the prognostic value of each investigation in justifying WLST, in addition to identifying the time from ICU admission to the formation of a reliable prognosis of severe brain injury (neuroprognostication time).
Manual analysis of 31 patients’ notes with suspected brain injury, identified using the ICNARC database between 1st January 2018–19th April 2019: 17 patients before the introduction of NSE (pre-NSE group), 14 patients who had NSE sampled (NSE group).
There was a prolonged average neuroprognostication time (6.92 days) in the NSE group compared to the pre-NSE group (2.33 days). The introduction of NSE resulted in a more multimodal approach as is recommended in guidelines4: 3.64 modalities were used on average in the NSE group compared to the average of 2.12 modalities in the pre-NSE group. NSE was found to be the most useful prognostic indicator of poor outcome as it indicated a poor prognosis in 64.29% of cases, followed by CT (51.61%), EEG (40%) and then MRI (28.57%). Furthermore, most major prognostic decisions were made following the return of NSE results. Consequently, this could indicate the importance of the role of NSE in providing diagnostic certainty to inform major decision making and to reduce distress to families.
0076
Virtual Reality in Critical Care – a feasibility study
Ceri Lynch and Gemma Jones
Cwm Taf Morgannwg University Health Board, Llantrisant, United Kingdom
Abstract
Patients in Intensive Care Units (ICU) frequently experience low mood, anxiety and fear.1 These symptoms are often a result of feeling vulnerable, lacking in stimulation or from an inability to relax and sleep. Anxiety also detrimentally affects perceived levels of pain and motivation for rehabilitation.2 Family members also experience depression, anxiety and fatigue during a relative’s ICU admission3 and ICU staff report anxiety, stress and burnout.4
Recently, there has been interest in virtual reality (VR) as a tool to improve outcomes in a variety of clinical settings. Non-immersive VR has shown clinical utility in reducing perioperative anxiety. With recent technological advances, immersive VR may be even more promising with studies citing beneficial clinical effects.5 Immersive VR involves the use of goggles and earphones to enable the user to see and hear a different world all around them, allowing complete distraction from reality.
To date, the use of VR has not been investigated in the management of stress, anxiety and pain in the critical care population. This is a group of patients who often suffer high anxiety levels, affecting their sleep and their quality of life. If there is a safe, non-pharmacological intervention that can help these patients to feel more relaxed and comfortable, it could be invaluable. The study aims to explore the feasibility of using VR with patients, relatives and staff in ICU and seek feedback from users about their experience.
Patients, relatives and staff members will be screened by members of the study team and those eligible will be offered the opportunity to try a VR experience. Eligibility criteria are: adults with capacity to consent. Exclusion criteria are: unable to consent, epilepsy with seizures triggered by lights, severe head or facial injury meaning the VR kit would not fit properly.
After informed consent, the user chooses from a selection of VR experiences, each lasting 7.5 minutes. Examples include: an underwater experience; a nature walk and a guided relaxation. Data collected will be in the form of visual analogue scales to assess pain and anxiety before and after the virtual reality experience and free text verbal quotes. If the VR is being explored for the effect on sleep, the length and quality of overnight sleep will be recorded the following day. If patients request repeated use of the VR equipment, this will be permitted and data from second or subsequent uses will be recorded as such.
Study ongoing and results to be presented at conference. Recruitment target is at least 50 uses of VR in a minimum of 25 patients.
VR is a new technology that allows users to immerse themselves in a different experience. This distraction can be beneficial for anxiety and stress. It will be interesting to explore whether VR is a feasible tool to use in ICU and whether these benefits are applicable to a population of critically ill patients, staff and relatives.
This study is ongoing and will be completed in time to present at the conference.
0077
Patient characteristics and outcomes amongst adults in ITU undergoing a protocolised spontaneous breathing trial in the context of randomised controlled trial examining the use of non-invasive ventilation to facilitate early liberation from ventilation
Thomas Abberton1 and Gavin Perkins2
1University Hospitals Birmingham, Birmingham, United Kingdom
2University of Warwick, Warwick, United Kingdom
Abstract
Prolonged invasive mechanical ventilation is associated with increased morbidity and mortality.1 International clinical practice guidelines suggest a stepwise approach to weaning. A spontaneous breathing trial (SBT) is the major diagnostic test to determine whether patients can be successfully extubated.2 Within the UK, Continuous positive airway (CPAP), T-piece and Pressure support (Psupp) are used to test a patients ability to breathe spontaneously prior to extubation.3
The objective was to assess patient characteristics and outcomes in patients who pass or fail a SBT using CPAP, T-piece or Psupp.
This prospective cohort study took place in the context of the Breathe Trial.4 Eligibility criteria were adult patients who had received invasive mechanical ventilation through an endotracheal tube continuously for more than 48 hours and ready to commence weaning. Continuous data analysed using linear regression models, adjusting for relevant baseline variables. Summary statistics were based on adjusted mean estimates and the 95% CI. P-values obtained using Chi-squared test and Fishers exact test. Categorical data analysed using logistic regression models, with the inclusion of important predictors to assess possible predictors of outcome. Statistical tests were 2-sided using P < .5 significance threshold. Statistical analyses performed using Stata version 15.1 (StataCorp).
Patients were recruited through March 2013 and October 2016 across 41 hospitals, with 1054 undergoing SBT. For most patients, pneumonia (35.7%) or post-surgical respiratory failure (21.4%) was the main reason for mechanical ventilation. The majority of patients passed a SBT (65%) with 35% who failed. The proportion of patients who failed a T-piece was 41/100 (41%) which was similar to the proportion who failed a CPAP SBT 186/545 (34%) OR 0.7 (0.48, 1.15) but lower than the proportion who failed a Psupp 119/390 (30%) OR 0.6 (0.40, 0.99). Factors associated with SBT failure on multi-variate analysis were height OR0.98 (0.97, 0.99), PaCO2 (KPa) OR 0.23 (1.09, 1.40), pressure support OR 1.08 (1.05, 1.12), PaO2 OR 0.94 (0.89, 0.99) exhaled minute volume OR 1.07 (1.02, 1.13) and respiratory rate OR 1.03 (1.01, 1.06). Amongst 690 patients who passed the SBT, 608 (88%) were successfully liberated, 81 (12%) experienced one of the composite outcomes of death, re-intubation or tracheostomy. During multi-variate analysis only haemoglobin OR 1.2 (1.07, 1.39), APACHE II score OR 0.97 (0.94, 0.99) and PaO2:FiO2 ratio OR 1.03 (1.01, 1.05) remained significantly with successful liberation when compared with composite outcomes.
This study found evidence of variation in the approaches used for conducting SBTs, with CPAP most frequently used, followed by pressure support, with T-piece least used. Two thirds of patients passed the first SBT. Patients with a SBT using pressure support were more likely to pass the SBT. SBT type did not influence the composite outcome of death, re-intubation or tracheostomy.
0078
The Perioperative Nutrition Screen (PONS), a novel and simple nutrition screening tool for adult elective major surgical patients, identifies patients at risk of malnutrition and a prolonged intensive care unit length of stay
Jatinder Pabla1, Gurinder Rayat2, James Otto2, Imogen Fecher-Jones2 and Denny Levett1,2,3
1General Intensive Care Unit, University Hospital Southampton, Southampton, United Kingdom
2Perioperative Medicine Team, University Hospital Southampton, Southampton, United Kingdom
3University of Southampton, Southampton, United Kingdom
Abstract
Malnutrition is independently associated with increased intensive care unit (ICU) length of stay (LOS), ICU readmission, infection, and mortality.1 Perioperative nutritional optimisation improves outcomes.2,3 However, nutritional screening is not routinely performed before major surgery in the UK and there is not consensus regarding the optimal preoperative nutritional screening tool. The Malnutrition Universal Screening Tool (MUST) is widely used in the UK. However, it is not a simple screening tool, takes time to calculate and is designed for use in hospitalised patients. The recently proposed Perioperative Nutrition Screen (PONS) is simpler to perform and designed to identify the preoperative patient at high risk of malnutrition.4 A MUST ≥ 2 or PONS positive score warrants patient referral to a dietician for nutritional assessment and optimisation (figure 1).
This study aimed to validate the PONS in elective major surgical patients against the MUST.
It is a single centre prospective observational study. Patients undergoing cardiopulmonary exercise testing as part of preoperative evaluation prior to elective major surgery were recruited over a 6-month period and followed up until hospital discharge post-surgery. Each patient was screened with PONS and MUST scores.
217 patients (mean age 67 years, 57.6% male) were admitted for elective major surgery. 27% were at risk of malnutrition. Lower GI, hepatobiliary and urology represented 70% of the patients.
If the MUST is considered the gold standard screening tool, then PONS had a sensitivity 97.1% (CI 84.7-99.9), specificity 83.2% (CI 76.6-88.7), positive predictive value 55.0% (CI 46.3-63.4), negative predictive value 99.3% (CI 95.1-99.9) and accuracy 85.6% (CI 79.9-90.2) in determining high risk of malnutrition (i.e. MUST ≥ 2).
Of the 27 (12%) patients who scored PONS positive but MUST negative 23 (85.2%) had a reduced dietary intake, 2 (7.4%) a low albumin (<30 g/L) and 2 (7.4%) both.
PONS negative patients had a shorter total hospital LOS (median 6 days, interquartile range (IQR) 4–9 days) than those who were PONS positive (median 8 days, IQR 6–12 days; p = 0.038). There was no significant difference in total hospital LOS when MUST 0 patients were analysed against the MUST ≥ 2 group.
PONS negative patients had a shorter ICU LOS (median 1 day, IQR 0–2 days) than those who were PONS positive (median 2 days, IQR 1–4 days; p = 0.004). MUST 0 patients had a shorter ICU LOS (median 1 day, IQR 0–2 days) than those who scored MUST ≥ 2 (median 2 days, IQR 1–5 days; p = 0.036).
Malnutrition is common in patients presenting for major elective surgery. PONS is a simpler tool than MUST to screen for patients at high risk of malnutrition. It has an excellent sensitivity, specificity and negative predictive value. PONS identifies a further subset of patients primarily with acutely reduced oral intake not identified by MUST. These patients are known to be at risk of malnutrition.4 Patients who score PONS positive should be referred for preoperative nutritional optimisation to reduce critical care and hospital length of stay as well as associated healthcare costs.
Figure 1.
Calculation and management guidelines according to MUST (left) or PONS (right).
0080
Feasibility of a comprehensive driving assessment to inform driving resumption following critical illness: an interventional cohort study
Chloe Apps1 and Joel Meyer2
1Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom
2Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Recovery from critical illness is often prolonged and challenging due to a combination of acquired physical, psychological and cognitive impairments.1 Resumption of driving is perceived as an important recovery milestone but it is estimated that only 68% of individuals return to driving at six months following hospital discharge. Returning to drive accelerates resumption of “normal life” including accessing hobbies, social activities and returning to work. Thus reducing avoidable delay to driving is vital in enhancing health-related quality of life following critical illness.
Objectives:
1 To determine the prevalence of driving-related impairments after critical illness
2 To measure driving status at 3, 6 and 12 months
3 To evaluate the acceptability and feasibility of the driving assessment and driving enablement interventions
Methods: This interventional cohort study will enrol adult intensive care survivors holding a UK category B (car) driving licence deemed at high risk of post-intensive care syndrome (>72 hours mechanical ventilation).
Participants (n = 80) will undergo an in-depth driving assessment at the two month time-point following hospital discharge. The driving assessment is a multi-disciplinary clinical and functional evaluation with accompanied on-road experience at a DVLA accredited driving assessment centre. This evaluation culminates in a comprehensive fitness-to-drive report. The primary outcome of the study is the prevalence of driving-related impairments. Secondary outcomes of the study are patient-reported driving status at 3, 6 and 12 months and acceptability and feasibility of the driving assessment and enablement interventions.
Participants will be followed up at 3, 6 and 12 months via the multidisciplinary Guy’s and St Thomas’ NHS Foundation Trust critical care recovery clinic. Qualitative experiential data will be captured through a driving diary and pre- and post- driving assessment questionnaires. An end-of-study half-day participant workshop will contextualise initial results and inform future work.
Analysis plan: Quantitative data including prevalence of driving impairments will be analysed with descriptive statistics. A time to event analysis of driving resumption delay will be done using Kaplan Meier. Regression analysis of clinical and demographic variables associated with driving outcome will also be performed. All qualitative data will be reported according to consolidated criteria for reporting qualitative research (COREQ)2 and analysed using thematic analysis methodology. Two researchers will independently classify and identify the themes before reaching agreement then undergo peer review by a third researcher.
Conclusion: Safe and early resumption of driving is key for enhancing quality of life after critical illness. Findings from this novel study will enhance the evidence base regarding survivorship and help towards establishing national guidance about driving resumption.
0082
Relocation of the Royal Papworth Hospital: planning and reflections of the road transfer of critical care patients
Rahul Herlekar1, Matthew Jones2, Bernadette Dear3, Jo-Anne Fowles3 and Alain Vuylsteke3
1School of Clinical Medicine, University of Cambridge, Cambridge, United Kingdom
2Judge Business School, Cambridge, United Kingdom
3Department of Anaesthesia and Intensive Care, Papworth Hospital NHS Foundation Trust, Cambridge, United Kingdom
Abstract
Background: Royal Papworth Hospital completed its move from Papworth Everard to the Cambridge Biomedical Campus on 7th May 2019. The move was staggered across departments, with the critical care unit relocating ten patients from bays to a single-room design in early May.
This case series examined two areas of the road transfer of the ten patients:
a. Logistical Operations
b. Patient Safety
Data was sourced from observational findings, staff discussions and medical records.
Case Presentation: Logistical Operations: A two-day transfer plan was made for the weekend of 4–5th May. However, two patients supported on ventricular-assist devices (VADs) awaiting heart transplant were transferred mid-week to ensure their availability for transplant at the new site. The transfer team consisted of a consultant intensivist, critical care transfer nurse, driver and additionally, a perfusionist for those patients on extracorporeal membrane oxygenation and VADs. Measures were taken to enable continuity of care in handover, an issue often cited in transfers (1):
i. Bedside nurses remained with their patients.
ii. The electronic medical record system was mirrored real-time at both sites.
To reduce the overall transfer time, two teams were used with staggered departures for the remaining eight patients (Fig. 1). Departures and arrivals were coordinated by a lead nurse on both sites.
When transfers ran ahead of schedule, it was determined all patients were to be moved on the first day, with each team successfully carrying out an additional run. The mean transfer time for the eight patients was 26.1 min ± 9.5 min for the 15.5-mile journey.
Patient safety: In order to systematically review patient status, a standardized form and pre-transfer checklist were completed: an effective and recognised safety measure (1). A VAD console was discovered to be vibrating abnormally in certain positions prior to the transfer of one patient. For safety, this was promptly replaced resulting in a short ten-minute delay in departure. Equipment issues are the most common source of incidents in critical care transfers (2). Moreover, transport arrangements should avoid disrupting the intensive care plan of a patient (3). Courtesy of this, a patient was weaned from mechanical ventilation as part of their ongoing management. The patient required some additional time to be stabilised and subsequently their transfer slot was adjusted to accommodate this. CAM-ICU scores are used to diagnose delirium in critically ill patients and have shown excellent reliability (4). It was initially thought a patient had become delirious on arrival at the new site, though on review, this patient and indeed no other patients had significant changes in CAM-ICU from baseline.
Conclusions: The success of the operation can be attributed to effective planning with room for flexibility, allowing all transfers to be completed on the first day, whilst not compromising routine care. The use of a dedicated team was in line with best practice (3). A limitation of this case series is that long-term endpoints such as length of stay and mortality are difficult to evaluate since the transfer represented a limited part of care.
Figure 1.
Schematic to show the initial schedule.
0084
A case study describing the use of Mechanical Insufflation: Exsufflation (MI: E) in an intubated and ventilated patient with high oxygen and positive end expiratory pressure (PEEP)
Rebecca Vokes and Zoe van Willigen
University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom
Abstract
Background: Acutely deteriorating patients admitted to the Intensive Care Unit (ICU) may require large amounts of sedation or neuromuscular blockade in order to manage their ventilation. These drugs can inhibit the cough reflex of an intubated patient which can lead to secretion pooling, atelectasis and respiratory tract infections, and may contribute to weaning failure and reintubation.1
MI: E has been demonstrated to be a possible treatment option to aid secretion clearance in patients with an endotracheal tube2 or tracheostomy.3 Recently, Moses et al4 produced a practical guideline for the application of MI: E with intubated patients and recommends a PEEP above 10 as a precaution for treatment. Alongside this, the therapy team at University Hospital Southampton (UHS) NHS Foundation Trust have produced a local standard operating procedure for the use of MI: E which has been adapted for the complexity of the caseload. At UHS, MI:E is being increasingly used to augment secretion clearance with patients who are requiring high levels of oxygen and/or PEEP and the following case study is presented to demonstrate the scope of MI:E treatment with this patient group.
Case Presentation: The patient was a 24 year old female, normally fit and well, admitted to the ICU with aspiration pneumonia. The patient was ventilated via a controlled mode with an initial fraction of inspired oxygen (FiO2) of 0.90 and a PEEP of 15. The patient had to be paralysed with atracurium and therefore had no cough reflex. MI: E was used with an insufflation pressure of +40cmH20 and an exsufflation pressure of – 45cmH20. Closed suctions were completed to coincide with the application of the exsufflation pressure.
Copious thick mucopurulent secretions were cleared with the treatment. Within 12 hours of the treatment commencing, the oxygen requirements were weaned to FiO2 0.45 via the ventilator. Arterial blood gas (ABG) results also demonstrated improved ventilation (Table 1). At 48 hours the patient had been extubated and was self-ventilating on room air and stepped down to a medical ward.
Conclusions: This case study is an example of patients who have benefitted from the use of MI: E on ICU, In our experience, MI: E appears to be a safe and feasible treatment option for intubated and ventilated patients requiring high oxygen requirement and/or high PEEP. We have seen no significant adverse events with the use of MI: E with this group of patients. More investigation is warranted to evaluate this further.
Table 1.
ABG results pre and post physiotherapy treatments.
| Physio Treatment session | Time after intubation (hours) | PEEP | FiO2 | pH | PCO2 | PO2 |
|---|---|---|---|---|---|---|
| Prior to 1st treatment | 3 | 15 | 0.90 | 6.980 | 12.8 | 11.6 |
| After treatment one | 4 | 15 | 0.90 | 7.091 | 10.6 | 11.1 |
| After treatment two | 9 | 12 | 0.85 | 7.252 | 6.47 | 14.8 |
| After treatment three | 12 | 12 | 0.45 | 7.343 | 5.03 | 11.4 |
0085
Pilot Study of Occupational Therapy Input Into Critical Care
Helen Turner, Emma Jackson and Nicola Williams
Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
Abstract
Introduction: Critical illness can have catastrophic and long-term consequences for survivors. Physical, cognitive and psychological impairments can result in reduced health-related quality of life which persists for many years following hospital discharge. In recent years the importance of survivorship, has been increasingly recognised. Early rehabilitation has been identified as improving outcomes, key to this is Allied Health Professionals (AHP) input into critical care. National guidance (NICE 83) and GPICS standards have highlighted the importance of Occupational Therapy in Critical Care.
Objective: The purpose of the pilot was to demonstrate the effectiveness and highlight the role of Occupational Therapy in critical care.
Methods: We introduced for a 3 month period a band 7 occupational therapist (OT) working over 5 days as part of the existing work force. Outcomes were assessed using the ausTom and IPAT measures. Opinions of staff within critical care were collated via a questionnaire before and after the pilot. In conjunction with the rehabilitation co-ordinator appropriate referrals were identified to provide an integrated approach to rehabilitation. Data was collected and reported in a descriptive and tabular format.
Results: 43 sessions were delivered to the critical care department enabling sixteen patients to be seen. Average clinical time with the patients was 3.5 hours. Length of time on case load ranged between 1–20 days. Twelve interventions were provided the most common being personal care and sitting balance. The ausTOMS was completed with 10 patients. 100% of patients improved or maintained within the functional areas measured. 100% of patients receiving intervention for upper limb use improved. 70% of patients involved in self-care improved. 67% of patients were identified as being at psychological risk with 40% receiving interventions to support this. 83% of patients decreased score following support. 100% improvement in symptoms was reported.
80% patients reported being extremely satisfied with the overall care received by the OT and 80% reported being extremely likely to recommend the service to friends and family if required.
Staff questionnaires identified: 36% were aware of a role of OT prior to the pilot; 93% reported that the role of the OT helped in the rehabilitation of patients and improved the functional state of patients; 57% recognised the impact OT can have on patient cognition; 21% recognised the uniqueness of the role in contrast to the existing professions; 79% felt their patient would have benefitted from more OT input.
Conclusion: The evaluation of the study indicated that the team reported an increased level of understanding of the role of OT and recognised benefits to the patients. The outcomes of the intervention all indicated functional improvement made by all patients both physically and psychologically. These results indicate the necessity of the role of OT for patients experiencing critical illness which may be limiting their functional, cognitive and psychological recovery.
0086
Calorie provision from citrate anticoagulation in Continuous Veno-Venous Hemofiltration (CVVHF)
Alice Rogers and Bethan Jenkins
General Intensive Care Unit, University Hospital Southampton, Southampton, United Kingdom
Abstract
Introduction: Citrate is used as a regional anticoagulant for continuous veno-venous haemofiltration (CVVHF). It is metabolised in the krebs cycle and provides 0.59 kcal/mmol.1 Previous studies have hypothesised CVVHF with citrate provides up to 1300 kcal/day dependent on the anticoagulant and replacement solutions used.1,2,3 It is important that the calorie load from citrate is established as overfeeding the critically ill has been found to lead to increased risk of morbidity and mortality.4,5
Objective: To establish the average calorie load and the variability in calorie provision from citrate anticoagulation in an adult general intensive care unit (ICU).
Methods: Anonymised clinical data was recorded on 20 consecutive patients admitted to our ICU between April and July 2018, who were commenced on citrate CVVHF. Clinical data recorded included; patient demographics, filter settings including blood flow, filtration factor, citrate dose and time on filtration daily. Patients were excluded if they were receiving CVVHF for less than two days. The citrate calorie load was defined as the difference between the citrate in the filter circuit and the removal by CVVHF. An equation derived from data in Oudemans-van Straaten’s 2012 paper2 was used to calculate calorie load from citrate.
Results: 20 critically ill patients were filtered for treatment of a new acute kidney injury; the mean age was 66 years; 65% male. Patients were on HF for a mean of 3.7 days (range 1–18). Mean duration of continuous renal replacement therapy was 20 hours per day (range 5–24). Mean filtration fraction, citrate dose and blood flow were 30%, 3 mmol/L and 123 ml/minute respectively. A mean of 9.5 ± 1.7 calories per hour were provided from citrate; with a mean daily calorie load of 196 ± 69 kcal.
Conclusions: CVVHF with a tri-sodium citrate solution provided an additional 196 ± 69 kcal per day in our patient group. The calorie load from citrate CVVHF should be calculated regularly as changes in filter settings can have a significant impact on calories provided. This calorie burden from citrate will necessitate alteration of feeding regimens to prevent overfeeding of calories whilst ensuring adequate protein and micronutrient delivery.
0087
Single centre experience of High Frequency Percussive Ventilation (HFPV) in patients admitted to ICU primarily for pulmonary infections
Bram Keunen1, Martijn Rongen2, David Schramme1, Margot Vander Laenen1 and Willem Boer1
1Ziekenhuis Oost-Limburg, Genk, Belgium
2AZ Klina, Brasschaat, Belgium
Abstract
Introduction: In HFPV (VDR-4, Percussionaire, Sandpoint, Idaho), high frequency oscillatory diffusive ventilation is superimposed on conventional tidal volume convective ventilation. HFPV, as distinct from HFOV, which has fallen out of favour, has been used in our centre as a rescue therapy in patients with respiratory (and ventilatory) failure for a number of years. Benefits include enhanced oxygenation and hemodynamics as well as alveolar recruitment.
Objective: Evaluation of HFPV in patients admitted to ICU primarily for pulmonary infections.
Methods: After permission from the local ethics committee, a retrospective observational study of data was performed.
Results: From 2009 until January 2018, 26 patients (male 17, female 9) on conventional mechanical ventilation, admitted primarily for pulmonary infection, were treated with HFPV (out of a total of 140, 19%). Mean age was 62 (±13.9) years in survivors and 67 (±11) years in non-survivors (p = 0.07). Overall median SOFA was 7.5 (4–13), median APACHE II 24 (16-32). Eleven (42%) patients suffered from chronic lung disease (no difference in survivors vs. non-survivors). One of 26 patients (4 %) was switched to ECMO, 2 out of 26 (8%) developed pneumothorax. Median PaO2/Fio2 ratio (mPFR) before switch to HFPV was 71 (53-87), 2 hours after it was 112 (68-166) (p = 0,006). mPFR after 24 hours was 206 (108-226) (compared to 2 hour value p = 0.001). Despite a significant improvement after initiation of HFPV, mPFR did not predict survival at any time. Survivors spent a median of 3 (2–24) days on conventional ventilation before VDR, a mean of 4.2 (±2.9) days on HFPV, and a median of 23 (9.5–29) total days on ventilation. There was a mean of 35 (±17) days on ICU and mean of 53 (±25) days in the hospital for survivors. 28-Day mortality was 46% (12/26), survival to discharge from hospital was 50% (13/26).
An APACHE II score of 24 in pulmonary infection predicts a mortality of 49.7%. However, expected hospital mortality for the SOFA score was 30%. A comparison of ECMO vs. conventional ventilation for ARDS (muscle relaxants, prone positioning, recruitment manoeuvres, NO) and similar PFR values, in a younger population (mean 56), demonstrated a 60-day mortality of 35% vs 46%, at 90 days of 37 vs 47%. Another study comparing prone vs conventional, with PFR < 150 demonstrated a mortality of 23% vs 41%, benefiting prone.
Conclusion: Based on the negative findings from this study, a standardised ventilation protocol favouring prone positioning and ECMO, has been implemented in our centre.
0088
Out of Hospital Cardiac Arrests and Under-Prediction of Mortality: A Case of Simpson’s Paradox?
Josephine Gordon1 and Neil Hall2
1Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
2United Lincolnshire Hospitals NHS Trust, Lincoln, United Kingdom
Abstract
Introduction: The Lincolnshire Heart Centre (LHC) opened in 2012 providing Percutaneous Primary Coronary Intervention (PPCI) to Lincolnshire.
Survival to discharge for ventilated non-traumatic out of hospital cardiac arrest (OOHCA) has improved from 8% to 51%. A pathway with intensive care exists such that when cardiology accept a patient intensive care guarantees an ITU bed without prior arrangement. This ensures short ‘call to balloon’ times. Counter-intuitively this has produced an increase in our risk-adjusted acute hospital mortality.
Approximately two-thirds of all patients admitted to ICUs after OOHCA die from Hypoxic Brain Injury (HBI).1 Our concern is that in patients with proven HBI the predicted mortality was an underestimate due to the delivery of a physiologically stable patient to the ICU. This leads to a low ICNARC physiology score and a under-prediction of mortality.
Simpson's paradox is a phenomenon in probability and statistics, in which a trend appears in different groups of data but disappears or reverses when groups are combined. We conjecture the ‘poor’ mortality result would be reversed by the removal of the patients with confirmed irreversible hypoxic brain injury which had occurred at the time of cardiac arrest.
Objectives: To identify which patients admitted to the Adult Intensive Care Unit (AICU) in Lincoln, following an Out-of-Hospital Cardiac Arrest (OOHCA), went on to have a confirmed, severe HBI as a direct result of their initial cardiac event.
Then to examine the effect of retrospectively excluding these patients from the overall predicted mortality data for the AICU on the basis that they had no prospect of meaningful recovery and so will skew predicted mortality data. It is our expectation that excluding this group will likely make our survival data better by excluding patients whose physiological parameters during the first 24 hours produced a low predicted mortality but had no prospect of a good outcome.
Methods: We examined the ICNARC database and patient notes. All 48 OOHCA patients from 2017 were included. Predicted mortality and actual mortality for the groups were calculated. Severe HBI leading to withdrawal of life sustaining therapy was based on a multimodal approach of MRI, EEG and clinical findings. No patients had an episode of hypoxia or hypotension causing HBI post their cardiac arrest. There were 48 OOHCA patients during 2017: 25 survived to hospital discharge, 23 died on ICU of which 12 had proven HBI.
Results:
| Patient Group | Mortality |
|---|---|
| Actual Group | 47.9% |
| Predicted Group | 42.18% |
| Actual Non-HBI | 30.5% |
| Predicted Non-HBI | 39.47% |
Conclusions: This shows a reversal of performance outcome after the patients with HBI are excluded. Instead of an excess mortality between actual and predicted of 5.72% there was a reduction in mortality of 8.97%. The higher the difference between the observed and expected mortality the higher the impact on the risk-adjusted acute hospital mortality.
We suggest that there is an argument for excluding patients with an outcome which cannot be influenced by the ICU admission, such as HBI sustained during an OOHCA, similar to patients admitted for organ donation alone are excluded from the ICNARC mortality analyses.
0089
Predictive value of measuring Brachial artery reactivity in septic patients
Ahmed Mohamed1, Walid Omar2, Kamel Abd aziz2 and Hatem Alazizi3
1kings college hospital, london, United Kingdom
2cairo university hospital, cairo, Egypt
3cairo university hospitals, cairo, Egypt
Abstract
Background: Endothelial dysfunction plays a major role in the pathophysiology of septic shock and organ dysfunction and has been suggested to be a predictor of mortality in sepsis. Ultrasound measurement of brachial artery reactivity in response to stagnant ischemia provides estimates of endothelial function(1).
Objective: To assess whether brachial artery reactivity correlates with outcome of patients with sepsis or not and to compare its prognostic value with C – reactive protein (CRP) and Microalbuminuria.
Methods: Fifty Septic patients were subjected to flow mediated dilatation (FMD) of brachial artery within 24 hours from ICU admission. Measurements were compared in sepsis survivors versus non-survivors. Microalbuminuria and CRP values were obtained also for patients that fulfill criteria of sepsis. Thirty healthy volunteers were taken as a control group to determine a normal reference range for FMD.
Results: Hyperemic Velocity (HV) was significantly lower in sepsis group versus control group (71.77 ±18.67 versus 81.64 ± 9.84, p 0.003). FMD was significantly lower in sepsis group in comparison to control group (3.72 ± 2.22 versus 5.29 ± 1.74, p 0.001). Change in Velocity was significantly lower in sepsis group as compared to control group (19.53 ± 10.80 versus 31.25 ±6.72, p < 0.001). Twenty percent of enrolled patients died within 28 days of hospital admission. Change in Velocity was significantly lower in non-survivors versus survivors (7.82 ± 2.26 versus 22.45 ± 10.081, p = 0.001) respectively. Microalbuminuria was significantly higher in non-survivor in comparison to survivors (54.00 ± 19.24 versus 30.33 ± 44.92, p = 0.006).
Conclusion: Brachial artery hyperemic change in blood velocity is a noninvasive indicator of microvascular function that independently predicts mortality in sepsis. In contrast, brachial artery flow-mediated dilation was not associated with mortality in our sepsis cohort.
Keywords
Brachial artery reactivity, hyperemic velocity, FMD, microalbuminuria, Sepsis
0091
‘An audit of QTc intervals and associated factors for emergency and elective patients admitted to the Neurosurgical Intensive Care Unit (N-ICU)'
Jonathan Hughes and Simon Raby
Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Abstract
Introduction: An admission electrocardiogram (ECG) is a vital screening tool for patients admitted to any intensive care unit (ICU). Patients admitted to the N-ICU often have medical reasons for prolongation of the corrected Q-T interval (QTc), for example raised Intra Cranial Pressure (ICP) and Sub-Arachnoid Haemorrhage (SAH). Furthermore, they often present with modifiable acquired causes for a prolonged QTc interval, such as hypothermia, hypokalaemia, hypomagnesaemia and newly introduced medication.
Prospective data of assessment of prolonged QTc intervals have shown an incidence of between 24–61% of patients admitted to general ICUs.1 Furthermore, QTc prolongation may be associated with an increased mortality2and severity of critical illness.
Following a critical incident on the N-ICU in 2017, with the development of an episode of 'Torsades de Pointes' in a patient with a prolonged QTc, we decided to assess patient QTc on admission to our unit. If prolonged, we then assessed the electrolyte levels and drug prescribing in this patient cohort as well as assessing staff recognition and the development of adverse events over the first 48 hours.
Methodology: Single standardised data capture form designed in advance of the audit.
Data entry on admission to the NICU over a four-month period in 2018.
Initial audit looking at whether an ECG was performed and if performed, was there any abnormality of QTc interval documented and acted upon.
Further data collected on patient age, sex, emergency or elective admission type and primary cause for admission.
If QTc was prolonged, we proceeded to a retrospective assessment of electrolytes and prescribing of drugs onto the electronic drug chart. Further assessment of whether a second follow up ECG was performed and subsequent QTc intervals.
Results: 79 patients were audited over the four month period.
The average patient age was 54.9 (range 22–81). 50 males and 29 female patients were included in the audit.
The three most common primary reason for admission included 22.7% with Sub-Arachnoid Haemorrhage, 21.5% with Intra-Cerebral Haemorrhage and 17.7% of patients with Traumatic Brain Injury.
The average QTc on admission was 455 with a range of 371–594 ms.
A total of 15/50 (30%) males and 17/29 (58.6%) of female patients had a prolonged QTc interval on admission to the intensive care unit.
There were a variety of drugs prescribed in the first 24 hours of admission that may have contributed to a risk of prolonging the QTc interval in patients with a documented long interval on admission. The most commonly associated drugs were;
• Metoclopramide.
• Erythromycin.
• Olanzapine.
• Ondansetron.
The average Mg2+ level on admission in patients with long QTc intervals was 0.89 and the average K+ level was 3.6.
Discussion: There are a variety of risk factors associated with prolonged QTc interval on admission to the N-ICU. The syndrome is common and often under-recognised. If left unmonitored there is a risk of deterioration to polymorphic ventricular tachycardia. The incidence on the N-ICU is more common than previously reported figures and may relate to the spectrum of disease presenting to a specialist neurosurgical intensive care unit.
0092
Case study: flaccid quadriplegia post-traumatic spinal injury: an unexpected therapeutic dilemma
Peter Lynas1, Benjamin Simpson1 and Emma Jackson2
1Royal Preston Hospital, Preston, United Kingdom
2Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
Abstract
Introduction and Objective: Guillain-Barré syndrome (GBS) is an inflammatory demyelinating polyneuropathy characterized by areflexic paralysis. This case examines an overlap with acute traumatic spinal cord injury, and the clinical implications where these two diagnoses co-exist.
Method: We describe the case of a 54-year-old man with a past medical history of ankylosing spondylitis. He was admitted to critical care after a fall resulting in stable C6 and T8, and unstable L5/S1 fractures, for which he required surgical stabilisation. Pre-operatively his neurology demonstrated a picture consistent with a C6 spinal cord lesion.
Despite surgical intervention, the patient’s neurological status declined progressively over a period of weeks. Diaphragmatic and shoulder function diminished (MRC grade 3 to 0), with near complete loss of cranial nerve function. Lateral eye movements were maintained. Alongside increasing confusion and delirium, it became impossible for him to communicate.
The patient also exhibited features of autonomic instability with significant bradycardias and periods of hypotension. Critical illness neuropathy did not fully explain these findings and a neurology opinion obtained. Lumbar puncture and electro-encephalogram results were consistent with a diagnosis of GBS and nerve conduction studies further categorised this as an AMSAN variant.
Results: Over a period of two months the patient was given two trials of intra-venous immunoglobulin [IVIG]. These had minimal effect, only facilitating improvements in eye and tongue movements. He was unable to demonstrate any progress along the local (Southport) spinal weaning protocol.
After three months of ventilation, the patient failed to make any further clinical improvement and it was deemed a treatment failure. Following a best interest meeting the decision was made to commence palliative care and the patient subsequently died.
Conclusion: GBS has rarely been noted as a post-traumatic phenomenon head injury1 and spinal injury.2 Alongside trauma its prognosis is usually poor.3 However, reports have shown potential for a functional neurological improvement over a period of months with GBS therapy.4 For our patient, the co-existence of a C6 spinal cord injury and GBS prevented clear assessment of capacity, rehabilitation potential and prognostication.
Conclusion: Trauma is rare but recognised cause of GBS; it is appropriate to commence IVIG or plasma exchange therapy as reversibility is possible and may facilitate a patient-led decision process.
0093
Administration of intraoperative low dose morphine during cardiac surgery significantly reduces time to extubation
Sashini Iddawela1, Priyantha Dissanayake2, Gunarathne Dissanayake2 and Nuwan Jayaweera2
1University of Birmingham, Birmingham, United Kingdom
2Department of Anaesthesiology, Teaching Hospital Kandy, Kandy, Sri Lanka
Abstract
Introduction: Morphine based cardiac anaesthesia has shown superior recovery compared to alternatives (1, 2). However, its effects on haemodynamic instability and respiratory depression are well documented, particularly in higher doses (3). There is no research on intraoperative dosing of morphine and effect on extubation, pain and ICU stay.
Objective: To determine associations between dose of IV morphine and time to extubation, pain score at extubation and ICU stay after cardiac surgery.
Methods: Patients undergoing cardiac surgery at a major tertiary care hospital in Kandy, Sri Lanka between 2015 and 2018 were prospectively recruited into a randomised study and allocated into high dose (0.6 mg/kg) and low dose (0.2 mg/kg) groups. Allocation was blinded. Demographics such as age, sex, height and weight were collected. Intraoperative variables including cross clamp time, cardiopulmonary bypass time and continuous monitoring of heart rate and blood pressure were recorded. Postoperative variables collected included time to extubation, pain score at extubation and ICU stay. Early extubation was defined as a duration of less than 6 hours, as per Society of Thoracic Surgeon guidelines (4). Pain at extubation was determined using a visual analogue scale. Intergroup differences were assessed using the independent samples T-test for continuous variables and Chi2 for categorical variables. Multivariate binary logistic regression was used to determine the association between dose of morphine and an early extubation.
Results: One hundred and ninety patients were recruited, 95 into the high dose arm and 95 into the low dose arm. Patients in the high dose group were more likely to be older (57 years compared to 53 years, p = 0.012), with no other significant intergroup differences. Time to extubation was significantly shorter in the low dose group (431 minutes compared to 511 minutes, p = 0.001). Multivariate regression demonstrated dose of morphine was an independent predictor of early extubation (OR 2.139, 95% CI 1.059 – 4.320, p = 0.03). Median pain score at extubation did not differ significantly between the groups (p = 0.731), nor did ICU stay (p = 0.549).
Conclusion: Administration of low dose IV morphine during cardiac surgery significantly reduces time to extubation, potentially reducing ventilator-induced complications, costs and improve clinical course in intensive care.
0094
EEG Correlates of Self-Managed Neurofeedback Treatment of Central Neuropathic Pain in Chronic Spinal Cord Injury
Aleksandra Vuckovic1, Manaf Kadum Hussein Altaleb2, Matthew Fraser3, Ciarán McGeady1 and Mariel Purcell3
1Rehabilitation and Assistive Devices, Biomedical Engineering Division, School of Engineering, University of Glasgow, Glasgow, United Kingdom
2Faculty of Electrical Engineering, Wasit University, Wasit, Iraq
3Queen Elizabeth National Spinal Injuries Unit, Queen Elizabeth University Hospital, Glasgow G51 4TF, United Kingdom
Abstract
Background: Neurofeedback (NFB) is a neuromodulatory technique that enables voluntary modulation of brain activity in order to treat neurological condition, such as central neuropathic pain (CNP). A distinctive feature of this technique is that it actively involves participants in the therapy. In this feasibility study, we present results of participant self-managed NFB treatment of CNP.
Methods: Fifteen chronic spinal cord injured (SCI) participants (13M, 2F), with chronic CNP equal or greater than 4 on the Visual Numeric Scale, took part in the study. After initial training in hospital (up to 4 sessions), they practiced NF at home, on average 2–3 times a week, over a period of several weeks (min 4, max 20). The NFB protocol consisted of upregulating the alpha (9–12 Hz) and downregulating the theta (4–8 Hz) and the higher beta band (20–30 Hz) power from electrode location C4, for 30 min. The output measures were pain before and after NFB, EEG before and during NFB and pain questionnaires. We analyzed EEG results and show NFB strategies based on the Power Spectrum Density of each single participant.
Results: Twelve participants achieved statistically significant reduction in pain and in eight participants this reduction was clinically significant (larger than 30%). The most successfully regulated frequency band during NFB was alpha. However, most participants upregulated their individual alpha band, that had an average dominant frequency at αp = 7.6 ± 0.8 Hz (median 8 Hz) that is lower than the average of the general population, which is around 10 Hz. Ten out of fifteen participants significantly upregulated their individual alpha power (αp ± 2 Hz) as compared to 4 participants who upregulated the power in the fixed alpha band (8–12 Hz). Eight out of the twelve participants who achieved a significant reduction of pain, significantly upregulated their individual alpha band power. There was a significantly larger increase in alpha power (p < 0.0001) and decrease of theta power (p < 0.04) in participant specific rather than in fixed frequency bands.
Conclusion: Neurofeedback is a neuromodulatory technique that gives participants control over their pain and can be self-administered at home. Regulation of individual frequency band was related to a significant reduction in pain.
Acknowledgement: Front. Neurosci., 25 July 2019 | https://doi.org/10.3389/fnins.2019.00762
(A) A member of the research team (who consented that his photo is provided) demonstrate the correct location of the EEG headset with an arrow pointing to the electrodes from which the EEG was provided. (B) Neurofeedback GUI; Horizontal black lines present an example of threshold values, they were not shown to users.
0095
Measuring compliance to Sedation guidelines in Critical Care
Oshine Saxena, James Ward and Lucy Halpin
Queen Alexandra Hospital, Portsmouth, United Kingdom
Abstract
The Critical Care department at Queen Alexandra Hospital has Sedation guidelines.1 They state a “sedation break” should be conducted daily unless contraindicated and that a Richmond Agitation and Sedation Score (RASS) should be assessed every 4 hours in all invasively ventilated sedated patients.2,3 The aim of this is to ensure sedative drugs are used in an appropriate way as excessive sedation is associated with worse outcomes including increased length of intensive care unit (ICU) admission, increased rates of nosocomial infections and reduced co-operation with nursing and physiotherapy care.4,5
Our audit measures compliance to Sedation guidelines in Critical Care at Queen Alexandra Hospital, Portsmouth.1
Departmental knowledge on sedation breaks was assessed by distributing a survey monkey questionnaire. The departmental electronic patient record system was utilised to conduct a retrospective assessment over 3 weeks of invasively-ventilated patients requiring sedation in November 2018. Data was inputted into Microsoft Excel and analysed using simple calculations. Excel was used to generate graphs and charts.
We received 72 responses from our questionnaire. The majority of responses came from nurses (52.8%, n = 38). Consultants made up 11.11% (n = 8), Junior doctors 5.56% (n = 4), ACCPs/tACCPs another 5.56% (n = 4) and 2.78% of responses came from physiotherapists (n = 2). 57.14% of responders selected sedation breaks should be an MDT-led decision.
37 invasively ventilated patients requiring sedation were admitted to the unit during our 3 week study period. 32% (n = 12) did not have daily sedation breaks with no documented explanation. Only 11% (n = 4) had 4 hourly RASS assessments.
It is likely nursing staff are doing regular sedation assessments but these aren’t being documented. Documentation of contraindications to sedation breaks was also sparse. We identified a large concern for nursing staff was the lack of airway trained practitioners on the unit during sedation breaks. Another barrier is the large changeover in nursing staff on our unit which may mean they often do not have the clinical confidence or feel empowered to initiate sedation breaks.
Our aim is to establish a “Sedation week” where focus is given to RASS scoring and sedation. This week will include lunchtime teaching led by junior doctors, ACCPs and senior nursing staff and one Consultant-led session. We are planning daily bedside teaching during this week to maximise involvement and exposure. We are creating Sedation-protocol “Pocket-Cards” to highlight they are mandatory unless there is a contraindication documented. We are establishing a mandatory sedation break time to create a sense of normality of these breaks occurring. 0800–1000 has been identified as most medical staff are on the unit at this time addressing the nursing concern of a lack of airway trained staff available during sedation breaks.
Overall, it is apparent our unit requires a change in culture regarding sedation breaks and this must be implemented via a multi-disciplinary approach.
0096
A New Presentation of Cryofibrinogenaemia Following Deep Hypothermic Circulatory Arrest (DHCA)
Claire Ellen Adams and Katrina Bramley
Royal Infirmary of Edinburgh, Edinburgh, United Kingdom
Abstract
Background: We present a case report of a patient newly diagnosed with cryofibrinogenaemia in the cardiac intensive care unit (CICU) following elective surgery for an aortic root aneurysm and aortic regurgitation. Cryofibrinogen is an abnormal protein which precipitates in plasma at cold temperatures and dissolves on rewarming to 37°C. It was first described by Korst and Kratochvil in 1955.1 Cryofibrinogenaemia is rare, with a reported prevalence varying between 0–7% of people, and increased prevalence in hospitalised patients.2 It can be primary (essential cryofibrinogenaemia) or secondary. A literature search revealed no previously reported cases of patients with cryofibrinogenaemia in the peri-operative period in cardiac surgery, however there are case reports of patients with cold agglutinins presenting for surgery involving CPB.3–5
Case Presentation: A 77 year-old woman with a past medical history of fibromyalgia and Raynaud’s phenomenon was referred to cardiac surgery having presented to the rapid access chest pain clinic with back pain and a widened mediastinum on chest X-ray. A transthoracic echocardiogram demonstrated a dilated aortic root, moderate aortic regurgitation, and normal left ventricular systolic function. She underwent an elective replacement of aortic valve, ascending aorta, aortic arch, and descending thoracic aorta. Intra-operative management included the institution of cardiopulmonary bypass (CPB) then DHCA, a process of cooling the patient to 20°C and ceasing all circulation for a short period to allow surgical access to vital structures. Following an uncomplicated intra-operative course, she was transferred to CICU intubated and ventilated for post-operative management. On the first post-operative day digital and nose ischaemia were noted in association with falling platelet count, low fibrinogen, and raised D-dimer. She developed anuric renal failure, with a normal renal ultrasound scan, and was commenced on haemofiltration. Following review by haematology and a positive test result she was diagnosed with cryofibrinogenaemia. She was commenced on prednisolone and plasma exchange to induce remission. After a brief improvement evidenced by necrotic areas demarcating, persistent upper gastrointestinal bleeding developed. Oesophagoduodenoscopy revealed gastritis and CT angiogram identified no bleeding point. She continued to deteriorate; high clinical suspicion of a perforated viscus was confirmed on laparotomy requiring a small bowel resection and anastomosis formation. Unfortunately she subsequently developed severe ischaemic colitis and remained too unstable for further plasma exchange. She sadly passed away 45 days after her initial operation. No cause of secondary cryofibrinogenaemia was identified.
Conclusions: To our knowledge this is the first reported case of cryofibrinogenaemia presenting in the immediate post-operative period following cardiac surgery. Astute clinical assessment and investigation led to early diagnosis. Consultation with haematology is essential in patients with known cryofibrinogenaemia. Pre-operative plasma exchange and glucocorticoids in addition to avoidance of hypothermia are potential management strategies.
0097
Responsiveness and Construct Validity of the Chelsea Critical Care Physical Assessment Tool in a Cardiothoracic ICU
Nicole Martin1, Chloe Meehan2, Ruthann Curran2, Katie Dowling2, Claire Purkiss2 and Evelyn J Corner2
1College of Health and Life Sciences, Brunel University London, London, United Kingdom
2The Royal Brompton and Harefield NHS Trust, London, United Kingdom
Abstract
Introduction: Intensive care unit acquired weakness (ICUAW) causes profound impairments in physical function (PF) long after a patient’s discharge from hospital.1 The Chelsea Critical Care Physical Assessment tool (CPAx) is a validated measure of PF in the general medical/surgical and burns ICU population.2–4 The CPAx consists of 10 commonly assessed respiratory and PF components2 graded from 0–50- this translates to dependence to complete independence respectively.2
To date there has been no work which looks specifically at validity of the CPAx in an adult cardiothoracic ICU (CICU).
Objectives:
To explore the:
1. Responsiveness of the CPAx in the CICU.
2. Construct validity of the CPAx in the CICU.
Methods: Retrospective observational cohort study in a CICU in London from 10/2018 to 02/2019. Inclusion criteria: admitted to ICU for at least 48 hrs with recorded CPAx scores.
Responsiveness: Patients were assessed on the CPAx at CICU admission, CICU discharge, High Dependency Unit (HDU) discharge and ward discharge. Differences in CPAx scores between these four time points were analysed to determine responsiveness.
Construct validity: Patients were separated into three survival categories and one non-survival category: home with no rehabilitation needs, home with community support, another rehabilitation facility, repatriated and nonsurvival from ICU. Differences in median CPAx sore at CICU discharge for each category was analysed to determine construct validity.
Data analysis: Data were analysed using descriptive statistics, Kruskal–Wallis test and Dunn’s multiple comparison test. Minimal Detectable Change (MDC) was also calculated using half of the standard deviation of the CPAx score at HDU discharge.
Results: A total of 59 patients were included; 67.8% male; mean age 56 years, mean APACHE II score of 19.
Responsiveness: there was a significant difference in median CPAx scores at all time points (p < 0.001) (Figure 1). Post hoc analysis showed between group differences were also significant (p < 0.05) for all time-points apart from HDU discharge and ward discharge scores. The CPAx MDC was 4. On ICU admission, 46% of patients scored 0 on the CPAx. No patients scored full marks on the CPAx at any time point.
Construct validity: 17 (29%) patients returned home with no rehabilitation needs, 5 (8%) returned home with community support, 17 (29%) went to another rehabilitation facility, 10 (17%) were repatriated and 10 (17%) died in the ICU. A significant difference was found in the median CPAx score between discharge location groups (P < 0.001) (Figure 2).
Those who returned home with no rehabilitation needs were associated with shorter duration of mechanical ventilation (mean, 6 days) and ICU stay (mean, 13 days), and a lower APACHE II score (mean, 16).
Conclusion: The CPAx is able to detect clinically important changes in patients’ PF throughout their hospital stay suggesting good responsiveness. The CPAx tool has a limited floor and ceiling effect from ICU admission to hospital discharge. A change in CPAx score of 4 reflects a true change in the score. The CPAx assessment in ICU has shown a strong association with care needs at hospital discharge.
Figure 1.
Figure 2.
0098
Improving patient and relative experience and staff morale in critical care through animal assisted therapy
Simon Riley-Fuller1, James Evans1 and Sarah Anderson2
1Leeds Teaching Hospitals NHS trust, Leeds, United Kingdom
2Pets As Therapy, Leeds, United Kingdom
Abstract
Introduction: As part of our vision to be #OutstandingCriticalCare we wanted to do something special for our patients and staff. Patients had commented how withdrawn they had become and how isolated they feel on ICU. Many of our patients had pictures of their loved ones around their bed space, including their pets.
Objectives: Our focus with Maggie was to simply improve the experience of our patients by enabling a positive experience in a very difficult time of patients’ lives and improve staff morale by them also having visits from Maggie. We wanted to bring a bit of ‘normality’ to critical care.
Methods:
• Verbal feedback at the time
• Facebook group
• Quantitative feedback forms
Results:
Time To Shine Award: We have recently won the Leeds Teaching Hospitals Kate Granger award for Improving Patient Experience for our ‘Oustanding’ CQC rating and Maggie, our PAT dog.
CQC report: Our CQC report from 2018, Maggie the PAT dog was mentioned in the caring section, rated as outstanding, as being an integral part of our team; ‘The service had a pet as therapy (PAT) dog, Maggie, who visited the units to interact with both patients, visitors and staff each Wednesday.’ (1 p, 56)
AAT Forum: Leeds Teaching Hospitals have set up a national Animal Assisted Therapy forum to produce best practice guidelines within the critical care environment.
Feedback:
• Staff, patients and their relatives have provided overwhelmingly supportive feedback.
• ICU nurse “I didn’t want to get up today but then I realised it was Maggie-day!”
• Maggie helped to calm down a confused patient. A few weeks later we met her saying thank you to ICU – she said “Hi Maggie, are you helping lots of people? You certainly helped me”
• Very poorly older gentleman was quite unresponsive but began to smile and stroke Maggie, his wife was really touched.
• Very humbling today to watch Maggie comforting a family whose relative had passed away minutes before we arrived. They were so pleased to see her and asked to spend some time with her, saying it was “perfect timing” as their relative had been looking forward to seeing Maggie but sadly hadn’t quite been able to. They hugged, cried, gave her carrots and took a photo. Hopefully Maggie was able to give them some comfort at such a sad time
• The last patient of today’s visit said “Maggie, you just made life worth living again”.
• Meeting Maggie on ICU really cheered me up making me feel hopeful for the future in what was a very dark period of my life.
Conclusions: While evidence/feedback is largely anecdotal, this, along with seeing first-hand the impact Maggie has had on our patients, relatives and staff has clearly helped us achieve our objective. Thinking outside the box to help us ‘humanise’ the ICU and bring some normality to a stressful and worrying environment has been one of our biggest achievements. Above all we have improved our patient and relatives experience and given them something to look forward to while with us on ICU.
0099
Utilisation of high flow nasal oxygen in a UK neurosurgical and major trauma critical care unit
Rachael Meredith and Rachel Jones
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Introduction: High flow nasal oxygen (HFNO) is an emerging treatment for acute respiratory failure and is used as an alternative to non-invasive ventilation (NIV). There is limited evidence of its use in neurosurgical and trauma patients. There is some evidence of benefit in the post extubation group (1).
Methods: A consecutive case review was conducted from 11/2/19 to 11/3/19 of all patients on the intensive care unit who required HFNO. Collected data included location of HFNO initiation, indication for HFNO, subsequent need to escalate ventilation and 30-day mortality. Arterial blood gases prior to HFNO initiation were recorded.
Results: 28 patients were started on high flow nasal oxygen during this period. Mean age was 63 years, with 65.5% male patients. HFNO was started in the intensive care unit in 89.3% of cases. Admission specialty distribution is shown in the table below:
3 trauma patients required HFNO; all had multiple rib fractures and the neurosurgical patient had a traumatic brain injury but a consistent Glasgow Coma Score (GCS) of 14. All had type 1 respiratory failure prior to treatment initiation (mean PaO2/FiO2 ratio 162.5, pH 7.43, PaCO2 5.7 kPa). None of these patients required subsequent intubation, and 30-day mortality was 0.
HFNO was started in the post-extubation phase in 42.9% cases (n = 12). 100% of these patients were admitted for medical reasons. Pre-extubation, mean FiO2 was 0.34(0.21–0.77) with PaO2/FiO2 ratio 265(75–425) and pH 7.44(7.35–7.55). 83.3% of those patients fulfilled criteria for adequate oxygenation and eligibility for spontaneous breathing trial pre-extubation (2). 10 patients had a high-risk of reintubation as per criteria applied in the Hernandez et al trial (3).
2 patients (16.7%) required re-intubation, in keeping with rates in previous studies (2, 3) and despite adequate oxygenation pre-extubation (mean FiO2 0.23 and PaO2/FiO2 ratio 379). 30-day mortality following reintubation was comparable to the overall study group (16.6% vs 14.3%, P value = 0.8537).
Conclusion: HFNO use amongst neurosurgical and trauma patients remains limited, but when applied to suitable patients it appears to be an effective therapy with no noted complications. Low incidence of its use in this group may be due to a high incidence of traumatic brain injury and low GCS, requiring intubation and tracheostomy weaning. Further data collection over a longer time period would be of benefit to further interpret outcomes in this subset of patients.
Post-extubation use of HFNO in medical patients is common and demonstrates similar outcomes to published studies, supporting its ongoing use for this indication.
| Parent specialty on admission | Number of patients (%) |
|---|---|
| Medical | 23 (82.1) |
| Surgical (Elective) | 2 (7.1) |
| Trauma (General) | 2 (7.1) |
| Trauma (Neurosurgical) | 1 (3.6) |
0100
The effect of anticoagulant regimes on human 25-hepcidin concentrations after cell salvage (CS) in coronary artery bypass grafting (CABG)
Sarah Schmitz1, Willem Boer2 and Margot Vander Laenen2
1Ziekenhuis Oost Limburg, Genk, Belgium
2Ziekenhuis Oost-Limburg, Genk, Belgium
Abstract
Introduction: Hemolysis during cardiopulmonary bypass may lead to iron-induced renal injury. Hepcidin, a disulfide rich antimicrobial peptide, regulates circulating iron by promoting iron sequestration by macrophages: hepcidin concentration is reduced by anemia and increased by inflammation. Both citrate and heparin are widely used as anticoagulant in CS but differ in mechanism of action. It was hypothesized thatAcid Citrate dextrose-anticoagulant (ACD-A) leads to less inflammation and oxidative stress in CS blood than heparin, by modifying the availability of extracellular Ca2+ with a direct effect on intracellular signalling.
Objectives: Exploring the effects of anticoagulant choice for CS on 25-hepcidin concentrationsin adults undergoing elective on pump CABG.
Methods: After approval by the local ethics committee, a prospective semi-blinded randomized controlled trial was conducted. Patient allocation to 2 groups: heparin or ACD-A. Blood samples were taken at 3 time points during the procedure: S1 just before incision, S2 after weaning from the extracorporeal circuit and before the transfusion of CS blood, and S3 after transfusion of CS blood.
Results: 56 patients were included (46 male, 10 female), 26 in the heparin group (22 men, 4 women) and 30 in the citrate group (24 men, 6 women). Mean age in the heparin group was 69.0 years, while in the citrate group it was 66.3 years (p = 0.329). Hepcidin values (in ng/ml) did not differ significantly between groups at S1 (citrate median 9.45 (4.25–19.72) heparin median 8.22 (4.79–22.50) p = 0.78) and at S2: citrate median 16.75 (8.37–32.14) heparin median 23.84 (9.69–29.57) p = 0.66. At S3 median hepcidin in citrate group was 15.80 (8.48–22.86) vs. in the heparin group 24.44 (11.68–29.44) p = 0.061. In both groups hepcidin values increased between S1 and S2 (citrate mean increase 7.65 p = 0.001, heparin group mean 11.75, p = 0.01) and remained significantly higher than at S1 after infusion of the CS blood. However, after CS transfusion hepcidin values fell by a mean of 3.12, p = 0.08 in the citrate group, but increased in the heparin group by a mean of 0.40, p = 0.81.
Conclusions: In both groups hepcidin levels rose after CABG, reflecting reactions to hemolysis and inflammation. There was is a non-significant association between lower hepcidin values after CS transfusion in the citrate group, compared to heparin. Compared to S2, hepcidin actually dropped after CS transfusion in the citrate group, while rising in the heparin group. These findings likely reflectimportant differences in inflammatory state in CSreservoir, dependent on the choice of anticoagulant. A recent study highlighted the effect of increased hepcidin values during CABG on the incidence of AKI post-operatively. Further studies investigating the value of citrate anticoagulation in CS are warranted.
0101
ICU Microbiology Ward Round Documentation
Callum Twohig, Bagrat Lalabekyan and Dan Harding
Critical Care Unit, Queen Elizabeth Hospital, Woolwich, London, United Kingdom
Abstract
Introduction: Appropriate and effective antimicrobial therapy is essential when treating patients with sepsis on the intensive care unit (ICU). Substandard prescribing of antibiotics can lead to increased length of stay, multidrug resistant infections, and mortality.1
Daily input from Microbiology in the intensive care unit has been found to contribute to more appropriate use of antibiotics, including an increase in appropriateness of empirical and targeted therapies and a reduction in broad-spectrum regimens.2
A provisional audit revealed that a proportion of decisions made on these microbiology rounds were not documented suitably and therefore not acted upon. This may have had a negative impact on patient outcomes.
Objectives:
• To audit the standard of documentation being recorded on the daily ICU microbiology ward rounds
• To produce a quality improvement tool to increase the standard and incidence of improved documentation during these rounds
• To re-audit the above to monitor documentation standard improvements
Method: A prospective audit was conducted which examined the frequency and appropriateness of microbiology ward round documentation. Following this a quality improvement project was devised compromising of a standardised ICU microbial plan on a sticker for the patient notes. The plan was discussed with the hospital microbiology team to ensure all necessary details were recorded. Re-audit of documentation standards post-intervention were undertaken for 2 weeks at a time, at the 1 week and 3 months intervals.
All patients admitted to the ICU were included. Patients were excluded if they were not receiving any antimicrobial therapies or were made fit for discharge from the ICU to the ward.
Results: A total of 350 documentation interventions were included in all audits – 103 pre-intervention, 146 immediately post-intervention, and 101 at 3 months. Pre-intervention, only 27% were documented appropriately in the notes with an additional 15% documented inappropriately on the ICU chart. 59% were not documented at all. Immediately post-intervention, all 146 documentation interventions were documented appropriately in the notes. At 3 months post-intervention, 76% of all documentation was recorded appropriately.
Conclusion: This quality improvement project has managed to improve the documentation standard and the incidence of this improved standard. Further work should be undertaken to audit the continuing use of appropriate microbiology ward round documentation on the ICU.
0103
Augmenting shared learning in ICU by combining simulation with online resources and QR codes
Toby Lewis, Catherine Patton, Andrew Foo and Sian Hughes
Gloucestershire Hospitals NHS Trust, Gloucester, United Kingdom
Abstract
Background: Gloucestershire Hospitals ICU department has over 200 staff. Shared learning is essential to facilitate the penetration of important messages throughout the department with any meaningful effect. This is especially important when learning from simulation, which typically involves limited numbers of staff.
The 4th National Audit Project (NAP4) by the Royal College of Anaesthetists identified the Intensive Care Unit as a common area affected by Airway Emergencies. NAP4 also identified that “airway emergencies on ICU were more likely to occur out of hours and to be managed by inexperienced staff”.1 With the development of the IMT programme there will be an increase in non-anaesthetists staffing our ICU from 2019.2 Airway supervisors and anaesthetic support are on site however the non-anaesthetist will still need to recognise the emergency and initiate basic respiratory support until help arrives.
Systematic reviews have proven the benefit of simulation in training for emergency situations.3 The authors initiated a simulation programme, augmented by the publication of essential learning points on the departmental website.
Methods: Simulations were performed in ICU, utilising members from across the Multi-Disciplinary Team and covering a wide range of airway emergencies. These include failed intubation, blocked tracheostomies and displaced Endo-Tracheal Tubes.
Feedback and learning points from the debrief were collated and uploaded to the departmental website. A dynamic QR code was displayed on posters around the Intensive Care Unit that directed the user to the latest simulation post. The team could also review the whole library of previous simulation reports published on the website, with a secure forum allowing further discussion within the department.
Google analytics was used to gather data on which pages were visited and how many times. This data aids in understanding department penetration for specific learning as well as clinical governance messages.
Results: Six times more people viewed the website articles than were present at the simulations. Despite only 5 members of staff attending each simulation, there were a combined total of 116 views for the simulation articles. No data was collected on individuals visiting the site; some views may have been by the same team members present during the simulation.
Conclusion: Simulation in addition to a secure online platform significantly increases the shared learning opportunities within an ICU department. It also facilitated discussion and engagement throughout the whole MDT. This is particularly relevant in a specialty involving rotating shifts where it is impossible to gather all team members together at one time. The use of posters with QR codes allowed summarised feedback to be widely advertised and easily accessible by all team members.
0104
‘Grow Your Own’: A Network approach to developing our future nurse leaders in Critical Care
Julie Platten1 and Lesley Durham2
1North of England Critical Care Network, Stockton, United Kingdom
2North of England Critical Care Network, North Sheilds, United Kingdom
Abstract
Introduction: Leadership development and succession planning is a challenging task for any organisation but is essential for the growth and sustainability of the NHS. There is a clear correlation between good leadership and making a positive difference to patient care, experience and outcomes,1 therefore, it is imperative to build future leadership capability.2 The North of England Critical Care Network (NoECCN) recognised the absence of available training opportunities and developed a short focused programme to help facilitate senior staff nurses with the transition into management and clinical leadership roles.
Objective:
• To prepare future nurse leaders in critical care across the NoECCN
• Raise awareness of important current issues impacting on practice
• Explore the theory of teams and the importance of emotional intelligence and resilience
• Through scenario based discussions identify critical issues in practice from a clinical leadership and management perspective
• Introduce change management and service improvement methodology to initiate positive change
Method: The programme is delivered twice a year over 1.5 days and is accessible to registered nurses wanting to develop their leadership and management skills. Attendance is authorised and supported by their line managers.
Day One – Faculty delivered interactive seminars and group work including: national drivers, leadership and management approaches, service improvement and change methodologies, problem solving, human factors, I-resilience, team working and the generation gap. Individuals or small groups then identify a service improvement within their own clinical area and undertake this over a six month period.
Day Two (1/2 Day) – Through a poster presentation method the service improvement projects are presented to the group and faculty. A small prize is awarded for the best project using predefined criteria.
Conclusion and Future Plans: A total of 277 nurses have undertaken the programme which evaluates extremely well. There have been some excellent service improvement projects which have significantly improved patient safety and both patient and staff experience. The best of these are selected to be presented at the NoECCN annual conference with further encouragement to disseminate at a national level.
Future plans
• Further develop the faculty to provide resilience
• Continue to review and refresh the programme content to ensure it is current
• Embed Step 4 of the National Competency Framework for Registered Nurses in Adult Critical Care (Leadership and Management) into all NoECCN units
0105
Flexible Bronchoscope suction performance: A Bench Study
Matt Rowe, Peter Sykes, Matthew Cole, Lucy Elliot and Chris Newell
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Introduction: Flexible bronchoscopy has numerous applications within a critical care setting.1 An important function of bronchoscopes used on intensive care units (ICU) is the capacity for suction. Many ICUs have traditionally relied upon reusable fibre optic bronchoscopes to perform tasks such as broncho-alveolar lavage (BAL) and secretion clearance. Repeated-use bronchoscopy, however, has several disadvantages. These may include high initial outlay and costs of repairs/maintenance, the need for decontamination and the potential for cross-contamination between patients. Previous work has focussed on operator opinion for ease of use, diagnostic yield of BAL, time taken to perform intubation/tracheostomy and cost effectiveness, but to our knowledge has not assessed suction performance.2 We propose that the use of single use Ambu-A bronchoscopes offer non-inferior performance in terms of suction capacity with significant potential advantages over traditional reusable bronchoscopy.
Objective: The aim of this bench study was to challenge a belief held locally that traditional re-usable fibre optic bronchoscopes are superior in performance to the single use Ambu-A Bronchsope system in terms of suction ability.
Methods: The suction performance of four different bronchoscopes were compared across a range of Newtonian liquids of known varying viscosities. The devices tested were:
1. Olympus Bronchoscope BF-P60 4.9/2.2
2. AMBU® aScope™ 4 Broncho Large (5.8/2.8)
3. AMBU® aScope™ 4 Broncho Regular (5.0/2.2)
4. AMBU® aScope™ 4 Broncho Slim (3.8/1.2)
Each scope was tested by calculating the fluid flow rate obtained using a vacuum pressure of −80 kPa. This flow rate was calculated by measuring the time taken to aspirate a given volume of three different fluids of known viscosity at room temperature. These fluids included – water, 20% dextrose and 40% dextrose.
Results:
Conclusion: The AMBU® aScope™ 4 bronchoscopes offer comparable or superior suction performance to the Olympus BF-P60 in all but the “slim” model which significantly underperformed for all fluid viscosities. We would argue that this model is inappropriate for use in an ICU setting if secretion clearance is required. Furthermore, we would suggest that single use bronchoscopy offers significant advantages over reusable bronchoscopes in critical care and could become a first line option for the majority of clinical indications.
0106
Vancomycin by continuous infusion in ICU; re-audit of processes following implement of changes demonstrates improvement
David Stanley and Zeshan Riaz
The Dudley Group NHS Foundation Trust, Dudley, United Kingdom
Abstract
Introduction: Antibiotic therapy is one of the few areas in Intensive Care with a solid evidence base for effectiveness. However, simply giving an antibiotic may not result in effect but taking levels goes some way to objectively achieving this. Vancomycin is a glycopeptide antibiotic active against Gram-positive bacteria. Effectiveness increases as the duration of time with serum concentration above the minimum inhibitory concentration (MIC) increases. A recommended blood level to achieve MIC is 15–25 mg/l, although for more severe infection 20–25 is suggested. In 2012 we audited Vancomycin levels aiming for a target of 15–25 mg/l when given by continuous infusion and found concentrations that were often sub-therapeutic (33%). Of more concern, a significant number of patients (23%) NEVER achieved levels above MIC, particularly when renal function was normal. Working with the Trust’s anti-microbiology pharmacist we used these results to revise our guideline; initial bolus and maintenance doses were increased and a further (reduced) bolus if level <10 was added. The loading and maintenance electronic drug prescriptions for vancomycin were modified to give clear weight and renal based options for prescribing matching the new guideline. An advisory warning if a vancomycin level was above 25 was also added.
Objective: Our primary objectives were to see whether the new guideline had produced improvement in the number of patients achieving satisfactory vancomycin levels faster without a significant increase in toxic levels. Secondary objectives were to see if correct doses were being given.
Method: All patients receiving Vancomycin on ICU during 2018 were identified from the ICU EPR (ICCA©, Philips). Patients excluded from analysis were those receiving an intermittent regime and those who died within 24 hours of the infusion being started. Weight (actual body-weight), creatinine clearance (Cockcroft-Gault method), bolus dose and time, infusion rate and time started, and all vancomycin levels and time of administration were obtained for all patients.
Results: 26 suitable patients received vancomycin by continuous infusion during 2018. All but three (3/26, 11.5%) patients achieved target levels compared with 23% previously (values too low to be statistically significant). The median time to achieving target level reduced from 31 to 6 hours The time to starting the infusion from the bolus starting reduced from 3 hours 41 minutes to 70 minutes. Levels at least therapeutic (>15 mg/l) increased from 66% to 73% (p = 0.31) and high (>25) increased from 9% to 18 % (p = 0.07). The initial bolus dose was prescribed as per guideline 50% of the time and starting infusion 62% of the time.
Conclusion: Our audit showed that target levels (15-25 mg/l) were achieved more quickly and were not associated with an increase in the number of high levels. We were unable to show a significant increase in the numbers of patients achieving target vancomycin levels and the number of correct target levels themselves, possibly because the audit was underpowered. Prescribing was often not as per guideline and as a retrospective audit we were unsure of the reasons (caution re; dynamic changes in renal function seen in ICU etc.).
0107
Factors Associated with Failed Extubation in a Cardiothoracic ICU
Kirsten Fleming1, Chloe Meehan2, Ruthann Curran2, Katie Dowling2, Claire Purkiss2 and Evelyn J. Corner1,2
1College of Health and Life Sciences, Brunel University London, London, United Kingdom
2The Royal Brompton and Harefield NHS Trust, London, United Kingdom
Abstract
Introduction: Mechanical ventilation (MV) is a lifesaving intervention, however, prolonged MV is associated with negative patient outcomes, e.g. pneumonia, diaphragmatic atrophy, Intensive Care Unit Acquired Weakness (ICUAW), and airway trauma.1,2 Additionally, patients that are re-intubated are seven times more likely to die.4 It is therefore important to understand local factors associated with failed extubation.
The Chelsea Critical Care Assessment (CPAx) tool is a validated measure of physical function in the ICU incorporating both respiratory and physical function components. It allows grading of function on a scale from 0–50, 0 representing full dependence, and 50 representing independence. As ICUAW is associated with MV, it is plausible that early CPAx scores may be associated with reintubation rates,5–7 which could help with clinical decision making.
Objectives: To explore the clinical characteristics associated with failed extubation.
Methods: Retrospective observational cohort study in a Cardiothoracic adult ICU in London from 24th October 2018 to 31st January 2019. Inclusion criteria: MV for3 48-hours and a CPAx score within 24-hours before extubation. Exclusion criteria were repatriation whilst MV, tracheostomy inserted before extubation and death whilst intubated.
The following data were collected from clinical records: failed extubation (defined as the requirement for non-invasive ventilation (NIV) or reintubation within 48-hours), age, gender, length of stay (LOS), total days of MV, admission diagnosis, APACHE II score and number of comorbidities.
Data were analysed using descriptive statistics and using Mann-Whitney U test. Sample size calculation with alpha set at 0.05 indicated 16 patients per group (total n = 32).
Results: 68 patients were admitted intubated during this time, 28 were included in final data analysis. The mean age was 54.4 (SD 17.9) years and 79% of the population were male. Ten patients failed extubation (35.7%) and the re-intubation rate was 17.86%. Comparisons between the patients who failed and those who were successfully extubated showed no significant difference between the groups for age, gender, number of comorbidities, APACHE II score, hospital length of stay and admission diagnosis (p > 0.05).
The median days of MV for the failed versus successful extubation group was 16.0 days (IQR 2.75–29.25) and 8.0 days (IQR 4.75–11.15) days respectively (p = 0.067) (Figure 1), and the median AICU LOS was 23.5 days (IQR 16.5–30.5) versus 11.00 days (IQR 4–18) respectively (p = 0.067). Failed extubation was associated with a longer duration of endotracheal tube intubation 8.0 days [IQR 3.75-12.25] versus 4.0 days [IQR 1.5–6.5] (p = 0.041). The median pre-extubation CPAx score was 4.5 (3-8.5) in the unsuccessful group versus 5.5 (IQR 2.5–11.75) (p = 0.648) in the successful group (p = 0.648).
Conclusion: Local reintubation rates are similar to national figures [8,9]. Longer duration of ETT prior to extubation was associated with extubation failure (Figure 2). There was an insignificant trend towards longer LOS and days of MV in those that failed extubation. Failed extubation did not appear to be associated with physical function as measured using the CPAx.
Limitations: This study was part of an MSc and was therefore time limited and underpowered.
0108
Survival of intubated patients with a diagnosis of haematological malignancy admitted to intensive care: A 5 year review
Ben Soni
St James University Hospital, Leeds, United Kingdom
Abstract
The admission of patients with haematological malignancy has been associated with high mortality rates (1.) although outcomes may have improved in recent years (2.). Physiological scoring systems (e.g. APACHE, SOFA) are not thought to be reliable in determining outcomes for these patients and number of organs requiring support may be more useful (1,3). We have reviewed the mortality rate for patients with haematological malignancy in our institution by haematological diagnosis, requirement for invasive ventilation and number of organs supported.
We conducted a retrospective review of patients, with haematological malignancy, admitted to St James University Hospital Intensive Care Unit (ICU) in the five-year period from 01/01/2013 to 31/12/2018. Patients were sub classified according to diagnostic group: myeloma, acute lymphoblastic leukaemia (ALL), acute myeloblastic leukaemia (AML), chronic lymphocytic leukaemia (CLL), chronic myelogenous leukaemia (CML), hodgkin's and non-hodgkin's lymphoma (NHL). The maximum number of organs supported was recorded along with requirement for intubation. ICU and hospital episode mortality rates were calculated for each diagnostic group.
318 patient records were included in the study. Mortality figures are shown in figure 1. Overall ICU mortality was 41.5% and hospital mortality was 58.5%. Admissions with acute leukaemia (AML and ALL) had the highest ICU mortality, 58% and 47% respectively and a hospital mortality of 67% and 63%.
Patients with 1 supported organ had a mortality of 39%, this increased to 78% with 3 or more supported organs. Data were limited for subgroup analysis but AML (n = 67) increased from a 40% mortality following single organ support to 89% with 3 or more organs supported. Similarly NHL (n = 93) increased from a 36% to 76% mortality with greater support requirements.
122 patients required intubation and invasive ventilation. 70 died on ICU and a further 18 died before hospital discharge (72%). Acute leukaemia was associated with the most deaths on ICU following intubation (79%) compared to 42% mortality in those not requiring intubation. NHL was the only group where intubation was not clearly associated with an increased mortality on ICU (38% of those intubated Vs 34% not intubated).
This review demonstrates that patients with haematological malignancy continue to have a high mortality associated with ICU. However, the heterogeneity of the group suggests that underlying diagnosis is an important predictor of outcome with escalating organ support. NHL mortality appears to have improved, compared to previous studies, where single organ support is required. Therefore, subgroup analysis is strongly recommended for future studies seeking to characterise ICU associated mortality of patients with haematological malignancy. This study may be limited by small numbers, patient selection bias when considering referral to ICU and limitations of diagnostic coding. It supports further research with subgroup analysis to aid clinical decision making and prognostication.
Figure 1.
Chart to show ICU and Hospital admission mortality. The underlying haematological diagnosis is shown in the x-axis starting with the cumulative total on the y-axis. Mortality is on the x-axis. The legend is below the chart. (n) is the number of patients in each group.
0109
Alcohol Misuse and Patient Outcomes Following Admission to the Intensive Care Unit at Royal Preston Hospital – Are We Making Good Use of Medical Resources?
Alexander Bohao Lee1,2 and Mark Pugh2,3
1The University of Manchester, Manchester, United Kingdom
2Royal Preston Hospital, Preston, United Kingdom
3The University of Manchester, Preston, United Kingdom
Abstract
A number of factors have led to the increased prevalence of alcohol misuse in the UK for the past few decades (1–3). Alcohol-related harm is now a leading cause of death (3,4), and has become a significant burden, especially to our healthcare system (1). A small number of these patients require admission to the intensive care unit (ICU) but their prognosis remains uncertain. There is inconsistent use of ICU regarding such individuals, which have inevitably impacted on the quality of patient care in this cohort.
In this retrospective audit study, we attempted to a) investigate the on-unit and long-term survival of patients who had been admitted to the ICU at Royal Preston Hospital as a result of alcohol misuse; b) explore various factors which might have contributed to such outcomes; c) discuss, in the context of the wider society, in order to explore the ethical implications of admitting such patients to the ICU, and how the decision making will inevitably impact on efficacy of treatment and resource allocation.
We reviewed 79 patients who were admitted to the ICU of Royal Preston Hospital following alcohol-related harm against their survival outcomes. Receiver Operating Characteristic Curves, logistical Regression and Kaplan-Meier Survival Curves were used to determine the association between patient markers and their prognoses.
These admissions were shown to be costly (approximately £900,432 over the 18-month period), and generally carried a poor prognosis (mortality rate = 38%). Child-Pugh scores and the Model for End-Stage Liver Disease (MELD) were associated with good prognostic power. In addition, several factors were demonstrated to be associated with worse survival outcomes: female gender (odds ratio = 6.67, p = 0.0002), hypoglycaemia (odds ratio = 4.33, p = 0.0044), hypothermia (odds ratio = 4.90, p = 0.0048), raised lactate (odds ratio =7.25, p = 0.0004), raised alkaline phosphatase (ALP, odds ratio = 4.03, p = 0.0078).
Many patients from this cohort would have benefited from end of life care, of which the stronger focus on symptom relief is in agreement with the principle of beneficence and non-maleficence. We noted that pre-agreed care plans that reflects individual patients’ realistic prognoses would have played an important role in guiding such admissions to protect their autonomy.
The question of resource allocation and social justice has become more important amid deteriorating national performance in cancer treatment (5). Elective cancer operations required shorter ICU stays (p = 0.0028) and came with a possible lower mortality rate (p = 0.5505). The bed days from alcohol-related admissions could have in theory accommodated 108 elective cancer surgeries per annum.
Preventative strategies and personal lifestyle choice alterations are urgently needed to combat alcohol-related harm. For the unfortunate patients who have become seriously ill from alcohol misuse, Child-Pugh scores, MELD scores, female gender, hypoglycaemia, hypothermia, raised lactate, raised alkaline phosphatase are found to be associated with adverse outcomes after admission to the intensive care unit.
Figure.
Kaplan-Meier Survival Curves (Percentages: Predicted Mortality Rates Based on MELD Scores).
0110
Long-term mortality risk after admission to Torbay Intensive Care Unit
Thomas Clark and Victoria Lewis
Torbay and South Devon NHS Foundation Trust, Torquay, United Kingdom
Abstract
Introduction: Patients who survive critical illness may continue to suffer from chronic health issues as a consequence of their intensive care episode; the ‘post intensive care unit (ICU) syndrome’. Whether this results in long-term excess mortality risk is poorly understood; estimations of long-term survival often ignore background mortality rates.
Background/Objectives: We wished to better understand long-term survival of patients admitted to our ICU and estimate for how long their daily/annual mortality risk exceeds that of the United Kingdom (UK) general population.
Methods: We undertook a relative survival analysis of all emergency patients, aged over 18 years old, admitted to our ICU between the dates of April 2008 and April 2012. Dates of death were collected for each individual and the follow-up period censored in July 2018. Net survival and probability of death was estimated for each year until censorship. This analysis adjusted cohort survival for UK population life expectancy (matched for age and sex).1 The dataset was also stratified into 3 adjusted age groups as per our a priori plan; 18–64, 65–79 and >79 years old (cohorts set by recent ICU studies). Our analysis used R studio version 3.5.0 ‘Joy of Playing’. See references for packages.2,3,4
Results: 1845 patients were included in final the cohort with 1008 events by final censorship. Median survival was 1960 days in unadjusted cohort (0.95 CI 2313–1685 days (5.4 years), median not reached in adjusted cohort). Median age of unadjusted cohort 66 years (IQR 52 – 78) and median APACHE-2 score 16 (IQR 12 – 21). See figure 1 for display of unadjusted vs adjusted cohort survival curves. See figure 2 for probability of death curves for 1) adjusted ICU cohort by age-group, and 2) UK background population.
Discussion: Patients admitted to our ICU have continued to carry a mortality risk in excess of the UK general population for at-least 6 years after their admission. However, when considering different age groups, it appears that the probability of death is consistently lower in the over 79 cohort versus the background population, whilst it is higher in the 18–64 and 65–79 cohorts for at-least 10 and 6 years respectively. This lower probability of death in the octogenarian population is likely due to selection bias, whilst the young are left with significant excess mortality for years after ICU admission.
Figure 1.
Net survival can be described as the ‘survival as if the disease in question (critical illness) is the only cause of death’. Death due to ‘all other causes’ is reflected in background population life expectancy curve (not shown) that was used in adjustment process.
Figure 2.
Probability of death for 3 adjusted age cohorts (solid lines, black = 18-64 year old age group, red = 65-79, blue = >79). Dashed lines represent expected probability of death for matched (age and sex) UK population.
0111
Improving compliance with HIV testing guidelines in patients admitted to the Intensive Care Unit at Hillingdon Hospital: results of a multidisciplinary quality improvement project
William Seligman, Mohammed Jawad, Michael Kelly and Elisa Kam
The Hillingdon Hospitals NHS Foundation Trust, London, United Kingdom
Abstract
The public health importance of early diagnosis of HIV infection cannot be overstated. International guidance supports opt-out HIV testing in medical settings where local HIV prevalence exceeds 2 per 1,000 individuals.1 HIV-related opportunistic infections result in critical care admissions for patients with undiagnosed HIV.2 It has been shown that approximately 30% of patients admitted to ICU qualified for testing according to UK HIV testing guidelines and yet only 5% were actually tested.2
The objective of this quality improvement project was to improve screening for undiagnosed HIV in patients admitted as an emergency to the ICU at a district general hospital in North West London.
Using PDSA methodology, a multidisciplinary team identified ways to improve compliance with HIV testing in eligible ICU patients. A retrospective audit of the medical records of patients admitted to ICU in January 2018 was undertaken. An ‘ICU Admissions Blood Test Profile’ script was then written into the hospital’s blood test requesting software. This profile included all tests that would routinely be collected on admission to ICU and would also include HIV as long as the patient was admitted as an emergency, and either had capacity to consent to testing and did so, or did not have capacity to consent to testing. After feedback from nurses during a pilot study, the script was simplified before launch to ensure ease of adoption. A retrospective audit of the medical records of patients admitted to the ICU between March and May 2019 was undertaken.
13% of eligible patients (3/23) had an HIV test performed during their ICU stay prior to intervention. Post-intervention, 85% of all eligible patients (45/53) were tested for HIV. Of those 20 patients admitted to ICU during the post-intervention study period who did not meet eligibility criteria for HIV testing on admission i.e. elective surgical patients, 40% (8/20) had HIV tests on admission.
This quality improvement project led to a significant improvement in adherence to national guidance on HIV testing in the critical care setting. The introduction of an ‘opt-out’ HIV test on admission to ICU is consistent with the policies of other London ICUs.2 Further work is needed to reduce the proportion of elective surgical patients inappropriately being tested for HIV.
ACKNOWLEDGEMENTS: Mr Adebayo Sodunke, Dr Andrew Smallbones, Dr Maria Mirza, Dr Benedict Holden
0113
Does poor sleep temporally correlate with delirium? – A UK single centre audit
Thomas Underwood1,2, Sudhindra Kulkarni2 and Shondipon Laha2
1University of Manchester, Manchester, United Kingdom
2Royal Preston Hospital, Preston, United Kingdom
Abstract
Introduction: Sleep and delirium are a significant problem on the intensive care unit (ICU). This is due to a variety of factors including emergency admissions, night time nursing intervention and sensory overload.1 A study by Elliott et al in 2013 used polysomnography to establish the median duration of sleep before waking to be just 3 minutes at a critical care unit in Australia.2 Delirium is a clinical syndrome that occurs commonly in patients on ICU’s and is characterised by a patients disturbance in conciousness, inattention and cognitive dysfunction, contributing to worsened patient outcomes and prolonged intensive care admissions.3,4
Objectives: This prospective audit aimed to establish a correlation between poor sleep quality in intensive care patients, and the associated delirium incidence in the following 24 hours. The audit specifically focused on patients being provided with level 2 care on the intensive care unit.
Methods: Patients fitting level 2 criteria were selected from a 28 bedded general and neuro critical care unit at Royal Preston Hospital, Lancashire Teaching Hospitals NHS Foundation Trust. Sleep was measured by asking patients to fill in a Richards Campbell Sleep Questionnaire (RCSQ). Delirium incidence was measured using the Confusion Assessment Method (CAM). The patients CAM assessment was documented for 24 hours following completion of the questionnaire. If the patient became delirious within 24 hours, they were recorded as 1. Patients who were currently CAM positive were excluded from completing the questionnaire. We especially focused on the perceived depth of sleep from the previous night, and the patients overall sleep assessment. In order to perform statistical analysis in the form of a Fisher exact test, results were categorised into 0, a poorer sleep, or 1, a good sleep.
Results: 100 patients completed the survey between the 8th of April 2019 and the 10th May 2019. Statistical analysis proved no statistical significance between the sleep assessment and incidence of delirium, although patients with a poor perceived depth and overall assessment of sleep were more likely to become delirious in the following 24 hours.
Conclusion: There is some correlation between diminished sleep quality and negative sleep reflection by patients and the risk of the patient developing delirium. The association between poor sleep quality and an increased incidence of delirium showed no direct statistical correlation, however this may be due to small numbers and other factors. The authors would recommend further research in this area with a more highly powered prospective study.
| Delirium assessment 24 hours following questionnaire |
||
|---|---|---|
| 0 | 1 | |
| Patient Sleep Depth assessment | ||
| 1 | 68 | 0 |
| 0 | 30 | 2 |
| Overall Patient Sleep assessment | ||
| 1 | 65 | 0 |
| 0 | 33 | 2 |
0114
CT or not CT:That is the question. Do drug overdoses admitted to ICU need a CT scan
Patrick Jerred and Ailbhe Brady
Warrington Hospital, Warrington, United Kingdom
Abstract
In 2017 there were 3,756 registered deaths in the UK related to drug poisoning. North West England has the second highest rate at 64 per 100,000. This is mostly due to opiate overdose. Many of these patients present with decrease GCS requiring a CT scan head. A CT head produces 2mv of radiation and there are costs of time delays. If there is a clear history of drug overdose do we need a CT scan? We decided to look at the ICU data for Warrington Hospital to see if we could address this.
We looked at patients who were admitted to Warrington hospital ICU in 2018 with a diagnosis of self-poisoning. Patients were Level 2 and Level 3. We used the national ICNARC data to retrieve this information. We gathered data on whether the patient had had a CT scan, the CT scan result and patient outcomes.
We had a total of 56 patients for 2018. 29 were Level 2 and 27 were Level 3.
Level 2: 26 patients had no CT. 3 patients had a CT, all normal
Level 3: 20 patients had CT. 19 normal. 1patient had an abnormality on CT which was ruled out on MRI scan. 7 patients had no CT
Presenting history of the 23 patients having CT:
9 patients had a record of overdose with evidence of trauma and 9 had overdose with no evidence of trauma. 5 had a history of collapse.
Outcome. There was only 1 mortality in the 56 patients. This patient died from cardiovascular collapse due to an overdose of cardiac drugs. There was full neurological recovery in the other 55 patients with average length of stay 2.1 days.
Our evidence on the 56 patients admitted to our ICU in 2018 would seem to support a policy of not scanning patients with drug overdose.
An unconscious patient admitted to AED with overdose could be transferred safely and seamlessly to Level 3 ICU. In fact in our cohort, this had happened in 7 cases.
This would circumvent delays in AED, delays in transferring patient to CT department, delays with radiology HUB and the radiation risk.
We presented our findings to our ICU Department audit meeting. Despite our evidence there was an uneasiness to change the current ad hoc practice even though there is also published evidence to support not scanning1
We hope that by presenting our data to a wider audience we can start a discussion leading to some common guidelines, in particular with regard to CT scan, in the management of patients with overdose.
0115
Collection of pain-related outcome data in critical care survivors
Harriet Kemp1, Helen Laycock1, Alice Costello2 and Stephen Brett3
1Imperial College London, London, United Kingdom
2Imperial School of Anaesthesia, London, United Kingdom
3Imperial College Healthcare NHS Trust, London, United Kingdom
Abstract
Over the last two decades, as mortality during admission to intensive care has decreased1,2, the challenges of ‘ICU survivorship’ have become an increasingly important focus.3 There is emerging evidence that chronic pain in ICU survivors may mediate physical, cognitive and psychological factors associated with post intensive care syndrome. Until recently the role of chronic pain has received little attention.4 Limited evidence exists for how best to collect pain outcomes in this cohort. This pilot work aimed to identify useful concepts and challenges in capturing pain-related outcomes in critical care survivors to inform future work.
Imperial Healthcare NHS Trust approved the project as service evaluation. All patients discharged from Hammersmith Hospital General ICU over 3 months were prospectively asked to complete paper questionnaires at ICU discharge and at 3 months post-discharge via the critical care follow-up services. Questionnaires included the PainDETECT, (pain intensity/presence of neuropathic qualities), the EQ-5D (health-related quality of life) and the Brief Pain Inventory (BPI) (pain intensity/interference). Subjects also reported pre-admission chronic pain diagnoses and analgesia. Nursing assessment of pain during ICU admission (‘0-3’ scores and the critical care pain observation tool (CPOT) scores) and demographic data were collected retrospectively from electronic records.
Of the 88 patients (48 (55%) surgical, 43 (49%) male) completing the discharge questionnaire, 57 (65%) reported a pre-admission chronic pain diagnosis but this was only recorded in 21 (37%) of inpatient medical records. Around half (n = 42, 48%) recalled pain during their admission, 55% of whom reported it as constant pain. Scores for nursing pain assessment and patient recall of pain is presented in Table 1, and suggests higher severity through patient recall (statistical comparison not appropriate). The EQ-5D was completed fully by 82 (93%) and the painDETECT by 78 (89%). At 3 months 29 (33%) of surviving patients completed the follow up questionnaire. All questionnaires were completed fully by 27 (93%). Pain was reported by 51%(n = 15), a third of whom did not report chronic pain pre-admission. ‘Worst pain’ intensity was reported as significantly higher (p = 0.02) on the painDETECT than the BPI.
Pain is a common complaint at ICU discharge and at 3 months post-discharge. Chronic pain conditions are recorded poorly during acute admission. There may be a discrepancy between nurse reported and patient recalled pain severity during ICU admission indicating both sources of data should be collected. In general questionnaires were well completed despite a relatively low response rate at 3 months.
Table 1.
| Median acute pain score | Converted NRS value* | Patient recall NRS | |
|---|---|---|---|
| CPOT ‘Average pain’ | 0.65 (0.21–1.35) | 1.0 | 5.5 (3.0–8.0) |
| CPOT ‘Worst pain’ | 2.0 0.0–5.0) | 4.0 | 9 (5.0–10.0) |
| 0–3 ‘Average pain’ | 0.47 (0.11–0.91) | 2.0 | 5.5 (3.0–8.0) |
| 0–3 ‘Worst pain’ | 1.5 (1.0–2.0) | 4.5 | 9 (5.0–10.0) |
*conversion to 11 point numerical rating scale (NRS) based on the non-linear association of the pain scales.
Table 2.
| At discharge n = 88 | At 3 month post-discharge n = 29 | |
|---|---|---|
| EQ-5D pain domain, n (%) | ||
| Moderate | 32 (36) | 5 (18) |
| Severe | 17 (19) | 0 (0) |
| Extreme | 5 (6) | 2 (4) |
| PainDETECT | ||
| Average pain, median (IQR) | 5.5 (3.0–8.0) | 1.0 (0.0–4.75) |
| Possible/Probable neuropathic pain, n(%) | 25 (28) | 6 (21) |
| Brief Pain Inventory | ||
| Intensity, median(IQR) | – | 0.75 (0.0–4.0) |
| Interference, median(IQR) | – | 1.0 (1.0–3.6) |
0116
Improvements in the management of severe traumatic brain injury patients following education and a multidisciplinary approach: a three year audit
Tae Lee and Tim Astles
Aintree University Hospital NHS Foundation Trust, Liverpool, United Kingdom
Abstract
Aintree University Hospital and the Walton Centre work together as the Major Trauma Centre Collaborative for Cheshire and Mersey. Patients with isolated traumatic brain injuries (TBI) or requiring direct neurosurgical intervention are managed at the Walton Centre, whereas patients with complex polysystem injuries are often managed at Aintree. This has led to an increase in the number of patients with TBI being managed at our Aintree Intensive Care Unit. The organisational separation between the Trusts can present logistical and pragmatical challenges. Our first 2016 audit found that 21.4% (6/28) of our severe TBI patients were not appropriately managed, based on both the Brain Trauma Foundation1 and our Aintree guidelines. Our objective therefore was to improve the management of severe TBI patients following a two-pronged approach with in-departmental education and an early, proactive multidisciplinary team engagement with the neurosurgical department.
Education was implemented within the department regarding best practice and awareness of the Aintree TBI guidelines. Furthermore, neurosurgical consultant presence at the daily major trauma multidisciplinary meetings was mandated and early ICU consultant to neurosurgical consultant discussions around management of severe TBI patients became routine practice. A two-year follow up audit (January 2017 to December 2018) was subsequently conducted. Data were obtained from the Trauma Audit Research Network and patients with severe TBI were identified (criteria included all of the following: GCS < 9, Abbreviated Injury Severity score of 3–5 for brain and intubated). We then looked into the electronic hospital notes to identify if each patient had been appropriately managed, specifically regarding strict adherence to physiological parameters, indications for intracranial bolt insertion and timely sedation holds for neuroprognostication.
Mean patient age was 50.6 years in 2017 and 44.9 years in 2018. Majority of the patients were male (17/22 in 2017, 16/19 in 2018), with vehicle collisions being the most common mechanism of injury (11/22 in 2017, 10/19 in 2018). The 2017 audit identified that 90.9% (20/22) of patients received appropriate management, with an increase to 100% (19/19) of patients in 2018 – this is in comparison to 78.6% (22/28) of patients in 2016. A greater proportion of patients also received appropriate timing of sedation holds (24–48 hours from the onset of injury) in 2018 (36.8% of patients) than in 2017 (13.6%).
TBI is often known as the silent epidemic and still causes significant morbidity and mortality in developed Western nations.2 Through this recognition, our results demonstrate a progressive three-year improvement in consistent and appropriate management of severe TBI patients, attributed to education and collaborative multidisciplinary effort.
0118
How resident is the ICU resident? A clinical activity assessment of the ICU residents who have ‘off-unit’ responsibilities at a tertiary centre
Brendan Spooner, Catherine Snelson and Joseph Seager
University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Introduction: The UK multi-agency Guidelines for the Provision of Intensive Care Services standards state that night-time and weekend intensive care resident to patient ratio should not normally exceed 1:8. However, this ratio may need to be reduced if the intensive care resident is expected to provide emergency care outside of the ICU (e.g. wards/emergency department).1 There is further off-unit demand for the ICU resident as deteriorating hospital patients should receive care from critical care outreach personnel,2 which in most NHS hospitals will involve an experienced ICU resident. There is no data on how to balance on-unit and off-unit workload with the current workforce.
Objective: This project sought to quantify the on-unit and off-unit workload of ICU residents in a tertiary centre in order to make informed decisions about staffing and to provide more support for them if needed.
Method: A prospective analysis of the clinical activity of all the resident clinicians (non-consultant) across a single site ICU of 78 beds for all non-daytime activity was undertaken for 4 weeks. The 78 ICU beds are divided into 4 separate units staffed outside of daytime hours by resident clinicians which includes; 5 senior ICU residents (registrars), 2 junior residents (FY2/SHO) and an ACCP. Data was collected prospectively by asking clinicians to complete a simple form indicating their activities for the duration of their non-daytime (1700-0800) shift in 15-minute periods. Qualitative data as free text was also recorded anonymously about the clinicians’ perceptions of their workload.
Results: A total of 2297 hours of clinical activity was recorded. Data was complete for 80% (45/56) of the shifts for the senior ICU resident responsible for the Liver ICU and ward referrals. They were ‘off-unit’ for up to 52% of their shift (range 0–52%, mean 18%, median 16%). This was mostly reviewing ward referrals. There was no difference in location of their clinical activity at night. Data was complete for 66% (37/56 shifts) for the senior ICU resident responsible for the Trauma/Burns ICU and the Emergency Department. They were ‘off-unit’ for up to 85% of their shift (range 0–85% mean 42%, median 44%), with 33% of their time in ED. Again, there was no difference recorded between evening and night work. Qualitative data indicated that on 14/82 shifts (17%) the junior ICU residents wanted more support when the senior resident was off-unit.
Conclusion: Intensive Care Medicine in NHS hospitals increasingly involves off-unit workload. This off-unit activity is vital, unpredictable and time-consuming, but may impact on the safe delivery of on-unit care. By quantifying this activity, informed decisions about staffing and expected workload can be made, especially for non-daytime working. This should improve patient safety and provide data that can help make a business cases for ACCPs or further residents to achieve the resident to patient ratios recommended by National Guidelines.1
0120
Post-operative delirium and implications for Neurointensive care: Our experience in a tertiary Neurosurgical centre
Will Angus, Sumantra Saha, Priya Nair and Raj Srinivasaiah
The Walton Centre NHS Foundation Trust, Liverpool, United Kingdom
Abstract
Delirium is an acute alteration in mental state characterised by fluctuation in cognition, inattention and activity. It is well recognised in intensive care and increasingly recognised in the immediate post-operative setting. Post-operative delirium can lead to delays in leaving the recovery area and potentially the need for admission to a higher level of care for pharmacological management and increased nursing requirements. Risk factors for post-operative delirium include age, pre-existing cognitive disturbance, major surgery and the use of perioperative opiates – many of which are unavoidable within Neurosurgery.
Decisions on whether to proceed with major elective surgery on the day are guided by clinical and non-clinical factors. Non-clinical factors may be the availability of equipment and staff and the availability of a post-operative bed. The potential requirement for Critical Care admission following surgery may delay an operation where a Critical Care bed is not available and the decision to proceed will be determined by the likelihood of that level of care being required.
A prospective audit was performed over two weeks to capture all patients under-going elective and emergency neurosurgery at the Walton Centre. Post-operative delirium as detected using the 4AT score, a rapid and validated bedside screening test for delirium. A retrospective case note review was subsequently performed on patients identified as having post-operative delirium. The objective was to discover the incidence of post-operative delirium in Neurosurgical patients and what management is required and to help decide whether the capacity of the Neurointensive care unit needs to be considered when deciding whether or not major elective Neurosurgical operations can proceed.
A total of 67 patients were identified during the audit period (38 female, 29 male, mean age 61.4). The mean duration of surgery was 2.5 hours. Approximately 60% of cases were spinal surgery and 30% intracranial surgery, with 10% being interventional neuroradiology procedures. 67% of anaesthesia was delivered using total intravenous anaesthesia (TIVA). Only 8 (11.9%) patients scored 3 or above on the 4AT score indicating possible delirium.
Of the patients identified as having post-operative delirium there was no notable difference in age, type of surgery (spinal vs intracranial), anaesthesia technique, use of intra-operative opiates or baseline patient risk factors.
On reviewing the case notes of each patient, none required any pharmacological management for delirium beyond analgesia for surgical pain. No patients required escalation of care to high dependency or intensive care. It was often noted that simple verbal reassurance and reorientation was effective.
This audit identified that post-operative agitation or delirium occurs in approximately 10% of patients undergoing neurosurgery. However, this settled with reorientation, reassurance and occasionally further analgesia. There were no serious sequelae or unplanned Critical Care admissions. One hypothesis for the low rates of post-operative delirium may be the stricter blood pressure targets generally adhered to during neuroanaesthesia.
Patients judged as high risk for post-operative delirium should not have their surgery delayed for lack of a Critical Care bed that would otherwise not be required.
0121
Sound and Sleep in Intensive Care; a study from the intensive care unit of a district general hospital
Jaspal Singh1 and David Hepburn2
1Cardiff School of Medicine, Cardiff, United Kingdom
2Royal Gwent Hospital, Newport, United Kingdom
Abstract
Sound in an Intensive Care unit (ICU) is unavoidable. Biomedical machinery and staff discussions are major sources of noise in intensive care. Excessive noise interferes with sleep architecture and ultimately leads to sleep deprivation, increasing ones predisposition to ICU-delirium1 and extending ones hospital recovery period.
The World Health Organisation (WHO) recommends sound in hospitals exceeds no more than 40 decibels (dB) and 35 dB during the day and night respectively.2 Is the 12-bed ICU of the Royal Gwent Hospital (RGH) meeting this recommendation? Furthermore, noting the number of hours of disturbed sleep critically ill patients achieve on the unit, across the same nights sound levels are monitored, should reveal the degree to which sound, alongside other environmental aspects, impacts sleep architecture.
Over 8 nights, sound levels in different locations across the unit were objectively recorded via a specialised application (pre-calibrated to the American National Institute for Occupational Safety and Health). Tailor-made sleep disturbance proformas were completed by staff overseeing each bed-space over the same 8 nights sound was monitored. To gain a subjective insight, patients were asked specific questions regarding sleep quality and sleep disruptions during an intensive care follow-up clinic.
A nocturnal mean sound level of 58.9 dB(A) (maximum: 101.5 dB(A), minimum: 47.0 dB(A)) was obtained, with daytime mean sound levels at 65.6 dB(A). 61 proformas were completed showing that on average per hour, approximately 33% of patients on the unit at that time had disturbed sleep. A Spearman’s rank correlation coefficient value of Rs: −0.343 (p value: 0.50) indicates a weak negative correlation between sound levels and sleep disturbances. Patient feedback highlights the importance of excessive sound precipitating sleep disturbances with 80% noting a sleep pattern disturbance and 60% attributing this to excessive noise.
Noise on the ICU of the RGH exceeds the WHO’s recommendations. Numerous factors contribute to circadian irritation therefore the degree to which sound does is difficult to truly assimilate, however patients did highlight the issue of excessive sound pollution. Further efforts should be made to investigate the role of sound with regards to sleep architecture, so that methods to mitigate excessive noise to preserve sleep quality can be implemented in future practise.
0122
Introduction of Universal HIV testing in critical care – time for a change of heart
Mohammed Arshad1, Meera Raithatha2, Fayaz Roked3 and Mamta Patel1
1University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
2SWBH NHSFT, Birmingham, United Kingdom
3National hospital for neurology and neurosurgery, London, United Kingdom
Abstract
Introduction: Infection with human immunodeficiency virus (HIV) has now become a chronic treatable disease rather than the untreatable invariably fatal disease it once was. It has been shown that HIV infected patients treated successfully with antiretroviral therapy can have a life expectancy close to that of the general population.1 Early detection of HIV is important in order to improve long term prognosis.1 In many healthcare settings, including antenatal care and sexual health clinics, universal HIV testing is routine. However, despite being a high risk cohort of patients, this is currently not the case in adult critical care (ICU). A large study looking at over 1000 patients admitted to an ICU showed 30% of patients had indications for HIV testing according to UK national testing guidelines but only 6% of admissions were tested for HIV.2,3 A recent large systematic review and meta-analysis has also shown that initiation of highly active anti-retroviral therapy on ICU for patients improves both ICU mortality and long term (>90 day) mortality.4 These are strong arguments for ensuring timely and appropriate HIV testing of patients admitted to ICU.
Sandwell and West Birmingham Hospitals (SWBH) is in an area of Birmingham that has a high prevalence of HIV (2.7 per 1000 population).5 Our objective was to implement a universal screening system in SWBH critical care in order to improve rates of HIV testing as a quality improvement initiative. We present our experience and results of implementing a universal HIV screening system.
Methods: We conducted a retrospective review of 100 ICU admissions in January 2017 across SWBH. We looked to see if the patients met criteria for a HIV test as per national reccomendations.3 We then looked to see if patients were screened for HIV. Following the initial review, we implemented a universal HIV testing system for all emergency admissions to SWBH ICUs. We then repeated a retrospective review of 100 ICU admissions in June 2018 and again looked at how many patients met criteria for testing and how many patients were actually tested.
Results: The initial review in January 2017 showed 30% (30/100) of patients had indications for HIV testing but only 50% (15/30) of these patients were tested. The proportion of admissions to ICU that meet criteria for testing at SWBH were similar to those mentioned in the literature.2 Following the implementation of universal screening, the review in June 2018 showed that 35% (35/100) of admissions had indications for testing and 69% (24/35) of these were tested (figure 1). Our results show that implementation of a universal HIV testing system for admissions to ICU is possible and results in a greater proportion of patients being screened appropriately.
Conclusions: The introduction of a universal HIV testing system on adult ICUs is feasible and results in a higher proportion of at risk patients being screened. Universal HIV testing for emergency adult ICU admissions is now routine at SWBH. We suggest HIV testing should be universal in all ICUs with a high local population prevalence of HIV.
Figure 1.
0123
Improving Quality of handover in critical care unit
Arenahalli Neelakanta Anil Kumar and ShashiKumar Chandrashekaraiah
Lancashire Teaching Hospitals NHS Foundation Trust., Preston, United Kingdom
Abstract
Introduction: Handover is an important part of patient care especially in critical care. High quality handover is crucial in maintaining continuity of care and improving patient safety.1 Along with communication of appropriate clinical details,2 good handover should happen in a time bound manner in a dedicated place, without interruptions(1,3).
Background and Objectives: There has been a major change in patient number, case-mix and junior doctors staffing at LTHTR critical care. The unit has expanded from a 20-bedded unit with 10 to 12 UK trained doctors, on a 2-tier rota to a 28-bedded unit with 24 junior doctors on a 3-tier rota, of which 60% are International medical graduates (IMGs). IMGs have always felt communication and inter-personal skills as one of the barriers during integration into NHS and there was concern that this would affect the quality of handover. Along with implementation of the recommendations from handover audit in 2013, several other measures were introduced which included increasing handover time from 30 to 45 mins, handover guide document to aide juniors/IMGs and regular simulation training for IMGs on communications and inter-personal skills. The aim of this re-audit was to assess the quality of handover using the “Quality and safety of handover in intensive care” a compendium of audit recipes, RCOA4 as the standard.
Methods: This is a prospective audit where we collected data on percentage of key staff attending, handovers starting within five minutes of scheduled time, interruptions during handover and percentage of relevant information handed over. Relevant information included patient identification, history, diagnosis, significant recent events, current issues and daily goals among others. Data was collected over a month by an independent senior staff, a band 7 nurse or senior trainee. It included final overall score for the handover out of 5.
Results: Handover was done in a separate room near ICU. It started within 5 minutes of designated time (0% delay). 67% of times, late coming staff were junior doctors whereas consultants (22%) and nurses (11%) scored better. Out of all the interruptions, 50% was due to on call bleep and remaining were patient care (37.5%) and phone calls (12.5%). However, there were no non-essential interruptions (0%). Out of 411 patients handed over, some of the important aspects like Diagnosis (72.5%), significant recent events (73.96%) and current issues (75.66%) were talked about more than History (32.84%) and Daily goals (27%). Overall quality of handover was slightly better compared to previous time (3.63 vs 3.43)
Conclusion: Both individuals and organisation have equal responsibilities in maintaining high quality handover and this can be achieved by providing adequate and dedicated time as well as location for handover to take place. Also important is training and support aimed specific to the staff group and regular review of these interventions to changing unit demographics to sustain the quality of handover. In our unit, after all the interventions mentioned above, the overall quality of handover was slightly better compared to previous time despite new International medical graduates.
0124
Red Flag Sepsis for Prediction of In-Hospital Mortality
Dr Barbara Salas1, Dr Ben Messer2, Iain McCullagh2, Melissa Burnside2, Dr Rachael Malligan2, Dr Ewan Hunter2, Dr Phil Laws2 and Ashley Price2
1Newcastle University Medical School, Newcastle upon Tyne, United Kingdom
2Newcastle Hospitals NHS Foundation Trust, Newcastle upon Tyne, United Kingdom
Abstract
Sepsis is a life-threatening multi-organ dysfunction that occurs due to a dysregulated immune response to infection1–3. It carries significant morbidity and mortality, and early identification is essential.4
We aimed to evaluate the predictive value of routinely collected clinical observations (in particular Red Flag Sepsis [RFS]) in order to identify highest risk patients diagnosed with Sepsis. This was the first step of a quality improvement (QI) project. After completion of the second part of the project (expected by 12/2019), we hope our results will inform subsequent electronic data gathering and future clinical practice.
We analysed the data from patients that arrived in the Emergency Department (ED) of two tertiary academic hospitals with signs of infection and were assessed by a clinician. If Sepsis was suspected, the “Sepsis 6 Order Set” was activated. The order was later identified by a data manager, who reviewed the clinical data and collected the desired parameters on Excel.
Binary logistic regression and Chi-square test were performed with IBM-SPSS to assess the impact of systolic blood pressure, lactate, heart rate, patient response/unresponsive, respiratory rate, oxygen saturations and rash on the likelihood that patients would survive or die.
117 patients aged >18 years were included in the study. In-hospital outcome was tested with each of the RFS variables. The only statistically significant RFS for predicting in-hospital mortality was lactate >2 mmol/L (OR: 8.906; CI 1.8-44.073; p = 0.007).
In summary, of the RFS, only lactate >2 mmol/L was statistically significant for prediction of in-hospital mortality. The analysis also showed that “Sepsis 6” is currently imperfectly adhered to, and that paper-based data collection has limitations; we will next testthe RFS with electronic data only.
0125
Euglycemic DKA – an evil of SGLT2 inhibitors, a newer age OHA
Soumyanil Saha
Leeds Teaching Hospital NHS Trust, Leeds, United Kingdom
Abstract
Background: Sodium-glucose cotransporter 2 (SGLT2) inhibitors (gliflozins) are newer hypoglycemic agents (OHA) for type 2 diabetes mellitus that prevent reabsorption of glucose at proximal renal tubules. Treatment reduces body weight, ameliorates insulin resistance, dyslipidemia, and nonalcoholic fatty liver disease. Their favourable clinical profile has increased interest in SGLT2 inhibitors. Diabetic ketoacidosis (DKA) is potentially life threatening acute complication of diabetes. Typically associated with marked hyperglycemia and dehydration, can also less commonly occur with moderately increased or normal blood glucose (BG) levels, latter being known as euglycemic (eu)DKA, was originally defined as DKA with a BG level < 16.6 mmol/dL, now recognized in BG < 11.1 mmol/dL. euDKA develops mostly in type 1 diabetes, rarely type 2 diabetes (1). Absolute/relative insulin deficiency leads to reduced glucose utilization and enhanced lipolysis; increased delivery of free fatty acids (FFAs) to the liver,raised glucagon levels promotes FFA oxidation and production of ketone bodies. In euDKA, insulin deficiency and insulin resistance are milder, glucose overproduction and underutilization lesser than DKA. Renal glucose clearance being twice as large with euDKA than DKA. euDKA is pathophysiologically similar to DKA except for the SGLT2-induced glycosuria that “artificially” lowers plasma glucose levels and predisposes to increased ketogenesis. (2), the lower insulin-glucagon ratio stimulates lipolysis with higher circulating FFAs, and enhanced lipid oxidation at the expense of carbohydrate oxidation In the face of lower glucose concentrations, glycogen synthesis and lactate release also falls (3).
Case presentation: 52 M, background of type 2 Diabetes (on empagliflozin), was admitted acutely unwell on 14/05/19 with 1 week history of vomiting and abdominal pain, raised CRP, urea and lactate. CT showed high grade bowel obstruction,. 15/05 patient had Laparotomy for relieving of the SBO. Meckel's diverticulum was excised, adhesiolysis and bowel anastomosis performed and patient was transferred to the ward post-op. He started having high NEWS (>7) Day 2 PO, tachycardia >115, tachypnoea >50 (bilateral air entry), altered GCS, profound metabolic acidosis [ABG : pH 7.138, pCO2 1.9, pO2 14.2 on 40% O2, BE −21.8,Lact 1.8, Serum ketones 6.7, blood glucose of 14.2],quite unclear cause, abdomen being soft. Required intubation and ventilation on ICU for airway compromise secondary to poor GCS. No LV/RV impairment on FICE echo. CT showed bi-basal consolidation, mild ileus, but no evidence of anastomotic leak or ischaemia.
DKA protocol commenced with fluid resuscitation and i/v insulin fixed dose,with potassium and phosphate replacement, Piperacillin -tazobactum to cover potential chest +/−abdominal sepsis. oxygen was weaned down overnight and he was extubated by mid- day, SGLT2 inhibitor was suspended, blood gases normalised within the next half day with good urine output and improving U&Es. He was discharged to the ward the day after, on TPN for ileus, with alternate glucose control.
Conclusion: euDKA, though rare, is potentially easily reversible and needs to be considered in differential when faced with such situations.
Image (2) : TGD, tissue glucose disposal; UGCr, urinary glucose clearance rate; EGP, endogenous glucose production.
0126
An intervention program to improve the quality of intubation of critically ill adults at Lincoln County hospital
James Shilston1, Louise Potter2, Yusuf Ghumra2 and Russell Barber3
1ST-5 ICM & Anaesthetics, Health Education East Midlands, Nottingham, United Kingdom
2ST-6 Anaesthetics, Health Education East Midlands, Nottingham, United Kingdom
3Consultant in ICM and Anaesthesia, United Lincolnshire Hospitals NHS Trust, Lincoln, United Kingdom
Abstract
Introduction: In October 2017 the Difficult Airway Society released guidelines1 for intubation of the critically ill adult patient as a “direct response” to the 4th national audit project2 of the Royal College of Anaesthetists that “highlighted deficient management of these extremely vulnerable patients leading to major complications and avoidable deaths”. As a group of senior anaesthetic / ICU trainees covering the ICU out of hours at a district general hospital we recognised the value of this guideline’s progressive recommendations and utilised them to try and improve the care of critically ill adults requiring intubation at Lincoln County Hospital.
Objective: Our primary objective was to instigate a staggered raft of educational interventions based on the new guideline targeting key audiences of: senior clinicians, trainees, operating department practitioners and critical care nursing staff over a 5-month period. Guideline themes promoted included a team approach, use of checklists to aid communication and expert tuition on technical proficiency. Our secondary objective was to collect data on all critically ill patients undergoing intubation who were admitted to ICU over this time period for a quality of care assessment.
Methods: Educational Interventions included: 1) An afternoon training session for trainees on videolaryngosopy and simulation from the trust airway lead 2) In situ simulation for ODPs and ICU nursing staff 3) Presentations at department meetings 4) Development of and integration of an airway checklist. Data from the intubation of all critically ill patients who were admitted to ICU was collected on: grade of intubator, pre-intubation resuscitation, pre-oxygenation, induction and neuromuscular blocker agent and dose, laryngoscope used, adverse events documented.
Results: We delivered educational sessions as outlined above. We captured data from 43 patients who underwent intubation over a 5-month period. Using a run plot we have demonstrated a trend to reduction in documented adverse events and increase in resuscitation prior to intubation over the 5 months.
Conclusion: National Guidelines are only effective if implemented at the “coal face” by front line staff. Established clinical practice can be challenging to change in the face of new recommendations, often ingrained by previous dogma and individual biases. We have demonstrated that implementing these guidelines as interventions that focus on the airway team as a whole may improve the quality of care around intubation of our sickest patients in a busy district general hospital setting.
Table 1.
Number of Level 3 patients admitted, their documented adverse event rate and pre-intubation resuscitation performed.

|
Chart 1. Run plot to show percentage of documented adverse events and pre-intubation resuscitation per month.
0128
Predicting mortality following traumatic brain injury or subarachnoid Haemorrhage: A comparison between the standardised mortality ratios obtained from the APACHE II and ICNARCH-2018 models with that of the overall population
Matt Rowe, Jules Brown, Julian Thompson and Aidan Marsh
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Background: Standardised mortality ratios (SMR) are an established means by which to measure the quality of critical care delivery in the United Kingdom (UK). The APACHE II and ICNARCH-2018 models are widely used in UK Intensive Care Units (ICU) in order to calculate SMR values against which the effectiveness of critical care measures can be evaluated.1 This study sought to assess the validity of these scoring systems in predicting mortality for patients admitted with traumatic brain injury (TBI) or aneurysmal subarachnoid haemorrhage (SAH) in whom the Glasgow coma score (GCS) may significantly impact on outcome.
Methods: A retrospective analysis of all UK intensive care unit admissions in a one-year period was performed. We compared the performance of the two models in the whole population against their performance in two subgroups (SAH and TBI) for three GCS levels. We then replicated this analysis in the patients admitted to a regional tertiary neuro, general and trauma centre ICU over a three-year time period.
Results: Overall, both models appear to predict mortality well for the overall population of patients admitted to critical care with a TBI or SAH. SMR values obtained, were 1.00 (95% CI 0.96–1.04) and 0.99 (95% CI 0.95–1.03) for the APACHE II and ICNARCH-2018 models respectively. However, when grouped by GCS, both models appear to significantly under predict mortality in patients who had an admission GCS of ≤ 8 [SMR 1.1 (95% CI 1.05–1.15)] or in those for which the GCS was missing or unavailable due to sedation [SMR 1.88 (95% CI 1.77–1.99)]. This pattern was replicated when analysing local data.
Discussion: Both the APACHE II and ICNARCH-2018 models appear to under predict mortality in patients suffering from TBI or SAH in patients where admission GCS is low or unrecordable. The impact of this effect on unit SMR will be amplified by increasing regional centralisation of brain injury treatment and by recent guidance to institute early neurocritical care prior to ICU admission.2,3 This raises important questions as to how accurately we can evaluate current critical care treatments, monitor potential improvements in care and perform comparisons between critical care centres.
Funding: The Southmead Hospital Intensive Care Unit Charitable Funds funded the ICNARC fee for access to national CMP data and initial analysis
| APACHE II (2013) | Combined |
Traumatic Brain Injury |
Aneurysmal SAH |
|||
|---|---|---|---|---|---|---|
| N | SMR (95% C. I.) | N | SMR (95% C. I.) | N | SMR (95% C. I.) | |
| GCS ≤ 8 | 1167 | 1.10 (1.05, 1.15) | 616 | 1.13 (1.05, 1.21) | 551 | 1.08 (1.01, 1.14) |
| GCS 9-15 | 3110 | 0.25 (0.21, 0.29) | 1131 | 0.37 (0.30, 0.46) | 1979 | 0.17 (0.13, 0.22) |
| GCS unrecordable* | 2067 | 1.88 (1.77, 1.99) | 1441 | 1.87 (1.72, 2.03) | 626 | 1.88 (1.73, 2.03) |
*GCS not available due to patient sedated and/or paralysed the whole of the first 24 hours
0129
Enterovirus D68 and acute flaccid paralysis – the new Polio epidemic in waiting?
Yang Min Ng1, Syeda Nafisa1, Pulak Paul2 and Milind Sovani1
1Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
2Sherwood Forest Hospitals NHS Foundation Trust, Sutton in Ashfield, United Kingdom
Abstract
Introduction: Enterovirus D68 (EV-D68) is a non-polio enterovirus sometimes implicated in respiratory illnesses.1 EV-D68 has recently been linked to acute flaccid paralysis (AFP) particularly affecting children.2 We report a case of a young adult presenting with acute neurological features linked to EV-D68 with subsequent prolonged recovery.
Case Presentation: A 22 year old gentleman presented to hospital with a 3 day history of productive cough and fever with 1 day history of headache, visual blurring and facial weakness. He was found to have global flaccid weakness with evidence of bulbar palsy. He was initially treated with intravenous antibacterial and antiviral therapy but rapidly deteriorated necessitating intubation and ventilation. Magnetic resonance imaging of the brain revealed abnormal high signal within the midbrain and dorsal pons/medulla. Cerebrospinal fluid analysis revealed high protein and pleocytosis. He was transferred to a tertiary neurology centre and was treated with intravenous immunoglobulin for presumed Miller Fisher Syndrome with no response. Bronchoalveolar lavage analysis later confirmed presence of EV-D68.
The patient received a percutaneous tracheostomy and had a prolonged stay in Intensive Care. He had quadriparesis with diaphragmatic palsy. An attempted decannulation at 6 months was unsuccessful due increased oral secretions and bulbar dysfunction. At 8 months he currently has an uncuffed tracheostomy but remains reliant on overnight non-invasive ventilation. He has regained limited function of his extremities, but requires ongoing assistance with all care.
Conclusion: Epidemiological studies have strongly suggested the association between AFP and EV-D68.2 The United Kingdom AFP Task Force identified 40 AFP cases in 2018, the majority affecting children.3 A large number of these patients required critical care admissions, and a significant proportion had prolonged neurological deficit.3 Diaphragmatic and bulbar palsies, such as in our patient, can be particularly difficult to manage. However, the natural history of this disease remains unclear, and it is uncertain why some patients with EV-D68 are more susceptible in developing AFP. Should the prevalence of EV-D68 increase in the future, the incidence of AFP may rise, with potential massive implications towards the provision of critical care and respiratory support for affected patients. Further studies are required to further elucidate the pathophysiology, progression and management strategy for this disease.
0130
Should High Flow Nasal Oxygen be used in patients with respiratory failure and metastatic malignancy?
Laurie Anderson, Bethan Walker, Frances Edwards, Kate Tredgett, Adam Usher, Simon Webster and David Windsor
Gloucestershire NHS Trust, Cheltenham, United Kingdom
Abstract
Introduction and Background: High Flow Nasal Oxygen (HFNO) is a relatively new(1) treatment for type 1 respiratory failure, usually administered in Respiratory High Care or Intensive Care. When used first line, it is associated with a reduction in both mortality and the need to escalate to Invasive Ventilation when compared to Non-Invasive Ventilation (NIV)(2). It is not tolerated as well as standard oxygen therapy but is better tolerated than NIV(3), and has been shown to be an effective way to reduce dyspnoea in patients with malignancy(4).
Methods: We examined the outcomes in a single oncology centre, for solid cancer and haematology patients with respiratory failure requiring HFNO. We conducted a retrospective review of 18 months of admissions to ITU for HFNO (21 patients), and six months for those admitted to Respiratory High Care (eight patients). The type of malignancy, reason for respiratory failure, evidence of an advance care planning (ACP) discussion (including preferred place of death) and the duration of HFNO therapy were all examined. Findings were consistent regardless of where HFNO was administered.
Results: All 17 patients with metastatic cancer, and sepsis as their primary cause of respiratory failure died either on HFNO, or as a result of weaning with palliative intent. Although only three patients had a curative malignancy and cancer treatment induced complication (eg. neutropenic sepsis), survival to discharge for this group was 100%. Evidence of ACP in the medical notes was lacking in over 60% of all patients receiving HFNO. If patients successfully weaned, this was generally within three days of commencing HFNO.
Conclusions:
1 HFNO did not improve survival for patients with metastatic cancer, particularly when respiratory failure is caused by sepsis. These patients died whilst receiving HFNO or shortly after weaning, meaning they received end of life care in a high care setting. Since there is often a lack of ACP, this might mean we are not meeting patient’s preferred place of death.
2 If overall survival is not improved, do we need to be explicit with patients about anticipated outcomes associated with HFNO? With no improvement in survival, perhaps HFNO should not be offered to this patient group. An alternative strategy would be to offer HFNO with the sole aim of providing symptomatic relief of dyspnoea. This raises a further question of whether this represents an appropriate use of resources.
3 Early involvement of specialist palliative care can improve symptom control for this group without relying soley on HFNO, and provide support for palliative weaning, if appropriate. Our findings suggest this should particularly take place if there has been no improvement within three days. Ideally ACP conversations ahead of the patient developing sepsis and respiratory failure may prevent emergency use of HFNO and admission to a high care setting, where this was not their preferred choice. Incorporating these discussions into already established frameworks such as ReSPECT, or as part of DNACPR decision-making could be one way to move this forward in the future, with HFNO becoming more widely available in UK hospitals.
0133
Out of Hospital Cardiac Arrest Care – Are we as good as we think? A Regional Audit
Amy Hill, John Culshaw and Timothy Astles
Aintree University Teaching Hospital, Liverpool, United Kingdom
Abstract
Introduction: An estimated fifty thousand people suffer an out of hospital cardiac arrest (OOHCA) each year, with an associated mortality of >90% attributed to neurological injury.1
Therapeutic hypothermia post OOHCA was standard care until recently, when evidence comparing temperatures of 33 versus 36 degrees for 28 hours showed no neurological benefit.2 Since then, a variance in practice surrounding temperature control, sedation duration, and timing of prognostication has been noted within and between intensive care units in the North West.
Consensus statements advise active temperature control for at least 24 hours (32–36 degrees), and prognostication no earlier than 72 hours post OOHCA, except in select cases e.g. brain stem death.2,3,4,5
Objective: To assess how far Mersey deviated from the evidence and recommendations surrounding post arrest temperature control and prognostication.
Method: A prospective audit of all intensive care units (ICU's) within Mersey over a 6-month period, including any patient admitted to ICU for OOHCA care. An identified person at each hospital completed a standard proforma, which was collated by a member of the audit team.
Results: 58 responses were received. Mean age was 62 years, with 94% being male. The causative rhythm was VF in 50% (29/58), PEA in 24% (14/58), asystole in 23% (13/58), and VT in 3% (2/58). Most OOHCA’s were witnessed (82%, 48/58), and most received bystander CPR (88%, 51/58). The majority of patients had a documented downtime of 40 minutes or less (84%, 49/58). A high proportion of patients had a low GCS on arrival to hospital (GCS 3/15 in 87%).
Presenting temperature was less than 37 degrees in 83% of patients. Targeted temperature management was only planned in 41 patients (71%). The most common method of temperature control was via the Arctic Sun device (26/41, 63%). Of the 53 patients in whom temperature was documented on day 1 post arrest, 24 patients had a temperature >37.1 degrees at least once, with 9 patients having a temperature >38 degrees on one or more occasion. Temperature control became less tight on day 2 post arrest, with 28 patients having a temperature >37.1 degrees (10 patients with a temperature >38 degrees). Temperature was recorded less reliably on day 3 post arrest, but 15 patients were noted to have a temperature above 37.1 degrees (3 patients with a temperature >38 degrees) at least once.
Early sedation breaks (within 24 hours) were performed in 25% of patients, and formal neurological prognostication was conducted at <72 hours in 57% (25/44). A combination of clinical examination and CT scanning were the most common modalities of assessment. Planned withdrawal of ICU treatment took place in 40 patients, 10 of whom died <24 hours post ICU admission.
Of the 42/58 patients that died, 32 deaths were attributed to a neurological cause.
Conclusion: Since the TTM trial, there appears to be a wide variation in clinical practice around post-arrest management. The trend towards higher temperatures, earlier sedation holds, and earlier neurological prognostication does not follow current guidelines, and is not supported by evidence.
0134
The Effect of Cardiac Output Monitoring on Intravenous Fluid Administration in Gynae-Oncology Surgery
Anna Newton, Gurmukh Chandan and John Bleasdale
Sandwell and West Birmingham NHS Hospitals., Birmingham, United Kingdom
Abstract
Current guidance advocates a restrictive approach to intra-operative fluid management in gynae-oncology surgery including the ERAS pathway (1). The use of cardiac output monitoring to guide fluid management in major surgery has been controversial (2, 3). ERAS guidelines for gynae-oncology surgery recommend goal-directed fluid therapy, which ‘may be facilitated by the use of minimally invasive haemodynamic monitoring’ (4).
This project investigated the intraoperative fluid management of patients undergoing major gynae-oncology surgery. Particularly, it assessed relationship between volume of fluid administered and prognostic indicators; drops in serum albumin and length of stay (LOS) in hospital and critical care, and the impact of cardiac output monitoring in fluid administered.
All patients (n = 64) admitted to our intensive care unit following Gynae-oncology surgery in from September 2017 to September 2018 were included. Data was collected from anaesthetic charts and patient notes. Cancer stages from 1 to 4 were represented in the sample (S1: 23%, S2: 8%; S3: 45%; S4: 25%). The majority had ovarian cancer. Operations lasted between 1.25 and 10 hours.
Total volumes of fluid varied considerably with a range of 1 L to 26 L (median: 5.6 L, IQR: 3.2-8.3 L). There was a linear association between amount of fluid given intraoperatively and the degree of albumin drop (p = <0.001). This remained true when the rate of fluid given intraoperatively was considered (p = 0.0023). There was an average albumin drop of 12.9 g/L in patients with no ascites vs 13.8 g/L with ascites. Intraoperative cardiac output monitoring did not reduce the intraoperative fluid use with an average of 6.2 L given when monitoring was not used, and 7.8 L when it was (non-significant; unpaired t test, p = 0.22). Albumin drop averaged 14.3 g/L in the patients where cardiac monitoring was used vs 12.7 g/L otherwise (non-significant; unpaired t test, p = 0.36). When cardiac output monitoring was used there was an average LOS of 11.35 days vs 9.85 days (non-significant on unpaired t test, p = 0.08).
The data showed no significant effect (both in total volume of fluid used and albumin drop) when cardiac output monitoring was used. However, no data was available on the reasons cardiac output monitoring was employed. This could be due to variations in individual practice, perceived complexity of case, but did not correlate with anaesthetic length (5.27 vs 5.75 hrs).
Larger volumes of IV fluid were associated with greater albumin drops, which has been demonstrated as a marker of poor prognosis (5). Our results showed a correlation between albumin drop and length of hospital stay, but not LOS in critical care. Notably, neither quantity of metaraminol used (mg) nor volume of interoperative fluid administered correlated significantly with total length of stay.
All patients survived to discharge; no data was collected on other complications.
Our findings suggest caution when advocating routine use of cardiac output monitoring in major gynae-oncology surgery, and suggest there is further scope for optimising practices in intra-operative fluid administration. Further research could examine more direct measures of poor outcome, such as survival and complications.
0135
Ventilator associated pneumonia on the intensive care unit in a teaching hospital and regional trauma centre general intensive care unit: Outcomes, patient characteristics and future directions for care
Benjamin Welham, Michael Ball and Ahilanadan Dushianthan
General Intensive Care Unit, University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom
Abstract
Introduction: Ventilator associated pneumonia (VAP) is a relatively common hospital acquired infection in the intensive care unit (ICU) setting and associated with significant morbidity and mortality. Studies have shown that VAP affects approximately 8–28% of intubated patients on the ICU, with a mortality of 24–76% (1,2). A key issue is the lack of a consensus definition for the diagnosis of VAP (3). Although, several definitions, scoring systems and tools exist, no ‘gold standard’ criteria have been agreed upon (3,4,5). It is therefore imperative that there are continued advances in our understanding of this condition and measures are in place for prevention, early identification and prompt, effective treatment.
Objectives: This retrospective study aimed to assess the management and outcomes of VAP in our ICU at a regional general intensive care unit trauma centre.
Methods: Electronic records of patients admitted to the ICU between 1st February 2016 and 31st January 2017 were reviewed. Patients who had been prescribed antibiotics specifically for the treatment of VAP were identified from an electronic database (MetaVision, iMDsoft). Four main domains were reviewed; Presence of objective evidence of VAP as defined by the HELICS protocol (5), microbiological sampling to assist the diagnosis of VAP/pneumonia, appropriate antibiotic prescribing (based on hospital guidelines or microbiological sensitivities) and whether antibiotic duration was eight or fewer days according to established guidelines.
Results: 1583 patients were admitted over this 12-month period. Forty-two patients were identified as having developed VAP. Two patients were excluded as admission records were unavailable. Twenty-nine patients were male, mean age was 61.3 and mean number of days intubated was 17.9 (median 13.5). Early onset VAP (<5 days after intubation) was seen in 40% of cases. Reasons for admission were trauma (30%), post-surgical (23%), cardiac arrest (13%) and other medical cause (35%).
Four main standards were assessed:
1. Twenty-two patients (55%) had objective evidence of VAP consistent with HELICS criteria.
2. Microbiological sampling was performed in 90% of patients
3. Appropriate antibiotics were prescribed in 80% of the cohort
4. Duration of antibiotics was ≤8 days in 65% of patients
The most common pathogens isolated from endotracheal samples and bronchial washings following diagnosis of VAP were coliforms (40.0%). Yeasts (17.5%), methicillin sensitive Staphylococcus aureus (15.0%) and Pseudomonas aeruginosa (15.0%) were also commonly seen. Positive microbiology results were available in 77.5% of patients after diagnosis. Mortality of the cohort was 25% at 30 days.
Conclusions: The data suggests that, despite appropriate antibiotic therapy, mortality remains high for those who develop VAP, which is in line with previous data (2). Pathogens isolated from these patients were typical for VAP (4). Diagnosis remains a difficult issue, with only 55% of patients meeting the HELICS criteria in this dataset. With no clear definition of VAP, this result was expected, and continues the call for gold standard diagnostic criteria. Implementation of local guidelines or assessment tools might assist clinicians whilst this is awaited. Our unit is currently in the process of developing a VAP diagnostic pathway for implementation in the near future.
0136
Do-not-resuscitate decisions in critically ill cancer patients on the Intensive Care Unit- a single centre retrospective cohort study
Esther van der Zee1, Jelle Epker1, Jan Bakker1,2,3,4, Dominique Benoit5 and Erwin Kompanje1
1Erasmus Medical Center, Rotterdam, The Netherlands
2New York University NYU Langone Medical Center, New York, The United States of America
3Columbia University Medical Center, New York USA, The United States of America
4Pontificia Universidad Católica de Chile, Santiago, Chile
5Ghent University Hospital, Ghent, Belgium
Abstract
Introduction: Decisions to withhold resuscitation in case of a circulatory arrest or in other life-threatening medical emergencies (do-not-resuscitate (DNR) decisions) are part of routine hospital practice.1 When properly executed, a DNR order is a useful method to ensure that preferences of a patients regarding CPR are honoured.2 However, the Intensive Care Unit (ICU) is an environment in which DNR decisions with patient involvement is almost always absent, as the majority of the ICU patients lack decision-making capacity.3 Advanced directives of patients are often not known. The number of patients with a malignancy admitted to the ICU has increased.4 Subsequently, DNR decisions in cancer patients admitted to the ICU may have to be made more frequently. Literature shows that stigma among health care providers concerning cancer patients do occur and that having a malignancy is associated with more DNR decisions made by the medical team.5
Objective: The aim was to provide an insight in DNR decisions in cancer patients admitted to the ICU.
Methods: We conducted a retrospective observational cohort study. By using our hospital database, we identified patients with and without a malignancy, admitted to the ICU in 2017. A DNR order was defined as an instruction not to perform cardiopulmonary resuscitation in case of a cardiac arrest, or an instruction not to perform other life-saving treatments, such as tracheal intubation and mechanically ventilation in case of respiratory insufficiency. We used an univariate and multivariate logistic regression analysis to identify factors associated with DNR orders.
Results: Of the 2486 patients admitted during the study period, 470 were cancer patients (18.9%). A higher incidence of DNR decisions in cancer patients prior to ICU admission was seen compared to our general ICU population (8.5% vs. 3.8%, p-value < 0.001). During ICU admission, a DNR decision was made in 8.9% of the cancer patients and in 8.6% of the patients without cancer (p-value 0.83). Age (OR 1.06, 95% CI 1.02−1.09, p-value 0.001), a haematological malignancy (OR 3.4, 95% CI 1.37−8.46, p-value 0.01), an unplanned ICU admission (OR 28.6, 95% CI 10.9-74.9, p-value <0.001), the SOFA score (OR 1.27, 95% CI 1.16−1.38, p-value <0.001) and sepsis (OR 12.8, 95% CI 6.39−25.6, p-value < 0.001) were associated with a DNR order during ICU admission. However, in a multivariate binary logistic regression analysis, only age (OR 1.04, 95% CI 1.00-1.08, p-value 0.04) and SOFA score (OR 1.27, 95% CI 1.16−1.38, p-value <0.001) remained as predictor of a new DNR order during ICU admission. All the DNR decisions during ICU admission were made by the medical team, only 2 included patient’s wishes as well (4.8%).
Conclusion: DNR decisions during ICU admission are generally made by the medical team and may not be determined by the presence of cancer, but by the severity of the critical illness and age. The presence of a malignancy was associated with a higher incidence of DNR decisions prior to the ICU admission.
0137
The benefits of an ‘elective’ to a lower middle income country as a senior trainee in EM/ICM
Ruth Creamer
Derriford Hospital, Plymouth, United Kingdom
Abstract
Objective: To gain experience in Emergency Medicine and Trauma in a lower middle income country as a senior trainee (during the second year of stage 2 training as a dual ICM/EM trainee)
Background: Emergency Medicine and ICM Registrar's rotas are gruelling, and finding an opportunity to be released for out of programme experience can be problematic; I used a combination of study leave and annual leave to spend 3 weeks at Nanyuki Teaching and Referral Hospital, (NTRH) Kenya, during my ST6 year of Emergency Medicine.
NTRH is a government funded referral hospital serving Laikipia County. Patients rarely arrive by ambulance; they arrive on the back of motorbikes, tuk-tuks, cars and on foot brought in by friends/relatives and passers-by. They are completely undifferentiated with no pre-alerts. Approximately 80% of ED patients seen are discharged.
Methods/Design: Using pre-existing links between hospitals in the South West of England and NTRH I was able to spend an ‘elective’ style voluntary period in Nanyuki ED.
I was able to see how patients are managed in a resource poor environment, with significantly less emphasis on laboratory investigations. I had the opportunity to see conditions less frequently seen in the UK (TB, HIV, widespread hypertension in young patients) along with abundant trauma mainly in the form of RTCs. As a supernumerary doctor I was able to follow patients up as inpatients, and participate in hospital wide CME.
I witnessed teamwork beyond that I have encountered in even the best EDs I have worked at in the UK. Staff were adaptable to ever changing conditions, and always ensured that all team members had ‘taken tea’.
As NTRH had no intensive care facility limitations of care were a very real issue for the sickest patients presenting to ED. During the 3 weeks I spent there no patients were transferred out to a critical care facility, and the contrast with UK practise for some patients was sobering. The opportunity to spend time in a healthcare system where the issue of cost of investigations and care heavily influences medical and patient/family decisions was a very useful learning experience.
Results/Conclusions: I gained invaluable insight into working in a resource poor setting, saw conditions I had never seen or treated before and had the opportunity to share ideas with ED staff and discuss ideas for future projects and fellows. I gained just as much, if not more, from this relatively short trip as I did to the medical elective undertaken at the end of medical school. I have a renewed appreciation of the NHS, our access to critical care for the sickest patients and ability to treat based on clinical need not ability to pay, and would thoroughly recommend similar placements to senior trainees in EM and ICM.
0138
Introduction of the Critical care Pain observation Tool across four Critical Care Units
Helen Hill, Sachiko Pearce, Katherine Howe, Anna Brookes and Alison Davidson
University Hospital Southampton FT, Southampton, United Kingdom
Abstract
In 2017, a Trust Essence of Care audit concluded that in Critical care: 'Pain assessment was not always performed with each set of observations (as per Essential Care Standard) and reduced further in the unconscious patient'. Potentially patients may not have received appropriate analgesia as their pain was unrecognised. This was attributed to varied staff knowledge on the non-verbal signs of pain, and the computer information system (CIS) allowing staff to choose to document the option “unable to assess” pain.
We decided to introduce the Critical Care Observation Tool (CPOT)1 across Critical Care at University Hospital Southampton NHS Foundation Trust. This involved implementing a change in practice with over 350 nursing staff. It was essential that this change occurred simultaneously on all four, as each of these units is managed separately. Nursing staff are regularly moved between units to maintain safe staffing levels and any change on the CIS system will occur on all units. A Practice Development Sister on each unit facilitated the change in their area during July 2018, and a re-audit was performed in January 2019.
The results indicated that the introduction of CPOT led to improved compliance on performing pain assessments with each set of observations. They also indicated that more patients were being assessed as being in pain for two consecutive hours. This may be attributed to nurses’ improved ability to assess non-verbal signs of pain using CPOT
Further analysis of nurses’ ability to assess non-verbal pain is recommended. It is also recommended that further education around using the correct tool and documenting position of pain is required. A future audit will be performed to ascertain if use of CPOT is now embedded in practice.
The introduction of CPOT demonstrated how practice change could occur on four separately run Critical Care Units simultaneously. This enabled staff to have the knowledge and skills to work on one of the other Critical Care units within the same Trust to support safe staffing numbers as outlined by the Intensive Care Society2 whilst complying to best practice principles for relocating critical care staff.3
0139
The impact of serum calcium concentration during major bleeding: a systematic review
Adam Boulton1,2 and Joyce Yeung1,2
1University of Warwick, Warwick, United Kingdom
2Heartlands Hospital, University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Calcium is crucial in normal physiological and is of particular significance in the bleeding patient due to its role in coagulation, platelet adhesion, smooth muscle contraction, and myocardial function.1–3 Observational studies have suggested that hypocalcaemia during major bleeding is associated with poorer outcomes. Subsequently, there has been recent interest in a possible therapeutic role for intravenous calcium during major bleeding.4 It is therefore of timely interest to review the current literature investigating blood calcium concentration during major bleeding.
Objectives: To summarise the pre-clinical and clinical literature concerning serum calcium concentration and hypocalcaemia during the hyperacute phase of major bleeding. Specifically:
• What changes occur in serum calcium levels during major bleeding?
• What clinical outcomes are associated with serum calcium levels during major bleeding?
• Has intravenous calcium been used as a treatment during major bleeding and what were its clinical effects?
Methods: This systematic review was prospectively registered on PROSPERO. A sensitive literature search strategy was constructed. OVID SP was used to search MEDLINE and EMBASE databases and data extracted using predetermined criteria from 01/01/1980 to 25/01/2019.
Results: The search yielded 554 results, of which 27 met eligibility criteria and included 19 original studies and eight review articles. Screening of reference lists of returned review articles revealed no further studies for inclusion. Clinical studies included 5,349 patients and were all observational in design with nine retrospective and eight prospective assessments. One study did not explicitly state its design, whilst another was a single case report of major obstetric haemorrhage. Most were in the context of trauma (n = 11, 2,142 patients), with the remainder concerning non-traumatic intracerebral haemorrhage (ICH) (n = 3, 2,487 patients), a mixture of bleeding causes (n = 3), or thermal injury (n = 1).
From the included studies, hypocalcaemia was common with a reported incidence of 11–97%, reflecting the variability of inclusion criteria and hypocalcaemia definitions. Most studies (n = 13) defined hypocalcaemia using ionised calcium levels, with the majority using <1.12 or <1.0 mmol/L. For trauma studies, many found hypocalcaemia to be inversely correlated with injury severity and number of blood products transfused. Multiple studies found hypocalcaemia was associated with mortality and three determined hypocalcaemia was an independent predictor of mortality. All studies of ICH found hypocalcaemia to be associated with increased haematoma volume and risk of expansion. One study assessed the effect of therapeutic intravenous calcium (N = 60). Patients receiving calcium concurrently with blood products in the pre-hospital military setting had a lower incidence of hypocalcaemia upon hospital arrival, however no assessment of clinical outcomes was made.
Conclusions: Multiple observational studies have found that hypocalcaemia is common in the context of major bleeding and appears to be associated with mortality, however this may be confounded by increased blood transfusions and injury severity. Increasing blood transfusions appear to worsen hypocalcaemia in a dose-dependent manner, which may be due to its citrate content. There is a scarcity of evidence to determine the therapeutic effects of intravenous calcium during the hyperacute phase of major bleeding and therefore interventional trials may be warranted.
0140
Service evaluation of duration of antimicrobial therapy for community-acquired pneumonia in a single UK critical care unit
Robbie Crooks1, Aurelio Majorino1, Ian Clement1, Ali Robb2 and Tom Hellyer1,3
1Critical Care, Royal Victoria Infirmary, Newcastle Upon Tyne, United Kingdom
2Department of Microbiology, Royal Victoria Infirmary, Newcastle Upon Tyne, United Kingdom
3Institute of Cellular Medicine, Newcastle University, Newcastle Upon Tyne, United Kingdom
Abstract
The optimum duration of antibiotics for community-acquired pneumonia (CAP) requiring admission to critical care is not established, as few studies include this population (1). The National Institute for Health and Care Excellence recommends a 5 day course for low-severity CAP and a 7–10 days course for moderate-severe CAP (2). The British Thoracic Society recommends a 7–10 day course but extension to 14–21 days in some cases (3).
We aimed to determine the proportion of patients who receive shorter (≤7 days) duration antibiotic therapy for CAP.
We retrospectively collected data from the Royal Victoria Infirmary, Newcastle. Data were collected from electronic and paper records. Patients with CAP were identified using the codes: ‘pneumonia – bacterial’, ‘pneumonia – viral’ and ‘pneumonia – no organism isolated’. Diagnosis was confirmed on case notes review. Patients were excluded if a condition was present that would require longer antibiotic therapy. Patients with healthcare-associated pneumonia were also excluded. Consecutive days of antibiotic administration, without interruption for >24 hours, counted towards the total duration of antibiotic therapy. A sample size of 96 patients was required to detect a proportion of 50% of patients receiving a shorter duration, with a precision of 10%.
A total of 98 patients admitted between January 2018 and April 2019 were included. The mean age was 55 (SD 22), 46.4% were female, 26.7% of patients had a CURB-65 score of ≥ 3, and the mean APACHE II score was 17.0 (SD 6.6). ICU-mortality was 15.3% and the mean length of hospital and ICU stay were 12.3 (SD 13.2) and 6.6 (SD 7.8), respectively. Excluding 12 patients who died while receiving antibiotics, the mean duration of antibiotics was 7.7 days (SD 4.2). The proportion of patients receiving ≤ 7 days was 52.3%. The mean duration of antibiotics for viral pneumonia was 6.5 days (SD 3.5) and for culture negative pneumonia was 6.4 days (SD 2.9). Severity of pneumonia did not influence duration of antibiotics, with a mean duration of 7.5 days (SD 4.1) for patients with a CURB-65 score of ≤ 2 and 8.1 days (SD 4.2) for patients with a CURB-65 of ≥ 3.
There is variation in the duration of antibiotics for CAP treated in critical care. The majority of patients have a low-moderate severity CURB-65 score and potential opportunities to reduce antibiotic duration could be missed. Patients with severe CAP receive a duration of antibiotics consistent with current recommendations.
0141
The Value of a Shared Approach to Radiological Imaging in a District General Hospital Intensive Care Unit
Nicola Johnson1, Timothy Wenham2 and Freya Brownlow2
1Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
2Barnsley Hospital NHS Foundation Trust, Barnsley, United Kingdom
Abstract
Radiological imaging is a vital resource for the intensive care clinician, but the method and persons interpreting radiological imaging for patients on intensive care units is variable nationwide.1 Although the provision of formal radiology meetings is not a standard in The Guidelines for Provision of Intensive Care Services (Second Edition), senior radiologist input is noted as valuable.2
Since 2017 our intensive care unit (ICU) has run a weekly radiology meeting, lead by two radiologists with an interest in critical care. This allows all patients currently on ICU to have all their recent imaging reviewed, ensuring a second radiology opinion and an opportunity for the intensivist to discuss scans and x-rays with the radiologist. We have found this meeting invaluable, as with a combined clinician and radiologist approach, we have identified additional information from scans that has led to changes in patient care. A close relationship between the intensivist and a radiologist who understands critical care also helps to secure additional radiological imaging and procedures that can sometimes be challenging to arrange. As well as benefits to patients we have also found these meetings valuable from an educational perspective, often attracting trainees and medical students with attachments based outside of intensive care.
Despite this we recently recognized that although decisions were being made after the meetings, our documentation was likely to be poor and therefore a potential communication issue. We decided to explore if this was a problem and, if so, formulate a plan to improve it. We set a standard that, after the radiology meeting, documentation in the notes should occur 100% of the time. A spot audit of this in March 2019 demonstrated that this only occurred 13% of the time. As a result we designed a proforma for documentation of the meeting. Its design prompts staff in line with the Royal College of Physicians “Generic medical record keeping standards”. This allows for documentation for each patient, which images were reviewed, any discussion points, any action plan resulting from this and documentation of the consultants leading the meeting. We printed it in bright orange to allow easy identification in the notes.
Re-audit has demonstrated that the percentage of patients with any documentation has increased to 88%. Of those who had form in their notes for any given radiology meeting 100% fully met the generic medical record keeping standards. Informal feedback from clinical colleagues has also been excellent.
For our ICU, we have found having a dedicated radiology meeting beneficial for both decision-making and education. A visible, dedicated proforma has significantly improved documentation standards and improved information sharing, including for those not in attendance at a given meeting. Further work investigating the proportion of patients who undergo a change in clinical management as a result of consultant radiologist input at the meeting is underway.
0143
Are We Verifying Deaths Like We Should?
Saba Tabish and Atul Garg
Walsall Manor Hospital, Walsall, United Kingdom
Abstract
There is no legal definition of death nor is there an international consensus on one. One definition used is the irreversible loss of capacity for consciousness combined with the irreversible loss of capacity to breathe.1 Verifying deaths in secondary care is a very common duty placed upon junior doctors and nursing staff, yet very few hospitals have a standardised process of doing so.
Objectives were to assess the quality of documentation of death verification after cardiopulmonary arrest, in Walsall Manor Hospital. Standards were set as per Academy of Medical Royal Colleges document “A Code of Practice for the Diagnosis and Confirmation of Death”.1 If results were below the desired target, to introduce a standardised proforma across the trust to improve compliance with the above guidance.
A data set of 100 patients was compiled retrospectively over a period of November 2018 to January 2019. The data was collated and analysed with the help of tables and graphs. QIP tool PDSA used throughout the process.
The criteria were documentation of the following:
• Central pulse
• Heart sounds
• Respiratory sounds
• Corneal reflex
• Pupillary reflex
• Response to pain
The target was set as 100% for all the verification criteria.
Of the 6 criteria to verify a death, 4% assessed all 6. 57% assessed 5 criteria, whereas 25, 10 and 3% assessed 4, 3 and 2 criteria respectively. 1 documentation had none of the criteria. The most commonly missed criteria were corneal reflex, followed by response to pain. (Fig. 1) Discrepancies were found in times of death between verification of death time and time of death documented in nursing documents in 29% of the cases, one case resulting in a change of date as well.
Results were discussed with relevant medical, nursing staff, and mortality surveillance group in the hospital. Standardised proformas with all 6 criteria were introduced on all wards. Data collected 6 weeks after introduction showed 95% improvement in results.
There is a wide variation found in the documentation of verification of death which can be a source of confusion and conflict for administration staff and families later. Use of a standardised proforma by all staff will promote consistency in the process.
0146
The development of an ACCP team in a specialist Neuro ITU to provide safe and effective second tier medical cover on call
Michael Jennings1 and Jennifer Cater2
1The Walton Centre NHS FoundationTrust, Liverpool, United Kingdom
2The Walton Centre NHS Foundation Trust, Liverpool, United Kingdom
Abstract
As part of medical workforce strategy the country’s only stand alone Neuroscience ITU, the Walton Centre, has devolped 6 WTE ACCPs. The role started in 2015 with 2 WTE and has expanded year on year in terms of staffing numbers and skill sets used! We now provide 24/7 cover and our model is demonstrated leadership within our critical care region as we are the only ITU to do this in Cheshire and Merseyside! As a specialist tertiary ITU we are the only unit in the country provide this level of medical cover. It is a diverse team with 5 Nurses and a 1 Physiotherapist as it’s base profession.
Our role encompasses a range of clinical skills that we have been able to benchmark and audit as safely as our medical peers. Such as insertion of complex vascular access, transferring critically ill patients, non-medical prescribing, critical care reviews, ordering diagnostic investigations and mentoring. We would like to present data that highlights we are safe at practicing these medical roles previously only carried out by Doctors.
We have recently had feedback from the the regional ITU and Anaesthetic trainees that we are an excellent service – one of only four markers to achieve excellence in the Cheshire and Merseyside area!
The role won’t stop here, we are at the start of an evolving process. We are currently setting up a transcranial Doppler service to try to reduce delayed cerebral ischemia in subarachnoid haemorrhage with two ACCPs trained in Transcranial Doppler.
0155
Appropriate Escalation of National Early Warning Scores (NEWS)
Jyothis Manalayil, Prathvi Shetty, Nikolaos Katsieris and Laura Horne
Blackpool Victoria Hospital, Blackpool, United Kingdom
Abstract
The National Early Warning Score (NEWS) was developed in 2012 by the Royal College of Physicians as a standardized tool across the NHS. It is effectively a “track-and-trigger system” to aide early detection and escalation of acutely ill patients. When utilized inappropriately, the recognition of acute deterioration is affected leading to no or delayed clinical response.
The aim was to improve the accuracy of documentation of patients’ vital signs, and reduce the error rate to 0% on a medical and surgical ward at BVH between July 2018-April 2019. Another aim of this project is to increase the rate of appropriate escalation to medical staff to 90% (or only 10% patients not escalated).
The project was implemented on medical and surgical wards at BVH during July 2018-April 2019. Two major interventions utilized in this project include:
• the implementation of the novel NEWS2 scoring system (with significant improvement)
• staff education of accurate documentation and appropriate escalation through individual and group teaching sessions.
On each ward, 10–12 random patients had their NEWS charts and notes reviewed over the previous 24-hour period and recorded in a pro forma. Some of the parameters investigated include: Incorrect observations, complete set of observations, whether concern was noted, overall score recorded correctly, whether the patient was escalated.
The first intervention of implementing the NEWS2 charts was a national executive decision. As with any introduction of a novel system, some confusion and errors are expected.
The second intervention was ward staff education; one-on-one and group sessions covering the NEWS2 chart, with emphasis on major changes from the previous version as well as clear/accurate documentation. These sessions also highlighted the local trust policy on the need of escalation for medical review by the appropriate staff grade.
Overall, the error rates, and escalation rates improved following the teaching session, after the NEWS2 charts were implemented at BVH.
The sole implementation of the novel NEWS2 charting system did account for increased error rates, which was expected. Following the education sessions there was marked improvement in the use of the NEWS2 chart, but note that this was close to the original baseline.
To conclude, it is apparent the implementation of the NEWS2 scoring system accounted for increased rates of errors throughout all parameters measured in this project. It is also apparent that effective individual/group education was required to improve the use of the NEWS2 charts. In conclusion, to improve the appropriate use of NEWS 2 chart, and improve the escalation of patients, therefore improve early detection and prevention, we must continue focused education to staff on the ward including physicians, nurses, and the allied health professionals.
| Baseline | Post NEWS2 Chart | Post Education | |
|---|---|---|---|
| Incorrect observations recorded | 22% | 25% | 21% |
| Total scores incorrect | 19% | 45% | 24% |
| Incomplete set of observations | 6% | 35% | 16% |
| Patients not escalated | 33% | 85% | 63% |
0156
ICU Anaesthetic Emergency Bags – Standardising Content and Process
Sophie Benoliel, Julian Wijesuriya and Timothy Jackson
The Royal Free Hospital, London, United Kingdom
Abstract
Introduction: The availability of pre-prepared specialist anaesthetic drugs and equipment can save time and reduce errors when managing critically ill patients requiring emergency airway management.1 Use of such pre-prepared equipment is common for critical care teams but provision may be variable in terms of contents and process.
Reliance on pre-drawn drugs and equipment that is not formally checked or standardised can result in delays, omissions and errors during time-critical patient emergencies, with the potential to adversely affect patient outcome. Checklists can be used as an aid to drug and equipment checks, but difficulties with clinician engagement are well recognised.2
In our institution, two emergency bags were provided for use by airway-trained registrars in managing airway emergencies in the ICU and throughout the wider hospital. The bags contained anaesthetic drugs (including pre-drawn syringes), medical emergency drugs, a videolaryngoscope with disposable blades, an end-tidal carbon dioxide monitoring device and a selection of ancillaries. The two bags were of different brands and had no standardised layout, contents or checks procedures in place, resulting in cluttered bags containing unnecessary or duplicate items, missing equipment and broken ampoules.
Objective: To standardise the contents, layout and processes relating to the ICU emergency bags, in order to reduce the potential for clinical and non-technical error.
Methods: A survey of airway-trained doctors who used the ICU emergency bags was conducted. Problem areas were identified and a multi-faceted intervention was introduced. This included procurement of two identical emergency bags, rationalisation and standardisation of the bag contents and layout, a formal process of daily checks and maintenance utilising a checklist and logbook. Two months following intervention, the survey was repeated.
Results: Pre-intervention, 85% of doctors reported having problems with the bags, 38% of which affected patient care. Post-intervention, this reduced to 36% with 0% affecting patient care. Reported ease and speed of finding items in the bags on a scale of 0–10 improved from 5.5 to 9.3 (mean average). Doctors’ awareness of the required bag contents or where to find this information improved from 0% to 100%. The frequency of full bag contents checks improved:
The type of bag check, when conducted, improved from 0% using a checklist pre-intervention to 75% using a checklist post-intervention. Associated with the introduction of a specified contents list and formal checks process, was a reduction in doctors reporting missing items from 92% to 18% and expired ampoules from 31% to 0%.
Conclusions: Standardising the contents and layout of the ICU emergency bags was associated with improvements in ergonomics and usability. Following intervention, doctors reported a lower incidence of problems and none that affected patient care. Knowledge of bag contents improved along with frequency of checks and use of checklists with which initial compliance was encouraging.
| Frequency of full bag checks | Pre- intervention | Post- intervention |
|---|---|---|
| Every shift | 8% | 36% |
| Most shifts/every day shift | 17% | 64% |
| Occasionally/never | 75% | 0% |
0158
Cervical discitis complicated by loss of consciousness
Venkat Sundaram, Xenia David and Divya Krishna Iyer
Glan Clwyd Hospital, Rhyl, United Kingdom
Abstract
Background: Cervical discitis is a rare spine infection that has a non-specific, insidious clinical presentation. This is a case of a patient who presented with neck pain, complicated by increasing drowsiness and upper limb paresis.
Case Presentation: A 73 year old female came to the emergency department with worsening neck pain. She had fallen unto her coccyx three weeks prior, but had otherwise been well. She had a right leg malunion from a previous road traffic accident, chronic kidney disease, hypothyroidism, and osteoarthritis. On admission, she had neck tenderness and restricted range of motion, no fever, a slightly elevated white cell count, and raised C-reactive protein. Cervical X rays showed osteoarthritic changes, and she was diagnosed with polymyalgia rheumatica. On day 5, the patient developed signs of infection and upper limb weakness. MRI showed loss of disc height at C3/4 and C6/7, with no evidence of discitis. Blood cultures grew Staphylococcus aureus. Cerebrospinal fluid analysis, abdomino-pelvic CT scan and echocardiogram did not show any infective source.
Her GCS dropped to 7 (E2V1M4), requiring intubation. Antibiotics given for discitis were modified to cover possible meningoencephalitis. A right internal jugular (IJ) vein thrombus was discovered, and therapeutic low-molecular weight heparin (LMWH) was started.
The patient began to awaken on day 14, but was unable to move both upper limbs. She was extubated with plans for rehabilitation. On day 21, she had a septic episode, and her haemoglobin dropped to 55 g/L. A CT scan revealed a large retroperitoneal haematoma. The LMWH was discontinued and blood transfusions were given. A repeat cervical MRI was then done, which showed discitis at C4/5 with an epidural abscess. The patient underwent surgical drainage of the abscess and subsequent neurorehabilitation.
Conclusions: Spondylodiscitis is a rare condition, affecting 1 to 2.5 per 100,000 patients per year. Risk factors include age, previous infections, vascular or cardiac implants, intravenous drug use, immunosuppression due to diabetes or cancer, renal or hepatic failure, and rheumatologic disease. Discitis may arise after a spinal operation, or spread haematogenously from another source, often from the genito-urinary tract. S. aureus is the most common pathogen. Symptoms are nonspecific and consist of pain, fever, and sensorimotor deficits. MRI is the imaging modality of choice, yielding high sensitivity and specifity. Conservative management includes six weeks to three months of antibiotics. Surgery is indicated when there is progressive neurologic debility or failure of medical treatment.
In this case, the patient was appropriately diagnosed with cervical discitis based on the clinical presentation, along with the isolation of S. aureus from blood cultures. However, her condition was unusually complicated by decreasing GCS, which could have been due to meningoencephalitis. The initial MRI did not show any signs of spine infection, which only appeared on repeat imaging after three weeks. The presence of a right IJ thrombus also contributed to a complicated stay in intensive care. This case highlights the necessity of treating discitis based on a high index of suspicion.
Initial cervical MRI.
Cervical MRI after three weeks.
0159
Tension gastrothorax – the lessons learnt
Rebecca Jennings1, Charlene Parton2 and Felicity Clark2
1University Hospitals North Midlands, Stoke-on-Trent, United Kingdom
2University Hospital North Midlands, Stoke-on-Trent, United Kingdom
Abstract
We present a case of tension gastrothorax and the lessons learnt.
30-week primip, 38 years old admitted following an emergency LSCS for severe pre-eclampsia having been admitted to hospital with difficulty in breathing and severe chest and abdominal pain. Suspected to be pre-eclampsia related symptoms.
PMH – Laparoscopic Nissen fundoplication and re-do, mesh repair in December 2018.
Severe respiratory distress at induction with evidence of LUL diversion and LLL collapse on CXR. Significant VQ mismatch intra-operatively with high airway pressures, PaO2 15kpa on 70% FiO2 & 7 PEEP.
CT scan demonstrated large diaphragmatic defect with entire, grossly distended stomach and a loop of transverse colon located within the right hemithorax with possible narrowing or outlet obstruction. Bilateral plural effusions noted, and a left sided intercostal drain was inserted.
Patient was extubated and was stable for a period before developing increasing pain and nausea. Urgent surgical opinion was sort, NGT reinserted and a follow up CT scan done.
During the scan the patient deteriorated with respiratory distress and hypoxia – treated with high flow O2. Blood pressure became compromised as previously required 50 mg/h (10ml/h) labetalol infusion to maintain SBP 170 mmHg was hypotensive. Labetalol was weaned off and SBP was 100. Fluid resuscitation was given and the alert to Critical Care to expect return of a deteriorating patient with the potential for intubation.
Following verbal CT report of large tension gastrothorax, the NGT was advanced and large volume of air aspirated. With on-going fluid replacement and decompression, the patient stabilised. Respiratory function improved with FiO2 requirements reduced and SBP maintained with low dose vasopressors.
Patient was placed on the emergency surgical list.
Surgical intervention included OGD, laparoscopy converted to laparotomy with thoracostomy and open abdomen before a re-look laparotomy for inspection of stomach and closure of wound with NJ insertion the following day. Furthermore, adequate analgesia and management of blood pressure ensued before successful extubation onto high flow O2.
A severely distended stomach misplaced into the thoracic cavity is a rare event caused by previous or existing hiatus hernia and simulates a tension pneumothorax with haemodynamic compromise and symptoms of respiratory distress.1 Often mistaken for a pneumothorax, diagnosis can occur when emergency treatment is deployed with little improvement and respiratory compromise not resolved. The tension gastrothorax is only relieved with the correct placement and decompression with an NG tube.2
The incidence of these hernias becoming necrotic and risk of vascular compromise is 5% with significant increased mortality, prompt treatment is imperative.3
Incidence of such hernias are low but run a high risk of becoming life threatening due to frequent miss-diagnosis and poor recognition.4 This diagnosis is often further complicated in the third trimester of pregnancy due to altered physiology secondary to increasing abdominal pressure exerted by the growing uterus. These patients commonly present in respiratory distress, with haemodynamic compromise and mediastinal shift.5
0160
Intermittent Vancomycin Dosing Does Not Achieve Therapeutic Targets in Critical Care: An Audit Project
Benjamin Shuker
University Hospitals Coventry and Warwickshire, Coventry, United Kingdom
Abstract
Introduction: Vancomycin is a glycopeptide antibiotic used intravenously in critical care to treat respiratory, skin, and soft tissue infections. It is also used for the treatment of difficult and deep-seated infections including endocarditis, bone, joint, and intracerebral infections. Importantly it is used for the treatment of methicillin-resistant staphylococcus aureus (MRSA).
Traditionally, multiple intermittent doses of vancomycin are given intravenously producing peaks and troughs in plasma concentration. Vancomycin is cleared almost exclusively by glomerular filtration. With normal renal function, a trough level is achieved approximately 11 hours after completing the infusion. Carefully timed trough levels must be taken to correctly monitor plasma concentration and adjust doses accordingly to target a therapeutic range of 10–20 mg/L.
Maintaining vancomycin in the target therapeutic range is essential as the primary parameter for efficacy of vancomycin is the area under the concentration curve (AUC) divided by the minimum inhibitory concentration (MIC) of the target organism. For vancomycin to be effective an AUC/MIC of >400 is required. In difficult infections the MIC is often increased necessitating higher trough concentrations (15–20 mg/L) to achieve clinical effectiveness. (1)
Vancomycin use in critical illness can be challenging as pharmacokinetic factors such as renal function, protein binding, and volume of distribution may be affected. Continuous renal replacement therapy techniques add complication by increasing clearance.
Objective: To determine if usual practice (intermittent infusion) reliably achieved target plasma concentrations of vancomycin in a population of critically ill patients.
Method: Retrospective audit in a major trauma centre general critical care unit. Patients were reviewed electronically if they had been listed as receiving vancomycin from critical care handover documentation. Patients were included if they had been admitted to general critical care and had at least one vancomycin level performed during their critical care admission. The standard target plasma vancomycin level (10–20 mg/L) was assumed.
Results: Fifty patients were identified as having received vancomycin between August 2018 and March 2019. Twelve patients did not meet the inclusion criteria.
Thirty-eight patients were reviewed (21 males, 17 females). The most frequent type of infections treated were intracerebral (28.9%) followed by sepsis of unclear source (23.7%). Other infections included respiratory (13.2%), skin (13.2%), intra-abdominal (7.89%), bacteraemia (5.26%), joint/bone (5.26%), and endocarditis (2.63%).
In total 259 vancomycin levels were performed. The mean number of levels taken per patient was 6.82 (minimum 1, maximum 50). Of these levels, only 110 were in range (42.5%). Of the remaining levels, 100 were below the target range (38.6%) and 49 were above (18.9%).
Conclusion: Standard intermittent infusion of vancomycin did not reliably achieve target vancomycin levels in a general critical care population with a broad range of infections. A significant proportion of levels were subtherapeutic, and therefore potentially not clinically effective.
Continuous infusion of vancomycin has been used in critically ill patients as an alternative method of delivery (2) and following this audit we have adapted Scottish guidance (3) for use in our trust.
0161
STEPS Study: using wearable technology to predict peri-operative high-risk patient outcomes
Suzanne Carey-Jones1, Matt PG Morgan2, Richard Davies1, Ashleigh Brownsdon1, Mark Kelson1, Laura Jones3, Rhys Thomas1, Nathan Riddell4, Mike Davies5 and Professor Monica Busse-Morris6
1University Hospital of Wales, Cardiff, United Kingdom
2Department of Anaesthetics, University Hospital of Wales, Cardiff, United Kingdom
3Department of Physiotherapy, University Hospital of Wales, Cardiff, United Kingdom
4Department of Critical Care, University Hospital of Wales, Cardiff, United Kingdom
5Department of General Surgery, University Hospital of Wales, Cardiff, United Kingdom
6Cardiff University, Cardiff, United Kingdom
Abstract
Background: Cardio-Pulmonary Exercise Testing (CPET) is a non-invasive method of investigating a patient’s heart and lung function at rest and during exercise and acts as a surrogate marker for a patient’s suitability for major surgery. It is, however, expensive, requiring a trained operator, specialist equipment and a significant time investment from both the patient and medical staff.
The use of consumer accelerometers is increasing due to their widespread availability and improving accuracy. Previous studies have shown that they are acceptable to patients for the purpose of monitoring physical activity and that patients struggle to accurately estimate their own levels of activity independently2. We aimed to establish the feasibility of using a Garmin Vivosmart HR+ smart activity tracker to gather information on patients’ activity levels, and use this information to screen for high risk patients prior to major abdominal surgery by comparison to their CPET testing parameters.
Methods: 42 patients scheduled for major elective intra- abdominal surgery, wore the watch for 6–7 days following Cardiopulmonary Exercise Testing (CPET). 36 of these patients completed an International Physical Activity Questionnaire (IPAQ). Information obtained from the watch included HR, total steps, floors climbed, distance from home travelled, sleep and temperature. Statistical modelling was then used to assess the correlation between parameters provided during CPET and those recorded by the Garmin Vivosmart HR+.
Results: There was moderate correlation between some of the data from the wearable device and CPET performance, which was increased using model fit diagnostics. Floors climbed, total steps and total distance all showed moderate correlation with Peak VO2 (R = 0.57, R = 0.59 and R = 0.62 respectively), anaerobic threshold (AT) (R = 0.37, R = 0.39, R = 0.42 respectively) and peak work (R = 0.56, R = 0.48, R = 0.50 respectively). A slower average or resting heart rate was associated with improved AT (R = −0.47 and R = −0.36) and Peak VO2 (R = −0.27 and R = −0.26). There was no correlation between intense minutes of activity, maximum recorded heart rate or total calories burned. There was little correlation between self-reported activity levels and CPET.
Conclusion: There was moderate correlation between floors climbed, total steps, total distance and heart rate parameters recorded by the wearable device and CPET performance, which was increased using model fit diagnostics. As expected, there was little correlation with self-reported activity levels and CPET. We will aim to further identify the correlation between wearable device data and CPET performance. Larger numbers are required to establish whether these variables are associated with post-operative outcomes, such as complications, length of stay, and 30-day mortality and hence whether the use of consumer accelerometers could be a suitable adjunct in pre-operative assessments.
0162
Eosinophilic myocarditis secondary to T-cell lymphoma; complicated by left ventricular apical thrombus and dissection identified by critical care transthoracic echocardiography
Aisha Hameed, Rosalba Spiritoso and Hazem Lashin
Barts Heart Centre, St Batholomew's Hospital, London, United Kingdom
Abstract
Background: This report describes the role of critical care transthoracic echocardiography (TTE) in detecting left ventricular (LV) apical dissection and thrombus in a patient with eosinophilic myocarditis secondary to T-cell lymphoma.
Case Presentation: A 54-year-old gentleman with a history of eosinophilic myocarditis, moderate LV impairment presented to cardiology clinic with increased neck swelling and a raised eosinophil count (19.7 × 109/L which rose further to 74.5 × 109/L). A computer tomography (CT) scan of the neck demonstrated lymphadenopathy suspicious of lymphoma with axillary lymph node biopsy confirming this. While in hospital, he suffered a seizure with a fall in consciousness level from a Glasgow coma scale (GCS) of 9 which later improved to 13. Subsequent CT brain demonstrated acute bilateral frontal and parietal infarcts. He was intubated and transferred to intensive care where critical care TTE was performed to investigate possible sources of embolism. This demonstrated an apical dissection with preserved apical architecture suggestive of intramural myocardial dissection resulting in a small apical cavity in continuity with the main LV cavity (Figure 1A). Small mobile structures were attached to dissected myocardium and thought to be the source of embolism (Figure 1B). Colour flow doppler interrogation revealed diastolic flow in the apical cavity (Figure 1D). Given the rising eosinophil count of 70 X109/L related to increased lymphoma activity, cyclophosphamide was commenced resulting in a partial response, with a reduction of eosinophil count to a range of 20–30 X109/L. Unfortunately, due to the partial response to treatment of the lymphoma and cardiac complications the patient suffered, the multidisciplinary team decision was to treat the patient palliatively.
Conclusion: This case demonstrates the importance of critical care TTE which identified left ventricular apical dissection as well as the importance of vigorous management in eosinophilic myocarditis to prevent complications, including LV thrombus formation (1). Echocardiography remains a portable, non-invasive, widely available modality which can provide additional information not identifiable with physical examination alone. For this reason, there has been interest in non-cardiology trained physicians to develop focused TTE skills. The increasing number of intensive care clinicians partaking in focused echocardiography has been shown to both help therapeutic management and when possible improve overall patient care (2). Critical care TTE revealed the underlying dissection and thrombus but unfortunately in this case it could not be treated.
0163
Anaphylaxis to Dialysis
Nikita Goel, Carol Wong, Darshan Pandit and Prasad Rajendran
Russell Hall Hospital, Dudley, United Kingdom
Abstract
A 42 year old man presented with a mixed overdose consisting of Ethylene Glycol, Ibuprofen and Citalopram. He presented with a severe metabolic acidosis and acute kidney injury. Post treatment with Fomepizole and intravenous fluids the creatinine level remained elevated and urine output decreased. A decision was made for haemodialysis due to intractable acidosis and ethylene glycol overdose. Initial Haemodialysis sessions showed minor drops in systolic blood pressure as expected with fluid removal. Subsequently on a haemodialysis session, the patient had a sudden severe drop in systolic blood pressure to 50 mmHg accompanied with a widespread maculopapular rash. Tryptase levels were taken at the time with a result of 14.6 (ref range 2–14) which then dropped to 8.2 (ref range 2–14) the following morning.
The patient was treated with ionotropic support; Metaraminol, Intravenous Adrenaline and Intravenous Hydrocortisone. Subsequently the patient was transferred to the Intensive care unit and it was noted that the same reaction did not occur on haemofiltration.
Further haemodialysis sessions gave the same reaction with a profound drop in systolic blood pressure. Complement levels were checked at 0, 30 and 60 minutes into dialysis which showed a drop in C3 complement level. Blood tests also revealed a persistently high eosinophil count and the maculopapular rash persisted. Due to the high suspicion of anaphylaxis to dialysis, parts of the dialysis machine and set up were changed each time to eliminate the causative agent. Ultimately the cause was found to be the ethylene oxide, which is used to sterilise the dialysis machine.
After this was removed the patient had a normal dialysis session without requirement of intravenous steroid or ionotropic support. This case highlights the rare presentation of anaphylaxis to dialysis, how it came to be diagnosed and how the causative agent was eliminated to provide the patient with a safe dialysis.
Figure 1.
A: Modified apical view demonstrating apical cavity with small masses attached to myocardium. B: Modified apical view demonstrating apical cavity continuation of LV cavity. C: Colour flow Doppler demonstrating diastolic flow into the apical cavity. D: Contract study defining thrombus within apical cavity.
0166
End of Life Audit – Recognition and Management of the Dying Patient in Blackpool Victoria Hospital
Jyothis Manalayil, Prathvi Shetty, Nikolaos Katsieris and Laura Horne
Blackpool Victoria Hospital, Blackpool, United Kingdom
Abstract
The local trust’s annual audit (60 Death Audit) found that for the patients that died in 2016 there was poor documentation of advance care plans and patient’s wishes. Only 34% of patients who were suitable for the End of Life (EOL) pathway were placed on one and only 9% of patients who were suitable for the Amber care bundle (ACB) pathway were placed on it. These 2 pathways make up the core management of the dying patient. The EOL pathway is for patients who are dying imminently or appear to be in the next 4 weeks. The Amber care bundle pathway is for patients who are clinically deteriorating and encompasses both escalation plans and the patient’s wishes should their condition deteriorate.
A hospital survey – Do Not Attempt Cardio-Pulmonary Resuscitation (DNACPR) Perspectives Project assessing hospital staff’s ideas and knowledge about the DNACPR, highlighted the presence of several misconceptions about the decision-making process of a DNACPR request. This prompted us to audit the recognition of patients who are at risk of dying and to assess whether they were appropriately managed.
Audit deaths within surgical department to assess:
• Recognition of patients at risk of dying
• Presence of communication and documentation between staff and dying person/those important to them
• Use of ACB and EOL Pathways
• Use and documentation of appropriate DNACPR
We looked at patients on surgical wards who died between August 2017 and July 2018. Qualitative and quantitative information was collected using an audit proforma which included patient demographics, cause and date of death, documentation of recognition of dying, documentation and timescale of ACB/EOL pathways or DNACPR and documentation with the patient/family.
A total of 29 sets of patient data were collected. The mean age of the patient was 80 with an average time in hospital of 10 days (<1 h-60 days). All patients had a DNACPR however 9 of them were not discussed with the patient, 5 not discussed with family and 1 not discussed with either. 17.2% of patients were referred to critical care inappropriately and only 38% referred to palliative care. 76% of all patients were recognised as dying at some stage and documented; on average this was done 1 day before the patient died. 95% of patients who were suitable for ACB were not on it, however 51% of patients were recognised and placed on the EOL pathway.
This audit highlights that there are still shortcomings when managing dying patients. Even though the clinicians were good at recognising a dying patient (76%), not all of them were appropriately discussed with the patient/family. Additionally, the use of the pathways (ACB especially) is very poor considering it offers a useful tool to document plans of escalation.
The main finding in this study was the lack of documentation – especially family discussions, recording patient’s wishes whilst they are well and having such conversations early. This will in turn improve the patient’s journey, and also prevent inappropriate escalation (i.e. referral to critical care without investigating baseline, or patient wishes).
0168
Evaluation of episodes of delirium in the current intensive care unit at Chelsea and Westminster Hospital
Emma Whiting1, Edward Liu1, Sabrina Monteregge2 and Marcela Vizcaychipi2
1Imperial College London, London, United Kingdom
2Chelsea and Westminster Hospital, London, United Kingdom
Abstract
Delirium is an acute, fluctuating confusional state, associated with impaired attention and perceptual disturbances. It has the highest incidence in Intensive Care Unit (ICU) patients.1 Delirium affects up to 48% of non-ventilated ICU patients and 69% of ventilated ICU patients and has been associated with increased mortality, longer hospital stays and poor functional outcomes.2 Various environmental factors have been shown to precipitate episodes of delirium, including noise, sleep disturbance, lighting and temperature. Addressing these elements may reduce the rates of delirium, resulting in improved outcomes for patients.
The objectives of the this study were to:
1. Assess the prevalence of delirium in the current ICU at Chelsea and Westminster Hospital
2. Relate the prevalence of delirium specifically to environmental factors, rather than patient factors
Each bed in the ICU was investigated to determine whether delirium occurred in it during that day, over 6 months (21/08/2018–21/02/2019). The Confusion Assessment Method for the ICU (CAM-ICU) was used to assess delirium. Exclusion criteria for patients included a Richmond Agitation-Sedation Scale (RASS) of −3 or less (intubated or sedated). Most data was collected on the day, but 36% was recorded retrospectively by reading communication notes. The beds in ICU were divided into different areas for analysis, based on the positioning of the beds within different areas of the ICU. The data was analysed in terms of delirium rate per 1000 days. The delirium day rate is the number of days in which there was delirium in that bed, per 1000 assessed days. The delirium episode rate is the number of episodes of delirium in that bed, per 1000 assessed days.
Over the entire ICU for the 6 month study period, there were 214 days of delirium/1000 days and 94 episodes of delirium/1000 days. The data was analysed by seasons, finding that delirium rates were highest in winter (January and February). Summer (August) had a high day rate but relatively low episode rate, suggesting that episodes of delirium lasted relatively longer. Analysing the results in terms of the area of ICU showed considerable variation between different areas and different beds, suggesting that environmental factors contributed.
The results suggest a degree of seasonal influence on the rates of delirium within ICU. Furthermore, the positioning of the beds within the ICU seemed to influence the delirium rates. These results, coupled with accurate monitoring of the environment, may be used to optimise the conditions for ICU patients to reduce rates of delirium.
0169
A survey of current practice in management of refractory seizures
Ashleigh Taylor1, Katie Donaldson2 and Cristina Niciu1
1Institute of Neurological Science, Glasgow, United Kingdom
2Insitute of Neurological Science, Glasgow, United Kingdom
Abstract
Introduction: The incidence of status epilepticus is estimated to be between 10–60 per 100,000 each year (1). Greater Glasgow and Clyde (GGC) therapeutics handbook (2) advocate the use of benzodiazepine followed by phenytoin intravenously for refractory seizures. This is supported by SIGN (3) (who also recommend valproate out with women of childbearing age) and NICE guidelines (4). The administration of phenytoin in the emergency situation can be challenging with the need for large bore intravenous access, continuous ECG monitoring and the requirement to calculate a loading dose based on patient weight, which may not all be immediately available. The aim of this study was to review compliance with current guidelines and identify reasons for deviation in practice.
Method: This was an observational study conducted via survey monkey in March 2019. An email link was distributed to anaesthetic, intensive care, medical and emergency medicine doctors of all grades across all major sites in Greater Glasgow and Clyde. Questions asked included grade and specialty, use of relevant guidelines, current practice, incidence of side effects or adverse outcomes and reasons for use of alternative agents to phenytoin.
Results: There were 188 responses, the majority of which were Consultant level across all specialties (56% n = 107). Of those who responded 24% (n = 46) were acute/general medicine, 55% (n = 105) were intensive care/anaesthetics and 19.6% (n = 37) were emergency medicine doctors. Despite an average of 79.2% (n = 149) stating they comply with NHS GGC policy, 27.6% (N = 52) would use levetiracetam as first line. 27% (n = 51) would additionally refer to SIGN and NICE guidelines. Intensive care/anaesthetic and acute/general medical doctors were more likely than emergency medicine doctors to use levetiracetam than phenytoin first line following a benzodiazepine (28% vs 24% respectively). Reasons for use of levetarcitem over phenytoin included ease of administration and availability, lack of dose calculation, less haemodynamic instability and avoidance of drug level monitoring.
Conclusions: Treatment of refractory seizures remains a common pathology presenting to acute specialties. There is increasing familiarity with use of levetiracetam which has many benefits over phenytoin as mentioned above, namely lack of requirement for monitoring and dose calculation and increased haemodynamic stability. This allows for quicker administration of a potential seizure terminating therapy, particularly in the patient cohort outwith the intensive care unit not already being fully monitored. This study would suggest growing support for the use of alternatives to IV phenytoin, namely levetiracetam, in this context and it may be there is a place for updating present guidelines to more accurately reflect current practice.
0170
Patients’ Experience Of Occupation Throughout Their Acute Critical Illness Recovery
Penelope Firshman1,2,3
1European Master of Science in Occupational Therapy, Amsterdam, The Netherlands
2Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom
3King's College Hospital NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Physical inactivity and prolonged bedrest can have acute and chronic consequences and studies have shown that early physical and occupational rehabilitation can improve functional outcomes (Schweickert, et al, 2009). However, research is now focused on early mobilisation with the focus on physical activity rather than occupational rehabilitation encompassing physical, cognitive and psychological components and there is little provision of occupational therapy on critical care units. Occupations are “everyday activities that people do as individuals, in families and with communities to occupy time and bring meaning and purpose to life.” (WFOT, 2019). Critical care patients report they found loss of control and autonomy over their daily lives frightening (Laerkner, et al., 2017). They reported feeling the greatest distress when they couldn't meet their basic needs, such as; lifting a glass to drink, pressing a call bell, feeling clean when washing, getting to the toilet, getting an extra blanket, wiping sweat off their brow and adjusting uncomfortable clothing (Field, Prinjha and Rowan, 2008.) There have been no studies of patient’s experience of occupation during critical illness recovery.
Objective: To explore the experiences of occupation for people who have been critically ill and have returned home within the last month.
Method: Discharges from critical care units in one trust were screened to gain a purposive sample of four participants. Inclusion criteria were; admission to critical care for ≥7 days, English speaking, living within an hour of the researcher for practicality. Exclusion criteria were; readmission to hospital, too unwell to participate, already discharged home and repatriated. Further face-to-face or telephone screening was completed to establish if participants could provide rich descriptions of their experience and were willing to participate. Semi-structured narrative interviews were completed utilising photo-elicitation. Two participants completed a further interview to allow deeper interpretation. Narrative analysis was used to emplot a single narrative.
Results: The overarching narrative was of loss of humanity and loss of the self due to critical care admission. Re-engagement in these usual occupations was seen as fundamental to regaining humanity and sense of self.
Three narrative plots were identified:
1. The vulnerability of becoming critically ill: “I thought I was going to die, I needed help”.
2. Loss of self and fear of permanent dependence: “I’ve lost myself. Where have I gone?”
3. Reality vs expectation: “wanting to run before you can walk”.
Conclusion: Gradual return to occupations is an important part of recovery and requires specialist occupational therapy input. Patients need time to adjust to the loss of their usual occupations and realistic expectations of their recovery potential. The right level of assistance and encouragement is required to enable return to independence in occupations through trial and error within a safe environment. Personal care tasks in particular help people regain their humanity and sense of self and should be supported as early as possible. Occupational therapists can provide information, education and rehabilitation focusing on regaining these occupations. Further research is warranted into the occupational role in early rehabilitation.
0171
Exploring the feelings and experiences of critical care nurses being deployed to cover shifts in the ward
Yingchang Huang and Naim Abdulmohdi
Anglia Ruskin University, Cambridge, United Kingdom
Abstract
Introduction: The shortage of nurses in the NHS is evident and has been recently considered as a ‘national emergency’.1 Staff are leaving the service due to low job satisfaction whilst recruitment and retention continues to be a growing problem.2 The NHS authorities are seeking ways to prioritise patients and preserve safety. Moving critical care nurses to the ward to cover for staff shortage is one of the deployment strategies to ensure the safe number of nurses for the number of patients. Whilst deploying critical care nurses does relieve the shortage of staff temporarily in the wards, this could leave critical care units with unsafe level of nursing staff,3 The stress among the critical care nurses due to being moved to work in the ward should not be ignored.
Method: This study adopted a phenomenological approach and a qualitative research methodology, the data was collected using a focus group interview. There were ten participants took part and they were critical care nurses from five different hospitals in England, all with different level of clinical experience. The aim was to discover their positive and negative experiences and feelings of working in the ward in order to cover for staff shortages.
Results: The results showed that critical care nurses experienced variety levels of stress and anxiety when being moved to work in the ward, depending on how often they are sent to work in the ward, what support they are receiving when they have been deployed to the ward. Several factors have been identified in this study, they are inadequate support and leadership, lack of ward experience, lack of knowledge of the local guidelines, an unfamiliar environment, and concern over patient’s safety and relative’s satisfaction. NMC (2015) code recommends that nurses should prioritise patients and preserve safety.4 All participants expressed the importance and willingness of supporting the ward, but there is a need for local guidelines or assessments to determine what critical nurses can or cannot do when they are deployed and that there should be more support in place from both the ward and the managers. Some participants suggested rotating critical care nurses to the ward on regular basis to ensure that they are familiar with the environment and the job in the ward when they are deployed. Some suggested that there should be assessment in the ward to assess the competency of the deployed nurses to establish their competencies before assigning them a group of patients and taking responsibilities.
Conclusion: Staff shortages exists across NHS hospitals and it is important that authorities actively listen to feedback from the nurses and take actions. Clinical mangers need to adopt a proactive approach to reduce the impact of regularly relocating critical care staff to general wards and perhaps having training or guidelines to support those staff when allocated to work in general wards.
0177
Incidence of venous thromboembolism in critically ill patients with sepsis
Alicia Waite1, GC Harris1, Y Alhamdi2, CH Toh2 and Ingeborg Walters2,3
1Royal Liverpool University Hospital, Liverpool, United Kingdom
2University of Liverpool, Liverpool, United Kingdom
3Intensive Care Unit, Royal Liverpool University Hospital, Liverpool, United Kingdom
Abstract
Introduction: Venous thromboembolism (VTE) is considered a significant burden in terms of associated morbidity, mortality and health economic implications.1 The incidence of VTE within the critical care population, and septic patients in particular, has not been well defined. There is also a paucity of evidence to determine whether there is a link between VTE and mortality.1
Objective: To identify the incidence of VTE in critically ill patients with sepsis up to one year following admission to critical care.
Methods: We reviewed the records of 1107 patients admitted to critical care at the Royal University Liverpool Hospital between 2008 and 2014. Demographic data, APACHE II scores, 28 day mortality rates and the presence of sepsis were identified. We reviewed radiological reports for up to 1 year from the time of admission to critical care, looking for evidence of venous thrombus or thromboembolic event (VTE), which we defined as a new DVT, PE or cerebral infarction or any combination of these.
Results: Out of 1107 patients, 598 patients had sepsis (54%). VTE was identified in 110 patients (9.9%), 66 of whom were septic (6.0%) and 44 of whom did not have sepsis (4.0%). We found a higher incidence of DVT, PE and stroke in patients with sepsis (Table 1 – percentages refer to the total population). Table 2 shows the number of septic and non-septic patients with or without evidence of VTE and their survival up to 28 days following critical care admission. This data shows that mortality rates were higher amongst septic patients than patients without sepsis.
Conclusion: VTE was identified in 10% of our critical care population. VTE appeared to have no effect on mortality in non-septic patients, but septic patients with VTE seemed to have a lower mortality than septic patients without VTE. This mortality difference may, however, be explained by the small number of patients. A larger dataset is therefore required to investigate the impact of VTE on mortality.
Table 1.
Number of septic and non-septic patients with a DVT, PE or stroke.
| DVT | PE | Stroke | |
|---|---|---|---|
| Sepsis | 27 (2.4%) | 18 (1.6%) | 25 (2.3%) |
| No Sepsis | 17 (1.5%) | 11 (1.0%) | 17 (1.5%) |
| Total | 44 (4.0%) | 29 (2.6%) | 42 (3.8%) |
Table 2.
28 day mortality rates of septic and non-septic patients with evidence of VTE.
| Alive | Dead | Total | |
|---|---|---|---|
| Sepsis | 458 (76.6%) | 140 (23.4%) | 598 (100%) |
| VTE | 59 (9.9%) | 7 (1.2%) | 66 (11%) |
| No VTE | 399 (66.7%) | 133 (22.2%) | 532 (89%) |
| No Sepsis | 437 (85.9%) | 72 (14.1%) | 509 (100%) |
| VTE | 37 (7.3%) | 7 (1.4%) | 44 (8.6%) |
| No VTE | 400 (78.6%) | 65 (12.8%) | 465 (91.4%) |
0179
Enteral nutrition administration in a Surgical Intensive care unit: "Reality is often disappointing"
Kumaresh Venkatesan, George Toh and Naville Chia
Khoo Teck Puat Hospital, Singapore, Singapore
Abstract
Background: The prevelence of malnutrition is a significant problem in hospitalised patients. Enteral nutrition is recommended as the route of choice for feeding critically ill patients. Underfeeding remains a major challenge in the intensive care unit where 30–50% of patients do not meeting their daily protein and energy requirements. Critical illness and inadequate delivery of nutrition can exacerbate this problem. The resulting energy, protein and other nutrients deficit can lead to higher complication rates, prolonged hospital stay, higher healthcare costs and poor outcomes.
Objectives: As a part of Clinical Practice Improvement program (CPIP), we set out to study baseline enteral nutrition delivery practices in our 14 bedded surgical intensive care unit. This would enable us to identify problems and then undertake a plan-do-study-act implementation strategy to optimise nutritional practices.
Methods: A retrospective audit was conducted over a 8 week period to evaluate the nutrition prescription and delivery from the electronic medical records. A total number of 21 patients were included. The enteral feeding volume ordered and administered for each patient were retrospectively collected for the first two weeks of ICU stay. Any feeding interruptions were recorded and identified. A multidisciplinary CPIP team comprising of intensivitsts, ICU nurses, dietician and pharmacist met and undertook brainstorming session – which reviewed the macro and micro workflow and various barriers to nutrition delivery with in the ICU. Cause-effect diagram was generated, root causes were identified and Pareto principle used to form priority interventions.
Results: The daily estimated energy and protein requirement were 1580 ± 275kcal/day and 75 ± 14 g/day respectively. The mean daily energy and protein received enterally throughout the first two weeks of ICU stay were 1020 ± 488 kcal/day and 44 ± 22 g/day. Feed interruption was identified as the key factor of inadequate nutrional delivery. There were total of 362.5hours and 39 episodes of feeding interruption/194 NG feed days. Out of this 362.5 hours, 70% (261hours) of feeding interruptions were considered avoidable. These reasons include prolonged fasting in preparation for surgical procedures, extubation/tracheostomy insertion/imaging investigations. Lack of induction, education & awareness of the existing feeding policies among the new nursing staff and rotating junior medical staff, Lack of procedure specific fasting guidelines were identified as the key root causes contributing to the feeding interruption.
Conclusions: Our baseline audit revealed that the nutritional delivery was less than the 80% of the daily requirment. Avoidable Feed interruption was a major impediment in our clinical setting. Strategies to improve nutriton delivery will include implementation of procedure specific fasting guidelines and regular education and periodic re-inforcing of ICU feeding policies.
0181
Mucoactive Agents in Acute Respiratory Failure: Point Prevalence Survey of UK Adult Critical Care
Mark Borthwick1, Murali Shyamsundar2, John Warburton3, Bronwen Connolly2,4, Judy Bradley2, Brenda O'Neill5, Bronagh Blackwood2, Marc Chikhani6,7, Paul Dark8,9,10 and Daniel McAuley2
1John Radcliffe Hospital, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
2Wellcome-Wolfson Institute for Experimental Medicine, Queen's University Belfast, Belfast, United Kingdom
3Bristol Royal Infirmary, University Hospitals Bristol NHS Foundation Trust, Bristol, United Kingdom
4Lane Fox Clinical Respiratory Physiology Research Centre, Guy’s and St. Thomas’ NHS Foundation Trust, London, United Kingdom
5Centre for Health and Rehabilitation Technologies, Institute of Nursing and Health Research, Ulster University, Newtownabbey, United Kingdom
6Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
7Division of Clinical Neuroscience, University of Nottingham, Nottingham, United Kingdom
8NIHR Manchester Biomedical Research Centre, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom
9Faculty of Life Sciences and Medicine, King's College, London, United Kingdom
10Salford Royal NHS Foundation Trust, Manchester, United Kingdom
Abstract
Introduction: Acute respiratory failure is common in critical illness, necessitating support with invasive and non-invasive ventilation. Mechanical ventilation is associated with a risk of secretion retention. Previous surveys have reported that the use of mucoactive agents to augment secretion clearance is common, but the actual prevalence of use in critically ill patients has not been described.
Objectives: This study aimed to determine the actual usage pattern of various mucoactive agents in clinical use at patient level in adult critical care units within the United Kingdom.
Methods: A data collection form was created for critical care pharmacists to record unit demographic data, information about newly prescribed mucoactive agents, and information about level of respiratory support received by patients prescribed mucoactive agents. Data were collected by the unit pharmacist for one day of their choosing between 18 March and 23 April 2019.
Invitations to participate and the data collection form were distributed via the critical care group of the United Kingdom Clinical Pharmacy Association. Forward distribution to personal contacts was encouraged and social media was used to advertise the survey. Response statistics were reported back on a weekly basis to further encourage participation. Data were accepted on a per unit basis, duplicate entries were not accepted. The denominator was set using the Intensive Care National Audit & Research Centre (ICNARC) case mix programme list (2018) for England, Wales and Northern Ireland, and the Scottish Intensive Care Society Audit Group (SICSAG) list (2017) for Scotland.
The project was registered as service improvement at the Oxford University Hospitals NHS Foundation Trust (number 5497). Ethical approval was not required.
Results: The overall response rate was 63.1% (221/350 SICSAG + ICNARC units), plus an additional 8 critical care units not registered with either ICNARC or SICSAG.
The total number of adult critically ill patients included was 2,498. Of these, 993 received invasive mechanical ventilation (39.8%), 606 received non-invasive mechanical ventilation / high flow nasal oxygen (24.2%) and 899 received no respiratory support (36.0%).
Excluding topically administered Sodium Chloride 0.9%, the number of patients receiving at least one mucoactive was 494/2498 (19.8%) (Figure 1).
The breakdown of mucoactive agent prescribed by level of respiratory support is shown in Table 1.
Conclusions: The use of mucoactive agents in UK adult critically ill patients is high. They are most prevalent in patients receiving invasive or non-invasive mechanical ventilation. Isotonic sodium chloride (0.9%) is widely used, followed by carbocisteine and hypertonic sodium chloride.
0182
Toxic Shock Syndrome: an uncommon but catastrophic offender of the 21st century
Rabea Etomi, Nabeel Chaudhry and Priti Gandre
North Middlesex University Hospital, London, United Kingdom
Abstract
Background: Streptococcal Toxic Shock Syndrome (TSS) is caused by Group A Streptococcus (GAS) and is an uncommon diagnosis in the 21st century.
GAS releases exotoxins which activate the immune system by bypassing the usual antigen-mediated immune response resulting in the release of large quantities of inflammatory cytokines.3 This causes capillary leak and tissue damage leading to multi organ failure and a high mortality risk.
Case presentation: A 31-year-old woman presented to A&E four days following a relatively uncomplicated home birth of a healthy boy with diarrhoea, vomiting and fever. She was in fulminant septic shock with BP 61/37 mmHg, sinus tachycardia 170 bpm, surface temperature 38.2∞C, serum lactate of 6.2 mmol/L and an erythematous rash covering most areas. Piperacillin-tazobactam and gentamicin were started as first-line antibiotics. Clindamycin was added later. The septic shock was refractory to fluids and she was admitted to ICU within hours of arrival to the hospital. Pelvic and transvaginal ultrasound scans did not reveal any abnormalities.
She rapidly developed disseminated intravascular coagulopathy, acute kidney injury, and deranged liver functions with persistent, severe lactataemia, requiring multi-organ support and multiple blood products transfusions.
A provisional diagnosis of TSS was made based on the clinical picture, and intravenous immunoglobulin (IVIG) was commenced urgently. TSS was later confirmed by positive blood culture. Subsequently, she developed extensive skin blisters and desquamation of more than 50 percent of her body surface area.
The multi-organ support could gradually be weaned off after four days and she was extubated. This relatively small period of serious multi-organ support had led to ischaemic necrosis of the nose, fingertips and distal legs. On day 10 of her ICU stay, she was transferred to a burns unit at a tertiary centre and received multiple skin grafts on her torso and arms. Sadly, she underwent bilateral below knee amputations due to unsalvageable gangrene.
Conclusion: Streptococcal TSS is often difficult to diagnose due to its rapid and nonspecific presentation. Diagnosis requires a high grade of suspicion and the treatment may require multi-organ support and IVIG to be started urgently. IVIG has been reported to reduce the 30-day mortality from 33.7 to 15.7 percent2.
Exfoliating skin lesions and acral ischaemia (Pictures 1, 2) are real threats for secondary infections and distal gangrene respectively. These require expert dermatological and plastic surgical input and a close liaison with these services in the tertiary centres is essential from the early stages to minimise life changing damage and risk of death.
We think prevention of TSS is hence the best strategy. In London and the South East of England between 2010 and 2016, the incidence of invasive GAS infection among women within 28 days postpartum was 109 per 100,000 deliveries.1 Average annual rates have been on the rise from 3.8 to 5.8 per 100,000 over the last ten years.1 However, all obstetric patients are not routinely screened for GAS in the UK. We think that this relatively inexpensive test can prevent TSS by administration of inexpensive oral antibiotics in selected high risk cases preemptively.
1:
2:
0183
A Snapshot of Delirium in a Tertiary CriticalCare Unit
Christopher Duncan, Caroline Higenbottam and Randeep Mullhi
Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Delirium during a Critical Care admission has been associated with multiple complications including prolonged length of stay1 and increased mortality.2 It is also linked to psychological sequelae including longterm cognitive dysfunction.3 However, consensus has not yet been reached as to what constitutes best pharmacological management.
Objectives: Queen Elizabeth Hospital Birmingham has a 100 bedded Critical Care Unit providing general and tertiary services. We aimed to identify patients admitted over a month period who received adjunct sedation for delirium management including benzodiazepines, alpha-2 agonists, typical and atypical antipsychotics. We also wanted to quantify the use of a delirium scoring system to identify delirium and whether scoring took place prior to administration of these drugs.
Methods: Queen Elizabeth Hospital Birmingham uses the Prescribing Information and Communications System (PICS). This is an electronic patient record incorporating drug prescribing, drug administration, medical and nursing noting. The record was interrogated to identify all patients during the specified period that were prescribed to manage delirium. Reason for administration was also recorded. The record also allows documentation of Confusion Assessment Method for the ICU (CAM-ICU) which is the chosen scoring system for the unit. We recorded if a score had been performed in patients being given treatment for delirium. The electronic nursing notes were interrogated when the medication was given to identify what signs of delirium the patients were exhibiting at the time.
Results: 128 patients were included in the data collection of which 29.7% received medication to treat delirium. 42.1% of these patients received more than one agent. Haloperidol (33.5%) and clonidine (20%) were the most commonly used agents followed by levomepromazine (17.8%),. Atypical antipsychotics were used less frequently with quetiapine (10.3%) the most prevalent. CAM-ICU was performed on only 10.9% of the days where drugs to manage delirium were administered. The average length of stay for patient receiving these drugs was 10.8 days compared with 4.0 days in those who did not.
Conclusions: This data demonstrated the significant burden of delirium with a large percentage of ICU patients receiving medication to manage it. These patients were treated with a variety of agents which reflects the lack of evidence for of these agents. There was significant use of multiple agents which indicates likely failure of the first agent.
Our data was consistent with studies that show delirium is associated with a longer length of stay which not only exposes patients to other complications of ICU but is also a significant financial burden. Therefore appropriate detection and management of delirium has a significant economic incentive.
The use of a scoring system has been demonstrated to improve identification4 especially in hypoactive delirium. Our low use of a scoring system may mean our incidence of delirium is actually higher than documented.
| 0 | 1 | 2 | 3 | |
|---|---|---|---|---|
| Respiratory | No Support | Metaraminol or NA < 5 ml/hr | NA > 5 ml/hr | High Dose Inotropes (double strength NA or >1 agent) |
| Cardiovascular | No Support | Nasal specs or Venturi <60% | NIV or HFNP or Venturi 60% | Intubated and Ventilated |
| Neurological | Alert, comfortable | CAM-ICU +ve or Pain | Agitated or Drowsy | Unconscious |
| Renal | No support/no concern | Kidneys at Risk/difficult fluid balance | Worsening U + E or Oliguric or Strict Fluid Balance | Renal Replacement Therapy |
0184
TASC: A novel real time clinical intervention based digital score to facilitate better workforce allocation and patient flow
Barney Kyle1 and Sara Stuckey2
1Musgrove Park Hopsital, Taunton, United Kingdom
2Musgrove Park Hospital, Taunton, United Kingdom
Abstract
Introduction: Utilisation of electronic Clinical Information Systems (CIS) has opened a wealth of opportunity to gather, process and use live data. We report on introduction of Taunton Acuity Score Calculation (TASC) as a tool to aid patient flow and plan resource allocation. This novel score, displayed in real time on digital whiteboards, provides rapid insight into individual patient support needs and overall unit workload.
Objectives: Whilst colour coding bed spaces on digital whiteboards according to Level of care is useful, it fails to differentiate extent of organ support requirements being non-summative. Existing scoring system are too complex for multiple daily inputs1. We developed and implemented a simple score assessing clinical interventions which improved visibility and unit overview. We use this score to plan nursing allocation, inform on overall unit workload and highlight potential discharges. We aim to share our experience and demonstrate feasibility and validity of TASC.
Methods: TASC is comprised of four organ support scores from 0 to 3 (approximating Level of Care for each organ system), giving a total patient score ranging from 0 to 12. We use Philips ICCA to calculate and display individual and total unit scores. Organ support assessment is made by the bed space nurse within the flowsheet, picking from a dropdown list. We reviewed nursing allocation with regard to seniority and skill set and outcomes related to score.
TASC score by organ system
Results: TASC scores from 765 patients were reviewed, overall 30 day mortality was 16%.
Peak TASC score with corresponding 30 day mortality rate
A target of 4 hourly TASC completion was set. This was achieved in the majority of patients. All patients admitted had TASC completed at least 3 times within a 24 hour period.
Subjective review of nursing allocation evidenced clear correlation between nursing level of experience and skill, and TASC score. It can be used to manage nursing workload, identify stressors and support needs, and improve staff wellbeing. Scores of 11 and 12 could justify a 3:2 or 2:1 nurse to patient ratio, conversely scores of 0 and 1 a 1:3 ratio.
Conclusion: In a data heavy environment, clarity and simplicity aid communication and improvem care. Visibility offered by TASC delivers numerous benefits and insights: a simple, reproducible, real time representation of individual and unit needs. There are clear correlations between TASC score, nursing workload and mortality risk. We have implemented and utilised TASC, demonstrating its feasibility as a clinical tool.
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | 0.02 | 0.02 | 0.6 | 0.6 | 13 | 49 | 19 | 18 | 38 | 57 | 30 | 65 | 69 |
Mean scores to 10 point questions for various parameters before and after ST.
| Parameter | Mean before | Mean after | Alpha | Significance (p) | z |
|---|---|---|---|---|---|
| Communication with staff | 5.67 | 7.13 | 0.89 | 0.003 | −2.96 |
| Communication with patients | 5.31 | 6.88 | 0.87 | 0.002 | −3.1 |
| End of life discussions | 4.63 | 6.56 | 0.8 | 0.002 | −3.1 |
| Telephone Conversations | 5.31 | 6.94 | 0.85 | 0.002 | −3.11 |
| Handover | 5.13 | 6.88 | 0.8 | 0.005 | −2.82 |
0188
Support of International Medical Graduates with simulation training
Sushruth Madanapalli Raghunath, ShashiKumar Chandrashekaraiah and James Wilson
1Lancashire Teaching Hospitals NHS Foundation Trust (LTHTR), Preston, United Kingdom
Abstract
Introduction: International medical graduates (IMGs) with their Primary Medical Qualification in non-EU Countries are an integral part of NHS accounting for around 25% of the registered doctors.1,2 There has been significant increase in IMGs coming to UK in 2018 following lifting of tier 2 visa cap,2 and support to these doctors is very important. Unfamiliarity with working of NHS, communication in challenging situations like end of life and resuscitation decisions, dealing with medical emergencies were some of the major barriers faced by IMGs after migrating to U.K.3 Simulation based education is an integral part of medical training in UK and evidence base for its effectiveness is growing.4
Background and Objectives: We have developed regular simulation training (ST) specific for IMGs at LTHTR on human factors and communications skills, major guidelines and critical incidents. We have organised around 20 sessions over 2 years and modified the sessions based on feedback. We wanted to assess the effectiveness of ST in helping IMGs integrate into NHS and also developing their communication and inter-personal skills.
Methods: 17 IMGs currently working in Critical Care department of LTHTR were invited to participate in the survey using Likert-scale type questions to explore the development of skills relevant to NHS practise before and after ST. Data was collected and analysed using descriptive statistics, test of reliability (Cronbach's alpha) and Wilcoxon signed rank test for significance.
Results: Response rate was 16/17 (94.11%). Around 40% of the respondents had less than 1 year of UK work experience. 4 (25%) of the IMGs had no prior experience with simulations. Everyone had some form of exposure to simulation after coming to UK.
Mean scores of 5 point scale questions indicate IMGs felt positively towards simulations improving communication skills (4.31), clinical skills (4.06), leadership (4.19), confidence (4.25), inter-personal skills (4) and patient safety (4.25). Familiarity with communication tools like SBAR was low among IMGs (3.06). Mean response score for simulations being less stressful was 2.81. Most felt that feedback after simulation exercise helped change their clinical practice (4) and regular simulations would be helpful (4.75).
Conclusion: Simulation training was perceived positively by IMGs and had a major role in developing communication and interpersonal skills. Regular ST specific to IMGs is valuable to familiarise IMGs with UK medical practice.
0189
Tracheostomy Educational Initiative- A Quality Improvement Project
Yasser Al-Raweshidy, Jo Noble and Jenny Townsend
King's College Hospital NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: The National Confidential Enquiry into Patient Outcomes and Death (NCEPOD) 2014 report demonstrated that there is significant morbidity and mortality relating to tracheostomised patients in the Intensive Care Unit (ICU) and consequently considerable preventable harm.1 It reported 24% of ICU patients experienced defined tracheostomy-related complications.1 Wide variations in tracheostomy management exist between hospitals resulting in a significant degree of confusion amongst healthcare professionals on how to provide optimal tracheostomy care. Key recommendations in the report state that “Staff caring for tracheostomy patients must be competent to recognise and manage common airway complications”.1
The evidence base is tremendously limited for most tracheostomy-related interventions because standard research methods (i.e. randomised controlled trials) are seldom logistically or economically practicable.
Objectives/Methods: At King’s College Hospital, London we developed an educational programme for ICU junior doctors to improve education around tracheostomies. Our ICUs cover all the major specialties and provide training to doctors from a mix of backgrounds and grades. This educational initiative came about after four separate safety incidents relating to tracheostomies over a short period of time. Analysis of these incidents showed there was a consistent knowledge gap that contributed to the cause of the incidents. An educational toolkit that includes a PowerPoint slide set and pre/post-teaching questionnaires were developed. Content included what, why, where and how tracheostomies are inserted with a particular focus on the risks/complications following insertion. Special circumstances were discussed, this included; speaking valves, tracheostomies in laryngectomy patients and tracheostomy emergencies. ICU trainees were invited to suggest improvements in tracheostomy care.
Results: To date we have delivered this pilot teaching to 35 trainees. Teaching feedback has been extremely positive and all trainees now feel more confident with tracheostomy management. We have been responsive to the constructive feedback and made adjustments to the programme accordingly. As such the educational initiative will now be embedded for new cohorts of doctors from August 2019.
Following feedback gained, the NCEPOD emergency tracheostomy algorithm will be placed above the patient’s bedside wall in all tracheostomy patients on the ICU. A new programme of simulation on tracheostomies via airway and novice workshops will shortly be introduced for junior doctors.
A large and extensive education programme for nursing staff has been also been established: focusing on bedside teaching with staff using the ‘Trachy-Tom’ simulator, teaching sessions on allocated team days and the development of a new local guideline document.
Further evaluation will be conducted over the next 6 months through analysis of complications via Datix submissions. To date no further tracheostomy-related adverse incidents have occurred since the educational programme was implemented.
Conclusions: ICU is a dynamic specialty training doctors from a variety of backgrounds with differing levels of airway experience. Tracheostomy care cannot be assumed knowledge and requires an educational package to be delivered to new doctors and the Multidisciplinary Team to help prevent the relatively rare but serious complications seen in adverse incidents. Early indications are that an education package can be swiftly and easily delivered to improve safety of tracheostomised patients in the ICU.
0190
Can 7-day Chelsea Critical Physical Assessment tool (CPAx) scores determine the need for a tracheostomy in Cardiothoracic Intensive Care Unit?
Richard Southcott1, Chloe Meehan2, Ruthann Curran2, Katie Dowling2, Claire Purkiss2 and Evelyn J Corner1,2
1College of Health and Life Sciences, Brunel University London, London, United Kingdom
2The Royal Brompton and Harefield NHS Trust, London, United Kingdom
Abstract
Introduction: The Chelsea Critical Care Physical Assessment Tool (CPAx) is a validated measure of physical function in the Intensive Care Unit (ICU).1,2 It grades patients in ten components of function giving an aggregate score from 0–50 (0 representing full dependence, and 50 representing independence). Previous data has indicated that a median CPAx score of <10 in the first five days of ICU stay is associated with longer ICU length of stay (LOS) (>10 days) and increased duration of advanced respiratory support.3
Insertion of a tracheostomy is often considered in patients with a predicted LOS of >10days.4 It is plausible that early changes in median CPAx scores may be an early clinical predictor of the need for a tracheostomy. This may allow for early tracheostomy, which has been proposed to reduce the deleterious consequences of mechanical ventilation.4
Objective: To determine whether CPAx scores in the first week of ICU admission are associated with the need for a tracheostomy.
Methods: Retrospective observational study of patients admitted to a cardiothoracic adult ICU in London between September 2018 and January 2019.
The following data was collected from case note review: age, gender, APACHE II score, admission diagnosis, mortality outcome, LOS data, days of mechanical ventilation, tracheostomy insertion, CPAx scores within the first week of admission.
Demographic data was analysed descriptively. Median CPAx scores over the first 7-days of a patient’s ICU stay were calculated. The Mann-Whitney U test was used to determine differences between groups (i.e. tracheostomy versus no tracheostomy). Relative risk of tracheostomy was calculated with CPAx score cut offs determined post hoc, based-on group differences.
Inclusion criteria: age ≥18years, ICU LOS of ≥48 hours.
Exclusion criteria: no outcome recorded (n = 6), inadequate data (n = 4)
Results: Fifty-two participants were included. Median age was 58 years (IQR 45–69), with average APACHE II scores of 20.9 (±4.3) and median of 11 days (IQR 3–24) of mechanical ventilation. 266 CPAx scores (73.1%) were recorded out of a possible 364 (one score per day for 7 days).
Twenty-two participants (42.3%) underwent a tracheostomy a median of 15 days (IQR 12–19) after admission. Tracheostomy was associated with a longer duration of mechanical ventilation, ICU and hospital LOS, but not associated with ICU survival. Those who required tracheostomy scored a median CPAx score of 1 (IQR 0–2) in the first 7 days, whilst those who did not scored a median of 9 (IQR 0–26) (p = 0.019).
A median CPAx score of ≤6 in the first seven days was associated with a relative risk of tracheostomy of 1.95 (95% CI, 1.30-2.92).
Conclusion: Results indicate that a CPAx score of ≤6 in the first week of admission to cardiothoracic ICU is associated with a two-fold increase in the need for a tracheostomy. This suggests that physical function, measured by the CPAx tool, may be of use when deciding whether to perform a tracheostomy procedure or considering early tracheostomy. Further large-scale studies are required to determine full prognostic value of the CPAx.
Limitations include the retrospective nature of this study.
0191
Severity of post intensive care syndrome in adult ICU survivors is associated with prior mental health diagnosis: a regression analysis
Peter Killeen1, Andrew Slack1, Helen Vollmer1, Louise Hjorth1, Kelly Morris1, Chole Apps1, Nicole Walmsley1, Anna Janssen1, Mervi Pitkanen2 and Joel Meyer1
1Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
2South London and Maudsley NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Life after critical illness can be complicated by ‘post intensive care syndrome’ (PICS) which is characterised by new impairments of cognitive, psychological and physical function. The Guy’s and St Thomas’ NHS Foundation Trust (GSTFT) Critical Illness Recovery Clinic delivers multimodal support to individuals and their families recovering after critical illness. Eligible individuals (adults mechanically ventilated >72 hours and/or received ECMO and/or ICU delirium) are evaluated at 2–3 months post hospital discharge by a multidisciplinary team including critical care consultant, critical care nurse, neuropsychiatrist, clinical psychologist, occupational therapist and physiotherapist. Individuals are screened for physical function, sexual function, quality of life, mental health and cognition.
Objective:
1.To present our experience of delivering a novel ‘carousel model’ critical illness outpatient recovery clinic.
2. To evaluate incidence of PICS features in a cohort of critical illness survivors attending clinic between 2015 and 2018.
Methods: We performed a single centre retrospective service evaluation of clinic records between 10/4/2015 and 22/6/2018. The primary outcome was incidence of PICS features. We analysed the frequency and severity of depression (PHQ9), anxiety (GAD7) and post-traumatic stress disorder (IESR) collected via self-rated questionnaires, as well as physical symptoms, sexual function (SCSR), cognition (MOCA), need for follow up, and onward referrals. We collected demographics, past medical history, illness severity, organ support, length of stay and did a regression analysis of factors associated with outcome.
Results: 268 clinic records were analysed for the period 10/4/2015 to 22/6/2018. Median age was 53 years, 43% were female. Median unit length of stay was 18 days, median advanced respiratory days was 11, median APACHE score of 17, median initial SOFA score of 5. 37% of our cohort received ECMO. Median time from hospital discharge to clinic attendance was 11 weeks (13 weeks from critical care unit discharge). The most common physical complaint found was generalised weakness (43%), followed by hair loss (20%), sensory changes (13%), neuropathic pain (11%), altered taste (9%), tracheostomy scar problems (6%), sexual dysfunction (5%), digital vascular problems (2%). 39% of patients had objective evidence of impaired cognition at clinic (MOCA ≤ 25), and subjectively 73% described reduced memory performance and 80% described reduced concentration/attention. 29% of patients displayed features of moderate/severe anxiety (GAD-7 ≥ 10), 42% of patients displayed features of moderate/severe depression (PHQ-9 ≥ 10). 33% of patients had a mental health intervention following the post critical care clinic (such as onward referral to the CMHT or commencement of antidepressant). 34% of patients re-attended the clinic for 6 or 12 month follow up, most commonly for clinical psychology intervention. Regression analysis showed that the presence of a previous mental health diagnosis was associated with a higher PHQ-9 and GAD-7 score at clinic assessment. No other patient or illness factors associated with clinic outcome.
Conclusion: The incidence of physical, psychological and cognitive impairments is considerable. Prior mental health status was associated with higher depression/anxiety scores. This study shows that comprehensive outpatient evaluation of patients recovering from critical illness is feasible and highlights the value of a multidisciplinary critical illness recovery service.
0192
An Audit to Demonstrate Clinical Pharmacist Interventions in Critical Care
Gursharan Virdee and Emma Graham-Clarke
Sandwell and West Birmingham NHS Trust, Birmingham, United Kingdom
Abstract
Introduction: Clinical pharmacists are a valuable member of the critical care multidisciplinary team (MDT) and promote high standard of care to intensive care patients. One study (PROTECTED-UK) investigated numerous interventions from twenty-one units over a 14-day period and highlighted the impact of pharmaceutical interventions in optimising patient care with consideration to different levels of pharmacists experience (Rudall et al. 2017). The study demonstrated that there was a moderate inverse correlation between intervention rate and the time spent on the CCU. A strong inverse association was observed between optimisation rate and the total number of prescriptions reviewed per day (Richard et al.,2018). Currently, at Sandwell and West Birmingham NHS Trust a clinical pharmacist spends four months cross-site during rotation on the Critical Care Unit (CCU) and attends daily consultant led ward-rounds The aim of this work is to collate pharmaceutical interventions recommended by the rotational clinical pharmacist during consultant-led ward rounds on CCU.
Objectives: To document clinical pharmacist interventions suggested during consultant-led ward rounds.
Method: Documentation of interventions were collated daily by a rotational pharmacist post-consultant ward round. Interventions were recorded onto Microsoft Excel® software by recording date, description of intervention and outcome. Retrospective data analysis was undertaken by the same rotational pharmacist to avoid bias. Categorising of pharmaceutical interventions was undertaken to reflect the types of interventions made.
Results: A total of 282 interventions were documented by the rotational pharmacist from 15th August to 31st December 2018. Graph 1 shows the number of interventions based on British National Formulary (BNF) chapters. Further categories of pharmaceutical interventions included drug-drug interactions, antibiotic stewardship/allergies, absorption/enteral feed administration, disease-drug interaction, advice provision, intravenous administration, drug history (DHX) discrepancy, prescription legal/appropriateness errors. Graph 2 shows as the rotational pharmacist developed, more proactive (advice-giving) interventions were made. Although reactive (e.g. wrong drug particulars) interventions initially exceeded proactive interventions, as the pharmacist developed more confidence and knowledge more sound clinical advice was provided. Advise requested by nurses (consult) remained continuous throughout the data collection process. 94% of recommended interventions by the clinical pharmacist were actioned by the medical team, whereas 6% were not. Interestingly, only one intervention was made for intravenous medication which demonstrates the robustness of the pre-prescribed intravenous prescriptions.
Limitations: Due to other rotational commitments the pharmacist was unable to record interventions daily therefore number of interventions may be greater than specified in Graph 1. Electronic prescribing will provide a platform to monitor and record interventions far more effectively.
Recommendation: Encourage further rotational pharmacists to document pharmaceutical interventions. Consider daily intervention form and collate information onto daily spreadsheet and regular feedback to medical teams.
Graph 1: Number of pharmaceutical interventions as per BNF Chapters
Graph 2: Pharmacist's development vs.type of interventions
0193
Falling into the ICU – An Overview of NOF Fracture Admissions
Jacyntha Khera, Jagdish Sokhi and Roger Davies
Magill Department of Anaesthesia and Intensive Care, Chelsea & Westminster Hospital NHS Foundation Trust, London, United Kingdom
Abstract
Introduction:
• An estimated 65,000 neck of femur (NOF) fractures occur annually in the UK, with the number expected to rise due to an ageing population.1
• The combination of old age, frailty, co-morbidities and surgery has the potential to increase unplanned ICU admissions.
• The 2017 NICE guideline “Management of hip fractures,” emphasises a timely pre-optimisation so that surgery can be achieved within 36 hours of admission.2
• There are no guidelines that identify which patients would benefit from ICU post-operatively for example national emergency laparotomy audit (NELA) and laparotomies.
Objectives:
1. How many patients are admitted and what level of care do they require?
2. Does the type of anaesthetic influence admission to ICU?
3. Does the type of operation influence admission to ICU?
Methods:
• Retrospective review of all NOF fracture patients within the last year (June 2018–19).
• Eligible patients identified from National Hip Fracture Database.
• Review of electronic patient records, including all perioperative documentation.
• A Chi squared test was used for statistical analysis.
Results:
• 207 patients underwent NOF fracture surgery. One patient was excluded due to incomplete notes, (n = 206).
• 15% (n = 31) of patients required ICU post-operatively.
• 42% (13/31) required Level 1; 58% (18/31) required Level 2; and no patients required Level 3 care.
• 89% (16/18) of patients on Level 2 care required metaraminol and 11% (2/18) noradrenaline (started intra-operatively).
• There was no statistical difference (p = 0.43) in the rates of ICU admission in those undergoing a general anaesthetic (GA) 17% (17/96) vs a regional anaesthetic (RA) 13% (12/89). (Figure 1)
• Although the numbers were low, total intravenous anaesthesia (TIVA) trended towards a reduced admission rate (6%;1/16), whereas, a combined GA/spinal approach had a higher relative admission rate (60%;3/5).
• The majority, 89% (27/31), of admissions were after hemiarthoplasties or intramedullary (IM) nails. (Figure 2)
• This represents 37% (18/49) of the total IM nails and 23% (15/65) of the total hemiarthoplasties performed that year.
Discussion:
• In our institution, 15% (approximately 1 in 7) patients require postoperative ICU care. Of these, 58% (18/31) require admission for on-going vasopressor support.
• The type of anaesthetic (GA vs RA) does not appear to influence postoperative ICU requirements. Our findings support the NICE guidance which states “offer patients a choice of spinal or general anaesthesia,’’ suggesting neither technique is inferior.2
• Further work is needed to ascertain whether TIVA reduces postoperative vasoplegia and hence ICU admissions, as well as the benefits/risks of using a combined GA/RA approach.
• IM nails/hemiarthoplasties are complicated, longer, and more challenging operations that have a higher incidence of requiring ICU.
Conclusions:
• To improve patient flow through theatres and minimise operative delays, our data suggests that the following patients would benefit from timely consideration for ICU admission:
^ Patients listed for hemiarthoplasties/IM nails
^ Patients undergoing a combined anaesthetic technique
^ Those that develop significant intra-operative vasopressor requirements
Figure 1.
Anaesthetic type and relative ICU admission.
Figure 2.
Operation type and relative admission to ICU.
0194
Inverted Takotsubo :A case report of inverted takotsubo syndrome secondary to sub-arachnoid haemorrhage
Avinash Jha, Peter Frank and Nicholas Truman
Lancashire Teaching Hospitals NHS Foundation Trust., Preston, United Kingdom
Abstract
Background: Inverted Takotsubo syndrome (ITS) is a rare variant of Takotsubo Syndrome (TTS), accounting for approximately 5% of cases. TTS typically displays a cardiomyopathy pattern involving more than one coronary artery territory, without evidence of obstruction on coronary angiography.1 The incidence of TTS is 1–3%.1 Compared to the classical variant, ITS can have features similar to an acute coronary syndrome (ACS) showing a hyperdynamic apex and hypokinetic basal ventricular regions. ITS is associated with cardiogenic shock (20% cases) and acute heart failure (45% cases).2 Although similar to ACS on echocardiography, there are important differences in their management.
Features of inverted Takotsubo versus classic variant
• Hyperkinetic apex and hypokinetic base
• younger age at presentation – hypothesized to more adrenoreceptors at base relative to apex in young compared to elderly
• ST-segment depression more prevalent in patients with atypical variants including ITS (10.8% vs:7.0%,P = .03) compared to TTS3
• More commonly associated with triggering factors such as mental or physical stress3
• Higher troponin-I elevations in rTTM (13.1 ng/ml vs:1.6 ng/ml,P = 0.001)4
• Significantly higher plasma epinephrine levels in rTTM (809 pg/ml vs:380 pg/ml,P = 0.04)5
Case details: Our patient was admitted to critical care unit for cardiorespiratory support. During the first 48 hours CVS instability developed and their noradrenaline requirement increased to 1.4mcg/kg/min. Hypovolemia was excluded using LidCO and focused echocardiogram, which suggested acute LV failure (Figure 1). Dobutamine was commenced at a dose of 4 mcg/kg/min. The formal echocardiogram revealed basal and mid ventricular hypokinesia and hyperkinetic apex of the LV. The initial troponin was 1016 and ECG showed ST depressions of 0.5 mm in leads V1-V4. Cardiovascular stability returned over the following 48 hours and a repeat echocardiogram (Figure 2) found that LV function had returned to normal.
A normal coronary angiogram is optimal for diagnosis for TTS, but it was not performed considering the age, absence of risk factors for coronary artery disease and early reversal of hemodynamic instability.
Management principles of Inverted TTS
The treatment of this syndrome is mainly supportive. The aim should be to maintain coronary perfusion pressure such that the oxygen/demand ratio is adequate and the cardiac workload is reduced. In our case we used dobutamine to augment the cardiac output without causing excessive afterload. As per the European consensus statement on TTS, mild cases are treated with ACE inhibitors and Beta-blockers. However, in cases with features of LV outlet obstruction or cardiogenic shock, beta-blockers are contraindicated. Levosimendan and ventricular assist devices may have a role in severe cases. Noradrenaline may worsen LV outflow tract obstruction and should be used cautiously under expert guidance with dynamic assessment of LV function.
Conclusion: ITS is a rare variant of TTS and consequently may be under-reported or even misdiagnosed as ACS. Early echocardiography and a low index of suspicion are key. Once recognized treatment requires maintenance of coronary perfusion pressure with avoidance of excessive vasopressors, which may worsen outflow obstruction. Angiography is required to definitely exclude ACS, but the risks of this procedure should be taken into account, especially in a patient cohort which is often young and low risk for atheromatous disease.
0196
Changes in Sedation Practices Within a Tertiary Critical Care Unit: 2012-Present day
Christopher Duncan, Caroline Higenbottam and Randeep Mullhi
Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Optimising sedation practices on intensive care aims to facilitate nursing and medical care whilst minimising associated complications. Frequently encountered complications of deep sedation include cardiovascular instability necessitating the use of vasopressor agents, prolonged invasive ventilation1, increased delirium rates2 and overall longer length of stay3
Objectives: We reaudited the practice of sedation across our 100 bedded critical care unit to gain a snapshot of current practice, the depth of sedation being targeted and whether there was diurnal variation in depth of sedation. Comparison was made to two previous audits conducted in 2012 and 2016 to assess change in practice with the aim of suggesting improvements.
Method: The Prescribing Information and Communications System (PICS), the electronic patient record system used at Queen Elizabeth Hospital Birmingham, was interrogated for sedation prescriptions, administrations and hourly Richmond Agitation Sedation Scoring (RASS) scores and then collated onto data collection sheets. Sedation holds were recorded and when they did not occur the nursing documentation was analysedto identify reasons. We had access to the data collected in both 2012 and 2016 audits to allow comparison.
Results: 128 patient episodes were interrogated. Propofol and alfentanil were the most commonly administered sedatives in 94.6% of patients. Morphine (2.2%) and midazolam (2.4%) usage has declined compared to 2012 when 19% of patients received morphine and midazolam for sedation. <1% of patients received remifentanil or ketamine.
The average RASS score during the day was −2.07 and night −1.45 with an overall average of −1.76. A sedation hold was performed on 62.7% of sedation days. The reason for a sedation hold not being performed was most commonly for clinical instability or reason undocumented. Therapeutic deep sedation for modifying secondary brain injury was only performed in 7.8% of patients.
Conclusion: This reaudit demonstrates the increased use of propofol and alfentanil with reduced use of morphine and midazolam. Alfentanil was commonly continued following a sedation hold and extubation in post-operative patients for analgesia.
Previous audits have demonstrated lower RASS scores throughout both day and night and have suggested patients are oversedated, particularly at night. Our findings revealed an apparent change in practice. We found overall higher average RASS scores. Interestingly average deeper sedation scores were found during the day and patients were less sedated overnight. The reason for this is unclear and is an area for further investigation.
Our data identified that on 37.3% of sedation days the patient did not receive a sedation hold and in many cases the reason was not documented. This shows little change from 2016 and 2012 when 40% and 41% of patients respectively did not have a sedation hold. Previous audits have found a lack of understanding around the reason for sedation hold and education implemented post previous audits does not appear to have impacted the figures.
0197
Introduction of checklist for airway trolley improves the safety of Emergency Department intubations
Fiqry Fadhlillah, Mike Dean and Ali Refson
London North West University Healthcare NHS Trust, London, United Kingdom
Abstract
Objectives/Background: The 4th National Audit Project of the Royal College of Anaesthetists (RCoA) and Difficult Airway Society (DAS) (NAP4) was designed, in part, to look at airway management in ED and highlight any deficiencies that have or could have led to serious harm. Analysis of cases highlighted gaps in care, which included inadequate equipment for intubation.
It is important that when presented with a complex and rapidly deteriorating airway, the ability to progress in the airway management strategy should not be constrained by the lack of equipment/drugs. This study was thus designed to develop a standardised checklist for the airway trolley in ED and evaluate its effectiveness at reducing equipment-related complications.
Methods/Design: A retrospective audit was conducted to evaluate the scale of the problem. Using the hospital’s Symphony programme, all attendances from 1st September 2017 until 1st September 2018 fulfilling one of the following criteria were searched to identify all adult (>18 years old) intubations performed in the Emergency Department:
• Transferred to another hospital
• Died in the Emergency Department
• Referred to Intensive Care Unit (ICU)
• Admitted to ICU
Scanned notes were scrutinised to identify probable equipment-related intubations. The contents of the airway trolleys in ICU and theatres were used as the basis for the creation of a new airway trolley checklist. Post-introduction compliance and analysis of cases were conducted to identify any complications.
Results/Conclusions: Overall, eight complications were reported in the pre-checklist period, two of which were probable equipment-related complications. Both were Cormack-Lehane grade III, developed oxygen desaturation and one required multiple attempts at intubation. Compliance against the checklist was recorded over a 10-week period; by week five of implementation, compliance was >90% and maintained at that value. There were no equipment-related complications in the post-introduction period.
0198
Dedicated teaching improves the confidence of Emergency Department nurses in managing difficult airway
Fiqry Fadhlillah, Mike Dean and Ali Refson
London North West University Healthcare NHS Trust, London, United Kingdom
Abstract
Objectives/Background: Intubation forms an integral role in the treatment of the critically ill or injured patients presenting to ED with a deteriorating airway. The acuity of their presentation may often necessitate a rapid placement of an endotracheal tube. Emergency intubations are not without risks, not least due to the emergency nature of the procedure.
The 4th National Audit Project of the Royal College of Anaesthetists (RCoA) and Difficult Airway Society (DAS) (NAP4) was designed, in part, to look at airway management in ED and highlight any deficiencies that have or could have led to serious harm. Analysis of cases highlighted the following gaps in care:
• Poor or delayed recognition of at-risk or deteriorating patients
• Inadequate preparation
• Insufficiently trained staff
• Inadequate equipment
The aim of the study was thus to devise a targeted teaching programme for Emergency Department nurses, in order to improve their confidence at managing airway difficulties and assisting in Emergency Department intubations.
Methods/Design: Pre-intervention surveys were distributed to Emergency Department nurses working at a district general hospital. Nurses took part and were given access to five targeted teaching programmes and material: (1) 30-minute slots were dedicated for theoretical learning, spread across eight study days; (2) 10-minute simulation scenarios were organised across an entire day; (3) aide-memoires were produced on intubating drugs, equipment, roles, difficult airway algorithm and emergency tracheostomy and laryngectomy management; (4) e-learning material and (5) online video were produced. Surveys were distributed post-intervention.
Results/Conclusions: 68 nurses took part in the programme. Pre-intervention surveys showed poor comprehension (% those with no or little understanding) of the decision-making process (42%), equipment (40%), drugs (60%), roles (50%) and the difficult airway algorithm (70%). This improved to 5%, 10%, 9%, 6% and 7% respectively. There was 100% satisfaction rate for teaching days, simulation scenarios and video, with 98% for e-learning and 97% for aide-memoires.
0199
P25/30 Somatosensory Evoked Potentials and their role in neurological prognosis of comatose survivors post out of hospital cardiac arrest
Nicholas Gourd1, Lucy Nye2, Colin Bigham1, Andrew MacCormick1, Nicola Broomfield2, Rosalyn Squire1, Nigel Hudson2 and Nikitas Nikitas1
1University Hospitals Plymouth NHS Trust, Derriford Hospital, Department of Intensive Care Medicine, Plymouth, United Kingdom
2University Hospitals Plymouth NHS Trust, Derriford Hospital, Department of Neurophysiology, Plymouth, United Kingdom
Abstract
Introduction: N20 Somatosensory evoked potentials [SSEPs] are used for neurological prognosis in comatose survivors post out of hospital cardiac arrest [OHCA]. The absence of N20 is correlated with poor neurological recovery.1 However, the presence of N20 is inconsistent with a positive functional outcome.2,3 Another slightly later component of the recorded SSEP, the P25/30 complex could potentially improve the prognostic value of N20 if analysed simultaneously.
Objectives: Analyse the early SSEP recording performed at 24–36hours [h] after return of spontaneous circulation [ROSC] in comatose survivors post OHCA who are not treated with therapeutic hypothermia, in order to:
1. To clarify the components of the 20–30msec SSEPs complex in each recording and resulting patterns of N20-P25/30 combinations.
2. To validate whether the presence or absence of [P25/30 s] in that complex could improve the prognostic value of N20.
Methods:
Design: Single-centre, prospective, observational, study.
Patients: Adult comatose survivors post non-traumatic OHCA without any acute or chronic neurological illness and without haemorrhagic shock. The first 9 months of the study, 29 patients have been recruited. On ICU, targeted temperature management at 36oC for the first 24 h and then 36–37oC for the next 48 h post ROSC and neuroprotection were applied. Patients remained sedated, intubated and ventilated for the first 24–36 h.
SSEP Recording: SSEPs were recorded as early as possible after 24 h post ROSC. The mean time of recordings in the first 29 patients was 26 h. Recordings were then interpreted for the N20 and P25/30 status by two neurophysiologists.
Follow-up: The cerebral performance category [CPC] was recorded on day of hospital discharge.
Preliminary results:
Patients characteristics: The main characteristics of the first 29 recruited patients are shown in table 1.
Results of recording:
The results of the analysis of the first 20 recordings are shown in table 2.
Conclusions: Based only on the small number of recordings analysed so far, the following could be suggested:
• Four distinct patterns of N20 and P25/30 combination could be identified: Present N20-present P25/30; present N20-absent P25/30; absent N20-present P25/30; absent N20-absent P25/30.
• In patients with present N20, the additional analysis of P25/30 could potentially increase N20’s positive predictive value.
• In patients with absent N20, its highest negative predictive value is maintained regardless of the presence or absence of the P25/30 in these cases.
It remains to be clarified whether the above preliminary suggestions become established while the number of patients enrolled to the study increases.
ClinicalTrials.gov Identifier: NCT03881865
Table 1.
| Mean age [years] | 62.9 |
|---|---|
| Gender [patients] | Female [12] Male [17] |
| Aetiology of cardiac arrest [patients] | cardiac [19]: arrhythmia [9]; MI [10] pulmonary embolism [1] respiratory arrest [5] |
| Cardiac arrest rhythm [patients] | VF/VT [15] PEA/asystole [10] |
| Bystander CPR [patients] | 22 |
| Mean anoxia time [min] | 28 |
| Mean ICU length of stay [days] | 5.8 |
| Mean hospital length of stay [days] | 11.2 |
| Mean GCS post ROSC | 3 |
Table 2.
| Neurological outcome Favourable: CPC 1-2 Unfavourable: CPC 3-5 | Number of patients |
||
|---|---|---|---|
|
N20 | |||
| Present | Absent | ||
| P25/30 | |||
| Present | Favourable | 6 | 0 |
| Unfavourable | 2 | 2 | |
| Absent | Favourable | 0 | 0 |
| Unfavourable | 1* | 9 | |
*Variable with different thresholds.
0200
Procalcitonin as an Outcome Predictor
Nabeel Amiruddin1, Michael Reay2 and Halden Hutchinson-Bazely2
1Dudley Group Hospitals NHS Foundation Trust, Dudley, United Kingdom
2The Dudley Group NHS Foundation Trust, Dudley, United Kingdom
Abstract
Introduction: Procalcitonin (PCT) is a marker of bacterial infection with greater specificity than C-reactive protein and white-cell count. It is utilised for the diagnosis of infection and informing the initiation, alteration or cessation of antibiotics. There is variability of how PCT is utilised with respect to interpretation of the initial and subsequent rates of change. At our Intensive Care Unit in Russells Hall Hospital, Dudley, we have been measuring PCT levels in our patients on an increasingly frequent and now daily basis.
Objective: We intended to evaluate the initial PCT and PCT clearance as predictors of ICU survival, hospital survival and duration of cardiovascular support in our patients.
Method: We conducted a retrospective analysis by extracting all PCT values, dates of PCT test and their associated hospital identification numbers since 1/1/2016 until 31/12/2018. Using data analytic software (RStudioTM), all patients without at least 2 PCT values associated with them were removed. The PCT clearance was calculated from the mean percentage decrease per day between the first and second PCT values. We matched each patient to outcomes including ICU survival, hospital survival, length of ICU stay and duration of cardiovascular support using our local ICNARC data. We used multivariate logistic and multilinear regressions to evaluate the degree to which these predictor variables are associated with the dependent variables. In addition, we used a non-linear machine learning model called Random forest to attempt predictions of hospital mortality using initial PCT and PCT clearance as predictors.
Results: 214 patients were found to have at least 2 PCT values and entered for analysis. 42 of the 214 died on ICU. Of the ICU survivors, 24 died in hospital. Neither the initial PCT nor PCT clearance were associated ICU survival (p = 0.683 and 0.725 respectively), hospital survival (p = 0.962 and 0.081 respectively) or duration of cardiovascular support (p = 0.220 and 0.513 respectively). However, after training our Random forest model with 75% of the dataset, the ICU and in-hospital mortality of the remaining 25% (54 patients) was predicted. The Random forest model predictions of both outcomes had an overall 86.8% and 90.7% accuracy respectively. 10 and 6 patients in the test-set of 54 were predicted to die in ICU and hospital respectively. Of these predicted mortalities, 50% in both groups actually died.
Conclusions: Initial PCT and PCT clearance do NOT perform as predictors of ICU survival, hospital survival or duration of cardiovascular support, neither individually not in combination. Although there was possibility a trend towards PCT clearance being positively associated with hospital mortality. Since we continue to utilise PCT in our routine practice, the analysis could be repeated in time with larger numbers of patients. We were able to able to predict both ICU and in-hospital mortality with 50% accuracy using a Random forest machine learning model, suggesting a non-linear relationship between the combination of initial PCT and PCT clearance and both survival outcomes.
0203
Anaemia and Thrombocytopaenia in ICU: When transfusion is not the answer!
Eleanor Richards C, Musarat Hussain and Kirsty Nweze
Queen's Hospital, Barking Havering and Redbridge Trust, Romford, United Kingdom
Abstract
Background: Anaemia and thrombocytopenia in critically unwell patients are common and often a complex diagnostic challenge. Initiating the correct early management often hinges on formulating this differential early on. Furthermore, given the higher morbidity and mortality if these group of patients rapid diagnosis is paramount, to allow delivery of time critical interventions. We present three unique cases, which exemplify the diagnostic challenges faced.
Case 1: 77 year old female with a background of hepatitis C presented with confusion, reduced mobility and jaundice over several weeks. Initial tests revealed a haemoglobin of 2.7 g/dL. Formal blood test results also demonstrated thrombocytopenia, acute kidney injury and raised inflammatory markers. Further haematological tests revealed low B12 and also a positive DAT (direct antiglobulin test). After initial stabilisation with vasopressors and haematology discussion the patient received B12 replacement as well as intravenous steroids for AIHA (autoimmune haemolytic anaemia). Intravenous antibiotics were initiated for possible urosepsis and transfusion of packed red cells was targeted to achieve a haemoglobin of no more than 5.0 g/dl within the first 24 hours of admission. Patient made a slow recovery on the unit. It was felt that she had a picture of a chronic B12 deficiency with superimposed urosepsis (ecoli found in urine culture).
Case 2: 25 year old female was admitted to the high dependency unit after an emergency C-section. The pregnancy was uncomplicated, in particular no evidence of preeclampsia. She fulfilled Sepsis 6 criteria and a working diagnosis of chorioamionitis with possible streptococcal sepsis made. She remained anuric and required single organ renal support. Bloods revealed evidence of intravascular haemolysis, thrombocytopenia and acute kidney injury. Urinalysis revealed active urinary sediment. ADAMTS13 was low (34). A diagnosis of atypical haemolytic uraemic syndrome (aHUS) made. The patient was transferred to a tertiary renal centre where a renal biopsy showed cortical necrosis. The patient continues to be dialysis dependent with a guarded prognosis and is preparing for renal transplantation.
Case 3: 39 year old 24 weeks gestation female presented to ICU with hypoxaemic respiratory failure. She had recently been diagnosed with T3N1M0 invasive ductal breast cancer and underwent a mastectomy 2 weeks before with a plan to start chemotherapy. A V/Q scan was indeterminate for a PE so she was empirically treated with LMWH. She remained oxygen dependent and over the next few days laboratory results revealed anaemia and thrombocytopaenia, a HIT screen was negative. Haematinics revealed high ferritin and B12. Further clinical deterioration with hypoxia and massive hepatomegaly necessitated intubation and ventilation, and emergency C-section. MDT discussion recommended a bone marrow biopsy which confirmed secondary Hemophagocytic lymphohistiocytosis syndrome. She was transferred to specialist obstetric haematology centre for ongoing management.
Conclusion: This case series demonstrates the need for a robust understanding of the array of conditions which lead to these haematological disturbances. Emphasis should be given to the most probable/life-threatening aetiology from an early stage. To aid this, we have created a bespoke, logical algorithm to simplify the creation and narrowing of this broad differential.
0204
“SALAD SIM”: In situ training for the emergency management of gastric aspiration
Matt Rowe1, Ed Gomm2 and Ed Miles1
1North Bristol NHS Trust, Bristol, United Kingdom
2Great Western Hospitals NHS Trust, Swindon, United Kingdom
Abstract
Aspiration is the single most common cause of death due to anaesthetic related events, far outweighing the much feared can’t intubate, can’t oxygenate scenario (CICO).1 Furthermore, at least one in four reported adverse airway events has been shown to occur on intensive care units (ICU) or in the emergency department.1 Whilst most patients in an emergency setting will undergo a rapid sequence induction, should aspiration occur it is a true emergency. Following a successful pilot, we used a part-task mannikin to deliver an in-situ training session for anaesthetists and intensivists in the emergency management of gastric regurgitation and aspiration.
A realistic regurgitating mannikin was procured for the training session (Life/formâ S.A.L.A.D Simulator). Pre-course and post-course questionnaires were used to assess prior experience of aspiration and the impact of training. A video laryngoscope was used to demonstrate the technique, but participants were encouraged to use direct laryngoscopy to reflect the equipment immediately available to them in each theatre. Teaching focussed on the S.A.L.A.D technique (Suction Assisted Laryngoscopy and Airway Decontamination)2 which focusses on concurrent suction and laryngoscopy to expedite endotracheal tube delivery.
Forty-one participants underwent training (21 consultants and 20 trainees or non-consultant grades). There were a total of 110 self-reported aspiration events and 19 self-reported CICO events during a combined 485 years of experience. In our department, per individual this equates to an average frequency of 4 years for aspiration and 27 years for a CICO event. Self-declared choice of positioning for managing aspiration changed as a result of the training (chart). Ninety-five percent of participants stated that if confronted with overwhelming airway soiling they would now use the SALAD technique and would recommend the training to their colleagues. Feedback was positive, with the session rated as a simple, well-demonstrated technique on a realistic simulator.
Despite being more frequent than a CICO event, intensivists rarely practice the management of overwhelming gastric regurgitation and aspiration. Conventional management involves a steep Trendelenburg position to promote passive drainage of gastric contents. However, this potentially makes securing the airway more difficult, may take longer and as is not always feasible.3 We have developed a targeted and realistic simulation session to address this training deficit, and taught a novel, practical technique for the emergency management of airway soiling. We have now embedded this in the simulation training course for acute care common stem trainees in our region.
0205
Faeco-Pneumothorax : An unusual and rare presentation of colonic anastomotic leak
Lewys Winfield Young
Princess of Wales Hospital, Bridgend, United Kingdom
Abstract
Faeco-Pneumothorax is an unusual and rare cause of respiratory failure. We report the case of a 64 year old gentleman with history of ischaemic heart disease and diabetes mellitus, who had a laparotomy and left hemicolectomy for an obstructing splenic flexure carcinoma. Five days post operatively he developed severe chest and abdominal pain alongside respiratory distress. Initial investigations revealed a pneumoperitoneum and a left sided pneumothorax. Following chest drain insertion, air and faeculent fluid was drained from the pleural cavity. A laparotomy revealed a perforation of the colon near the anastamosis which was adherent to the left copula of the diaphragm and penetrating through it. This case report highlights the rarity of faeco-pneumothorax as well as the possible complication of anastomotic surgery
0207
Airway obstruction in an adult due to a retained nasopharyngeal foreign body – a potential "coroner's meat"
Xenia David, Venkat Sundaram and Lakhbir Kaur
Glan Clwyd Hospital, Rhyl, United Kingdom
Abstract
Background: Nasopharyngeal foreign bodies (FBs) are uncommon, but potentially life-threatening. We present a case where a FB concealed in the nasopharynx caused airway obstruction on extubation.
Case Presentation: A 48-year-old male was brought to the emergency department (ED) after he choked on a piece of meat. His medical history included epilepsy, hypertension, and stroke with mild residual left-sided weakness. He had a previous choking incident requiring a brief hospital admission.
His family heard choking sounds from the kitchen, and rushed in to find the patient unconscious on the floor. They did CPR and called in paramedics, who revived him with bag-mask ventilation (BMV). The foreign body was said to have been expelled. The patient managed to sit up, but had a seizure and collapsed. There was difficulty in ventilating him, and he was transferred to the ED.
On admission, the patient was GCS 3, extremely cyanosed, with saturation ranging from 60 to 80%. Intubation was immediately done using a McGrath videolaryngoscope. A grade 1 airway was seen, with no visible FB in the oropharynx. Despite a succesful intubation, the patient's saturation hovered at 70%. A bronchoscopy showed frothy secretions in the tracheobronchial tree, and the chest x-ray revealed diffuse hazy infiltrations. The patient was diagnosed with negative pressure pulmonary oedema and brought to the ICU for ventilatory support.
On day 2 the patient had markedly improved, though he continued to have bloody, foul-smelling secretions. He was extubated fully awake, but desaturated and developed stridor and wheezes shortly after. His saturation continued to drop despite nebulised salbutamol and intravenous steroids. BMV was done and he was intubated. On laryngoscopy, a grayish mass was seen in the posterior pharynx, which disappeared into the nasopharyngeal space behind the uvula. The FB – a decomposing piece of beef – was fished out using a Magill’s forceps. A bronchoscopy showed bits of organic material in both bronchi.
The patient eventually improved on supported ventilation and antibiotics, and was extubated on day 8. His swallowing was found to be possibly impaired, and he was advised to have a videofluoroscopic assessment.
Conclusions: Most nasopharyngeal FBs are found in children who introduce objects into their nasal passages. The FB can orally reach the nasopharynx through regurgitation, coughing, Heimlich maneuvre, or by being in a supine position. Though uncommon in adults, it may happen in those with neurological impairment, altered sensorium, or through traumatic penetration. Such FBs may be missed, and can be detectable through X-rays (if radio-opaque) or naso-endoscopy.
During ENT procedures such as adenotonsillectomies, the concealed nasopharyngeal object may be a blood clot which can cause fatal airway obstruction upon extubation – hence the term “coroner’s clot.” In this incident, a FB was thought to have been expelled following a choking incident, and was not visible on intubation. In choking cases where a FB has not been retrieved, it is advisable to examine the nasopharyngeal space prior to extubation.
Figure 1.
Retrieving a foreign body concealed in the nasopharynx.
0208
A prospective cohort study evaluating the performance of a new screening tool to identify intensive care unit survivors at high risk of 90-day unplanned hospital readmission
Ellen Pauley, Jo Thompson, Lucy Barclay, Eddie Donaghy, James Marple and Tim Walsh
University Dept of Anaesthetics, Critical Care and Pain Medicine, University of Edinburgh, Edinburgh, United Kingdom
Abstract
Introduction: A high 90-day unplanned hospital readmission rate has been reported in intensive care unit (ICU) survivor patients in Scotland (25%).1 Pre-critical illness factors e.g. pre-existing comorbidity, are stronger predictors of readmission than more acute factors [1,2]. The Preventing Early Unplanned Hospital Readmission After Critical Illness (PROFILE) study identified a dichotomy of readmission contexts: medically unavoidable readmissions, and readmissions resulting from complex health and psychosocial patient needs, which may have been preventable.3 Factors contributing to readmission e.g. poor social support, were identified from patient and carer perspectives.3
Supporting Community recovery and reducing reAdmission Risk Following critical illness (SCARF) is a quality improvement project with the aim of reducing this readmission rate by using a new screening tool to identify ‘high risk’ ICU survivors. This assesses risk factors for readmission based on those identified in the PROFILE study.3 The screening tool was piloted whilst an anticipatory care pathway for high risk survivors was evaluated.
Objective: To evaluate the validity and predictive value of the screening tool for 90-day unplanned hospital readmission, and inform whether the tool effectively identifies high risk ICU survivors.
Methods: All ICU patients 01/06/2018–25/02/2019 at the Royal Infirmary Edinburgh were screened using the SCARF screening process. The SCARF-tool assessed previously identified risk factors for readmission: living alone, polypharmacy, pre-existing mental health/mobility problems, comorbidity. Post-ICU physical and psychological status was also assessed. The screening process was semi-subjective i.e. there was no cut-off number of risk factors required to screen SCARF-positive. The screening process was completed by 3 members of the SCARF team prospectively using information in the electronic medical record (TrakCare). The primary outcome was 90-day unplanned hospital readmission (also determined prospectively through TrakCare). The readmission rates in SCARF-positives and negatives were compared, and the tool performance was evaluated with diagnostic test parameters.
Results: 946 ICU survivor patients were screened by SCARF 01/06/2018–25/02/2019: 257 (27.2%) and 689 (72.8%) screened SCARF-positive (high-risk of readmission) and SCARF-negative (low-risk) respectively. 99/194 (51.05%) SCARF-positives vs 102/510 (20.0%) SCARF-negatives alive at 90-days post-ICU discharge experienced 90-day hospital readmission. The relative risk of readmission was 2.55 (95% confidence intervals: 2.04-3.18) (p < 0.0001) with screening SCARF-positive.
The SCARF-tool was 49.3% sensitive and 81.1% specific. Positive and negative predictive values were 51.0% and 80.0%. Positive and negative likelihood ratios were 2.61 and 0.63.
Conclusions: The SCARF screening tool effectively identified ICU-survivors at high risk of 90-day readmission. The tool performed best as a rule-in test (to include high-risk survivors in the anticipatory care pathway). SCARF may therefore contribute to reducing the readmission rate by flagging up patients who require increased support in their recovery. However, not all readmitted patients screened as ‘high-risk’ and the proportion of unpreventable readmissions is uncertain. Future analysis and development of the SCARF anticipatory care pathway is warranted.
0209
The EIC-ICU (Enhancing Interprofessional Collaboration in the Intensive Care Unit) toolkit: one institution’s experience with a new quality improvement initiative
Jessica Partington1 and Anthony Cochrane2
1University of Plymouth, Plymouth, United Kingdom
2St Helens and Knowsley Teaching Hospitals NHS Trust, Whiston, United Kingdom
Abstract
Introduction: Effective interprofessional collaboration (IPC) in intensive care units (ICUs) has been associated with better patient outcomes such as reduced mortality rates and length of ICU stay. The level of IPC also predicts the degree to which team members report understanding their patient care goals and how productive they are at achieving these goals. This way of working increases team function and morale and leads to a reduced staff turnover.
Objectives: Reeves et al. (2016) published the EIC-ICU toolkit to aid IPC improvement efforts in intensive care. This details effective methods of evaluating barriers to IPC and selecting appropriate interventions. Using this toolkit, we undertook a quality improvement project to increase the level of IPC in a single-centre intensive care unit in the North West of England. We structured the project using a ‘Plan, Do, Study, Act’ (PDSA) cycle framework.
Methods: Qualitative data was collected through ethnographic observation and one to one interviews. Field notes on interprofessional interactions were collected over approximately 20 hours of observation across varied shift patterns and locations on the unit. Members of the ICU team were invited for semi-structured interviews. Questions explored their perception of different professions’ roles and responsibilities, their relationships with different healthcare professionals and their perceived barriers to effective IPC. Quantitative data was also collected using a 5-point scale questionnaire.
These results were used to facilitate an interprofessional workshop, with the primary aim of raising awareness of the importance of IPC in intensive care. Attendees included ICU physicians, nurses, pharmacists, physiotherapists, dieticians, occupational therapists, speech and language therapists and healthcare assistants. The observational and interview data was presented at this workshop and used to construct a perception of roles matrix to explore the interactions between different professional groups. The workshop facilitated various group activities, both educational and team building, which encouraged participants to elaborate on our observational findings using the PROC (processual, relational, organizational, and contextual) framework. In exploring these themes participants were invited to offer suggestions for how to improve IPC on the unit.
Results: Our data indicated that good relationships existed between physicians and nurses and that conflict seldom occurred. Physicians interacted less frequently with the other members of the intensive care team such as physiotherapists and dieticians. The major barriers to these interactions were time constraints and workload. Many unit staff members cover multiple wards and therefore do not have the time available to attend daily ward rounds or multi-disciplinary meetings. Further barriers included different priorities in care across professional groups, the lack of consistency in leadership, and frequent staff rotations without introductions.
The IPC workshop received positive feedback from participants. The outcomes of the workshop included a number of suggestions for improvement, which we grouped into four themes (Team-building, simulation/educational, MDT meeting and handover improvements). Post workshop staff members undertook a prioritisation exercise to identify which interventions to implement. These will then be assessed as part of further PDSA cycles.
Conclusion: The EIC-ICU toolkit provides a useful structure for exploring and enhancing IPC in an Intensive Care Unit.
0211
Low magnesium and albumin levels within the first 48 hours of admission appear to predict poor outcome in septic patients
Pranav Osuri, Aditya Kuravi and Ranjit Bains
Walsall Manor Hospital, Walsall, United Kingdom
Abstract
Introduction: Magnesium is the fourth most abundant ion in the body and is a co-factor for many immunological processes. Hypomagnesaemia has been shown to reduce both cell-mediated and humoral immunity.1 Hypomagnesaemia has a prevalence of 7–11% in hospitalised patients.2
Albumin is a ubiquitous protein. A normal level in the blood stream signifies normal vascular integrity and synthetic function. Hypoalbuminaemia is a common sequela in sepsis.3 A large-scale study showed 21% of acutely ill hospitalised patient were hypoalbuminaemic and their in-hospital mortality was 14%.4
Objective: Assessment of the effect of low magnesium and albumin levels on one-year mortality for patients diagnosed with sepsis.
Methods: A retrospective analysis of magnesium and albumin levels of patients admitted to Walsall Manor Hospital over a four-month period (1/4/2017 – 31/7/2017) with an admitting Healthcare Resource Group (HRG) diagnosis coded as sepsis.
Magnesium and albumin levels in the first 48 hours were collected along with age, comorbidities and mortality data. The serum magnesium level of less than 0.7 mmol/L and albumin level of less than 30 g/l were considered low for the purpose of this study.
Results: A total of 314 patients were admitted with a diagnosis of sepsis.
Twenty three percent (n = 73) of patients had their magnesium levels measured within 48 hours of admission, thirty six percent (n = 26/73) were found to be hypomagnesaemic. The one-year mortality in hypomagnesaemic group was 65% (n = 17/26) in contrast to 47% mortality (n = 22/47) in the remaining sixty four percent eu-magnesaemic group (n = 47/73), with a P = 0.1.
Over ninety nine percent (n = 313) of patients had their albumin levels measured within 48 hours of admission, fifteen percent (n = 47/313) were found to be hypoalbuminaemic. The one-year mortality in hypoalbuminaemic group was 81% (n = 38/47) in contrast to 33% mortality (n = 88/266) in the remaining eighty five percent of eu-albuminaemic patients (n = 266/313), with a P < 0.01.
Five patients were both hypomagnesaemic and hypoalbuminaemic. This subgroup had a one-year mortality of 100% while the one-year mortality in the entire cohort was only 53%.
Conclusion: This retrospective data set demonstrated a trend towards increased one-year mortality rate with an abnormally low level of either magnesium or albumin within 48 hours of hospitalization. This correlation with poor outcome and lower levels of the measured variables was stronger when both variables were used. A large-scale study could validate the robust nature of this correlation and the impact of correction of low albumin and magnesium level on outcome.
0213
Critical Care admissions in patients aged 80 or older at Rotherham Hospital
Ben Marshall and Anil Hormis
Rotherham Hospital, Rotherham, United Kingdom
Abstract
Introduction: In the UK, we have an aging population. The suitability of admitting these patients critical care has been controversial; they are typically resource-demanding and often have poor outcomes.
We collected data on admissions aged >80 years old at Rotherham Hospital, a medium sized critical care Unit in South Yorkshire without specialist surgical services but with a large burden of disease in the local population, unit comprises of 5 Level 3 and 8 Level 2 beds.
We looked at admission data and outcomes to gain a clearer understanding of who we admit to critical care and look for trends regarding their outcomes.
Objective: Our objective was to study critical care admissions of patients aged 80+ to gain a clearer understanding of who we admit and observe any trends regarding their outcome.
Methods: We collected data on admissions to critical care in those aged 80+ since 2017. We collected their reason for admission, frailty score, length of stay before admission, SOFA score, length of ITU stay, which organs were supported, ITU outcome and 30 d mortality. The data was assessed and trends were obtained.
Results: We collected data from 155 patients ranging from 80 to 94 with a mean age of 84. 57% were aged 80–84, 30% were 85–90 and 13% were 90+. 55% of patients were female.
Frailty Index (Rockwood scale) ranged from 2–9 (mean 4.6). The modal score was 3/10 (29%), followed by 4/10 (28%) and 5/10 (15%). We admitted very few patients with low (1-2) or high (8-9) scores.
The most common reason for admission was circulatory failure (21%), followed by post-elective surgery (19%) and respiratory failure (12%).
The overall mortality was 22%.
Frailty score was correlated to mortality (3 = 9% vs. 8 = 25%) and length of stay. However, frailty did not correlate to the number of organs supported.
Respiratory failure produced the longest length of stay (mean 310 hours) followed by severe sepsis (106 h) and polytrauma (69 h). The lowest was head injury (20 h), combined respiratory/circulatory failure (25 h) and elective surgery (46 h).
Combined respiratory/circulatory failure had highest mortality (66%) followed by respiratory failure (39%) and circulatory failure (27%). Conversely, severe sepsis had lower mortality (22%). There was no correlation between frailty score and mortality.
Conclusion: This demonstrates that a significant proportion of elderly patients admitted to critical care have a favourable outcome. It suggests that age should not be a barrier to admission. There is significant work looking at frailty and outcome and this study supports the consensus that lower frailty scores lead to shorter ITU stays and favourable outcomes.
This study shows that patients with combined respiratory/circulatory failure and respiratory failure (without circulatory failure) have the longest stay and highest mortality. Those with sepsis generally do well.
Although European studies have considered this, further work should be conducted in the United Kingdom. We feel our data has a significant number of patients and suggests that correct patient identification may be the key to favourable outcomes. Early involvement from critical care physicians in unwell patients may help this.
0214
Interventions for promoting family member involvement in adult intensive care settings: a mixed-method systematic review
Andreas Xyrichis1, Simon Fletcher2, Sally Brearley3, Julia Philippou1, Edward Purssell1, Marius Terblanche1,4 and Anne Marie Rafferty1
1King's College London, London, United Kingdom
2Kingston & St George's University London, London, United Kingdom
3Kingston and St George's University London, London, United Kingdom
4Guy's and St Thomas' Hospital, London, United Kingdom
Abstract
Background: There has long been a need for greater family member involvement in healthcare. This is especially relevant in intensive care units (ICUs), since the family provide a key communicative and practical link between patient and professional.1–2 There has been no standardised evidenced-based approach that explores research on family member involvement, and the range and quality of contributions remains unclear.3
Objective: To undertake a mixed-method systematic review assessing the evidence base for interventions promoting family member involvement in ICUs; and develop a working typology of interventions for use by health professionals and family members.4
Methods: Bibliographic databases were searched without date restriction: MEDLINE, EMBASE, CINAHL; the Cochrane Central Register of Controlled Trials, Joanna Briggs and Cochrane Libraries. Back issues of leading ICU and patient experience journals were searched, as were the reference lists of included studies. Unpublished literature was sought through the GreyLit/ OpenGrey databases. All evaluation studies of intervention activities promoting family member involvement in adult ICUs were included; all research designs and outcome measures were eligible. Abstracts and papers were independently screened by two reviewers. Included papers were quality assessed by two reviewers independently and in duplicate. Data on interventions, evaluation methods and outcomes were collated using a predetermined extraction table. Heterogeneity of interventions, designs, outcomes and data available meant the synthesis followed a narrative approach. A service user group met with the research team termly for feedback on the process and input to the study conclussions.
Results: Out of 5,109 possible citations a total of 21 studies were included. Published between 1989 and 2018, these were predominantly North American. Most of the studies followed an experimental or observational quantitative design (n = 16), four studies were qualitative, and one adopted a mixed-methods approach. The overall evidence base was assessed as moderate to weak, with only a few exceptions of high-quality studies. Synthesis involved grouping identified interventions based on their distinguishing characteristics, and positioned within a continuum of low to high involvement: i) environmental unit changes (n = 2), ii) web-based support (n = 4), iii) discussion-based support (n = 6), iv) multicomponent support (n = 4), v) participation in rounds (n = 3), and vi) participation in physical care (n = 1). Six main outcomes were identified from the studies analysed for the review, grouped under two categories: i) Involvement outcomes: Communication, Decision making, Satisfaction; and ii) Health outcomes: Family Trauma, Family Wellbeing, Patient outcomes. The findings from the qualitative studies were thematically analysed to identify features of the interventions that participants perceived to influence success: accessibility, simplicity, supplementarity, contextualisation, interprofessionality, consistency, relationship, and confidence development. We developed a typology outlining types of family member involvement interventions alongside their key features, expected outcomes and evidence level.
Conclusions: Future interventions should be developed with much closer family member input and designed by taking into account the key success features identified. We call for interventions to be multi-layered, allowing for a greater or lesser level, and different kind, of involvement for family members, the decision of which should be informed by a baseline diagnostic of family members’ needs, readiness and preparedness for involvement.
0216
Take me out: I can be shocking! A Quality Improvement (QI) project to review and improve the practice of checking for retained tampons in women of reproductive age admitted to the Intensive Care Unit
Lucinda Whitton and Hannah Hall
Intensive Care Unit, Royal United Hospital Bath, Bath, United Kingdom
Abstract
Background: Toxic Shock Syndrome (TSS) first made headlines in the 1980s due to its high morbidity and mortality in previously healthy young females.1 The advent of ultra-absorbent tampons saw this incidence peak, triggering an urgent need for physicians to consider this important differential in shocked female patients.2 Women admitted to Intensive Care Units in hospital may represent a particularly vulnerable patient population, due to difficulty obtaining an accurate menstrual history and high rates of immunocompromise.3 A literature review conducted through PubMed using search terms: (“ICU” OR “Intensive treatment unit” OR “ITU”) AND (“TSS” OR “Toxic shock syndrome”) yielded 25 papers citing case reports of TSS in ICU; many papers reflected on delays in diagnosing TSS and recognising retained tampons.
Junior doctors working in the Intensive Care Unit at the Royal United Hospital in Bath suspected that the opportunity to screen for and remove retained tampons, either in the Emergency Department or upon admission to the Intensive Care Unit, would be concordantly low, leaving patients at risk of potentially fatal Toxic Shock Syndrome. A QI project was therefore designed to improve documentation of tampon presence and removal on admission to either ED or ICU, to decrease the potential risk of TSS.
Methods: The notes from twenty admissions of female patients aged below 60 to the ICU at the Royal United Hospital in Bath over a six-month period were analysed to determine the proportion of patients who received a documented tampon check, and, where appropriate, removal.
Following this, several interventions were implemented. “International Tampon Alert Day,” was celebrated in the department and saw “shocking” toxic shock themed cupcakes brought into the ICU coffee room alongside the display of educational posters regarding the risks of TSS. The local ICU admission checklist was also amended to prompt a tampon check, alongside the well-established urinary catheterisation check.
After implementation of such interventions, the notes of ten subsequent admissions to the unit were analysed.
A second round of the quality improvement project involved educational intervention through departmental teaching and further educational posters. After this intervention, ten further subsequent admissions will be analysed.
Results: Of the twenty notes reviewed of women presenting to ITU from August 2018 to February 2019, no notes documented a tampon check, removal or discussion with the patient. Outstanding results following our interventions will be presented and discussed.
Conclusion: The initial results of this project highlight a clear deficit at a local level in the screening process for retained tampons; posing a potential risk of TSS. We hope to see improvement in practice following our two-cycle QI project and hope to raise awareness to other ICUs of the dangers of the forgotten, retained tampon.
0218
Rectus sheath catheter infusions: two cases of local anaesthetic toxicity following hemihepatectomies
Robert Crichton and Thomas Faulkner
University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Background: Opiate sparing analgesia post midline laparotomies has previously been focused upon neuroaxial techniques. Rectus sheath catheters (RSCs) may provide a non-inferior level of analgesia with reduced complications and are therefore becoming increasingly popular.1,2
As the use of RSCs becomes more commonplace, there is a growing need for consensus on the accepted dosage. Currently there is a lack of data describing plasma drug levels during infusions.3,4
The following case presentations highlight two cases of local anaesthetic systemic toxicity (LAST) following bupivacaine RSC infusions post right hemihepatectomies. No similar cases have been published.
Case presentation 1: A 72-year-old, 69 kg male was admitted to the Intensive Care Unit (ICU) following a right hemihepatectomy for liver metastases from a colorectal primary. He lived independently, drank minimal alcohol and had a good exercise tolerance.
Bilateral 0.25% bupivacaine 5 ml/hour RSCs were placed intra-operatively. The patient was delirious over the first 48 hours. On day 2 the patient had two 1 minute tonic-clonic seizures. Over the next 48 hours; 2 EEGs, a plain CT head, a CT head venogram, an MRI head and an LP were all normal.
After extensive negative investigations, a diagnosis of LAST was concluded. The RSC infusions were stopped and there was no further evidence of toxicity.
Case presentation 2: A 75-year-old, 58 kg female was admitted to the ICU following a right hemihepatectomy for liver metastases from a colorectal primary. She was fit and well with a diagnosis of atrial fibrillation, lived independently, rarely drank alcohol and had a good exercise tolerance.
Bilateral 0.25% bupivacaine 5 ml/hour RSCs were placed intra-operatively. The patient was delirious over the first 48 hours. On day 2 the patient had a 30 second tonic-clonic seizure. This was suspected to be LAST. The rectus sheath catheters were stopped and Intralipid® was administered. A CT performed later that day was normal.
The patient improved with no further signs of toxicity.
Conclusions: Bupivacaine testing from urine and plasma revealed its presence in both patients; quantitate assays are not currently available within the NHS. There is little published data regarding the expected plasma concentrations of local anaesthetics during peripheral infusions. Two studies of transverse abdominal plane infusions found several cases exceeding toxic plasma levels with varying degrees of symptoms.3,4
The above two cases occurred following right hemihepatectomies, and therefore a link with acute hepatic dysfunction should be considered. A potential reduction in bupivacaine metabolism via CYP450 and/or a reduction in alpha-1-glycoprotein production could result in higher concentrations of free drug.4
The incidence of LAST following peripheral administration is rare at approximately 8.7/10,000.5 These cases occurred in one ICU within two months, representing a striking need for further study and consensus guidelines on dosing RSCs. A guideline based on the current literature and experience for University Hospitals Birmingham has been developed in order to standardise practice.
0220
SRAVI (Speech Recognition App for the Voice Impaired) – A feasibility study into the use of Visual Speech Recognition software to aid communication in the ICU environment
William Flesher, Jacqueline Twamley, Mark Verlander, Shravan Nanda, Sushruth Madanapalli Raghunath, Alexandra Williams and Shondipon Laha
Lancashire Teaching Hospitals NHSFT, Preston, Lancashire, United Kingdom
Abstract
Introduction: Acute barriers to vocal communication by patients are common in the ICU and are multifactorial in origin, predominantly affecting patients with airway adjuncts.1 They impair effective communication of basic needs and consent, and contribute towards frustration and anxiety amongst patients and caregivers.2,3
SRAVI (Speech Recognition for the Voice Impaired) is a smartphone app developed by Liopa which uses Visual Speech Recognition software to read the lips of individuals and present a best fit.4 It has been identified that this may be useful for patients with acute communication impairment in the ICU.
Objectives: To understand the communication needs of patients, care providers and relatives in ICU, to train SRAVI with natural language based on the above needs and ultimately to assess the app’s efficacy.
To survey attitudes towards SRAVI amongst staff and patients.
Methods: As part of a funded study from Innovate UK, with the University of Belfast, patients with a tracheostomy in the ICU in Royal Preston Hospital, alongside their families and care providers, were given a questionnaire asking “What top five questions would you like/would your relative/patient like to be able to say?” The top 20 phrases were chosen and were sent to Liopa to be built into SRAVI.
All patients with tracheostomies capable of mouthing words were then recruited. Staff members were recruited in a separate database. Staff and patients were asked to repeat the 20 phrases, and video of this was captured and sent back to Liopa via the cloud.
Staff and patients were asked their opinions on SRAVI after experiencing it.
Results: 33 staff members and 10 patients have been recruited so far. All participants were able to utilise the app adequately, and all reviewed SRAVI positively.
Conclusions: This is an ongoing study and we intend to recruit more participants and expand the vocabulary of the app so that a wider variety of speech can be understood.
The findings so far are encouraging for the use of SRAVI in ICU. All participants were generally supportive with one recently decannulated patient noting that “this would have helped me so much to say what I wanted to say”.
0221
Ready, Steady, Go! Testing the evacuation process in an ECMO centre using high-fidelity in situ simulation
Rosie Cervera-Jackson, Jolana Sykorova, Stephane Ledot, Rosie Smith, Catherine Philpott and John Calvert
Royal Brompton Hospital, London, United Kingdom
Abstract
Introduction: Hospital care providers are required to risk assess, plan, train and test emergency preparedness, resilience and response (EPRR). In a highly specialised adult Extracorporeal Membrane Oxygenation (ECMO) centre, a risk was identified that Very Dependent Patients receiving life-sustaining therapies would take at least 30 minutes to evacuate in an emergency like a hospital fire. To the authors’ knowledge, evacuation of an ECMO patient had never been simulated before in the United Kingdom (UK).
Objectives: To test the timing and process for rapid evacuation of a patient on ECMO to a place of safety during a hospital fire, using existing generic guidance; To determine the minimum number of personnel required; To create specific guidance on triage and evacuation of Very Dependent Patients.
Methods: The simulation faculty from the adult intensive care unit (ICU), along with the hospital fire officer and emergency preparedness officer, led live simulation exercises to time and test evacuation processes and develop a specific evacuation procedure and triage guidance for Very Dependent Patients.
The first exercise was a high fidelity in-situ simulation, using the Simulated Interprofessional Team Training (SPRinT) programme methodology. A fire was simulated above a room in ICU containing a mannequin connected to a monitor, ventilator, continuous infusions and ECMO. Participants were required to respond by activating the fire alarm and conducting a horizontal evacuation, followed by a vertical evacuation of the “patient”. Both participant and faculty groups were multi-professional and included medical, nursing, perfusion and non-clinical staff.
Timing and processes observed during the test were used to create a Standard Operating Procedure (SOP) for rapid evacuation of Very Dependent Patients.
This was tested in a second exercise which involved practising evacuating the mannequin from a room in ICU to the next fire compartment, while connected to different therapies including ECMO, Intra-Aortic Balloon Pump, Nitric Oxide and Haemofilter.
Analysis of the exercise was used to refine the SOP and develop specific triage guidance for managing Very Dependent Patients during an emergency.
Results: The first exercise, conducted using generic training and guidance, took 5 minutes 30 seconds and required five personnel to move the “patient” to a place of safety (the next fire compartment). It was observed that participants followed the process for a planned clinical transfer. An SOP was created for evacuation of a Very Dependent Patient which streamlined the process for rapid and safe evacuation.
The second exercise, conducted using the new SOP, took 2 minutes 33 seconds and required three personnel to move the same “patient” to the next fire compartment.
The exercises revealed latent safety threats including training needs for evacuation as a separate process from planned clinical transfer, operating lifts in fire evacuation mode and availability of transfer equipment at the bedside.
Conclusions: Multi-professional high-fidelity in situ simulation exercises can reveal the potential capabilities of and challenges to hospital teams during fire evacuation. The method is suitable for risk assessment, planning, refining and testing EPRR in a hospital and for supporting the development of specific EPRR guidance for Very Dependent Patients.
0223
Improving the efficiency and documentation of lumbar punctures in critical care
Rachael Meredith, David Haydock and Jessica Casey
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Introduction: CSF sampling via lumbar puncture is a common procedure in critical care units. In our centre, we identified a lack of standardisation in lumbar puncture performed by trainees, leading to inefficiency and poor documentation compared to other similarly invasive procedures on the unit.
Objectives:
1. Reduce time taken to carry out lumbar punctures on the unit and standardise equipment in line with current best practice
2. Improve procedural documentation for clinical and medico-legal purposes
Methods: A prospective audit of lumbar puncture documentation was carried out over 30 days. 11 lumbar punctures were performed on the unit in this time period. Documentation was audited for compliance against standards identified through NatSSIP guidance (1), AAGBI guidelines (2), literature review (3,4) and existing trust protocol.
Contemporaneously, seven trainees performed self-timed kit collection to identify the average time taken to prepare for lumbar puncture on the unit.
After initial audit, a lumbar puncture pack was introduced containing a newly developed LocSSIP. Following this we carried out a re-audit of documentation and feedback survey of colleagues who had used the pack to quantify improvement.
Results: Pre-intervention audit demonstrated 55% compliance in documentation against pre-defined standards (target 100%). Re-audit of 12 lumbar punctures performed post-intervention revealed documentation compliance of 94.3%. Documentation of pre-procedure safety checks (contraindication and coagulopathy screens) showed particular improvement from 30% compliance pre-intervention to 86% post-intervention.
The mean time taken to gather lumbar puncture equipment during self-timed kit collection was 32 minutes (range 15–120 mins), with some colleagues leaving the unit to find equipment. Post-intervention, the mean time taken to collect a pack from the equipment cupboard was 4 minutes.
A post-intervention survey completed by 9 trainees was overwhelmingly positive, with 100% of respondents stating that they felt the lumbar puncture pack was an improvement over previous practice, and that they found the LocSSIP clear and easy to use.
Conclusions: The introduction of a lumbar puncture pack and LocSSIP on our unit demonstrated significant improvements in efficiency and documentation of lumbar puncture. This brought practice in line with other invasive procedures including insertion of central lines and chest drains and was universally supported by trainees.
Following the success of these interventions, we are designing a pre-prepared LP pack to be put together by a manufacturer to our specification. We hope this will be adopted trust-wide, standardising lumbar puncture in other departments in addition to the critical care unit.
0224
Treatment escalation planning in acutely unwell patients – are we missing opportunities?
Kerrie Aldridge, Nick Sherwood and Jonathan Hulme
Sandwell and West Birmingham NHS Trust, Birmingham, United Kingdom
Abstract
Introduction: Collaborative planning regarding treatment escalation plans (TEPs) and cardiopulmonary resuscitation (CPR) is a cornerstone of good clinical care, particularly in patients with significant comorbidity. High mortality rates seen in frail patients in the year after an acute admission1 underscore the importance of these considerations to avoid provision of ineffective and medically inappropriate interventions to those who are unlikely to benefit. Locally, there were perceptions that opportunities to plan for deterioration were being missed. This project aimed to assess the reality of this perception.
Objectives:
• Assess the proportion of acute admissions with documented consideration of TEPs or CPR status.
• Identify patients at high risk of deterioration who did / did not have TEPs discussed during their hospital admission.
• Identify how many patients required emergency decision making.
Methods: All acute admissions (excluding obstetrics) over three 24-hour periods in March 2019 were identified, and notes retrospectively reviewed. Data were collected on demographics, admission diagnoses, comorbidities, functional capacity and whether TEPs were documented. Functional status was quantified using a locally developed 5 point scale, and patients at subjectively high risk of deterioration were identified by considering the commonly proposed question ‘Would you be surprised if this patient died in in the next 12 months?’. Data were analysed using Microsoft Excel and GraphPad.
Results: 233 medical patients (MPs) and 49 surgical patients (SPs) were admitted over the study period. 42/184 (22.8%) MPs had significant functional impairment: 16/184 (8.7%) bedbound or fully dependent; rates were lower in SPs – 3/49 (6.1%). TEPs were considered for 47/284 (16.7%) admissions: 0 SPs and 47 (20.1%) MPs. In those with no TEP, death within 12 months would not be a surprise in 65/184 (35.3%) MPs and 7/49 (14.3%) SPs. Of patients with a TEP, 22/47 (46.8%) were for CPR but none of these patients had documented discussions regarding their wishes. 34/47 (72.3%) TEPs were completed at first senior review. 82/116 (70.6%) patients with a hospital stay >24 hours had no TEP, but were significantly more likely to be expected to die within 12 months compared to those who stayed <24 hours (36/82 versus 36/115, P = 0.002). 4 patients had no TEP in place at the time of rapid deterioration/cardiac arrest, resulting in decision-making in an emergency situation.
Conclusion: Despite local and national guidelines emphasising the importance of TEPs, the majority of patients admitted to hospital acutely are not having TEP discussions. This promotes situations leading to the requirement for emergency decision-making, where it may no longer be possible to involve the patient. Barriers to TEP discussions can include lack of clinician time, concern that discussion may distress patients or lead to complaints, and lack of clinician confidence.2 Locally, we plan to improve the quality and quantity of TEP discussions by exploring the influence of some of these common barriers, highlighting the harms of missing opportunities for TEP discussions, and using the new electronic patient record to allow easier ongoing audit of TEPs.
0225
The use of cross professional healthcare assistants to support the rehabilitation of critical care patients
sarah dyson
Royal Liverpool and Broadgreen University Hospitals NHS Trust, Liverpool, United Kingdom
Abstract
To work at its best rehabilitation of critically ill patients needs to occur 24 hours per day, 7 days a week or does it ??
Few units are lucky enough to have the MDT staff to support this and offer a true around the clock service,or at least a service that operates outside of normal office hours, despite standards and recommendations from NICE CG 83 and GPICS V2.
Locally our rehab service was only Monday to Friday, meaning that patients missed out on vital, therapy and rehab opportunities at the weekend. Rehab has always been seen as a team effort but nursing and therapy establishment meant that out of office hours not a great deal occurred.
In September 2018 the therapy teams and critical care management team came up with a proposal to release a member of the nursing HCA staff to work with and support the therapy teams in providing rehab to our critically ill patient population.
This role included taking on duties that are seen as part of physiotherapy, occupational therapy, speech and language therapy and dietetic roles.
To facilitate this a set of multi professional competencies were developed, which supported the staff member carrying out the role. The HCA staff member was able to facilitate therapy and rehab input during extended hours and at weekends, feeding back to the rest of the rehab team on the progress of patients. We were able to monitor this progress and the effectiveness of the new service by recording mobility levels for all the patients using the Johns Hopkins Highest Level of Mobility score (JH HLM) and personal care scores, as well as mid upper arm circumference measurements (MUAC) and SALT recommendations.
There has been very positive feedback and results from this innovative new service and staff report that the rehab services now feel more cohesive and that the new HCA role has bridged the gap between therapy and nursing staff. We have been able to collate some of the data collected and show improvements in mobility and personal care scores for patients on discharge form critical care when compared to admission scores.
This popular role is now offered on a 6 monthly rotational basis to all HCA staff on the critical care unit and is due to be rolled out to high dependency areas in the near future.
0226
Assessment of Patient Alertness and Sedation on the Cardiac Intensive Care Unit
Haleema Siddique1,2 and Krishna Pasupuleti1
1University Hospital North Midlands, Stoke-on-Trent, United Kingdom
2Keele University School of Medicine, Stoke-on-Trent, United Kingdom
Abstract
Introduction: Sedation is a fundamental element to the treatment of the critically ill patient. It is used to facilitate intensive care (ICU) therapies and to ease the patient through a distressing environment. Maintaining light levels of sedation in stable adult ICU patients is associated with improved clinical outcomes by allowing for a shorter duration of mechanical ventilation and length of stay in the ICU.1 Care must be taken to ensure that optimal amounts are given, thus avoiding the side effects of over-sedation.2 ‘Sedation breaks’ have been encouraged,3 a sedation scoring system will help to facilitate this. The Richmond Agitation-Sedation Scale (RASS) is an example of a scoring system that can be used. The AVPU scale, Critical-Care Pain Observation Tool (CPOT), and Glasgow Coma Scale (GCS) are also tools that are commonly used by the nursing staff for measuring patient alertness. The patient data management systems (PDMS) have facilitated easier access to entering these scores onto hospital databases. The choice of sedation scale is probably less important than a unit familiarising itself with a single validated sedation scale by using it regularly and auditing its use.
Objectives: Evaluation of the awareness and use of appropriate scoring systems within ICU to ascertain appropriate levels of sedation for patients post-operatively, and its impact on recovery rates and any complications it may pose.
Methods: Within the discussed ICU there are 2 pods, 16 beds, 80 nurses and 2 nursing educators. Information was obtained via customised questionnaires from nursing staff within the cardiac ICU. Results were categorised by thematic analysis.
Results: 45 nurses participated in the study. 89% were aware of scoring systems being used as a measure of patient alertness. 33% used RASS as their initial scoring of patient alertness. 78% of the nursing staff were aware of RASS in general. 7% were more familiar with the GCS and 2% the CPOT. 13% were unable to comment on how they would measure patient alertness. 42% of the nursing staff had stated that they had previous training in using these scoring systems. Of the aforementioned, 40% felt confident with the training that they had. On actively asking the members of staff to use the scoring system, 40% answered correctly with 93% using RASS. When assessing their own patients at the bedside, 82% accurately assessed their patients. 9% thought it was more appropriate to use GCS. 4% were unable to comment and 5% of the nursing staffs scores were in discrepancy with the RASS scoring equivalent of the patient’s status at the time.
Conclusion: Overall, it was found that there is an awareness of scoring systems for sedation. There is a PDMS online source to enter patients RASS score. The problem arises with the level of awareness and ability to submit the data successfully. Further nursing education would be highly beneficial such as with face-to-face nurse training and the creation of user-friendly online training modules. Re-auditing would be valuable to establish further improvement with these modifications.
0227
Should Low Serum Bicarbonate be used in Addition to Standard Early Warning Score and AKI Alerts to Idenitfy Patients at Risk of Deterioration?
James Lennard
Northumbria Healthcare NHS Foundation Trust, Cramlington, United Kingdom
Abstract
Introduction: A recent project within our trust identified that patients with low serum bicarbonate during their hospital stay have a 30-day mortality of up to 40%. (Our laboratory reports serum bicarbonate as part of the standard urea and electrolyte results.)
This built upon previous work that showed that up to 40% of patients with a stage 2 AKI or worse do not trigger a senior review based on standard NEWS parameters (total score ≥ 5 or score ≥ 3 in any one domain). This led to patients with AKI alerts of stage 2 or higher being reviewed by critical care outreach and the development of an AKI pathway and AKI steering group.
Background/Objective: The aim of this current piece of work is to identify whether there is a need to incorporate low serum bicarbonate into current methods of identifying patients at risk of deteriorating such as NEWS and AKI alerts.
Methods: After Caldicott approval was granted, data for all patients presenting to Northumbria Specialist Emergency Care Hospital in January and February 2019 with low serum bicarbonate (<18) was gathered from the biochemistry lab. This data also included whether the patient had a stage 2 or greater AKI. The electronic observation recording system was then interrogated to see if the patient triggered for review around the time the blood sample was taken. Only the first reading below 18 was analysed for each patient. Patients with DKA were excluded, as were children (<16), maternity patients and patients form wards that did not use the electronic observation system.
Results: 370 individual patients were identified over the two months with a median age of 73. Overall 30-day mortality was 29.5%. The patients were then split into three groups depending on the bicarbonate result for further analysis (≤10, 11–15, 16–17). Results are shown in the table below:
The records of those patients who died within 30 days without any AKI or NEWS trigger were then analysed in more detail to see if there were any trends or learning points. There was no evidence that any of the deaths were av
Conclusions: These results support previous work that suggests that low serum bicarbonate is associated with significant mortality even where the fall in bicarbonate is relatively small. Nearly half of all patients with low serum bicarbonate do not trigger on our current scoring systems (NEWS/AKI). Outreach review of all the patients who do not trigger would overwhelm outreach services and is not justified based on these results. Introduction of a low bicarbonate alert on the results reporting system may help to draw attention to these patients.
Table 1.
| Serum Bicarbonate | ≤10 | 11–15 | 16–17 |
|---|---|---|---|
| Number of Patients | 18 | 133 | 219 |
| 30 day mortality (%) | 5 (28) | 54 (41) | 49 (22) |
| AKI ≥ Stage 2 (%) | 10 (56) | 39 (29) | 35 (16) |
| NEWS Trigger (%) | 15 (84) | 59 (44) | 70 (32) |
| No AKI/NEWS Trigger (%) | 1 (5) | 55 (41) | 127 (58) |
| Died in 30 days and no AKI/NEWS Trigger (%) | 0 (0) | 14 (11) | 17 (8) |
0229
Airway clearance techniques and use of mucoactive agents for adult critically ill patients with acute respiratory failure: A qualitative study exploring UK physiotherapy practice
Bronwen Connolly1, Matthew Barclay2, Bronagh Blackwood1, Judy Bradley1, Rohan Anand1, Mark Borthwick3, Marc Chikhani4, Paul Dark5, Murali Shyamsundar1, John Warburton6, Daniel McAuley1 and Brenda O'Neill7
1Queen's University Belfast, Belfast, United Kingdom
2Guy's and St. Thomas' NHS Foundation Trust, London, United Kingdom
3Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
4University of Nottingham, Nottingham, United Kingdom
5University of Manchester, Manchester, United Kingdom
6University Hospitals Bristol NHS Foundation Trust, Bristol, United Kingdom
7Ulster University, Belfast, United Kingdom
Abstract
Introduction: Mechanical ventilation, the cornerstone of management of critically ill patients with acute respiratory failure (ARF), is associated with the risk of secretion retention secondary to altered secretion rheology and impaired mucociliary clearance. Respiratory physiotherapy incorporates airway clearance techniques (ACT) to facilitate secretion clearance, and may be supplemented by use of mucoactive agents. However whilst international data are available to characterise respiratory physiotherapy in this patient population, data describing UK practice are limited despite this forming part of national guidelines on patient management. The use of mucoactive agents in clinical practice is common even with limited evidence for effectiveness; a recent UK survey of ICU-level practice demonstrated the majority of adult ICUs used this pharmacotherapy but with wide prescribing variability. However survey data may lack granularity, and a more in-depth exploration using qualitative methodology could define current respiratory physiotherapy practice in this area.
Objectives: To explore and describe current UK physiotherapy practice relating to ACT and mucoactive agents in critically ill adult patients with ARF in the intensive care unit (ICU).
Method: A descriptive, qualitative study using focus group interviews with senior physiotherapists (minimum 2 years’ clinical experience), clinically active in critical care, and performing ACT in the ICU. This study was approved by King’s College London Research Ethics Committee (MRA-18/19-8906). Focus groups were digitally audio-recorded and independently transcribed with additional cross-checking from the research team. Anonymised data were analysed by two independent members of the research team using thematic analysis, with themes identified at a semantic (manifest) level.
Results: Fifteen physiotherapists, with experience ranging from 3–27years and working across diverse ICU specialties, participated. Five themes relating to ACT were identified; ‘Repertoire of airway clearance techniques’, ‘Staffing and skillset’, ‘Commencing airway clearance techniques’, ‘Technique selection’, and ‘Determining effectiveness’. A further five themes emerged relating to use of mucoactive agents; ‘Use in clinical practice’, ‘Decision to commence’, ‘Selection of agent’, ‘Stopping mucoactive agents’, and ‘Determining effectiveness’. From the collective content across all themes, key features of standard practice for ACT were summarised and included the following:
• Patient-centred approach
• Individualised assessment to determine clinical need
• Tailored treatment to specific patient presentation using a range of available techniques
• Evaluation of airway clearance technique effectiveness based on changes in subjective (e.g. more effective cough, increased ease of secretion clearance, patient tolerance of treatment etc) and/or objective (e.g. improved oxygen saturation levels, reduced oxygen requirements, cardiovascular stability etc) outcome measures
• Mucoactive agents typically commenced to assist with management of “thick” secretions
Conclusion: Current UK clinical physiotherapy practice of ACT is patient-centred, and targeted to individual need, with adjunctive use of mucoactive agents to enhance and optimise patient management if required. Based on this study, we have captured a summary description of standard care, which could be used in future trials involving ACT as part of usual care.
0232
Rationalising the use of Sugammadex: a quality improvement project
Dr Christopher Dixon, Dr Peter Hutchings, Dr Laura Dixon
CHFT, Huddersfield and Calderdale, United Kingdom
Abstract
Background: Sugammadex is a specific cyclodextrin reversal agent for the aminosteroid neuromuscular blocking drug Rocuronium. Sugammadex can provide rapid reversal of neuromuscular blockade in airway emergencies and prevent post-operative residual curarization;1 particularly in patients at high risk of pulmonary complications. It has potential to reduce unplanned admissions to the Intensive Care Department (ICU). The drug is expensive; our trust spent £75,000 over a year when access was unrestricted and predominantly paper based documentation in our trust made it difficult to trace drug use. Our aim was to establish traceable use of Sugammadex and achieve a safe reduction in expenditure.
Methods: We followed a plan, do, study, act methodology. Sugammadex was placed in the controlled drug (CD) cupboards and difficult airway trolleys from October 2018 and required ‘sign out’ in the CD book. This enabled traceable usage; we looked at anaesthetic charts retrospectively after upload to our electronic record EDMS system. Information about indication, dosage, surgery type and grade of doctor using the drug were recorded. We looked at usage in theatres in two cycles (October 2018 to February 2019 and April to June 2019). Results were discussed at departmental clinical governance meetings. Posters were used to signpost how to access the drug. Usage in the Intensive Care Department were explored by a departmental online survey (cycle 3, July 2019), which also aimed to achieve consensus as to when use of the drug was justified.
Results: Trust expenditure on Sugammadex fell by £15,000 over nine months. Forty-four patients received Sugammadex in cycle 1 and thirty-nine in cycle 2. There were no recorded uses of the drug from the difficult airway trolley. Usage was predominantly by consultants. Documentation improved; there was an indication for use on 39% of anaesthetic charts in cycle 1 and 64% in cycle 2. Drug dosage was recorded on 70% of charts in cycle 1 and 95% of charts in cycle 2 and there was increased documented use of train of four monitoring. The commonest indications for use were residual neuromuscular weakness post neostigmine and anticipated pulmonary complications in obesity. There were no documented difficulties in obtaining the drug. Our survey received thirty-three responses which highlighted use of the drug in bariatric surgery and anticipated difficult airways and routine use on the ICU as reversal for rocuronium infusions prior to extubation.
Conclusions: Our trust comprises two district general hospitals (eighteen theatres, two ICUs) and £75,000 was an unsustainable expenditure which was greater than the local teaching hospitals combined spend. Our interventions led to a significant cost saving and an ability to audit practice. Documentation improved due to staff education. We were unable to demonstrate any adverse consequences to patient safety. A change in culture has meant use of the drug has now become a cost versus benefit decision.
0233
Introducing routine opt-out HIV testing at ICU admission in a district general hospital
Nicola Lungu1,2 and Richard Fisher2
1Princess Royal University Hospital, Orpington, United Kingdom
2King's College Hospital NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: People living with HIV in the UK starting treatment early have normal life expectancy, and with viral suppression it is impossible to transmit to others.1
HIV testing happens routinely in sexual health clinics and maternity services. To reach people outside these services, 2016 NICE Guidelines recommend testing all patients admitted to hospital where local HIV prevalence >2/10002, which is cost-effective3,4. Where this is appropriate but not yet performed, the Intensive Care Unit (ICU) can introduce routine HIV testing. The primary goal of HIV testing at ICU admission is to identify and treat causes of illness; however, there are wider benefits including increasing staff awareness, and creating a local model of routine testing which could be exported to the hospital admission process.
Opt-out HIV testing was introduced at a London ICU in 2012; all patients were tested using a best interests principle in the context of local HIV prevalence.5
Objective: We aimed to introduce routine HIV testing at ICU admission in our outer-London district general hospital (DGH) where local HIV prevalence 2.8/1000.
Only 3.3% new HIV diagnoses in UK are in people over 65 years so in our setting routinely testing patients 18–65 years is most effective. Our laboratory test cost £3.87, and combining HIV testing with other admission blood tests avoids additional phlebotomy time, equipment or test transportation.
Methods: We retrospectively reviewed six months ICU electronic patient records (EPR) to understand how many patients aged 18–65 years had been tested, and by whom.
A 3rd generation HIV test was added to EPR ICU admission order set and an information board made available for staff. Patients unable to consent are tested using the principle of best interests. Patients who can consent are advised HIV testing is part of normal admission blood tests and they may opt-out.
Routine HIV testing was introduced over one month and no data gathered in this time. EPR was reviewed for the subsequent two months, and ICU staff were asked to provide anonymous qualitative feedback.
Results: Our ICU admits on average 24 patients aged 18–65 years each month. Prior to routine HIV testing 12% eligible patients were tested; all tests initiated by a doctor for clinical reasons after the first day of admission. After introducing opt-out testing 76% eligible patients were tested, most on their first day, with 60% tests initiated by nurses.
Staff feedback is largely positive, appreciating an opportunity to diagnose a treatable condition. Some feel testing patients provides protection for staff. Several are concerned about the loss of traditional verbal consent for a disease which remains stigmatised, and concerns about cost-effectiveness were raised.
Conclusions: Routine HIV testing at admission to ICU in a DGH is feasible and ensures most eligible patients are screened. Staff awareness has increased and most find opt-out testing acceptable. It is valuable to discuss consent relating to all investigations and care provided in best interests.
When HIV testing becomes a normal part of healthcare where prevalence >2/1000, more people currently undiagnosed will receive treatment and live healthy lives without further HIV transmission.
0234
Learning Critical Care Simulation
Edit Chase, Stephen Hutchinson, Suhas Kumar and Jemma Looker
Norfolk and Norwich University Hopsital, Norwich, United Kingdom
Abstract
Introduction: Simulation in healthcare is a well-recognised phenomenon; the value and benefits is widely published in the literature.
A number of barriers to delivering a simulation program are well recognised (1). Simulation may feel unrealistic, staff may feel anxious and concerned about assessment rather than learning. Participants do not value acting outside their normal professional role and are reluctant to engage if workload is high, and they do not value the simulation learning.
Modifying the simulation program may help with overcoming some of these barriers and result in better engagement, improved process learning, organizational learning, patient safety and perhaps staff wellbeing. Last year we presented the effect of in-situ simulation on organisational learning (2). Whilst benefits were realised, these were small, and we speculated about the dose-response relationship being responsible.
Objectives: We set about to establish and evaluate staff perceptions of our critical care simulation program. Multi-professional in-situ simulation was delivered alongside a planned, time protected, nurse-only simulation program. Specific attention during briefing was dedicated to ensuring the safety of the learning environment and debriefing was deliberately open-minded and positive. Clinical governance and critical incidents were fed into simulation scenarios whilst learning from simulation then fed back into the governance processes.
Methods: We conducted 24 simulation training sessions for a total of 163 participants. All participants provided anonymous feedback.
Results:
• 90%‘agreed’ or ‘strongly agreed’ that the scenario felt real
• 94%‘agreed’ or ‘strongly agreed’ that, as a consequence of this training, they would feel more confident in similar situations
• 99%‘agreed’ or ‘strongly agreed’ that this training should be routine in our ICU
• 99%‘agreed’ or ‘strongly agreed’ that they would recommend this training to others
• 99%felt the content, pitch, and relevance to practice were ‘good’ or ‘excellent’.
The word cloud (larger the words, the more often they featured) of combined subjective comments provided this qualitative feedback, demonstrating their learning in a safer environment.
Conclusion: By understanding the barriers to the introduction of a simulation training program and modification of the program to address these barriers, it is possible to deliver effective training.
The training has been well received and appears to be a sustainable strategy to improve patient safety in our critical care unit. Careful briefing makes simulation seem more realistic and less threatening. Debriefing makes clear the integration of simulation with learning from critical incidents and clinical governance. Feedback has illustrated that we have been able, through simulation, to deliver process-specific learning objectives (3). This provides a concrete learning process for local organisational learning.
Beyond the clear safety benefits, we contend that there is also significant benefit on workplace wellbeing. Burnout in critical care is prevalent. Coaching strategies to understand and manage human factors such as cognitive overload and performance anxiety will reduce workplace stress in critical care. The opportunity to contribute to patient safety in a clear and visible way through the safe learning environment of a simulation debrief is also a powerful tool for engagement.
0235
Reducing Rates of Microbiology Specimen Rejection in Critical Care Services
Jennifer Hancox, Helena Wells and Santhana Kannan
Sandwell and West Birmingham NHS Hospitals., Birmingham, United Kingdom
Abstract
Introduction: Rejection of critical care specimens by laboratory has significant adverse consequences including need for re-tests, treatment delays and suboptimal use of resources.1,2 Large scale studies show that rejection rates should be ≤3%1,2,3.
Objective: This Quality Improvement Project looked at assessing the rejection rates of microbiological samples from critical care services at Sandwell and West Birmingham Hospitals NHS Trust and to implement changes to reduce the same.
Methods: Baseline data (Cycle 1) entailed retrospective review of all samples for microbiological testing sent from critical care over a two-week period in Jan 2019. Data collected included specimen rejection rate, nature of test rejected and reason (s) for rejection such as container and documentation errors. A Plan-Do-Study-Act cycle methodology was used. Focussed interventions were introduced to reduce rates of rejection. Individual email and posters campaign showing the correct containers was undertaken. Data collection over a two-week period was then repeated in March 2019 (Cycle 2). Based on the results, a sticker intervention was introduced where a ‘culture’ sticker in bright colour was applied on the containers to serve as a visual cue for staff. Data collection on sample rejections was repeated in May 2019 (Cycle 3) to assess its impact.
Results: The total number of microbiology urine samples sent in each cycle ranged from 267 to 342. Baseline data demonstrated an overall rejection rate of 5.3%. The majority of these were rejected urine samples (3.2%). The number of rejected urine samples alone equated to 1200 per annum with an estimated 100 hours of wasted nursing time spent on sample collection in addition to cost of consumables. Most urine samples were rejected due to use of incorrect container and we targeted our interventions to address this. Cycle 2 data after email and poster campaign did not show a significant reduction in rejection rates. After introduction of ‘stickers’ on containers, the overall sample rejection rate reduced to 3%, with rates of rejected urine samples reducing to 1.2% on Cycle 3 audit.
Conclusions: Baseline audit showed higher than average rates of sample rejection in our critical care unit. Overall rejection rates improved following interventions. Posters and email communications were less effective. Introduction of a bright coloured ‘culture’ sticker on the containers as a visual cue was highly effective at reducing urine culture rejection rate and provided a low-cost solution.
0237
Daily Dashboard produces sustained improvement in Critical Incident/Learning Event reporting rate for Morbidity and Mortality Review Processes
Hugh Gifford1,2 and Pauline Austin1,2
1NHS Tayside, Dundee, United Kingdom
2University of Dundee, Dundee, United Kingdom
Abstract
Background/Objectives: Critical incidents/learning events are common in critical care; reporting and analysis can assist staff in reducing related morbidity and mortality (M&M) (1). Previous research has shown that the use of structured reporting tools can assist staff learning (2). We aimed to improve the local monthly reporting rate via the use of daily surveillance tools. This took place in parallel with an intensification of M&M review processes to maximize learning.
Methods: We undertook a Quality Improvement Project in an eight bed Level 3 Intensive Care Unit in the East of Scotland over 24 months. Five improvement cycles included: (1) monitoring baseline critical incident reporting (2) introducing a five-question safety brief at the multidisciplinary ward round (e.g. drug and equipment problems) (3) changing the timing of the brief to handover (4) introducing a twelve-item dashboard of defined critical incidents/learning events (e.g. inadvertent hypoglycaemia) with weekly M&M meetings and monthly written dissemination of learning points (5) reducing written dissemination to bimonthly. Data were collected and analysed in Microsoft Excel 2017.
Results: All critical incident/learning event reports were included. Mean staff concordance with the daily safety brief was low at the ward round (22.8%) and handover (30.0%), but very high with the daily dashboard (94.3%, Fig. 1). This was similar after reducing written dissemination from monthly to bimonthly (96.2% before, 91.8% after). The baseline rate of critical incident reporting was initially low (0-1/month, mean 0.2) and did not increase with the use of a safety brief (Fig. 2). The safety brief did record a significant number of incidents (0-13/month, mean 6.9) but did not capture detail. The daily dashboard, however, did increase the rate of detailed formal reporting (8-29/month, mean 15.9), resulting in near total capture (94.1%).
Conclusions: Daily Dashboard use was associated with a dramatic improvement in staff engagement in critical incident reporting compared to safety briefing. The concurrent weekly M&M meetings and written summary reporting will have reinforced and rewarded daily dashboard use. Surveillance, regular review and dissemination forms part of the Ottawa M&M Model (3), recommended by the Scottish Mortality and Morbidity Programme (4). This systematic approach to critical incident/learning event reporting can also be used to monitor future interventions and outcomes.
0238
Interruption to Tube Delivered Enteral Feed While On ICU
Graham Picton, Jessica Zekavica and Michele Bossy
Royal Surrey County Hospital, Guildford, United Kingdom
Abstract
Introduction: Nutrition is an important part of patients care while on ICU. Failure to provide adequate nutrition can impede a patient’s progress and recovery.1 Delivery of enteral feed can be interrupted for a number of reasons in intensive care; these can broadly be categorised as issues with tube for delivery of feed, pre procedure fasting to reduce the risk of aspiration, clinical contraindication with continuing feed or other reasons. Currently our unit lacks standard operating protocols to provide guidance to nurses in order to identify when and for how long eternally delivered feed should be held. We have undertaken to perform a baseline audit of the current practice on the unit with regards to reasons for and duration of breaks in enteral feeding.
Objectives: To perform a retrospective audit of patients admitted to intensive care and during their admission receive an enteral feed regime via a tube-feeding device. During this feeding to audit any documented breaks in the feeding received
Methods: Retrospective analysis of electronic patient records for all patients admitted to the intensive care unit at Royal Surrey County Hospital between 1stApril 2018 and 30th September 2018. Each patient has any enteral feed income documented on an electronic patient records system (ICCA, Philips) this was then analysed for breaks in feed, feeding route, and medical notes were reviewed for the reasons for any breaks in feed. Individual reasons for breaks and duration of breaks where recorded. Speciality of admitting team was also documented to allow subgroup analysis for medical patients admitted to the ICU
Results: 610 patients where admitted to our ICU in the time frame we where analysing. Of these 101 (31 medical) needed enteral feed via a tube feeding device. For these patients there were a total of 119 (59 for medical patients) documented breaks in feeding which where not due to the prescribed regime. Median break duration was 5 hours. Reasons for breaks to feed where classified into airway based interventions 38, clinical 20, procedure 13 (of these 4 (30%) the planned procedure did not take place), transfer for radiology investigation 13, availability of feeding route 15, operation 4, unknown 9, and other 7.
Conclusion: We identified a variety of practice within our unit with regard to breaks in feed, and this is only breaks we have been able to identify retrospectively. By endeavouring to produce a standard operating protocol we will aim to encourage a more uniformed and standardised practice and this we will assess this through re audit following introduction of our protocol.
0241
Unplanned admission to intensive care unit: Incidence and comparison of characteristics and clinical outcomes between conventional referral and medical emergency response system
Narayana Raj kumar SATYAVOLU SUBRAMANYA1, Mohammed Ishaq Ruknuddeen2 and Natalie Soar3
1Senior Registrar, Lyell Mc Ewin Hospital, Adelaide, Australia
2clinical Senior Lecturer, University of Adelaide, Adelaide, Australia
3Research Coordinator, Lyell Mc Ewin Hospital, Adelaide, Australia
Abstract
Background: Unplanned admission to intensive care unit (ICU) is associated with increased mortality and morbidity. Data is sparse on the incidence of unplanned ICU admission and comparison of clinical characteristics between the two pathways of unplanned ICU admissions namely conventional referral and activation of medical emergency team (MET) system.
Objective: To determine the incidence of unplanned ICU admission and compare the characteristics and clinical outcomes of patients having unplanned ICU admissions by conventional ICU referral and activation of MET system.
Methods: We performed a retrospective, observational study at a metropolitan hospital in Australia by analysing the ICU data submitted to the Australian and New Zealand Intensive Care Society adult patient and the hospital MET databases from July 2017 till June 2018. Patients aged3 18 years and having unplanned ICU admissions from hospital wards via activation of MET system and conventional referral were included. Incidence (expressed in 100 person years) was defined as the ratio of number of unplanned ICU admission over the total number of patients admitted to the hospital for that year. The Patients’ characteristics (demographic and clinical), morbidity [ICU and hospital length of stay (LOS, hours), ICU readmissions (frequency %)] and hospital mortality were compared between unplanned ICU admissions due to conventional referral and activation of MET system. Continuous data was reported as median with inter-quartile range (IQR) and compared by Mann-Whitney U test. Categorical data was reported as proportion (percentage) and compared using Chi-square test. The relationship between hospital mortality and the pathway of unplanned ICU admission (conventional referral vs. MET) was tested by binary logistic regression unadjusted and adjusted to a number of covariates [Odds ratio (ORs) with 95% confidence intervals (CIs)].
Results: Out of 1761 patients requiring ICU admission, 1691 (96%) were unplanned. Out of 38628 patients admitted to the adult wards, 682 had unplanned ICU admission (2%). The incidence of unplanned ICU admission was 5 per 100 person years. Out of 2153 MET calls activated, 352 required ICU admission (16%). Out of 453 conventional ICU referrals, 330 (73%) required ICU admission. Unplanned ICU admission was significantly associated with ICU referral compared to MET activation (73% vs.16%, P < 0.001). Compared to MET system, patients with conventional ICU referral had higher admission during business hours (56% vs 44%, P = 0.001), lesser pre-ICU hospital LOS (median hours 23 vs. 49, P < 0.001), APACHE 3 scores (median 50 vs 59, P < 0.001), risk of death (ANZROD median 5% vs 12%, P < 0.001), ICU LOS (median hours 26 vs. 43, P < 0.001), ICU readmissions (26% vs.58%, P < 0.001) and ICU mortality (33% vs.67, P = 0.04). Conventional ICU referral was associated with significantly lower hospital mortality compared to MET system on univariate analysis [OR 0.6(0.4-0.9), P = 0.02] but not multivariate binary logistic regression [OR 0.9 (0.5-1.4), P = 0.66].
Conclusions: Majority of ICU admissions were unplanned. Compared to MET system, conventional ICU referral had lower frequency but significantly higher unplanned ICU admissions. Compared to post-MET ICU admissions, conventional ICU referral may be associated with better clinical outcomes. We need larger, multicentric, randomised trials to validate our findings.
0242
Serum lactate is not useful for detection of ischemic bowel post-angioembolization for lower gastrointestinal bleeding
Jiayan Wee, Lynn Yeo Seo Hoon and Venkatesan Kumaresh
Khoo Teck Puat Hospital, Singapore, Singapore
Abstract
Background: Angioembolization of bleeding vessels is a management strategy considered for patients who present with lower bleeding gastrointestinal tract (LBGIT). Development of acute mesenteric ischemia is a known complication post angioembolization, with an incidence of up to 8%. Acute mesenteric ischemia leads to bowel ischemia, with a mortality rate of up to 80%. Hence, early detection is paramount. It is still common practice to use serial serum lactate levels to identify and diagnose acute development of ischemic bowel.
We report 2 cases of ischemic bowel following angioembolization with normal serum lactate levels. Diagnosis was made based on clinical suspicious and on computed tomography (CT scan). Our results suggest that use of serial serum lactate to monitor for bowel ischemia is not useful, and should not be used routinely.
Case Presentation: We report 2 cases of large bowel ischemia following angioembolization for LBGIT in our hospital between 2017 and 2019.
First report was a 65 year old male with no significant past medical history, presented with rectal bleeding from hepatic flexure diverticulum, and subsequently under went angio-embolization of right colic artery. 48 hours later, diagnosed to have ischemic bowel and eventually had right hemicolectomy performed.
Our second patient, was a 84 year old female, who underwent angioembolization of inferior mesenteric artery for rectal bleeding secondary to diverticulum from descending colon. Within 24 hours of angioembolization, found to have colonic ischemia from the splenic flexure down to the rectosigmoid junction and underwent laparotomy with bowel resection.
Both patients developed abdominal pain post-angioembolization but serial abdominal examination was equivocal. In both cases, serial serum lactate measured was not significantly elevated. Contrasted computed tomography of abdomen and pelvis was then performed and revealed findings suspicious of ischemic bowel. There was marked leukocytosis, with counts of 30 × 109/L.
Conclusion: Serum lactate levels and metabolic acidosis appear to be less sensitive as compared to abdominal pain and leukocytosis to detect bowel ischemia. Serial trending of lactate post-angioembolization for early detection of bowel ischemia may not be useful. Serum lactate levels are not significantly raised and lack of metabolic acidosis should not delay detection of bowel ischemia if clinical suspicious is high.
0246
RESPCT QI: Rapid Evaluation of Serum Procalcitonin Point of Care Testing in a General Intensive Care. A Quality Improvement Project
Susan Stevenson, Vallish Bhardwaj, Owen Hicks, Jake Collins and Keenan Louly-Nathan
Broomfield Hospital, Chelmsford, United Kingdom
Abstract
Background: Antimicrobial therapy overuse is associated with resistance, complications and increased healthcare expenditure.1 Rationalised prescribing practices aim to reduce duration and broad-spectrum antibiotic use. De-escalation presents a diagnostic challenge in ITU as the features of the systemic inflammatory response syndrome occur in both infective and non-infective causes. Research has aimed to identify biomarkers such as Procalcitonin (PCT) which can aid decision making. Previous trials have demonstrated a reduction in antibiotic duration associated with PCT testing2 with recent Surviving Sepsis guidelines advocating the use of PCT in shortening antibiotic therapy duration.3
Methods: An observational retrospective and prospective audit cycle of antimicrobial prescribing practices before and after the introduction of PCT Point-of-Care (POC) testing was performed. Patients admitted with a primary diagnosis of sepsis and receiving a known and completed duration of antibiotics were included. Duration, absolute number of doses and proportion of intended antibiotic course duration were compared across two, three month periods. Procalcitonin levels were measured using the standard laboratory analyser and POC machine were compared. The clinical decision regarding antibiotic discontinuation and that dictated by the PCT value were compared. Clinicians were unblinded to the value of the PCT and in making decision regarding de-escalation. A cost analysis was performed looking at the potential savings and costs had PCT values been followed.
Results: Thirty-two patients were identified during the retrospective review as having sepsis and 32 patients had PCT testing during the prospective period, 29 of which completed their course. Both groups were similarly matched in terms of age, sex, antibiotic indication and antibiotic prescribing practices. The mean duration of antibiotic courses in terms of days was 104% and 87% of the intended days in the retrospective and prospective groups respectively. Of the 42 occasions where PCT was tested, only 32 values were used in the decision related to antibiotic discontinuation and in only 64% was the appropriate decision made relative to the PCT value. In 4 instances the decision to stop antibiotics occurred despite a high PCT and in 7 cases, antibiotics were continued despite a low PCT.
There overall cost of all antibiotics given during the prospective period was £5890. Based on the antibiotics prescribed, the potential costs and savings for the retrospective and prospective reviews was £44 and £579 respectively, with an overall saving of potentially £535, representing 9% of the overall cost. Each POC test costed £13. Based on the 32 times when PCT levels were used appropriately, this would have incurred a cost of £416, with an overall potential saving of £119 within this specific observational group. Labotory and POC values were well correlated with a correlation co-efficient of 0.997.
Conclusion: The introduction of PCT testing was successful at reducing the quantity of antibiotics in terms of the proportion of intended course given. This occurred despite poor compliance with PCT guidance. Furthermore, potential PCT value compliance was associated with a potential saving in antibiotic costs supporting the use of POC PCT testing in ICU.
0247
A Single Centre Audit of the Implementation of a Post-Operative Cardiac Physiotherapy Screening Tool
Luke Newey and Hannah Toghill
Swansea Bay University Health Board, Swansea, United Kingdom
Abstract
Introduction: At a time when time, money and staffing are limited in the NHS, streamlining and targeted provision of services enable those in the most need to receive the appropriate interventions in a timely manner. This is no different in the provision of post-operative Cardiac Physiotherapy in Morriston Hospital, Swansea.
Background/Objectives: Surgical cardiac patients routinely receive physiotherapy post-operatively for both their respiratory and physical function.1,2 Following assessment each patient completes a physiotherapy led rehabilitation programme to facilitate progression to discharge. The cohort within the cardiac surgery population is varied; both in age, comorbidities and initial presenting complaint.3 Given the varied nature of the patient cohort it would seem prudent to provide those in the most need with the resources to facilitate quicker functional recovery and reduce their length of stay. In order to do this a criteria was created to identify patients most in need based on a number of risk factors.3–5
The objective of this project was to see if the implementation of a Cardiac Post-Operative Screening Tool could facilitate the prioritisation of service provision to those with greater need and to see if this was safe to adopt as regular practice.
Methods: We used a Multidisciplinary Team (MDT) approach in the creation of the Screening Tool using an evidence base of post-operative complication risk factors as well as pre-operative functional indicators that would likely hamper recovery. Patients fitting any of the criteria were deemed as high risk and treated with standard physiotherapy interventions. Those that did not were identified as low risk and provided with an incentive spirometer and post-operative exercise booklet (as were high risk patients) but they were progressed functionally with the nursing staff. There was an open re-referral system so that any member of the MDT could refer low risk patients for physiotherapy review at any time.
Having disseminated to the MDT the proposed start date, the screening tool itself and its practical implications, we carried out a three-month trial period collecting data for all cardiac surgical patients admitted during this time. The data was collated and analysed to assess its efficacy during the trial period of delivering safe and targeted intervention.
Results: In total 181 patients were screened with 37 identified as low risk, representing a 24.73% reduction in caseload for physiotherapy. Of the 37 low risk patients we had 4 re-referrals from the MDT for either respiratory or mobility review. The overall average length of stay (LOS) in days for the entire cohort was 9.1. Comparatively the average LOS for the high and low risk groups were 9.6 and 7.9 respectively. Of the high risk group 53 patients (39% of the high risk cohort) triggered on age alone. No adverse events were found during the trial period.
Conclusion: The findings of this trial would support that the use of a Cardiac Screening Tool is safe and enables therapies to target intervention at those with the most need. From our experience an MDT approach ensures unit collaboration and a unified care approach.
0248
Delivery of non-invasive ventilation clinical simulation through a locally developed self-breathing patient model
Alasdair Munro, Manisha Shah and Rahul Sarkar
Medway Maritime Hospital, Gillingham, United Kingdom
Abstract
Introduction: Non-invasive ventilation (NIV) is a common intervention in critical care. Junior doctors taking up placement in critical care can often have little prior training in NIV, preventing optimum decision making. High fidelity NIV simulation are challenging as the 3G mannequins cannot trigger the ventilator.
Objectives: Our aim was to develop confidence and competence of junior critical trainees in NIV through a combination of conventional teaching methods and high-fidelity simulation. A locally modified tailormade model was used for the NIV simulation, to simulate patient triggering.
Methods: One end of long oxygen tubing was placed within the oral cavity of the mannequin with the other end attached to a three-way cannula and a suction device (pictures 1 and 2). This transmitted-25 kPa of suction pressure to the oral cavity which could be intermittently occluded every 2–3 seconds, synchronising with the mannequin respiratory rate, generating a pressure gradient in the mannequin oral cavity (Picture 2). This triggers the non-invasive ventilator to provide a breath after each occlusion manoeuvre. This modification cost under £5.
Eight candidates, ranging from foundation year 1 to senior house officers, were orientated to the room and non-invasive ventilator. A short teaching session delivered by a critical care consultant regarding indication and trouble-shooting NIV, and on clinical features supporting failure of NIV. Two simulation scenarios were run each with two candidates participating and six candidates observing. A debrief discussion followed each scenario. Pre and post session candidates were asked to self-assess their competence at; identifying the need commence NIV, managing and adjusting NIV settings in response to arterial blood gases, identifying when NIV is no longer adequate. This ranged from ‘not competent’ to ‘happy to teach’ in a Likert scale. Overall confidence pre and post simulation was self-assessed on a 1–10 rating scale.
Results: Self-assessed competence at identifying the need for commencing non-invasive ventilation improved post simulation training. Pre-session, the majority felt either ‘not competent’ or only happy to initiate NIV under direct supervision. Post-session, all candidates felt that they could perform this under indirect supervision.
None of the candidates pre-training were comfortable managing and adjusting NIV in response to arterial blood gases under indirect supervision. Following the session, seven candidates felt competent to do this at least under indirect supervision.
Improved candidate competence at identifying NIV failure was noted post scenario with 6 candidates happy to do this at least under indirect supervision. Average candidate confidence using NIV increased from 3.1 pre scenario to 7.2 post. No candidates mentioned difficulty with the mannequin; the facilitator reported the smooth use of the model modification.
Conclusions: In this small-scale study, a clear improvement in self assessed competence and confidence following simulation training could be achieved. This suggests that these sessions would be of benefit for new trainees covering critical care areas. This highlights the need for high fidelity simulation training in this widely utilised treatment modality in critical care and wards. Our modification of the mannequin was effective and cheap in simulating patient-triggered breaths and can be utilised widely.
0249
Similarities in perceived sleep quality between surgical and medical ICU patients
Timo Tolppa1,2, Sabrina Monteregge1, Yaami Premakumar1,2 and Marcela Vizcaychipi1,2
1Chelsea and Westminster Hospital NHS Trust, London, United Kingdom
2Imperial College London, London, United Kingdom
Abstract
Introduction: Improving patients’ quality and quantity of sleep in the intensive care unit (ICU) is of vital importance due to the role sleep plays in immune function and cognition.1–3 Sleep quality has been characterised in specific ICU populations,4–5 but less so in mixed units consisting of medical and surgical as well as high dependency unit patients. Identifying similarities and differences in factors contributing to sleep disturbance in distinct groups of critically ill patients helps determine whether a ‘one size fits all’ approach to improving sleep in ICU is more appropriate than bespoke sleep interventions.
Objective: To compare perceived sleep quality and factors disrupting sleep between medical and surgical adult ICU patients reported by patients and nurses as part of baseline data collection conducted for a quality improvement project assessing the impact of environmental improvements in the ICU.
Method: The project team administered the validated Richards-Campbell Sleep Questionnaire (RCSQ) to all adult patients admitted to the ICU from March to June 2019. The RCSQ assesses five domains of sleep including depth, latency, awakenings, quality and percentage time spent awake, and produces an aggregate sleep index.6 A question was incorporated to identify factors contributing to poor sleep,3 and admission data was also captured. Patients were approached daily in the mornings if they were alert and negative for the Confusion Assessment Method for the ICU (CAM-ICU) during the previous night. Nursing staff were asked to fill in the RCSQ for patients who had communication difficulties or were CAM-ICU positive.7 Responses from the RCSQ were recorded in MS Excel and results analysed in STATA.
Results: A total of 333 sleep episodes were captured with a response rate of 74.2%. Of these, 36.3% (n = 121) were surgical and 63.7% (n = 212) medical patients. The overall sleep index score was 60 (IQR 32.2-81.2) and only 9.4% (n = 30) stated that nothing disturbed their sleep. The most commonly reported disturbing factors were pathophysiological (pain, coughing) and care-related factors (medical or nursing care), which equally disturbed sleep in 39.3% (n = 125) of cases, followed by environmental factors (light, noise) in 32.7% (n = 104) of sleep episodes. The medical and surgical patients differed significantly (p > 0.05) in their demographics, including age, sex, APACHE II score and quality of sleep at home, however the median sleep index for surgical (60, IQR 24–75) and medical (61, IQR 36–85) patients was not statistically different (p = 0.13). There were also no differences between medical and surgical patients regarding factors disturbing their sleep, including environmental, care-related, pathophysiological and psychological factors. Elective and emergency surgical patients did not differ from one another in their average sleep index or factors disturbing sleep. A higher proportion of patients reported the environment as a disrupting factor (43.5%, n = 83) than nurses (16.5%, n = 21).
Conclusion: Poor sleep and various factors disturbing sleep were equally reported by all critically ill patients regardless of reason for admission, mode of admission or disease severity. Interventions to promote better sleep can therefore be applied widely to all patients within ICUs to address poor baseline perceived quality of sleep.
0250
Taking care of BISSness – the Biochemistry In Sepsis Score: Guiding treatment and prognostication with point-of-care testing. A pilot study
George Chapman1, Ruby Carrington1, Andrew Chapman2 and James Malycha3
1Buckinghamshire Healthcare NHS Trust, Aylesbury, United Kingdom
2University of Bath Mathematics Resources Centre, Bath, United Kingdom
3Oxford University Hospitals NHS Trust, Oxford, United Kingdom
Abstract
Background: Sepsis continues to be an important cause of death in hospitals worldwide. Early warning scores utilising patient observations are widely used and have proven utility. With the increasing availability of point-of-care testing in emergency departments and acute medical units there is increasingly rapid access to biochemical results. A simple biochemical scoring system, modelled on the CURB-65 score, may aid clinical decision making in new admissions with sepsis.
Objectives:
Primary: develop a biochemistry in sepsis score (BISS) to aid early clinical decision making.
Secondary: test the feasibility of developing a similar scoring system with a significantly larger dataset.
Methods: Retrospective data was collected from 101 patients coded with sepsis (regardless of source) on admission to a district general hospital in Buckinghamshire. The outcome was defined as admission to intensive care during the first seven days or mortality within 30 days. Odds ratios were calculated using univariate logistic regression. Thresholds for biochemical values were chosen and performance tested using receiver operating characteristic curves.
Results: Lactate, urea and C-reactive protein (CRP) were associated with the defined outcome. LUC-75, where one point is scored for each of lactate >3 mmol/L, urea >12 mmol/L, CRP > 100 mg/L and age >75 years was significantly associated with the outcome. There were no intensive care admissions or 30-day mortalities in the cohort with a LUC-75 score of zero. Performing similarly to CURB-65,1 and stratifying according to risk, a LUC-75 score of one yielded 17% defined outcomes; score of two, 26%; score of three, 27%; score of four, 40%. A total n = 101 with 20 outcomes limited the statistical analysis of this study.
Conclusion: The LUC-75 score shows promise as an aid to clinical decision making in patients with sepsis. Further research in studies designed with greater statistical power are needed.
0251
Trends in extubation practice over two years in a mixed medical/surgical ICU
Mark Giza, Owen Gustafson and Benjamin Millette
Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Abstract
Introduction: Liberation from mechanical ventilation is an important cornerstone of intensive care practice as failed extubation is associated with a significant morbidity and mortality. Several methods and processes of care are available to minimise the risk of failed extubation. The “optimal” rate of failed extubation is unknown but some have proposed 5–10%.1
Objectives: We sought to characterise the extubation practices of our tertiary medical/surgical intensive care unit comparing with data collected two years previously to identify any trends in care or areas for improvement.
Methods: Using electronic health records, we retrospectively identified consecutive patients ventilated for more than 24 h who went on to be extubated. Palliative extubations were excluded. We collected data on demographics, whether formal spontaneous breathing trial (SBT) was conducted, ventilator settings prior to extubation, time of extubation, method of respiratory support post extubation, adverse events and reintubation rate at 48 h. Two cohorts of patients were analysed from 2017 and 2019. Differences in categorical variables were analysed using Fisher’s exact test.
Results: 100 and 71 patients were analysed in the 2017 and 2019 cohorts respectively. Baseline characteristics between the cohorts were similar. Mean FiO2 at extubation was.3 and.31 for 2017 and 2019. Rates of extubation out of hours (1700-0800) were similar (4% vs 4.8%). Rates of formal SBT (on ventilator settings of 5/5 or lower) decreased from 87% in 2017 to 62% in 2019 (p = .0002).
High flow nasal oxygen was the most common form of respiratory support following extubation in both cohorts (76% and 83%). There was no difference in use of NIV (5.6% and 4.8%). The rate of reintubation at 48 h did not change significantly from 2017 (11%) to 2019 (11%).
Comparing adverse events between cohorts, the rates of desaturation <80% and use of rescue NIV did not differ significantly. However significantly more patients in 2017 required more than 50% oxygen following extubation (32% vs 11% p = .0013).
Conclusions: Extubation practice in our institution seems to have remained mostly stable during this time period and our rate of failed extubation of 11% is not far off the proposed “optimal” rate of 5–10%. The increased need for >50% oxygen in the 2017 cohort does not seem to have led to an increase in reintubation or other adverse events so it is likely not clinically significant. The high use of HFNO for respiratory support post extubation is supported by several RCTs showing reduced reintubation rate with this strategy2,3. The reduced rate of SBT in the 2019 cohort is concerning, especially as five of the eight reintubations in this group did not have an SBT. We have highlighted this to our department and will continue to monitor our extubation practice to drive improvements in the future.
0253
Ultrasound-guided subclavian venous access: development of a multispecialty teaching programme in a major trauma centre
Benjamin Millette, Tim Wait and Nick Suarez
Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Abstract
Introduction: Subclavian central venous access (SCVA) has a lower rate of infective and thrombotic complications compared to femoral and internal jugular venous access (1). This data also demonstrates higher rates of mechanical complications such as pneumothorax, but in the context of high rates of insertion guided by landmark technique (1). The use of real time ultrasound results in decreased rates of mechanical complications that are similar to the jugular insertion site (2).
We established (by means of a survey) that few anaesthetic or intensive care medicine (ICM) trainees in our region have received formal training in landmark or ultrasound-guided SCVA and are not confident in it. We taught a short teaching session with live human ultrasound scanning and subclavian gel phantom needling practice to improve confidence.
Having developed this teaching programme, we had a great deal of interest in developing these skills from consultants in anaesthesia and intensive care as well as from consultants and trainees in emergency medicine (EM). We therefore refined and extended it to further promulgate these skills in our local major trauma centre.
Objectives: We aimed to increase local use of ultrasound-guided SCVA in order to minimise central line-associated bloodstream infection (CLABSI) and mechanical complications associated with SCVA.
Methods: We performed several teaching sessions comprising lectures followed by in vivo scanning of the subclavian vein, needling a subclavian gel phantom with real time ultrasound and practising sequential needle tip tracking on a separate phantom.
We gathered data on participant grade, specialty, formal teaching experience in SCVA and number of times they had inserted SCVA. We compared their confidence in performing ultrasound-guided SCVA before and after the training session using a visual analogue scale (VAS) running from 0 to 100.
Continuous data were checked for normality using the Shapiro-Wilk test. When this failed to detect normality, data were compared using the Mann-Whitney test.
Results: 48 physicians in total were then taught over four teaching sessions. 87.5% had received no previous instruction in ultrasound-guided SCVA. 66.6% had inserted no subclavian lines under ultrasound guidance and 83% had inserted five or fewer. The median confidence in SCVA prior to teaching was 12 and after the session this rose to 57.5 on the VAS (p < 0.001 by Mann-Whitney U test) (Fig 1). The sessions were highly valued by trainees and consultants alike.
Discussion: This study demonstrates that our local anaesthetic/ICM/EM physicians have little experience in inserting SCVA and receive little formal training in it. Furthermore, we have shown that a short training session can improve their confidence, making them more likely to seek out further training opportunities in their routine practice. We have used the teaching sessions to encourage familiarity with and use of this technique in order to help minimise overall complications of central venous access including CLABSI and mechanical complications such as pneumothorax and arterial puncture. Further teaching sessions are planned to continue as there is an ongoing demand for these skills in our region.
Figure 1.
0254
HDU in the Post-Anaesthesia Care Unit – Resource and Tariff Implications
Tom Brougham1 and Marcin Pachucki2
1University Hospitals Bristol NHS Foundation Trust, Bristol, United Kingdom
2Gloucestershire NHS Trust, Cheltenham, United Kingdom
Abstract
Objective: This project aimed to assess the number and characteristics of patients receiving High Dependency Unit (HDU) care in the Post-Anaesthesia Care Unit (PACU) and the costs associated with this at Gloucestershire Royal Hospital.
Background: Gloucestershire Royal Hospital is a large district general hospital with a total of 683 inpatient beds. There are 17 physical critical care beds, divided into a 13-bed intensive care unit (staffed to a dependency of 10) and a separate 4-bed surgical HDU opened when needed and staffing allows. There are just over a thousand critical care admissions annually. As with most critical care units, surgical patients requiring HDU care often have a delayed admission from PACU to critical care due to bed and staffing pressures.
The level 2 bed day tariff applies if a patient receives one or more of a specific list of HDU interventions in critical care. This tariff does not apply to patients receiving HDU interventions in PACU.
Method: Data on delayed critical care admissions was collected prospectively by PACU nursing staff over 21 weeks during June to November 2018. Timings of admission and discharge, surgical speciality and HDU interventions were captured. Additional cases were identified from electronic health records.
Results: 186 patients were identified with a total of 96 bed days of HDU care provided in PACU. Due to incomplete data, this translates to an estimated 379 ‘missed’ level 2 bed days per year. The HDU care provided in PACU represents 6.5% of the maximum total number of chargeable Level 2/3 bed days.
The patients fell into two groups. Firstly, patients referred to critical care and accepted but for whom admission was delayed, or who were not admitted at all, due to lack of capacity. These patients were predominately high-risk elective general surgical and maxillo-facial patients. Secondly, patients who were never referred to critical care despite receiving HDU care and interventions in PACU. These patients were mostly emergency orthopaedic patients, often elderly and operated on for neck of femur fractures. In both groups of patients, the most common HDU interventions received were invasive arterial monitoring and vasopressor infusions.
Patients receiving HDU interventions had a prolonged PACU stay, with a median stay of 4.5 hours, rising to 13.5 hours for patients who were never admitted to critical care. These patients often stayed in PACU overnight when staffing levels were lowest. Currently, only about 25% of PACU staff have formal HDU competencies.
Conclusion: This project found that approximately 379 bed days of HDU care were provided in PACU. This represents a major loss of revenue for critical care as this equates to 6.5% of the total annual chargeable level 2/3 bed days for the hospital. These patients create a significant workload for PACU nursing staff, many of whom do not have formal HDU training.
Possible solutions include prioritising critical care discharges, referring all patients receiving HDU care to critical care, increasing use of Surgical HDU, training PACU nursing staff in HDU competencies and expanding critical care capacity.
0255
Both hyperdynamic and depressed left ventricular function is associated with mortality in patients with septic shock – a retrospective cohort study
Minesh Chotalia1,2, Mansoor Bangash1,2, Tracie Matthews1,2, Dhruv Parekh1,2 and Jaimin Patel1,2
1University of Birmingham, Birmingham, United Kingdom
2University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Septic shock is characterised by collapse of the cardiovascular system in response to an abnormal host response to infection,1 which is initially mediated by vasoplegia and accompanied by an increase in cardiac output (hyperdynamic circulation). As shock progresses the hyperdynamic circulation is often replaced with myocardial depression, with previous studies reporting between 20–60% of patients experiencing a depression in left ventricular function (LV).2 The impact of changes in LV function upon patient outcomes remains uncertain.
Objective: To assess whether abnormal left ventricular function, defined as either a hyperdynamic circulation or myocardial depression, as visualised by transthoracic echocardiography (TTE), was associated with mortality in septic shock.
Methods: Patients admitted with a diagnosis of septic shock (Sepsis 3) and who had a formal cardiologist TTE between April 2016 and July 2019 to the Queen Elizabeth Hospital, Birmingham were included. Patient data and TTE reports were retrieved using electronic patient records. LV function was defined as either normal, hyperdynamic (based on TTE report) or depressed (LV ejection fraction £45% or grade II diastolic dysfunction). The primary outcome was 90-day mortality. Continuous data are presented as mean (SD). Catergorical data were analyzed using a chi-squared test.
Results: 878 patients were admitted with septic shock. 363 (42%) had a TTE whilst admitted in intensive care. The mean day of the TTE was 5 days ± 1.1 post admission. The majority of patients were male (60%) with a mean age of 60.6 ± 1.9 years and APACHE II 20.6 ± 0.7. Mean ITU length of stay was 14.3 ± 2 days and 90-day mortality was 39%. Overall 234 (65%) had normal LV function, with 128 (35%) having an abnormal TTE. 66 (18%) were hyperdynamic and 62 (17%) had depressed LV function. LV dysfunction was associated with a significantly higher 90-day mortality (66% vs. 25%, p < 0.0001). 90-day mortality in patients with a hyperdynamic LV was 76% compared to 55% in those with a depressed LV (p = 0.015). LV dysfunction also correlated with significantly higher need for invasive ventilation (81% vs 70%, p = 0.03). There was no difference in age, APACHE II, day of TTE, length of ITU, hospital stay, need for advanced vasopressor or renal support between abnormal and normal LV function cohorts.
Conclusion: This is one of the first studies to demonstrate that abnormal LV function is associated with increased 90-day mortality in patients with septic shock. Interestingly a hyperdynamic LV was associated with a higher mortality than depression of the LV which challenges the paradigm of early goal directed therapy to maximise oxygen delivery. Perhaps future research should aim to normalise LV function in critically ill patients.
0257
Schmidt Syndrome: An Unusual Presentation
Michael Argent1, Ryan Stephens1 and Bethan Gibson2
1University Hospital Wales, Cardiff, United Kingdom
2Cwm Taf Morgannwg University Health Board,., United Kingdom
Abstract
Background: Polyglandular autoimmune syndrome type 2, also known as Schmidt syndrome, is a rare cause of immune mediated, multiple endocrine failure, usually presenting in the third decade of life. Its diagnosis requires the presence of autoimmune adrenal insufficiency (Addison’s disease) with autoimmune hypothyroidism and/or type 1 diabetes mellitus. It is associated with many other endocrine and non-endocrine component autoimmune diseases including Coeliac disease. Malabsorption of levothyroxine is a rare but recognised complication of Coeliac disease, owing to atrophy of the villous architecture of the small intestine, the main site of absorption of levothyroxine.
We herein describe a case of a 30-year-old female with Schmidt syndrome who was admitted to our unit with a diagnosis of coeliac induced hypothyroid crisis, presenting with out-of-hospital cardiac arrest and hypothyroid induced renal failure.
Case Presentation: A 30-year-old Caucasian female with a known history of Schmidt syndrome and newly diagnosed Coeliac disease suffered an out-of-hospital VF cardiac arrest. This was preceded by a short history of visual disturbances, lethargy, myalgia, unintentional weight loss and cognitive impairment. Despite this she remained compliant with all of her drug treatment. Following successful resuscitation, the patient was admitted to ITU for multi-organ support.
Clinical examination revealed profound circulatory collapse, with drug-resistant bradycardia and marked hypothermia. Initial investigations demonstrated a prolonged QTc (591 ms), deranged renal function (Na 127, K 6.4, Ur 22.4, Cr 349) with marked metabolic acidosis, and severe hypothyroidism (T4, TSH > 200).
Based on the clinical history, examination and biochemical results a diagnosis of myxoedema coma with the presentation due to associated complications including prolonged QTc induced VF arrest and hypothyroid induced renal failure.
Initial management included mechanical ventilation, cardiovascular support in the form of isoprenaline and adrenaline infusions, renal replacement therapy, intravenous liothyronine and hydrocortisone treatment. Within 6 days the patient had made a good recovery and was discharged to the ward under the joint care of cardiology and endocrinology. The patient was followed up after hospital discharge in ITU clinic and has made a full recovery and has returned to full time employment.
Conclusions: A pertinent point in this patient’s presentation was the recent diagnosis of Coeliac disease. This was viewed as a significant contributory factor to the ensuing myxoedema coma and VF arrest owing to the malabsorption of levothyroxine. This association whilst rare is recognized in medical literature and is important in view of the increased incidence of Coeliac disease in patients with co-existing autoimmune endocrine disorders.
This case also highlights the wide scope of potential causes for cardiac arrest in younger patients and the importance of identifying the underlying disease processes, in view of the reversible nature.
0258
Moving Beyond Audit; Embracing QI Methodology to Drive Improvements in Lung Protective Ventilation
Chamene Welhengama, Daniel Watkin, Robert Normanton, Alexander Wallis, Joe Watson, Mike Irvine, James Watmore, Norman Main and Maryam Crews
Intensive Care Unit, Royal Liverpool University Hospital, Liverpool, United Kingdom
Abstract
Introduction: Mechanical ventilation is used to support patients during critical illness. Evidence suggests that large tidal volumes (Vt > 8 ml/kg ideal body weight (IBW)) cause lung damage, increasing mortality and morbidity.1 Despite this, most critical care units fail to reduce Vt, with many studies demonstrating that only 40–60% of patients on mandatory ventilation receive Vt < 8 ml/kg.2–3 This is due to several complex factors such as time demand, knowledge, and cognitive load. With this in mind, we introduced a QI project to improve our unit’s adherence to low tidal volume ventilation. We named it LIVES (Low tIdal VolumES).
Objective: Patients receive Vt < 8 ml/kg IBW for over 85% of their time on mandatory ventilation, by the end of an 8-month period (ending November 2019).
Methods: Due to the complexity of the problem, we chose QI methodology to drive continuous improvement, using a novel project team strategy. Team lead roles and responsibilities were assigned, including Project Lead, Data Collection and Analysis Leads, Comms Lead, and Nursing Lead.
We undertook a broad-based strategy to diagnose the root cause of the problem, including stakeholder interviews and brainstorming sessions utilising QI tools such as fishbone diagrams. The project was co-ordinated through the Life QI web platform.
Over a 6-week period, baseline data was collected from every mandatory ventilated patient on the unit. Analysis showed Vt < 8 ml/kg was achieved only 60.1% of the time on mandatory ventilation.
We constructed a Driver Diagram with a series of Change Ideas. Interventions were determined from the change ideas and introduced in series as follows:
• A broad based, continuous, multidisciplinary education programme.
• Introduction of an easily accessible bedside LIVES Ventilation Protocol.
• Use of daily prompts to maintain the standard via the critical care safety brief and nursing huddles.
• A comprehensive communications strategy with weekly anonymised Vt reports delivered automatically to staff using Google Data Studio with access to data in real time.
The Intervention Phase of the project was commenced with PDSA cycles carried out for each Change Idea and modified as required.
Results: As of 18th July 2019, over 3000 Vt data points were collected and analysed using a Statistical Process Control Chart to easily visualise the effects of Change Ideas and shifts in adherence (Fig 1).
Current results show a dramatic improvement in adherence to lung protective ventilation. Time spent on mandatory ventilation with Vt < 8 ml/kg improved to 82.8%, compared to 60.1% baseline. We expect to comfortably reach our target of 85% by the time of project completion.
Further analysis shows reduced incidence of extreme tidal volumes (Fig 2). We expect this to reduce Ventilator-Induced Lung Injury, leading to improvements in morbidity, mortality, and Unit and hospital length of stay.
Conclusion: The use of QI methodology to implement low tidal volume ventilation has shown a statistically significant improvement in the delivery of lung protective ventilation in the Critical Care Unit.
We suggest that using QI methodology and a novel team set up is central to the success of the project and recommend the approach to teams struggling with complex clinical problems.
Figure 1.
Figure 2.
0262
Changing Cultures in the ICU: Gap analysis of ICCQIP data collection in a District General Hospital
Chelcie Jewitt and Kathryn Tizard
Countess of Chester Hospital NHS Foundation Trust, Chester, United Kingdom
Abstract
Introduction: The Infection in Critical Care Quality Improvement Project (ICCQIP)1 was introduced in 2012, following national drive to capture the rate of healthcare associated infections (HAI), within the Critical Care setting, specifically related to indwelling central venous catheters (CVCs). Following the Matching Michigan project,2 the overarching aim of the ICCQIP initiative is to improve the care of critical care patients by clarifying the incidence of catheter related blood stream infections (CRBSIs) in England and promoting the implementation of local quality improvement projects to minimize infection rates.
There have been difficulties in data collection amongst many Critical Care units within our region, despite participation in ICCQIP being included in the D05 Service Specification for Adult Critical Care.3 Following a gap analysis we have implemented several changes to the ICCQIP data collection at the Countess of Chester Hospital over the past 12 months, with the aim of making the process more accurate and sustainable.
Objectives:
1. Streamline the data collection process for ICCQIP data
2. Improve mandatory data collection for central catheter related blood stream infections (CCRBSIs)
3. Highlight contribution CCRBSIs make to hospital acquired infections
4. Improve patient care by promoting local QIPs improving CCRBI rates
Methods: An initial gap analysis was performed which demonstrated discrepancies between the data already collected by the trust and with that necessary to complete the mandatory ICCQIP data sets. Systematic barriers were investigated, and sustainable changes were implemented to improve the efficiency of data collection.
We have worked in collaboration with IT leads to change the minimum data set page on our hospital computer system to enable ICU nursing staff to easily record necessary CVC denominator data every 24 hours. We liaised with the microbiology team to time analyse paired blood culture samples in the laboratory in order to provide the necessary differential data required. Specific standardized documentation was designed in order to collate paired culture data, patients’ clinical data and blood culture results. A programme of education and ongoing positive reinforcement of medical and nursing staff was undertaken to empower the ICU team to take paired cultures when indicated and accurate documentation of paired cultures with likely infection source at time of suspicion.
Once a month, the data was interrogated manually to review errors, erase duplicates and refine the data collection process.
Results: The introduction of a standardized form has improved documentation when taking blood cultures, enabling the nominator ICCQIP data to be collected in a more accurate and simplified way.
This has consequently led to the monthly uploading of data to ICCQIP and feedback from Public Health England regarding our local unit and benchmarking data, informing and improving clinical practice.
Conclusions: Local data collection has improved following the changes made, leading to closer analysis of CRSBI rates, enabling surveillance of local infection rates in a more sustainable way and compliance with the mandatory PHE ICCQIP.
This is an ongoing project where our experience has been shared with the Cheshire and Merseyside critical care network, which is exploring further solutions to streamline data collection at a regional level.
0264
Improving documentation in ICU
Madhavi Gudipati, James Turner and Derrick Clarence
Walsall Manor Hospital, Walsall, United Kingdom
Abstract
Introduction: Documentation in ICU is extremely important as it serves not only as a safety tool for patient welfare but also as an important medico-legal document. During daily ward round, we realised that our documentation of the daily review of patients was inadequate. The daily review within our unit is documented in a printed booklet which includes space for assessment of all items based on the local ICU daily review checklists. There is a separate space for review of the risk of ventilator acquired pneumonia, microbiological treatment, limitations of treatment and the DNAR status.
We elected to carry out an audit on documentation in our ICU which was based against the local and national ICM guidelines.
Objectives: The main objectives of our audit were:
a. To verify if the ICU booklet was being appropriately completed
b. Implementation of the recommendations to improve documentation
c. Re-audit
Methods: All ICU booklets were audited over a period of two weeks. The audited documentation consisted of the following aspects of the checklist: Ventilator Associated Pneumonia, Microbiological Treatment, Daily Treatment Plan, Limitations of Treatment and DNAR status. Booklets were considered ‘fully completed’, ‘partially completed’ or ‘not completed’, depending on how many categories had valid documentation.
The re-audit was carried out 8 months after the first audit and against the same criteria, as well as the audit of a checklist (FASTHUG), which was included in the booklet following the recommendations of the initial audit.
Results: Though the ‘fully completed’ rate fell from 63% to 36% from the first audit to the re-audit, there was an increase in the ‘partially completed’ rate from 17% to 60%. All aspects of the documentation showed some improvement. The ‘not completed’ rate improved from 20% in the first audit to 5% in the re-audit. FASTHUG compliance in the re-audit was 62%.
Conclusions: The initial problem identified was the inadequate completion of the documentation of the ICU daily review. Following the introduction of checklists as a cognitive aid to prevent human error, there was some improvement in the overall documentation of the daily review.
However, we realised while doing this audit that even though there are checklists in ICU for guidance, the reliance on the clinician alone to deliver 100% documentation at all times is difficult to achieve. This has been shown not just in our project, but also by audits done previously in different hospitals.
Thus, it was agreed that there is a need for teamwork to ensure consistent compliance with ICU checklist documentation. Teamwork has helped achieve near 100% compliance using the WHO checklist in the operating theatre. We therefore plan to introduce a “team brief” with a “stop moment” before leaving the patient’s bedside, analogous to the WHO pre-operative surgical “time out”. This would involve the entire ward round staff, including the bedside nurse and nurse-in-charge, to ensure that the necessary documentation is completed and the relevant aspects of patient care have been considered.
0265
Improving compliance with Enhanced Recovery After Surgery (ERAS) guidelines in the critical care setting: a quality improvement project
Adrian Mawhinney1,2, Kenneth McGrattan2, Anil Kumar2, Christine Marshall2 and Matt Hargreaves2
1The University of Manchester, Manchester, United Kingdom
2Royal Preston Hospital, Preston, United Kingdom
Abstract
Introduction/Objective: Enhanced recovery principles have been shown to improve patient outcomes and decrease hospital length of stay.1,2 The aim of this project was to evaluate our compliance with national guidelines and to improve the quality of patient care being received within our critical care unit (CrCU)
Methods: Elective colorectal and gynaecologic patients requiring a post-operative bed within the critical care unit were the chosen cohort. Utilising ERAS guidelines1,2 and a Quality improvement model, a pro-forma of targets was made. We retrospectively analysed patients during January 2019. Meetings, presentations, posters and information leaflets were utilised to help improve patient compliance and raise staff awareness. Patients were met pre-operatively, educated on their pending experience within critical care and advised regarding enhanced recovery principles in order to empower them in their own recovery. Data was then collected prospectively during May 2019 and re-analysed.
Results: IV fluid prescription is still non-compliant with NICE but is improving. A 35% improvement of cessation of IV fluids was noted but overall fluid balance was poorer. Opiate use was reduced by 20%. Marginal gains were made across most aspects of the project and further insight gained into avenues which could be further improved.
Conclusion: Utilising a Quality improvement approach, we have made improvements to the provision of enhanced recovery within the department. Further cycles will be carried out in future to continue this progress. It is our opinion that a designated ERAS clinician/nurse specialist would help facilitate ERAS transition and staff compliance. The use of a traffic light system to highlight performance to the whole team could be implemented.
0266
Post-operative Pulmonary Complications following major Hepato-biliary Surgery: A prospective observational study at a large tertiary centre
Lafi Olayan1, Jonathan Weblin2, Rajashankar Rao3, Bobby Dasari4, Randeep Mullhi3, Dhruv Parekh1,3, Fang Gao Smith1 and Jaimin Patel1,3
1Institute of Inflammation and Ageing, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2Department of Physiotherapy, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
3Department of Anaesthesia & ICM, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
4Department of HPB and liver transplantation, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Major surgeries are common and in general performed safely (1). However, approximately 10% of patients develop complications following surgery which has significant consequences in terms of both morbidity and mortality (2). Postoperative Pulmonary Complications (PPCs) are one of the commonest complications following major abdominal surgery (3).
Objectives: To determine the incidence and severity of PPCs after hepato-pancreatic-biliary (HPB) surgery at the Queen Elizabeth Hospital Birmingham (QEHB), which is one of the largest HPB centres in the UK.
Methods: Patient who underwent HPB surgery at QEHB and who had been enrolled in the Perioperative Quality Improvement Programme (PQIP) study between May 2018 and May 2019 were included. PQIP is a prospective observational study of patients undergoing major surgery. The primary outcome was the incidence of PPCs at day 7 measured by the Postoperative Morbidity Survey (POMS) (4), with severity of the PPCs determined using the StEP-COMPAC definitions (5). Secondary outcomes were length of stay (LOS) and 30-day mortality. Data analysis was performed using Man-Whitney U test for continues variables and Chi-Square test for categorical variables.
Results: A total of 145 patients were enrolled in the study with 89 (61.4%) males and 56 (38.6%) females. The median (IQR) age of the patients was 66 (57.5-73) years with most patients classified as ASA grade II (61.3%) or III (38%). The majority of HPB surgery was open (n = 130; 89.6%). Based on POMS, PPCs occurred in 18.6% (n = 27) of patients. The majority of patients developed PPCs on day 1 postoperatively (n = 8; 30%). Atelectasis was the commonest PPCs (67%), followed by pleural effusion (15%) and pneumonia (11%). Patients who developed a PPC were significantly older (70{IQR 64–77} years vs. 65{56-72} years, p = 0.027). There were no other preoperative differences between the two groups. The majority of PPCs were mild (n = 24; 88.9%) requiring only supplemental oxygen, with only 3 patients (11.1%) developing severe PPCs that required ventilatory support. The development of a PPC was associated with a significantly longer LOS (14 {9-23} days vs. 6 {5-7} days; p < 0.001) and higher chance of infectious complications (14 vs 4; p < 0.001).
Conclusion: This study has shown that using POMS and the StEP-COMPAC definitions that PPCs are extremely common following major HPB surgery and that the development of even mild PPCs has a significant impact on patient morbidity and LOS. The use of PQIP has helped to identify major morbidities and risk factors associated with PPCs. Future interventions should focus on reducing PPCs, with interventions targeted perioperatively.
0268
Targeted training improves the performance of critical care transfer teams
Helen Vesey1, Sarah Masterson1, Jonathan Bedford2 and Jonathan Birks1
1Northampton General Hospital NHS Trust, Northampton, United Kingdom
2Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Abstract
Introduction: It is not known whether transfer training effects the performance of critical care transfer teams. The quality of a critical care transfer can be assessed against a number of quantifiable measures known as "key performance indicators" (KPIs).
Objectives: We sought to identify the association between transfer training, staff seniority and out-of-hours transfers on KPIs for inter-hospital transfers from a district general hospital to neurosurgical specialist centres.
Methods: We analysed transfer records collected between May 2017 and April 2019 inclusive.
We analysed the compliance with locally set, physiologically-based KPIs for emergency transfers to neurosurgical specialist centres (mean arterial pressure (MAP), peripheral capillary oxygen saturation (SpO2), end-tidal CO2, body temperature, head up position and pupil monitoring). We also collected data on evidence of recent local transfer training of the transferring staff member, the seniority of said staff member, and the time of day of the transfer.
The primary outcome of interest was failure to achieve one or more KPIs.
We performed multivariable logistic regression analysis to determine the impact of transfer training, staff seniority, and out-of-hours transfers on the primary outcome.
Junior staff members were defined as those below the level of St3.
Results: We identified 136 transfer records. Of these, 82 represented transfers to a neurosurgical centre. Of these 82 transfers, 43 had evidence of one or more physiological KPI not being achieved (52.4%).
We found no association between being a junior member of staff or out-of-hours transfers with failure to achieve one or more physiological performance indicators (OR 0.52 (95% CI 0.17-1.52) and OR 1.25 (95% CI 0.50-3.13) respectively).
We identified a significant association between lack of evidence of transfer training and failure to achieve one or more physiological KPIs (OR 4.50 (95% CI 1.24-21.74)).
Conclusions: Lack of evident transfer training was associated with failure to achieve one or more physiological KPIs in transfers to neurosurgical specialist centres.
Staff seniority and out-of-hours transfer was not associated failure to achieve one or more physiological KPIs. These results emphasize the importance of local transfer training programmes and suggests staff seniority is of less importance.
0270
Introduction of a joint ICU and anaesthetic night safety huddle at St Helier Hospital – Cultivating collaborations between the ICU and anaesthetic teams with the aim of improving patient safety
Samuel Kestner1, Michael Robson2, Thomas Hansen3, Natashia Schneider1, John Dixon1 and Paul Bathke1
1Epsom and St Helier University Hospitals NHS Trust, South West London & Surrey, United Kingdom
2Royal Surrey County Hospital NHS Foundation Trust, Guildford, United Kingdom
3Lewisham and Greenwich NHS Trust, London, United Kingdom
Abstract
Introduction: The Fourth National Audit Project identified that at least 25% of major airway events occurred in ICU or in the emergency department. A lack of appropriately skilled staff and poor identification of high-risk patients were common themes which contributed to poor decision making.1
It is not always possible for ICUs to ensure that for every night shift there is an airway trained2 doctor on duty. Conversely, those covering ICU may have extensive airway training whilst the anaesthetists may be relatively junior.
St Helier Hospital is a District General Hospital with a 13 bedded ICU staffed by two ICU doctors overnight. The hospital has two on-site anaesthetists covering labour ward and the emergency theatre.
Historically, the on-site anaesthetists were contacted ad hoc by non-airway trained2 ICU doctors to assist in airway issues occurring outside of theatres, and there was no structured framework for the anaesthetists to flag potentially difficult theatre cases taking place overnight to the ICU team.
Objectives: To assess whether St Helier would benefit from a structured joint ICU and anaesthetic night safety huddle with a view to subsequent implementation and ongoing evaluation of its use.
Methods: To identify potential benefits a survey was sent (June 2018) to all 28 doctors covering ICU and anaesthetic night shifts.
Following this the night safety huddle and huddle proforma (Figure 1) were introduced (August 2018). This comprises a face to face huddle between the two ICU doctors and the two on-site anaesthetists after their respective handovers.
To evaluate the use of huddle (post-introduction) we retrospectively analysed the completed huddle proformas of 14 consecutive shifts (March 2019).
Results: There was a 64% (18/28) response rate to the June 2018 survey. Of the 18 respondents 5 (28%) did not always know the grade and airway competency of their night colleagues, 15 (84%) did not always know the presence and details of high-risk patients in other areas of the hospital, 11 (61%) thought that a formal introduction would ease night communications, and 16 (89%) felt that a face to face huddle would be preferential to telephone handovers.
In our March 2019 (post-introduction) analysis, over the 14 nights both ICU doctors and the emergency theatre anaesthetist were involved in the huddle 100% (14/14) of the time, with the labour ward anaesthetist definitely being involved 79% (11/14) of the time. On 93% (13/14) of these shifts there was at least one patient with a difficult airway3 present in the hospital whose existence was consequentially flagged to all huddle members.
Conclusions: We have successfully introduced a joint ICU and anaesthetic night safety huddle in St Helier Hospital. Our analysis, seven months after its introduction, has shown it reliably takes place, and flags up patients with difficult airways3 to both night teams. This model could be introduced in other hospitals to promote greater collaboration between ICU doctors and anaesthetists, with the aim of improving patient safety and reducing the number of airway incidents in ICU.
Figure 1.
Contents of the joint ICU and anaesthetics night safety huddle proforma.
0271
An Audit of High Flow Nasal Oxygen in a Large Intensive Care Unit in the UK
Saklain Farooq, Alexandra Efimov, Ali Zainul Abideen, Muzzammil Ali, Shraddha Goyal, Usman Awan, Tracie Matthews, Catherine Snelson and Jaimin Patel
University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Introduction: High-flow nasal oxygen (HFNO) delivers 50–60 L/min of oxygen via specifically designed nasal cannulae, provides up to 5cmH20 of positive end expiratory pressure, washes out the dead-space and increases end-expiratory lung volume. The use of HFNO has increased in critically ill patients over the past few years due to improved patient compliance and comfort despite the lack of clinical evidence of patient benefit1,2
Objective: The aim was to audit the use of HFNO according to the local trust protocol following its introduction in August 2018. The trust protocol advises that HFNO be used for hypoxaemic respiratory failure, and that in cases of treatment failure patients should be intubated rather than transitioned to NIV or CPAP.
Methods: A retrospective study of patients admitted to the Queen Elizabeth Hospital Birmingham (QEHB) intensive care unit (ICU) who received HFNO between August 2018 and February 2019. QEHB is one of the largest single site ICUs in Europe admitting 3520 patients/annum. Data collected included age, APACHE II, primary reason for admission, indication for HFNO, escalation of respiratory support, length of stay (LOS) and mortality. Ethical approval was not required. Continuous data is presented as median (range) and categorical data as percentage (n). A Chi-squared test was used for statistical analysis of categorical data.
Results: 272 patients received HFNO during the study period. 7 patients were excluded due to incomplete data, with 265 patients’ data being analysed. The median age was 61 (17–95 years) with a median APACHE II score of 18 (4–38). 81% (n = 214) were initiated on HFNO for type 1 respiratory failure, 11% (n = 31) had type 2 respiratory failure, and 1% (n = 2) of patients had HFNO as part of palliative care with 7% (n = 18) without a clear documented indication. 31% (n = 83) of patients had respiratory support escalated, of which 68% were directly intubated (n = 57) and 31% (n = 26) escalated to non-invasive ventilation with 50% (n = 13) of these then being intubated. Median ICU LOS was 8 days (1-166) and ICU mortality was 14%. Escalation of respiratory support was associated with a significantly higher mortality (8% vs. 27%), with those escalated to NIV having a higher mortality (35%) compared to those directly intubated (25%), although this failed to reach statistical significance.
Conclusion: This large audit of patients who received HFNO shows adequate compliance with the local protocol. Use of HFNO alone has a low mortality and as anticipated escalation of therapy was associated with increased mortality. Higher rates of mortality were seen in those progressing from HFNO to NIV than invasive ventilation. This supports the notion that delayed intubation due to failure of NIV, however delivered, increases mortality and morbidity.2
0272
Outcome of Patients with Liver Cirrhosis Referred to Critical Care in a District General Hospital
Najam Pervez, Putul Sarkar, Stanislaw Jankowski and John Dixon
Epsom and St Helier University Hospitals NHS Trust, London, United Kingdom
Abstract
Introduction: Chronic liver failure is frequently a terminal event, unless there is a specific and potentially reversible precipitant, such as variceal haemorrhage. Increasing organ failure carries a poor prognosis, with renal failure having a “particularly high mortality”.1
It has also been well-established that patients with, or without, a specific and potentially reversible precipitant have a mortality in excess of 89% when three or more organs (including the liver) have failed. This figure is much higher when patients with a specific, and potentially reversible, precipitant are excluded. Most available literature is from tertiary liver centres.2,3,4
Objectives:
1. To investigate the ICU-mortality of patients with liver cirrhosis referred to ICU in a district general hospital (DGH)
2. To assess the mortality within one year
Method: Data was collected over a one year period from 1st April 2018 to 31st March2019 by retrospectively reviewing patient notes, Wardwatcher®, and ICU referrals audit data.
Patients were classed as having liver cirrhosis if they had documented biopsy or radiological evidence of liver cirrhosis before referral to ICU and had been reviewed in a hepatology clinic for management of chronic liver disease.
Results: 39 patients were referred to ICU with liver cirrhosis: 21 (54%) were admitted to ICU, 7 (18%) improved following an endoscopy, 2 (5%) were transferred to a specialist centre, 7 (18%) required level 1 care and 1 (2.5%) required end of life care.
15 patients were admitted to ICU due to decompensated liver cirrhosis, and 6 were admitted for other reasons (e.g pneumonia). ICU mortality was 87% (13 patients) in the decompensated liver disease group and 93% (14 patients) at 1 year, All patients with cirrhosis admitted to ICU for other reasons survived ICU, however, 1-year mortality was 33%. 1-year mortality was 19% in the patients not admitted to ICU.
Conclusion: Patients with liver cirrhosis have a high mortality regardless of the reason for ICU admission. Most patients admitted to ICU with decompensated liver cirrhosis, as their main problem, died; no patients with liver cirrhosis died in ICU if their primary reason for admission was not related to liver cirrhosis. Outcomes from our ICU are similar to the literature. It is likely we have under-estimated mortality because follow-up was less than 1 year in most cases.
We recommend that patients with liver cirrhosis should be assessed on an individual basis and be considered for ICU admission if there is a potentially reversible cause for their clinical presentation.
We advise ward-based teams have discussions with regional specialist centres at an early stage to assess whether an episode of decompensation is potentially reversible (e.g. Transjugular Intrahepatic Portosystemic Shunt or liver transplant). Daily consultant reviews of patients could avoid late referrals, improve the rate of timely interventions and may avoid the need for critical care.
0273
Case Report: An Overdose of Melanotan 2 – the Barbie Drug
Emily Gibney and Emma Findlay
St Helens and Knowsley Teaching Hospitals NHS Trust, Whiston, United Kingdom
Abstract
Background: We present a case of accidental Melanotan 2 overdose. Melanotan 2 is an illegal injectable drug consisting of an Alpha Melanocyte Stimulating Hormone analogue used to increase tanning and sexual performance, and known colloquially as the Barbie Drug. Currently the evidence base for management of Melanotan 2 overdose is limited to several case reports and animal studies.
Case Presentation: This is a case of a 38-year-old woman with a history of Anxiety, PTSD and chronic pain who presented two hours post accidental overdose of Melanotan 2. She had intended to take 0.1 ml of a 10 mg/ml solution, however had given herself 1 ml (10 mg). On admission, she was hypertensive (BP 157/89), vomiting, tachycardic (120bpm), diaphoretic and anxious. She was also experiencing profound muscle spasms which had not responded to initial simple analgesia. After she failed to respond to significant doses of opiate and benzodiazepine we consulted both Toxbase and the National Poisons service and adopted a multimodal approach to management including opiates, high dose benzodiapines and ketamine. This case was complicated by the fact that the patient, diagnosed with chronic back pain, took significant doses of long and short acting opiates daily to manage her pain. The patient was admitted to Intensive Care overnight for observation and discharged home the following day. There is a limited evidence base for managing these cases however case reports suggest sympathomimetic symptoms (1) including those experienced by our patient and priapism (2), with extreme cases developing raised Creatinine Kinase levels and Rhabdomyolysis (2).
Conclusions: In this case we discuss the use of polypharmacy in the approach to managing severe acute pain and muscle spasms, particularly with regard to chronic pain patients. Melanotan 2 is an illegal drug which requires the user to mix, draw and dose themselves correctly, with limited instruction and with increasingly common use it can be expected that more cases of toxicity will be seen. Therefore, understanding different possible approaches to management is required.
0274
International Questionnaire: Nutritional and intensive care management in specialized burns unit
asako shida1,2,3, Vasiliki Kalogianni4, Omar Zakieh4, Sundhiya Mandalia2 and Marcela Vizcaychipi1,2,3
1Imperial College London, London, United Kingdom
2Chelsea & Westminster Hospital NHS Trust, Chelsea, United Kingdom
3Imperial School of Anaesthesia, London, United Kingdom
4Medical Student, Imperial College London, London, United Kingdom
Abstract
Introduction: Over ninty percent of burns injuries occur in developing countries. (1,2)Severe burns injuries require multiple surgical input over a long period. The nature of severe burns injuries is known to compromise victims’ physiology, often requiring intensive care treatment. Inability to provide adequate care can increase the case fatality. Not only are increased manpower and expensive equipment required to provide adequate care, but the management of catabolism can be challenging in any care setting. There is little evidence of variation in nutritional management across different countries.
Objectives: The purpose of this study was to ascertain burns-related nutritional management and to describe differences in intensive care facilities between the: high; high-middle; low-middle; and low- income countries.
Methods: Using an online platform Qualtrics, 42 questions were set up and sent to health care professionals working with burns. The questions focused on demographics, whether intensive care facilities were available and if available how nutrition was managed. Contact details were obtained from conferences, published papers, charities, burns associations, non-governmental organisations and hospital websites. Participants were classified according to the countries’ income status, defined by World Bank data.(3)In total, 3380 emails were sent and 44 phone calls were made. Statistical analysis was completed using software GRAPHPAD.
Results: A total of 103 responses was obtained. 72 responses from high-income countries, 12 responses from high middle-income countries, 14 from low middle-income countries and 5 responses from low-income countries. The response rate was lower in low-income group for multiple reasons: difficulty identifying burns unit, no access to contact details and language barrier. High-income countries were more likely to have the following to compared to low-income countries: Specialized burns units (92% versus 60%), intensive care units (94% versus 80%), have less shortages of beds (1.17 beds / month versus 51 beds / month), more likely to have dieticians (72% versus 40%), and have access to indirect calorimetry (43% versus 0%).
The use of Nasogastric tubes were similar across all 4 groups. However, the availability of nutritional supplements differed hugely: 80% of responses from low-income countries lacked nutritional supplements versus 10% in high-income countries. One hospital from Nepal uses boiled eggs as the source of protein. 76% of high-income countries use estimated equations to feed patients whereas only 20 % do so in low income countries. Centres from high-income countries uses Harris Benedict (3%), Schofield (16%) and Currei (16%) formulas whereas no response was obtained from low-income countries.
Conclusions: Our survey has identified important obstacles in managing burns patients and difference in how burns patients are managed arising from the income status of the country. We found that low income countries have shortages of staff, equipment, facilities, specialised burns unit and medicines to manage patients’ nutritional status. Given that severe burns patients require timely initiation of debridement, pain control, control of sepsis, careful nutritional input and fluid administration, findings from this study may reflect a substantial clinical risk to poorer income countries. Reducing the barrier to care may help improve the outcome of burns injuries.
0275
A Multidisciplinary Team (MDT) Approach to Rehabilitating a Patient with an Impella Device- Case Study
Katherine Atkin, Jo-Anne Fowles and Marius Berman
Royal Papworth NHS Foundation Trust, Cambridge, United Kingdom
Abstract
Background: The Impella, a percutaneous left ventricular assist device, is increasingly used to support patients with severe heart failure, cardiogenic shock, and during high-risk Percutaneous Coronary Interventions. This case describes the first experience of rehabilitating a patient with an Impella at Royal Papworth Hospital NHS Foundation Trust.
Due to the specialist nature of the Impella there was a lack of evidence to guide the Physiotherapists and the MDT in the rehabilitation of the patient. This case study will outline the management strategies used by the MDT in the rehabilitation of the patient.
Case Presentation: The case study focuses on a 29 year old patient transferred for ongoing management of heart failure post myocardial infarction. The patient arrived on peripheral Veno-Arterial Extra Corporeal Membrane Oxygenation, support was then converted to the Impella to allow rehabilitation to begin.
As the Impella is a new device on our Critical Care unit and to ensure safety and build confidence, teaching sessions were provided by the senior nursing and education team. This took the form of practical teaching sessions and online tutorials. Until a clear teaching plan was established for the Physiotherapy team treatment sessions were led by senior Physiotherapists with junior staff assisting to gain knowledge and experience.
Initiation and progression of rehabilitation was a collaborative process between the Consultant Intensivists, Surgeons, Cardiologists, Physiotherapists and Specialist Nurses, ensuring patient safety and delivery of excellent patient care. Family involvement was encouraged and utilised throughout all rehabilitation to comfort the patient. A variety of rehabilitation modalities were used and supported by regular goal setting, maintaining a rehabilitation diary and the use of the Chelsea Critical Care Physical Assessment Tool (CPAx). Patient involvement in planning the day’s activities ensured a coordinated approach to all sessions and had positive impact on rehabilitation. Rehabilitation did not solely focus on physical strength and function. In the initial stages as the patient was intermittently delirious, sessions focused on reorientation including positioning the patient to face the window during the day together with setting and following daily plans.
No adverse events were reported during rehabilitation. Rehabilitation was not undertaken on two days due to the patient being re-intubated and was limited on one day due to the patient experiencing epistaxis and bleeding from a leg wound. Over the weekend, rehabilitation was led by the nursing team and Physiotherapy assistant practitioners.
The patient participated in daily/twice daily rehabilitation sessions for seven days whilst supported on the Impella and showed anecdotal evidence of improvement. This included increased physical strength and function, with a CPAx score increasing from nine to twenty two, improved respiratory function weaning to room air and increased cough strength. Her delirium resolved with increased engagement with her family and participation in decision making about her own rehabilitation and care.
Conclusion: This case study demonstrates that with the involvement of the MDT it is safe, feasible and beneficial for patients to rehabilitate whilst supported on the Impella.
0276
Stop the Splash: A multi-disciplinary, multi-cycle, multi-site qualitatively driven quality improvement programme
Nicholas Plummer, Liz Barley, Tom Beadman and Gareth Gibbon
Nottingham University Hospitals NHS Trust, Nottingham, United Kingdom
Abstract
Introduction: Up to a quarter of critcally ill patients carry blood-born viruses (BBVs),1 and over 50% of operations result in splashes to the face.2 As hepatitis and HIV can be transmitted through splashes to mucous membranes3 this suggests that splash injuries are an underappreciated risk for transmission of BBVs in critical care.
Background: Across three critical care areas, spread over two hospital sites, 23 splash injuries were reported over two year. Anecdotal evidence suggested that this was both significantly under-reported, and that team members didn’t feel equipment to avoid it was universally available. An audit as a result of this showed that appropriate PPE was not uniformly available at all bed spaces.
Methods:
1. Structured interviews utilising Critical Decision Making methodology4 were undertaken to understand team members’ feelings towards the risks of splash injury, use of PPE, and barriers to its implementation. This informed our intervention design (personal issue face protection and top-down education).
2. Six months later a further round of interviews were held to understand how and why culture across the units had changed, leading to a second intervention focussed on peer-to-peer education.
3. Subsequent interviews at six months were performed, with a view to design a further intervention cycle.
Results: We initially interviewed 4 junior doctors, 9 nurses, and 3 AHPs. The key themes identified were:
• Splashes are under-reported (61%), and as a team it is felt we are not doing enough to prevent them (75%)
• Staff don’t appreciate the risks of transmission of BBVs, and would change behaviour if a patient was known to have a BBV.
• The major barrier to use is the time and effort to find and apply PPE.
• There are cultural barriers to face and eye protection within Western society, and that masks can impair communication.
• Mandating PPE could be interpreted as a slight on professionals’ decision making.
• Potential solutions include personal issue PPE, increased bed-space availability, and a “grass-roots” education drive while simultaneously addressing our unit culture to “normalise” the use of PPE.
After introduction of face protection, 39% of staff had face protection imediately available when interviewed. Awareness of the campaign was 71%, with 73% aware of the key themes of the intervention. There was found to be a significant difference between units as to perception of risk (85% vs72% vs 61%, p = 0.001).
Following peer-to-peer education, 98% were aware of the campaign, and 85% aware of the key themes. Barriers were identified in availability of and damage to face protection immediately at the bed space, and a lack of uptake by clinical and nursing leadership.
Conclusions: Qualitative methodology is a powerful tool in quality improvement to understand how and why interventions do and don’t succeed. Solutions in QI often appear superficially simple, but qualitative explorations can reveal complex cultural and psychological reasons for their failure requiring an adjusted, itterative approach to QI. Driving cultural change by empowering and educating staff responsible for making the change is critical in sustainably improving standards, yet is an under-appreciated aspect of most QIPs.
0277
Quality Improvement Project to Improve Documentation of Predicted Body Weight and Ideal Tidal Volume on the Intensive Care Unit Admission Pro Forma
Zoe Syrimi, Eleanor Tanqueray and Anthony Cochrane
St Helens and Knowsley Teaching Hospitals NHS Trust, Liverpool, United Kingdom
Abstract
Introduction: In patients with acute lung injury or acute respiratory distress syndrome, there is a significantly lower mortality when ventilated with a lower tidal volume (TV) of 6 ml per kg of predicted body weight (PBW) than the traditional TV of 12 ml per kg of PBW.1
In our Intensive Care Unit (ICU), it was noticed that height, PBW and ideal TV were often not being documented on the admission pro forma. There was a guide attached to every ventilator which could be used to aid calculation of ideal TV, however this was not easy to use, requiring multiple conversions between units.
Objective: To improve documentation rates of height, PBW and ideal TV on the ICU admission pro forma.
Methods: All patients that were invasively ventilated at admission were included in the study. Baseline data was obtained from admissions during a 6-week period in August-September 2018. In the first cycle of change, we designed a guide that made estimating height and PBW from ulnar length and then calculation of ideal TV much simpler. This new guide was then attached to every ventilator. Documentation rates were then re-audited during another 6-week period in October-November 2018. In the second cycle of change, tape measures were added to admission packs for convenient measurement of ulnar length. At doctors’ induction, information was given on how to use the new guide and a reminder email was sent out soon afterwards. Documentation rates were then re-audited during another 6-week period in April-May 2019.
Results: At baseline (n = 19), height, PBW and ideal TV documentation rates were 26%, 21% and 26% respectively. After the new guide was attached to ventilators (n = 36), documentation rates were 22%, 25% and 17% respectively. After the addition of tape measures to the admission packs and publicising the new guide (n = 43), documentation rates were 48%, 52% and 56% respectively. There were statistically significant improvements in documentation rates of PBW (X2 = 5.10, p = 0.02) and ideal TV (X2 = 4.68, p = 0.03) after the second cycle of change.
Conclusion: Documentation of PBW and ideal TV on the admission pro forma of invasively ventilated patients improved significantly after the second cycle of change. Before publicising the new guide and explanation of how to use it, there were insignificant changes in documentation rates. This demonstrates the importance of ensuring that people involved in the change process are well informed, understand the need for implementing change and the benefits to patient outcome.
Despite the improvement made, still only just over half of patients being invasively ventilated had their ideal TV documented on their admission pro forma, indicating the need for ongoing improvement. As a result, work has been done to formalise the process of introducing the guide during doctors’ induction, to ensure all doctors new to the unit are informed about the importance of documenting height, PBW and ideal TV.
0278
Palliative Care in the Critical Care
David Harvie1, Robert Chambers1 and Carol Davis2
1University Hospital Southampton NHS Foundation Trust, Southampton, United Kingdom
2University Hospital Southampton, Southampton, United Kingdom
Abstract
Introduction: Recent ICNARC data states there's a 14%(21,950patients) unadjusted mortality in UK critical care units (1). As Intensive Care Physicians our role in the patients' death and their families experience is vital. This is recognised by the Faculty of Intensive Care Medicines Critical Futures Initiative, having recently setup an ‘End of Life Working Party (EoLWP), addressing areas faced by the critical care team. (2)
However, there is recognition of the requirements for Palliative Care to be integrated into the Intensive Care curriculum by FICM and is a core competency. How that education is met can be variable.
At present there is little formalised education, three models for incorporating palliative care in the ICU have beenproposed: the integrative model (education in primary
palliative care skills for ICU clinicians); the consultative model (access to palliative care specialists); and the mixed model that uses both of these approaches simultaneously. (4,5)
There is emerging evidence to re-enforce the usefulness of palliative care education within the ICU, Saft et al, showed the quality of palliative care training in critical care medicine programs and the use of bedside tools were independently associated with reduced ICU use at the end-of-life. (6)
Objectives: To gain insight into the prevalence of Palliative Care in Intensive Care Units around Wessex, the education received and the desire to engage in more training.
Method: We surveyed ICM trainees in the region about aspects of palliative care in the ICU. A nine-question anonymised survey focusing on;
1. Exposure to Palliative Care in ICU.
2. Training received in Palliative care.
3. What education in palliative care would be desired.
Results: We had 23respondents of the 32 ICM trainees in Wessex with two trainees out-of-training when the survey was undertaken. A had response rate of 72%
Nearly 70% of respondents had provided palliative care to greater that 5patients in ICU over the last year (see Fig 1.)
Over 60% of respondents felt they had not received an appropriate amount of training in palliative care for their level of ICU training. Over 85% of respondents felt it is the role of ICU to provide palliative care for patients, it is unsurprising that nearly 75% of respondents wanted more formalised palliative care teaching (Fig 2).
Conclusion: Trainees in the region currently have a lot of exposure to patients with palliative care needs.
There was a strong feeling amongst trainee that palliative care is part of ICU’s role, this was reflected in the desire for more training. In what form of training was more variable, but most respondents opted for regional level teaching with some interest in a fellowship or short placement in palliative care.
Improving the palliative care we provide, has the potential to reduce ICU length-of-stay and improve the relatives experience.
Implementation of a regional education programme for palliative care is now in place. We want to see if the results in the Wessex region are reflected nationally; potential to develop a palliative care placement/fellowship for ICM training.
Figure 1.
Respondents exposure to palliative care on the ICU.
Figure 2.
Desire for formalised training in palliative care.
0279
An audit of oxygen prescription and management of hyperoxia in out of hospital cardiac arrest patients on a cardiac ICU
Sophie Risbridger1, Mairi Hollows1, Adrian Mellor2 and Jonathan Brand2
1Newcastle University Medical School, Newcastle upon Tyne, United Kingdom
2James Cook University hospital, Middlesbrough, United Kingdom
Abstract
Introduction: Research suggests hyperoxia is harmful to patients following cardiac arrest and increases mortality (1). Hyperoxia is a non-physiological event and has been shown to produce radical oxygen species which damage tissues through cellular apoptosis, stimulate inflammatory responses in the lungs, and reduce capillary perfusion (2).
National British Thoracic Society (BTS) guidelines (3) state that all patients should have oxygen prescribed to target ranges, rather than a concentration of oxygen or FiO2, and to appropriate saturations for their hypercapnia risk.
Objectives: To compare our practice against current BTS guidelines (3) for oxygen prescription in the acutely ill patient. Target saturations should be written in the daily plans on CICU charts, and appropriate for the patient’s hypercapnic risk status.
To establish a baseline to identify how many OOHCA patients are hyperoxic on admission to CICU.
To establish whether normoxia can be reached within 24 of admission.
Methods: Collection of CICU patient charts for the previous 18 months of any patient recorded as having an OOHCA. Recording of demographics, co-morbidities, time of admission, and oxygen target saturations. Then collecting the data on oxygen delivery device, FiO2, SaO2, and PaO2 every 6 hours from admission to 72 hours.
SaO2 hyperoxic defined at >97%, normoxia as 95–97%, hypoxia as <95%. PaO2 severely hyperoxic as >39kpa, moderately hyperoxic as 13.5-39kpa, normoxic as 8–13.5kpa, and hypoxic as <8kpa. Normoxia recorded if 3 consecutive results are within the normoxia range, with the earliest normal value recorded as time achieved.
Results: A total of 34 charts were identified for the 18 month period, four were unavailable. It was found that none of these charts had target oxygen saturations written in the daily plans, making it impossible to determine if they were appropriate for the patient’s risk status.
All patients had been admitted to CICU following OOHCA. All had been intubated and ventilated on arrival. Only 20% (n = 12) achieved normoxia in either category within 24 hours of admission. One patient achieved normoxia in both categories. All the patients who were at risk of hypercapnic respiratory failure ended the 72-hour period hyperoxic in either or both SaO2 and PaO2.
Conclusions: Patient saturations tended to be titrated to the upper limits of normoxia or to moderate hyperoxia. To improve patient outcomes, a consensus should be made among CICU consultants about acceptable oxygen levels and frequency of saturation target setting for their unique patient group.
Very few patients ever achieved normoxia. This could be attributed to the lack of target saturations, meaning FiO2 is titrated to limit hypoxia without considering hyperoxia.
Limitations: Retrospective review meant that not all charts were available at the time of audit.
| Admission Saturations | Patients %(n) | Normoxic Within 24 Hours %(n) | Never Achieving Normoxia %(n) | |
|---|---|---|---|---|
| SaO2 | >97% (Hyperoxic) | 65.5 (19) | 10.2 (2) | 63.2 (12) |
| 95-97% (Normoxic) | 20.7 (6) | |||
| <94% (Hypoxic) | 13.8 (4) | 75 (3) | 25 (1) | |
| PaO2 | >39kpa (Severely Hyperoxic) | 6.7 (2) | 50 (1) | 50 (1) |
| 13.6-39kpa (Moderately Hyperoxic) | 66.7 (20) | 30 (6) | 55 (11) | |
| 8-13.5kpa (Normoxic) | 20 (6) | |||
| <8kpa (Hypoxic) | 6.7 (2) | 0 (0) | 100 (2) |
0280
What are the Barriers and Enablers towards Implementing the Sepsis Six care bundle within NHS hospitals? BLISS-2: A multi-center study using the Theoretical Domains Framework
Guy Hooper1, Neil Roberts1, Fabiana Lorencatto2, Adam Pollard3, Micheal Spivey3, Wendell Storr3, Deborah Webster1, Alan Eccles4, George Ramsay5, Jan Jansen6, Ruth Thomas7, Helen Bounds7, Micheal Eddie7, Stephen Knight8, Robert Pearson8, James Ng8, Theresa Weldring9, Sandra Courtiour10, Laura Smith10, Nicola DeVeaux11 and Biju Cherian12
1University of Plymouth Hospitals Trust, Plymouth, United Kingdom
2Centre for Behaviour Change, University College London, London, United Kingdom
3Royal Cornwall Hospitals NHS Trust, Truro, United Kingdom
4Torbay and South Devon NHS Foundation Trust, Torquay, United Kingdom
5Raigmore Hospital, Inverness, United Kingdom
6University of Alabama School of Medicine, Birmingham, The United States of America
7Dorset County Hospital, Dorchester, United Kingdom
8Monklands General Hospital, Airdrie, United Kingdom
9Kingston Hospital, London, United Kingdom
10Poole Hospital, Poole, United Kingdom
11Great Western Hospitals NHS Trust, Swindon, United Kingdom
12Hull Royal Infirmary, Hull, United Kingdom
Abstract
Introduction: As part of an ongoing drive to improve sepsis care, the ‘Sepsis Six’ care bundle is a package of simple measures that should be undertaken in a timely manner in septic patients. Performance has been variable. Better targeting of important factors affecting performance could improve this. Previous research has used implementation methodology to identify these in single sites.
Objectives: This study uses a previously validated Theoretical Domains Framework (TDF)-based questionnaire to identify important barriers and enablers towards Sepsis Six performance and to assess the generalizability of previous single center results across a national sample.
Methods: Structured, TDF-based questionnaire with 54 relevant belief statements was circulated to all nurses, consultants and junior doctors in medical and surgical admissions and emergency departments at ten UK hospitals. Likert scales were used to score each statement for importance and for agreement (in order to score as a barrier or an enabler). Results were analyzed across participant groups and individual hospitals as well as overall. Graphical methods were used to identify discordant beliefs particularly relevant for behavior change. Logistic regression was used to identify beliefs showing significant differences between participant groups in order to identify high value beliefs important to all.
Results: 616 questionnaire responses were received from 10 hospitals. (216 from ED, 214 from MAU, 186 from SAU, 99 Consultants, 244 junior doctors, 273 nurses). Response rate was variable, as was the participant split across hospitals.
Important barriers included lack of sufficient staffing, time or beds available to look after septic patients. Important enablers included having the knowledge and skills to perform the Sepsis Six, having enough equipment, believing it positively affects outcome, and believing it to be part of the participant’s role to identify sepsis and perform the bundle. Most of these were consistently important across all hospitals and participant groups, though there was often significant variation in agreement scores, with some hospitals having a belief as more of a barrier or enabler than others. There were significant differences in average scores given by different participant groups for both agreement and importance, though this did not affect which beliefs were most important.
Conclusions: National interventions to improve Sepsis Six performance should focus on addressing resource shortages, maintaining skills and knowledge, maintaining beliefs of beneficial effect and maintaining ‘it’s my role to do this’ as a core belief. Given identified differences between participant groups, individual hospitals and departments should supplement this with their own improvement processes to identify particular high value barriers or enablers for behavior change interventions.
0281
An Audit of Anti-Psychotic use on a General Adult Intensive Care Unit
Camilla E. St. A. Jackson and Elaine Armstrong
John Radcliffe Hospital, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Abstract
Introduction: The use of anti-psychotics on the Intensive Care Unit (ICU) as pharmacological management of delirium is well established despite the potential, particularly cardiac, side-effects in the critically ill. Recent evidence suggests that anti-psychotics ‘do not significantly alter the duration of delirium’ (1). Coupled with their side-effect profile this suggests they may not be the most suitable drug of choice. Historically, anti-psychotics were widely prescribed in our ICU, and outpatient follow-up clinics demonstrated these were often continued post-discharge without a clear indication. Anti-psychotic prescribing practice had not been formally reviewed in our ICU before.
Objectives: The audit objectives were to characterise current anti-psychotic prescribing in our ICU including: patient groups requiring anti-psychotics, drugs used, indication and if they were continued on discharge from ICU and from hospital. The aim was to use this to guide further prescribing practices.
Methods: Drug charts of all patients discharged from the John Radcliffe and Churchill Hospital Adult ICUs from 01.08.2018 to 31.01.2019 inclusive were reviewed for the presence of an anti-psychotic prescription. Anti-psychotics were defined as per the British National Formulary. For those prescribed an anti-psychotic, the patient demographics were recorded: age, reason for admission, length of stay, 30-day mortality and mortality on discharge from ICU and hospital. The indication for the prescription, drug used, whether the drug was stopped on discharge from ICU or from hospital were also recorded.
Inclusion Criteria: All General Adult ICU discharges 01.08.2018 to 21.01.2019 inclusive
Exclusion Criteria: Paediatric cases, drugs prescribed but never given.
Results: Of 747 patients discharged over six months, 89 were prescribed anti-psychotics during their ICU stay = 11.9%.
Demographics of those receiving anti-psychotics: Mean Age = 59.1 years (17–89), Mean length of stay =9.97 days, Mortality on discharge from ICU = 12.4%, discharge from hospital = 23.6% and at 30 days = 23.6%.
Reasons for admissions were widespread. Sepsis, trauma and general surgical emergencies were the top three causes.
Most common indications for prescription were delirium (28/89), agitation (21/89) and established psychiatric diagnosis (15/89). No indication was recorded in 15/89 cases.
The most common anti-psychotics prescribed were: haloperidol and olanzapaine.
67/89 patients had a single agent prescribed, 22/89 had two agents. No patients were prescribed more than two agents.
In 31/89 cases the anti-psychotic was continued on discharge from ICU to the ward. In fifteen cases the drug was continued on discharge home. Twelve cases were the continuation of a regular anti-psychotic prescription whilst three cases (3.4%) were a new prescription. One was an anti-emetics, one had a clear plan to stop and the thrid case was for nocturnal delirium.
Conclusions: Anti-psychotics are prescribed in 11.9% of patients in our Adult ICU. Anti-psychotics commenced in ICU are continued on discharge home in 3.4% of cases. This audit will be repeated to see if practice changes following recent published data.
0283
Cerebral edema during correction of hyperglycaemic crises
Sumit Kumar, Bhuvanshyam Bhaktavatsalam and Venkat Sundaram
Glan Clwyd Hospital, Rhyl, United Kingdom
Abstract
Background: Hyperosmolar Hyperglycaemic State (HHS), a diabetic emergency, typically occurs in elderly and is seen to be commonly precipitated by infections or missed insulin doses. HHS in comparison to DKA, presents over a number of days resulting in excessive dehydration and electrolyte imbalances. The name changed from HONK (Hyperosmolar non ketotic coma) is due to the fact that some patients may be extremely ill but not comatose and may also be acidotic. Delayed presentation and serious metabolic derangements necessitate early diagnosis and treatment. Neurological complications including cerebral oedema and cerebral pontine myelinolysis have been identified rare but potentially fatal.
Case Presentation: A 68-year-old gentleman, known case of type 2 diabetes on treatment, had presented with recurrent vomitings after feeling unwell for few days. It was found that his therapy was recently modified as he developed complications with metformin and gliclazide. He had a past history of bladder cancer repaired surgically six months back along with bladder and bowel stoma. In ED, he was febrile with extreme hyperglycaemia and dehydration. He was commenced on Tazocin, HHS resuscitation regimen which included IV Insulin, potassium replacement. HDU admission was sought and upon arrival he was already showing drop in blood pressure, hypernatremia and high serum osmolality. After 48 hrs of HDU admission his blood cultures showed gram negative rods and biochemically he had renal and hepatic function decline, thrombocytopenia and hyperchloraemic acidosis. He exhibited signs of cerebral irritation ie confusion, agitation and was then intubated and cerebral protective measures were followed. His therapy was aimed to maintain normal serum osmolality and manage sepsis. He started to show improvement to therapy after 3 days of ITU admission and we were able to extubate him next day. He showed significant metabolic improvement and started taking orally. He was then shifted to ward for further treatment.
Conclusion: HHS is a serious medical emergency which requires a prompt recognition and management. Although more common in Type 2 Diabetes Mellitus, there is increasing evidence that it may manifest in young Type 1 Diabetes mellitus patients.1 The patient is at risk of life threatening complications and out of these, Cerebral oedema is invariably fatal unless detected timely.3 Early recognition of neurological deterioration is hence of prime importance.
0284
Unit-acquired blood stream infections: An incomparable comparator?
Nicholas Plummer and David Sperry
Nottingham University Hospitals NHS Trust, Nottingam, United Kingdom
Abstract
Introduction: Nottingham University Hospitals (NUH) has three critical care units spread across two sites. The adult intensive care unit (AICU) at Queen’s Medical Centre (QMC) was a significant outlier (>3 SD) for unit-acquired infections (UAI) in the ICNARC 2017–2018 annual quality report, whereas the other two units were closer to comparators. This was a deterioration compared to 2016–2017 (2-3 SD).
Background: As the regional tertiary referral centre and major trauma centre, AICU at QMC predominantly receives neurosurgical, trauma, and complex hepatobiliary patients when compared to the other two units, and the number of such cases is increasing yearly. As such the patient population disproportionately reflects patients with intracranial, spinal, and complex intraabdominal pathologies. We investigated the impact of these patient populations on rates of UAI.
Method: All patients admitted to the April 2017 to August 2018 were reviewed alongside blood culture results.
Results: 1039 patients were admitted for >48 hours. 135 patients (13.0%) had 184 blood stream infections (BSI), of which 150 were UAI by ICNARC criteria (acquired after 48 hours). 32 patients (3.1%) had >1 infection, and 4 (0.4%) had >3 (all long-stay pancreatitis patients, with 18 BSI between them). There was a strong link between length of stay and rate of BSI. Patients staying <1 week had a 1:18 BSI rate, whereas patients staying longer than 1 week (418 patients, 40.2%) had a 1:8.5 rate of BSI. Patients staying longer than 3 weeks had a BSI rate of 1:2.7.
22 patients (36 BSI) had culture or radiological evidence of an intra-abdominal source. Many were in long stay patients, particularly pancreatitis (8) or intra-abdominal vascular disease. BSI either arose early (week 1) or late (week 4).
66 patients (89 BSI) had culture or radiological evidence of a pulmonary source. All but 15 patients were admitted with community acquired pneumonia, intracranial pathology (primary or traumatic), following spinal injury, or following cardiac arrest. BSI occurred predominantly within the first two weeks, suggesting that patients with intracranial pathology are being admitted with a high risk of early severe pneumonia leading to BSI.
Patients with BSI did not have an excess mortality against predicted.
Conclusions: As neurological injuries and severe trauma are bypassing other hospitals in our region, and complex HPB is being referred in through a functional network plan, we have two patient groups in AICU with a disproportionately high susceptibility to infection. This makes our outlier status for UAI likely to continue.
Although ICNARC “strongly discourages use of these results to create rankings or league tables”, standards measured in quality reports are used by clinicians and non-clinicians to rate the standard of individual units. In this case, we feel that UAIs poorly reflect the quality of care delivered, and instead reflect the increasingly homogeneous patient population of a tertiary referral centre in the context of increasing centralisation of services. Alternative measures and comparators should be sought to account for this.
0285
Source of Infection is associated with mortality in patients with septic shock – a retrospective cohort study
Dr Minesh Chotalia1,2, Mansoor Bangash1,2, Tracie Matthews1,2, Dhruv Parekh1,2 and Jaimin Patel1,2
1University of Birmingham, Birmingham, United Kingdom
2University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Sepsis is defined as an abnormal host response to infection causing life threatening organ dysfunction.1 Site of infection may alter site and degree of organ dysfunction and thus outcomes from septic shock.2
Objective: To determine the association between source of infection and 90-day mortality in patients with septic shock.
Methods: Patients admitted with a diagnosis of septic shock (Sepsis 3) between April 2016 and July 2019 to the Queen Elizabeth Hospital, Birmingham were included. Patient data was retrieved using electronic patient records. The primary outcome was all cause 90-day mortality. Secondary outcomes included need for invasive ventilation, advanced vasopressor support (defined as needing 2 or more vasopressors at the same time-point) and renal replacement therapy (RRT). Continuous data are presented as mean (SD). Categorical data were analysed using a chi-squared test.
Results: 878 patients were admitted to ITU with septic shock. Most patients were male (60%) with a mean age of 60.6 ± 1.9 years and APACHE II of 20.6 ± 0.7. Mean ITU length of stay was 14.3 ± 2 days and 90-day mortality was 39%. Sources of septic shock were as follows: 43% respiratory, 22% gastro-intestinal (GI), 9% hepato-pancreato-biliary (HPB), 8% urinary/renal, 6% skin/soft tissue and 11% other. Respiratory infections were the commonest with a significantly higher 90-day mortality (46% vs 36%, p = 0.01) compared to the remainder of the cohort. This subgroup also had a greater need for invasive ventilation (83% vs 70%, p < 0.0001) and advanced vasopressor support (73% vs 63%, p < 0.0001) but unexpectedly, a lower need for RRT (12% vs 17%, p = 0.003). Urinary/renal infections, in direct contrast, had a significantly lower 90-day mortality (24% vs 40%, p = 0.01) in comparison to the remaining population. This correlated with a lower need for invasive ventilation (47% vs 72%, p = 0.0003) and advanced vasopressor support (42% vs 64%, p = 0.0002), but a higher need for RRT (36.4% vs 16%, p < 0.0001). HPB infections had the highest mortality (51% vs 38% p = 0.03) but were less common and had no difference in other outcomes. All other infection subgroups analysed had no difference in 90-day mortality or other outcomes when compared to the remaining cohort. Furthermore, there was no difference in age or APACHE II score between infection subgroups.
Conclusions: Anatomic source of infection altered mortality and important patient outcomes such as need for invasive ventilation, advanced vasopressor support and RRT. Given the observed differences, the pathophysiology of septic shock, and thus the success of treatments attempting to counter it, may vary according to site of infection. This is often neglected in trial design and analysis.
0286
Prevalance and Predictors of Critical Care Use Across Scotland at the End of Life
Nazir Lone1, Jonny Mayes2 and Natalie Pattison3
1University Dept of Anaesthetics, Critical Care and Pain Medicine, University of Edinburgh, Edinburgh, United Kingdom
2University of Edinburgh, Edinburgh, United Kingdom
3University of Hertfordshire, Hertfordshire, United Kingdom
Abstract
Background: Internationally there is variation in critical care use at the end of life from 8.2% in Germany to 40% in the USA.1 Understanding the demographics of patients using critical care at the end-of-life (EoL) is an essential step before further research can be undertaken. These are currently unknown in Scotland and the rest of the UK.
Objectives:
1. To describe the prevalence of critical care use during 30-day, 180-day and 1-year periods before death stratified by age, sex and socioeconomic status
2. To identify predictors of critical care use in the 30-days prior to death
Methods: This was a cohort study of decedents. It included residents ≥16 years old who died in Scotland from 2005 to 2017. National Records Scotland Death Records identified all deaths in Scotland. This was linked to the Scottish Intensive Care Society Audit Group (SICSAG) database. Chi-squared tests were used to test for significance across stratification variables. Univariable/multivariable binary logistic regression identified predictors of EoL critical care use. Odds ratios (95%CI) were calculated relative to the youngest age group (16-30 y), the most socioeconomically deprived group, female sex and, for cause of death, relative to cancer.
Results: There were 710,829 deaths of Scottish residents between 2005–2017 in Scotland. 55,087 (7.7%) patients were admitted to Critical Care (ICU or HDU) within the 30 d prior death, 72,509 (10.2%) in the 180 d prior and 83,213 (11.7%) within 365 d.
Those aged 40–50 y had the highest proportion of critical care use within 30 d of death (15.2%), followed by 30–40 y (14.8%). The lowest was 90–115 y (1.1%). Within 365 d of death, 40–50 y had the highest EoL use (21.6%), followed by 50–60 y (20.9%). Men vs women had higher EoL critical care use within 30 d (8.7% vs 6.9% p < 0.01), 180 d (11.5% vs 9.0% p < 0.01) and 365 d (13.2% vs 10.3% p < 0.01). Prevalence of critical care use increased with increasing social deprivation (8.7% vs 6.6% most vs least deprived, p < 0.01).
Univariable analysis suggested predictive factors of 30 d EoL critical care use included being male (OR 1.32 95% CI 1.29,1.35), lower socio-economic group (Most Deprived OR 1.35 95% CI 1.31,1.39), and being aged 40–50 y (OR 1.11 95% CI 1.03,1.19). On multivariable analysis, male sex was no longer predictive (OR 0.99 95% CI 0.96,1.01). Those aged 50–60 demonstrated the highest risk of end-of-life critical care use (OR 1.35 95% CI 1.25,1.45). The least socially deprived group now had the highest risk (OR 1.10 CI 1.06,1.13). Causes of death associated with highest use were liver disease (OR 6.43, 95% CI 6.15,6.72), accidents (OR 4.96, 95% CI 4.69,5.25), and respiratory disease (OR 4.32, 95% CI 4.18,4.45). Causes with lowest use included dementia (OR 0.18, 95% CI 0.16,0.21).
Conclusion: In the general population for those aged 16–60, 1 in 7 people will be admitted to critical care within 30 days of death. Training clinicians in managing patients and bereaved families is crucial. Identifying predictive factors of death in critical care may help to guide which patients and families may need support.
0287
Understanding the sympathetic storm and it's impact on apoptosis in an organotypic rat ex-vivo hippocampal slice model
Nick Talbot1,2, Amrita Bansal3, Hannah Botfield1 and Tonny Veenith2,3
1Institute of Inflammation and Ageing, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
3University of Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Following traumatic brain injury (TBI) two cellular injury patterns are present. Primary injury results in necrosis, whilst secondary injury leads to an apoptotic pattern. Selective neuronal loss can be driven by sympathetic hyperactivity. Observational studies demonstrate early administration of beta-blockers result in improved patient survival. Beta-blockers demonstrate anti-apoptotic effects in the heart and kidneys, and recent evidence suggests an anti-apoptotic action in the brain. Propranolol, a non-selective β-adrenoceptor antagonist inhibits cytochrome-c release from isolated rat brain mitochondria. Hippocampal slice culture provides a controlled organotypic environment in which to determine if catecholamine induced neurotoxicity can be ameliorated by beta-blockers.
Objectives: To assess whether beta-blockers can ameliorate catecholamine excess and reduce apoptotic cell loss in an ex-vivo brain tissue model.
Methods: Male Sprague-Dawley rats were culled using a rising concentration of carbon dioxide. The brains were removed, cerebella excised, and the cerebral hemispheres divided. The hippocampus was isolated using blunt dissection and divided into 250 µm slices. Slices were cultured on sterile 0.4 µm Millicell micropore membrane in 1 mL of supplemented neurobasal A medium. On day 3 the slices underwent complete media change and each well was dosed as below. On day 5 the slices were stained with Nucview 488 caspase-3 substrate, a cell membrane permeable fluorescent marker which labels cells undergoing caspase-3 mediated apoptosis.
Results: Cell survival is presented as a percentage of total cells counted across 3 regions in the hippocampus – the dentate gyrus, CA1 and CA2. The control sample exhibited the most apoptosis with a cell survival of 36, 39 and 38 percent in CA1, CA2 and dentate gyrus respectively. Treatment with propranolol alone reduced mean apoptotic cell loss by 12.2% (p < 0.0001) and treatment with propranolol in the presence of catecholamines lead to a similar reduction in apoptosis (12.2%, p < 0.0001). Treatment with catecholamines only did not reduce the levels of apoptosis compared to control, p = 0.06.
Conclusion: Treatment of brain tissue slices with propranolol led to a reduction in caspase-3 mediated apoptosis across all studied regions of the hippocampus. This anti-apoptotic effect was independent of the presence of catecholamines and direct catecholamine treatment did not promote caspase-3 mediated apoptosis. This indicates that adrenergic hyperactivity is not directly pro-apoptotic.
| Treatment group | Dosing concentrations |
|---|---|
| sNBA only (control) | – |
| sNBA plus catecholamine | Noradrenaline 30 µM Adrenaline 5 µM |
| sNBA plus beta blocker | Propranolol 30 µM |
| sNBA plus catecholamines and beta blocker | Noradrenaline 30 µM Adrenaline 5 µM Propranolol 30 µM |
| Intervention | Region of interest | Mean cell survival ± SD(Range) |
|---|---|---|
| Control | CA1 | 36.5 ± 12.2(7.9–52.3) |
| CA2 | 39.5 ± 8.4(20.7–52.1) | |
| Dentate gyrus | 38.3 ± 13.2(3.7–56.8) | |
| Catecholamines | CA1 | 44.6 ± 7.4(28.6–61.94) |
| CA2 | 42.8 ± 10.4(18.6–62.2) | |
| Dentate gyrus | 44.2 ± 10.7(18.5–58.7) | |
| Propranolol | CA1 | 51.8 ± 7.8(29.1–65.8) |
| CA2 | 50.8 ± 9.2(24.8–67.6) | |
| Dentate gyrus | 50.1 ± 8.0(33.0–65.8) | |
| Catecholamines + propranolol | CA1 | 50.5 ± 7.8(36.4–64.0) |
| CA2 | 51.0 ± 6.7(35.8–66.2) | |
| Dentate gyrus | 49.4 ± 9.0(27.2–63.4) |
0288
Critical illness and post-hospitalisation healthcare use in Wales: a population-based data linkage study using the SAIL databank
Tamas Szakmany1, Mohammad Alsallakh2, Richard Pugh3, Ashley Akbari2 and Ronan Lyons2
1Cardiff University, Cardiff, United Kingdom
2Swansea University, Swansea, United Kingdom
3Betsi Cadwaladr UHB, Rhyl, United Kingdom
Abstract
Introduction: It has been shown that critical care survivors have higher mortality and more frequent readmissions to hospital, compared to the general population (1). We have previously described patient-level predictors of long-term survival (2). There is no data available in Wales on the association of critical care survivorship and comprehensive healthcare use in the NHS, compared to non-critical hospitalised patients.
Objective: To investigate the association between critical illness and post-hospitalisation healthcare use.
Methods: Using the Secure Anonymised Information Linkage (SAIL) Databank, we identified critical illness survivors and non-critical inpatients who were discharged from Welsh hospitals in 2015 at the age of 16 of older. We compared healthcare use in the year following hospital discharge between the two groups using negative binomial regression adjusted for gender, age group, modified Charlson Comorbidity Index (CCI), and follow-up length.
Results: We identified 5,352 critical illness survivors and 831,558 non-critical inpatients, of which 45.4% and 57.6% were females, with a median age of 66.0 (IQR = 52.1, 75.9) and 61.4 (41.1, 74.1), and a median CCI of 8 (0, 14) and 8 (0, 22), respectively.
The critical care and non-critical care groups had median numbers of general practitioner (GP) events of 31 (0, 52) and 22 (1, 40), outpatient visits of 5 (2, 9) and 4 (1, 8), emergency department (ED) visits of 0 (0, 1) in both groups, and hospital stay of 14 (5, 35) and 3 (0, 14) days, respectively.
Critical illness was associated with 29% more GP events (IRR = 1.29 [1.27, 1.32]), 43% more ED visits (1.43 [1.36, 1.50]), 28% more outpatient visits (1.28 [1.24, 1.32]), and almost 3 times longer hospital stay (2.84 [2.70, 2.99]) in the year following hospital discharge (all p-values < 0.00001).
Conclusion: Critical care survivors use significantly more healthcare resources than hospitalised patients who did not require critical care. It appears that the use of advanced organ support techniques is associated with higher downstream resource utilisation, regardless of initial patient characteristics. As critical care survivors consist only a small fraction of hospitalised patients every year, their increased resource utilisation might not be highlighted for the primary care providers. This underlines the importance of good communication and appropriate follow-up of these patients from the critical care practicioners. Further studies are needed to identify critical care patient populations at highest risk for increased primary and secondary care use. This data can inform future interventional trials addressing post-critical care resource allocation.
0289
Quantification and Characterisation of Patients with Psychiatric and Addiction Diagnoses in a General Adult Intensive Care Unit
Camilla E. St. A. Jackson and Elaine Armstrong
John Radcliffe Hospital, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
Abstract
Introduction: Psychiatric illness and addiction are common in the general population. Little evidence has been published about the proportions of patients admitted to the Intensive Care Unit (ICU) with concurrent psychiatric or addiction diagnoses and the impact this has on the reason for ICU admission, progress in ICU, nursing requirements, development of complications, recovery and quality of life post-ICU. The importance of both physical and mental health is emphasised in patient-centred care. This study will quantify the proportions of patients with psychiatric or addiction diagnoses admitted to ICU and their outcomes.
Objectives: The objectives of this study were to quantify the proportion of patients in a general adult ICU with psychiatric or addiction diagnoses and to further characterise this patient group including patient demographics, psychiatric diagnosis, if ICU admission was directly caused by psychiatric illness and subsequent patient outcomes.
Methods: The notes of all patients discharged from general adult ICUs at the John Radcliffe and Churchill Hospitals from 01.01.2019 to 28.02.2019 inclusive were reviewed and those with a psychiatric or addiction diagnosis identified. Of these cases, the patient demographics were recorded: age, reason for admission, the specific psychiatric or addiction diagnosis and if this diagnosis was a direct cause of their ICU admission or not. Outcomes for length of ICU stay, development of delirium in ICU, mortality on ICU, mortality pre-hospital discharge and 30-day mortality were recorded.
Inclusion Criteria: All general adult ICU discharges 01.01.2019 to 28.02.2019 inclusive.
Exclusion Criteria: Patients aged less than 16 years.
Results: Of 230 patients discharged from ICU from 01.01.2019 to 28.02.2019, 82 had a psychiatric or addiction diagnosis (35.7%). Of those, 41 had only a psychiatric diagnosis, 14 had only an addiction diagnosis. 20 had dual psychiatric and addiction diagnoses.
The psychiatric diagnoses were widespread. Depression and anxiety were most common. Alcohol addiction was the most common addiction.
Of those with psychiatric diagnoses: mean age = 54.0 years (17–84), mean length of ICU stay = 5 days, mortality in ICU = 18.3%, mortality prior to hospital discharge = 20.7%, 30-day mortality = 19.5%.
16/82 (19.5%) of patients with a psychiatric or addiction diagnoses were admitted to ICU as a direct cause of their psychiatric or addiction diagnosis.
26/82 (31.7%) of those with a psychiatric or addiction diagnosis had a recorded diagnosis of delirium in ICU, however this was not well documented and may be an underestimate.
Conclusion:One in three patients admitted to this general adult ICU had a psychiatric or addiction diagnosis. Of those, 19.5% were admitted as a direct result of their psychiatric or addiction diagnosis. This is a sub-set of ICU patients that requires further analysis.
0290
Procalcitonin to guide antimicrobial stewardship in the ICU: Are we consistent in our approach?
Thomas Hirst
East Kent Hospitals University NHS Foundation Trust, Ashford, United Kingdom
Abstract
Introduction: Procalcitonin (PCT) has emerged as a serum marker of infection since its first description in 1975, with a relative specificity for bacterial over viral pathogens. A rapid rise in conditions of infection and similarly rapid fall following treatment have led to evaluations of PCT to guide antimicrobial therapy. Since 2009 single and multi-centre studies have sought to determine whether PCT testing can safely guide the initiation and discontinuation of antibiotic therapy, based on both absolute levels and rates of change over time. Algorithms to guide decision making however have varied in frequency of PCT testing and thresholds for modifying therapy.
Objectives: To determine the variation in recently published literature in use of procalcitonin levels and kinetics to guide discontinuation of antimicrobial therapy in critical care.
Methods: A literature search was undertaken across Medline, Embase, Scopus and Cochrane for studies published between May 2013 and May 2018 comparing PCT-guided antimicrobial therapy to standard therapy in the critical care setting. Methodology of studies was reviewed to determine protocols for PCT testing and thresholds for discontinuing antimicrobial therapy.
Results: There was notable variation in the absolute PCT levels and percentage reduction in PCT which prompted stopping antibiotic therapy, as well as frequency of PCT testing. A total of 10 studies were included in analysis including 5 randomised controlled trials, 3 prospective and 2 retrospective studies. Settings included general ICU patients with infection, postoperative peritonitis, burns, and exacerbations of COPD.
PCT levels used to stop antibiotics ranged from 0.1 to 1 ng/dL with a level of 0.1 ng/dL the most frequently used in 4 studies. 9 studies included relative fall in PCT in their criteria to stop antibiotics and a reduction 90% was most commonly used as a threshold to stop in 6 studies. There was variation whether this decrease was from peak level or baseline level at study commencement. Frequency of PCT testing after baseline included a delay until day 4–5 in 2 studies, but generally daily testing was more frequent in 6 studies with 48 hourly testing in 4 studies. In one study there was no set guidance on PCT usage, but it was disclosed that most participating physicians used the algorithm from the PRORATA trial.1
Conclusions: There remains clear variation in use of procalcitonin to guide antimicrobial usage in the critical care setting. While in part this may represent the diversification of clinical settings in which PCT is being trialled, it still presents a challenge to clinicians wishing to adopt PCT-guided stewardship for their service. At present there is study providing direct comparison between PCT algorithms with regards to testing frequency and cut-off values. This would potentially inform on clinical and financial differences between approaches, aiding those wising to adopt PCT testing in their practice.
0291
Mathematical modelling of critical care flow: new hospital, old challenges
Elizabeth Williams1, Izabela Spernaes2, Tamas Szakmany3,4, Babu Muthuswamy4 and Penny Holborn1
1University of South Wales, Treforest, United Kingdom
2Aneurin Bevan UHB, Caerleon, United Kingdom
3Cardiff School of Medicine, Cardiff, United Kingdom
4Aneurin Bevan University Health Board, Newport, United Kingdom
Abstract
Introduction/Hypothesis: This research aims to determine the effects on occupancy levels within critical care units (CCUs) and the impact of critical care redesign. Currently, low number of critical care beds and high level of delayed transfer of care (DTOC) episodes prevent our ICUs to comply with the Welsh Government recommended maximum occupancy level of 75%. The work conducted focuses on the building of a new Specialist Critical Care Centre (SCCC) within South East Wales, UK and the amalgamation of two CCUs, following the mapping of patient flows, however the techniques applied and insights gained are applicable to other services as well (1).
Methods: We utilised electronic health records of 2,650 patients admitted into the Aneurin Bevan University Health Board (ABUHB) CCUs at Royal Gwent Hospital (RGH) and Nevill Hall Hospital (NHH) between January 2016 to December 2017. To determine how the bed occupancy of the unit will change through different and potential future scenarios, the use of the simulation software, Simul8, was used in this study to generate a replica model of the CCU being constructed. Simul8 is a discrete event simulation software, which is able to use real world constraints and capacities.
Results: The results produced from the model were validated against the health records of the 2,650 patients with the current number of 23 beds for a two year period. The average length of stay (LOS) for a patient equates to 5.7 days with 85% of time spent with the unit at full occupancy. In total 63% of patients were classified as DTOC and remained in the unit for an extra 37 hours and 17 minutes on average. A variety of different scenarios were tested including increasing the bed numbers to 28, reducing proportion of patients experiencing DTOC and also an increase in critical care demand by 4% every year to determine the effect on occupancy levels. Our model highlights the pressure the critical care unit will face even by a small, 4% increase, including the expected unmet demand of 126 patients. For a 4% increase with 23 beds, 95.52% of time is spent above 75% occupancy, with 77% of time spent at full occupancy. In this scenario, by increasing bed numbers to 28, 75% of time is spent above 75% occupancy levels with an 11% increase compared to a 0% increase in arrival rate. In a best case scenario, with increasing demand, an increase to 28 beds along side a 20% reduction in the proportion of DTOC patients to 51% results in an average bed occupancy of 21 (74% utilisation), ensuring the CCU is on average working within the 75% safe government guidelines.
Conclusions: Use of simulation methods based on current bed occupancy, admission and discharge data enables healthcare planning to better determine priorities to deal with increasing demand in a reproducible and flexible way. Our data indicates that reducing the proportion of patients with DTOC had a greater effect in reducing occupancy levels than increasing bed numbers or decreasing length of DTOC.
0292
Neuron Specific Enolase – an underrated prognostic indicator after cardiac arrest?
Iana Martini, Elizabeth Ashton and Rebecca Gray
Royal Sussex County Hospital, Brighton, United Kingdom
Abstract
Hypoxic brain injury is very common in patients presenting with out of hospital cardiac arrest.1 Often death will occur after a decision is made to withdraw treatment due to predicted poor neurological outcome. Early identification of these patients avoids unnecessary treatment and potential suffering in this patient group. These decisions are therefore both important and regularly encountered challenges in critical care.
The literature suggests a multimodal approach to prognostication of these patients. Neuron specific enolase (NSE) is a biomarker that can be utilised for this purpose. NSE is a protein-based enzyme found chiefly within neurons; serum levels of NSE rise following traumatic and ischaemic brain injury. Zandbergen et al2 suggest an NSE level of 33 micrograms/L after 24 hours as representative of poor neurological outcomes following ischemic insult – and this has since been validated by the PROPAC study in 2006.3 The reliability of this test was further corroborated in 2017 by Streitberger et al in a prospective study of over 1000 patients.4
Based on this evidence and after personal experience of working in an institution where NSE is utilised routinely post cardiac arrest we undertook a telephone survey to investigate the its use in intensive care units across the United Kingdom. Of the 135 acute trusts operating at the time of the survey, only seven were found to test NSE regularly in their post-arrest patients. Of these, just three had clear protocols in place to guide timing of serum sampling and had guidelines to aid interpretation of NSE levels.
Prognostication of these patients is a complex process based on clinical findings, scientific evidence and clinicians previous experiences. NSE is a simple, non-invasive and inexpensive test with proven relevance in this field and its value alongside other tests should not be dismissed. Increased uptake would improve confidence in its interpretation and facilitate further large scale studies into its efficacy.
Ultimately, surely we should all be striving to adopt the information afforded to us by validated, novel investigations in order to facilitate dignified decision making for our patients.
0293
Implementing HIV Testing for All Unscheduled Admissions to a Large Tertiary Intensive Care Unit in Europe – a Quality Improvement Project
Lewis Hitchen, Howard Smith, Jaimin Patel, Tracie Matthews, Jodie Beth-Willamson, Claire Scanlon, Atul Garg and Katerine Laver
Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: HIV remains a relevant public health issue in the UK. In 2017, 4363 people were newly diagnosed with the virus and there were 428 AIDS-related deaths.1 Late diagnosis remains the leading cause of morbidity and mortality2 and there are an estimated 7800 people currently living undiagnosed. HIV testing is an essential component of tackling the epidemic. The 2016 NICE guideline on HIV testing suggests that in areas of high and extremely-high prevalence, testing should be offered on admission to hospital, to everyone who has not been previously diagnosed.3 Public Health England defines areas of extremely-high prevalence as >2 in 1000 of the population.1 The prevalence of diagnosed HIV in Birmingham, UK, is 2.74 per 1000.4
Objectives: The aim of this project was to implement HIV testing for all unscheduled admissions to The Queen Elizabeth Hospital’s Intensive Care Units (ICUs). This is a large, university-affiliated, tertiary ICU with 100 beds and is one of the largest in Europe,5 admitting over 3500 patients per annum with a varied surgical and medical case-mix.
Methods: An initial retrospective audit of 1500 unscheduled admissions to ICU between April 2016 and April 2017 demonstrated that only 25% of patients were being screened for HIV during their inpatient stay. A policy of universal testing for all unscheduled admissions was approved in July 2018 by the ICU team and implemented in September 2018 following an advertising campaign directed at all clinical staff. In an iterative process of quality improvement, monthly screening rates across the ICUs were cascaded to all staff via email, and posters were widely displayed. Additionally, stickers serving as a reminder were placed on nurses’ computer workstations. Finally, in March 2019, an automated testing process was implemented through the Trust’s IT system, which protocolised HIV screening alongside other routine admission bloods.
Results: There has been a significant, sustained increase in the percentage of unscheduled admissions being tested for HIV. In the ten months following policy implementation, the percentage tested increased from 25% to >90%, sustained over three months. During the audit period, there were 1539 admissions, of which 1000 were tested with 4 new HIV diagnoses, giving an incidence rate of 0.4%. Initially, the increase in percentage tested was less-well sustained whilst relying on reminder-based interventions. Automation of the testing process led to the largest increase in percentage tested which has been sustained.
Conclusion: The automation of HIV screening tests at QEHB has led to a dramatic and sustained increase in the percentage of patients being tested for the virus to meet with national guidance. The high positive test rate justifies the routine testing for HIV in ICUs. Advances in anti-retroviral therapy have led to significant improvements in patient outcomes. In the four patients with positive results, only one would have been tested for HIV based on their admission diagnosis. The early diagnosis of these patients led to early initiation of treatment and contact tracing. This study demonstrated that HIV screening in a large ICU is possible, cost-effective and has a significant impact on patient outcomes.
0296
What effect does citrate based anticoagulation have on renal replacement therapy circuit life and blood product use compared with heparin based anticoagulation?
Sergio Mura1, William Ford2 and Mark Borthwick1
1Pharmacy Department, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
2School of Pharmacy, Cardiff University, Cardiff, United Kingdom
Abstract
Introduction: Continuous Renal Replacement Therapy (CRRT) is commonly used in critically ill patients affected by Acute Kidney Injury (AKI) (1,2). Anticoagulants are used to prevent thrombus formation within the extracorporeal CRRT circuit, which would otherwise lead to circuit failure and suboptimal CRRT therapy. Heparin has been widely used for CRRT, but is returned to the patient from the CRRT circuit and increases the patient’s risk of bleeding (3). In recent years, citrate based anticoagulation has gained popularity. It has the potential to provide CRRT circuit anticoagulation without anticoagulating the patient, provide a longer CRRT circuit lifespan, and so may provide longer CRRT without increasing the patient’s haemorrhage risk (4,5). Lower rates of CRRT circuit loss and reduced patient haemorrhage rates may reduce the requirement for blood products.
Objectives: To compare a cohort of patients who received heparin based CRRT with a cohort of patients who received citrate based CRRT to evaluate any effect that the anticoagulation method has on CRRT circuit life and use of blood products.
Methods: This was a before and after style study. Six months of data were collected retrospectively for two groups of patients requiring CRRT on the adult general critical care units of the Oxford University Hospitals NHS Foundation Trust, a heparin CRRT group and a citrate CRRT group. Data were collected on the number of CRRT circuits used, duration of therapy, and units of red blood cells, platelets and fresh frozen plasma administered during the period the patient required CRRT. Data were recorded in an Excel spreadsheet and reported using descriptive statistics. An Excel statistics add-in was used to conduct statistical analysis.
Results: There were 38 patients in the heparin group and 36 in the citrate group. A total of 119 CRRT circuits used for 1782 hours in the heparin group and 75 CRRT circuits used for 2349 hours in the citrate group. The median circuit life was 11 (IQR 6–18) in the heparin group and 19 (IQR 10–46) in the citrate group (Figure 1.) (difference = 8hours, p < 0.01, Mann Whitney U).
The use of blood products is shown in Figure 2.
Conclusions: The implementation of the new Citrate CRRT protocol was associated with significantly longer CRRT circuit life, but there were no significant differences in quantities of blood products used.
0297
Think Delirium
Abigail Johnson and Kaylee Yildiz
East Lancashire Teaching Hospital, Blackburn, United Kingdom
Abstract
Introduction: ICU Delirium is a common clinical diagnosis within the critical care setting, which is distinguished by disturbances in conscious levels, impaired cognitive function and/or perception. Delirium presents with an acute onset but often has a fluctuating course. The incidence of delirium is prevalent within critical care today; in recent years it has been recognised as a serious condition associated with important clinical outcomes. However, it is possible to be prevented if treatment is commenced in a timely manner.
Objectives: The aim of the ‘Dreams and Sleep’ bundle introduced on the critical care network is to help prevent and reduce the incidence of delirium. Elements identified for improvement included:
• Documentation and information.
• Rehabilitation.
• Early identification.
• Aids to communication.
• Medication.
• Sleep.
Methods: Over the last twelve months we have introduced both of the bundles on our unit. It was evident more training was required around assessment of delirium and the use of the CAM ICU tool. Educational boards were created and displayed throughout the unit and waiting areas. One to one teaching was provided to all staff. Delirium leaflets and information were made more accessible to patients and relatives. As research shows patient diaries can be of benefit and can help to fill gaps in memory loss. This was an area of improvement identified and a diary was created and at present is being trialled. Monthly audit tools have been designed and are monitored. Working as a multidisciplinary and ensuring doctor’s daily review of medication, reduction in sedation where appropriate, prescribing of sleeping tablets if needed and review of delirogenic drugs. The implementation of the sleep bundle is being used as a measure to improve the quality of patient’s sleep, which can reduce the risk of delirium developing.
Results: Since we started auditing the elements of the ‘Dreams’ bundle in April 2019, compliance in most elements has improved. Results have highlighted areas such as sleep which require improvement. In comparison to the number of patients admitted our incidence of delirium is relatively low.
• April 2019 6.61%
• May 2019 2.38%
• June 2019 5.42%
• July 2019 3.47% (percentage of patients admitted with incidence of delirium).
Conclusion: It is apparent delirium is still evident in critical care. Steps are still being made to reduce these numbers further. With the implementation of the bundles and further education this will continue to be an ongoing progress.
0298
Views of senior intensive care trainees and intensive care nurses on the use of simulation training to develop communication skills in AICU
zehanah izmeth1 and Elaine Armstrong2
1Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
2Oxford University Hospital, Oxford, United Kingdom
Abstract
Background: There is limited evidence for the use of multi-disciplinary team simulation communication skills training in Adult Intensive Care (Levy 2001).
Method: We have a psychiatrist working in our unit and with their input we used the communication competencies described in the Faculty of Intensive Care medicine curriculum to design scenarios. We used professional actors and developed linked scenarios to depict the journey of a patient through Intensive Care. Participants included ICM higher trainees and intensive care nurses and the faculty was made up of consultants in intensive care and psychiatry, with in-depth debriefs following each scenario focussed on communication skills theory and its application in Intensive Care.
Results: Semi-structured interviews were conducted and analysis of transcripts produced the following themes:
Factors affecting communication simulation
The debriefs were sufficiently detailed to add value e.g. “analysis was so sophisticated … I felt like I’ve grown.” The skills of the actors meant participants “took things very seriously…made you behave as you would in practice.”
Impact of communication simulation
The participants were able to gain an appreciation of how and why their experiences were different, even though they were looking after the same patient: “for me (doctor) these very intense experiences have walls around them and I can’t imagine how (nurses) deal with it when it’s just dripping through at the bedside.” The participants described better team cohesion and improved morale: “if I’m able to be effective in communicating with others then it will make us a better team,” and both doctors and nurses felt there had been a change in their practice “giving context to someone dying, I’ve tried to do that more and more.”
Participants' experience of having a multi-disciplinary faculty
The faculty composition was unique to this particular communication simulation, which was well received by all participants. The presence of the intensive care consultants gave participants validation of their practice and allowed the opportunity to explore different communication styles and their likely impact in real life: “gave a nice angle in terms of giving the context to the situation, where it might go.” The presence of psychiatrists added a different dimension to training: “you’ve got to have someone understand how you get better and I haven’t found that before … it just gave me more respect for the discipline.” The participants found it helpful to incorporate communication skills theory within the debriefs “theory behind the communication skills in the context that we deliver the discussion is really important, something I didn’t appreciate.”
Conclusion: Development of communication skills using simulation training is a highly rewarding experience for participants and faculty. In order to optimise the benefit of this type of training, scenarios should be designed around curriculum competencies and it is imperative that faculty have the relevant skills set.
0299
Embedding use of Local Safety Standards for Invasive Procedures (LocSSIP) within a unit safety culture
Charlotte Kane and Norman Main
Critical Care Department, Royal Liverpool University Hospital, Liverpool, United Kingdom
Abstract
Introduction: Central venous catheters are routinely used in Critical Care for the administration of fluids, vasopressors and provision of renal replacement therapy (RRT). CVC insertion is associated with a number of risks and guide wire retention is a serious but preventable complication. Faculty of Intensive Care Medicine (FICM) and Intensive Care Society (ICS) have produced a Local Safety Standards for Invasive Procedures (LocSSIP) for CVC insertion.1 Following a retained guide wire never event, Royal Liverpool University Hospital (RLUH) critical care unit adapted the use of a LocSSIP document. Critical care unit policy is that LocSSIP, be used whenever a central line is inserted. A key step in safe CVC insertion is confirmation of guide wire removal. Documentation of this is included in the LocSSIP form.
Objective: The aim of this audit was to check the compliance of the use of LocSSIP for CVCs inserted in critical care and their recorded complications.
Methods: A retrospective audit was conducted for all CVCs inserted in critical care over a three-month period (Feb – April 2019). Patient records were reviewed and documentation of the insertion of CVCs was analysed.
Results: 60 CVCs were inserted over a two-month period. 70% (42/60) were inserted into a jugular vein, 28.3% (17/60) in a femoral vein, and 1.7% (1/60) in a subclavian vein. 63.3% (38/60) were quad lumen lines, 36.6% (22/60) were vascaths for RRT.
The LocSSIP form was completed for 90% (54/60) of CVC insertions. 5% (3/60) was freehand documentation. 5% (3/60) of the lines were inserted with no formal documentation.
Removal of the guide wire was documented for 91.7% (55/60) of the CVC insertions. Of these, 100% of the LocSSIPs form confirmed guidewire removal and one case had free hand documentation.
Complications were documented for 11/60 CVCs. These were as follows: high VIP score (3/11), HF line with poor flow or high pressures (3/11), suspected line infection (3/11), jugular line displaced into a subclavian vein (1/11) and line contaminated due to patient being faecally incontinent (1/11).
Conclusions: The National Safety Standards for Invasive Procedures (NatSSIPs) aim to reduce the number of patient safety incidents related to invasive procedures in which surgical never events could occur. LocSSIPS are based on framework document produced by NHS Englands Patient Safety Domain and the NatSSIP group.2
Our audit demonstrates a 90% compliance with use of LocSSIP. Although there has been no reported never event following introduction of LocSSIP, our practice can be improved by achieving a 100% compliance.
The audit findings were presented in the departmental audit and safety meetings and the recommendations are incorporated in doctors and nurses induction.
We have highlighted the need to embed use of LocSSIP within our unit culture and aim to re-audit to ensure increased compliance.
0301
Saving Lives, Giving Hope: Improving Organ Donation Referrals in a Scottish District General Hospital Intensive Care Unit
Scott James1, Radha Sundaram2, Megan Reid3 and Kevin Rooney2,4
1Core Anaesthetic Trainee, South East Scotland School of Anaesthesia, Edinburgh, United Kingdom
2Consultant in ICM, RAH Paisley, Paisley, United Kingdom
3Specialist Nurse in Organ Donation, Paisley, United Kingdom
4Professor in Care Improvement, University of the West of Scotland, Paisley, United Kingdom
Abstract
Introduction: Organ donation is lifesaving with one donor able to help as many as 9 individuals through organ and up to 50 through tissue donation. Across the UK we are moving towards an opt-out system of organ donation. The Scottish Government has identified an ambitious target of increasing authorisation for donation after cardiac death to 80% by 2020.
Background/Objectives: The Intensive Care Unit (ICU) at the Royal Alexandra Hospital (RAH) in Paisley is a 7 bedded DGH unit that admits approximately 380 patients per year. A proportion of patients admitted will not survive and for many of these patients there is an opportunity to approach families with regards to proceeding to organ donation. We wished to identify areas where we could improve practice and increase our referral rate.
Methods: A survey was undertaken of nursing staff that identified areas of end of life (EOL) care that could be improved. Once those were identified a bundle was developed and tested in an iterative fashion. The Plan, Do, Study, Act cycles introduced a COMFRT bundle for EOL Care (C for consensus, O for opportunity to facilitate donation, M for medical documentation, F for family, R for religious or spiritual support and T for tasks post event). This was initially used as a prompt at EOL discussions. We also introduced prompts at handover, nursing ward round, weekly meetings and clinical governance meetings. All deaths between Jan 2017 and Jun 2019 were identified using the WardWatcher system. Medical notes were examined to identify whether organ donation had been considered and whether it progressed. This was cross checked with the Specialist Nurse for Organ Donation data. The data gained was entered into a Microsoft Excel spreadsheet and a run chart produced to highlight the number of deaths referred for organ donation.
Results: The monthly rate of referral increased from 18% up to a peak of 83% representing a mean of 43%. This unfortunately decreased to a mean of 14% between May 18 and Mar 19 prior to it increasing again to 33% with further interventions. There were two proceeding donations each year since the project was commenced. Although other measures were difficult to quantify such as nursing satisfaction, offers of spiritual help and keepsakes that were accepted by patients and completion of medical documentation, there was a sense that EOL care had improved overall.
Conclusions: A limitation of the data collection may have been that the denominator was all deaths, rather than deaths where organ donation may have been possible once authorisation had been obtained. The introduction of the COMFRT bundle, although initially promising has not been consistent in improving referrals and much work needs to be done to make conversations about organ donation an integral part of all EOL conversations. It will be interesting to observe the impact of the new legislation on referral rates. It has to be noted though that 21 lives have been saved or enriched as a consequence of this improvement project at the RAH in the last few years.
0302
Simulation Based Education: does it improve Allied Health Professionals (AHPs) tracheostomy management skills?
Aeron Ginnelly1,2, Amanda J Thomas2,3 and Stephanie K Mansell2,4
1Therapy services, Royal Free London NHS Foundation Trust, London, London, United Kingdom
2University College London Partners, London, United Kingdom
3Critical Care Outreach Team, Barts Health NHS Trust, London, United Kingdom
4Therapy services, Royal Free London NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Simulation-based education (SBE) is routinely accessed by medical staff for both undergraduate and post-graduate training. SBE access for Allied Health Professionals (AHPs) is currently limited despite the proven effects of SBE on non-technical skill learning and development. The National Confidential Enquiry into Patient Outcomes and Death (NCEPOD) “On the Right Trach” report (2014) investigated outcomes for patients with tracheostomies. One of the primary recommendations of the report included multidisciplinary team (MDT) care being part of the routine pathway for patients with tracheostomies. Key professions identified by the NCEPOD report included Physiotherapists and Speech and Language Therapists (SLT). We theorised that a two-profession specific SBE course could be a powerful tool for enhancing knowledge and skills in the management of patients with tracheostomies.
Objective: The objective of this project was to assess the impact of SBE on AHP’s self-assessed ability to manage patients with tracheostomies. Furthermore we aimed to evaluate bi-professional SBE as an educational tool in this participant cohort.
Methods: The course was assessed using the Bart’s Health Simulation Centre Post Course Questionnaire (BHSQ) and a bespoke, content specific Pre and Post Course Self-Assessment Tool: SIMTRACH self-assessment tool. Participants were physiotherapists and SLT. Data were analysed using weighted scores and percentage change scores in the pre and post self-assessment questionnaires. Weighted scores were calculated by giving categorical data a numerical value and multiplying this value by the number of participants who responded in that manner. p values were calculated in SPSS using a paired t-test.
Results: Between 2016 and 2018, 84 participants attended SIMTRACH. There was a significant improvement in SIMTRACH self-assessment tool scores following the course (Mean difference 9.08 (95% CI 7.44 to 10.73) p < 0.0001)
As seen in table 1, from the SIMTRACH self-assessment tool, the largest changes in scores were seen in the 2 domains associated with communication (talking to other team members and teaching others), where a greater than 100% change in weighted scores were observed (184% and 109% respectively). Large changes in scores were also observed in items relating to the emergency management of patients with tracheostomies and resuscitation (50% and 87% respectively).
Data from the BHSQ is displayed in Figure 1. There was strong agreement with all dimensions of the BHSQ completed post training. Qualitative content analysis from the post course BHSQ showed the most frequently occurring comment was the participants belief that they benefitted from the opportunity to practice technical and non–technical skills in a safe and non–threatening environment.
Conclusion: The biggest impact of this bi-professional SBE tracheostomy course related to improved participant confidence in communication dimensions. SIMTRACH also improved patient safety dimensions as demonstrated by the improvement in resuscitation and emergency situation questions on the SIMTRACH self-evaluation. SBE should be available to all healthcare professionals managing patients with tracheostomy.
0306
National Early Warning Score 2 (NEWS2): We need to ‘Focus on 5’
Najade Sheriff, Matthew Benjamin, Sherry Dutt and Jerome Mccann
Warrington and Halton NHS Foundation Trust, Warrington, United Kingdom
Abstract
Introduction: Following the launch of NEWS2 in Warrington and Halton Trust, we audited a key theme highlighted in the NEWS2 update: ‘A NEWS score of 5 or more is a key trigger threshold for an urgent clinical alert and response’.1
A threshold chosen by Royal College of Physicians (RCP) based on research by Smith et al in 2013.2
The report emphasizes the importance of considering serious sepsis in these patients and ensuring acute care teams (ACT) are available 24/7 and free of other clinical responsibilities.
Objectives: To audit the compliance of this NEWS2 theme in our trust – whether ACT had been alerted.
We have then administered an intervention before re-auditing with the aim to raise awareness of the importance of a NEWS score of 5 as a potential risk of serious acute clinical deterioration.
Methods: Observation notes of all inpatients in 4 acute wards were retrieved on a weekday in September 2018. The hospital numbers of patients identified as having scored a 5 or more during a 24-hour period was cross-checked with ACT records.
Following this, we designed a campaign called ‘Focus on 5’ to raise awareness of this key trigger threshold. Nurses were asked to inform the ACT of every patient scoring a 5 or above by contacting them.
We re-audited on a weekday in June 2019 the exact same way as the pre-intervention study albeit with a larger number of wards, 13 in total. The original 4 wards were included in this total. This allowed us to assess the direct impact of the Focus on 5 initiative. had on the initiative.
Results: The pre-intervention audit looked at 112 patients. 15 patients scored a 5 or above within the previous 24 hours. Of these, only 1 patient was known to the ACT; indicating 6% awareness rate. The post-intervention study looked at 280 patients. 28 patients in total scored a NEWS2 of 5 or above within the previous 24 hours and 16 of these were known to the ACT; with an awareness rate of 57%.
The re-audit of the 4 original wards identified 9 patients who scored a 5 or above.
The ACT were aware of 7 patients resulting in an improved awareness rate of 78% when compared to 6% found pre-intervention.
Conclusions: Focus on 5 showed to significantly improve ACT awareness of potentially unwell patients. It is not surprising that human factors inhibit a flawless rollout of a new standard and culture. Our plan involves targeting the wards who have particularly poor compliance, understanding nurses views and aiming towards electronically recorded observation which will eliminate human factors affecting compliance.
Furthermore, our audit demonstrates that there is a scope to recruit more ACT nurses to help manage this increased workload.
Finally, The National Suspicion of Sepsis is a growing movement and there is evidence that if we ‘Focus on 5’ we could identify cases of sepsis at an earlier stage which is vital for a better outcome.
0308
Driving resumption after acute or critical illness: A scoping review
Chloe Apps and Joel Meyer
Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Driving resumption after acute and critical illness is viewed as a recovery milestone for many survivors. Returning to drive brings the ability to access hobbies, social activities and recommence employment, all of which are imperative for quality of life and financial stability. Driving is a complex task necessitating intact cognition, physical ability and emotional preparedness. These may all be affected after a period of illness. It is estimated that only 68% of individuals resume driving six months after discharge from hospital. Existing DVLA guidance provides limited advice on driving for generally deconditioned or multi-modally impaired patients such as those recovering from acute or critical illness. As this area has not been extensively evaluated, a scoping review to map the existing literature and collate findings is vital to gain a greater understanding of this topic.
Objectives:
1. To review the current literature on driving after acute and critical illness
2. To ascertain if individuals do, or do not, resume driving after acute or critical illness
3. To gain insight into driving practices of individuals following acute or critical illness
Methods: This scoping review will follow the methodological framework proposed by Arksey and O’Malley1 alongside the amendments made by the Joanna Briggs Institute.2 The six stages of the framework comprise of: (1) identifying the research question, (2) identifying relevant studies; (3) study selection; (4) charting the data; (5) collating, summarising and reporting results; and (6) consultation. Databases including MEDLINE, Embase and CINAHL will be searched with key terms to ensure all relevant articles are retrieved. Grey literature will also be searched. Two reviewers will independently perform screening and selection. No limitations will be placed on study design, intervention type or outcomes of studies.
Results: The PRISMA-ScR (Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews)3 checklist will be used to report results. Pertinent findings from the literature review and research questions not yet addressed in the literature will be highlighted in this presentation.
Conclusion: This review will explore the existing body of work in the field of driving resumption after critical illness and will help to inform future research.
0311
A re-audit of emergency intubations performed in a tertiary centre critical care following the introduction of a multi-disciplinary simulation programme
Phillip El-Dalil1, Kathleen Ford1, Lucy Clare-Banayos2 and David Balthazor1
1Queen Elizabeth Hospital, University Hospitals Birmingham UHB NHS, Birmingham, United Kingdom
2University Hospital Birmingham NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Introduction: Non-theatre intubation of the critically ill patient is associated with an increased risk of adverse events compared to intubation within a theatre environment.1 Simulation has been shown to have a positive impact upon the acquisition and maintenance of knowledge, technical skills and non-technical skills, and therefore may have a role in mitigating these increased risks.
Objectives: This re-audit aimed to review rates of peri-intubation adverse events on critical care following the introduction of an emergency intubation simulation programme.
Methods: A critical care based multi-disciplinary emergency intubation simulation programme was initiated in July 2017. Following its introduction a prospective audit of emergency intubations performed in the Queen Elizabeth Hospital Birmingham, Critical Care was undertaken between January 2018 and July 2019. A self-administered questionnaire was used to collect data on; indication for intubation, intubation technique and peri-intubation complications.
Results: Data was collected for 74 intubations; 5% were reported as “Crash” intubations, 8% were anticipated difficult airways whilst the remaining 87% were standard rapid sequence inductions. Respiratory failure was the most common indication for intubation accounting for 62% of patients. Intubation was successful at the first attempt in 89% of cases. 24% of patients suffered at least one adverse event, with hypotension most prevalent; additional complications included desaturation, airway trauma, oesophageal intubation and cardiac arrest.
Conclusion: A complication rate of 24% compares favourably with a previously reported figure of 39% in a similar cohort.2 Furthermore when compared to the original audit results, a positive trend towards improved cardiovascular stability is illustrated (see Table 1). Changes in clinical practice secondary to partaking in the simulation programme may account for these positive findings, a conclusion supported by previous observational research.3
The authors acknowledge the risks of response bias due to the methods of data collection. This has instigated the introduction of an electronic intubation form in conjunction with the electronic noting system within the trust. This will be employed as the mandatory record of the procedure with the additional aim of facilitating future clinical governance endeavours.
In view of the encouraging results of this audit and the overwhelmingly positive candidate feedback, the simulation programme will be continued within the department. The format and content of the incumbent pre-intubation checklist has been developed and incorporated into the simulated scenarios so as to familiarise staff with their use. A further re-audit will be necessary in the future to reassess complication rates, as well as to review checklist compliance and the utility of the electronic procedure record.
Table 1.
A comparison of peri-intubation cardiovascular stability following the introduction of a simulation programme.
| Intubations | Mean % fall in SBP* post intubation | Intubations associated with >10% fall in SBP (%) | Intubations associated with >20% fall in SBP (%) | |
|---|---|---|---|---|
| 2016/17 Audit | 50 | 12 | 58 | 37 |
| 2018/19 Audit | 74 | 8 | 43 | 28 |
*SBP = Systolic blood pressure.
0313
Have we ‘normalised’ diarrhoea in the Critical Care patient?
Pegeen Fisher and Gursharan Vryaparj
Sandwell and West Birmingham NHS Trust, Birmingham, United Kingdom
Abstract
Introduction: This abstract summarises the preliminary work undertaken that provided the evidence to proceed with a quality improvement initiative. The aim of the initiative is to reduce incidences of patient harm caused by non – infective diarrhoea and skin breakdown on Sandwell and West Birmingham (SWBH) Critical Care (CC).
Background: 40% of CC patients experience acute faecal incontinence with diarrhoea (AFID),1 placing the already vulnerable patient at additional clinical risks of: haemodynamic instability; electrolyte imbalances; metabolic acidosis; malnutrition; AKI; hypovolaemic shock; delayed mobilisation; delayed weaning from mechanical ventilation; extended use of invasive lines; cross contamination to other wounds; increased skin colonisation; and extended CC stay.1–3 Diarrhoea in the CC patient is infrequently caused by infective aetiology,2 reinforcing the requirement for a multi-disciplinary assessment.
Incontinence associated dermatitis (IAD) is a type of moisture associated skin breakdown (likened to a burn), due to exposure to faeces, that affects around 40% of CC patients.5 IAD’s are now reportable incidents, with additional scrutiny on this aspect of care. At SWBH diarrhoea is managed using a faecal management system. These are invasive devices that pose their own risks, and are never as successful as removing the source of the irritation.
Methods/Objectives:
• Identify the prevalence of diarrhoea and IAD in the SWBH CC patient population
• Confirm stool infection rates over the last 12 months @ SWBH
• Benchmark practice @ SWBH with other CC units across the network
• Search for a National diarrhoea management protocol
• Undertake a literature review to clarify the impact on the CC patient of diarrhoea
• Identify any cost/benefit aspects to reducing incidences of diarrhoea
Results:
1. An audit across the 2 CC units identified that 53% of patients had experienced type 6/7 stool twice or more in the previous 24 hours. (N = 104 patients). 36% of those with AFID had IAD.
2. From a microbiology perspective, 224 stool samples were analysed for C&S and all were negative. Of 225 stool samples for Clostridium difficile, 10 samples were positive.
3. Similar practices to SWBH were confirmed across the 5 CC units that responded. No CC unit used a protocol to guide this aspect of care.
4. No National validated bowel management protocol was identified. A limited number of bowel management protocols identified in the literature did not have the required detail around pharmacological options or enough risk mitigation around C.diff. The literature confirmed that patient outcomes can be enhanced through a standardised approach to this patient population3
5. The maximum cost of loperamide is 88 pence per day. 1 CC bed £1200-£1500/day
Conclusions: This evidence was presented at the CC MDT meeting. The consensus was that diarrhoea had been “normalised”, the clinical risks were significant and a diarrhoea management protocol was required to mitigate some of those risks. The CC sister had the go ahead to assemble a core MDT team (CC sister, CC Consultant, CC pharmacist and Consultant CC microbiologist) and begin the next phase, which is currently underway.
0315
Predictive applicability of intubation criteria in burns patients with suspected inhalational injury
Dr Christine Pirrone, Dr Minesh Chotalia, Dr Thomas Mangham, Dr Randeep Mullhi, Dr Kaye England and Tomasz Torlinski
Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Inhalation injury alone carries a mortality of 5–8%. Inhalation injuries can have a delayed presentation of airway obstruction, this leads to difficulty in predicting which patients need intubation. The University Hospitals Birmingham (UHB) guideline reflect traditional teaching and recommend early intubation to avoid potential airway obstruction.i The American Burn Association (ABA) released guidelines in 2011 which aim to decrease inappropriate intubations.
Objectives: To establish the predictive applicability of guidelines in determining the need for intubation in patients with suspected inhalational injury.
Methods: Patients who sustained a burn injury and received intubation between April 2016 and May 2019 at UHB were included. Case notes were retrospectively analysed to determine if ABA or UHB guideline criteria for intubation were present at initial presentation (Table 1). This was correlated with clinical data confirming presence or absence of inhalation injury. Multiple clinical parameters were collected including initial blood gas. An intubation was deemed inappropriate in patients with suspected inhalational injury if extubation occurred within 48 hours. Patients who died within 24 hours or had insufficient data were excluded.
Results: A total of 62 patients were intubated for suspected inhalational injury. Of these, 46 had a confirmed inhalational injury and 16 did not.
Patients intubated for confirmed inhalational injury: 100% met UHB criteria and 96% (44/46) met ABA criteria. Of the 16 patients who were intubated and did not have an inhalational injury: 100% met UHB criteria, and 12.5% (2/16) met ABA criteria. This gave the UHB intubation criteria a sensitivity of 100% and specificity of 0%, and the ABA criteria a sensitivity of 95.7% and specificity of 87.5%.
Blood gas results were then combined with each intubation criteria and there was no increase in sensitivity or specificity (Table 2).
Conclusions: Both intubation guidelines are sensitive for inhalational injury. Our audit found high specificity with the ABA guidelines compared to no specificity with the UHB guidelines. The ABA guidelines reduced inappropriate intubations and were the best indicator for intubation in patients with suspected inhalational injury.
Table 1.
ABA and UHB Guidelines for intubation.
| ABA | UHB |
|---|---|
| Full-thickness facial burn | Facial burn |
| Stridor | Stridor/cough/ hoarse voice |
| Respiratory distress | Bronchospasm/ dyspnoea/ chest pain |
| Airway swelling on laryngoscopy | Enclosed space |
| Airway trauma | Soot around mouth/nose |
| Altered mentation | Loss of consciousness |
| Hypoxia/ hypercarbia | Hypoxia/hypercarbia/raised carbon monoxide |
| Haemodynamic Instability | Carbonaceous sputum |
Table 2.
Sensitivity and specificity of guidelines.
| Sensitivity | Specificity | |
|---|---|---|
| ABA | 95.7 | 87.5 |
| ABA + pH | 84.4 | 45.5 |
| ABA + CO2 | 52.3 | 87.5 |
| ABA + PF ratio | 55.9 | 66.7 |
| ABA + O2 | 9.8 | 83.3 |
| UHB | 100 | 0 |
| UHB + pH | 88.9 | 0 |
| UHB + CO2 | 54.5 | 0 |
| UHB + PF ratio | 55.9 | 0 |
| UHB + O2 | 12.2 | 0 |
0316
Thrombolysis in Pulmonary Embolism: a Busy District General Critical Care Experience
Musarat Hussain, Megan Woolford, Joshua Mark and Joyce Paul
BHR Hospitals NHS Trust, Romford, United Kingdom
Abstract
Introduction: We have conducted an audit looking at current practice of the use of thrombolysis to treat pulmonary embolism (PE) within Barking, Havering and Redbridge (BHR) NHS Trust critical care units.
Background: Pulmonary embolism (PE) causes approximately 25,000 hospital admissions year, many of which are managed in critical care. European Society of Cardiology(ESC) (1) guidelines advises the use of thrombolysis in the ‘massive’ subtype of PE, which can be defined as those with hypotensive cardiovascular instability. However guidance on the ‘sub massive’ or intermediate high risk category of PE remains less clear. Recent studies looking at alternative options such as half dose thrombolysis as well as catheter directed thrombolysis have further added to this confusion.
Objectives:
1. What is our thrombolysis practice in critical care and does it adhere to national guidelines:
a. Indications?
b. What dose is being used? If half-dose then was the reason documented?
c. Which patient groups are we using it for?
2. Are there surrogate markers other than cardiovascular instability, associated with high morbidity and mortality which could suggest alternative indications for thrombolysis?
Methods:
1. Inclusion criteria:
a. PE as primary diagnosis necessitating critical care admission
b. hrombolysis indication PE
2. Patient data was collected from June 2017- January 2019 from the critical care pharmacy records (JAC) of alteplase use and theIntensive Care National Audit and Research Centredata.
3. Medical notes were obtained from the Clinical audit office at Queen’s Hospital and these were used in conjunction with Medway, Cyberlaband PACsystems, to collect data.
4. Patients who received thrombolysis for any other indication than PE were excluded.
Results: Between June 2017 and Jan 2019 there were 21 cases of PE as the primary cause for admission to Intensive Care. Patients had a mean comorbidity index of 3 and a clinical frailty index (CFS) of 3.
48% were thrombolysed with the predominant reasons being combination of right heart strain with one of hypotension or hypoxia (90%). There was equal use of full dose and half dose thrombolysis
Patients who were thrombolysed required less NIV ventilatory support (20% vs 80%). Patients requiring thrombolysis had a marginally higher APACHE II score (9.3 vs 12) and ECG were more likely to have right strain and T wave changes
Length of stay (LOS) for intensive care (2.1 days vs 3.1 days) and hospital (7 days vs 8.8 days) was lower in the thrombolysed group. 30 day survival of patients receiving thrombolysis was higher (90% vs 72%) than if not thrombolysed.
Conclusion: BHR management of thrombolysis of haemodynamically unstable PE complies to national standards. Thrombolysis in submassive PE was based on evidence of right heart strain with hypoxia/hypotension as per ESC guidelines. Although given the very small numbers use of thrombolysis based on the combination of right heart strain and one of either hypotension or hypoxia resulted in less need of NIV support, lower inpatient stay and higher 30 day survival. A larger cohort analysis is needed to determine if these are statistically significant.
0317
The benefit of procalcitonin to guide antimicrobial therapy in critically ill patients with viral respiratory tract infections
Thomas Hirst1 and Paul Hayden2
1East Kent Hospitals University NHS Foundation Trust, Ashford, United Kingdom
2Medway Maritime Hospital, Gillingham, United Kingdom
Abstract
Introduction: Procalcitonin (PCT) has gained recognition as a biomarker for bacterial infection within critical care, with a relative specificity for bacterial pathogens. A difficulty for the clinician in the intensive care unit (ICU), particularly in the winter months, is to identify patients with viral illness where antibiotic therapy may add to morbidity and mortality rather than treating infections. This is further complicated by the knowledge that viral infection may lead to a superimposed bacterial infection in some patients. Adding PCT testing in the ICU setting may help to identify these patients and guide appropriate antimicrobial therapy. In our ICU PCT testing is routinely carried out following admission (Day 1) and subsequently every 48 hours in patients with suspected sepsis or receiving antibiotic therapy. A PCT level of less than 0.25 ng/dL is felt to represent absence of bacterial infection and strongly supports immediate cessation of antibiotic therapy. A fall of greater than 75% in serum PCT levels or a PCT level of less than 0.5 ng/mL are considered to represent resolution of infection and support cessation of antibiotic therapy.
Objectives: To determine the relationship between PCT and CRP levels in critically ill patients with viral respiratory tract infections. 2. To evaluate the benefit of PCT testing to guide antimicrobial therapy in patients with respiratory tract infections in ICU.
Methods: Patients with a positive respiratory viral PCR admitted to our intensive care unit were retrospectively identified from January 2015 to April 2019. CRP and PCT levels on day 1, 3 and 5 were analysed for each patient. Patients with at least 1 CRP and PCT level were included.
Results: 37 patients were identified for analysis. In 18 patients (48.65%) PCT testing supported discontinuation of antibiotics, in 7, 6 and 5 patients on day 1, 3 and 5 respectively. In patients where antibiotic cessation was recommended on day 1, mean and median CRP levels were 139.89 and 145.2 respectively. In patients where cessation was recommended on day 3, mean and median CRP levels were 114.1 and 142 respectively. In total, 8 patients had PCT levels supporting cessation of antibiotics while concurrent CPR levels were greater than 100. PCT testing supported cessation of antibiotic therapy in one patient with rising CRP levels and supported continuation of antibiotic therapy in 4 patients with falling CRP levels.
Conclusions: Our data suggested that CRP and PCT levels varied independently in our patient population. In particular, there was a subset of patients with very low PCT levels on day 1 where there was no suggestion of bacterial infection in spite of significantly raised CRP. Considering the delay in obtaining respiratory PCR results for up to 72 hours, PCT testing may assist in identifying patients with isolated viral infections where antibiotic therapy is not indicated, often where CRP testing alone would support continued use of antibiotics. In the presence of a positive viral PCR result, elevated PCT may support continued use of antibiotic therapy where CRP results may be ambiguous.
0318
Gain in Insight Whilst Gaining in Skill: The Hidden Bonus of Clinical Simulation for Critical Care Staff
Alasdair Munro, Vipal Chawla, Rahul Sarkar and Manisha Shah
Medway Maritime Hospital, Gillingham, United Kingdom
Abstract
Introduction: Medical simulation has been shown to be effective in teaching critical care medicine.1 In our hospital, a simulation-based training program was designed for multidisciplinary critical care staff to address clinical skills and knowledge. We report an important learning outcome from these sessions.
Objectives: To observe the change in self-assessed competence and confidence level in different clinical domains within staff group sessions following attendance in clinical simulation.
Methods: High fidelity clinical simulation scenarios was provided for staff; based on real life clinical incidents in the hospital. Simulation sessions were led by a specialty doctor, supervised by the consultant in intensive care, beginning with a short introductory lecture and followed by a debrief session. Not all candidates underwent all simulation scenarios. Sessions were spread over a 10 months from October 2018 and are currently ongoing.
Trainees ranged from foundation year doctors to year 6 specialty trainees and nurses (band 5–7) in critical care. They filled out a Likert scale questionnaire (1-10, 1 = completely unconfident, 10 = fully confident) for confidence before and after the sessions. Competence was measured with a self-assessed graded response (“not competent,” “needs direct supervision”, “needs indirect supervision”, “independent”, “happy to teach”) on clinical domains related to each scenario.
Scenarios included the management of; acute hypotension, acute respiratory distress syndrome, rapid sequence induction (RSI), displaced endotracheal tube and tracheostomy tube, pneumothorax, central venous catheter (CVC) insertion complications and non-invasive ventilation (NIV).
Results: Fifty-six candidates underwent training. Median of 7 candidates per scenario. Self-assessed average numeric confidence decreased in three scenarios (1-10 score); in RSI from 7.5 to 6.6, pneumothorax management from 6.6 to 6 and CVC line insertion complications from 5.6 to 4.6. Confidence mainly dropped in the junior cohort except in CVC line complications. In all other scenarios, confidence increased on average by 1.7 with greatest increase of 4.1 following NIV simulation.
Despite the fact that groupwise confidence decreased in pneumothorax related scenarios, it was noticed that self-assessed competence improved, with no one feeling “not competent” post-session, whilst 2 candidates felt “not competent” pre-session. Following RSI and managing CVC complications self-assessed competency remained similar or decreased.
Conclusions: The confidence and competence following simulation-based training improved in general. During three specific scenarios there was a reduction in confidence and minimal improvement in competence. Confidence decrease in this cohort could be explained by the Dunning-Kruger effect2, which explains how a learner’s confidence may initially go down in the initial phase of acquiring new knowledge and skill. This suggests candidates may need frequent training and experience to build competence and confidence having gained insight.
Furthermore, Simulation sessions may provide the space for open transparent discussion to generate psychological safety among trainees, where they could express their actual competence level without fear of being judged by colleagues.
Critical care staff not only gain in their knowledge and skill base through simulation based training, but also make a gain in insight in certain clinical scenarios they may previously been overconfident in – this phenomenon may have significance in enhancing patient safety within critical care.
0320
Caring for the Homeless individual in Critical Care; A Quality Improvement Project
Amy Silver
Manchester Royal Infirmary, Manchester, United Kingdom
Abstract
Homelessness is a prominent issue in Manchester. Manchester Royal Infirmary is a large, inner city hospital, and sees an ever-increasing number of homeless, or at risk of homelessness, individuals. Admission to hospital can also directly impact on benefit payments, ability to present to local services, and difficult behaviours. Homeless service users are often described as ‘tri-morbid’ and often, alongside their presenting complaint, will have accompanying physical and mental ill health, and issues with substance use.
An informal discussion was completed across the Critical Care MDT to identify areas for improvement. Two key issues were:
1. There had been no formal guidance provided in North West Critical Care Units surrounding the best way to manage these patients, despite the rising amount of admissions of those of no fixed abode and a number of readmissions.
2. There was a lack of staff education regarding what services were available, and little in-reach from other services
Therefore, a quality improvement project was conducted to both improve patient experience, and work on staff education. A retrospective audit of homeless patient admissions to Critical Care was carried out and a minimum data set created to provide an accurate description of care, and to inform the ongoing project.
The data audited was collected via ICNARC and the Clinical Information System (CIS), between 2017–2019. It showed that there was an escalating admission rate of homeless patients, and high readmission rate; three patients accounted for fifteen admissions. The average length of stay was around six days, with 2.5 organs supported. The majority of the admissions were male, and between the age of 20–51. 86% of the patients were discharged from Critical Care, but only half of the patients identified were registed to a GP or primary care centre, thus making them vulnerable to readmission.
Working with the Homeless in-reach team, I was able to design and implement a care plan to be embedded via my unit's online observation system for staff to use. Bedside teaching was employed to educate staff, and a flow sheet was designed to guide staff as to what to do if these patients wished to discharge themselves from Critical Care. A study day for medics and nurses was carried out on the topic to relay the data and present a forward strategy for our homeless admissions.
The presentation will demonstrate the demographic of our homeless population who are admitted to Critical Care; what has been done to improve our response to the issue of homeless in Manchester; and how this has positively impacted on staff/patient relations.
| Number of serotonergic agents | Pre-admission | Additional during ICU admission |
|---|---|---|
| 0 | 52% (n=26) | 22% (n=11) |
| 1 | 30% (n=15) | 22% (n=11) |
| 2 | 10% (n=5) | 34% (n=17) |
| 3 | 6% (n=3) | 10% (n=5) |
| 4 | 2% (n=1) | 10% (n=5) |
| 5 | 2% (n=1) |
0321
Incidence of serotonergic agent usage in a critical care population
Ashleigh Taylor, Neil Brain and Alistair Meikle
University Hospital Crosshouse, Kilmarnock, United Kingdom
Abstract
Objective: Serotonin toxicity ranges in severity from mild to severe with a spectrum of symptoms from tremor and agitation, through to clonus and seizures. It may be diagnosed using the Hunter Criteria. (1) It can be triggered through inhibiting reuptake (sertraline), stimulating release of (tramadol), reducing metabolism of (selegiline) or mimicking the action of serotonin at its receptor site (mirtazapine). There is a well-documented interaction between selective serotonin reuptake inhibitors (SSRIs) and proton pump inhibitors (PPI), which reduce their metabolism by inhibition of cytochrome P450 subsequently increasing serotonin levels further. (2) During critical illness patients are often commenced on multiple serotonergic agents, which can interact, resulting in adverse effects such as delirium and agitation.
The aim of this study is to identify the incidence of serotonergic agent usage in patients prior to admission, and to determine how many new agents are commenced during their ICU stay.
Methods: We retrospectively reviewed casenotes of 50 patients admitted to University Hospital Crosshouse intensive care unit (ICU) over a 3-month period from May to July 2019. The hospital clinical information system and electronic prescribing software were used to review pre-admission medications, serotonergic drugs commenced during ICU stay, and discharge medications. Patients admitted on the combination of a PPI and SSRI were recorded.
Results:
Figure 1 – Use of serotonergic agents prior to and during ICU stay
The most commonly commenced agents included alfentanil (46% n = 23), haloperidol (32% n = 16), ondansetron (26% n = 13) and oxycodone (24% n = 12).
22% (n = 11) of patients died. 34% (n = 17) remain hospital inpatients. 4 patients were discharged home on a new serotonergically active agent (2 on mirtazapine, 1 on oxycodone and 1 on gabapentin).
5 patients were admitted on a combination of PPI and SSRI and 2 were commenced on this combination during their admission.
Conclusions: As seen above nearly half (48%) of the patietns admitted were on a seotonergically active medication and over three quarters were started on at least one additional agent. 56% (n = 28) were commenced on 2 or more new agents. This highlights both the growing use of these drugs in the community and how frequently we start serotonergic agents in ICU. Given the non-specific nature of the symptoms of serotonin toxicity it is unlikely to be diagnosed without active consideration. Clinicians should be particularly wary of patients already on multiple agents when commencing new therapies.
0322
Readmission to the Intensive Care Unit: A structured case series review
Geoffrey Ball1 and Jeremy Bewley2
1University Hospitals Bristol NHS Foundation Trust, Bristol, United Kingdom
2University Hospitals Bristol, Bristol, United Kingdom
Abstract
Background: Readmission to the intensive care unit (ICU) is associated with increased morbidity and mortality as well as increased length of hospital stay and associated costs. Readmissions within 48 hrs are monitored as an ICNARC quality indicator. We have noted a rise in unplanned readmissions to our intensive care unit in the past year prompting this piece of work. Numerous studies exist assessing factors associated with ICU readmission however specific guidelines regarding detailed discharge criteria are unusual.
Methods: We conducted a structured case note review of patients readmitted to our intensive care unit from March 2018- March 2019. We focussed on timing of discharge, illness severity at discharge (measured by NEW score and SOFA score), diagnosis and organ support requirement causing readmission to ICU and unit dependency at the time of discharge. The aim was to characterise factors associated with readmission to our unit.
Results: There were 45 readmissions to the intensive care unit in the 1 year study period. 15 patients were readmitted early (within 48 hours) (2.1% of discharges). 35/45 overall and 11/15 early readmissions were among surgical patients, the majority following major surgery.
There were no discharges at night (2200-0600) within the audit period. 18/45 readmissions and 5/15 early readmissions were discharged within 48 hours of admission.
No patients had required Invasive ventilation or renal replacement therapy within 24 hours of ICU discharge however among early readmissions 3/15 had required vasopressors within 24 hours. 10/45 overall and 6/15 early readmissions had a SOFA score of >4 at discharge.
The majority of readmissions appeared to occur either due to a surgical complication requiring return to theatre (19/45 overall and 5/15 early) or development of respiratory failure requiring respiratory support (16/45 overall and 8/15 early).
12/15 Early readmission occurred where the patient was discharged on a day when the intensive care unit was at or over maximum dependency.
Conclusions: The main factors noted within to be common among early readmissions to intensive care were; discharge within 48 hours of major surgical procedure and ongoing organ dysfunction at the time of discharge based on SOFA score. This raises the possibility of writing guidance on discharge criteria that includes expected periods of ICU observation care following different surgical procedures and cut of illness severity scores.
The most important reason for readmission to ICU was the development of respiratory failure. Possibly consideration of factors that are not so readily identifiable from patient notes such as frequency of repositioning, suctioning, physio and adequacy of analgesia needs to be considered to predict patients who may deteriorate rapidly from a respiratory point of view on ward discharge.
We hope to use this to guide further work comparing successful discharges with readmissions to help guide practice and reduce readmission rates.
0323
Central venous heat exchange catheters and incidence of venous thromboembolism in adult Burns patients
Judit Szent-Ivanyi
Chelsea and Westminster Hospital NHS Trust, London, United Kingdom
Abstract
Introduction: Central venous catheter placement is known to be associated with an increased risk of venous thromboembolism (VTE) amongst critically ill burns patients.1 The use of central venous heat exchange catheters is becoming increasingly prominent in this cohort, who often require targeted temperature control techniques to mitigate against the adverse multi-organ system effects of burns-associated thermodysregulation. Despite being at high risk of VTE, pharmacological thromboprophylaxis is often contraindicated in high percentage total body surface area burns patients, due to burns associated coagulopathies and risk of bleeding in the context of extensive surgical debridement. Multiple studies have demonstrated an increased incidence of VTE in association with larger diameter central venous catheters4 and also with central venous heat exchange catheters,2,3 but none have investigated the incidence in the critically ill burns cohort.
Objectives: The aim of this audit was to establish the incidence of VTE associated with the placement of central venous thermoregulatory catheters and the fidelity of our practice to manufacturers guidance in the use of such catheters in adult burns intensive care patients.
Methods: The audit was conducted at Chelsea and Westminster Hospital, Burns intensive care unit. A systematic review of patient notes and radiology reports was undertaken using the local electronic patient record system; all records of admissions to Burns ICU between 12thApril 2017–31stMay 2019 were reviewed. The primary outcome was the rate of VTE in patients with Thermoguard XP central venous heat exchange catheters. Inclusion criteria were as follows: adult patients (>18 years old);admitted to Burns ICU; Thermoguard XP catheter placement.
Results: 87 patient records were reviewed; 66 were excluded. Amongst the 21 patients included in the study, the total number of Thermoguard catheters inserted was 39. The average number of days in situ per device was 5.46 days. The number of confirmed VTE was 2 (incidence per patient 9.5%; incidence per device inserted 5%). Pharmacological thromboprophylaxis was administered in 11 cases (n = 11 (53%) vs n = 10 (47%)), with 7 cases having a documented contraindication to anticoagulation (documented contraindication n = 6 (28%) vs no documented contraindication n = 15 (39%). Of the 2 cases of VTE, 1 received no anticoagulation and 1 partially (suboptimal) anticoagulated; in both cases the device was in situ for >4 days.
Conclusions: Our unit has an incidence of VTE in keeping with published data in respect of Thermoguard catheter insertion. The study highlights the need to have a high index of suspicion for VTE in patients when using central venous thermoregulatory catheters; as well as careful consideration of the use of pharmacological thromboprophylaxis and the expeditious re-establishment of such therapy at the resolution of contra-indication to minimise the risk of VTE. Concurrently, our audit demonstrated catheters remained in situ for >4 days (outside manufacturers guidance) in 57% of cases (n = 12). Alongside the optimisation of pharmacological thromboprophylaxis, this is an area to be targeted in the creation of a de novo protocol to assist use of the Thermoguard XP. It has been suggested that patients should routinely undergo Doppler ultrasound investigation at the resolution of critical illness.
0325
Avoiding a Trache Situation: A review of Physiotherapy practice to minimise the use of tracheostomies on an adult Cardio-Thoracic Critical Care Unit
Dalia Barghouthy, Anna Makower and Laura Breach
University Hospitals of Leicester, Leicester, United Kingdom
Abstract
Introduction: Tracheostomies are frequently used on adult intensive care units (ICU) around the country1 and there is a paucity of literature on the topic of tracheostomy avoidance and physiotherapy. The most common reasons for tracheostomy are airway protection, bronchial hygiene and to facilitate weaning from mechanical ventilation (MV). However, half of all airway related deaths were attributed to tracheostomy complications in the ‘On The Right Trach’ NCEPOD report (2014).2 Therefore, we raised the question could some tracheostomies be avoided?
Aims and Objectives: To establish whether pro-active evidence based physiotherapy interventions contribute to minimising the use of tracheostomies on an adult intensive care unit. Furthermore, does minimising the use of tracheostomies reduce length of stay on both the ICU and ward?
Method: All patients were screened via medical notes, handover and multi-disciplinary team (MDT) discussion, between April and December 2018. Inclusion criteria included; patients that were identified as requiring a tracheostomy for bronchial hygiene, to facilitate weaning from mechanical ventilation and those who were at risk of reintubation having undergone one trial of extubation. An MDT approach was fundamental in collaborating practice, such as early extubation in an attempt to avoiding a tracheostomy. These patients received exercise (42%), rehabilitation with ETT (17%),3 intermittent positive pressure breathing (IPPB) (24%),4 mechanical insufflation-exsufflation (2%) and non-invasive ventilation (13%).5 Patients excluded were those that had; upper airway abnormalities, progressive neurological condition, Glasgow Coma Scale (GCS) <9, pre-existing tracheostomy or patients receiving Extracorporeal Membrane Oxygenation (ECMO).
Results: A total of 21 patients met the inclusion criteria. Of these 21 patients, 19 did not receive a tracheostomy as a result of physiotherapy and non-invasive ventilation. Therefore 90% of patients that were identified as requiring a tracheostomy did not go on to receive one. Furthermore, a difference of 24 ICU bed days and an additional 10 ward bed days on median average was demonstrated within the tracheostomy avoidance group in comparison to the patients in the tracheostomised group. Our project did involve small numbers of patients in both the tracheostomy and tracheostomy avoidance groups; therefore this is an important factor to consider when evaluating the impact on length of stay. We were unable to avoid a tracheostomy in two patients during the project period. Both of these patients presented with diaphragmatic dysfunction post-surgery, which was not identified until post extubation.
Conclusion: Physiotherapy intervention contributes to minimising the use of tracheostomies. Reducing the number of tracheostomies may reduce ICU length of stay, therefore having positive financial implications. Further work is required to assess the wider economic impact of this practice.
Given that no uplift in staffing was required, we believe this approach could be easily adopted within similar centres, with appropriate skill mix and equipment. The emerging topic of research into inspiratory muscle training could compliment further research into tracheostomy avoidance, particularly given the impact of diaphragm impairment within this project.
0326
Different models of physiotherapy weekend working in Critical Care and the impact on physiotherapy-led rehabilitation provision and associated costs
Alicia Fernandez Butler, Claire Bradley, Susannah Betteridge and Charles Reilly
King's College Hospital NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Benefits of early physical rehabilitation following critical illness are well documented; demonstrating improved patient outcomes and reduced hospital costs (1-2). NICE (3) and GPICS (4) recommendations support this; however, delivery is dependent on staff and resources. Additionally, NHS England’s 5-Year Plan (5) for seven-day service provision is driving therapy service transformation to create the safest, highest quality health and care service.
Our department’s locally-agreed target for Critical Care is a minimum of 5 active physiotherapy sessions per week according to patient need. Subsequently, a change to seven-day working occurred between July and November 2018.
Objectives: To explore different models of weekend working for Physiotherapists on Critical Care, reviewing the impact on physiotherapy-led rehabilitation provision and financial implications.
Method: Three models of Critical Care physiotherapy weekend service were reviewed over 9-week periods, across 4 Critical Care Units, March to November 2018.
• Model A: 3 respiratory physiotherapists (overtime rates of pay)
• Model B: 4 Critical Care specialist physiotherapists (receiving enhanced pay)
• Model C: 2 Critical Care specialist physiotherapists and 1 respiratory physiotherapist (2 receiving enhanced pay, and 1 receiving overtime rates of pay)
Model C was pragmatic due to organisational restructure, and reviewed at 6 months to assess further changes.
The numbers of physiotherapy-led rehabilitation sessions missed per week were collected retrospectively using ward book data.
Financial impact and yearly forecast expenditure was calculated based on:
• Mid-scale pay point Band 6 (including higher cost of living allowance) on previous Agenda for Change scale (AfC) at overtime (Models A and C) and enhanced pay rates for weekend working (Models B and C)
• Mid-scale pay-point Band 6 and Band 5 annual salary on previous AfC scale (Model B)
Results: Across all 4 units, within the 9 week period, the mean number of weeks the standard was met in Model A was 11% (1 /9 weeks), Model B 72% (6.5/ 9 weeks) and Model C was 42% (3.75 /9 weeks).
Rehabilitation provision improved from Model A to B, with an overall increase in number of weeks (1 to 6.5) meeting the standard by 61% and a reduction of missed sessions per week by 85% (24 to 3.5).
Between models A and C, compliance to the standard increased by 31% (1 to 3.75 weeks) being sustained at 6 months. Number of missed sessions per week reduced by 52% (24 to 12), however this was not sustained at 6 months, with a gradual increase to near Model A levels (12 to 18).
Compared to Model A, Model B required significant investment to employ 2 additional physiotherapists, and a change in weekend costs to enhanced pay. Through redistribution of existing staff, financial savings were achieved adopting Model C.
Conclusions: Service restructure to an enhanced seven-day critical care physiotherapy service leads to improvements in physiotherapy rehabilitation provision and financial savings. However there is a need for appropriate investment to sustain efficient service delivery long-term, alongside ongoing review of current practices and re-evaluation of service targets in-line with current guidelines.
0327
Beyond the theory clinical practice gap – an ongoing reflection of an Advanced Critical Care Practitioner programme
Sue Faulds1 and Sonya Stone2
1University of Southampton, Southampton, United Kingdom
2Academic Department of Critical Care, Portsmouth Hospitals NHS Trust, Portsmouth, United Kingdom
Abstract
Advanced Critical Care Practitioner’s are defined by the Faculty of Intensive Care Medicine as “clinical professionals who have developed their skills and theoretical knowledge to a very high standard.” Following a two years curriculum designed by the FICM, the partnership between the Higher Education Institution (HEI) and the Local Clinical Education Leads is key to success. This presentation reflects on work to date, firstly with the HEI’s perspective and then the ACCP’s (as a student and a qualified ACCP).
The academic’s perspective.
Working and educating in the field of advanced practice is challenging. Firstly no-one can really define advanced practice even though many have tried but there are three commonly referred to parts (1) clinical knowledge (2) decision making and (3) clinical competence. The ACCP needs to be a master of all of these and the education component of their programme needs to support their development, not only the knowledge and skill but the critical thinking and the attitude required to push boundaries in a safe and professional manner.
The University of Southampton commenced the educational element of supporting the training of ACCP’s in 2012 working with NHS Trusts to develop 30 (and counting) ACCP’s. Fundamental to making the complex programme work was, and is the close relationship and open dialogue with Consultant intensivists to understand local need, their perception of role development to develop and sustain a programme concentrating on the three elements in the context of critical care.
The ACCP’s perspective.
Two years of clinical work, training, and MSc level education is challenging. The ACCP role was initially developed at Portsmouth Hospital NHS Trust to meet service demands and is achieving it’s desired outcome with 4 trained and 5 training (I was one of the original trainee’s).
The nature of this advanced clinical role is such that it attracts ambitious individuals with a desire to drive change and development. It is such that the ACCP role is now far more than service delivery or a filler to a rota gap, a nationally recognised starting point. It's an opportunity, an avenue to new adventures and opportunities.
The ACCP role demands hard work, resilience and ambition alongside a high level of clinical acumen and decision-making and technical skills. Two years of rigorous training, assesments and exams resulted in qualification – arguably the starting point of the biggest learning curve. Three years off the starting blocks and the development of an ACCP academic role within the HEI is starting to demonstrate the ongoing need for stronger links between theory and practice.
The future success of the ACCP role will be dependent on it’s sustainability and the continued development of those within.
Conclusion: Is it easy? No, not always, but with recognition that all elements are essential to success and that theory must underpin and inform clinical practice and clinical practice must inform theory, it works. The future needs even stronger links between theory and practice and joint appointments may well be the solution.
0328
Post-ICU Nutrition Practices: A Single Centre Experience
Tom Hollis1 and Patricia Sanz Morales2
1Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
2Kings College London, London, United Kingdom
Abstract
Introduction: Nutrition-related symptoms post-Intensive Care Unit (ICU) such as undernutrition, weakness and loss of appetite, are common (1). There are limited studies investigating the role of nutrition in rehabilitation after critical illness and the lack of specificity within the NICE Clinical Guidelines, CG83 (2), and Quality Standards, QS158, (3) reflect this.
Given that patients typically receive only 60–80% of their prescribed protein and energy targets when enterally fed on ICU, then face further nutritional deficits in the post-ICU phase (4), the potential detrimental impact on nutritional status and rehabilitation from critical illness is clear.
Objectives: To explore:
1 Local compliance with the NICE Quality Standards for rehabilitation after Critical Illness (QS158).
2 Feasibility of an alternative method of nutrition screening on discharge from ICU.
3 Knowledge and attitudes of ward dietitians towards post-ICU nutrition.
Methods: This prospective, observational service evaluation included adult (≥18 years) patients who had been on the ICU for over three days before being discharged to the ward. Data pertaining to nutrition aspects of NICE QS158 were collected, including:
• Was a structured handover provided within 48–72 hours of ICU discharge?
• Was nutrition screening undertaken on ICU discharge?
To determine the feasibility of an alternative nutrition screening method, handgrip strength was measured in appropriate patients within 72 hours of ICU discharge. The revised European Working Group definitions for Sarcopenia were used to determine nutrition risk (5). Lastly, the knowledge and attitudes of clinical dietitians towards post-ICU nutrition were assessed via electronic, anonymised survey (on SurveyMonkey®; www.surveymonkey.com).
Results: A total of 50 patients were included. 49 patients were handed over to the ward dietitian within the appropriate timeframe. Short and medium term goals were not specified for any patient. Malnutrition Universal Screening Tool (MUST) scores were recorded for 56% of patients. Scores were incomplete in 96.4% of cases, as no new weight was recorded at ICU discharge. Only 13 patients (26%) had MUST scores recorded weekly up until hospital discharge. The median MUST score on ICU discharge was 1 (0-2) and 11 (39%) MUST scores would have led to a referral to the ward dietitian. Handgrip strength was undertaken in 31 patients and 21 of these were considered sarcopenic. Two of these patients received a MUST score of 0.
The survey was sent to 90 adult inpatient dietitians, with a response rate of 17% (15) and a completion rate among those of 98%. 20% of respondents were aware of Post-Intensive Care Syndrome, 53% were not, and 27% were unsure. 73% of respondents knew about neither NICE CG83 nor NICE Quality standards QS 158. 27% knew only about NICE CG83.
Conclusions: Overall compliance with nutrition related aspects of NICE QS158 was considered substandard. Several aspects were noted locally that may improve this, including the urgent need to increase dietitians’ awareness of the evidence contributing to NICE QS158 and the use of an additional screening method to identify patients at high nutrition risk post-ICU. Further work in this area is required to understand the impact on patient outcomes.
0329
Aneurysmal subarachnoid haemorrhage: an analysis of 663 consecutive patients admitted to a regional neurosurgical intensive care unit
Andrew Baird, Georgia Kirby and Aidan Marsh
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Introduction: Despite improvements with specialised management, including endovascular coiling, aneurysmal subarachnoid haemorrhage (aSAH) remains a disease with a high mortality. Furthermore, treatment of these patients incurs a high financial cost, both within the intensive care unit and longer term. Previous multi-centre studies have identified predictors of poor functional recovery and in-hospital mortality. The mortality within the intensive care unit (ICU), and the predictive value of factors such as presentation World Federation of Neurological Surgeons (WFNS) grade, age and requirement for CSF drainage, has been less well defined.
Background/ Objectives: The aim of this study was to establish the mortality of patients with aSAH prior to ICU discharge and to determine independent predictors of ICU mortality.
Methods: Data on patients with aSAH admitted to the intensive care unit of a regional neurosurgical centre was collected prospectively between January 2011 and December 2018 using the Intensive Care National Audit and Research Centre (ICNARC) database. Electronic records of all patients coded as having aSAH were reviewed retrospectively and only those with confirmed aSAH on angiogram were included in the analysis. Demographics including age, sex, WFNS grade, length of stay and outcome at ICU discharge were extracted from the ICNARC data. Patient records were reviewed to ascertain the anatomical location of the aneurysm, treatment received (endovascular coiling or clipping) and if CSF diversion (via external ventricular drain (EVD) or lumbar drain) was performed.
Univariate and multivariate analysis of data was performed.
Results and Conclusion: The median age (interquartile range, IQR) of 663 consecutive patients with confirmed aSAH was 59 (18). 72% of patients were female. The overall mortality prior to discharge from ICU was 17.6%. 84% of patients were treated by endovascular coiling, this increased to 89.9% once those patients who died within 24 hours of admission were excluded. WFNS grading was available for 81% of patients, with 56% of those presenting with Grades 1–3 and 44% Grades 4–5. CSF diversion with EVD or lumbar drain was performed in 49% of patients. Median (IQR) ICU length of stay (LOS) was 4.85 (7.8) days and hospital LOS was 17 (13) days.
Binary logistic regression revealed that WFNS grade 4–5 at presentation was predictive of mortality. Age was not predictive, despite previous studies showing worse long term functional outcome with increasing age. Male gender was borderline predictive of mortality (p = 0.06). Univariate analysis showed that the requirement for CSF drainage was significantly higher (p = 0.003) in the group that died on ICU, however was not an independent predictor of ICU mortality in multivariate analysis. Anatomical location and number of aneurysms were not predictive of ICU mortality.
This study shows that the mortality of aSAH remains high- 17.6% of patients will die before ICU discharge. Worse WFNS grade at presentation remains the clearest predictor of mortality. Increasing age does not appear to affect ICU mortality, though may be associated with worse functional outcomes.
0330
Delivering Anaesthesia: Designing a workbook to meet Collegiate, University and Medical Student learning outcomes whilst on placements within Anaesthesia and Intensive Care
Jonathon Lowe1,2 and Helena Jennison2
1Defence Medical Services, Lichfield, United Kingdom
2University Hospitals Plymouth NHS trust, Plymouth, United Kingdom
Abstract
Introduction: With the launch of the Royal College of Anaesthetists (RCoA) competency framework for medical students1, 'Science, Skills and Safety' outlined key areas of undergraduate education that should encompass the learning outcomes for students during anaesthetic, intensive care and pain medicine placements. Although the document carries strong links to the General Medical Council (GMC) publications relating to graduate outcomes2 and professional behaviour3, it was not immediately evident if undergraduates were aware of any of the key learning objectives or if these related to both clinical placement learning outcomes or examination expectations as part of their training.
Background/Objectives: In order to review students understanding and to support them during their time in relevant placements, a workbook was proposed that would encompass the key areas of the speciality. The workbook would need to meet the requirements of the RCoA and GMC whilst also being aligned to the learning outcomes expected by the local Medical School (Plymouth University Peninsula School of Medicine) during placements or modules within anaesthesia or perioperative medicine.4
The primary objective for the workbook would be to support small group, bedside or theatre based teaching sessions through the provision of teaching topics for discussion and relevant clinical skills for students to complete when opportunities were presented. The workbook would be required to support students over two academic years.
Methods: After review of the relevant RCoA and GMC publications, a questionnaire was designed and distributed to those students currently undertaking clinical placements within anaesthesia. The questionnaire was designed to cover certain key themes that included both theoretical and practical topics related to anaesthesia, intensive care medicine and pain medicine whilst also permitting the students to outline topics they felt were related and not covered or, practical skills that were not demonstrated. Once complete, the student answers were compared with the recommended areas for study from both the GMC and RCoA in order to generate a list of subjects and skills without duplication. These were then applied to the learning outcomes expected of the university.
Results: A total of 24 student responses were used to outline a list of 11 practical skills and 15 discussion topics that were compared to the RCoA guidance. When overlaid with the university learning outcomes, a final list of 49 discussion topics and 23 practical skills were then used to generate the workbook.
Conclusions: The initial launch of the workbook proved positive with uptake by both Anaesthetic Consultants and students. It was noted that the first released workbook using all subjects in an alphabetical order may impede learning if students made limited progress and did not move beyond those topics starting with A or B. A redrafted workbook was therefore issued with clinical topics divided between essential (meeting RCoA, University and GMC requirements) and desirable (aligned to the former but not explicitly stated in the reviewed curricula) with practical skills arranged in order of requirement for foundation training competency (again aligned to GMC expectations). Review of the workbook and its uptake is scheduled for Autumn 2020.
0332
Physician level variation in admission, discharge and withdrawal of life sustaining treatment decisions in a United Kingdom Intensive Care Unit
Rowena Johnson, Matt Thomas and Ben Walton
North Bristol NHS Trust, Bristol, United Kingdom
Abstract
Introduction: Decisions to begin or end a period of intensive therapy have significant implications for patients and healthcare providers. Gaining a deeper understanding of these decisions may open up ways of improving efficiency and effectiveness of care. The extent of variation between physicians, and hence the potential for efficiency gains or better outcomes, is not known.
Background/Objectives: Southmead Hospital, Bristol has a 46 bed ICU/HDU in a 996 bed tertiary hospital. More than two-thirds of patients are admitted as emergencies. Senior medical cover is provided by a team of 22 consultants. There is no sub-specialisation within the ICU.
Our aim was to document the extent of physician-level variation in practice. Our primary objectives were to document the rates of emergency admissions, ward discharges and WLST for each consultant. Secondarily we assessed the influence of a) of discharge rates on readmission; b) of consultant experience on decision making.
Methods: Wardwatcher (Critical Care Audit Ltd) was the primary data source. We used the period between 1 December 2015 and 30 November 2017. Dates of ICU admission, medically fit for discharge decision and of any decision for WLST were matched to the consultant rota. Readmissions were classed as within 48 hours or within 7 days of discharge from the ICU. The year of qualification was used as an index of clinical experience. Pearson correlation was used to analyse association between variables.
Results: The overall mean number of emergency admissions in each 24 hour period was 4.44 (SD 0.44). Individual consultant mean admissions per 24 hour period ranged from 3.29 to 5.32.
The overall mean number of patients declared medically fit for discharge was 1.29 (SD 0.18) per consultant per day. Individual consultant mean number of discharge decisions per day ranged from 0.95 to 1.69.
Withdrawal of life sustaining treatment decisions ranged from one decision per 4.7 days worked to one decision per 30.5 days worked.
1.3% of patients were readmitted to the unit within 48 hours and 3.1% of patients within 7 days. Rates for individual consultants were 0–3.1% (48 hours) and 0–8.1% (7 days). There was no association between discharge rate and readmission at 48 hours or 7 days.
Consultant experience ranged from 12 to 37 years post-qualification. Consultants with less experience were more likely to make discharge decisions (p = 0.046). There was no association between experience and admission or WLST decisions, or between experience and rates of readmission.
Conclusions: The range of variation in practice is clinically significant and could make a difference to the efficiency of the ICU. The variation in WLST decisions has a direct impact on patient outcome and resource use.
Documenting differences in key frequent treatment allocation decisions is the first step to reducing undesirable variation. Within intensive care the sheer number of decisions and their impact the critically ill means intensivists may have the most to gain from acknowledging the fact of variation, learning from it and improving services for patients.
0334
Hand Dysfunction Following Critical Illness: an Exploratory Study
Caitlin Williams1, Kelly Morris1, Penelope Firshman2 and Alexandra Curtis1
1Department of Physiotherapy, Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
2Department of Occupational Therapy, Guy's and St Thomas' NHS Foundation Trust, London, United Kingdom
Abstract
Introduction: Survivors of critical illness often report long-term physical disability and a decreased health related quality of life. A previous study has identified shoulder impairment is highly prevalent following admission to the intensive care unit (ICU) with a significant impact on upper limb function.1 To date, no study has looked specifically at the prevalence of hand dysfunction in ICU survivors, however, those attending an intensive care follow up clinic have reported impairments including stiffness and reduced dexterity.
Objectives: To identify the prevalence and type of impairment that may result in hand dysfunction amongst ICU survivors at ICU discharge.
Methods: Forty consecutive patients with a length of stay (LOS) in ICU > 72 hours had hand function assessed at ICU discharge. Assessment comprised of a bespoke combination of hand assessment tools, included the Kapandiji score of thumb range, gross sensory assessment, and ability to contact fingertips to distal palmer crease as well as achieve full extension of all fingers and thumb. Patients were also asked if they perceived any hand dysfunction. Following initial data analysis, a further 40 patients with LOS > 72 hours had grip strength measured at ICU discharge. Additional information was also collected including age, LOS, ICU admission diagnosis, number of days with Richmond Agitation and Sedation Scale (RASS) Score of <−1, number of RASS episodes <−1, and presence of risk factors for long term hand dysfunction including presence of RA/OA, neurological condition CVA/residual weakness, pre-morbid hand injury or reduced range.
Results: At ICU discharge a change in hand function was reported by 21/40 (52.5%) of the patients. On assessment 11/40 (27.5%) had range of motion defects, whilst only 3 had sensory deficits. Seven of those affected had risk factors that may have contributed to hand dysfunction. Mild deficits occurred in 9/11 (81.8%), losing 2/10 points on the Kapandji assessment. The remaining 2 had moderate deficits, however, one had a hand pathology whilst the other an ICU readmission. Grip strength in the second cohort of patients was <80% of age and gender predicted norms in 38/40 (95%), while 11/40 (27.5%) had grip strengths <20% of age and gender predicted norms.2 There was poor correlation between grip strength and LOS (left and right R2 = 0.12) and weak correlation between grip strength and number of days with a RASS < 1 (left R2 = 0.27 and right R2 = 0.21).
Conclusions: At ICU discharge hand grip weakness appears to be highly prevalent amongst ICU survivors and may account for the number of patients who perceive a change in their hand function. Other impairments that might contribute to dysfunction, such as range of motion and sensation, were generally found to be mild. Grip weakness may be reflective of global deconditioning and ICU acquired weakness rather than a reflection of hand dysfunction in isolation. Future research is required to determine the trajectory of hand strength after ICU discharge and the relationship between this and hand function.
0336
The story of a follow up service on a shoe string!
Joanna Mann and Rebecca Carvell
University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Introduction and Objectives: ‘Given the individual impact on patients, and ripple effects on families and society in general, poor-quality rehabilitation and impaired recovery from severe illness should be regarded as a major public health issue’ (1).
It is widely recognised that post hospital discharge, Intensive Care Unit (ICU) patients experience stress, anxiety and depression, which can lead to long term psychological conditions, including Post Traumatic Stress Disorder (2). Effects of critical illness on patients and their families is modelled through four stages; uncertainty, disruption, regaining self, and regaining wellness (3), yet overcoming each stage requires support.
The Guidelines for the Provision of Intensive Care Services (GPICS) (4) recommend the psychological effects of ICU should be facilitated through the writing of a diary and the provision of patient support groups post discharge. In January 2015, Coffee Mornings for ex-ICU patients and a 'diary project' during patient admission commenced at Heartlands and Good Hope Hospitals; Backman et al. (5) recognising patients given a diary during admission, with follow up during recovery, had statistically significant higher scores in general health and vitality after six months.
Objective: Offer diaries to ICU patients’ relatives and provide follow up support at Coffee Mornings although unfunded and run by a small team of staff in their own time.
Methods:
• Diaries are offered to relatives of ICU patients ventilated more than 3 days.
• Patients invited to Coffee Mornings 2 months post hospital discharge.
• Coffee Mornings – held over a weekend, every 3 months. Support and advice sheets and a tour of ICU provided.
Results: Patients and relatives ‘have a voice’ and can express experiences and concerns. Coffee Mornings receive excellent feedback and staff sustain support for regular attendees. Feedback from Coffee Mornings is given to all ICU staff to help improve care.
Discussion and Conclusion: The psychological and physical consequences of ICU admissions for individuals goes beyond hospital discharge. Continued follow up and support is essential for effective recovery.
Although unfunded, the resilience of staff determined to provide support for patients and relatives has proven to assist recovery and subsequent feedback continues to enable staff development, therefore enhancing care for future patients.
0337
The association between initial lactate level and massive transfusion in severe trauma patients with and without traumatic brain injury
Dong Seob Kim and Dong Hun Lee
Chonnam National University Hospital, Gwangju, The Republic Of Korea
Abstract
Background: Exsanguination is fatal and a major cause of death in severe trauma patients. This study aimed to analyze the predictive performance of the initial lactate level for massive transfusion (MT) in severe trauma. Furthermore, we divided the patients according to the subgroups traumatic brain injury (TBI) and non-TBI. Methods: This retrospective study included patients admitted for severe trauma between January 2016 and December 2017. Patients with head Abbreviated Injury Scale scores greater than 3 were defined as TBI patients. Receiver operating characteristic analysis was performed to examine the prognostic performance of injury severity score (ISS), revised trauma score (RTS), hemoglobin level, and lactate level. Multivariate logistic regression analyses were performed to evaluate the relationship between MT and lactate level. The primary outcome was MT. Results: Of the 553 patients included in the study, MT was performed in 62 (11.2%) patients. The area under the curve (AUC) of lactate level for predicting MT was 0.779 (95% confidence interval [CI], 0.742–0.813). The AUCs of lactate level in TBI and non-TBI patients were 0.690 (95% CI, 0.627–0.747) and 0.842 (95% CI, 0.796–0.881), respectively. In multivariate analyses, lactate level was independently associated with MT (odds ratio [OR], 1.213; 95% CI, 1.117–1.318). Lactate level was independently associated with MT in non-TBI patients (OR 1.469; 95% CI 1.262–1.710) but not in TBI patients. Conclusions: Lactate level was an independent factor for predicting MT in severe trauma. Further, lactate level had good prognostic performance in predicting MT in non-TBI patients.
0342
SIM-IT: A Simulation-based course for Multidisciplinary ICU staff
Ravi Bhatia1, Chao-Ying Kowa2 and Joe Zhang1
1Kings College Hospital NHS Foundation Trust, London, United Kingdom
2Queen's Hospital, Barking Havering and Redbridge Trust, Romford, United Kingdom
Abstract
Introduction: Simulation is a vital part of clinical training, with multidisciplinary team (MDT)-based scenarios encouraging the development of teamwork skills between various healthcare professionals. With UK Medical SHO training transitioning from the two-year “Core Medical Training” to a three-year “Internal Medical Training” (IMT), the Royal College of Physicians has stipulated that IMT trainees should undergo Intensive Care (ICU) training and simulation-based learning (1). It is anticipated that IMT trainees will come from the foundation year programme and the majority will have had little ICU experience – this may make them unfamiliar with common issues encountered by ICU patients, and unaware of the skills of the ICU MDT. To help bridge this gap, we have designed and delivered a one-day course: Simulation for the Multi-professional Intensive Therapy Unit (SIM–IT).
Objectives: We aimed to provide participants with more confidence when dealing with common ICU emergencies, along with experience working within and developing a leadership role with teams who may have less ICU experience.
Methods: SIM-IT was aimed at doctors, ICU nurses, and physiotherapists. The programme included four common emergency scenarios both on and off ICU: cardiac arrest; total spinal; blocked tracheostomy; admission of a patient with motor neurone disease in respiratory distress. We ensured that each scenario involved a mix of MDT participants. A debrief was performed following each scenario, with an emphasis on Crisis Resource Management. The pilot course was run twice at Barts Health Simulation Suite. Participants were asked to fill out a pre and post course survey involving statements of their perceptions of various aspects of working in ICU (selection from a ten-point scale), along with the option of free text. We used a paired-samples Wilcoxon test to compare pre and post-course ratings.
Results: A total of 14 participants (2 Physiotherapists, 5 Nurses, 7 Doctors) attended SIM-IT. There was a statistically significant increase in participants' confidence working in an ICU setting (p = 0.016, median scores 6 to 8), confidence in approaching the deteriorating ICU patient (p = 0.005, median scores 6.5 to 8), and how well they understood their role in the ICU setting (p = 0.005, median scores 7 to 8). Participants felt that the skills gained from the course were beneficial in their practice (median score 9), with one commenting that it was a "brilliant course, so beneficial to do as MDT". Interestingly, participants' perceptions of the roles of ICU MDT staff were unchanged.
Conclusion: Overall, the course was highly rated by participants and successful at increasing confidence at managing unstable ICU patients. Participants found the MDT simulation experience valuable. The participants' median ICU experience was 11 months, which could explain why no significant change in perceptions of the roles of ICU MDT staff was observed. Given the positive feedback received and the findings from the data, we would hope to run SIM-IT for all ICU novices including those in non-training posts starting ICU.
We thank UCLPartners, NHS Health Education England, and the team at Barts Health Simulation for their support.
0343
The relationship between lactate, critical care admission, and death amongst patients in the Royal Infirmary of Edinburgh. Should patients with high enough results get automatically referred to critical care?
Callum Taylor, Christopher Black, Murray Blackstock, Neil Young, Kenneth Baillie and Gregor McNeill
NHS Lothian, Edinburgh, United Kingdom
Abstract
Introduction: Serum lactate measurement is recommended for the assessment of acutely ill patients by national (1) and international guidance (2).
Often described as a surrogate marker for tissue hypoperfusion (2), raised serum lactate levels appear to predict in-hospital mortality. (3) The Surviving Sepsis Campaign recommend checking serum lactate within one hour of suspecting sepsis, and using the result to guide therapy (>4 mmol/L as a trigger for fluid resuscitation). In the Royal Infirmary of Edinburgh, Intensive Care are considering advising other hospital specialities to use a raised serum lactate over a certain threshold, as a trigger for referral to critical care.
Objectives: We completed an audit of lactate samples taken over one year at the Royal Infirmary of Edinburgh (RIE) to determine whether raised serum lactate was associated with increased mortality or admission to critical care for our patient cohort.
This is part of a quality improvement project aimed at improving the assessment of deteriorating patients in Edinburgh, looking at the feasibility and potential benefits of raised serum lactate prompting critical care referral and review.
Methods: We obtained laboratory lactate results from the TrakCare Patient Management System, for the financial year 2018/2019.
Inclusion criteria were all laboratory samples from patients taken in a ward setting (including medical and surgical receiving units). We excluded all samples taken in critical care (General and Cardiothoracic HDU and ICU). For each attendence, we selected the maximum lactate result.
Data was analysed using R version 3.5.2.
Results: We identified 13444 samples, and 6204 unique hospital attendences. The three most commonly occuring specialities were General Medicine (2513 patients), General Surgery (889), and Obstetrics (618).
Table One provides the total patient numbers and figures for percentages seen in Figure One.
Figure One demonstrates the relationship between serum lactate and patient percentages for mortality and critical care admission.
Among the more common diagnoses (>=10 cases in the RIE/year) the highest median lactate was seen with “Vascular disorder of intestine” (4.4 mmol/L), with 40% patient mortality and 20% admission to critical care. “Other complications of labor and delivery”, had the third highest median lactate (2.45 mmol/L), with zero deaths/critical care admissions.
A threshold of 4 mmol/L for lactate (the value used by the Surviving Sepsis Campaign), to highlight patients at risk of admission to critical care or dying, would have a: Positive Predictive Value of 0.45, Negative Predictive Value of 0.82, Sensitivity of 15%, and Specificity of 95% for our dataset.
Conclusion: 10% mortality amongst all patients is high, and likely reflects bias in who receives lactate sampling on the ward. Accepting this limitation, our cohort does demonstrate a relationship between increasing maximum serum lactate and proportion of deaths.
45% of patients with a maximum lactate greater than 4 mmol/L later died or were admitted to critical care.
It may be appropriate to not admit patients with raised lactates to Critical Care, depending on other factors. Our next project will look at undifferentiated patients in the emergency department, and critical care reviews, to assess whether earlier review can be achieved for higher risk groups.
0344
Advancing Use of Ultrasound for Assessment of Shock in Low Resource Environments
Nelson Kamali1,2, Nicholas James3 and Menno Bakker1
1Mae Tao Clinic, Mae Sot, Thailand
2York Teaching Hospital NHS Foundation Trust, Scarborough, United Kingdom
3North Lincolnshire and Goole NHS Trust, Grimsby, United Kingdom
Abstract
Introduction: Point of care ultrasound (PoCUS) is used frequently in emergency and critical care medicine in high income countries. It is increasingly used in low to middle income countries as a cost-effective imaging investigation, predominantly in obstetric medicine.1 However, there is little literature on the use of ultrasound in guiding treatment of critically unwell patients in resource poor settings2,3.
We conducted a feasibility study at a low resource medical facility, delivering intensive teaching to non-physician healthcare workers with basic ultrasound skills.
Background: The Mae Tao Clinic provides medical care to marginalised and displaced people at the Thai-Myanmar border. It offers basic critical care treatment consisting of oxygen, intravenous fluids (including blood products) and antibiotics; however lacks invasive haemodynamic monitoring and advanced imaging. Treatment is provided by locally trained staff who diagnose and treat a broad range of conditions including severe illness such as heart failure, sepsis and shock.
Differentiating the cause of shock is often challenging due to mixed pathology, conflicting clinical signs and limited access to diagnostic imaging. Our aims were to both improve knowledge in treating undifferentiated shock and assess if these techniques could be taught simply in a sustainable fashion to those working in low resource settings.
Methods: Teaching involved didactic methods that included physiology and interpretation of ultrasound findings, followed by a practical session on identifying important landmarks. Ultrasound findings focused on IVC diameter and respiratory variation, aorto/caval index and visually estimating cardiac function.4 Participants were divided into two groups, locally-trained healthcare workers (LHWs) and those with a Western medical education (senior medical students and volunteer doctors).
The study was reviewed and approved by the health management team and senior healthcare workers. It was deemed unethical to use a control group that did not receive any teaching as this would deprive local staff of educational opportunities. Therefore baseline and post-teaching questionnaires and knowledge tests were devised.
The questionnaire assessed subjective confidence in assessment of shock with PoCUS using Likert-type scales. The knowledge test used a single best answer (SBA) format test to assess effectiveness of teaching. Significance testing was performed with student’s t-tests.
Results: Eleven LHWs and four western educated participants were enrolled. All enrolled subjects completed the formal training.
Baseline and post-teaching questionnaires were returned in 8 participants in the LHW group demonstrating an improvement in subjective confidence in assessment of shock from a mean of 62.5% to 78% (P = <0.0001).
Baseline knowledge scores for 11 participants in the LHW group averaged 25.9% and improved to 60.1% post-teaching (P = 0.0002). Four participants were assessed in the Western educated group with mean score improving from 71.3% to 98.0% (P = 0.046).
Conclusions: We have demonstrated that focused teaching can improve knowledge and confidence with regards to shock assessment by LHWs. In addition, this is feasible to perform in resource poor healthcare settings. Further study is needed to assess knowledge retention and the impact on health outcomes.
0345
Optimising blood transfusion practice in a critical care unit (completed audit loop)
Amit Parmar
Broomfield Hospital, Chelmsford, United Kingdom
Abstract
Objective: Blood transfusions are common in clinical practice with up to 10% taking place in the general intensive care unit. They are however associated with significant risks and complications which can worsen patient outcomes i.e. Transfusion reactions. My aim was to assess if our department adhered to current recommendations of having a restrictive transfusion strategy with a haemoglobin threshold of 70 g/L or below.
Method: This retrospective audit reviewed patient data collected from patients admitted to GICU over one month. Data available on system Metavision.
Results and changes: 10 transfusions took place in the first audit cycle of which 40% were when the haemoglobin exceeded 70 g/L. In 60% of the transfusions, two units of red blood cells was transfused. Thresholds and targets for transfusions were poorly documented with two transfusions missing documentation. I presented my findings to the department and helped educate them on current recommendations. We changed clinical practice to document indications, targets and thresholds for transfusions during ward rounds. On re-audit, 13 transfusions took place of which only 20% occurred when haemoglobin exceeded 70 g/l. There was only minor improvement in single unit transfusion from 60% to 50%. Documentation stating thresholds and clinical justifications also significantly improved.
Conclusion: This audit helped improve practice by adopting a restrictive transfusion strategy by lowering transfusion thresholds and improving documentation. This will likely reduce the number of unnecessary transfusions that take place and therefore reduce risk and complication from them.
0347
A single centre audit of rehabilitation of patients on VV and VA Extra Corporeal Membrane Oxygenation (ECMO)
Allaina Eden1, Alain Vuylsteke2, Jo-Anne Fowles2 and Katherine Atkin3
1Royal Papworth Hospital NHS Foundation Trust, Cambridge, United Kingdom
2Royal Papworth Hospital Intensive Care Unit, Cambridge, United Kingdom
3Royal Papworth Hospital, Cambridgeshire, United Kingdom
Abstract
Introduction: The benefits of commencing rehabilitation early ICU are well documented.1 Experience in rehabilitating complex ICU patients has led to confidence in waking patients on ECMO and commencing early rehabilitation. At Royal Papworth Hospital, the ECMO physiotherapy and nursing team routinely transfer patients supported on ECMO to the chair. In addition to this, the same level of rehabilitation is provided to patients on ECMO as all long term ICU patients.
Objectives: To review the amount and type of rehabilitation performed by the physiotherapy team with patients on ECMO.
Methods: We reviewed all consecutive patients supported with ECMO between April 2013 and October 2017 and evaluated participation in active rehabilitation, using the Chelsea Critical Care Physical Assessment tool (CPAx) to track patient’s ability and progress.2 We are reporting the highest recorded CPAx score during admission whilst on ECMO, the use of pedals, the use of tilt table to stand, and ambulation away from the bed space whilst on ECMO.
Results: 236 patients were analysed with 206 on veno-venous ECMO, 30 on VA ECMO support.
The highest CPAx score was 36 (out of 45) indicating a high level of physical ability requiring little or no assistance.
No adverse incidents were recorded.
Conclusion: Experienced multidisciplinary teams can provide a range of safe and effective rehabilitation of patients supported on either VV and VA ECMO.
| Activity | Number of patients | VV ECMO/ VA ECMO (n) |
|---|---|---|
| Sit on edge of bed | 35 | 31/4 |
| Sit to stand practise | 14 | 12/2 |
| Chair pedals | 15 | 14/1 |
| Bed pedals | 18 | 17/1 |
| Tilt table | 4 | 4/0 |
| Ambulation | 2 | 1/1 |
0348
Intensive Care Unit Ward Rounds: Audit of Task Completion
Balaji Shanmugam, Arun Prasad Ravichandran and Jayprakash Patil
The Royal Oldham Hospital, OLDHAM, United Kingdom
Abstract
Introduction: Various clinical decisions are made during the consultant ward rounds in ICU every day. It is essential that 100% of the tasks are completed by end of the given day to provide optimal patient care.1 However, to achieve that goal in the real world appears to be an unrealistic one.
Objectives: The aims of this audit were to identify the compliance of task completion in our unit, reasons for incomplete tasks as well as suggest corrective measures to improve patient safety. The authors could not find any national/international standards to compare with.
Method: Initial audit was carried out in November 2018, over a period of 5 days at 1800 hrs (end of standard day). We counted the number of tasks in the consultant daily review, and the number of tasks documented in the clinical notes as completed. Any task that was not documented was noted as incomplete. Cross checks with the staff nurse and juniors were done if an attempt was made to complete the task, and to ascertain cause for the incomplete task. The results were analyzed, recommendations were made and a Re-audit was done in July 2019.
Results: Our initial audit in November 2018 revealed that 88.2% of tasks were completed (79.7% completed and 8.4% attempted). Lack of documentation (76.19%) was the main reason for tasks being noted as incomplete, followed by lack of communication (14.2%), and work pressures (9.5%). Following the initial audit, recommendations were made and disseminated to all the staff members. These included documentation, the nurse co-ordinator to accompany the consultant ward round and the staff nurse in-charge of the particular patient for the day should be present at the bedside during the ward round. A dairy was procured and juniors were encouraged to note down all the jobs during rounds and recheck the dairy daily at 1600 hrs for any pending jobs. All pending jobs at end of the day had to be notified to consultant and nurse in-charge so that it can be noted and handed over to the next team.
A re-audit done in July 2019 showed encouraging results. The task completion was 93.85% (87% Completed + 6.8% Attempted). Overall documentation had significantly improved, lack of documentation was attributed in 44.44% of incomplete jobs this time, followed by work pressures (22.22%) and miscellaneous (33.33%). No tasks were incomplete due to lack of communication.
The reasons for tasks being attempted but left incomplete included primarily specialty team referrals.
Conclusion: This audit highlights the simple changes that can be made in day today practice to enhance patient safety. We want to iterate that although we aspire to achieve a 100% task completion consistently everyday, certain factors are beyond our control.
0349
Determinants of longer-term mortality in hospital survivors of critical illness
Thomas Clark and Victoria Lewis
Torbay Hospital, Torbay and South Devon NHS Foundation Trust, Torquay, United Kingdom
Abstract
Introduction: Patients admitted to our Intensive Care Unit (ICU) may have an excess mortality risk for over six years following admission.1 We poorly understand what the risk factors are that determine this shortening of life-expectancy.
Background/Objectives: Our primary objective was to undertake a pilot statistical analysis of patients admitted to Torbay ICU who survived until hospital discharge to identify co-variates that might be used in future analyses and also estimate a longer-term event rate for future multivariable model construction.
Methods: All emergency patients aged over 18 who were admitted to our ICU between April 2008 and April 2012 and survived until hospital discharge were included in analysis. Date of death and deprivation score data were collected for each individual patient from trust database and the follow-up period censored in July 2018. Co-variate data was obtained from our local ICNARC database (age, sex, APACHE score, pre-dependency category, IPPV and length, CVVHDF and length, ICU length of stay, hospital outcome). An accelerated failure time model was constructed. Alpha set at 0.05. Analysis completed using R studio version 3.5.0 ‘Joy of Playing’. See references for packages.2,3,4
Results: 1410 of 1929 patients admitted to our ICU survived to hospital discharge (73%). There were 595 events by censorship. Median life-expectancy was not met. See figure 1 for Kaplan-Meier curve of entire cohort. Final ‘simplest’ accelerated failure time model used age, sex, year, APACHE, IPPV, CVVHDF, pre-dependency category as well age interactions with IPPV and deprivation score as covariates (AIC 10871, loglik difference 222). The model overestimated survival. See table 2 for hazard ratios and event time ratios. Age, APACHE, deprivation score and pre-dependency categories of B and C were the five covariates with p values < 0.05.
Discussion: Our ‘best fit’ and 'simplest' model infers that age, APACHE score, dependency category B and C and deprivation score are covariates that may be correlated with a shortened survival time. This model overestimated life-expectancy suggesting that there are important covariates not accounted for that shorten survival time. Our event proportion was 0.42. This data may help future statistical study design.
Table 1.
Final model covariates with hazard ratios (HR) and event time ratios (ETR). ETR estimate the percentage change in survival time for each unit increase in co-variate.
| Covariate | HR (0.95 CI) | ETR |
|---|---|---|
| Age | 1.03 (1.02 – 1.05) | 0.96 (0.94 – 0.97) |
| Sex | 1.06 (0.9 – 1.25) | 0.93 (0.76 – 1.14) |
| Year | 1.04 (0.96 – 1.12) | 0.96 (0.87 – 1.05) |
| APACHE | 1.06 (1.04 – 1.08) | 0.93 (0.91 – 0.95) |
| IPPV | 1.60 (0.69 – 3.7) | 0.55 (0.12 – 1.6) |
| CVVHDF | 0.74 (0.52 – 1.06) | 1.45 (0.93 – 2.27) |
| Dependency B | 1.3 (1.05 – 1.62) | 0.71 (0.54 – 0.94) |
| Dependency C | 2.46 (1.70 – 3.56) | 0.32 (0.2 – 0.51) |
| Dependency D | 3.68 (0.52 – 1.06) | 0.19 (0.02 – 2.38) |
| Deprivation score | 0.82 (0.69 – 0.97) | 1.29 (1.04 – 1.61) |
| Age * IPPV | 0.99 (0.98 – 1) | 1.01 (0.1 – 1.02) |
| Age * deprivation score | 1 (1-1) | 1 (0.99 – 1) |
0350
Prediction of mortality in critically-ill elderly trauma patients: A single centre retrospective observational study and comparison of performance of trauma scores
Rebecca Egglestone, David Sparkes and Ahilanandan Dushianthan
General Intensive Care Unit, University Hospital Southampton, Southampton, United Kingdom
Abstract
Introduction: The elderly population represents the largest major trauma cohort and this is expected to continue to increase significantly over the coming decades.1 For outcome prediction, the most commonly used trauma outcome scoring systems [Injury Severity Score (ISS) and Trauma Score Injury Severity Score (TRISS)] are not specific for patients > 65 years of age. However, a scoring system which reliably predicts outcome in elderly trauma patients may allow early prognostication with objective decision-making to help minimise inappropriate interventions, particularly in an intensive care unit (ICU) setting. More recently, a new trauma scoring system specific to elderly patients [Geriatric Trauma Outcome Score (GTOS)] has been developed in the United States, which seems to perform better as a predictive model in the elderly population.2
Objectives: This study looks at the ability of the injury severity scale and the geriatric trauma outcome score to predict mortality in elderly major trauma patients admitted to critical care in a UK level 1 major trauma centre.
Methods: Retrospective data was collected for all major trauma patients over the age of 65 admitted to intensive care between January 2012 and December 2017. The median ISS and GTOS between the survivors and non-survivors were compared using the Mann-Whitney U test, and the ability of the score to predict mortality was assessed using receiver operator characteristic (ROC) curves.
Results: 255 trauma patients over the age of 65 were admitted to the Intensive Care Unit during this study period. Overall 30-day survival was 76%. The difference between the ISS and GTOS scores of survivors and non-survivors were both statistically significant (p < 0.001). Both scores had a statistically significant AUROC (Area Under Receiver Operating Characteristic curve), with the GTOS performing slightly better with an AUROC of 0.68 compared with 0.66 for the ISS. Best cut-off points for ISS and GTOS were >28 and >142, respectively.
Conclusion: In our centre the GTOS performed slightly better than the ISS. However, the AUROC for GTOS was significantly lower than both the original publication and the follow up validation.3 Further prospective work to investigate prognostication for this group of challenging patients with the European Trauma experience would be valuable.
Figure 1.
Kaplan-Meier curve for entire cohort.
0352
Impact of a post critical illness follow up Health and Wellbeing programme on patients recovery
James Bruce1,2, Lorraine Henderson2 and Thomas Clark2
1Intensive Care Society, London, United Kingdom
2Torbay and South Devon NHS Foundation Trust, Torquay, United Kingdom
Abstract
Introduction: Exercise limitation, physical and psychological sequelae, decreased physical quality of life, and increased costs and use of health care services have been observed 5 years post ICU survival within an ARDS population (1) Torbay hospital Intensive Care Unit utilises a follow-up Health and Wellbeing rehabilitation programme to improve functional and physical recovery following critical illness.
Methods: Cohort analysis of all patients invited to attend a Health and Wellbeing programme as part of their post-ICU outpatient follow-up. All patients admitted to Torbay ICU are screened using a NICE 83 guideline screening tool. All patients who are deemed of high rehab need undergo a comprehensive assessment of their physical and non-physical needs. At discharge from the acute hospital these patients are encouraged to attend an outpatient-based health and wellbeing exercise program. Patients are screened by a rehabilitation fitness instructor and an Occupational Therapist to set their goals and explore their motivations to recover.
The group consists of an exercise-based program, with informal discussions about home transition and psychological recovery. Outcomes are taken at session 1 and at session 6. ‘6-minute walk distance’ (metres) and ‘Time to get up and go’ (seconds) are measured pre and post programme as objective markers of change in exercise capacity. ‘Self-assessment of ADL ability’ (6 questions, scale 10–60), ‘Extent of physical recovery’ (%) and ‘Extent of psychological recovery’ (%) are measured in a similar fashion as subjective markers of functional recovery. Non-parametric data compared using a paired Wilcoxon test with an adjusted alpha of 5% presumed as significant.
Results: See figure 1 (6 panel plot). 122 patients attended exercise programme in total. Median 6-minute walk distance improved from 270 m to 380 m (p < 0.001), median Time to Get-up and Go (seconds) reduced from 14 to 10 (p < 0.001) Only 7 patients did not have an improvement in their 6-minute walk distance. Median percentage physical recovery increased from 50 to 80% (p < 0.001), median percentage psychological recovery increased from 60to 85% (p < 0.001) and median ADL ability increased from 37 to 60 (p < 0.001).
Discussion: Patients who participate in our post critical illness Health and Wellbeing rehabilitation programme show significant improvements in their exercise capacity and subjective markers of well-being. It is unknown whether they would have shown this improvement without the programme. This data is not proof of treatment but rather seen as a means of quality improvement, but it is reassuring to know that patients do experience this level of recovery.
Future developments: We hope to rescore these outcomes 6 weeks after the patient’s final group session to measure if patients maintain their level of confidence and fitness.
0353
The Implementation of Physiotherapy led ‘Tracheostomy Round' in a Cardiothoracic Critical Care Area
Annie Ryan and Katherine Atkin
Royal Papworth Hospital NHS Foundation Trust, Cambridge, United Kingdom
Abstract
Objective: To describe the experience of implementing a physiotherapy led tracheostomy round (TR) on a cardiothoracic Critical Care Area (CCA).
Guidelines for the Provision of Intensive Care Services (GPICS, 2019) outline that physiotherapists should have a key collaborative role in tracheostomy weaning plans. Current practice on our CCA involves the medical team prescribing a daily weaning plan.
The aim was to implement a daily physiotherapy TR for patients with a tracheostomy. A weaning plan would then be agreed with the patient, nurse and CCA team.
Methods: Data was collected for each patient and set questions were asked each day during TR regarding weaning.
Results:
• Over a 4 month period, TR round was completed on 29 out of a possible 81 days.
• TR initially occurred on average once per week. In the later 2 months TR took place at least 3–5 days per week.
• Barriers to TR included: lack of staff, no patients with a tracheostomy and time constraints.
• Data collected shows that the weaning plan was consistently communicated within the CCA nurse. The plan was not consistently discussed with the patient or CCA medical team.
Conclusion: Current practice is not in line with the GPICS standards. The implementation of a TR is a step closer to physiotherapists having a collaborative role in tracheostomy weaning plans. A factor limiting collaborative working is the absence of central documentation of TR and absence of discussion with CCA MDT. Future work needs to focus on the establishing meaningful MDT discussion regarding weaning plans.
0357
Comparison of Dexmedetomidine and Remifentanil in patients with delirium requiring Non-Invasive Ventilation (NIV) in a UK Cardiothoracic Intensive Care Unit (CT – ICU)
Ee Lyn Chan1, Sundeep Kaul2 and Charlotte Pereira2
1Imperial College Healthcare NHS Trust, London, United Kingdom
2The Royal Brompton and Harefield NHS Trust, London, United Kingdom
Abstract
Introduction: Non-Invasive Ventilation (NIV) is commonly used as treatment for acute respiratory failure. However, the use of sedatives during NIV remains controversial. There is little published data on comparing the safety and efficacy of different sedatives during NIV in acute respiratory failure in ICU patients.
Objectives: Comparing the efficacy and safety of Dexmedetomidine and Remifentanil in patients with delirium and acute respiratory failure requiring NIV.
Methods: A retrospective single-centre observational study was carried out in a UK Tertiary CT –ICU. Data from 32 patients were collected and compared.
Results: A total of 32 patients were included. In the Dexmedetomidine group, N = 18 patients (78% male; 22–86 years) and in the Remifentanil group, N = 14 patients (72% male; 23–79 years).
Indications for NIV included Type 1 and 2 respiratory failure; most common aetiologies of respiratory failure included cardiogenic pulmonary oedema (28%; n = 9), pneumonia (25%; n = 8) and bibasal collapse (9%, n = 3). Both agents were initiated for delirium (median RASS 2).
Results are reported as Dexmedetomidine versus Remifentanil throughout;
Average duration on agent was 22.1 hours (SD = 16.6) versus 15.6 hours (SD = 13.1). Average dose used was 0.52 µg/kg/hr (0.1–1.4 µg/kg/hr) versus 0.06 µg/kg/min (0.01–0.25 µg/kg/min).
Duration on NIV was 29.8 hours (IQR 2–190) versus 19.1 hours (IQR 3–57); (P = 0.72) whilst median time to pH normalisation 6.1 hours (IQR 2–190) versus 2.3 hours (IQR 0 – 14); (P = 0.0001).
The primary end point was rate of intubation which showed no statistical significance between Dexmedetomidine and Remifentanil cohort respectively (38.9% versus 50%; P = 0.53). Tracheostomy insertion rate was 16.7% versus 42.9%; (P = 0.10) and length of ICU stay was 14.7 days versus 17.9 days (P = 0.25). Overall, mortality was 22% versus 7% (P = 0.075).
Causes of mortality that are un-related to sedation or NIV included undrainable pericardial effusion, cardiogenic arrhythmia, and sepsis related to multi-organ failure.
Conclusions: To our knowledge this is the first report of data comparing the use of two sedative agents in patients with delirium and acute respiratory failure requiring NIV in a UK CT-ICU. The use of either agent appears safe, feasible and efficacious. Difference in intubation rates were not statistically significant between the two groups, however, there were trends towards reduction in tracheostomy insertion and length of stay in the Dexmedetomidine cohort.
Our study reveals clinically significant differences however an adequately powered study is required to assess the true effectiveness of these sedatives on patient outcomes. These results supports the view that a prospective multi centred randomised controlled trial is required.
0358
Evaluation of antibiotic administration in Septic Shock patients from the Intensive Care Unit- Royal Gwent Hospital, Newport
Brianne Archer1, Tamas Szakmany2,3 and David Hepburn2,3
1Cardiff University, Cardiff, United Kingdom
2Royal Gwent Hospital, Newport, United Kingdom
3Aneurin Bevan University Health Board, Newport, United Kingdom
Abstract
Introduction: Prompt, appropriate, antibiotic administration is essential after the recognition of sepsis and septic shock since increased mortality is associated with antibiotic delay1 and insufficient antibiotic cover.2 Clear clinical guidelines have been established with targets of antibiotic delivery within one hour from meeting sepsis criteria.
Objective: This audit aims to analyse time between recognition of septic shock and antibiotic administration, assessing compliance with NICE one-hour target from meeting high-risk criterion.3 Antibiotic usage, microbiology review and course length shall be reviewed to appraise unit antimicrobial stewardship.
Methods: Data was collected from patients admitted to the 16-bed mixed adult ICU Royal Gwent Hospital, Newport. 53 patient notes accessed on Clinical Workstation (CWS) with diagnoses coded as “septic shock” from ICNARC database 01.01.2018-01.01.2019. Retrospective chart review searching; time of presentation and antibiotic administration, antibiotic used, date of microbiology review, antibiotic course length, patient outcome. Audited against NICE Clinical Guidelines (CG) 51 one-hour target3 and Aneurin Bevan University Health Board (ABUHB) antibiotic guidelines.4
Results: 35 patients coded as “septic shock” have fulfilled clinical consensus criteria for septic shock according to the Sepsis-3 definitions.5 The remaining 18 patients had sepsis according to the Sepsis-3 definitions. ICU mortality was 40.0% for septic shock and 5.6% for sepsis patients. 51.4% septic shock and 61.1% sepsis patients received antibiotics within one-hour. 51.4% septic shock patients received antibiotics resembling ABUHB guidelines. Median (IQR) time to Consultant microbiology review was 2 (2.75) in both groups. Median (IQR) length antibiotic treatment was 6 (11) days in septic shock population. The top 3 antibiotics prescribed were: metronidazole, gentamicin and tazobactam/piperacillin.
Conclusions: Clinical coding and current septic shock definitions only matched in a proportion of patients, highlighting discrepancies between research driven definitions and clinical perception. Despite a decade of education, only half of septic shock patients received prompt antibiotics before ICU admission. Further insight is needed in what organisational factors are responsible for this delay. Antibiotic checklists in ICU daily reviews would promote antimicrobial stewardship.
0359
Wheel-and-spoke expansion of peer-led resuscitation training in UK Medical schools: a national model for delivering undergraduate healthcare students Basic Life Support training
Emily Beesley1, Nicholas Coffin2, Rebecca Everitt1, Jonathan Hulme1,3, Joseph Alderman1,4 and Andrew Owen1,3
1College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2Department of Anaesthesia, Russells Hall Hospital, Birmingham, United Kingdom
3Department of Anaesthesia and Critical Care Medicine, Sandwell and West Birmingham NHS Trust, Birmingham, United Kingdom
4Department of Anaesthesia and Critical Care Medicine, Queen Elizabeth Hospital, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Background: Resuscitation for Medical Disciplines (RMD) Birmingham is an innovative peer-led Basic Life Support (BLS) training course established in 1995 at the University of Birmingham (UoB). (1) Over 24 years RMD has developed a teaching course which has grown to teach in excess of 800 UoB healthcare students annually in BLS, automated emergency defibrillation (AED) and delivery of first aid as a curriculum component of first year students’ degree programmes. Course candidates are taught by senior student peers: European Resuscitation Council (ERC) instructors trained on our dedicated instructor training programme. Competence is assessed via summative assessment for the qualification of European Resuscitation Council BLS provider status, by assessors who have been trained by RMD’s dedicated assessor training programme. (2,3) Training is overseen by a committee of experienced healthcare students.
Methods: Since 2017 RMD Birmingham has been working with other Universities to develop satellite courses under the same governance. This “Phase 1 expansion” was tested with a pilot stage delivering instructor training to 40 students at the University of Manchester in partnership with their faculty.
Following this successful pilot, RMD Birmingham subsequently partnered with the University of Bristol to deliver training to their faculty and senior healthcare students, and provide follow-on faculty support, allowing establishment of the RMD training programme at Bristol (now in its second year). In 2018, RMD Birmingham partnered with Warwick Medical School in the same manner, establishing our near-peer training model at a fourth site. Warwick’s first cohort of candidates commence their training this coming academic year.
Results: The experience gained in Phase 1 of our expansion and the pilot stages has shown that this unique model of BLS training can be readily adapted and delivered to a high standard at-scale at other University centres within the UK (see Table 1). The RMD model encompasses multiple-level oversight of training to ensure quality is maintained during expansion. RMD delivers an ERC certified qualification and are the only body to do so in the UK. In collaboration with the ERC and the UK resuscitation council RMD has gained a number of exemptions from the usual course regulations to enable the delivery of large scale courses using our framework and have become a representative course with accreditation from the Faculty of Intensive Care Medicine as well as a previous citation as an example of excellence by the GMC. Phase 2 of our expansion will follow the formal ratification of our model by the UK resuscitation council enabling our framework to be used in further expansion across the UK and enable us to confer ERC qualifications on those who are trained using this framework.
Conclusions: Our work shows that it is feasible to undertake a peer-led training course across multiple sites using a common framework without detriment to the quality of the course delivery or organisation. By gaining course recognition from U and international bodies we are able to devise a national framework for certifying BLS training at UK medical schools.
0364
Temperature Management in Cardiac Arrest Patients Admitted to Intensive Care: evaluating change in UK practice following publication of the Targeted Temperature Management Trial
Izabella Orzechowska1, Manu Shankar-Hari2,3, David Harrison1, Jasmeet Soar4, Gavin Perkins5,6 and Jerry Nolan5,7
1Intensive Care National Audit and Research Centre, London, United Kingdom
2Guy’s and St Thomas’ NHS Foundation Trust, LONDON, United Kingdom
3Peter Gorer Department of Immunobiology, King's College London, London, United Kingdom
4Southmead Hospital, North Bristol NHS Trust, Bristol, United Kingdom
5Warwick Clinical Trials Unit, University of Warwick, Coventry, United Kingdom
6Heartlands Hospital, University Hospitals Birmingham, Birmingham, United Kingdom
7Royal United Hospitals NHS Foundation Trust, Bath, United Kingdom
Abstract
Background: Until 2013, patients admitted to intensive care units (ICUs) following out-of-hospital cardiac arrest (OHCA) were typically cooled to 33°C to reduce hypoxic-ischaemic brain injury. In December 2013, the Targeted Temperature Management (TTM) trial reported similar outcomes between temperature targets of 33°C and 36°C in these patients.1 We hypothesised that there has been widespread adoption of the higher temperature target in UK ICUs, without changes in mortality, similar to practice change reported in Australian and New Zealand ICUs.2
Methods: This was a retrospective cohort study of mechanically ventilated adults admitted to ICU following OHCA, using the ICNARC Case Mix Programme database. The primary exposure was admission before vs after publication of the TTM trial. Univariable comparisons and hierarchical multivariable regression analyses were performed to assess the association of admission period with lowest body temperature, fever (temperature >38°C) and hospital mortality. Temporal trends were evaluated using segmented linear regression.
Results: There were 30,268 OHCA admissions to 230 ICUs between 1 January 2010 and 31 December 2017. We observed a significant increase in mean lowest body temperature of 1.12°C (95%CI 1.08, 1.16), from 33.6 (SD 1.8) pre-TTM to 34.6 (SD 1.6) post-TTM, with greater prevalence of fever in the post-TTM period (24.75% vs 14.66%, OR = 1.91, 95%CI 1.80, 2.03). Although there was no difference in risk-adjusted mortality (OR = 1.00, 95%CI 0.97, 1.04) between the pre and post-TTM periods, the trend of decreasing crude mortality seen before publication of the TTM trial has reversed after December 2013. Temporal trends for mean hospital mortality and mean lowest body temperature are shown in Figure 1 and Figure 2, for extended dates (2008-2018).
Conclusion: Our observations show that average lowest temperature among OHCA patients admitted to UK ICUs has increased following the publication of the TTM trial, but adjusted hospital mortality is unchanged. The frequency of fever in the first 24 hours increased after publication of this trial.
Figure 1.
Temperature by month and year before vs after TTM Trial publication (unadjusted). −0.18°C change in temperature per year pre-TTM +0.19°C change per year post-TTM
Figure 2.
Hospital mortality by month and year before vs after TTM Trial publication (unadjusted). −0.54% absolute change in mortality per year pre-TTM +0.78% change per year post-TTM
| Distance walked (in meters) | Rest time required (in seconds) | Rate of Perceived Exertion | |
|---|---|---|---|
| Pre-Rehabilitation without MPV | 10 | 253 | 10 |
| Pre-Rehabilitation with MPV | 14 | 237 | 10 |
| Post-Rehabilitation without MPV | 80 | 179 | 8 |
| Post-Rehabilitation with MPV | 122 | 81 | 7 |
0365
The use of mouthpiece ventilation (MPV) to support rehabilitation in a patient with bilateral diaphragm paralysis (BDP) due to phrenic nerve injury (PNI) post lung transplantation
Liam Campbell1 and Rachel DeGiovanni2
1Specialist Physiotherapist in Assisted Ventilation, Newcastle Upon TYne Hospitals NHS Foundation Trust, Newcastle Upon Tyne, United Kingdom
2Specialist Physiotherapist in Critical Care and Respiratory Medicine, Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle Upon Tyne, United Kingdom
Abstract
Rationale: A known possible complication of lung transplant is PNI, which can lead to diaphragm paralysis. Gutierrez1 found an incidence rate of 6.9%. Dube2 states BDP from PNI is associated with dyspnoea that worsens during exertion. Exercise impairment, peak exercise reduced 40% to 60% of predicted values, is common post-transplantation but can be improved with rehabilitation as presented by Langer.3 Borel4 found non-invasive ventilation (NIV) during exercise in patients with chronic respiratory failure has found to be successful with Mehta5 finding NIV interface crucial. The need to ensure effective rehabilitation not limited by dyspnoea is necessary to prevent poor long term outcomes.
Background: 60 year old male, post lung transplantation for Idiopathic Pulmonary Fibrosis. Slow wean from mechanical ventilation due to requirement for extracorporeal membranous oxygenation, bilateral diaphragm paralysis and intensive care acquired weakness. Requiring nocturnal NIV due to hypercapneic respiratory failure. Poor exercise function limited by dyspnoea.
Objective: To ascertain if the use of MPV decreases dyspnoea and improves rehabilitation outcomes compared to no respiratory support.
Methods: A 6-minute walk test (6MTW) was performed with and without MPV, pre and post rehabilitation. The patient used MPV during rehabilitation each session, attached to a 4-wheeled walker they pushed independently. A recovery period of 24 hours given between 6MWTs with and without MPV and each 6MWT completed at the same time of day. Patient reported dysponea using the Rate of Perceived Exertion was collected. Ventilator settings were also recorded.
Results:
Whilst exercise remained limited despite rehabilitation, MPV improved total walk distance by more than 50% with a significant reduction in rest time required. Perceived exertion also diminished. Ventilator settings remained the same throughout.
Conclusion: Non-invasive ventilation is already known to reduce work of breathing and relieve symptoms of dyspnoea. This single patient case study suggests that MPV during exercise in this patient population may improve their rehabilitation outcomes and reduce perceived exertion levels. As the patient used MPV throughout rehabilitation it is difficult to ascertain the 6MWT value had they not, therefore further study with a matched control limb is required.
0366
A qualitative investigation into communication of the complex issues around subarachnoid haemorrhage between staff, patients and relatives in the critical care environment
Edel McAuley1, Helen Close2, Stephen Bonner1, Keith Hugill1, Nitin Mukerji1, Amanda Ellison3, Nasima Akhter4, Adetayo Kasim4, Manjunath Prasad1, Paul Chazot4, John Brigham4, Boguslaw Obara4, Charles Augarde4 and Lian Gan4
1Department of Critical Care and department of neurosurgery, James Cook University Hospital, South Tees NHS Foundation Trust, Middlesbrough, United Kingdom
2NIHR Research Design Service North East, Health Research Methodologist, Institute of health and society, Newcastle University, Newcastle, United Kingdom
3On Behalf Of Teesside Aneurysm Group (TAG), University of Durham, Durham, United Kingdom
4TAG, University of Durham, Durham, United Kingdom
Abstract
Introduction: Subarachnoid haemorrhage (SAH) is a devastating often unexpected illness. A relatively small incidence in the UK of 8 per 100,000 population (Linn et al, 1996) but the illness has a huge impact on individuals, their family and the overall community. SAH generally affects a greater proportion of younger people than other strokes and often has a poor outcome, it is a major cause of adult disability and employment difficulties. It has been noted that within the general population the loss of productive life years from aneurysmal SAH, is as large as that from brain infarcts, the most common type of stroke (Johnston et al, 1998). Suffering a SAH or even the detection of an intracranial aneurysm (ICA) results in many complex psychological effects, both on the patient and their family.
It is well known that it is challenging to communicate information to patients and relatives about complex medical issues, particularly within the extremely stressful critical care environment. A study by Azoulay et al, 2000 showed that half the families of intensive care unit patients experience inadequate communication with medical staff.
Objectives: Our aims are to investigate what the problems often are with communication about this condition between staff and relatives or patients. As well as raising awareness of these issues so they can be addressed. This will be done using a phenomenological approach within a qualitative framework.
Methods: A qualitative phenomenological approach was used to hold five focus groups with full ethical approval. They consisted of subjects who have had an ICA and or a SAH (affected to varying degrees) and their relatives and members of familial groups. They were all treated in the same critical care unit and hospital. The interviews explored how each individual felt about the diagnosis, treatment and recovery of their or their relative’s condition with particular refence to the communication within the critical care environment.
Results: The themes discussed by the groups covered a wide range of topics including: perceived misinformation & information deficits, the use of new technology to aid information transfer.
As well as special targeted support for certain groups, in particular children or members of a familial group. The concept of the MRI or CT scan as a therapeutic modality was raised by several patients and their families.
Conclusions: Novel points from this research included: there are often mis-understandings about this condition within the patients and their relatives in particular what exactly it is and significant confusion about either a SAH is a stroke or not?
Technology could play a larger role in passing information to patients and relative, e.g. charity websites and use of graphics.
There is a real need to target information to defined groups e.g. children and familial groups as the one size fits all approach is often not valid.
If these issues with communication can be recognized early, particularly in certain groups such as children and families with multiple affected members, this may help to avoid later perceived problems with quality of care (Korzick et al, 2018).
0367
Major haemorrhage management in a District General Hospital – enough to warrant ROTEM?
Jennifer Ridenton, Simon Gill, Christopher Pritchett and Catherine Ralph
Royal Cornwall Hospitals NHS Trust, Truro, United Kingdom
Abstract
Introduction: Viscoelastic tests such as rotational thromboelastometry (ROTEM) are growing in popularity, providing more rapid results of haemostasis when compared to standard lab tests (SLTs).1 The British Society of Haematology (BSH) has responded by issuing pragmatic recommendations to guide their use.2 This audit investigates whether, as a non-cardiac/ hepatic centre we see enough major haemorrhages to warrant adopting ROTEM into daily practice.
Methods: This retrospective study obtained data from the Royal Cornwall Hospital electronic blood bank database between June 2018 and June 2019. All patients who had four or more units of blood products requested and went on to receive a transfusion were included (n = 247). Patients transfused secondary to chronic disease were excluded (n = 38). Aetiology of bleeds was collected from electronic patient records and categorised. Averages for blood products requested were then calculated for each category.
Results: 209 patients presented with major haemorrhage requiring 4 or more blood products to be requested. Commonly presenting aetiologies from most to least were: upper gastrointestinal (UGI) bleed 39.7%, peri-operative 19.6%, rectal 9.6%, Trauma 7.2%, abdominal aortic aneurysm (AAA) 6.2%, obstetric 5.3%, disseminated intravascular coagulopathy (DIC) 4.3%, other 4.3%, elective procedure 2.9% and haematuria 1.0%.
AAA had the highest mean total of blood products requested (average of 19.3 units; 10.3 RBC, 8.1 FFP, 0.6 platelets, 0.5 cryoprecipitate) and haematuria group the lowest (average of 4 units red cells only). The DIC patient group received the highest mean number of platelets and cryoprecipitate (1.1 platelets, 2.1 cryoprecipitate). Obstetric bleeds received a lower number of FFP units compared to RBC units transfused (2.5 FFP units, 6.5 RBC respectively).
Conclusion: The BSH guidelines recommend using viscoelastic tests in key haemorrhage types potentially relevant to a DGH: Liver failure, obstetrics and trauma.
We believe this data supports the adoption of ROTEM in our DGH for the following reasons:
1. 209 patients represents a sizable cohort.
2. UGI bleeds are the most frequent cause of major haemorrhage (39.7%), many of these were patients with liver failure.
3. UGI, obstetric and trauma haemorrhages account for almost half of our major haemorrhage population (n = 109). This sub group of haemorrhages account for almost half of all FFP requested in major haemorrhage (343 units) and just over half of all cryoprecipitate used (40 units).
Recent work by Stoneham et al. has demonstrated impressive results in limiting transfusion during elective open AAA repair.3 Given the number of products requested in this group, ROTEM may help address this.
0368
Developing leadership skills in tomorrow’s intensivists through a peer-peer pedagogic resuscitation training model for medical students
Rebecca Everitt1, Emily Beesley1, Nicholas Coffin2, Jonathan Hulme1,3, Andrew Owen1,3 and Joseph Alderman1,4
1College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2Department of Anaesthesia, Russells Hall Hospital, Birmingham, United Kingdom
3Department of Anaesthesia and Critical Care Medicine, Sandwell and West Birmingham NHS Trust, Birmingham, United Kingdom
4Department of Critical Care and Anaesthesia, Queen Elizabeth Hospital, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Background: In the modern and increasingly complex NHS, leadership skills in medical practitioners are increasingly important attributes. However, teaching and training of undergraduates and postgraduates has rarely focussed on these skills, instead combining them with other professional domains such as “professionalism” or “communication”. (1) In 2014 The King’s Fund undertook a body of work completed in 2018 highlighting the problem of NHS leadership vacancies, demonstrating a lack of progression to senior leadership roles within the medical profession. (2) Only one third of NHS Chief Executives have a clinical background. (3) Since 1995 the University of Birmingham has provided peer-led resuscitation training to all of its undergraduate students. (4) This novel model of life support training has allowed the incorporation of leadership and management training for students and we describe below the experience offered to our students.
Methods: Since 1995 students at the University of Birmingham have coordinated and led peer to peer life support training. Initially devised for medical and dental students the course has subsequently expanded to other disciplines.
Leadership positions in our organisation are attained in a stepwise manner and include a competitive application process. Instructors are recruited from the cohort of students trained in the previous year. (5) Examiners and committee members are recruited from the cohort of instructors with at least 1 years teaching experience, and serve up to 3 years in this role. At graduation, students are invited to join the faculty to supervise weekly teaching, annual instructor training, and research.
Results: A team of 10 senior students form the committee, providing oversight to 75 trained instructors and 20 examiners delivering teaching and assessment to over 800 candidates per year. Overall supervision is provided by a faculty of medical doctors, all of who previously served on the student committee.
In the decade from 2008 to 2018 there were 25 graduates from our network. Of these, 8 have been awarded training posts in Anaesthesia and 3 in Intensive Care Medicine. Graduates from our group are more likely than the national average to train in anaesthesia or intensive care medicine (Figure 1).
Students from our group have presented 18 projects at national and international conferences over 7 years. Additionally, our graduates have secured 9 academic training posts at foundation or higher level, and two have obtained funding for PhD study. Several of our senior alumni are now leaders in research, resuscitation and education internationally.
Conclusions: Graded leadership experience from the University of Birmingham’s peer-peer life support training course attracts medical students to pursue training in anaesthesia and intensive care medicine, and affords them leadership experience needed to excel in research, education and training later in their careers.
0369
Understanding antimicrobial prescribing in suspected ventilator-associated pneumonia: a prospective cohort study
Callum Docherty1, Iain White1, Jonathan Bannard-Smith2, Ben Morton3, Ingeborg Walters4, Yun Xu4, Stephen Roberts1, Ronan McMullan5, Roy Goodacre4, Paul Dark1, Stephen Fowler1 and Timothy Felton1
1NIHR Manchester Biomedical Research Centre, Faculty of Biology, Medicine and Health, University of Manchester, Manchester, United Kingdom
2Manchester Royal Infirmary, Manchester, United Kingdom
3Clinical Sciences, Liverpool School of Tropical Medicine, Liverpool, United Kingdom
4The University of Liverpool, Liverpool, United Kingdom
5Queen's University Belfast, Belfast, United Kingdom
Abstract
Introduction: Ventilator-associated pneumonia (VAP) occurs commonly and is associated with significant healthcare cost, morbidity, and mortality.1 Identification of patients with VAP is difficult, resulting in over-diagnosis and excessive use of broad-spectrum empirical antimicrobial therapy.2 In addition, the clinical significance of some organisms in the airways of critically ill patients, in particular Candida species, is unknown.3
Objectives: The primary objective of this study was to identify the prevalence of laboratory-confirmed VAP in a population of patients commenced on antibiotics for suspected VAP. Secondary objectives were to: (a) identify the spectrum of causative organisms; (b) describe the associated antimicrobial therapies and; (c) explore the impact of a variety of co-variants on 30-day mortality.
Methods: A prospective, observational, cohort study was conducted across five intensive care units in the North-West of England. Participants were enrolled within 24 hours of commencing antimicrobial therapy for suspected VAP. Laboratory-confirmed VAP was defined by culture of a known pneumonia-causing pathogen at ≥104 CFU/ml or (++) for bronchoalveolar and non-directed bronchial lavage, and ≥ 105 CFU/ml or (+++) for tracheal aspirate samples.4
Variables were compared through Pearson’s chi-squared for categorical data and Mann-Whitney U tests for continuous data. Univariate logistic regression was used to analyse the impact of laboratory-confirmed VAP, APACHE II, and culture of Staphylococcus aureus and Candida species on 30-day mortality.
Results: Ninety-six patients were enrolled, of whom 67% were male, the median age was 61 (range 17–85) years, and the median body mass index 26.5 (range 16.2–48.6) kg/m.2 The median Sequential Organ Failure Assessment (SOFA) score on enrolment was 7 (range 0–15), and the mean APACHE II score was 16 ± 6. The most common ICU presenting conditions were neurological (34%), respiratory (17%), and cardiovascular (15%). The median number of antimicrobials per patient was 1 (range: 1–4).
The prevalence of laboratory-confirmed VAP was 43/96 (44%), with 50 significant bacteria identified. The most frequently cultured bacteria in patients with laboratory-confirmed VAP were Staphylococcus aureus, 18/50 (36%), Enterobacteriaceae, 14/50 (28%), and Haemophilus influenzae, 7/50 (14%). Candida species were identified in 32/96 patients (33%). The most commonly prescribed antimicrobials were β-lactams (72%), fluoroquinolones (16%), and glycopeptides (5%). Antifungal treatment (fluconazole) was administered in one patient.
Overall 30-day mortality was 22/96 (26%) and there was no significant difference between the patients with laboratory-confirmed VAP and those without (28% compared to 23% respectively, odds ratio 1.29, 95% CI 0.49 to 3.40; p = 0.80). None of the variables analysed were significantly associated with 30-day mortality, except for culture of Candida species, which was significantly associated with survival (odds ratio 0.26, 95% CI 0.07 to 0.98; p = 0.047).
Conclusions: Ventilator-associated pneumonia was confirmed in less than half the patients commenced on antimicrobial therapy for suspected VAP. To facilitate antimicrobial stewardship, improved diagnostic strategies for VAP are urgently required. In our clinical practice, we do not treat Candida species as pathogenic in VAP, and indeed, identification of Candida species in our study was not associated with excess 30-day mortality.
0370
Can the UK 24-item Family Satisfaction in the Intensive Care Unit questionnaire be used to evaluate quality improvement strategies aimed at improving family satisfaction with the ICU? A qualitative study
Susannah Lyes1, Alvin Richards-Belle2, Bronwen Connolly2, Kathryn M. Rowan2, Lisa Hinton1 and Louise Locock3
1Health Experiences Research Group, Nuffield Department of Primary Care Health Sciences, University of Oxford, Oxford, United Kingdom
2Clinical Trials Unit, Intensive Care National Audit & Research Centre (ICNARC), London, United Kingdom
3Health Services Research Unit, University of Aberdeen, Aberdeen, United Kingdom
Abstract
Introduction: The experiences and satisfaction of family members of patients are important indicators of health care quality in the intensive care unit (ICU). The Family Satisfaction in the ICU (FS-ICU-24) is a self-completed, 24-scored item questionnaire, developed in Canada and now validated in the UK, that is becoming the gold standard measure to evaluate family members’ satisfaction with the ICU.1,2 The UK FS-ICU-24 also includes three questions, at the end, inviting open-text responses.
Background/Objectives: To inform future use of the UK FS-ICU-24 to evaluate quality improvement strategies aimed at improving family satisfaction with the ICU, we set out to explore the extent to which the 24-scored items and domains of the UK FS-ICU-24 reflect common suggestions and priorities for quality improvement self-reported by family members in the UK.
Methods: Two data sources were thematically analysed – 1) open-text responses from family members who completed the UK FS-ICU-24 in a large observational cohort study 2) a set of quality improvement activities generated by patients, family members and ICU staff through experience-based co-design in a mixed-methods study.2,3
Anticipating that the content of open-text responses would vary by overall family satisfaction score and to address representativeness, stratified sampling was used to ensure that responses from the full spectrum of overall level of satisfaction were included.
Summarised themes, of the suggestions and priorities for quality improvement strategies aimed at improving family satisfaction with the ICU, were then mapped to the 24-scored items and domains of the UK FS-ICU-24 to assess coverage by the UK FS-ICU-24 (face validity).
Results and conclusions: An inductively derived coding framework, capturing all topics and themes emerging from 240 open-text responses and from the set of 38 improvement activities, was developed. The framework comprised six topics, five of which related to care in the ICU, each containing several themes (Table 1).
We found a good degree of coverage between the topics and themes identified as important to family members, from our thematic analysis, with the items and domains of the UK FS-ICU-24 – both in terms of specificity and in the number of questions relating to the topics – particularly for the ‘care of patient and person’, ‘care of family members’ and ‘communication and decision-making’ topics.
Our study confirms the face validity of the UK FS-ICU-24 and indicates that its inclusion as an outcome measure for evaluating quality improvement strategies aimed at improving family satisfaction with the ICU is appropriate.
Table 1.
Coding framework.
| Topic | Theme |
|---|---|
| The physical environment | Improving orientation and reducing boredom |
| Importance of rest and sleep | |
| Quality of the waiting room | |
| Care of patient and person | Knowing the person |
| Preserving dignity | |
| Coping with hallucination and assisted ventilation | |
| Care of family members | Improving contact with sick relatives |
| Orientation for family members | |
| Emotional support from staff | |
| Privacy of grieving | |
| Communication and decision-making | Improving family contact with doctors |
| Improving day-to-day communication | |
| Improving patient communication | |
| Care of staff | Staff training |
| Staff support | |
| Hospital journey | Leaving ICU |
| Communication with other departments |
0373
Better Access to Magnetic Resonance Imaging Out-of-Hours than During Plain-Time – Should Critical Care Requests Receive Greater Prioritisation Over Elective Scans?
Martin Murphy, Ian Johnson and Thearina De Beer
Queen's Medical Centre, Nottingham, United Kingdom
Abstract
Introduction: As a limited resource, Magnetic Resonance Imaging (MRI) is subject to competing demands both from Critical Care and the wider hospital economy: at the Queen’s Medical Centre in Nottingham, waiting time for scans has been perceived as a recurrent 'rate-limiting step' in the advancement of care for Critical Care Patients, but we had been unable to supply evidence for this.
Objectives: The purpose of this Service Evaluation was to review all MRI requests made for patients in Critical Care over a 1-year period to determine the true wait time, and whether there are emergent themes which associate with scan delay.
Method: The radiology information system (CRIS) was used to generate a list of all patients who had received an MRI scan in the Trust over a 1 year period: this was then cross-referenced with the Patient Administration System (PAS) to create a list of all patients who had an MRI scan requested whilst also an inpatient in Critical Care. These cases were then reviewed to determine: the indication for scan; the condition of the patient, the true magnitude of their wait and whether there was any documented consequence of waiting, (if delayed).
The resulting data were then explored both qualitatively and quantitatively to impute emergent patterns.
Result and Conclusions: 7693 inpatient MRIs were carried out on 4795 patients at Queens Medical Centre in the year to 31st July 2018 of which 181 were unique requests for MRIs on 116 patients in Critical Care (136 'scan sessions').
The median wait time for scan was 24–48 h, of which 27% were delayed more than 72 h. These times were markedly dispersed, and when the waits were transformed according to time spent waiting “out-of-hours” or “plain time” (non-bank holiday weekdays, 0800–1800), it became apparent that patients waiting “in hours” were less likely to have their scan within a day (the modal wait increased from <24 h to 24–48 h). This possibly indicates a competition for resource between Critical Care and elective services, this is despite the fact Critical Care scans are usually logistically more challenging and often require additional anaesthetic support.
To explore this further, requests and scans were categorised according to whether they occurred in “plain-time” or “out-of-hours”. When plotted, it was clear that requests during plain time usually resulted in scans in hours and the corresponding was true for scans out-of-hours. Additionally, it appears that out-of-hours requests were carried out in a more consistently short timescale which might represent an increased availability of scan facilities as well as some differences in the nature of these requests.
Review of the data also revealed a disconnect between the clinical urgency relayed in the casenotes and the urgency code recorded on the CRIS system which suggests more can be done to improve interprofessional communication with radiology staff.
This evaluation found that performance out-of-hours for MRI scanning was markedly better than performance in-hours, and suggests that more should be done to protect the resources available to Critical Care patients during normal working hours to avoid overburdening on-call teams.
0374
A Trust wide audit exploring escalation decision-making and communication to Intensive Care
Lucy Wyld1, Andrew Breen2, Isobel Morton3, Sophie Hood4 and Adam Hurlow5
1Palliative Medicine ST6, Leeds Teaching Hospitals Trust, Leeds, United Kingdom
2Consultant in Anaesthesia and Intensive Care Medicine, Leeds, United Kingdom
3Junior Doctor, West Yorkshire Deanery, Leeds, United Kingdom
4Adminisrations Manager, Quality Governance Team, Leeds Teaching Hospitals Trust, Leeds, United Kingdom
5Consultant in Palliative Medicine, Leeds Teaching Hospitals Trust, Leeds, United Kingdom
Abstract
Introduction: Critical Care speciality experiences one of the greatest number of adult inpatient deaths in Leeds Teaching Hospitals NHS Trust (LTHT).1 In light of acknowledged recognition of ICU-associated morbidity and the increasing medical complexity of patients, the decision process surrounding escalation is far from straight forward.
One key area in advanced care planning is the recognition of clinical deterioration with uncertain potential for recovery and the timely communication of this to patients and carers. This recognition and communication of uncertain outcomes and goals of care is particularly important when considering escalation to Intensive Care, where the balance of benefits and burdens is fine.
Objectives: This audit aims to evaluate current practice with respect to patient selection, advanced care planning and communication in the escalation of patients to Level 2 or 3 Care, against the gold standards detailed in National Guidance.2,3
Methods: Each speciality performed a retrospective case note review of 10 consecutive adult patients who died having had at least one stay in Critical Care during their final admission (August 2017 and November 2017).
Data was entered into Excel and analysed. A subgroup analysis was conducted with patients divided into complex vs non-complex (based on the presence of one or more marker of clinical complexity).
Results: Data from 67 patients, across 12 specialties was collected, divided into those with one or more markers of clinical complexity (53) and those with none (14).
Higher levels of medical complexity were associated with higher levels of communication. Discussions regarding CPR, goals of escalation and consultant involvement in decision making were more common amongst complex patients when compared to non-complex patients, 62% vs. 21%; 42% vs 14% and 29% vs 20% repectively. However in the majority of all cases, communication with the patient, prior to escalation, regarding risk of death and risk of Critical Care associated morbidity was not achieved (39% and 3%).
Conclusion: Patients had a high level of clinical complexity and as such, decision surrounding escalation of care requires consideration as to the goals of treatment and the values and preferences of each patient.
Communication with the patient regarding the risk of death and the risk of Critical Care associated morbidity was rarely achieved. Clinicians highlighted lack of awareness as to the prevalence and impact of ICU associated morbidity. Discussions surrounding patients’ goals and preferences are infrequent prior to escalation. This represents a significant area for improvement as the goal of critical care is to return patients to a quality of life that is acceptable to them, this cannot be achieved without exploring the values and preferences of each individual.
0375
Repatriation from Tertiary Critical Care Unit to Local Hospital
Thomas Lightburn, Carl Edward Oakden and Shondipon Laha
Royal Preston Hospital, Preston, United Kingdom
Abstract
Introduction: Tertiary Critical Care beds are at a premium within the current Critical Care environment within the United Kingdom. We hoped to identify opportunities to repatriate patients from our regional, specialist non-cardiac tertiary Critical Care unit in the North West of England, consisting of 24 beds of mixed use. We serve a large geographical area and provide specialist tertiary care for trauma, neurosurgery and neurology, vascular surgery, nephrology and gynaecological oncology for these patients.
Methods: We analysed case notes retrospectively from patients remaining within the critical care unit after 10 clinical days during a 12 month period between April 2018 and March 2019. Inclusion criteria consisted of adult patients whose normal residence was not within the normal catchment area for local services, who had been receiving continuous clinical care within our critical care unit for a period of 10 or more days, and whom had been admitted initially under the care of a specialist service. Case notes were reviewed alongside patient demographic information and length of stay data using the information supplied to the ICNARC dataset.
Results: During this period, 89 patients remained on the critical care unit for 10 or more days. Of these patients, 9 patients (9.8%) had formal discussion between the specialist clinical team and the critical care team regarding repatriation. 3 patients (3.4%) were repatriated to their local hospital for ongoing care with a further single patient repatriated to their local hospital the day after discharge from critical care. 17 patients received no further direct input from their specialist clinical team for more than 24 hours prior to discharge from critical care. The average length of time between cessation of specialist input and discharge from critical care is 15.2 days (range 0.7-123.2 days).
Conclusion: This work reveals a significant time period between cessation of specialist input and discharge time from a tertiary critical care, which may have an impact on bed state for the specialist centre. It may represent a missed opportunity to ensure patients receive appropriate care and also are able to be cared for by their local centres when specialist input is no longer required. Further work must be done to analyse the direct impact of these findings both for the patient and their relatives and the impact upon our limited tertiary centres.
0378
The relationship between the timing of high National Early Warning Scores (NEWS) and the risk of unplanned transfers to the intensive care unit
Emma Smith1, Oliver Redfern2, James Malycha2, J Duncan Young3 and Peter J Watkinson3
1Oxford University Medical School, Medical Sciences Division, University of Oxford, Oxford, United Kingdom
2Kadoorie Centre for Critical Care Research and Education, Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom
3Nuffield Department of Clinical Neurosciences, University of Oxford, Oxford, United Kingdom
Abstract
Background & Objectives: Early Warning Scores (EWSs), which stratify patients based on vital sign abnormalities, are used to identify patients at risk of deterioration. In the UK, the National Early Warning Score (NEWS) is now mandated for use in all acute hospitals.1 It is recommended that patients with a NEWS of seven or above are reviewed by critical care teams.2 We hypothesised that the relationship between abnormal physiology and the risk of adverse outcomes (death, unplanned admissions to intensive care) might be related to the amount of time patients have been exposed to medical interventions. The aim of this study was to examine the risk of unplanned admissions to the intensive care unit (UICU) and in-hospital mortality for patients with a NEWS ≥ 7.
Methods: We included adults (>15 years old) admitted as emergencies to a large acute hospital in the UK between 2016 and 2017. The NEWS was calculated for each observation set using the most recently measured vital signs in the first three days of hospital admission. Observation sets with a NEWS of ≥7 were divided into five sub-groups based on the time they were measured relative to the patient’s admission to hospital: 0–0.5 hrs, 0.5–4 hrs, 4–24 hrs, 24–48 hrs and 48–72 hrs. These relate to key stages in the admission pathway, representing the patient’s initial presentation, time in the emergency department, then days 1, 2 and 3 of admission. For each sub-group, we calculated the proportion of observations that were followed by the first of an unplanned ICU admission or in-hospital death. Exact binomial confidence intervals for proportions were calculated using the Pearson-Klopper method.
Results: 79,642 patients were admitted during the study period, of which 11,171 (14%) had a high NEWS (≥7) in the first three days of their admission. On average, patients with a high NEWS were older (median age 77 vs 59), with substantially higher rates of in-hospital mortality (16.8% vs 1.1%) and unplanned ICU admissions (6% vs 0.6%). Over the first three days of admissions, the percentage of high NEWS observations followed by an unplanned ICU admissions dropped from a peak of 9.72% (in 0.5–4 hours) to 4.09% (48–72 hours). In contrast, rates of in-hospital mortality rose substantially from 18.01% to 34.12% (Table 1).
Conclusions: Our study shows that among patients scoring a NEWS ≥ 7, the time at which this score is recorded is associated with likelihood of adverse outcomes. Specifically, scoring ≥7 later in admission is associated with increased mortality, whereas the risk of unplanned ICU admission reduces. This suggests these outcomes are less related than might be expected, and may represent different patient populations.
Funding: This abstract presents independent research commissioned by the Health Innovation Challenge Fund (HICF-R9-524; WT-103703/Z/14/Z), a parallel funding partnership between the United Kingdom Department of Health and Wellcome Trust. The views expressed here are those of the authors and not necessarily those of the Department of Health or Wellcome Trust.
Table 1.
Percentage of high risk vital sign observations (NEWS ≥ 7) followed by an unplanned ICU admission or in-hospital death.

|
0379
Nasogastric tubes check: difficult to spot the best method, easy to find the worst problems. A systematic review in the adult population
Fiqry Fadhlillah1, Francesca Rubulotta2 and John Mcnally-Reilly1
1London North West University Healthcare NHS Trust, London, United Kingdom
2Imperial College Healthcare NHS Trust, London, United Kingdom
Abstract
Nasogastric tubes (NGs) are commonly used within the hospital setting for enteral feeding in dysphagic, comatose and ventilated critically ill patients. NG tubes are generally accepted as being safe pieces of equipment. Nevertheless, misplacement of NGs into the respiratory tract still occurs, and this relates to dire consequences especially if not detected prior to commencement of feeding.
The objective of this systematic review is to identify the safest, most reproducible and cost contained method to verify the correct position of NG tubes in the digestive tract.
MEDLINE, EMBASE, CINAHL and Cochrane were searched using pre-determined keywords, for studies reporting on the accuracy and sensitivity of methods used to verify NG tube correct position. Authors excluded percutaneous or external opening (gastrostomy) tubes and studies focusing solely on nasojejunal/transpyloric tubes. Authors focused on the adult population and excluded paediatric patients who cannot be exposed to radiation. Two independent reviewers appraised the evidence and literature between 1900 and 2019.
Overall, 77 studies were included namely: 1 randomised controlled, 1 non-randomised experimental trial and 75 observational studies. The gold standard was identified as being the chest x ray, followed by the use of pH strips. 17 studies reported the use of capnogram or colorimetric capnometry, 11 the use of ultrasound techniques and auscultation. Mostly single centre studies described new techniques such as: enzymes, electromagnetic, inspection of aspirates, camera, tube length and pressure gauge. The systematic review could not find superiority in the use of chest x rays compared to other techniques.
There was no conclusive evidence of the superiority of any one method compared to x-rays. X-Rays have stochastic risks which are not conventionally measured. The use of ultrasounds might change practice
0381
Closing the audit loop. A re-audit of sedation hold practice within the Intensive Care Unit at George Eliot Hospital, Nuneaton: compliance with international guidelines
Rosanna Stopford, Mudassar Aslam and Sam George
George Eliot Hospital, Nuneaton, United Kingdom
Abstract
Introduction: Patients requiring mechanical ventilation are pharmacologically sedated in order to minimise the stress response and psychological sequalae. However, excessive sedation may lead to hypotension, venous thrombosis, increased risk of ventilator associated pneumonia, prolonged ventilation and longer stays on the intensive care unit (ICU).1 This is associated with increased costs to the NHS. Daily sedation holds in mechanically ventilated individuals limit drug bioaccumulation and reduce the duration of mechanical ventilation and associated compilations.1,2
The American College of Critical Care Medicine (ACCM) recommends that i) all mechanically ventilated patients should have daily interruptions in sedation or a target level of sedation (unless clinically unstable); ii) where there is no sedation hold, there must be a valid and documented reason; iii) the Richmond Agitation-Sedation Scale (RASS) and Sedation-Agitation Scale (SAS) are the most valid and reliable sedation assessment tools for monitoring quality and depth of sedation in adults in ICU and sedation must be altered accordingly; iv) sedation using non-benzodiazepine sedatives (propofol or dexmedetomidine) may be preferred over sedation with benzodiazepines; and v) delirium must be monitored routinely.3 There are accepted contraindications for daily sedation holds including: raised intracranial pressure, FiO2 > 60% or neuromuscular blockade, amongst others.
Objectives: This re-audit aimed to i) establish adherence to the guidelines set out by ACCM in the ICU at George Eliot Hospital; ii) compare current practice against the previous audit in 2017 and iii) identify areas for improvement.
Methods: A retrospective re-audit was carried out between November 2018 and April 2019. All mechanically ventilated patients (>24 hours) were included in this audit. Data were obtained from ICU charts and patient medical records.
Results: Thirty patients were mechanically ventilated for >24 hours between November 2018 and April 2019. Data were not available for 2 patients (n = 28). Of these patients, 46.4% (n = 13) received daily sedation holds (17% in the 2017 audit). Of the patients not receiving daily sedation holds (55.6%, n = 15), 73.3% (n = 11) had valid reasons (20% in 2017); increasing or high FiO2 requirements (n = 6), haemodynamic instability (n = 2), awaiting procedure (n = 2), raised intracranial pressure (n = 1). All patients on ICU were sedated using propofol and alfentanil. Benzodiazepines were not used. RASS scores were documented in all patients and all patients had sedation titrated accordingly (100%). Delirium was monitored routinely in all patients (100%). There was a higher incidence of ventilator associated pneumonia in patients who did not have daily sedation holds (13.3% vs 0%).
Conclusions: Significant improvements in compliance to international guidelines have occurred since 2017 following staff education and changes to documentation in ICU. These simple interventions have led to substantial changes in clinical practice. However, there remains room for improvement. Education for ICU staff will be provided and incorporated into staff inductions and a re-designed ICU chart will facilitate documentation of reasons for non-compliance.
0382
Critical events during intra hospital transport of critically ill patients at a tertiary intensive care
Mohd Qurram Parveez, Narayana Yaddanapudi and Vikas Saini
Post Graduate Institute Medical Education and Research,Chandigarh, Chandigarh, India
Abstract
Background: Intra-hospital transport (IHT) of critically ill patients is frequently required for diagnostic or therapeutic procedures that cannot be performed in Intensive Care Unit (ICU). Adverse events are common in both in- and out-of-hospital transports, the most common being equipment malfunction. Studies have reported equipment problems and mishap in 11 to 34% of all transport episodes. Knowledge about the potential complications associated with IHT is essential to determine the safest way to transport patients reducing mortality and morbidity. Therefore, the decision of transporting the patients is based on the potential benefit to patients against the possibility of critical events occurring during transport. This study was planned to determine the incidence and types of adverse events occurring during transport of critically ill patients in a tertiary care hospital.
Methods: This prospective observational study was conducted in intensive care unit of a tertiary care hospital for a duration of eight month after ethical clearance from institute ethics committee. All patients transported out of the intensive care unit during the audit period for diagnostic or therapeutic procedures were included in the study. Vitals and several study parameters were recorded before, during and after shifting patients to and from intensive care unit. Various critical events were noted during transport and classified into major and minor critical events based on the potential consequences.
Results: One hundred and sixty patients were studied for consecutive intra hospital transport to and from intensive care unit. The patients were most commonly transported for imaging studies (58.1%) than other reasons were for minor surgery (31.8%) and major surgery (2.5%) and others (7.5%). A total of 248 critical events were observed in 104 intra hospital transports (65%; 95% Confidence Interval [95CI] 57.4-72.1%). So, an average of 2.38 critical events per patients during the transport. Out of 248 critical events nearly one third were airway related (31.9%; 95CI: 26.3-37.9%), followed by 33 events due to cardiovascular cause (13.3%; 95CI: 9.5–18.0%). There was no major cardiovascular event such as cardiac arrest. There were 13 (5.2%; 95CI: 2.9–8.6%) respiratory system related critical events out of 248 critical events. There were 31 major events among the 248 critical events (12.5%; 95CI: 8.8–17.1%).
Conclusion: Critical events during intra-hospital transport are common in critically ill ICU patients. Standard guidelines with regard to the accompanying personnel, and monitoring need to be followed during intra-hospital transport. Conduct of minor surgical procedures in the intensive care unit and better bed-side diagnostic procedures may be considered for the future.
0383
Anti-ma2 encephalitis presenting after curative surgery for testicular cancer
Muzzammil Ali and Misha Khilji
Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Background: Ma2-antibody is highly specific for paraneoplastic encephalitis. In young males the primary tumour is usually of testicular origin.1 Where appropriate, treatment is with immunosuppression and tumour removal. Here we present an unusual case where curative surgery preceded the presentation of encephalitis. This can either suggest pre-existing circulating anti-Ma2, or non-radiologically apparent microscopic disease.
Case presentation: A 49-year-old was referred to clinic with a 3-week history of a right testicular lump. Although his tumour markers were normal, both a testicular ultrasound and CT-TAP suggested malignancy, with a radiological staging of pT1. He subsequently had a right inguinal orchidectomy, the histology of which revealed a mixed germ cell tumour.
Six months later, he presented to A&E with a GCS of 11 (E4V1M6). An MRI-head showed extensive T2-signal changes in the medial thalamus, 3rd ventricles, periaqueductal regions, dorsal brainstem and mammillary bodies. An EEG showed no epileptiform activity, a lumbar puncture was unremarkable, a CT-TAP showed no evidence of metastatic disease, and tumour markers were negative.
He was started on dexamethasone for a presumed brain tumour following discussion in MDT. However one day later, he dropped his GCS to 9 (E2V1M6). A CT-Head at that point showed no new changes. Further drops and fluctuation in GCS (between 3 and 7) with associated respiratory failure necessitated admission to critical care for NIV. Although a source of infection was not identified, he was started on broad-spectrum antibiotics due to pyrexia, raised inflammatory markers and a high oxygen requirement.
With further deterioration, haemodynamic instability and impending airway compromise, the option of palliation was discussed and agreed upon with the patient’s family. Specific treatment limitations were therefore put into place.
Not long after this however, the critical care unit were informed that he tested positive for anti-Ma2. Anti-Ma2 is highly specific for paraneoplastic encephalitis which carries a good prognosis. Dexamethasone was therefore changed to methylprednisolone.
Hours later, his GCS improved to 13 and one day later, was 15. Two subsequent MRIs at 1 and 3 weeks showed marked intracranial improvement. Although a PET scan revealed mild omental disease, multiple CT-guided and laparoscopic biopsies were unremarkable for malignancy. At week 5, he was able to walk independently without any neurological deficit.
Conclusions: The interest of this case lies not only in its rarity, but the fact that the presentation of encephalitis occurred following curative surgery. All published case reports of this condition either occurred as the first presentation of malignancy, or less frequently in the context of known malignancy.2,3
Another interesting feature of this case is the importance of considering autoimmune screening in patients with low GCS. Onconeurological antibody identification can be extremely helpful to guide management and to prognosticate. Some forms of autoimmune encephalitis, for example, carry a good prognosis, including anti-NMDAR and anti-Ma2, while others such as anti-Hu and anti-Yo, carry a poor prognosis.1,3,4
The nature of presentation in this patient means that it is important for him to have annual PET scans to help identify any hidden malignancy that has not yet been detected.
0385
Shedding Sound Waves on a Diagnostic Conundrum: How I used Point of Care Ultrasound as a Trainee and Discovered an Unexpected Broken Heart
Kath Fok
Royal Cornwall Hospitals NHS Trust, Truro, United Kingdom
Abstract
Background: Ultrasonography is no longer a tool confined to radiologists (1). During Core Training I attended a formal point of care ultrasound course (POCUS). As an Emergency Department physician I scanned a patient whose presentation did not fit any disease constellation. My unexpected discovery altered and expedited the course of this patient’s hospital stay.
Case presentation: VE, a 29 year old female had spent a week in bed with fatigue following a recent return to work. She described generalised muscle aches but no focal symptoms. PMHx: depression and chronic fatigue. O/E: afebrile, BP 101/73, HR 105 bpm. Physical examination normal except for tender liver edge. VBG: lactate 4. ECG: SR, TWI V2. Blood tests: NAD except raised ALT.
Without a clear differential, I decided to see if POCUS could explain her RUQ pain. With my limited experience, I felt that the liver looked grossly homogeneous. With the ultrasound in hand I decided to continue by doing an eFAST and unexpectedly found a pericardial effusion. I then focused in with an echocardiogram. I found:
• 2 cm pericardial effusion
• Severe left ventricular systolic dysfunction
• Left ventricle hypertrophy
• Radiological evidence of cardiac tamponade: bowing of the right ventricular free wall due to external pressure from the pericardial effusion
Importantly she was not clinically in cardiac tamponade. I referred her to the medical team without a clear diagnosis but emphasising that she was at risk of cardiogenic shock. Her cardiology referral was expedited. The team continued supportive care, treated for heart failure and investigated her atypical cardiomyopathy. A formal ECHO confirmed my findings. A cardiac MRI a week later showed she had recovered completely normal cardiac function. She was discharged with the presumed diagnosis of Takotsubo’s cardiomyopathy (aka broken heart syndrome) given the reversibility of her condition. An ECHO at three months remained normal.
Conclusions: Even as a junior trainee working towards accreditation in POCUS, I was able to use ultrasound as an invaluable diagnostic adjunct. I remain acutely aware that I am not a radiologist or echosonographer and that I am at risk of over or under interpreting findings.
Current POCUS availability in the UK is variable and dependent on individual clinicians attending informal teaching or undertaking an accreditation programme. It rightly emphasises a “rule in” process in the clinical context, where positive findings should go on to have formal investigation. This example of how POC ultrasound by trained non-radiologists can positively impact patient care.
With appropriate governance, ultrasound training can provide an invaluable diagnostic tool that transforms patient care and should be developed for all acute physicians (1, 2).
Figure 1.
Subxiphoid view: a homogenous liver (L) and a pleural effusion (eff). Left ventricle (LV) surrounded by thickened myocardium (Mo).
Figure 2a, 2b.
Parasternal long and short views: ventricular myocardial thickening, pericardial effusion, compression of right ventricle (RV), the left atrium (LA).
0386
Post Operative Gut Dysfunction – time to ditch the Opioids
Sonia Sathe and Anushka Sieunarine
Princess of Wales Hospital, Bridgend, United Kingdom
Abstract
Introduction: A change in direction about effective strategies for analgesia for colorectal surgery is urgently needed in light of the opioid epidemic afflicting the world.
Specific recommendations include central neuraxial blockade or peripheral nerve blocks and use of non-opioid analgesic adjuncts, early oral intake, early mobilization and optimal analgesia.1,2,3
A post-operative package of care which incorporates these specific recommendations would result in faster recovery times and decreased morbidity for these patients with decreased burden on Critical Care Units and Hospitals.1,2
Objectives: We examined current peri-operative anaesthetic practices for care of both emergency and elective colorectal patients to inform the formulation of an Enhanced Recovery Program for these patients.
Methods: A retrospective audit was carried out on post-op colorectal surgical patients admitted to the Critical Care Unit at Princess of Wales Hospital between May 2018 and May 2019. Data collected included demographics, frailty score, type of surgery, analgesia provided intra-op, post op recovery times, times to enteral feeding, mobilization and discharge from ITU.
Results: In patients who received central neuraxial blockade vs those who received intravenous opioids – patients who received intrathecal opioids had post- operative pain scores on day 1 of 0–1 with very occasional use of additional intravenous opioids. In patients who received opioids intra operatively pain scores were 4–8 with more frequent use of additional opioids.
Patients who received intrathecal opioids also had reduced post-operative gut dysfunction as evidenced by reduced time to first oral intake – post operative day 1–3 as compared to post-operative day 3–5 for patients who received intra venous opioids.
Patients with intrathecal opioids also received less anti emetic medications in the post-operative period.
Time to mobilisation and time to trial without catheter was 1–3 days in patients who received intrathecal opioids as compared to 3–5 days in those who received intra venous opioids.
Average length of stay on ITU was 24 to 48 hours in patients who received intrathecal opioids as compared to 96+ hours for patients who received intravenous opioids.
This Audit was used to formulate an ERP for Colo-Rectal patients.
Conclusions: An opioid sparing strategy utilising intrathecal opioids with no intravenous opioids, early enteral feeding and early mobilisation may improve morbidity in these patients.
0388
Identifying the need for a BrainBox: a survey to assess logistical challenges in delivering neuroprotection across the South London Adult Critical Care Network
Jennifer Gosling1 and Peter Beaumont1,2
1King's College Hospital NHS Foundation Trust, London, United Kingdom
2South London Adult Critical Care Network, London, United Kingdom
Abstract
Introduction: Immediately on presumption of significant primary brain injury, neuroprotective measures should be employed to mitigate against secondary brain injury (SBI) until a definitive neurological plan is made.1,2
Operating in a hub and spoke model, individual clinicians at non-neuroscience facilities may provide care for the acutely brain injured infrequently and so lack the recency of knowledge as to physiologic targets, referral processes, and necessary pharmacologic interventions.
This survey assessed the practical challenges encountered in providing these treatments across South London Adult Critical Care Network (SLACCN) partner Trusts.
Objectives: We aimed to assess local knowledge about how to administer important components of neuroprotection (e.g. osmotics and rapid sequence drugs) amongst clinicians potentially involved in the initial treatment of acute brain injuries.
Methods: An electronic clinician survey was conducted for 4 weeks between December 2018 and January 2019 across SLACCN Trusts. Tertiary neurosurgical centres were included as transferred patients may be temporised in the Emergency Department (ED) pending re-imaging or theatre availability.
A telephone survey was conducted to determine the most appropriate contacts in each trust to generate an email cascade. An electronic survey for distribution was sent to as many as possible of the following: anaesthetics secretaries, critical care departments, senior Operating Department Practitioner, SLACCN contacts, ED matrons & consultants.
Responses were collected anonymously using a standardised survey on GoogleForms and analysed using MS Excel V16.12.
Results: 113 responses were received, with approximately even split between ED (42 = 37.2%), Anaesthetics (37 = 32.7%) and ICM (29 = 25.7%). At least one response was received from every hospital surveyed, 88% from district general hospitals.
Both doctors (n = 76, 67%) and nurses (n = 31, 27%) responded. A minority knew where in ED to find either mannitol (27%) or hypertonic saline (19%). More than 10%, mostly anaesthetic middle grades, did not know either where in the hospital these drugs could be found, or if they were stocked at all. A majority stated they would need to check dosing for both drugs (mannitol 73% vs hypertonic saline 67%).
68 respondents (60%) knew exactly where RSI drugs were in ED and an additional 35 (31%) were confident they were available in ED though unsure where. Respondents were generally confident about physiological targets without need for references (73%).
49/113 (43%) identified a need for easily accessible information about prevention of SBI in the form of guidelines or cue cards.
Free text responses highlighted many difficulties with the logistics of neurosurgical referral. Several respondents explicitly denied caring for patients at risk of SBI because they did not work in a major trauma centre.
Conclusion: Focussed resources may benefit clinicians caring for patients at risk of SBI, particularly outside tertiary care facilities.
Data gathered will be used to inform development and distribution of both standardised SLACCN-wide neurocritical care guidelines & education and a physical container, collectively termed the “Brain Box”.
0389
WHEN HOSPITAL DISCHARGE HITS HOME. A qualitative study on hospital to home transition experience among survivors of critical illness and their relatives
Mel Major1,2,3, Marike Van der Schaaf2,3, Fenna Van Nes4, Stephan Ramaekers1,2 and Raoul Engelbert2,3
1European School of Physiotherapy, Amsterdam University of Applied Sciences, Amsterdam, The Netherlands
2Faculty of Health, Center of Expertise Urban Vitality, Amsterdam University of Applied Sciences, Amsterdam, The Netherlands
3Amsterdam UMC, University of Amsterdam, Department of Rehabilitation medicine, Amsterdam, The Netherlands
4School of Occupational therapy, Amsterdam University of Applied Sciences, Amsterdam, The Netherlands
Abstract
Background: In the Netherlands, annually approximately 25,000 survivors of critical illness develop post-intensive care syndrome (PICS). PICS and PICS-Family comprise clusters of physical and psychological problems which develop as a result of critical illness and prolonged intensive care unit (ICU)-stay, warranting a thorough needs assessment at hospital discharge. In light of existing evidence on physical and psychological consequences of critical illness for both patient and family, it is as yet unclear if current hospital discharge procedures suffice to meet the needs of this group.
Objectives: The aim of our study was: 1) to explore experiences of critical illness survivors and their relatives around the hospital discharge process, and 2) to identify perceived barriers and enablers for a positive perceived transition from hospital to home or rehabilitation facility.
Methods: We performed a grounded theory study with semi-structured interviews among a group of survivors of critical illness and their relatives (N = 35) discharged from 16 hospitals across the Netherlands. Interviews were audio recorded and transcribed verbatim. Using constant comparative methods, initial and focused coding was applied to the data, which were further labeled into major and subcategories, ultimately leading to the identification of key concepts. Triangulation was applied through several reflexivity meetings at different stages of the study.
Results: Thirty-five participants (22 patients and 13 relatives) were included in this study (mean age: 53 (SD ± 11.2), 60% female). Median ICU and hospital length of stay were 14 days (IQR 9.75-24.5) and 35 days (IQR 21.75-57.25) respectively. Participating patients' median mechanical ventilation duration was 11.5 days (IQR 7.8-18.0).
Thematic analyses led to identification of seven key concepts, representing barriers and enablers to a positive transition experience. 'Existing in a fragmented reality', ‘being overlooked’ and ‘feeling disqualified’, were identified barriers and 'feeling empowered', 'encountering empathic and expert professionals', 'managing recovery expectations' and 'family engagement' were identified as enablers for a positive perceived transition experience.
Conclusion (s): Findings of this study suggest that current hospital discharge practice for survivors of critical illness is driven by speed and efficiency, rather than by individual needs assessments, despite advocacies for patient- and family centered care. Discharge strategies should be customized to facilitate adequate and comprehensive assessment of aftercare needs, conducted at the right time and within the right context, encouraging empowerment and a positive perceived transition from hospital to home.
0390
Use of alternative diagnostic tests to guide antibiotic stewardship in critically ill patients with pneumonia – a quality improvement project
Valerie Page1, Jacques Carver1, Chris Allen2, Rachel Hilson1, Brice Djeugam3, Joel Sugarman3 and Hala Kandil1
1Watford General Hospital, Watford, United Kingdom
2Northwick Park Hospital, Harrow, United Kingdom
3University College of London, London, United Kingdom
Abstract
Background/Objectives: The importance of good antimicrobial stewardship cannot be underestimated. It requires an inter-professional effort for:
• Timely and optimal selection, dose and duration of an antimicrobial
• The best clinical outcome for the treatment of infection
• Minimal toxicity to the patient
• Minimal impact on resistance and ecological adverse events such as C. difficile.1
Our consultant intensivists and microbiologists liaise closely regarding the antimicrobial prescriptions. We use both BioFire® FilmArray® respiratory panel (RP) diagnosis and standard diagnostic techniques (culture and sensitivity).
The primary aims are to explore the potential and cost effectiveness of using an upgraded version of rapid molecular diagnosis of pneumonia in critically ill patients, +/− serum procalcitonin levels on antimicrobial stewardship.2 This was a prospective exploratory case series review.
Method: Paired samples of sputum from 32 critically ill patients with new onset, radiological confirmed pneumonia were taken for standard culture and sensitivity and molecular diagnosis using The BioFire® FilmArray® Pneumonia Panel. Serum procalcitonin levels were measured.
A consultant microbiologist had access to all results. The microbiologist liaised directly with the intensivist to review the patient’s clinical status and discuss antimicrobial prescription recommendations.
A microbiologist (HK) and intensivist (VJP) together reviewed antimicrobial prescriptions, inflammatory markers, procalcitonin results and daily SOFA data to determine:
1. Changes in antimicrobial prescription
2. Missed opportunities to change antimicrobial prescriptions e.g. stopping
Results: Of 32 patients one patient had missing data, one patient was transferred to another ICU so data on 30 patients were included, 21 men, age range 26 to 86 (mean 60.9), APACHE score range 7 to 38 (mean 17).
The pneumonia panel resulted in the early detection of 13 bacteria not cultured using standard technique. Antibiotic prescriptions were changed (stopped or de-escalated) in eight patients with missed opportunities to change prescriptions in seven more patients. Resistance was detected in two bacteria by panel not culture, in one case early resistance (MRSA) was missed. In 14 instances prescriptions were not changed but the panel record enabled earlier diagnosis (2 to 3 days) and reassurance. Viruses were detected in 7 patients.
The pneumonia panel missed one mycoplasma and one legionella infections. While the legionella titres in treated infection were likely too low to detect the mycoplasma negative result cannot be easily explained.
The procalcitonin result had an impact on two instances, antibiotics were stopped, nine additional instances were identified where the antibiotics could have been stopped. There were eight instances when a procalcitonin would have been helpful in informing the clinical discussion.
The cost effectiveness data is still being reviewed.
Conclusion: The results of this exploratory project suggest that pneumonia panel and appropriate procalcitonin results provide valuable information, with potential for better antimicrobial stewardship, specifically shorter courses. Depending on the likelihood of atypical infection additional results may be needed before stopping macrolide drugs.
The next steps will be to review the cost effectiveness data with a view to drafting a business case for the routine use of these diagnostics in critical care patients then draft guidance regarding their use in clinical practice.
0392
Screening for delirium in critical care: impact of a ‘Delirium Week’ intervention
Nicholas Wroe, James Lalloo and David Moir
Leeds Teaching Hospital NHS Trust, Leeds, United Kingdom
Abstract
Background: Delirium is common in intensive care, and is associated with increased mortality, length of stay and risk of cognitive impairment. Hyperactive delirium is evident through monitoring the Richmond Agitation-Sedation Scale (RASS), whereas hypoactive delirium – which confers a worse prognosis – may lie undetected without active surveillance. The Confusion Assessment Method-ICU (CAM-ICU) is an effective bedside screening tool for hypoactive delirium in intensive care.
Methods: We reviewed the medical and nursing notes of 37 patients across critical care at the LGI to identify whether CAM-ICU had been performed, or whether it was contraindicated (e.g. sedation).
Results:
Audit step 1:
Of the 37 patients we studied, 1 had suffered brainstem death, and a further 7 were sedated, meaning that CAM-ICU was contraindicated. Two patients were agitated. Zero (0%) of the remaining patients had CAM-ICU recorded.
Intervention: Delirium Week
We carried out teaching sessions as part of a broader ‘delirium week’ in critical care across SJUH and LGI. This comprised awareness posters, further teaching and nomination of a ‘delirium champion’ for each ward.
Audit Step 2:
We identified 29 patients, of which 9 were sedated. A further 2 patients were receiving ward level care. There were 7 agitated patients (RASS 1 or 2). CAM-ICU was performed in 5 of 18 (28%) eligible patients. CAM-ICU was not performed in the remaining 13 eligible patients.
Conclusions: Delirium week was a trust-wide initiative aiming to incorporate delirium screening into daily nursing practice. A prevalent view was that CAM-ICU was ‘not applicable in neuro ICU’, despite challenging this in delirium week. Notably, 12/24 (50%) of neuro ICU patients studied were suitable for delirium screening. Informal ‘delirium screening’ occurs on the ICU; space on the ICU charts could formalise and document this.
Moving Forward: ‘Delirium Week’ interventions seemed to increase in the number of CAM-ICU assessments performed. Work needs to be done to raise the priority of delirium screening, particularly across neuro-ICU.
0393
Prolonged Unconsciousness in Perampanel Overdose: A Case Report
Guy Parsons1,2, Jon Bailey2 and Freddie Bailey2
1Nuffield Department of Clinical Neurosciences, Oxford University, Oxford, United Kingdom
2Department of Critical Care, Milton Keynes University Hospital, Milton Keynes, United Kingdom
Abstract
Background: Clinical experience of overdoses of Perampanel,1 a novel antiepileptic drug (an AMPA glutamate receptor antagonist) with a long half-life up to 129 hours,2 is markedly limited. The scant literature available identifies potential for prolonged unconsciousness in overdose.3 We report a case of prolonged stupor following Perampanel overdose requiring protracted endotracheal intubation with eventual complete recovery. This case represents the longest known period of deranged consciousness prior to full recovery in Perampanel overdose at 14 days.
Case Presentation: A 27 year old male with no known health problems was admitted having been found unconscious with evidence of an overdose of his partner’s medication in a suspected suicide attempt. This was a mixed overdose of Perampanel, Levothyroxine and Pregabalin, medicines to which he had no prior exposure. Exact doses taken were unclear but a clinical impression of 42 mg of Perampanel (3.5 times the maximum daily dose) and trivial amounts of Levothyroxine and Pregabalin was formed from review of medication packets.
Initial assessment identified a fluctuating conscious level (Glasgow Coma Score 7–10) with periods of severe agitation. Pupillary reflexes were intact, airway reflexes preserved and there was no respiratory or haemodynamic compromise. Initial laboratory investigations were unremarkable and a CT brain scan identified no intracranial pathology. Electrocardiographs did not reveal any abnormalities and blood gas testing was reassuring. Admission was arranged for ongoing monitoring while awaiting neurological improvement and psychiatric review.
On day 2 ongoing stupor interspersed with marked agitation was noted requiring intermittent restraint to prevent injury. Severe Type-2 Respiratory Failure and Aspiration Pneumonia developed and intubation was performed with Intensive Care admission arranged for further management. An Acute Respiratory Distress Syndrome (ARDS) arose which was managed with pronation, paralysis, and bronchoscopy for secretion clearance. Referral to a Extracorporeal Membrane Oxygenation (ECMO) centre was made but the ARDS improved with conventional management and ECMO was not required. Microbiological advice was sought and Toxbase consulted with conservative management advocated.
The patient remained neurologically inappropriate on daily sedation holds with disorientation, stupor and periods of agitation for a further 12 days. CSF sampling was not performed and Electroencephalography was not available. An interval CT brain scan on day 6 did not reveal any new intracranial pathology. A minor improvement of the patient’s conscious level was noted on day 12 warranting a successful trial of extubation. The patient returned to normal consciousness at day 14 with no evidence of persisting neurological deficit. He was subsequently discharged home following a reassuring psychiatric review.
Conclusions: This case is noteworthy as it contributes to the sparse literature available on Perampanel overdose and helps inform decision making within Critical Care. It reveals that Perampanel overdose may not initially cause systemic effects such as cardiac toxicity or metabolic disturbance but can cause protracted altered consciousness with secondary compromise before complete recovery. Early airway protection should be considered in overdose and prolonged Intensive Care support offered. This case is the longest known period of altered consciousness from the available literature with full recovery at 14 days.4,5
0394
An audit of lung protective ventilation
Jasbir Chhabra, Claire Irwin, Sharon Parkinson, Janine Morris, Rebecca Frank, Daniel Cottle and Matt Hargreaves
Royal Preston Hospital, Preston, United Kingdom
Abstract
Introduction: Since The Acute Respiratory Distress Syndrome Network publication in 20001ventilation with volumes of 6 ml/kg ideal body weight has been accepted as good intensive care practice in the prevention of acute respiratory distress syndrome.
Background/Objective: The aim of this audit was to assess our intensive care units compliance with 6 ml/kg ventilation ideal body weight in patients with sepsis. Following this the results were analysed to establish reasons why compliance was poor and to introduce a care package to improve patient care.
Methods: Data was collected over a 12 month period between April 2018 and April 2019. Mandatory ventilated patients who were on antibiotics and vasopressors were included. Neurosurgical patients and patients post cardiac arrest were excluded from the audit.
The patients ideal body weight was calculated and then their tidal volume documented hourly over a 24 hour period. Data from ten patient days per month was collected.
Results: The initial audit showed that compliance with lung protective ventilation was poor, with more than 60% of the recorded tidal volumes greater than 6 ml/kg ideal body weight. Analysis of the data identified several reasons for this. Firstly the patients weight was often incorrectly estimated on arrival to the intensive care, leading to incorrect calculation of 6 mg/kg tidal volumes. Secondly, the data suggested that if the wrong weight was inputted into the ventilator at first set up then the patient would remain over ventilated throughout the 24 hour period. Patients with ideal tidal volumes of less than 300 ml were also more likely to be ventilated at volumes greater than 6 ml/kg.
A care package was introduced to address the problems identified. An ideal body weight calculator was provided on the respiratory observation chart and on the ventilator to ensure the patients correct weight was used.A checklist for setting up the ventilator was implemented to ensure the ventilator was set up correctly from the start, along with its inclusion on the daily ward round checklist. As an on going reminder, ventilation prescriptions were established at the back of every bed and colour coded electronic tidal ventilation observations highlighted when patients were ventilated at greater than 6 ml/kg. These interventions were supported by multi disciplinary education.
As the above interventions were implemented compliance with 6 ml/kg ventilation targets gradually improved to 80%. (Figure1)
Conclusion: Despite the widespread acceptance of the use of 6 mg/kg ventilation in septic patients an audit of the practice on our unit showed this was not adhered to. On our unit a care buddle including several interventions along with multi disciplinary education improved implementation of lung protective ventilation.
0395
What factors influence participant’s course outcomes in Advanced Life Support?
Chris Thorne1, Peter Kimani2 and Gavin Perkins3
1North Bristol NHS Trust, Bristol, United Kingdom
2University of Warwick, Warwick, United Kingdom
3Heart of England NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Introduction: Competence in Advanced Life Support (ALS) is mandatory for healthcare professionals working in intensive care units. The Resuscitation Council (UK) ALS course is the largest course in the UK and provides a structured and standardised approach to the management of critically unwell patients.1 The high training standards promote an efficient chain of survival2, aiming to maximise patient outcomes from cardiac arrest. There is a relative paucity of research regarding factors that influence ALS course outcomes.3
Objectives: We sought to identify which participant, course type and centre factors were associated with course outcomes.
Methods: Participants enrolled on ALS courses between 1st December 2017 and 30th November 2018 were included. Demographic data was obtained when participants registered on the Learning Management System (LMS). Assessment data comprised a post-course MCQ and practical cardiac arrest management simulation test (CAS-Test). In order to achieve ALS competency, participants needed to pass both aspects.
Anonymised data were summarised with descriptive statistics. Univariate linear and logistic regression models identified factors associated with favourable course outcomes. Significant predictor variables underwent multivariate regression analyses. Odds ratios (OR), 95% confidence intervals and P-values were reported, with statistical significance set at P-values of <0.05.
Results: 17,690 participants were enrolled on an ALS course during the study period. There were 9,190 on the two-day ALS course, 7,336 on the e-ALS course, 1,120 on the recertification course and 44 on the modular course.
The mean post-course MCQ score was 86.7% (SD = 6.7). The multivariate analysis is seen in Figure 1. Factors associated with a favourable MCQ score were; increasing seniority, pre-course MCQ score, previous ALS experience, being a core member of the resuscitation team and the number of cardiac arrests attended in the preceding three months. Factors associated with a worse MCQ score were; increasing age, being on the e-ALS course (compared with two-day ALS), working in a private hospital, all professions (except resuscitation officers) when compared to doctors.
The first attempt CAS-Test pass rate was 82.6% and overall course pass rate 94.4%. The multivariate analysis is shown in Figure 2. Variables associated with a good CAS-Test outcome were; pre-course MCQ score, being a core member of the resuscitation team, previous ILS and ALS experience and increasing seniority. Increased age was associated with a worse outcome. There was a variation in terms of ethnicity with both MCQ and CAS-Test results, although there was no significant difference in the overall course multivariate analysis (not shown). The number of candidates on an ALS course and the number of courses run by a course centre had no effect on outcomes.
Conclusion: Increasing seniority and regular day-to-day management of critically unwell patients is most strongly associated with favourable ALS course outcomes. Identifying candidate demographics associated with worse assessment performance will allow course centres to identify candidates who may struggle at an earlier stage. This will allow them to have additional support during courses.
Figure 1.
Multivariate analysis of variables that predict post-course MCQ outcome.
Figure 2.
Multivariate analysis of variables that predict CAS-Test outcome.
0396
An Evaluation of the Intra-Hospital Transfer of Critically ill Patients at a Tertiary Centre
James Blair1, James Sherwin2 and Tonny Veenith2
1College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2Queen Elizabeth Hospital, University Hospitals Birmingham UHB NHS, Birmingham, United Kingdom
Abstract
Background: The safest environment for a critically ill patient is an intensive care unit (ICU). However, there may be situations where patients are required to leave the ICU such as for surgery or imaging procedures. Transfer between hospital departments involves many risks and requires careful planning to ensure safety and avoid complications.1 The transport of a critically ill patient is associated with life threatening adverse events and increased morbidity. Such events can include: brady- and tachyarrhythmias; hypo- and hypertension; increased intracranial pressure; cardiac arrest; brady- and tachypnoea; hypo- and hypercapnia and hypoxaemia. It has been suggested that adverse effects may occur in up to 70% of transfers.1 The procedure for transferring a critically ill patient is not currently standardised throughout the UK and published guidelines are inconsistent.2 The UK Intensive Care Society (ICS) sets ‘guidelines for the transport of the critically ill adult’.3
Objectives: To assess the effectiveness of patient transfer between the ICU and CT imaging department and to identify: 1. The average number of CT scans completed daily across the ICU. 2. The average length of time involved in patient transfer. 3. Adverse events associated with transfer and their incidence. 4. The number of CT scan results that contributed to a change in the patient’s management plan. 5. Measures to help reduce adverse outcomes associated with patient transfer.
Methods: Patients were screened for eligibility from September 2016 – November 2016. The study population was selected using pre-defined inclusion criteria (transfer to CT from the ICU). A proforma was designed and divided into two parts. A critical care team member accompanying the transfer completed the first part prospectively. The second part involved retrospective data extraction from online clinical systems. Datasets collected: basic demographics; inotropic, sedation and ventilation settings; pre and post-CT vital signs and ABG results; time taken to prep patient, transport and perform CT, and hand back over to ICU; issues and adverse events; medical grade of transfer team members and change of patient management due to the CT results.
Results: Over 54 days, 203 CT scans were performed, giving an average value of 3.8 scans per day. Average total disruption time: 51–60 minutes. Total number of adverse events: 44 (21.7%). Number of CT scan results that contributed to a change in the patient’s management plan: 184 (90.6%).
Conclusions: 57.6% of transfers were accompanied by either an ST4 or ST5 level doctor, 20.7% had no doctor and only 1 was supervised by a consultant. The association between staff grade and incidence of adverse events is unclear. On average, it took 51–60 minutes to transfer patients to/from CT imaging, with more adverse events occurring in those absent from ICU the longest. Attempting to reduce the transfer time may further compromise patient safety. Over 21% of patients transferred had an associated adverse event. Further analysis is required to establish the significance of current findings.
0397
Advanced Life Support – what factors influence candidate feedback?
Chris Thorne1, Peter Kimani2 and Gavin Perkins3
1North Bristol NHS Trust, Bristol, United Kingdom
2University of Warwick, Warwick, United Kingdom
3Heart of England NHS Foundation Trust, Birmingham, United Kingdom
Abstract
Introduction: Modern day business is driven by feedback. It shapes a company’s reputation and often dictates the allocation of resources. Healthcare institutions are increasingly recognising the importance of collecting feedback about an individual’s experience,1 whether this be patient feedback,2 staff feedback or candidate course feedback.3 Despite routine collection of feedback being commonplace on life support courses, there is a paucity of research into what candidate and course variables determine this feedback.
As part of an ongoing quality improvement initiative, the Resuscitation Council (UK) launched a new feedback platform on the 1st December 2017 which collated quantitative and qualitative feedback about the overall structure, organisation and delivery of the course.
Objectives: We aimed to ascertain which candidate, course and centre factors were associated with aspects of course feedback.
Methods: Participants enrolled on ALS courses between 1st December 2017 and 30th November 2018 were included. Demographic data was obtained when candidates registered on the Learning Management System (LMS). On completion of the course, candidates completed a feedback form which asked questions about the organisation, structure and delivery of the course with responses recorded on a Likert scale from 1 (strongly agree) to 6 (strongly disagree). Average feedback scores were calculated for different course types and course centres. Due to the non-parametric distribution of feedback scores they were recoded into binary categorical outcome variables with scores of <3 categorised as a positive feedback score and ≥3 as a negative feedback score.
Data were summarised with descriptive statistics. Univariate logistic regression models identified variables associated with course feedback. Significant predictor variables were subject to multivariate analysis. Odds ratios (OR), 95% confidence intervals and P-values were reported, with statistical significance set at P-values of <0.05.
Results: 17,690 candidates were included: 9,190 two-day ALS course, 7,336 e-ALS course, 1,120 recertification course, 44 modular course. Significant predictor variables of positive feedback in the multivariate analysis were high pre-course MCQ score (OR (95%CI) 1.07 (1.03, 1.12), P = 0.001), white ethnicity (compared to Asian, 1.18 (1.02, 1.15), P = 0.026), nursing background (compared with doctors, 1.26 (1.03, 1.56), P = 0.002). Predictor variables significantly associated with a lower feedback score included being on the e-ALS course compared to the two-day ALS (0.81 (0.71, 0.92), P < 0.001). Increasing seniority, when compared to an FY1 was a significant predictor: FY2 (0.81 (0.66, 0.99), P = 0.039), middle grade doctor or band 6 nurse (0.76 (0.59, 0.97), P = 0.025), and being a senior grade doctor or band 7–9 nurse (0.71 (0.51, 0.98), P = 0.038).
Conclusion: Feedback scores were generally better from younger, less experienced candidates and those from a nursing background. This suggests that those who are less familiar with the material engage better and find the course more rewarding. The e-ALS course demonstrated significantly worse feedback than the two-day course which may be due to the condensed nature of the course rendering it more time pressured. These data will allow the Resuscitation Council (UK) to refine the course, with particular focus on tackling the discrepancy between e-ALS and two-day ALS feedback and the perceived lack of satisfaction with increasing seniority.
0398
Costs of Continuous Renal Replacement Therapy: Regional Citrate Anticoagulation versus Heparin Anticoagulation
Sergio Mura1, William Ford2 and Mark Borthwick1
1Pharmacy Department, Oxford University Hospitals NHS Foundation Trust, Oxford, United Kingdom
2School of Pharmacy, Cardiff University, Cardiff, United Kingdom
Abstract
Introduction: Continuous Renal Replacement Therapy (CRRT) is commonly used in critically ill patients affected by Acute Kidney Injury (AKI) (1,2). Anticoagulants are used to prevent thrombus formation within the extracorporeal CRRT circuit, which would otherwise lead to circuit failure and suboptimal CRRT therapy. Heparin has been widely used for CRRT, but is returned to the patient from the CRRT circuit and increases the patient’s risk of bleeding (3). In recent years, citrate based anticoagulation has gained popularity. It has the potential to provide CRRT circuit anticoagulation without anticoagulating the patient, provide a longer CRRT circuit lifespan, and so provide uninterrupted CRRT without increasing the patient’s haemorrhage risk (4,5). Some consumable costs of citrate based CRRT are more expensive than with heparin, but it has been argued that because citrate circuits last longer and the patient haemorrhage risk is reduced, citrate based CRRT may be less expensive due to reduced blood transfusion requirements and reductions in other complications of therapy (5).
Objectives: To evaluate the real world CRRT related costs of a cohort of patients who received heparin based CRRT compared with a cohort of patients who received citrate based CRRT
Methods: This was a before and after style study. Six months of data were collected retrospectively for two groups of patients requiring CRRT on the adult general critical care units of the Oxford University Hospitals NHS Foundation Trust, a heparin CRRT group and a citrate CRRT group. Data were collected about the number of CRRT circuits used, units of blood products (red blood cells, platelets and fresh frozen plasma) used during the period the patient required CRRT support, the number of vascular catheters used, and volumes of CRRT related fluids consumed. Data were recorded in an Excel spreadsheet and reported using descriptive statistics. An Excel statistics add-in was used to conduct statistical analysis
Results: There were 38 patients in the heparin group (119 CRRT circuits) and 36 in the citrate group (75 CRRT circuits).
The average cost per patient of CRRT related consumables and fluids was £555 (median 339, 193–568) in the heparin group and £859 (median: 515, 301–1043) in the citrate group (p = 0.016, Mann Whitney U) (Figure 1).
There was no significant difference in the costs of blood products used between the two groups (Mann-Whitney U, p = 0.72) (Figure 2)
Conclusions: The implementation of the new Citrate CRRT protocol was associated with a significant increase of the cost of the treatment in regards of consumables and fluids. There was no significant difference between groups with regards to costs associated with blood products.
0399
Impact of delirium on carers of patients admitted to hospital – a national survey
Ahmed Gilani1, Randeep Mullhi2, Daman Mullhi3, Oliver Jones3, Larry Matthews3, Fang Gao-Smith4 and Tonny Veenith5
1Queen Elizabeth Hospital, University Hospitals Birmingham UHB NHS, Birmingham, United Kingdom
2University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
3The UK Sepsis Trust, Birmingham, United Kingdom
4University of Birmingham, Birmingham, United Kingdom
5Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Delirium is a reversible state of impaired cognition, inattention and altered level of consciousness.1 It has been associated with increased length of stay in intensive care, increased use of healthcare resources, and poorer functional recovery.1 Societies such as the National Institute for Health and Care Excellence and the American Society of Anesthesiologists recognise the prevention of delirium as a public health priority.2–4There is a scarcity of evidence of the experiences of delirium from a patient carer’s outlook, and its long-term impact from a physical and neurocognitive perspective. We present the largest known qualitative data set as collated from a national survey.
Objectives: This survey was part of a tripartite national survey to assess the impact of experiences of delirium in hospital by patients, carers, and medical professionals. It aimed to give credence to the paucity of evidence demonstrating the detrimental impact and experiences of delirium on patients and carers, and their quality of life after hospital discharge. This survey aimed to assess the physical and neurocognitive impact of delirium on patients as viewed by their carer.
Methods: This study was a simple anonymous patient survey after discharge from hospital – ethics approval was sought and not required; the project was electronically registered with the University Hospitals Birmingham Clinical Audit department. We conducted a nation-wide self-administered survey from carers of patients who had delirium identified via the UK Sepsis Trust. The survey was conducted securely electronically using internet-based software, and assessed carer’s experiences in three parts: experiences of delirium recalled by the carer of a patient, carer’s perceptions of patient’s quality of life after delirium, and the effect of the admission on the carer.
Results: Of the 144 respondents, most were female (84%) and identified as white (98%). Respondent ages ranged from 26 -55. Patients cared for were primarily admitted due to infection or sepsis-related illness, with 63% of the respondent’s relatives being admitted to intensive care. The commonest reported symptoms of delirium as assessed by carers included hallucinations (76%), agitation (74%), disorientation (72%), and memory-impairment (67%). Almost half of carers strongly agreed with the statement that their relative’s quality of life post-discharge had suffered as a result of their experience of delirium. Almost all carers stated they suffered with painful memories associated with the delirium episode. When posed the question ‘Studies suggest that the presence of carers may have an important role in reducing delirium by reducing stress and anxiety: with this in mind would you have liked to be involved in day to day care of your relative (e.g. mobilisation, efforts at communication etc.) whilst they were unwell?’, 80% of carers agreed or strongly agreed.
Conclusion: This survey adds credence of the distressing nature of delirium upon carers of patients, and its potential long-term neurocognitive impact. It further suggests the potential to involve carers of patients who are delirious as part of a mixture of pharmacological and non-pharmacological interventions that allow for a ‘marginal gains approach’ to the treatment of delirium.
0400
A less positive fluid balance is associated with survival in patients with pneumonia and septic shock – a retrospective cohort study
Minesh Chotalia1,2, Mansoor Bangash1,2, Tracie Matthews1,2, Dhruv Parekh1,2 and Jaimin Patel1,2
1University of Birmingham, Birmingham, United Kingdom
2University Hospitals Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Accumulation of a positive fluid balance is common in septic shock patients and has a well-known association with adverse outcomes.1 This harm may be secondary to aggressive fluid resuscitation or a consequence of a lower urinary output. It is unclear whether restricting early net fluid balance can improve outcomes from septic shock.
Objective: To assess whether cumulative fluid balance, intravenous fluid administration, urinary output and furosemide use at day 4 post ITU admission is associated with 90-day mortality in septic shock patients with pneumonia.
Methods: Patients admitted with a diagnosis of septic shock (Sepsis 3) secondary to a pneumonia (radiologically diagnosed) between April 2016 and July 2019 to the Queen Elizabeth Hospital, Birmingham were included. Patient data was retrieved using electronic patient records. Patients who died within 48 hours or had inaccuracies in recorded fluid balance were excluded. The primary outcome was 90-day mortality. Continuous data are presented as mean (SEM) and analysed using an unpaired t-test. Categorical data was analyzed using chi-squared test. Testing was performed using GraphPad Prism.
Results: 381 patients were admitted with septic shock secondary to pneumonia, of which 141 (37%) were excluded. 86% of exclusions were due to inaccurate fluid balance recording secondary to renal replacement therapy (RRT), reducing its incidence from 35% to 5%. Of the remaining 240 patients, the majority were male (60%) with a mean age of 60.6 ± 1.9 years, APACHE II 20.6 ±1.7 and CURB-65 score 3.9 ± 1.2. 90-day mortality was 41%, with 85% requiring invasive ventilation. Patients who died had a more positive balance, lower urinary output, greater incidence of AKI, but no difference in intravenous fluid or total input at day 1 and day 4 compared to survivors (Table 1). Intravenous furosemide use was significantly greater in survivors. However, patients who needed mechanical ventilation did have more intravenous fluid (6876 ± 271mls vs 5047 ±632mls; p = 0.008) and a more positive balance (3715 ± 314mls vs 1874 ± 644mls; p = 0.019) at day 4 compared to those that did not. There was no difference in urinary output (6918 ± 268 vs 6835 ± 689mls; p = 0.9), or use of furosemide (13% vs 16%; p = 0.36) between these cohorts.
Conclusion: This study found no difference in the volume of intravenous fluid administered between survivors and non-survivors of pneumonia and septic shock. Instead, a higher urinary output reducing net fluid balance was associated with survival. The effect of RRT on outcomes is poorly characterised in this study. The use of intravenous furosemide or early RRT to augment early fluid removal represents a potentially beneficial therapeutic strategy that merits prospective validation.
Table 1.
| Survived (141) | Died (99) | P value | |
|---|---|---|---|
| Day 1 | |||
| Cumulative Fluid Balance (ml) | 829 ± 143 | 1768 ± 165 | <0.0001 |
| Intravenous fluid (ml) | 2038 ± 134 | 1205 ± 92 | 0.14 |
| Urinary output (ml) | 1697 ± 94 | 1.20 ± 0.09 | 0.0004 |
| Day 4 (cumulative) | |||
| Fluid Balance (ml) | 2260 ± 366 | 5101 ± 405 | <0.0001 |
| Intravenous Fluid (ml) | 6642 ± 330 | 6413 ± 396 | 0.66 |
| Urinary output (ml) | 8376 ± 289 | 4814 ± 352 | <0.0001 |
| Creatinine (mg/dL) | 91.3 ± 5.8 | 117 ± 9.2 | 0.013 |
| AKI | 21 (15%) | 43 (43%) | <0.0001 |
| Furosemide | 26 (18%) | 6 (6%) | 0.006 |
| RRT | 6 (4%) | 6 (6%) | 0.94 |
0401
A Quality Initiative Retrospective Study on Vasopressor Use and Length of stay in a Tertiary Cardiac Intensive Care Unit
Mafalda Tasso de Almeida Ribeiro Reis Cocco1,2, Nicola Jones2,3 and Vasileios Zochios4,5
1Royal Papworth Hospital Intensive Care Unit, Cambridge, United Kingdom
2School of Clinical Medicine, University of Cambridge, Cambridge, United Kingdom
3Royal Papworth Hospital NHS Foundation Trust, Cambridge, United Kingdom
4Birmingham Acute Care Research Group, Institute of Inflammation and Ageing, Centre of Translational Inflammation Research, University of Birmingham, Birmingham, United Kingdom
5University Hospitals of Leicester NHS Trust, Department of Anaesthesia and Intensive Care Medicine, Glenfield Hospital, Leicester, United Kingdom
Abstract
Introduction: In predominantly surgical intensive care units (ICU), where the majority of admissions are elective surgical cases, scheduling of operative lists should consider patient flow through the ICU so as to minimise cancellations.
Background/Objective: Patients undergoing major surgery may need elective postoperative admission to ICU. Cancellation rates at the last minute in the NHS are reported as 1.1%, and the cause is often due to lack of ICU capacity. Cancellations have negative impact on patient, family, staff, hospital, and the wider NHS. Means to predict ICU availability / capacity based on predicting patient length of stay (LoS) in ICU might be useful in terms of scheduling of elective surgeries. We sought to determine whether vasopressor use post cardiac surgery was associated with LoS as this could then be used to help predict ICU capacity.
Methods: This quality initiative retrospective cohort study used retrospective data of all cardiac surgical patients admitted to Royal Papworth Hospital ICU following cardiac surgery from January 1, 2018 to December 31, 2018. Patients were divided into two groups: a group which required vasopressor medication (dopamine, noradrenaline or vasopressin) during their stay in ICU after surgery, and a control group which did not required any vasopressor use during their stay in ICU,
Results: Of the 1784 cardiac surgical patients admitted to ICU during 2018, 983 required vasopressors during their ICU stay, whereas 801 did not. The mean duration of stay in ICU was significantly higher for those patients who had vasopressors compared to the control group (84.1 v 27.9 hours [p < 0.001]), indicating that vasopressor use may predict a longer stay in ICU after cardiac surgery. In addition, this association was more pronounced in urgent and emergency surgical cases compared to elective surgical cases (106.9 v 72.4 hours [p < 0.001]).
Conclusions: This study shows that vasopressor use after cardiac surgery could be one of the factors influencing the duration of patient stay in ICU. Further studies are needed, evaluating this and other predictive factors, so that a prediction method can be created to help management of elective cardiac surgical patients and improve patient flow through cardiac ICU.
0402
CAM ICU is a useful tool to measure the impact of delirium in unselected critical care patients admitted to general, neurological and cardiac critical units?
Rebecca Boot1, Elizabeth Felton2, Fiona Howroyd2, Catherine Snelson1 and Tonny Veenith1
1Department of Anaesthesia & ICM, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
2Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Delirium is common (in up to 70% of admissions) and often under-recognised in critical care units (CCU).1 It is associated with mortality, morbidity, cognitive dysfunction (Leutz, et al., 2010) and has a significant impact on CCU survivorship. Delirium is linked to prolonged ventilation, ICU and hospital stay2-4 and adds to the morbidity of post-intensive care syndrome.
Objective: This study aimed to identify our prevalence, impact and assess our compliance with using CAM-ICU (Confusion Assessment Method for the Intensive Care Unit), the gold standard screening tool for identifying patients with delirium in the critical care setting.5
Methods: A prospective longitudinal cohort study was undertaken in a 75 bedded tertiary referral UK critical care unit, between August 2018 to December 2018. Patients were reviewed consecutively for two weeks between 14:00 and 16:00 hrs, during which a Richmond Agitation and Sedation Score (RASS) was completed. For patients that were found to have a RASS score > -1, CAM-ICU was completed. 106 Patients were excluded (106 patients) due to a length of stay less than two days, a previous known cognitive dysfunction, non-English speaking or were <18 years old.
Results and Conclusions: Two hundred seventeen patients were identified. A RASS score was completed on 111 patients, of which 24% of patients were found to be CAM-ICU positive within the 2 week snapshot period. 61% had a negative CAM-ICU, and 14% were unable to be assessed for delirium due to their RASS of <1 throughout the study. Higher rates of CAM-ICU positive were found in patients admitted to the neuro and cardiothoracic speciality areas, 50% and 32% respectively. CAM-ICU positive scores was more likely to be seen in males and after emergency admissions. No differences in ICNARC or APACHE II scores were identified between the two groups. The compliance with CAM-ICU was poor, out of 311 opportunities identified; CAM-ICU was only completed on 52 occasions (19%). Of the CAM positive group, only 14 percent had been screened for delirium. Patients that were found to be CAM-ICU positive had long lengths of ITU stay (18.4 +/− 11.9 vs. 14.3 +/− 29.8), longer lengths of hospital stay (44.9 +/− 29.7 vs. 36.8 +/− 41.8) and were less likely to be discharged back to their usual place of residence (53% vs. 15%).
Delirium in critical care is effecting a quarter of our patients yet continues to be underdiagnosed. This study validated the use of CAM ICU in general and specialist critical care areas such as neurological and cardiac critical care. Further work is required to increase compliance with CAM-ICU screening to identify patients at risk and implement an intervention to minimise the long-term effects associated with ICU delirium. Following this study, CAM-ICU screening became a mandatory feature on our electronic observation chart to be conducted, at a minimum, every 12 hourly.
0403
A Lot of Insulin
Tom Chad1, Marco Ulla1, Vanesa Garnelo Rey1 and Carlos Gómez2
1Imperial College Healthcare NHS Trust, London, United Kingdom
2Imperial School of Anaesthesia, London, United Kingdom
Abstract
Background: β-blockers and calcium channel blockers (CCB’s) account for a significant amount of cardiovascular drug exposures and contribute disproportionally to deaths secondary to cardiovascular medications.1 Overdose of these and other medications can result in cardiogenic shock refractory to common treatment modalities (catecholamines, glucagon, calcium replacement).
High-dose insulin infusion is an efficacious treatment for cardiogenic shock in this circumstance. This is a safe therapy with minimal associated adverse events in doses in the region of 0.5–10units/kg/hour.2 Proposed mechanisms include 1) enhanced glucose uptake and utilisation by cardiomyocytes, 2) increased inotropy via calcium independent and dependent pathways and 3) enhanced endothelial nitric oxide synthase action.2 Consensus suggests early initiation of this therapy is important. Interestingly no ceiling effect has been established.
Case Presentation: A 79-year-old male presented 9 hours after intentionally ingesting 300 tablets (in uncertain proportions) of amlodipine, aspirin, bisoprolol, diazepam, doxazosin, isosorbide mononitrate and ramipril. The medical history was significant for recent non-ST elevation myocardial infarction (ten days earlier) which was managed medically.
The initial heart rate (HR) and blood pressure (BP) (52bpm and 82/36 mmHg) worsened in the ED despite treatment with intravenous (IV) fluids, glucagon and calcium chloride. At the nadir of 42bpm and 56/27 mmHg noradrenaline was initiated. An insulin bolus (100units actrapid with IV dextrose 20%) then infusion (at 2 units/kg/hour) was given concurrently.
Upon ICU admission treatment was titrated against a persistently low HR and BP. The insulin infusion rate was up titrated to 20units/kg/hour within 4 hours (1600units/hour in our patient). Noradrenaline peaked at 0.59 µg/kg/hour. Dobutamine 5 µg/kg/hour was added 4 hours into ICU admission. An appreciable improvement in haemodynamic status was seen at the 14-hour mark.
Adverse events were observed (3 episodes of hypoglycaemia, 2 episodes hypokalaemia), however these were amenable to reactive IV replacement and none had significant sequelae. The highest rate of insulin infusion was maintained for 32 hours and weaned to zero by 57 hours (total dose; 61,334units). Glucose requirement remained relatively stable at an average of 33.8 g/hour.
Conclusions: The exact contribution of each agent to the clinical picture was not known in this case, which likely reflects the reality of large mixed overdoses in clinical practice. However, the ensuing syndrome of cardiogenic shock seen here likely reflects ingestion of toxic amounts of bisoprolol and amlodipine, with sustained hypotension and acute kidney injury exacerbated by the other agents involved.
Treatment failure with other measures (IV fluid, IV glucagon, IV calcium replacement) is well documented and reflected here.2 Use of catecholamine therapy is controversial where animal studies suggest limited benefit in this circumstance.3 Limiting catecholamine therapy was important in our patient with recent myocardial infarction. In fact the peak dose of noradrenaline is lower than has previously been required in CCB/β-blocker overdose, which may reflect a catecholamine sparing effect of aggressive up titrating of insulin.4
We provide evidence that safety and efficacy of a high-dose insulin infusion extended to a rate of 20units/kg/hour, the highest rate sustained in the literature.
0404
A longitudinal qualitative study of ICU survivors' health and social care support needs in the year post-ICU discharge
Pam Ramsay1, Lisa Salisbury2, Janice Rattray3, Guro Huby4, Tim Walsh5 and Susanne Kean5
1Edinburgh Napier University, Edinburgh, United Kingdom
2Queen Margaret University, Edinburgh, United Kingdom
3University of Dundee, Dundee, United Kingdom
4Ostfold University College, Ostfold, Norway
5University of Edinburgh, Edinburgh, United Kingdom
Abstract
Introduction: Survival following critical illness is associated with long-term physical and psychosocial sequelae. Supporting survivorship has been identified as an international research priority,1 yet little is known about ICU survivors’ health and social care support needs following hospital discharge, and how they evolve over time. Longitudinal support needs assessment tools have successfully been developed for use among other patient populations (notably cancer) but do not currently exist for ICU survivors.
Background: Originally developed for use among family members of stroke survivors, the Timing it Right (TIR) framework2 provides a practical, temporal framework within which to explore survivors' needs at key transitions and throughout the survivorship journey: the ICU admission; ward-based care; the return to community living, and longer-term recovery. It comprises 4 theoretically-derived categories of support need: informational, instrumental (equipment, training or practical help with everyday tasks), emotional (addressing psychological distress) and appraisal (feedback, evaluation or reassurance from clinicians and/or family members on progress towards recovery). Its previous use among a small sample of ICU survivors and family members suggest that it may usefully inform phase-specific interventions3, but detail is lacking.
Methods: Our study protocol and a constuctivist grounded theory of ICU survivorship have been published elsewhere.4,5 We conducted semi-structured, longitudinal interviews with 22 ICU survivors who had required ≥2days mechanical ventilation in one of two adult general ICUs in the east of Scotland. Interviews were conducted at 4 time points: prior to hospital discharge (n = 22), and at 4–6 weeks (n = 20), 6 months (n = 17) and 12 months (n = 17) following ICU discharge. Data were transcribed verbatim, managed and analysed using qualitative data analysis software (NVIVO). We undertook a thematic analysis, with reference to the needs identified in the TIR framework and explored their nature, relative importance and evolution over time. We also explored whether and how these needs were met, when, by whom, and the implications of unmet need.
Results: We developed a nuanced understanding of survivors’ support needs across the 4 categories of identified need. Although these were highly individualised and were interwoven in unanticipated ways, we devised a preliminary, over-arching matrix of support needs within and across key transitions in care. For example, survivors’ emotional support needs commonly included: making sense of the critical illness experience (including illness severity, amnesia and dreams, hallucinations or flashbacks); making sense of physical, psychological and emotional frailty; a perceived lack of understanding among clinicians; social isolation; a sense of vulnerability regarding the limits and timescale of recovery (including fear of recurrence), and concern for family members (including the perceived psychological and socioeconomic burden of critical illness). The relative importance of emotional support needs and its “make-up” varied widely over time and may, in many instances may have been mediated by addressing survivors' (unmet) informational, instrumental and/or appraisal needs.
Conclusion: This work supports the use of the TIR as a framework for phase-specific service development, although a population-level understanding of survivors’ support needs is needed. This work will therefore inform the development of a needs assessment questionnaire for use amongst the wider UK patient population.
0406
Performance-importance plots for improving family satisfaction with ICU care in the UK
Doug Gould, Izabella Orzechowska, Alvin Richards-Belle, Paloma Ferrando-Vivas, David Harrison and Kathryn M. Rowan
Intensive Care National Audit & Research Centre (ICNARC), London, United Kingdom
Abstract
Introduction: Eliciting the views and experiences of patients is essential to delivering a high-quality service.1 However, given that around 20% of patients admitted to an intensive care unit (ICU) do not survive, and those that do, are often unable to recall their experiences, measuring patient experience in ICU is challenging. Family members, therefore play an important role in eliciting the views and experiences of ICU care.
Background and objectives: The Family Satisfaction in the Intensive Care Unit (FS-ICU) questionnaire is the most widely validated measure of family experiences of ICU care.2 The FS-ICU 24-item questionnaire (FS-ICU-24) describes satisfaction with care overall and across three domains – satisfaction with care, information, and decision-making process.3 We sought to describe how responses from the FS-ICU-24 questionnaire can be displayed as performance-importance plots, to identify items that form likely candidates for quality improvement initiatives.
Methods: Using data from the Family Reported Experiences Evaluation (FREE) study4 which received completed FS-ICU-24 questionnaires from 7173 family members of 4615 patients from 20 representative ICUs, a performance-importance plot for overall family satisfaction with ICU care in the UK was created where each point in the performance-importance plot corresponds to one item of the FS-ICU-24. The Spearman’s rank correlation between each item and the overall family satisfaction score was plotted on the y-axis against the percentage of respondents rating the item as ‘excellent’ on the x-axis. The plot was divided into quadrants at the mean values on the x-and y-axes. Points in the upper left quadrant correspond to items that are highly correlated with overall satisfaction but have a lower than average proportion of ‘excellent’ ratings and therefore show potential for improvement.
Results: The performance-importance plot for the overall family satisfaction score suggests that the highest-priority items for quality improvement relate to the provision of information and how well the ICU staff provide emotional support to the family member. The item relating to the atmosphere (mood) in the ICU waiting room had the lowest proportion of ‘excellent’ ratings, but was ranked a lower priority for quality improvement because of its lower correlation with the overall family satisfaction score and the satisfaction with care domain score.
Conclusions: We have demonstrated the utility of performance-importance plots for identifying areas for quality improvement that may be targeted in efforts to improve family satisfaction with ICU care in the UK. While we report here the areas for improvement highlighted from the FREE study, this method can also be applied to identify important areas for quality improvement in individual ICUs.
0408
Pain Management in Rib Fractures in the Non-Trauma Centre Setting
David Clarke and Denise Stott
Buckinghamshire Healthcare NHS Trust, Aylesbury, United Kingdom
Abstract
Introduction and Background: Rib fractures are identified in 9–10% of trauma patients and are frequently concomitant with solid organ or visceral injury. (1) Mortality from chest wall trauma is high, ranging from 4–60% in the literature and complications are myriad (2). Poor outcomes related to pneumothorax, haemothorax, pulmonary contusion and laceration of the abdominal organs are common acutely, but more insidious complications related to pain such as hypoventilation, atelectasis and pneumonia are also frequent (3). Elderly patients show increased mortality and morbidity in the 24 hours post admission, but also increased risk of delayed complications such as pneumonia. There is evidence to suggest that early diagnosis through computed tomography and early analgesia can significantly improve outcomes in this group of patients. (4). Regional anaesthesia techniques have been shown to reduce mortality and morbidity in chest trauma (5)
Objectives: Given the high morbidity noted within this patient population we aimed to analyse our own admissions to inform a guideline for the management of pain in rib fractures in our District General Hospital Trauma Unit.
Methods: We performed a retrospective analysis of data related to patients referred to the pain service with rib fractures. Our study period was January 2018 to December 2018. We had no guideline in place prior to starting this project. We reviewed time to pain team referral, mode of analgesia, length of stay, requirement for chest drain, 28 day mortality, and requirement for critical care input via either critical care outreach or HDU/ITU admission.
Results: Among 23 patients presenting to our service over the specified period 22 patients presented following trauma, 6 of these patients were described as frail elderly, the further 1 patient sustained rib fractures during CPR. 7 patients required a chest drain for either pneumothorax or haemothorax. The median patient age was 65 years old with a median length of stay of 7 days. 2 patients (8.7%) were dead at 28 days post admission. Of the 23 patients 11 (48%) required critical care outreach referral, 5 (21%) were admitted to ITU. 13 patients were prescribed a PCA and only 3 received regional anaesthesia. The average time to pain team referral was 48 hours post admission.
Conclusions: Analysis of our service showed a significant morbidity and mortality in patients admitted with rib fractures and a sluggish response to the management of their pain. In response to this we have developed a guideline focussed on highlighting the vulnerability of this patient group. We encourage rapid referral to the pain team and early physiotherapy input. We use rib fracture scoring alongside an algorithmic approach to ensure early consideration of regional anaesthesia techniques, with explicit criteria for referral to critical care outreach and ICU when required. We also worked with our radiology department to agree that all patients admitted with chest trauma would be assessed with CT and have the number, and location, of rib fractures documented to allow rib fracture scoring. We aim to perform a repeat analysis in one year to assess impact of the guideline.
0409
Can patients with severe diabetic ketoacidosis be managed safely outside of critical care?
Danny McLernon-Billows, Alison Hall and Norman Main
Royal Liverpool University Hospital Critical Care Department, Liverpool, United Kingdom
Abstract
Introduction: The Joint British Diabetes Societies (JBDS) considers pH < 7.0 a marker of severe diabetic ketoacidosis (DKA), warranting critical care review.1 Despite producing profound metabolic disturbances DKA usually responds well to prompt treatment and carries a mortality of less than 1%.1 Around 13% of DKAs are admitted to UK critical care units.2 Reducing unnecessary admissions safely requires a reliable evidence base, however, there is a surprising lack of evidence regarding the safe triage of patients with DKA towards, or away from, critical care.3,4 Royal Liverpool University Hospital (RLUH) guidelines suggest all patients with a pH < 7.1 are referred to critical care.
Objectives: We aimed to find out whether DKA with a lowest pH of <7.0 is safely managed outside of critical care at RLUH and what features are associated with a need for organ support.
Methods: Electronic records of adults admitted in 2018 with discharge diagnosis of DKA were retrospectively reviewed. The RLUH protocol uses a fixed-rate insulin infusion based on JBDS (2013) guidelines.1 Patients were excluded if they did not meet DKA criteria (Table 1) or had missing data. The lowest pH during first 12 hours from diagnosis was identified. Organ support was defined as any intervention that could not be provided in a ward environment. Other suggested features of severe DKA as per JBDS (2013) were reviewed.1
Results: 241 admissions were screened and 135 met DKA criteria. 21% (29/135) had a lowest pH < 7.0, 79% (23/29) of whom were referred to critical care. 48% (14/29) were admitted to critical care and 31% (9/29) required organ support (central venous access 100%; inotropic support 56%; intubation and ventilation 44%; renal replacement therapy 33%). 5% (6/106) of patients with a pH > 7.0 were admitted to critical care and 4 required organ support, all for indications unrelated to DKA (e.g. stroke, dialysis-dependent kidney disease). The strongest overall predictors for needing organ support were: lowest pH < 6.9 (sensitivity 69%; specificity 98%; PPV 82%); and GCS < 14 (sensitivity 85%; specificity 96%; PPV 69%).
52% (15/29) of patients with a pH < 7.0 were managed outside of critical care – initially in the ED before transfer to a ward. These patients had an increased incidence of hypoglycaemia (glucose < 4 mmol/L) during first 24hours of treatment versus those in critical care (53% vs. 29%; p-value:0.2). However, all were discharged home with no inpatient mortality.
The overall inpatient mortality rate was 1.5% (2/135). Both deaths were planned withdrawals of care on critical care for conditions unrelated to the DKA.
Conclusions: The majority of patients with severe DKA (lowest pH < 7.0) were managed safely outside of critical care. Non-critical care management had a higher incidence of hypoglycaemia which was not statistically significant. The small cohort of patients with pH > 7.0 needing organ support did so for pathologies unrelated to DKA. The strongest predictors for needing organ support were pH < 6.9 and GCS < 14. The generalisability of our findings is limited by the small sample size and the single centre, retrospective nature of our study.
Table 1.
DKA Criteria1.
| Diabetic | Ketotic | Acidosis |
|---|---|---|
| Glucose >11 mmol/L OR Known diabetes | ≥3 mmol/L OR Ketonuria ≥ 2+ | pH < 7.30 OR HCO3 < 15 |
0410
Delivering appropriate transfusions during major haemorrhage: Do we really need viscoelastic tests, or will laboratory tests suffice?
Simon Gill, Jennifer Ridenton, Christopher Pritchett and Jonathan Cheung
Royal Cornwall Hospitals NHS Trust, Truro, United Kingdom
Abstract
Introduction: Detection and correction of coagulopathy during major haemorrhage is difficult. Current recommendations are still to use standard laboratory tests (SLTs), sent every 30 to 60 minutes to guide transfusion of required products.1 Such tests are acknowledged to have inherent limitations – particularly in relation to turn-around times.2 The British Society of Haematology have recently released pragmatic guidance for use of viscoelastic tests (such as ROTEM and TEG).3 This audit establishes current use of SLTs in major haemorrhage at a large District General Hospital, to assess the potential benefits of introducing Rotational thromboelastometry (ROTEM).
Methods: This retrospective study obtained data from the Royal Cornwall Hospital electronic blood bank database between June 2018 and June 2019. All patients who had ≥4 units of blood product requested and ≥1 units transfused were included (n = 247). Patients transfused secondary to chronic disease were excluded (n = 38). We analysed 1) Time of blood product request. 2) Time of SLT result publication. 3) Whether transfusion was ‘clinical’ or ‘scientific’ – eg: were blood products given before or after the result was available. 4) Where lab data was available, whether it supported delivery of the transfused products.
Results: The number of acute major haemorrhages identified was n = 209. 100% of major haemorrhage patients had an SLT sent. 49.3% had SLT results available prior to blood product transfusion. Of those patients who had a SLT result available prior to transfusion, 69% were given blood products in line with local transfusion guidelines (Hb < 75 g/L, INR >1.6, Platelets <75 × 109/L, Fibrinogen <2.0 g/l). Of the patients who did not have a SLT available prior to transfusion, 8% were transfused in line with local guidelines.
Conclusion: Transfusion in major haemorrhage depends on a number of issues, not laboratory values alone. In certain circumstances it may be necessary to transfuse prior to results being available. However, it is disappointing that less than half of patients received SLT guided transfusions. Where SLT data was available it would appear blood products were used more in line with local transfusion policy.
We conclude that by making coagulation data available more readily and quickly at the point-of-care, ROTEM may help reduce unnecessary transfusions, aid earlier diagnosis of coagulopathy and help direct its treatment.
0411
Trends in incidence and outcomes for ICU patients admitted following out-of-hospital cardiac arrest in Scotland
Chanh Ho1, Gareth Clegg2, Mark Dunn3, Nynke Halbesma1 and Nazir Lone1,3,4
1Usher Institute, University of Edinburgh, Edinburgh, United Kingdom
2University of Edinburgh, Edinburgh, United Kingdom
3Royal Infirmary of Edinburgh, Edinburgh, United Kingdom
4University Dept of Anaesthetics, Critical Care and Pain Medicine, University of Edinburgh, Edinburgh, United Kingdom
Abstract
Introduction: Out-of-hospital cardiac arrest (OHCA) is a significant healthcare challenge and usually associated with a poor prognosis. In Scotland, over 3,500 people suffer from OHCA where resuscitation was attempted by the Scottish Ambulance Service (SAS).1 In recent years, there have been many improvements in pre-hospital and developments in post-resuscitation care.2 No research has evaluated whether the incidence and mortality of OHCA patients who were admitted to Scottish ICU have changed over time.
Objectives: We aimed to evaluate the trends in incidence, 30-day and 1-year mortality following ICU admission after OHCA. Additionally, we aimed to investigate independent predictors of mortality at these time points.
Methods: A population-based retrospective cohort study was conducted, comprising 1131 OHCA patients, aged ≥16 years, admitted to Scottish ICUs during 1/1/2011-31/12/2016. OHCA due to trauma or those in whom resuscitation was not attempted were excluded. Data were obtained from the SAS database and linked to the Scottish Intensive Care Society Audit Group database and death records. Outcomes: 30-day and 1-year mortality. Change in incidence was examined using Poisson regression. Independent predictors and trends over time of mortality were evaluated using logistic regression.
Results: The overall age-/sex-standardised incidence of OHCA patients admitted to ICU was significantly increased from 3.8 cases per 100 000 to 5.3 cases per 100 000 Scottish residents between 2011 and 2016 (p < 0.001). Patients aged 16–49 years (p < 0.0001), being male (p < 0.0001), and having non-shockable heart rhythm (p = 0.006) experienced the largest increases in incidence rates. Median severity of illness (measured using APACHE II score) was lower, whereas median lowest temperature within the first 24 hours of admission was higher over the study period. The overall 30-day and 1-year mortality following ICU admission after OHCA were 61.7% and 64.4% respectively. 30-day mortality and 1-year mortality did not change significantly during the duration of the study in pre-specified subgroups and overall. Change in mortality varied between age groups. Male patients and those with shockable heart rhythm admitted to ICU in 2016 we re more likely to die at 30 days and 1 year compared with 2011. Finally, age >72 years, highest deprivation, higher severity of illness score, non-shockable presenting rhythm, lowest temperature within the first 24 hours of less than 32oC, treatment with mechanical ventilation or vasoactive therapy within the first 24 hours were significantly associated with increased mortality 30-day and 1-year mortality.
Conclusions: This population-level cohort study has demonstrated that there was no change in the 30-day and 1-year mortality from 2011 to 2016 in Scotland. Age, social deprivation, severity of illness, lowest temperature and treatment of organ support within the first 24 hours were independent predictors of 30-day and 1-year mortality. These findings identify areas for further research and practice to improve the outcomes, as well as providing longer-term outcome data to inform clinical decision-making in practice.
0413
Neuroinflammatory pathways in moderate to severe TBI – protein and micro RNA analysis
Nick Talbot1,2, Animesh Acharjee3, Sandeep Gudibande4, Tony Whitehouse2, Antonio Belli1,2 and Tonny Veenith2
1Institute of Inflammation and Ageing, College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
3Institute of Cancer and Genomic Sciences, University of Birmingham, Birmingham, United Kingdom
4Lancashire Teaching Hospitals NHS Foundation Trust., Preston, United Kingdom
Abstract
Introduction: Traumatic brain injury (TBI) releases a cascade of messengers activating processes that cause secondary brain injury. These include excitotoxicity, reactive oxygen species production, blood-brain barrier disruption and mitochondrial dysfunction. Neuroinflammation and cytokine release are a common mechanistic link between these processes. Attempts to develop clinically applicable blood tests have been hampered by heterogeneity in pathology and inter-patient variability in injury response.
Objectives: To understand the temporal profile and underlying epigenetics of the immune response that contributes to neuronal death in patients with moderate to severe TBI.
Methods: Nine moderate to severe TBI patients admitted to neurocritical care had serum samples drawn at the time of injury and then every 24 hours up to 72 hours. Protein analysis was conducted by O-link using their systemic inflammatory and neurology protein biomarkers immunoassay. Whole genome microRNA (miRNA) sequencing was performed by Qiagen using their next generation sequencing technology.
We performed univariate student t-test with the Benjamini–Hochberg (BH) method to control the False Discovery Rate (FDR) and Random Forest (RF) machine learning to identify relevant biomarkers for TBI. Missing values were imputed using the minimum concentrations across all patients and protein and miRNA data further normalized using auto-scaling (subtracting the mean and dividing by standard deviation).
Results: Univariate t-test analysis identified five serum proteins with differential expression over time: PLXNB1, PDGF-R-alpha, IL10-RB, PD-L1 and CDH3. The most consistent change in expression was found in PLXNB1, PDGF-R-alpha and IL-10RB.
RF machine learning analysis ranked the top four proteins as GFR-alpha-1, IL-10RB, PLXNB1, PDGF-R-alpha.
Abstract
RF analysis ranked the greatest change in normalised concentration in microRNAs: miR-1296-5, miR-206, miR-195-5p, miR-143-3p and miR-1307-5p over the first 72 hours after injury. miR-1296-5 and miR-206 showed an increase over time whereas miR-195-5p and miR-143-3p expression value was decreased.
Conclusion: PLXNB1 is a member of the semaphorin family of proteins that coordinate neurite outgrowth, remodelling and synaptic plasticity. PDGF-R-alpha signalling on astrocytes promotes blood brain barrier permeability and neuronal injury in a range of neuropathological conditions. IL-10 is a prototypical anti-inflammatory cytokine that has neurotrophic effects in vivo. miR-206 features in a panel of circulating brain derived extracellular vesicle that can classify patients with mild TBI versus healthy controls. miR-206 is over expressed in human Alzheimer’s patients and in experimental models regulates brain derived neurotrophic factor.
Understanding the temporal changes in inflammatory response and the epigenomic signature after TBI will enhance our knowledge of the disease process, guide neurotherapeutic interventions and identify putative biomarkers to assess treatment response.
| List of proteins | p value (raw) | p value (FDR corrected) | Significant differences over time (hours) |
|---|---|---|---|
| PLXNB1 | 1.90E-05 | 0.00349 | 0 – 24, 0 – 48, 0 – 72, 24 – 72, 48 – 72 |
| PDGF-R-alpha | 5.16E-05 | 0.004746 | 0 – 24, 0 – 48, 0 – 72, 24 – 48 |
| IL-10RB | 0.000599 | 0.032957 | 0 – 48, 0 – 72, 24 – 72 |
| PD-L1 | 0.000716 | 0.032957 | 0 – 24, 0 – 48, 0 – 72 |
| CDH3 | 0.001215 | 0.044706 | 0 – 48, 0 – 72, 24 – 72 |
0414
A national survey of speech and language therapy service provision in ICU: what’s the state of play?
Claire Mills1,2, Aeron Ginnelly3, Christina Iezzi4, Emma Cowpe5, Anna-Liisa Sutt6,7,8, Helen Newman3, Susan McGowan9 and Sarah Wallace10,11
1Speech & Language Therapy, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom
2Academic Unit of Health Economics, University of Leeds, Leeds, United Kingdom
3Speech & Language Therapy, Royal Free London NHS Foundation Trust, London, United Kingdom
4Speech & Language Therapy, Guy's & St Thomas' NHS Foundation Trust, London, United Kingdom
5Speech and Language Therapy, Royal Hospital for Neuro-disability, London, United Kingdom
6Speech & Language Therapy, Barts Health NHS Trust, London, United Kingdom
7Critical Care Research Group, The Prince Charles Hospital, Brisbane, Australia
8Northside Medical School, University of Queensland, Brisbane, Australia
9National Hospital for Neurology & Neurosurgery, London, United Kingdom
10Wythenshawe Hospital, Manchester University NHS Foundation Trust, Manchester, United Kingdom
11Chair RCSLT Tracheostomy Clinical Excellence Network, London, United Kingdom
Abstract
Introduction: Best practice for Speech and Language Therapy (SLT) services in the intensive care unit (ICU) is outlined in UK national guidance documents.1,2,3,4 Whilst wide variation in access to SLT is suspected, actual clinical service provision and skill mix in UK ICUs is unknown and this was the aim of the study.
Methods: An online survey was compiled by the Royal College of Speech and Language Therapists Tracheostomy Clinical Excellence Network (CEN) committee and distributed to UK SLT networks, and via social media, between December 2018 and March 2019. The survey targeted SLTs working in adult, paediatric and neonatal ICUs and respondents completed one survey per service. Quantitative data was analysed using Microsoft Excel® (2016).
Results: Sixty-four responses were received from a range of district general (n = 29, 45%), university teaching (n = 30, 47%) and specialist (n = 5, 8%) hospitals, including three from paediatric services. Responses included 68 hospitals (25% of all ICUs) and 56 Trusts/Boards (34% of all Trusts/Boards). There were no responses from Scotland or Northern Ireland. Inadequate SLT service provision was reported for communication (n = 56, 88%), swallowing (n = 54, 84%), and tracheostomy weaning interventions (n = 57, 89%). Forty-two per cent (n = 27) of services did not have access to Fibreoptic Endoscopic Evaluation of Swallowing (FEES). Although 91% of services (n = 58) use Passy Muir Valves in their ICUs, 20% of respondents (n = 12) stated SLT were never or rarely involved in the assessment process. Furthermore, 22% (n = 14) stated that they were never or rarely involved in the identification of appropriate communication aids for patients. Under-referral of patients was reported by 80% (n = 51) of services, and 48% of respondents (n = 31) stated that referrals were not timely. Poor attendance at MDT meetings included 64% (n = 41) of services never attending ward rounds and 45% (n = 29) never attending tracheostomy rounds. Eighty-eight per cent (n = 56) of services provide teaching or training to the MDT and 30% of services (n = 19) conduct research or audit. The majority of SLT services were unable to provide daily (n = 44, 69%), weekend (n = 62, 97%) or bank holiday cover (n = 60, 94%). Seventy-three per cent of SLT services (n = 47) failed to meet GPICS2 requirement to see all tracheostomised patients and 3% of services (n = 2) provide 45 minutes of daily therapy (NICE CG833). The majority of respondents reported receiving no funding from ICU for SLT service provision (Figure 1). Respondents reported an actual median staffing ratio of 0.03 whole time equivalent (WTE) per paediatric ICU bed (range: 0.01–0.04) and 0.01 WTE per adult ICU bed (range: 0.001–0.05).
Conclusions: Whilst the ideal staffing levels and skill mix of SLTs in ICU would depend on patient case mix, the current situation with SLT service provision in the UK is deeply concerning. Lack of direct funding for SLT services in UK ICUs is leading to poor compliance with national guidance and significant unmet patient need. This risks substandard care in the management of swallowing, communication and tracheostomy weaning and worse patient experience and outcomes. Dedicated ICU funding for SLT is required to facilitate SLT best practice and research in ICUs.
0415
Long-term outcomes following cardiopulmonary resuscitation in a British District General Hospital
James Heggie and Michael Reay
The Dudley Group NHS Foundation Trust, Dudley, United Kingdom
Abstract
It is estimated that less than 1 in 10 patients suffering an out-of-hospital cardiac arrest will survive to hospital discharge. Russells Hall Hospital is a District General Hospital in Dudley in the United Kingdom. The Intensive Care Unit (ICU) frequently deals with immediate survivors of cardiac arrest. We evaluated outcomes in patients surviving to receive ICU care in order to better counsel patients and relatives suffering this devastating event.
We performed a retrospective service evaluation of all patients admitted to the Intensive Care unit in the years 2013 to 2017 (the duration of our electronic record) who had received CPR within the 24 hours prior to admission whilst not admitted to the hospital. Pre-admission events were obtained by locating electronic emergency department records and ambulance sheets. Data regarding their post-ICU hospital course was obtained by manually reviewed the paper record. The General practitioners of survivors were contacted for information regarding health status following discharge. This took the form of a questionnaire requesting whether the patient was alive, their date of death if not, whether the GP had listed them on their Gold Standard Framework (a GP record of patients approaching the end of their life), a brief assessment of their functional status, and the number of ongoing interactions with healthcare.
125 patients were identified. 60 patients (48%) survived to be discharged from ICU. 42 patients (34%) survived to be discharged from the hospital. Of the 18 patients who died in hospital after discharge from ICU, 14 (78%) had been identified as dying prior to discharge and received palliative care elsewhere in the hospital.
We received 30 responses for the 42 patients discharged (71% response rate). Of these 20 (67%) were alive as of August 2019. Were this rate to apply to all successful discharged within this period, we would expect approximately 28 survivors from 125 admission giving an overall survival rate of 22%. Unfortunately, the date of death field was incomplete in the majority of cases therefore it has not been possible to calculate rates of death or survival to specific time-points. Only one patient was identified by the GSF record as being in the last year of life. No patient required more than 3 visits to their GP in the time following their discharge from hospital. No patient required more than 3 visits to secondary care following their discharge from hospital. We have previously reported that 24 patients (57%) were able to walk by the time of hospital discharge and that 20 of these (48%) were able to do so independently. Most patient discharged were living in their own home as of August 2018 although with varying degrees of additional support required.
In this selected population our estimated overall survival to at least 8 months of 22% exceeds the reported survival rates for all comers. The functional status of survivors appears good.
0416
Impact of non-pandemic influenza on a single centre critical care unit : winter 2018–19 at University Hospitals North Midlands NHS Trust (UHNM)
David Cartlidge, Matt Rowley, Prabhjoyt Kler and Bryan Carr
University Hospitals North Midlands, Stoke-on-Trent, United Kingdom
Abstract
Introduction: Non-pandemic flu infections have routinely led to peaks of critical care admissions during the winter periods. The most predominant strain is influenza A and these cohorts of patients have a high incidence of acute respiratory distress syndrome (ARDS).1 Influenza can lead onto secondary bacterial infections in both the respiratory tract and blood-stream further impacting on the morbidity and mortality in this patient group.1 The primary mechanism is the viral infection causing inflammation of the lung parenchyma and immunosuppression leading to systemic spread and opportunistic infections.2
Figures for the 2015–16 flu season reported 2190 patients were admitted to critical care units in England of which 165 deaths occured.1 Whilst most patients have self-limiting viral infections which resolve within 2–5 days, those with more complicated illness may need intensive care unit (ICU) admission for organ support.1
Methods/objectives: The aim of our study was to look at the demographics and outcomes of non-pandemic influenza admission to UHNM critical care unit. This was a retrospective case-based review looking at all primary admissions over the period 1st October 2018 to 28th February 2019 with a diagnosis of influenza.
Results: A total of 27 patients were admitted to the critical care unit at UHNM during this period with a positive flu swab. Of these 13/27 (48%) were male with a median age 50 years (range 19–81). 13 (48%), required advanced respiratory support with 7 being proned and 9 received neuromuscular blockade from this group. 96% required both respiratory and cardiovascular organ support. The median APACHE II score for our patient cohort was 29.35 with a predicted mortality of 21%. Actual ICU mortality was 19%. 14.8% (4/27) of patients had proven bacterial infection coexisting with influenza infection within the first 48 hours, with 25.9% of patients developing hospital acquired bacterial respiratory infections after 48 hours of admission. Of the 27 patients, 13 had no risk factors of being an at risk group for complicated seasonal influenza (48%). The result of this seasonal influenza cohort meant a total of 336 ICU bed days were used at UHNM, 7.3% of bed days for this period.
Conclusion: Influenza requiring critical care admission carries a high mortality, in line with patient severity of illness. Risk factors appear of limited value in predicting requirement for critical care admission in these patients, with almost half of patients in our cohort with no prior co-morbidities. Community acquired, and unit acquired bacterial infections are common, Even without pandemic status, seasonal influenza imposes a significant burden on scarce critical care resources. Our single centre study has highlighted potential further education for early admission to ICU for deteriorating flu positive patients, alongside further study of patients with zero risk factors and severity of illness.
0417
Dinitrophenol – The Deadly Diet Drug
Jonarthan Thevanayagam1, Jonathon Coates2, Helen Peet3 and Adam Smith3
1Queen Alexandra Hosptial, Portsmouth, United Kingdom
2Queen Alexandra Hospital, Portsmouth, United Kingdom
3Queen Alexandra Hospital, Queen Alexandra Hospital, United Kingdom
Abstract
We describe a case of a 31-year old man who presented after taking 5 g of 2,4-dinitrophenol (DNP). The toxidrome from this readily available drug is rare and striking and we believe others should be aware of it.
Case Presentation: He presented with an initially with mild hyperthermia, diaphoresis, tachycardia and respiratory alkalosis. This progressed quickly to an agitated state, despite fluid and benzodiazepine administration and his hyperthermia was resistant to external cooling. He was sedated and ventilated and within minutes lost cardiac output and cardiopulmonary resuscitation started. His immediate resuscitation blood gas confirmed a marked metabolic acidosis which worsened during arrest. His skin took on a bright yellow colour and his perspiration was tinged yellow. Approximately 16-minutes into the resuscitation attempt he developed extreme muscle rigidity compromising chest compressions, and facial muscle rigidity prevented suctioning of the endotracheal tube past the teeth, although end-tidal carbon dioxide monitoring was never lost. A 90-minute resuscitation attempt was performed as per ALS algorithm with asystole throughout and cardiac standstill found on repeated echocardiograms. Lung ultrasound ruled out pneumothorax. Treatments given included 16 mg adrenaline, 20 ml 10% calcium gluconate, 200 ml 8.4% sodium bicarbonate, 22units actrapid insulin and 100 ml 50% glucose, 100 mg rocuronium and 200 mg dantrolene. Advice was also taken from the National Poisons service and resuscitation attempt was stopped with the family and chaplain present.
Background: DNP is a precursor to trinitrotoluene (TNT) and during the First World War DNP was used in the production of explosives. Factory workers manufacturing DNP described lethargy, weight loss, fever and perspiration.1,2 This sparked Tainter and Cutting’s studies into DNP, finding it to increase basal metabolic rate. It was marketed as a weight loss pill in the interwar period. However, deaths related to its use indicated its toxicity, and it was soon banned. In more recent years it has been available widely over the internet.
DNP is highly toxic if ingested, inhaled or topical absorption occurs.3 Due to individual variation toxicity to DNP can occur with doses recommended for weight loss (2–10 mg/kg/d). The mechanism of toxicity is by uncoupling mitochondrial oxidative phosphorylation, leading to energy production without adenosine triphosphate (ATP) generation. Cells, therefore, rely on anaerobic respiration leading to pyruvate generation and lactic acidosis. Hyperpyrexia leads to widespread effects on a cellular level leading to enzyme denaturing, cell apoptosis and cell lysis. ATP depletion is thought to lead to cytosolic release of calcium in the sarcoplasmic reticulum, resulting in muscle rigidity[4,5]. The resultant massive cell death leads to multiorgan failure and ultimately death.
Mortality is high but treatment options attempted within the literature include charcoal, benzodiazepines, sedation and ventilation, muscle paralysis, active cooling, correcting acidosis with sodium bicarbonate, methylene blue for methaemoglobinaemia, dantrolene and haemodialysis including the use of specialised filters[6,7,8,9,10].
Conclusion: Many treatments have been attempted with limited success in DNP exposure, and NPIS revealed that no one has survived 2 g ingestion of DNP. We would advocate early intervention, securing the airway and alternative forms of CPR as the muscle rigidity compromised the resuscitation attempt.
0418
National speech and language therapy service provision in ICU: why isn't it good enough?
Claire Mills1,2, Helen Newman3, Aeron Ginnelly4, Christina Iezzi5, Emma Cowpe6, Anna-Liisa Sutt7,8,9, Jude Sadiq10, Susan McGowan11 and Sarah Wallace12,13
1Speech & Language Therapy, Leeds Teaching Hospitals NHS Trust, Leeds, United Kingdom
2Academic Unit of Health Economics, University of Leeds, Leeds, United Kingdom
3Speech & Language Therapy, Royal Free London NHS Foundation Trust, Barnet, United Kingdom
4Speech & Language Therapy, Royal Free London NHS Foundation Trust, London, United Kingdom
5Speech & Language Therapy, Guy's & St Thomas' NHS Foundation Trust, London, United Kingdom
6Speech and Language Therapy, Royal Hospital for Neuro-disability, London, United Kingdom
7Speech & Language Therapy, Barts Health NHS Trust, London, United Kingdom
8Critical Care Research Group, The Prince Charles Hospital, Brisbane, Australia
9Northside Medical School, University of Queensland, Brisbane, Australia
10Speech & Language Therapy Department, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, United Kingdom
11National Hospital for Neurology & Neurosurgery, London, United Kingdom
12Wythenshawe Hospital, Manchester University NHS Foundation Trust, Manchester, United Kingdom
13Chair RCSLT Tracheostomy Clinical Excellence Network, London, United Kingdom
Abstract
Introduction: The Guidelines for the Provision of Intensive Care Services 2 (GPICS)1 recommends a speech and language therapy (SLT) staffing ratio of 0.1 WTE per bed and for all tracheostomy patients to be seen by SLT. Inadequate SLT staffing, skill mix, resources and referral variability across UK Intensive Care Units (ICUs) is suspected. This study aimed to explore underlying reasons for inadequate SLT staffing, identify barriers and possible solutions for ICU SLT service provision.
Methods: An online survey was compiled by the Royal College of Speech and Language Therapists Tracheostomy Clinical Excellence Network (RCSLT Trache CEN) committee and distributed to UK SLT networks, and via social media between December 2018 and March 2019. The survey targeted SLTs working in adult, paediatric and neonatal ICUs. Content analysis of the qualitative data was carried out using QSR International’s NVivo 12 software. Three authors completed independent coding of the data and achieved consensus.
Results: Sixty-four responses were received from district general (n = 29, 45%), university teaching (n = 30, 47%) and specialist (n = 5, 8%) hospitals, including three paediatric services. Responses included 68 hospitals and 56 Trusts/Boards. There were estimated 25% hospital and 34% Trust/Board response rates for the whole of the UK; with no responses from Scotland or Northern Ireland. Five respondents (8%) reported adequate SLT resources for swallowing, communication and tracheostomy weaning intervention with a further 6 (9%) reporting it for one/two areas. The most common factors contributing to adequate staffing were MDT support (33%; n = 3) and co-opting resources from other areas (22%; n = 2). Fifty-nine SLTs (92%) reported inadequate staffing due to lack of funding (54%; n = 32), business case declined (10%; n = 6), historical staffing (8%; n = 5), increased demand (8%; n = 5), skill limitation (8%; n = 5), pressures elsewhere (5%; n = 3) and lack of MDT understanding SLT role (5%; n = 3). Thirty SLTs (47%) indicated that their ICU service is provided by the generic SLT cover, and 16 SLTs (25%) specifically stated that their service is provided by non-ICU specialist SLTs.
Fifty-one SLTs (78%) stated that under-referral was a problem and 33 (52%) thought referrals were not timely. The primary reasons for under-referral were lack of MDT understanding of SLT role and impact (46%; n = 24), lack of awareness of problem (25%; n = 13; this included lack of understanding of post-extubation dysphagia n = 6), and MDT perceiving poor SLT capacity (12%; n = 6). Respondents reported various risks associated with insufficient SLT staffing, see Table 1. Nineteen (30%) respondents were conducting audit or service evaluation, of which 63% audit, 16% Global Tracheostomy Collaborative data collection, 16% service evaluation. Two of the sixty-four services (3%) were conducting research.
Conclusions: Substantial work is needed within the SLT profession and amongst ICU MDT members to address identified issues. Increased knowledge would likely lead to improved integration of SLTs within ICU teams, which in turn would help minimise patient complications, and contribute to improving patient outcomes and quality of life.
Table 1.
Risks associated with insufficient SLT staffing.

|
0419
Development of a Multi- Disciplinary Intensive Care Unit (ICU) liberation working group as n intervention for the management of delirium and introduction of the ABCDEF bundle within the ICU
Rebecca Lewis, Vinoth Ravi, Jiehan Yeo, Angel Choy, Adam Riedlinger, Fenella Smith, Emily Flowers, Niall Mcdermott, Ritesh Maharaj and Reena Mehta
Kings College London, London, United Kingdom
Abstract
Background: Delirium is a frequent diagnosis within the ICU and is a condition that is both preventable and potentially reversible that can lead to increased mortality, increased length of stay and poor outcomes. It can also be one of the most difficult conditions to manage within the ICU. The ABCDEF bundle for ICU liberation has been developed to consider the management of delirium within the bigger picture and co-ordinate multiple aspects of care to focus on highlighting delirium management optimisation (1).
Objectives: Our aim was to develop a multi- disciplinary ICU liberation group to improve the management of delirium within our ICU and introducing the concept of the ABCDEF bundle.
Methods: The working group was formed from multiple team members within the ICU. The group is chaired by a senior pharmacist with representation from ICU consultant, ICU registrar and junior doctors, senior ICU nurses, physiotherapist, occupational therapist and speech and language therapists. As the bundle encompasses all areas of care each member of the group are able to contribute their specialist knowledge to develop an audit tool based on the ABCDEF bundle. The group meet every 4–6 weeks to discuss ongoing issues raised, improvement strategies and development of ongoing audit.
A complex audit tool has been developed using surrogate information from data routinely collected within the ICU for each section of the bundle. This tool has been used to complete a cross sectional audit of patients over a 24 hour period. It was conducted in a large central London 73 bed critical care unit and completed at 3 time points.
Results: The results from all 3 audits were combine and results analysed. Our group found 74% of patients had pain assessed regularly and the CAM ICU tool complete in 84% of patients. Sedation was also assessed regularly in 77% of patients and a Sedation hold complete if appropriate in 79%, however sedation targets were only set in 20% of patients medical notes. Unfortunately, only 55% of patients underwent a spontaneous breathing trial in appropriate cases but 66% of patients were actively mobilised on the ICU. It was only document in the medical notes that the family had been updated in 47% of patients, however it appears that it is likely that this happens at the bedside but not formally recorded.
Conclusion: With the development of a MDT ICU liberation working group we have begun to co-ordinate and align improvement in the management and prevention of many aspects of delirium applying the ABCDEF bundle. This group is still within its infancy but has already achieved the development of an ongoing complex audit tool to direct further work, patient information leaflets and teaching programmes. There are many more planned interventions from this group including awareness weeks and specific teaching aspects with certain roles
0420
A retrospective analysis of injuries and analgesia given to patients with rib fractures in a Major Trauma Center
Gabor Trembickij, Andrew Nash and Ahilanadan Dushianthan
Southampton General Hospital, Southampton, United Kingdom
Abstract
Introduction: Rib fractures (RF) are very common and associated with significant morbidity. Pain management for patients with RF is challenging but effective analgesia improves ventilation and reduces secondary pulmonary complications.
Objectives: Our objective was to review the type of analgesia given to patients, who were admitted to the hospital with rib fractures.
Method: Retrospective analysis of consecutive patients admitted with a chest injury from January 2017 to December 2018. Patients were identified from the TARN database. All clinical data was obtained from hospital electronic databases. We calculated a rib fracture score (RFS = [number of fractured ribs x sides]+ age factor) and compared the analgesia prescribed with the Rib fracture management guideline in accordance with a published guidance.1
Results: 64 patients were identified, 60% male with a mean age of 68 years (range 30–95). The commonest mechanism of injury was fall < 2m (61%) followed by RTC (20%). Seventeen (27%) patients were admitted (27%) to a level2/level3 area. Average intensive care unit (ICU)/ high dependency unit (HDU) length of stay (LOS) was 4 (± SD 4) days and mean hospital LOS was 12 (± SD 13) days. Other patients were admitted to medical, surgical or orthopaedic wards.
We have the details of analgesia prescription for 61 patients. Of those, almost all patients received paracetamol (95.7%) and more than third had NSAIDs (36%). More patient had oral morphine prescribed (90%) than dihydrocodeine (70.5%) and 15% had IV Morphine. From the RFS 1–6 and 7–10 group 92% of the patients had the recommended analgesia prescribed. However for the most injured patients (RFS score more than 7) it was only 40%. Also only 6 patients had Gabapentin prescribed and only 4 patients had a patient controlled analgesia (PCA). Regional anaesthesia was only performed for one patient and one patient had rib fixation.
Conclusions: This study demonstrates a low PCA and local anaesthetic catheter usage in patients with severe chest injury. Our practice was well below the recommended guidelines published recently. This may be due to lack of appropriate information and local guidance. As a result, we have started introducing a local management pathway for patients admitted with rib fractures. We hope this will increase awareness among physicians to provide a better analgesic strategy to improve patient outcomes.
0421
Neuron specific enolase in the prognostication of patients following out of hospital cardiac arrest
Craig Sell and John Gorst
Morriston Hospital, Swansea, United Kingdom
Abstract
Introduction: Prognostication of functional status and neurological outcome following cardiac arrest can be a difficult diagnostic and communicative challenge, with no single test conclusively determining where life-sustaining therapy is futile or otherwise.
Neuron specific enolase (NSE) is an isoenzyme biomarker released from neural tissue following injury. Assays for this biomarker are being introduced in some centres as an adjunct to prognostication with increasingly elevated levels indicating worse neurological outcomes through higher cerebral performance categories.
Methods:
At Morriston Hospital, Swansea, neuron specific enolase assaying has been introduced to aid the process of prognostication, along with new guidance on the investigation and management of this patient population on the intensive care unit.
Following case series analysis, outcomes for the twelve month period prior to the introduction of NSE testing and in the twelve months since are compared, along with radiological imaging, electroencephalography results, temperature management and clinical signs as part of the audit process to assess the utility of this new modality of investigation.
Final results and data collection are due in September of 2019.
Results: We share our experiences of introducing neuron specific enolase testing at our 28-bed general intensive care unit in a district general hospital. Whilst there are inherent limitations to NSE investigation like any biochemical marker, it must be taken alongside the overall clinical picture. Final data collection pending; we anecdotally believe neuron specific enolase sampling to have been an invaluable addition to the diagnostic process for patients following cardiac arrest and that this will be supported by the data. Where appropriate the benefits of NSE testing can extend beyond simply the diagnostic tool for clinicians, by also providing an aid to communicating the prognosticating process with relatives and guiding expectations.
0422
Incidence of Contrast Induced Nephropathy in a District General Hospital
claudia porteous and helen threlfall
Arrowe Park Hospital, Wirral, United Kingdom
Abstract
Background: Contrast induced nephropathy (CIN) is defined as a 25% increase in creatinine or an increase in creatinine equal to or greater than 0.5 mg/dl, within 72 hours of exposure to contrast where no alternative explanation is plausible.1,2 The postulated pathophysiology is a direct nephrotoxic effect of intravenous contrast agents.3,4 CIN is quoted as having an incidence of between 4–6%,5 and a significant effect on morbidity and mortality.3 However, recently the existence of contrast nephropathy has been disputed.3,4
Methods: We reviewed the medical notes of all adult patients with an acute kidney injury (AKI) stage III alert between November 2018 and June 2019, the patients who underwent a computerised tomography (CT) scan with and without contrast were identified. Serum creatinine (ummol/l) levels were compared pre scan, twenty-four hours after and between two to five days post scan, on all patients irrespective of whether they received contrast or not. We excluded all patients who had dialysis, or a nephrostomy sited within the data collection period.
Results: In the eight months reviewed, 50 patients received a CT scan, 35 without contrast and 15 with. The average baseline creatinine was 251 in those who received contrast and 296 in those who didn’t, at 24 hours post CT scan the average creatinine value was 259 in those who received contrast and 302 in those who had unenhanced scans. The creatinine level at two to five days post scan was 269 in those who didn’t receive contrast, and 208 in those who did. The diagnostic criteria for CIN was met in 3 patients in the contrast arm and seven in the none contrast arm, the calculated relative risk of developing CIN was 1. When the average baseline creatinine was compared with the average creatinine 2–5 days post contrast there was no significant increase in either arm.
Conclusion: This is a small one centre study, which is restricted by limited numbers, in particular in the contrast arm. We noted equal risk of creatinine rises to a level sufficient to diagnoses contrast induced nephropathy, in both cohorts of patients, adding further weight to the discussion that creatinine rises may not be causally related to contrast administration.5 The data also highlights that there is ongoing hesitancy to perform contrast enhanced scans in patients with acutely impaired renal function. In 6 unenhanced scans, it was noted that the diagnostic capability was restricted by the absence of contrast. Therefore, we may be potentially inappropriately limiting quality of radiographic diagnostic investigations and the treatment based upon it.
0423
Does the provision of High Flow Nasal Oxygen outside of Critical Care prevent or inappropriately delay Critical Care admission?
claudia porteous and tom williams
Arrowe Park Hospital, Wirral, United Kingdom
Abstract
Background: High flow nasal oxygen (HFN02) is a novel treatment for acute hypoxic respiratory failure.1 It is less invasive than intubation or none invasive ventilation1,2. It has less side effects1,3and can be safely used outside of critical care.4 Critical care admission can cause a significant negative effects for patients, and is associated with significant health care cost. It has been postulated that high flow nasal oxygen (HFN02) can prevent intubation1and therefore critical care admission, but there has been some concern that HFN02 may inappropriately delay admission to critical care2, and therefore worsen patient outcomes.5
Methods: This is a retrospective cohort analysis of six months (January 2019 – July 2019) of HFN02 use outside critical care, on a cohort of adult patients who were deemed appropriate for escalation, by the critical care team. HFN02 could be started on any wards outside critical care, provision of care was provided by Critical Care Outreach Nurses. We collected data on the number of critical care admission, the average time from the incitation of HFN02 and critical care admission, intubation rates, the peak fraction of inspired oxygen (Fi02) given and twenty eight day mortality.
Results: 106 patients received HFN02 outside of critical care between January 2019 and July 2019, of these 34 were deemed appropriate for escalation of care. 20 patients were admitted, of those, 3 were ventilated. The mean time between incitation of HFN02 and admission was 0.85 days. The 28-day mortality for the whole cohort was 20.83%, for those who were admitted it was 25%, all those who weren’t admitted survived to discharge. The 28 day mortality for patients, was further broken down into number of days between administration of HFN02 and admission to ITU; two days between these events resulted in a 28 day mortality of 33%(n = 3), one day had a mortality of 18% (n = 11) and those admitted on the same day 16% (n = 6). Of those not admitted (n = 14) twelve received HFN02 with a Fi02 of greater than 60% for one day or longer.
Conclusion: We postulate that the 12 patients, who received HFN02 with a Fi02 of equal to or greater than 0.6 for duration exceeding 24 hours, would have been admitted to intensive care had in not have been for the provision of HFN02 in the ward setting. Therefore, this service results in the prevention of two critical care admissions a month. Of those who required critical care admission, our results suggest that on average they are admitted on the same day as HFN02 is started, however there was a correlation with 28-day mortality and increasing duration of time to admission. This is a small single centre study, with limited numbers, which restricts the strength of our findings. However, the data collected does indicate that HFN02 can potentially prevent critical care admissions, and simultaneously not inappropriately delay treatment.
0424
A service evaluation assessing the impact of the implementation of the All Wales Devastating Brain Injury Guidelines in Morriston Hospital
Luke Newey1,2, Ceri Battle1,2, Ioan Humphreys2 and Jaynie Rance2
1Swansea Bay University Health Board, Swansea, United Kingdom
2Swansea University, Swansea, United Kingdom
Abstract
Introduction: The definition for those with brain injuries deemed so severe at the time of admission, intervention limitations or Withdrawal of Life Sustaining Treatment (WLST) is being considered, has recently been defined as a Devastating Brain Injury (DBI)1–3. Lack of guidance on the management of this patient cohort, it was feared, could lead to a self-fulfilling prophecy following WLST.2 Following the clarification in definition, guidelines published by the Faculty of Intensive Care Medicine (FICM) and in Wales the Welsh Intensive Care Society (WICS) sought to rectify this.
Background/Objectives: Following the publication by the Neurocritical Care Society in the United States4, the UK developed their own DBI guidance documents1, with a devolved Welsh version published by WICS.3 These guidelines aimed to increase prognostic accuracy and allow opportunity for more people to survive such severe brain injuries. The guidelines also identified the need for audit but this was never carried out. This study aimed to begin to analyse the implications of the commencement of DBI guidelines use in Morriston Hospital, Swansea.
Methods: Due to the retrospective nature of the data collection, creation of objective criteria was needed to be able to find and identify DBI patients. Following this initial identification, refinement strategies involving both electronic and paper records were implemented to refine the results. Cohorts identified, retrospectively, for a six-month period before and after the implementation of the guidelines into clinical practice were collected for statistical analyses. The study identified the patients at the point of admission and tracked their admission mapping key timeline points within the guidelines. Along with this data, guideline recommendation compliance was recorded through tracking the patient admission pathway and referrals, noting the patient’s final destination for care and their length of stay.
Results: 5091 patients were identified in Accident and Emergency (A&E) as being admitted with neurological pathology warranting Computer Tomography (CT) Scan of the head. Following the comparison of these patients to the inclusion and exclusion criteria, refinement strategies and cross-referencing of the paper and electronic records were utilised to identify 39 patients as having DBI’s. 20 patients were found in the pre-implementation data and 19 in the post implementation periods. Statistical analysis indicates no difference in survival rates, with all 39 patients dying during their time of admission (p = 1.00). Using Chi-square analysis the admission destination pre and post implementation was found to be statistically insignificant. Final patient destinations were spread across four main areas; A&E, the Acute Medical Assessment Unit, Intensive Care and the stroke ward. Rates of referral to the local Intensive Care and nearest Neurosurgical centre were found to happen no more frequently.
Conclusion: The initial findings of this study would support that the implementation of the guidelines at Morriston Hospital has not increased the rate of survival. Patient destination for care varied in both cohorts and referrals to Intensive Care did not increase, as the guidelines would advocate1,3. Overall, the implementation of the guidelines seems to have had very little effect in Morriston Hospital.
0425
A Review of the use of High Flow Nasal Oxygen, in patients not appropriate for critical care admission
claudia porteous and tom williams
Arrowe Park Hospital, Wirral, United Kingdom
Abstract
Background: High Flow Nasal Oxygen (HFN02) is a novel treatment for acute hypoxic respiratory failure.1 Its use in critical care, in the pre and post-operative period have been well reviewed.1 Its clinical use is expanding past this evidence base into a cohort of patients, who require high fraction of inspired oxygen (Fi02) but who are not suitable for more invasive ventilation strategies.2,3 HFN02 in this cohort of patients has a variety of potential positive effects ranging from increased symptom control,2,3 improving patient tolerance of high Fi02 (as a result of humidification), and better oxygenation; secondary to a combination of factors including providing positive end expiratory pressure, and a decrease in physiological dead space.3,4
Methods: This is a retrospective cohort analysis of six months (January 2019 – July 2019) of HFN02 use outside critical care, on patients who were deemed not appropriate for escalation of care to level two or three. HFN02 was started on any wards outside critical care, provision of care was provided by Critical Care Outreach Nurses. Data was collected on the peak Fi02 given, duration of HFN02 treatment, length of hospital stay and twenty-eight-day mortality. If patients who were receiving HFN02 were palliated we also recorded if HFN02 was stopped prior to death.
Results: In a six-month period from January 2019 to July 2019, 106 patients received HFN02 outside of critical care, 34 were deemed appropriate for critical care, 6 had no documentation of the appropriateness of escalation, and 66 were not suitable for critical care admission. The average age of the patients not suitable for critical care admission was 74, they typically spent 4 days on HFN02 with an average peak fraction of inspired oxygen of 80%. The average length of hospital stay was 21 days and the twenty-eight-day mortality was 60%. The most common underlying pathology was pneumonia, accounting for 68% of all patients, other pathology included aspiration pneumonitis, pulmonary fibrosis, pulmonary hypertension, rib fractures and lung cancer. Of the patients palliated on HFN02, this was stopped prior to death in 50% of cases.
Conclusion: There is expansion of HFN02 outside critical care, this is an area in which this treatment has a limited evidence base,4 this review of clinical practice in a district general hospital demonstrates several areas worthy of further exploration. It can be reasonable presumed that in frail patients, an acute illness which required Fi02 of 80% for 4 days, could be expected to have a higher mortality than 50%,5 therefore potentially this is a lifesaving alternative oxygenation technique which is suitable for a larger proportion of patients. Evidently this hypothesis would be more appropriately tested via a prospective randomised control trial. It is also of note that once started, HFN02 can be a difficult therapy to be withdrawn and potentially could be prolonging quantity and not quality of life in palliative patients.
0426
Late tracheostomy – should we bother? A single centre retrospective study of outcomes in patients receiving tracheostomy after 14 days
Peter Outlaw, Alicia Waite and Norman Main
Critical Care Department, Royal Liverpool University Hospital, Liverpool, United Kingdom
Abstract
Introduction: Tracheostomy is routinely performed in critically ill patients requiring prolonged mechanical ventilation to improve patient comfort and facilitate weaning.
Optimal timing of tracheostomy is contentious. The TracMan study, comparing early (4 days) versus late (>10 days) tracheostomy, did not show any mortality or morbidity benefits.1 A meta-analysis on timing of tracheostomy concluded that timing did not significantly alter clinical outcomes in critically ill patients.2
The Royal Liverpool University Hospital is a tertiary referral centre for pancreatic and vascular patients and the complexity of these conditions often leads to prolonged critical care admissions, in addition to long-stay general medical and surgical patients. Practice within our unit is variable and timing of tracheostomy is based on patient factors, clinician experience and clinical judgement.
Objectives:
1. Identify the percentage of patients ventilated for more than 14 days receiving a tracheostomy.
2. Investigate whether there is a mortality difference between patients with or without a tracheostomy when ventilated for more than 14 days.
3. Investigate whether tracheostomy after 14 days of ventilation has an impact on length of stay.
Methods: We retrospectively reviewed electronic records of adult patients admitted to critical care between April 2018 – March 2019 and ventilated for >14 days. Patients transferred from another hospital with a tracheostomy were excluded.
Results: 32 patients underwent ventilation for more than 14 days. Of these, 44% (14) underwent tracheostomy. Median time for tracheostomy following laryngeal intubation was 19 days (15–28). Median length of critical care stay was 32 days (23-115) and in-hospital mortality in the tracheostomy group was 21% (3 patients).
56% (18 patients) did not undergo a tracheostomy. Median length of critical care stay in this non-tracheostomy group was 22 days (9–33) and in hospital mortality was 44% (8 patients).
Conclusions: Our study shows that 56% of patients who were ventilated for more than 14 days did not receive a tracheostomy. There was increased in-hospital mortality and shorter length of stay in patients who did not receive a tracheostomy.
Our findings are limited by the small sample size, single centre involvement and retrospective nature of our study. Further investigation of tracheostomy in patients receiving prolonged ventilation in a larger patient cohort is warranted.
0428
An unusual aetiology for acute pancreatitis
Claire Froneman, Mohamed Kamara and Rahul Sarkar
Medway Maritime NHS Trust, Gillingham, United Kingdom
Abstract
Background: Severe acute pancreatitis has a high morbidity and mortality with documented mortality rates of 10%.1 Overall the condition accounts for 56 cases per 100 000 people per year.2 The aetiological factors vary but it is generally accepted that gall stones and alcohol excess account for up to 70% of cases.3
Following this, metabolic causes are common in younger patient populations. Hypercalcaemia is one such rare cause accounting for between 1.5–7.0% of cases.4 It is important to identify this early on in the patient’s admission, as recovery may be delayed or potentially unlikely, without correction of the hypercalcemia. The underlying causes for hypercalcaemia could range from hyper-parathyroidism to malignancy.
To demonstrate this, we report a case of hypercalcaemia induced pancreatitis in a young patient of unknown cause.
Case Presentation: A 22- year old Caucasian male with a background of type 1 diabetes mellitus was admitted to the acute medical take with abdominal pain and a three-day history of vomiting. The patient had been managed on an insulin pump for approximately 10 years and reported only occasional alcohol intake. Upon admission the patient exhibited normal observations. A leucocytosis was noted (WCC 19.7 × 109 l) on initial blood testing. The initial arterial blood gas additionally showed a raised lactate (4.6 mmol/l) but remained well compensated. Further blood investigations found a raised amylase level of 530 IU/L. A CT abdomen and pelvis was performed which showed acute interstitial pancreatitis but no evidence of gall stones. The patient denied any history of trauma. Calcium on admission was noted to be significantly raised (4.84 mmol/l) with normal renal function (creatinine 108 µmol/l, urea 8.0 mmol/l).
The patient was initiated on intra-venous crystalloids, insulin infusion and bisphosphonates. Other supportive measures were instituted. By day three the calcium level showed only marginal improvement (4.49 mmol/l) and thus calcitonin was given with good effect. The patient stabilised initially but subsequently developed a severe metabolic alkalosis, renal impairment and type 2 respiratory failure. This was thought to be due to fluid overload and hypoventilation related to diaphragmatic splinting.
The causes for the hypercalcaemia were investigated including blood investigations, autoimmune screen and full body imaging. Parathyroidism, hyper-triglyceridaemia, sarcoidosis, malignancy, viral causes, phaechromocytoma and carcinoid syndrome were excluded. Hypercalcaemia was considered the main aetiological factor with documented mechanisms including calcium deposition and trypsinogen activation within the pancreas.3
The patient was subsequently discharged home following a total of a 30-day admission. Upon review one-week later blood tests showed a stable adjusted calcium level. No clear cause for the hypercalcaemia was elucidated and the patient remains under investigation.
Conclusion: The above case highlights hypercalcemia to have caused severe pancreatitis in a young adult. Although rare, this is well described in the literature and clinicians should be mindful of this as a potential aetiology in relevant patient groups. The rare incidence in this specific subgroup allows for the potential of a missed/ delayed diagnosis with potential catastrophic consequences.
0429
The Changing Face of Critical Care in a District General Hospital 2011–2019
Thomas Noteman1 and Martyn Hawkins2
1Forth Valley Royal Hospital, Larbert, United Kingdom
2Forth Valley Royal Hosptial, Larbert, United Kingdom
Abstract
Background: Forth Valley Royal Hospital (FVRH) is an 860-bed district general hospital in Larbert, Scotland. Since opening in July 2011, FVRH has operated a 19-bed combined HDU/ITU. We had the impression that the number of patients being discharged home directly from the unit was increasing and that this was changing the demands on the clinical and administrative staff in our unit. We have therefore collected data to investigate the changes in characteristics and outcomes of the unit patient population over this 8 year period in order to drive change in our organisational processes.
Methods: Monthly reports for 2011–2019 were generated from a locally held database of all critical care admissions since the hospital's opening. We analysed specifically the number of discharges home from our unit, as well as a number of standard metrics such as unit bed days at level 2 and level 3 care, APACHE II admission score, and length of stay. Linear regression trends generated and analysed for significance using prism 8 statistical software.
Results: Our data show that the number of patients being discharged home directly from our unit has increased approximately 2 fold over 8 years. Patient acuity on admission and while in the unit has decreased significantly as measured by APACHE II on admission and ratio of level 2: level 3 bed days while in the unit.
Conclusions: The reasons for these changes in patient characteristics and outcomes in our HDU/ICU are likely multifactorial and cannot be easily disentangled. Earlier recognition and escalation of acute illness, increasing use of level 2 care in patients not fit for multi-organ support and bed pressures preventing ICU discharge to the wards may all be playing a part. The observational data which we have collected will allow us to drive change within our unit to facilitate multi-disciplinary discharge planning, staff training and adequate follow up.
0430
Getting the Basic’s Right – introduction of a daily review reminder for trainee’s
Emma Jackson and Enya Magill
Blackpool Victoria Hospital Critical Care, Blackpool, United Kingdom
Abstract
Introduction: Critical Care is a complex field with multiple facets to provide the best care for our patients. It can be overwhelming for new doctors to the field and doctors who don’t routinely practice in Critical Care for example those providing on-call cover. We know that if get the basics right we improve outcomes for our patients, but all too frequently these basic care bundles are forgotten or simply not known about. We wanted to look at whether we were providing the optimum daily review for all our patients and if not how we could improve compliance with getting the basics right.
Methods: We wanted to assess whether there was a need to improve the daily review of basic care provision for our patients and look at ways to improve this.
We carried out a spot audit of the daytime daily review, looking at all grades of medical professional. We compared whether there was documentation of review of 22 basic parameters which we felt were essential in the basic management of Critical Care patients. We also looked at whether the daily review met the basic standards set of basic medical record keeping.
Results: We audited 31 daily reviews over a week long period. Reviews were present from all grades of trainees and consultants. Areas that performed well with a greater than 50% documentation included; airway assessment, ventilation settings, use of vasopressors, fluid balance review, feeding plan, bowels open, review of blood tests and review of recent microbiology and appropriate antibiotics. Areas that were frequently missed (frequency less than 50%) included; review of sedation and RASS targets, the patient’s delirium status, blood sugar control, status of venous access, whether the family has been updated, consideration of resuscitation status/ escalation plans for the patient and stress ulcer prophylaxis.
When looking at medical record keeping there was good compliance with time and date 94% and 100% respectively. The location of the review was only documented in 68% of reviews. GMC number was only documented in 29% of reviews and the grade of medical professional performing the review in 84% of reviews.
Conclusions: Following on from our audit we have introduced a double-sided card which attaches to the back of every Intensive Care Trainee’s badge. (Figure 1) On one side it has the emergency intubation checklist. On the other side it has the 22 basic criteria that we felt were essential in providing good basic care for our Critical Care patients to ensure optimal recovery. The current results have been disseminated to all the Critical Care doctors and staff, as well as displayed on our electronic update system on our Critical Care. We plan to re-audit the daily reviews in 1 months’ time following from the introduction of the checklist to see if the checklist has improved our basic standard of care.
Figure 1.
0431
An unusual presentation of mycotic aneurysms secondary to infective endocarditis; A case report
Radia Choudhury and Neil Crooks
Intensive care unit, Good Hope Hospital, Birmingham, United Kingdom
Abstract
Infective endocarditis (IE) is a disease with significant morbidity and has a mortality rate of 20% at 30 days.1 Presentation is frequently non-specific, and a high index of suspicion is required in those with risk factors such as intravenous drug abuse, implanted intracardiac devices and prosthetic cardiac valves.1 It is an uncommon pathology with an estimated incidence of 3–10 per 100,000. Neurological complications are a relatively common occurrence in 25% of cases, however mycotic aneurysms are very rare, occurring in only 2–4% of IE patients.2
We report the case of a 53-year-old gentleman referred to hospital by his GP with a short history of non-specific symptoms including lethargy, confusion and persistent vomiting. The presenting feature of confusion was in fact expressive dysphasia. Routine blood tests on admission were unremarkable and initial clinical examination revealed only a systolic murmur on auscultation. The patient was afebrile and haemodynamically stable with normal inflammatory markers. On the evening of admission, he went into status epilepticus, necessitating intubation and transfer to ICU. A computed tomography (CT) head revealed an irregular cortical lesion in the left parietal lobe, with similar findings in the right frontal lobe and left Sylian cortex felt to be suspicious of cerebral metastases.
A month prior to admission he had been referred for endoscopy and a CT abdomen and pelvis to investigate weight loss. A diagnosis of achalasia and oesophageal candidiasis was made. Although no primary malignancy was identified, the symptoms and CT head findings prompted referral to a neuro-oncology cancer of unknown primary multidisciplinary team meeting. A magnetic resonance imaging (MRI) scan of the brain was carried out demonstrating areas of haemorrhage. Although these features were atypical, it was felt radiologically to represent metastatic disease.
A transthoracic echocardiogram, performed in ICU to investigate his systolic murmur, revealed a large vegetation on the mitral valve with prolapse of the posterior leaflet. In light of this, blood cultures were taken which grew Streptococcus salivarius, a rarely isolated group of Streptococcus viridians in patients with IE4 and a commensal of the oropharyngeal and gastrointestinal tract associated with opportunistic endocarditis infections.5 On further review of the imaging a working diagnosis of mycotic aneurysms secondary to IE was made and antibiotics were started immediately.
After two days, the patient was successfully extubated and transferred to cardiology. However shortly after transfer, another seizure ensued, necessitating intubation and ventilation. A CT head at this time revealed new acute bilateral subdural haemorrhage. The patient returned to ICU but unfortunately passed away. No intervention was performed as the neurosurgical team deemed this to be an un-survivable haemorrhage, not amenable to surgery.
This is an unfortunate case of a gentleman who had an unusual presentation of IE. His risk factors included diabetes mellitus and high alcohol intake.5 There was no suspicion of infection in his presentation and no peripheral stigmata of IE; history and investigations were all initially felt to be related to brain metastases.
0432
Impact of experiences of delirium on patients admitted to intensive care – a national survey
Ahmed Gilani1, Randeep Mullhi2, Daman Mullhi3, Oliver Jones3, Larry Matthews3, Fang Gao-Smith4 and Tonny Veenith5
1Queen Elizabeth Hospital, University Hospitals Birmingham UHB NHS, Birmingham, United Kingdom
2University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
3The UK Sepsis Trust, Birmingham, United Kingdom
4University of Birmingham, Birmingham, United Kingdom
5Department of Anaesthesia & ICM, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Delirium is a reversible state of impaired cognition, inattention and altered level of consciousness.1 It has been associated with increased length of stay in intensive care, increased use of healthcare resources, and poorer functional recovery.1 Societies such as the National Institute for Health and Care Excellence recognise the prevention of delirium as a public health priority.2–3 There is a scarcity of evidence of the experiences of delirium from a patient’s outlook, and its long-term impact from a physical and neurocognitive perspective. We present the largest known qualitative data set as collated from a national survey.
Objectives: This survey was part of a tripartite national survey to assess the impact of experiences of delirium in hospital by patients, carers, and medical professionals. It aimed to give credence to the paucity of evidence demonstrating the detrimental impact and experiences of delirium on patients and carers, and their quality of life after hospital discharge. This survey aimed to assess the physical and neurocognitive impact of delirium on patients after discharge.
Methods: This study was considered a simple anonymous patient survey after discharge from hospital – ethics approval was sought and not required; the project was electronically registered with the University Hospitals Birmingham Clinical Audit department. We conducted a nation-wide self-administered patient survey sent to patients identified via the UK Sepsis Trust. The survey was conducted securely electronically using internet-based software, and assessed patient’s experiences in two parts: experiences of delirium recalled by the patient, and experiences of their management of delirium while in hospital.
Results: From the 488 respondents, 62% were admitted to intensive care – the majority owing to sepsis. Of the respondents, 53% recalled undergoing painful procedures, 70% experienced hallucinations, and 90% remembered being confused and agitated. Descriptions of hallucinations included ‘seeing the devil writing on the wall’ and ‘I thought I was in a warehouse for bodies’, with many other descriptions of being incarcerated, deprived of liberty, experimentation, and the deceased talking. During these experiences, 64% felt their hallucinations were real and were unable to differentiate them from reality. Many cited a disturbance in their sleep/awake cycle and noise levels to have contributed to their delirium episode. Post-discharge, neurocognitive effects of depression and hopelessness appear to linger, with 85% seeking help for neuropsychiatric symptoms post-discharge. Examples of post-traumatic stress disorder included ‘I was in a coma for three weeks and was locked in terrible nightmares which will never leave me’.
Conclusion: Delirium presents a substantive impairment in neurocognition and reduction in quality of life post-discharge from hospital as evident from patient experiences. Emphasis on neurocognitive follow-up care was suggested by patients who experienced delirium in intensive care, including pleas to reduce noise levels, maintenance of awake/sleep routinisation, and communication on the impact of delirium prior to discharge with offers of support. From a patient’s perspective – ‘I was in intensive care for four months, rehab for three months. I still remember the confusion and the illusions even now. The mental side of things far outweighed the physical for me’.
0433
A curious case of coma in a peritoneal dialysis patient in an Intensive care unit
faryal Zaman and vikram anumakonda
Russell Hall Hospital, Dudley, United Kingdom
Abstract
Background: Peritoneal dialysis is not a common modality of renal replacement in UK these days. Renal physicians consider switching renal replacement therapy from peritoneal dialysis alone to haemodialysis or combined therapy of Peritoneal dialysis and Haemodialysis in cases with severe decline in residual renal function.1 However, this switch is sometimes avoided, as continuing assisted Peritoneal dialysis is more suitable than switching to Haemodialysis or combined therapy with respect to their physical tolerance levels and lifestyles.2 The differential diagnosis of encephalopathy in peritoneal dialysis patients can be challenging and primarily includes uremic encephalopathy, dialysis disequilibrium syndrome, dialysis dementia, cerebrovascular accident, central nervous system infection, and intoxication.3 Herein we describe the case of a patient treated with Peritoneal dialysis alone despite his an-uric status who subsequently developed coma.
Presentation: A 47 years old gentleman with history of chronic renal failure secondary to diabetes on home peritoneal dialysis, awaiting pancreatic and renal transplant, presented with worsening headache, irritability, vomiting, confusion and low GCS. His bilateral pupils were reactive & plantars were up going. Due to his low GCS, he was Intubated and ventilated. His investigations including CT &MRI Head, Liver Function Tests, Ammonia, Cerebro spinal fluid Analysis, auto immune profile for cerebral angitis, paraneoplastic screen, autoimmune encephalitis screen and peritoneal fluid analysis were all unremarkable. EEG finding consistent with metabolic and uraemic encephalopathy. He had no seizures, no fever. Off the sedatives, he tolerated endotracheal tube, but developed twitches and myoclonic jerks, with bilateral up going plantars and hyper reflexia. A repeat Lumbar Puncture and repeat MRI was performed on the advice of neurologist, which were unremarkable again. He was treated with a 5 day methyl-prednisolone regime with no benefit. During all these days of ICU stay, he underwent regular peritoneal dialysis.
In view of no significant neurological improvement, rescue haemodialysis sessions were commenced to assess any reversible pathology. After 24 hours of Haemodialysis, he started responding, understanding and following commands, moving his limbs and his GCS improved remarkably. He was extubated, transferred to renal unit and is on permanent haemodialysis; awaiting Transplant.
Discussion and conclusion: Encephalopathy can occur as a result of multiple disorders associated with acute or chronic renal failure and is characterised by acute or subacute onset of reversible neurological symptoms.4 Current guidelines for peritoneal dialysis adequacy are based on kinetics of small water-soluble molecules and do not consider the role of other compounds such as middle molecules and protein-bound solutes. Information on the elimination characteristics of the latter solutes by peritoneal dialysis is limited. During peritoneal dialysis p-cresol behaves like b2m, probably due to its protein binding. The total clearance of both molecules is significantly lower as compared to water soluble solutes and mainly depends on residual renal function. Further studies suggest that protein-bound solutes are involved in the pathophysiology of uraemic symptoms and neurological impairment.5
We recommend that, the cohort of patients on peritoneal dialysis presenting with unexplained encephalopathy must be offered a trial of haemodialysis if the clinical picture and investigations were strongly suggestive of uraemic encephalopathy.
0434
Delirium management by medical professionals in intensive care – a national survey
Ahmed Gilani1, Randeep Mullhi2, Fang Gao-Smith3 and Tonny Veenith1
1Department of Anaesthesia & ICM, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
2University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
3University of Birmingham, Birmingham, United Kingdom
Abstract
Introduction: Delirium is a reversible state of impaired cognition, inattention and altered level of consciousness.1 It has been associated with increased length of stay in intensive care, increased use of healthcare resources, and poorer functional recovery.1 Societies such as the National Institute for Health and Care Excellence recognise the prevention of delirium as a public health priority.2–3Anectodally, it is recognised that the management of delirium varies in different intensive care settings nationally.
Objectives: This survey was part of a tripartite national survey to assess the impact of experiences of delirium in hospital by patients, carers, and medical professionals. We surveyed medical professionals in intensive care to assess their experiences of managing delirium, and the variation in practice.
Methods: This study was a simple anonymous survey sent to medical professionals who work in intensive care; ethics approval was sought and not required. The project was electronically registered with the University Hospitals Birmingham Clinical Audit department. We conducted the nation-wide self-administered survey sent to medical professionals who work in intensive care electronically using internet-based software. The survey assessed the treatment and management strategies in various intensive care units.
Results: Of the 438 respondents, the majority were consultants (31%) or intensive care nurses (37%). Baseline demographics of their intensive care settings were sought, with 83% practicing in England. 90% agreed delirium was distressing to patient’s carers and relatives, with 88% feeling delirium added additional workload in their units. 44% stated their unit conducted a formal screening method for delirium on every patient daily. The most common tool employed was the CAM-ICU (Confusion Assessment method for the ICU) method. Only 25% of respondents had a protocol for the pharmacological treatment/prophylaxis of delirium; the commonest first choice for pharmacological prophylaxis of delirium was anti-psychotics (50%) with only 3 respondents using antiepileptics. Further data relating to their first-, second-, and third-line choices to treat hyperactive and hypoactive delirium was obtained, along with their strategies to wean treatment.
Conclusion: There is a great amount of variation in practice in the prophylaxis and treatment of delirium; of note, there is less emphasis on the use of non-pharmacological methods compared to pharmacological intervention. This heterogenous variation may represent clinical experience and familiarly with agents and assessments, superimposed by the dearth of positive research results. We believe the survey gives credence for the need of research currently ongoing to help tackle what is a huge burden on intensive care resources. Of note is the interest in using antiepileptic agents as prophylaxis in certain susceptible patient groups.
0435
Morphine induced respiratory depression in an adult sickle cell disease patient
Job Gogo Otokwala1,2
1Dr., Port Harcourt, Nigeria
2UNIVERSITY OF PORTHARCOURT, PORTHARCOURT, Nigeria
Abstract
Background: Sickle cell disease (SCD) is a common genetic abnormality in Nigeria and one of the commonest complications associated with it is the vaso-occlusive crisis which results in both acute and chronic painful states. Pain relief is an integral part of the management.
The opioids such as morphine, hydromorphone, and the non-steroidal anti-inflammatory analgesics are routine analgesics for their ease of access, global availability and cost. For such chronic painful states, one of the concerns about the use of opioids is the risk for drug dependence and addiction. Morphine has increased plasma clearance rate from increase in hepatic blood flow, renal blood flow and glomerular filtration rate in some adult sickle cell disease patients. The risk of morphine toxicity increases in the presence of renal impairment. This was observed in this patient who was a known SCD patient with diabetes mellitus and acute kidney injury and had been on both hydromorphone and morphine and suddenly developed severe respiratory depression.
Case presentation: A 40year old lady, on social visit from a high income economy known SCD, diabetes mellitus and obesity was referred for haemodialysis on account of sudden loss of consciousness, reduced urine output, difficulty with words, and left sided body weakness. Ancillary investigations:CT mid brain infarct only, HB 8.2 g%, WBC (43 × 103/l), HbA1c 6.6%, urinalysis showing red blood cells of 298 mg/dl. Creatinine 6.35 µmol/l, urea 122.35 mg/dl, Sodium 133 mmol/l, potassium 4.3 mmol/l, chloride 105 mmol/l, total protein 6.4 g/dl, serum albumin 2.8 g/dl. Alanine transaminase 308.6/l, aspartate transaminase 575iu/l, alkaline phosphatase 7 iu/l. total bilirubin 1.23 mg/dl. Conjugated bilirubin 0.60 mg/dl.
The past medical history. Multiple blood transfusions and haemodialysis.
Drug history: Sc clexane 40 mg daily, sc regular insulin, sc lantus insulin 33iu nocte, IV metoclopramide 10 mg OD, tablets omeprazole 40mg BD, dicyclomine 20 mg 6hourly, folic acid 5 mg daily hydromorphone 8 mg 8hourly, losartan 25 mg daily, magnesium oxide 400 mg daily, morphine sulphate ER 100 mg (a tablet) 8hourly, trazodone 100mg nocte, vitamin B12 100 mcg daily, aspirin 325 mg daily.
Clinical examination at the intensive care unit showed an obsese lady, with a GCS: eye opening 3, verbal response 2, motor response 4, 9/15, pupils pin pointed, pale, icteric. BP 80/40 mmHg, PR 104/min, RR 6cycles/min. In view of the drug history and the renal impairment, morphine toxicity was suspected. Intravenous naloxone at 400 micrograms diluted and administered as an infusion was given and the respiratory rate improved spontaneously and the patient became fully conscious to give her history. The blood pressure was supported with dopamine and with five sessions of haemodialysis, the patient was discharged home after 4 days.
Conclusion: Adult sickle cell disease patients may have renal impairment which could affect drug clearance. Regular assessment of renal function and adaptation of drug use is strongly advised.
0436
Initial Experiences of Designing a Psychological Counselling Service in Critical Care
Victoria Heather Jones, Anita Bowman, Paul Hayden and Rahul Sarkar
Medway NHS Foundation Trust, Gillingham, Kent, United Kingdom
Abstract
Background: The psychological burden for patients,1 family members2 and among staff3 is well described in critical care. NICE guidelines advocate a locally available psychological counselling service in intensive care units (ICU).4 Community-based counselling services are associated with significant waiting time and there could be suboptimal understanding of critical care specific issues by the community provider.
Objective: A hospital-based critical care counselling service was set up for patients, families and multi-disciplinary staff. Here we describe the initial experience in initiating the service and challenges associated with it.
Methods: In recognition that the psychological needs of patients, staff and family members were not being addressed locally, a business case was developed (late 2018) for a psychological counselling service. Target recipient groups for the service were: 1. in-patients with high anxiety burden 2. Discharged patients with Post-Traumatic Stress Disorder (PTSD), depression and anxiety. 3. Family members with psychological stress and strain (identified by nursing staff) 4. Staff members (self-referral).
The service was designed for one day a week initially and was planned to run in parallel to the already established nurse-led ICU post-discharge clinic. Three to six sessions for each patient were planned. An appropriate onward referral pathway to manage acute psychological/psychiatric crisis issues was put in place (for strong suicidal ideation/self-harm etc).
Validated psychological scoring systems [Hospital Anxiety and Depression Scale (HADS), Patient Health Questionnaire (PHQ9), the General Anxiety Disorder (GAD7) and the Trauma Screening Questionnaire (TSQ)] were used to monitor progress of service users.
At this stage, a survey showed that 50% staff agreed/strongly agreed about feeling stressed at work, 39% agreed/strongly agreed that workplace support for stress was suboptimal and 76% were willing to engage with local counselling service.
Emails, flyers and staff team meetings were used to publicise the service. Group sessions were held during nursing training days.
Results: In the post-discharge clinic, 13 patients have been seen in 6 months (average sessions of 5 for each patient). Twelve in-patients were seen (1–2 sessions/patient) during this period. Nine staff members were seen during these 6 months, with 8 staff having had one session each, and the other staff member having 5 sessions.
Mean pre and post counselling score are given below (Table 1). One patient noticed worsening of symptoms due to a life events whilst the counselling was ongoing. It was noted that 4 patients had pre-existing psychological diagnosis.
Challenges faced while designing the service were 1. Finding an appropriate financial metric that could be incorporated within the business case (most powerful metric proved to be potential saving from reduced staff sickness) 2. Finding office space for the counsellor to see patients and staff away from ICU. 3. Commencing a seamless relationship with the local mental health team.
Conclusion: Despite initial challenges, the ICU psychological counselling service has had a successful launch, was welcomed by the recipients. It removed the waiting time to access counselling for the patients, who derived significant objective benefit. A number of staff engaged with this local service.
Table 1.
| Score | Pre-counselling | Post-Counselling |
|---|---|---|
| HADS | 17 | 15 |
| PHQ9 | 15.1 | 5.5 |
| GAD7 | 13.4 | 4.4 |
| TSQ | 6.4 | 3.9 |
0437
Lactate kinetics in patients following elective partial hepatic resection
Joseph Alderman1,2, Andrew Owen1,2, Bobby Dasari3 and Nicholas Murphy2
1College of Medical and Dental Sciences, University of Birmingham, Birmingham, United Kingdom
2Department of Anaesthesia and Critical Care Medicine, Queen Elizabeth Hospital, University Hospitals Birmingham NHS Foundation Trust, Birmingham, United Kingdom
3Department of HPB and liver transplantation, University Hospitals Birmingham NHS Foundation Trust -Queen Elizabeth Hospital Birmingham, Birmingham, United Kingdom
Abstract
Introduction and background: Cancers affecting the liver are an important – and rising – cause of morbidity and mortality in the UK. ‘Liver cancers’ are more accurately thought of as a diverse range of malignancies, either primary or metastatic, and affecting liver parenchyma or biliary tissue. (1) Most liver cancers are metastatic in origin, usually colorectal carcinoma (CRC). The most common primary liver cancer is hepatocellular carcinoma (HCC), which is commonly associated with viral hepatitis, and other causes of cirrhosis. Whilst overall cancer rates are projected to fall across the UK, incidence of HCC is predicted to rise significantly in the coming decades. (2) Treatment often involves surgery, the extent of which depends on cancer spread within the liver, and may be subcategorised according to regions of liver excised. Hepatic resection has low postoperative mortality, though many patients will require stabilisation postoperatively on the Intensive Care Unit. Early complications include haemorrhage, infection, acute liver failure, and persistent hyperlactataemia.
Though not fully understood, extensive evidence from the sepsis literature (3), and growing evidence in trauma (4) suggest hyperlactataemia, when present, is a poor prognostic factor. Some evidence exists that this may also apply following liver resection. (5)
University Hospitals Birmingham NHS Foundation Trust hosts one of the largest hepatobiliary services in the UK. We present herein an analysis of the lactate kinetics following hepatic resection in 1275 patients.
Methods: A database was collated of all patients who underwent hepatic resection between 2015 and 2019. Up to 50 blood lactate readings were obtained for each patient from hospital electronic records, and analysed. Descriptive statistics were performed using SPSS v20. Sequential lactate data were combined into a scatterplot of lactate against time for subsequent kinetic analysis.
Results: A total of 1275 patients were included (58.4% male). CRC accounted for 57.0% of tumours, cholangiocarcinoma 10.4% and HCC 9.8%. The mean number of lactate readings following a procedure was 18 (0-50) with a mean lactate value of 2.3 mmol. L−1 (0–19.2). Statistical modelling was undertaken to describe usual lactate kinetics following partial hepatectomy in this case series.
Conclusion: This study is the first to our knowledge to quantify lactate levels following liver resection. Whilst mean levels are relatively low, peak values seen may allow prognostication. Further work to determine if these can be used to predict the need for critical care admission is required. An additional follow up prospective study is planned to assess the validity of the kinetic model formulated from these retrospective data.
0438
Post-Operative Anaemia in General Surgical Patients
Gillian Best and John Strange
Belfast City Hospital, Belfast, United Kingdom
Abstract
Introduction: Pre-operative anaemia has well established negative outcomes, including increased length of hospital stay, post-operative complications and mortality.1 However there has been less research into the impact and duration of post-operative anaemia, despite occurring in up to 90% of patients after major surgery.2
Objectives: To identify the incidence and duration of post-operative anaemia in general surgical patients admitted to critical care post-operatively, the response to oral iron supplementation and the duration of anaemia following hospital discharge.
Methodology: We undertook a retrospective audit of all patients admitted to critical care following a general surgical procedure over a period of 3 months. Data collected included patient demographics, pathology, pre-operative haemoglobin, post operative haemoglobin trends and length of critical care and hospital stay.
Results: 54 patients were identified, with a median age of 65. 61% were male. 87% were non emergency cases and 72% were undergoing surgery for gastrointestinal malignancy.
39 patients (72%) were anaemic (Hb < 130 g/L) pre-operatively with 11% having a pre-operative Hb < 100 g/L.
Mean haemoglobin fall post operatively was 31 g/L, on average occurring at day 6.
40 patients (74%) had a lowest post operative haemoglobin less than 100 g/L. This corresponded to a longer ICU stay (3.3d vs 2d) and a longer hospital stay (21.3d vs 10.2d).
53 patients survived to hospital discharge. Only 8% of patients had a discharge haemoglobin > 130 g/L and 70% a discharge haemoglobin > 100 g/L.
45 patients were discharged from hospital with a haemoglobin less than their pre-operative haemoglobin.
On discharge 57% of patients received no additional iron supplementation, 28% received low dose oral iron and 15% received high dose oral iron.
There was no improvement in recovery time to pre-operative haemoglobin in the cohorts receiving oral iron at 15, 30 or 60 days post operatively, compared to those who did not receive oral iron.
For those patients with a lowest post operative haemoglobin > 100 g/L, recovery to the pre- operative haemoglobin concentration occurred on average at day 30. However patients with a lowest post operative haemoglobin < 100 g/L, recovery of haemoglobin concentration occurred at day 44.
Conclusions: There is a high incidence of anaemia in general surgical patients admitted to critical care post-operatively which persists post hospital discharge and is not responsive to oral iron supplementation. The presence of a lowest post operative haemoglobin less than 100 g/L potentially represents a group at higher risk of prolonged anaemia, who could be a target for intravenous iron replacement.
0439
A rare case of a mal-positioned central line catheter
Prashant Kumar
Queen Elizabeth University Hospital, Glasgow, United Kingdom
Abstract
Background: Mal-positioning of central line catheters (CVC) is an uncommon but potentially serious event. Most commonly, the tips of misplaced CVCs are positioned in veins that are distal to the site of insertion, with reports of CVC tips looping back to lie within the same vein as insertion being relatively rare. Due to the more indirect anatomical course from the insertion vessel towards the right atrium, such occurrences usually involve either the left internal jugular vein (IJV), left subclavian or right subclavian vessels. However, as reported on this occasion, there are rare cases in which central venous cannulation has resulted in a CVC tip looping back to lie within the right IJV.
Case Presentation: A 61-year-old patient was admitted to hospital after developing a community-acquired pneumonia. Unfortunately, despite treatment with intravenous antibiotics, she deteriorated clinically, developing type one respiratory failure. She was subsequently transferred to the intensive care unit where she was intubated and ventilated. A quad-lumen CVC was placed under ultrasound guidance into the right IJV, using a seldinger technique. However resistance was felt upon attempting to thread the guidewire. The guidewire was therefore retracted and re-threaded, with no further resistance noted. Guidewire placement within the vein was confirmed with repeat ultrasound imaging. The remainder of the procedure was performed as normal, with a nick to the skin, dilation of the tract and threading of the CVC over the guidewire. Upon aspiration of the lumens however, one middle lumen appeared blocked with an inability to aspirate blood, although flushing normal saline was still possible and achieved without resistance. The remaining three lumens were free to aspirate and flush. Interestingly the follow-up chest x-ray demonstrated a fish-hook appearance of the CVC, in which the catheter had looped back on itself, with the tip facing cephalad within the IJV. It became apparent that the resistance to guidewire placement had most likely occurred at the junction between the IJV and the subclavain vein. When the guidewire was re-threaded it is likely to have double-backed on itself, with the CVC subsequently being fed over the guidewire. In hindsight, it is likely that on repeat ultrasound imaging of the guidewire, there would have been two separate hyperechoic points within the lumen of the vein, but that in real-time assessment this phenomenon was missed by the operator. The CVC was subsequently removed with a new CVC inserted into the left IJV without complication.
Conclusions: CVC malposition is a known complication of the procedure. However, with only five reported cases to date, it is highly unusual to find a CVC tip coiled back to sit within the right IJV, when that same vessel has been used as the site of insertion.1-5 This case highlights that CVC insertion remains a risky procedure and that the operator must remain vigilant. It re-affirms the importance of intra- and post-procedure imaging, either with ultrasound or X-ray, to prevent potentially serious complications prior to use of the CVC, such as venous thrombosis, perforation and catheter dysfunction.
0440
Outcome of surgical admissions at the intensive care unit of the University of Portharcourt Teaching Hospital Nigeria
Job Gogo Otokwala
University of Port-Harcourt, Port-Harcourt, Nigeria
Abstract
Background: The university of Port-Harcourt teaching hospital is a tertiary referral hospital in the southern part of Nigeria and it sub serves a population of about five million people with an acute bed capacity of eight hundred beds. The intensive care unit is open and admits both medical and surgical patients. General surgery and the various sub sets of surgery such as orthopaedics, Neuro Surgery, Paediatric Surgery, EMT, OMF, Plastic Surgery and the OBGYM. admit and co manage critically ill pre-operative cases for optimization and post-operative cases for stabilization.
Objective: The objective of this study was to look at the outcome of the patients admitted from the various surgical sub-specialties, the indications for admission and interventions that were implemented.
Method: It was a prospective study involving all surgical patients (EXCLUDING MATERNITY) that were admitted in the ICU between August 2018 to August 2019, ethical clearance was obtained from the university’s ethical committee. Details; The patient’s demographics, indications for ICU admission, Interventions in the ICU, and possible outcomes were obtained from the ICU case notes, of the patients. Exclusion criteria were maternity cases. Data, Result, statistical analysis used were obtained through SPSS version 20.
Result: Total Number of patients admitted in the ICU during the study period = 150, Total number of surgical Patients = 89 (59.3%), Mean Duration of stay = 5 days ± 2.7
mean age = 44 ± 3.0
sex (female) = 36 (40.1%)
sex (male) = 53 (59.9%)
General surgical patients involving abdominal procedures contributed 60% of the mortalities, while Neuro Surgical procedures contributed 20%, Gynae-oncology 15% and Thoracic Surgery 5%.
Conclusion: At the University of Port-Harcourt Teaching Hospital Intensive Care Unit General Surgical cases involving the abdomen and Neuro Surgical cases contributed more to mortality, extreme care should be focused on these surgical specialties.
.
Unit Statistics
| Surgical Unit | Number Admitted |
|---|---|
| General Surgery | 35 |
| Urology | 2 |
| Orthopaedics | 7 |
| Paediatrics | 3 |
| Neuro Surgery | 8 |
| Thoracic Surgery | 10 |
| EMT | 6 |
| OMF | 5 |
| Gynae-oncology | 11 |
| Plastic Surgery | 2 |
.
Outcome
| Good outcome | 64 patients = 61% |
| Mortality | 25 patients = 39% |
0442
Decontamination of a “live” intensive care unit
Ifor Capel, Greg Manning, Leanne Franklin, Sally Scott and Prad Shanmuga
Buckinghamshire Healthcare NHS Trust, Aylesbury, United Kingdom
Abstract
Introduction: The intensive care unit (ICU) environment plays a major role in acquisition of nosocomial infections. Significant interest exists in the use of no-touch technologies for decontamination. Hydrogen peroxide vapour decontamination (‘fogging’) is superior to wiping at reducing frequency of positive cultures from high-touch surfaces1 and reduces acquisition of multi-drug resistant organisms in ICU.2 Automated mobile devices that emit ultraviolet light C (UV-C) are effective against both vegetative bacteria and spores.3 These techniques cannot be used on open units due to risk of harm to patients and staff. Previous ICU reports2,4 moved patients to alternate sites within the hospital prior to decontamination. Due to infrastructural limitations, this was not possible in our hospital.
Objectives: To use fogging and UV-C to decontaminate an active ICU, without reducing capacity, or moving level 3 patients to an alternate facility.
Methods: Stoke Mandeville hospital has a 12 bed ICU, comprising 5 isolation rooms and 7 open-plan beds. On the 1st September, area 1 was isolated for approximately 6 hours and decontaminated. Over 7th-9th Sept, four level 2 patients were moved to a 4-bed day surgery recovery unit, leaving the ICU with 6 ventilated patients. Equipment not in use was moved into area 2, which was then isolated and decontaminated overnight on the 7th Sept (Image 1). After decontamination and equipment clearance, ventilated patients were moved into areas 1 and 2 and the process continued sequentially (Figure 1).
Results: The process was completed over two weekends with no delayed admissions to the ICU or loss of patient bed-days. The only adverse incident during the process was accidental activation of the fire alarm system by the fogging process.
Conclusions: Our experiences demonstrate that it is possible, without closing beds or losing bed-days, to successfully clean an open-plan intensive care unit, through a carefully planned approach of selective partitioning and phased decontamination.
0447
A review of massive /Sub-massive pulmonary embolism admitted to ICU
Alarmeluvalli sivaramakrishnan1 and Vikram Anumakonda1,2
1Russell Hall Hospital, Dudley, United Kingdom
2University of Birmingham, Birmingham, United Kingdom
Abstract
Objectives: A retrospective analysis of a case series of patients presenting with massive/SmPE admitted to an ICU over a period of 6 years needing cardiorespiratory support in a DGHsetting. EPR, echocardiogram, CT imaging and biomarkers were reviewed in addition to other demographics.
Methods: A retrospective analysis was undertaken of data collected prospectively of all the massive/Sm PE needing critical care support. Data was retrieved using SQL data bases from ICU EPR records. Two clinicians independently reviewed CT imaging and ECHO finding retrospectively. In addition, lab parameters and biomarkers were collected. PE presenting as in or out of hospital cardiac arrest were excluded.
Results: 14 patients were admitted with a primary diagnosis of PE to ICU. Out of this, 4 patients were discharged following ICU stay and 10 were deceased. In the survivor group, there were 1 male and 3 females. In the deceased group, there were 5 males and 5 females. The mean age in the discharged cohort was 60.5 years versus 70.3 years in the deceased group. Mean length of stay was 5 days in the discharged vs 3.9 days in the deceased group. One out of four patients had massive PE in the discharged group versus 7 out of 10 in the deceased group. 75% had consolidation on CT amongst survivors vs 60% in the non-survivors. One patient was thrombolysed in the survivor group and 6 patients in the deceased group.
2 out of 4 patients were ventilated in the survivor group with mean ventilation period of 3 days. 9 out of 10 patients were ventilated in the non-survivor group with mean ventilation period of 3 days.
The mean white cell count and CRP were 14.5 and 94.4 in the survivor group compared to 17 and 108 in the deceased group. The mean procalcitonin level was 15.07 in the survivor group versus 21.5 in the group of deceased patients. 7 out of 10 patients had evidence of right ventricular strain in the deceased group compared with 1 out of 4 amongst survivors. 3 out of 4 required vasopressors in the survivor group whereas all the 10 patients required vasopressor support in the deceased group.
Conclusions: Elderly adults with large clot load admitted to ICU are less likely to survive. Patients needing mechanical ventilation or thrombolysis have less survival. A significant proportion of patients have lung parenchymal changes in both survivors and non survivors on CT imaging. Procalcitonin levels are raised in both groups suggesting possible co-existent infection and the incidence of right ventricular strain is more common in the non-survivor group. Vasopressor requirement was more in the deceased group. Therefore, we conclude that age, clot load, need for thrombolysis and the need for mechanical ventilation are factors that predict survival in patients admitted to ICU with PE.