Abstract
BACKGROUND
Total joint arthroplasty is one of the most common surgeries performed in the United States with total knee arthroplasty (TKA) being one of the most successful surgeries for restoring function and diminishing pain. Even with the demonstrated success of TKA and a higher prevalence of arthritis and arthritis related disability among minorities, racial and gender disparity remains a constant issue in providing care for the adult reconstruction patient.
AIM
To assess the role of demographics and expectations on differences in perioperative patient reported outcomes (PRO) following TKA.
METHODS
One hundred and thirty-three patients scheduled for primary unilateral TKA secondary to moderate to severe osteoarthritis were enrolled in this two-institution prospective study. Validated PRO questionnaires were collected at four time points. Statistical analysis was conducted to determine the impact of gender, ethnic background and expectation surveys responses to assess PRO at these time points.
RESULTS
Females were associated with worse preoperative Knee Injury and Osteoarthritis Outcome Scores (KOOS) for symptoms, pain, and activities of daily living. African Americans were associated with worse KOOS for pain, activities of daily living, and quality of life. Despite worse preoperative scores, no difference was noted in these categories between the groups postoperatively. Additionally, all pre-operative psychometric scales were equivalent across groups except Geriatric Depression scale, which was significantly different between groups within the Race and Age Group (P < 0.05). Conversely, Pain Catastrophizing Scale, was significantly different for all subscales and total score within Age Group (P < 0.05), and the Magnification, Helplessness subscales as well as the Total score were significantly different between groups for Race and Relationship Status (P < 0.01).
CONCLUSION
We conclude that female and African American patients have lower preoperative KOOS scores compared to white male patients. No postoperative differences in outcomes between these groups.
Keywords: Knee, Joints, Arthroplasty, Osteoarthritis, Race, Gender, Postoperative, Outcomes
Core tip: Total knee arthroplasties (TKA) are one of the most common surgeries performed in the United States. Even with its popularity, it has been shown that African Americans and women are offered this surgery less than their white male counterparts. We explore the role of potential factors connected to the underutilization of TKA in minorities and women as well as assess patient expectations and outcomes associated with race and gender. We conclude that there are no differences in outcomes between race and gender which leads us to believe that TKA should be offered to everyone equally to remedy disparities.
INTRODUCTION
Total joint arthroplasty is one of the most common surgeries performed in the United States for patients who are suffering from end stage osteoarthritis. By the year 2050 it is estimated that 60 million Americans will carry the diagnosis of osteoarthritis[1]. The good news is that total joint arthroplasty is also amongst the most successful of surgeries, with total knee arthroplasty (TKA) having a 90% success rate for restoring function and diminishing pain[2]. It has been shown that pre-operative education is associated with improved clinical outcomes in joint replacement surgery as it increases patient understanding of the process, which in turn empowers patients and subsequently alleviates the anxieties surrounding total joint arthroplasty (TJA)[3].
However, even with the demonstrated success of TKA at improving quality of life for patients, pre-operative education offered, and a higher prevalence of arthritis and arthritis related disability among minorities, racial disparity is still a concern. In many cases black patients experience worse postoperative results following the procedure and there is decreased utilization observed in black patients[2]. In an extended report by Singh et al[4], in 2008 the use of primary TKA for African Americans was a concerning 39.7% lower than Caucasians. Regardless of race, the United States population is aging which makes the elderly in all ethnic and demographic groups susceptible to osteoarthritis with 1 in every 115 Americans over the age of 65 having already had a joint replacement surgery[5]. Similarly, women present for TKA with more advanced diseases prior to TKA compared to their male counterparts and are also more likely to develop osteoarthritis (OA). However, even with it being more prevalent, there is an underuse of TKA amongst women. According to the Arthritis Foundation, women aged 45 and older experience OA at 7.2%-18.7% whereas males experience this at 5.9%-13.5%.
The purpose of this study was to determine and explore potential factors connected to differences in utilization and outcomes of TKA associated with race and gender and to determine the role of patient expectations.
MATERIALS AND METHODS
Data source and study population
One hundred and thirty-three patients undergoing primary TKA were enrolled into this multi-institutional prospective study conducted from 2013 through 2015. Both institutions combined perform roughly around 3600 primary joint arthroplasties per year. Patients were eligible if they were between 18 to 79 years old, had a primary diagnosis of osteoarthritis of the knee, and could read and write in English for purposes of collecting the most accurate information. We excluded patients who have had prior history of TKA, lower extremity amputation, or fracture. Demographic characteristics, such as age, gender, marital status, race, and ethnicity, were collected. There were 69 (51.9%) black patients, 55 (41.4%) white patients, 3 (2.3%) Hispanics, 2 (1.5%) Asian patients, and 4 (3%) patients of unknown race. One hundred and four patients in our study were women, 58 were black and 40 white. There were 29 males, 15 of those were white and 11 black. The average age of our participants was 61.6. All participants consented to participate in the study.
Outcome measures
Patients in the study were asked to complete questionnaires either via email, telephone, or at their pre- and post-operative office visits. The questionnaires were completed at different study points. Study point 1: Prior to their operation; Study point 2: 4-8 wk; Study point 3: 9 to 14 mo post-operatively. The validated patient reported outcome measure (PROM) questionnaires included the following.
Study point 1: (1) HSS patient expectation questionnaire; (2) Social support survey; (3) Pain catastrophizing survey; (4) Visual analogue pain scale; (5) Geriatric depression scale; (6) Knee Injury and Osteoarthritis Outcome Scores (KOOS) (Knee)- routinely collected as part of standard care at this time; and (7) E-5D- routinely collected as part of standard of care at this time.
Study point 2: (1) HSS patient expectation questionnaire; (2) Visual analogue pain scale; (3) KOOS (Knee)- routinely collected as part of standard care at this time; and (4) E-5D- routinely collected as part of standard of care at this time.
Study point 3: (1) Visual analogue pain scale; (2) KOOS (Knee)- routinely collected as part of standard care at this time; and (3) E-5D- routinely collected as part of standard of care at this time.
Statistical analysis
The Kolmogorov–Smirnov test (K–S test or KS test) was used to examine the data for confirmation to the normal distribution. Hypothesis testing was completed using nonparametric methods. Demographic variables were evaluated for distribution equity using the one-sample binomial or the one-sample χ2 test. Pre-operative psychosocial scales were evaluated for between subject effects using MANOVA. The Wilcoxon signed ranks test was used to compare the pre- vs post-operative expectations. Post-operative outcomes were evaluated over three time points (Pre-op, Post-op 4-8 wk, and Post-op 9-14 mo) with the Friedman’s two-way analysis of variance by ranks. Standard descriptive techniques were used to summarize continuous variables as appropriate. The maximum number of participants used in the analysis was n = 133. The continuous variable, age, was recoded into a categorical variable, “age group” for certain analyses. Imputation methods for missing data were not used.
RESULTS
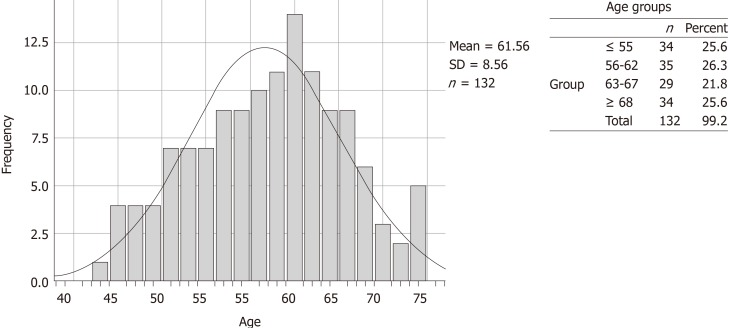
The K-S test revealed that the data did not follow a normal distribution (P < 0.01). The demographic breakdown of the overall initial cohort is shown in both Table 1 and in Figure 1. Seventy-eight percent of the patients that were analyzed were females. In other categories with multiple options, we observed bi-modal choices dominating over all other selections. Within Relationship status, Married or Single comprised 80.4% of the cohort. African Americans (51.9%) and Whites (41.4%) comprised 93.3% of the Racial Demographics reported. Our participants reported their insurance type as private 58.6% of the time and as Medicare 38.3%, accounting for 96.9% of respondents. Figure 1 shows the full age distribution and summary statistics of the cohort (mean age 61.56 years ± 8.56 years) as well as how these were recoded into the revised categorical variable Age Group.
Table 1.
Summary of initial cohort demographics
| n | Percent | ||
| Gender1 | Male | 29 | 21.8 |
| Female | 104 | 78.2 | |
| Total (n) | 133 | 100 | |
| Relationship status1 | Married | 54 | 40.6 |
| Single | 53 | 39.8 | |
| Divorced | 10 | 7.5 | |
| Significant other | 1 | 0.8 | |
| Widowed | 13 | 9.8 | |
| Partner | 1 | 0.8 | |
| Total (n) | 132 | 99.2 | |
| Race1 | African American | 69 | 51.9 |
| Asian | 2 | 1.5 | |
| Hispanic | 3 | 2.3 | |
| White | 55 | 41.4 | |
| Unknown/Other | 4 | 3 | |
| Total (n) | 133 | 100 | |
| Insurance type1 | Private | 78 | 58.6 |
| Medicare | 51 | 38.3 | |
| Workman's comp | 3 | 2.3 | |
| Total (n) | 132 | 99.2 | |
The null hypothesis, that the categories occur with equal probabilities, is rejected using the One-Sample Chi-square test, P < 0.01.
Figure 1.
Age distribution and grouping for enrollment cohort.
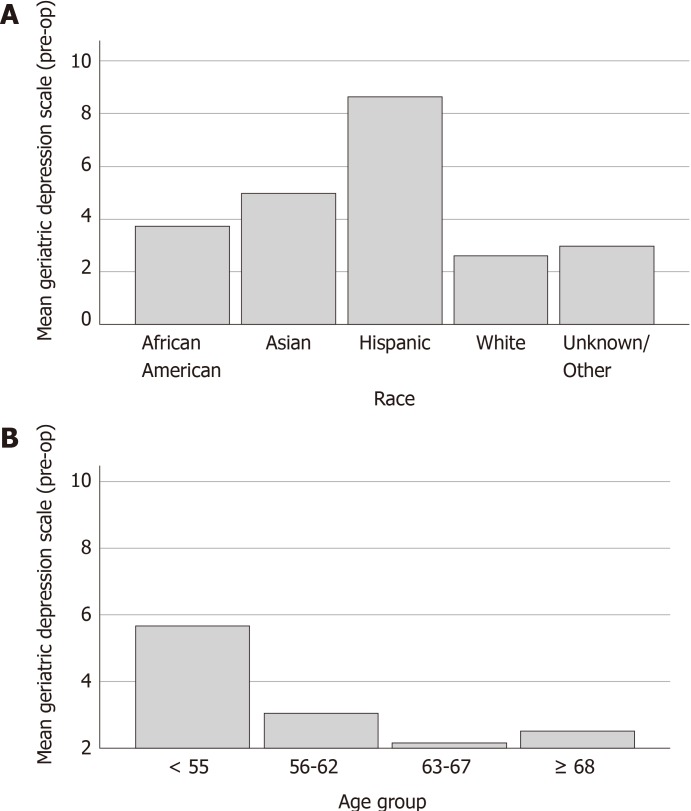
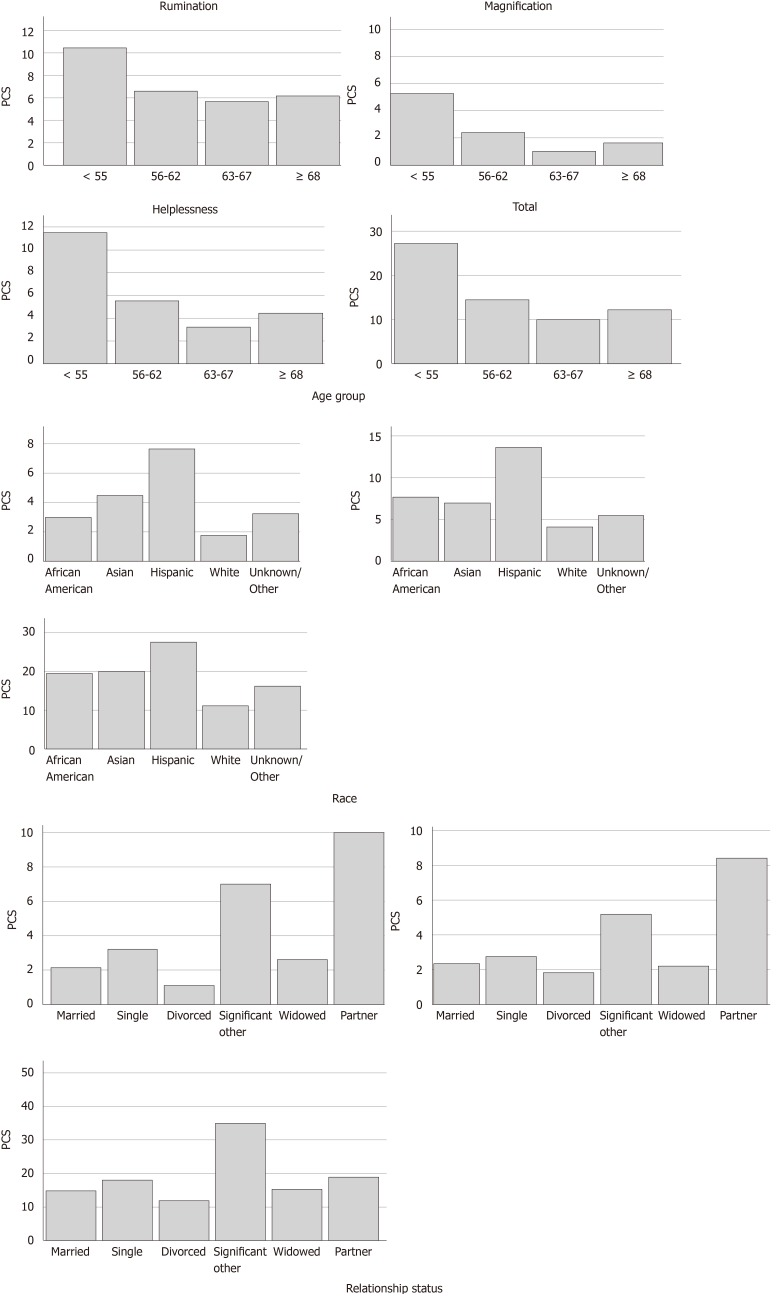
The pre-operative psychometric scales and pain catastrophizing scale are summarized in Table 2 along with the number of friends and the pre-operative and post-operative (4-8 wk) expectations scores. There was no difference observed across any demographic category for number of friends (P = NS). All pre-operative psychometric scales were equivalent across groups (P = NS) except for geriatric depression, which was significantly different between groups within the race and age group (P < 0.05). The detailed differences within each category are shown graphically in Figure 2. The pain catastrophizing scale, was significantly different for all subscales and total score within age group (P < 0.05), and the magnification, helplessness subscales as well as the total score were significantly different between groups for race and relationship status (P < 0.01). These differences are expanded graphically in Figure 3. The only observed gender-based differences in these measures were for post-op expectations, with mean score for females (65.5 ± 31.5) significantly lower than males (84.5 ± 21.5, P < 0.05).
Table 2.
Summary statistics of pre-operative assessments and expectations
|
n |
Mean | Median | Mode | SD | Minimum | Maximum | |||
| Valid | Missing | ||||||||
| Number of friends | 133 | 0 | 7.47 | 5 | 10 | 7.7 | 0 | 50 | |
| Pre-Op Psychometric Scales | Emotional/ Informational support score | 133 | 0 | 85.34 | 96.9 | 100 | 20.9 | 3 | 100 |
| Tangible support score | 133 | 0 | 82.02 | 94 | 100 | 24.2 | 0 | 100 | |
| Affectionate support score | 133 | 0 | 88.84 | 100 | 100 | 19.3 | 0 | 100 | |
| Overall medical outcomes support index | 133 | 0 | 85.28 | 90.8 | 100 | 18.7 | 1 | 100 | |
| Geriatric depression scale1 | 133 | 0 | 3.39 | 3 | 2 | 3 | 0 | 13 | |
| Positive social support | 133 | 0 | 86.28 | 100 | 100 | 22.5 | 0 | 100 | |
| Pre-Op Pain Catastrophizing Scale | Rumination2 | 133 | 0 | 7.28 | 7 | 16 | 5.1 | 0 | 16 |
| Magnification3 | 133 | 0 | 2.63 | 2 | 0 | 3.2 | 0 | 12 | |
| Helpnessness3 | 133 | 0 | 6.29 | 4 | 0a | 6.1 | 0 | 24 | |
| Total3 | 126 | 7 | 16.2 | 13 | 6a | 12.9 | 0 | 52 | |
| Expectations | Pre-op | 69 | 64 | 81.98 | 89.5 | 97 | 17.7 | 23 | 100 |
| Post-op (4-8 wk)4 | 70.97 | 86.8 | 100 | 29.8 | 3 | 100 | |||
Using General Linear Modeling (GLM) Multivariate Analysis (MANOVA), differences between groups was observed for Race and Age Group, P < 0.05;
Using GLM and MANOVA, differences between groups was observed within Age Group, P < 0.05;
Using GLM and MANOVA, differences between groups were observed for Age Group (P < 0.05), Race (P << 0.01), and Relationship Status (P << 0.01);
Using GLM and MANOVA, differences between groups was observed for Gender (P <0.05).
Multiple modes exist. The smallest value is shown.
Figure 2.
Geriatric depression score. A: Race; B: Age group.
Figure 3.
Graphic distributions of pain catastrophizing scores where significant differences were found within categories (P < 0.05).
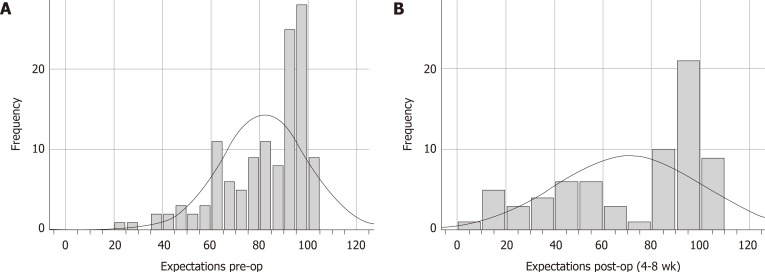
The overall differences in pre- vs post-operative expectations is shown as a histogram in Figure 4. The mean pre-op score was 81.98 ± 17.74. The pre-op range was 23.08-100.00 (n = 126). The mean post-op score was 70.97 ± 29.82. The post-op range was 2.56 -100.00 (n = 69). The difference between pre- vs post-op expectations is significant, P < 0.01, using the Wilcoxon signed rank test.
Figure 4.
Histograms of pre- vs post-operative expectations.
The overall differences in pre- vs post-operative expectations is shown as a histogram in Figure 4. The mean pre-op score was 81.98 ± 17.74. The pre-op range was 23.08-100.00 (n = 126). The mean post-op score was 70.97 ± 29.82. The post-op range was 2.56-100.00 (n = 69). The difference between pre- vs post-op expectations is significant, P < 0.01, using the Wilcoxon signed rank test.
Outcome measures were collected for 4 time points, pre-operative (Baseline, T1), post-operative follow up 1 (4-8 wk, T2), post-operative follow up 2 (9-14 mo, T3) and post-operative follow up 3 (20-26 mo, T4). The n for each sampling period varied somewhat for each instrument for unknown reasons (T1, n ≈ 130.25; T2, n ≈ 104; T3, n ≈ 54.25; and T4, n ≈ 9). The T4 time point was removed from the analysis. There was an overall loss to follow up of 58% for the study between T1 and T3.
Table 3 shows the summary of all the outcome measures taken for the cohort. VAS, KOOS-Pain, KOOS-ADL, and KOOS-QOL- improved significantly overall and significantly at each interval. EQ5D did not improved significantly between T1 and T2 but did improve significantly between T2 and T3 and overall from T1 to T3. Both EQ5D-VAS and KOOS-Sport showed significant overall improvements from T1 to T3 but the interval improvements were not significant. KOOS-Symptom improved significantly between T1 and T2 and for the overall period T1- T3 but did not change significantly between T2 and T3.
Table 3.
Outcome measures for 3 time points pre-op (T1), post-operative (4-8 wk) (T2), and post-operative (9-14 mo) (T3)
| n | Mean | SD | Mean rank |
P |
|||||
| T2 vs T11 | T3 vs T11 | T3 vs T21 | Overall2 | ||||||
| VAS | T1 | 133 | 7.64 | 1.99 | 2.71 | 0 | 0 | 0.02 | 0.05 |
| T2 | 103 | 4.81 | 2.61 | 1.93 | |||||
| T3 | 52 | 4.02 | 3.44 | 1.36 | |||||
| EQ5D | T1 | 129 | 0.59 | 0.193 | 1.59 | 0.38 | 0 | 0.02 | 0.05 |
| T2 | 103 | 0.67 | 0.204 | 1.91 | |||||
| T3 | 54 | 0.74 | 0.229 | 2.5 | |||||
| EQ5D-VAS | T1 | 131 | 69.31 | 20.435 | 1.71 | 0.66 | 0.01 | 0.2 | 0.05 |
| T2 | 105 | 75.52 | 17.04 | 1.96 | |||||
| T3 | 54 | 76 | 17.1 | 2.33 | |||||
| KOOS-pain | T1 | 130 | 37.3 | 18.53 | 1.3 | 0.01 | 0 | 0 | 0.05 |
| T2 | 104 | 56 | 19.51 | 1.91 | |||||
| T3 | 54 | 70.87 | 25.38 | 2.79 | |||||
| KOOS-symptom | T1 | 130 | 40.64 | 15.71 | 1.27 | 0 | 0 | 0.07 | 0.05 |
| T2 | 105 | 55.19 | 14.59 | 2.14 | |||||
| T3 | 56 | 61.54 | 18.22 | 2.59 | |||||
| KOOS-ADL | T1 | 129 | 42.22 | 20.97 | 1.32 | 0 | 0 | 0.01 | 0.05 |
| T2 | 105 | 64.42 | 21.29 | 2.04 | |||||
| T3 | 54 | 70.7 | 26.31 | 2.64 | |||||
| KOOS-sport | T1 | 130 | 38.61 | 37.9 | 1.51 | 0.05 | 0 | 0.05 | 0.05 |
| T2 | 103 | 55.16 | 41.11 | 2 | |||||
| T3 | 55 | 62.29 | 37.32 | 2.49 | |||||
| KOOS-QOL | T1 | 130 | 17.17 | 18.99 | 1.34 | 0 | 0 | 0.01 | 0.05 |
| T2 | 104 | 34.31 | 19.95 | 2.02 | |||||
| T3 | 55 | 47.29 | 30.93 | 2.64 | |||||
Each row tests the null hypothesis that the sample 1 and sample 2 distributions are the same. Asymptotic significances (2-sided tests) are displayed. The significance level is 0.05. Significance values have been adjusted by the Bonferroni correction for multiple tests;
Related samples, Friedman’s two-way analysis of variance by Ranks.
Evaluation of all demographic variables, psychometric scales, pain catastrophizing scale, and expectations vs outcomes in this cohort revealed that despite the demonstrated variations from multiple sources within the cohort, all subjects who were evaluated through to the 9–14 mo post-operative period did not show disparate outcomes (data not shown). Further, there was no higher likelihood of dropout based on any of the preoperative characteristics evaluated.
The statics methods of this study were reviewed by Dr. Annamarie Horan, Director of Clinical Research, University of Pennsylvania, Department of Orthopaedic Surgery.
DISCUSSION
This study explored the role that gender and race play on patient expectations and preoperative and postoperative patient reported outcome scores following TKA. Previous studies have identified and explored TKA utilization disparities associated with race and gender exploring both patient and provider factors. Our study focuses on patient expectations pre- and post-surgery and characteristics such as, social support, pain catastrophizing, and depression in their lives that may have played a role in these results and may offer additional understanding into race and gender disparities associated with TKA. Lower expectations could lead to lower utilization and decreased desire for patients to pursue TKA. Lower expectations may lead to poorer outcomes and satisfaction by way of a self-fulfilling prophesy, on the other hand, lower expectations may lead to better outcomes and improved satisfaction as a consequence of the results being far better than anticipated. However, in our study we found no difference in outcomes when related to pre- and post-operative expectations. Even though TKA is highly successful and cost effective there is a lower and/or later utilization when it comes to blacks, Latinos, lower income individuals, and women.
Social support
Undergoing surgery or choosing to undergo surgery may cause many patients added stress due to the lack of control and predictability patients have during this time[6]. Studies have looked into the potential role that social support plays in patients both pre and post-operatively which may have a significant effect on patient expectations and outcomes. In a 2005 study, Khrohne et al investigated the influence of social support on indicators of perioperative adaptation, specifically the perceived accessibility to emotional and informational support. They reported that women with low support had significantly more anxiety compared to men. In addition, there was a significant difference in length of stay between patients. Patients who scored below the median stayed longer than expected, resulting in a difference of 1.42 d[6]. Vina et al[7] studied the role of social support when dealing with race, gender, and total knee replacements. They surveyed 514 white and 285 African American patients undergoing total knee replacements and found that compared to whites, African American were more likely not married and had overall less emotional support structures and were also less likely to consider the surgery. However, there was not a significant association with social support and willingness to undergo TKR in the African American patients. In our cohort, patients whose relationship status were with a “partner” or “significant other” experienced a significant increase in helplessness and magnification than those patients who were “single” or “divorced” which can lead us to believe that when it comes to social support, relationship status doesn't alleviate certain stressors for patients as expected from similar studies[6,7].
Pain catastrophizing
Expectations and outcomes of surgery are influenced by many different elements of a patient's life. Like social support, pain catastrophizing may play a significant role in the expectations and outcomes patients experience when undergoing TKA. Pain catastrophizing is the act of magnifying the threat value of pain stimulus and to feel helpless in relation to pain and has also been linked to many clinical pain related outcomes including measure of pain severity, pain related activity interference, depression, disability, and an increased behavioral expressions of pain, as well as illness behaviors[8]. Our study analyses pain catastrophizing by looking at magnification and helplessness in patients. When we looked at African American patients in comparison to Caucasian patients, there was a significant increase in both levels of magnification and helplessness, which identifies African Americans as experiencing more pain catastrophizing than Caucasians. While African Americans experienced pain catastrophizing more, Hispanics experienced the highest levels of pain catastrophizing in our study. In addition to pain catastrophizing, African Americans and Hispanics experienced higher levels of depression, which can be a consequence of their relationship to pain.
Many studies have suggested that pre-surgical pain catastrophizing predicts poorer recovery from TKA. In a 2011 study, Fabian et al[9] examined differences in pain responses by ethnicity where 62 participants ages 18 to 25 completed screening questionnaires. Similar to our results, this study showed that African Americans and Asian/Pacific Islanders reported significant greater pain intensity than Caucasians and African Americans also reported significant greater situational catastrophizing in comparison to Caucasians and Asian/Pacific Islander. In a meta-analysis by Meints et al[10], 19 studies were analyzed to compare the differences in pain coping between black and white Americans. This study reported that while black individuals used pain coping strategies like praying, more often than white individuals, they were also pain catastrophizing more often. Similarly, women are found to also pain catastrophize more often when compared to men and have increased pain intensity.
Disparities in TKA
In our study, we tried to find underlying reasons or variables for the disparities we observe within TKA. We narrowed down potential explanations for racial and gender disparities to the following: Societal/socioeconomic factors, clinician and health care provider factors (bias, communication, perception of poorer outcomes), and patient factors (preferences, expectations, health literacy, trust, burden of disease, comorbidities precluding TKA, and bias/communication). Goodman et al[11] conducted a retrospective study of patients undergoing TKA between 2007 and 2011 to assess the association of race and socioeconomic factors when dealing with patient-reported outcomes after a TKA in New York, New Jersey, and Connecticut. In their analysis they confirmed that black patients have worse WOMAC pain and function after TKA when compared to white patients in these states at a 2-year follow up. The difference is found to be heavily associated with the census tract poverty level especially pointing out that black patients living in impoverished communities resulted in WOMAC pain and function scores 7 to 8 points lower than black patients living in wealthier communities[11]. Our study found that female sex was associated with worse preoperative KOOS for symptoms, pain, and activities of daily living, which may be a result of women presenting later with symptoms. Women also experience worse outcome after TKA due to pre-operative factors such as negative mental health state, and poorer preoperative pain due to late presentation[12].
In addition to socioeconomic factors, provider and patient factors are a significant contributor to disparities observed in TKA. Provider factors may include items like unconscious bias where physicians unconsciously allow certain patient characteristics to dictate their methods of treatments. Lopez et al[13] surveyed 596 male patients with OA of the knee or hip to determine their perception of access to care and referral to specialists in order to observe possible differences in patients who are referred to an orthopedic or rheumatology specialist. While the differences were not significant they did note that white patients were referred to specialists more often than their black counterparts at 24.2% vs 17.4% respectively[13]. In a study by Dy et al[14] they evaluated the effect of possible surgeon bias when dealing with recommendations for TKA. They used four computerized scenarios with combinations of black or white patients and male or female patients with end stage knee OA. All patients in the study had similar history and surgeons were asked if they would recommend TKA. The study concluded that patient race and sex were not associated with surgical recommendation percentages. While significant differences were not observed in these studies, there may be a significant contrast at different stages of the patient-physician interaction[13]. In a 2008 study[15] of 71 physicians (38 family physicians and 33 orthopaedic surgeons), it was noted that 67% of physicians recommended TKA for male patients and only 33% recommended the female patients. A study by Schulman et al[16], reported that patients race and sex contributed significantly to the physicians decision to refer patients with chest pain for a cardiac catheterization, with black females being the least to obtain a referral.
Disparities in medicine may also be enhanced by patient factors. Many studies have observed that differences in health literacy/communication, preference/willingness, and expectations are significant issues and contributors of racial/gender disparities in medicine. Health literacy is essential for patients to comprehend completely the information they are receiving. In America, limited health literacy affects about 90 million people and prevents these patients from receiving adequate care. It is often the case that many patients and their caregivers both lack the level of skills needed to understand information related to medications, wound care, self-monitoring, follow up schedules, and prevention behaviors[17]. In a recent study by Menendez et al[18], patients with limited health literacy were found to ask fewer questions in their visits before surgery. Non-white patients were also found to ask fewer questions than white patients, which may suggest a significant association between limited health literacy, and non-white patients. Communication, like health literacy is also a critical factor in patient’s decision to undergo TKA. In a population-based study by Hawker et al[19], of patients presenting with moderate to severe knee OA only 33% of women reported speaking about arthroplasty with their physician and 19% ever speaking with an actual orthopaedic surgeon. Alternatively, 42% men reported discussing with their physician and 26% with an orthopaedic surgeon. The lack of communication between patient and physician may add to the under usage of TKA in women as well as their presenting at later, more advanced stages of OA.
Patient preference/willingness is also a prevalent factor linked to these inequalities. Compared to Caucasians, African Americans rely on methods other than hospital visits or surgery to relieve pain or discomfort associated with arthritis. They preferred to use prayer, natural or folk remedies, or lotions before considering surgery and many believed that their health was in God’s control[1]. The unwillingness to opt for surgery may also be caused by an expectation of having surgery related complications. Patients who receive TKA in low volume hospitals by low volume surgeons were found to have had worse functional outcomes 2 years after the procedure and African Americans are more likely to attend low volume/low quality hospitals when compared to Caucasian patients[20,21]. Low quality arthroplasty results can garner mistrust in the surgery as well as in the physicians. To this effect it is noted that black patients are more likely to expect worse outcomes following joint replacement surgery. In a study of 596 elderly male African American or white patients, African American patients were more likely to expect more pain, functional disability following the surgery, and a longer duration of hospital course compared to the white patients[5].
In conclusion, our results indicate that women and black patients undergoing TKA presented with worse preoperative KOOS scores compared with white patients. We also noticed that black and Hispanic patients experience pain catastrophizing and depression more when compared to white patients. However, outcomes were good among all groups postoperatively, and neither race nor gender was associated with compromised post-operative outcomes in relation to pain, ADLs or QOL. These findings may be valuable in counseling patients and surgeons regarding the value of increase utilization of TKA in these patient populations. Further study is necessary to better understand the lower utilization or later presentation observed in these populations.
Limitations
We acknowledge limitations associated with our study that requires the need to analyze the results with that in mind. The limitations included sample size as well as loss to follow up between the preoperative time point and time point 3 (9-14 mo). Furthermore, limitations include a higher bias toward women, a near binary ethnic representation (African Americans and Whites over all others) and we failed to consider the role comorbidities may play in affecting baseline expectations and postoperative outcome scores.
ARTICLE HIGHLIGHTS
Research background
Total joint arthroplasty is one of the most common surgeries performed in the United States with total knee arthroplasty being one of the most successful surgeries for restoring function and diminishing pain. Even with the demonstrated success of total knee arthroplasty and a higher prevalence of arthritis and arthritis related disability among minorities, many studies have shown that pre-operative expectations regarding pain relief after total joint replacement differ by gender and race, affecting post-operative outcomes. Racial and gender disparity remains a constant issue in providing appropriate care for the adult reconstruction patient.
Research motivation
The purpose and motivation behind this non-interventional study is to measure pre-operative patient expectations and correlate them with post-operative expectations, satisfaction and clinical outcomes after total joint replacement as it relates to race and gender. Clinical research examining patient expectations will increase awareness in the orthopaedic community to address the challenge of musculoskeletal health disparities and stimulate future research and focused strategies on how to manage patient’s surgical expectations and improve patient outcomes across racial and ethnic groups.
Research objectives
Our main objective was to determine and explore potential factors connected to differences in utilization and outcomes of total knee arthroplasties (TKA) associated with race and gender, and to determine the role of patient expectations. Our study looked into characteristics such as, social support, pain catastrophizing, and depression in patients’ lives that may have led to these results and may offer additional understanding into race and gender disparities within TKA.
Research methods
One hundred and thirty-three patients undergoing primary TKA were enrolled into this study from 2013 through 2015. Demographic characteristics, such as age, gender, marital status, race, and ethnicity, were collected. Patients in the study were asked to complete questionnaires either via email, telephone, or at their pre- and post-operative office visits. The questionnaires were completed at different study points. Study point 1: prior to their operation, Study point 2: 4 to 8 wk, Study point 3: 9 to 14 mo post-operatively. The validated patient reported outcome measure (PROM) questionnaires included: (1) HSS patient expectation questionnaire; (2) Social support survey; (3) Pain catastrophizing survey; (4) Visual analogue pain scale; (5) Geriatric depression scale; (6) Knee Injury and Osteoarthritis Outcome Scores (KOOS) (Knee)- routinely collected as part of standard care at this time; and (7) E-5D- routinely collected as part of standard of care at this time.
Research results
In our findings, females were associated with worse preoperative KOOS for symptoms, pain, and activities of daily living. African Americans were associated with worse KOOS for pain, activities of daily living, and quality of life. Despite worse preoperative scores, no difference was noted in these categories between the groups postoperatively. Additionally, Pain Catastrophizing Scale, was significantly different for all subscales and total score within Age Group (P < 0.05), and the Magnification, Helplessness subscales as well as the Total score were significantly different between groups for Race and Relationship Status (P < 0.01). Our results indicate that women and black patients undergoing TKA presented with worse preoperative KOOS scores compared with white patients. However, outcomes were good among all groups postoperatively, and neither race nor gender was associated with compromised post-operative outcomes in relation to pain, ADLs or QOL. Due to this, the question still remains, why is TKA underutilized within these groups and what can we do to aid in fixing the disparities.
Research conclusions
Our study concluded that there are multiple variations in pre-operative demographic variables, psychometric scale, pain catastrophizing scale and expectation vs outcomes. We noticed that while female and African American patients have lower preoperative KOOS scores compared to white male patients, their outcomes are not affected. Irrespective of these findings and due to lack of postoperative differences in outcomes between these groups, TKA is a valid option for minorities and should be offered at the same rate as their white counterparts. These findings may be valuable in counseling patients and surgeons regarding the value of increased utilization of TKA for African Americans and women. Further study is necessary to better understand the lower utilization or later presentation observed in these populations.
Research perspectives
It is necessary to continue research on the disparities found in TKA within African American communities and women. While our study explores certain factors like social support, depression, pain catastrophizing, and bias, there is more to be considered before any determinations can be concluded. What we do know, however, regardless of the factors, we as physicians have a responsibility to tackle these disparities in hopes of providing equal and quality care to all races and genders.
Footnotes
Institutional review board statement: The study was reviewed and approved by the NYU School of Medicine’s Institutional Review Board and the University of Pennsylvania’s Institutional Review Board.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: The authors declare that they have no conflict of interest.
CONSORT 2010 statement: The authors have read the CONSORT 2010 Statement, and the manuscript was prepared and revised according to the CONSORT 2010 Statement.
Manuscript source: Invited Manuscript
Peer-review started: January 1, 2020
First decision: February 19, 2020
Article in press: April 8, 2020
Specialty type: Orthopedics
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bolshakova GB S-Editor: Wang YQ L-Editor: A E-Editor: Liu MY
Contributor Information
Brian A Perez, Department of Orthopedics, University of Pennsylvania, Philadelphia, PA 19104, United States.
James Slover, Department of Orthopedic Surgery, New York University Langone Health, New York, NY 10016, United States.
Emmanuel Edusei, Department of Orthopedic Surgery, New York University Langone Health, New York, NY 10016, United States.
Annamarie Horan, Department of Orthopedics, University of Pennsylvania, Philadelphia, PA 19104, United States.
Afshin Anoushiravani, Department of Orthopedic Surgery, New York University Langone Health, New York, NY 10016, United States.
Atul F Kamath, Department of Orthopaedic Surgery, Cleveland Clinic, Cleveland, OH 44195, United States.
Charles L Nelson, Department of Orthopedics, University of Pennsylvania, Philadelphia, PA 19104, United States.
Data sharing statement
No additional data is available.
References
- 1.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Variation in perceptions of treatment and self-care practices in elderly with osteoarthritis: a comparison between African American and white patients. Arthritis Rheum. 2001;45:340–345. doi: 10.1002/1529-0131(200108)45:4<340::AID-ART346>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 2.Goodman SM, Parks ML, McHugh K, Fields K, Smethurst R, Figgie MP, Bass AR. Disparities in Outcomes for African Americans and Whites Undergoing Total Knee Arthroplasty: A Systematic Literature Review. J Rheumatol. 2016;43:765–770. doi: 10.3899/jrheum.150950. [DOI] [PubMed] [Google Scholar]
- 3.O' Reilly M, Mohamed K, Foy D, Sheehan E. Educational impact of joint replacement school for patients undergoing total hip and knee arthroplasty: a prospective cohort study. Int Orthop. 2018;42:2745–2754. doi: 10.1007/s00264-018-4039-z. [DOI] [PubMed] [Google Scholar]
- 4.Singh JA, Lu X, Rosenthal GE, Ibrahim S, Cram P. Racial disparities in knee and hip total joint arthroplasty: an 18-year analysis of national Medicare data. Ann Rheum Dis. 2014;73:2107–2115. doi: 10.1136/annrheumdis-2013-203494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ibrahim SA, Siminoff LA, Burant CJ, Kwoh CK. Differences in expectations of outcome mediate African American/white patient differences in "willingness" to consider joint replacement. Arthritis Rheum. 2002;46:2429–2435. doi: 10.1002/art.10494. [DOI] [PubMed] [Google Scholar]
- 6.Krohne HW, Slangen KE. Influence of social support on adaptation to surgery. Health Psychol. 2005;24:101–105. doi: 10.1037/0278-6133.24.1.101. [DOI] [PubMed] [Google Scholar]
- 7.Vina ER, Cloonan YK, Ibrahim SA, Hannon MJ, Boudreau RM, Kwoh CK. Race, sex, and total knee replacement consideration: role of social support. Arthritis Care Res (Hoboken) 2013;65:1103–1111. doi: 10.1002/acr.21925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing: a critical review. Expert Rev Neurother. 2009;9:745–758. doi: 10.1586/ERN.09.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fabian LA, McGuire L, Goodin BR, Edwards RR. Ethnicity, catastrophizing, and qualities of the pain experience. Pain Med. 2011;12:314–321. doi: 10.1111/j.1526-4637.2010.01015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meints SM, Miller MM, Hirsh AT. Differences in Pain Coping Between Black and White Americans: A Meta-Analysis. J Pain. 2016;17:642–653. doi: 10.1016/j.jpain.2015.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goodman SM, Mandl LA, Parks ML, Zhang M, McHugh KR, Lee YY, Nguyen JT, Russell LA, Bogardus MH, Figgie MP, Bass AR. Disparities in TKA Outcomes: Census Tract Data Show Interactions Between Race and Poverty. Clin Orthop Relat Res. 2016;474:1986–1995. doi: 10.1007/s11999-016-4919-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mehta S, Palaganas M, Perruccio AV, Davis AM. Do women have poorer outcomes following total knee replacement for osteoarthritis? Osteoarthritis Cartilage. 2014;22:S15–S16. doi: 10.1016/j.joca.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Lopez JP, Burant CJ, Siminoff LA, Kwoh CK, Ibrahim SA. Patient perceptions of access to care and referrals to specialists: a comparison of African-American and white older patients with knee and hip osteoarthritis. J Natl Med Assoc. 2005;97:667–673. [PMC free article] [PubMed] [Google Scholar]
- 14.Dy CJ, Lyman S, Boutin-Foster C, Felix K, Kang Y, Parks ML. Do patient race and sex change surgeon recommendations for TKA? Clin Orthop Relat Res. 2015;473:410–417. doi: 10.1007/s11999-014-4003-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Borkhoff CM, Hawker GA, Kreder HJ, Glazier RH, Mahomed NN, Wright JG. The effect of patients' sex on physicians' recommendations for total knee arthroplasty. CMAJ. 2008;178:681–687. doi: 10.1503/cmaj.071168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, Dubé R, Taleghani CK, Burke JE, Williams S, Eisenberg JM, Escarce JJ. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340:618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 17.Hadden KB, Prince LY, Bushmiaer MK, Watson JC, Barnes CL. Health literacy and surgery expectations in total hip and knee arthroplasty patients. Patient Educ Couns. 2018;101:1823–1827. doi: 10.1016/j.pec.2018.05.021. [DOI] [PubMed] [Google Scholar]
- 18.Menendez ME, van Hoorn BT, Mackert M, Donovan EE, Chen NC, Ring D. Patients With Limited Health Literacy Ask Fewer Questions During Office Visits With Hand Surgeons. Clin Orthop Relat Res. 2017;475:1291–1297. doi: 10.1007/s11999-016-5140-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hawker GA, Wright JG, Glazier RH, Coyte PC, Harvey B, Williams JI, Badley EM. The effect of education and income on need and willingness to undergo total joint arthroplasty. Arthritis Rheum. 2002;46:3331–3339. doi: 10.1002/art.10682. [DOI] [PubMed] [Google Scholar]
- 20.Cai X, Cram P, Vaughan-Sarrazin M. Are African American patients more likely to receive a total knee arthroplasty in a low-quality hospital? Clin Orthop Relat Res. 2012;470:1185–1193. doi: 10.1007/s11999-011-2032-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Katz JN. Preferences, quality, and the (under)utilization of total joint arthroplasty. Med Care. 2001;39:203–205. doi: 10.1097/00005650-200103000-00001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No additional data is available.