Abstract
Background
Dietary intakes of B vitamins (eg, folate) are related to cognitive function according to epidemiological studies in western countries. But prospective studies in Asian populations are scarce. This study evaluated the relationships of dietary intakes of six B vitamins in midlife with cognitive impairment in old age in a Chinese population living in Singapore.
Methods
This study included 16,948 participants from the Singapore Chinese Health Study, a population-based prospective cohort. Baseline dietary intakes of B vitamins were assessed using a validated 165-item food frequency questionnaire when the participants were aged 45–74 years (1993–1998). After an average follow-up of 20 years, cognitive function was examined using a Singapore-modified version of Mini-Mental State Examination scale in 2014–2016, and cognitive impairment was defined using education-specific cutoffs. Logistic regression models were applied to estimate the association between B vitamins and cognitive impairment. All the six B vitamins were mutually adjusted in the final model.
Results
In the 2014–2016 interview, 2,443 participants were defined as cognitive impairment. Riboflavin and folate were significantly and independently associated with cognitive impairment in a dose-dependent manner: the odds ratio (95% confidence interval) comparing the highest with the lowest quartile was 0.82 (0.69, 0.97) for riboflavin and 0.83 (0.70, 0.98) for folate (both p-trend <.05). Dietary intakes of thiamine, niacin, vitamin B-6, and B-12 were not significantly associated with risk of cognitive impairment.
Conclusions
Higher dietary intakes of riboflavin and folate in midlife were associated with a lower risk of cognitive impairment in late-life in the Chinese population.
Keywords: Cognitive function, MMSE, Riboflavin, Folate, Cohort study
In Asia, the percentage of people aged 60 years or older in 2017 was 12.2% and was estimated to keep rising in the following decades to about 24.2% in 2050 (1). The numbers are even higher in China with 16.2% in 2017 and 35.2% in 2050 (1). Cognitive impairment is common in the elderly population and a key clinical feature of dementia. With the dramatically rapid rate of aging in Asia, the burden of cognitive impairment would correspondingly increase, thus making the maintenance of cognitive function in the old age a major public health priority in Asian populations.
Since the landmark postulation of the “homocysteine hypothesis” of dementia (2), B vitamins have received extensive attention in the preservation of cognition due to their homocysteine-lowering effects (3–5). At present, nonhomocysteine-related pathways, such as hypo-methylation or the effects on mitochondrial energy metabolism, have also been found to support the independent effect of B vitamins on cognitive function (6,7). Several prospective cohort studies have assessed the associations between dietary intakes of B vitamins and cognitive function, dementia or Alzheimer’s disease, and some have reported significant associations for at least one subtype of B vitamins, for example niacin (ie, vitamin B-3) (8,9), vitamin B-6 (8,10,11), folate (ie, vitamin B-9) (8,12–15), and vitamin B-12 (8,11). Nevertheless, few studies have simultaneously assessed the relationships of all B vitamin subtypes with cognition (8,10), and large and long-term cohort studies in Asian populations are scarce in this research area.
Thus, we conducted this study by using data from a population-based cohort of Chinese living in Singapore to examine the relationships of dietary intakes of B vitamins in midlife with the risk of cognitive impairment in old age.
Methods
Study Design
The Singapore Chinese Health Study is a population-based prospective cohort study established between April 1993 and December 1998 (16). The cohort recruited 63,257 participants aged 45–74 years and residing in the government housing estates, where 86% of the Singapore population resided during the period of enrollment. The participants were either from the Hokkien dialect group that originated from the Fujian province in Southern China or from the Cantonese dialect group that originated from the contiguous Guangdong province.
The participants were contacted every 5–6 years to update information on selected lifestyle factors and medical history through follow-up interviews. The third follow-up was conducted during the period of 2014–2016, and a total of 17,107 participants aged 61–96 years were successfully interviewed at their homes. After exclusion of those with missing responses to cognitive assessment (n = 55) and those who were not able to speak (n = 1), see (n = 55), or hear (n = 48), 16,948 participants were included in this analysis.
Ethics
This study was approved by the institutional review board at the National University of Singapore, and informed consent was obtained from each participant.
Dietary Assessment
Participants’ habitual dietary intakes in the past year were assessed at baseline using a 165-item semiquantitative food frequency questionnaire to collect information on intake frequency and portion sizes of various food items and dishes. The intakes of the six B vitamins, that is thiamin, riboflavin, niacin, vitamin B-6, folate, and vitamin B-12 were computed by linking dietary intakes to the Singapore Food Composition Database, which was developed specifically for this cohort (16). In addition, a vegetable–fruit–soy diet pattern was derived using principal component analysis, which was characterized by high intakes of vegetables, fruit, and soy foods and shown to be associated with lower risks of diabetes (17), hip fracture (18), and mortality (19) in this cohort. The food frequency questionnaire had been validated before and details are shown in Supplementary Material.
Cognition Measurement
Our research staff conducted face-to-face interviews at participants’ homes at the third follow-up. Interviewers were trained by professional psychological specialist (L. Feng), and they were allowed to conduct the interviews after passing the training examination. All interviews were audio-recorded and 20% of these records were randomly selected for quality control. Cognitive function of participants was assessed face-to-face using a Singapore-modified version of Mini-Mental State Examination (SM-MMSE) that consisted of six dimensions that included orientation, immediate recall, attention, delayed recall, language, and construction (20). The total score of this test ranged from 0 to 30, with higher scores indicating better cognition. Considering the strong influence of education on cognitive function, we adopted education-specific cutoff points from the Shanghai Dementia Survey, which had participants of comparable educational levels as those in our study (21). The cutoff points for individuals with no formal education, 1–6 years of education, and 7 or more years of education were 17/18, 20/21, and 24/25, respectively.
Assessment of Covariates
At baseline, our trained staff interviewed the participants to collect information about demographics, medical history, and lifestyle habits (e.g., tobacco smoking, alcohol consumption, and physical activity) using structured questionnaires. (see Supplementary Material for details).
Statistical Analysis
Dietary intakes of B vitamins were adjusted for total energy intake using the residual method (22). The baseline characteristics were compared across the quartiles of dietary B vitamin intakes by chi-square test, analysis of variance, or Kruskal–Wallis rank test whenever appropriate. The correlations among the B vitamins and vegetable-fruit-soy dietary pattern score were evaluated using Spearman’s rank correlation coefficients.
The logistic regression method was used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) for the association between the dietary intakes of B vitamins and cognitive impairment. In the first model, we adjusted for age at cognitive assessment, sex, level of education, marital status, dialect group, body mass index, and total energy intake. In the second model, we additionally adjusted for cigarette smoking status, alcohol consumption, physical activity level, sleep durations, and baseline history of hypertension, diabetes, heart attack, stroke, and cancer. In the third model, we additionally adjusted for vegetable–fruit–soy dietary pattern score in quartiles. In the final model, we included all the six B vitamins simultaneously to test for independent associations of the vitamins. We performed multivariable generalized linear models to examine the associations using SM-MMSE score as a continuous outcome variable. We also examined the association between age (years) and SM-MMSE score (both as continuous variables) to indirectly evaluate the association between dietary vitamin intakes and the equivalent reduction for age in terms of cognitive function.
Stratified analyses were conducted to examine whether the associations were modified by education, body mass index, age at cognitive assessment, and sex, and interactions were tested by including a cross-product term between the ordinal value of the intake in quartiles (ie, 0, 1, 2, and 3) and the stratification factor in the model.
The following sensitivity analyses were conducted: (i) age at baseline was adjusted in the model instead of age at cognitive assessment; (ii) excluding those with extreme energy intakes (≤600 or ≥3,000 kcal per day); (iii) excluding those with baseline history of cancer or cardiovascular disease; (iv) using the MMSE cutoff point of 23/24, which is widely used in western populations.
A two-sided p value of less than .05 was defined as statistical significance. All statistical analyses were performed with SAS (version 9.4; SAS Institute, Inc., Cary, NC).
Results
The mean age of participants was 53.5 (SD: 6.2) years at baseline and 73.2 (SD: 6.4) years at cognitive assessment, and 40.8% of them were men. The average daily intakes of B vitamins in this population are shown in Supplementary Table 1. Compared with those in the lowest quartile, participants in the highest quartiles of intake for B vitamins were younger and more likely to be women. They had higher education level and physical activity level (except for vitamin B-12) and were less likely to be smokers or drinkers (except for niacin and vitamin B-6; see Table 1 and Supplementary Table 2). The Spearman’s rank correlation coefficients between B vitamins were from .13 to .56 and ranged from .04 to .45 between B vitamins and the vegetable-fruit-soy dietary pattern (Supplementary Table 3).
Table 1.
Characteristics of the Participants and by Extreme Quartiles of Dietary Riboflavin and Folate Intake at Baseline (1993–1998) in the Singapore Chinese Health Study (n = 16,948)
| All subjects | Riboflavin (mg) | Folate (μg) | |||
|---|---|---|---|---|---|
| Q1 | Q4 | Q1 | Q4 | ||
| Median daily intake | — | 0.72 | 1.22 | 110.99 | 213.88 |
| Baseline age (y) | 52.50 | 52.98 | 52.34 | 53.19 | 51.86 |
| Follow-up age (y) | 72.18 | 72.87 | 71.74 | 73.05 | 71.41 |
| Body Mass Index (kg/m2) | 23.05 | 23.03 | 22.97 | 22.97 | 23.12 |
| Female (%) | 59.20 | 43.85 | 66.77 | 45.86 | 63.32 |
| No formal education (%) | 18.84 | 20.01 | 15.01 | 22.45 | 12.72 |
| Primary school (%) | 44.77 | 50.53 | 41.33 | 49.26 | 39.91 |
| Secondary school (%) | 28.99 | 24.00 | 33.21 | 23.37 | 37.05 |
| Diploma or higher (%) | 7.40 | 5.45 | 10.46 | 4.93 | 10.31 |
| Married (%) | 88.60 | 89.05 | 87.61 | 89.00 | 88.65 |
| Cantonesea (%) | 49.83 | 49.68 | 54.21 | 46.12 | 58.08 |
| Current smoker (%) | 13.06 | 19.94 | 8.73 | 21.76 | 8.76 |
| Daily drinker (%) | 2.76 | 3.47 | 2.48 | 3.28 | 2.71 |
| Hypertension (%) | 19.38 | 18.57 | 19.59* | 17.35 | 21.27 |
| Heart attack (%) | 2.08 | 1.75 | 2.41* | 1.72 | 2.34* |
| Stroke (%) | 0.48 | 0.38 | 0.80 | 0.45 | 0.50* |
| Diabetes (%) | 4.89 | 3.45 | 6.61 | 4.30 | 5.40* |
| Cancer (%) | 1.89 | 1.30 | 2.60 | 1.46 | 2.15* |
| Daily energy intake (kcal) | 1,506.32 | 1,660.83 | 1,594.83 | 1,685.69 | 1,580.87 |
Note: N for each quartile was 4,237. Values were medians or percentages as appropriate. Follow-up age was recorded at cognitive assessment. Other values were all assessed at baseline in 1993–1998. Q = quartile.
aCantonese is one of the two father dialects of our study population, the other is Hokkien.
*p ≥ .05; All others were significant at p < .05.
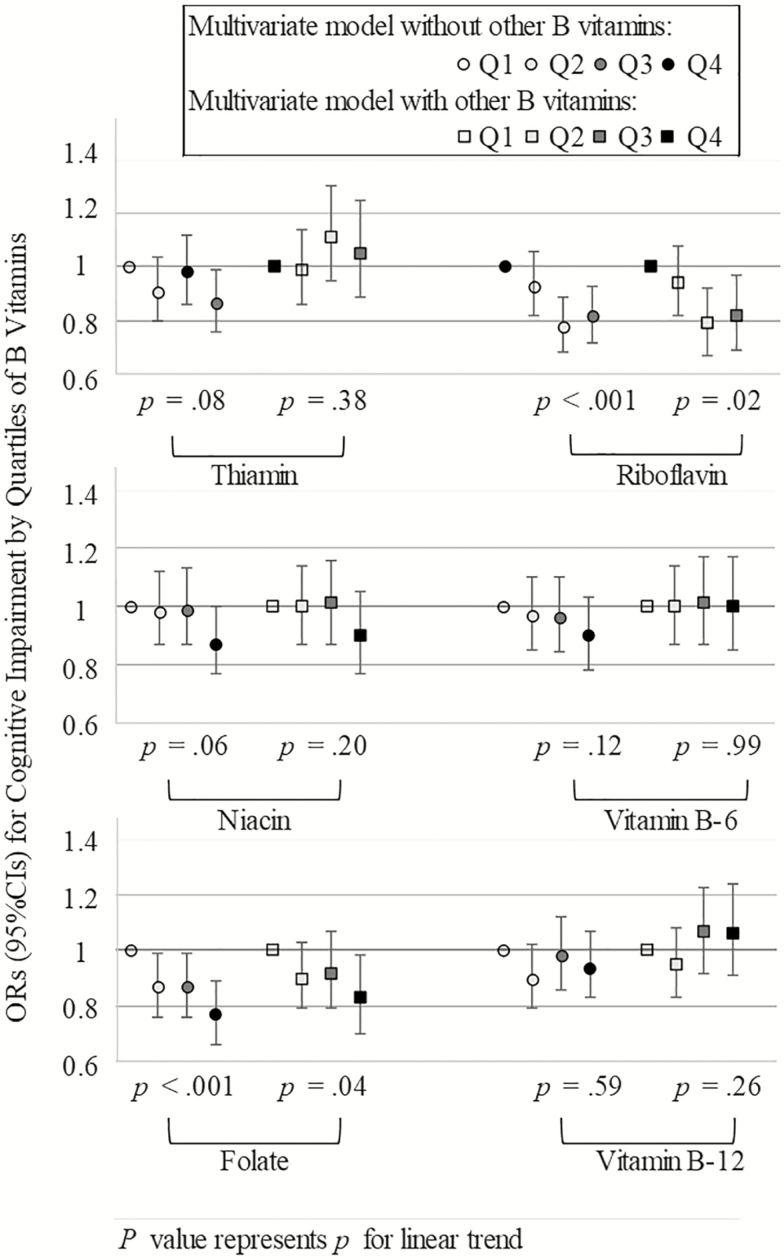
The mean value of SM-MMSE score was 24.8 (SD: 3.9), and 14.4% of them were defined as cognitive impairment in 2014–2016. The associations between dietary intakes of B vitamins and risk of cognitive impairment are shown in Figure 1 and Supplementary Table 4. In Model 3 that included demographic and lifestyle factors, dietary intakes of thiamine, niacin, folate, and riboflavin were associated with a lower risk of cognitive impairment. However, in the final model that mutually adjusted for all B vitamins, only the associations of riboflavin and folate remained significant: the OR (95% CI) comparing the highest with the lowest quartile was 0.82 (0.69, 0.97) for riboflavin, and 0.83 (0.70, 0.98) for folate (both p-trend < .05; Figure 1 and Supplementary Table 4). In the generalized linear models, the adjusted mean difference of SM-MMSE scores also increased significantly in a dose-dependent manner with higher quartile intake of riboflavin and folate (mean difference of the highest comparing to the lowest quartile was 0.30 for riboflavin and 0.31 for folate; both p-trend ≤ .003; Table 2). The mean differences in SM-MMSE scores comparing extreme quartiles for intake of riboflavin and folate were equivalent to the differences in scores comparing age difference of 1.67 and 1.69 years, respectively.
Figure 1.
Odds ratios (95% confidence interval) of cognitive impairment by quartiles of B vitamins intake in the Singapore Chinese Health Study (n = 16,948). p Values for linear trend were tested by treating the median values of quartiles as a continuous variable; Reference group is Q1; Multivariate model without other B vitamins was adjusted for age at cognitive assessment, sex, education level, marital status, dialect group, body mass index, total energy intake, cigarette smoking status, alcohol consumption, physical activity level, sleep duration, baseline history of hypertension, diabetes, heart attack, stroke, cancer and vegetable–fruit–soy dietary pattern; Multivariate model with other B vitamins additionally included all the six subtypes of B vitamins simultaneously. CI = confidence interval, OR = Odds Ratio, Q = quartile.
Table 2.
Least-Squares Means (95% Confidence Interval) of SM-MMSE Score by Quartiles of Riboflavin and Folate Intake in the Singapore Chinese Health Study (n = 16,948)
| SM-MMSE score | ||||
|---|---|---|---|---|
| Least-squares means (95% CI) | β | p Value | p Trend | |
| Riboflavin | <.001 | |||
| Q1 | 24.18 (23.73, 24.64) | |||
| Q2 | 24.27 (23.82, 24.72) | 0.09 | .23 | |
| Q3 | 24.52 (24.07, 24.97) | 0.34 | <.001 | |
| Q4 | 24.49 (24.04, 24.93) | 0.30 | <.001 | |
| Folate | .003 | |||
| Q1 | 24.18 (23.72, 24.63) | |||
| Q2 | 24.41 (23.96, 24.86) | 0.23 | .002 | |
| Q3 | 24.40 (23.95, 24.85) | 0.22 | .005 | |
| Q4 | 24.48 (24.03, 24.93) | 0.31 | <.001 |
Note: Linear trend was tested by treating the median values of quartiles as a continuous variable; The statistical model was the same as the multivariate model with other B vitamins in Figure 1; , SM-MMSE = Singapore-modified version of Mini-Mental State Examination; Q = quartile.
No significant interactions were found between various factors and riboflavin and folate, with risk of cognitive impairment, except that sex modified the association between folate intake and cognitive impairment and the inverse association was significant among women but not in men (p-interaction = .01; Supplementary Table 5).
Overall, the findings of the inverse relations of riboflavin and folate with cognitive impairment were consistent in the various sensitivity analyses of adjustment of age at baseline (Supplementary Table 6), excluding those with extreme energy intakes (Supplementary Table 7) or baseline history of cancer or cardiovascular disease (Supplementary Table 8), or using the MMSE cutoff point of 23/24 (Supplementary Table 9).
Discussion
In this study that comprehensively examined dietary intakes of six B vitamins in a Chinese population living in Singapore, we found that higher dietary intakes of riboflavin and folate in midlife were associated with a lower risk of developing cognitive impairment in old age.
A number of cohort studies reported that higher dietary intake of folate was associated with better cognitive function (8), and a lower risk of cognitive impairment (12), cognitive decline (13) or Alzheimer’s disease (14,15), which concurs with our findings. A randomized controlled trial conducted in China found that a short-term folate supplementation of 400 μg/day was beneficial for cognitive functioning among Chinese older adults with mild cognitive impairment (23). However, some cohort studies have found a null relation (10,24) or even a positive association (25) between folate intake and cognitive impairment. One study was conducted in the United Kingdom with a small sample size (n = 155) (10). The other two studies were conducted among the elder people in the United States (24,25). With widespread multivitamin use and folic acid fortification in the United States, folate deficiency became less a concern. Because our study population did not have mandatory folic acid fortification of selected foods and also had low prevalence of supplement use at the time of recruitment (26), we have a unique opportunity to examine the association of dietary folate from food intake with risk of cognitive impairment. Furthermore, the intake levels in the UK and US populations (average above 310 μg/day) (24,25) were substantially higher compared to ours (154 μg/day). Therefore, it is possible that higher folate intakes may not provide benefits for cognitive function in the western populations who already have high intake levels, whereas our study suggests that folate could help reduce the risk of cognitive impairment in populations with relatively lower intake levels.
In our study, we did not find significant relationships of cognitive impairment with the other two folate-related B vitamins, namely vitamin B-6 and B-12. A systematic review of two randomized controlled trials and six cohort studies also showed either null or inconsistent associations between vitamin B-12 intake and cognitive function (27). Some previous studies suggested that the association between vitamin B-12 and cognitive function could be influenced by the genetic predisposition (e.g., ApoE genotype) and depression status (28–30). The association between vitamin B-6 and cognitive function was also inconsistently reported in the literature (8,10,15,24). Several meta-analyses of randomized controlled trials also did not support the protective effect of vitamin B-6 and B-12 on cognitive impairment or decline or Alzheimer’s disease (31–33).
At present, researchers found that riboflavin may also influence plasma homocysteine concentration (34,35), and thus play an important role in the maintenance of brain health (36). Besides, riboflavin deficiency may cause an insufficiency of prosthetic groups of flavin mononucleotide and flavin adenine dinucleotide, in turn leading to an adverse impact on cytochrome P450 reductase (37), and a consequent accumulation of hemin to eventually damage brain cells (36). In our study, dietary riboflavin intake was inversely associated with risk of cognitive impairment. However, several studies in the western populations did not find significant associations (10,11,38). Again, we postulate that a possible reason for this discrepancy could be the higher intake levels in these previous studies (average 1.6–2.8 mg/day) (10,11,38) compared with the lower intake level in our study population (mean 0.9 mg/day). Second, the follow-up period in these studies (4–6 years) (10,11) may not be long enough to observe a modest association compared to the much longer follow-up period in our study.
In this study, the inverse association between niacin and cognitive impairment was marginally significant before adjusting for other B vitamins, but not statistically significant in the final model including all B vitamins in the same model. In two cohort studies in the US population, the authors reported that dietary niacin intake was inversely associated with both cognitive decline and Alzheimer’s disease (8,9). The inconsistency between different studies might be related to differences in statistical methods, adjustment of covariates and characteristics of the participants. The association between niacin and cognitive impairment needs to be further evaluated in future studies. Very few studies have investigated the association between thiamin and cognitive impairment, and a 13-year cohort study in 4,809 French elderly women reported a null association (38), which is consistent with our study.
This study has several strengths, including the large sample size (n = 16,948), a long follow-up period (about 20 years) through midlife to late-life, and a comprehensive study of six subtypes of B vitamins. We were also able to examine the relationships of dietary intakes of B vitamins at low doses with cognitive function, because our study population had relatively lower dietary intakes of these vitamins, a low prevalence of supplement use, and Singapore did not have mandatory fortification of selected foods during the study period, which is commonly practiced in western countries. A limitation of this study was the examination of cognitive function only at one time-point, thus precluding us from studying the association with cognitive decline. In addition, we did not exclude participants with cognitive impairment or dementia at baseline. However, because all participants had completed a set of complex questionnaires, including dietary information, at recruitment, it was unlikely for those with substantial cognitive impairment or dementia to have been included in the study. Furthermore, dietary habits were only explored at baseline and we are unable to take into account the impact of potential changes during follow-up time. The measurement error of dietary assessment is inevitable. However, the food frequency questionnaire was validated using two different methods and reasonable correlation coefficients were observed. In addition, we did not collect blood samples at baseline and the dietary intake levels may not be equivalent to the circulating blood concentrations (39). We did not have ApoE genotype data or depression status at baseline and could not assess the influences of those factors on the observed associations. Finally, our final model included vegetable–fruit–soy dietary pattern and all B vitamins in the same model. Because the major dietary contributors of both riboflavin and folate were vegetables (26), the final model may be overadjusted, but the possibility of residual confounding still cannot be eliminated. Further studies on different food sources of B vitamins in relation to cognitive function are also needed.
In conclusion, our study found that higher intakes of riboflavin and folate in midlife were associated with a lower risk of cognitive impairment in late-life in the Chinese population living in Singapore. Our results need further validation by other high-quality cohort studies and well-designed randomized controlled trials. If the relations are causal, our findings have significant public health importance for improving cognitive health in the elderly populations by increasing dietary intakes of riboflavin and folate in their midlife.
Funding
The study was supported by grants from the National Medical Research Council, Singapore (NMRC/CSA/0055/2013 to W.P.K.); the US National Institutes of Health (R01 CA144034 and UM1 CA182876 to J.M.Y.); the National Key Research and Development Program of China (2017YFC0907504 to A.P.) and Hubei Province Science Fund for Distinguished Young Scholars (2018CFA033 to A.P.). The Saw Swee Hock School of Public Health, National University of Singapore also provided funding for the implementation of follow-up visits of the cohort.
Conflict of Interests
None of the authors reported a conflict of interest related to the study.
Supplementary Material
Acknowledgments
We thank Siew-Hong Low of the National University of Singapore for overseeing the fieldwork of the Singapore Chinese Health Study and Renwei Wang for the development and maintenance of the cohort study database. We also thank Mimi C. Yu for being the founding and longstanding principal investigator of the Singapore Chinese Health Study.
References
- 1. United Nations, Department of Economic and Social Affairs, Population Division. World Population Ageing. 2017;2017 https://www.un.org/en/development/desa/population/publications/pdf/ageing/WPA2017_Report.pdf. Accessed December 30, 2017. [Google Scholar]
- 2. Clarke R, Smith AD, Jobst KA, Refsum H, Sutton L, Ueland PM. Folate, vitamin B12, and serum total homocysteine levels in confirmed Alzheimer disease. Arch Neurol. 1998;55:1449–1455. doi: 10.1001/archneur.55.11.1449 [DOI] [PubMed] [Google Scholar]
- 3. Morris MC, Schneider JA, Tangney CC. Thoughts on B-vitamins and dementia. J Alzheimers Dis. 2006;9:429–433. doi: 10.3233/JAD-2006-9409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smith AD, Refsum H. Homocysteine, B vitamins, and cognitive impairment. Annu Rev Nutr. 2016;36:211–239. doi: 10.1146/annurev-nutr-071715-050947 [DOI] [PubMed] [Google Scholar]
- 5. Kuo HK, Sorond FA, Chen JH, Hashmi A, Milberg WP, Lipsitz LA. The role of homocysteine in multisystem age-related problems: a systematic review. J Gerontol A Biol Sci Med Sci. 2005;60:1190–1201. doi: 10.1093/gerona/60.9.1190 [DOI] [PubMed] [Google Scholar]
- 6. Mattson MP, Shea TB. Folate and homocysteine metabolism in neural plasticity and neurodegenerative disorders. Trends Neurosci. 2003;26:137–146. doi: 10.1016/S0166-2236(03)00032-8 [DOI] [PubMed] [Google Scholar]
- 7. Depeint F, Bruce WR, Shangari N, Mehta R, O’Brien PJ. Mitochondrial function and toxicity: role of the B vitamin family on mitochondrial energy metabolism. Chem Biol Interact. 2006;163:94–112. doi: 10.1016/j.cbi.2006.04.014 [DOI] [PubMed] [Google Scholar]
- 8. Qin B, Xun P, Jacobs DR Jr, et al. Intake of niacin, folate, vitamin B-6, and vitamin B-12 through young adulthood and cognitive function in midlife: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Clin Nutr. 2017;106:1032–1040. doi: 10.3945/ajcn.117.157834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morris MC, Evans DA, Bienias JL, et al. Dietary niacin and the risk of incident Alzheimer’s disease and of cognitive decline. J Neurol Neurosurg Psychiatry. 2004;75:1093–1099. doi: 10.1136/jnnp.2003.025858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hughes CF, Ward M, Tracey F, Hoey L, Molloy AM, Pentieva K, et al. B-Vitamin intake and biomarker status in relation to cognitive decline in healthy older adults in a 4-year follow-up study. Nutrients. 2017;9. doi: 10.3390/nu9010053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. La Rue A, Koehler KM, Wayne SJ, Chiulli SJ, Haaland KY, Garry PJ. Nutritional status and cognitive functioning in a normally aging sample: a 6-y reassessment. Am J Clin Nutr. 1997;65:20–29. doi: 10.1093/ajcn/65.1.20 [DOI] [PubMed] [Google Scholar]
- 12. Agnew-Blais JC, Wassertheil-Smoller S, Kang JH, et al. Folate, vitamin B-6, and vitamin B-12 intake and mild cognitive impairment and probable dementia in the Women’s Health Initiative Memory Study. J Acad Nutr Diet. 2015;115:231–241. doi: 10.1016/j.jand.2014.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Morris MC, Wang Y, Barnes LL, Bennett DA, Dawson-Hughes B, Booth SL. Nutrients and bioactives in green leafy vegetables and cognitive decline: Prospective study. Neurology. 2018;90:e214–e222. doi: 10.1212/WNL.0000000000004815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Luchsinger JA, Tang MX, Miller J, Green R, Mayeux R. Relation of higher folate intake to lower risk of Alzheimer disease in the elderly. Arch Neurol. 2007;64:86–92. doi: 10.1001/archneur.64.1.86 [DOI] [PubMed] [Google Scholar]
- 15. Corrada MM, Kawas CH, Hallfrisch J, Muller D, Brookmeyer R. Reduced risk of Alzheimer’s disease with high folate intake: the Baltimore Longitudinal Study of Aging. Alzheimers Dement. 2005;1:11–18. doi: 10.1016/j.jalz.2005.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hankin JH, Stram DO, Arakawa K, et al. Singapore Chinese Health Study: development, validation, and calibration of the quantitative food frequency questionnaire. Nutr Cancer. 2001;39:187–195. doi: 10.1207/S15327914nc392_5 [DOI] [PubMed] [Google Scholar]
- 17. Odegaard AO, Koh WP, Butler LM, et al. Dietary patterns and incident type 2 diabetes in Chinese men and women: the Singapore chinese health study. Diabetes Care. 2011;34:880–885. doi: 10.2337/dc10-2350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dai Z, Butler LM, van Dam RM, Ang LW, Yuan JM, Koh WP. Adherence to a vegetable-fruit-soy dietary pattern or the Alternative Healthy Eating Index is associated with lower hip fracture risk among Singapore Chinese. J Nutr. 2014;144:511–518. doi: 10.3945/jn.113.187955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Odegaard AO, Koh WP, Yuan JM, Gross MD, Pereira MA. Dietary patterns and mortality in a Chinese population. Am J Clin Nutr. 2014;100:877–883. doi: 10.3945/ajcn.114.086124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Feng L, Chong MS, Lim WS, Ng TP. The modified mini-mental State examination test: normative data for Singapore Chinese older adults and its performance in detecting early cognitive impairment. Singapore Med J. 2012;53:458–462. PubMed ID: 22815014. [PubMed] [Google Scholar]
- 21. Katzman R, Zhang MY, Ouang-Ya-Qu, et al. A Chinese version of the Mini-Mental State Examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol. 1988;41:971–978. doi: 10.1016/0895-4356(88)90034-0 [DOI] [PubMed] [Google Scholar]
- 22. Willett W. Nutritional Epidemiology. 3rd ed.New York: Oxford University Press; 1998. [Google Scholar]
- 23. Ma F, Wu T, Zhao J, et al. Effects of 6-month folic acid supplementation on cognitive function and blood biomarkers in mild cognitive impairment: a Randomized Controlled Trial in China. J Gerontol A Biol Sci Med Sci. 2016;71:1376–1383. doi: 10.1093/gerona/glv183 [DOI] [PubMed] [Google Scholar]
- 24. Nelson C, Wengreen HJ, Munger RG, Corcoran CD. Dietary folate, vitamin B-12, vitamin B-6 and incident Alzheimer’s disease: the cache county memory, health and aging study. J Nutr Health Aging. 2009;13:899–905. doi:10.1007/s12603-009-0249-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morris MC, Evans DA, Bienias JL, Tangney CC, Hebert LE, Scherr PA, et al. Dietary folate and vitamin B12 intake and cognitive decline among community-dwelling older persons. Arch Neurol. 2005;62:641–645. doi: 10.1001/archneur.62.4.641 [DOI] [PubMed] [Google Scholar]
- 26. Dai Z, Wang R, Ang LW, Yuan JM, Koh WP. Dietary B vitamin intake and risk of hip fracture: the Singapore Chinese Health Study. Osteoporos Int. 2013;24:2049–2059. doi: 10.1007/s00198-012-2233-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Doets EL, van Wijngaarden JP, Szczecińska A, et al. Vitamin B12 intake and status and cognitive function in elderly people. Epidemiol Rev. 2013;35:2–21. doi: 10.1093/epirev/mxs003 [DOI] [PubMed] [Google Scholar]
- 28. Bunce D, Kivipelto M, Wahlin A. Apolipoprotein E, B vitamins, and cognitive function in older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:P41–P48. doi: 10.1093/geronb/60.1.p41 [DOI] [PubMed] [Google Scholar]
- 29. Feng L, Li J, Yap KB, Kua EH, Ng TP. Vitamin B-12, apolipoprotein E genotype, and cognitive performance in community-living older adults: evidence of a gene-micronutrient interaction. Am J Clin Nutr. 2009;89:1263–1268. doi: 10.3945/ajcn.2008.26969 [DOI] [PubMed] [Google Scholar]
- 30. Vogiatzoglou A, Smith AD, Nurk E, et al. Cognitive function in an elderly population: interaction between vitamin B12 status, depression, and apolipoprotein E ε4: the Hordaland Homocysteine Study. Psychosom Med. 2013;75:20–29. doi: 10.1097/PSY.0b013e3182761b6c [DOI] [PubMed] [Google Scholar]
- 31. Ford AH, Almeida OP. Effect of homocysteine lowering treatment on cognitive function: a systematic review and meta-analysis of randomized controlled trials. J Alzheimers Dis. 2012;29:133–149. doi: 10.3233/JAD-2012-111739 [DOI] [PubMed] [Google Scholar]
- 32. Clarke R, Bennett D, Parish S, et al. ; B-Vitamin Treatment Trialists’ Collaboration Effects of homocysteine lowering with B vitamins on cognitive aging: meta-analysis of 11 trials with cognitive data on 22,000 individuals. Am J Clin Nutr. 2014;100:657–666. doi: 10.3945/ajcn.113.076349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wald DS, Kasturiratne A, Simmonds M. Effect of folic acid, with or without other B vitamins, on cognitive decline: meta-analysis of randomized trials. Am J Med. 2010;123:522–527.e2. doi: 10.1016/j.amjmed.2010.01.017 [DOI] [PubMed] [Google Scholar]
- 34. Jacques PF, Bostom AG, Wilson PW, Rich S, Rosenberg IH, Selhub J. Determinants of plasma total homocysteine concentration in the Framingham Offspring cohort. Am J Clin Nutr. 2001;73:613–621. doi: 10.1093/ajcn/73.3.613 [DOI] [PubMed] [Google Scholar]
- 35. Hustad S, Ueland PM, Vollset SE, Zhang Y, Bjørke-Monsen AL, Schneede J. Riboflavin as a determinant of plasma total homocysteine: effect modification by the methylenetetrahydrofolate reductase C677T polymorphism. Clin Chem. 2000;46(8 Pt 1):1065–1071. [PubMed] [Google Scholar]
- 36. Coimbra CG, Junqueira VB. High doses of riboflavin and the elimination of dietary red meat promote the recovery of some motor functions in Parkinson’s disease patients. Braz J Med Biol Res. 2003;36:1409–1417. doi: 10.1590/S0100-879X2003001000019 [DOI] [PubMed] [Google Scholar]
- 37. Wang M, Roberts DL, Paschke R, Shea TM, Masters BS, Kim JJ. Three-dimensional structure of NADPH-cytochrome P450 reductase: prototype for FMN- and FAD-containing enzymes. Proc Natl Acad Sci U S A. 1997;94:8411–8416. doi: 10.1073/pnas.94.16.8411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Vercambre MN, Boutron-Ruault MC, Ritchie K, Clavel-Chapelon F, Berr C. Long-term association of food and nutrient intakes with cognitive and functional decline: a 13-year follow-up study of elderly French women. Br J Nutr. 2009;102:419–427. doi: 10.1017/S0007114508201959 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Vogiatzoglou A, Smith AD, Nurk E, et al. Dietary sources of vitamin B-12 and their association with plasma vitamin B-12 concentrations in the general population: the Hordaland Homocysteine Study. Am J Clin Nutr. 2009;89:1078–1087. doi: 10.3945/ajcn.2008.26598 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.